Abstract
Developmental theories of borderline personality disorder (BPD) propose that harsh, invalidating parenting of a child with poor self-control and heightened negative emotionality often leads to a coercive cycle of parent-child transactions that increase risk for BPD symptoms such as emotion dysregulation. Although parenting practices and child temperament have previously been linked with BPD, less is known about the prospective influences of caregiver and child characteristics. Using annual longitudinal data from the Pittsburgh Girls Study (n = 2450), our study examined how reciprocal influences among harsh parenting, self-control, and negative emotionality between ages 5 and 14 predicted the development of BPD symptoms in adolescent girls ages 14 to 17. Consistent with developmental theories, we found that harsh punishment, poor self-control, and negative emotionality predicted BPD symptom severity at age 14. Only worsening self-control between ages 12 and 14, however, predicted growth in BPD symptoms from 14 to 17. Furthermore, the effects of harsh punishment and poor self-control on age 14 BPD symptoms were partially mediated by their earlier reciprocal effects on each other between ages 5 and 14. Our findings underscore the need to address both child and parental contributions to dysfunctional transactions in order to stem the development of BPD symptoms. Moreover, problems with self-regulation in early adolescence may indicate heightened risk for subsequent BPD. Altogether, these results increase our understanding of developmental trajectories associated with BPD symptoms in adolescent girls.
Keywords: Borderline personality disorder, developmental psychopathology, harsh parenting, self-control
Borderline personality disorder (BPD) is a debilitating mental disorder characterized by emotion dysregulation, interpersonal dysfunction, impulsive behavior, poor identity, and self-injurious and suicidal behavior (American Psychiatric Association, 2013). In addition to the subjective misery and poor quality of life that typify BPD (Cramer, Torgersen, & Kringlen, 2006), patients with BPD often require long-term intensive treatment (Zanarini, Frankenburg, Hennen, & Silk, 2004), and mental health treatment costs are enormous (Bateman & Fonagy, 2003; Bender et al., 2001). Retrospective reports of adult patients suggest that the onset of BPD symptoms typically occurs in late adolescence (Clarkin, Levy, Lenzenweger, & Kernberg, 2004; Zanarini, Frankenburg, Khera, & Bleichmar, 2001). Furthermore, studies of adolescents in the community have estimated that BPD affects 0.9% to 3% of youth, consistent with adult prevalence rates (Bernstein et al., 1993; Lenzenweger, Lane, Loranger, & Kessler, 2007; Lewinsohn, Rohde, Seeley, & Klein, 1997).
Although there has been some hesitancy to diagnose BPD in adolescents, perhaps because of the maturation of personality that occurs during this period (Terr & Kernberg, 1990), a growing body of research has demonstrated the reliability and validity of the BPD construct in youth (Miller, Muehlenkamp, & Jacobson, 2008; Stepp, Pilkonis, Hipwell, Loeber, & Stouthamer-Loeber, 2010). Semi-structured interviews based on the DSM-IV/5 criteria can be used to diagnose BPD in youth with good inter-rater reliability that is comparable to adult studies (Becker et al., 1999; Blais, Hilsenroth, & Fowler, 1999). Mean-level and rank-order stability of BPD symptoms are comparable across adolescents and adults (Chanen et al., 2004; Crawford, Cohen, & Brook, 2001; Lenzenweger, 1999), although symptoms remit in many individuals over time (Gunderson et al., 2011). Symptoms of BPD (and more broadly, Cluster B PDs) are frequently stable from adolescence into early adulthood, often exceeding the stability of Axis I symptom dimensions (Crawford et al., 2001), which suggests that the presence of BPD symptoms in youth often portends BPD-related impairment in adulthood. Moreover, BPD symptoms in youth are associated with significant functional impairment (e.g., risky sexual behavior; Chanen, Jovev, & Jackson, 2007) and increased prospective risk for adult psychopathology (Johnson, Cohen, Skodol, et al., 1999).
Despite the accumulating evidence for the reliability, validity, and public health significance of BPD symptoms in youth, less is known about its etiology. Preliminary evidence from developmental studies of BPD have identified maltreatment, harsh discipline, executive dysfunction, family history of psychopathology, and temperament as potential etiological factors (Belsky et al., 2012; Johnson, Cohen, Chen, Kasen, & Brook, 2006; Livesley & Jang, 2008; Zelkowitz, Paris, Guzder, & Feldman, 2001), but there have been few prospective studies (Stepp, Burke, Hipwell, & Loeber, 2012). The biosocial theory of BPD proposes that impulsivity and emotional reactivity are biologically based dimensions of temperament that negatively interact with invalidating, harsh, or coercive parenting behaviors to produce emotion dysregulation typical of BPD (Crowell, Beauchaine, & Linehan, 2009; Linehan, 1993). More specifically, parent-child interactions characterized by emotional invalidation, poor modeling of emotion expression, and punishment of emotion-related behaviors may lead to emotional sensitivity, as well as intense and rapidly shifting emotions in a temperamentally vulnerable child (Beauchaine, Klein, Crowell, Derbidge, & Gatzke-Kopp, 2009; Hinshaw et al., 2012). Indeed, a recent study found that during more aversive periods of a mother-child conflict discussion, depressed adolescents became both physiologically and behaviorally dysregulated, providing initial support of parent-child transactions associated with emotion dysregulation (Crowell et al., 2014).
The emergence of BPD during adolescence occurs in the broader context of a developmental transition to adult social roles and responsibilities between ages 12 and 17 (Crone & Dahl, 2012; Spear, 2000). Normative increases in emotional intensity and mood lability occur during this period, which reflect, in part, neuroendocrine changes related to sexual maturation (Dahl, 2004; Steinberg et al., 2006). Socially, adolescents typically increase their valuation of peer relationships, develop greater psychological distance from parents, and renegotiate boundaries and responsibilities in family relationships (Fuligni & Eccles, 1993; Steinberg, 2001). These changes in the social and affective landscape place increased demands on self-regulatory processes, particularly emotion regulation (Posner & Rothbart, 2000).
Adolescents who experience intense negative emotions that overwhelm their ability to regulate such feelings are likely at the greatest risk for developing BPD symptoms. Because of the heightened emphasis on peer social standing, behaviors associated with emotion dysregulation (e.g., angry outbursts) expressed during adolescence may be particularly costly, evoking rejection responses from peers and further exacerbating social dysfunction that is characteristic of BPD (Crowell et al., 2009; Hill et al., 2008). Moreover, increases in suicidal, self-injurious, and impulsive behaviors (e.g., substance use) that accompany emotion dysregulation often represent attempts to regulate negative emotions (Brown, Comtois, & Linehan, 2002). Thus, the emergence of BPD during adolescence likely reflects a mismatch among social competence demands, increased emotional intensity, and immature self-control (Crowell et al., 2009; Linehan, 1993).
Our study sought to test how reciprocal interactions among negative parenting, self-regulation, and negative emotionality between ages 5 and 14 prospectively predict the development of BPD symptoms in adolescent girls ages 14 to 17. Consistent with previous research on impulsive temperament in BPD (Posner et al., 2003), we were specifically interested in the deliberate, effortful suppression of immediate/dominant responses on behalf of achieving broader goals, which has been termed effortful control (Rothbart, Ahadi, & Evans, 2000). Impulsive behaviors in BPD often reflect failures to inhibit maladaptive responses in the face of intense distress (e.g., self-injurious behavior after interpersonal rejection), rather than motor hyperactivity or inattentiveness more characteristic of attention deficit hyperactivity disorder. Furthermore, impulsive behaviors in BPD often occur in the context of interpersonal relationships (Koenigsberg et al., 2001), and the manifestation of impulsive temperament depends on context (e.g., school-versus interpersonal-related impulsivity; Tsukayama, Duckworth, & Kim, 2013) and environmental influence, including parenting style (Hinshaw, 2002). Thus, our study focused on poor self-control defined by failures to suppress immediate negative responses in interpersonal interactions in order to engage in positive social behaviors. Examples of poor self-control include failures to inhibit anger or responding defensively when interacting with peers and caregivers. The self-control literature includes a range of definitions such as performance on delay of gratification and executive function tasks (for a review, see Duckworth & Kern, 2011), and self-control on non-social tasks may be affected in BPD (Fertuck, Lenzenweger, Clarkin, Hoermann, & Stanley, 2006; Lawrence, Allen, & Chanen, 2010). Nevertheless, we focus here specifically on inhibitory failures in social interactions (e.g., escalating arguments with a parent) because these are most likely to have evocative effects on parenting behavior and be associated with reinforcement of emotional lability thought to lead to the development of emotion dysregulation in BPD (Crowell et al., 2009).
Several parenting behaviors have been associated with elevated risk for personality dysfunction, including harsh punishment, inconsistent discipline, neglect, low affection, and physical and sexual abuse (Johnson, Cohen, Brown, Smailes, & Bernstein, 1999; Johnson et al., 2006; Widom, Czaja, & Paris, 2009; cf. Bornovalova et al., 2013). We focused specifically on harsh punishment as defined by psychological aggression (e.g., insulting or swearing at the child) and spanking because such parenting of a child with poor self-control may lead to a cycle of coercive parent-child transactions that exacerbate difficulties with aggression and disrupt the normative development of self-regulation (Patterson, DeBaryshe, & Ramsey, 1989). Our operationalization also aligns with accounts of how emotionally negative parenting of a highly reactive child promotes the development of vacillating, intense emotions (Scaramella & Leve, 2004), which are characteristic of BPD (Crowell et al., 2009). That said, an emotionally invalidating environment is likely composed of a combination of maladaptive parenting behaviors and the risk of BPD may increase as the level of parenting dysfunction increases (Johnson et al., 2006; Winsper, Zanarini, & Wolke, 2012).
We predicted that there would be reciprocal prospective influences of harsh punishment on poor self-control and vice versa between ages 5 and 14. Furthermore, we hypothesized that harsh punishment and poor self-control in childhood to early adolescence would predict both the severity of BPD symptoms at age 14 and their rate of development between ages 14 and 17. We expected that the effects of harsh punishment and poor self-control on BPD would be mediated in part by their reciprocal influences on each other. More specifically, we predicted that the relationship between harsh punishment in childhood and BPD symptoms in adolescence would be partially mediated by the prospective influence of harsh punishment on poor self-control. Likewise, we anticipated that the effect of poor self-control on adolescent BPD symptoms would be partially mediated by its prospective influence on harsh punishment. We hypothesized that negative emotionality in childhood would predict the severity of BPD symptoms at age 14. Consistent with the biosocial theory (Crowell et al., 2009), we also anticipated that childhood negative emotionality would prospectively predict greater harsh punishment (i.e., an evocative effect of child temperament on parenting behavior), and that harsh punishment would prospectively predict poor self-control. Finally, we predicted that the relationship between childhood negative emotionality and adolescent BPD symptoms would be mediated by prospective influences of negative emotionality on poor self-control and harsh punishment. As a secondary aim, we also compared whether caregiver-versus child-reported harsh punishment and poor self-control between ages 10 and 14 were differentially predictive of BPD symptoms in adolescence.
