Abstract
Background
The primary objective of the study was to evaluate the association between the minimum apparent diffusion coefficient (ADCmin) and Ki-67, an index for cellular proliferation, in non-small cell lung cancers. Also, we aimed to assess whether ADCmin values differ between tumour subtypes and tissue sampling method.
Methods
The patients who had diffusion weighted magnetic resonance imaging (DW-MRI) were enrolled retrospectively. The correlation between ADCmin and the Ki-67 index was evaluated.
Results
Ninety three patients, with a mean age 65 ± 11 years, with histopathologically proven adenocarcinoma and squamous cell carcinoma of the lungs and had technically successful DW-MRI were included in the study. The numbers of tumour subtypes were 47 for adenocarcinoma and 46 for squamous cell carcinoma. There was a good negative correlation between ADCmin values and the Ki-67 proliferation index (r = −0.837, p < 0.001). The mean ADCmin value was higher and the mean Ki-67 index was lower in adenocarcinomas compared to squamous cell carcinoma (p < 0.0001). There was no statistical difference between tissue sampling methods.
Conclusions
Because ADCmin shows a good but negative correlation with Ki-67 index, it provides an opportunity to evaluate tumours and their aggressiveness and may be helpful in the differentiation of subtypes non-invasively.
Keywords: diffusion weighted-magnetic resonance imaging, apparent diffusion coefficient, Ki-67 index, adenocarcinoma, squamous cell carcinoma
Introduction
Diffusion weighted magnetic resonance imaging (DW-MRI) is a promising MRI technique used in the evaluation of lung tumours. It has been increasingly used for the detection, differential diagnosis and evaluation of tumour characteristics, including grading and prediction of the therapeutic response.1–7 DW-MRI is a functional imaging technique that reveals physiological information by quantifying the diffusion of water molecules in tissues. The extent of this diffusion is measured using the apparent diffusion coefficient (ADC). Malignant tissues tend to have a lower ADC and demonstrate higher signal intensity on a DW-MRI image due to their increased cellularity and larger nuclei with abundant macromolecular proteins.8,9
The Ki-67 protein (also known as MKI67) is a cellular proliferation marker. During interphase, the Ki-67 antigen can only be detected within the cell nucleus; however, in mitosis, most of the Ki-67 is relocated to the surface of the chromosomes. Ki-67 protein is present during all active phases of the cell cycle (G1, S, G2, and mitosis), but is absent in resting cells (G0). The Ki-67 proliferation index, one of the biological markers used in histopathological evaluation, is an important criterion in the differentiation of benign and malignant tumours.10–12 It is also correlated with the clinical course of cancer and has been shown to have prognostic value for treatment response, tumour recurrence and survival in brain, breast, bladder and prostate tumours, meningioma and nephroblastoma.13–19 The Ki-67 index has also been used routinely in the evaluation of lung tumours and has been shown to be an important prognostic factor for lung cancer.3,6,20–27 Although a few studies have evaluated the association of ADC with Ki-67 index in lung tumours3,6, no study has previously investigated differences in the ADC/Ki 67 correlation in different tumour subtypes.
In this study, our primary objective was to evaluate whether there is an association between the minimum ADC (ADCmin), determined on DWMRI, and Ki-67, which is a cellular proliferative index. Our secondary aim was to assess whether ADCmin values differ between the adenocarcinomas and squamous cell carcinomas of the lungs and also differ according to the pathologic sampling method used, surgical excision specimen and biopsied material.
Methods
Study population
Between January 2012 and December 2013, records for 104 consecutive patients with histopathologically proven primary adenocarcinoma and squamous cell carcinoma of the lungs, and who had technically successful images on DW-MRI were retrieved from the hospital’s pathology database. The patients who were previously treated (n = 5) and\or had an interval of more than 15 days between DW-MRI and biopsy (n = 6) were excluded from the study. All measurements, including calculation of Ki-67 index and ADCmin values, were done in the same lesion for each patient. The protocol of the retrospective study was approved by the institutional ethics committee and the requirement for informed consent was waived.
Imaging technique, DW-MRI
It was performed with a 3 tesla scanner (MAGNETOM Skyra, Siemens Healthcare, Erlangen, Germany). Conventional MRI included an axial T1-weighted sequence (repetition time, 104 ms; echo time, 4.92 ms; 1 excitation) and an axial T2-weighted sequence (repetition time, 1400 ms; echo time, 101 ms; 1 excitation). Breath-free DW-MRI was performed in the axial plane using a single-shot, spin-echo echo-planar imaging sequence with the following parameters: repetition time, 6500 ms; echo time, 61 ms; real spatial resolution in the phase-encoding direction, 3.7 mm; flip angle, 90°; diffusion gradient encoding in three orthogonal directions; b value b = 50, b = 400 and b = 800 s/mm2; field of view, 380 mm × 380 mm × 310 mm; matrix size, 113 × 192; slice thickness, 6 mm; section gap, 0 mm; 2 signals acquired.
