Abstract
Sleep is an important pillar of health and a modifiable risk factor for diabetes, stroke and obesity. Little is known of diet and sleep patterns of Hispanics/Latinos in the US. Here we examine eating behavior as a function of sleep duration in a sub-sample of 11,888 participants from the Hispanic Community Health Study/Study of Latinos, a community-based cohort study of Hispanics aged 18–74 years in four US cities. Using a cross-sectional probability sample with self-report data on habitual sleep duration and up to two 24-hour dietary recalls, we quantified the Alternative Healthy Eating Index (AHEI-2010) score, a measure of diet quality, and intake of selected nutrients related to cardiovascular health. Linear regression models were fit to estimate least-square means of usual nutrient intake of saturated fats, potassium density, fiber, calcium, caffeine and the AHEI-2010 score by sleep duration adjusting for age, sex, Hispanic/Latino background, income, employment status, education, depressive symptomology, and years lived in the US. Distribution of calories over the day and association with sleep duration and BMI were also examined.
Short sleepers (≤ 6 hr) had significantly lower intake of potassium, fiber and calcium and long sleepers (≥9 hr) had significantly lower intake of caffeine compared to others sleepers after adjusting for covariates. However no difference in the AHEI-2010 score was seen by sleep duration. Significantly more long sleepers, compared to intermediate and short sleepers, reported having ≥30% total daily calories before bedtime. Not consuming a snack or meal within three hours before bedtime was associated with higher AHEI-2010 scores. These findings identify novel differences in dietary patterns by sleep duration in a Hispanic/Latino population in the U.S.
INTRODUCTION
There is limited information on the impact of dietary patterns on sleep duration and vice versa in the mainstream US population (Grandner, Jackson, Gerstner & Knutson, 2013; Grandner, Jackson, Gerstner & Knutson, 2014; Kant & Graubard, 2014). Studies examining diet and sleep duration in US Hispanics are sparse and especially lacking for non-Mexican-American Hispanics. It is not known, for example, whether diet and sleep patterns change as Hispanics migrate to the US; how length of residency in the US can impact sleep and diet patterns and how in turn these factors can impact health.
Recent data from NHANES suggest that the architecture of eating behavior differs by sleep duration with short sleepers skipping main meals and consuming more energy from snacks; additionally consumption of sugars, fiber, caffeine and alcohol also differs by sleep duration (Kant & Graubard, 2014). As Mexicans in the US were the only group included in the afore-mentioned NHANES study and data on their eating behavior are not separately described, little is known as to whether there are differences in eating behavior by sleep duration between minority groups such as Hispanics/Latinos and non-Hispanics in the US. This information is of importance as Hispanics/Latinos living in the US are at increased risk for obesity, diabetes and stroke and are more likely to report extremes of sleep duration compared to non-Hispanic US whites (Daviglus et al., 2012; Kaplan et al., 2014; Patel, Malhotra, Gottlieb, White & Hu, 2006; Schneiderman et al., 2014; Stamatakis, Kaplan & Roberts, 2007). According to epidemiologic data short sleep duration is associated with unfavorable metabolic factors such as impaired glucose tolerance, insulin resistance, increased ghrelin, decreased leptin and increased body mass index (Ayas et al., 2003; Knutson, Spiegel, Penev & Van Cauter, 2007; Patel & Hu, 2008; Spiegel, Tasali, Penev & Van Cauter, 2004). Untreated sleep-disordered breathing is associated with diabetes and hypertension and decreased quantity and quality of sleep, especially short sleep duration and insomnia which are linked to diabetes among a diverse cohort of Hispanics/Latinos in the U.S. (Cespedes et al., 2015; Redline et al., 2014). Short sleep duration is also significantly associated with obesity in same population (Patel et. al., 2015). Diet-related associations with short sleep include low-nutrient energy-dense foods and hunger for high fat, high carbohydrate foods and snacks (Grandner, Kripke, Naidoo & Langer, 2010; Shi, McEvoy, Luu & Attia, 2008; Stern et al., 2014; Weiss et al., 2010.) Prolonged sleep (≥ 9hrs) is associated with significant morbidity as well as mortality; however its association with calorie intake and food patterns is less consistent (Patel & Hu, 2008).
Timing of intake may also impact sleep duration; calorie intake after 8 pm for example is associated with obesity (Baron, Reid, Kern & Zee, 2011). Eating a meal that is heavier than usual is associated with onset of acute coronary syndrome a few hours later (Lipovetzky et al., 2004; Nawrot, Perez, Kunzli, Munters & Nemery, 2011).
Overall there appears to be a bi-directionality in the association between sleep and diet. Possible mechanisms by which dietary intake may disturb sleep include metabolism, body temperature and respiratory quotient (Gluck et al., 2011). This study explores the association of self-reported sleep duration with diet quality and meal size before bed-time among participants in the Hispanic Community Health Study/Study of Latinos (HCHS/SOL), an NIH-funded study of Hispanics/Latinos in four urban US cities: Bronx, NY, Chicago, IL, Miami, FL, and San Diego, CA.
MATERIALS & METHODS
Sample
The HCHS/SOL is a community-based cohort study of 16,415 Hispanic/Latino participants aged 18–74 years living in four US cities including the following backgrounds: Central American, Dominican, Cuban, Mexican, Puerto Rican and South American. The goals of the HCHS/SOL are to describe the prevalence of risk and protective factors for chronic conditions (e.g. cardiovascular disease (CVD), diabetes and pulmonary disease), and to quantify all-cause mortality, fatal and non-fatal CVD and pulmonary disease, and pulmonary disease exacerbation over time. The baseline clinical examination (2008–2011) included comprehensive biological (e.g., anthropometrics, blood draw, oral glucose tolerance test, ankle brachial pressure index, electrocardiogram), behavioral (e.g. dietary intake assessed with two 24-hour recalls, sleep habits, overnight sleep exam for apneic events) and socio-demographic (e.g., socio-economic status, migration history) assessments (Lavange et al., 2010; Sorlie et al., 2010). HCHS/SOL selected households with a stratified 2-stage probability sampling design. The first stage randomly sampled census blocks by Hispanic/Latino concentration and proportion of high and low socioeconomic status. The second stage randomly selected households within the census blocks from stage one by US Postal Service registries. Further details of the sample design and cohort selection have been previously described (Lavange et al., 2010). The Institutional Review Boards of the participating institutions approved the study protocol and all participants provided written informed consent.
This analysis describes results from 11,888 participants as reflected in Tables 1–3; 4,527 participants were excluded for the following non-exclusive reasons: missing self-reported sleep data (n = 885), invalid dietary data [includes participants for whom energy intakes are considered implausible ((< 600 kcal for women and < 800 kcal for men) (Subar et al., 2001) or considered unreliable by interviewer (n = 149)). In this sample exclusions were not made at the upper end as the highest calorie intake was 2,813 kcal for women and 3,996 kcal for men, which was deemed plausible since two-thirds of the sample were overweight or obese. Participants did not have to have both dietary recalls to be included in the analyses; those with at least one valid dietary recall were included. In general completion rate of the two 24 hr dietary recalls was extremely high with 97% of the participants completing the first recall and 91% of participants completing the second recall.
Table 1.