Methods
Participants
The Pittsburgh Girls Study (PGS) consists of 2,450 girls initially assessed at ages 5–8 who have been followed annually using an accelerated longitudinal cohort design. To identify the study sample, low income neighborhoods were oversampled, such that all Pittsburgh neighborhoods in which at least 25% of families were living at or below poverty level were included and a random sample of 50% of households in all other neighborhoods was included (see Hipwell et al., 2002 for details on study design and recruitment). The analyses reported here focus on symptoms of BPD assessed between ages 14 and 17, and data for 2,228 girls with at least one assessment of borderline symptoms were available (90.9% of the original sample). Girls included in our analyses did not differ from those excluded on minority race, family poverty, or single parenthood in wave 1. Data regarding self-control, harsh punishment, negative emotionality, borderline symptoms, and other predictors of interest were available for virtually all participants (M missingness = 4.5%, range = .05% – 7.9%). A single item reflecting identity disturbance had greater missingness at ages 14 (52%) and 15 (29%) than other BPD features because this item was added to the protocol after some participants had already completed the assessment of BPD symptoms.
Data Collection
Separate in-home interviews for both the girl and caregiver were conducted annually by trained interviewers using a laptop computer. At each assessment, girls and caregivers reported on parenting practices, girls’ characteristics, and caregiver psychopathology in the past year. The assessment of self-reported BPD symptoms began at age 14 for all girls. All study procedures were approved by the University of Pittsburgh Institutional Review Board. Families were compensated for their participation.
Measures
Harsh punishment
Harsh punishment was assessed using caregiver and child reports on the Conflict Tactics Scale: Parent-Child version (CTSPC; Straus et al., 1998). Items referring to the primary caregiver were used and were scored on a 3-point scale (1=never, 2=sometimes, 3=often). Five items from the psychological aggression subscale (e.g. from caregiver-report, In the past year, if your daughter did something that she is not allowed to do or something that you didn’t like, how often did you shout, yell, or scream at her?) were combined with a single item on spanking to produce the harsh punishment construct. Satisfactory discriminant and construct validity has been previously reported for the psychological aggression scale (Straus et al., 1998). In the current sample, the average CTSPC internal consistency was acceptable for a brief scale (Nunnally & Bernstein, 1994), but may have attenuated the strength of its relationship with other variables (Schmitt, 1996). For caregiver-report, average internal consistency was α = 0.74, with values ranging from α = 0.69 (wave 1) to α =0.77 (age 13). For child-report the average internal consistency was α = 0.75, with values ranging from α = 0.72 (Wave 1) to α = 0.77 (age 14).
Negative Emotionality
Child negative emotionality was measured by caregiver report at the first wave of data collection and at age 11 using the Emotionality, Activity, and Sociability Temperament Survey (Buss & Plomin, 1984). The negative emotionality subscale consists of five items (e.g., “She cries easily”) scored using a 5-point scale (1 = a little, 5 = a lot). This subscale has demonstrated construct validity in comparisons of girls with and without depression in a community sample (Goodyer, Ashby, Altham, Vize, & Cooper, 1993). In our study, the internal consistency coefficient for the emotionality scale at wave 1 was α = 0.82 and α = 0.81 at the age 11 assessment.
Poor Self-Control
Poor self-control was measured using caregiver and child reports on the self-control subscale of the Social Skills Rating Scale (Gresham & Elliott, 1990) between the age 10 and age 14 assessments. Caregivers also rated self-control at wave 1 (ages 5–8). The self-control subscale consists of 10 items (e.g., “Controls temper when arguing with other children”) rated on a 3-point scale (2 = never, 1 = sometimes, 0 = very often). Note that this subscale was scored such that higher values reflected poorer self-control. In our study, the average internal consistency coefficient for the child-report self-control subscale was α = 0.77, with values ranging from α = 0.74 (age 11) to α = 0.80 (age 13). The average internal consistency for the caregiver-report self-control subscale was α = 0.82, with values ranging from α = 0.80 (age 10) to α = 0.83 (age 14).
Poverty
Poverty was measured by whether the caregiver was receiving public assistance (0 = no, 1 = yes) at the first wave of data collection (between ages 5 and 8). Consistent with the oversampling of low-income neighborhoods, 40.0% of families were receiving public assistance at the first wave.
Race
Minority race was included as a binary covariate in structural equation models to control for racial differences. Of participants included in our analyses, 60.2% self-identified a primary identification with a minority race, whereas 39.2% reported a primary identification as Caucasian.
Borderline Personality Symptoms
Child-reported symptoms of BPD were assessed using the International Personality Disorder Examination – Screen (IPDE-S; Lenzenweger, Loranger, Korfine, & Neff, 1997), a nine-item questionnaire of the DSM-IV BPD diagnostic criteria. An additional item was added in Wave 9 assessing identity disturbance to increase the content validity of the measure (Feelings about myself change frequently). One item from the IPDE-S, I show my feelings for all to see, was frequently endorsed (44% – 49%) and had very low point-biserial correlations with the total score, r = −.03 – .06. Thus, this item was dropped from the scale, leaving nine items that demonstrated acceptable internal consistency at each age, Cronbach’s α = .82 – .86. Dropping this item did not detract from the content validity of the scale because additional items about anger and moodiness were among the items retained.
Although the IPDE-S was originally developed for adults, its concurrent validity, sensitivity, and specificity compared to BPD clinical diagnosis were found to be adequate in a sample of youth (Chanen et al., 2008), and its diagnostic efficiency compared favorably with substantially longer self-report measures of BPD symptoms. The upper quartile of our sample had an average IPDE-S score of 4, which is in the clinically significant range compared to previous reports (Smith, Muir, & Blackwood, 2005). In a smaller sub-study of BPD features at age 16 in the PGS sample, IPDE-S BPD symptom scores were significantly correlated with clinician-rated BPD symptoms assessed using the Structured Interview for DSM-IV Personality (Pfohl, Blum, & Zimmerman, 1997), r(111) = 0.6, p < .001, which is comparable with previous reports of convergence between self-report and clinician-assessed BPD features (Hopwood et al., 2008).
Results
Analytic Approach
In order to test our hypotheses, we used a series of latent curve models (LCMs; Bollen & Curran, 2005) to characterize the level and rate of change in poor self-control, harsh punishment, and BPD symptoms. Distributional statistics for all variables considered are reported in Table 1, and correlations among variables are reported in Table 2. Prior to testing a larger structural equation model representing reciprocal influences of poor self-control and harsh punishment on BPD symptoms, we tested the measurement and growth models associated with each component of the larger analysis to ensure that there were no serious misspecifications in each component (Tomarken & Waller, 2003; cf. Heene, Hilbert, Freudenthaler, & Bühner, 2012). Models were fit using the mean-and-variance-adjusted weighted least squares (WLSMV) estimator in Mplus 7.2 software (Muthén & Muthén, 2013), which was optimal for modeling the categorical BPD item data.1.
Table 1.
Descriptive statistics for variables included in longitudinal models.
| Variable | M | SD | Skewness | Kurtosis |
|---|---|---|---|---|
| Wave 1 Harsh Punishment | 9.45 | 1.85 | 0.45 | 0.15 |
| Wave 1 SSRS Self-Control | 7.54 | 3.31 | 0.11 | 0.03 |
| Wave 1 Negative Emotionality | 13.05 | 4.95 | 0.36 | −0.58 |
| Age 11 Negative Emotionality | 12.53 | 4.64 | 0.38 | −0.38 |
| Age 10 Poor Self-Control | 6.4 | 3.79 | 0.41 | −0.12 |
| Age 11 Poor Self-Control | 6.56 | 3.58 | 0.24 | −0.23 |
| Age 12 Poor Self-Control | 6.9 | 3.61 | 0.15 | −0.17 |
| Age 13 Poor Self-Control | 8.74 | 4.26 | 0.28 | −0.06 |
| Age 14 Poor Self-Control | 9.98 | 4.12 | 0.01 | −0.1 |
| Age 10 Harsh Punishment | 8.53 | 2.28 | 1.15 | 1.24 |
| Age 11 Harsh Punishment | 8.47 | 2.18 | 1.16 | 1.29 |
| Age 12 Harsh Punishment | 8.64 | 2.3 | 1.06 | 0.9 |
| Age 13 Harsh Punishment | 8.78 | 2.32 | 0.94 | 0.61 |
| Age 14 Harsh Punishment | 8.92 | 2.43 | 0.9 | 0.41 |
| Age 14 BPD symptoms (factor score) | 0.04 | 0.98 | 0.27 | −0.5 |
| Age 15 BPD symptoms (factor score) | 0.09 | 0.99 | 0.22 | −0.6 |
| Age 16 BPD symptoms (factor score) | −0.0007 | 1.05 | 0.23 | −0.52 |
| Age 17 BPD symptoms (factor score) | −0.14 | 1.04 | 0.3 | −0.44 |
| Age 14 IPDE-S BPD symptom total | 2.25 | 2.05 | 0.85 | 0.15 |
| Age 15 IPDE-S BPD symptom total | 2.29 | 2.04 | 0.79 | −0.11 |
| Age 16 IPDE-S BPD symptom total | 2.22 | 2.07 | 0.86 | 0.05 |
| Age 17 IPDE-S BPD symptom total | 2.02 | 2.01 | 0.98 | 0.4 |
Note. Wave 1 variables were rated by caregivers. Variables between ages 10 and 17 were rates by girls. BPD symptom factor scores were derived from the strict invariance confirmatory factor analysis described in the body of the manuscript. IPDE-S BPD symptom totals represent the sum of the 9 IPDE-S items included in reported analyses (range 0–9).
Table 2.
Bivariate correlations among variables included in longitudinal models.
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 - Minority Race (Yes/No) | 1.00 | |||||||||||||||||||
| 2 - Wave 1 Public Assistance (Yes/No) | 0.56 | 1.00 | ||||||||||||||||||
| 3 - Wave 1 Harsh Punishment | 0.33 | 0.25 | 1.00 | |||||||||||||||||
| 4 - Wave 1 Poor Self-Control | 0.17 | 0.27 | 0.29 | 1.00 | ||||||||||||||||
| 5 - Wave 1 Negative Emotionality | 0.04 | 0.11 | 0.22 | 0.37 | 1.00 | |||||||||||||||
| 6 - Age 11 Negative Emotionality | 0.04 | 0.10 | 0.17 | 0.30 | 0.49 | 1.00 | ||||||||||||||
| 7 - Age 10 Poor Self-Control | 0.19 | 0.13 | 0.09 | 0.17 | 0.05 | 0.09 | 1.00 | |||||||||||||
| 8 - Age 11 Poor Self-Control | 0.25 | 0.16 | 0.12 | 0.21 | 0.08 | 0.09 | 0.46 | 1.00 | ||||||||||||
| 9 - Age 12 Poor Self-Control | 0.18 | 0.12 | 0.14 | 0.23 | 0.12 | 0.14 | 0.39 | 0.46 | 1.00 | |||||||||||
| 10 - Age 13 Poor Self-Control | 0.06 | 0.10 | 0.04 | 0.12 | 0.02 | −0.03 | 0.11 | 0.15 | 0.20 | 1.00 | ||||||||||
| 11 - Age 14 Poor Self-Control | 0.01 | 0.02 | −0.01 | 0.05 | 0.00 | −0.04 | −0.02 | 0.00 | −0.01 | 0.42 | 1.00 | |||||||||
| 12 - Age 10 Harsh Punishment | 0.29 | 0.13 | 0.24 | 0.12 | 0.07 | 0.08 | 0.23 | 0.18 | 0.22 | 0.04 | 0.02 | 1.00 | ||||||||
| 13 - Age 11 Harsh Punishment | 0.38 | 0.14 | 0.27 | 0.14 | 0.09 | 0.09 | 0.20 | 0.24 | 0.25 | 0.08 | 0.02 | 0.56 | 1.00 | |||||||
| 14 - Age 12 Harsh Punishment | 0.35 | 0.16 | 0.25 | 0.18 | 0.06 | 0.07 | 0.20 | 0.24 | 0.34 | 0.11 | 0.02 | 0.47 | 0.57 | 1.00 | ||||||
| 15 - Age 13 Harsh Punishment | 0.33 | 0.13 | 0.26 | 0.15 | 0.05 | 0.12 | 0.16 | 0.21 | 0.27 | 0.11 | 0.02 | 0.41 | 0.50 | 0.59 | 1.00 | |||||
| 16 - Age 14 Harsh Punishment | 0.31 | 0.12 | 0.29 | 0.16 | 0.06 | 0.11 | 0.12 | 0.17 | 0.21 | 0.11 | 0.02 | 0.35 | 0.45 | 0.54 | 0.63 | 1.00 | ||||
| 17 - Age 14 BPD symptoms (factor score) | 0.20 | 0.13 | 0.19 | 0.21 | 0.16 | 0.19 | 0.17 | 0.20 | 0.32 | 0.10 | −0.03 | 0.19 | 0.25 | 0.27 | 0.31 | 0.38 | 1.00 | |||
| 18 - Age 15 BPD symptoms (factor score) | 0.24 | 0.15 | 0.20 | 0.21 | 0.15 | 0.20 | 0.19 | 0.21 | 0.32 | 0.11 | −0.02 | 0.21 | 0.25 | 0.29 | 0.31 | 0.37 | 0.88 | 1.00 | ||
| 19 - Age 16 BPD symptoms (factor score) | 0.24 | 0.16 | 0.21 | 0.21 | 0.15 | 0.20 | 0.18 | 0.20 | 0.30 | 0.11 | −0.01 | 0.23 | 0.26 | 0.29 | 0.33 | 0.37 | 0.83 | 0.92 | 1.00 | |
| 20 - Age 17 BPD symptoms (factor score) | 0.25 | 0.16 | 0.19 | 0.21 | 0.14 | 0.18 | 0.17 | 0.20 | 0.29 | 0.10 | −0.01 | 0.21 | 0.25 | 0.28 | 0.31 | 0.35 | 0.76 | 0.87 | 0.92 | 1.00 |
Note. Correlations |r| > .07 are statistically significant at p < .001.
