Abstract
Background
Some oral hypoglycemic agents (OHAs) have been suggested to reduce the risk of cardiovascular disease (CVD) in type-2 diabetes mellitus (T2DM). We ascertained if OHAs affect CVD risk in a cohort analysis of a multicenter medical-cost accounting database in Japan.
Methods
Data of 4095 and 1273 T2DM patients in study 1 and study 2, respectively, were extracted from the database based on the following conditions: (i) began treatment with a single OHA (sulfonylurea, biguanide, thiazolidinedione, α-glucosidase inhibitor, glinide, or dipeptidyl peptidase-4 inhibitor) and continued the medication for ~1–1.4 years; (ii) hemoglobin (Hb)A1c level at baseline was available; (iii) age at baseline was 40–70 years; (iv) presence or absence of CVD history was not considered in study 1, but presence of CVD history was considered in study 2. Effects of OHAs relative to sulfonylurea on CVD risk according to ICD-10 were analysed using Kaplan-Meier curves during 104 weeks.
Results
In study 1 targeting T2DM patients with and without a history of CVD, initial and baseline treatment with a biguanide significantly lowered the risk of CVD compared with that with a sulfonylurea, and was independent of HbA1c control. In study 2, a similar significant preventive effect of a biguanide on CVD risk relative to a sulfonylurea was observed in T2DM patients with history of CVD.
Conclusions
Initial treatment and baseline treatment with a biguanide can reduce CVD risk relative to a sulfonylurea independent of the blood glucose-lowering effect of the biguanide in Japanese T2DM patients.
Electronic supplementary material
The online version of this article (doi:10.1186/s12902-015-0045-y) contains supplementary material, which is available to authorized users.
Background
Subjects with diabetes mellitus (DM) carry a higher risk of cardiovascular disease (CVD) than healthy individuals. A total of 40.4 % of individuals with type-2 DM (T2DM) die from CVD [1]. In an observational study in Finland, the prevalence of myocardial infarction (MI) in T2DM patients without a history of MI and in non-T2DM patients with a history of MI was similar (20.2 and 18.8 %, respectively) [2]. In Japan, the relative risk of coronary heart disease or cerebral infarction has been reported to be 3.0 compared with subjects with normal tolerance to glucose [3]. If MI occurs in a patient with DM, the risk of future mortality can increase by up to 4.6-fold compared with patients without DM without a history of MI [4]. However, the risk of CVD cannot be predicted completely by measuring levels of fasting blood glucose or hemoglobin (Hb)A1c, which is usually measured to observe the efficacy of anti-DM drugs for lowering glucose levels in blood. Several clinical trials have attempted to examine the incidence of CVD as a feature of drug efficacy [5–7].
Roumie et al. analyzed the efficacy of oral hypoglycemic agents (OHAs) for the prevention of cardiovascular events. They reported that metformin showed a significant reduction in the prevalence of death compared with a sulfonylurea (SU) [5]. The Study to Prevent Non-Insulin Dependent Diabetes Mellitus (STOP-NIDDM) revealed that the incidence of cardiovascular events or hypertension was reduced significantly in patients using one type of α-glucosidase inhibitor (α-GI): acarbose [7]. Meta-analyses of seven clinical trials focusing on acarbose showed similar results [8]. The thiazolidinedione (TZD) pioglitazone has been shown to slow atherosclerosis in T2DM patients as estimated by progression of maximal carotid intima-media thickness [9] and coronary atherosclerosis [10] compared with glimepiride. Glucagon-like peptide (GLP)-1-based therapy, which includes dipeptidyl peptidase (DPP)-4 inhibitors and GLP-1 receptor agonists, has become a popular treatment for patients with T2DM. The DPP-4 inhibitor sitagliptin has been speculated to lower the prevalence of CVD [11]. However, recent large-scale studies reported that, among patients with T2DM who had experienced acute coronary syndrome recently, the prevalence of major adverse cardiovascular events was not increased or decreased with the DPP-4 inhibitors saxagliptin [12] or alogliptin [13], as compared with placebo despite better control of HbA1c levels with both DPP-4 inhibitors than with placebo. Even if inconclusive, these results suggest that some OHAs may have beneficial effects in reducing CVD events in individuals with T2DM.
The actual treatment goal of HbA1c by OHAs is recommended to be 7.0 % (NGSP; National Glycohemoglobin Standardization Program) for the prevention of diabetic complication in Japan [14]. There are numerous difficulties in assessment of the reduction of cardiovascular risk by OHAs because a large volume of patient information must be collected. Moreover, few reliable medical databases are available in Japan, so data analyses are difficult. Consequently, in Japan, there is little evidence regarding reduction in cardiovascular risk by OHAs. One way to solve this problem may be to extract information from the National Health Insurance program in Japan. This program offers universal health coverage for all citizens (including comprehensive medical services and prescription medicines) and covers >99 % of Japanese citizens.
Previously, we investigated the utility of this type of multicenter medical-cost accounting database from T2DM patients in 15 hospitals (Medical Data Vision Co., Ltd. (MDV), Tokyo, Japan) by retrospective analyses. Statistical data of subjects showed an almost identical tendency with that of Patient Survey 2008 conducted by the Ministry of Health, Labour and Welfare in Japan (MHLWJ; estimated number of subjects = 2,386,000), including the ratio of patients according to sex, age distribution, and complications (e.g., dyslipidemia, hypertension). These findings suggested that the MDV database could reflect the current situation of T2DM in Japan [15]. Actually, the increased risk of acute pancreatitis in patients with T2DM using the MDV database has been reported recently [16]. In the present study, we wanted to ascertain if differences in reduction of the risk of CVD among various OHAs could be observed using the MDV database.