Image analysis
We analysed the lesions using DW-MRI images in association with T1- and T2-weighted images in order to identify accurately. The ADC of the tumour was then calculated to quantitatively analyse the degree of diffusion, using the following formula: ADC = −ln(S/S0) / (b−b0), where S0 and S are the signal intensities, obtained at three different diffusion gradients (b = 50, b = 400 and b = 800 s/mm2). The ADC maps were reconstructed at a workstation. While establishing the size and region for the ROI, positioning in the larger area was considered in order to minimize the effect of region on hemodynamic inhomogeneity of tumour by avoiding necrotic, cystic or calcific areas by referring to T2 and T1-weighted images.28,29 The ADCmin values within the ROI were then used in statistical analyses (Figure 1). In analyses workstation (Syngo Via Console, software version 2.0, Siemens AG Medical Solutions, Erlangen, Germany) was used.
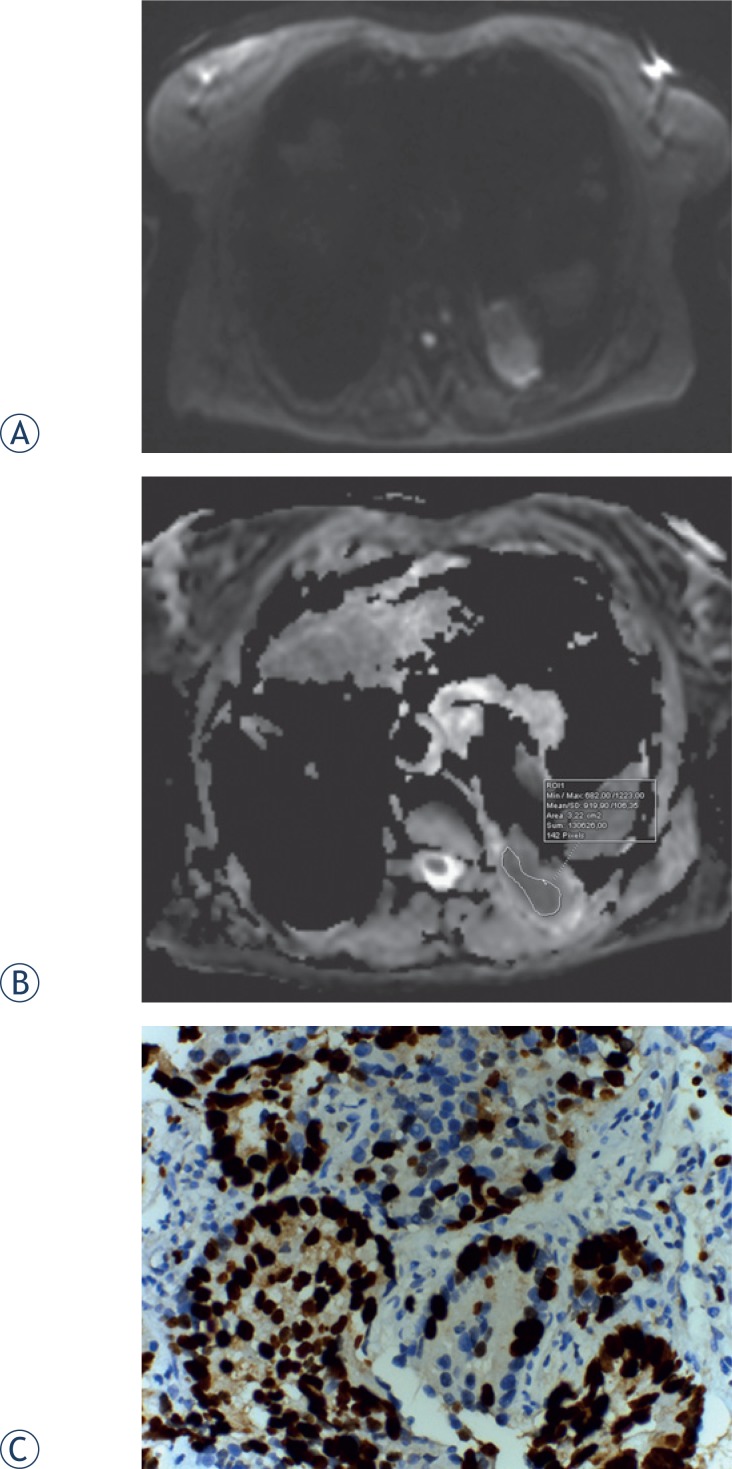
FIGURE 1.