Measurement and Longitudinal Change of BPD Symptoms (Ages 14–17)
An important issue in longitudinal developmental research is whether the measurement of a construct of interest is consistent across time (Widaman, Ferrer, & Conger, 2010). In order to test for measurement invariance of the BPD construct (measured by the IPDE-S) between ages 14 and 17, we first tested a relatively unrestricted configural invariance confirmatory factor analysis (CFA) model where factor loadings and thresholds were free to vary at each age and residual item variances were fixed to unity over time for identification (Millsap & Yun-Tein, 2004). In addition, residual covariances for each item were estimated over time to allow for unique item variability (Bollen & Curran, 2005). The configural model fit the data well: χ2(534) = 1203.98, CFI = .98, RMSEA=0.024 (90% CI = .022–.026). Allowing for a contemporaneous residual covariance between the mood fluctuations and anger items further enhanced model fit, Wald χ2(4) = 151.47, p < .0001, suggesting residual item variation attributable to negative affect.
When the 136-parameter configural model was constrained to enforce strict invariance (i.e., factor loadings and item thresholds were equated over time, while residual item variances remained fixed to unity), model fit remained excellent, χ2(578) = 1065.72, CFI = .98, RMSEA=0.019 (90% CI = .018–.021). A comparison of the configural and strict models suggested that the strict model fit was statistically worse, Wald χ2(48) = 71.24, p = .02, yet practical fit indices (CFI and RMSEA) were at least as good, and examination of model residuals did not suggest worse fit due to these constraints. In large samples, model comparison tests are often over-powered, identifying “significant” deviations from invariance that are of trivial substantive value (Widaman et al., 2010). Finally, we constrained residual covariances among items to be equal over time, representing that the similarity of items to one another was of similar magnitude regardless of the specific timing. This eliminated an additional 45 parameters while maintaining excellent fit, χ2(623) =1124.65, CFI = .98, RMSEA=0.019 (90% CI = .017–.021). Although the model difference test was significant, Wald χ2(45) = 68.02, p = .02, we retained the constrained model because none of the practical fit indices was degraded and the model was much more parsimonious (less than half as many parameters as the strict invariance model).
Altogether, our results corroborated that the latent structure of borderline personality symptoms between 14 and 17 was measurement invariant, which supported moving forward with additional models of BPD symptoms in adolescence, as well as predictors of these features. We next fit a second-order LCM (Hancock, Kuo, & Lawrence, 2001) to the symptom data to model the level and rate of change in BPD symptoms, where BPD was measured by a latent trait at each age. This model was adapted from the strict measurement invariance CFA such that all equality constraints on factor loadings, item thresholds, and item residual covariances were preserved, but two factors measuring initial level and linear change over time were estimated. The second-order LCM fit the data very well, χ2(628) = 1149.05, CFI = .98, RMSEA = 0.019 (90% CI = .018 – .021), suggesting that a linear model adequately captured the growth patterns in BPD symptoms during the adolescent period. There was a significant, if small, decrease in mean BPD symptoms between ages 14 and 17, B = −.02, p < .0001, as well as significant inter-individual variability both in the severity of BPD symptoms at age 14, Ψαα = .13, p < .0001, and the rate of change over time, Ψββ = .009, p < .0001. There was a negative association between BPD symptoms at age 14 and the rate of change in symptoms over time, r = −.23, p < .0001, indicating that individuals with the highest levels of symptoms at age 14 tended to experience the least change over adolescence.
Longitudinal Change in Self-Control and Harsh Punishment
Prior to characterizing the relationships among self-control, harsh punishment, and BPD symptoms, we first verified that the longitudinal models for self-control and harsh punishment adequately captured developmental patterns between ages 10 and 14. The linear LCM for child-reported harsh punishment fit the data well, χ2(10) = 40.96, CFI = .99, RMSEA = 0.037 (90% CI = .026 – .05). Child reports of harsh punishment increased significantly between ages 10 and 14, B = .11, p < .0001, and there was a significant negative relationship between level at age 10 and rate of change, r = −.35, p < .0001. The negative association between age 10 level and rate of change suggests that those with the lowest levels of harsh punishment at age 10 reported the greatest increases in harsh punishment between 10 and 14 (cf. Seltzer, Choi, & Thum, 2003). Variability in the level of harsh punishment and rate of change over time was also significant, Ψαα = 3.08, p < .0001 and Ψββ = .20, p < .0001, respectively.
A linear LCM for child-reported self-control did not adequately capture the pattern of change between ages 10 and 14, χ2(10) = 567.76, CFI = .61, RMSEA = 0.16. Exploration of the observed data and model residuals indicated that there was modest average growth in self-control problems between 10 and 12, but that these problems increased much more rapidly from 12 to 14, perhaps reflecting the transition to adolescence. To account for the variable pattern of change over this period, we fit a piecewise LCM with two linear slope components, one between ages 10 and 12, and the other between 12 and 14. This model fit the data well, χ2(6) = 23.56, CFI = .99, RMSEA = 0.04 (90% CI = .022 – .052). Growth in self-control problems was modest, but significant, between ages 10 and 12, B = .28, p < .0001, whereas there was much greater growth, on average, between ages 12 and 14, B = 1.55, p < .0001. The severity of self-control problems at age 10 was negatively correlated with growth in self-control problems, both from ages 10 to 12 (r = −.46, p < .0001) and from ages 12 to 14 (r = −.44, p < .0001). Inter-individual variability in the rate of change was significantly greater between 12 and 14, , than between 10 and 12, , p < .0001.
Next, we fit a parallel LCM for child-reported poor self-control and harsh punishment that built upon the univariate LCMs. This model allowed for covariation among the level and rate of change factors for both constructs, as well as residual item covariances at each age to account for age-specific variability not captured by the growth factors. This model fit the data well, χ2(30) = 88.05, CFI = .99, RMSEA = 0.03 (90% CI = .022 – .037). As the final step before testing the hypothesized etiological model of BPD, we added caregiver-reported poor self-control, harsh punishment, and negative emotionality from the first wave of data collection (spanning ages five to eight), as well as wave 1 poverty and race, as predictors of the self-control and harsh punishment LCM factors from 10 – 142. We also included age 11 negative emotionality as a predictor of change in poor self-control from ages 12 – 14. In this model, we also regressed linear slopes for harsh punishment and self-control on the intercept factors for both constructs. This step ensured that estimates of change in self-control and harsh punishment from 10 – 14 were independent of the initial level at age 10, aiding the interpretability of results linking initial levels of harsh punishment at age 10 with changes in self-control between 10 and 14 and vice versa (see also Seltzer et al., 2003).
Level and Rate of Change in Adolescent BPD Features Predicted by Harsh Punishment, Negative Emotionality, and Poor Self-Control
To test the prospective effects of harsh punishment, negative emotionality, and poor self-control on the level and rate of change in BPD symptoms in adolescence, we fit a structural equation model that combined the age 14–17 BPD second-order LCM and the parallel process age 10–14 LCM for harsh punishment and poor self-control, including the wave 1 predictors as above, as well as age 11 negative emotionality. The severity of BPD symptoms at age 14 and the change in BPD symptoms between ages 14 and 17 were regressed on age 10 – 14 harsh punishment and self-control intercept and slope factors, as well as wave 1 harsh punishment, self-control, negative emotionality, poverty, and race. As above, age 10–14 harsh punishment and self-control were regressed on wave 1 predictors. This model fit the data well, χ2(1242) = 2160.38, CFI = .98, RMSEA = 0.018 (90% CI = .017 – .019).
Direct predictors of BPD symptom severity at age 14
BPD symptoms at age 14 were significantly associated with the level of child-reported harsh punishment at age 10, as well as the rate of growth in harsh punishment between ages 10 and 14 (see Table 3). Both the level and rate of growth in poor self-control between ages 10 and 12 significantly predicted higher BPD symptom severity, whereas the rate of change in self-control between 12 and 14 was negatively associated with BPD symptoms. Finally, higher negative emotionality at age 11 was predictive of age 14 BPD symptoms. Altogether, these predictors accounted for 41.7% of the variance in age 14 borderline symptoms.
Table 3.
