Abstract
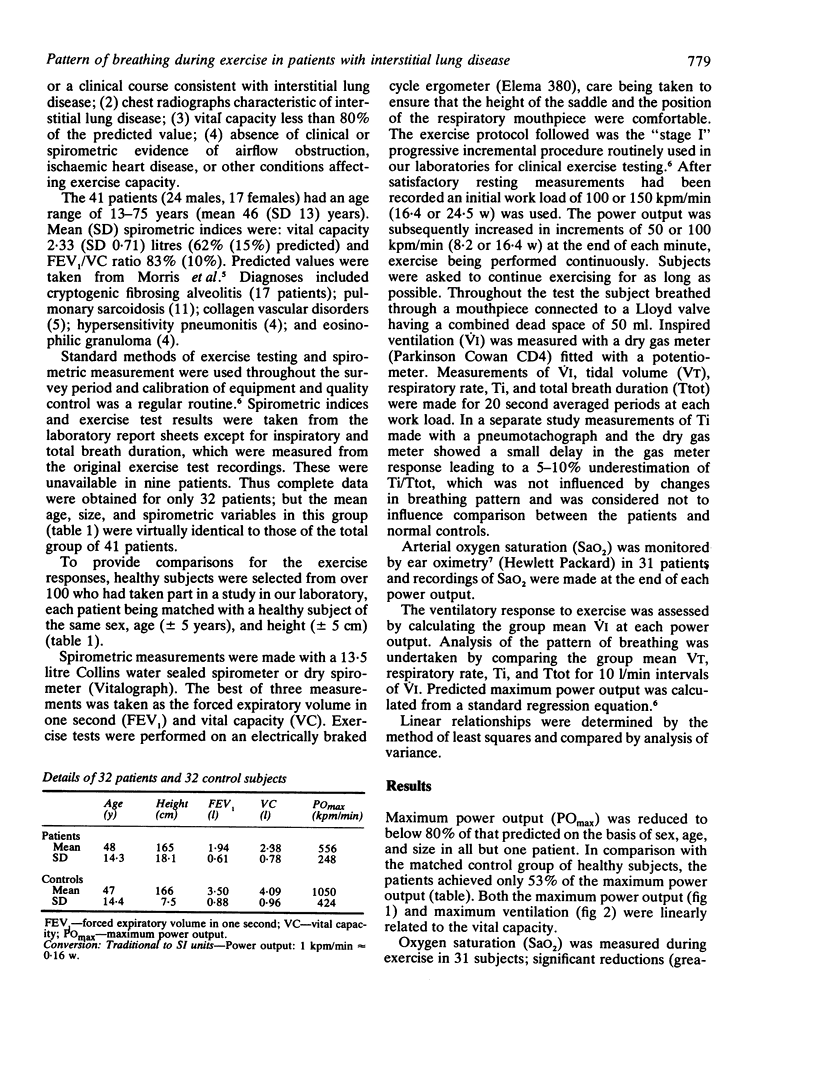
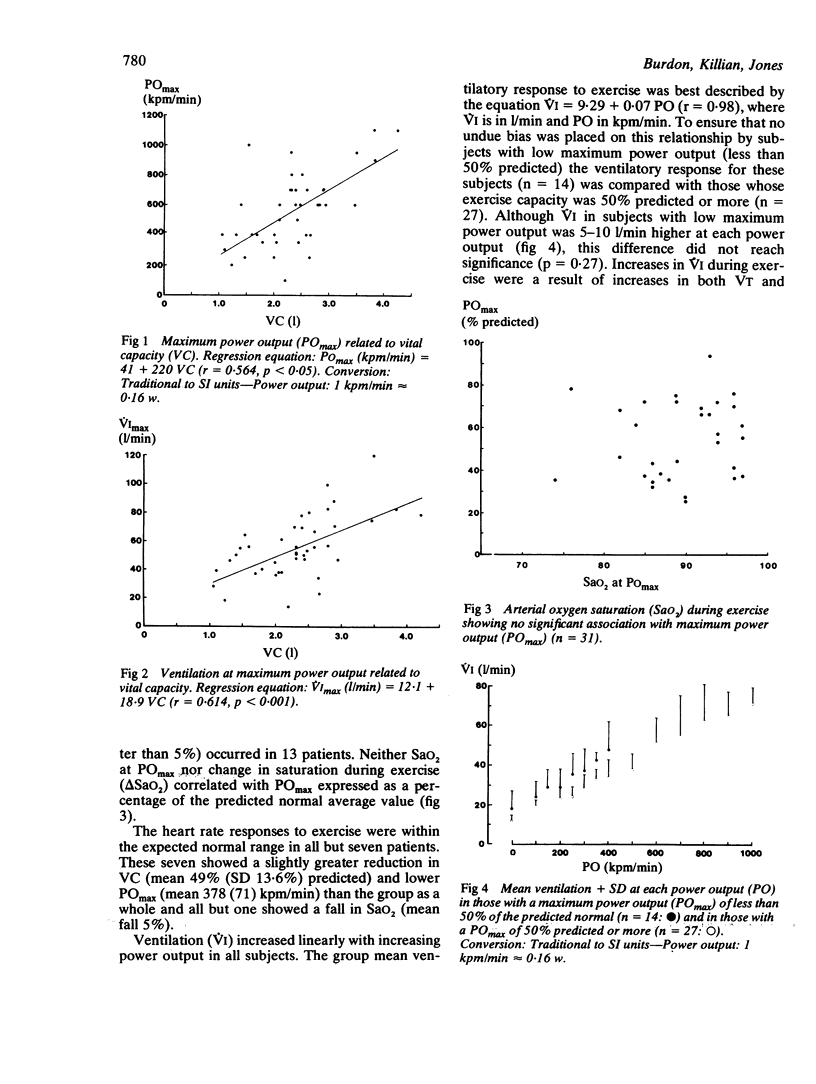
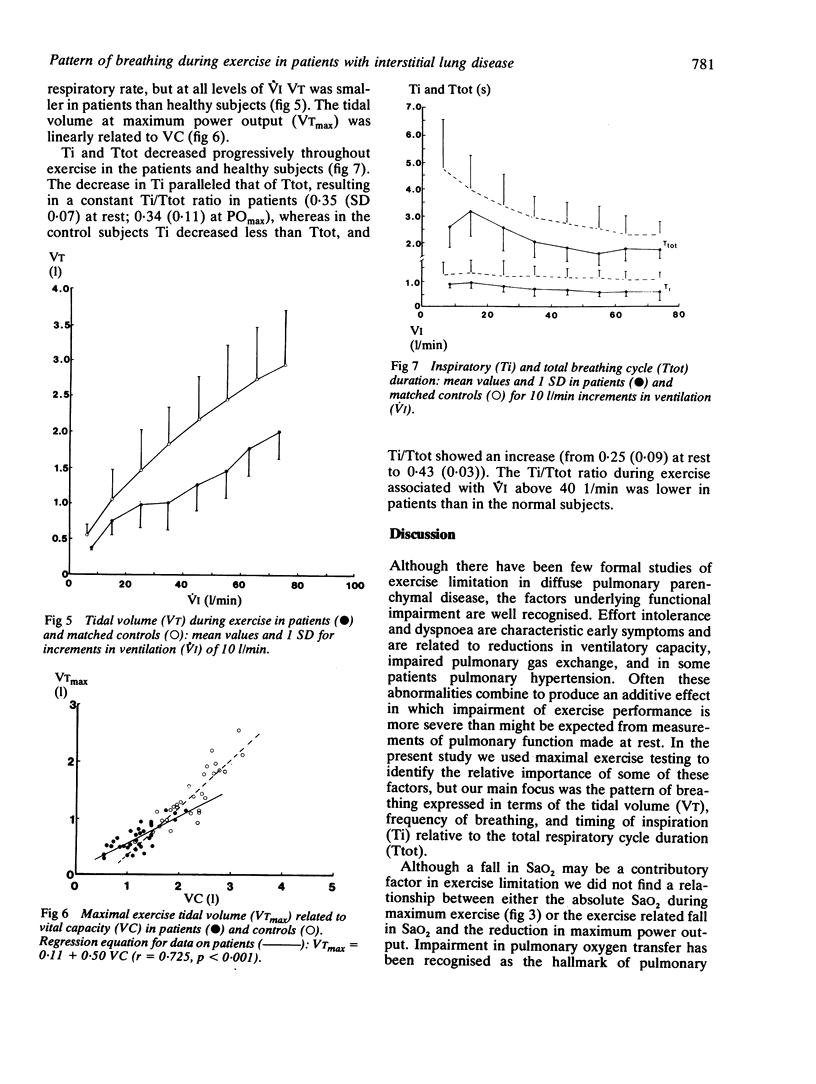
The responses to exercise were studied in 41 patients with pulmonary fibrosis, in whom vital capacity (VC) was reduced to 62% of predicted normal values. Maximum power output (POmax) was 53% predicted; there was a significant relationship between POmax and VC (r = 0.564). The maximum ventilation achieved during exercise was also related to VC (r = 0.614). Although arterial oxygen saturation (SaO2) fell by more than 5% in 13 of 31 patients, there was no relationship between either SaO2 at POmax or the exercise related fall in SaO2 and POmax. Heart rate responses were higher than normal predicted values in seven patients, all of whom showed a low POmax (36% predicted); this finding was due only in part to a fall in SaO2. The ventilatory response to exercise was within normal limits for the patients as a whole; those subjects with the lowest POmax showed relatively higher ventilatory responses to exercise but the difference was not significant. The pattern and timing of breathing was studied in 32 patients and compared with control subjects matched by sex, age, and size. Tidal volume (VT) was low in the patients; maximum VT was related to VC (r = 0.761), but at low values of VC VTmax was higher than in healthy subjects with comparable VC. The total breathing cycle time (Ttot) fell with progressive exercise in