Abstract
Background
Adults are at substantial risk for vaccine-preventable disease, but their vaccination rates remain low.
Objective
To assess practices for assessing vaccination status and stocking recommended vaccines, barriers to vaccination, characteristics associated with reporting financial barriers to delivering vaccines, and practices regarding vaccination by alternate vaccinators.
Design
Mail and Internet-based survey.
Setting
Survey conducted from March to June 2012.
Participants
General internists and family physicians throughout the United States.
Measurements
A financial barriers scale was created. Multivariable linear modeling for each specialty was performed to assess associations between a financial barrier score and physician and practice characteristics.
Results
Response rates were 79% (352 of 443) for general internists and 62% (255 of 409) for family physicians. Twenty-nine percent of general internists and 32% of family physicians reported assessing vaccination status at every visit. A minority used immunization information systems (8% and 36%, respectively). Almost all respondents reported assessing need for and stocking seasonal influenza; pneumococcal; tetanus and diphtheria; and tetanus, diphtheria, and acellular pertussis vaccines. However, fewer assessed and stocked other recommended vaccines. The most commonly reported barriers were financial. Characteristics significantly associated with reporting greater financial barriers included private practice setting, fewer than 5 providers in the practice, and, for general internists only, having more patients with Medicare Part D. The most commonly reported reasons for referring patients elsewhere included lack of insurance coverage for the vaccine (55% for general internists and 62% for family physicians) or inadequate reimbursement (36% and 41%, respectively). Patients were most often referred to pharmacies/retail stores and public health departments.
Limitations
Surveyed physicians may not be representative of all physicians.
Conclusion
Improving adult vaccination delivery will require increased use of evidence-based methods for vaccination delivery and concerted efforts to resolve financial barriers, especially for smaller practices and for general internists who see more patients with Medicare Part D.
Primary Funding Source
Centers for Disease Control and Prevention.
Vaccination remains underutilized in adults. An annual average of more than 30 000 Americans die of vaccine-preventable diseases, mostly influenza, and more than 95% of these persons are adults (1). The Advisory Committee on Immunization Practices recommends 12 vaccines for adults, including vaccines recommended universally, vaccines for persons who did not receive them in childhood (“catch up”), and vaccines for those in high-risk groups (2). According to recent estimates (3, 4), only 62% and 65% of adults aged 65 years or older received a pneumococcal or influenza vaccine, respectively; only 20% of high-risk adults aged 19 to 64 years received a pneumococcal vaccine; and only 16% of adults aged 60 years or older received a herpes zoster vaccine. All of these percentages are well short of Healthy People 2020 goals (5).
None of the studies that examined reasons for low rates of adult vaccination (6 –12) comprehensively examined adult vaccination. Furthermore, the context of adult vaccination has changed in recent years: There are newly recommended adult vaccines, some vaccines are now covered by Medicare Part D (a pharmaceutical benefit), and the site of vaccine delivery has shifted away from primary care settings. Almost half of adult seasonal influenza vaccinations in the 2010–2011 season occurred in health departments, pharmacies, work places, or other nonmedical locations (13), but physician perceptions regarding collaboration with alternate vaccinators have only been documented limitedly (14).
Given the increase in the number of vaccines recommended for adults and the increasing importance of alternative sites for vaccine delivery, we sought to describe the following among U.S. primary care physicians: practices regarding assessing vaccination status and stocking of recommended adult vaccines; barriers to stocking and administering vaccines; characteristics of physicians who report greater financial barriers to delivering vaccines; and practices, experiences, and attitudes regarding vaccination outside of the medical home.
Methods
Study Setting
From March to June 2012, we administered a survey to a network of primary care physicians (Supplement, available at www.annals.org). The Human Subjects Review Board at the University of Colorado Denver approved this study as exempt research that did not require written informed consent.
Study Sample
The Vaccine Policy Collaborative Initiative conducted this study (15). The Initiative was designed collaboratively with the Centers for Disease Control and Prevention (CDC) to perform rapid-turnaround surveys to assess physician attitudes about vaccine issues. We developed a network of primary care physicians for this program by recruiting general internists (GIMs) and family medicine physicians (FMs) from the memberships of the American College of Physicians (ACP) and the American Academy of Family Physicians (AAFP). We conducted quota sampling (16) to ensure that network physicians were similar to the ACP and AAFP memberships with respect to region, urban versus rural location, and practice setting (GIMs only). We previously demonstrated that survey responses from network physicians compared with those of physicians randomly sampled from American Medical Association physician databases (which reflect all practicing physicians and not just members of the American Medical Association) had similar demographic characteristics, practice attributes, and attitudes about a range of vaccination issues (16).
Survey Design
We developed a survey appraising physician practices regarding assessment of vaccination status for and stocking of the 11 adult vaccines routinely recommended in 2012 (17), as well as referral practices to alternate vaccinators when vaccines were not stocked. We used 4-point Likert scales for questions assessing attitudes about the role of different adult vaccine providers (“strongly agree” to “strongly disagree”) and barriers to stocking and administering vaccines in the practice (“major barrier” to “not a barrier”) (18). For brevity, certain questions were asked in a generic manner and were not related to specific vaccines. After an advisory panel of GIMs (n = 6) and FMs (n = 7) pretested the survey, we modified it on the basis of their feedback. The survey was then piloted by 86 primary care physicians (63 GIMs and 23 FMs) and further modified according to this feedback.
Survey Administration
According to physician preference, we sent the survey either over the Internet (Verint; Melville, New York) or through the U.S. Postal Service. We sent the Internet group an initial e-mail with up to 8 e-mail reminders, and we sent the mail group an initial mailing and up to 2 additional reminders. Nonrespondents in the Internet group were also sent a mail survey in case of problems with e-mail correspondence. We patterned the mail protocol on Dillman’s tailored design method (19).
