Abstract
Background and purpose
We performed a systematic review and a survey in order to (1) evaluate the evidence for the impact of spine registries on the quality of spine care, and with that, on patient-related outcomes, and (2) evaluate the methodology used to organize, analyze, and report the “quality of spine care” from spine registries.
Methods
To study the impact, the literature on all spinal disorders was searched. To study methodology, the search was restricted to degenerative spinal disorders. The risk of bias in the studies included was assessed with the Newcastle-Ottawa scale. Additionally, a survey among registry representatives was performed to acquire information about the methodology and practice of existing registries.
Results
4,273 unique references up to May 2014 were identified, and 1,210 were eligible for screening and assessment. No studies on impact were identified, but 34 studies were identified to study the methodology. Half of these studies (17 of the 34) were judged to have a high risk of bias. The survey identified 25 spine registries, representing 14 countries. The organization of these registries, methods used, analytical approaches, and dissemination of results are presented.
Interpretation
We found a lack of evidence that registries have had an impact on the quality of spine care, regardless of whether intervention was non-surgical and/or surgical. To improve the quality of evidence published with registry data, we present several recommendations. Application of these recommendations could lead to registries showing trends, monitoring the quality of spine care given, and ultimately improving the value of the care given to patients with degenerative spinal disorders.
Lumbar spine disorders are a heterogeneous group of conditions with a lack of diagnostic clarity. Thus, in both surgical and non-surgical spinal interventions there are large variations in practice. The increasing frequency of spine-related interventions with increasing costs has led to a shift towards the delivery of value-based spine care (Hoy et al. 2014). Here, value is expressed as patient-centered outcomes (safety and effectiveness; quality) divided by the related costs of care or per unit cost (Porter 2010). While randomized clinical trials (RCTs) are considered to be the gold standard for assessing the efficacy of interventions, the difficulties with RCTs—specifically for assessment of surgical procedures in spinal disorders—are acknowledged (Jacobs et al. 2012a). Some barriers are surgeon preferences, patient selection, patients’ reluctance regarding randomization, difficulties in blinding, high cost, the need for long-term follow-up, the often high proportion of loss to follow-up, and the problem with crossover. Well-designed observational cohort studies, reflecting daily clinical practice, have been reported to produce as trustworthy and externally valid results as RCTs (Benson and Hartz 2000, Concato et al. 2000, Weinstein et al. 2009, Concato et al. 2010, Colditz 2010, Jacobs et al. 2012b, Phillips et al. 2013).
An outcome registry is an organized system that uses observational study methods (Gliklich and Dreyer 2010) based on STROBE recommendations (von Elm et al. 2007). Registries could therefore be used to describe care patterns, including appropriateness of care and disparities in the delivery of care. Registry data could also be used to understand variations in treatment and outcomes, and to identify and select subgroups in the heterogeneous chronic low back pain population with a probability of successful or poor outcome. The ultimate goal of health service registries is to increase the value of care delivered (i.e. outcome per unit cost) (Kuenen et al. 2011). Moreover, it has been suggested that measuring with continuous feedback (audit cycles) of outcomes captured in registries raises awareness and improves the quality of care (Larsson et al. 2010, van Leersum et al. 2011). However, as yet, little is known about the effect of spine registries on the quality of spine care and the methods for registering and feedback.
This study had 2 aims: (1) to evaluate the available evidence for the effect and possible impact of introducing and using spine registries on the quality of spine care after any intervention and on patient-related outcomes; (2) to evaluate the methodology used to organize, analyze, and report the “quality of spine care” from spine registries.
Methods
We performed a systematic review according to the PRISMA statement for reporting in systematic reviews and meta-analyses (PRISMA 2014). In addition, for the second aim (regarding methodology) a survey among spine registry representatives was performed to acquire information about the current status of existing spine registries. The complete protocol for this study was presented at the preconference meeting of the International Society for the Study of the Lumbar Spine 2014 (ISSLS) (Jacobs et al. 2014).
Selection of studies and appraisal of their quality was performed independently by MH and WJ. Discrepancies were discussed during consensus meetings, with mediation by a third author (PW) where disagreements persisted.
Search
A comprehensive search was conducted because terminology in the field of chronic low back pain is not yet standardized, and because we aimed to include both randomized and non-randomized studies. The search was performed by one of the authors (WJ) on May 12, 2014, using the most common databases: the CBRG trials register (up to the search date), MEDLINE (from 1966 to the search date), EMBASE (from 1980 to the search date), and ISI Web of Science (up to the search date). The search string for MEDLINE is given in Appendix 1 (see Supplementary data) and was adapted for the other databases. No language or date restrictions were made. References and citations of selected articles were tracked and included in the search.
Impact of registries on the quality of spine care
Articles were included if they met the following criteria.
Types of studies
Studies on spine registries based on results from prospectively acquired data were included. To comply with the definition of patient or outcomes registry, we used the following registry characteristics: inclusion principle, mergeable data, standardized dataset for all consecutively included patients, rules for data collection (i.e. systematically and prospectively collected, including pre-intervention data), knowledge about patient-related outcomes, and observations collected over time (i.e. follow-up assessments) (Drolet and Johnson 2008). Studies were included if published between 2000 and May 2014 and written in English.
Types of spine disorders
We included patients of all ages with spine disorders who underwent any elective or acute, non-surgical or surgical spinal intervention. The following specific disorders were defined: degenerative disc disease (DDD; “non-specific” and/or chronic low back pain, segmental pain), spinal stenosis, disc herniation, spondylolisthesis/-lysis (isthmic/degenerative), failed back surgery syndrome, spinal deformities (degenerative deformity: de novo, osteoporotic; idiopathic, neuromuscular, congenital), spinal oncology, spine trauma, and infections of the spine.
Types of interventions
Interventions were included that provide a system to register the quality of spine care, i.e. outcomes, including a system for feedback: quality improvement strategies (Shoania et al. 2006, Tricco et al. 2012, Munce et al. 2013). These strategies include those targeted: health systems (e.g. team changes), healthcare professionals (e.g. reminders), and patients (e.g. reminders). Specific improvement strategies included: (clinical) audit and feedback, (electronic) patient registries, case management, clinician education, (promotion of) self-management, patient reminder systems, and continuous quality improvement.
Types of outcome measures
Quality of care is a multidimensional concept and is defined in many ways, e.g. “doing the right thing, at the right time, in the right way, for the right person, and having the best possible results” (AHRQ 2014). Following this definition, the outcomes of spine interventions are a proxy for quality of care. As measures for quality of spine care, we included patient-related outcome indicators: patient-reported outcome measures (PROMs) and clinical outcome measures. PROMs (McCormick et al. 2013) are functional status (e.g. the Roland and Morris disability questionnaire (RMDQ), the Oswestry disability index (ODI), Scoliosis Research Society-22 (SRS22)), pain intensity—back and leg (e.g. visual analog scale (VAS), numeric pain rating scale (NPRS)), and health-related quality of life (e.g. Short Form-36 (SF36), EuroQol 5 dimensions (EQ5D)). Clinical outcomes were regarded as reintervention (i.e. reoperation), complications, and failed back surgery syndrome (FBSS).
The search did not reveal any studies related to the first aim of this study (impact) concerning the effect and possible impact of introducing and using spine registries on the quality of spine care and on patient-related outcomes (Figure).