Diffusion-weighted (DW)-MRI, apparent diffusion coefficient (ADC) map of a 62-year-old female with adenocarcinoma. (A) Tumour shows heterogeneously high signal intensity on DW-MRI, for which the b value is 800 s/mm2. (B) On the ADC map, the tumour demonstrates heterogeneous diffusion restriction. (C) Proli ferative index 95% in glandular epithelium (Ki-67X400).
Calculation of Ki-67 index
Archived paraffin blocks belonging to the patients were transferred to polylysine glass slides with 4-micron thick sections. Immunochemistry was performed using a Lecia Bond-max automated immunostainer (Leica Microsystems, Newcastle, UK), as described manufacturers protocol. For Ki-67 staining, Ki-67 antibody (NCL-L-Ki67-MM1, monoclonal, 1:60, Novocostra, Newcastle, UK) was used. The sections prepared for examination were evaluated by two pathologists who were blinded to each-other. Firstly, ten areas having highest expression of Ki-67 were determined at low magnification. Then, these areas were further analysed at a single high power field (400 × magnification). Ki-67 expression was defined as the percent of Ki-67-positive tumour cells divided by the total number of tumour cell within one high power field.26,30 In the last step, Ki-67 index was calculated as the average percentage of those fields.
Statistical Analysis
Analyses were performed using IBM SPSS 20.0 for Mac software. The correlation between ADCmin and the Ki-67 index was evaluated using Spearman’s correlation coefficient. Mann-Whitney U tests were used to assess the difference between the ADCmin and the Ki-67 index for the different tumour subtypes. A p value of less than 0.05 was considered statistically significant.
Results
Ninety three patients, with a mean age 65 ± 11 years ranged between 43 and 84, with histopathologically proven primary adenocarcinoma (n = 47) and squamous cell carcinoma (n = 46) of the lungs and had technically successful DW-MRI were included in the study. Histopathological diagnoses were obtained through transthoracic or transbronchial biopsy in 65 subjects and 28 patients underwent surgery.
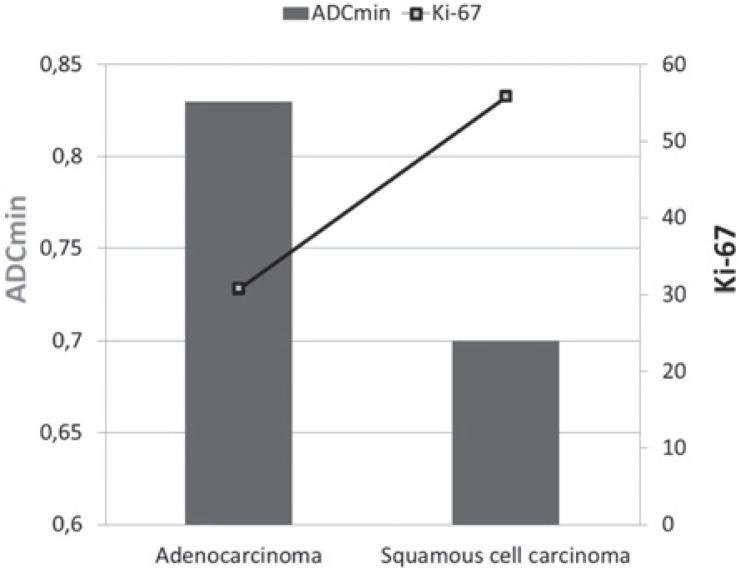
The mean ADCmin value for all the lesions was 0.77 ± 0.15 × 10−3 mm2/sec (range, 0.50–1.00 × 10−3 mm2/sec). The mean ADCmin value for adenocarcinomas was 0.83 ± 0.12 × 10−3 mm2/sec and that of squamous cell carcinomas was 0.70 ± 0.16 × 10−3 mm2/sec; there was a significant difference between these values (p < 0.0001). The mean Ki-67 was 43.5 ± 22.2 for all the tumours (range, 5–96), with a mean of 30.8 ± 14.1 for adenocarcinomas and 55.9 ± 21.8 for squamous cell carcinoma; the difference between tumour subtypes was significant (p < 0.0001).
