Abstract
Background
Cardiovascular disease is the leading cause of death in the United States, making improving cardiovascular health a key population health goal. As part of efforts to achieve this, the American Heart Association has developed the first comprehensive cardiovascular health index (CVHI). Our objective was to investigate the changes in CVHI in US states from 2003 to 2011.
Methods and Results
CVHI was examined using Behavioral Risk Factor Surveillance System data between 2003 and 2011 (odd-numbered years). Total CVHI decreased from 3.73±0.01 in 2003 to 3.65±0.01 in 2009. The majority of states (88%) experienced a decline in CVHI and an increase in the prevalence of “poor” CVHI between 2003 and 2009. Among CVHI components, the highest prevalence of “ideal” was observed for blood glucose followed by smoking, whereas the lowest prevalence of “ideal” was observed for physical activity and diet. Between 2003 and 2009, prevalence of “ideal” smoking and diet status increased, while “ideal” prevalence of blood pressure, cholesterol, blood glucose, body mass index, and physical activity status decreased. We observed statistically significant differences between 2009 and 2011, outside the scope of the 2003–2009 trend, which we hypothesize are partially attributable to differences in sample demographic characteristics related to changes in Behavioral Risk Factor Surveillance System methodology.
Conclusions
Overall, CVHI decreased, most likely due to decreases in “ideal” blood pressure, body mass index, and cholesterol status, which may stem from low prevalence of “ideal” physical activity and diet status. These findings can be used to inform state-specific strategies and targets to improve cardiovascular health.
Keywords: 2020 Strategic Impact Goals, cardiovascular health, epidemiology, states, trends
In 2009, 83.6 million American adults had cardiovascular disease (CVD) and there was an overall CVD-attributable mortality rate of 235.5 per 100 000.1 At an estimated total cost to the United States of $315.4 billion, CVD presents a larger economic burden than any other disease.1 Despite advances in treatment and decreases in risk factors including smoking,2 CVD remains the cause of 1 in 3 deaths.1 Both the prevalence and cost of CVD are expected to increase over the coming decades3 due to an aging population and projected increases in obesity and diabetes, moderated by only limited improvements in diet and physical activity.4,5 These concerns place an emphasis on primordial prevention, where public health efforts, including policy measures, target younger age groups to prevent risk factor formation, thus decreasing the likelihood of CVD and CVD-related mortality later in life.6,7
The American Heart Association’s 2020 Strategic Impact Goals3 and Healthy People 2020 objectives8 both emphasize the improvement of cardiovascular health as a priority. To this end, the American Heart Association recently developed a comprehensive measure of cardiovascular health for use in individuals and populations. This cardiovascular health index (CVHI) incorporates biological health (total cholesterol, blood pressure, body mass index (BMI), and fasting plasma glucose) and behavioral (smoking, physical activity, and diet) factors.3 The CVHI is presented as a total aggregate score ranging from 0 to 7 and as a classification of “poor”, “intermediate”, or “ideal” based on the status of components.
Prevalence of cardiovascular health, as measured with CVHI, has been examined in various populations globally9–12 and within the United States in both adults13–17 and adolescents.18 “Ideal” CVHI is associated with decreased CVD17,19,20 and decreased risk of death.7,21 “Ideal” CVHI during childhood has been associated with “ideal” levels of blood pressure, total cholesterol, and glucose later in life.22 Studies have also reported that increased CVHI is associated with decreased unhealthy vascular changes,23–27 decreased symptoms of depression,28 increased cognitive functioning,29 and decreased incident cancer.30
Two studies have examined temporal changes in CVHI and its components in the United States.4,21 Both reported improvement in smoking behavior, declines in “ideal” BMI and blood glucose levels, and no change in “ideal” cholesterol, blood pressure, or physical activity. Whereas Yang et al reported no changes in “ideal” diet, Huffman et al reported a slight improvement in diet in men but not in women.
While geographic disparities in CVD and stroke are recognized, with the southeastern United States having the highest all-cause and CVD-specific mortality rates in the nation,1,31–33 only 1 study has examined state-based differences in CVHI.34 Currently, no studies have examined geographic differences in CVHI over time. The objective of this study was to investigate the change in CVHI in US states from 2003 to 2011 using Behavioral Risk Factor Surveillance System (BRFSS) data. A secondary objective emerged during analysis, based on observations of substantial differences between 2009 and 2011; thus, we also report results of this subanalysis.
Methods
CVHI and its individual components were examined across the United States and then stratified by demographic characteristics and state. Time trends for each state were determined with a time variable (BRFSS study year) using Poisson regression for total CVHI and logistic regression for individual CVHI components. All models were adjusted for socioeconomic and demographic covariates.
Data Source
BRFSS is an annually administered national telephone survey collecting information in each US state on health risk behaviors, chronic health conditions, and use of preventive services.35 State health departments, with support from the Centers for Disease Control and Prevention, use random-digit dialing to interview adults 18 years of age and older who are part of the civilian, non-institutionalized population. Detailed descriptions of the BRFSS study design and methods are available elsewhere.35 Only odd years and core component questions were included in this study, a limitation necessitated by the availability of data for all CVHI components.
Study Population
All respondents of the 2003, 2005, 2007, 2009, and 2011 BRFSS surveys not living in Guam, Puerto Rico, or the Virgin Islands were examined to determine eligibility (n=1 953 902) for this study. Ineligible participants included those missing any information necessary to calculate the CVHI (n=563 734), and females if pregnant or of unknown pregnancy status (n=8643). The final, eligible study population was 1 381 525 individuals.
Calculation of CVHI
We applied the adapted methodology from Fang et al34 to determine CVHI using self-report BRFSS data. CVHI consists of 7 components: blood pressure, cholesterol, blood glucose, BMI, smoking behavior, physical activity, and diet. Definitions used to determine an individual’s status for each component are outlined in Table1. The nature of BRFSS questions (self-reported “yes” or “no”) for hypertension, high cholesterol, and diabetes does not allow for the determination of the “intermediate” category for these factors. For consistency, all other CVHI components were also classified as either “ideal” or “not ideal.”
Table 1.
