Abstract
Background: Laryngeal mask airway (LMA) placement is now considered a common airway management practice. Although there are many studies which focus on various airway techniques, research regarding difficult LMA placement is limited, particularly for anesthesiologist trainees. In our retrospective analysis we tried to identify predictive factors of difficult LMA placement in an academic training program.
Methods: This retrospective analysis was derived from a research airway database, where data were collected prospectively at the Memorial Hermann Hospital, Texas Medical Center, Houston, TX, USA, from 2008 to 2010. All non-obstetric adult patients presenting for elective surgery requiring general anesthesia, were enrolled in this study: anesthesiology residents primarily managed the airways. The level of difficulty, number of attempts, and type of the extraglottic device placement were retrieved.
Results: Sixty-nine unique Laryngeal Mask Airways (uLMAs) were utilized as a primary airway device. Two independent predictors for difficult LMA placement were identified: gender and neck circumference. The sensitivity for one factor is 87.5% with a specificity of 50%. However with two risk factors, the specificity increases to the level of 93% and the sensitivity is 63%.
Conclusion: In a large academic training program, besides uLMA not been used routinely, two risk factors for LMA difficulty were identified, female gender and large neck circumference. Neck circumference is increasingly being recognized as a significant predictor across the spectrum of airway management difficulties while female gender has not been previously reported as a risk factor for difficult LMA placement.
Keywords: airway management, LMA, anesthesia, neck circumfrence
Introduction
Since its introduction into clinical practice in 1983 1, the laryngeal mask airway (LMA) has found a place in everyday anesthesia practice 2– 4, including its use as a primary airway device in the elective or pre-hospital emergency settings, as well as a rescue airway device in either settings 5, 6. Additionally, the LMA placement has become a common airway management technique, particularly in ambulatory surgery 2, 3, and is associated with shorter recovery time, earlier patient discharge and lower associated costs 7, 8. Even if the LMA is considered a very safe airway device 9 with a low incidence of complications, there may be situations where it either does not function properly or is difficult to place 10. Importantly, the association between difficult LMA placement and increased incidence of Difficult Mask Ventilation (DMV) has been recognized 11.
Appropriate sizing is critical for correct LMA application 12, while the selection of the device type seems to play a less significant role, yet the prediction of the correct size is not easy. This can be attributed to the absence of a coherent and universal standard sizing system 13. Most of the manufacturers suggest a weight-based size selection, however there is no consistency between weight and oropharyngeal anatomy 14.
Alternative recommendations for the selection of the appropriate size of a LMA, regarding age, height and gender, as well as anatomical landmarks, are still under investigation 15– 17.
As a result, the concepts of difficult LMA placement and effective usage have prompted new research, focusing on the prediction of difficult LMA placement 18.
A simple, objective, predictive score to identify patients at risk of difficult LMA placement at the bedside does not currently exist, however to achieve such score a comprehensive airway assessment based analysis of risk identification needs to be accomplished first. Based on recorded outcomes at a major teaching hospital that utilized a comprehensive airway assessment 19 we aimed to identify predictive factors for difficult LMA placement.
Methods
Data for this retrospective analysis were derived from a database of airway assessments, management plans, and outcomes collected prospectively from August, 2008 to May, 2010 at a Level 1 academic trauma center (Memorial Hermann Hospital, Texas Medical Center, Houston, TX, USA) 11. The study was sponsored by an educational grant from the Foundation for Anesthesia, Education and Research (FAER), and other educational funds from the Department of Anesthesiology at University of Texas Medical School at Houston. After obtaining IRB approval, (HSC-MS-07-0144) all non-obstetric adult patients presenting for elective surgery requiring general anesthesia were enrolled in this study (n=8364). All uLMA placements were carried out by anesthesiology residents. In the ‘mother study’, residents were randomized into two groups—an experimental group, which used a comprehensive airway assessment form 11, 20 in addition to the existing anesthesia record, and a control group, which used only the existing anesthesia record. For the purpose of the present analysis, only the experiment (n=2348) group data was utilized, since the comprehensive airway assessment needed to be linked to the airway device that was utilized. We identified 110 cases-used of LMA, disposable laryngeal mask (uLMA, North America, San Diego, CA), and 69 of those as primary airway device, which we utilized for our analysis. Difficult LMA placement was defined as either inability to physically place a LMA device or inadequacy of ventilation, oxygenation, or airway protection after placement that required conversion to an alternative technique. The level of difficulty and the number of attempts of the uLMA placement were documented by the anesthesiology residents.