Standardized effects from the final structural equation model incorporating public assistance, minority race, harsh punishment, poor self-control, and negative emotionality as predictors of BPD symptoms
| Ages 5–8 | Age 10 | Ages 10–14 | Ages 14–17 | Std. β | S. E. | p |
|---|---|---|---|---|---|---|
| Wave 1 Public assistance → | Harsh punishment (Intercept) | −0.007 | 0.027 | 0.799 | ||
| Wave 1 Public assistance → | Poor self-control (Intercept) | 0.039 | 0.03 | 0.182 | ||
| Wave 1 Public assistance → | Negative emotionality Age 11 | −0.01 | 0.02 | 0.605 | ||
| Wave 1 Public assistance → | Rate of change in poor self-control Ages 10–12 (Slope) | 0.008 | 0.04 | 0.845 | ||
| Wave 1 Public assistance → | Rate of change in poor self-control Ages 12–14 (Slope) | 0.021 | 0.028 | 0.443 | ||
| Wave 1 Public assistance → | Rate of change in harsh punishment Ages 10–14 (Slope) | −0.028 | 0.028 | 0.308 | ||
| Wave 1 Public assistance → | BPD symptom severity Age 14 (Intercept) | 0.008 | 0.031 | 0.787 | ||
| Wave 1 Public assistance → | Rate of change in BPD symptoms Ages 14–17 (Slope) | 0.041 | 0.044 | 0.348 | ||
|
| ||||||
| Minority race → | Harsh punishment (Intercept) | 0.253 | 0.026 | < .0001 | ||
| Minority race → | Poor Self-Control (Intercept) | 0.179 | 0.03 | < .0001 | ||
| Minority race → | Negative emotionality Age 11 | −0.031 | 0.021 | 0.145 | ||
| Minority race → | Change in poor self-control Ages 10–12 (Slope) | −0.002 | 0.043 | 0.959 | ||
| Minority race → | Change in poor self-control Ages 12–14 (Slope) | 0.004 | 0.028 | 0.884 | ||
| Minority race → | Change in harsh punishment Ages 10–14 (Slope) | 0.125 | 0.029 | < .0001 | ||
| Minority race → | BPD symptom severity Age 14 (Intercept) | 0.032 | 0.033 | 0.337 | ||
| Minority race → | Rate of change in BPD symptoms Ages 14–17 (Slope) | 0.062 | 0.049 | 0.204 | ||
|
| ||||||
| Wave 1 Harsh punishment → | Harsh punishment (Intercept) | 0.224 | 0.024 | < .0001 | ||
| Wave 1 Harsh punishment → | Poor Self-Control (Intercept) | 0.026 | 0.03 | 0.378 | ||
| Wave 1 Harsh punishment → | Negative emotionality Age 11 | 0.027 | 0.021 | 0.205 | ||
| Wave 1 Harsh punishment → | Change in poor self-control Ages 10–12 (Slope) | 0.02 | 0.044 | 0.641 | ||
| Wave 1 Harsh punishment → | Change in poor self-control Ages 12–14 (Slope) | −0.041 | 0.028 | 0.145 | ||
| Wave 1 Harsh punishment → | Change in harsh punishment Ages 10–14 (Slope) | 0.154 | 0.025 | < .0001 | ||
| Wave 1 Harsh punishment → | BPD symptom severity Age 14 (Intercept) | 0.018 | 0.034 | 0.585 | ||
| Wave 1 Harsh punishment → | Rate of change in BPD symptoms Ages 14–17 (Slope) | −0.001 | 0.047 | 0.989 | ||
|
| ||||||
| Wave 1 Poor self-control → | Harsh punishment (Intercept) | 0.059 | 0.026 | 0.024 | ||
| Wave 1 Poor self-control → | Poor Self-Control (Intercept) | 0.192 | 0.032 | < .0001 | ||
| Wave 1 Poor self-control → | Negative emotionality Age 11 | 0.11 | 0.021 | < .0001 | ||
| Wave 1 Poor self-control → | Rate of change in poor self-control Ages 10–12 (Slope) | 0.187 | 0.041 | < .0001 | ||
| Wave 1 Poor self-control → | Rate of change in poor self-control Ages 12–14 (Slope) | 0 | 0.027 | 0.998 | ||
| Wave 1 Poor self-control → | Rate of change in harsh punishment Ages 10–14 (Slope) | 0.093 | 0.029 | 0.002 | ||
| Wave 1 Poor self-control → | BPD symptom severity Age 14 (Intercept) | 0.009 | 0.036 | 0.815 | ||
| Wave 1 Poor self-control → | Rate of change in BPD symptoms Ages 14–17 (Slope) | 0.021 | 0.052 | 0.686 | ||
|
| ||||||
| Wave 1 Negative emotionality → | Harsh punishment (Intercept) | 0.014 | 0.026 | 0.593 | ||
| Wave 1 Negative emotionality → | Poor Self-Control (Intercept) | −0.03 | 0.03 | 0.309 | ||
| Wave 1 Negative emotionality → | Negative emotionality Age 11 | 0.441 | 0.017 | < .0001 | ||
| Wave 1 Negative emotionality → | Rate of change in poor self-control Ages 10–12 (Slope) | 0.054 | 0.031 | 0.193 | ||
| Wave 1 Negative emotionality → | Rate of change in poor self-control Ages 12–14 (Slope) | −0.015 | 0.03 | 0.618 | ||
| Wave 1 Negative emotionality → | Rate of change in harsh punishment Ages 10–14 (Slope) | −0.026 | 0.028 | 0.346 | ||
| Wave 1 Negative emotionality → | BPD symptom severity Age 14 (Intercept) | 0.035 | 0.035 | 0.317 | ||
| Wave 1 Negative emotionality → | Rate of change in BPD symptoms Ages 14–17 (Slope) | −0.017 | 0.049 | 0.725 | ||
|
| ||||||
| Harsh punishment (Intercept) → | Negative emotionality Age 11 | 0.037 | 0.028 | 0.184 | ||
| Harsh punishment (Intercept) → | Rate of change in poor self-control Ages 10–12 (Slope) | 0.163 | 0.058 | 0.005 | ||
| Harsh punishment (Intercept) → | Rate of change in poor self-control Ages 12–14 (Slope) | −0.047 | 0.041 | 0.256 | ||
| Harsh punishment (Intercept) → | Rate of change in harsh punishment Ages 10–14 (Slope) | −0.457 | 0.033 | < .0001 | ||
| Harsh punishment (Intercept) → | BPD symptom severity Age 14 (Intercept) | 0.206 | 0.046 | < .0001 | ||
| Harsh punishment (Intercept) → | Rate of change in BPD symptoms Ages 14–17 (Slope) | 0.09 | 0.061 | 0.139 | ||
|
| ||||||
| Poor self-control (Intercept) → | Negative emotionality Age 11 | 0.076 | 0.028 | 0.008 | ||
| Poor self-control (Intercept) → | Rate of change in poor self-control Ages 10–12 (Slope) | −0.589 | 0.053 | < .0001 | ||
| Poor self-control (Intercept) → | Rate of change in poor self-control Ages 12–14 (Slope) | −0.424 | 0.041 | < .0001 | ||
| Poor self-control (Intercept) → | Rate of change in harsh punishment Ages 10–14 (Slope) | 0.008 | 0.04 | 0.852 | ||
| Poor self-control (Intercept) → | BPD symptom severity Age 14 (Intercept) | 0.304 | 0.058 | < .0001 | ||
| Poor self-control (Intercept) → | Rate of change in BPD symptoms Ages 14–17 (Slope) | −0.053 | 0.078 | 0.499 | ||
|
| ||||||
| Negative emotionality Age 11 → | Rate of change in poor self-control Ages 12–14 (Slope) | −0.071 | 0.022 | 0.002 | ||
| Negative emotionality Age 11 → | BPD symptom severity Age 14 (Intercept) | 0.111 | 0.032 | < .0001 | ||
| Negative emotionality Age 11 → | Rate of change in BPD symptoms Ages 14–17 (Slope) | 0.021 | 0.047 | 0.657 | ||
|
| ||||||
| Rate of change in poor self-control Ages 10–12 (Slope) → | BPD symptom severity Age 14 (Intercept) | 0.392 | 0.079 | < .0001 | ||
| Rate of change in poor self-control Ages 10–12 (Slope) → | Rate of change in BPD symptoms Ages 14–17 (Slope) | −0.183 | 0.111 | 0.099 | ||
|
| ||||||
| Rate of change in poor self-control Ages 12–14 (Slope) → | BPD symptom severity Age 14 (Intercept) | −0.101 | 0.037 | 0.007 | ||
| Rate of change in poor self-control Ages 12–14 (Slope) → | Rate of change in BPD symptoms Ages 14–17 (Slope) | 0.136 | 0.055 | 0.014 | ||
|
| ||||||
| Rate of change in harsh punishment Ages 10–14 (Slope) → | BPD symptom severity Age 14 (Intercept) | 0.297 | 0.046 | < .0001 | ||
| Rate of change in harsh punishment Ages 10–14 (Slope) → | Rate of change in BPD symptoms Ages 14–17 (Slope) | 0.021 | 0.065 | 0.751 | ||
Note. Parameter estimates reflect the standardized effect of a predictor (left) on an outcome (right), as indicated by the arrow. Measures between ages 5–8 were based on parent report. From ages 10–14, harsh parenting and poor self- control were child-reported. BPD symptoms in adolescence were child-reported. Age 11 negative emotionality was parent-reported. Wave 1 refers to the first wave of data collection, which occurred between ages 5 and 8, depending on the cohort.
Predictors of changes in BPD symptoms between ages 14 and 17
Growth of child-reported poor self-control between ages 12 and 14 was the only significant predictor of BPD symptoms change between ages 14 and 17 (Table 3), accounting for 6.1% of the variance.
Developmental pathways to BPD symptom severity at age 14
As anticipated, the direct effects of harsh punishment, poor self-control, and negative emotionality on BPD symptom severity at age 14 partly reflected the influence of earlier developmental experiences. To characterize pathways that predicted the level of BPD symptoms at age 14, we computed the indirect effects of developmentally antecedent variables on BPD severity via the significant direct predictors mentioned above (e.g., harsh punishment at age 10). Each indirect effect represents a single statistical test of a given prospective pathway, suggesting that the direct effect of a proximal predictor of BPD is mediated in part by earlier experiences. Given that the harsh punishment and poor self-control slope factors were regressed on initial levels of the same variable at age 10 primarily to unconfound initial severity and rate of change, indirect effects that included the within-construct intercept–slope path were not described here because they were not of substantive interest.
Consistent with our hypothesis, poor self-control at wave 1 significantly influenced age 14 BPD symptoms via its effect on harsh punishment at age 10 (Table 4). That is, poor-self control at wave 1 predicted greater harsh punishment at age 10 (controlling for wave 1 harsh punishment), which in turn predicted greater BPD symptoms at age 14. We also found that the influence of wave 1 poor self-control on age 14 BPD symptoms was partially mediated by increases in harsh punishment between ages 10 and 14. Conversely, age 14 BPD symptom severity also reflected the prospective effects of harsh punishment on poor self-control. Child-reported harsh punishment at age 10 predicted more rapid increases in poor self-control between ages 10 and 12, which predicted more severe age 14 BPD symptoms. Although caregiver-rated harsh punishment at wave 1 was not directly associated with poor self-control between ages 10 and 14, wave 1 harsh punishment indirectly influenced age 14 BPD symptoms via its influence on harsh punishment at age 10, which in turn predicted greater self-control problems and subsequent BPD symptoms. There was also a significant indirect effect of poor self-control at both wave 1 and age 10 on age 14 BPD symptoms via negative emotionality at age 11.
Table 4.