BRFSS Questions and Definitions for Classification of “Ideal” for CVHI Individual Components
| CVHI Component | Definition of “Ideal” | BRFSS Questions From 2003, 2005, 2007, and 2009 | BRFSS Questions 2011 |
|---|---|---|---|
| Blood pressure | Participant had never been told by a health professional they had high blood pressure | Have you ever been told by a doctor, nurse, or other health professional that you have high blood pressure? | |
| Cholesterol | Participant had previously had their cholesterol screened and never been told by a health professional they had high cholesterol | Blood cholesterol is a fatty substance reported in the blood. Have you ever had your blood cholesterol checked?
|
|
| Glucose | Participant had never been told by a doctor they had diabetes | Have you ever been told by a doctor that you have diabetes? | |
| BMI | BMI was between 18.5 and 24.9 | About how much do you weigh without shoes?
|
|
| Smoking status | Participant had not smoked at least 100 cigarettes in their lifetime or reported smoking 100 cigarettes in their lifetime but not currently smoking | Have you smoked at least 100 cigarettes in your entire life?
|
|
| About how long has it been since you last smoked cigarettes regularly, that is, daily? | |||
| Physical activity | Participant did enough moderate or vigorous physical activity to meet the recommendation of ≥150 minutes a week of moderate-intensity activity, ≥75 minutes of vigorous-intensity activity, or an equivalent combination of physical activity | Now, thinking about the moderate physical activities you do in a usual week, do you do moderate activities for at least 10 minutes at a time, such as brisk walking, bicycling, vacuuming, gardening, or anything else that caused small increases in breathing or heart rate? How many days per week do you do these moderate activities for at least 10 minutes at a time? On days when you do moderate activities for at least 10 minutes at a time, how much total time per day do you spend doing these activities? Now, thinking about the vigorous physical activities you do in a usual week, do you do vigorous activities for at least 10 minutes at a time, such as running, aerobics, heavy yard work, or anything else that caused large increases in breathing or heart rate? How many days per week do you do these vigorous activities for at least 10 minutes at a time? On days when you do vigorous activities for at least 10 minutes at a time, how much total time per day do you spend doing these activities? |
During the past 30 days, other than your regular job, did you participate in any physical activities or exercise such as running, calisthenics, golf, gardening, or walking for exercise? How many times per week or per month did you take part in this activity during the past month? And when you took part in this activity, for how many minutes or hours did you usually keep at it? Estimated Activity Intensity for First Activity (Calculated by BRFSS) How many times per week or per month did you take part in this activity during the past month? And when you took part in this activity, for how many minutes or hours did you usually keep at it? Estimated Activity Intensity for Second Activity (Calculated by BRFSS) |
| Diet | Participant consumed 5 or more servings of fruits and vegetables per day | Not counting juice, how often do you eat fruit? How often do you eat green salad? How often do you eat potatoes not including french fries, fried potatoes, or potato chips? How often do you eat carrots? Not counting carrots, potatoes, or salad, how many servings of vegetables do you usually eat? |
During the past month, not counting juice, how many times per day, week, or month did you eat fruit? Count fresh, frozen, or canned fruit. During the past month, how many times per day, week, or month did you eat orange-colored vegetables such as sweet potatoes, pumpkin, winter squash, or carrots? During the past month, how many times per day, week, or month did you eat dark green vegetables, for example, broccoli or dark leafy greens including romaine, chard, collard greens, or spinach? Not counting what you just told me about, during the past month, about how many times per day, week, or month did you eat OTHER vegetables? |
BMI indicates body mass index; BRFSS, Behavioral Risk Factor Surveillance System; CVHI, cardiovascular health index.
Total CVHI was the total number of factors categorized as “ideal” and ranged from 0 to 7. Overall, CVHI was considered “ideal” if a participant was categorized as “ideal” for 6 or 7 individual factors, “intermediate” for 3 to 5 factors, and “poor” for 2 or fewer factors.
BRFSS was modified between 2009 and 2011,35,36 both in methodology (cellular phone numbers were added to the sampling frame) and question content (of relevance to this study, both diet and physical activity questions). Our adaptation to the CVHI scoring methodology for 2011 is outlined in Table1.
Independent Variables
Based on the study question, the key independent variables were the year in which the participant completed the BRFSS survey and state, as identified by the Federal Information Processing Standards (FIPS) code. Additional covariates included age, sex, race/ethnicity (Non-Hispanic White, Non-Hispanic Black, Hispanic, and Other), and level of education (Less than High School, High School, and Some College). Income was considered as a covariate, but was not included due to the high percentage of missing observations in BRFSS (13.8%). A secondary analysis found that, while income was significantly associated with CVHI, it did not alter the relationships between CVHI and other covariates, or substantially attenuate the magnitude of the associations.
Statistical Analysis
Population demographic characteristics were estimated using weighted means and percentages of each covariate for each BRFSS year. Differences in demographic characteristics were tested using a Pearson χ2. Age-standardized mean CVHI and prevalence of “ideal” status for each component were determined for the entire United States and each state using the 2000 US projected population distribution weight, which utilized the age groups 18 to 24 years, 25 to 44 years, 45 to 64 years, and ≥65 years.37 Estimates for the entire United States were not adjusted for state. As there was a statistically significant interaction between state and time (P<0.0001), subsequent analyses were stratified by state. Poisson regression was used for analyses in which total CVHI was the dependent variable; logistic regression was used for analyses in which individual CVHI components were the dependent variables. Using methods similar to Yang et al,21 we assessed time trends for each state by including a time variable corresponding to the BRFSS study year. Linear trends were assessed using contrast statements that applied the Christoffel-Darboux recurrence formula for computing orthogonal polynomial contrasts.38 Differences in total CVHI and individual CVHI components between 2003 and 2009 and 2009 and 2011 were calculated; the Wald test was used to assess for significant differences. For each state, we plotted the change in total CVHI versus change in the prevalence of “poor” CVHI between 2003 and 2009.
To assess the impact of the 2009 BRFSS change in smoking behavior questions, we conducted a sensitivity analysis to determine whether differences between 2011 and 2009 smoking behavior were related to the change in question definition. Using both definitions, 2009 and 2011 smoking behavior were determined and Pearson’s χ2 tests were used to determine significance between years.
All analyses were performed using survey procedures to account for survey weights and design. All models were adjusted by sex, age, race/ethnicity, and education. Stata Statistical Software: Release 13 (College Station, TX: StataCorp LP) was used for all statistical analyses. Maps were made using ArcGIS 10.2 (ArcGIS Desktop: Release 10.1; Redlands, CA: Environmental Systems Research Institute).
This study was approved as non–human subjects research by the West Virginia University Institutional Review Board.
Results
Demographic characteristics of the eligible and noneligible study populations are described in Table2. There were significant differences between eligible and noneligible populations for all demographic variables. The noneligible population was younger, more likely to be male, be from a minority race/ethnicity, and have less than a college education. Both eligible and noneligible populations changed across years similarly, with populations in later years being older, more likely to be from a minority race/ethnicity, and have a higher level of education.
Table 2.