Statistical analysis
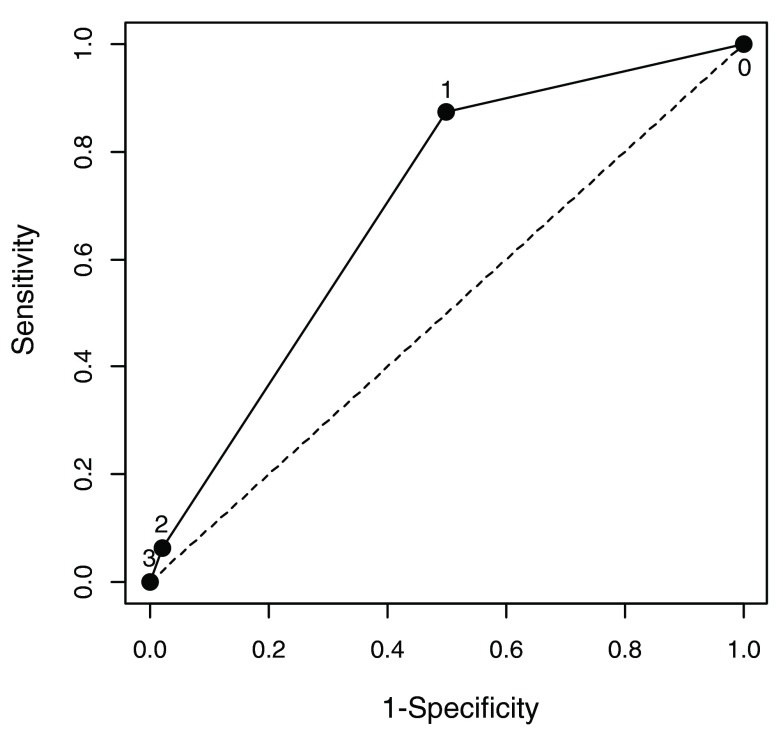
Sixty nine uLMA placements were completed and an analysis was performed (based on “per protocol” and not intention to treat). The mean and standard deviation were used to summarize continuous variables, and frequency (percentage) was summarized for categorical variables. A two-tailed sample t-test was applied to compare continuous variables and Chi-square or Fisher exact tests as appropriate were performed for categorical variables between patients with or without uLMA placement difficulty. Using multivariate logistic regression models, the variables associated with uLMA placement difficulty were identified. All variables with a p-value ≤0.25 in univariate analysis and variables of known biological importance (e.g., age and BMI) were entered into a full model. A backward selection method was used to identify significant independent predictors. A receiver-operating-characteristic (ROC) area under the curve was also calculated to evaluate the resulting model’s predictive value, ( Figure 1) as well as adjusted odds ratios and their 95% confidence intervals. Continuous variables were included after the dichotomization and the best cut-off was determined by maximizing the sum of sensitivity and specificity using the ROC curve. Age distribution for our population was assessed by using descriptive statistics including mean, standard deviation, and median values. All statistical analyses were conducted using SAS 9.3 (SAS Institute, Cary, NC, USA). A p-value <0.05 was considered significant.
Figure 1. A receiver-operating-characteristic (ROC) curve evaluating the sensitivity and specificity of preoperative independent risk factors for LMA difficulty.
