Abstract
Background
Overweight, obesity and their consequences are challenges to sustainable social and economic development in Pacific island countries and territories (PICTs). Complementing previous analyses for adults, the purpose of this paper is to synthesise available data on overweight, obesity and their risk factors in adolescents in the region. The resulting Pacific perspective for the younger generation will inform both the national and regional public health response to the crisis of noncommunicable diseases.
Methods
We examined the prevalence of overweight, obesity, physical activity and carbonated sugar-sweetened beverage (SSB) consumption, by using published results of two cross-sectional surveys: the Global School-Based Student Health Survey (GSHS) and the Youth Risk Behavior Surveillance System (YRBSS). GSHS was conducted in ten PICTs between 2010 and 2013 and provided results for 13–15 year olds. YRBSS surveys, conducted repeatedly in five PICTs between 1999 and 2013, provided results for grade 9–12 students (approximately 14–18 years) and enabled examination of trends.
Results
Obesity prevalence ranged from 0 % in female students in Vanuatu to 40 % in males in Niue (GSHS). Among grade 9–12 students (YRBSS), obesity was highest in American Samoa (40 % of males; 37 % of females). Approximately 60 % of students in the Cook Islands, Niue and Tonga (GSHS) and American Samoa (YRBSS), were overweight. In both surveys, less than half of students reported engaging in sixty minutes of physical activity on at least 5 days of the past week. Daily consumption of carbonated SSBs in the past month was reported by over 42 % of students in six PICTs (GSHS), and in the past week by more than 18 % of students in three PICTs (YRBSS). In PICTs conducting YRBSS, obesity prevalence remained high or increased within the period 1999–2013.
Conclusion
There is a need for urgent action on overweight, obesity and their risk factors in Pacific youth. The multiple social, economic and physical determinants of this public health crisis must be addressed. This requires all sectors within government and society in PICTs to implement and evaluate policies that will protect and promote the health of their populations across the life course.
Background
For over 60 years, 22 Pacific island countries and territories (PICTs), referred to here as the Pacific region, have worked together on issues of health and development, as members of the Secretariat of the Pacific Community [1]. In 1995, through the Yanuca Island Declaration, Ministers of Health representing these PICTs set forth the vision of Healthy Islands, a “unifying theme for health protection and health promotion in the island nations of the Pacific for the twenty-first century [2].” Twenty years later, PICTs have declared a crisis of noncommunicable diseases (NCD) [3]. Risk factors for NCDs, including high body mass index (BMI), are leading contributors to death and disability in the region [4].
Globalisation, trade liberalisation and increasing urbanisation are contributing to nutrition and physical activity transitions [5–7]. In the Pacific, traditional diets of root crops, vegetables, fruits, fresh fish and meat are being replaced by imported and processed energy dense, low nutrient foods [8–11]. The availability, affordability and convenience of these products promotes their purchase and consumption [12, 13]. Increasing demand and reliance on processed foods may also threaten local farming and fishing practices and the extensive opportunities for physical activity that these occupations provide. Further, urban living in the islands can be associated with lower levels of work and travel related physical activity [14].
The impact of these changing environments on younger generations is concerning. Obesity in youth adversely affects their psychological, musculoskeletal, cardiovascular and respiratory health [15, 16]. Furthermore, it is associated in the long-term with adult obesity, Type II diabetes, hypertension, cardiovascular morbidity and premature mortality [17].
Adult overweight and obesity prevalence in PICTs has recently been described [18]. To complement this, the objective of this paper is to synthesise, present and interpret available data for adolescents from two school-based surveys of obesity, overweight, physical activity and consumption of carbonated sugar-sweetened beverages (SSBs), across 15 PICTs. This work will inform national and regional NCD strategies and action plans, assist with evaluation of their impact and help track progress in the Pacific towards the global target of halting the rise in obesity [19].
Methods
Setting
The Melanesian, Polynesian and Micronesian islands of the Pacific region are culturally and socioeconomically diverse. The populations of PICTs vary in size; Tokelau has a population of 1400, while there are over 7 million in Papua New Guinea (PNG). In Kiribati, Nauru and PNG, life expectancy at birth is under 65 years, whereas it exceeds 78 years in Guam [20]. Enrolment in secondary school ranges across the region; for example, the net enrolment ratio is 13 % in PNG and 89 % in Palau [20].
Data sources and study design
We selected the World Health Organization (WHO) Global School-Based Student Health Survey (GSHS) [21] and the Centers for Disease Control and Prevention (CDC) Youth Risk Behavior Surveillance System (YRBSS) [22] as the data sources for this work. Participating countries and survey years are listed in Table 1. GSHS has been conducted in ten PICTs, and YRBSS in five PICTs which are also known as United States affiliated Pacific Islands (USAPIs). These surveys provided the widest coverage of the region and the opportunity for two subregional analyses on account of the standardised methodologies used.
Table 1.
GSHS and YRBSS surveys undertaken in the Pacific and included in this analysis
| Global School Based-Student Health Survey (GSHS) | Youth Risk Behavior Surveillance System (YRBSS) | |
|---|---|---|
| American Samoa | 1999 2007 2011 | |
| Commonwealth of the Northern Mariana Islands | 2003 2005 2007 | |
| Cook Islands | 2011 | |
| Fiji | 2010 | |
| Guam | 2001 2007 2011 2013 | |
| Kiribati | 2011 | |
| Nauru | 2011 | |
| Niue | 2010 | |
| Palau | 1999 2001 2003 2005 2007 2009 2011 | |
| Republic of the Marshall Islands | 2003 2007 | |
| Samoa | 2011 | |
| Solomon Islands | 2011 | |
| Tonga | 2010 | |
| Tuvalu | 2013 | |
| Vanuatu | 2011 |
Global School-Based Student Health Survey
Of the ten PICTs conducting GSHS between 2010 and 2013, seven employed a two-stage sampling design to obtain a representative sample of students. Schools were selected by probability proportional to size and then classes within these schools were selected randomly. All students in these classes were eligible to participate. In the Cook Islands, Nauru and Niue, a census was used to obtain data on the target student population.
