Abstract
Background/Objectives
Inflammation and oxidative stress are central in many disease states. The major anti-oxidative enzymes contain selenium. The selenium intake in Europe is low, and supplementation with selenium and coenzyme Q10, important anti-oxidants, was evaluated in a previous study. The aim of this study was to evaluate response on the inflammatory biomarkers C-reactive protein, and sP-selectin, and their possible impact on cardiovascular mortality.
Subjects/Methods
437 elderly individuals were included in the study. Clinical examination, echocardiography, electrocardiography and blood samples were drawn. The intervention time was 48 months, and median follow-up was 5.2 years. The effects on inflammation/atherosclerosis were evaluated through analyses of CRP and sP-selectin. Evaluations of the effect of the intervention was performed using repeated measures of variance. All mortality was registered, and endpoints of mortality were assessed by Kaplan-Meier plots.
Results
The placebo group showed a CRP level of 4.8 ng/mL at the start, and 5.1 ng/mL at the study end. The active supplementation group showed a CRP level of 4.1 ng/mL at the start, and 2.1 ng/mL at the study end. SP-selectin exhibited a level of 56.6 mg/mL at the start in the placebo group and 72.3 mg/mL at the study end, and in the active group the corresponding figures were 55.9 mg/mL and 58.0 mg/mL. A significantly smaller increase was demonstrated through repeated measurements of the two biomarkers in those on active supplementation. Active supplementation showed an effect on the CRP and sP-selectin levels, irrespective of the biomarker levels. Reduced cardiovascular mortality was demonstrated in both those with high and low levels of CRP and sP-selectin in the active supplementation group.
Conclusion
CRP and sP-selectin showed significant changes reflecting effects on inflammation and atherosclerosis in those given selenium and coenzyme Q10 combined. A reduced cardiovascular mortality could be demonstrated in the active group, irrespective of biomarker level. This result should be regarded as hypothesis-generating, and it is hoped it will stimulate more research in the area.
Introduction
Inflammation is part of the atherosclerotic process in the body[1], but also in other processes, including different disease states such as e.g. cardiometabolic syndrome, acute coronary syndromes [2, 3], heart failure with preserved ejection fraction [4, 5] as well as heart failure with reduced ejection fraction [6, 7] and also in aortic stenosis [8] and rheumatoid inflammations that may predispose a patient to cardiovascular disease. Aging itself is also associated with an increased inflammatory response [9]. An increased inflammatory response in disease states or in the elderly can be a marker of disease progression as well as an indicator of a poorer prognosis [10]
Inflammation and atherosclerosis are interrelated conditions that are also associated with increased oxidative stress in the body [11]. The selenium-containing enzymes glutathione peroxidase, selenoprotein P and thioredoxin reductase are some of the major contenders in the defence against oxidative stress in the body [12]. An association between ischemic heart disease and intake of selenium has been discussed for a long time, [13, 14]. However, there are also conflicting reports on the effectiveness of intervention with selenium in cardiovascular disease [15–19].
The intake of selenium is generally low in Europe, and has been estimated to be around 40 μg/day [20]. The required intake of selenium in order to obtain optimal function of the intracellular enzyme glutathione peroxidase, and the extracellular protector selenoprotein P has been discussed, and Xia et al. reported a needed intake of 75 μg/day of selenium for adult Caucasians [21]. During conditions of increased oxidative stress and inflammation there is an increased need for intake of selenium [22]. A possible association between cardiovascular disease and death and intake of selenium has been discussed in the literature. Salonen et al. reported a 2.9 fold increase in cardiovascular mortality in those with a low selenium intake [14]. However, conflicting reports regarding the effectiveness of intervention with selenium on cardiovascular disease have also been published [15–19].
Coenzyme Q10 (ubiquinone) is present in all living cells in the body where it is an important antioxidant, but is also active in the mitochondrial respiratory chain. However, the endogenous production of coenzyme Q10 declines after the age of 20, and in the myocardial cells it is reduced to about half at the age of 80 years [23]. As observed by Xia et al. there is an important interrelationship between selenium and coenzyme Q10, as selenium (selenocystein) is needed for the reduction of ubiquinone to ubiquinol, the active form of coenzyme Q10 [24, 25]. This interrelationship might explain the conflicting results in studies performed in areas with low selenium intake, where just one of the substances has been supplemented.
There is sparse information of the supplementation of selenium and coenzyme Q10 combined. However, Kuklinski, in a small study, reported lower mortality, a decreased plasma level of the biomarker N-terminal fragment of proBrain Natriuretic Peptide (NT-proBNP), and increased cardiac function according to echocardiography in patients with myocardial infarction who received supplementation with selenium and coenzyme Q10 in combination. We have recently presented data from a prospective double-blind, placebo controlled study of elderly Swedish healthy individuals, given dietary supplementation of either selenium and coenzyme Q10 or placebo during four years of intervention [26]. The result was a reduction of cardiovascular mortality, increased cardiovascular function as seen in echocardiography, and a smaller increase in NT-proBNP as a result of the combined intervention.
The rationale for the present analysis is that selenium and coenzyme Q10 are two major contenders in the human oxidative defence system [12, 27–29]; thus, a possible contributable mechanism to the positive results might be a decreased inflammatory response by the dietary supplementation of selenium and coenzyme Q10.
One of the most commonly used biomarkers for inflammatory response in clinical practice is C-reactive protein (CRP). CRP is an acute phase reactant and a general marker of systemic inflammation, but also a well-known biomarker for cardiovascular risk[30]. sP-selectin (CD62P) is a cell adhesion molecule expressed on activated endothelial cells and involved in their leukocyte attachment during inflammation [31]. The predominant part of sP-selectin found in plasma originates from activated platelets, and is a biomarker for atherosclerosis. sP-selectin has also been reported to give reliable prognostic information regarding the atherothrombotic process and cardiovascular risk [32, 33].
The aim of the present study was to evaluate the effect of selenium and coenzyme Q10 on the inflammatory response as reflected by CRP and sP-selectin. A second aim was to determine whether selenium and coenzyme Q10 had an impact on the association between inflammation and mortality.
Methods
Study population
This is a secondary analysis of a prospective randomized double-blind placebo-controlled trial in an elderly community population of 443 individuals with an age between 70–88 years that has been previously reported [26, 34]. The present evaluation of sP-selectin and CRP, is a post hoc analysis, whereas the evaluation the effect of the intervention on inflammation was prespecified.