Methods
Source of data
The study protocol was approved by the Review Board on Clinical Research of Fukuoka University (Fukuoka, Japan). This retrospective observational study was done using a hospital-based composite database stored in hospital electronic-information systems constructed by MDV. MDV data were purchased by FUJIFILM Pharma Co., Ltd. A contract between FUJIFILM Pharma Co., Ltd., and Fukuoka University Hospital enabled analyses to be carried out. The current database of MDV has been expanded to a much greater extent than that reported previously [15]. The database of the medical information of patients (including laboratory data) was extracted from the medical-cost accounting system of 103 institutions (19 hospitals with <200 beds; 66 hospitals with 200–499 beds; and 18 hospitals with ≥500 beds) in Japan. This database contains information about age, sex, diagnosis, International Classification of Diseases (ICD)-10 code, surgical history, outpatient/inpatient status, prescriptions, and laboratory data. Written informed consent was not obtained from each patient because all data were extracted from the database retrospectively. Nevertheless, patient anonymity was guaranteed.
Population
Two studies (study 1 and study 2) were undertaken. The population of patients extracted in the present study satisfied the following conditions: (i) began treatment with a single OHA from 1 April 2008 to 30 April 2013; (ii) HbA1c level (NGSP) at baseline was available; (iii) age at baseline was 40–70 years; (iv) the presence or absence of CVD history was not considered in study 1, but the presence of CVD history was considered in study 2.
Exclusion criteria were: (i) began treatment with insulin, GLP-1 analog, or compounding agent at baseline; (ii) began treatment with ≥2 types of OHA; (iii) admitted to hospital at baseline; (iv) an anti-cancer drug was used before baseline measurements were taken; (v) The patient who was judged having a missing data by MDV Co., Ltd. The MDV database in 2013 contained the data of 225,197 individuals. Among them, the baseline value of HbA1c was available for 29,074 patients. After careful adherence to inclusion and exclusion criteria, 4095 and 1273 individuals were subjected to cohort analyses of study 1 and study 2, respectively. Outlines as well as the classification of inclusion and exclusion in study 1 and study 2 are summarized in Figs. 1 and 2. Patients with cancer or liver cirrhosis were not listed in any drug groups. However, renal failure was noted in study 1: 2/629 (0.3 %) in the SU group, 4/1305 (0.3 %) in the BG group, 2/592 (0.3 %) in the α-GI group, 2/351 (0.6 %) in the TZD group, 2/223 (0.9 %) in the glinide group, and 6/995 (0.6 %) in the DPP-4 inhibitor group. Renal failure was also noted in study 2: 1/228 (0.4 %) in the SU group, 0/325 (0 %) in the BG group, 0/203 (0 %) in the α-GI group, 1/140 (0.7 %) in the TZD group, 2/70 (2.9 %) in the glinide group, and 6/307 (2.0 %) in the DPP-4 inhibitor group. However, there was no significant difference in the involvement of renal failure among the above 6 groups by Chi-squared test, suggesting little impact on the analysis. So we retained these data for the analysis.
Fig. 1.
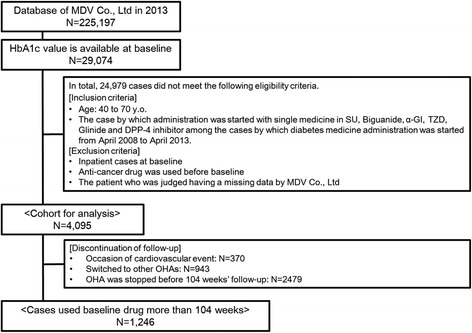
Outline and flowchart of the protocol for patient selection for analyses of cardiovascular events in study 1
Fig. 2.
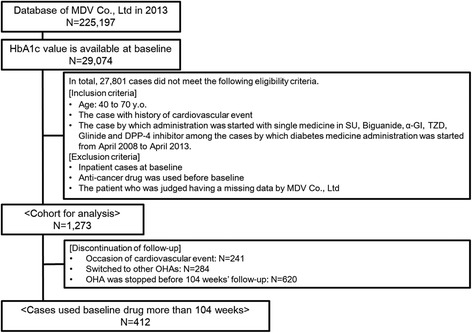
Outline and flowchart of the protocol for patient selection for analyses of cardiovascular events in study 2
Definition of a cardiovascular event
Information regarding cardiovascular events was obtained from the MDV database. A cardiovascular event was defined as suffering angina pectoris (codes I200, I201, I208 and I209), MI (I210–I213, I219, I220, I221 and I229), heart failure (I500, I501 and I509), cerebral infarction (I630–I635, I638 and I639), cerebral hemorrhage (I614 and I619), or subarachnoid hemorrhage (I600–I602, I604, I605 and I609).
Follow-up study
Observation was stopped at the time of: (i) a cardiovascular event; (ii) changing of the OHA at baseline; (iii) discontinuation of the drug at baseline before a prescription period of 2 years. However, observation was not suspended if a new OHA was added to the first drug. Finally, 1246 subjects and 412 cases in study 1 and study 2, respectively, were treated continuously by a baseline drug without a cardiovascular event being recorded for >2 years (summarized in Figs. 1 and 2).
Data analyses
Baseline characteristics of patients (sex, age, HbA1c level, use of other drugs (anti-hypertension or anti-dyslipidemia)) and cardiovascular events were analyzed. Subjects were divided into six groups according to the baseline drug. Prevalence of CVD and change in HbA1c level from baseline in each drug group was assessed.
Statistical analyses
To verify the independence of the analysis in the present study, statistical evaluation was undertaken by a specialist organization (ING Corp., Tokyo, Japan). ING Corp., are in no way associated with our institution or any drug company (including FUJIFILM Pharma Co., Ltd.). Statistical analyses were done using SAS v9.1.3 for Windows (SAS Institute, Cary, NC, USA). Prevalence of CVD in each group was investigated by Kaplan-Meier analyses. Comparisons between groups were achieved using the Cox-proportional hazard model adjusted for sex, age, HbA1c level (NGSP), use or non-use of anti-hypertensive drugs, and use or non-use of anti-dyslipidemia drugs. For consideration of the type-1 error in the Student’s t-test, patient characteristics at baseline between two groups (SU vs BG, SU vs α-GI, SU vs TZD, SU vs glinide, and SU vs DPP-4 inhibitor) were compared by the Dunnett test. P < 0.05 was considered significant.