Local policies and practices govern whether parental approval is required for students to participate in GSHS. Parents are usually notified of the survey in writing and permission requested as needed [23]. Students aged 13–17 years in the selected classes complete a self-administered, anonymous questionnaire which includes questions on demographics, diet and physical activity. Survey staff measure participants’ height and weight beforehand and provide these results in writing to each individual for them to transfer to their computer-scannable answer sheet. Data are weighted to account for sampling design, population distribution by grade and sex, and non-response. A response rate of over 60 % is required for results to be weighted and therefore generalized to the target population [24]. The surveys included in this analysis had overall response rates of 72 % or higher. We extracted data from factsheets of GSHS which provided results for the subset of the survey population aged 13–15 years [25–34].
Youth Risk Behavior Surveillance System
YRBSS surveys have been conducted at least twice in five USAPIs between 1999 and 2013. Local polilcies guide procedures for gaining parental permission and may include obtaining written consent from parents for students to take part in the survey [35]. The sampling design and analysis of YRBSS are similar to GSHS [24, 35]. Generally, in USAPIs apart from Guam, surveys were designed to include all members of the target population. In YRBSS, students in grades 9–12 (approximately 14–18 years) complete an anonymous questionnaire on a range of risk and protective behaviours. Height and weight are self-reported. A response rate of 60 % or more is required for results to be weighted [35]. We extracted results primarily from CDC’s database, Youth Online [22]. For CNMI, we also used results published by Lippe et al. [36]. For each USAPI, we examined the most recent year for which sex-specific weighted data were available. We also analysed trends over time in overweight and obesity prevalence.
Variables
The variables used for this analysis and their definitions are listed in Table 2. Overweight and obesity (defined by WHO as abnormal or excessive fat accumulation that presents a risk to health) [37] are classified in GSHS and YRBSS according to Body Mass Index (BMI)-for-age-and-sex WHO 2007 and CDC 2000 growth references, respectively [38, 39]. In GSHS, overweight is defined as > +1 standard deviation from the median BMI and obesity as > +2 standard deviations. In YRBSS, overweight is reported as a BMI ≥85th and <95th percentile, and obesity as a BMI ≥95th percentile. For the first part of our analysis, we added the prevalence of overweight and obesity from YRBSS to match the GSHS concept of overweight. For the trend analysis of YRBSS data, we examined overweight and obesity according to their standard definitions. We selected time spent in physical activity on account of the well-established evidence base for association with overweight and obesity, the global recommendation (60 mins of moderate to vigorous intensity activity daily for adolescents) and the global voluntary target (to reduce the prevalence of insufficiently physically active adolescents by 10 % by 2025) [19, 40, 41]. Consumption of sugar-sweetened beverages (SSBs), which include soda/soft drinks, juices and flavoured milks, is also an important risk factor for overweight and obesity and related diseases such as type 2 diabetes [42]. The World Health Organization has recently strongly recommended free sugars intake be reduced to less than 10 % of total energy intake [43]. Both GSHS and YRBSS examined daily carbonated SSB consumption (sodas/soft drinks, excluding diet versions) over the past month and week, respectively.
Table 2.
Selected indicators from GSHS and YRBSS
| Global School-Based Student Health Survey | Youth Risk Behavior Surveillance System | |
|---|---|---|
| Overweighta | Percentage of students who were > +1 SD from median for BMI by age and sex. | Percentage of students who were ≥85th and <95th percentile for BMI by age and sex. |
| Obesitya | Percentage of students who were > +2 SD from median for BMI by age and sex. | Percentage of students who were ≥95th percentile for BMI by age and sex. |
| Physical activityb | Percentage of students who were physically active for a total of at least 60 min per day on five or more days during the past seven days. | Percentage of students who were physically active at least 60 min per day on five or more days during the seven days before the survey. |
| Sugar-sweetened beverage consumptionc | Percentage of students who usually drank carbonated soft drinks one or more times per day during the past 30 days. | Percentage of students who drank a can, bottle, or glass of soda or pop one or more times per day during the seven days before the survey. |
SD standard deviation, BMI body mass index
aOverweight and obesity in GSHS and YRBSS are defined using World Health Organization (2007) and Centers for Disease Control (CDC) (2000) growth reference charts, respectively. Height and weight were self-reported in YRBSS
bGSHS questionnaires for Fiji and Nauru advised students to exclude time spent in physical education/gym class. GSHS and YRBSS define physical activity in the questionnaires as “any activity that increases your heart rate and makes you get out of breath some of the time” and provided examples
cGSHS and YRBSS questionnaires provided examples of carbonated soft drinks and asked students not to include diet soft drinks/soda/pop
Ethical approval for this work was not sought as data used were aggregate, unidentifiable and accessible within the public domain.
Results
Overweight and obesity
Among students aged 13–15 years (GSHS), prevalence of overweight exceeded 50 % in males in three PICTs, and in females in four PICTs (see Table 3). For males, prevalence was highest in Tonga, Niue, the Cook Islands and Samoa, and for females in Samoa, the Cook Islands, Tonga and Tuvalu. In contrast, the percentage of overweight students was below 23 % for both sexes, in Fiji, the Solomon Islands and Vanuatu. In the USAPIs for those in grades 9–12 (YRBSS), overweight prevalence was highest in American Samoa (61 % of males, 60 % of females), and lowest in Palau where approximately a quarter of students were overweight (Table 3). Gender differences observed by YRBSS were less marked than in GSHS in which 13–15 year old females had a higher point prevalence of overweight in eight PICTs.
Table 3.
