Abstract
Introduction
Area-level indicators of socio-economic variation are frequently included in models of individual health outcomes. Area disadvantage is linearly related to smoking prevalence, but its relation to cessation outcomes is less well understood.
Aims
To explore the relationship between area-level disadvantage and prospective data on smoking cessation.
Design and Methods
The Australian cohort of the International Tobacco Control 4-Country survey (N = 3503) was used to prospectively examine the contribution of area-level socio-economic disadvantage to predicting three important smoking-cessation outcomes: making a quit attempt, achieving 1 month abstinence, and achieving 6 months abstinence from smoking, while controlling for individual-level socio-economic indicators and other individual-level covariates related to smoking cessation.
Results
Only two independent associations were observed between socio-economic disadvantage and cessation outcomes. Area-level disadvantage was related to 1-month abstinence in a non-linear fashion, and the individual experience of smoking-induced deprivation was associated with a lower likelihood of making quit attempts.
Discussion
Despite the documented higher prevalence of smoking among the more disadvantaged and in more disadvantaged areas, socio-economic disadvantage was not consistently related to making quit attempts, nor to medium-term success. Nevertheless, indirect effects of disadvantage, like its impact on psychological distress, cannot be ruled out, and considering smokers’ individual psychosocial circumstances is likely to aid cessation efforts.
Conclusion
Socio-economic disadvantage, particularly at the area-level poses few direct barriers to smoking cessation.
Keywords: Smoking, Socio-economic status, area-based measures, Australia
Introduction
In developed nations, smoking and social disadvantage are becoming increasingly intertwined as the discrepancy in smoking rates between the most and least advantaged members of society gets wider [1; 2]. Rising cigarette prices increase the financial burden of marginalized groups who research has consistently shown find it harder to quit, translating to further health, psychological, and financial difficulties, and making smoking a potential contributor to social inequalities as well as a possible consequence [3].
Individual factors such as income, educational attainment, and ethnic minority status have all been linked to smoking [1; 4-6]. Increasingly though, the contribution of area-level differences is also being recognized. Neighbourhood disadvantage can be quantified by the relative percentage of, for example, government housing, unemployed residents, minority groups, and university graduates, from sources like national census surveys. A significant linear gradient of increasing smoking prevalence with increasing area disadvantage has been reported in many developed nations, often independent of individual factors [7-10].
Prevalence of smoking in Australia has been found to increase modestly but significantly with increasing neighbourhood disadvantage, over and above individual characteristics [11; 12]. Moreover, although overall mortality rates have declined in Australia over time, evidence suggests that the gap between areas of high and low disadvantage is widening, especially for mortality rates attributable to smoking-related causes like lung cancer and chronic lung disease [13; 14].
Areas of high disadvantage are perceived to pose fewer barriers to smoking (e.g. less social stigma, less well-enforced smoking bans) [15] and may even encourage it [16]. However, while higher smoking prevalence may go hand in hand with greater area-level disadvantage, the link between area disadvantage and smoking cessation outcomes is less clear. One Australian study observed higher prevalence rates but no differences in intentions to quit or in prior quitting activity with increasing area disadvantage [2]. In the UK too, area-level disadvantage did not predict quit success after individual factors had been considered [17]. The seemingly offhand inclusion of area-based measures in Australian health research has raised some concern [18] and their contribution to smoking cessation outcomes needs to be better understood so that resources may be directed toward the most appropriate interventions, be they at the area or individual level.
An important consideration is whether the possible effects of area-level factors are mediated through effects on other individual-level factors, or whether they have direct, unmediated effects. We know that a range of individual level factors predict successful smoking cessation or relapse over and above individual-level measures of disadvantage. These include motivations and intention to quit, level of nicotine dependence, the recency of the last quit attempt, the length of the longest prior quit attempt, and self-efficacy [19; 20]. Individual-level measures of disadvantage also predict cessation outcomes. Smoking-induced deprivation (spending money on cigarettes that would be better spent on household essentials like food and bills) has been found to be more prevalent among Australian smokers (33% versus 20% in the United Kingdom and 28% in the USA and Canada) and associated with making fewer quit attempts, though not with successful cessation [21]. Financial stress (inability to pay important bills like rent or electricity on time) has also been linked to greater interest in quitting, but a lower likelihood of successful cessation, independent of other important correlates of smoking cessation [22; 23].
The present aim is to investigate the degree to which area-level disadvantage is associated with smoking cessation outcomes in an Australian sample and the extent to which it adds predictive value over individual level measures of disadvantage and other known predictors of cessation.
Method
Participants
Participants were 3503 smokers aged 18 years or older from the Australian arm of the International Tobacco Control 4 Country cohort study (ITC4) [24]. Random-digit dialling was used to obtain a stratified sample, broadly representative of national demographic norms (response rates ≈42%), who were interviewed using computer-assisted telephone surveying. Participants in the ITC4 are followed-up regularly and were eligible for the present analysis if they had taken part in at least two consecutive surveys (typically conducted about 1 year apart, with 8 waves available at present, spanning from 2002 to 2011), and we could match them to area level disadvantage scores. While any individual may have participated in multiple waves, only data from their first two waves were considered.
Measures
Socio-Economic Indexes For Areas (SEIFA)
The Australian Bureau of Statistics calculated four area-level indexes from the 2006 national census and these were matched to the present sample using participants’ reported residential addresses. Each index is based on the percentage of households meeting specified criteria within a given area, with all areas in the country ranked from lowest to highest. The smallest area (matched for 2990 participants) was the census collection district (CD, around 220 dwellings). For 513 participants, we were only able to match data at the postal area level (POA, approximately 6 times larger than the CD). The indexes are derived using principle components analysis of the criterion variables, resulting in some overlap, however they are very different measures [see 24, pp. 6-16]. The Index of Relative Socio-economic disadvantage (IRSD: 17 criteria) considers many factors (income, education, occupation, housing, minority status) but focuses strictly on indicators of disadvantage. The Index of Relative Socio-economic Advantage and Disadvantage (IRSAD: 21 criteria) is similarly broad but also includes indicators of advantage. The Index of Economic Resources (IER: 15 criteria) focuses only on material wealth, and the Index of Education and Occupation (IEO: 9 criteria) focuses only on skills and qualifications. Indexes are provided as standardized scores (M = 1000, SD = 100) and deciles, which we also further coded into quintiles. All indexes were coded so that higher scores indicated relatively greater disadvantage. Extensive technical documents detailing the SEIFA indexes are available [24].