Statistical Analysis
We pooled Internet and mail surveys together for analyses because other studies have found that physician attitudes are similar when obtained by either method (20–22). We compared respondents with nonrespondents on all available characteristics using Wilcoxon and chi-square analyses. Characteristics of nonrespondents were obtained from the recruitment survey for the sentinel networks. We found financial barriers to be commonly reported and therefore assessed whether certain characteristics of primary care physicians were associated with perceiving more financial barriers because this information could lead to actionable policymaking. To assess associations with perception of financial barriers and to avoid issues associated with multiple comparisons, we created a financial barriers scale composed of 8 financial barrier survey questions (Table 1). We combined the scores of these 8 variables (not a barrier = 0; minor barrier = 1; moderate barrier = 2; major barrier = 3) and divided that sum by the number of questions answered. We excluded respondents who had answered fewer than 5 of the 8 questions on financial barriers. A Cronbach α was calculated to determine the internal consistency of the financial barriers scale. We used this scale as the outcome measure to evaluate associations between financial barriers and demographic and practice characteristics (sex, age, region, practice location, practice setting, number of providers in the practice, and proportion of patients with Medicare Part D and Medicaid) in a multivariable linear regression model for each specialty. Analyses were done by using SAS, version 9.2 (SAS Institute, Cary, North Carolina).
Table 1.
Perceived Barriers to Stocking and Administering Vaccines for Adult Patients in Respondents’ Practice
| Barriers | GIMs, % (n = 352) | FMs, % (n = 255) | ||||||
|---|---|---|---|---|---|---|---|---|
| Major Barrier |
Moderate Barrier |
Minor Barrier |
Not a Barrier |
Major Barrier |
Moderate Barrier |
Minor Barrier |
Not a Barrier |
|
| Lack of adequate reimbursement for vaccine purchase* | 28 | 25 | 24 | 23 | 31 | 28 | 19 | 22 |
| Difficulty determining if a patient’s insurance will reimburse for a vaccine* | 27 | 32 | 22 | 19 | 26 | 35 | 23 | 16 |
| Patients not having insurance coverage for vaccines* | 22 | 35 | 27 | 16 | 24 | 39 | 26 | 11 |
| Lack of adequate reimbursement for vaccine administration* | 22 | 23 | 28 | 27 | 22 | 30 | 25 | 23 |
| Upfront costs of buying vaccines* | 19 | 21 | 27 | 33 | 21 | 29 | 26 | 24 |
| Acute problems taking precedence over vaccinating | 17 | 33 | 37 | 13 | 18 | 31 | 36 | 15 |
| Patients refusing vaccines for financial reasons* | 15 | 32 | 33 | 20 | 15 | 35 | 38 | 12 |
| Patients refusing vaccines because they do not think they need them | 15 | 36 | 42 | 7 | 11 | 41 | 41 | 7 |
| Potential financial loss due to expiration of vaccine prior to use* | 11 | 16 | 32 | 41 | 14 | 19 | 38 | 29 |
| Other preventive services taking precedence during time limited visits | 11 | 29 | 41 | 19 | 12 | 33 | 35 | 20 |
| Difficulty determining whether a patient has received particular vaccine | 11 | 38 | 41 | 10 | 10 | 44 | 37 | 9 |
| Patients refusing vaccines because they feel they are unlikely to get a vaccine-preventable disease | 10 | 37 | 44 | 9 | 11 | 37 | 44 | 8 |
| Not having enough patients needing vaccines to justify the cost of stocking all vaccines* | 9 | 15 | 24 | 52 | 10 | 16 | 26 | 48 |
| Patients refusing vaccines for issues of safety | 9 | 32 | 48 | 11 | 4 | 32 | 52 | 12 |
| The fact that patients can receive vaccines elsewhere | 6 | 11 | 42 | 41 | 3 | 17 | 43 | 37 |
| Patients refusing vaccine for issues of efficacy | 5 | 16 | 54 | 25 | 2 | 16 | 53 | 29 |
| The hassle of storing vaccines | 5 | 12 | 38 | 45 | 6 | 16 | 38 | 40 |
| Patients not coming in regularly for office visits | 4 | 17 | 45 | 34 | 7 | 24 | 44 | 25 |
| The hassle of ordering vaccines | 4 | 8 | 35 | 53 | 5 | 15 | 35 | 45 |
| Uncertainty about a particular vaccine’s effectiveness | 3 | 6 | 35 | 56 | 2 | 8 | 28 | 62 |
| Not remembering to screen patients for needed vaccines | 2 | 10 | 47 | 41 | 3 | 20 | 47 | 30 |
FM = family physician; GIM = general internist.
Question used in the financial barrier scale.
Role of the Funding Source
Investigators at the CDC were involved with the survey design, analysis, and the decision to submit the manuscript for publication.
Results
Survey Response Rates and Respondent Characteristics
Response rates were 79% for GIMs (352 of 443) and 62% for FMs (255 of 409). All questions had fewer than 8% missing items, with most having fewer than 5% missing. The number of missing items did not differ between GIMs and FMs or between physicians who responded by Internet and those who responded by mail. No GIMs and only 2 FMs were from the same practice site. Respondents and nonrespondents did not differ significantly by sex, age, region, practice location, practice setting, or number of providers in the practice. Table 2 displays characteristics of respondents and their practices and patient populations.
Table 2.