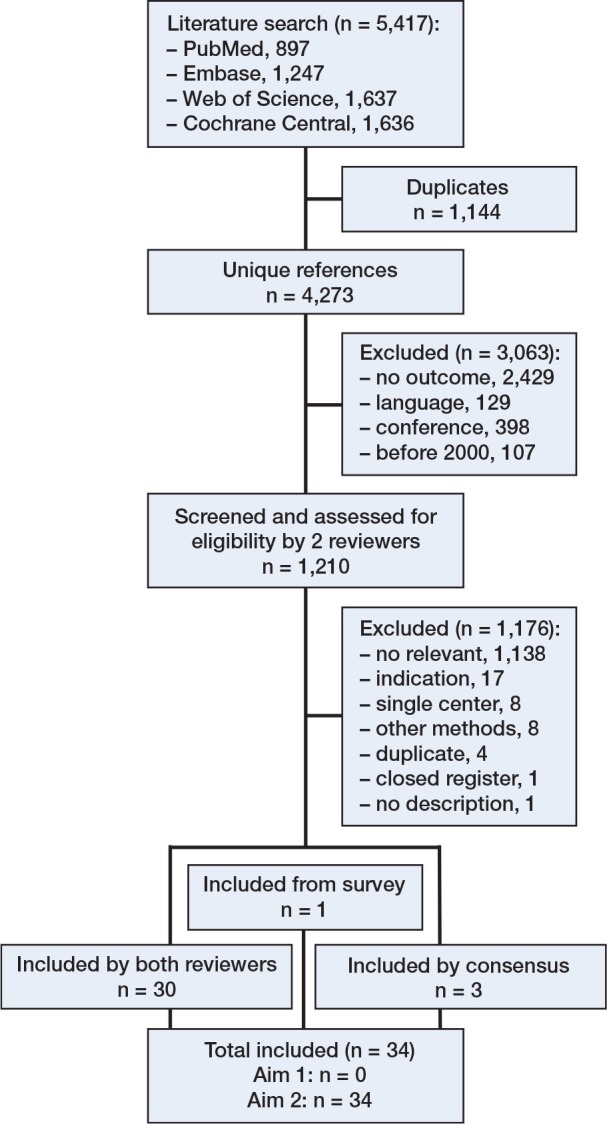
Flow chart of studies through the different phases of the systematic review.
Methodology used in existing spine registries
Selection criteria
The same criteria were used as for the first aim, but they were restricted to include studies with patients with degenerative lumbar spine disorders: degenerative disc disease (DDD, “non-specific” and/or chronic low back pain, segmental pain), spinal stenosis, disc herniation, spondylolisthesis/-lysis (isthmic/degenerative), and spinal deformities (degenerative deformity: de novo, osteoporotic).
Risk of bias assessment
The studies included were assessed for methodological quality, to get an impression of the quality of published scientific studies based on registries. Quality was assessed with the Newcastle-Ottawa scale (NOS; Appendix 2, see Supplementary data) for cohort studies (Wells et al. 2008). Studies were considered to be of high quality if the total score was 6 or more (75% of the maximum score). The clinical relevance of study results was assessed with 3 questions: (1) “Are the patients described in detail so that you can decide whether they are comparable to those that you see in your practice?”; (2) “Are the interventions and treatment settings described well enough so that you can provide the same for your patients?”; 3) Were all clinically relevant outcomes measured and reported?”.
Data extraction and management
Using forms already developed, the following data were extracted: authors (affiliation, sponsoring), name and type of registry (i.e. based on exposure: health service, disease/condition, and medical devices (Gliklich and Dreyer 2010)), setting (nationwide, multicenter), diagnosis, methods (purpose, study design, outcomes, covariates, statistical analysis, patient numbers recruited and included), follow-up response, non-responder analysis, conclusion. MH extracted the data and WJ checked the data; inconsistencies were discussed and PW was consulted if necessary.
Survey
A web-based survey, built using the Harvard Business Online Qualitrics Survey Software and provided by International Consortium for Health Outcomes Measurement (ICHOM), was performed among spine registry representatives. The survey consisted of 21 questions regarding: (1) organizational structure and financing, (2) methodology used and outcome assessment, (3) procedures concerning response rates and missing data, and (4) approaches for analysis and reporting.
The sample included participants of the ICHOM Low Back Pain Working Group, representatives of spine registries identified through spine registry websites, and corresponding authors of publications on spine registries as identified in this systematic review. All recipients were contacted by e-mail and asked to participate in an online survey. Subjects who did not respond were sent a reminder after 2 weeks.
Analyses
Results from the studies included in the review were not pooled; instead, we compared and reported on the methods used in these studies. The data from the survey are described and support the results found in the review. The PROMs used were checked with the ICHOM-LBP PROMs criteria (ICHOM 2014): (1) functional status (ODI [0–100] version 2.1a); (2) pain intensity (NPRS [0-10] back and leg; average pain during the last 7 days); (3) health-related quality of life (EQ5D-3L and EQ-VAS); (4) timeline assessments included were baseline, 3 and 6 months, and 1, 2, and 5 years after the “index event” (3-month and 5-year assessments were optional). The index event was defined as the first intervention episode reported.
Results
Impact of registries on quality of spine care
Studies included
4,273 unique references were identified, 1,210 of which were eligible for screening and assessment (Figure). No studies on the effect of spine registries on quality of care were identified.
Methodology used in existing spine registries
Studies included
34 studies were identified for study of the methodology used to organize, analyze, and report the quality of spine care in degenerative lumbar spine disorders (Appendix 3, see Supplementary data; Table 1). The 34 studies were based on 11 separate registries, representing 7 countries. Indications included were disc herniation (3), spinal stenosis (9), chronic low back pain (5), adult deformity (5), and spinal disorders (7). In 3 studies, a mixture of indications (non-specific subacute and chronic neck, back, and low back pain) was included, but these allowed us to extract data concerning the methodology used for separate indications.
Table 1.
Risk of bias assessment according to Newcastle-Ottawa scale (NOS)
| Study | Spine registry | Selection |
Comparability |
Outcome |
Total *score b | Clinical relevance |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5a | 5b | 6 | 7 | 8 | 1 | 2 | 3 | |||
| Nerland et al. 2014 | NORspine | a * | a * | a * | a * | yes * | yes * | c | a * | n.a. | 7 (7) a | n.a. | n.a. | n.a. |
| Solberg et al. 2013 | NORspine | a * | n.a. | d | b | no | no | c | a * | c | 2 (7) | no | no | yes |
| Corcoll et al. 2006 | NRT en el SNS | a * | n.a. | b * | a * | no | no | c | b | c | 3 (7) | yes | yes | yes |
| Kovacs et al. 2012 | NRT en el SNS | b * | n.a. | b * | a * | yes * | yes * | c | b | b * | 6 (7) a | no | yes | yes |
| Kovacs et al. 2007 | NRT en el SNS | b * | n.a. | d | a * | yes * | yes * | c | b | c | 4 (7) | yes | yes | yes |
| Royuela et al. 2014 | NRT en el SNS | a * | n.a. | d | b | yes * | yes * | c | b | c | 3 (7) | yes | yes | yes |
| Fritzell et al. 2014 | SweSpine | a * | n.a. | c | a * | no | yes * | c | a * | c | 4 (7) | no | no | yes |
| Forsth et al. 2013 | SweSpine | a * | a * | a * | a * | yes * | yes * | c | a * | c | 7 (8) a | no | no | yes |
| Jansson et al. 2005 | SweSpine | a * | n.a. | d | a * | yes * | yes * | c | a * | c | 5 (7) a | no | no | yes |
| Jansson et al. 2009 | SweSpine | a * | n.a. | d | a * | yes * | yes * | c | a * | c | 5 (7) a | no | no | yes |