Results
Validity of the database
The Japanese Patient Survey of 2011 for patients with DM was published by the MHLWJ. Hence, we compared our extracted database from 2013 with that of the MHLWJ. Our database contained 225,197 subjects and the percentage of males was 60.7 %. Based on data from the MHLWJ, the estimated number of subjects with DM in Japan was 2,700,000, and the percentage of males was 55.1 %. Age distribution of subjects with DM in our database was 5.8 % in their forties, 13.8 % in their fifties, 28.6 % in their sixties, 29.9 % in their seventies, and 15.8 % in their eighties, whereas that for the MHLWJ was 5.6, 13.7, 32.4, 31.1, and 13.4 %, respectively. The percentage of males in our database was 71.5 % in their forties, 68.7 % in their fifties, 65.6 % in their sixties, 60.2 % in their seventies, and 47.3 % in their eighties, whereas that of MHLWJ was 68.2, 61.2, 57.8, 53.8 and 40.9 %, respectively. These results suggested that our database could reflect the current situation of DM in Japan, as reported previously.
Baseline characteristics of patients
Baseline characteristics of 4095 subjects in study 1 and 1273 subjects in study 2, including the six groups based on the type of OHA (i.e., SU, biguanide, α-GI, TZD, glinide, DPP-4 inhibitor) are shown in Tables 1 and 2, respectively. Mean age of biguanide and TZD groups was slightly (but significantly) younger than the SU group in study 1 and study 2. Treatment with anti-hypertension and anti-dyslipidemia drugs was undertaken in all OHA groups. The detailed classification of antihypertensive drugs and anti-dyslipidemia drugs used in subjects of study 1 and 2 are shown in Additional files 1 and 2, respectively. Mean HbA1c levels (NGSP) of biguanide, α-GI, TZD and glinide were slightly (but significantly) lower than those of the SU group in study 1 and study 2. Prevalence of patients with a high HbA1c value (≥6.5 %) was not significantly different between the SU group and the other groups in study 1 and study 2. Mean duration of administration of baseline drugs was 320–457 days in study 1 and 330–540 days in study 2. In study 1, the duration of administration of BG, α-GI, TZD and glinide was not significantly different from that of SU, but that of DPP-4 inhibitor was significantly shorter than that of SU. In study 2, the duration of administration of BG was significantly longer than that of SU, and that of DPP-4 inhibitor was significantly shorter than that of SU.
Table 1.
Clinical profiles of T2DM patients treated with oral hypoglycemic agents (OHAs) in study 1
| SU | BG | α-GI | TZD | Glinide | DPP-4 inhibitor | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N = 629 | N = 1305 | P-value | N = 592 | P-value | N = 351 | P-value | N = 223 | P-value | N = 995 | P-value | ||
| Age | 62 (60.8 ± 7.1) | 59 (58.0 ± 7.9) | <0.001 | 61 (60.1 ± 7.3) | 0.38 | 60 (59.5 ± 7.2) | 0.044 | 61 (60.4 ± 6.9) | 0.95 | 62 (60.0 ± 7.6) | 0.15 | |
| Male | 454 (72.2) | 823 (63.1) | - | 393 (66.4) | - | 236 (66.4) | - | 140 (62.8) | - | 634 (63.7) | - | |
| Anti-hypertensive agent and anti-dyslipidemia agent | None | 181 (28.8) | 486 (37.2) | - | 176 (29.7) | - | 93 (26.5) | - | 79 (35.4) | - | 310 (31.2) | - |
| Both of them | 174 (27.7) | 318 (24.4) | - | 212 (25.8) | - | 115 (32.8) | - | 51 (22.9) | 302 (30.4) | - | ||
| One of them | 274 (43.6) | 501 (38.4) | - | 204 (34.5) | - | 143 (40.7) | - | 93 (41.7) | - | 383 (38.5) | - | |
| HbA1c (NGSP %) | 7.4 (7.9 ± 1.7) | 7.2 (7.7 ± 1.6) | 0.004 | 6.7 (6.9 ± 1.2) | <0.001 | 6.7 (6.9 ± 1.2) | <0.001 | 7.0 (7.1 ± 1.3) | <0.001 | 7.4 (7.8 ± 1.5) | 0.90 | |
| Minimum | 4.7 | 5.0 | 4.9 | 5.1 | 4.6 | 5.1 | ||||||
| Maximum | 14.5 | 15.1 | 15.5 | 12.2 | 15 | 17.7 | ||||||
| <6.5 % | 100 (15.9) | 216 (16.6) | 224 (37.8) | 125 (35.6) | 60 (26.9) | 89 (8.9) | ||||||
| - | - | - | - | - | ||||||||
| 6.5% ≤ | 529 (84.1) | 1089 (83.5) | 369 (62.2) | 226 (64.4) | 163 (73.1) | 906 (91.1) | ||||||
| Duration of administration of baseline drug (days) | 537 (457 ± 282) | 612 (476 ± 278) | 0.45 | 486 (453 ± 273) | 1.00 | 521 (473 ± 249) | 0.86 | 575 (499 ± 246) | 0.16 | 281 (320 ± 241) | <0.001 | |
Data are n(%) or median (mean ± standard deviation). P-value: Dunnett’s test for SU
Table 2.