Unadjusted measures of diet quality by socio-demographic and health characteristics (n=11,888)a
| Characteristic | Saturated fats density (% total energy) |
Potassium density (mg per 1,000 kcal) |
Caffeine (mg per 1,000 kcal) |
AHEI-2010 (per 1,000 kcal) |
|
|---|---|---|---|---|---|
| N | Mean (95% CI) | Mean (95% CI) | Mean (95% CI) | Mean (95% CI) | |
| Hispanic/Latino background | |||||
| Dominican | 1073 | 9.26 (9.17, 9.35)*** | 1374 (1353, 1396)** | 41.01 (37.87, 44.14)*** | 31.45 (30.58, 32.32)*** |
| Central American | 1248 | 9.58 (9.50, 9.65)*** | 1262 (1246, 1278)*** | 53.09 (49.83, 56.34) | 26.60 (25.86, 27.33)* |
| Cuban | 1637 | 10.08 (10.02, 10.14) | 1254 (1240, 1268)*** | 64.18 (60.33, 68.03)*** | 21.87 (21.43, 22.30)*** |
| Mexican (Ref) | 4849 | 10.16 (10.09, 10.22) | 1327 (1315, 1340) | 50.54 (47.63, 53.44)** | 27.84 (27.50, 28.19) |
| Puerto Rican | 2028 | 10.50 (10.42, 10.58)*** | 1172 (1156, 1187)*** | 61.68 (57.58, 65.77)*** | 24.02 (23.44, 24.59)*** |
| South American | 713 | 9.51 (9.40, 9.62)*** | 1336 (1309, 1362)*** | 54.73 (49.34, 60.13) | 25.63 (24.73, 26.53) |
| Mixed/Other | 340 | 10.35 (10.17, 10.52) | 1229 (1198, 1261)*** | 49.64 (40.97, 58.30) | 24.48 (23.45, 25.52) |
| Sex | |||||
| Female (Ref) | 7561 | 10.03 (9.98, 10.08) | 1341 (1332, 1351) | 58.72 (56.61, 60.82) | 29.41 (29.01, 29.80) |
| Male | 4327 | 10.07 (10.01, 10.12) | 1211 (1201, 1221)*** | 48.90 (46.63, 51.17)*** | 21.85 (21.54, 22.15)*** |
| Age Group (year) | |||||
| 18–29 (Ref) | 2031 | 10.39 (10.32, 10.45) | 1140 (1130, 1151) | 34.00 (31.39, 36.60) | 22.41 (21.99, 22.82) |
| 30–39 | 1777 | 10.10 (10.01, 10.18)*** | 1236 (1223, 1248)*** | 51.97 (48.45, 55.49)*** | 24.57 (24.03, 25.12)*** |
| 40–49 | 3056 | 9.97 (9.90, 10.03)*** | 1318 (1303, 1334)*** | 61.25 (58.40, 64.11)*** | 26.43 (25.88, 26.97)*** |
| 50–59 | 3053 | 9.82 (9.76, 9.88)*** | 1388 (1373, 1403)*** | 73.14 (68.88, 77.41)*** | 29.33 (28.65, 30.01)*** |
| 60–69 | 1621 | 9.65 (9.57, 9.73)*** | 1477 (1460, 1493)*** | 70.56 (65.50, 75.61)*** | 31.92 (31.15, 32.69)*** |
| 70–74 | 346 | 9.57 (9.41, 9.73)*** | 1535 (1502, 1568)*** | 62.10 (53.94, 70.25)*** | 32.55 (31.09, 34.00)*** |
| Education | |||||
| Less than HS (Ref) | 4534 | 9.90 (9.84, 9.96) | 1311 (1297, 1325) | 52.39 (49.49, 55.29) | 28.05 (27.56, 28.55) |
| HS equivalent | 3008 | 10.12 (10.05, 10.18)*** | 1250 (1238, 1262)*** | 49.83 (47.56, 52.11) | 24.70 (24.26, 25.15)*** |
| More than HS | 4125 | 10.13 (10.07, 10.20)*** | 1283 (1272, 1295)** | 59.08 (56.18, 61.98)** | 25.36 (24.97, 25.74)*** |
| Income | |||||
| Less than $10,000 (Ref) | 1789 | 9.98 (9.89, 10.06) | 1298 (1279, 1318) | 54.41 (50.22, 58.60) | 27.33 (26.67, 28.00) |
| $10,001–$20,000 | 3561 | 9.97 (9.91, 10.03) | 1294 (1283, 1305) | 54.04 (50.96, 57.11) | 26.60 (26.11, 27.09) |
| $20,001–$40,000 | 3620 | 10.05 (9.99, 10.10) | 1278 (1265, 1290) | 53.18 (50.67, 55.69) | 25.56 (25.10, 26.01)*** |
| $40,001–$75,000 | 1415 | 10.23 (10.13, 10.32)** | 1272 (1251, 1293) | 57.30 (53.08, 61.52) | 25.22 (24.64, 25.81)*** |
| More than $75,000 | 452 | 10.20 (10.05, 10.35) | 1306 (1270, 1342) | 66.10 (56.98, 75.22) | 25.01 (23.98, 26.03)** |
| Not reported | 1051 | 10.06 (9.97, 10.15) | 1257 (1235, 1279) | 49.38 (44.99, 53.77) | 26.14 (25.22, 27.07) |
| Employed | |||||
| Retired not currently employed | 1181 | 9.69 (9.61, 9.78) | 1465 (1447, 1484) | 64.35 (59.93, 68.77) | 31.55 (30.77, 32.33) |
| Not retired, not employed | 5536 | 10.14 (10.09, 10.18)*** | 1265 (1255, 1275)*** | 51.39 (48.86, 53.92)*** | 25.95 (25.52, 26.39)*** |
| Employed part-time (≤35 hrs/week) | 1604 | 10.00 (9.92, 10.09)*** | 1289 (1273, 1304)*** | 50.47 (46.95, 53.99)*** | 26.44 (25.87, 27.01)*** |
| Employed full-time (>35 hrs/week) (Ref) | 3567 | 10.01 (9.95, 10.07)*** | 1264 (1250, 1277)*** | 58.53 (55.66, 61.39) | 24.66 (24.24, 25.07)*** |
| Current occupation | |||||
| Non-skilled worker | 1649 | 9.87 (9.78, 9.95)*** | 1271 (1256, 1286)*** | 50.57 (46.84, 54.30) | 25.54 (25.00, 26.08)*** |
| Service worker | 913 | 9.99 (9.89, 10.09)** | 1281 (1261, 1301)*** | 58.92 (53.02, 64.81)** | 25.70 (24.97, 26.43)*** |
| Skilled worker | 1236 | 10.14 (10.04, 10.23) | 1270 (1251, 1289)*** | 57.94 (53.46, 62.43)*** | 25.12 (24.52, 25.72)*** |
| Professional | 643 | 10.14 (10.00, 10.27) | 1293 (1265, 1320)*** | 65.74 (58.60, 72.87)*** | 25.64 (24.86, 26.41)*** |
| Other | 730 | 9.99 (9.89, 10.09)** | 1245 (1223, 1267)*** | 50.78 (46.05, 55.52) | 23.78 (22.97, 24.60)*** |
| Homemaker | 4244 | 9.97 (9.91, 10.03)*** | 1360 (1347, 1373)*** | 58.90 (56.06, 61.73)*** | 29.73 (29.24, 30.22)*** |
| Not employedb (Ref) | 2473 | 10.20 (10.14, 10.27) | 1211 (1199, 1222) | 46.20 (43.00, 49.40) | 23.05 (22.59, 23.51) |
| Marital status | |||||
| Living with partner (Ref) | 6137 | 10.11 (10.06, 10.15) | 1253 (1244, 1262) | 51.75 (49.40, 54.11) | 25.54 (25.17, 25.92) |
| Not living with partner | 5738 | 9.98 (9.93, 10.04)*** | 1317 (1305, 1328)*** | 57.16 (54.61, 59.71)** | 26.68 (26.24, 27.11)*** |
| Underweight | 95 | 10.41 (10.07, 10.76) | 1146 (1083, 1208)** | 33.98 (24.53, 43.43)** | 21.95 (20.64, 23.26)* |
| Normal weight (Ref) | 2484 | 10.11 (10.05, 10.18) | 1254 (1240, 1267) | 51.42 (48.07, 54.77) | 24.41 (23.93, 24.90) |
| Overweight | 4614 | 9.98 (9.92, 10.04)* | 1297 (1285, 1308)*** | 53.88 (51.21, 56.56) | 26.28 (25.89, 26.66)*** |
| Obese | 4658 | 10.06 (10.01, 10.12) | 1294 (1283, 1306)*** | 57.44 (54.73, 60.16)* | 27.10 (26.65, 27.54)*** |
| High depressive symptomology | |||||
| Yes (≥10) | 3577 | 10.05 (10.00, 10.09) | 1282 (1273, 1291) | 52.77 (50.86, 54.68) | 25.71 (25.37, 26.05) |
| No (<10) (Ref) | 8249 | 10.04 (9.98, 10.10) | 1290 (1277, 1302) | 58.70 (55.45, 61.96)** | 27.07 (26.56, 27.58)*** |
| Frequency of eating outside of home | |||||
| No recalls (Ref) | 7871 | 10.00 (9.96, 10.04) | 1308 (1298, 1318) | 53.64 (51.42, 55.87) | 26.83 (26.40, 27.27) |
| 1 recall | 2800 | 10.17 (10.09, 10.24)*** | 1246 (1233, 1258)*** | 54.26 (51.10, 57.43) | 24.90 (24.49, 25.30)*** |
| Both recalls | 1217 | 10.04 (9.95, 10.13) | 1233 (1215, 1250)*** | 59.35 (54.98, 63.71) | 24.48 (23.89, 25.07)*** |
| Mainly/Mostly Hispanic foods | |||||
| Yes (Ref) | 9084 | 10.27 (10.20, 10.33) | 1247 (1233, 1261) | 55.25 (51.74, 58.75) | 25.42 (24.94, 25.90) |
| No | 2778 | 9.97 (9.93, 10.01)*** | 1297 (1288, 1307)*** | 54.19 (52.18, 56.19) | 26.33 (25.93, 26.74)** |
| Nativity/Years in US | |||||
| US Born (Ref) | 2117 | 10.55 (10.49, 10.61) | 1155 (1143, 1166) | 48.62 (45.42, 51.81) | 22.97 (22.60, 23.33) |
| FB, ≥ 10 yrs in US | 6479 | 9.85 (9.80, 9.90)*** | 1353 (1343, 1363)*** | 59.20 (56.98, 61.42)*** | 28.57 (28.17, 28.97)*** |
| FB, < 10 yrs in US | 2797 | 9.97 (9.91, 10.03)*** | 1276 (1261, 1290)*** | 52.07 (48.80, 55.34) | 24.66 (24.05, 25.26)*** |
All values, except n, account for complex survey design and incorporate sample weights. Level of significance calculated with Bonferroni correction to account for multiple comparisons.
Not employed = includes both retired and not retired
Abbreviation and definitions: HS = high school; hrs = hours; underweight is BMI < 18.5; normal weight is BMI ≥ 18.5 and < 25; overweight is BMI ≥ 25 and < 30; obese is BMI ≥ 30; CES-D10 = Center for Epidemiology Study Depression scale; US born = born within 50 US states; FB = foreign-born, outside of 50 US states;
for P < 0.05;
for P < 0.01;
for P < 0.001
Table 3.
| Total saturated fats density (% total energy) |
Potassium density (mg per 1,000 kcal) |
Caffeine density (mg per 1,000 kcal) |
AHEI-2010 Score per 1,000 kcalb |
Calcium (mg per 1,000 kcal) |
Fiber (g per 1,000 kcal) |
|
|---|---|---|---|---|---|---|
| Sleep duration | Mean (95% CI) | Mean (95% CI) | Mean (95% CI) | Mean (95% CI) | Mean (95% CI) | Mean (95% CI) |
| Short | 10.0 (9.9, 10.1) | 1265.5 (1249.8, 1281.3) | 58.5 (53.7, 63.2) | 25.7 (25.1, 26.3) | 408.6 (401.0, 416.3) | 8.97 (8.82, 9.12) |
| Intermediate (Ref) | 10.1 (10.0, 10.1) | 1284.9 (1278.7, 1291.2) | 55.7 (53.9, 57.6) | 26.1 (25.9, 26.4) | 421.7 (419.0, 424.5) | 9.20 (9.14, 9.26) |
| Long | 10.1 (10.0, 10.1) | 1277.3 (1266.4, 1288.1) | 47.9 (45.2, 50.6) | 25.9 (25.5, 26.3) | 416.5 (411.6, 421.4) | 9.16 (9.06, 9.27) |
All values account for complex survey design and incorporate sample weights.
Definitions: CI = confidence interval; sleep duration - short is ≤ 6 hours; intermediate is > 6 and ≤ 9 hours; long is > 9 hours
AHEI-2010 score = Alternative Healthy Eating Index-2010 measures adherence to 2010 Dietary Guidelines for Americans for the following 11 components: vegetables without potatoes, whole fruit, whole grains, sugar sweetened beverages and fruit juice, nuts and legumes, red/processed meat, trans fat, long-chain fats, polyunsaturated fatty acids, sodium, and alcohol.