The first participant was included in January 2003, and the last participant concluded the study in February 2010. All participants received the intervention for 48 months during which they were re-examined every six months. During the study, all mortality was registered. In the study, 221 individuals received active supplementation of 200 μg/day organic selenium (SelenoPrecise®, Pharma Nord, Denmark), plus 200 mg/day of coenzyme Q10 (Bio-Quinon®, Pharma Nord, Denmark), and 222 individuals received a placebo. At inclusion all participants went through a clinical examination, new patient records were obtained, the New York Heart Association functional class was assessed, and an ECG and Doppler-echocardiography was performed. Informed consent was obtained from each patient. The study was approved by the Regional Ethical Committee and conforms to the ethical guidelines of the 1975 Declaration of Helsinki. (The Medical Product Agency declined to review the study protocol since the study was not considered a trial of a medication for a certain disease but rather one of food supplement commodities that are commercially available). This study was registered at Clinicaltrials.gov, and has the identifier NCT01443780.
Blood samples
Blood samples were collected while the participants were resting in supine position. Pre-chilled, EDTA-vials were used. The vials were centrifuged at 3000g, +4°C, and were then frozen at -70°C. No sample was thawed more than once.
sP-selectin
Soluble sP-selectin (sCD62P) was analysed utilizing an ELISA from R&D (Abingdon, UK). The intra-assay coefficient of variation (CV) was about 5% and the inter-assay CV about 9%.
C-reactive protein
hs-CRP was analysed on an Advia 1800 instrument (Siemens Healthcare Diagnostics, Stockholm, Sweden) using a latex-enhanced immunochemistry method with reagents from the same company. The detection limit was 0.12 mg/L. The total CV was 1.1% at 13.3 mg/L and 2.9% at 0.99 mg/L.
Statistics
Descriptive data are presented as percentages or mean ± SD. The Student’s unpaired two-sided T-test was used for continuous variables. Kaplan-Meier analyses and plots of cardiovascular mortality for the period of up to 5.2 years were made separately for CRP and sP-selectin, each divided in two at their median levels. Censored participants were those still living at the end of the study, or who had died for reasons other than cardiovascular disease. Completed participants were those who had died due to cardiovascular disease. Evaluating the P-values between the two groups of mortality at 1900 days was based on lifetable analyses using cumulative proportional surviving, and standard error of cumulated survivals to obtain a z-value. Evaluation of the effects of treatment were based on the group mean, but where the values of the individual participant were identified during the three different measured time points using a repeated measures of variance analysis. P-values < 0.05 were considered significant, based on a two-sided evaluation. All data were analysed using standard software (Statistica v. 12.0, Statsoft Inc, Tulsa, OK, USA.).
Results
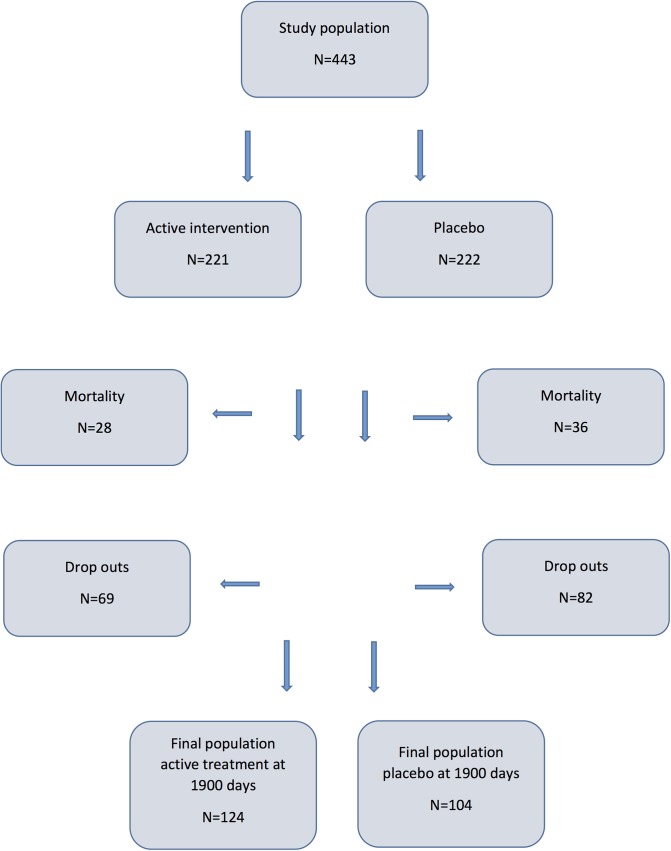
The baseline characteristics of the study population are presented in Table 1, and a CONSORT flow chart of the study is presented in Fig 1.
Table 1. Baseline characteristics of the study population receiving intervention of a dietary supplementation of selenium and coenzyme Q10 combined during 4 years.
| Active | Placebo | p-value | |
|---|---|---|---|
| N | 216 | 221 | |
| Age years mean (SD) | 76.9 (3.5) | 77.3 (3.4) | 0.35 |
| Males/Females n | 112/104 | 110/111 | |
| History | |||
| Smokers (present) n (%) | 20 (9.3) | 20 (9.0) | 0.94 |
| Diabetes n (%) | 46 (21.3) | 48 (21.7) | 0.91 |
| Hypertension n (%) | 155 (71.8) | 168 (76.0) | 0.31 |
| IHD n (%) | 45 (20.8) | 52 (23.5) | 0.50 |
| NYHA class I n (%) | 117 (54.2) | 107 (48.4) | 0.23 |
| NYHA class II n (%) | 58 (26.9) | 64 (29.0) | 0.62 |
| NYHA class III n (%) | 40 (18.5) | 47 (21.3) | 0.47 |
| NYHA class IV n (%) | 0 | 0 | |
| Medications | |||
| ACEI n (%) | 32 (14.8) | 53 (24.0) | 0.02 |
| ARB n (%) | 10 (4.6) | 13 (5.9) | 0.56 |
| Beta blockers n (%) | 75 (34.7) | 72 (32.6) | 0.64 |
| Digitalis n (%) | 10 (4.6) | 11 (5.0) | 0.87 |
| Diuretics n (%) | 68 (31.5) | 88 (39.8) | 0.07 |
| Statins n (%) | 42 (19.4) | 50 (22.6) | 0.41 |
| Examinations | |||
| EF<40% n (%) | 14 (6.5) | 17 (7.7) | 0.65 |
| NT-proBNP ng/L mean (IQR) | 537 (398) | 516 (330) | 0.86 |
| sP-Selectin mg/mL mean (IQR) | 55.9 (27.7) | 56.6 (31.4) | 0.75 |
| CRP mg/mL mean (IQR) | 4.0 (3.6) | 4.9 (4.0) | 0.45 |
Note: ACEI: ACE- inhibitors; ARB; Angiotension receptor blockers; EF: Ejection fraction; IHD; Ischemic heart disease; IQR: Inter quartile range; NT-proBNP: N-terminal fragment of proBNP; NYHA: New York Heart Association functional class; SD: Standard Deviation.