Individual-level socio-economic indicators
The individual level measures we had that were analogous to the variables used to derive at least one of the SEIFA indexes were main language spoken at home (English or not); marital status; highest level of education attained (completed high-school or less; completed community/ trade/ technical school, or some university but no degree; completed university degree or higher); and equivalized annual household income, which takes into consideration the number of adults and children in the household using the “Organisation for Economic Co-operation and Development (OECD)-modified scale” [25]. Income was stratified into quintiles with those who did not report their income coded as a separate, valid category.
In addition, we also examined smoking-induced deprivation (“In the last 6 months, have you spent money on cigarettes that you knew would be better spent on household essentials like food?”), which was only assessed in waves 1 to 5 of the ITC4. Separate analyses were conducted using the valid subgroup (n = 3040) to examine its contribution to the outcome measures.
Smoking-related covariates
Variables related to smoking behaviour were the Heaviness of Smoking Index (HSI) combining reported cigarettes smoked per day with minutes to the first cigarette [26]; length of the longest lifetime quit attempt (none, under 1 month, 1 month – under 6 months, or 6 months or more); whether a quit attempt of any length had been made in the past year; and baseline smoking frequency (daily versus weekly/ monthly).
Cognitive and attitudinal measures included participants’ intention to quit (none, beyond 6 months, within 6 months, or within 1 month); overall opinion of smoking (positive/ neutral, negative, or very negative); perceived self-efficacy to succeed at quitting (1 = not at all to 5 = extremely sure); the degree to which they expected health and other benefits from quitting (1 = not at all to 5 = extremely); how worried they were about the health consequences of smoking (the average of two items: that smoking would damage their health, or lower their quality of life, each coded on 4-point scales from 1 = not at all to 4 = extremely worried); and the degree to which they held favourable attitudes toward smoking (the average of two items: smoking is an important part of life, and too good to give up for good, each coded on 5-point scales from 1 = strongly agree to 5 = strongly disagree). (see also [19]).
Other control variables
We included age group, sex, and, to account for varying inter-survey intervals, the time (in months) elapsed between participants’ baseline and follow-up surveys, which ranged from 5.8 to 20.5 months (M = 9.1, SD = 3.1).
Outcome measures
Three binary outcome measures were assessed: (1) whether or not participants had made a quit attempt of any length between their baseline and follow-up waves; and among those who had made a quit attempt whether or not they had stayed quit for (2) at least 1 month or (3) at least 6 months since their baseline wave, irrespective of whether they were still quit at follow-up (N.B. some of those meeting these criteria may have made other less successful attempts as well).
Analyses
We employed a cumulative strategy of a sequence of logistic regressions for each outcome separately, and for each SEIFA measure. We first tested the univariate associations. Next, we added all the individual-level socio-economic indicators, plus age and sex, (Model 2). Finally, we added the individual-level smoking-related covariates, and elapsed time since last being surveyed (Model 3). A forced-entry procedure was used with each model to ensure the inclusion of all predictor variables, to enable a better comparison of their relative contribution to the outcome measures.
For all reported analyses we combined SEIFA indexes for the group who had CD-level data with those who only had POA-level data to ensure the maximum degree of accuracy for each individual. In these analyses we did not control for area-level clustering, which was minimal. In addition, we ran more conservative analyses using POA-level data for all participants, adjusting the standard error of regression coefficients for area-level clustering. Those few that made a small difference are reported in the footnotes to Table 4 and Table 5.
Table 4.
Predictors of having quit for at least 1 month since last being surveyed, among those with quit attempts
| SEIFA Univariate |
Model 2 |
Model 3 |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| N | OR | 95% CI | N | OR | 95% CI | N | OR | 95% CI | |
| Total N | 1359 | 1310 | 1240 | ||||||
| Index of Relative Socio-Economic Disadvantage (IRSD) | |||||||||
| Lowest disadvantage | 198 | Ref | (p < .001) | 192 | Ref | (p < .001) | 183 | Ref | (p < .01) |
| Low disadvantage | 262 | 0.5** | 0.4 – 0.8 | 258 | 0.6** | 0.4 – 0.8 | 246 | 0.6* | 0.4 – 0.9 |
| Moderate disadvantage | 271 | 0.9 | 0.6 – 1.2 | 257 | 0.9 | 0.6 – 1.4 | 241 | 1.0 | 0.7 – 1.6 |
| High disadvantage | 300 | 0.5*** | 0.3 – 0.7 | 292 | 0.5** | 0.3 – 0.7 | 275 | 0.5** | 0.4 – 0.8 |
| Highest disadvantage | 328 | 0.7* | 0.5 – 0.9 | 311 | 0.7 | 0.5 – 1.1 | 295 | 0.8 | 0.5 – 1.2 |
| Main language spoken at home | |||||||||
| English | 1163 | Ref | (p = .763) | 1107 | Ref | (p = .836) | |||
| Not English | 147 | 0.9 | 0.7 – 1.4 | 133 | 1.0 | 0.7 – 1.6 | |||
| Equivalized household incomea | |||||||||