Adjusted for age, sex, Hispanic/Latino background, education, income, employment status, depressive symptomology, and years lived in mainland US. Bold values indicate the mean is statistically different than the reference group of intermediate sleepers at P<0.05
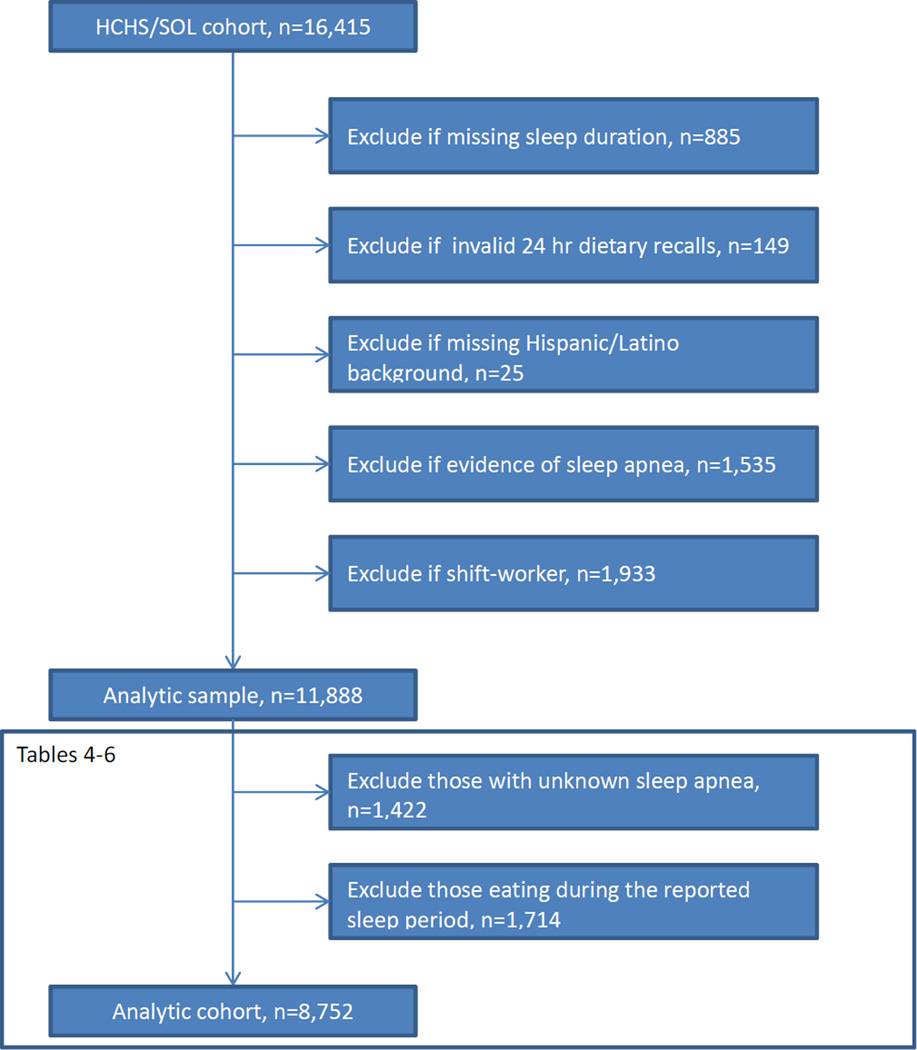
Additionally participants with missing Hispanic/Latino background (n = 25) were excluded (See Figure 1.) To minimize confounding relating to physiological or unusual sleep, participants classified as having moderate or more severe sleep apnea [n = 1,535; apnea hypopnea index ≥ 15 events/hour] based on overnight home sleep apnea testing (Redline et al, 2014), and shift workers (n = 1,933) were also excluded. Shift-workers were defined as individuals who self-reported their usual work schedule as being night shift, split shift, irregular shift/on-call, or rotating shift. Because Tables 4–8 focus on distribution of calorie intake during the day and also the association of BMI, sleep timing and meal size, individuals who had unknown sleep apnea status (n=1,422) and those who reported eating in the middle of the night (n = 1,714), i.e. eat during the reported sleep period, were additionally excluded from analyses done in Tables 4–8.
Figure 1.
Flow diagram of analytic sample, Hispanic Community Health Study/Study of Latinos
Table 4.
Percent (95% CI) consuming ≥30% total daily kcal at last meal or snack before bedtime by socio-demographic characteristics among (n= 8,752), HCHS/SOLa
| ≥30% of total daily kcal at last meal or snack near bedtimeb |
|||
|---|---|---|---|
| Socio-demographic characteristic |
Subgroup N | % (95% CI) | Pc |
| Overall | 8,752 | 16.5 (15.4, 17.8) | |
| Age Group (years) | |||
| 18–29 | 1,408 | 15.6 (13.3, 18.1) | |
| 30–39 | 1,344 | 15.7 (13.1, 18.8) | |
| 40–49 | 2,284 | 19.0 (16.6, 21.7) | |
| 50–59 | 2,253 | 16.2 (14.4, 18.3) | |
| 60–69 | 1,209 | 15.7 (13.0, 18.9) | |
| 70+ | 250 | 16.3 (10.0, 25.6) | |
| Hispanic/Latino Background | *** | ||
| Dominican | 759 | 15.0 (12.0, 18.7) | |
| Central American | 880 | 18.3 (15.4, 21.6) | |
| Cuban | 1,103 | 23.9 (21.0, 27.1) | |
| Mexican | 3,848 | 14.7 (12.9, 16.7) | |
| Puerto Rican | 1,392 | 13.5 (11.1, 16.3) | |
| South American | 545 | 14.1 (11.1, 17.6) | |
| Mixed/Other | 225 | 17.1 (11.3, 25.0) | |
| Sex | *** | ||
| Women | 5,646 | 14.1 (12.8, 15.5) | |
| Men | 3,106 | 19.7 (17.9, 21.8) | |
| Education | |||
| Less than HS | 3,367 | 15.9 (14.2, 17.9) | |
| HS equivalent | 2,203 | 18.6 (16.3, 21.2) | |
| More than HS | 3,018 | 15.7 (13.9, 17.6) | |
| Yearly household income | * | ||
| Less than $10,000 | 1,275 | 15.7 (13.3, 18.4) | |
| $10,001–$20,000 | 2,628 | 18.4 (16.0, 21.0) | |
| $20,001–$40,000 | 2,718 | 15.4 (13.6, 17.5) | |
| $40,001–$75,000 | 1,039 | 13.9 (11.0, 17.3) | |
| More than $75,000 | 344 | 12.7 (8.3, 18.9) | |
| Missing | 748 | 21.6 (18.3, 25.4) | |
| Nativity/Years in US | *** | ||
| US Born | 1,487 | 15.2 (12.9, 17.9) | |
| FB, ≥ 10 yrs in US | 4,823 | 14.5 (13.2, 16.0) | |
| FB, < 10 yrs in US | 2,080 | 20.8 (18.5, 23.3) | |
All values except subgroup N account for complex survey design and incorporate sample weights.
Near bedtime is defined as being within 3 hours of bedtime with a buffer of one hr
P value obtained from Chi-square tests at
for P < 0.05;
for P < 0.01;
for P < 0.001.
Abbreviations and definitions: CI = confidence interval; HS = high school; US born = born within 50 US states; FB = foreign-born, born outside 50 US states.
Table 8.
| Night 0:00–6:00 |
Morning 6:00–12:00 |
Afternoon 12:00–18:00 |
Evening 18:00–24:00 |
||
|---|---|---|---|---|---|
| Subgroup n |
Mean (95% CI) | Mean (95% CI) | Mean (95% CI) | Mean (95% CI) | |
| Sleep duration | |||||
| Short | 787 | 6.6 (5.0, 8.3) | 20.2 (18.8, 21.5) | 33.5 (31.5, 35.5) | 29.3 (27.6, 31.1) |
| Intermediate (Ref) | 6,501 | 6.3 (5.2, 7.4) | 21.0 (20.5, 21.5) | 33.0 (32.4, 33.6) | 28.1 (27.3, 28.8) |
| Long | 1,464 | 10.0 (4.7, 15.2) | 19.6 (18.6, 20.5)** | 32.2 (30.9, 33.4) | 26.8 (25.7, 28.0) |
| BMI | |||||
| Underweight | 70 | 5.5 (3.8, 7.2) | 19.6 (17.0, 22.2) | 32.8 (28.2, 37.3) | 29.1 (24.6, 33.5) |
| Normal weight (Ref) | 1,810 | 5.5 (3.8, 7.2) | 19.8 (19.0, 20.6) | 32.5 (31.4, 33.6) | 29.3 (28.1, 30.5) |
| Overweight | 3,506 | 7.3 (5.7, 8.9) | 21.1 (20.4, 21.8)* | 32.8 (31.9, 33.7) | 27.9 (27.0, 28.8) |
| Obese | 3,345 | 6.3 (5.2, 7.5) | 20.9 (20.3, 21.6) | 33.3 (32.5, 34.2) | 27.0 (26.1, 27.9)** |
All values except N account for complex survey design and incorporate sample weights.
Adjusted for midpoint of sleep with centering of midpoint of sleep at 3:30 am
Definitions: CI = confidence interval; sleep duration - short is ≤ 6 hours; intermediate is > 6 and ≤ 9 hours; long is > 9 hours; underweight is BMI < 18.5 kg/m2; normal weight is BMI ≥ 18.5 and < 25 kg/m2; overweight is BMI ≥ 25 and < 30 kg/m2; obese is BMI ≥ 30 kg/m2.
P value obtained from t-tests at
for P < 0.05;
for P < 0.01;
for P < 0.001.