Fig 1. CONSORT diagram illustrating the design of the study.
In the population, 437 individuals were evaluated as 6 participants of the 443 did not deliver blood samples for analyses of sP-selectin. Almost equal numbers of males versus females were found (222 males versus 215 females). The two groups (active treatment versus placebo) were well balanced at the start except regarding treatment with ACE-inhibitors, regarding which a significantly greater part were on treatment in the placebo group (14.8% versus 24.0%; P = 0.02).
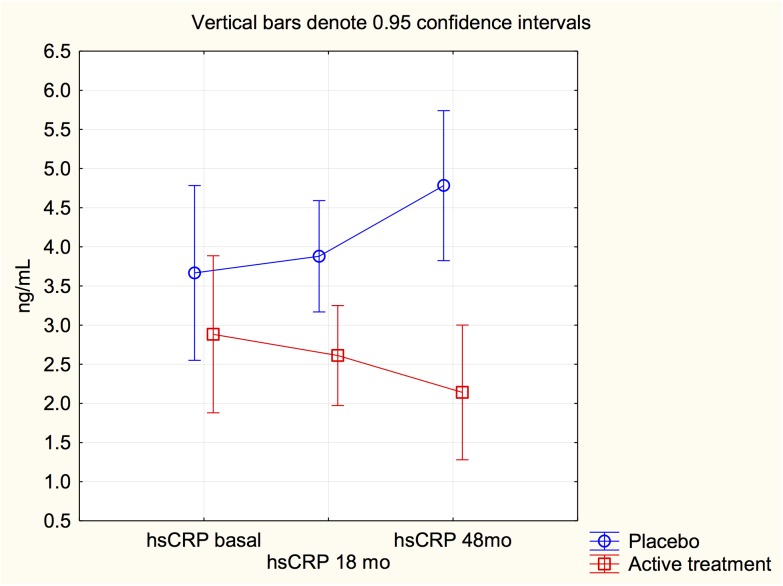
In the placebo group the mean concentration of CRP at study start was 4.8 ng/mL, whereas the mean concentration at study end was 5.1 ng/mL (P = 0.91) (Table 2).
Table 2. Levels of C-reactive protein and sP-selectin at study start, after 18 months and at study end in the placebo group, and in the active treatment group.
| CRP baseline (mg/mL) | CRP 18 months (mg/mL) | CRP 48 months (mg/mL9 | sP-selectin baseline (ng/ml) | sP-selectin 18 months (ng/mL) | sP-selectin 48 months (ng/mL) | |
|---|---|---|---|---|---|---|
| Placebo group, mean (SD) | 4.84 (12.0) | 3.69 (3.7) | 5.05 (6.2) | 56.6 (26.3 | 57.9 (24.8) | 72.3 (35.9) |
| Active treatment, mean (SD) | 4.06 (11.7) | 2.61 (3.2) | 2.07 (2.3) | 55.9 (22.4) | 54.5 (21.1) | 58.0 (19.2) |
Note: CRP: C-reactive protein.
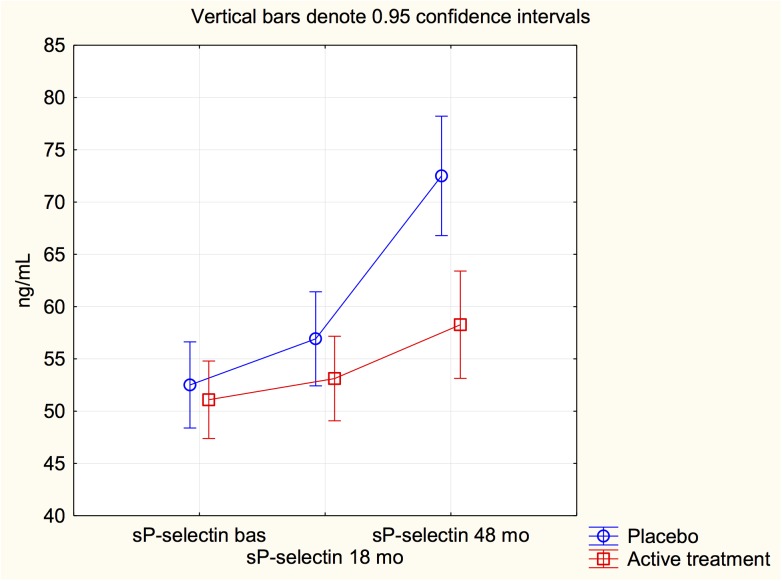
However, in the active treatment group the mean concentration of CRP at study start was 4.1 ng/mL and the concentration at study end was 2.1 ng/mL (t = -1.75; P = 0.08). Evaluating the soluble part of sP-selectin showed a concentration in the placebo group of 56.6 mg/mL at study start and a concentration of 72.3 mg/mL at study end (t = 4.39; P<0.0001). In the active treatment group a concentration of sP-selectin at study start of 55.9 mg/mL was found, and a concentration of 58.0 mg/mL at study end (t = 0.03; P = 0.97). Thus, a significant difference in sP-selectin concentration between the two groups during the intervention of 48 months could be seen, and a trend against difference comparing the concentration of CRP between the two groups.
However, to evaluate a possible treatment effect a repeated measures of variance was performed. The model which included the two groups (active and placebo) and the measured levels at three different time points (baseline, 18 and 48 months) showed a significant treatment effect on the CRP level (F = 8.67; P = 0.004), indicating that a significant difference between active intervention and placebo could be found. Evaluation of the interaction revealed a significant interaction (F = 4.73; P = 0.009) indicating that the obtained treatment effect was not based on difference in CRP level at start, but to a significantly reduced level of CRP due to the intervention (Fig 2).
Fig 2. Graph illustrating C-reactive protein measurements at study start, after 18 months and at study stop at 48 months in the study population given selenium and coenzyme Q10 combined, or placebo.
Note: Analysis according repeated measures of variance.
Performing the same procedure on the sP-selectin level showed a significant treatment effect (F = 6.52; P = 0.01), and a significant interaction (F = 7.08; P = 0.0009). Thus a significant treatment effect as seen on the sP-selectin level (Fig 3).
Fig 3. Graph illustrating sP-selectin measurements at study start, after 18 months and at study stop at 48 months in the study population given selenium and coenzyme Q10 combined, or placebo.
Note: Analysis according repeated measures of variance.
Association between inflammation and cardiovascular mortality
Of those having a CRP or sP-selectin concentration above or below the median value the distribution of cardiovascular death was examined as shown in Table 3.