| Low | 272 | Ref | (p = .051) | 257 | Ref | (p = .253) | |||
| Low-moderate | 211 | 1.3 | 0.9 – 1.8 | 193 | 1.2 | 0.8 – 1.8 | |||
| Moderate | 234 | 1.4 | 0.96 – 2.0 | 223 | 1.4 | 0.9 – 2.1 | |||
| High-moderate | 250 | 1.3 | 0.9 – 1.9 | 238 | 1.1 | 0.7 – 1.6 | |||
| High | 265 | 1.9** | 1.3 – 2.7 | 258 | 1.5* | 1.02 – 2.3 | |||
| Not disclosed | 78 | 1.2 | 0.7 – 2.0 | 71 | 1.0 | 0.6 – 1.9 | |||
| Education | |||||||||
| Low | 813 | Ref | (p = .286) | 763 | Ref | (p = .722) | |||
| Moderate | 295 | 1.2 | 0.9 – 1.6 | 282 | 1.0 | 0.8 – 1.4 | |||
| High | 202 | 1.2 | 0.8 – 1.7 | 195 | 0.9 | 0.6 – 1.3 | |||
| Marital Status | |||||||||
| Married | 465 | Ref | (p = .407) | 445 | Ref | (p = .389) | |||
| Separated/ divorced/ widowed | 282 | 0.8 | 0.6 – 1.2 | 266 | 0.9 | 0.6 – 1.2 | |||
| DeFacto | 205 | 0.9 | 0.6 – 1.3 | 196 | 0.9 | 0.6 – 1.3 | |||
| Single | 358 | 0.8 | 0.6 – 1.1 | 333 | 0.7 | 0.5 – 1.05 | |||
| Age group (years) | |||||||||
| 18 – 24 | 200 | Ref | (p < .05) | 191 | Ref | (p < .05) | |||
| 25 – 39 | 468 | 0.7* | 0.5 – 0.95 | 448 | 0.7 | 0.4 – 1.003 | |||
| 40 – 54 | 419 | 0.6** | 0.4 – 0.8 | 400 | 0.5** | 0.3 – 0.8 | |||
| 55 and older | 223 | 0.6* | 0.4 – 0.9 | 201 | 0.6* | 0.3 – 0.96 | |||
| Sex | |||||||||
| Female | 731 | Ref | (p = .555) | 688 | Ref | (p = .204) | |||
| Male | 579 | 1.1 | 0.8 – 1.4 | 552 | 1.2 | 0.9 – 1.5 | |||
| Heaviness of Smoking Index | |||||||||
| 0 | 228 | Ref | (p = .105) | ||||||
| 1 to 2 | 374 | 0.7 | 0.5 – 1.02 | ||||||
| 3 to 4 | 492 | 0.6* | 0.4 – 0.9 | ||||||
| 5 to 6b | 146 | 0.6* | 0.3 – 0.99 | ||||||
| Longest prior quit attempt | |||||||||
| None | 119 | Ref | (p < .001) | ||||||
| Under 1 month | 311 | 0.4** | 0.2 – 0.7 | ||||||
| 1 month – under 6 months | 300 | 1.1 | 0.6 – 1.7 | ||||||
| 6 months or longer | 510 | 1.2 | 0.7 – 1.9 | ||||||
| Quit attempts in the last year? | |||||||||
| Yes | 741 | Ref | (p = .316) | ||||||
| No | 499 | 0.9 | 0.6 – 1.2 | ||||||
| Baseline smoking frequency | |||||||||
| Daily | 1080 | Ref | (p < .01) | ||||||
| Weekly or monthly | 160 | 1.8** | 1.2 – 2.7 | ||||||
| Intention to quit | |||||||||
| None | 127 | Ref | (p = .658) | ||||||
| Beyond 6 months | 405 | 1.1 | 0.7 – 1.7 | ||||||
| Within 6 months | 420 | 1.2 | 0.8 – 2.0 | ||||||
| Within 1 month | 288 | 1.0 | 0.6 – 1.7 | ||||||
| Overall opinion of smoking | |||||||||
| Positive or neutral | 428 | Ref | (p = .683) | ||||||
| Negative | 515 | 1.0 | 0.8 – 1.4 | ||||||
| Very negative | 297 | 1.2 | 0.8 – 1.7 | ||||||
| Self-efficacy to quit | 1240 | 1.1* | 1.02 – 1.3 | ||||||
| Expected benefits of quitting | 1240 | 0.8** | 0.7 – 0.9 | ||||||
| Worries about health effects | 1240 | 1.0 | 0.9 – 1.2 | ||||||
| Favourable attitudes to smoking | 1240 | 1.1 | 0.9 – 1.2 | ||||||
| Time (months) since baseline | 1240 | 1.13*** | 1.09 – 1.18 | ||||||
| Likelihood ratio: | χ2(2) = 93.7, p < .001 | χ2(2) = 234.5, p < .001 | |||||||
Note: Overall significance levels for each categorical variable are provided in brackets next to the reference category.
In the postal-area (POA)-level analyses controlling for clustering, the overall effects of this variable were significant (p < .05) in the Model 2 analysis
In the POA-level analyses controlling for clustering, this category did not reach statistical significance relative to the reference in the Model 3 analysis.
p < .05
p < .01
p < .001.
Table 5.
Predictors of having quit for at least 6 months since last being surveyed, among those with quit attempts.
| SEIFA Univariate |
Model 2 |
Model 3 |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| N | OR | 95% CI | N | OR | 95% CI | N | OR | 95% CI | |
| Total N | 1332 | 1283 | 1217 | ||||||
| Index of Relative Socio-Economic Disadvantage (IRSD) | |||||||||
| Lowest disadvantage | 195 | Ref | (p = .057) | 189 | Ref | (p = .243) | 181 | Ref | (p = .387) |
| Low disadvantage | 259 | 0.6 | 0.3 – 1.1 | 255 | 0.7 | 0.4 – 1.3 | 243 | 0.7 | 0.3 – 1.3 |
| Moderate disadvantage | 268 | 0.7 | 0.4 – 1.3 | 254 | 0.9 | 0.5 – 1.6 | 239 | 0.9 | 0.5 – 1.8 |
| High disadvantage | 292 | 0.4** | 0.2 – 0.8 | 284 | 0.5 | 0.3 – 1.02 | 268 | 0.6 | 0.3 – 1.2 |
| Highest disadvantage | 318 | 0.8 | 0.4 – 1.3 | 301 | 0.9 | 0.5 – 1.8 | 286 | 1.1 | 0.6 – 2.1 |
| Main language spoken at home | |||||||||
| English | 1142 | Ref | (p = .875) | 1089 | Ref | (p = .500) | |||
| Not English | 141 | 1.0 | 0.6 – 1.9 | 128 | 1.2 | 0.7 – 2.4 | |||
| Equivalized household income | |||||||||
| Low | 267 | Ref | (p = .061) | 254 | Ref | (p = .160) | |||
| Low-moderatea | 204 | 2.1 | 1.0 – 4.1 | 187 | 1.9 | 0.9 – 4.0 | |||
| Moderate | 227 | 1.0 | 0.5 – 2.2 | 216 | 0.8 | 0.4 – 1.9 | |||
| High-moderate | 249 | 1.8 | 0.9 – 3.5 | 238 | 1.4 | 0.7 – 2.8 | |||
| High | 258 | 2.0* | 1.01 – 3.9 | 251 | 1.5 | 0.7 – 3.2 | |||
| Not disclosed | 78 | 2.7* | 1.2 – 6.2 | 71 | 2.3 | 0.9 – 5.7 | |||
| Education | |||||||||
| Low | 792 | Ref | (p = .072) | 745 | Ref | (p = .566) | |||
| Moderate | 290 | 1.5 | 0.9 – 2.3 | 278 | 1.3 | 0.8 – 2.1 | |||
| High | 201 | 1.7* | 1.03 – 2.9 | 194 | 1.3 | 0.7 – 2.3 | |||
| Marital Status | |||||||||
| Married | 458 | Ref | (p = .115) | 438 | Ref | (p = .120) | |||
| Separated/ divorced/ widowed | 276 | 0.6 | 0.3 – 1.04 | 262 | 0.6 | 0.3 – 1.1 | |||
| DeFacto | 200 | 1.1 | 0.6 – 1.9 | 192 | 1.2 | 0.7 – 2.1 | |||
| Single | 349 | 0.7 | 0.4 – 1.1 | 325 | 0.7 | 0.4 – 1.3 | |||
| Age group (years) | |||||||||