Characteristics of BRFSS Eligible and Noneligible Study Populations Stratified by Study Year
| 2003 | 2005 | 2007 | 2009 | 2011 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Eligible | Noneligible | Eligible | Noneligible | Eligible | Noneligible | Eligible | Noneligible | Eligible | Noneligible | P Value | |
| N | 176 931 | 87 753 | 244 962 | 111 150 | 307 205 | 123 707 | 310 768 | 121 839 | 341 659 | 164 808 | |
| Age (mean±SE) | 49.6±0.08 | 38.1±0.10 | 50.0±0.07 | 37.7±0.10 | 50.2±0.07 | 38.5±0.10 | 50.4±0.07 | 39.0±0.10 | 51.1±0.06 | 39.1±0.08 | †‡§ |
| Male, n (%*) | 70 065 (48.0) | 34 334 (48.9) | 93 956 (47.9) | 42 245 (49.5) | 114 592 (48.0) | 46 159 (49.8) | 117 829 (47.9) | 46 132 (50.0) | 133 161 (47.8) | 65 651 (50.1) | † |
| Race/ethnicity, n (%*) | †‡§ | ||||||||||
| Non-Hispanic white | 147 643 (75.8) | 61 589 (62.6) | 205 220 (76.0) | 77 754 (59.8) | 257 053 (74.9) | 86 279 (59.4) | 258 923 (74.1) | 85 006 (59.1) | 276 605 (72.5) | 114 463 (59.5) | |
| Non-Hispanic black | 12 977 (9.8) | 8322 (10.4) | 17 823 (9.5) | 10 722 (10.3) | 22 603 (9.6) | 11 589 (10.4) | 23 680 (10.4) | 11 973 (10.9) | 27 295 (11.2) | 13 318 (11.8) | |
| Hispanic | 8008 (9.6) | 11 644 (20.7) | 10 188 (9.6) | 15 351 (24.2) | 13 718 (9.8) | 17 592 (23.7) | 14 155 (10.4) | 15 920 (23.3) | 16 947 (11.0) | 21 771 (22.2) | |
| Other | 7317 (4.8) | 5386 (6.3) | 10 100 (4.9) | 6036 (5.7) | 11 781 (5.8) | 6847 (6.5) | 11 785 (5.1) | 7236 (6.8) | 11 899 (5.3) | 9043 (6.5) | |
| Education, n (%*) | †‡§ | ||||||||||
| Less than High School | 16 759 (9.7) | 12 438 (16.8) | 21 855 (9.1) | 16 347 (18.4) | 26 830 (8.6) | 18 034 (16.9) | 24 750 (8.1) | 16 323 (15.7) | 26 244 (12.4) | 20 179 (20.0) | |
| High School | 52 020 (29.0) | 28 613 (32.9) | 72 821 (28.3) | 37 009 (33.0) | 90 982 (27.0) | 40 651 (32.2) | 90 098 (26.5) | 65 303 (31.2) | 98 142 (28.4) | 51 245 (30.5) | |
| Some College | 107 932 (61.3) | 46 277 (50.3) | 149 968 (62.6) | 57 204 (48.7) | 188 997 (64.5) | 64 151 (50.9) | 195 540 (65.5) | 65 303 (53.1) | 216 775 (59.3) | 91 953 (49.6) | |
Participants were noneligible if missing any responses needed to calculate CVHI; females with a positive or unknown pregnancy status; and those living in Puerto Rico, Guam, or US Virgin Islands. BRFSS indicates Behavioral Risk Factor Surveillance System; CVHI, cardiovascular health index.
Percentages are weighted frequencies using survey procedures.
Significance at the P=0.05 level for the comparison of eligible vs noneligible across years.
Significance at the P=0.05 level for the comparison of eligible across years.
Significance at the P=0.05 level for the comparison of noneligible across 2003–2009.
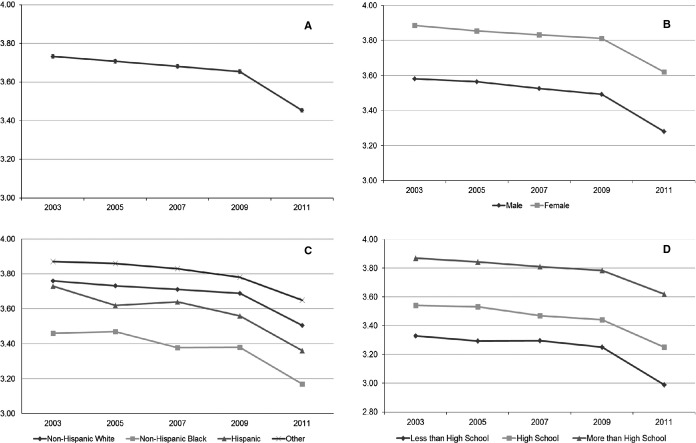
Age-standardized mean CVHI for years 2003–2011 are shown in Figure1. CVHI was 3.73±0.01 for 2003 and declined in each subsequent year (3.71±0.01, 3.68±0.01, 3.65±0.01, and 3.45±0.01, respectively). Age-standardized mean CVHI and CVHI stratified by demographic characteristics are also shown in Figure1. There were disparities in CVHI within each demographic variable, as assessed by interactions. Females had higher CVHI (in 2009) than males in 2009 (3.81±0.007 versus 3.49±0.008, respectively) and in every subsequent study year (P=0.0096). Within race/ethnic groups, the “Other” race/ethnicity category had the highest CVHI, followed by non-Hispanic whites, Hispanic, and non-Hispanic blacks (in 2009: 3.78±0.02, 3.69±0.006, 3.56±0.02, and 3.38±0.02, respectively; P=0.0034). Within educational strata, those with some college had the highest CVHI and those with less than a high school education had the lowest (in 2009: 3.78±0.006 versus 3.25±0.02, respectively; P<0.0001).
Figure 1.
Age-standardized mean cardiovascular health index (CVHI) for 2003–2011. (A) Overall CVHI; (B) Overall CVHI stratified by sex; (C) Overall CVHI stratified by race/ethnicity; (D) Overall CVHI stratified by education level.
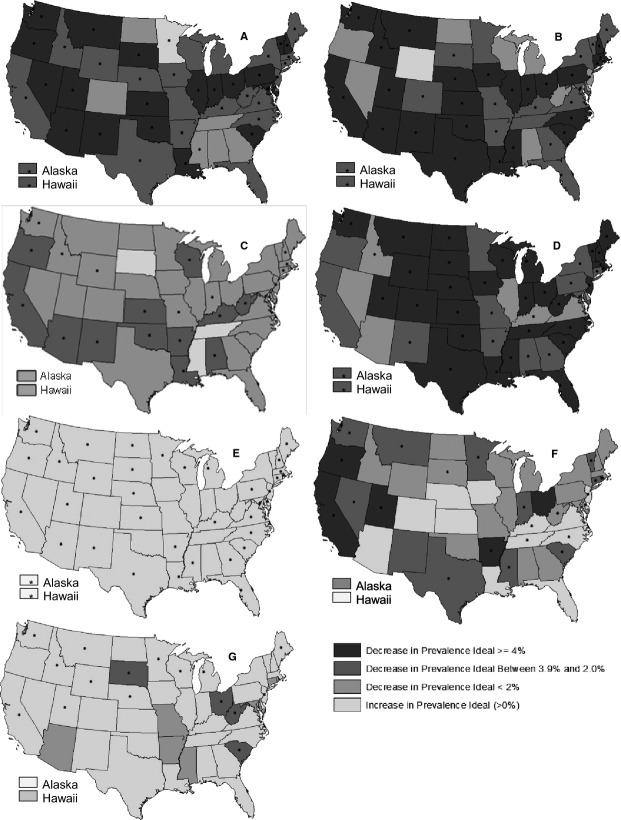
Disparities in CVHI were also observed between individual states (interaction P<0.0001) and are shown in Figure2. In 2009, CVHI ranged from a high of 3.87±0.05 in Colorado to a low of 3.37±0.05 in Mississippi. States in the South Central and South Atlantic regions had the lowest CVHI and states in the Northeast, Pacific, and Mountain regions had the highest CVHI. Results of linear trend tests (2003–2009) for each state, presented in Table S1, demonstrated a significant decreasing linear trend in all but 9 states (Delaware, DC, Connecticut, Massachusetts, Michigan, Nevada, Tennessee, Wisconsin, Wyoming; trend not statistically significant).