Table 3. Distribution of cardiovascular mortality in placebo and active treatment groups above and below median value of C-reactive protein, and sP-selectin in the study population during 5 years of follow-up.
| CRP > median value | CRP < median value | sP-selectin > median value | sP-selectin < median value | |
|---|---|---|---|---|
| Active treatment | 8/103 | 5/113 | 8/104 | 5/112 |
| Placebo | 15/108 | 13/113 | 16/111 | 12/110 |
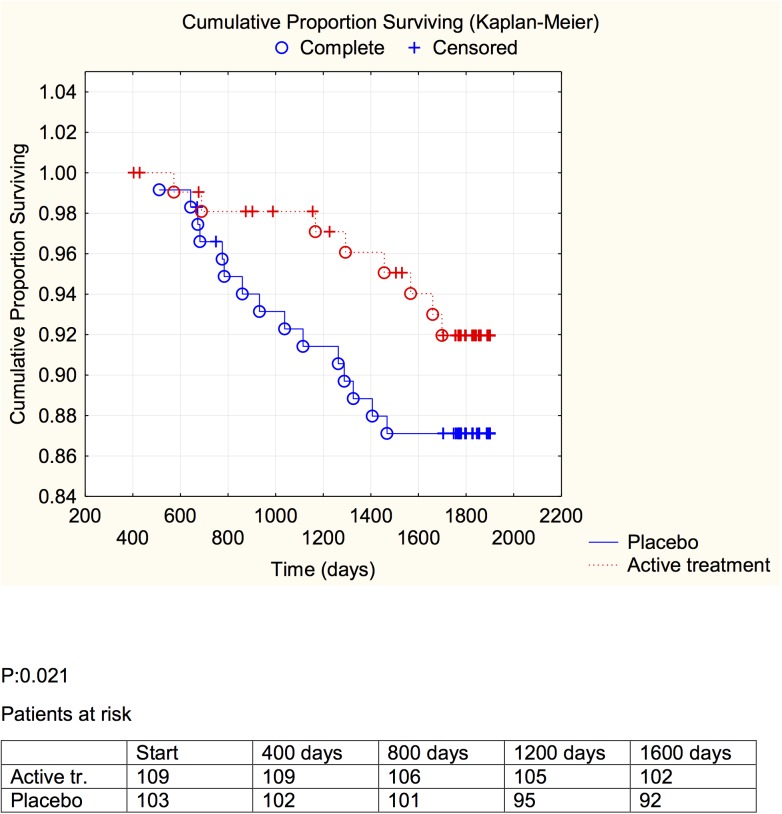
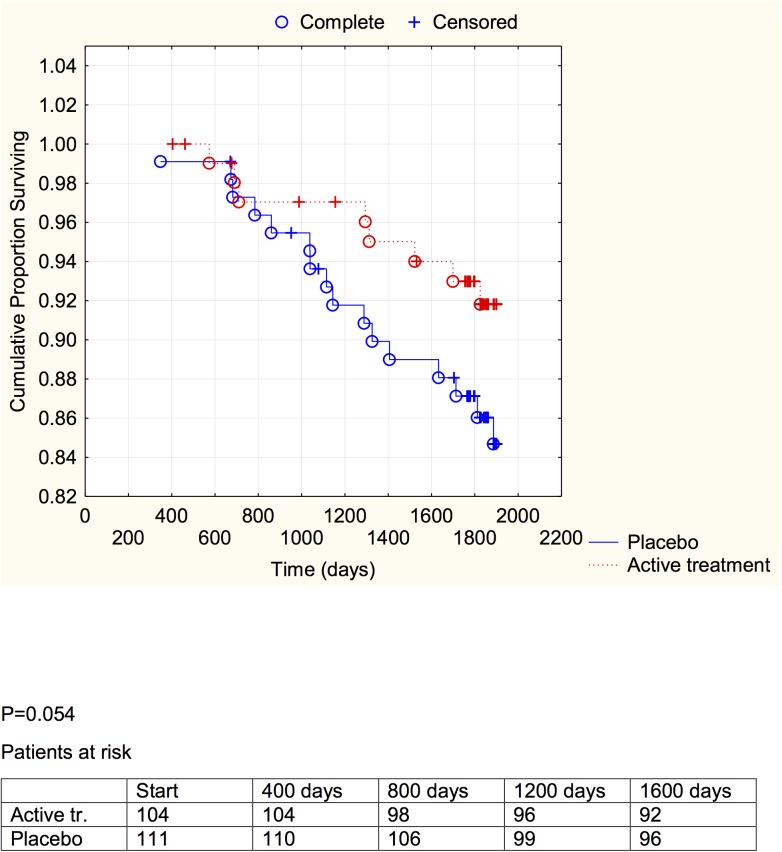
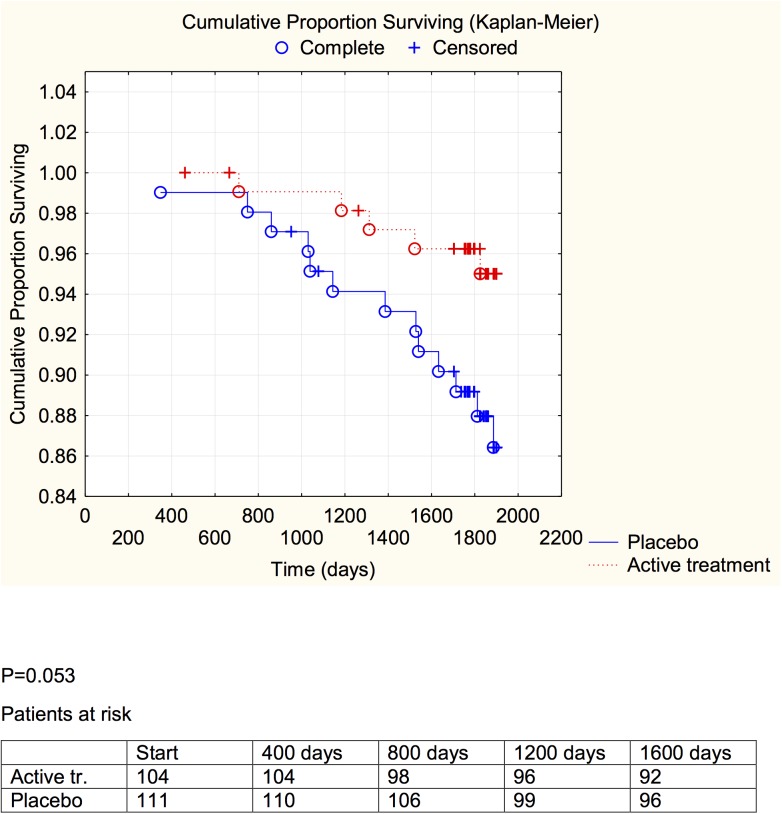
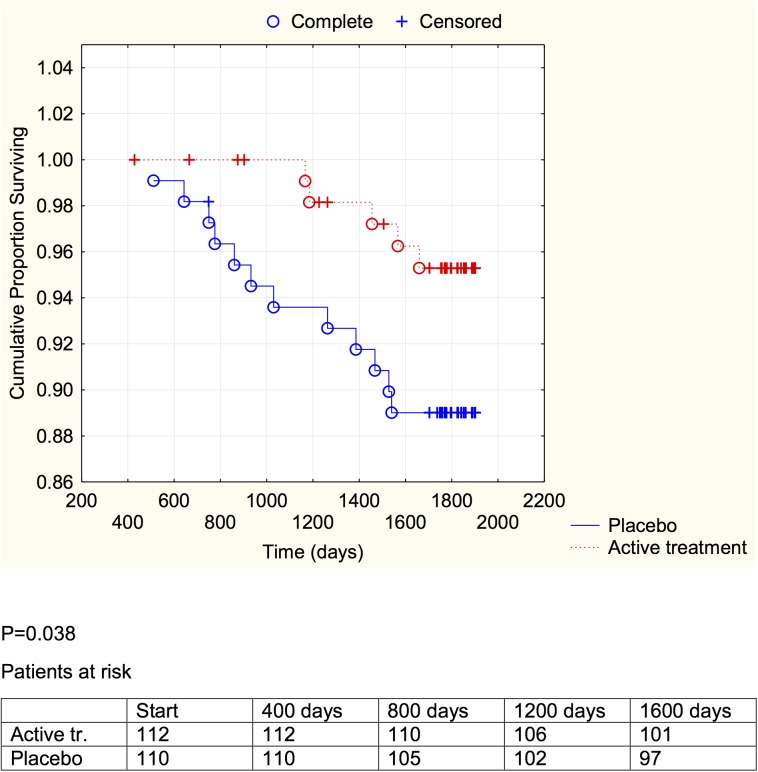
The extent of cardiovascular mortality in the active treatment group was about half of that in the placebo group, even though the size of the samples was small (Table 3). Using Kaplan-Meier graphs we also demonstrate the cardiovascular mortality during the study, in the active treatment and the placebo groups, evaluating the group having CRP or sP-selectin above and below median levels of the two biomarkers (Figs 4–7).
Fig 4. Distribution of cardiovascular mortality among those with a C-reactive protein concentration below median in those who received active supplementation of selenium and coenzyme Q10 combined versus placebo during follow-up of 5.2 years.
Fig 7. Distribution of cardiovascular mortality among those with a sP-selectin concentration above median in those who received active supplementation of selenium and coenzyme Q10 combined versus placebo followed during 5.2 years.
Fig 5. Distribution of cardiovascular mortality among those with a C-reactive protein concentration above median in those who received active supplementation of selenium and coenzyme Q10 combined versus placebo during follow-up of 5.2 years.
Fig 6. Distribution of cardiovascular mortality among those with a sP-selectin concentration below median in those who received active supplementation of selenium and coenzyme Q10 combined versus placebo during follow-up of 5.2 years.
A significant difference between the active treatment and placebo groups could be demonstrated in the groups with the inflammation markers below median (CRP: P = 0.021; sP-selectin: P = 0.038), and a weaker evidence, significant at the P<0.1 (CRP: P = 0.053; sP-selectin; P = 0.054) was found in the groups with above median concentration of the biomarker.
Discussion
In the present study, the dietary supplementation with selenium and coenzyme Q10 combined reduced the inflammatory response in elderly humans, as judged from measurements of CRP and the soluble part of sP-selectin.
We have previously reported an increase of sP-selectin in elderly community inhabitants as the participants became older [35], and this could be verified in the present study. Interestingly, the mean concentrations of sP-selectin as well as of CRP decreased during the intervention with selenium and coenzyme Q10 (Table 2), compared to the placebo group. We also performed evaluations using repeated measures of variance and thereby observed a significant difference between the active treatment, and the placebo groups, with lowered inflammatory biomarkers in the actively treated individuals. In the placebo group a small increase in both CRP and sP-selectin could be seen, which might reflect an age-related increase in the atherosclerosis