| 18 – 24 | 194 | Ref | (p = .204) | 186 | Ref | (p = .148) | |||
| 25 – 39 | 461 | 0.7 | 0.4 – 1.3 | 442 | 0.8 | 0.4 – 1.5 | |||
| 40 – 54b | 411 | 0.5* | 0.3 – 0.97 | 393 | 0.5* | 0.2 – 0.98 | |||
| 55 and older | 217 | 0.6 | 0.3 – 1.3 | 196 | 0.6 | 0.3 – 1.6 | |||
| Sex | |||||||||
| Female | 720 | Ref | (p = .836) | 679 | Ref | (p = .526) | |||
| Male | 563 | 1.0 | 0.7 – 1.4 | 538 | 1.1 | 0.7 – 1.8 | |||
| Heaviness of Smoking Index | |||||||||
| 0 | 226 | Ref | (p = .194) | ||||||
| 1 to 2 | 369 | 0.7 | 0.4 – 1.2 | ||||||
| 3 to 4 | 479 | 0.5* | 0.3 – 0.9 | ||||||
| 5 to 6 | 143 | 0.5 | 0.2 – 1.3 | ||||||
| Longest prior quit attempt | |||||||||
| None | 117 | Ref | (p < .05) | ||||||
| Under 1 month | 304 | 0.8 | 0.3 – 2.1 | ||||||
| 1 month – under 6 months | 290 | 1.5 | 0.6 – 3.7 | ||||||
| 6 months or longer | 506 | 1.9 | 0.9 – 4.3 | ||||||
| Quit attempts in the last year? | |||||||||
| Yes | 726 | Ref | (p = .998) | ||||||
| No | 491 | 1.0 | 0.6 – 1.6 | ||||||
| Baseline smoking frequency | |||||||||
| Daily | 1062 | Ref | (p = .541) | ||||||
| Weekly or monthly | 155 | 1.2 | 0.7 – 2.2 | ||||||
| Intention to quit | |||||||||
| None | 126 | Ref | (p = .876) | ||||||
| Beyond 6 months | 398 | 0.8 | 0.4 – 1.7 | ||||||
| Within 6 months | 412 | 0.8 | 0.4 – 1.7 | ||||||
| Within 1 month | 281 | 0.7 | 0.3 – 1.6 | ||||||
| Overall opinion of smoking | |||||||||
| Positive or neutral | 422 | Ref | (p = .080) | ||||||
| Negative | 501 | 1.8* | 1.1 – 3.0 | ||||||
| Very negative | 294 | 1.8 | 0.9 – 3.3 | ||||||
| Self-efficacy to quit | 1217 | 1.2 | 0.999 – 1.4 | ||||||
| Expected benefits of quitting | 1217 | 0.9 | 0.8 – 1.2 | ||||||
| Worries about health effects | 1217 | 1.0 | 0.7 – 1.3 | ||||||
| Favourable attitudes to smoking | 1217 | 1.0 | 0.8 – 1.3 | ||||||
| Time (months) since baseline | 1.2*** | 1.1 – 1.3 | |||||||
| Likeihood ratio: | χ2(2) = 83.0, p < .001 | χ2(2) = 114.2, p < .001 | |||||||
Note: Overall significance levels for each categorical variable are provided in brackets next to the reference category.
In the postal-area (POA)-level analyses controlling for clustering, this category was significantly different from the reference (p < .05) in the Model 2 analysis.
In the POA-level analyses controlling for clustering, this category was no longer significantly different from the reference category in the Model 3 analysis.
p < .05
p < .01
p < .001.
Results
Participants’ socio-demographic characteristics are detailed in Table 1, and as expected from the known distributions [27], the proportion of smokers increased with increasing area disadvantage. The four SEIFA indexes were highly correlated (see Table 2), and there were few significant associations between the indexes and our outcome variables. The analyses using quintiles were generally most interpretable and the Index of Relative Socio-economic Disadvantage (IRSD) was generally most strongly associated with the outcomes, so these sets of analyses are reported in the Tables 3-5. Of note, the continuous measures showed no effect, and as will be seen the quintile measures showed significant non-linearity.
Table 1.
Socio-demographic characteristics among all participants (N = 3503) and only those who made quit attempts (n = 1379).
| All participants |
Only quit attempters |
|||
|---|---|---|---|---|
| Percent | 95% CI | Percent | 95% CI | |
| Index of Relative Socio-Economic Disadvantage (IRSD) | ||||
| Lowest disadvantage | 14.6 | 13.4 – 15.8 | 14.7 | 12.9 – 16.6 |
| Low disadvantage | 18.6 | 17.3 – 19.9 | 19.4 | 17.3 – 21.4 |
| Moderate disadvantage | 19.9 | 18.5 – 21.2 | 20.0 | 17.9 – 22.1 |
| High disadvantage | 22.0 | 20.6 – 23.4 | 22.0 | 19.9 – 24.2 |
| Highest disadvantage | 25.0 | 23.5 – 26.4 | 23.9 | 21.6 – 26.1 |
| Main language spoken at home | ||||
| English | 88.1 | 87.0 – 89.2 | 88.8 | 87.2 – 90.5 |
| Not English | 11.8 | 10.7 – 12.9 | 11.1 | 9.4 – 12.8 |
| Equivalized household income | ||||
| Low | 20.6 | 19.3 – 22.0 | 20.6 | 18.5 – 22.7 |
| Low-moderate | 17.2 | 16.0 – 18.5 | 16.0 | 14.1 – 18.0 |
| Moderate | 19.1 | 17.8 – 20.4 | 18.4 | 16.4 – 20.5 |
| High-moderate | 18.8 | 17.5 – 20.1 | 19.2 | 17.1 – 21.3 |
| High | 18.1 | 16.8 – 19.3 | 19.9 | 17.8 – 22.0 |
| Not disclosed | 6.2 | 5.4 – 7.0 | 5.9 | 4.6 – 7.1 |
| Education | ||||
| Low | 64.5 | 62.9 – 66.1 | 61.9 | 59.4 – 64.5 |
| Moderate | 21.7 | 20.3 – 23.1 | 22.6 | 20.4 – 24.8 |
| High | 13.7 | 12.5 – 14.8 | 15.2 | 13.3 – 17.1 |
| Marital Status | ||||
| Married | 38.1 | 36.4 – 39.7 | 34.5 | 32.0 – 37.0 |
| Separated/ divorced/ widowed | 21.2 | 19.9 – 22.6 | 21.0 | 18.8 – 23.1 |
| DeFacto | 13.3 | 12.2 – 14.4 | 14.9 | 13.1 – 16.8 |
| Single | 25.2 | 23.8 – 26.6 | 26.3 | 23.9 – 28.6 |
| Smoking-induced deprivationa | ||||
| No | 57.4 (65.9) | 55.7 – 59.0 | 50.9 (60.2) | 48.3 – 53.5 |
| Yes | 29.7 (34.1) | 28.2 – 31.2 | 33.6 (39.8) | 31.2 – 36.1 |
| Missing | 12.9 | 11.8 – 14.0 | 15.4 | 13.5 – 17.4 |
| Age group (years) | ||||
| 18 – 24 | 12.0 | 10.9 – 13.1 | 15.0 | 13.1 – 16.9 |
| 25 – 39 | 33.4 | 31.8 – 35.0 | 35.2 | 32.7 – 37.7 |
| 40 – 54 | 37.0 | 35.4 – 38.6 | 32.6 | 30.1 – 35.0 |
| 55 and older | 17.6 | 16.4 – 18.9 | 17.3 | 15.3 – 19.3 |
| Sex | ||||
| Female | 54.8 | 53.2 – 56.5 | 55.6 | 53.0 – 58.2 |
| Male | 45.2 | 43.5 – 46.8 | 44.4 | 41.8 – 47.0 |
Note: Data was missing for < 5% of the total sample on the following variables: Main language spoken at home (0.1%); Education (0.1%); and Marital status (2.2%).