Significant indirect effects of developmentally antecedent variables on age 14 BPD symptom severity and change in BPD symptoms between ages 14 and 17
| BPD Outcome | Direct Predictor of BPD | Indirect Pathway | Std. β | S. E. | p |
|---|---|---|---|---|---|
| Age 14 BPD symptom severity (Intercept) | ← Harsh punishment Age 10 (Intercept) | ← Harsh punishment Wave 1 | 0.046 | 0.011 | < .001 |
| ← Harsh punishment Age 10 (Intercept) | ← Poor self-control Wave 1 | 0.012 | 0.006 | 0.041 | |
|
| |||||
| ← Harsh punishment Age 10–14 (Slope) | ← Harsh punishment Wave 1 | 0.046 | 0.011 | < .001 | |
| ← Harsh punishment Age 10–14 (Slope) | ← Poor self-control Wave 1 | 0.028 | 0.01 | 0.004 | |
|
| |||||
| ← Poor self-control Age 10 (Intercept) | ← Poor self-control Wave 1 | 0.059 | 0.014 | < .001 | |
|
| |||||
| ← Poor self-control Age 10–12 (Slope) | ← Poor self-control Wave 1 | 0.073 | 0.023 | 0.001 | |
| ← Poor self-control Age 10–12 (Slope) | ← Harsh punishment Age 10 (Intercept) | 0.064 | 0.027 | 0.018 | |
| ← Poor self-control Age 10–12 (Slope) | ← Harsh punishment Age 10 (Intercept) ← Harsh punishment Wave 1 | 0.014 | 0.006 | 0.02 | |
|
| |||||
| ← Negative emotionality Age 11 | ← Negative emotionality Wave 1 | 0.049 | 0.014 | < .001 | |
| ← Negative emotionality Age 11 | ← Poor self-control Wave 1 | 0.012 | 0.004 | 0.004 | |
| ← Negative emotionality Age 11 | ← Poor self-control Age 10 (Intercept) | 0.009 | 0.004 | 0.025 | |
| ← Negative emotionality Age 11 | ← Poor self-control Age 10 (Intercept) ← Poor self-control Wave 1 | 0.002 | 0.001 | 0.037 | |
|
| |||||
| ← Poor self-control Age 12–14 (Slope) | ← Negative emotionality Age 11 ← Negative emotionality Wave 1 | 0.003 | 0.001 | 0.033 | |
| ← Poor self-control Age 12–14 (Slope) | ← Negative emotionality Age 11 ← Poor self-control Wave 1 | 0.001 | 0.0005 | 0.047 | |
|
| |||||
| Change in BPD symptom severity between ages 14 and 17 (Slope) | ← Poor self-control Age 12–14 (Slope) | ← Negative Emotionality Age 11 | −0.01 | 0.005 | 0.042 |
| ← Poor self-control Age 12–14 (Slope) | ← Negative Emotionality Age 11 ← Negative Emotionality Wave 1 | −0.004 | 0.002 | 0.043 | |
Note. Parameter estimates reflect the product of the standardized effects of one or more predictors (Indirect Pathway) on BPD symptomatology (BPD Outcome) via a direct predictor of BPD, as indicated by the arrows. Wave 1 refers to the first wave of data collection, which occurred between ages 5 and 8, depending on the cohort.
Developmental pathways to changes in BPD symptoms between ages 14 and 17
There was a significant indirect effect of negative emotionality on BPD symptom change in adolescence via changes in poor self-control between ages 12 and 14. More specifically, negative emotionality at age 11 predicted slower growth of poor self-control between 12 and 14, which may reflect an asymptotic growth pattern such that those with high levels of negative emotionality by age 11 may already have greater problems with self-control. In turn, increasing problems with self-control between 12 and 14 predicted more rapid increases in BPD symptoms between 14 and 17.
Comparison of findings with caregiver-reported poor self-control and harsh punishment between ages 10 and 14
As mentioned above, ratings of poor self-control, harsh punishment, and negative emotionality were only provided by caregivers at the first wave of data collection, whereas BPD symptom ratings were only obtained from girls, not their caregivers, between ages 14 and 17. However, between ages 10 and 14, both caregivers and children provided ratings of harsh punishment and poor self-control. To explore whether our results were sensitive to the source of information, we ran the same structural model described above substituting LCMs of caregiver-reported self-control and harsh punishment as predictors of BPD symptoms in adolescence. Model fit was verified for each component of the structural model3. As above, a linear LCM best fit the trajectory of caregiver-reported harsh punishment, whereas a piecewise LCM with separate slopes for ages 10–12 and 12–14 characterized poor self-control.
The full structural model incorporating caregiver-reported harsh punishment and poor self-control as predictors of BPD symptoms fit the data well, χ2(1242) = 2288.13, CFI = .97, RMSEA = 0.019 (90% CI = .018 – .021). Consistent with the child-report analysis, poor self-control at age 10 and increasing problems with self-control between ages 10 and 12 significantly predicted BPD symptoms at age 14, although the magnitude of these effects was somewhat smaller (see online supplement Table S1). Unlike the child-report results, caregiver-reported changes in self-control problems between ages 12 and 14 were not predictive of change in BPD symptoms between 14 and 17. Interestingly, caregiver-reported harsh punishment between ages 10 and 14 was not associated with BPD symptoms at age 14. In addition, in the caregiver model, minority race was associated with more severe age 14 BPD symptoms, as well as more rapid growth in BPD symptoms from 14–17.
Discussion
Although harsh parenting practices and impulsive and emotionally reactive child temperament have previously been linked with BPD symptoms (Belsky et al., 2012; Johnson et al., 2006; Zelkowitz et al., 2001), this is one of the first prospective studies to characterize how the interplay between these processes in childhood influences the development of BPD symptoms in adolescence. Consistent with the biosocial developmental model of BPD (Crowell et al., 2009), we found that harsh punishment, poor self-control, and negative emotionality were predictive of BPD symptoms at age 14. Only worsening self-control between ages 12 and 14, however, predicted growth in BPD symptoms between ages 14–17. Furthermore, we found that the effects of poor self-control and harsh punishment on each other between ages 5 and 14 contributed to BPD symptoms in adolescence. More specifically, early poor self-control (ages 5 – 8) predicted greater harsh punishment at age 10 and increasing harsh punishment between ages 10 and 14. Conversely, early harsh punishment predicted poorer self-control between ages 10 and 12. Crucially, the effects of harsh punishment and poor self-control on BPD symptoms were partly mediated by their earlier reciprocal effects on each other. Contrary to our hypothesis, however, we did not observe significant bidirectional prospective relationships between negative emotionality and harsh punishment or poor self-control.
Our results are consistent with a larger literature on bidirectional parent-child influences on externalizing behavior (Scaramella, Conger, Spoth, & Simons, 2002) and how escalating, coercive parent-child conflict leads to conduct problems and emotion dysregulation (Patterson et al., 1989; Snyder, Schrepferman, & Peter, 1997). Indeed, negative escalation and lower cohesiveness during caregiver-child conflict discussion tasks have been linked with BPD symptom severity (Whalen et al., 2014) and self-harm (Crowell et al., 2008) in adolescence. Our findings also support the idea that BPD is most likely to emerge in an individual with a vulnerable temperament (poor self-control and high negative emotionality) who experiences environmental adversity such as harsh parenting (Carlson, Egeland, & Sroufe, 2009). Although our study cannot speak directly to the quality of parent-child interactions, it does point to a troubling feedback loop between harsh punishment and self-control that unfolds over childhood and early adolescence that portends BPD symptoms in teen girls. Children who react to parental requests with intense negative emotions or defiance are more likely to elicit negative emotions and demands for compliance in the parent (Braungart-Rieker, Garwood, & Stifter, 1997). Conversely, harsh punishment prospectively predicts increased disruptive behaviors and noncompliance (Hipwell et al., 2008), and parental displays of negative emotion are associated with poorer peer relationships (Carson & Parke, 1996).
A key proposal of the biosocial theory of BPD (Beauchaine et al., 2009; Crowell et al., 2009) is that emotion dysregulation in BPD is the product of parent-child transactions characterized by emotionally reactive outbursts by the child (reflecting emotional reactivity and poor self-control, heritable dimensions of temperament) that meet with harsh, invalidating parental responses intended to punish such outbursts. These ideas draw on the broader literature on coercive parent-child cycles, especially the model articulated by Scaramella and Leve (2004)4. Most pertinent to our study, the coercion model proposes that 1) children who are temperamentally prone to emotional arousal and impulsive behaviors may evoke harsh parenting responses; 2) children with such temperaments may also struggle to develop self-control because of the potency of their reactions; 3) parenting strategies that do not complement the child’s reactivity may further exacerbate self-control problems; 4) children who struggle to develop self-control and emotion regulation may evoke further harsh parenting; and 5) self-regulatory problems that develop from ineffective parent-child interactions are likely to generalize to interpersonal problems with peers.
Although our study addressed only a subset of these ideas, the results are consistent with the coercion model in a number of ways. First, poor self-control in childhood (e.g., struggling to compromise with parents or teachers over a disagreement) predicted subsequent increases in harsh punishment (e.g., spanking), suggesting an evocative effect of child characteristics on parenting. Second, the severity of child-reported harsh punishment at age 10 predicted increases in self-control problems between ages 10 and 12, consistent with an exacerbation of self-control problems due to ineffective parenting strategies. Third, poor self-control in childhood was associated with greater negative emotionality at age 11 (controlling for earlier negative emotionality), suggesting that poor self-control may exacerbate emotional problems that undermine the development of emotion regulation. Fourth, and somewhat more speculatively, the prospective link from harsh punishment to poor self-control to adolescent BPD symptoms may reflect in part the generalization of ineffective parent-child interactions to other relationships, including peers. Interpersonal dysfunction is a central aspect of BPD, defined by unstable and intense relationships and difficulty enacting appropriate social responses depending on the context (e.g., expectations of exclusivity are more relevant to romance than to friendship; Hill et al., 2008). Although negative emotionality was predictive of BPD symptoms, we did not find that children with greater negative emotionality were significantly more likely to experience harsh punishment. Neither did we observe that harsh punishment predicted subsequent increases in negative emotionality.
We were interested to find that poor self-control was a potent predictor of BPD symptoms in adolescence and was the only predictor of changes in BPD symptoms between ages 14 and 17. This is consistent with the emphasis on impulsivity and emotion dysregulation as potential predisposing vulnerabilities or precursors of BPD in both theoretical (Crowell et al., 2009) and empirical (Stepp et al., 2010) accounts. Indeed, our selection of the SSRS self-control subscale to measure poor self-control may have been particularly sensitive to BPD symptoms because many items tap into failures of inhibitory control in emotionally arousing interpersonal situations. Thus, rather than informing an understanding of general failures of self-control, our results may speak more to negative urgency, a facet of impulsivity defined by behaving rashly when upset that is particularly characteristic of BPD (Peters, Upton, & Baer, 2013). Indeed, although poor self-control has been linked with impulsive behaviors such as self-injury and problematic drinking (MacKillop, Mattson, Anderson Mackillop, Castelda, & Donovick, 2007), in a recent study, negative urgency was the only facet of impulsivity that mediated the relationships between self-control and self-injury, eating problems, and problematic alcohol use (Dir, Karyadi, & Cyders, 2013). Our findings suggest that future developmental studies may wish to focus on understanding how negative urgency plays a role in the expression of BPD symptoms such as self-injury.
The magnitude and developmental timing of the prospective effects of self-control on BPD symptoms in adolescence also have clinical implications. The only significant predictor of the longitudinal course of BPD symptoms in adolescence (ages 14–17) was the growth of child-reported self-control problems between ages 12 and 14. Moreover, our analyses revealed that there was substantially greater growth in self-control problems, on average, between 12 and 14 than ages 10 and 12, consistent with prior research findings that sensation seeking and risk-taking behaviors increase substantially in adolescence, which may be linked to pubertal timing (Romer, Duckworth, Sznitman, & Park, 2010; Steinberg et al., 2008). Our findings suggest that rapid increases in self-control problems in early adolescence may be an important precursor of BPD-related pathology in adolescence. This is also consistent with a prior report from the PGS in which we found that growth in attention deficit hyperactivity disorder and oppositional defiant disorder symptoms between ages 8 and 13 predicted greater BPD symptoms at age 14 (Stepp et al., 2012), as well as another report linking disruptive behavior disorders with PDs in adolescence (Helgeland, Kjelsberg, & Torgersen, 2005). Yet our findings extend beyond previous reports by identifying a specific transdiagnostic dimension, poor self-control, that is tightly linked with the development of BPD pathology and that aligns with theoretical accounts (Beauchaine et al., 2009).