Overweight and obesitya prevalence in the Pacific Region, GSHS and YRBSS, 2007-2013
| Global School-Based Student Health Surveys (GSHS) (13-15 years) | ||||
| Overweight (including obese) | Obese | |||
| Country | Males | Females | Males | Females |
| % (95 % CI) | % (95 % CI) | % (95 % CI) | % (95 % CI) | |
| Cook Islands 2011 | 58.2 | 58.9 | 29.0 | 19.0 |
| Fiji 2010 | 17.9 (13.0–24.2) | 20.4 (16.1–25.4) | 5.9 (4.0–8.8) | 4.5 (3.0–6.7) |
| Kiribati 2011 | 31.9 (27.1–37.1) | 46.4 (41.9–51.0) | 7.8 (5.0–12.0) | 8.5 (6.8–10.5) |
| Nauru 2011 | 40.0 | 48.9 | 17.8 | 15.7 |
| Niue 2010 | 60.3 | --- | 39.9 | --- |
| Samoa 2011 | 43.4 (39.0–47.9) | 59.1 (55.5–62.6) | 15.7 (12.4–19.6) | 22.3 (19.1–25.8) |
| Solomon Islands 2011 | 17.6 (13.1–23.2) | 22.4 (16.7–29.5) | 1.5 (0.7–3.1) | 2.9 (1.2–6.7) |
| Tonga 2010 | 61.2 (57.7–64.6) | 58.0 (53.8–62.0) | 24.7 (21.9–27.7) | 19.1 (15.8–22.8) |
| Tuvalu 2013 | 44.3 | 52.2 | 22.1 | 20.9 |
| Vanuatu 2011 | 8.9 (4.3–17.5) | 13.6 (8.0–22.0) | 0.3 (0.0–2.2) | 0.0 |
| Youth Risk Behavior Surveillance System (YRBSS) (Grades 9–12) | ||||
| Overweight (including obese) | Obese | |||
| Country | Males | Females | Males | Females |
| % (95 % CI) | % (95 % CI) | % (95 % CI) | % (95 % CI) | |
| American Samoa 2011 | 60.7 | 59.8 | 40.4 | 37.3 |
| Guam 2013 | 37.2 | 36.8 | 22.8 (18.9–27.2) | 17.1 (14.1–20.6) |
| Palau 2011 | 24.4 | 24.8 | 12.5 | 11.5 |
| Commonwealth of the Northern Mariana Islands 2007 | 32.3 | 30.4 | 16.0 | 12.9 |
| Republic of the Marshall Islands 2007 | 38.7 | 40.4 | 26.3 | 23.4 |
Confidence intervals were not reported for Cook Islands, Nauru, Niue, American Samoa, Republic of the Marshall Islands, Commonwealth of the Northern Mariana Islands and Palau, as surveys were designed to include all members of the target population. Confidence intervals were not reported for Tuvalu
Prevalence for females in Niue was not reported due to small sample size (less than 20 students)
Results for CNMI for 2007 were obtained from: Lippe J, Brener N, Kann L. et al. Youth risk behavior surveillance - Pacific Island United States Territories, 2007 MMWR Surveillance Summaries. 2008;57(12):28–56
CI Confidence Interval
aOverweight was defined in GSHS as Body Mass Index (BMI) > +1 standard deviation from the median for BMI for age and sex based on World Health Organization reference. Obesity was defined in GSHS as BMI > +2 standard deviations from the median. For the United States affiliated Pacific Islands, we estimated overweight from the addition of YRBSS results for overweight (BMI ≥85th and <95th for BMI for age and sex based on the 2000 Centers for Disease Control and Prevention reference) and obesity (defined as ≥95th percentile for BMI for age and sex). Height and weight were self-reported in YRBSS
Among males aged 13–15 years, obesity was virtually absent in Vanuatu, but affected 40 % in Niue. In six PICTs, over 15 % of males in this age range were obese. Prevalence of obesity in females was highest in Samoa, affecting 22 % (95 % CI: 19–26) of students, and exceeded 15 % in five PICTs. Differences between the sexes varied among PICTs; in three islands, the point prevalence of obesity was higher in females. Among those in grades 9–12 in the USAPIs, obesity prevalence was highest in American Samoa (40 % of males, 37 % of females). Prevalence was lowest in females in Palau (12 %). Overall, more males than females were obese in the USAPIs (Table 3).
Trends (YRBSS, grade 9–12 students)
There was a statistically significant increase in the prevalence of overweight in females in Guam between 2001 and 2013 (Fig. 1). In American Samoa, CNMI and Palau, prevalence of overweight was consistently high at 9.5 % or more within the period of study. For both sexes in RMI, there was a steep decline in overweight prevalence and a marked increase in obesity prevalence, between 2003 and 2007. There were also statistically significant increases in obesity prevalence among females in Guam between 2001 and 2011, and in American Samoan males and females between 1999 and 2011.
Fig. 1.
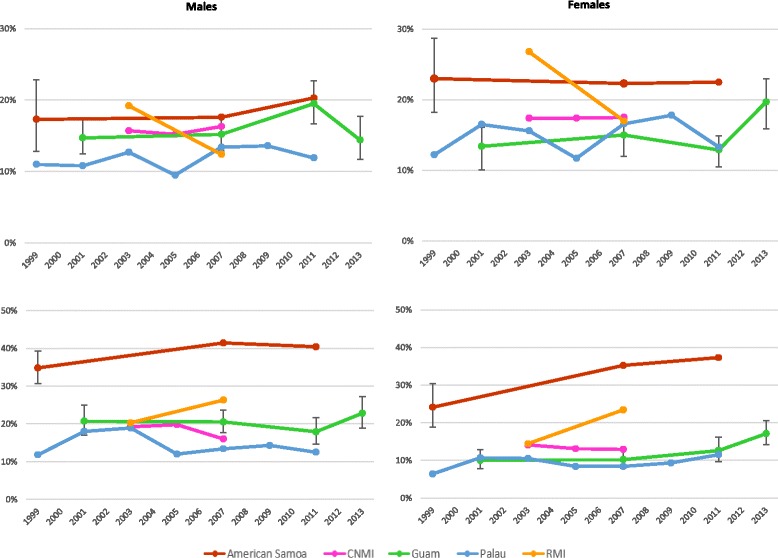
Prevalence of overweight (above) and obesity (below) in grade 9 to 12 students, 1999 to 2013. Source: Youth Risk Behavior Surveillance System (YRBSS) in United States affiliated Pacific Islands between 1999 and 2013. CNMI: Commonwealth of the Northern Mariana Islands. RMI: Republic of the Marshall Islands. Overweight was defined as ≥85th and < the 95th percentile for body mass index (BMI) by age and sex. Obesity was defined as ≥95th percentile for BMI for age and sex. Height and weight were self-reported. Confidence intervals were reported for Guam and American Samoa (1999) only as other surveys in American Samoa, CNMI, Palau and RMI were designed to include all members of the target student population
Physical activity
Less than half of students aged 13–15 years in nine PICTs engaged in sixty minutes of physical activity on five or more days of the past week (Table 4). Prevalence of physical activity ranged widely between islands. For both sexes, around 45 % of students were physically active in Vanuatu. In contrast, 18 % of males and 13 % of females were physically active in Nauru. Among grade 9–12 students in the USAPIs, prevalence of physical activity was highest in males in Guam (44 % 95 % CI: 40–48). Over a third of students were physically active in Palau, and over 20 % were physically active in American Samoa. Males were more active than females in the USAPIs, as observed in other PICTs by GSHS.