| Knutsson et al. 2013 | SweSpine | a * | n.a. | d | a * | yes * | yes * | c | a * | c | 5 (7) a | no | no | yes |
| Robinson et al. 2013 | SweSpine | a * | a * | d | a * | yes * | yes * | c | a * | c | 6 (8) a | no | no | yes |
| Sanden et al. 2011 | SweSpine | a * | a * | d | a * | yes * | yes * | c | a * | c | 6 8) a | no | no | yes |
| Sigmundsson et al. 2012 | SweSpine | a * | n.a. | a * | a * | yes * | yes * | c | a * | d | 6 (7) a | yes | yes | yes |
| Sigmundsson et al. 2013 | SweSpine | a * | n.a. | d | a * | no | no | c | b | d | 2 (7) | no | no | yes |
| Sigmundsson et al. 2014 | SweSpine | a * | a * | d | a * | yes * | yes * | c | a * | c | 6 (8) a | no | no | yes |
| Stromqvist et al. 2012 | SweSpine | a * | n.a. | d | a * | no | no | c | a * | c | 3 (7) | no | no | yes |
| Berg et al. 2010 | SSE Spine Tango | b * | a * | a * | a * | no | no | c | a * | b * | 6 (8) a | yes | yes | yes |
| Grob and Mannion 2009 | SSE Spine Tango | c | n.a. | d | b | no | no | c | a * | b * | 2 (7) | no | no | yes |
| Porchet et al. 2009 | SSE Spine Tango | c | a * | d | a * | no | no | c | a * | d | 3 (8) | no | no | yes |
| Aghayev et al. 2012 | SWISSspine | a * | b | d | a * | yes * | yes * | c | a * | d | 5 (8) | no | no | yes |
| Aghayev et al. 2010 | SWISSspine | b * | a * | d | a * | yes * | yes * | c | a * | c | 6 (8) a | no | no | yes |
| Schluessmann et al. 2009 | SWISSspine | a * | n.a. | d | a * | yes * | yes * | c | a * | c | 5 (7) a | no | yes | yes |
| Zweig et al. 2011 | SWISSspine | a * | n.a. | d | a * | yes * | yes * | c | a * | d | 5 (7) a | yes | yes | yes |
| McGirt et al. 2013 | N2QOD | a * | a * | d | a * | n.a. | n.a. | c | a * | n.a. | 4 (5) a | n.a. | n.a. | n.a. |
| Deer et al. 2004 | Nat Outc Reg c | b * | n.a. | c | a * | no | no | c | a * | c | 3 (7) | no | yes | yes |
| Taylor et al. 2000 | Com outc m study d | b * | n.a. | d | b | yes * | yes * | c | a * | c | 4 (7) | no | no | no |
| Bridwell et al. 2007 | A D O Database e | b * | n.a. | d | a * | no | yes * | c | a * | d | 4 (7) | yes | no | yes |
| Glassman et al. 2009 | A D O Database e | b * | n.a. | d | a * | no | yes * | c | a * | d | 4 (7) | no | no | yes |
| Glassman et al. 2007 | A D O Database e | b * | n.a. | d | a * | yes * | yes * | c | a * | d | 5 (7) a | yes | no | yes |
| Kasliwal et al. 2012 | A D O Database e | b * | a * | d | a * | yes * | yes * | c | a * | d | 6 (8) a | yes | no | yes |
| Schwab et al. 2008 | A D O Database e | a * | n.a. | d | b | yes * | yes * | c | a * | c | 4 (8) | yes | no | yes |
| Adogwa et al. 2014 | Multicenter reg f | a * | a * | d | a * | no | yes * | c | a * | d | 5 (8) | no | no | yes |
| Seng et al. 2013 | Singapore GH Reg g | b * | a * | c | a * | no | no | c | a * | a * | 5 (8) | no | yes | yes |
| Percentage with *, a or yes | 94 | 92 | 17 | 86 | 59 | 71 | 0 | 85 | 13 | 50 | 31 | 31 | 97 | |
n.a.: not applicable.
* score NOS.
a high quality.
b n items, considering n.a.
c National Outcomes Registry
d Community outcomes management study
e Adult Deformities Outcomes Database
f Multicenter registry for lumbar spine surgery
g Singapore General Hospital Spine Outcomes Registry
Explanation of NOS, including description of items a–d and method of scoring, is given in Appendix 2:
Selection: 1 representativeness exposed cohort; 2 selection non-exposed cohort; 3 ascertainment exposure; 4 outcome not present at start study.
Comparability: 5a and 5b comparability cohorts on the basis of design/analysis.
Outcome: 6 outcome assessment; 7 follow-up long enough; 8 adequacy follow-up.
Explanation of clinical relevance (yes/no):
1: Are the patients described in detail so that you can decide whether they are comparable to those that you see in your practice?
2: Are the interventions and treatment settings described well enough so that you can provide the same for your patients?
3: Were all clinically relevant outcomes measured and reported?
Risk of bias
Half of the studies were classified as having a high methodological quality (17 of 34; Table 1). Although selection of the non-exposed cohort (item 2) scored high quality (i.e. low risk of bias), 21 studies were rated “n.a.” as these studies did not include a control group. In 20 of the 34 studies, a low risk of bias in comparability (item 5a) was seen, meaning studies controlled for the most relevant case-mix variables (i.e. diagnosis and baseline outcome score). In all studies, the assessment of outcome (item 6) was rated “self-report” (c), and with that scoring low quality. The follow-up was long enough for outcomes to occur (item 7; 29 of 34). However, low quality was seen in the adequacy of follow-up of cohorts (item 8; 18 of 32). Although in almost all the studies the clinically relevant outcomes were measured and reported (31 of 32; clinical relevance item 3), in less than one-third of the studies (10/32) the description of patients and intervention (clinical relevance items 1 and 2) was sufficiently detailed.
Survey
We identified 25 spine registries, representing 14 countries, within the ICHOM Low Back Pain Working Group (ICHOM-LBP WG; 10) through the literature (10; 4 overlap with ICHOM-LBP WG) and through internet searches (9). We were unable to make contact with representatives of 7 of the multicenter registries; the remaining 18 were invited to participate in the survey. 16 of them responded, representing 12 countries and 2 including “diverse” countries (Spine Tango and the European Spine Study Group database (ESSG)). The non-responders were representatives of Russian and Indian registries.
An overview of existing spine registries is presented in Table 2: survey responders (16) and searches though internet and literature (6). 3 multicenter registries in the USA were found through internet searches, but we were unable to obtain relevant information (NASS Spine Registry, SMISS Prospective Data Registry, and Scolisoft Scoliosis Database (see references for websites)); these registries were not included in Table 2.
Table 2.