Two independent predictors for LMA difficulty were identified using logistic regression: Female and NeckCirc of 44 or greater. The area under the curve was 0.69. The area under the curve was calculated to evaluate the resulting model’s predictive value. The adjusted odds ratios and their 95% confidence interval were calculated. Continuous variables were included after the dichotomization and the best cut-off was determined by maximizing the sum of sensitivity and specificity using the ROC curve. Analyses were conducted using SAS 9.3 (SAS Institute, Cary, NC, USA).
Results
Patient demographics are presented in Table 1 and Table 2. Of the airway evaluations performed using a comprehensive airway assessment tool 69 LMAs were utilized as a primary airway device ( Table 3). Of these, 67 were successful (97.1%) and 2 were unsuccessful (2.9%), with 17 (24.6%) uLMA placements considered as difficult ( Table 4). Multivariate logistic regression models identified two independent predictors of difficult airway: gender and neck circumference ( Table 5). The risk of difficult LMA placement was significantly higher for female patients and patients with a neck circumference (≥44 cm). The model’s c-statistic score is 0.69 ( Table 6). When at least one of two identified risk factors as a cut-off for predicting difficult LMA placement is present, the sensitivity is 87.5% and the specificity is 50%. If we use two risk factors as a cut-off, the specificity increases to the level of 98% and sensitivity is 63% ( Table 5).
Table 1. Preoperative patient characteristics by LMADiff status.
| Variables | LMADiff | p-value | |
|---|---|---|---|
| False (LMADiff=0)
N=52 |
True (LMADiff=1)
N=17 |
||
|
Age (year), mean±SD
<35, n (%) |
48±19
1
17 (33.3) |
51±16
2 (11.8) |
0.608
0.121 |
| Male, n (%) | 33 (64.7) 1 | 8 (47.1) | 0.198 |
|
Height (cm), mean±SD
<175, n (%) |
172.8±10.9
3
23 (46.9) |
169.1±8.5
12 (70.6) |
0.206
0.092 |
| Weight (kg), mean±SD | 79.9±16.0 | 78.9±23.9 | 0.870 |
|
BMI (kg/m
2), mean±SD
<30, n (%) |
26.9±5.8
1
39 (81.3) |
27.5±8.2
2
12 (70.6) |
0.744
0.493 |
|
Neck Circumference, mean±SD
<44, n (%) |
39.3±4.3
1
43 (84.3) |
40.0±6.6
4
10 (62.5) |
0.686
0.082 |
| InterIncisors distance, mean±SD | 4.4±0.8 | 4.3±1.0 | 0.515 |
| Thyromental distance, mean±SD | 8.9±1.5 1 | 9.1±0.9 4 | 0.561 |
| Sternomental distance, mean±SD | 16.2±2.4 1 | 16.1±2.1 4 | 0.835 |
|
Neck Mobility Grade, n (%)
1 2,3 |
36 (69.2) 16 (30.8) |
13 (76.5) 4 (23.5) |
0.568 |
|
Mallampati, n (%)
I, II III, IV |
n=51
32 (62.8) 19 (37.3) |
n=17
9 (52.9) 8 (47.1) |
0.474 |
|
U BiteTest
A B C |
41 (78.9) 10 (19.2) 1 (1.9) |
10 (58.8) 6 (35.3) 1 (5.9) |
0.245 |
| Cervical Spine Abnormality, n (%) | 3 (5.8) | 2 (11.8) | 0.591 |
| NoTeeth, n (%) | 7 (13.5) | 4 (23.5) | 0.445 |
| Facial Hair, n (%) | 11 (21.2) | 4 (23.5) | 1.0 |
| Facial Trauma, n (%) | 1 (1.9) | 2 (11.8) | 0.148 |
| Nasal Defect, n (%) | 3 (5.8) | 0 (0) | NR |
| Neck Trauma, n (%) | 2 (3.9) | 0 (0) | NR |
| Short Neck, n (%) | 1 (1.9) | 2 (11.8) | 0.148 |
| Obstructive Sleep Apnea, n (%) | 25 (48.1) | 8 (47.1) | 1.0 |
| Thyroid, n (%) | 2 (3.9) | 1 (5.9) | 1.0 |
1N=51; 2N=14; 3N=49; 4N=16; NR: not reported due to zero cells; p-values are obtained by two sample t-test for continuous variables and Chi-square test or Fisher’s exact test as appropriate for categorical variables
Table 2. Age distribution of our population.