Clinical profiles of T2DM patients treated with oral hypoglycemic agents (OHAs) in study 2
| SU | BG | α-GI | TZD | Glinide | DPP-4 inhibitor | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N = 228 | N = 325 | P-value | N = 203 | P-value | N = 140 | P-value | N = 70 | P-value | N = 307 | P-value | ||
| Age | 63.5 (62.4 ± 6.3) | 61 (60.8 ± 6.7) | 0.025 | 63 (61.3 ± 6.9) | 0.27 | 62 (60.5 ± 6.7) | 0.028 | 62 (61.1 ± 6.1) | 0.50 | 63 (61.6 ± 6.8) | 0.52 | |
| Male | 183 (80.3) | 206 (63.4) | - | 152 (74.9) | - | 101 (72.1) | - | 50 (71.4) | - | 216 (70.4) | - | |
| Anti-hypertensive agent and anti-dyslipidemia agent | None | 24 (10.5) | 49 (15.1) | - | 21 (10.3) | - | 20 (14.3) | - | 11 (15.7) | - | 34 (11.1) | - |
| Both of them | 109 (47.8) | 141 (43.4) | - | 126 (62.1) | - | 67 (47.9) | - | 30 (42.9) | - | 166 (54.1) | - | |
| One of them | 95 (41.7) | 135 (41.5) | - | 56 (27.6) | - | 53 (37.9) | - | 29 (41.4) | - | 107 (34.9) | - | |
| HbA1c (NGSP %) | 7.3 (7.6 ± 1.5) | 6.9 (7.1 ± 1.1) | <0.001 | 6.6 (6.7 ± 1.0) | <0.001 | 6.5 (6.8 ± 1.2) | <0.001 | 6.9 (6.9 ± 0.9) | <0.001 | 7.3 (7.6 ± 1.3) | 0.97 | |
| Minimum | 4.7 | 5.4 | 4.9 | 5.1 | 4.8 | 5.1 | ||||||
| Maximum | 14.1 | 14.4 | 11.4 | 11.8 | 9.4 | 13.7 | ||||||
| <6.5% | 44 (19.3) | 78 (24.0) | 87 (42.9) | 62 (44.3) | 21 (30.0) | 29 (9.4) | ||||||
| - | - | - | - | - | ||||||||
| 6.5 % ≤ | 184 (80.7) | 24.7 (76.0) | 116 (57.1) | 78 (55.7) | 49 (70.0) | 278 (90.6) | ||||||
| Duration of administration of baseline drug (days) | 616 (477 ± 279) | 730 (540 ± 261) | 0.022 | 700 (510 ± 263) | 0.56 | 596.5 (499 ± 251) | 0.90 | 524.5 (485 ± 251) | 1.00 | 302 (330 ± 245) | <0.001 | |
Data are n(%) or median (mean ± standard deviation). P-value: Dunnett’s test for SU
Prevalence of cardiovascular events in each group
Detailed data on the prevalence of cardiovascular events in study 1 and study 2 are shown in Table 3A and B, respectively. Based on these data, composite (cardiac and cerebrovascular) cardiovascular events were used mainly for statistical analyses subsequently because meaningful values could not be obtained in the analysis of cerebral events only due to the small number of events. The number of cardiovascular events (1000 person-years) is shown in Table 4A and B.
Table 3.
Number of cardiovascular events in subjects in study 1 (A) and study 2 (B)
| OHAs (Administration of one medicine) | Cardiovascular events (patients) | Cardiac events (patients) | Stroke (patients) | Analysis |
|---|---|---|---|---|
| (A) | ||||
| SU | 80 | 71 | 10 | 629 |
| Biguanide | 84 | 76 | 10 | 1305 |
| α-GI | 63 | 58 | 7 | 592 |
| TZD | 35 | 29 | 6 | 351 |
| Glinide | 21 | 19 | 3 | 223 |
| DPP-4 inhibitor | 87 | 80 | 8 | 995 |
| (B) | ||||
| SU | 58 | 53 | 6 | 228 |
| Biguanide | 47 | 48 | 4 | 325 |
| α-GI | 40 | 40 | 3 | 203 |
| TZD | 26 | 24 | 3 | 140 |
| Glinide | 14 | 14 | 1 | 70 |
| DPP-4 inhibitor | 56 | 57 | 3 | 307 |
Cardiovascular event: angina pectoris, myocardial infarction, heart failure, cerebral infarction, cerebral hemorrhage and subarachnoid hemorrhage
Cardiac event: angina pectoris, myocardial infarction and heart failure
Stroke event: cerebral infarction, cerebral hemorrhage and subarachnoid hemorrhage
Table 4.
Number of cardiovascular events (1000 person-years) in subjects in study 1 (A) and study 2 (B)
| N | The number of cardiovascular events | 1000 person-years | |
|---|---|---|---|
| (A) | |||
| SU | 629 | 80 | 108.9 |
| BG | 1305 | 84 | 51.0 |
| α-GI | 592 | 63 | 91.3 |
| TZD | 351 | 35 | 82.3 |
| Glinide | 223 | 21 | 71.2 |
| DPP-4 inhibitor | 995 | 87 | 105.2 |
| (B) | |||
| SU | 228 | 58 | 224.0 |
| BG | 325 | 47 | 106.2 |
| α-GI | 203 | 40 | 159.4 |
| TZD | 140 | 26 | 154.7 |
| Glinide | 70 | 14 | 162.1 |
| DPP-4 inhibitor | 307 | 56 | 222.7 |
Kaplan-Meier curves for T2DM patients who experienced ≥1 cardiovascular event in each group and statistical comparisons between SU and other drugs in study 1 are shown in Fig. 3. For determination of the hazard ratio (HR), the Cox proportional hazard model was adjusted for sex, age, HbA1c value (NGSP), use or non-use of anti-hypertensive drugs, and use or non-use of anti-dyslipidemia drugs. During a 104-week observation period, patients who began treatment with BG showed a significantly lower risk of cardiovascular events compared with those who started treatment with SU. HR of BG relative to SU was 0.603 (95 % confidence interval [CI], 0.439–0.829, P = 0.002). Significant risk reduction by BG relative to SU was also observed in analyses of cardiac events only (HR, 0.613; 95 % CI, 0.438–0.857; P = 0.004). However, α-GI, TZD, glinide and DPP-4 inhibitor did not show such significant reduction in risk compared with SU in terms of cardiovascular events and cardiac events (data not shown). A similar analysis using Kaplan-Meier curves targeting T2DM patients who did not have a history of cardiovascular events (n = 2822) did not show a significant difference in the prevalence of cardiovascular events between SU and other OHAs (data not shown).