Table 4.
Physical activitya and daily soda/soft drink consumptionb prevalence in the Pacific Region, GSHS and YRBSS, 2010–2013
| Global School-Based Student Health Survey (GSHS) | ||||
| Physical activitya | Soft drink consumptionb | |||
| Males | Females | Males | Females | |
| (95 % CI) | (95 % CI) | (95 % CI) | (95 % CI) | |
| Cook Islands 2011 | 44.3 | 34.5 | 59.7 | 63.6 |
| Fiji 2010 | 37.1 (31.8–42.8) | 30.0 (24.2–36.6) | ||
| Kiribati 2011 | 32.8 (27.7–38.3) | 21.9 (18.8–25.3) | 18.4 (14.0–23.7) | 25.6 (22.7–28.7) |
| Nauru 2011 | 17.5 | 12.5 | ||
| Niue 2010 | 41.4 | 73.9 | ||
| Samoa 2011 | 19.8 (17.1–22.8) | 22.1 (19.2–25.2) | 54.6 (50.1–59.0) | 52.5 (48.6–56.4) |
| Solomon Islands 2011 | 30.0 (25.4–35.0) | 25.1 (18.0–33.8) | 46.4 (39.1–53.7) | 42.5 (35.6–49.6) |
| Tonga 2010 | 25.6 (21.0–30.9) | 25.7 (22.7–29.0) | 56.2 (52.0–60.3) | 57.8 (54.3–61.1) |
| Tuvalu 2013 | 48.5 | 55.0 | ||
| Vanuatu 2011 | 45.7 (32.1–60.0) | 46.7 (30.0–64.1) | 37.2 (27.1–48.5) | 38.5 (30.9–46.8) |
| Youth Risk Behavior Surveillance System (YRBSS) | ||||
| Physical activitya | Soft drink consumptionb | |||
| Males | Females | Males | Females | |
| (95 % CI) | (95 % CI) | (95 % CI) | (95 % CI) | |
| American Samoa 2011 | 27.5 | 21.7 | 30.3 | 38.7 |
| Guam 2013 | 44.0 (39.7–48.3) | 30.2 (24.7–36.3) | 18.7 (15.3–22.6) | 19.2 (15.5–23.4) |
| Marshall Islands 2007 | ||||
| Commonwealth of the Northern Mariana Islands 2007 | ||||
| Palau 2011 | 37.6 | 35.7 | 23.7 | 28.9 |
Confidence intervals were not applicable to results from the Cook Islands, Nauru, Niue, American Samoa, Commonwealth of the Northern Mariana Islands (CNMI), Republic of the Marshall Islands (RMI) and Palau, as surveys were designed to include all members of the target population. Confidence intervals were not reported for Tuvalu results
Results for females in Niue were not reported on account of small sample size (less than 20 students)
Physical activity results were not available for Tuvalu, RMI and CNMI. Soft drink consumption results were not available for Fiji, Nauru, RMI and CNMI
Results for CNMI for 2007 were obtained from: Lippe J, Brener N, Kann L. et al. Youth risk behavior surveillance - Pacific Island United States Territories, 2007 MMWR Surveillance Summaries. 2008;57(12):28–56
CI confidence interval
aIn GSHS and YRBSS, this indicator was the proportion of students who were physically active (defined as engaging in any activity that increases the heart rate and makes one get out of breath some of the time) for at least 60 min per day on at least five of more days during the past seven days. Questionnaires for Fiji and Nauru advised students to exclude time spent in physical education/gym class
bGSHS reported the percentage of students who drank carbonated soft drinks one or more times per day during the past 30 days. YRBSS reported the percentage of students who drank a can, bottle or glass of soda or pop one or more times per day during the 7 days before the survey
Daily carbonated sugar-sweetened beverage consumption (soft drink/soda)
In seven of the eight PICTs for which data were available, over 37 % of 13–15 year old students consumed at least one carbonated soft drink/soda per day over the course of the past 30 days (Table 4). Prevalence of daily consumption was lowest in Kiribati and highest in Niue where 74 % of males drank soft drinks every day. Prevalence was often similar between the sexes, though notably higher in females in the Cook Islands (64 %) and Tuvalu (55 %). The proportion of students in grades 9–12 who drank soda at least once per day in the past week varied in the three USAPIs for which data were available. Prevalence ranged from a low of 19 % (95 % CI: 15–23) of males in Guam, to 39 % of female students in American Samoa. Notably more females than males in Palau and American Samoa drank soda daily.
Discussion
Overweight and obesity are determined by individual factors and risk behaviours, which are in turn affected by the interaction of economic and political forces with local environments [44]. The high prevalence of overweight and obesity in Pacific adolescents demonstrates the gravity of the public health problem in the region. Further, prevalences of overweight and obesity in USAPIs have remained high over time, with increases observed in the latter. Less than half of youth obtain sixty minutes of physical activity on five days of the past week, indicating many are not meeting the global recommendation [41]. In addition, there is excessive consumption of carbonated SSBs among students across the region.
Regional and international comparisons
Estimates for the Global Burden of Disease (GBD) Study 2013 indicate that the prevalence of overweight and obesity in youth (under 20 years) in developed countries has risen between 1980 and 2013, from 16.9 to 23.8 % in males, and 16.2 to 22.6 % of females. In developing countries prevalence has risen from 8.1 to 12.9 % in males, and from 8.4 to 13.4 % in females [45]. Some of the highest estimates of obesity in the GBD study for this age group were in Pacific islands - 22.9 % of males and 36.0 % of females in Kiribati, and 23.7 % of males and 29.6 % of females in Samoa [45]. This finding is reflected in the results presented here, and echoed in national surveys undertaken in other PICTs. In a 2010 cross-sectional survey of the oral health of school children in New Caledonia, 20.5 % of 12 year olds were obese (WHO growth reference) [46]. In French Polynesia, the national prevalence of obesity (WHO growth reference) in 2008 was 21.4 % in boys and 19.2 % in girls 5–14 years [47].