patients and controls; Ttot for a given ventilation was shorter in the patients. Inspiratory time (Ti) was shorter in patients than controls, as was Ti/Ttot. In most patients with diffuse pulmonary fibrosis exercise is limited by a reduced ventilatory capacity, despite the adoption of a short Ti and high inspiratory flow rate, both of which serve to optimise tidal volume and breathing frequency and presumably reduce both the force developed by inspiratory muscles and the sensation of breathlessness.
Full text
PDF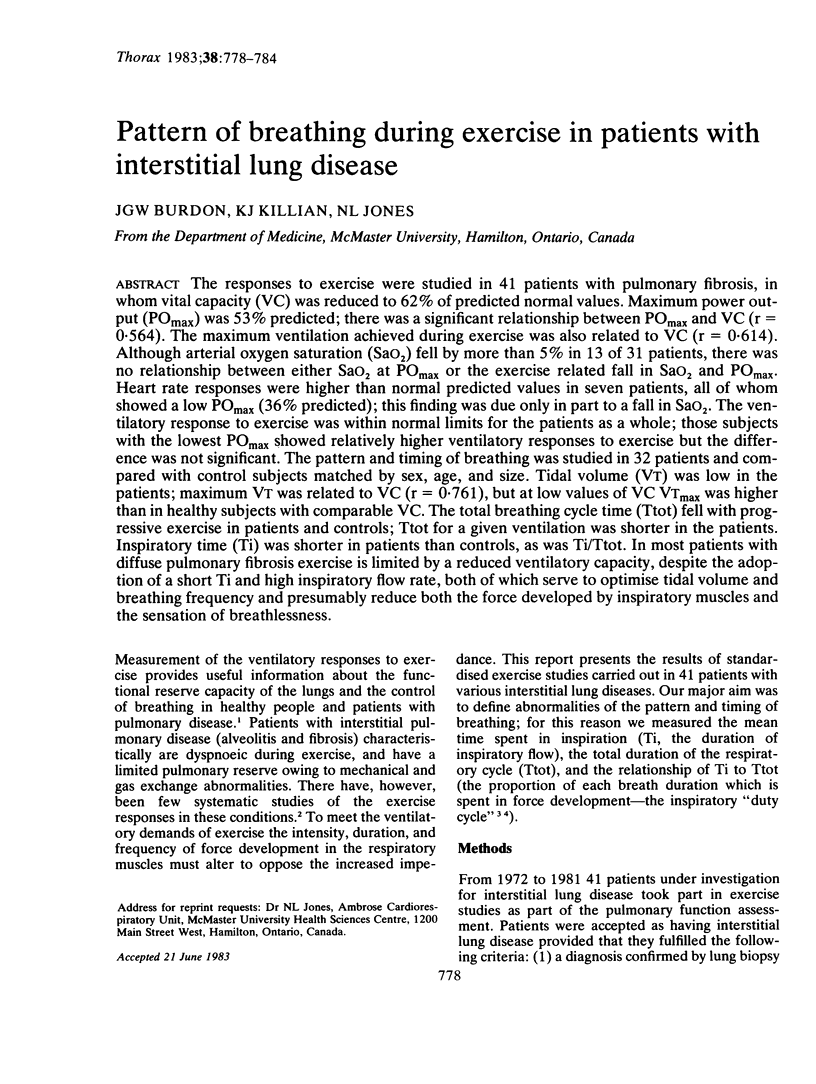
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- AUSTRIAN R., McCLEMENT J. H., RENZETTI A. D., Jr, DONALD K. W., RILEY R. L., COURNAND A. Clinical and physiologic features of some types of pulmonary diseases with impairment of alveolar-capillary diffusion; the syndrome of "alveolar-capillary block". Am J Med. 1951 Dec;11(6):667–685. doi: 10.1016/0002-9343(51)90019-8. [DOI] [PubMed] [Google Scholar]
- Agostoni E., D'Angelo E., Piolini M. Breathing pattern in men during inspiratory elastic loads. Respir Physiol. 1978 Aug;34(2):279–293. doi: 10.1016/0034-5687(78)90034-8. [DOI] [PubMed] [Google Scholar]
- Bland S., Lazerou L., Dyck G., Cherniack R. M. The influence of the "chest wall" on respiratory rate and depth. Respir Physiol. 1967 Aug;3(1):47–54. doi: 10.1016/0034-5687(67)90023-0. [DOI] [PubMed] [Google Scholar]