Covariates
Demographic factors, socioeconomic factors, employment information, and screening information about depressive symptoms from the shortened Center for Epidemiologic Studies Depression Scale (CES-D10) (Andresen, Malmgren, Carter & Patrick, 1994) were obtained from questionnaires at the baseline examination. Consistent with prior studies, the distribution of CES-D10 scores was dichotomized for analysis, with elevated depressive symptomology defined where participants scored ≥ 10 on the CES-D10 (Li et al., 2012). This cut-point denotes elevated depressive symptoms, which may reflect clinical depression, but is not equivalent to a clinical diagnosis. Analyses were not adjusted for self-reported physical activity because no association was seen between self-reported physical activity and a composite diet score related to cardiovascular disease that included fiber, calcium, saturated fats and potassium. Physical activity related accelerometry data were not used for this analysis as they had high missingness rate of 22.3%.
Sleep duration
Information on sleep duration was based on the Sleep Heart Health Study Sleep Questionnaire (Lind et al., 2003). This questionnaire was translated and back-translated into Spanish by certified translators. Participants were asked about bedtimes and wake-times on both week-days and week-ends. [Questions consisted of the following: “What time do you usually go to bed? (On weekdays? On weekends?) What time do you usually wake up? (On weekdays? On weekends?”)] Sleep duration was computed as the difference between wake up time and bedtime and a weighted average of weekday and weekend durations was computed for habitual sleep duration. Habitual sleep duration was categorized as short (≥3 and ≤ 6 hours), intermediate (> 6 and ≤ 9 hours) and long (>9 and ≤ 14 hours). The cut-off of 6 hr represents approximately the 10th percentile in the analytic sample and has been associated with increased risk of adverse health outcomes and 9 hr the 80th percentile in sleep duration in this cohort. These extreme values are associated with increased risk of chronic disease in adults (Patel & Hu, 2008).
Dietary variables
As this is an exploratory study to investigate eating behavior by sleep duration we examined both nutrients and a healthy dietary pattern score. Dietary variables were derived from two 24-hour dietary recalls (one in-person at baseline and a second telephone recall performed five days to three months later) collected at the baseline examination (Siega-Riz et al., 2014). The 24-hour dietary recalls were collected using Nutrition Data System for Research (NDSR) (University of Minnesota). Certified bilingual interviewers conducted the dietary interviews at each site. Usual intake of total energy and micronutrients was estimated using the National Cancer Institute (NCI)-method with valid recalls only, which accounts for intra-person variability by taking into account multiple 24-hour dietary recalls and covariates. For this analysis these include: adjustment for age, sex, Hispanic/Latino background, clinical center, week-end (including Friday) sequence (1st recall-conducted in person or 2nd recall majority conducted by phone), self-reported intake amount (more or less than usual intake) (Tooze et al., 2010; 2006). Nutrients were assessed per 1,000 kcal to control for calories and mitigate effects of measurement error that might result in misreporting of energy. Of all the dietary data of interest only two pairs of dietary variables as expected correlated highly: predicted percentage of calories from saturated fats plus predicted percentage of calories from total fats correlated positively and predicted percentage of calories for carbohydrates plus predicted percentage of calories from total fats correlated negatively. Therefore all dietary data of interest are presented.
A food based dietary scoring system the Alternative Healthy Eating Index-2010 (AHEI-2010) was used to provide a comprehensive view of dietary quality (Liu et al., 2012; Chiuve et al., 2012). The AHEI-2010 score is the sum of 11 individual components (vegetables, whole fruit, whole grains, sugar sweetened beverages and fruit juice, nuts and legumes, red/processed meat, trans fat, long-chain fats, polyunsaturated fatty acids, sodium, and alcohol) which each has a range from 0 to 10 with 10 being the best score. The AHEI-2010 score ranges from 0 – 110 and a higher score represents healthier eating habits and has been associated with reduced risks for diabetes and coronary heart disease (Chiuve et al., 2012).
Calories eaten outside the home (work, deli/take-out store, restaurant/cafeteria/fast food, etc.) were summed by dietary recall. Only data on location where meals and snacks were eaten were available; it was not possible to ascertain whether meals and snacks purchased outside the home were eaten at home. If the percentage of calories consumed outside the home was ≥ 50%, then the participant was classified as “frequent” for the day. The “eating out” variable is a 3-level variable: not frequent both recalls; frequent, 1 recall only; frequent, both recalls.
In addition to the 24 hour dietary recall, participants were asked about their tendencies to eat more Hispanic versus American foods as they defined them. This question consisted of the following: “How often do you or your family usually eat: mainly Hispanic/Latino foods; mostly Hispanic/Latino and some American food; equal amounts of both Hispanic/Latino and American foods; mainly American foods and some Hispanic/Latinos foods; mostly American foods.” The 5-level response was dichotomized into a binary variable as low food acculturation when a participant reported mainly or mostly eating Hispanic/Latino foods, or high acculturation when otherwise.
Meal timing
More than 30% of our analytic sample reported eating and/or drinking during their self-reported sleep times. Since awakening time and bed time on the day of the dietary recall were not collected and these times are based on data from a separate questionnaire that assessed usual awakening time and bed times, a buffer of one hour was created to tolerate plausible eating and or drinking surrounding the sleep period on the specific day of the dietary recall. For example, a participant may indicate eating at 10:30 pm on the 24 hr recall, but report usual bed time as 10 pm on the sleep questionnaire. For this person the acceptable buffer of time for meal or snack intake was 1 hour after bedtime (up to 11 pm) and the meal or snack consumed at 10:30 pm was included in the analysis. Beyond this window, participants who reported eating during sleep hours were excluded from the meal and snack timing analysis since they may have been (1) eating during reported sleep period, (2) could have had suspect meal and snack timing data due to data entry error or (3) have highly variable mealtimes. We also explored whether participants had consumed a meal or snack with a relatively large percentage of daily calories near bedtime as indicated by ≥ 30% of total daily calorie intake. Near bedtime was defined as three hours before bedtime not including the one hour buffer mentioned earlier because eating after 8 pm is linked to risk for obesity and median sleep time in our sample was approximately 11 pm. (Baron, Reid, Van Horn & Zee, 2013).
In order to explore the association of meal and snack timing with sleep duration, calorie intake distribution over the 24-hour period was quantified over four bins a day that indicate six hour intervals during which meals and snacks could be consumed: morning (6:00 am – < 12:00 pm), afternoon (12:00 pm – < 18:00 pm), evening (18:00 pm – < 24:00 pm) and night (0:00 am – < 6:00 am). The mean percentage of kilocalories consumed during each time bin was adjusted for midpoint of sleep to account for differences in bedtime. This accounting was done using data from the sleep questionnaire. The midpoint for sleep time was defined as the average time midpoint (time between wake and sleep time) during the week. Midpoint of sleep for weekday and weekend days was derived using the sleep questionnaire data. The weighted mean (i.e. 2/7 for weekend days and 5/7 for weekdays) of the two midpoints was used in the analysis. In order to preserve the sleep midpoint as a continuous covariate within a 24 hr clock, each person’s midpoint of sleep was converted to a distance from 3:30 am—the average midpoint of sleep for this population.
Statistical analysis
Unadjusted means of usual intake of saturated fat, potassium, calcium, fiber and other nutrients as well as the AHEI-2010 score were calculated by socio-demographic and health characteristics. Differences in mean usual intake were calculated using t-tests; level of significance was calculated with a Bonferroni correction to account for multiple comparisons. Linear regression was used to estimate least-square means of usual nutrient intakes related to cardiovascular health and the AHEI-2010 score by sleep duration adjusting for age, sex, Hispanic/Latino background, education, income, employment status, depressive symptomology, and years lived in mainland US. Only the measures of saturated fat, potassium, calcium and fiber-dietary variables related to cardiovascular health (Liu et al., 2012), the AHEI-2010 score and caffeine were adjusted by this larger set of covariates.
Eating any food near bedtime and ≥ 30 % total daily calories near bed-time by socio-demographic characteristics, sleep duration and BMI category were calculated using cross-tabulations. Differences in the percent of any meal or snack or eating ≥30% total daily calories at a meal or snack before bedtime by socio-demographic characteristics were quantified with Chi-square tests. To estimate the distribution of meals and snacks eaten during time of day, defined as time bin, the percentage of total calories consumed during each time bin for each person was calculated; then the mean proportion of kilocalories per day was estimated within each time bin by sleep duration and BMI category using linear regression models. Differences in the proportion of kilocalories per day between short and long sleep duration sleepers compared to intermediate sleep duration sleepers were quantified using t-tests in separate linear regression models by time bin. Differences between non-normal weight BMI category compared to normal weight by this method were also assessed. All statistical tests were considered significant at P <0.05. All analyses were performed on SAS (version 9.3, 2011, SAS Institute Inc.) and SAS-callable SUDAAN (version 11.0, 2012, Research Triangle Institute) to account for the complex survey design and the sampling weights in HCHS/SOL.
RESULTS
Characteristics of the Sample
From the 16,415 HCHS/SOL cohort, 11,888 participants were included in this analysis. The excluded (n=4,527) and analytic sample (n = 11,888) differed in the following manner: the analytic sample had a significantly higher proportion of females (63.6% versus 50.2% in excluded group, P < 0.0001). BMI also differed significantly (P < 0.0001) between the two samples with the analytic sample having a higher percentage of normal and overweight participants (21.0% and 38.9% respectively) and lower percentage of obese participants (39.3%) compared with normal weight (15.7%), overweight (33.4%) and obese (50.1%) participants in the excluded sample. Age distribution was similar between the excluded and the included participants.
Mean age of participants in the analytic sample was 45 years, SD=14 and mean BMI was 29.4 kg/m2, SD=5.9. Overall, 56.5% were not employed (including retired); 35.4% had more than a high school education, 17.8% were US mainland born, 76.6% described their diet as mainly or mostly Hispanic/Latino foods and 33.8% ate out frequently (half or more of their calories) at least on one diet recall.