Fig. 3.

Kaplan-Meier curve for cardiovascular events during 104 weeks in patients with T2DM with or without a history of cardiovascular events. Number of patients in each drug group is listed in Table 1. Numbers of those in which 104-week follow-up was completed were 629 in SU, 1305 in biguanide, 592 in α-GI, 351 in TZD, 223 in glinide, and 995 in DPP-4 inhibitor groups, respectively (Table 1). Numbers of those in which a cardiovascular event was observed were 80 in SU, 84 in biguanide, 63 in α-GI, 35 in TZD, 21 in glinide, and 87 in DPP-4 inhibitor groups, respectively (Table 3A). Statistical comparison of cardiovascular events during 104 weeks in patients with T2DM with a history of cardiovascular events is shown in the inserted small table. Hazard ratio, Cox proportional hazard model adjusted by sex, age, HbA1c value (NGSP), use or non-use of anti-hypertensive drugs, use or non-use of anti-dyslipidemia drugs. CI indicates a 95 % confidence interval. **P < 0.01
Kaplan-Meier curves for T2DM patients who had history of CVD events (study 2) revealed that the BG group also significantly reduced the risk of cardiovascular events relative to the SU group. The Cox proportional hazard model was adjusted for sex, age, HbA1c value (NGSP), use or non-use of anti-hypertensive drugs, and use or non-use of anti-dyslipidemia drugs, and HR was determined to be 0.566 (95 % CI, 0.376–0.852, P = 0.006). However, a significant reduction in risk by BG relative to SU was not observed if analyses were restricted to cardiac events or stroke events (data not shown). With regard to all other OHAs, significance was not observed in the risk reduction of cardiovascular events, cardiac events, or stroke events (data not shown).
Changes in HbA1c levels during the observation period
Changes in HbA1c levels from baseline (0 week) to 2 years (104 weeks) in patients in whom a cardiovascular event was observed were compared among OHAs. In patients who began treatment with SU, BG, α-GI, a TZD, glinide or DPP-4 inhibitor, the HbA1c level was reduced with SU, BG, α-GI, a TZD and DPP-4 inhibitor, but was increased with glinide. The maximum lowering effect in HbA1c level was observed in the DPP-4 inhibitor group. The difference in the change in HbA1c level between SU (−0.31 ± 0.07, N = 236) and glinide (0.08 ± 0.12, N = 81), and between SU and DPP-4 inhibitor (−0.75 ± 0.11, N = 95) was significant (P = 0.0005 and P < 0.0001, respectively). However, the extent of change in the level of BG (−0.30 ± 0.05, N = 542), α-GI (−0.21 ± 0.08, N = 195) and TZD (−0.31 ± 0.11, N = 92) relative to that of SU was not significant (P = 0.90, P = 0.37 and P = 0.95, respectively). Similar results were observed in study 2. The difference in the change in HbA1c level between SU (−0.43 ± 0.11, N = 80) and TZD (−0.003 ± 0.16, N = 42) and between SU and glinide (0.50 ± 0.20, N = 24) was significant (P = 0.029 and P < 0.001, respectively). However, the extent of change in the level of BG (−0.19 ± 0.08, N = 159), α-GI (−0.19 ± 0.11, N = 80) and DPP-4 inhibitor (−0.27 ± 0.20, N = 27) relative to that of SU was not significant (P = 0.069, P = 0.12 and P = 0.48, respectively).
Discussion
In the present study, T2DM patients who started treatment with BG showed a significantly lower prevalence of cardiovascular events compared with those who started treatment with SU. This phenomenon was unrelated to the presence or absence of CVD history.
Our results are based on a comparison of OHAs with SU, and do not suggest that cardiovascular risk is reduced by BG but increased with SU. There were slight differences in the backgrounds of patients in the six OHA groups (e.g., slightly lower mean age and HbA1c level in the BG group compared with the SU group). For determination of the HR, the Cox proportional hazard model was adjusted for sex, age, HbA1c value (NGSP), use or non-use of anti-hypertensive drugs, and use or non-use of anti-dyslipidemia drugs. As a result, 2-year (104-week) observation of patients with T2DM (age, 40–70 years) who began treatment with a single OHA revealed that BG significantly reduced the prevalence of cardiovascular events compared with SU.
Meta-analyses focusing on the efficacy of BG for a reduction in cardiovascular risk have been reported [17]. In that report, metformin (a type of BG) reduced the incidence of CVD compared with placebo/non-treated subjects. Survival was also favorable in the metformin group, but was reduced if metformin was administered with SU. Another report made a direct comparison between BG and SU in which metformin reduced the incidence of cardiovascular events and mortality [5]. The results of the present study are in accordance with the results of those reports. Compared with SU, BG has been reported to have favorable effects on body weight, lipid levels, and blood pressure [18]. BG has also been reported to reduce the activity of plasminogen activator inhibitor-1, which is a factor for thrombogenesis [19] and exerts its protective effect against ischemia-reperfusion injury after MI. These effects are considered not to be explained fully by the lowering effect of blood glucose [20]. Some SU drugs bind to the SUR2A/B receptor (located in the myocardium and smooth muscle cells in coronary arteries) and reduce the effect of ischemic preconditioning, and possibly increase the risk of cardiovascular events [21]. Thus, the risk reduction of cardiovascular events by BG relative to SU in the present study can be accounted for (at least in part) by the mechanisms of action of BG and SU stated above. Namely, a possibility of increased risk of CV events by SU and a possibility of reduced risk of CV evenyts by BG may result in our results.