process. However, the combined intervention appeared to protect against cardiovascular mortality irrespective of the increase in the inflammatory biomarkers (Table 3). Kaplan-Meier analyses of cardiovascular mortality were made separately for sP-selectin and CRP, each divided in two at their median value, a protective effect of active intervention with selenium and coenzyme Q10 could be revealed in both groups, although this was of marginal significance in those with the higher inflammatory response.
The mechanisms behind the effect of intervention with selenium and coenzyme Q10 combined, could be a result of several reactions:
It should be noted that the mean serum selenium concentration in the trial participants at baseline was low, viz. only about 67 μg/L [36]. The activity of the protective extracellular selenoprotein P does not plateau until a serum selenium concentration of about 120 μg/L is reached[37], and platelet GPX requires comparable selenium levels to be optimized [38]. Thus, selenoproteins that reduce oxidative stress and inflammation and thereby protect endothelial cells may operate sub-optimally in this un-supplemented elderly population, whereas supplementation may have raised and optimized platelet GPX and extracellular selenoprotein P in the majority of treated individuals.
Previous studies in comparable groups have shown that selenium supplementation decreased NF-κB activation and down-regulated the expression of inflammatory genes [39, 40].
The two selenoproteins GPX and thioredoxin reductase have been shown to protect endothelial cells from oxidants including oxidised LDL [41, 42]. In addition, selenoprotein P, which is recruited to the endothelial cells in areas of inflammation, scavenges inflammatory agents and shields endothelial membranes [43, 44]. Furthermore, another selenoprotein, selenoprotein S, plays a key role in the control of the inflammatory response [45]. Thus, a decreased inflammatory response may result from selenium supplementation alone. However, we consider it to be plausible that the observed anti-inflammatory effect results from a synergistic action of selenium and coenzyme Q10[11, 27]. Also, in an interventional study administering coenzyme Q10 to forty-three patients with coronary artery disease, Lee et al. reported signs of reduced oxidative stress as seen by decreased levels of malondialdehyde by 28% [46]. The correlations between CRP and sP-selectin in our groups were low or insignificant: for the placebo group the correlation was .27 (P = .007) and for the treatment group it was insignificant (r = .03). This indicates that the common variance was seven percent in the placebo group, and in the treatment group CRP and sP-selectin responses were independent. Accordingly, the different anti-inflammatory processes reflected by the two biomarkers were independent or differentiated in the treated group. Correspondingly, activation of platelets and inflammation form different parts of the atherothrombotic process, and the different parts may not have been synchronized in the treated group. However, our analyses suggest that intervention with selenium and coenzyme Q10 is effective, irrespective of the size of the inflammatory responses in the present elderly population with suboptimal selenium status.