Variation of diet by demographics, depression symptoms, and eating out
Mean sleep duration was 8.0 (SE=0.02) hours in the analytic sample: 8.2% were short sleepers (≤ 6 hours), 71.7% were intermediate sleepers (> 6 and ≤ 9 hours) and 20.1% were long sleepers (> 9 hours). Table 1 shows the variation of dietary quality by socio-demographic characteristics. AHEI-2010 scores (per 1,000 kcal) were higher in older participants with the youngest group (18–29 yr) having the lowest score [18–29 yr: 22.41 (95% CI, 21.99, 22.82)] vs.[70–74 yr: 32.55 (95% CI, 31.09, 34.00)]. Participants who did not eat out frequently in either dietary recall had significantly lower usual saturated fat intake compared to those who ate out frequently in either recall. Additionally Dominicans had the highest AHEI-2010 scores per 1,000 kcal and higher AHEI-2010 scores per 1,000 kcal were associated with being female, having < high school education, being a homemaker, being obese and foreign-born (outside of US mainland) versus born in mainland US. The AHEI-2010 scores were slightly higher in participants with low income and higher among individuals who were retired. Intakes of potassium density (mg/1,000 kcal) also tracked patterns seen with AHEI-2010. Saturated fats density (proportion of total daily calories from saturated fats) was highest in Puerto Ricans, 30–39 yr olds, participants with > high school education, income ($40,0001–$75,000), US Born and eating mainly Hispanic foods. Caffeine intake (mg/1,000 kcal) was highest among Cubans, females, 50–59 yr olds, income >$75,000, retired and individuals in professional occupations as well as participants not living with a partner, obese individuals, individuals with no depressive symptomology, and who were foreign born and lived ≥ ten years in the U.S.
Variation of diet by sleep duration
There were no statistically significant differences in total energy, saturated fat intake, percentage of calories from carbohydrates or from protein by sleep duration (Table 2). Further, there were no differences in these aforementioned variables by sleep duration stratified by sex. Table 2 additionally illustrates differences in the quality of the diet by sleep duration. Short sleepers had a lower quality diet compared to intermediate sleepers with significantly lower intakes per 1,000 kcal of fiber, calcium, pectin, vegetables, nuts & legumes, dietary folacin, vitamins B6, B12, C and potassium and a higher sodium-to-potassium ratio. Long sleepers, on the other hand, differed from intermediate sleepers by having significantly lower intakes per 1,000 kcal of calcium, magnesium, fruits, vegetables, alpha-tocopherols, vitamin B6 and also higher sodium-to-potassium ratio. After adjusting for sex, education, years lived in mainland US, age, income, employment status, depressive symptomology and Hispanic/Latino background AHEI-2010 scores were not significantly different by sleep duration (Table 3). The differences in mean measures expressed as density (per 1,000 kcal) for potassium, calcium and fiber by sleep duration, however, persisted in adjusted analyses with short sleepers having lower intakes than intermediate sleepers. Caffeine intake was significantly lower in long sleepers [47.9 mg/1,000 kcal (95% CI: 45.2, 50.6)] after adjustment by full set of covariates, compared to other sleep duration groups. No significant differences were seen in alcohol or sugar intakes by sleep duration.
Table 2.
| Short Sleeper (≤6 hours) (n=1,059) |
Intermediate Sleeper (6–9 hours) (n=8,588) |
Long Sleeper (≥9 hours) (n=2,241) |
|
|---|---|---|---|
| Nutrient or Food group | Mean (95% CI)b | Mean (95% CI) b | Mean (95% CI) b |
| Calories (kcal) | 1983.3 (1945.5, 2021.2) | 1956.0 (1943.4, 1968.6) | 1937.3 (1916.2, 1958.5) |
| Protein density (% total energy) | 16.9 (16.7, 17.0) | 16.9 (16.9, 17.0) | 16.8 (16.8, 16.9) |
| Total fats density (% total energy) | 30.5 (30.3, 30.7) | 30.6 (30.6, 30.7) | 30.7 (30.5, 30.8) |
| Saturated fats density (% total energy) | 10.0 (9.9, 10.1) | 10.1 (10.1, 10.2) | 10.1 (10.0, 10.1) |
| Cholesterol (mg/1000 kcal) | 146.4 (144.3, 148.6) | 148.3 (147.4, 149.2) | 149.1 (147.5, 150.7) |
| Total carbohydrates density (% total energy) | 51.5 (51.2, 51.7) | 51.4 (51.3, 51.6) | 51.5 (51.3, 51.7) |
| AHEI-2010 (per 1,000 kcal) | 25.8 (25.2, 26.4) | 26.1 (25.9, 26.3) | 26.1 (25.8, 26.5) |
| Fiber (g per 1,000 kcal) | 8.95 (8.80, 9.11)*** | 9.25 (9.18, 9.31) | 9.18 (9.08, 9.28) |
| Calcium (mg per 1,000 kcal) | 408.8 (400.6, 416.9)** | 422.2 (419.5, 424.9) | 416.9 (412.1, 421.6)* |
| Phosphorus density (mg per 1,000 kcal) | 616.0 (599.6, 632.4) | 623.7 (619.2, 628.1) | 618.5 (610.2, 626.8) |
| Pectin (g per 1,000 kcal) | 1.18 (1.12, 1.23)* | 1.24 (1.22, 1.26) | 1.21 (1.18, 1.25) |
| Sucrose (g per 1,000 kcal) | 25.5 (23.9, 27.0) | 24.3 (23.9, 24.7) | 23.7 (23.1, 24.4) |
| Lycopene (micrograms per 1,000 kcal) | 2894.3 (2843.1, 2945.4) | 2947.9 (2929.9, 2965.9) | 2959.6 (2928.9, 2900.2) |
| Magnesium (mg per 1,000 kcal) | 146.1 (141.7, 150.6) | 148.5 (147.1, 149.9) | 144.3 (142.0, 146.7)** |
| Fruits (svg/day per 1,000 kcal) | 0.56 (0.53, 0.58) | 0.57 (0.56, 0.58) | 0.55 (0.53, 0.57)* |
| Vegetables (svg/day per 1,000 kcal) | 0.99 (0.96, 1.02)* | 1.03 (0.02, 1.04) | 1.01 (0.99, 1.02)* |
| Nuts and legumes (svg/day per 1,000 kcal) | 0.32 (0.30, 0.33)* | 0.33 (0.32, 0.33) | 0.33 (0.32, 0.34) |
| Dietary folacin (microgram / 1,000 kcal) | 265.7 (261.8, 269.7)*** | 274.4 (272.6, 276.2) | 273.1 (270.2, 276.0) |
| Alpha-tocopherols (mg/1,000 kcal) | 3.95 (3.70, 4.20) | 4.00 (3.93, 4.08) | 3.83 (3.73, 3.93)** |
| Vitamins B6 (mg/1,000 kcal) | 1.00 (0.99, 1.02)** | 1.03 (1.02, 1.03) | 1.01 (1.00, 1.02)* |
| Vitamin B12 density (micrograms/1,000 kcal) | 2.39 (2.33, 2.46)** | 2.50 (2.47, 2.52) | 2.50 (2.44, 2.55) |
| Vitamin C density (mg/1,000 kcal) | 48.2 (46.8, 49.7)* | 50.0 (49.5, 50.6) | 49.5 (48.7, 50.3) |
| Zinc density (mg/1,000 kcal) | 5.74 (5.54, 5.93) | 5.79 (5.73, 5.85) | 5.67 (5.56, 5.78) |
| Sodium density (mg per 1,000 kcal) | 1702.6 (1684.0, 1721.2) | 1699.7 (1692.5, 1707.0) | 1711.1 (1698.5, 1723.7) |
| Potassium density (mg per 1,000 kcal) | 1263.4 (1246.6, 1280.2)** | 1287.9 (1281.2, 1294.6) | 1279.0 (1281.2, 1294.6) |
| Sodium-to-potassium ratio | 1.39 (1.37, 1.41)* | 1.36 (1.35, 1.37) | 1.38 (1.37, 1.40)** |
| Caffeine (mg per 1,000 kcal) | 58.8 (54.02, 63.5) | 56.2 (54.4, 58.0) | 46.3 (43.6, 48.9)* |
| Alcohol (g per 1,000 kcal) | 0.13 (0.11, 0.15) | 0.12 (0.11, 0.13) | 0.12 (0.11, 0.14) |
All values account for complex survey design;
Adjusted for age, sex, and Hispanic/Latino background Bold values indicate the mean is statistically different compared to the reference group of intermediate sleepers at
for P < 0.05;
for P < 0.01;
for P < 0.001
Meals and snacks before bedtime & sleep duration
The sample was 8,752 after exclusions (see Figure 1). Overall 74.6% (95% CI, 73.1, 76.1) of participants and more participants who were foreign-born and <10 yrs in US 78.7%: (95% CI, 76.0, 81.2) ate near bed-time (data not shown). Overall 16.5% (95% CI, 15.4, 17.8) reported consuming ≥30% calories of total daily calories at the last meal or snack (Table 4). Cubans: 23.9% (95% CI, 21.0, 27.1), men: 19.7% (95% CI, 17.9,21.8), participants with lower levels of income ($10,000 – $20,000): 18.4% (95% CI, 16.0, 21.0) and foreign-born participants who had been in mainland US <10 yrs: 20.8% (95% CI, 18.5, 23.3) were significantly more likely to consume ≥30% calories of total daily calories near bedtime compared to other Hispanics/Latinos, women, other income categories and US or foreign-born participants who had resided ≥10 yr in the US.
Table 5 shows that significantly more long sleepers: 23.1% (95% CI, 20.1, 26.4) consumed ≥30% total daily calories near bedtime compared to other sleepers and that eating ≥ 30% total daily calories near bedtime was not associated with BMI. Table 6 shows statistically significant differences in consumption of the following nutrients when comparing individuals who consume a meal or snack within three hours of bedtime to individuals who do not consume a meal or snack during this period: higher calories: 1986 kcal (95% CI, 1974, 1998) vs. 1877 kcal (95% CI, 1856,1898), lower percentage of calories from protein: 16.9% (95% CI, 16.8,16.9) vs. 17.0 (95% CI, 16.9, 17.1), lower cholesterol intake: 146.3 mg/1,000 kcal (95% CI, 145.6, 147.1) vs. 151.8 mg/1,000 kcal (95% CI 150.4, 153.1), higher percentage of total calories from carbohydrates: 51.5% (95% CI 51.4, 51.6) vs. 51.3% (95% CI, 51.1,51.5) and lower AHEI-2010 score (per 1,000 calories): 25.5 (95% CI, 25.4, 25.7) vs. 27.1 (95% CI, 26.8, 27.5) and lower vegetable intake: 1.01 svg/day per 1,000 kcal (95% CI, 1.01, 1.02) vs. 1.05 svg/day per 1,000 kcal (95% CI 1.03, 1.06). By comparison Table 7 indicates that there are few differences in nutrient consumption between individuals who consume >30% of total daily calories near bedtime versus those who do not. These are in intakes of fiber: 9.07 g/1,000 kcal (95% CI, 8.96, 9.19) vs. 9.24 g/1,000 kcal (95% CI, 9.18, 9.30), and fruit: 0.54 svg/day per 1,000 kcal (95% CI, 0.52, 0.56) vs. 0.57 svg/day per 1,000 kcal (95% CI 0.56, 0.58).