Figures in brackets refer to percentages within the non-missing sample only.
Table 2.
Correlations between the continuous standardized Socio-Economic Indexes for Areas (N = 3505).
| 1. | 2. | 3. | 4. | |
|---|---|---|---|---|
| 1. Relative Socio-economic Disadvantage (IRSD) | 1.0 | |||
| 2. Relative Socio-economic Advantage-Disadvantage (IRASD) | .939 | 1.0 | ||
| 3. Economic Resources (IER) | .936 | 870 | 1.0 | |
| 4. Education and Occupation (IEO) | .775 | .907 | .628 | 1.0 |
Note: All indexes are coded in the same direction, with higher values indicating greater relative disadvantage.
Association are Pearson's correlation coefficients, r, all significant at p < .001 (two-tailed).
Table 3.
Predictors of making a quit attempt since last being surveyed.
| SEIFA Univariate |
Model 2 |
Model 3 |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| N | OR | 95% CI | N | OR | 95% CI | N | OR | 95% CI | |
| Total N | 3503 | 3419 | 3237 | ||||||
| Index of Relative Socio-Economic Disadvantage (IRSD) | |||||||||
| Lowest disadvantage | 511 | Ref | (p = .937) | 501 | Ref | (p = .775) | 478 | Ref | (p = .665) |
| Low disadvantage | 651 | 1.1 | 0.8 – 1.3 | 642 | 1.1 | 0.9 – 1.4 | 608 | 1.2 | 0.9 – 1.6 |
| Moderate disadvantage | 696 | 1.0 | 0.8 – 1.3 | 675 | 1.1 | 0.8 – 1.4 | 639 | 1.1 | 0.9 – 1.5 |
| High disadvantage | 770 | 1.0 | 0.8 – 1.2 | 753 | 1.1 | 0.6 – 1.4 | 718 | 1.2 | 0.9 – 1.5 |
| Highest disadvantage | 875 | 0.9 | 0.7 – 1.1 | 848 | 1.0 | 0.8 – 1.3 | 794 | 1.2 | 0.9 – 1.6 |
| Main language spoken at home | |||||||||
| English | 3012 | Ref | (p = .241) | 2871 | Ref | (p = .470) | |||
| Not English | 407 | 0.9 | 0.7 – 1.1 | 366 | 0.9 | 0.7 – 1.2 | |||
| Equivalized household income | |||||||||
| Low | 704 | Ref | (p = .289) | 663 | Ref | (p = .421) | |||
| Low-moderate | 585 | 0.9 | 0.7 – 1.1 | 551 | 0.9 | 0.7 – 1.1 | |||
| Moderate | 648 | 0.9 | 0.7 – 1.1 | 616 | 0.9 | 0.7 – 1.2 | |||
| High-moderate | 644 | 1.0 | 0.8 – 1.3 | 611 | 1.0 | 0.8 – 1.3 | |||
| High | 623 | 1.1 | 0.9 – 1.4 | 603 | 1.1 | 0.8 – 1.4 | |||
| Not disclosed | 213 | 0.9 | 0.7 – 1.3 | 193 | 1.2 | 0.9 – 1.8 | |||
| Education | |||||||||
| Low | 2206 | Ref | (p < .05) | 2075 | Ref | (p = .755) | |||
| Moderate | 741 | 1.1 | 0.9 – 1.3 | 712 | 1.1 | 0.9 – 1.3 | |||
| High | 472 | 1.3* | 1.1 – 1.6 | 450 | 1.1 | 0.9 – 1.4 | |||
| Marital Status | |||||||||
| Married | 1331 | Ref | (p = .145) | 1267 | Ref | (p = .294) | |||
| Separated/ divorced/ widowed | 740 | 1.2 | 0.97 – 1.4 | 700 | 1.2 | 0.96 – 1.5 | |||
| DeFacto | 465 | 1.2 | 0.98 – 1.5 | 444 | 1.2 | 0.9 – 1.6 | |||
| Single | 883 | 1.0 | 0.8 – 1.3 | 826 | 1.1 | 0.9 – 1.4 | |||
| Age group (years) | |||||||||
| 18 – 24 | 416 | Ref | (p < .001) | 399 | Ref | (p < .05) | |||
| 25 – 39 | 1149 | 0.7** | 0.6 – 0.9 | 1099 | 0.8 | 0.6 – 1.07 | |||
| 40 – 54 | 1256 | 0.5*** | 0.4 – 0.7 | 1191 | 0.7* | 0.5 – 0.9 | |||
| 55 and older | 598 | 0.6** | 0.5 – 0.8 | 548 | 0.9 | 0.7 – 1.3 | |||
| Sex | |||||||||
| Female | 1870 | Ref | (p = .320) | 1770 | Ref | (p = .949) | |||
| Male | 1549 | 0.9 | 0.8 – 1.1 | 146 | 1.0 | 0.8 – 1.2 | |||
| Heaviness of Smoking Index | |||||||||
| 0 | 482 | Ref | (p = .079) | ||||||
| 1 to 2 | 861 | 1.0 | 0.8 – 1.3 | ||||||
| 3 to 4 | 1418 | 0.8 | 0.6 – 1.1 | ||||||
| 5 to 6 | 476 | 0.8 | 0.5 – 1.1 | ||||||
| Longest prior quit attempt | |||||||||
| None | 529 | Ref | (p = .110) | ||||||
| Under 1 month | 833 | 1.1 | 0.8 – 1.5 | ||||||
| 1 month – under 6 months | 698 | 1.3 | 0.9 – 1.7 | ||||||
| 6 months or longer | 1177 | 1.3* | 1.02 – 1.8 | ||||||
| Quit attempts in the last year? | |||||||||
| Yes | 1394 | Ref | (p < .001) | ||||||
| No | 1843 | 0.5*** | 0.4 – 0.6 | ||||||
| Baseline smoking frequency | |||||||||
| Daily | 2947 | Ref | (p < .001) | ||||||
| Weekly or monthly | 290 | 1.7** | 1.3 – 2.4 | ||||||
| Intention to quit | |||||||||
| None | 799 | Ref | (p < .001) | ||||||
| Beyond 6 months | 1258 | 1.7*** | 1.3 – 2.1 | ||||||
| Within 6 months | 784 | 3.2*** | 2.4 – 4.1 | ||||||
| Within 1 month | 416 | 5.7*** | 4.2 – 7.9 | ||||||
| Overall opinion of smoking | |||||||||
| Positive or neutral | 1411 | Ref | (p = .401) | ||||||
| Negative | 1207 | 1.1 | 0.9 – 1.4 | ||||||
| Very negative | 619 | 1.1 | 0.9 – 1.4 | ||||||
| Self-efficacy to quit | 3237 | 1.1 | 0.99 – 1.1 | ||||||
| Expected benefits of quitting | 3237 | 1.0 | 0.9 – 1.1 | ||||||
| Worries about health effects | 3237 | 1.3*** | 1.1 – 1.4 | ||||||
| Favourable attitudes to smoking | 3237 | 1.0 | 0.9 – 1.1 | ||||||
| Time (months) since baseline | 3237 | 1.1*** | 1.07 – 1.13 | ||||||
| Likelihood ratio: | χ2(2) = 184.0, p < .001 | χ2(2) = 861.0, p < .001 | |||||||