Regarding risk factors for overweight and obesity, GSHS results across 34 countries revealed that only 23.8 % of boys and 15.4 % of girls were physically active for 60 mins on at least five days of the week [48]. From the present analysis, in comparison more students were physically active in the PICTs conducting GSHS. Fewer male students in the USAPIs were physically active compared to the 2013 YRBSS national United States estimate (57.3 %) [22]. The prevalence of daily consumption of carbonated soft drinks (not including diet soda) in students aged 13–15 years in PICTs was akin to that in the Eastern Mediterranean WHO Region where it ranged from 30.8 % in the Syrian Arab Republic to 74.3 % in Kuwait [49].
Strengths and limitations
By collating the most recent available and comparable data from GSHS and YRBSS across 15 PICTs, this work fills a critical gap in evidence on overweight, obesity and their associated risk factors in Pacific adolescents. The analysis presented is based on the information provided from the data sources, in addition to resource guides on the general methodology of these surveys.
Although this work provides an important regional perspective on adolescent obesity, our analysis is limited due to incomplete coverage of the Pacific; critically, it does not include representative data for the most populous nation, Papua New Guinea. In addition, the prevalence of obesity and associated risk factors may have changed since the surveys used for our analysis were undertaken. Of note, more recent sex-specific YRBSS results from CNMI, RMI, Palau and American Samoa were not available through Youth Online.
Both GSHS and YRBSS are subject to potential biases. GSHS and YRBSS are representative only of those in formal education and at school on the day of the survey. As risk factor behaviour is self-reported, the surveys may underestimate or overestimate prevalence according to the social desirability of response. Further, it is known that YRBSS can underestimate the prevalence of obesity due to participants under-reporting their weight and over-reporting their height [50]. Regarding reliability, in a small sample of indigenous Fijian adolescent females, the test-retest reliability for GSHS questions on dietary behaviour was found to be lower than that for other risk behaviour domains, suggesting caution may be needed in interpretation of GSHS results [51].
Due to the different growth references from WHO and CDC used in the Pacific, we are only able to examine overweight and obesity prevalence at the sub-regional level. Estimates of the population prevalence of overweight and obesity are affected by the reference used; the WHO 2007 growth reference can yield higher estimates compared to the CDC 2000 growth reference [52]. Therefore, applying the WHO reference to the USAPIs may produce higher overweight and obesity estimates than those observed currently. This hypothesis and the effect of different references on Pacific data warrant further formal investigation.
We have not examined inequalities by ethnicity, socioeconomic status or rural/urban residence in this analysis, and have only studied a limited number of risk factors. Analyses of disparities and examination of a wider range of risk and protective behaviours would enable a more comprehensive understanding of overweight and obesity in Pacific youth. Importantly, further statistical analysis is essential to understand the magnitude of the contribution of all risk factors to the prevalence of overweight and obesity observed, in order to shape policy. Lastly, this work is focused on adolescents; national prevalence data on overweight and obesity in early childhood is required to inform the life course approach to prevention.
Implications for policy and practice
The evidence presented justifies concern for the present and future health of Pacific youth and warrants decisive preventative action on obesity. Such action must fundamentally address the global and national drivers outlined earlier, as well as the more proximal food, physical and socio-cultural contexts which affect diet and exercise patterns of youth in PICTs. For example, in Tonga and Fiji, the availability and ease of access to food and drinks high in fat and sugar near schools and within their canteens enables youth to purchase unhealthy options [53, 54]. With regards to physical activity, safety concerns, poorly maintained roads, and the distance to recreational facilities are frequently cited barriers to engaging in exercise by youth in Apia, Samoa [55]. Culture and social values, such as the centrality of food to express nurture and care, higher esteem afforded to imported foods, and structures of rank and status may differentially influence the type and amount of food consumed within communities in the Pacific [12, 56, 57]. For indigenous Fijian and Tongan males, desire and pressure to perform well in sport and to achieve a robust muscular body may affect eating and exercise accordingly [57]. In contrast, females’ opportunities for physical activity may be constrained by gendered social norms [56].
With cognisance of this context, change at the national level, as well as across multiple-settings in communities, is essential. To increase the availability and affordability of healthier food and drink options in communities, PICTs can consider investing in local agriculture and fisheries, constructing tariff schedules to incentivise the importation and consumption of healthier products, and restricting imports of unhealthy foods [7]. Precedent in the Pacific exists - several PICTs have imposed taxes on SSBs for health benefits and/or revenue raising potential [58]. Tokelau has banned the importation of soft drinks [59]. These policy interventions may contribute to reductions in free sugars intake in accordance with WHO recommendations. Domestic policy space may, however, be constrained by international trade agreements, as demonstrated by the reversal of Samoa’s ban on the importation of turkey tails in order to comply with World Trade Organisation requirements [60].
Considering the influence exerted by advertising on young people’s food preferences, PICTs can implement recommendations to restrict the marketing of unhealthy products to children and adolescents [61]. PICTs can also ensure schools provide safe drinking water, and that school policies support physical activity opportunities [62] and improve the nutritional quality of food and drinks in school canteens [63]. Urban planning options may be explored which enable active transport and increase community recreational facilities and opportunities that are safe, accessible and acceptable for all genders. Prioritisation of the full array of options is required, a process which will be informed by the work of the WHO Commission on Ending Childhood Obesity.
Additional research on the similarities and differences between PICTs in the determinants of obesity and overweight is needed, in order to understand and account for the regional variation in adolescent prevalence. The inter-country variation may be indicative of different stages of the epidemiological transition; in islands where prevalence is lower, there may be a potential rise in obesity to come. For PICTs continuing to face the burden of infectious disease and under-nutrition, alongside increasing risks of overweight and obesity, an integrated approach to improve young people’s health and nutrition, focusing on healthy growth, is invaluable [64, 65].