Table 5.
Percent (95% CI) consuming ≥ 30% total daily kcal at last meal or snack before bedtime by sleep duration and BMI group a
| ≥30% of total daily kcal at last meal or snack near bedtimeb (n= 8,752) |
|||
|---|---|---|---|
| Characteristic | Subgroup N | % (95% CI) | Pc |
| Sleep duration | *** | ||
| Short | 787 | 9.9 (7.2, 13.3) | |
| Intermediate | 6,501 | 15.7 (14.4, 17.1) | |
| Long | 1,464 | 23.1 (20.1, 26.4) | |
| BMI | |||
| Underweight | 70 | 16.1 (6.2, 35.7) | |
| Normal weight | 1,810 | 17.8 (15.5, 20.4) | |
| Overweight | 3,506 | 16.3 (14.4, 18.3) | |
| Obese | 3,345 | 16.0 (14.3, 17.9) | |
All values except subgroup N account for complex survey design and incorporate sample weights.
Near bedtime is defined as being within 3 hours of bedtime with a buffer of one hr
P value obtained from Chi-square tests at
for P < 0.05;
for P < 0.01;
for P < 0.001.
Definitions: CI = confidence interval; sleep duration - short is ≤ 6 hours; intermediate is > 6 and ≤ 9 hours; long is > 9 hours; underweight is BMI < 18.5; normal weight is BMI ≥ 18.5 and < 25; overweight is BMI ≥ 25 and < 30; obese is BMI ≥ 30.
Table 6.
| Consuming a meal or snack near bedtime? | |||
|---|---|---|---|
| No N=2,082 |
Yes N=6,670 |
||
| Nutrient or food group | Adj. mean (95% CI)a | Adj. mean (95% CI)a | Pc |
| Total energy (g) | 1877 (1856, 1898) | 1986 (1974, 1998) | *** |
| Protein density (% total energy) | 17.0 (16.9, 17.1) | 16.9 (16.8, 16.9) | ** |
| Total fats density (% total energy) | 30.7 (30.6, 30.8) | 30.7 (30.6, 30.7) | |
| Cholesterol (mg/1000 kcal)` | 151.8 (150.4, 153.1) | 146.3 (145.6, 147.1) | *** |
| Total carbohydrates density (% total energy) | 51.3 (51.1, 51.5) | 51.5 (51.4, 51.6) | * |
| AHEI-2010 (per 1,000 kcal) | 27.1 (26.8, 27.5) | 25.5 (25.4, 25.7) | *** |
| Fiber (g per 1,000 kcal) | 9.17 (9.08, 9.27) | 9.22 (9.16, 9.29) | |
| Fruits (svg/day per 1,000 kcal) | 0.57 (0.55, 0.59) | 0.57 (0.56, 0.58) | |
| Vegetables (svg/day per 1,000 kcal) | 1.05 (1.03, 1.06) | 1.01 (1.01, 1.02) | ** |
| Nuts and legumes (svg/day per 1,000 kcal) | 0.33 (0.32, 0.34) | 0.33 (0.32, 0.33) | |
All values, except subgroup N, account for complex survey design.
Adjusted for age, sex and Hispanic/Latino background.
Near bedtime is defined as being within 3 hours of bedtime with a buffer of one hr
P value obtained from Chi-square tests at
for P < 0.05;
for P < 0.01;
for P < 0.001.
Definitions: CI = confidence interval
Table 7.
Adjusted mean nutrient intakea by eating a heavy (>30% of total energy) meal or snack near bedtimeb status
| Consuming a heavy (>30% of total energy) meal or snack near bedtime? | |||
|---|---|---|---|
| No N=7,350 |
Yes N= 1,402 |
||
| Nutrient or food group | Adj. mean (95% CI)a | Adj. mean (95% CI)a | Pc |
| Total energy (g) | 1959 (1948, 1970) | 1949 (1922, 1975) | |
| Protein density (% total energy) | 16.9 (16.9, 16.9) | 16.9 (16.8, 17.0) | |
| Total fats density (% total energy) | 30.7 (30.6, 30.7) | 30.8 (30.6, 30.9) | |
| Cholesterol (mg/1000 kcal)` | 147.6 (146.9, 148.4) | 148.6 (146.8, 150.3) | |
| Total carbohydrates density (% total energy) | 51.5 (51.4, 51.6) | 51.3 (51.1, 51.5) | |
| AHEI-2010 (per 1,000 kcal) | 26.0 (25.8, 26.2) | 25.9 (25.5, 26.3) | |
| Fiber (g per 1,000 kcal) | 9.24 (9.18, 9.30) | 9.07 (8.96, 9.19) | ** |
| Fruits (svg/day per 1,000 kcal) | 0.57 (0.56, 0.58) | 0.54 (0.52, 0.56) | ** |
| Vegetables (svg/day per 1,000 kcal) | 1.02 (1.02, 1.03) | 1.01 (0.99, 1.03) | |
| Nuts and legumes (svg/day per 1,000 kcal) | 0.33 (0.32, 0.33) | 0.33 (0.32, 0.34) | |
All values, except subgroup N, account for complex survey design.
Adjusted for age, sex and Hispanic/Latino background.
Near bedtime is defined as being within 3 hours of bedtime with a buffer of one hr
P value obtained from Chi-square tests at
for P < 0.05;
for P < 0.01;
for P < 0.001.
Definitions: CI = confidence interval
Lastly Table 8 shows that long sleepers consumed a significantly lower proportion of their daily calories during the morning compared to intermediate sleepers: 19.6% (95% CI, 18.6, 20.5) vs. 21.0% (95% CI, 20.5, 21.5). Overweight participants consumed a significantly higher mean proportion of daily calories in the morning compared to normal weight participants: 21.1% (95% CI, 20.4, 21.8) vs. 19.8% (95% CI, 19.0, 20.6). Obese participants consumed a significantly lower mean proportion of daily calories in the evening compared to normal weight participants: 27.0%, (95% CI: 26.1, 27.9) vs. 29.3% (CI, 28.1, 30.5)
DISCUSSION
We have studied for the first time the association between sleep patterns and diet quality in a large and diverse cohort of Hispanics/Latinos in the U.S. and have identified several novel associations regarding a) dietary quality and sleep duration; and b) meal or snack timing, bedtime and sleep duration.
Dietary quality and sleep duration
Short sleepers reported significantly lower intakes of calcium, fiber and potassium (per 1,000 kcal) compared to other sleepers, although differences were small. Of note, the overall mean potassium intake in the analytic sample of 2,454.2 mg/day (95% CI, 2,431.9, 2,476.5) is considerably lower than the USDA dietary recommendation of 4,700 mg/day. This nutrient is often overestimated via self-report possibly because of social desirability related to over-reporting of healthy foods such as fruits and vegetables, therefore the extent of deficiency of this nutrient may be even greater (Huang et al., 2014). While the intermediate sleepers have slightly higher intake of vegetables, vitamin B6 and lower sodium-to-potassium ratio compared to both the short and long sleepers, all groups had sub-optimal intake of vegetables with mean intake below two servings per day compared to USDA dietary recommendation of 2–3 servings per day. The low intake of dietary folacin, especially among short sleepers, is noteworthy indicating low intake of green leafy vegetables and other foods high in folate. This is particularly worrisome for individuals with the 677C-T polymorphism in the MTHFR gene that leads to lower serum folate levels (Yang et al., 2008). In sum, novel differences in alternative food selection patterns were identified and may inform nutrients worthy of studying in future research on sleep and diet.
A second novel finding was lower intake of caffeine in long sleepers. This conclusion supports a role for caffeine in modulating alertness and sleep behaviors, and possibly in setting circadian rhythms (Sherman et al., 2011). Contrary to prior studies (Kant & Graubard, 2014) no significant differences were seen in alcohol or sugars intake by sleep duration
Despite differences in nutrient intake, there were no differences in the AHEI-2010 scores by sleep duration when adjusted for covariates. Overall the AHEI-2010 scores were somewhat lower in this analytic sample (47.9 for male short and 46.0 for female long sleepers) compared with 52.4 for men in the Health Professionals Follow-Up Study and 47.6 for women in the Nurses’ Health Study (Chiuve et al., 2012). Likely the differences in scores reflect the different background of participants in the cohorts—both the Health Professionals Follow-Up Study and the Nurses’ Health Study are composed primarily of a highly educated and health conscious group of Euro-Americans that differ from the HCHS/SOL participants who are of diverse Hispanic/Latino and educational backgrounds. Additionally the AHEI-2010 scores from the Nurses’ Health Study were derived from food frequency questionnaires which assess longer term intakes (3 months to 1 yr) compared to 24 hr dietary recalls which assess intake in the past 24 hr which may explain the lower scores. The finding of no difference between the AHEI scores by sleep duration once adjusted by income, depressive symptomology, Hispanic/Latinos background, age, sex, education, years in mainland US and employment status may relate to the challenges in identifying the independent contributions of specific risk factors that are highly correlated with numerous covariates.
Meal or snack timing, bedtime & sleep duration
The finding that men, Cubans, participants with lower levels of income and those who have been in the mainland US < 10 years consumed higher calorie meals and snacks near bed-time is noteworthy and may indicate persistence of cultural dietary patterns related to eating late in the evening or that the evening meal or snack may be prioritized as a means of spending time together after a long work day (Sliwa, Must, Perea & Economus, 2015). Overall there is a paucity of data on patterns of meal and snack consumption among US Hispanics, particularly for recent immigrants such as the Cubans in this study who may be undergoing changes in eating behavior as they settle in the US. It is likely that certain cultural patterns such as eating near bed-time persist, while other aspects such as eating a large meal at mid-day change because of limitations relating to the workplace.