In our analyses, the reduction in cardiovascular risk between drugs relative to SU was not associated with the reduction in HbA1c level. Several clinical trials, including Action to Control Cardiovascular Risk in Diabetes (ACCORD) [22], Action in Diabetes and Vascular Disease (ADVANCE) [23] and Veterans Affairs Diabetes Trial (VADT) [24], have shown that intensive control of glycemia does not consistently reduce the prevalence of cardiovascular events and, in some cases, may be harmful. One reason for the failure in the reduction in the prevalence of cardiovascular events is speculated to be hypoglycemia [25]. Hypoglycemia is associated with increased activation of the sympathetic nervous system, which has been suggested to be a major risk factor for adverse events [23]. Although not observed as often as that seen with insulin, SU carries a relatively greater risk of hypoglycemia [26]. This phenomenon may explain (at least in part) the relative increase in the prevalence of cardiovascular events in the SU group compared with BG groups even though a similar degree of reduction in the HbA1c level was achieved.
Our study had several important limitations. First, despite being a population-based study using a hospital database, the sample size for analysis was not very large because the inclusion and exclusion criteria of subjects had to be considered. Second, this study was not a prospective type of cohort analysis, making correct evaluation of the clinical impact of each OHA very difficult. Even though the first OHA was continued as the baseline drug for ~1–1.4 years according to mean values, the first OHA was sometimes switched to other OHAs, used with other OHAs from certain time-points, or stopped before 104 weeks. Third, the duration of follow-up (2 years) may be relatively short for comparison of the prevalence of cardiovascular events. Fourth, information of antihypertensive drugs, antiplatelet or anticoagulant medications and anti-dyslipidemia drugs which can affect CV outcomes, were partly but not fully available from the database. We could not completely rule out a possibility that these drugs might have some impact on the CV outcome in this study.
In the present study, the effect of α-GI on reduction in cardiovascular risk was not favorable compared with that for SU, a result that is in contrast with other clinical studies [7, 8]. α-GI might have had little impact on the prevalence of cardiovascular events because of its relatively lower level of HbA1c at the start of our study. The vascular-protective effects of TZD or DPP-4 inhibitor relative to SU was not demonstrated in our study despite some favorable evidence in recent years [9–11, 27, 28], though this topic remains controversial [12, 13]. DPP-4 inhibitors are effective and safe [29] and now expanding the OHA market in Japan enormously, which will enable this type of population-based analyses to be undertaken again. Hence, the vascular-protective effect of OHAs (including α-GI and DPP-4 inhibitor) seems to be inconclusive and needs more careful interpretation in the context of the limitations of our study. A slightly shorter duration of administration of DPP-4 inhibitor relative to SU in our study might have affected the results. Nevertheless, we can say with confidence that initial treatment with BG and its baseline treatment for a certain period of time could aid prevention of CVD events in T2DM patients in Japan.
Despite the study limitations detailed above, our study analyzing a database containing information on Japanese individuals with T2DM in 103 hospitals revealed that first treatment and baseline treatment for a certain duration with BG could significantly reduce the prevalence of cardiovascular events compared with SU, and that this effect was independent of its blood glucose-lowering effect. The American Diabetes Association and European Association for the Study of Diabetes issued guidelines [30] that incorporated information from clinical trials focusing on cardiovascular outcomes [22–24]. Those guidelines recommend initial treatment with BG and emphasize a patient-centric approach to treatment rather than adherence to stricter control of glycemia [29]. BG does not have strong glucose-lowering effects, but our findings will aid the choice of anti-DM drugs for the prevention of cardiovascular events beyond glycemic control.
Conclusions
In Japanese subjects with T2DM, initial treatment and baseline treatment with BG can reduce CVD risk relative to that of SU, and this effect is independent of the blood glucose-lowering effect of BG.
Availability of data and materials
Not applicable.
Acknowledgement
We thank Mr. Kazumasa Tanzawa for statistical evaluation and constructive advice.
Funding
This research was supported by research funding from faculty of medicine, Fukuoka university.
Abbreviations
- OHA
Oral hypoglycemic agent
- CVD
Cardiovascular disease
- T2DM
Type-2 diabetes mellitus
- DPP-4
Dipeptidyl peptidase-4
- ICD
International Classification of Diseases
- MI
Myocardial infarction
- BG
Biguanide
- SU
Sulfonylurea
- α-GI
α-glucosidase inhibitor
- TZD
Thiazolidinedione
- GLP-1
Glucagon-like peptide-1
- MHLWJ
Ministry of Health, Labour, and Welfare in Japan
- HR
Hazard ratio
Additional files
Details of antihypertensive drugs and anti-dyslipidemia drugs used for subjects in study 1. (PPTX 70 kb)
Details of antihypertensive drugs and anti-dyslipidemia drugs used for subjects in study 2. (PPTX 71 kb)
Footnotes
Competing interests
RM and KM have no competing interests. MT, TN and TY have received speaker fees or chairman fees from MSD K.K., Sanofi K.K., Takeda Pharmaceutical Co., Ltd., Dainippon Sumitomo Pharma Co., Ltd., Sanwa Chemistry Co., Ltd., Eli Lilly Japan K.K., Novo Nordisk Pharma Ltd., Daiichi Sankyo Co., Ltd., Novartis Pharma K.K., and Astellas Pharma Inc. TY was supported financially in his research by MSD K.K., Sanofi K.K., Takeda Pharmaceutical Co., Ltd., Daiichi Sankyo Company Ltd., Dainippon Sumitomo Pharma Co., Ltd., Sanwa Chemistry Co., Ltd., Eli Lilly Japan K.K., Novo Nordisk Pharma Ltd., Novartis Pharma K.K., Kowa Co. Ltd., and Fujifilm Pharma Co., Ltd. The Department of Bioregulatory Science of Life-related Diseases of Fukuoka University (Fukuoka, Japan) was supported financially by a donation from MSD K.K.