To comprehensively and effectively tackle the NCD crisis, all sectors and agencies must be engaged. The Pacific NCD Road Map clearly describes the synergistic roles and responsibilities of different Ministries in tackling the NCD crisis, including the Prime Minister’s Office, Ministries of Trade, Finance, Agriculture, Fisheries, Customs and Excise, Education and Communications [66]. Furthermore, considering the influence that development organisations exert on the determinants of health, inter-agency coordination and harmonisation of such action is vital. The Pacific NCD Partnership, which brings together multiple agencies in the region, has recently been established to achieve this objective [67].
Conclusion
Immediate action on obesity in the Pacific is imperative. Community based initiatives and population health approaches need to be sufficiently supported by national leadership, sustained funding and strengthened surveillance systems for monitoring the prevalence of obesity and its determinants, in addition to the inequalities within [63]. Both national and regional action are necessary to prevent NCDs from overwhelming health systems and jeopardising sustainable development in the islands. Such concerted efforts will be instrumental in preventing NCDs, including obesity and its consequences, and will enable PICTs to realise the vision of Healthy Islands [2].
Acknowledgements
We are grateful to Dr Colin Tukuitonga and Dr Paula Vivili who contributed to the concept for this article. We also thank Dr Yvan Souarès for his guidance with this work, and Dr Terry Quirke for review of a first version of this article. We gratefully acknowledge the contribution of national health staff in the Pacific who undertook the surveys that were used to inform this paper. We also appreciate the contribution of the World Health Organization and the Centers for Disease Control and Prevention to this process.
Footnotes
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
TK and DH contributed to the concept, interpreted data and drafted the manuscript. NG contributed to acquisition and interpretation of data. JM, NG, OM, JP, AR and PW revised the study design, contributed to interpretation of data, and provided critical review and revision of the manuscript. All authors read and approved the final manuscript.
Contributor Information
Tara Kessaram, Phone: +687 262000, Email: tarakessaram@gmail.com.
Jeanie McKenzie, Email: jeanie.mckenzie@hotmail.com.
Natalie Girin, Email: natalieg@spc.int.
Onofre Edwin A. Merilles, Jr., Email: extjojom@spc.int
Jessica Pullar, Email: jessicap@spc.int.
Adam Roth, Email: adamr@spc.int.
Paul White, Email: paulw@spc.int.
Damian Hoy, Email: damianh@spc.int.
References
- 1.Déclaration de Tahiti Nui – Tahiti Nui Declaration (revised November 2011), Noumea, New Caledonia. Secretariat of the Pacific Community. 2012. http://www.spc.int/images/publications/ef/Corporate/ef-tahiti-nui-declaration.pdf. Accessed 3 February 2015.
- 2.World Health Organization. Yanuca Island Declaration, Yanuca Island, Fiji. World Health Organization. 1995. http://www.pihoa.org/fullsite/newsroom/wp-content/uploads/downloads/2012/09/WPR_RC46_INF_DOC1.pdf. Accessed 3 February 2015.
- 3.Pacific Islands Forum Secretariat. Forty-Second Pacific Islands Forum Communique. September 7–8 2011, Auckland, New Zealand. 2011. http://www.forumsec.org/pages.cfm/newsroom/documents-publications/forum-communiques. Accessed 3 February 2015.
- 4.Hoy D, Roth A, Viney K, Souares Y, Lopez A. Findings and implications of the Global Burden of Disease 2010 study for the Pacific Islands. Prev Chronic Dis. 2014;11:130344. doi: 10.5888/pcd11.130344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hawkes C. Uneven dietary development: linking the policies and processes of globalization with the nutrition transition, obesity and diet-related chronic diseases. Global Health. 2006;2(1):4. doi: 10.1186/1744-8603-2-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Asian Development Bank. The state of Pacific towns and cities: Urbanization in ADB’s Pacific developing member countries. Mandaluyong City, Philippines: Asian Development Bank; 2012. http://www.adb.org/sites/default/files/publication/29765/state-pacific-towns-cities.pdf. Accessed 4 March 2015.
- 7.Thow AM, Heywood P, Schultz J, Quested C, Jan S, Colagiuri S. Trade and the nutrition transition: strengthening policy for health in the Pacific. Ecol Food Nutr. 2011;50:18–42. doi: 10.1080/03670244.2010.524104. [DOI] [PubMed] [Google Scholar]
- 8.Dancause KN, Dehuff C, Soloway LE, Vilar M, Chan C, Wilson M, et al. Behavioral changes associated with economic development in the South Pacific: health transition in Vanuatu. Am J Hum Biol. 2011;23:366–376. doi: 10.1002/ajhb.21146. [DOI] [PubMed] [Google Scholar]
- 9.Saweri W. The rocky road from roots to rice: a review of the changing food and nutrition situation in Papua New Guinea. P N G Med J. 2001;44:151–163. [PubMed] [Google Scholar]
- 10.Hughes RG, Lawrence M. Globalisation, food and health in Pacific Island countries. Asia Pac J Clin Nutr. 2005;14(4):298–306. [PubMed] [Google Scholar]
- 11.Seiden A, Hawley NL, Schulz D, Raifman S, McGarvey ST. Long‐term trends in food availability, food prices, and obesity in Samoa. Am J Hum Biol. 2012;24:286–295. doi: 10.1002/ajhb.22237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Corsi A, Englberger L, Flores R, Lorens A, Fitzgerald MH. A participatory assessment of dietary patterns and food behavior in Pohnpei, Federated States of Micronesia. Asia Pac J Clin Nutr. 2008;17(2):309–316. [PubMed] [Google Scholar]
- 13.Evans M, Sinclair RC, Fusimalohi C, Liava’a V. Globalization, diet, and health: an example from Tonga. Bull World Health Organ. 2001;79:856–862. [PMC free article] [PubMed] [Google Scholar]
- 14.Bauman A, Ma G, Cuevas F, Omar Z, Waqanivalu T, Phongsavan P, et al. Cross-national comparisons of socioeconomic differences in the prevalence of leisure-time and occupational physical activity, and active commuting in six Asia-Pacific countries. J Epidemiol Community Health. 2001;65(1):35–43. doi: 10.1136/jech.2008.086710. [DOI] [PubMed] [Google Scholar]
- 15.Reilly JJ, Methven E, McDowell ZC, Hacking B, Alexander D, Stewart L, et al. Health consequences of obesity. Arch Dis Child. 2003;88:748–752. doi: 10.1136/adc.88.9.748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Smith SM, Sumar B, Dixon KA. Musculoskeletal pain in overweight and obese children. Int J Obes. 2014;38:11–15. doi: 10.1038/ijo.2013.187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Reilly JJ, Kelly J. Long-term impact of overweight and obesity in childhood and adolescence on morbidity and premature mortality in adulthood: systematic review. Int J Obes. 2010;35:891–898. doi: 10.1038/ijo.2010.222. [DOI] [PubMed] [Google Scholar]
- 18.Kessaram T, McKenzie J, Girin N, et al. Noncommunicable diseases and risk factors in adult populations of several Pacific Islands: results from the WHO STEPwise approach to surveillance. Aust N Z J Public Health. 2015 doi: 10.1111/1753-6405.12398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.World Health Organization . Global action plan for the prevention and control of noncommunicable diseases 2013–2020. Geneva, Switzerland: WHO; 2013. [Google Scholar]
- 20.Secretariat of the Pacific Community. National Minimum Development Indicators. Pacific Regional Information System, Statistics for Development, SPC. http://www.spc.int/nmdi/. Accessed 23 January 2015.