Figure 2.
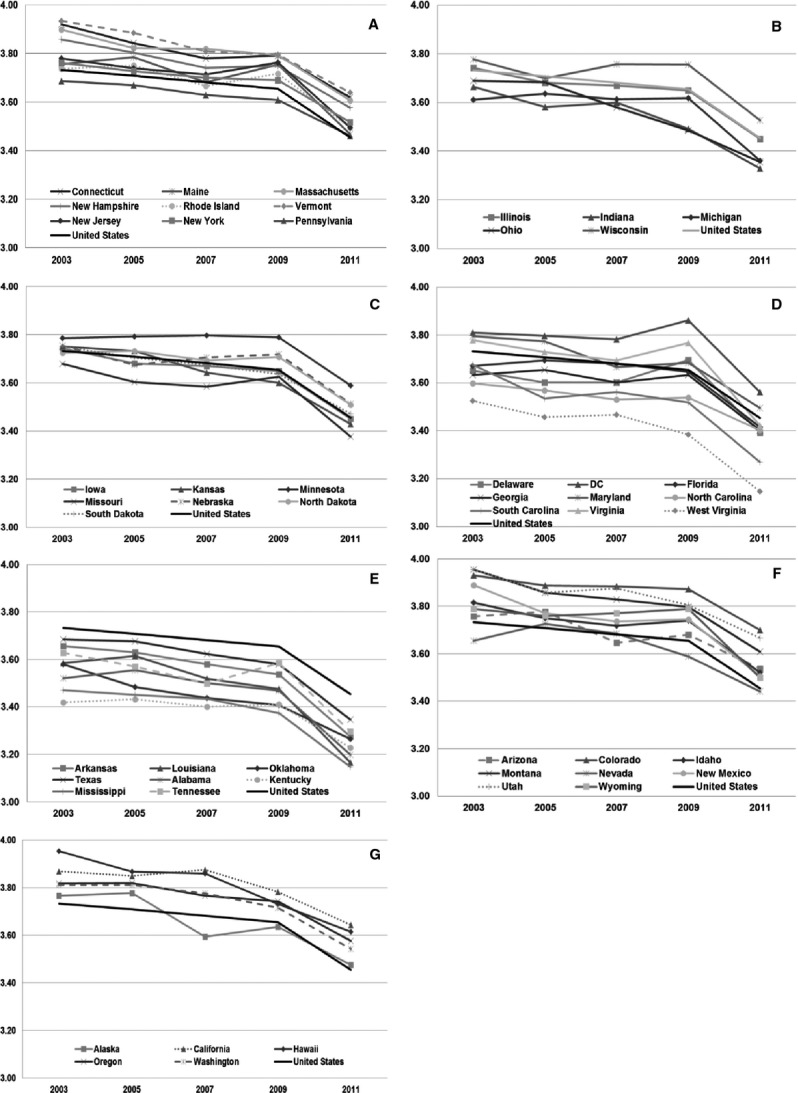
Age-standardized mean cardiovascular health index stratified by US state and presented by Census Division, 2003–2011: (A) Northeast; (B) East North Central; (C) West North Central; (D) South Atlantic; (E) South Central; (F) Mountain; and (G) Pacific.
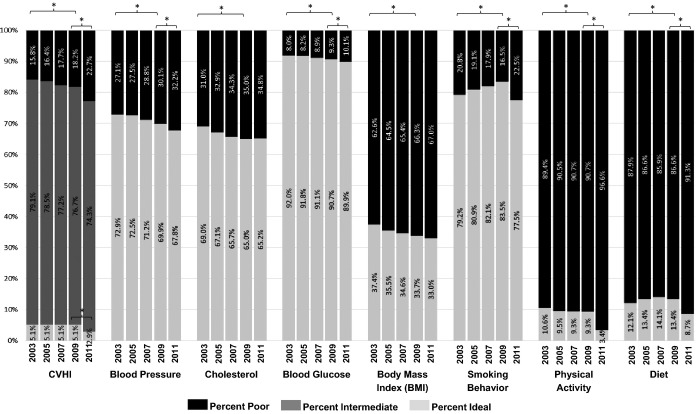
The prevalence of “ideal,” “intermediate,” or “poor” overall CVHI, and “ideal” or “poor” status for individual CVHI components are reported in Figure3. The prevalence of “ideal” CVHI has remained constant at 5.1%; however, the prevalence of “poor” CVHI was significantly higher in 2009 compared to 2003. Blood glucose and smoking were the components with the highest prevalence of “ideal” CVHI. Prevalence of “ideal” smoking status increased from 79.2% to 83.5% between 2003 and 2009. Diet and physical activity were the components with the lowest prevalence of “ideal.” Prevalence of “ideal” diet increased from 12.1% to 13.4% between 2003 and 2009, whereas prevalence of “ideal” status for all other components (blood pressure, cholesterol, blood glucose, physical activity) decreased. Differences outside of these trends were seen for smoking and diet status between 2009 and 2011, which correspond to 2011 BRFSS methodological changes (discussed further below).
Figure 3.
Age-adjusted prevalence estimates for “poor,” “intermediate,” and “ideal” overall cardiovascular health index (CVHI) and the prevalence of “poor” and “ideal” for each CVHI individual component, 2003–2011. *P<0.05 for Pearson χ2 test between 2009 and 2011 or 2003 and 2009.
Figure4 summarizes the state-level changes between 2003 and 2009 for each individual CVHI component. While 1 state (Minnesota) had an increase in the prevalence of “ideal” blood pressure (Figure4A), no state experienced a significant increase in the prevalence of “ideal” cholesterol, while most states had a decrease in the prevalence of “ideal” cholesterol status (Figure4B). Furthermore, no state experienced an increase in the prevalence of “ideal” BMI, though 86% of states experienced a decrease in the prevalence of “ideal” BMI greater than 4 percentage points (Figure4D). All states experienced no change or an increase in the prevalence of “ideal” smoking status, which ranged from a 2.1% increase in Utah to an increase of 11.9% in Alaska (Figure4E). Six percent of states experienced increases in the prevalence of “ideal” physical activity, though 74% experienced decreases in “ideal” physical activity (Figure4F). All states experienced an increase or no change in the prevalence of “ideal” diet, except 4 states, which experienced decreases in “ideal” diet status (Figure4G).