| Gender | Age | |
|---|---|---|
| mean±SD | Median (min, max) | |
| Female (N=27) | 51.1±17.4 | 53 (18, 79) |
| Male (N=41) | 47.3±18.1 | 50 (20, 80) |
| All population (N=68) | 48.8±17.8 | 51.5 (18, 80) |
Table 3. LMA size and expected outcome by LMADiff status.
| Variables | LMADiff | p-value | |
|---|---|---|---|
| False
(LMADiff=0) N=52 |
True
(LMADiff=1) N=17 |
||
|
LMA Size, n (%)
3,4 5 |
n=27
18 (66.7) 9 (33.3) |
n=7
3 (42.9) 4 (57.1) |
0.387 |
|
No of Attempts
1 >1 |
n=29
28 (96.6) 1 (3.5) |
n=4
1 (25.0) 3 (75.0) |
0.003 |
|
Ideal size by weight
3,4 5 |
n=50
15 (30.0) 35 (70.0) |
n=17
6 (35.3) 11 (64.7) |
0.684 |
|
Ideal size by height
3,4 5 |
n=48
28 (58.3) 20 (41.7) |
n=17
14 (82.4) 3 (17.7) |
0.087 |
| ExpecDMV, n (%) | (11.5) | 3 (17.7) | 0.679 |
| ExpecDLMA, n (%) | 4 (7.7) | 2 (11.8) | 0.631 |
| ExpecDL, n (%) | 11 (21.2) | 10 (58.8) | 0.003 |
| ExpecDI, n (%) | 7 (13.5) | 3 (17.7) | 0.699 |
| ExpecDSA, n (%) | 1 (1.9) | 4 (23.5) | 0.012 |
Expec: predicted, expected, at airway assessment; DMV: difficult mask ventilation; DLMA: difficult Laryngeal Mask Airway; DL: Difficult Laryngoscopy; DI: Difficult Intubation; DSA: Difficult Surgical Airway
Table 4. Summary statistics for LMADiff and LMASuccess.
| Outcome | Frequency (percentage) N=69 |
|---|---|
| LMADiff
0 1 |
52 (75.4) 17 (24.6) |
| LMASuccess
0 1 |
2 (2.9) 67 (97.1) |
Table 5. Two independent predictors of LMA difficulty.
| Predictor | β Coefficient | Standard Error | P value | Adjusted odds ratio
(95% Confidence Interval) |
|---|---|---|---|---|
| Female | 1.466 | 0.723 | 0.043 | 4.33 (1.05, 17.85) |
| Neck>=44 | 1.810 | 0.787 | 0.021 | 6.11 (1.31, 28.56) |
Table 6. Diagnostic value of the cut-off for the number of risk factors in predicting a difficult mask ventilation.
| Cut-off for
number of risk factors |
Sensitivity | Specificity | Likelihood
ratio positive |
Likelihood
ratio negative |
Positive
predictive value |
Negative
predictive value |
|---|---|---|---|---|---|---|
| 1 | 0.875 | 0.500 | 1.75 | 0.25 | 0.359 | 0.926 |
| 2 | 0.063 | 0.980 | 3.50 | 0.956 | 0.500 | 0.766 |
Likelihood ratio positive=Sensitivity/(1-Specificity)
Likelihood ratio negative=(1-Sensitivity)/Specificity
The table displays the sensitivity and specificity if we use the given value of the number of risk factors possessed by patients as a cut-off to classify LMA difficult. For example, when we use number of risk factors at 1 as a cut-off, i.e., any patients with >=1 risk factors will be classified as LMA Diff=1 and any patients with <1 risk factors will be classified as LMA Diff=0, the sensitivity will be 0.875 and specificity will be 0.500.