An important finding is that participants who did not consume a snack or meal three hours before bedtime had a lower energy intake, a slightly higher protein intake and higher AHEI-2010 scores. This finding could indicate that eating a healthy diet, for example one high in fruits/vegetables keeps appetites satiated so there is no need to eat right before bedtime.
More long sleepers also reported consuming ≥30% daily calories before bedtime compared to short sleepers. This high percentage may be related to the fact that long sleepers have an early bedtime and that the average bedtime is within 3 hours of typical meal time. High consumption of calories before bed-time has been noted in relation to longer duration of sleep in toddlers (Diethelm, Remer, Jilani, Kunz & Buyke, 2011). Additionally the distribution of calories consumed during the 24-hour period differed by sleep duration and BMI; however under-reporting of calories that vary by participant characteristics such as body size may have biased the results. For example the finding that overweight participants consumed a greater proportion of their meals and snacks in the morning and obese participants were less likely to have large meals and snacks at night compared to normal weight participants may reflect under-reporting of calories. A recent ancillary study of this cohort noted that higher body size was related to under-estimation of calories when self-reported energy was compared to the biomarker doubly labeled water (Mossavar-Rahmani et al., 2015).
Strengths and limitations
The study had several strengths. This is the most comprehensive study of diverse Hispanic/Latino backgrounds in the US to date with a wealth of data on diet, sleep and health outcomes. A novel finding is that recent immigrants compared to immigrants residing longer in the US and, men compared to women, were more likely to report a diet higher in calories before bedtime. These findings suggest possible targets for clinical intervention given that eating a high calorie meal or snack before bedtime is associated with sub-optimal health outcomes. As these are exploratory findings additional research is needed to validate differences in eating behavior in relation to sleep duration in this diverse sample of US Hispanics/Latinos. Objective measures such as actigraphy and polysomnography for sleep duration and doubly labeled water, a biomarker for energy intake, are needed to support these findings.
Despite the strengths, the study also had several limitations. Sleep data were based on self-report data which are prone to measurement error; for example short sleep durations may be viewed as socially undesirable to report, leading to biased responding. However in a sample of middle-aged adults in Chicago, subjective reports of habitual sleep were moderately correlated with actigraphy based measures of sleep (Lauderdale, Knutson, Yan, Liu & Rathouz, 2008). Additionally because sleep was self-reported and sleep latency- the time interval measured from “lights out,” or bedtime to the beginning of sleep- was not assessed, it is possible that sleep duration was overestimated (Mallon, Broman & Hetta, 2002; Qureshi, Giles, Croft & Bliwise, 1997). Also participants may not accurately recall the time that it takes to fall asleep or awakenings during the night. Future studies should incorporate sleep and wake-times in the 24 hr dietary recall in order to improve our understanding of sleep duration and diet.
Another limitation of the present study is the timing of the 24-hour dietary recall and sleep questionnaire. The 24-hour dietary recalls focused on foods eaten the previous day, whereas the sleep questionnaire was designed to query participants about usual sleep times. However we did use the NCI-adjusted method to estimate usual dietary intake from the 24 hr dietary recalls and the first diet recall and the sleep questionnaire were queried on the same day at baseline. Also past conceptual framework has focused primarily on the impact of sub-optimal sleep on unhealthy eating habits. Here the association between sleep and diet was investigated cross-sectionally thereby precluding assessment of direction of association or causality.
CONCLUSIONS
In summary caffeine, calcium, fiber and potassium intakes differed significantly by sleep duration, but not the AHEI-2010 score in this cohort of diverse Hispanics/Latinos in the US. The persistence of cultural patterns related to eating a greater proportion of daily calories before bedtime, especially among new immigrants, Cubans and men in particular, offer important avenues for dietary intervention.
This study identified novel differences in dietary patterns by sleep duration in a Hispanic/Latino population in the US.
Not consuming a snack or meal within three hours before bedtime was associated with higher AHEI-2010 scores and lower energy intake
Short sleepers (≤ 6 hr) had significantly lower intake of potassium, fiber and calcium
Long sleepers (≥9 hr) had significantly lower intake of caffeine compared to others sleepers
No difference in the AHEI-2010 score was seen by sleep duration
Acknowledgments
Sources of financial support:
This work was supported by grant -R01HL095856 and R01HL098297 from the National Heart, Lung, and Blood Institute (NHLBI). The Hispanic Community Health Study/Study of Latinos (HCHS/SOL) was carried out as a collaborative study supported by contracts from the NHLBI to the University of North Carolina (NO1-HC65233), University of Miami (N01-HC65234), Albert Einstein College of Medicine (N01-HC65235), Northwestern University (N01-HC65236), and San Diego State University (N01-HC65237).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The following Institutes/Center/Offices contribute to the HCHS/SOL through a transfer of funds to the NHLBI: the National Center on Minority Health and Health Disparities, the National Institute of Deafness and Other Communications Disorders, the National Institute of Dental and Craniofacial Research, the National Institute of Diabetes and Digestive and Kidney Diseases, the National Institute of Neurological Disorders and Stroke, and the Office of Dietary Supplements. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. The authors thank the HCHS/SOL investigators and staff for their valuable contributions. For a complete list of staff and investigators see: Sorlie P., et al. in Ann Epidemiol. 2010 Aug; 20: 642–649 and http://www.cscc.unc.edu/hchs/.
Conflicts of interest: none
ClinicalTrials.gov Identifier: NCT02060344
REFERENCES
- Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depresson Scale) American Journal of Preventive Medicine. 1994;10:77–84. [PubMed] [Google Scholar]
- Ayas NT, White DP, Manson JE, Stampfer MJ, Speizer FE, Malhotra A, Hu FB. A prospective study of sleep duration and coronary heart disease in women. Archives of Internal Medicine. 2003;163(2):205–209. doi: 10.1001/archinte.163.2.205. [DOI] [PubMed] [Google Scholar]
- Baron KG, Reid KJ, Kern AS, Zee PC. Role of sleep timing in caloric intake and BMI. Obesity (Silver Spring, MD) 2011;19(7):1374–1381. doi: 10.1038/oby.2011.100. [DOI] [PubMed] [Google Scholar]
- Baron KG, Reid KJ, Van Horn L, Zee PC. Contribution of evening macronutrient intake to total calorie intake and body mass index. Appetite. 2013;60(1):246–251. doi: 10.1016/j.appet.2012.09.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cespedes EM, Dudley KA, Sotres-Alvarez D, Zee PC, Daviglus ML, Shah MA, Talavera GA, Gallo LC, Matter J, Qi Q, Ramos AR, Schneiderman N, Espinoza Giacinto RA, Patel SR. Joint associations of insomnia and sleep duration with prevalent diabetes: The Hispanic Community Health Study/Study of Latinos (HCHS/SOL) Journal of Diabetes. 2015;7(4) doi: 10.1111/1753-0407.12308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiuve SE, Fung TT, Rimm EB, Hu FB, McCullough ML, Wang M, Stampfer MJ, Willett WC. Alternative dietary indices both strongly predict risk of chronic disease. Journal of Nutrition. 2012;142(6):1009–1018. doi: 10.3945/jn.111.157222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daviglus ML, Talavera GA, Aviles-Santa ML, Allison M, Cai J, Criqui MH, Gellman M, Giachello AL, Gouskova N, Kaplan RC, LaVange L, Penedo F, Perreira K, Pirzada A, Schneiderman N, Wassertheil-Smoller S, Sorlie PD, Stamler J. Prevalence of major cardiovascular risk factors and cardiovascular diseases among Hispanic/Latino individuals of diverse backgrounds in the United States. Journal of the American Medical Association. 2012;308(17):1775–1784. doi: 10.1001/jama.2012.14517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diethelm K, Remer T, Jilani H, Kunz C, Buyke AE. Associations between the macronutrient composition of the evening meal and average daily sleep duration in early childhood. Clinical Nutrition. 2011;30:640–646. doi: 10.1016/j.clnu.2011.05.004. [DOI] [PubMed] [Google Scholar]