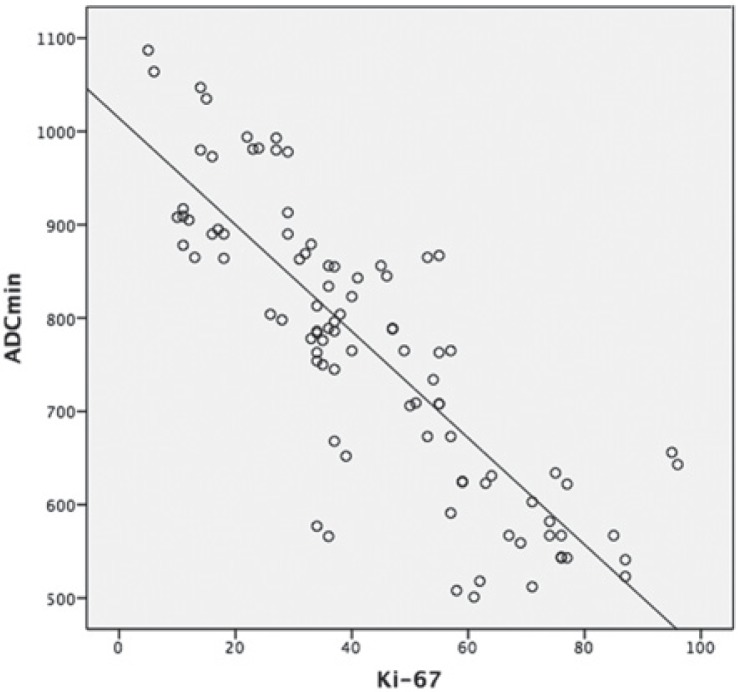
There was a negative correlation between ADCmin values and the Ki-67 proliferation index (p < 0.001, r = −0.837) (Figure 2). The ADCmin values were lower in the cases with higher Ki-67 grades. The mean ADCmin values and Ki-67 index for adenocarcinomas and squamous cell carcinomas of the lung are shown in Figure 3. There was no statistical difference of Ki-67 and ADCmin values between biopsied material and surgical specimen. The mean Ki-67 was 45.3 ± 22.8 vs 39.3 ± 19.8 and the mean ADCmin value was 0.76 ± 0.16×10−3 vs 0.78 ± 0.14 × 10−3 for biopsied material and surgical specimen, respectively. In the comparative evaluation of correlation between ADCmin and the Ki-67 proliferation index that measured either in surgical specimen or biopsied material, the Ki-67 index of surgical specimens was slightly better correlated with ADCmin values without statistical significance (r = −0.870 vs. −0.617) compared to biopsied material.
FIGURE 2.
The graph shows a negative correlation between the minimum apparent diffusion coefficient (ADCmin) and the Ki-67 index in lung tumours (r = −0.837, p < 0.001).
FIGURE 3.
The graph shows average minimum apparent diffusion coefficient (ADCmin) values for adenocarcinoma and squamous cell carcinoma according to Ki-67 index. Bars are for ADCmin values and line is for Ki-67.
Discussion
Our results showed that there is a negative correlation between the ADCmin and the Ki-67 index of lung cancers, which reflects aggressiveness of a tumour. ADCmin values for adenocarcinomas were higher than those for squamous cell carcinomas. This finding indicates that ADCmin may have a role in discriminating adenocarcinomas from squamous cell carcinomas, as well as being used for evaluating the aggressiveness of the tumour. Also, a low ADCmin value can potentially be used as a non-invasive surrogate biomarker for the Ki-67 index for the evaluation of lung tumour characteristics, regardless of subtype.
Lung cancer is the leading cause of cancer-related deaths.31 Until now, the Ki-67 proliferation index, reflecting aggressiveness of a tumour has been used to determine the prognosis. Malignant tumours are characterized by increased Ki-67 proliferation index due to their cellularity, larger nuclei with more abundant macromolecular proteins, a larger nuclear/cytoplasmic ratio and less extracellular space relative to normal tissue. As these characteristics also restrict the diffusion of water molecules, ADCmin decreases in malignant tumours.8,9,32
Because ADCmin is found to have stronger correlation with Ki-67 index compared to ADCmean, we used ADCmin in our study.15 Apparent diffusion coefficient can be used in the non-invasive assessment of suspicious masses, for example, to differentiate metastatic lymph nodes from those that are benign when they cannot be differentiated by size criteria.5 ADC values also correlate with tumour grades.4,17,18 Recent studies have shown that ADC may be more useful than FDG-PET in the differentiation of malignant tumours from benign lesions3,6 and the new approaches using PET\MRI may provide more promising results in the future.33 Among primary lung cancers, ADC values are usually low in cases with small cell carcinomas, but the values for adenocarcinomas and squamous cell carcinomas are usually similar.3,4 However Matoba et al. stated that ADCs of well-differentiated adenocarcinoma appear to be higher than those of other histologic lung carcinoma types.23 Our findings demonstrate that adenocarcinomas showed higher ADC values than squamous cell carcinomas, and had weaker staining diffusivity and intensity of Ki-67.