Discussion
In the present investigation, risk factors in 69 LMA primary airway management placements were assessed. The incidence of difficult LMA placement in our study was 24.6% and the LMA failure rate was 2.9%. Moreover, the incidence of failed LMA placement in our study is consistent with previous studies 9, 13, 18, 21, 22, ranging from 0.19 to 4.7%.
Although from a large database, the study resulted only in a few placements, which is consistent with the practice of our teaching academic center and that could give a possible explanation to the increased incidence of difficult LMA placement in our study. Beside the limited number of uLMAs utilized electively, the study provides an interesting perspective on predictive factors pertaining laryngeal mask placement: indeed, two independent risk factors were found, neck circumference ≥44 cm and female gender. A predictive score that would assist the clinician in identifying difficult LMA placement was also developed, resulting in a model with low sensitivity but specificity of 98% and a negative likelihood ratio of 95.6% (for instance, excluding difficult LMA placement in male patients with neck circumference <44 cm).
The current study supports previous findings regarding the correlation of obesity and difficult airway 23– 26, since increased neck circumference is also an independent risk factor for difficult mask ventilation (DMV) and difficult intubation. The most interesting finding of this study is that female gender, rather than male gender is associated with difficult LMA placement in this study population. In contrast, Ramachandran et al. found that male gender was a predictive factor for failed LMA placement 13, 18.
Age distribution of our population was considered as a cause for this difference. Indeed, age distribution of our female population could be associated with an increased proportion of postmenopausal women. Previous studies have demonstrated that the prevalence and severity of Obstructive Sleep Apnea (OSA) is increased in postmenopausal women, as compared to pre-menauposal women, which may be related to functional changes 27. However, history of OSA was not an independent predictive factor in our population. This can be attributed to the retrospective nature of our study, where OSA assessment was assessed only by patient history. Of interest, a recent but unpublished study has highlighted that the female gender was a predictor for difficult LMA placement in a study population of more than 400 patients, where LMA placement was performed by a single skilled clinician 28.
Of the other airway variables that were evaluated in our study, none was identified as an independent predictor of LMA failure: this finding differs from that of Ramachandran et al., who recognized the absence of teeth as an independent predictor of LMA failure, and the differences could be attributed to population included in the two studies, particularly the limited number of outcomes of our study, possible underutilization of the LMA as a primary airway device, as compared to other airway devices, the increased incidence of difficult LMA placements in our population, and the placements by trainees. Discussing the limitations of the present investigation, it is necessary to mention the retrospective nature as well the stepwise selection that may contribute to bias the study, and the subjective nature of the definition of difficult LMA placement. Additionally, we assumed that all anesthesiology residents had similar educational skills based on a previous study 19, which also could have affected our findings.
In conclusion, two risk factors for LMA placement difficulty were identified: female gender and large neck circumference. Considering the airway as an entity, neck circumference is being increasingly recognized as a significant predictive factor for difficulty with airway management, especially when it is considered across the spectrum of difficulties.
Data availability
The data referenced by this article are under copyright with the following copyright statement: Copyright: © 2015 Katsiampoura AD et al.
Data have been obtained from databases at the Memorial Hermann Hospital, Texas Medical Center, Houston, IRB approval HSC-MS-07-0144. The author can support applications to the Institutional Board to make the data accessible upon individual request. Please forward your requests to Davide Cattano.
Funding Statement
This study was sponsored by the Foundation in Anesthesia, Education and Research as the 2007 FAER Education Grant. Dr. Carin A. Hagberg was the Principle Investigator and Dr. Davide Cattano, the Co-Investigator.