The selenium intake among Europeans in general is low, as a result of low selenium content in the European soil, resulting in suboptimal levels for at least two of the major selenium containing enzymes, platelet glutathione peroxidase, and selenoprotein P [20]. Moreover, as the endogenous production of coenzyme Q10 declines after the age of 20, and at the age of 80 [47], only half of the coenzyme Q10 production can be found in the heart, a benefit from supplementation could be that it restores the intracellular antioxidant and anti-inflammatory potential. Thus, the effects on CRP and sPs-selectin could be a combined result of optimised selenium-containing enzymes [14, 48–50], combined with a restoration of decreased coenzyme Q10 levels. The positive results of our intervention in this minor cohort may be of importance for large-scale interventions on public health in Europe.
It is therefore important to stimulate further research in the area in order to expand our knowledge regarding the possibilities to interact in the process of antioxidative defence and inflammation.
Limitations
The study has a limited size, which is why some statistical evaluations are not meaningful, which restricts the information of this report. Also, the age span of the included participants was restricted to elderly persons, which makes extrapolations into other age groups difficult. However, we argue that the report should be regarded as a hypothesis-generating study, and as such it has interesting information that could be used in further research.
Conclusions
In this study, blood samples from more than 440 elderly community inhabitants in an intervention study using selenium and coenzyme Q10 combined as a dietary supplement were evaluated regarding the biomarkers C-reactive protein, and sP-selectin, which are markers for inflammation and atherosclerosis. It could be shown that in those treated with active supplementation, a significant reduction of both CRP and sP-selectin occurred compared to those receiving placebo over an intervention period of four years. The mechanism behind this effect is probably the anti-oxidative effects of both selenium and coenzyme Q10. As previously reported, reduced cardiovascular mortality has been demonstrated, which is probably associated with the decreased oxidative state in those receiving active supplementation. However, this is a small study, and further research is needed to shade light on the mechanisms.
Supporting Information
(DOCX)
Data Availability
Under Swedish Law, the authors cannot share the data underlying this study and cannot do any further research that what is specified in the ethical permissions application. For inquires on the data, researchers should first reach out to the owner of the database, the University of Linköping. Please reach out to the corresponding author with requests and for assistance with data requests. If the university approves the request, researchers can submit an application to the Regional Ethical Review Board for the specific research question that the researcher wants to examine.
Funding Statement
This work was supported by the County Council of Östergötland, Linköping University. The funder had no role in the design, management, analysis, interpretation of the data, preparation, review or approval of the manuscript.
References
- 1. Rafieian-Kopaei M, Setorki M, Doudi M, Baradaran A, Nasri H. Atherosclerosis: process, indicators, risk factors and new hopes. Int J Prev Med. 2014;5(8):927–46. [PMC free article] [PubMed] [Google Scholar]
- 2. Shantsila E, Tapp LD, Lip GY. Free Light Chains in patients with acute coronary syndromes: Relationships to inflammation and renal function. Int J Cardiol. 2015;185:322–7. 10.1016/j.ijcard.2015.03.105 . [DOI] [PubMed] [Google Scholar]
- 3. Libby P, Tabas I, Fredman G, Fisher EA. Inflammation and its resolution as determinants of acute coronary syndromes. Circ Res. 2014;114(12):1867–79. 10.1161/CIRCRESAHA.114.302699 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Glezeva N, Voon V, Watson C, Horgan S, McDonald K, Ledwidge M, et al. Exaggerated inflammation and monocytosis associate with diastolic dysfunction in heart failure with preserved ejection fraction: evidence of M2 macrophage activation in disease pathogenesis. J Card Fail. 2015;21(2):167–77. 10.1016/j.cardfail.2014.11.004 . [DOI] [PubMed] [Google Scholar]
- 5. Matsubara J, Sugiyama S, Nozaki T, Sugamura K, Konishi M, Ohba K, et al. Pentraxin 3 is a new inflammatory marker correlated with left ventricular diastolic dysfunction and heart failure with normal ejection fraction. J Am Coll Cardiol. 2011;57(7):861–9. 10.1016/j.jacc.2010.10.018 . [DOI] [PubMed] [Google Scholar]
- 6. Kalogeropoulos AP, Tang WH, Hsu A, Felker GM, Hernandez AF, Troughton RW, et al. High-sensitivity C-reactive protein in acute heart failure: insights from the ASCEND-HF trial. J Card Fail. 2014;20(5):319–26. 10.1016/j.cardfail.2014.02.002 . [DOI] [PubMed] [Google Scholar]
- 7. Askevold ET, Gullestad L, Dahl CP, Yndestad A, Ueland T, Aukrust P. Interleukin-6 signaling, soluble glycoprotein 130, and inflammation in heart failure. Curr Heart Fail Rep. 2014;11(2):146–55. 10.1007/s11897-014-0185-9 . [DOI] [PubMed] [Google Scholar]
- 8. Wallby L, Steffensen T, Jonasson L, Broqvist M. Inflammatory Characteristics of Stenotic Aortic Valves: A Comparison between Rheumatic and Nonrheumatic Aortic Stenosis. Cardiol Res Pract. 2013;2013:895215 10.1155/2013/895215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Guarner V, Rubio-Ruiz ME. Low-grade systemic inflammation connects aging, metabolic syndrome and cardiovascular disease. Interdiscip Top Gerontol. 2015;40:99–106. 10.1159/000364934 . [DOI] [PubMed] [Google Scholar]