A high Ki-67 and low ADCmin value indicates that a tumour has a high proliferation rate. Ki-67 values obtained using an invasive method reflect only the level in the sampled tissue; this is a particular problem when using biopsy. Since lung carcinomas are not always homogenous, the biopsy site can influence the results. This could be reflected in the fact that in our study the correlation between ADCmin and Ki-67 proliferation index was stronger for surgical than for biopsy samples. Unlike these invasive sampling methods, ADCmin values obtained by DW-MRI in a non-invasive manner can be calculated from anywhere in the tumour, providing an entire and reproducible assessment of the tumour. Furthermore, since the region with the lowest ADCmin value is likely to be the most aggressive portion.17,34 DWI could also help in the selection of an appropriate biopsy site within the tumour.
An association between the ADC value and the Ki-67 index has been shown for various kinds of tumours2,14–18,34–38, including lung cancer.3,6 Wang et al., in their study on DWI in pancreatic endocrine tumours, reported a correlation coefficient of −0.702, while Onishi et al. reported a correlation coefficient of −0.825 for mucinous breast carcinoma.15
Previous studies reporting ADC values of lung carcinoma have been conducted under various magnet strengths, and reported ADC values are lower in magnets with a stronger field. Matoba et al. reported mean ADC values of 1.63 × 10−3 mm2/sec ± 0.5 (mean ± SD) for squamous cell carcinomas, 2.12 × 10−3 mm2/sec ± 0.6 for adenocarcinomas, 1.30 × 10−3 mm2/sec ± 0.4 for large-cell carcinomas, and 2.09 × 10−3 mm2/sec ± 0.3 for small-cell carcinomas, using a 1.5 T scanner. Usuda et al.6 found that malignant nodules had a mean ADC of 1.27 ± 0.35 ×10−3 mm2/sec on a 1.5T system. Using a 3.0 T scanner, Zhang et al. reported that malignant pulmonary nodules had a mean ADC of 0.87 ± 0.16 × 10−3 mm2/ sec. Similarly, we found a mean ADCmin of 0.77 ± 0.12 × 10−3 mm2/sec in our study conducted on a 3.0 T scanner. These values are lower than those were reported by the studies conducted using 1.5 T systems.6,23 However, Kivrak et al. noted that ADC values vary for different MRI systems with the same magnetic field strength (1.5 T).39 On the other hand, some authors reported that ADC values might not change for different organ systems under different magnetic fields.40 However, they only used healthy volunteers and neither pathologic conditions nor image quality was not assessed. Further work is still needed to investigate the effect of magnetic field strength on the ADC of different organ systems.
One of the strongest side of our study was that we used 3 tesla MRI, which has increased signal to noise ratio, spatial resolution, temporal resolution, etc. Thus, decreased imaging time increased patients’ cooperation and we had better qualified images. Our study had a few limitations. Our study population was relatively small and, although our results are robust, prospective studies with larger series are warranted to confirm our results. Additionally, to be able to generalize our results to all subtypes of lung cancer, such as small cell carcinomas and the other subtypes of non-small cell lung cancer, which we had very limited number of such cases during the study period, need to be included in future studies. Because we had no data about survival of the cases, we could not conclude any association between ADCmin or Ki-67 and survival. However, use of ADCmin may provide new insight to the evaluation of lung cancer including benign-malignant discrimination, the possibility of evaluation all lesions and lymph nodes noninvasively, even in the cases that tissue sampling is difficult, as well as predicting the prognosis of tumour by using it as a surrogate marker of Ki-67 index.
In conclusion, our results suggested that ADCmin values were inversely correlated with Ki-67 index in non-small cell lung cancer and may be used as a surrogate marker of Ki-67 index in the evaluation of tumour aggressiveness with the advantage of its non-invasiveness and without requirement of tissue sampling of all the lesions.
Footnotes
Disclosure: No potential conflicts of interest were disclosed.