Our study also compared whether the prediction of borderline symptoms by harsh punishment and poor self-control differed between caregiver and child respondents. We found reasonable agreement between caregivers and children that poor self-control between ages 10 and 14 predicted greater BPD symptoms at age 14. Only girls, not caregivers, however, reported a prospective link between harsh punishment and BPD. This finding suggests at least two nonexclusive possibilities. First, girls’ subjective experience of parenting quality may be more closely associated with BPD symptoms than overt harsh parenting behaviors (e.g., coercive discipline). Indeed, individuals with BPD are often highly sensitive to perceived rejection and prone to assign high salience to social threat cues (Berenson et al., 2009). Thus, girls who tend to experience their caregivers as harsh or invalidating because of a bias toward perceived rejection may internalize negative representations of others and may also be at greater risk for BPD symptoms. Alternatively, caregivers may have been more likely to minimize their reports of harsh parenting due to a social desirability bias or because they view their disciplinary efforts as adaptive, not coercive. Our study was not designed to tease apart these alternatives, but we hope that future research will elucidate the relevance of self-versus other-reported negative parenting in the etiology of BPD.
In a previous report on this sample (Stepp et al., 2014), we characterized the reciprocal influences of harsh parenting and BPD symptoms in girls 14–17, finding that there was a moderate association in the rates of change over time in parenting and BPD symptoms. We also found that year-to-year fluctuations of BPD were related to subsequent changes in parenting. This report extends upon these findings in three important ways: 1) this study focused specifically on poor self-control as a key construct that predicts the development of BPD; 2) we characterized how reciprocal influences of poor self-control and harsh punishment in childhood prospectively predict BPD symptoms in adolescence; and 3) we developed a robust measurement model of BPD symptoms in adolescence that is more likely to be sensitive to developmental changes.
A strength of the prospective developmental design of our study was that it was not subject to retrospective biases that have limited the generalizability of prior reports in adults (Zanarini et al., 1997). The annual assessments of girls between ages 5 and 17 also provided rich longitudinal data that allowed us to characterize how reciprocal influences between harsh punishment and poor self-control influence BPD symptoms in adolescent girls. Another strength of our study was the large demographically representative community sample, which permitted us to test rich developmental structural equation models and to identify effects that are more likely to generalize to the general population than clinical or treatment-seeking samples. Lastly, by leveraging a measurement model of BPD that exhibited strict measurement invariance over adolescence, rather than relying on summed symptom scores, we are confident that our primary measure of BPD represented the same underlying latent construct across adolescence.
This study also had some limitations that constrain the interpretation of our findings. First and foremost, girls were assessed annually by trained interviewers, yet the coercive parent-child transactions that may have the greatest effect on the development of BPD unfold on a much faster timescale, likely minutes or hours (Crowell et al., 2008). Thus, the reciprocal effects of harsh punishment and poor self-control identified in our research probably reflect the aggregation of many such transactions that occur consistently over childhood. Nevertheless, although behavioral observations of parent-child dynamics in BPD have yielded important insights (Whalen et al., 2014), there is value in knowing the long-term effects of such transactions across development. Second, BPD symptoms were first assessed at age 14, opening the possibility that some of the prospective effects reported (e.g., poor self-control at age 10 predicting BPD symptoms at age 14) may partly reflect co-occurring contemporaneous problems, rather than true precursors of BPD. Likewise, although we observed a significant prospective effect of negative emotionality on BPD symptoms in adolescence, elevated negative emotionality, particularly affective instability, is a defining characteristic of the BPD construct (Kendler, Myers, & Reichborn-Kjennerud, 2011). Thus, the finding that negative emotionality predicts BPD symptoms should be interpreted with caution because of potential criterion contamination and because there may be a nonspecific relationship between neuroticism and psychopathology (Lahey, 2009). Finally, although BPD symptoms are more common in women in clinical samples, the prevalence of BPD in community samples is approximately equal in men and women (Lenzenweger et al., 2007). Thus, because our sample did not include males, our findings only pertain to the developmental trajectories of girls. Future developmental research on BPD symptoms in both sexes may reveal interesting differences in the expression and longitudinal course of this disorder.
Altogether, our findings corroborate a key assertion of the biosocial developmental theory (Crowell et al., 2009), namely that poor self-control in the child and negative parenting strategies contribute to the development of BPD symptoms via reciprocal effects on each other. In addition to their indirect effects on BPD via reciprocal influences, the direct effects of harsh punishment and poor self-control in childhood on the severity of BPD symptoms in adolescence were substantial. This underscores the need to address both child and parental contributions to dysfunctional transactions in order to stem the development of emotion dysregulation and interpersonal dysfunction characteristic of BPD (also see Crowell et al., 2014). Indeed, interventions for children with conduct problems that incorporate parents and teachers have been successful in reducing disruptive behaviors (e.g., Webster-Stratton, Reid, & Hammond, 2004). Extending such results, our findings suggest the need to monitor and potentially address self-control problems in early adolescence, as these were most clearly linked to the longitudinal course of BPD symptoms between ages 14 and 17. Intervention development for adolescents with BPD symptoms may be informed by programs developed for adolescent conduct problems (Dodge & Pettit, 2003) or by extending treatments for adults with BPD (Miller, Rathus, & Linehan, 2006). Although greater negative emotionality predicted the severity of BPD symptoms at age 14, this effect was much weaker than the effects of poor self-control and harsh punishment, suggesting that negative emotionality plays a smaller role in the development of BPD. Future research is needed to test other key assertions of the biosocial model, such as the idea that emotion dysregulation precedes clinically impairing BPD symptoms and influences the development of interpersonal problems that exacerbate BPD pathology. In addition, our study focused solely on harsh punishment, and additional caregiver factors, such as neglect, should be pursued in prospective studies of BPD (Johnson et al., 2006).
Supplementary Material
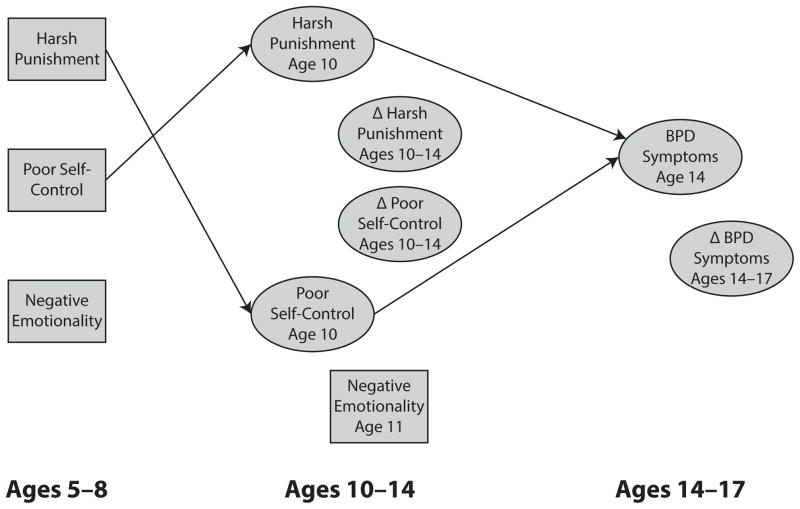
Figure 1.
Conceptual diagram of key variables in structural equation model of adolescent BPD symptoms. Rectangles denote observed variables, whereas ellipses denote latent variables derived from latent curve models. Paths depicting two of the indirect effects of harsh punishment and poor self-control on BPD symptoms via reciprocal influences on each other are included for illustration. For a summary of all structural relationships, see Table 1.
Acknowledgments
This research was supported by grants from the National Institute of Mental Health (MH056630) and the National Institute on Drug Abuse (DA012237), and by funding from the Office of Juvenile Justice and Delinquency Prevention, the FISA Foundation, and the Falk Fund.
Further support was provided by K01 MH097091 (to M.N.H.) and K01 MH086713 (to S.D.S.).
Footnotes
To mitigate the possibility that our results were unduly sensitive to missing observations, we also tested models using a full-information maximum likelihood (ML) estimator omitting residual correlations among categorical items, which is more robust than WLSMV to observations missing at random (Asparouhov & Muthén, 2010). Our results were not substantially different using the ML and WLSMV estimators.
Although the age difference between wave 1 (ages 5–8) and age 10 differed by cohort, exploratory analyses indicated that the effect of wave 1 variables on age 10 harsh punishment and poor self-control did not significantly differ by cohort.
Model fit statistics for parent-reported submodels are available from the corresponding author.
Although this model emphasizes the role of parent-child transactions during early childhood, we believe the key assertions have broader developmental significance and are pertinent to the development of BPD symptoms.