Comparison of Respondents and Nonrespondents and Additional Characteristics of Respondents’ Practices
| Characteristic | GIMs | FMs | ||
|---|---|---|---|---|
| Respondents (n = 352) |
Nonrespondents (n = 91) |
Respondents (n = 255) |
Nonrespondents (n = 154) |
|
| Men, % | 63 | 74 | 55 | 60 |
| Mean age (SD), y | 53.9 (8.8) | 54.2 (9.1) | 52.5 (9.9) | 52.0 (10.1) |
| Region of the country, % | ||||
| Midwest | 20 | 26 | 26 | 30 |
| Northeast | 26 | 26 | 17 | 13 |
| South | 31 | 35 | 35 | 38 |
| West | 23 | 12 | 22 | 19 |
| Practice location, % | ||||
| Urban, inner city | 45 | 40 | 26 | 27 |
| Urban, non–inner city/suburban | 42 | 43 | 46 | 49 |
| Rural | 13 | 18 | 28 | 24 |
| Practice setting, % | ||||
| Private practice | 70 | 77 | 70 | 73 |
| Community-or hospital-based | 22 | 20 | 23 | 22 |
| HMO or MCO | 9 | 3 | 7 | 5 |
| Median providers in practice, n | 7 | 7 | 5 | 5 |
| Proportion of patients aged <18 y | ||||
| 0% | 49 | – | 5 | – |
| 1%–9% | 47 | – | 42 | – |
| ≥10% | 4 | – | 53 | – |
| Proportion of patients aged 18–49 y | ||||
| <10% | 16 | – | 8 | – |
| 10%–24% | 61 | – | 42 | – |
| 25%–49% | 19 | – | 43 | – |
| ≥50% | 4 | – | 7 | – |
| Proportion of patients aged 50–64 y | ||||
| 0%–24% | 22 | – | 33 | – |
| 25%–49% | 66 | – | 57 | – |
| ≥50% | 11 | – | 11 | – |
| Proportion of patients aged ≥65 y | ||||
| <10% | 3 | – | 17 | – |
| 10%–24% | 13 | – | 28 | – |
| 25%–49% | 44 | – | 37 | – |
| ≥50% | 40 | – | 17 | – |
| Reported contractual relationship with insurer | ||||
| Medicare | 87 | – | 90 | – |
| Medicaid | 63 | – | 75 | – |
| Private Insurance | 85 | – | 90 | – |
| Proportion of uninsured patients | ||||
| 0% | 13 | – | 7 | – |
| 1%–9% | 72 | – | 62 | – |
| 10%–24% | 11 | – | 20 | – |
| ≥25% | 4 | – | 11 | – |
| Proportion of patients with Medicare Part B | ||||
| <10% | 7 | – | 17 | – |
| 10%–24% | 21 | – | 41 | – |
| 25%–49% | 37 | – | 28 | – |
| ≥50% | 34 | – | 14 | – |
| Proportion of patients with Medicare Part D | ||||
| <10% | 8 | – | 22 | – |
| 10%–24% | 27 | – | 35 | – |
| 25%–49% | 31 | – | 23 | – |
| ≥50% | 24 | – | 10 | – |
| Don’t know | 11 | – | 11 | – |
| Proportion of patients with Medicaid | ||||
| <10% | 72 | – | 52 | – |
| 10%–24% | 18 | – | 25 | – |
| ≥25% | 10 | – | 24 | – |
| Proportion of patients with private insurance | ||||
| 0%–24% | 25 | – | 23 | – |
| 25%–49% | 35 | – | 31 | – |
| 50%–100% | 40 | – | 47 | – |
FM = family physician; GIM = general internist; MCO = managed care organization.
Current Practices Regarding Assessing Need for and Stocking of Routinely Recommended Adult Vaccines
Almost all physicians reported assessing patients’ vaccination status at annual visits (GIMs and FMs, 97%) or initial visits (GIMs, 94%; FMs, 89%), whereas fewer physicians (GIMs, 29%; FMs, 32%) reported doing so at every visit. The most commonly reported method for assessing immunization status was to check the medical record (GIMs, 95%; FMs, 96%). Although most physicians reported asking patients about vaccination status verbally (GIMs, 89%; FMs, 90%), by questionnaire (GIMs, 57%; FMs, 52%), or by having a staff member ask (GIMs, 57%; FMs, 66%), very few (GIMs, 1%; FMs, 2%) relied exclusively on patient-supplied information. A minority used immunization information systems (IISs) (GIMs, 8%; FMs, 36%). Forty-six percent of GIMs and 48% of FMs reported that it was “moderately/very difficult” to determine an adult patient’s vaccination status for vaccines other than seasonal influenza.
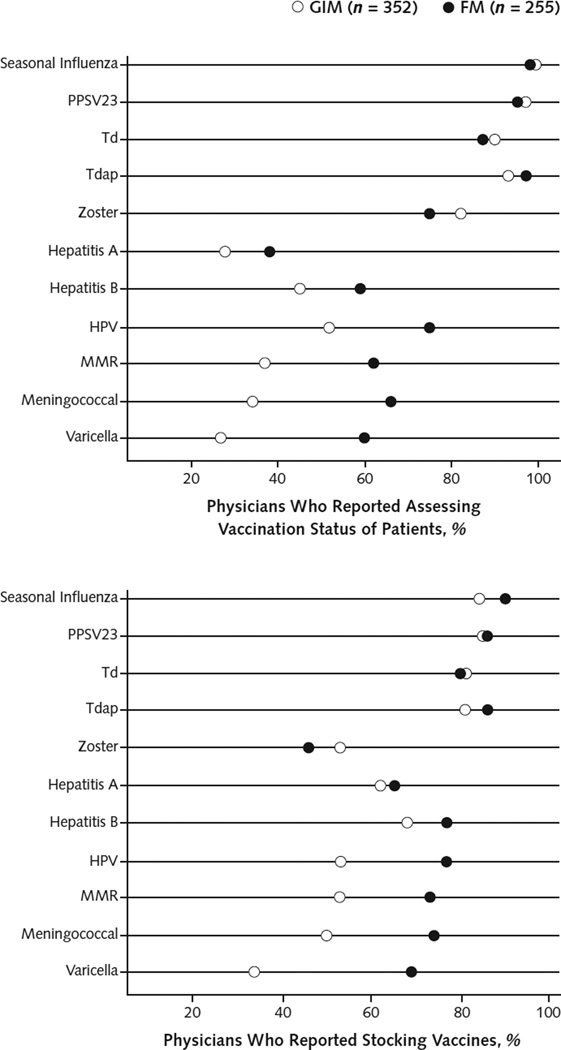
Almost all physicians reported assessing the vaccination status for seasonal influenza; pneumococcal; tetanus and diphtheria (Td); tetanus, diphtheria, and acellular pertussis (Tdap); and zoster vaccines. Fewer reported assessing the status for the remainder of the recommended vaccines (Figure 1). Family physicians were more likely than GIMs to assess the need for hepatitis A; hepatitis B; measles, mumps, and rubella (MMR); human papillomavirus; meningococcal; and varicella vaccines.
Figure 1.
Percentage of physicians who reported assessing vaccination status of patients and stocking vaccines.
FM = family physician; GIM = general internists; HPV = human papillomavirus; MMR = measles, mumps, and rubella; PPSV23 = pneumococcal polysaccharide; Td = tetanus and diphtheria; Tdap = tetanus, diphtheria, and acellular pertussis.
Most physicians reported stocking seasonal influenza, pneumococcal, Td, and Tdap vaccines (Figure 1). Physicians were less likely to stock hepatitis vaccines, catch-up vaccines (human papillomavirus, MMR, varicella, and meningococcal), and zoster vaccine. Family physicians more often reported stocking hepatitis B and catch-up vaccines than did GIMs; large proportions of both FMs and GIMs reported not stocking zoster vaccine. Thirty-one percent of FMs and 20% of GIMs reported stocking all 11 adult vaccines recommended for routine use in 2012.