- Gluck ME, Venti CA, Salbe AD, Votruba SB, Krakoff J. Higher 24-h respiratory quotient and higher spontaneous physical activity in nighttime eaters. Obesity(Silver Spring, MD) 2011;19(2):319–323. doi: 10.1038/oby.2010.206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grandner MA, Kripke DF, Naidoo N, Langer RD. Relationships among dietary nutrients and subjective sleep, objective sleep, and napping in women. Sleep Medicine. 2010;11(2):180–184. doi: 10.1016/j.sleep.2009.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grandner MA, Jackson N, Gerstner JR, Knutson KL. Sleep symptoms associated with intake of specific dietary nutrients. Journal of Sleep Research. 2014;23:22–34. doi: 10.1111/jsr.12084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grandner MA, Jackson N, Gertner JR, Knutson KL. Dietary nutrients associated with short and long sleep duration. Data from a nationally representative sample. Appetite. 2013;64:71–80. doi: 10.1016/j.appet.2013.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang Y, Van Horn L, Tinker LF, Neuhouser ML, Carbone L, Mossavar-Rahmani Y, Thomas F, Prentice RL. Measurement error corrected sodium and potassium intake estimation using 24-hour urinary excretion. Hypertension. 2014;63(2):238–244. doi: 10.1161/HYPERTENSIONAHA.113.02218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kant AK, Graubard BI. Association of self-reported sleep duration with eating behaviors of American adults: NHANES 2005–2010. American Journal of Clinical Nutrition. 2014;100(3):938–947. doi: 10.3945/ajcn.114.085191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaplan RC, Aviles-Santa ML, Parrinello CM, Hanna DB, Jung M, Castañeda SF, Hankinson AL, Isasi CR, Birnbaum-Weitzman O, Kim RS, Daviglus ML, Talavera GA, Schneiderman N, Cai J. Body mass index, sex, and cardiovascular disease risk factors among Hispanic/Latino adults: Hispanic community health study/study of Latinos. Journal of the American Heart Association. 2014;3(4):e000923. doi: 10.1161/JAHA.114.000923. pii. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knutson KL, Spiegel K, Penev P, Van Cauter E. The metabolic consequences of sleep deprivation. Sleep Medicine Reviews. 2007;11(3):163–178. doi: 10.1016/j.smrv.2007.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lauderdale DS, Knutson KL, Yan LL, Liu K, Rathouz PJ. Self-reported and measured sleep duration: how similar are they? Epidemiology (Cambridge, MA) 2008;19(6):838–845. doi: 10.1097/EDE.0b013e318187a7b0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lavange LM, Kalsbeek WD, Sorlie PD, Avilés-Santa LM, Kaplan RC, Barnhart J, Liu K, Giachello A, Lee DJ, Ryan J, Criqui MH, Elder JP. Sample design and cohort selection in the Hispanic Community Health Study/Study of Latinos. Annals of Epidemiology. 2010;20(8):642–649. doi: 10.1016/j.annepidem.2010.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y, Mirzaei F, O’Reilly EJ, Winkelman J, Malhotra A, Okereke OI, Ascherio A, Gao X. Prospective study of restless legs syndrome and risk of depression in women. American Journal of Epidemiology. 2012;176(4):279–288. doi: 10.1093/aje/kws016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lind BK, Goodwin JL, Hill JG, Ali T, Redline S, Quan SF. Recruitment of healthy adults into a study of overnight sleep monitoring in the home: experience of the Sleep Heart Health Study. Sleep & Breathing. 2003;7(1):13–24. doi: 10.1007/s11325-003-0013-z. [DOI] [PubMed] [Google Scholar]
- Lipovetzky N, Hod H, Roth A, Kishon Y, Sclarovsky S, Green MS. Heavy meals as a trigger for a first event of the acute coronary syndrome: a case-crossover study. Israel Medical Association Journal. 2004;6(12):728–731. [PubMed] [Google Scholar]
- Liu K, Daviglus ML, Loria CM, Colangelo LA, Spring B, Moller AC, Lloyd-Jones DM. Healthy lifestyle through young adulthood and the presence of low cardiovascular disease risk profile in middle age: the Coronary Artery Risk Development in (Young) Adults (CARDIA) study. Circulation. 2012;125(8):996–1004. doi: 10.1161/CIRCULATIONAHA.111.060681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mallon L, Broman JE, Hetta J. Sleep complaints predict coronary artery disease mortality in males: a 12-year follow-up study of a middle-aged Swedish population. Journal of Internal Medicine. 2002;251(3):207–216. doi: 10.1046/j.1365-2796.2002.00941.x. [DOI] [PubMed] [Google Scholar]
- Mossavar-Rahmani Y, Shaw PA, Wong WW, Sotres-Alvarez D, Gellman MD, Van Horn L, Stoutenberg M, Daviglus ML, Wylie-Rosett J, Siega-Riz AM, Ou F-S, Prentice RL. Applying recovery biomarkers to calibrate self-report measures of energy and protein in the Hispanic Community Health Study/Study of Latinos. American Journal of Epidemiology. 2015;181(12):996–1007. doi: 10.1093/aje/kwu468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nawrot TS, Perez L, Kunzli N, Munters E, Nemery B. Public health importance of triggers of myocardial infarction: a comparative risk assessment. Lancet. 2011;377(9767):732–740. doi: 10.1016/S0140-6736(10)62296-9. [DOI] [PubMed] [Google Scholar]
- Patel SR, Malhotra A, Gottlieb DJ, White DP, Hu FB. Correlates of long sleep duration. Sleep. 2006;29(7):881–889. doi: 10.1093/sleep/29.7.881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel SR, Hu FB. Short sleep duration and weight gain: a systematic review. Obesity (Silver Spring, MD) 2008;16(3):643–653. doi: 10.1038/oby.2007.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel SR, Sotres-Alvarez D, Castañeda SF, Dudley KA, Gallo LC, Hernandez R, Medeiros EA, Penedo FJ, Mossavar-Rahmani Y, Ramos AR, Redline S, Reid KJ, Zee PD. Social and Health Correlates of Sleep Duration in a US Hispanic Population: Results from the Hispanic Community Health Study/Study of Latinos. Sleep. 2015 Jun 11; doi: 10.5665/sleep.5036. epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qureshi AI, Giles WH, Croft JB, Bliwise DL. Habitual sleep patterns and risk for stroke and coronary heart disease: a 10-year follow-up from NHANES I. Neurology. 1997;48(4):904–911. doi: 10.1212/wnl.48.4.904. [DOI] [PubMed] [Google Scholar]
- Redline S, Sotres-Alvarez D, Loredo J, Hall M, Patel SR, Ramos A, Shah N, Ries A, Arens R, Barnhart J, Youngblood M, Zee P, Daviglus ML. Sleep-disordered breathing in Hispanic/Latino individuals of diverse backgrounds. The Hispanic Community Health Study/Study of Latinos. American Journal of Respiratory Critical Care Medicine. 2014;189(3):335–344. doi: 10.1164/rccm.201309-1735OC. 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneiderman N, Llabre M, Cowie CC, Barnhart J, Carnethon M, Gallo LC, Giachello AL, Heiss G, Kaplan RC, LaVange LM, Teng Y, Villa-Caballero L, Avilés-Santa ML. Prevalence of diabetes among Hispanics/Latinos from diverse backgrounds: the Hispanic Community Health Study/Study of Latinos (HCHS/SOL) Diabetes Care. 2014;37(8):2233–2239. doi: 10.2337/dc13-2939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherman H, Butman R, Capnik N, Meylan J, le Coutre J, Froy O. Caffeine alters circadian rhythms and expression of disease and metabolic markers. International Journal of Biochemistry & Cell Biology. 2011;43(5):829–38. doi: 10.1016/j.biocel.2011.02.008. [DOI] [PubMed] [Google Scholar]
- Shi Z, McEvoy M, Luu J, Attia J. Dietary fat and sleep duration in Chinese men and women. International Journal of Obesity. 2008;32(12):1835–1840. doi: 10.1038/ijo.2008.191. [DOI] [PubMed] [Google Scholar]
- Siega-Riz AM, Sotres-Alvarez D, Ayala GX, Ginsberg M, Himes JH, Liu K, Loria CM, Mossavar-Rahmani Y, Rock CL, Rodriguez B, Gellman MD, Van Horn L. Food-group and nutrient-density intakes by Hispanic and Latino backgrounds in the Hispanic Community Health Study/Study of Latinos. American Journal of Clinical Nutrition. 2014;99(6):1487–1498. doi: 10.3945/ajcn.113.082685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sliwa SA, Must A, Perea F, Economos CD. Maternal employment, acculturation, and time spent in food-related behaviors among Hispanic mothers in the United States. Evidence from the American Time Use Survey. Appetite. 2015;87:10–19. doi: 10.1016/j.appet.2014.10.015. [DOI] [PubMed] [Google Scholar]
- Sorlie PD, Aviles-Santa LM, Wassertheil-Smoller S, Kaplan RC, Daviglus ML, Giachello AL, Schneiderman N, Raij L, Talavera G, Allison M, Lavange L, Chambless LE, Heiss G. Design and implementation of the Hispanic Community Health Study/Study of Latinos. Annals of Epidemiology. 2010;20(8):629–641. doi: 10.1016/j.annepidem.2010.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spiegel K, Tasali E, Penev P, Van Cauter E. Brief communication: Sleep curtailment in healthy young men is associated with decreased leptin levels, elevated ghrelin levels, and increased hunger and appetite. Annals of Internal Medicine. 2004;141(11):846–850. doi: 10.7326/0003-4819-141-11-200412070-00008. [DOI] [PubMed] [Google Scholar]
- Stamatakis KA, Kaplan GA, Roberts RE. Short sleep duration across income, education, and race/ethnic groups: population prevalence and growing disparities during 34 years of follow-up. Annals of Epidemiology. 2007;17(12):948–955. doi: 10.1016/j.annepidem.2007.07.096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stern JH, Grant AS, Thomson CA, Tinker L, Hale L, Brennan KM, Woods NF, Chen Z. Short sleep duration is associated with decreased serum leptin, increased energy intake, and decreased diet quality in postmenopausal women. Obesity (Silver Spring, MD) 2014;22(5):E55–E61. doi: 10.1002/oby.20683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Subar AF, Thompson FE, Kipnis V, Midthune D, Hurwitz P, McNutt S, McIntosh A, Rosenfeld S. Comparative validation of the Block, Willett, and National Cancer Institute food frequency questionnaires : the Eating at America’s Table Study. American Journal of Epidemiology. 2001;154(12):1089–1099. doi: 10.1093/aje/154.12.1089. [DOI] [PubMed] [Google Scholar]
- Tooze JA, Kipnis V, Buckman DW, Carroll RJ, Freedman LS, Guenther PM, Krebs-Smith SM, Subar AF, Dodd KW. A mixed-effects model approach for estimating the distribution of usual intake of nutrients: the NCI method. Statistics in Medicine. 2010;29(27):2857–2868. doi: 10.1002/sim.4063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tooze JA, Midthune D, Dodd KW, Freedman LS, Krebs-Smith SM, Subar AF, Guenther PM, Carroll RJ, Kipnis V. A new statistical method for estimating the usual intake of episodically consumed foods with application to their distribution. Journal of the American Dietetic Association. 2006;106(10):1575–1587. doi: 10.1016/j.jada.2006.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss A, Xu F, Storfer-Isser A, Thomas A, Ievers-Landis CE, Redline S. The association of sleep duration with adolescents’ fat and carbohydrate consumption. Sleep. 2010;33(9):1201–1209. doi: 10.1093/sleep/33.9.1201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang QH, Botto LD, Gallagher M, Friedman JM, Sanders CL, Koontz D, Nikolova S, Erickson JD, Steinberg K. Prevalence and effects of gene-gene and gene-nutrient interactions on serum folate and serum total homocysteine concentrations in the United States: findings from the third National Health and Nutrition Examination Survey DNA Bank. American Journal of Clinical Nutrition. 2008;88(1):232–246. doi: 10.1093/ajcn/88.1.232. [DOI] [PubMed] [Google Scholar]