- 21.World Health Organization. Chronic diseases and health promotion. Global School-Based Student Health Survey. WHO; 2014. http://www.who.int/chp/gshs/en/. Accessed 3 February 2015.
- 22.Centers for Disease Control and Prevention. 1991–2013 High School Youth Risk Behavior Survey Data.http://nccd.cdc.gov/youthonline/. Accessed 26 January 2015.
- 23.Centers for Disease Control and Prevention and World Health Organization . Part 6 Preparing for the Survey. 2014. [Google Scholar]
- 24.Centers for Disease Control and Prevention and World Health Organization. 2013 GSHS Data User’s Guide. http://www.cdc.gov/gshs/pdf/gshs-data-users-guide.pdf. Accessed 26 January 2015.
- 25.Ministry of Health, Cook Islands. Global School-based Student Health Survey 2011 Fact Sheet. http://www.who.int/chp/gshs/factsheets/en/. Accessed 4 June 2014.
- 26.Ministry of Health, Fiji. Global School-based Student Health Survey 2010 Fact Sheet. http://www.who.int/chp/gshs/factsheets/en/. Accessed 4 June 2014.
- 27.Ministry of Health and Medical Services, Republic of Kiribati. Global School-based Student Health Survey 2011 Fact Sheet. http://www.who.int/chp/gshs/factsheets/en/. Accessed 4 June 2014.
- 28.Healthy Island Promotion Centre, Nauru. Global School-based Student Health Survey 2011 Fact Sheet. http://www.who.int/chp/gshs/factsheets/en/. Accessed 4 June 2014.
- 29.Niue. Global School-based Student Health Survey 2010 Fact Sheet. http://www.who.int/chp/gshs/factsheets/en/. Accessed 4 June 2014.
- 30.Ministry of Health, Samoa. Global School-based Student Health Survey 2011 Fact Sheet. http://www.who.int/chp/gshs/factsheets/en/. Accessed 4 June 2014.
- 31.Ministry of Education and Ministry of Health and Medical Services, Solomon Islands. Global School-based Student Health Survey 2011 Fact Sheet. http://www.who.int/chp/gshs/factsheets/en/. Accessed 4 June 2014.
- 32.Ministry of Health, Tonga. Global School-based Student Health Survey 2010 Fact Sheet. http://www.who.int/chp/gshs/factsheets/en/. Accessed 4 June 2014.
- 33.Ministry of Health, Tuvalu. Global School-based Student Health Survey 2013 Fact Sheet. http://www.who.int/chp/gshs/factsheets/en/. Accessed 4 June 2014.
- 34.Ministry of Health, Vanuatu. Global School-based Student Health Survey 2011 Fact Sheet. http://www.who.int/chp/gshs/factsheets/en/. Accessed 4 June 2014.
- 35.Centers for Disease Control and Prevention Methodology of the youth risk behavior surveillance system - 2013. MMWR. 2013;62:1. [Google Scholar]
- 36.Lippe J, Brener N, Kann L, Kinchen S, Harris W, McManus T, et al. Youth risk behavior surveillance - pacific island united states territories, 2007. MMWR Surveill Summ. 2008;57(12):28–56. [PubMed] [Google Scholar]
- 37.World Health Organization. Global Strategy on Diet Physical Activity and Health. What is overweight and obesity? http://www.who.int/dietphysicalactivity/childhood_what/en/. Accessed 24 February 2015.
- 38.World Health Organization. WHO Reference 2007. Growth reference data 5–19 years. http://www.who.int/growthref/en/. Accessed 3 February 2015.
- 39.Centers for Disease Control and Prevention. CDC Growth Charts 2000. http://www.cdc.gov/growthcharts/cdc_charts.htm. Accessed 3 February 2015.
- 40.Janssen I, LeBlanc AG. Systematic review of the health benefits of physical activity and fitness in school-aged children and youth. Int J Behav Nutr Phys Act. 2010;7:40. doi: 10.1186/1479-5868-7-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.World Health Organization . Global recommendations on physical activity for health. Geneva, Switzerland: World Health Organization; 2010. [PubMed] [Google Scholar]
- 42.Hu FB. Resolved: there is sufficient scientific evidence that decreasing sugar‐sweetened beverage consumption will reduce the prevalence of obesity and obesity‐related diseases. Obes Rev. 2013;14(8):606–619. doi: 10.1111/obr.12040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.World Health Organization . Guideline: sugars intake for adults and children. Gevena, Switzerland: World Health Organization; 2015. [PubMed] [Google Scholar]
- 44.Swinburn BA, Sacks G, Hall KD, McPherson K, Finegood DT, Moodie ML, et al. The global obesity pandemic: shaped by global drivers and local environments. Lancet. 2011;378(9793):804–814. doi: 10.1016/S0140-6736(11)60813-1. [DOI] [PubMed] [Google Scholar]
- 45.Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384:766–781. doi: 10.1016/S0140-6736(14)60460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Agence sanitaire et sociale de la Nouvelle Calédonie. Overweight and obesity in New Caledonian children-results report. 2014. http://www.ass.nc.