Figure 4.
Absolute change in the prevalence of “ideal” status for each cardiovascular health index individual component, 2003–2009 (calculated as % “ideal” in 2009—% “ideal” in 2003); (A) blood pressure, (B) cholesterol, (C) blood glucose, (D) body mass index, (E) smoking behavior, (F) physical activity, and (G) diet. *P<0.05 for Pearson χ2 comparing 2003 and 2009 values.
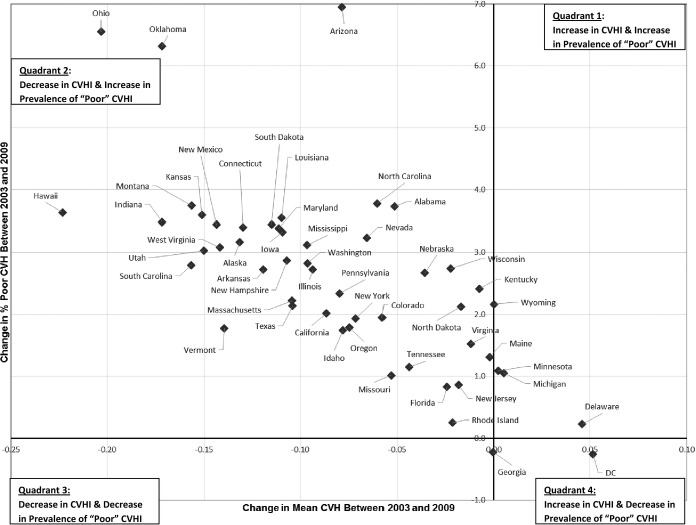
To provide information that could enable priority setting and decision making for states, state-specific changes in age-standardized mean CVHI compared to the state’s change in the prevalence of “poor” CVHI between 2003 and 2009 are presented in Figure5. States were assigned to 1 of 4 quadrants which, from most to least preferable, are: Quadrant 4 (improved mean CVHI and reduced prevalence of “poor” CVHI); Quadrant 1 and Quadrant 3 (mixed results suggesting a change in the distribution of CVHI); and Quadrant 2 (decreased mean CVHI and increased prevalence of “poor” CVHI). Quadrant 4 contains only 1 state, the District of Columbia; there are no states in Quadrant 3 and only a few in Quadrant 1. The substantial majority of states (88%) are in Quadrant 2, indicating that these states had both a decline in mean CVHI and an increase in the prevalence of “poor” CVHI between 2003 and 2009. From visual inspection, the 4 states with the largest deterioration in CVHI during the study period were Hawaii, Ohio, Oklahoma, and Arizona.
Figure 5.
Change in a state’s age-standardized mean cardiovascular health index (CVHI) (2003–2009) compared to the change in a state’s prevalence of “poor” CVHI, 2003–2009.
Subanalysis Assessing the Impact of Methodological Changes in BRFSS Between 2009 and 2011
We observed statistically significant differences in the demographic characteristics and outcome variables between 2009 and 2011 that were outside of the scope of the trend observed between 2003 through 2009. In visual examination of Figure1, there is a decreasing trend from 2003 to 2011 but a larger decrease between 2009 and 2011 than between any adjacent years. This larger-than-expected drop between 2009 and 2011 is significant for mean CVHI as well as all individual CVHI components except cholesterol and BMI (Figure3). As reported in Figure3, between 2003 and 2009 the prevalence of “poor” CVHI and prevalence of “ideal” for each CVHI component were both significantly different. As reported in Table3, with the exception of cholesterol and BMI, these same individual CVHI components were significantly different between 2009 and 2011. Further, comparing the absolute differences in CVHI between 2003 and 2009 with 2009 and 2011, the magnitude of the 1-year change for total CVHI and 3 out of 7 individual CVHI components (2009–2011) was larger than the 6-year changes (2003–2009).
Table 3.
Summary of Differences in Overall CVHI and CVHI Individual Components, 2009 Versus 2011
| United States Overall | Average for States | |||||||
|---|---|---|---|---|---|---|---|---|
| Difference 2003 to 2009 | Difference 2009 to 2011 | |||||||
| Difference 2003 to 2009 | Difference 2009 to 2011 | * | * | |||||
| Mean overall CVHI | −0.08 | <0.0001 | −0.20 | <0.0001 | −0.08 | 74.5 (38/51) | −0.21 | 98.0 (50/51) |
| % “Poor” CVHI | 2.4 | <0.0001 | 4.5 | <0.0001 | 2.6 | 84.3 (43/51) | 4.6 | 92.3 (47/51) |
| % “Ideal” CVHI | 0.0 | 0.12 | −2.1 | <0.0001 | 0.004 | 9.8 (5/51) | −2.1 | 90.2 (46/51) |
| % “Ideal” blood pressure | −3.0 | <0.0001 | −2.1 | <0.0001 | −3.4 | 80.4 (41/51) | −2.1 | 39.2 (20/51) |
| % “Ideal” cholesterol | −4.1 | <0.0001 | 0.3 | 0.83 | −4.0 | 78.4 (40/51) | 0.08 | 17.6 (9/51) |
| % “Ideal” blood glucose | −1.3 | <0.0001 | −0.8 | 0.0002 | −1.2 | 43.1 (22/51) | −1.1 | 19.6 (10/51) |
| % “Ideal” BMI | −3.7 | <0.0001 | −0.7 | 0.18 | −4.0 | 84.3 (43/51) | −0.9 | 5.9 (3/51) |
| % “Ideal” smoking behavior | 4.4 | <0.0001 | −6.0 | <0.0001 | 4.6 | 74.5 (38/51) | −6.7 | 90.2 (46/51) |
| % “Ideal” physical activity | −1.3 | <0.0001 | −5.9 | <0.0001 | −1.1 | 45.1 (23/51) | −5.7 | 98.0 (50/51) |
| % “Ideal” diet | 1.3 | <0.0001 | −4.7 | <0.0001 | 1.0 | 31.4 (16/51) | −4.3 | 94.1 (48/51) |
BMI indicates body mass index; CVHI, cardiovascular health index.
Percentage of states that have a significant difference between the 2 years.
Upon further evaluation, we observed that the eligible population in 2011 was significantly older, had a greater percentage of non-Hispanic blacks and Hispanics, and a higher percentage of individuals with a high school or less education compared to those in previous BRFSS years. Sensitivity analysis for changing smoking behavior definitions showed that no matter which combination of definitions were used, there was significantly lower “ideal” smoking behavior between 2009 and 2011 (Table4). The change between the years ranged from 2.3 to 6 percentage points.