- Bradley G. W., Crawford R. Regulation of breathing during exercise in normal subjects and in chronic lung disease. Clin Sci Mol Med. 1976 Dec;51(6):575–582. doi: 10.1042/cs0510575. [DOI] [PubMed] [Google Scholar]
- Burdon J. G., Killian K. J., Campbell E. J. Effect of ventilatory drive on the perceived magnitude of added loads to breathing. J Appl Physiol Respir Environ Exerc Physiol. 1982 Oct;53(4):901–907. doi: 10.1152/jappl.1982.53.4.901. [DOI] [PubMed] [Google Scholar]
- Clark F. J., von Euler C. On the regulation of depth and rate of breathing. J Physiol. 1972 Apr;222(2):267–295. doi: 10.1113/jphysiol.1972.sp009797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibson G. J., Pride N. B. Pulmonary mechanics in fibrosing alveolitis: the effects of lung shrinkage. Am Rev Respir Dis. 1977 Oct;116(4):637–647. doi: 10.1164/arrd.1977.116.4.637. [DOI] [PubMed] [Google Scholar]
- Hey E. N., Lloyd B. B., Cunningham D. J., Jukes M. G., Bolton D. P. Effects of various respiratory stimuli on the depth and frequency of breathing in man. Respir Physiol. 1966;1(2):193–205. doi: 10.1016/0034-5687(66)90016-8. [DOI] [PubMed] [Google Scholar]
- Hey E. N., Lloyd B. B., Cunningham D. J., Jukes M. G., Bolton D. P. Effects of various respiratory stimuli on the depth and frequency of breathing in man. Respir Physiol. 1966;1(2):193–205. doi: 10.1016/0034-5687(66)90016-8. [DOI] [PubMed] [Google Scholar]
- Jones N. L. New tests to asses lung function. Exercise tesing in pulmonary evaluation: clinical applications. N Engl J Med. 1975 Sep 25;293(13):647–650. doi: 10.1056/NEJM197509252931308. [DOI] [PubMed] [Google Scholar]