Note: Overall significance levels for each categorical variable are provided in brackets next to the reference category.
p < .05
p < .01
p < .001.
Quit attempts
Overall, 39.4% reported quit attempts, and this was unrelated to area-level disadvantage (see Table 3), nor were there any consistent non-significant trends. In Model 2 the likelihood of having made a quit attempt increased with high education and decreased with age, however in Model 3, age remained the only significant non smoking-related predictor. In Model 3, strong independent predictors were more proximal intentions to quit, greater worries about the health effects of smoking, being a non-daily smoker, having made a quit attempt in the past year, and a longer elapsed time since the baseline measurements.
Having quit for at least 1 month
Of 1359 smokers who made quit attempts, 41.7% managed to stay quit for at least 1 month. Table 4 shows that, relative to the least disadvantaged area, participants residing in areas of low and high disadvantage were less likely to have abstained for 1 month, whereas those in areas of moderate or extreme disadvantage were no less likely. This “zigzag” effect of area remained significant across all models tested (see Figure 1). Although there was a trend for high income to predict successful 1-month abstinence, age remained the only significant non smoking-related individual-level predictor, with older participants being less likely to have abstained for 1 month in both Models 2 and 3. In Model 3, being a non-daily smoker, having greater self-efficacy to quit, and a longer time since baseline were all associated with a greater likelihood of 1-month abstinence. Relative to having made no prior attempts to quit, having a longest prior quit attempt of less than 1 month lowered the likelihood of 1-month abstinence, as did higher scores on the HSI, and the expectation of greater benefits from quitting.
Figure 1.
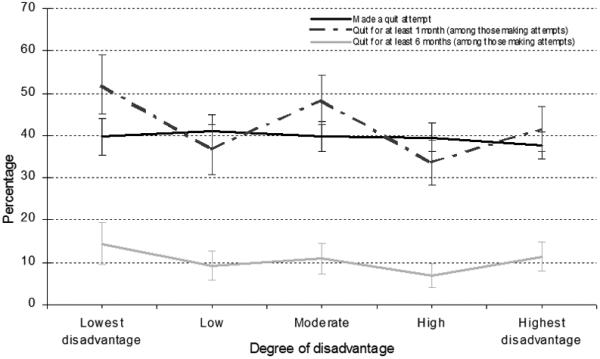
Cessation behaviours since follow-up across the Index of Relative Socio-economic Disadvantage (IRSD) quintiles (error bars represent ±95% confidence intervals).
Having quit for at least 6 months
Of the 1332 eligible smokers who made a quit attempt, 10.3% remained quit for at least 6 months. Although the zigzag relationship with the IRSD observed for 1-month abstinence was still evident (see Figure 1) no statistically significant overall association between IRSD and 6-months abstinence were observed. Indeed, none of the indicators of disadvantage achieved any statistically significant overall association with 6-months abstinence (see Table 5). In Model 3, having made longer quit attempts in the past and a longer time since baseline were the only significant predictors of successful 6-months abstinence, and also a non-significant trend for greater self-efficacy to predict success (p = .051).
Smoking induced deprivation
For the separate analyses where we had measured smoking-induced deprivation (SID: n = 3040), its inclusion did not alter the associations of the outcomes with any of the other predictor variables (including both area- and individual-level disadvantage). At the univariate level, having experienced SID was associated with a greater likelihood of making a quit attempt (OR = 1.5, 95% CI = 1.3 – 1.7), but a lower likelihood of 1-month (OR = 0.7, 95% CI = 0.6 – 0.9) and 6-month abstinence success (OR = 0.6, 95% CI = 0.4 – 0.95). These relationships were attenuated with the inclusion of the SEIFA and individual-level indicators of disadvantage in Model 2, and the association between SID and 6-month abstinence was no longer statistically significant. In Model 3, only the association between smoking-induced deprivation and making quit attempts remained statistically significant (OR = 1.2, 95% CI = 1.02 – 1.5).
Discussion
Area-level disadvantage had no consistent predictive associations with smoking cessation for Australian smokers. Smokers residing in areas of the highest disadvantage were no less likely to make quit attempts than those in the least disadvantaged areas. Among those who made quit attempts area disadvantage was a significant independent predictor of reaching cessation milestones, but not in a linear fashion. Relative to the least disadvantaged areas, both low and high (but not the highest) area disadvantage predicted a lower likelihood of achieving 1-month abstinence. For 6-months abstinence, this zigzag relationship was no longer statistically significant, especially after considering individual factors like length of the longest prior quit attempt.