Registry characteristics
| Registry name 1 | Location | Setting 2 | Since | Location spine 3 | Outcomes lumbar spine |
PROMs assessments 7 | ICHOM-LBP PROMS criteria | Benchmark | Scientific publication 8 | NOS risk of bias score 9 | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Functional Status 4 | Pain 5 | Quality of life 6 | ||||||||||
| Survey respondents | ||||||||||||
| SweSpine | Sweden | N | 1998 | L; C; D; T; I; M | ODI | VAS B&L | SF36; EQ5D | B; P; 12; 24; O, 5y | Yes | average & individual centers | Yes; 12 | 5.3 (2–7) 10 |
| NORspine | Norway | N | 2006 | L; D | ODI | NPRS B&L | EQ5D | B; P; 3; 12 | No | average | Yes; 2 | 4.5 (2–7) |
| DaneSpine | Denmark | N | 2009 | L; C; D; T; I; M | ODI | VAS B&L | EQ5D; SF36 occasion. | B; P; 3; 6; 12; 24; O, 5y; 10y | No | average | No | |
| Dutch Spine Surgery Registry | The Nether-lands | N | 2014 | L & D(mainly)C; T; I; M | ODI | NPRS B&L | SF36; EQ5D | B; P; 2/6; 12; 24* | Yes | average & individual centers(planned) | No | |
| British Spine Registry | UK | N | 2012 | L; C; D; T; I; M | ODI | VAS B&L | EQ5D | B; 3; 12; 24; O, 5y | No | average & individual centers(planned) | No | |
| NRT en el SNS | Spain | N | 2002 | L; C | RMDQ | NPRS B&L | not meas. | B; P; 3; O, each 3 mo # | No | only own data | Yes; 4 | 4.0 (2–6) |
| SWISSspine | Switzerland | N | 2005 | L; C; D; T; I; M | NASS; COMI | NPRS B&L | EQ5D | B; P; 3; 6; 12; 24; O, 5y;10y | No | average | Yes; 4 | 5.3 (5–6) 10 |
| SSE Spine Tango | Diverse | M | 2002 | L; C; D; T; I; M | ODI; COMI | COMI: NPRS B&L | EQ5D occasion. | B; P; 6w; 3; 12; 24 $ | Yes | average | Yes; 3 | 3.3 (2–5) |
| Canadian a | Canada | N/M | 2012 | L; C; T | ODI | VAS B&L | SF12; EQ5D | B; P; 3; 12; 24 | No | average | No | |
| Singapore b | Singapore | N/I | 2001 | L; C; D; T; I; M | ODI; NASS | NPRS B&L | SF36 | B; 1; 3; 6; 24 | No | only own data | Yes; 1 | 5 |
| Newro Foundation | Australia | I | 2010 | L; C | ODI; RMDQ | NRS B&L | SF12, future EQ5D | B; 6w; 3; 6; 12; 24 | No | only own data | No | |
| Texas Back Institute | USA | I | New | L; C; D; T; I; M | ODI | VAS B&L | SF12, future EQ5D | B; 3 % | No | only own data | No | |
| Kaiser Permanente | USA | M | 2009 | O, instru-meneted procedures | n.a. | n.a. | n.a. | P | No | only own data | Yes | |
| N²QOD d | USA | M | 2012 | L; C; D | ODI | NPRS B&L | EQ5D | B; 3; 12 | No | average | Yes; 1 | 4 10 |
| Schön-Clinics Spine Registry | Germany | M/I | 2010 | L; C; D; T; I; M | ODI | VAS B&L | EQ5D | B; P; 3; 12; 24 | No | average & individual centers | Yes | |
| European Spine Study Group | Diverse | M | 2010 | D | ODI; SRS22r; COMI | NRS B&L | SF36 | B; P; 6w; 6; 12; 24 | n.a. | n.a. | Yes | |
| Other sources | ||||||||||||
| Russian Spine Registry 11;12 | Russia | M | 2012 | L | ODI | VAS | SF36 | B; P; not reported | No | Not found | Yes | |
| Indian Spine (surgery) Registry 12 | India | M; future N | Plan. | L | Not found | Not found | Not found | Not found | No | Not found | Not found | |
| National Spine Network e | USA | M | 1995 | L; C | ODI | Not found | SF36 or SF12 or Sf8 | B; 12 optional: 3; 6; 24 | Not found | Not found | Yes; 1 | 3 |
| Multicenter registry f | USA & Canada | M | 2003 | L | ODI | VAS B&L | Not found | B; P; 12; 24 | No | Not found | Yes; 1 | 5 |
| ADO Database g | USA h | M | 2002 | D | SRS-22; ODI | SRS22(pain) | SF12 | B; 6; 12; 24; 5y; 10y; 15y; 20y; 25y | n.a. | Not found | Yes; 5 | 4.6 (4–6) |
| ATSD Database i | USA h | M | 2010 | D | SRS-22 ODI | SRS22(pain) | SF36 | B; 12; 24 | n.a. | Not found | Yes | |
n.a.: not applicable.
1 Registry names:
a Canadian Spine Outcomes and Research Network
b Singapore General Hospital Spine Outcomes Registry
c Kaiser Permanente Spine Implant Registry
d National Neurosurgery Quality and Outcomes Database
e National Spine Network Spine Outcomes Registry (SpineChart) 12
f Multicenter registry for lumbar spine surgery 13
g Adult Deformity Outcomes Database 14
h USA Spine Deformity Study Group
i Adult Thoracolumbar Spinal Deformity Database 15
2 Settings: N National, M Multicenter, I Institutional
3 Locations: L lumbar spine; C cervical spine; D spinal deformity; T spine trauma; I spinal infections; M spinal metastases; O other.
4 Functional status: ODI Oswestry disability index; RMDQ Roland and Morris disability questionnaire; NASS North American Spine Society lumbar spine outcome scale; COMI core outcome measures Index; SRS22 Scoliosis Research Society 22 questions.
5 Pain: B&L back and leg; VAS visual analog scale; NPRS numeric pain rating scale.
6 Quality of life: SF8, SF12, SF36 Short Form 8 or 12 or 36 questions; EQ5D EuroQol 5 dimensions (including EuroQol VAS).
7 PROMS at: B baseline; P perioperative; 6w 6 weeks; 1 1 month; 3 3 months; 6 6 months; 12 12 months; 24 24 months; O other, …; * 2 months in hernia/stenosis; # until discharge; $ at least 1 follow-up; % variabel: when patient returns to clinic.
8 n; according to Appendix 2; Table 1
9 NOS Risk of bias score Newcastle-Ottawa scale – total score; median (range) according to Table 1
10 high quality.
11 Shevelev et al. 2013;
12 See references for websites.
13 Adogwa et al. 2013;
14 e.g. Kasliwal et al. 2012 (see Table 1);
15 Scheer et al. 2013.
Organization and methods used in spine registries
Organization (Table 2)
9 of 22 registries are organized on a nationwide basis. Most spine registries started within the last decade. All registries are health services registries—except for Kaiser Permanente, which is a device or implant registry, and SWISSspine, a device or implant registry for health technology assessment purposes.
Methods (Table 2)
All registries incorporated the main patient-reported outcome domains. ODI, NPRS back and leg, and EQ5D are mainly used as PROMs. In the majority of the registries, clinical outcomes (e.g. complications and reoperations) are also registered. All registries have baseline and 12- and 24-month follow-up assessments, except for NORspine and N²QOD (with only a 12-month follow-up). Although 15 registries report on lumbar spine disorders, only 3 fulfill all the ICHOM-LBP criteria for PROMs. The Adult Deformity Outcomes Database registry has the longest follow-up (25 years). To improve the response rate, all registries use postal, e-mail, or telephone reminders.
Analysis and reporting
In the 34 scientific publications, various analytical approaches were used (Appendix 3, see Supplementary data, Table 4), varying from descriptive statistics, all studies, to multivariate techniques such as mixed linear modeling (Nerland et al. 2014, Robinson et al. 2013) and propensity modeling (Kasliwal et al. 2012, Adogwa et al. 2014). To evaluate the study purpose, all studies used 1 or more PROMs as an outcome measure. In 8 studies, secondary clinical outcomes were defined: complications (Schwab et al. 2008, Kasliwal et al. 2012, Adogwa et al. 2014, Nerland et al. 2014), reoperation (Bridwell et al. 2007), BMI (Knutsson et al. 2013), adverse events (Deer et al. 2004), and Bridwell classification for fusion rates (Seng et al. 2013). In 5 studies, no adjustment for covariates was performed to explain variation in outcomes (Corcoll et al. 2006, Grob and Mannion 2009, Murray et al. 2012, Seng et al. 2013, Sigmundsson et al. 2013). In the remaining 29 studies, patient characteristics were used as covariates, varying from 17 predefined covariates (Royuela et al. 2014) to adjustment for baseline PROMs only (Solberg et al. 2013). Adjustment for baseline PROMs was not performed in 8 studies (Deer et al. 2004, Bridwell et al. 2007,Glassman et al. 2009, Zweig et al. 2011, Kovacs et al. 2012, Sigmundsson et al. 2012, McGirt et al. 2013, Adogwa et al. 2014). In 8 studies, a dropout analysis was performed to compare baseline characteristics (missing data on assessment) with the remaining cases. To handle missing data, multiple imputation techniques were used in 2 studies (Kovacs et al. 2012, Royuela et al. 2014). In the remaining studies, complete case analysis was performed.