Reported Barriers to Stocking and Administering Adult Vaccines
Physicians reported various barriers to stocking and administering vaccines (Table 1), but financial barriers dominated the list. Internal consistency of the financial barriers scale was high for both specialties (Cronbach α > 0.85). Basic distributional statistics were similar for the financial barriers scale for each specialty (GIM: mean, 1.3 [SD, 0.8]; median, 1.4; 25th to 75th percentiles, 0.8 to 2.0. FMs: mean, 1.5 [SD, 0.8]; median, 1.5; 25th to 75th percentiles, 0.9 to 2.0). Table 3 lists the characteristics associated with reporting financial barriers. Physician characteristics significantly associated with reporting greater financial barriers included private practice setting, fewer than 5 providers in the practice, Southern region, West region for FMs only, and Midwest region and having a higher proportion of patients with Medicare Part D for GIMs only. All statistically significant effect sizes represented approximately one half of to a full SD difference from the reference group, which we considered clinically significant.
Table 3.
Characteristics Associated With Perception of Financial Barriers to Stocking and Administering Vaccines in Practice*
| Characteristic | Estimated Mean Difference (95% CI) | |
|---|---|---|
| GIMs (n = 340) | FMs (n = 250) | |
| Sex | ||
| Male | Reference | Reference |
| Female | 0.09 (−0.07 to 0.25) | −0.05 (−0.23 to 0.14) |
| Age | ||
| 30–49 y | Reference | Reference |
| 50–59 y | −0.01 (−0.20 to 0.17) | 0.06 (−0.15 to 0.27) |
| ≥60 y | 0.04 (−0.16 to 0.25) | 0.00 (−0.23 to 0.27) |
| Region of the country | ||
| South | Reference | Reference |
| Midwest | −0.15 (−0.37 to 0.06) | −0.37 (−0.59 to −0.14) |
| Northeast | −0.36 (−0.56 to −0.16) | −0.38 (−0.64 to −0.11) |
| West | −0.42 (−0.63 to −0.21) | −0.14 (−0.38 to 0.11) |
| Practice location | ||
| Urban, inner city | Reference | Reference |
| Urban, non–inner city/suburban | 0.06 (−0.10 to 0.22) | 0.19 (−0.03 to 0.41) |
| Rural | 0.02 (−0.22 to 0.25) | 0.20 (−0.05 to 0.45) |
| Practice setting | ||
| Private practice | Reference | Reference |
| Community-or hospital-based | −0.33 (−0.54 to −0.13) | −0.37 (−0.60 to −0.14) |
| HMO or MCO | −0.38 (−0.66 to −0.09) | −0.79 (−1.16 to −0.41) |
| Number of providers in practice | ||
| 1–4 | Reference | Reference |
| ≥5 | −0.52 (−0.68 to −0.36) | −0.31 (−0.49 to −0.12) |
| Proportion of patients with Medicare Part D | ||
| 0%–24% | Reference | Reference |
| ≥25% | 0.31 (0.14 to 0.47) | −0.01 (−0.21 to 0.18) |
| Do not know | 0.18 (−0.10 to 0.47) | −0.01 (−0.30 to 0.28) |
| Proportion of patients with Medicaid | ||
| 0%–9% | Reference | Reference |
| ≥10% | 0.13 (−0.05 to 0.31) | 0.09 (−0.11 to 0.29) |
| Do not know | −0.57 (−1.03 to −0.11) | 0.21 (−0.47 to 0.88) |
FM = family physician; GIM = general internist; MCO = managed care organization.
Values in the table are estimated mean differences in the financial barriers scale between each subgroup and the reference. The financial barriers scale was created as the average of 8 questions related to financial barriers (see Table 1) and varied from 0 (no barrier) to 3 (major barrier). Negative values indicate lower scores (fewer barriers), and positive values indicate higher scores (more barriers) as compared with the reference group.
Current Practice Regarding Referring Patients to Alternate Vaccinators
Most physicians reported that they refer patients elsewhere for vaccines they did not stock. When they did not stock the vaccine, physicians most often reported referring patients to a pharmacy/retail store (GIMs: 26% “often or always” and 35% “sometimes”; FMs: 24% “often or always” and 38% “sometimes”) and the public health department (GIMs: 17% “often or always” and 37% “sometimes”; FMs: 26% “often or always” and 45% “sometimes”). The most commonly reported reasons for referring patients elsewhere for vaccines included insurance not covering the vaccine (GIMs: 18% “often or always” and 39% “sometimes”; FMs: 18% “often or always” and 48% “sometimes”) or inadequate insurance reimbursement (GIMs: 13% “often or always” and 25% “sometimes”; FMs: 10% “often or always” and 34% “sometimes”).
Communication With Alternate Vaccinators
Physicians reported using multiple information sources regarding vaccination of their patients by alternate vaccinators. The preferred source was the vaccinator (GIMs, 84%; FMs, 83%), followed by an IIS (GIMs, 25%; FMs, 44%); fewer preferred relying on patient report (GIMs, 20%; FMs, 15%). Several physicians reported rarely (<10% of the time) receiving information on vaccines administered by the following vaccinators: workplace (GIMs, 74%; FMs, 76%), senior center (GIMs, 68%; FMs, 74%), public health department (GIMs, 65%; FMs 63%), another physician’s office (GIMs, 50%; FMs, 54%), hospital or emergency department (GIMs, 54%; FMs, 42%), and pharmacy or retail store (GIMs, 34%; FMs, 38%). The most common methods for recording information received from alternate vaccinators were to enter information in a specific vaccine field in the electronic health record (EHR) (GIMs, 78%; FMs, 77%), enter information in a progress note in the EHR or paper medical record (GIMs, 66%; FMs, 71%), or record information on a specific immunization sheet in a written record (GIMs, 31%; FMs, 28%). Eight percent of GIMs and 36% of FMs recorded information in a state or regional IIS.