References
- 1.Yabuuchi H, Hatakenaka M, Takayama K, Matsuo Y, Sunami S, Kamitani T, et al. Non-small cell lung cancer: detection of early response to chemotherapy by using contrast-enhanced dynamic and diffusion-weighted MR imaging. Radiology. 2011;26:598–604. doi: 10.1148/radiol.11101503. [DOI] [PubMed] [Google Scholar]
- 2.Wang Y, Chen ZE, Yaghmai V, Nikolaidis P, McCarthy RJ, Merrick L, et al. Diffusion-weighted MR imaging in pancreatic endocrine tumors correlated with histopathologic characteristics. J Magn Reson Imaging. 2011;33:1071–9. doi: 10.1002/jmri.22541. [DOI] [PubMed] [Google Scholar]
- 3.Zhang J, Cui LB, Tang X, Ren XL, Shi JR, Yang HN, et al. DW MRI at 3.0 T versus FDG PET/CT for detection of malignant pulmonary tumors. Int J Cancer. 2014;134:606–11. doi: 10.1002/ijc.28394. [DOI] [PubMed] [Google Scholar]
- 4.Li F, Yu T, Li W, Zhang C, Cao Y, Su D, et al. Correlation of apparent diffusion coefficient with histologic type and grade of lung cancer. Zhongguo Fei Ai Za Zhi. 2012;15:646–51. doi: 10.3779/j.issn.1009-3419.2012.11.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Xu L, Tian J, Liu Y, Li C. Accuracy of diffusion-weighted (DW) MRI with background signal suppression (MR-DWIBS) in diagnosis of mediastinal lymph node metastasis of nonsmall-cell lung cancer (NSCLC) J Magn Reson Imaging. 2014;40:200–5. doi: 10.1002/jmri.24343. [DOI] [PubMed] [Google Scholar]
- 6.Usuda K, Sagawa M, Motono N, Ueno M, Tanaka M, Machida Y, et al. Diagnostic performance of diffusion weighted imaging of malignant and benign pulmonary nodules and masses: comparison with positron emission tomography. Asian Pac J Cancer Prev. 2014;15:4629–35. doi: 10.7314/apjcp.2014.15.11.4629. [DOI] [PubMed] [Google Scholar]
- 7.Türkbey B, Aras Ö, Karabulut N, Turgut AT, Akpinar E, Alibek S, et al. Diffusion-weighted MRI for detecting and monitoring cancer: a review of current applications in body imaging. Diagn Interv Radiol. 2012;18:46–59. doi: 10.4261/1305-3825.DIR.4708-11.2. [DOI] [PubMed] [Google Scholar]
- 8.Koh DM, Collins DJ. Diffusion-weighted MRI in the body: applications and challenges in oncology. AJR Am J Roentgenol. 2007;188:1622–35. doi: 10.2214/AJR.06.1403. [DOI] [PubMed] [Google Scholar]
- 9.Padhani AR, Liu G, Koh DM, Chenevert TL, Thoeny HC, Takahara T, et al. Diffusion-weighted magnetic resonance imaging as a cancer biomarker: consensus and recommendations. Neoplasia. 2009;11:102–25. doi: 10.1593/neo.81328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Scholzen T, Gerdes J. The Ki-67 protein: from the known and the unknown. J Cell Physiol. 2000;182:311–22. doi: 10.1002/(SICI)1097-4652(200003)182:3<311::AID-JCP1>3.0.CO;2-9. [DOI] [PubMed] [Google Scholar]
- 11.Raĭkhlin NT, Bukaeva IA, Smirnova EA, Gurevich LE, Delektorskaia VV, Polotskiĭ BE, et al. Significance of the expression of nucleolar argyrophilic proteins and antigen Ki-67 in the evaluation of cell proliferative activity and in the prediction of minimal (T1) lung cancer. Arkh Patol. 2008;70:15–18. [PubMed] [Google Scholar]
- 12.Gerdes J, Lemke H, Baisch H, Wacker HH, Schwab U, Stein H. Cell cycle analysis of a cell proliferation-associated human nuclear antigen defined by the monoclonal antibody Ki-67. J Immunol. 1984;133:1710–15. [PubMed] [Google Scholar]
- 13.Zhu L, Ren G, Li K, Liang ZH, Tang WJ, Ji YM, et al. Pineal parenchymal tumours: minimum apparent diffusion coefficient in prediction of tumour grading. J Int Med Res. 2011;39:1456–63. doi: 10.1177/147323001103900434. [DOI] [PubMed] [Google Scholar]