All 16 registry representatives reported in the survey, to describe the population and outcomes using descriptive statistics and to provide feedback reports on a regular basis to all participating institutions and spine societies. Benchmarking is performed against the average value of participating institutions in 10 registries (Table 2). The 12-month follow-up responses on PROMs vary from 20% (British Spine Registry) to 88% (the Neuroreflexotherapy Registry of the Spanish National Health Service (NRT en el SNS))
Discussion
We found a lack of evidence to support or refute the effect that spine registries may have on the quality of spine care and on patient-related outcomes. Nonetheless, the publications that have resulted from the spine registries have yielded relevant evidence on interventions or predictive factors for spinal disorders. We have therefore described the methodology used to organize, analyze, and report the “quality of spine care” from spine registries. To improve the quality of results published from registry data and to study the effects of spine registries in future, we have formulated and included several recommendations, which are summarized in Table 3. First of all, the registries should be methodologically well constructed, and we need to learn from existing registries so that a more standardized approach to registering and analysis can be achieved to allow international collaboration, to allow national and international benchmarking, and to make sure that in future spine care is value-based (Table 3, recommendation (rec.) 1).
Table 3.
Recommendations to improve the quality of study results published from registry data
| Organization and method |
| 1. Use a standardized approach to registering in design, methodology, and analysis to allow international collaboration, to achieve benchmarking, and to make sure that in future spine care is value-based. |
| 2. Study and incorporate strategies to improve quality of care, e.g. continuous feedback and audit cycles of results collected in spine registries, on spine care delivered. |
| 3. To increase the quality of registry studies, the population needs to be well-defined in terms of diagnosis and indications for surgery. Both at the developmental stage of a registry and when reporting on registry data, follow the STROBE guidelines. |
| 4. Include a minimum follow-up period of 1 year for surgically treated patients. |
| 5. To meet the definition of a patient registry, all characteristics of a registry should be present (Drolet and Johnson 2008). This means an inclusion principle, mergeable data, standardized dataset for all consecutively included patients, rules for data collection (i.e. systematically and prospectively collected, including pre-intervention data), knowledge about patient-related outcomes, and observations collected over time (i.e. follow-up assessments). |
| Patient-related outcomes |
| 6. Patient-reported outcome measures for degenerative lumbar spine disorders are PROMs with good measurement properties, and as recommended by ICHOM. Although often defined as patient-related clinical outcomes (i.e. reoperation, complications, and failed back surgery syndrome), these indicators are in fact process measures for a complicated course. |
| Analysis and reporting |
| 7. To explain differences in outcomes with advanced multivariate analytical techniques, include a reliability adjustment and an adjustment for covariates. For degenerative lumbar spine disorders, the recommended factors in ICHOM could be used as covariates. |
| 8. To reduce bias in results a 60-80% 12-months follow-up response is recommended. |
| 9. To increase PROM response at follow-up, reminders could be sent by text messaging or e-mail. |
| 10. To understand potential sources of bias, a non-responder analysis on baseline characteristics should be provided, including a quantitative sensitivity analysis in order to evaluate the extent to which the results are affected by bias. |
| 11. Multiple imputation techniques are recommended for sensitivity analysis when missing data are randomly divided. |
| Practical issues a |
| 12. Linkage between electronic medical records and registry data to avoid double data entry and to enhance routine in daily practice. |
| 13. Participating departments should have direct access to their own data and should have real-time comparisons with other departments and, if available, with the national mean. |
| 14. After approval, analyzed results corrected for case mix should be presented for public access on open web pages in order to increase credibility and to allow adequate and relevant comparisons. |
a not discussed in this study.
Quality improvement in spine care
Although we did not find any scientific evidence for an effect of introducing and using spine registries on the quality of spine care, in 16 registries feedback reports are compiled and disseminated on a regular basis to the participating institutions and the spine societies in order to improve the quality of spine care delivered. In general, improvement strategies include (clinical) audit and feedback, (electronic) patient registries, case management, clinician education, (promotion of) self-management, patient reminder systems, and continuous quality improvement (Shojania et al. 2006, Tricco et al. 2012, Munce et al., 2013) (Table 3, rec. 2).
That registries can have an important effect on the quality of healthcare has, however, been reported in other fields. For example, the Swedish Hip Register has shown that prospectively and systematically collected data have reduced revision rates by describing trends in outcomes adjusted for case-mix factors and early problems (Karrholm 2010). Antibiotic treatment for patients with hard-to-heal ulcers was reduced from 71% before registration to 29% after registration and feedback (Oien and Forssell 2013). A collaborative cohort study of 5 ICUs in the USA showed that an evidence-based intervention resulted in a large sustained reduction (up to 66%) in the rate of catheter-related bloodstream infection, which was maintained throughout the 18-month study period (Pronovost et al. 2006). A study of 13 patient registries in 5 countries demonstrated that these systems have great potential to improve health outcomes and lower healthcare costs (Kuenen et al. 2011).
Recently, reports from Sweden have indicated that spine registries have a positive effect on healthcare, i.e. on patient-related outcomes (complying with the recommendations in Table 3). For example, today the national mean length of stay (LoS) for surgery for lumbar disc herniation is 2 days, with a range of 0–4 days. After introduction of new routines, the LoS in 1 university hospital was reduced from 4 days to 2.5 days, giving the same patient-related outcomes at lower costs (Stromqvist et al. 2014). Another example is a change in surgical procedures in elderly patients with lumbar spinal stenosis (LSS). 2-year registry data on 8,785 elderly patients showed that surgery can be limited to an invasive procedure of decompression alone, in order to avoid unnecessary complications associated with fusion procedures (Forsth et al. 2013). These registry findings have recently been confirmed with a multicenter RCT involving 229 elderly patients with 1- or 2-level LSS. After 2 years, no benefit from adding fusion to decompression surgery was found, which means that in this population a less invasive procedure of decompression can reduce the number of complications and costs to society (Forsth et al. 2014).
Quality of studies based on registry data
In the present study, only half of the publications could be regarded as having a low risk of bias, as assessed on the Newcastle-Ottawa scale (NOS). The main weaknesses of the studies included were the inaccurate descriptions of the patients and of the interventions studied, and the lack of long-term assessment of the outcome. We therefore recommend use of the STROBE guidelines for reporting of observational studies (von Elm et al. 2007) (Table 3, rec. 3). Moreover, as it is known that changes in patient-related outcomes are seen during the first year after spine surgery (Weinstein et al. 2009, Desai et al. 2013, Mannion et al. 2013, Adogwa et al. 2014); a minimum follow-up period of 1 year is recommended (Table 3, rec. 4). As stability of patient-reported outcome measures (PROMs) results is seen between 2 and 4 years (Weinstein et al. 2009, Adogwa et al. 2014), longer follow-up periods are desirable. Another weakness causing high risk of bias according to NOS is that the assessment of outcomes in all studies was performed with PROMs. As PROMs are self-reported measures, these measures are assessed as being of low quality by NOS (Appendix 2, see Supplementary data). Although of lower quality methodologically, PROMs are the recommended outcome measures in spine surgery (McCormick et al. 2013), as there is no valid biomedical measure currently available to evaluate recovery after a spinal intervention. Although they are usually defined as patient-related clinical outcomes, reoperation and complications are in fact process measures for a complicated course to an endpoint defined by PROMs.
Methodology of studies based on registries
Although all 34 studies met the 6 inclusion criteria for registry characteristics (Drolet and Johnson 2008) (Table 3, rec. 5), we found various analytical approaches. Thus, we cannot give the best approach to use when comparing institutions in the search to identify best practices. In measurement of patient-based outcomes, the PROMs used should ideally fulfill the criteria for good measurement properties (Terwee et al. 2007). Recently, consensus was reached within the ICHOM collaboration on which PROMs should be recommended for the evaluation of outcomes of interventions for degenerative lumbar spinal disorders (Oswestry disability index (ODI), numeric pain rating scale (NPRS)—back and leg, and EuroQol 5 dimensions (EQ5D) (ICHOM, 2014) (Table 3, rec. 6). Although as yet only 3 lumbar spine patient registries (SweSpine, Dutch Spine Surgery Registry, and Spine Tango) use the specific ICHOM PROMs, every other registry studied has already evaluated functional status, pain intensity, and quality of life with PROMs, but the assessment used other tools.