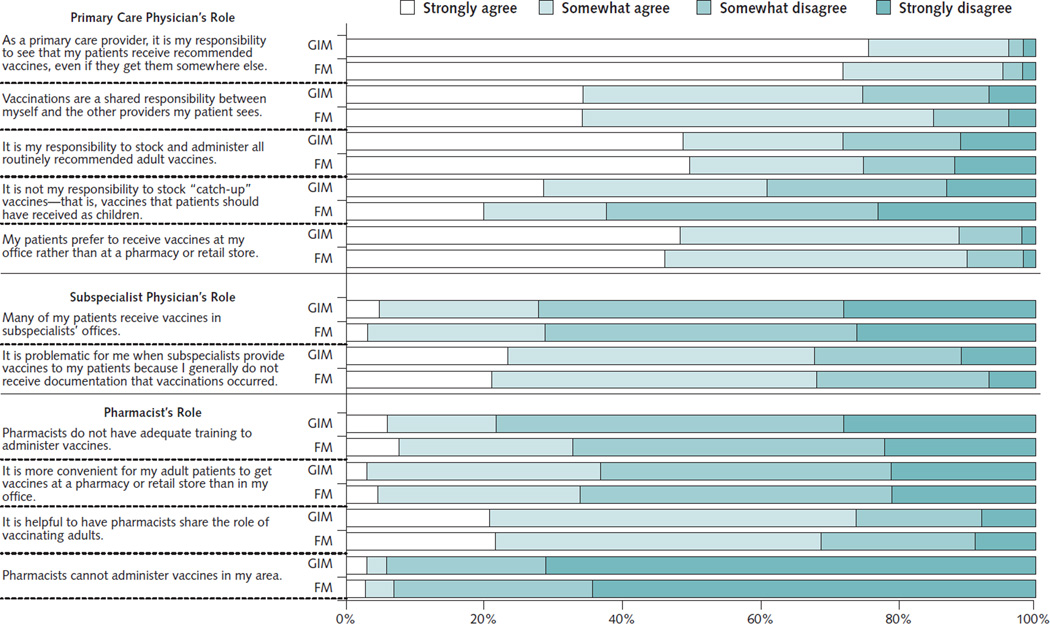
Attitudes Regarding the Role of Different Vaccinators
Figure 2 presents attitudes regarding the role of different adult vaccinators. Of note, almost all physicians agreed that it was the primary care physician’s responsibility to see that patients receive recommended vaccines even if they did so elsewhere. Most agreed it was helpful to have pharmacists share a role in vaccinating adults. Physicians generally considered vaccination by subspecialists to be problematic because they do not receive documentation of such vaccination.
Figure 2.
Physicians’ attitudes and beliefs regarding the role of different adult vaccine providers.*
FM = family physician; GIM = general internist.
* Number of FMs = 255; number of GIMs = 352.
Discussion
This study assessed important aspects of current practices for U.S. adult vaccination from the physician perspective. We identified problems and barriers relating to the delivery of adult vaccines in the primary care setting, including inconsistent assessment of vaccination status, insufficient stocking of certain recommended vaccines, inadequate insurance reimbursement, large financial outlays for vaccine purchase, and challenges relating to the transfer and documentation of vaccination information from alternate vaccinators.
Our study suggests that missed opportunities for adult vaccination are common, partially because vaccination status is not being assessed at every visit, which is admittedly an ambitious goal. In addition, most physicians are not stocking all recommended adult vaccines. Our results are consistent with those of other studies documenting general failure to review vaccination status at each visit, with resulting undervaccination of adult patients (23, 24) and the lack of stocking of some vaccines (25). Zoster vaccine has been recommended since 2008 (26), but uptake of the vaccine has remained low (4, 27). One likely contributing factor for low rates of stocking this vaccine is the difficulty in physician reimbursement for zoster vaccine. The vaccine is covered under Medicare Part D, a pharmaceutical benefit with often substantial out-of-pocket costs for the patient, and not Part B, an office-based benefit that covers seasonal influenza and pneumococcal vaccines. Most Medicare beneficiaries enroll in Medicare Part B, but in 2009 only 58% enrolled in Medicare Part D, pointing to a potential lack of coverage for this vaccine altogether (28).
In a previous study (25), more GIMs than FMs reported not stocking MMR, meningococcal conjugate, varicella, and hepatitis A vaccines because few of their patients needed these vaccines. Similarly, we found more general internists than family medicine physicians (61% vs. 37%) agreeing that stocking of catch-up vaccines was not their responsibility. These sentiments probably stem from caring for different patient populations; FMs see pediatric patients, who more regularly need these vaccines. Stocking of all recommended vaccines may not be practical given competing demands in primary care. Not stocking vaccines probably contributes to low national coverage (3, 4), but pneumococcal, seasonal influenza, Td, and Tdap vaccine coverage remains suboptimal, even though most physicians report stocking these vaccines. This finding suggests that stocking alone is insufficient to improve coverage.
Primary care physicians are generally accepting of the increased access that adults now have to vaccination outside of the medical home; however, communication between alternate vaccinators and primary care physicians is perceived as suboptimal, and one third of physicians have reservations about pharmacists as vaccinators. Few studies have evaluated communication between primary care physicians and pharmacists (14, 29, 30), but 1 previous study found that concerns about inadequate documentation and pharmacists’ ability to administer seasonal influenza vaccine were important barriers to collaboration (14). Pharmacists have been involved in adult immunization delivery since the mid-1990s (31); they are now authorized to administer seasonal influenza vaccine in all states and many other routinely recommended vaccines in most states (32).
The most commonly reported reasons for referral to alternate vaccinators were related to insurance coverage. However, such referrals can increase patients’ out-of-pocket costs when alternate providers are considered “out of network” (33).
Our analysis of barriers to adult vaccine delivery sheds light on why physicians are not stocking and administering vaccines. Our results confirm that financial barriers may partially explain these findings (10, 12). Physicians in smaller, private practices often assume more risks from stocking of expensive vaccine inventories and may be particularly affected by these financial barriers.
Although our results suggest that fundamental problems exist for adult vaccination delivery in the United States, primary care physicians see themselves as having a central role in the system. This indicates that with the proper tools, they can be instrumental in increasing vaccination rates among adults.
Information technology provides one such set of tools. Applications are available to enhance assessment of vaccination status (34–36) and, if incorporated into EHRs and computerized clinic decision support systems, could be a means for practices to systematically assess vaccination status. Use of EHR alerts (37) and clinic decision support systems (38) increases rates of specific vaccines delivered to targeted populations, but such interventions could be broadened to encompass all routinely recommended vaccines and the adult population in general. Clinic decision support systems can be used to reduce the decision-making burden of vaccination on physicians and staff.