- 14.Choi SY, Chang YW, Park HJ, Kim HJ, Hong SS, Seo DY. Correlation of the apparent diffusion coefficiency values on diffusion-weighted imaging with prognostic factors for breast cancer. Br J Radiol. 2012;85(1016):e474–9. doi: 10.1259/bjr/79381464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Onishi N, Kanao S, Kataoka M, Iima M, Sakaguchi R, Kawai M, et al. Apparent diffusion coefficient as a potential surrogate marker for Ki-67 index in mucinous breast carcinoma. J Magn Reson Imaging. 2015;41:610–5. doi: 10.1002/jmri.24615. [DOI] [PubMed] [Google Scholar]
- 16.Mesko S, Kupelian P, Demanes DJ, Huang J, Wang PC, Kamrava M. Quantifying the ki-67 heterogeneity profile in prostate cancer. Prostate Cancer. 2013;2013:717080. doi: 10.1155/2013/717080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kobayashi S, Koga F, Kajino K, Yoshita S, Ishii C, Tanaka H, et al. Apparent diffusion coefficient value reflects invasive and proliferative potential of bladder cancer. J Magn Reson Imaging. 2014;39:172–8. doi: 10.1002/jmri.24148. [DOI] [PubMed] [Google Scholar]
- 18.Tang Y, Dundamadappa SK, Thangasamy S, Flood T, Moser R, Smith T, et al. Correlation of apparent diffusion coefficient with Ki-67 proliferation index in grading meningioma. AJR Am J Roentgenol. 2014;202:1303–8. doi: 10.2214/AJR.13.11637. [DOI] [PubMed] [Google Scholar]
- 19.Martin B, Paesmans M, Mascaux C, Berghmans T, Lothaire P, Meert AP, et al. Ki-67 expression and patients survival in lung cancer: systematic review of the literature with meta-analysis. Br J Cancer. 2004;91:2018–25. doi: 10.1038/sj.bjc.6602233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Usuda K, Zhao XT, Sagawa M, Aikawa H, Ueno M, Tanaka M, et al. Diffusion-weighted imaging (DWI) signal intensity and distribution represent the amount of cancer cells and their distribution in primary lung cancer. Clin Imaging. 2013;37:265–72. doi: 10.1016/j.clinimag.2012.04.026. [DOI] [PubMed] [Google Scholar]
- 21.Ohno Y, Koyama H, Yoshikawa T, Matsumoto K, Aoyama N, Onishi Y, et al. Diffusion-weighted MRI versus 18F-FDG PET/CT: performance as predictors of tumor treatment response and patient survival in patients with nonsmall cell lung cancer receiving chemoradiotherapy. AJR Am J Roentgenol. 2012;198:75–82. doi: 10.2214/AJR.11.6525. [DOI] [PubMed] [Google Scholar]
- 22.Tanaka R, Horikoshi H, Nakazato Y, Seki E, Minato K, Iijima M, et al. Magnetic resonance imaging in peripheral lung adenocarcinoma: correlation with histopathologic features. J Thorac Imaging. 2009;24:4–9. doi: 10.1097/RTI.0b013e31818703b7. [DOI] [PubMed] [Google Scholar]
- 23.Matoba M, Tonami H, Kondou T, Yokota H, Higashi K, Toga H, et al. Lung carcinoma: diffusion-weighted MR imaging—preliminary evaluation with apparent diffusion coefficient. Radiology. 2007;243:570–7. doi: 10.1148/radiol.2432060131. [DOI] [PubMed] [Google Scholar]
- 24.Martin B, Paesmans M, Mascaux C, Berghmans T, Lothaire P, Meert AP, et al. Ki-67 expression and patients survival in lung cancer: systematic review of the literature with meta-analysis. Br J Cancer. 2004;91:2018–25. doi: 10.1038/sj.bjc.6602233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Warth A, Cortis J, Soltermann A, Meister M, Budczies J, Stenzinger A, et al. Tumour cell proliferation (Ki-67) in non-small cell lung cancer: a critical reappraisal of its prognostic role. Br J Cancer. 2014;111:1222–9. doi: 10.1038/bjc.2014.402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tabata K, Tanaka T, Hayashi T, Hori T, Nunomura S, Yonezawa S, et al. Ki-67 is a strong prognostic marker of non-small cell lung cancer when tissue heterogeneity is considered. BMC Clin Pathol. 2014;14:23–30. doi: 10.1186/1472-6890-14-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ahn HK, Jung M, Ha SY, Lee JI, Park I, Kim YS, et al. Clinical significance of Ki-67 and p53 expression in curatively resected non-small cell lung cancer. Tumour Biol. 2014;35:5735–40. doi: 10.1007/s13277-014-1760-0. [DOI] [PubMed] [Google Scholar]