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-5. 5. Washington, D.C: American Psychiatric Publishing; 2013. [Google Scholar]
- Asparouhov T, Muthén BO. Weighted least squares estimation with missing data. Los Angeles, CA: 2010. Aug 4, Retrieved from http://www.statmodel.com/download/GstrucMissingRevision.pdf. [Google Scholar]
- Bateman A, Fonagy P. Health service utilization costs for borderline personality disorder patients treated with psychoanalytically oriented partial hospitalization versus general psychiatric care. American Journal of Psychiatry. 2003;160(1):169–171. doi: 10.1176/appi.ajp.160.1.169. [DOI] [PubMed] [Google Scholar]
- Beauchaine TP, Klein DN, Crowell SE, Derbidge C, Gatzke-Kopp L. Multifinality in the development of personality disorders: A Biology × Sex × Environment interaction model of antisocial and borderline traits. Development and Psychopathology. 2009;21(3):735–770. doi: 10.1017/S0954579409000418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker DF, Grilo CM, Morey LC, Walker ML, Edell WS, McGlashan TH. Applicability of personality disorder criteria to hospitalized adolescents: evaluation of internal consistency and criterion overlap. Journal of the American Academy of Child and Adolescent Psychiatry. 1999;38(2):200–205. doi: 10.1097/00004583-199902000-00020. [DOI] [PubMed] [Google Scholar]
- Belsky DW, Caspi A, Arseneault L, Bleidorn W, Fonagy P, Goodman M, Moffitt TE. Etiological features of borderline personality related characteristics in a birth cohort of 12-year-old children. Development and Psychopathology. 2012;24(1):251–265. doi: 10.1017/S0954579411000812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bender DS, Dolan RT, Skodol AE, Sanislow CA, Dyck IR, McGlasgan TH, Gunderson JG. Treatment utilization by patients with personality disorders. American Journal of Psychiatry. 2001;158(2):295–302. doi: 10.1176/appi.ajp.158.2.295. [DOI] [PubMed] [Google Scholar]
- Berenson KR, Gyurak A, Ayduk Ö, Downey G, Garner MJ, Mogg K, Pine DS. Rejection sensitivity and disruption of attention by social threat cues. Journal of Research in Personality. 2009;43(6):1064–1072. doi: 10.1016/j.jrp.2009.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernstein DP, Cohen P, Velez CN, Schwab-Stone M, Siever LJ, Shinsato L. Prevalence and stability of the DSM-III-R personality disorders in a community-based survey of adolescents. The American Journal of Psychiatry. 1993;150(8):1237–1243. doi: 10.1176/ajp.150.8.1237. [DOI] [PubMed] [Google Scholar]
- Blais MA, Hilsenroth MJ, Fowler JC. Diagnostic efficiency and hierarchical functioning of the DSM-IV borderline personality disorder criteria. The Journal of Nervous and Mental Disease. 1999;187(3):167–173. doi: 10.1097/00005053-199903000-00006. [DOI] [PubMed] [Google Scholar]
- Bollen KA, Curran PJ. Latent Curve Models: A Structural Equation Perspective. Wiley-Interscience; 2005. [Google Scholar]
- Bornovalova MA, Huibregtse BM, Hicks BM, Keyes M, McGue M, Iacono W. Tests of a direct effect of childhood abuse on adult borderline personality disorder traits: a longitudinal discordant twin design. Journal of Abnormal Psychology. 2013;122(1):180–194. doi: 10.1037/a0028328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braungart-Rieker J, Garwood MM, Stifter CA. Compliance and noncompliance: the roles of maternal control and child temperament. Journal of Applied Developmental Psychology. 1997;18(3):411–428. doi: 10.1016/S0193-3973(97)80008-1. [DOI] [Google Scholar]
- Brown MZ, Comtois KA, Linehan MM. Reasons for suicide attempts and nonsuicidal self-injury in women with borderline personality disorder. Journal of Abnormal Psychology. 2002;111(1):198–202. doi: 10.1037//0021-843x.111.1.198. [DOI] [PubMed] [Google Scholar]
- Buss AH, Plomin R. Temperament: Early Developing Personality Traits. Hillsdale, N.J: Psychology Press; 1984. [Google Scholar]
- Carlson EA, Egeland B, Sroufe LA. A prospective investigation of the development of borderline personality symptoms. Development and Psychopathology. 2009;21(04):1311. doi: 10.1017/S0954579409990174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carson JL, Parke RD. Reciprocal negative affect in parent-child interactions and children’s peer competency. Child Development. 1996;67(5):2217–2226. [PubMed] [Google Scholar]
- Chanen AM, Jackson HJ, McGorry PD, Allot KA, Clarkson V, Yuen HP. Two-year stability of personality disorder in older adolescent outpatients. Journal of Personality Disorders. 2004;18(6):526–541. doi: 10.1521/pedi.18.6.526.54798. [DOI] [PubMed] [Google Scholar]
- Chanen AM, Jovev M, Djaja D, McDougall E, Yuen HP, Rawlings D, Jackson HJ. Screening for borderline personality disorder in outpatient youth. Journal of Personality Disorders. 2008;22(4):353–364. doi: 10.1521/pedi.2008.22.4.353. [DOI] [PubMed] [Google Scholar]
- Chanen AM, Jovev M, Jackson HJ. Adaptive functioning and psychiatric symptoms in adolescents with borderline personality disorder. The Journal of Clinical Psychiatry. 2007;68(2):297–306. doi: 10.4088/jcp.v68n0217. [DOI] [PubMed] [Google Scholar]
- Clarkin JF, Levy KN, Lenzenweger MF, Kernberg OF. The Personality Disorders Institute/Borderline Personality Disorder Research Foundation randomized control trial for borderline personality disorder: rationale, methods, and patient characteristics. Journal of Personality Disorders. 2004;18(1):52–72. doi: 10.1521/pedi.18.1.52.32769. [DOI] [PubMed] [Google Scholar]
- Cramer V, Torgersen S, Kringlen E. Personality disorders and quality of life. A population study. Comprehensive Psychiatry. 2006;47(3):178–184. doi: 10.1016/j.comppsych.2005.06.002. [DOI] [PubMed] [Google Scholar]
- Crawford TN, Cohen P, Brook JS. Dramatic-erratic personality disorder symptoms: I. Continuity from early adolescence into adulthood. Journal of Personality Disorders. 2001;15(4):319–335. doi: 10.1521/pedi.15.4.319.19182. [DOI] [PubMed] [Google Scholar]
- Crone EA, Dahl RE. Understanding adolescence as a period of social–affective engagement and goal flexibility. Nature Reviews Neuroscience. 2012;13(9):636–650. doi: 10.1038/nrn3313. [DOI] [PubMed] [Google Scholar]
- Crowell SE, Baucom BR, Yaptangco M, Bride D, Hsiao R, McCauley E, Beauchaine TP. Emotion dysregulation and dyadic conflict in depressed and typical adolescents: Evaluating concordance across psychophysiological and observational measures. Biological Psychology. 2014;98:50–58. doi: 10.1016/j.biopsycho.2014.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crowell SE, Beauchaine TP, Linehan MM. A biosocial developmental model of borderline personality: Elaborating and extending Linehan’s theory. Psychological Bulletin. 2009;135(3):495–510. doi: 10.1037/a0015616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crowell SE, Beauchaine TP, McCauley E, Smith CJ, Vasilev CA, Stevens AL. Parent-child interactions, peripheral serotonin, and self-inflicted injury in adolescents. Journal of Consulting and Clinical Psychology. 2008;76(1):15–21. doi: 10.1037/0022-006X.76.1.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dahl RE. Adolescent brain development: A period of vulnerabilities and opportunities. Annals of the New York Academy of Sciences. 2004;1021(1):1–22. doi: 10.1196/annals.1308.001. [DOI] [PubMed] [Google Scholar]
- Dir AL, Karyadi K, Cyders MA. The uniqueness of negative urgency as a common risk factor for self-harm behaviors, alcohol consumption, and eating problems. Addictive Behaviors. 2013;38(5):2158–2162. doi: 10.1016/j.addbeh.2013.01.025. [DOI] [PubMed] [Google Scholar]
- Dodge KA, Pettit GS. A biopsychosocial model of the development of chronic conduct problems in adolescence. Developmental Psychology. 2003;39(2):349–371. doi: 10.1037/0012-1649.39.2.349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duckworth AL, Kern ML. A meta-analysis of the convergent validity of self-control measures. Journal of Research in Personality. 2011;45(3):259–268. doi: 10.1016/j.jrp.2011.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fertuck EA, Lenzenweger MF, Clarkin JF, Hoermann S, Stanley B. Executive neurocognition, memory systems, and borderline personality disorder. Clinical Psychology Review. 2006;26(3):346–375. doi: 10.1016/j.cpr.2005.05.008. [DOI] [PubMed] [Google Scholar]
- Fuligni AJ, Eccles JS. Perceived parent-child relationships and early adolescents’ orientation toward peers. Developmental Psychology. 1993;29(4):622–632. doi: 10.1037/0012-1649.29.4.622. [DOI] [Google Scholar]
- Goodyer IM, Ashby L, Altham PME, Vize C, Cooper PJ. Temperament and Major Depression in 11 to 16 Year Olds. Journal of Child Psychology and Psychiatry. 1993;34(8):1409–1423. doi: 10.1111/j.1469-7610.1993.tb02099.x. [DOI] [PubMed] [Google Scholar]
- Gresham FM, Elliott SN. Social skills rating system (SSRS) Circle Pines, MN: American Guidance Service; 1990. [Google Scholar]
- Gunderson JG, Stout RL, McGlashan TH, Shea MT, Morey LC, Grilo CM, Skodol AE. Ten-year course of borderline personality disorder: Psychopathology and function from the Collaborative Longitudinal Personality Disorders Study. Archives of General Psychiatry. 2011;68(8):827–837. doi: 10.1001/archgenpsychiatry.2011.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hancock GR, Kuo WL, Lawrence FR. An Illustration of Second-Order Latent Growth Models. Structural Equation Modeling: A Multidisciplinary Journal. 2001;8(3):470–489. doi: 10.1207/S15328007SEM0803_7. [DOI] [Google Scholar]
- Heene M, Hilbert S, Freudenthaler HH, Bühner M. Sensitivity of SEM Fit Indexes With Respect to Violations of Uncorrelated Errors. Structural Equation Modeling: A Multidisciplinary Journal. 2012;19(1):36–50. doi: 10.1080/10705511.2012.634710. [DOI] [Google Scholar]
- Helgeland MI, Kjelsberg E, Torgersen S. Continuities between emotional and disruptive behavior disorders in adolescence and personality disorders in adulthood. American Journal of Psychiatry. 2005;162(10):1941–1947. doi: 10.1176/appi.ajp.162.10.1941. [DOI] [PubMed] [Google Scholar]
- Hill J, Pilkonis P, Morse J, Feske U, Reynolds S, Hope H, Broyden N. Social domain dysfunction and disorganization in borderline personality disorder. Psychological Medicine. 2008;38(1):135–146. doi: 10.1017/S0033291707001626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hinshaw SP. Process, mechanism, and explanation related to externalizing behavior in developmental psychopathology. Journal of Abnormal Child Psychology. 2002;30(5):431–446. doi: 10.1023/a:1019808712868. [DOI] [PubMed] [Google Scholar]
- Hinshaw SP, Owens EB, Zalecki C, Huggins SP, Montenegro-Nevado AJ, Schrodek E, Swanson EN. Prospective follow-up of girls with attention-deficit/hyperactivity disorder into early adulthood: Continuing impairment includes elevated risk for suicide attempts and self-injury. Journal of Consulting and Clinical Psychology. 2012;80(6):1041–1051. doi: 10.1037/a0029451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hipwell A, Keenan K, Kasza K, Loeber R, Stouthamer-Loeber M, Bean T. Reciprocal influences between girls’ conduct problems and depression, and parental punishment and warmth: a six year prospective analysis. Journal of Abnormal Child Psychology. 2008;36(5):663–677. doi: 10.1007/s10802-007-9206-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hopwood CJ, Morey LC, Edelen MO, Shea MT, Grilo CM, Sanislow CA, Skodol AE. A comparison of interview and self-report methods for the assessment of borderline personality disorder criteria. Psychological Assessment. 2008;20(1):81–85. doi: 10.1037/1040-3590.20.1.81. [DOI] [PubMed] [Google Scholar]
- Johnson JG, Cohen P, Brown J, Smailes EM, Bernstein DP. Childhood maltreatment increases risk for personality disorders during early adulthood. Archives of General Psychiatry. 1999;56(7):600–606. doi: 10.1001/archpsyc.56.7.600. [DOI] [PubMed] [Google Scholar]
- Johnson JG, Cohen P, Chen H, Kasen S, Brook JS. Parenting behaviors associated with risk for offspring personality disorder during adulthood. Archives of General Psychiatry. 2006;63(5):579–587. doi: 10.1001/archpsyc.63.5.579. [DOI] [PubMed] [Google Scholar]