Immunization information systems provide another important technological tool. These confidential, computerized systems collect and consolidate vaccination data from multiple health care providers (39, 40). In 2010, the Task Force on Community Preventive Services recommended IIS use as a means to increase vaccination rates (41). These systems can alert physicians about the vaccination status of their patients, thereby preventing missed opportunities for vaccination and preventing unnecessary vaccination. Although initially implemented for the pediatric population, IISs are potentially more critical for adults given the increased complexity of the adult immunization schedule and because adults are more likely to receive immunizations at multiple locations. Indeed, IISs could help alleviate the reported communication barriers between primary care physicians and alternate vaccinators. However, to be most effective, IIS use needs to be widespread. Our data indicate that awareness and use of the IISs for adult vaccinations are limited. Use of IISs should increase with adoption of meaningful use phase 2 requirements for reporting immunizations to IISs from EHRs, but additional resources may be needed to educate physicians about IISs and enroll them.
Policy tools can play an important role in improving adult vaccination. By mandating private health plans to cover Advisory Committee on Immunization Practices–recommended vaccinations with first-dollar coverage (that is, no copayment) when delivered by in-network providers, the Affordable Care Act addresses financial barriers to vaccination for privately insured patients (42). The effect of the law on physician financial barriers to vaccination is less certain. The law does not change coverage of vaccines by Medicare. Seasonal influenza and pneumococcal vaccines, Td vaccine for wound management, and hepatitis B vaccine for provider-diagnosed high-risk persons are covered by Medicare Part B; other vaccines (Tdap, herpes zoster, and any future vaccines) are included in Medicare Part D. The latter was designed as a pharmacy benefit and for some time has been recognized as a barrier to physician-based vaccination (12); indeed, the financial burden reported by general internists was directly correlated to the proportion of their patients having Medicare Part D. Recommendations for legislative corrections have been made (28, 43).
Performance measures are another policy-based strategy used to improve vaccination rates for specific vaccines and populations (44, 45). Current performance measures focus on seasonal influenza and pneumococcal vaccines (46). Additional performance measures for other adult immunizations or for combined end points that include vaccination with other preventive services may be considered.
Our study has limitations. Although the sample of sentinel physicians surveyed was designed to be representative of ACP and AAFP memberships, the attitudes, experiences, and practices of sentinel physicians may not be fully generalizable. In addition, although this survey had a high response rate, nonrespondents may have held different views than respondents. The survey relied on self-report of practice rather than observation of practice. Finally, in considering policy implications of our study, cross-sectional surveys enhance our understanding of complex issues but cannot be used to demonstrate causality.
Vaccines provide an important but underutilizd opportunity to reduce the burden of vaccine-preventable disease among adults. Although primary care physicians appear motivated to ensure that patients are up to date on vaccinations, many barriers exist. Implementation of system changes, including adopting practices that improve communication between primary care physicians and alternate vaccinators, more widespread use of effective tools (IISs and clinic decision support systems), and removing policy-related barriers, could improve adult vaccination in the United States.
Supplementary Material
Context
Vaccination rates in adults are low, even though more than 95% of Americans who die of vaccine-preventable disease each year are adults. General internists and family medicine physicians were surveyed about vaccine perceptions and practices.
Contribution
Barriers related to vaccine delivery included lack of regular assessment of vaccine status, insufficient stocking of some vaccines, and financial disincentives for vaccination in the primary care setting. Use of electronic tools to record and prompt vaccination was low. Most physicians surveyed accepted vaccination outside of the medical home but believed communication between themselves and alternate vaccinators was suboptimal.
Implication
System changes are necessary to improve adult vaccination in the United States.
—The Editors
Acknowledgments
The authors thank all general internists and family physicians in the networks for participating in and responding to the survey.
Grant Support: By the Centers for Disease Control and Prevention (SIP–5U48DP001938).
Footnotes
Disclaimer: The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Potential Conflicts of Interests: None disclosed. Forms can be viewed at www.acponline.org/authors/icmje/ConflictOfInterestForms.do?msNum=M13-2332.
Reproducible Research Statement: Study protocol: Available from Dr. Hurley (Laura.Hurley@dhha.org). Statistical code and data set: Certain portions of the analytic data set are available to approved individuals through written agreements with Dr. Hurley and the Centers for Disease Control and Prevention.
Current author addresses and author contributions are available at www.annals.org.
Author Contributions: Conception and design: C.B. Bridges, R. Harpaz, S.T. O’Leary, M. Brtnikova, A. Jimenez-Zambrano, F. Ahmed, A. Kempe.
Analysis and interpretation of the data: C.B. Bridges, R. Harpaz, S.T. O’Leary, M. Brtnikova, B.L. Beaty, C. Hales, A. Kempe.
Drafting of the article: R. Harpaz, S.T. O’Leary, M. Brtnikova, A. Jimenez-Zambrano, A. Kempe.
Critical revision of the article for important intellectual content: C.B. Bridges, R. Harpaz, S.T. O’Leary, M. Brtnikova, B.L. Beaty, F. Ahmed, C. Hales, A. Kempe.
Final approval of the article: C.B. Bridges, R. Harpaz, S.T. O’Leary, M. Brtnikova, B.L. Beaty, A. Jimenez-Zambrano, F. Ahmed, C. Hales, A. Kempe.
Provision of study materials or patients: A. Kempe.
Statistical expertise: S.T. O’Leary, M. Brtnikova, B.L. Beaty, A. Kempe.
Obtaining of funding: A. Kempe.
Administrative, technical, or logistic support: S.T. O’Leary, M. Brtnikova, A. Jimenez-Zambrano, A. Kempe.
Collection and assembly of data: M. Brtnikova, A. Jimenez-Zambrano, A. Kempe.
References
- 1.National Vaccine Advisory Committee. A pathway to leadership for adult immunization: recommendations of the National Vaccine Advisory Committee: approved by the National Vaccine Advisory Committee on June 14, 2011. Public Health Rep. 2012;127(Suppl 1):1–42. doi: 10.1177/00333549121270s101. [PMID: 22210957] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bridges CB, Woods L, Coyne-Beasley T ACIP Adult Immunization Work Group. Advisory Committee on Immunization Practices (ACIP) recommended immunization schedule for adults aged 19 years and older—United States, 2013. MMWR Surveill Summ. 2013;62(Suppl 1):9–19. [PMID: 23364303] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention. FluVax View. Accessed at www.cdc.gov/flu/fluvaxview/index.htm on 25 October 2012.