- 28.Alper F, Kurt AT, Aydin Y, Ozgokce M, Akgun M. The role of dynamic magnetic resonance imaging in the evaluation of pulmonary nodules and masses. Med Princ Pract. 2013;22:80–6. doi: 10.1159/000339475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Karaman A, Kahraman M, Bozdoğan E, Alper F, Akgün M. Diffusion magnetic resonance imaging of thorax. Tuberk Toraks. 2014;62:215–30. [PubMed] [Google Scholar]
- 30.Araz O, Demirci E, Ucar EY, Calik M, Karaman A, Durur-Subasi I, et al. Roles of Ki-67, p53, transforming growth factor-β and lysyl oxidase in the metastasis of lung cancer. Respirology. 2014;19:1034–9. doi: 10.1111/resp.12345. [DOI] [PubMed] [Google Scholar]
- 31.Siegel R, Naishadham D, Jemal A. Cancer statistics, 2013. CA Cancer J Clin. 2013;63:11–30. doi: 10.3322/caac.21166. [DOI] [PubMed] [Google Scholar]
- 32.Zhang Z, Zhou Y, Qian H, Shao G, Lu X, Chen Q, et al. Stemness and inducing differentiation of small cell lung cancer NCI-H446 cells. Cell Death Dis. 2013;16:e633. doi: 10.1038/cddis.2013.152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Schaarschmidt BM, Buchbender C, Nensa F, Grueneien J, Gomez B, Köhler J, et al. Correlation of the apparent diffusion coefficient (ADC) with the standardized uptake value (SUV) in lymph node metastases of non-small cell lung cancer (NSCLC) patients using hybrid 18F-FDG PET/MRI. PLoS One. 2015;10(1):e0116277. doi: 10.1371/journal.pone.0116277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yoshida S, Kobayashi S, Koga F, Ishioka J, Ishii C, Tanaka H, et al. Apparent diffusion coefficient as a prognostic biomarker of upper urinary tract cancer: a preliminary report. Eur Radiol. 2013;23:2206–14. doi: 10.1007/s00330-013-2805-2. [DOI] [PubMed] [Google Scholar]
- 35.Yoshida S, Koga F, Kobayashi S, Ishii C, Tanaka H, Tanaka H, et al. Role of diffusion weighted magnetic resonance imaging in predicting sensitivity to chemoradiotherapy in muscle-invasive bladder cancer. Int J Radiat Oncol Biol Phys. 2012;83:e21–e7. doi: 10.1016/j.ijrobp.2011.11.065. [DOI] [PubMed] [Google Scholar]
- 36.Wieduwilt MJ, Valles F, Issa S, Behler CM, Hwang J, McDermott M, et al. Immunochemotherapy with intensive consolidation for primary CNS lymphoma: a pilot study and prognostic assessment by diffusion-weighted MRI. Clin Cancer Res. 2012;18:1146–55. doi: 10.1158/1078-0432.CCR-11-0625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Srinivasan A, Chenevert TL, Dwamena BA, Eisbruch A, Watcharotone K, Myles JD, et al. Utility of pretreatment mean apparent diffusion coefficient and apparent diffusion coefficient histograms in prediction of outcome to chemoradiation in head and neck squamous cell carcinoma. J Comput Assist Tomogr. 2012;36:131–7. doi: 10.1097/RCT.0b013e3182405435. [DOI] [PubMed] [Google Scholar]
- 38.Pope WB, Lai A, Mehta R, Qiao J, Young JR, Xue X, et al. Apparent diffusion coefficient histogram analysis stratifies progression-free survival in newly diagnosed bevacizumab-treated glioblastoma. AJNR Am J Neuroradiol. 2011;32:882–9. doi: 10.3174/ajnr.A2385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kıvrak AS, Paksoy Y, Erol C, Koplay M, Özbek S, Kara F. Comparison of apparent diffusion coefficient values among different MRI platforms: a multi-center phantom study. Diagn Interv Radiol. 2013;19:433–7. doi: 10.5152/dir.2013.13034. [DOI] [PubMed] [Google Scholar]
- 40.Rosenkrantz AB, Oei M, Babb JS, Niver BE, Taouli B. Diffusion-weighted imaging of the abdomen at 3.0 Tesla: image quality and apparent diffusion coefficient reproducibility compared with 1.5 Tesla. J Magn Reson Imaging. 2011;33:128–35. doi: 10.1002/jmri.22395. [DOI] [PubMed] [Google Scholar]