To prevent selection bias (Wood et al. 2004) and to explain real differences in outcomes between institutions, multivariate approaches with adjustment for covariates (corrections for differences in characteristics of patients treated in hospitals; “case-mix adjustments”) and correction for chance variation (reliability adjustments) are needed (Iezzoni 1995, Wouters et al. 2008, Dimick et al. 2010, Desai et al. 2013) (Table 3, rec. 7). A shortcoming of these techniques is that they only account for known covariates. In this systematic review, we found that a large variety and number of covariates are included in different registries. A recently published study showed that a large number of patient characteristics (biomedical, psychosocial, and health-related indicators) could influence the outcome of interventions for lumbar spinal disorders or maintain the complaints (van Hooff et al. 2014). Within the ICHOM collaboration, consensus was reached to use a minimum set of factors: age, sex, education level, work status, duration of sick leave, smoking status, comorbidities, BMI, duration of back/leg pain, morbidity state, diagnosis and indication surgery, need for continuous analgesic use, prior intervention, baseline patient-reported disability, back and leg pain baseline, and health-related quality of life (ICHOM 2014) (Table 3, rec. 7). Currently, none of the registries collect data on all of these recommended factors. In the countries influenced by the SweSpine registry format (Sweden, Norway, Denmark, and the Netherlands), consensus has been reached to implement all these factors in the registry, to allow them to be used as covariates in future benchmark analyses. When benchmarking across centers, it has been suggested recently that together with these patient-related covariates, center-specific characteristics might also influence the outcome of surgery in degenerative lumbar spine disorders (Desai et al. 2013).
In the registries, the 12-month follow-up on PROMs varied from 20% (British Spine Registry) to 88% (NRT en el SNS). A suggested rule of thumb is that a loss to follow-up of more than 20% would probably lead to bias in the results, whereas a rate of less than 5% would not (Sackett et al. 2000, Schulz and Grimes 2002). A recently performed study on Norwegian registry 2-year follow-up data on 633 patients showed that a loss to follow-up of 22% would not alter conclusions about the outcome of interventions (Solberg et al. 2011). Efforts should be made to increase 12- and 24-month follow-up responses to 60–80% (Table 3, rec. 8). Although patients are 3 times more likely to respond when invited for follow-up visits (Solberg et al. 2011), it is too demanding for all parties involved to arrange long-term follow-up visits in large patient registries (Fritzell et al. 2006). Solberg et al. (2011) found that forgetfulness is the most important reason for not responding, which could possibly be prevented by modern communication techniques such as text messages and e-mail (Table 3, rec. 9). To handle missing data in most registries, analyses are only performed on complete cases. To understand potential sources of bias, a non-responder analysis on baseline characteristics should be provided (Table 3, rec. 10). Statistical sensitivity techniques are available to test whether there is bias present. When data are missing at random, indicating that the missing data are related to other observed or documented patient data but not to unobserved outcomes, we recommend multiple imputation techniques (Table 3, rec. 11). The major advantage of this method over single imputation techniques or “complete cases only” is that it does not underestimate variability (Twisk and de Vet 2002, Donders et al. 2006).
Strengths and limitations
To evaluate the risk of bias in the studies included, as a quality assessment, we defined a cutoff value (total score ≥ 6 (75%)) on the Newcastle-Ottawa scale (NOS) for cohort studies. However, research is needed to identify whether this is the correct tool for assessment of the risk of bias in patient registries. Another limitation is that selection bias might be present in the spine registries identified. We identified 2 types of registries: national and institutional. The national registries are in most cases part of an obligatory, government- or insurer-driven need for quality control and/or audit. The multicenter institutional registries carry the risk of selection bias (e.g. many institutional registries include premier spine institutes with selected patients) and even more when they are sponsored by industry (ESSG, SWISSspine, Canadian Spine Outcomes, and the Research Network, Indian Spine Registry) or by membership (SSE Spine Tango, British Spine Registry, National Spine Network Spine Outcomes Registry). Although we performed a thorough search and gained an overview of 25 large registries for degenerative spinal disorders, we cannot rule out that more spine registries exist.
The main strength of this study was that we adopted a systematic approach, including a systematic search and an appraisal of quality. In addirion, we conducted a survey among representatives of all the known registries to add information to that found in the literature. To increase the response, we contacted (successfully) all the representatives of the spine registries to complete our data.
Conclusions
Currently, despite there being some evidence in other fields of healthcare, there is a lack of evidence to either support or refute the impact that spine registries may have on the quality of spine care and, with that, on patient-related outcomes. To improve the quality of results published from registry data, we have formulated several recommendations. With the first indications of the effects of the SweSpine registry already known (e.g. improved outcomes after feedback on length of stay and no patient-related benefit from adding fusion to decompression surgery), we believe that application of these recommendations could lead to spine registries demonstrating trends and outcomes, monitoring the quality of spine care delivered, resolving controversies in the management of degenerative spinal disorders, and ultimately improving the value of the care given to our patients.
Supplementary data
Appendices 1–3 are available at Acta’s website (www.actaorthop.org), identification number 8170.
Acknowledgments
MH, WJ, and PF had the idea for the study. All authors contributed to the design of the study. RO provided methodological input, and MK and PF provided clinical input during the protocol phase. MH and WJ designed the search strategy for the literature search and developed the survey. They performed the study selection, appraised the quality of the literature, and performed the data extraction. They also analyzed the data both for the systematic review and for the survey. All the authors contributed to interpretation of the results. MH, WJ, and PF drafted the manuscript. MH and WJ wrote the appendices. All the authors critically revised the manuscript and read and approved the final version.
We thank the members of the ICHOM Low Back Pain Working Group and all the participants who completed the spine registry survey. We especially thank Caleb Stowell (ICHOM) for his support in building and managing the survey in the Harvard Business Qualitrics online web-application and Serge Stommels for his support in translating Russian texts in relation to the Russian Spine Registry.
No competing interests declared.
References
- Adogwa O, Huang M I, Thompson P M, et al. No difference in postoperative complications, pain, and functional outcomes up to 2 years after incidental durotomy in lumbar spinal fusion: a prospective, multi-institutional, propensity-matched analysis of 1,741 patients. Spine J. 2014;14(9):1828–34. doi: 10.1016/j.spinee.2013.10.023. [DOI] [PubMed] [Google Scholar]
- AHRQ. 2014. http://archive.ahrq.gov/consumer/qnt/qntqlook.html. 2015 Feb 09; Available. Accessed.