- Johnson JG, Cohen P, Skodol AE, Oldham JM, Kasen S, Brook JS. Personality disorders in adolescence and risk of major mental disorders and suicidality during adulthood. Archives of General Psychiatry. 1999;56(9):805–811. doi: 10.1001/archpsyc.56.9.805. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Myers J, Reichborn-Kjennerud T. Borderline personality disorder traits and their relationship with dimensions of normative personality: a web-based cohort and twin study. Acta Psychiatrica Scandinavica. 2011;123(5):349–359. doi: 10.1111/j.1600-0447.2010.01653.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koenigsberg HW, Harvey PD, Mitropoulou V, New AS, Goodman M, Silverman J, Siever LJ. Are the interpersonal and identity disturbances in the borderline personality disorder criteria linked to the traits of affective instability and impulsivity? Journal of Personality Disorders. 2001;15(4):358–370. doi: 10.1521/pedi.15.4.358.19181. [DOI] [PubMed] [Google Scholar]
- Lahey BB. Public health significance of neuroticism. The American Psychologist. 2009;64(4):241–256. doi: 10.1037/a0015309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawrence KA, Allen JS, Chanen AM. Impulsivity in borderline personality disorder: reward-based decision-making and its relationship to emotional distress. Journal of Personality Disorders. 2010;24(6):786–799. doi: 10.1521/pedi.2010.24.6.785. [DOI] [PubMed] [Google Scholar]
- Lenzenweger MF. Stability and change in personality disorder features: The Longitudinal Study of Personality Disorders. Archives of General Psychiatry. 1999;56(11):1009–1015. doi: 10.1001/archpsyc.56.11.1009. [DOI] [PubMed] [Google Scholar]
- Lenzenweger MF, Lane MC, Loranger AW, Kessler RC. DSM-IV personality disorders in the National Comorbidity Survey Replication. Biological Psychiatry. 2007;62(6):553–564. doi: 10.1016/j.biopsych.2006.09.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lenzenweger MF, Loranger AW, Korfine L, Neff C. Detecting personality disorders in a nonclinical population. Application of a 2-stage procedure for case identification. Archives of General Psychiatry. 1997;54(4):345–351. doi: 10.1001/archpsyc.1997.01830160073010. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Rohde P, Seeley JR, Klein DN. Axis II psychopathology as a function of Axis I disorders in childhood and adolescence. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36(12):1752–1759. doi: 10.1097/00004583-199712000-00024. [DOI] [PubMed] [Google Scholar]
- Linehan MM. Cognitive-Behavioral Treatment of Borderline Personality Disorder. Guilford Press; 1993. [Google Scholar]
- Livesley WJ, Jang KL. The behavioral genetics of personality disorder. Annual Review of Clinical Psychology. 2008;4:247–274. doi: 10.1146/annurev.clinpsy.4.022007.141203. [DOI] [PubMed] [Google Scholar]
- MacKillop J, Mattson RE, Anderson Mackillop EJ, Castelda BA, Donovick PJ. Multidimensional assessment of impulsivity in undergraduate hazardous drinkers and controls. Journal of Studies on Alcohol and Drugs. 2007;68(6):785–788. doi: 10.15288/jsad.2007.68.785. [DOI] [PubMed] [Google Scholar]
- Miller AL, Muehlenkamp JJ, Jacobson CM. Fact or fiction: diagnosing borderline personality disorder in adolescents. Clinical Psychology Review. 2008;28(6):969–981. doi: 10.1016/j.cpr.2008.02.004. [DOI] [PubMed] [Google Scholar]
- Miller AL, Rathus JH, Linehan M. Dialectical behavior therapy with suicidal adolescents. 1. The Guilford Press; 2006. [Google Scholar]
- Millsap RE, Yun-Tein J. Assessing factorial invariance in ordered-categorical measures. Multivariate Behavioral Research. 2004;39(3):479–515. [Google Scholar]
- Muthén LK, Muthén BO. Mplus User’s Guide (version 7.0) Los Angeles, CA: Muthén and Muthén; 2013. [Google Scholar]
- Nunnally JC, Bernstein IH. Psychometric Theory. 3. New York: McGraw-Hill; 1994. [Google Scholar]
- Patterson GR, DeBaryshe BD, Ramsey E. A developmental perspective on antisocial behavior. American Psychologist. 1989;44(2):329–335. doi: 10.1037/0003-066X.44.2.329. [DOI] [PubMed] [Google Scholar]
- Peters JR, Upton BT, Baer RA. Brief report: relationships between facets of impulsivity and borderline personality features. Journal of Personality Disorders. 2013;27(4):547–552. doi: 10.1521/pedi_2012_26_044. [DOI] [PubMed] [Google Scholar]
- Pfohl B, Blum N, Zimmerman M. Structured Interview for DSM-IV Personality. Washington, DC: American Psychiatric Publishing; 1997. [Google Scholar]
- Posner MI, Rothbart MK. Developing mechanisms of self-regulation. Development and Psychopathology. 2000;12(3):427–441. doi: 10.1017/s0954579400003096. [DOI] [PubMed] [Google Scholar]
- Posner MI, Rothbart MK, Vizueta N, Thomas KM, Levy KN, Fossella J, Kernberg O. An approach to the psychobiology of personality disorders. Development and Psychopathology. 2003;15(4):1093–1106. doi: 10.1017/s0954579403000506. [DOI] [PubMed] [Google Scholar]
- Romer D, Duckworth AL, Sznitman S, Park S. Can Adolescents Learn Self-control? Delay of Gratification in the Development of Control over Risk Taking. Prevention Science: The Official Journal of the Society for Prevention Research. 2010;11(3):319–330. doi: 10.1007/s11121-010-0171-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rothbart MK, Ahadi SA, Evans DE. Temperament and personality: Origins and outcomes. Journal of Personality and Social Psychology. 2000;78(1):122–135. doi: 10.1037//0022-3514.78.1.122. http://dx.doi.org.pitt.idm.oclc.org/10.1037/0022-3514.78.1.122. [DOI] [PubMed] [Google Scholar]
- Scaramella LV, Conger RD, Spoth R, Simons RL. Evaluation of a Social Contextual Model of Delinquency: A Cross-Study Replication. Child Development. 2002;73(1):175–195. doi: 10.1111/1467-8624.00399. [DOI] [PubMed] [Google Scholar]
- Scaramella LV, Leve LD. Clarifying Parent–Child Reciprocities During Early Childhood: The Early Childhood Coercion Model. Clinical Child and Family Psychology Review. 2004;7(2):89–107. doi: 10.1023/B:CCFP.0000030287.13160.a3. [DOI] [PubMed] [Google Scholar]
- Schmitt N. Uses and abuses of coefficient alpha. Psychological Assessment. 1996;8(4):350. [Google Scholar]
- Seltzer M, Choi K, Thum YM. Examining relationships between where students start and how rapidly they progress: Using new developments in growth modeling to gain insight into the distribution of achievement within schools. Educational Evaluation and Policy Analysis. 2003;25(3):263–286. [Google Scholar]
- Snyder J, Schrepferman L, Peter CS. Origins of Antisocial Behavior Negative Reinforcement and Affect Dysregulation of Behavior as Socialization Mechanisms in Family Interaction. Behavior Modification. 1997;21(2):187–215. doi: 10.1177/01454455970212004. [DOI] [PubMed] [Google Scholar]
- Spear LP. The adolescent brain and age-related behavioral manifestations. Neuroscience and Biobehavioral Reviews. 2000;24(4):417–463. doi: 10.1016/s0149-7634(00)00014-2. [DOI] [PubMed] [Google Scholar]
- Steinberg L. We know some things: Parent–adolescent relationships in retrospect and prospect. Journal of Research on Adolescence. 2001;11(1):1–19. doi: 10.1111/1532-7795.00001. [DOI] [Google Scholar]
- Steinberg L, Albert D, Cauffman E, Banich M, Graham S, Woolard J. Age differences in sensation seeking and impulsivity as indexed by behavior and self-report: Evidence for a dual systems model. Developmental Psychology. 2008;44(6):1764–1778. doi: 10.1037/a0012955. [DOI] [PubMed] [Google Scholar]
- Steinberg L, Dahl R, Keating D, Kupfer DJ, Masten AS, Pine DS. The study of developmental psychopathology in adolescence: Integrating affective neuroscience with the study of context. In: Cicchetti D, Cohen DJ, editors. Developmental Psychopathology: Developmental Neuroscience. 2. 1–3, 2. Hoboken, NJ: John Wiley & Sons; 2006. pp. 710–741. [Google Scholar]
- Stepp SD, Burke JD, Hipwell AE, Loeber R. Trajectories of attention deficit hyperactivity disorder and oppositional defiant disorder symptoms as precursors of borderline personality disorder symptoms in adolescent girls. Journal of Abnormal Child Psychology. 2012;40(1):7–20. doi: 10.1007/s10802-011-9530-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stepp SD, Pilkonis PA, Hipwell AE, Loeber R, Stouthamer-Loeber M. Stability of borderline personality disorder features in girls. Journal of Personality Disorders. 2010;24(4):460–472. doi: 10.1521/pedi.2010.24.4.460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stepp SD, Whalen DJ, Scott LN, Zalewski M, Loeber R, Hipwell AE. Reciprocal effects of parenting and borderline personality disorder symptoms in adolescent girls. Development and Psychopathology. 2014;26(02):361–378. doi: 10.1017/S0954579413001041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terr LC, Kernberg PF. Resolved: Borderline personality exists in children under twelve. Journal of the American Academy of Child & Adolescent Psychiatry. 1990;29:478–483. doi: 10.1097/00004583-199005000-00025. [DOI] [PubMed] [Google Scholar]
- Tomarken AJ, Waller NG. Potential problems with “well fitting” models. Journal of Abnormal Psychology. 2003;112(4):578–598. doi: 10.1037/0021-843X.112.4.578. [DOI] [PubMed] [Google Scholar]
- Tsukayama E, Duckworth AL, Kim B. Domain-specific impulsivity in school-age children. Developmental Science. 2013;16(6):879–893. doi: 10.1111/desc.12067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webster-Stratton C, Reid MJ, Hammond M. Treating children with early-onset conduct problems: intervention outcomes for parent, child, and teacher training. Journal of Clinical Child and Adolescent Psychology. 2004;33(1):105–124. doi: 10.1207/S15374424JCCP3301_11. [DOI] [PubMed] [Google Scholar]
- Whalen DJ, Scott LN, Jakubowski KP, McMakin DL, Hipwell AE, Silk JS, Stepp SD. Affective behavior during mother-daughter conflict and borderline personality disorder severity across adolescence. Personality Disorders. 2014;5(1):88–96. doi: 10.1037/per0000059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Widaman KF, Ferrer E, Conger RD. Factorial Invariance within Longitudinal Structural Equation Models: Measuring the Same Construct across Time. Child Development Perspectives. 2010;4(1):10–18. doi: 10.1111/j.1750-8606.2009.00110.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Widom CS, Czaja SJ, Paris J. A prospective investigation of borderline personality disorder in abused and neglected children followed up into adulthood. Journal of Personality Disorders. 2009;23(5):433–446. doi: 10.1521/pedi.2009.23.5.433. [DOI] [PubMed] [Google Scholar]
- Winsper C, Zanarini M, Wolke D. Prospective study of family adversity and maladaptive parenting in childhood and borderline personality disorder symptoms in a non-clinical population at 11 years. Psychological Medicine. 2012;42(11):2405–2420. doi: 10.1017/S0033291712000542. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Frankenburg FR, Hennen J, Silk KR. Mental health service utilization by Borderline Personality Disorder patients and Axis II comparison subjects followed prospectively for 6 years. Journal of Clinical Psychiatry. 2004;65(1):28–36. doi: 10.4088/jcp.v65n0105. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Frankenburg FR, Khera GS, Bleichmar J. Treatment histories of borderline inpatients. Comprehensive Psychiatry. 2001;42(2):144–150. doi: 10.1053/comp.2001.19749. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Williams AA, Lewis RE, Reich RB, Vera SC, Marino MF, Frankenburg FR. Reported pathological childhood experiences associated with the development of borderline personality disorder. The American Journal of Psychiatry. 1997;154(8):1101–1106. doi: 10.1176/ajp.154.8.1101. [DOI] [PubMed] [Google Scholar]
- Zelkowitz P, Paris J, Guzder J, Feldman R. Diatheses and stressors in borderline pathology of childhood: the role of neuropsychological risk and trauma. Journal of the American Academy of Child and Adolescent Psychiatry. 2001;40(1):100–105. doi: 10.1097/00004583-200101000-00022. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.