Table 4.
Sensitivity Analysis Comparing Changes in Smoking Behavior Definitions Over the Change in Behavioral Risk Factor Surveillance System Sampling and Weighting, 2009–2011
| Percent of Population With “Ideal” Smoking Behavior | 2009 Versus 2011 | |
|---|---|---|
| 2009 results using 2003–2009 definition | 83.5 | <0.0001 |
| 2011 results using 2011 definition | 77.5 | |
| 2009 results using 2003–2009 definition | 83.5 | <0.0001 |
| 2011 results using 2003–2009 definition | 81.2 | |
| 2009 results using 2011 definition | 81.3 | <0.0001 |
| 2011 results using 2011 definition | 77.5 |
Discussion
This is the first study to evaluate temporal state-level trends in the United States. Results demonstrated a linear decrease in CVHI between 2003 and 2009 in both the United States overall and in most individual states. We also observed differences in overall CVHI and its individual components between 2009 and 2011, which we partially, but only partially, attribute to methodological changes in BRFSS.
Our estimated of prevalence of “ideal” CVHI, 5.1%, is higher than previous National Health and Nutrition Examination Surveys (NHANES) studies of CVHI, which have reported prevalence estimates closer to 1%.13,21 Differences in these prevalence estimates may be attributable to methodologic differences between BRFSS and NHANES. All BRFSS results are self-report, whereas CVHI can be determined using lab values in studies using NHANES. Additionally, participants with undiagnosed hypertension, diabetes, and hypercholesterolemia would be misclassified as “ideal” in the BRFSS adaptation of the CVHI determination. Furthermore, self-report of height and weight is known to be biased39 and may have resulted in an overestimation of “ideal” BMI. Finally, diet questions used in the NHANES studies include more varied questions, while BRFSS questions are more limited, which may have resulted in an overestimation of “ideal” diet status. However, NHANES does not allow for the examination of temporal trends at the state level, which is a distinct advantage of using BRFSS.
We observed an increase in the prevalence of “poor” CVHI from 15.8% (2003) to 18.2% (2009). This represents an additional 7 million individuals with an increased risk of CVD and all-cause mortality. Prevalence of “ideal” CVHI is low and did not change between 2003 and 2009. Our estimate of “poor” CVHI for 2009, 18.2%, is higher than that reported by Fang et al, a study that also used BRFSS and that reported 11.4% prevalence of “poor” CVHI.34 Different exclusion criteria may explain the higher prevalence of “poor” CVHI reported here.
We observed significant disparities in CVHI within demographic groups and between states. Women, those with higher levels of education, and those identifying as Other race/ethnicity had the highest levels of CVHI. While a few states have made strides in CVHI improvement, 47 states are at high risk of continuing their decreasing trend in CVHI. In particular, Ohio, Arizona, Oklahoma, and Hawaii were observed to have had the largest declines in CVHI.
Much of the decreasing trend in CVHI between 2003 and 2009 is likely due to decreases in “ideal” blood pressure, cholesterol, and BMI. The decreases in these factors were only slightly tempered by increases in “ideal” smoking status. The prevalence of “ideal” diet increased in many states, while the prevalence of “ideal” physical activity decreased or did not change in most states. The simultaneous improvement in diet but decrease in the prevalence of “ideal” cholesterol may be attributed to an increased overall consumption of food, both fruits and vegetables as well as unhealthy options, increased diagnosis of hypercholesterolemia, or lower cut-off levels for the initiation of statins. There may also be a lag time, where a change in diet is noted before any substantial changes in cholesterol levels are seen. In addition, the threshold for the amount of change in diet needed to produce a noticeable change in cholesterol levels may not have been met in this population. Smoking, diet, and physical activity are not only risk factors themselves, but contribute to the development of the biological CVHI components. These should be a main target of public health efforts as well as local, state, and national policies. The continuing decline in the prevalence of “ideal” blood pressure is also a major contributor to the burden of disease and health care costs.
The overall trends in smoking, BMI, and blood glucose reported here are consistent with previously reported national trend data using NHANES.4,21 Whereas here we report a decreasing trend in “ideal” blood pressure, cholesterol, and physical activity, Huffman et al and Yang et al reported no changes in these individual CVHI components. We observed increases in the prevalence of “ideal” diet, which is consistent with findings in men reported by Huffman et al. Differences in the data source, sample size, and years of data examined could explain these differences in observed trends, as Yang et al and Huffman et al examined a much larger time span using data at time points averaged over many years as a strategy to increase sample size. Huffman et al predicted that, by 2020, overall CVHI will improve by 6%.4 While this projected improvement is shy of the American Heart Association 2020 Strategic Impact goal of a 20% improvement in cardiovascular health, the implications of our findings suggest that, with only improvements in smoking and diet status, it is unlikely that either the 6% improvement or the 20% improvement (Strategic Impact Goal) will be met.
Assessing Impact of Methodological Changes in BRFSS Between 2009 and 2011
Changes to BRFSS questions and sampling and weighting procedures starting in 2011 have resulted in cautions from the Centers for Disease Control and Prevention regarding interpretation and comparability of 2011 data versus previous years.36 As BRFSS data are one of the only sources states have to monitor health,39 we aimed to assess the differences in overall CVHI and its individual components between 2009 and 2011. Changes between 2009 and 2011 are larger than changes seen in the previous 6-year period for overall CVHI and the prevalence of all individual components except the prevalence of “ideal” BMI and cholesterol, which demonstrated no change.
It was expected that, while the magnitude of changes between previous years and 2011 would be different, the overall shape and slope of the trend would not change.36 Our findings support this initial change, particularly for the prevalence of “ideal” smoking and diet status. Changes in the prevalence of “ideal” smoking status were significant even after examining changes in the BRFSS questions used to define “ideal” smoking status (Table1). Future time points will need to be assessed to determine whether the shape and slope of the trend will continue.
Between 2009 and 2011, the changes observed in the prevalence of “ideal” diet and physical activity status may be partially due to changes in questions for those individual CVHI components (Table1) as well as to changes in the demographic characteristics resulting from changes in the survey sampling and weighting procedures. Specifically, cell phone numbers were included in the sampling frame for the first time, which was expected to increase respondents in lower income, lower education, and younger ages, as these are demographic groups more likely to use cell phones exclusively.36 While our observations are consistent with the expected changes in education, our observation of a slightly older average age in 2011 versus 2009 (51.1 and 50.4 years old, respectively) was different from a priori expectations. Changes to the weighting procedures in 2011 allowed for the addition of more demographic variables, including education level, marital status, and home ownership, to the weighting calculation. These changes, while increasing the accuracy of the weighting scheme, may also have contributed to the changes in the demographic characteristics of the sample and, subsequently, the differences in CVHI.