- Benson K, Hartz A J. A comparison of observational studies and randomized, controlled trials. N Engl J Med. 2000;342(25):1878–86. doi: 10.1056/NEJM200006223422506. [DOI] [PubMed] [Google Scholar]
- Bridwell K H, Berven S, Glassman S, et al. Is the SRS-22 instrument responsive to change in adult scoliosis patients having primary spinal deformity surgery? Spine (Phila Pa 1976) 2007;32(20):2220–5. doi: 10.1097/BRS.0b013e31814cf120. [DOI] [PubMed] [Google Scholar]
- Colditz G A. Overview of the epidemiology methods and applications: strengths and limitations of observational study designs. Crit Rev Food Sci Nutr. 2010;50(Suppl 1):10–12. doi: 10.1080/10408398.2010.526838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Concato J, Shah N, Horwitz R I. Randomized, controlled trials, observational studies, and the hierarchy of research designs. N Engl J Med. 2000;342(25):1887–92. doi: 10.1056/NEJM200006223422507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Concato J, Lawler E V, Lew R A, Gaziano J M, Aslan M, Huang G D. Observational methods in comparative effectiveness research. Am J Med. 2010;123(12 Suppl 1):e16–e23. doi: 10.1016/j.amjmed.2010.10.004. [DOI] [PubMed] [Google Scholar]
- Corcoll J, Orfila J, Tobajas P, Alegre L. Implementation of neuroreflexotherapy for subacute and chronic neck and back pain within the Spanish public health system: audit results after one year. Health Policy. 2006;79(2-3):345–57. doi: 10.1016/j.healthpol.2005.11.001. [DOI] [PubMed] [Google Scholar]
- Deer T, Chapple I, Classen A, et al. Intrathecal drug delivery for treatment of chronic low back pain: report from the National Outcomes Registry for Low Back Pain. Pain Med. 2004;5(1):6–13. doi: 10.1111/j.1526-4637.2004.04011.x. [DOI] [PubMed] [Google Scholar]
- Desai A, Bekelis K, Ball P A, et al. Variation in outcomes across centers after surgery for lumbar stenosis and degenerative spondylolisthesis in the spine patient outcomes research trial. Spine (Phila Pa 1976) 2013;38(8):678–91. doi: 10.1097/BRS.0b013e318278e571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dimick J B, Staiger D O, Birkmeyer J D. Ranking hospitals on surgical mortality: the importance of reliability adjustment. Health Serv Res. 2010;45(6 Pt 1):1614–29. doi: 10.1111/j.1475-6773.2010.01158.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donders A R, van der Heijden G J, Stijnen T, Moons K G. Review: a gentle introduction to imputation of missing values. J Clin Epidemiol. 2006;59(10):1087–91. doi: 10.1016/j.jclinepi.2006.01.014. [DOI] [PubMed] [Google Scholar]
- Drolet B C, Johnson K B. Categorizing the world of registries. J Biomed Inform. 2008;41(6):1009–1020. doi: 10.1016/j.jbi.2008.01.009. [DOI] [PubMed] [Google Scholar]
- Forsth P, Michaelsson K, Sanden B. Does fusion improve the outcome after decompressive surgery for lumbar spinal stenosis?: A two-year follow-up study involving 5390 patients. Bone Joint J. 2013;95-B(7):960–5. doi: 10.1302/0301-620X.95B7.30776. [DOI] [PubMed] [Google Scholar]
- Forsth P, Carlsson T, Michealsson K, Sanden B. No benefit from fusion in decompressive surgery for lumbar spinal stenosis. Two-year results from the Swedish spinal stenosis study. A multicenter RCT of 229 patients. Abstract EuroSpine conference 2014; Lyon France. [Google Scholar]
- Fritzell P, Stromqvist B, Hagg O. A practical approach to spine registers in Europe: the Swedish experience. Eur Spine J. 2006;15(Suppl 1):S57–S63. doi: 10.1007/s00586-005-1051-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glassman S D, Schwab F, Bridwell K H, Shaffrey C, Horton W, Hu S. Do 1-year outcomes predict 2-year outcomes for adult deformity surgery? Spine J. 2009;9(5):317–22. doi: 10.1016/j.spinee.2008.06.450. [DOI] [PubMed] [Google Scholar]
- Gliklich R E, Dreyer N A. Registries for Evaluating Patient Outcomes. A User’s Guide. 2nd. 2010. ed. [PubMed]
- Grob D, Mannion A F. The patient’s perspective on complications after spine surgery. Eur Spine J. 2009;18(Suppl 3):380–5. doi: 10.1007/s00586-009-1005-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoy D, March L, Brooks P, et al. The global burden of low back pain: estimates from the Global Burden of Disease 2010 study. Ann Rheum Dis. 2014;73(6):968–974. doi: 10.1136/annrheumdis-2013-204428. [DOI] [PubMed] [Google Scholar]
- ICHOM. (International Consortium for Health Outcomes Measurements) Standard Set for Low Back Pain. http://www.ichom.org/project/low-back-pain/ 2014 Available from. Accessed on: 09 February 2015.
- Iezzoni LI. Risk adjustment for medical effectiveness research: an overview of conceptual and methodological considerations. J Investig Med. 1995;43(2):136–150. [PubMed] [Google Scholar]
- Jacobs W, Hooff van ML, Stoefs J, towell C, Fritzell P. ISSLS Focus Group Global Collaboration of Spine Registries. International Society for the Study of the Lumbar Spine (ISSLS) Seoul Korea. 2014.
- Jacobs WC, Kruyt MC, Verbout AJ, Oner FC. Effect of methodological quality measures in spinal surgery research: a metaepidemiological study. Spine J. 2012a;12(5):339–48. doi: 10.1016/j.spinee.2012.01.015. [DOI] [PubMed] [Google Scholar]
- Jacobs WC, Kruyt MC, Verbout AJ, Oner FC. Spine surgery research: on and beyond current strategies. Spine J. 2012b;12(8):706–13. doi: 10.1016/j.spinee.2012.08.424. [DOI] [PubMed] [Google Scholar]
- Karrholm J. The Swedish Hip Arthroplasty Register. Acta Orthop. 2010;81(1):3–4. doi: 10.3109/17453671003635918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kasliwal MK, Smith JS, Shaffrey CI, et al. Does prior short-segment surgery for adult scoliosis impact perioperative complication rates and clinical outcome among patients undergoing scoliosis correction? J Neurosurg Spine. 2012;17(2):128–33. doi: 10.3171/2012.4.SPINE12130. [DOI] [PubMed] [Google Scholar]
- Knutsson B, Michaelsson K, Sanden B. Obesity is associated with inferior results after surgery for lumbar spinal stenosis: a study of 2633 patients from the Swedish spine register. Spine (Phila Pa 1976) 2013;38(5):435–41. doi: 10.1097/BRS.0b013e318270b243. [DOI] [PubMed] [Google Scholar]
- Kovacs FM, Seco J, Royuela A, Corcoll RJ, Abraira V. Predicting the evolution of low back pain patients in routine clinical practice: results from a registry within the Spanish National Health Service. Spine J. 2012;12(11):1008–20. doi: 10.1016/j.spinee.2012.10.007. [DOI] [PubMed] [Google Scholar]
- Kuenen JW, Mohr R, Larsson S, Van Leeuwen W. Zorg voor waarde. Meer kwaliteit voor minder geld: wat de Nederlandse gezondheidszorg kan leren van Zweden. http://www.bcg.nl/documents/file65689.pdf. 2011 Available from: Accessed on: 17 April 2015.
- Larsson S, Lawyer P, Siverstein MB. Putting Value-Based Healthcare into Practice in Sweden: The Boston Consultancy Group (BCG); 2010. From concept to reality. Available from: Accessed on: 17 April 2015. [Google Scholar]
- Mannion AF, Brox JI, Fairbank JC. Comparison of spinal fusion and nonoperative treatment in patients with chronic low back pain: long-term follow-up of three randomized controlled trials. Spine J. 2013;13(11):1438–48. doi: 10.1016/j.spinee.2013.06.101. [DOI] [PubMed] [Google Scholar]
- McCormick JD, Werner BC, Shimer AL. Patient-reported outcome measures in spine surgery. J Am Acad Orthop Surg. 2013;21(2):99–107. doi: 10.5435/JAAOS-21-02-99. [DOI] [PubMed] [Google Scholar]
- McGirt MJ, Speroff T, Dittus RS, Harrell FE, Jr, Asher AL. The National Neurosurgery Quality and Outcomes Database (N2QOD): general overview and pilot-year project description. Neurosurg Focus. 2013;34(1):E6. doi: 10.3171/2012.10.FOCUS12297. [DOI] [PubMed] [Google Scholar]
- Munce SE, Perrier L, Tricco AC, et al. Impact of quality improvement strategies on the quality of life and well-being of individuals with spinal cord injury: a systematic review protocol. Syst Rev. 2013;2:14. doi: 10.1186/2046-4053-2-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray CJ, Vos T, Lozano R, Naghavi M, Flaxman AD, Michaud C, et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2197–223. doi: 10.1016/S0140-6736(12)61689-4. [DOI] [PubMed] [Google Scholar]
- Nerland US, Jakola AS, Solheim O, et al. Comparative effectiveness of microdecompression and laminectomy for central lumbar spinal stenosis: study protocol for an observational study. BMJ Open. 2014;4(3):e004651. doi: 10.1136/bmjopen-2013-004651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oien RF, Forssell HW. Ulcer healing time and antibiotic treatment before and after the introduction of the Registry of Ulcer Treatment: an improvement project in a national quality registry in Sweden. BMJ Open. 2013;3(8):e003091. doi: 10.1136/bmjopen-2013-003091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillips FM, Slosar PJ, Youssef JA, Andersson G, Papatheofanis F. Lumbar spine fusion for chronic low back pain due to degenerative disc disease: a systematic review. Spine (Phila Pa 1976) 2013;38(7):E409–E422. doi: 10.1097/BRS.0b013e3182877f11. [DOI] [PubMed] [Google Scholar]
- Porter ME. What is value in health care? N Engl J Med. 2010;363(26):2477–2481. doi: 10.1056/NEJMp1011024. [DOI] [PubMed] [Google Scholar]
- PRISMA statement and checklist. http://www.prisma-statement.org/index.htm. Available from: Accessed on: 09 February 2015.