- 47.Daigre JL, Atallah A, Boisson JL, Jean-Baptiste G, Kangambega P, Chevalier H, et al. The prevalence of overweight and obesity, and distribution of waist circumference, in adults and children in the French Overseas Territories: the PODIUM survey. Diabetes Metab. 2012;38:404–411. doi: 10.1016/j.diabet.2012.03.008. [DOI] [PubMed] [Google Scholar]
- 48.Guthold R, Cowan MJ, Autenrieth CS, Kann L, Riley LM. Physical activity and sedentary behavior among schoolchildren: a 34-country comparison. J Paediatr. 2010;157:43–49. doi: 10.1016/j.jpeds.2010.01.019. [DOI] [PubMed] [Google Scholar]
- 49.World Health Organization Regional Office for the Eastern Mediterranean. Health education and promotion. Multi country comparisons - GSHS. http://www.emro.who.int/health-education/global-student-health-survey/multi-country-comparisons-gshs.html. Accessed 3 February 2015.
- 50.Brener ND, Mcmanus T, Galuska DA, Lowry R, Wechsler H. Reliability and validity of self-reported height and weight among high school students. J Adolesc Health. 2003;32:281–287. doi: 10.1016/S1054-139X(02)00708-5. [DOI] [PubMed] [Google Scholar]
- 51.Becker AE, Roberts AL, Perloe A, Bainivualiku A, Richards LK, Gilman SE, et al. Youth health-risk behavior assessment in Fiji: The reliability of Global School-based Student Health Survey content adapted for ethnic Fijian girls. Ethn Health. 2010;15:181–197. doi: 10.1080/13557851003615552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Mushtaq MU, Gull S, Mushtaq K, Abdullah HM, Khurshid U, Shahid U, et al. Height, weight and BMI percentiles and nutritional status relative to the international growth references among Pakistani school-aged children. BMC Paed. 2012;12(1):31. doi: 10.1186/1471-2431-12-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Waqa G, Mavoa H. Sociocultural factors influencing the food choices of 16–18 year-old Indigenous Fijian females at school. Pac Health Dialog. 2006;13:57–64. [PubMed] [Google Scholar]
- 54.Cacavas K, Mavoa H, Kremer P, Malakellis M, Fotu K, Swinburn B, et al. Tongan adolescents’ eating patterns: opportunities for intervention. Asia Pac J Public Health. 2011;23:24–33. doi: 10.1177/1010539510390781. [DOI] [PubMed] [Google Scholar]
- 55.Tuagalu C. Young People’s perceptions and experiences of physical activity in Apia. Samoa Pac Health Dialog. 2011;17:55–64. [PubMed] [Google Scholar]
- 56.Mavoa H, McCabe MP. Sociocultural factors relating to Tongans’ and Indigenous Fijians’ patterns of eating, physical activity and body size. Asia Pac J Clin Nutr. 2008;17(3):375–384. [PubMed] [Google Scholar]
- 57.McCabe MP, Mavoa H, Ricciardelli LA, Schultz JT, Waqa G, Fotu KF. Socio‐cultural agents and their impact on body image and body change strategies among adolescents in Fiji, Tonga, Tongans in New Zealand and Australia. Obes Rev. 2011;12(s2):61–67. doi: 10.1111/j.1467-789X.2011.00922.x. [DOI] [PubMed] [Google Scholar]
- 58.Thow AM, Quested C, Juventin L, Kun R, Kahn AN, Swinburn B. Taxing soft drinks in the Pacific: implementation lessons for improving health. Health Promot Int. 2011;26(1):55–64. doi: 10.1093/heapro/daq057. [DOI] [PubMed] [Google Scholar]
- 59.Pak N, McDonald AM, McKenzie J, Tukuitonga C. Soft drink consumption in Pacific Island countries and territories: a review of trade data. Pacific Health Dialog. 2014;20(1):59–66. [PubMed] [Google Scholar]
- 60.Snowdon W, Thow AM. Trade policy and obesity prevention: challenges and innovation in the Pacific Islands. Obes Rev. 2013;14(S2):150–158. doi: 10.1111/obr.12090. [DOI] [PubMed] [Google Scholar]
- 61.World Health Organization . Set of recommendations on the marketing of foods and non-alcoholic beverages to children. Geneva: Switzerland; 2010. [Google Scholar]
- 62.World Health Organization . A guide for population-based approaches to increasing levels of physical activity: implementation of the WHO global strategy on diet, physical activity and health. Geneva, Switzerland: World Health Organization; 2007. [Google Scholar]
- 63.World Health Organization . Population-based approaches to childhood obesity prevention. Geneva, Switzerland: World Health Organization; 2012. [Google Scholar]
- 64.Dancause K, Vilar M, Chan C, DeHuff C, Wilson M, Soloway LE, et al. Patterns of childhood and adolescent overweight and obesity during health transition in Vanuatu. Public Health Nutr. 2012;15:158–166. doi: 10.1017/S1368980011001662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Lobstein T, Jackson-Leach R, Moodie ML, Hall KD, Gortmaker SL, Swinburn BA, et al. Child and adolescent obesity: part of a bigger picture. Lancet. 2015 doi: 10.1016/S0140-6736(14)61746-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.World Bank. Non-Communicable Disease (NCD) Roadmap Report. Washington, DC: World Bank Group; 2014. http://documents.worldbank.org/curated/en/2014/07/19778739/non-communicable-disease-ncd-roadmap-report. Accessed 3 February 2015.
- 67.Pacific NCD Partnership for a Multi-sector Approach to Prevent and Control NCDs (Pacific NCD Partnership). UN Conference on Small Island Developing States, Apia, Samoa 1–4 September 2014. United Nations Department of Economic and Social Affairs, Division for Sustainable Development; 2014. http://www.sids2014.org/index.php?page=view&type=1006&nr=2759&menu=1507. Accessed 3 February 2015.