Cai’s research was supported by the National Institutes of Health’s Clinical and Translational Science Award grant (UL1 TR000371), awarded to the University of Texas Health Science Center at Houston in 2012 by the National Center for Clinical and Translational Sciences.
[version 1; referees: 2 approved
References
- 1. Brain AI: The laryngeal mask--a new concept in airway management. Br J Anaesth. 1983;55(8):801–5. 10.1093/bja/55.8.801 [DOI] [PubMed] [Google Scholar]
- 2. White PF: Ambulatory anesthesia advances into the new millennium. Anesth Analg. 2000;90(5):1234–5. 10.1097/00000539-200005000-00047 [DOI] [PubMed] [Google Scholar]
- 3. Suhitharan T, Teoh WH: Use of extraglottic airways in patients undergoing ambulatory laparoscopic surgery without the need for tracheal intubation. Saudi J Anaesth. 2013;7(4):436–41. 10.4103/1658-354X.121081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Brimacombe J: The advantages of the LMA over the tracheal tube or facemask: a meta-analysis. Can J Anaesth. 1995;42(11):1017–23. 10.1007/BF03011075 [DOI] [PubMed] [Google Scholar]
- 5. Apfelbaum JL, Hagberg CA, Caplan RA, et al. : Practice guidelines for management of the difficult airway: an updated report by the American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Anesthesiology. 2013;118(2):251–70. 10.1097/ALN.0b013e31827773b2 [DOI] [PubMed] [Google Scholar]
- 6. Berlac P, Hyldmo PK, Kongstad P, et al. : Pre-hospital airway management: guidelines from a task force from the Scandinavian Society for Anaesthesiology and Intensive Care Medicine. Acta Anaesthesiol Scand. 2008;52(7):897–907. 10.1111/j.1399-6576.2008.01673.x [DOI] [PubMed] [Google Scholar]
- 7. Apfelbaum JL, Walawander CA, Grasela TH, et al. : Eliminating intensive postoperative care in same-day surgery patients using short-acting anesthetics. Anesthesiology. 2002;97(1):66–74. [DOI] [PubMed] [Google Scholar]
- 8. Lubarsky DA: Fast track in the post-anesthesia care unit: unlimited possibilities? J Clin Anesth. 1996;8(3 Suppl):70S–72S. 10.1016/S0952-8180(96)90016-1 [DOI] [PubMed] [Google Scholar]
- 9. Verghese C, Brimacombe JR: Survey of laryngeal mask airway usage in 11,910 patients: safety and efficacy for conventional and nonconventional usage. Anesth Analg. 1996;82(1):129–33. 10.1097/00000539-199601000-00023 [DOI] [PubMed] [Google Scholar]
- 10. Buckham M, Brooker M, Brimacombe J, et al. : A comparison of the reinforced and standard laryngeal mask airway: ease of insertion and the influence of head and neck position on oropharyngeal leak pressure and intracuff pressure. Anaesth Intensive Care. 1999;27(6):628–31. [DOI] [PubMed] [Google Scholar]
- 11. Killoran P, Maddukuri V, Altamirano A, et al. : Use of a comprehensive airway assessment form to predict difficult mask ventilation. Anesthesiology. 2014;A442 Reference Source [Google Scholar]
- 12. Brimacombe J, Keller C: Laryngeal mask airway size selection in males and females: ease of insertion, oropharyngeal leak pressure, pharyngeal mucosal pressures and anatomical position. Br J Anaesth. 1999;82(5):703–7. 10.1093/bja/82.5.703 [DOI] [PubMed] [Google Scholar]
- 13. Van Zundert TC, Hagberg CA, Cattano D: Standardization of extraglottic airway devices, is it time yet? Anesth Analg. 2013;117(3):750–2. 10.1213/ANE.0b013e31829f368b [DOI] [PubMed] [Google Scholar]