- 10. Matera G, Puccio R, Giancotti A, Quirino A, Pulicari MC, Zicca E, et al. Impact of interleukin-10, soluble CD25 and interferon-gamma on the prognosis and early diagnosis of bacteremic systemic inflammatory response syndrome: a prospective observational study. Crit Care. 2013;17(2):R64 10.1186/cc12596 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Abramson JL, Hooper WC, Jones DP, Ashfaq S, Rhodes SD, Weintraub WS, et al. Association between novel oxidative stress markers and C-reactive protein among adults without clinical coronary heart disease. Atherosclerosis. 2005;178(1):115–21. Epub 2004/12/09. 10.1016/j.atherosclerosis.2004.08.007 . [DOI] [PubMed] [Google Scholar]
- 12. Fairweather-Tait SJ, Bao Y, Broadley MR, Collings R, Ford D, Hesketh JE, et al. Selenium in human health and disease. Antioxid Redox Signal. 2011;14(7):1337–83. Epub 2010/09/04. 10.1089/ars.2010.3275 . [DOI] [PubMed] [Google Scholar]
- 13. Eaton CB, Abdul Baki AR, Waring ME, Roberts MB, Lu B. The association of low selenium and renal insufficiency with coronary heart disease and all-cause mortality: NHANES III follow-up study. Atherosclerosis. 2010;212(2):689–94. Epub 2010/08/10. doi: S0021-9150(10)00511-3 [pii] 10.1016/j.atherosclerosis.2010.07.008 . [DOI] [PubMed] [Google Scholar]
- 14. Salonen JT, Alfthan G, Huttunen JK, Pikkarainen J, Puska P. Association between cardiovascular death and myocardial infarction and serum selenium in a matched-pair longitudinal study. Lancet. 1982;2(8291):175–9. Epub 1982/07/24. . [DOI] [PubMed] [Google Scholar]
- 15. Rees K, Hartley L, Day C, Flowers N, Clarke A, Stranges S. Selenium supplementation for the primary prevention of cardiovascular disease. Cochrane Database Syst Rev. 2013;1:CD009671 Epub 2013/02/27. 10.1002/14651858.CD009671.pub2 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Stranges S, Marshall JR, Trevisan M, Natarajan R, Donahue RP, Combs GF, et al. Effects of selenium supplementation on cardiovascular disease incidence and mortality: secondary analyses in a randomized clinical trial. Am J Epidemiol. 2006;163(8):694–9. Epub 2006/02/24. doi: kwj097 [pii] 10.1093/aje/kwj097 . [DOI] [PubMed] [Google Scholar]
- 17. Venardos KM, Perkins A, Headrick J, Kaye DM. Myocardial ischemia-reperfusion injury, antioxidant enzyme systems, and selenium: a review. Curr Med Chem. 2007;14(14):1539–49. Epub 2007/06/23. . [DOI] [PubMed] [Google Scholar]
- 18. Navas-Acien A, Bleys J, Guallar E. Selenium intake and cardiovascular risk: what is new? Curr Opin Lipidol. 2008;19(1):43–9. Epub 2008/01/17. 10.1097/MOL.0b013e3282f2b261 . [DOI] [PubMed] [Google Scholar]
- 19. Alissa EM, Bahijri SM, Ferns GA. The controversy surrounding selenium and cardiovascular disease: a review of the evidence. Med Sci Monit. 2003;9(1):RA9-18. Epub 2003/01/29. . [PubMed] [Google Scholar]
- 20. Rayman MP. Selenium and human health. Lancet. 2012;379(9822):1256–68. Epub 2012/03/03. 10.1016/S0140-6736(11)61452-9 . [DOI] [PubMed] [Google Scholar]
- 21. Xia Y, Hill KE, Li P, Xu J, Zhou D, Motley AK, et al. Optimization of selenoprotein P and other plasma selenium biomarkers for the assessment of the selenium nutritional requirement: a placebo-controlled, double-blind study of selenomethionine supplementation in selenium-deficient Chinese subjects. Am J Clin Nutr. 2010;92(3):525–31. Epub 2010/06/25. 10.3945/ajcn.2010.29642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Manzanares W, Biestro A, Galusso F, Torre MH, Manay N, Pittini G, et al. Serum selenium and glutathione peroxidase-3 activity: biomarkers of systemic inflammation in the critically ill? Intensive Care Med. 2009;35(5):882–9. Epub 2008/11/27. 10.1007/s00134-008-1356-5 . [DOI] [PubMed] [Google Scholar]
- 23. Sanoobar M, Eghtesadi S, Azimi A, Khalili M, Khodadadi B, Jazayeri S, et al. Coenzyme Q10 supplementation ameliorates inflammatory markers in patients with multiple sclerosis: a double blind, placebo, controlled randomized clinical trial. Nutr Neurosci. 2014. Epub 2014/03/14. 10.1179/1476830513Y.0000000106 . [DOI] [PubMed] [Google Scholar]
- 24. Xia L, Nordman T, Olsson JM, Damdimopoulos A, Bjorkhem-Bergman L, Nalvarte I, et al. The mammalian cytosolic selenoenzyme thioredoxin reductase reduces ubiquinone. A novel mechanism for defense against oxidative stress. J Biol Chem. 2003;278(4):2141–6. . [DOI] [PubMed] [Google Scholar]
- 25. Norman JA, Little D, Bolgar M, Di Donato G. Degradation of brain natriuretic peptide by neutral endopeptidase: species specific sites of proteolysis determined by mass spectrometry. Biochem Biophys Res Commun. 1991;175(1):22–30. . [DOI] [PubMed] [Google Scholar]
- 26. Alehagen U, Johansson P, Bjornstedt M, Rosen A, Dahlstrom U. Cardiovascular mortality and N-terminal-proBNP reduced after combined selenium and coenzyme Q10 supplementation: a 5-year prospective randomized double-blind placebo-controlled trial among elderly Swedish citizens. Int J Cardiol. 2013;167(5):1860–6. Epub 2012/05/26. 10.1016/j.ijcard.2012.04.156 . [DOI] [PubMed] [Google Scholar]
- 27. Onur S, Niklowitz P, Jacobs G, Nothlings U, Lieb W, Menke T, et al. Ubiquinol reduces gamma glutamyltransferase as a marker of oxidative stress in humans. BMC Res Notes. 2014;7:427 10.1186/1756-0500-7-427 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Duran-Prado M, Frontinan J, Santiago-Mora R, Peinado JR, Parrado-Fernandez C, Gomez-Almagro MV, et al. Coenzyme Q10 protects human endothelial cells from beta-amyloid uptake and oxidative stress-induced injury. PLoS One. 2014;9(10):e109223 10.1371/journal.pone.0109223 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Lee BJ, Tseng YF, Yen CH, Lin PT. Effects of coenzyme Q10 supplementation (300 mg/day) on antioxidation and anti-inflammation in coronary artery disease patients during statins therapy: a randomized, placebo-controlled trial. Nutr J. 2013;12(1):142 10.1186/1475-2891-12-142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Koenig W, Sund M, Frohlich M, Fischer HG, Lowel H, Doring A, et al. C-Reactive protein, a sensitive marker of inflammation, predicts future risk of coronary heart disease in initially healthy middle-aged men: results from the MONICA (Monitoring Trends and Determinants in Cardiovascular Disease) Augsburg Cohort Study, 1984 to 1992. Circulation. 1999;99(2):237–42. Epub 1999/01/20. . [DOI] [PubMed] [Google Scholar]