- 4.Centers for Disease Control and Prevention (CDC) Noninfluenza vaccination coverage among adults - United States, 2011. MMWR Morb Mortal Wkly Rep. 2013;62:66–72. [PMID: 23364272] [PMC free article] [PubMed] [Google Scholar]
- 5.U.S. Department of Health and Human Services. Healthy People 2020. Immunization and infectious diseases. 2012 Accessed at http://healthypeople.gov/2020/topicsobjectives2020/objectiveslist.aspx?topicId_23 on 25 October 2012.
- 6.Johnson DR, Nichol KL, Lipczynski K. Barriers to adult immunization. Am J Med. 2008;121:S28–S35. doi: 10.1016/j.amjmed.2008.05.005. [PMID: 18589065] [DOI] [PubMed] [Google Scholar]
- 7.Szilagyi PG, Shone LP, Barth R, Kouides RW, Long C, Humiston SG, et al. Physician practices and attitudes regarding adult immunizations. Prev Med. 2005;40:152–161. doi: 10.1016/j.ypmed.2004.05.010. [PMID: 15533524] [DOI] [PubMed] [Google Scholar]
- 8.Kempe A, Hurley L, Stokley S, Daley MF, Crane LA, Beaty BL, et al. Pneumococcal vaccination in general internal medicine practice: current practice and future possibilities. J Gen Intern Med. 2008;23:2010–2013. doi: 10.1007/s11606-008-0800-0. [PMID: 18830765] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Daley MF, Hennessey KA, Weinbaum CM, Stokley S, Hurley LP, Crane LA, et al. Physician practices regarding adult hepatitis B vaccination: a national survey. Am J Prev Med. 2009;36:491–496. doi: 10.1016/j.amepre.2009.01.037. [PMID: 19362798] [DOI] [PubMed] [Google Scholar]
- 10.Hurley LP, Harpaz R, Daley MF, Crane LA, Beaty BL, Barrow J, et al. National survey of primary care physicians regarding herpes zoster and the herpes zoster vaccine. J Infect Dis. 2008;197(Suppl 2):S216–S223. doi: 10.1086/522153. [PMID: 18419400] [DOI] [PubMed] [Google Scholar]
- 11.Robert Wood Johnson Foundation. Adult immunization: shots to save lives. 2010 Accessed at http://healthyamericans.org/assets/files/TFAH2010AdultImmnzBrief13.pdf on 25 October 2012. [Google Scholar]
- 12.Hurley LP, Lindley MC, Harpaz R, Stokley S, Daley MF, Crane LA, et al. Barriers to the use of herpes zoster vaccine. Ann Intern Med. 2010;152:555–560. doi: 10.7326/0003-4819-152-9-201005040-00005. [PMID: 20439573] [DOI] [PubMed] [Google Scholar]
- 13.Centers for Disease Control and Prevention (CDC) Place of influenza vaccination among adults—United States, 2010–11 influenza season. MMWR Morb Mortal Wkly Rep. 2011;60:781–785. [PMID: 21681175] [PubMed] [Google Scholar]
- 14.Hurley LP, Wortley P, Allison MA, O’Leary S, Daley MF, Babbel C, et al. Seasonal influenza vaccination in adults: practice and attitudes about collaborative delivery with community vaccinators. Vaccine. 2011;29:8649–8655. doi: 10.1016/j.vaccine.2011.08.126. [PMID: 21933693] [DOI] [PubMed] [Google Scholar]
- 15.University of Colorado Children’s Outcomes Research. Vaccine Policy Collaborative Initiative. Accessed at www.ucdenver.edu/academics/colleges/medicalschool/programs/outcomes/childrensoutcomesreserach/VaccinePolicy CollaborativeInitiative/Pages/default.aspx on 6 November 2013. [Google Scholar]
- 16.Crane LA, Daley MF, Barrow J, Babbel C, Stokley S, Dickinson LM, et al. Sentinel physician networks as a technique for rapid immunization policy surveys. Eval Health Prof. 2008;31:43–64. doi: 10.1177/0163278707311872. [PMID: 18184632] [DOI] [PubMed] [Google Scholar]
- 17.Advisory Committee on Immunization Practices. Recommended adult immunization schedule: United States, 2012. Ann Intern Med. 2012;156:211–217. doi: 10.7326/0003-4819-156-3-201202070-00388. [PMID: 22298576] [DOI] [PubMed] [Google Scholar]
- 18.Schuman H. Questions and Answers in Attitude Surveys: Experiments on Form, Wording, and Context. Thousand Oaks, CA: Sage; 1996. [Google Scholar]
- 19.Dillman DA. Mail and Internet Surveys: The Tailored Design Method. New York: J Wiley; 2000. [Google Scholar]
- 20.McMahon SR, Iwamoto M, Massoudi MS, Yusuf HR, Stevenson JM, David F, et al. Comparison of e-mail, fax and postal surveys of pediatricians. Pediatrics. 2003;111:e299–e303. doi: 10.1542/peds.111.4.e299. [PMID: 12671142] [DOI] [PubMed] [Google Scholar]
- 21.Dillman DA, Smyth JD, Christian LM. Internet, Mail, and Mixed-Mode Surveys: The Tailored Desgin Method. 3rd ed. New York: J Wiley; 2009. [Google Scholar]
- 22.Atkeson LRAA, Bryant LA, Ziberman L, Saunders KL. Considering mixed mode surveys for questions in political behavior: using the Internet and mail to get quality data at reasonable costs. Political Behavior. 2011;33:161–178. [Google Scholar]
- 23.Nowalk MP, Zimmerman RK, Feghali J. Missed opportunities for adult immunization in diverse primary care office settings. Vaccine. 2004;22:3457–3463. doi: 10.1016/j.vaccine.2004.02.022. [PMID: 15308372] [DOI] [PubMed] [Google Scholar]
- 24.Nowalk MP, Zimmerman RK, Cleary SM, Bruehlman RD. Missed opportunities to vaccinate older adults in primary care. J Am Board Fam Pract. 2005;18:20–27. doi: 10.3122/jabfm.18.1.20. [PMID: 15709060] [DOI] [PubMed] [Google Scholar]
- 25.Freed GL, Clark SJ, Cowan AE, Coleman MS. Primary care physician perspectives on providing adult vaccines. Vaccine. 2011;29:1850–1854. doi: 10.1016/j.vaccine.2010.12.097. [PMID: 21216314] [DOI] [PubMed] [Google Scholar]
- 26.Harpaz R, Ortega-Sanchez IR, Seward JF Advisory Committee on Immunization Practices (ACIP) Centers for Disease Control and Prevention (CDC) Prevention of herpes zoster: recommendations of the Advisory Committee on Immunization Practices (ACIP) MMWR Recomm Rep. 2008;57:1–30. [PMID: 18528318] [PubMed] [Google Scholar]
- 27.Centers for Disease Control and Prevention (CDC) Adult vaccination coverage—United States, 2010. MMWR Morb Mortal Wkly Rep. 2012;61:66–72. [PMID: 22298302] [PubMed] [Google Scholar]
- 28.U.S. Government Accountability Office. Medicare: many factors, including administrative challenges, affect access to Part D vaccinations. 2011. Accessed at www.gao.gov/products/GAO-12-61 on 7 December 2012.