- Jones N. L., Rebuck A. S. Tidal volume during exercise in patients with diffuse fibrosing alveolitis. Bull Eur Physiopathol Respir. 1979 Mar-Apr;15(2):321–328. [PubMed] [Google Scholar]
- Kaltreider N. L., McCann W. S. RESPIRATORY RESPONSE DURING EXERCISE IN PULMONARY FIBROSIS AND EMPHYSEMA. J Clin Invest. 1937 Jan;16(1):23–40. doi: 10.1172/JCI100836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Killian K. J., Bucens D. D., Campbell E. J. Effect of breathing patterns on the perceived magnitude of added loads to breathing. J Appl Physiol Respir Environ Exerc Physiol. 1982 Mar;52(3):578–584. doi: 10.1152/jappl.1982.52.3.578. [DOI] [PubMed] [Google Scholar]
- LOURENCO R. V., TURINO G. M., DAVIDSON L. A., FISHMAN A. P. THE REGULATION OF VENTILATION IN DIFFUSE PULMONARY FIBROSIS. Am J Med. 1965 Feb;38:199–216. doi: 10.1016/0002-9343(65)90174-9. [DOI] [PubMed] [Google Scholar]
- Margaria C. E., Iscoe S., Pengelly L. D., Couture J., Don H., Milic-Emili J. Immediate ventilatory response to elastic loads and positive pressure in man. Respir Physiol. 1973 Sep;18(3):347–369. doi: 10.1016/0034-5687(73)90098-4. [DOI] [PubMed] [Google Scholar]
- Morris J. F., Koski A., Johnson L. C. Spirometric standards for healthy nonsmoking adults. Am Rev Respir Dis. 1971 Jan;103(1):57–67. doi: 10.1164/arrd.1971.103.1.57. [DOI] [PubMed] [Google Scholar]