Individual-level indicators of disadvantage were also largely unrelated to cessation outcomes after we controlled for the smoking-related covariates. Notably, quit attempts were more likely among smokers who had experienced smoking-induced deprivation, independent of the other covariates, however it was not independently associated with 1-month or 6-month abstinence.
A major strength of the present research was the use of four different area-level indexes of relative disadvantage. Our results were not likely, therefore, to be a product of the idiosyncrasies of any one measure, nor a function of measurement sensitivity, as three gradations (quintiles, deciles, and continuous) and two area sizes (CD and POA) were explored. A limitation, however, is that extremely disadvantaged individuals (e.g. homeless, institutionalized, mentally ill, or otherwise addicted) are typically underrepresented in surveys such as the ITC4 and our findings may not generalise to these groups. All these groups tend to be of lower SES and have lower success rates for quitting [28; 29]. It is probable that we would find SES effects if they were equally represented, but would expect the effects to disappear when these factors were controlled for, so it is likely that this sampling bias does not materially affect our conclusions.
Our findings are consistent with previous research [2] showing little relation of disadvantage to cessation outcomes. An evaluation of smokers’ responses to the recent Australian tax increase on tobacco found that the more disadvantaged smokers, at both an individual- and area-level, were no less likely to try to quit or cut down their cigarette consumption [30]. The increased prevalence of smoking among disadvantaged groups is seemingly more attributable to them ever having started rather than being unable or unwilling to quit [10; 31].
Given the large number of analyses we conducted, we also cannot rule out the possibility that the few significant results we did find were chance effects. Given our long follow-up period, we acknowledge that the forgetting of quit attempts may have led to artificially high cessation outcome rates [32], however we can think of no reason why this would differentially affect individuals from different areas or individual SES, so we do not expect that memory effects would impact our general conclusions. We have been unable to interpret the non-linear relationship observed between area disadvantage and medium-term cessation, and await future research to shed light on why it may be the smokers from “moderately disadvantaged” and “moderately advantaged” areas who are finding it most difficult to stay quit.
A factor that may be more closely related to smoking cessation [23; 33] and to which socioeconomic disadvantage is a contributing factor is psychological distress, and we think future research focussing on this would be useful. In conclusion, however, what ultimately emerges from our findings is an encouraging scenario suggesting that the socio-economic circumstances of disadvantaged smokers provide few direct barriers to their making quit attempts and achieving medium-term quit success. Supporting individuals to quit and dealing with their personal circumstances in doing so is likely to remain an effective strategy, and attempts to improve overall social conditions, however important for overall well-being and social equity, may not play a major role in reducing smoking prevalence.
Acknowledgements
The ITC Four-Country Survey is supported by multiple grants including the National Health and Medical Research Council of Australia (265903, 450110), R01 CA 100362 and P50 CA111236 (Roswell Park Transdisciplinary Tobacco Use Research Center) and also in part from grant P01 CA138389 (Roswell Park Cancer Institute, Buffalo, New York), all funded by the National Cancer Institute of the United States, Robert Wood Johnson Foundation (045734), Canadian Institutes of Health Research (57897, 79551), Cancer Research UK (C312/A3726), Canadian Tobacco Control Research Initiative (014578); with additional support from Centre for Behavioural Research and Program Evaluation, National Cancer Institute of Canada/Canadian Cancer Society. We would like to thank members of the Data Management Core at the University of Waterloo for assistance in preparing the data for this analysis.
Footnotes
Ethics clearance: All waves of the study have received ethical approval from the relevant institutional review board or research ethics committee at The Cancer Council Victoria (Australia) HREC 0211, Roswell Park Cancer Institute (USA), University of Waterloo (Canada), and University of Strathclyde (UK).
Declaration of Interest: The authors declare that they have no competing interests
References
- 1.Hill SE, Blakely TA, Fawcett JM, Howden-Chapman P. Could mainstream anti-smoking programs increase inequalities in tobacco use? New Zealand data from 1981-96. Aust N Z J Public Health. 2005;29:279–284. doi: 10.1111/j.1467-842x.2005.tb00769.x. [DOI] [PubMed] [Google Scholar]
- 2.Miller C, Hickling J. Smoking and social inequalities. Cancer Forum. 2004:28. [Google Scholar]
- 3.Siahpush M. Smoking and social inequality. Aust N Z J Public Health. 2004;28:297. doi: 10.1111/j.1467-842x.2004.tb00711.x. [DOI] [PubMed] [Google Scholar]
- 4.Huisman M, Kunst AE, Mackenbach JP. Inequalities in the prevalence of smoking in the European Union: comparing education and income. Prev Med. 2005;40:756–764. doi: 10.1016/j.ypmed.2004.09.022. [DOI] [PubMed] [Google Scholar]
- 5.Siahpush M, Heller G, Singh G. Lower levels of occupation, income and education are strongly associated with a longer smoking duration: Multivariate results from the 2001 Australian National Drug Strategy Survey. Public Health. 2005;119:1105–1110. doi: 10.1016/j.puhe.2005.03.004. [DOI] [PubMed] [Google Scholar]
- 6.Delva J, Tellez M, Finlayson TL, Gretebeck KA, Siefert K, Williams DR, Ismail AI. Cigarette smoking among low-income African Americans: A serious public health problem. Am J Prev Med. 2005;29:218–220. doi: 10.1016/j.amepre.2005.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chuang Y-C, Cubbin C, Ahn D, Winkleby MA. Effects of neighbourhood socioeconomic status and convenience store concentration on individual level smoking. J Epidemiol Community Health. 2005;59:568–573. doi: 10.1136/jech.2004.029041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lakshman R, McConville A, How S, Flowers J, Wareham N, Cosford P. Association between area-level socioeconomic deprivation and a cluster of behavioural risk factors: cross-sectional, population-based study. J Public Health. 2011;33:234–245. doi: 10.1093/pubmed/fdq072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Reijneveld SA. The impact of individual and area characteristics on urban socioeconomic differences in health and smoking. Int J Epidemiol. 1998:27. doi: 10.1093/ije/27.1.33. [DOI] [PubMed] [Google Scholar]