- 14. Goodman EJ EU, Dumas SD: Correlation of pharyngeal size to body mass index in the adult. Anesth Analg. 1997. [Google Scholar]
- 15. Cattano D CR, Wojtzcak J, Cai C, et al. : Radiologic Evaluation of Internal Airway Anatomy Dimensions. Anesthesiology. 2014;A1139 Reference Source [Google Scholar]
- 16. Gu Y, McNamara JA, Jr, Sigler LM, et al. : Comparison of craniofacial characteristics of typical Chinese and Caucasian young adults. Eur J Orthod. 2011;33(2):205–11. 10.1093/ejo/cjq054 [DOI] [PubMed] [Google Scholar]
- 17. Cattano D VZT, Wojtczak J, Cai C, et al. : A New Method to Test Concordance Between Extraglottic Airway Device Dimensions and Patient Anatomy. Anesthesiology. 2014;A3148 Reference Source [Google Scholar]
- 18. Ramachandran SK, Mathis MR, Tremper KK, et al. : Predictors and clinical outcomes from failed Laryngeal Mask Airway Unique™: a study of 15,795 patients. Anesthesiology. 2012;116(6):1217–26. 10.1097/ALN.0b013e318255e6ab [DOI] [PubMed] [Google Scholar]
- 19. Cattano D, Killoran PV, Iannucci D, et al. : Anticipation of the difficult airway: preoperative airway assessment, an educational and quality improvement tool. Br J Anaesth. 2013;111(2):276–85. 10.1093/bja/aet029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Cattano D, Ferrario L, Maddukuri V, et al. : A randomized clinical comparison of the Intersurgical i-gel and LMA Unique in non-obese adults during general surgery. Minerva Anestesiol. 2011;77(3):292–7. [PubMed] [Google Scholar]
- 21. Grady DM, McHardy F, Wong J, et al. : Pharyngolaryngeal morbidity with the laryngeal mask airway in spontaneously breathing patients: does size matter? Anesthesiology. 2001;94(5):760–6. [DOI] [PubMed] [Google Scholar]
- 22. Rose DK, Cohen MM: The airway: problems and predictions in 18,500 patients. Can J Anaesth. 1994;41(5 pt 1):372–83. 10.1007/BF03009858 [DOI] [PubMed] [Google Scholar]
- 23. Mohsenin V: Gender differences in the expression of sleep-disordered breathing : role of upper airway dimensions. Chest. 2001;120(5):1442–7. 10.1378/chest.120.5.1442 [DOI] [PubMed] [Google Scholar]
- 24. Guilleminault C, Quera-Salva MA, Partinen M, et al. : Women and the obstructive sleep apnea syndrome. Chest. 1988;93(1):104–9. 10.1378/chest.93.1.104 [DOI] [PubMed] [Google Scholar]
- 25. Michael Mathis MD, Satya K. Ramachandran MD, et al. : The Failed Intraoperative Laryngeal Mask Airway: A Study of Clinical and Intraoperative Risk Factors. Anesthesiology. 2011;BOC01 Reference Source [Google Scholar]
- 26. Brodsky JB, Lemmens HJ, Brock-Utne JG, et al. : Morbid obesity and tracheal intubation. Anesth Analg. 2002;94(3):732–6. 10.1097/00000539-200203000-00047 [DOI] [PubMed] [Google Scholar]
- 27. Dancey DR, Hanly PJ, Soong C, et al. : Impact of menopause on the prevalence and severity of sleep apnea. Chest. 2001;120(1):151–5. 10.1378/chest.120.1.151 [DOI] [PubMed] [Google Scholar]
- 28. Leavittn O, Haisook K, Robert A, et al. : B-7 A Randomized Comparison of Laryngeal Mask Airway Insertion Methods Including a Novel External Larynx Lifting- Inflating Air (ELLIA) technique on Postoperative Pharyngolaryngeal Complications Society for Airway Management annual meeting, Seattle, WA, Sept 19–21.2014. [Google Scholar]