- OTIS A. B., FENN W. O., RAHN H. Mechanics of breathing in man. J Appl Physiol. 1950 May;2(11):592–607. doi: 10.1152/jappl.1950.2.11.592. [DOI] [PubMed] [Google Scholar]
- Patton J. M., Freedman S. The ventilatory response to CO 2 of patients with diffuse pulmonary infiltrations or fibrosis. Clin Sci. 1972 Jul;43(1):55–69. doi: 10.1042/cs0430055. [DOI] [PubMed] [Google Scholar]
- Pope H., Holloway R., Campbell E. J. The effects of elastic and resistive loading of inspiration on the breathing of conscious man. Respir Physiol. 1968 May;4(3):363–372. doi: 10.1016/0034-5687(68)90041-8. [DOI] [PubMed] [Google Scholar]
- Roussos C. S., Macklem P. T. Diaphragmatic fatigue in man. J Appl Physiol Respir Environ Exerc Physiol. 1977 Aug;43(2):189–197. doi: 10.1152/jappl.1977.43.2.189. [DOI] [PubMed] [Google Scholar]
- STAUB N. C. Alveolar-arterial oxygen tension gradient due to diffusion. J Appl Physiol. 1963 Jul;18:673–680. doi: 10.1152/jappl.1963.18.4.673. [DOI] [PubMed] [Google Scholar]
- Saunders N. A., Powles A. C., Rebuck A. S. Ear oximetry: accuracy and practicability in the assessment of arterial oxygenation. Am Rev Respir Dis. 1976 Jun;113(6):745–749. doi: 10.1164/arrd.1976.113.6.745. [DOI] [PubMed] [Google Scholar]
- de Troyer A., Yernault J. C. Inspiratory muscle force in normal subjects and patients with interstitial lung disease. Thorax. 1980 Feb;35(2):92–100. doi: 10.1136/thx.35.2.92. [DOI] [PMC free article] [PubMed] [Google Scholar]