- 29.Blake EW, Blair MM, Couchenour RL. Perceptions of pharmacists as providers of immunizations for adult patients. Pharmacotherapy. 2003;23:248–254. doi: 10.1592/phco.23.2.248.32083. [PMID: 12587814] [DOI] [PubMed] [Google Scholar]
- 30.Welch AC, Ferreri SP, Blalock SJ, Caiola SM. North Carolina family practice physicians’ perceptions of pharmacists as vaccinators. J Am Pharm Assoc (2003) 2005;45:486–491. doi: 10.1331/1544345054475414. [PMID: 16128505] [DOI] [PubMed] [Google Scholar]
- 31.Hogue MD, Grabenstein JD, Foster SL, Rothholz MC. Pharmacist involvement with immunizations: a decade of professional advancement. J Am Pharm Assoc (2003) 2006;46:168–179. doi: 10.1331/154434506776180621. [PMID: 16602227] [DOI] [PubMed] [Google Scholar]
- 32.Rothholz MC. The role of community pharmacies/pharmacists in vaccine delivery in the United States. 2013 Accessed at http://media.pharmacist.com/imz/ACIPpresentationRothholzJune2013.pdf on 15 July 2013. [Google Scholar]
- 33.Tan L. Impact of the Affordable Care Act on immunizations—new opportunities and challenges. Accessed at www.nhipconference.com/uploads/Impact_of_ACA_on_Immunizations_-_LJ_Tan.pdf on 17 July 2013. [Google Scholar]
- 34.American College of Physicians. ACP Immunization Advisor App. Accessed at http://immunization.acponline.org/app/ on 6 November 2012. [Google Scholar]
- 35.Centers for Disease Control and Prevention. Adult Immunization Scheduler. 2012 Nov 6; Accessed at www.cdc.gov/vaccines/schedules/Schedulers/adult-scheduler.html on 6 November 2012.
- 36.Smalley HK, Keskinocak P, Engineer FG, Pickering LK. Universal tool for vaccine scheduling: applications for children and adults. Interfaces. 2011;41:436–454. [Google Scholar]
- 37.Ledwich LJ, Harrington TM, Ayoub WT, Sartorius JA, Newman ED. Improved influenza and pneumococcal vaccination in rheumatology patients taking immunosuppressants using an electronic health record best practice alert. Arthritis Rheum. 2009;61:1505–1510. doi: 10.1002/art.24873. [PMID: 19877088] [DOI] [PubMed] [Google Scholar]
- 38.Swenson CJ, Appel A, Sheehan M, Hammer A, Fenner Z, Phibbs S, et al. Using information technology to improve adult immunization delivery in an integrated urban health system. Jt Comm J Qual Patient Saf. 2012;38:15–23. doi: 10.1016/s1553-7250(12)38003-3. [PMID: 22324187] [DOI] [PubMed] [Google Scholar]
- 39.Centers for Disease Control and Prevention (CDC) Immunization information systems progress—United States, 2006. MMWR Morb Mortal Wkly Rep. 2008;57:289–291. [PMID: 18354373] [PubMed] [Google Scholar]
- 40.Centers for Disease Control and Prevention (CDC) Progress in immunization information systems—United States, 2009. MMWR Morb Mortal Wkly Rep. 2011;60:10–12. [PMID: 21228762] [PubMed] [Google Scholar]
- 41.Guide to Community Preventive Services. Universally recommended vaccinations: immunization information systems. The Guide to Community Preventive Services. 2010 Accessed at www.thecommunityguide.org/vaccines/imminfosystems.html on 4 December 2012. [Google Scholar]
- 42.Tan L. Impact of the Affordable Care Act on immunization. Accessed at http://www.preventinfluenza.org/NAIS_2012/NAIS-1_tan_impact.pdf on 3 December 2013. [Google Scholar]
- 43.Medicare Payment Advisory Commission. Issues in Medicare coverage of drugs. Report to the Congress: Promoting Greater Efficiency in Medicare. 2007:157–186. Accessed at www.medpac.gov/chapters/Jun07_Ch07.pdf on 27 December 2012.
- 44.Fairbrother G, Siegel MJ, Friedman S, Kory PD, Butts GC. Impact of financial incentives on documented immunization rates in the inner city: results of a randomized controlled trial. Ambul Pediatr. 2001;1:206–212. doi: 10.1367/1539-4409(2001)001<0206:iofiod>2.0.co;2. [PMID: 11888402] [DOI] [PubMed] [Google Scholar]
- 45.Kouides RW, Bennett NM, Lewis B, Cappuccio JD, Barker WH, LaForce FM. Performance-based physician reimbursement and influenza immunization rates in the elderly. The Primary-Care Physicians of Monroe County. Am J Prev Med. 1998;14:89–95. doi: 10.1016/s0749-3797(97)00028-7. [PMID: 9631159] [DOI] [PubMed] [Google Scholar]
- 46.Agency for Healthcare Research and Quality. National Quality Measures Clearinghouse. doi: 10.1080/15360280802537332. Accessed at www.qualitymeasures.ahrq.gov/index.aspx on 6 November 2012. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.