Strengths and Limitations
The key strength of this study is its use of BRFSS, which is a large, nationally representative sample, available for multiple years, and which allows for stratification and analysis at the state level. The primary limitation of this study is the self-report methodology of BRFSS which, as discussed above, may result in an overestimation of “ideal” CVHI. However, in a comparison of 3 major health surveys (NHANES, National Health and Nutrition Examination Survey, and BRFSS), Li et al reported that estimated prevalence rates for chronic diseases in BRFSS were comparable to that of NHANES and National Health Interview Survey and those for hypertension showed only small differences between all 3 surveys40 Similarly, Pierannunzi et al also reported the validity and reliability of BRFSS to be comparable to other surveys, with differences limited primarily to physical measure questions due to the self-reported nature of BRFSS.39 Finally, there is possible bias in this study resulting from the proportion of BRFSS respondents ineligible for this study due to missing data (≈30%). Ineligible younger individuals would be more likely to have “ideal” CVHI, whereas ineligible less educated and male individuals would be more likely to have poorer CVHI.
Conclusions
Understanding cardiovascular health patterns and its determinants in populations allows for primordial prevention and health-supporting approaches to be initiated before individuals or communities develop disease or risk factors. While the decrease in cardiovascular disease attributable deaths has been ascribed to both treatment advances and risk factor modification,2 it is important to consider that, with either risk factor modification or early risk factor treatment, morbidity can be decreased or compressed into the latest years.41,42 In conclusion, this study provides trends in CVHI and its components both nationwide and for each individual US state. This information can be used to inform state-specific strategies that will be most effective in improving overall cardiovascular health. Future research into the causes of changes in CHVI may inform policies and interventions that can improve population health.
Acknowledgments
The authors wish to thank Dr D. Leann Long from the West Virginia University School of Public Health for her very helpful statistical advice during this study.
Sources of Funding
This study was supported in part by the West Virginia Stroke CoBRE from the National Institutes of Health, National Institute of General Medical Sciences (NIGMS) grant P20GM109098 (J.W. Simpkins, PI; S.J. Frisbee Sub-Project PI).
Disclosures
None.
Supporting Information
Table S1. Age-Standardized Mean Overall CVHI and Percent of Population With “poor” and “ideal” CVHI Stratified by State and Year, 2003–2011
References
- Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Blaha MJ, Dai S, Ford ES, Fox CS, Franco S. Heart disease and stroke statistics—2014 update: a report from the American Heart Association. Circulation. 2014;129:399–410. doi: 10.1161/01.cir.0000442015.53336.12. [DOI] [PubMed] [Google Scholar]
- Ford ES, Ajani UA, Croft JB, Critchley JA, Labarthe DR, Kottke TE, Giles WH, Capewell S. Explaining the decrease in US deaths from coronary disease, 1980–2000. N Engl J Med. 2007;356:2388–2398. doi: 10.1056/NEJMsa053935. [DOI] [PubMed] [Google Scholar]
- Lloyd-Jones DM, Hong Y, Labarthe D, Mozaffarian D, Appel LJ, Van Horn L, Greenlund K, Daniels S, Nichol G, Tomaselli GF. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association’s Strategic Impact Goal through 2020 and beyond. Circulation. 2010;121:586–613. doi: 10.1161/CIRCULATIONAHA.109.192703. [DOI] [PubMed] [Google Scholar]
- Huffman MD, Capewell S, Ning H, Shay CM, Ford ES, Lloyd-Jones DM. Cardiovascular health behavior and health factor changes (1988–2008) and projections to 2020: results from the National Health and Nutrition Examination Surveys (NHANES) Circulation. 2012;125:2595–2602. doi: 10.1161/CIRCULATIONAHA.111.070722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heidenreich PA, Trogdon JG, Khavjou OA, Butler J, Dracup K, Ezekowitz MD, Finkelstein EA, Hong Y, Johnston SC, Khera A. Forecasting the future of cardiovascular disease in the United States: a policy statement from the American Heart Association. Circulation. 2011;123:933–944. doi: 10.1161/CIR.0b013e31820a55f5. [DOI] [PubMed] [Google Scholar]
- Lloyd-Jones DM, Leip EP, Larson MG, D’Agostino RB, Beiser A, Wilson PW, Wolf PA, Levy D. Prediction of lifetime risk for cardiovascular disease by risk factor burden at 50 years of age. Circulation. 2006;113:791–798. doi: 10.1161/CIRCULATIONAHA.105.548206. [DOI] [PubMed] [Google Scholar]
- Ford ES, Greenlund KJ, Hong Y. Ideal cardiovascular health and mortality from all causes and diseases of the circulatory system among adults in the United States. Circulation. 2012;125:987–995. doi: 10.1161/CIRCULATIONAHA.111.049122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. 2013. Healthy People 2020 heart disease and stroke objectives. [DOI] [PubMed]
- Wu H-Y, Sun Z-H, Cao D-P, Wu L-X, Zeng Q. Cardiovascular health status in Chinese adults in urban areas: analysis of the Chinese Health Examination Database 2010. Int J Cardiol. 2012;168:760–764. doi: 10.1016/j.ijcard.2012.09.235. [DOI] [PubMed] [Google Scholar]
- Zeng Q, Dong S-Y, Song Z-Y, Zheng Y-S, Wu H-Y, Mao L-N. Ideal cardiovascular health in Chinese urban population. Int J Cardiol. 2012;167:2311–2317. doi: 10.1016/j.ijcard.2012.06.022. [DOI] [PubMed] [Google Scholar]
- Lee H-J, Suh B, Yoo T-G, Lee H, Shin DW. Trends in cardiovascular health metrics among Korean adults. Korean J Fam Med. 2013;34:403–412. doi: 10.4082/kjfm.2013.34.6.403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Del Brutto OH, Mera RM, Montalván M, Del Brutto VJ, Zambrano M, Santamaría M, Tettamanti D. Cardiovascular health status and metabolic syndrome in Ecuadorian natives/Mestizos aged 40 years or more with and without stroke and ischemic heart disease—an Atahualpa Project case–control nested study. J Stroke Cerebrovasc Dis. 2013;23:643–648. doi: 10.1016/j.jstrokecerebrovasdis.2013.06.001. [DOI] [PubMed] [Google Scholar]