- 10.Siahpush M, Borland R. Socio-demographic variations in smoking status among Australians aged ≥ 18: multivariate results from the 1995 National Health Survey. Aust N Z J Public Health. 2001;25:438–442. [PubMed] [Google Scholar]
- 11.Migliorini C, Siahpush M. Smoking, not smoking: how important is where you live? Health Promot J Aust. 2006;17:226–232. doi: 10.1071/he06226. [DOI] [PubMed] [Google Scholar]
- 12.Adams RJ, Howard N, Tucker G, Appleton S, Taylor AW, Chittleborough C, Gill T, Ruffin RE, Wilson DH. Effects of area deprivation on health risks and outcomes: a multilevel, cross-sectional, Australian population study. Int J Public Health. 2009;54:183–192. doi: 10.1007/s00038-009-7113-x. [DOI] [PubMed] [Google Scholar]
- 13.Turrell G, Mathers C. Socioeconomic inequalities in all-cause and specific-cause mortality in Australia: 1986-1987 and 1995-1997. Int J Epidemiol. 2001;30:231–239. doi: 10.1093/ije/30.2.231. [DOI] [PubMed] [Google Scholar]
- 14.Bentley R, Kavanagh AM, Subramanian SV, Turrell G. Area disadvantage, individual socio-economic position, and premature cancer mortality in Australia 1998 to 2000: a multilevel analysis. Cancer Causes Control. 2008;19:183–193. doi: 10.1007/s10552-007-9084-7. [DOI] [PubMed] [Google Scholar]
- 15.Paul CL, Ross S, Bryant J, Hill W, Bonevski B, Keevy N. The social context of smoking: A qualitative study comparing smokers of high versus low socioeconomic position. BMC Public Health. 2010;10:211. doi: 10.1186/1471-2458-10-211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Stead M, MacAskill S, MacKintosh A-M, Reece J, Eadie D. “It's as if you're locked in”: qualitative explanations for area effects on smoking in disadvantaged communities. Health Place. 2001;7:333–343. doi: 10.1016/s1353-8292(01)00025-9. [DOI] [PubMed] [Google Scholar]
- 17.Chandola T, Head J, Bartley M. Socio-demographic predictors of quitting smoking: how important are household factors? Addiction. 2004;99:770–777. doi: 10.1111/j.1360-0443.2004.00756.x. [DOI] [PubMed] [Google Scholar]
- 18.McCracken K. Into a SEIFA SES cul-de-sac? Aust N Z J Public Health. 2001;25:305–306. doi: 10.1111/j.1467-842x.2001.tb00584.x. [DOI] [PubMed] [Google Scholar]
- 19.Hyland A, Borland R, Li Q, Yong H-H, McNeill A, Fong GT, O'Connor RJ, Cummings KM. Individual-level predictors of cessation behaviours among participants in the International Tobacco Control (ITC) Four Country Survey. Tob Control. 2006;15:iii83–iii94. doi: 10.1136/tc.2005.013516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhou X, Nonnemaker J, Sherrill B, Gilsenan AW, Coste F, West R. Attempts to quit smoking and relapse: Factors associated with success or failure from the ATTEMPT cohort study. Addict Behav. 2009;34:365–373. doi: 10.1016/j.addbeh.2008.11.013. [DOI] [PubMed] [Google Scholar]
- 21.Siahpush M, Borland R, Yong H-H. Sociodemographic and psychosocial correlates of smoking-induced deprivation and its effect on quitting: findings from the International Tobacco Control Policy Evaluation Survey. Tob Control. 2007;16:1–7. doi: 10.1136/tc.2006.016279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Siahpush M, Carlin JB. Financial stress, smoking cessation and relapse: results from a prospective study of an Australian national sample. Addiction. 2006;110:121–127. doi: 10.1111/j.1360-0443.2005.01292.x. [DOI] [PubMed] [Google Scholar]
- 23.Siahpush M, Yong H-H, Borland R, Reid JL, Hammond D. Smokers with financial stress are more likely to want to quit but less likely to try or succeed: findings from the International Tobacco Control (ITC) Four Country Survey. Addiction. 2009;104:1382–1390. doi: 10.1111/j.1360-0443.2009.02599.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pink B. Australian Bureau of Statistics. [October 2011];Socio-Economic Indexes for Areas (SEIFA) - technical paper. 2006 Available at: http://www.ausstats.abs.gov.au/Ausstats/subscriber.nsf/0/72283F45CB86E5FECA2574170011B271/$File/2039055001_socio-economic%20indexes%20for%20areas%20(seifa)%20-%20technical%20paper_2006.pdf.
- 25.Organization for Economic Cooperation and Development [October 2011];What are equivalence scales. 2009 Available at: http://www.oecd.org/dataoecd/61/52/35411111.pdf.
- 26.Heatherton TF, Kozlowski LT, Frecker RC, Rickert W, Robinson J. Measuring the heaviness of smoking: using self-reported time to the first cigarette of the day and number of cigarettes smoked per day. Brit J Addict. 1989;84:791–800. doi: 10.1111/j.1360-0443.1989.tb03059.x. [DOI] [PubMed] [Google Scholar]
- 27.Australian Institute of Health and Welfare. [October 2011];2010 National drug strategy household survey report. 2011 Drug statistics series no. 25. Cat. no. PHE 145. Available at: www.aihw.gov.au/WorkArea/DownloadAsset.aspx?id=10737419578&libID=10737419577.
- 28.Okuyemi KS, Caldwell AR, Thomas JL, Born W, Richter KP, Nollen N, Braunstein K, Ahluwalia JS. Homelessness and smoking cessation: Insights from focus group. Nicotine Tob Res. 2006;8:287–296. doi: 10.1080/14622200500494971. [DOI] [PubMed] [Google Scholar]
- 29.Fagerstrom K, Aubin H-J. Management of smoking cessation in patients with psychiatric disorders. Curr Med Res Opin. 2009;25:551–518. doi: 10.1185/03007990802707568. [DOI] [PubMed] [Google Scholar]
- 30.Dunlop SM, Perez D, Cotter T. Australian smokers' and recent quitters' responses to the increasing price of cigarettes in the context of a tobacco tax increase. Addiction. 2011;106:1687–1695. doi: 10.1111/j.1360-0443.2011.03492.x. [DOI] [PubMed] [Google Scholar]
- 31.Hill DJ, White VM. Australian adult smoking prevalence in 1992. Aust J Public Health. 1995;19:305–308. doi: 10.1111/j.1753-6405.1995.tb00449.x. [DOI] [PubMed] [Google Scholar]
- 32.Borland R, Partos TR, Yong HH, Cummings KM, Hyland A. How much unsuccessful quitting activity is going on among adult smokers? Data from the International Tobacco Control 4-Country cohort survey. Addiction. doi: 10.1111/j.1360-0443.2011.03685.x. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Dube SR, Carballo RS, Dhingra SS, Pearson WS, McClave AK, Strine TW, Berry JT, Mokdad AH. The relationship between smoking status and serious psychological distress: findings from the 2007 Behavioral Risk Factor Surveillance System. Int J Public Health. 2009;54:568–574. doi: 10.1007/s00038-009-0009-y. [DOI] [PubMed] [Google Scholar]