Authors' contributions
MT carried out the data arrangement and drafted the manuscript. TN and TY conceived the study, participated in its design and coordination, carried out data arrangement, and helped to draft the manuscript. RM and KM reviewed and edited the manuscript. All authors read and approved the final version of the manuscript.
Authors' information
Not applicable.
Contributor Information
Makito Tanabe, Email: mtanabe@live.jp.
Takashi Nomiyama, Email: tnomiyama@fukuoka-u.ac.jp.
Ryoko Motonaga, Email: r_nagaishi@hotmail.com.
Kunitaka Murase, Email: kunitaka@fukuoka-u.ac.jp.
Toshihiko Yanase, Email: tyanase@fukuoka-u.ac.jp.
References
- 1.de Marco R, Locatelli F, Zoppini G, Verlato G, Bonora E, Muggeo M. Cause-specific mortality in type 2 diabetes. The Verona Diabetes Study. Diabetes Care. 1999;22:756–761. doi: 10.2337/diacare.22.5.756. [DOI] [PubMed] [Google Scholar]
- 2.Haffner S, Lehto S, Rönnemaa T, Pyörälä K, Laakso M. Mortality from coronary heart disease in subjects with type 2 diabetes and in nondiabetic subjects with and without prior myocardial infarction. N Engl J Med. 1998;339:229–234. doi: 10.1056/NEJM199807233390404. [DOI] [PubMed] [Google Scholar]
- 3.Fujishima M, Kiyohara Y, Kato I, Ohmura T, Iwamoto H, Nakayama K, Ohmori S, Yoshitake T. Diabetes and cardiovascular disease in a prospective population survey in Japan: The Hisayama Study. Diabetes. 1996;45(Suppl. 3):S14–S16. doi: 10.2337/diab.45.3.S14. [DOI] [PubMed] [Google Scholar]
- 4.Mukamal KJ, Nesto RW, Cohen MC, Muller JE, Maclure M, Sherwood JB, Mittleman MA. Impact of diabetes on long-term survival after acute myocardial infarction: comparability of risk with prior myocardial infarction. Diabetes Care. 2001;24:1422–1427. doi: 10.2337/diacare.24.8.1422. [DOI] [PubMed] [Google Scholar]
- 5.Roumie CL, Hung AM, Greevy RA, Grijalva CG, Liu X, Murff HJ, Elasy TA, Griffin MR. Comparative effectiveness of sulfonylurea and metformin monotherapy on cardiovascular events in type 2 diabetes mellitus: a cohort study. Ann Intern Med. 2012;157:601–610. doi: 10.7326/0003-4819-157-9-201211060-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bolen S, Feldman L, Vassy J, Wilson L, Yeh HC, Marinopoulos S, Wiley C, Selvin E, Wilson R, Bass EB, Brancati FL. Systematic review: comparative effectiveness and safety of oral medications for type 2 diabetes mellitus. Ann Intern Med. 2007;147:386–399. doi: 10.7326/0003-4819-147-6-200709180-00178. [DOI] [PubMed] [Google Scholar]
- 7.Chiasson JL, Josse RG, Gomis R, Hanefeld M, Karasik A, Laakso M, STOP-NIDDM Trial Research Group Acarbose treatment and the risk of cardiovascular disease and hypertension in patients with impaired glucose tolerance: the STOP-NIDDM trial. JAMA. 2003;290:486–494. doi: 10.1001/jama.290.4.486. [DOI] [PubMed] [Google Scholar]
- 8.Hanefeld M, Cagatay M, Petrowitsch T, Neuser D, Petzinna D, Rupp M. Acarbose reduces the risk for myocardial infarction in type 2 diabetic patients: meta-analysis of seven long-term studies. European Heart J. 2004;25:10–16. doi: 10.1016/S0195-668X(03)00468-8. [DOI] [PubMed] [Google Scholar]
- 9.Mazzone T, Meyer PM, Feinstein SB, Davidson MH, Kondos GT, D'Agostino RB, Sr, Perez A, Provost JC, Haffner SM. Effect of pioglitazone compared with glimepiride on carotid intima-media thickness in type 2 diabetes: a randomized trial. JAMA. 2006;296:2572–2581. doi: 10.1001/jama.296.21.joc60158. [DOI] [PubMed] [Google Scholar]
- 10.Nissen SE, Nicholls SJ, Wolski K, Nesto R, Kupfer S, Perez A, Jure H, De Larochellière R, Staniloae CS, Mavromatis K, Saw J, Hu B, Lincoff AM, Tuzcu EM, PERISCOPE Investigators Comparison of pioglitazone vs glimepiride on progression of coronary atherosclerosis in patients with type 2 diabetes: The PERISCOPE randomized controlled trial. JAMA. 2008;299:1561–1573. doi: 10.1001/jama.299.13.1561. [DOI] [PubMed] [Google Scholar]
- 11.Ussher JR, Drucker DJ. Cardiovascular biology of the incretin system. Endocr Rev. 2012;33:187–215. doi: 10.1210/er.2011-1052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Scirica BM, Bhatt DL, Braunwald E, Steg PG, Davidson J, Hirshberg B, Ohman P, Frederich R, Wiviott SD, Hoffman EB, Cavender MA, Udell JA, Desai NR, Mosenzon O, McGuire DK, Ray KK, Leiter LA, Raz I, SAVOR-TIMI 53 Steering Committee and Investigators Saxagliptin and cardiovascular outcomes in patients with type 2 diabetes mellitus. N Engl J Med. 2013;369:1317–1326. doi: 10.1056/NEJMoa1307684. [DOI] [PubMed] [Google Scholar]
- 13.White WB, Cannon CP, Heller SR, Nissen SE, Bergenstal RM, Bakris GL, Perez AT, Fleck PR, Mehta CR, Kupfer S, Wilson C, Cushman WC, Zannad F, EXAMINE Investigators Alogliptin after acute coronary syndrome in patients with type 2 diabetes. N Engl J Med. 2013;369:1327–1335. doi: 10.1056/NEJMoa1305889. [DOI] [PubMed] [Google Scholar]