- 31. Hayashi S, Watanabe N, Nakazawa K, Suzuki J, Tsushima K, Tamatani T, et al. Roles of P-selectin in inflammation, neointimal formation, and vascular remodeling in balloon-injured rat carotid arteries. Circulation. 2000;102(14):1710–7. . [DOI] [PubMed] [Google Scholar]
- 32. Zamani P, Schwartz GG, Olsson AG, Rifai N, Bao W, Libby P, et al. Inflammatory biomarkers, death, and recurrent nonfatal coronary events after an acute coronary syndrome in the MIRACL study. J Am Heart Assoc. 2013;2(1):e003103 Epub 2013/03/26. 10.1161/JAHA.112.003103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Chen WS, Chen SJ, Lee CC, Cherng WJ, Liu MH, Wang CH. Plasma P-selectin predicts long-term cardiovascular events in hospitalized patients with suspected coronary artery disease and preserved left ventricular function: a 10-year follow-up study. Biomed J. 2013;36(3):137–43. Epub 2013/06/29. 10.4103/2319-4170.113231 . [DOI] [PubMed] [Google Scholar]
- 34. Johansson P, Dahlstrom O, Dahlstrom U, Alehagen U. Effect of selenium and Q10 on the cardiac biomarker NT-proBNP. Scand Cardiovasc J. 2013;47(5):281–8. Epub 2013/07/31. 10.3109/14017431.2013.820838 . [DOI] [PubMed] [Google Scholar]
- 35. Alehagen U, Lindahl TL. sP-selectin is a useful biomarker for cardiovascular risk; findings from an elderly primary healthcare population. Cardiovascular Endocrinology. 2015;4(1):22–7. [Google Scholar]
- 36. Alehagen U, Johansson P, Bjornstedt M, Rosen A, Post C, Aaseth J. Relatively high mortality risk in elderly Swedish subjects with low selenium status. Eur J Clin Nutr. 2015. 10.1038/ejcn.2015.92 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Hurst R, Armah CN, Dainty JR, Hart DJ, Teucher B, Goldson AJ, et al. Establishing optimal selenium status: results of a randomized, double-blind, placebo-controlled trial. Am J Clin Nutr. 2010;91(4):923–31. Epub 2010/02/26. 10.3945/ajcn.2009.28169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Neve J. Physiological and nutritional importance of selenium. Experientia. 1991;47(2):187–93. . [DOI] [PubMed] [Google Scholar]
- 39. Vunta H, Davis F, Palempalli UD, Bhat D, Arner RJ, Thompson JT, et al. The anti-inflammatory effects of selenium are mediated through 15-deoxy-Delta12,14-prostaglandin J2 in macrophages. J Biol Chem. 2007;282(25):17964–73. 10.1074/jbc.M703075200 . [DOI] [PubMed] [Google Scholar]
- 40. Vunta H, Belda BJ, Arner RJ, Channa Reddy C, Vanden Heuvel JP, Sandeep Prabhu K. Selenium attenuates pro-inflammatory gene expression in macrophages. Mol Nutr Food Res. 2008;52(11):1316–23. 10.1002/mnfr.200700346 . [DOI] [PubMed] [Google Scholar]
- 41. Brigelius-Flohe R, Banning A, Schnurr K. Selenium-dependent enzymes in endothelial cell function. Antioxid Redox Signal. 2003;5(2):205–15. 10.1089/152308603764816569 . [DOI] [PubMed] [Google Scholar]
- 42. Lewin MH, Arthur JR, Riemersma RA, Nicol F, Walker SW, Millar EM, et al. Selenium supplementation acting through the induction of thioredoxin reductase and glutathione peroxidase protects the human endothelial cell line EAhy926 from damage by lipid hydroperoxides. Biochim Biophys Acta. 2002;1593(1):85–92. . [DOI] [PubMed] [Google Scholar]
- 43. Arteel GE, Briviba K, Sies H. Protection against peroxynitrite. FEBS Lett. 1999;445(2–3):226–30. . [DOI] [PubMed] [Google Scholar]
- 44. Traulsen H, Steinbrenner H, Buchczyk DP, Klotz LO, Sies H. Selenoprotein P protects low-density lipoprotein against oxidation. Free Radic Res. 2004;38(2):123–8. . [DOI] [PubMed] [Google Scholar]
- 45. Gao Y, Hannan NR, Wanyonyi S, Konstantopolous N, Pagnon J, Feng HC, et al. Activation of the selenoprotein SEPS1 gene expression by pro-inflammatory cytokines in HepG2 cells. Cytokine. 2006;33(5):246–51. 10.1016/j.cyto.2006.02.005 . [DOI] [PubMed] [Google Scholar]
- 46. Lee BJ, Huang YC, Chen SJ, Lin PT. Coenzyme Q10 supplementation reduces oxidative stress and increases antioxidant enzyme activity in patients with coronary artery disease. Nutrition. 2012;28(3):250–5. 10.1016/j.nut.2011.06.004 . [DOI] [PubMed] [Google Scholar]
- 47. Kalen A, Appelkvist EL, Dallner G. Age-related changes in the lipid compositions of rat and human tissues. Lipids. 1989;24(7):579–84. Epub 1989/07/01. . [DOI] [PubMed] [Google Scholar]
- 48. Suadicani P, Hein HO, Gyntelberg F. Serum selenium concentration and risk of ischaemic heart disease in a prospective cohort study of 3000 males. Atherosclerosis. 1992;96(1):33–42. Epub 1992/09/01. . [DOI] [PubMed] [Google Scholar]
- 49. Akbaraly NT, Arnaud J, Hininger-Favier I, Gourlet V, Roussel AM, Berr C. Selenium and mortality in the elderly: results from the EVA study. Clin Chem. 2005;51(11):2117–23. Epub 2005/08/27. 10.1373/clinchem.2005.055301 . [DOI] [PubMed] [Google Scholar]
- 50. Millan Adame E, Florea D, Saez Perez L, Molina Lopez J, Lopez-Gonzalez B, Perez de la Cruz A, et al. Deficient selenium status of a healthy adult Spanish population. Nutr Hosp. 2012;27(2):524–8. 10.1590/S0212-16112012000200026 . [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
Data Availability Statement
Under Swedish Law, the authors cannot share the data underlying this study and cannot do any further research that what is specified in the ethical permissions application. For inquires on the data, researchers should first reach out to the owner of the database, the University of Linköping. Please reach out to the corresponding author with requests and for assistance with data requests. If the university approves the request, researchers can submit an application to the Regional Ethical Review Board for the specific research question that the researcher wants to examine.