- Pronovost P, Needham D, Berenholtz S, et al. An intervention to decrease catheter-related bloodstream infections in the ICU. N Engl J Med. 2006;355(26):2725–32. doi: 10.1056/NEJMoa061115. [DOI] [PubMed] [Google Scholar]
- Robinson Y, Michaelsson K, Sanden B. Instrumentation in lumbar fusion improves back pain but not quality of life 2 years after surgery. A study of 1,310 patients with degenerative disc disease from the Swedish Spine Register SWESPINE. Acta Orthop. 2013;84(1):7–11. doi: 10.3109/17453674.2013.771300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Royuela A, Kovacs FM, Campillo C, Casamitjana M, Muriel A, Abraira V. Predicting outcomes of neuroreflexotherapy in patients with subacute or chronic neck or low back pain. Spine J. 2014;14(8):1588–600. doi: 10.1016/j.spinee.2013.09.039. [DOI] [PubMed] [Google Scholar]
- Sackett D L, Richardson WS, Rosenberg W, Haynes RB. Evidence-based medicine: how to practice and teach EBM. 2000. Chrurchill and Livingstone Edinburgh.
- Schulz KF, Grimes DA. Sample size slippages in randomised trials: exclusions and the lost and wayward. Lancet. 2002;359:781–5. doi: 10.1016/S0140-6736(02)07882-0. [DOI] [PubMed] [Google Scholar]
- Schwab FJ, Lafage V, Farcy JP, Bridwell KH, Glassman S, Shainline MR. Predicting outcome and complications in the surgical treatment of adult scoliosis. Spine (Phila Pa 1976) 2008;33(20):2243–7. doi: 10.1097/BRS.0b013e31817d1d4e. [DOI] [PubMed] [Google Scholar]
- Seng C, Siddiqui MA, Wong KP, et al. Five-year outcomes of minimally invasive versus open transforaminal lumbar interbody fusion: a matched-pair comparison study. Spine (Phila Pa 1976) 2013;38(23):2049–2055. doi: 10.1097/BRS.0b013e3182a8212d. [DOI] [PubMed] [Google Scholar]
- Shojania KG, Ranji SR, McDonald KM, et al. Effects of quality improvement strategies for type 2 diabetes on glycemic control: a meta-regression analysis. JAMA. 2006;296(5):427–40. doi: 10.1001/jama.296.4.427. [DOI] [PubMed] [Google Scholar]
- Sigmundsson FG, Kang XP, Jonsson B, Stromqvist B. Prognostic factors in lumbar spinal stenosis surgery. Acta Orthop. 2012;83(5):536–42. doi: 10.3109/17453674.2012.733915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sigmundsson FG, Jonsson B, Stromqvist B. Impact of pain on function and health related quality of life in lumbar spinal stenosis. A register study of 14,821 patients. Spine (Phila Pa 1976) 2013;38(15):E937–E945. doi: 10.1097/BRS.0b013e3182955989. [DOI] [PubMed] [Google Scholar]
- Solberg TK, Sorlie A, Sjaavik K, Nygaard OP, Ingebrigtsen T. Would loss to follow-up bias the outcome evaluation of patients operated for degenerative disorders of the lumbar spine? Acta Orthop. 2011;82(1):56–63. doi: 10.3109/17453674.2010.548024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solberg T, Johnsen LG, Nygaard OP, Grotle M. Can we define success criteria for lumbar disc surgery? : estimates for a substantial amount of improvement in core outcome measures. Acta Orthop. 2013;84(2):196–201. doi: 10.3109/17453674.2013.786634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stromqvist B, Fritzell P, Hagg O, Knutsson B, Sanden B. The Swedish Spine Register. Swedish Society of Spinal Surgeons. http://www.4s.nu/pdf/ 2014 report SweSpine. Available from: Report_2014_Swespine_Engl_ver_141204.pdf. Accessed on: 25 March 2015.
- Terwee CB, Bot SD, de Boer MR, et al. Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol. 2007;60(1):34–42. doi: 10.1016/j.jclinepi.2006.03.012. [DOI] [PubMed] [Google Scholar]
- Tricco AC, Ivers NM, Grimshaw JM, et al. Effectiveness of quality improvement strategies on the management of diabetes: a systematic review and meta-analysis. Lancet. 2012;379(9833):2252–61. doi: 10.1016/S0140-6736(12)60480-2. [DOI] [PubMed] [Google Scholar]
- Twisk J, de Vet W. Attrition in longitudinal studies. How to deal with missing data. J Clin Epidemiol. 2002;55(5):329–37. doi: 10.1016/s0895-4356(01)00476-0. [DOI] [PubMed] [Google Scholar]
- van Hooff ML, van Loon J, van Limbeek J, de Kleuver M. The Nijmegen decision tool for chronic low back pain. Development of a clinical decision tool for secondary or tertiary spine care specialists. PLoS One. 2014;9(8):e104226. doi: 10.1371/journal.pone.0104226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Leersum NJ, Kolfschoten NE, Klinkenbijl JH, Tollenaar RA, Wouters MW. [‘Clinical auditing’, a novel tool for quality assessment in surgical oncology] Ned Tijdschr Geneeskd. 2011;155(45):A4136. [PubMed] [Google Scholar]
- von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370(9596):1453–7. doi: 10.1016/S0140-6736(07)61602-X. [DOI] [PubMed] [Google Scholar]
- Weinstein JN, Lurie JD, Tosteson TD, et al. Surgical compared with nonoperative treatment for lumbar degenerative spondylolisthesis. four-year results in the Spine Patient Outcomes Research Trial (SPORT) randomized and observational cohorts. J Bone Joint Surg Am. 2009;91(6):1295–304. doi: 10.2106/JBJS.H.00913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wells GA, Shea B, O’Connell D, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. http://www.ohri.ca/programs/ Available from: clinical_epidemiology/oxford.asp. Accessed on: 09 February 2015.
- Wood AM, White IR, Thompson SG. Are missing outcome data adequately handled? A review of published randomized controlled trials in major medical journals. Clin Trials. 2004;1(5):368–76. doi: 10.1191/1740774504cn032oa. [DOI] [PubMed] [Google Scholar]
- Wouters MW, Wijnhoven BP, Karim-Kos HE, et al. High-volume versus low-volume for esophageal resections for cancer: the essential role of case-mix adjustments based on clinical data. Ann Surg Oncol. 2008;15(1):80–87. doi: 10.1245/s10434-007-9673-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zweig T, Hemmeler C, Aghayev E, Melloh M, Etter C, Roder C. Influence of preoperative nucleus pulposus status and radiculopathy on outcomes in mono-segmental lumbar total disc replacement: results from a nationwide registry. BMC Musculoskelet Disord. 2011;12:275. doi: 10.1186/1471-2474-12-275. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