- 14.Tajima M, Noda M, Origasa H, Noto H, Yabe D, Fujita Y, et al. Evidence-based practice guideline for the treatment for diabetes in Japan 2013. Diabetol Int. 2015; doi: 10.1007/s13340-015-0206-2
- 15.Yanase T, Takenoshita H, Murase K, Nagaishi R, Nomiyama T, Akehi Y. Utility study of a basic database collected from patients with diabetes mellitus in 15 hospitals by retrospective analysis. Pharma Medica. 2011;29:145–152. [Google Scholar]
- 16.Urushihara H, Taketsuna M, Liu Y, Oda E, Nakamura M, Nishiuma S, Maeda R. Increased risk of acute pancreatitis in patients with type 2 diabetes: an observational study using a Japanese hospital database. PLoS One. 2012;7 doi: 10.1371/journal.pone.0053224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lamanna C, Monami M, Marchionni N, Mannucci E. Effect of metformin on cardiovascular events and mortality: a meta-analysis of randomized clinical trials. Diabetes Obes Metab. 2011;13:221–228. doi: 10.1111/j.1463-1326.2010.01349.x. [DOI] [PubMed] [Google Scholar]
- 18.Chan JC, Tomlinson B, Critchley JA, Cockram CS, Walden RJ. Metabolic and hemodynamic effects of metformin and glibenclamide in normotensive NIDDM patients. Diabetes Care. 1993;16:1035–1038. doi: 10.2337/diacare.16.7.1035. [DOI] [PubMed] [Google Scholar]
- 19.Nagi DK, Yudkin JS. Effects of metformin on insulin resistance, risk factors for cardiovascular disease, and plasminogen activator inhibitor in NIDDM subjects. A study of two ethnic groups. Diabetes Care. 1993;16:621–629. doi: 10.2337/diacare.16.4.621. [DOI] [PubMed] [Google Scholar]
- 20.Whittington HJ, Hall AR, McLaughlin CP, Hausenloy DJ, Yellon DM, Mocanu MM. Chronic metformin associated cardioprotection against infarction: not just a glucose lowering phenomenon. Cardiovasc Drugs Ther. 2013;27:5–16. doi: 10.1007/s10557-012-6425-x. [DOI] [PubMed] [Google Scholar]
- 21.Meier JJ, Gallwitz B, Schmidt WE, Mugge A, Nauck MA. Is impairment of ischemic preconditioning by sulfonylurea drugs clinically important? Heart. 2004;90:9–12. doi: 10.1136/heart.90.1.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Action to Control Cardiovascular Risk in Diabetes Study Group. Gerstein HC, Miller ME, Byington RP, Goff DC, Jr, Bigger JT, Buse JB, Cushman WC, Genuth S, Ismail-Beigi F, Grimm RH, Jr, Probstfield JL, Simons-Morton DG, Friedewald WT. Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med. 2008;358:2545–2559. doi: 10.1056/NEJMoa0802743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.ADVANCE Collaborative Group Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Engl J Med. 2008;358:2560–2572. doi: 10.1056/NEJMoa0802987. [DOI] [PubMed] [Google Scholar]
- 24.Duckworth W, Abraira C, Moritz T, Reda D, Emanuele N, Reaven PD, Zieve FJ, Marks J, Davis SN, Hayward R, Warren SR, Goldman S, McCarren M, Vitek ME, Henderson WG, Huang GD for the VADT Investigators Glucose control and vascular complications in veterans with type 2 diabetes. N Engl J Med. 2009;360:129–139. doi: 10.1056/NEJMoa0808431. [DOI] [PubMed] [Google Scholar]
- 25.Frier BM, Schernthaner G, Heller SR. Hypoglycemia and cardiovascular risks. Diabetes Care. 2011;34(Suppl.2):S132–137. doi: 10.2337/dc11-s220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.UK Prospective Diabetes Study (UKPDS) Group Intensive blood-glucose control with sulfonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33) Lancet. 1998;352:837–53. doi: 10.1016/S0140-6736(98)07019-6. [DOI] [PubMed] [Google Scholar]
- 27.Terawaki Y, Nomiyama T, Kawanami T, Hamaguchi Y, Takahashi H, Tanaka T, Murase K, Nagaishi R, Tanabe M, Yanase T. Dipeptidyl peptidase-4 inhibitor linagliptin attenuates neointima formation after vascular injury. Cardiovasc Diabetol. 2014;13:154. doi: 10.1186/s12933-014-0154-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ervinna N, Mita T, Yasunari E, Azuma K, Tanaka R, Fujimura S, Sukmawati D, Nomiyama T, Kanazawa A, Kawamori R, Fujitani Y, Watada H. Anagliptin, a DPP-4 inhibitor, suppresses proliferation of vascular smooth muscles and monocyte inflammatory reaction and attenuates atherosclerosis in male apo E-deficient mice. Endocrinology. 2013;154:1260–1270. doi: 10.1210/en.2012-1855. [DOI] [PubMed] [Google Scholar]
- 29.Nomiyama T, Akehi Y, Takenoshita H, Nagaishi R, Terawaki Y, Nagasako H, Kudo T, Kodera T, Kobayashi K, Urata H, Yanase T, CHAT Contributing factors related to efficacy of the dipeptidyl peptidase-4 inhibitor sitagliptin in Japanese patients with type 2 diabetes. Diabetes Res Clin Pract. 2012;95:e27–28. doi: 10.1016/j.diabres.2011.08.016. [DOI] [PubMed] [Google Scholar]
- 30.American Diabetes Association Standards of medical care in diabetes 2012. Diabetes Care. 2012;35(Suppl.1):S11–S63. doi: 10.2337/dc12-s011. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.