- Shay CM, Ning H, Allen NB, Carnethon MR, Chiuve SE, Greenlund KJ, Daviglus ML, Lloyd-Jones DM. Status of Cardiovascular Health in US Adults Prevalence Estimates From the National Health and Nutrition Examination Surveys (NHANES) 2003–2008. Circulation. 2012;125:45–56. doi: 10.1161/CIRCULATIONAHA.111.035733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bostean G, Roberts CK, Crespi CM, Prelip M, Peters A, Belin TR, McCarthy WJ. Cardiovascular health: associations with race–ethnicity, nativity, and education in a diverse, population-based sample of Californians. Ann Epidemiol. 2013;23:388–394. doi: 10.1016/j.annepidem.2013.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim JI, Sillah A, Boucher JL, Sidebottom AC, Knickelbine T. Prevalence of the American Heart Association’s “ideal cardiovascular health” metrics in a rural, cross-sectional, community-based study: the Heart of New Ulm Project. J Am Heart Assoc. 2013;2:e000058. doi: 10.1161/JAHA.113.000058. doi: 10.1161/JAHA.113.000058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bambs C, Kip KE, Dinga A, Mulukutla SR, Aiyer AN, Reis SE. Low prevalence of “ideal cardiovascular health” in a community-based population. The Heart Strategies Concentrating on Risk Evaluation (Heart SCORE) study. Circulation. 2011;123:850–857. doi: 10.1161/CIRCULATIONAHA.110.980151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Folsom AR, Yatsuya H, Nettleton JA, Lutsey PL, Cushman M, Rosamond WD. Community prevalence of ideal cardiovascular health, by the American Heart Association definition, and relationship with cardiovascular disease incidence. J Am Coll Cardiol. 2011;57:1690–1696. doi: 10.1016/j.jacc.2010.11.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shay CM, Ning H, Daniels SR, Rooks CR, Gidding SS, Lloyd-Jones DM. Status of cardiovascular health in US adolescents: prevalence estimates from the National Health and Nutrition Examination Surveys (NHANES) 2005–2010. Circulation. 2013;127:1369–1376. doi: 10.1161/CIRCULATIONAHA.113.001559. [DOI] [PubMed] [Google Scholar]
- Dong C, Rundek T, Wright CB, Anwar Z, Elkind MS, Sacco RL. Ideal cardiovascular health predicts lower risks of myocardial infarction, stroke, and vascular death across whites, blacks, and hispanics: the northern Manhattan study. Circulation. 2012;125:2975–2984. doi: 10.1161/CIRCULATIONAHA.111.081083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu S, Huang Z, Yang X, Zhou Y, Wang A, Chen L, Zhao H, Ruan C, Wu Y, Xin A. Prevalence of ideal cardiovascular health and its relationship with the 4-year cardiovascular events in a northern Chinese industrial city. Circ Cardiovasc Qual Outcomes. 2012;5:487–493. doi: 10.1161/CIRCOUTCOMES.111.963694. [DOI] [PubMed] [Google Scholar]
- Yang Q, Cogswell ME, Flanders WD, Hong Y, Zhang Z, Loustalot F, Gillespie C, Merritt R, Hu FB. Trends in cardiovascular health metrics and associations with all-cause and CVD mortality among US adults. JAMA. 2012;307:1273–1283. doi: 10.1001/jama.2012.339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laitinen TT, Pahkala K, Magnussen CG, Viikari JS, Oikonen M, Taittonen L, Mikkilä V, Jokinen E, Hutri-Kähönen N, Laitinen T. Ideal cardiovascular health in childhood and cardiometabolic outcomes in adulthood: the Cardiovascular Risk in Young Finns Study. Circulation. 2012;125:1971–1978. doi: 10.1161/CIRCULATIONAHA.111.073585. [DOI] [PubMed] [Google Scholar]
- Zhang Q, Zhang S, Wang C, Gao X, Zhou Y, Zhou H, Wang A, Wu J, Bian L, Wu S. Ideal cardiovascular health metrics on the prevalence of asymptomatic intracranial artery stenosis: a cross-sectional study. PLoS One. 2013;8:e58923. doi: 10.1371/journal.pone.0058923. doi: 10.1371/journal.pone.0058923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oikonen M, Laitinen TT, Magnussen CG, Steinberger J, Sinaiko AR, Dwyer T, Venn A, Smith KJ, Hutri-Kähönen N, Pahkala K. Ideal cardiovascular health in young adult populations from the United States, Finland, and Australia and its association with CIMT: the International Childhood Cardiovascular Cohort Consortium. J Am Heart Assoc. 2013;2:e00244. doi: 10.1161/JAHA.113.000244. doi: 10.1161/JAHA.113.000244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pahkala K, Hietalampi H, Laitinen TT, Viikari JS, Rönnemaa T, Niinikoski H, Lagström H, Talvia S, Jula A, Heinonen OJ. Ideal cardiovascular health in adolescence: effect of lifestyle intervention and association with vascular intima-media thickness and elasticity (the Special Turku Coronary Risk Factor Intervention Project for Children [STRIP] study) Circulation. 2013;127:2088–2096. doi: 10.1161/CIRCULATIONAHA.112.000761. [DOI] [PubMed] [Google Scholar]
- Alman AC, Maahs DM, Rewers MJ, Snell-Bergeon JK. Ideal cardiovascular health and the prevalence and progression of coronary artery calcification in adults with and without type 1 diabetes. Diabetes Care. 2014;37:521–528. doi: 10.2337/dc13-0997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogagarue ER, Lutsey PL, Klein R, Klein BE, Folsom AR. Association of ideal cardiovascular health metrics and retinal microvascular findings: the Atherosclerosis Risk in Communities Study. J Am Heart Assoc. 2013;2:e000430. doi: 10.1161/JAHA.113.000430. doi: 10.1161/JAHA.113.000430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- España-Romero V, Artero EG, Lee D-C, Sui X, Baruth M, Ruiz JR, Pate RR, Blair SN. A prospective study of ideal cardiovascular health and depressive symptoms. Psychosomatics. 2013;54:525–535. doi: 10.1016/j.psym.2013.06.016. [DOI] [PubMed] [Google Scholar]
- Reis JP, Loria CM, Launer LJ, Sidney S, Liu K, Jacobs DR, Zhu N, Lloyd-Jones DM, He K, Yaffe K. Cardiovascular health through young adulthood and cognitive functioning in midlife. Ann Neurol. 2013;73:170–179. doi: 10.1002/ana.23836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rasmussen-Torvik LJ, Shay CM, Abramson JG, Friedrich CA, Nettleton JA, Prizment AE, Folsom AR. Ideal cardiovascular health is inversely associated with incident cancerclinical perspective. The Atherosclerosis Risk in Communities Study. Circulation. 2013;127:1270–1275. doi: 10.1161/CIRCULATIONAHA.112.001183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Labarthe DR. Epidemiology and Prevention of Cardiovascular Diseases: A Global Challenge. Sudbury, MA: Jones & Bartlett Learning; 2011. [Google Scholar]
- Cooper R, Cutler J, Desvigne-Nickens P, Fortmann SP, Friedman L, Havlik R, Hogelin G, Marler J, McGovern P, Morosco G. Trends and disparities in coronary heart disease, stroke, and other cardiovascular diseases in the United States: findings of the National Conference on Cardiovascular Disease Prevention. Circulation. 2000;102:3137–3147. doi: 10.1161/01.cir.102.25.3137. [DOI] [PubMed] [Google Scholar]
- Mensah GA, Mokdad AH, Ford ES, Greenlund KJ, Croft JB. State of disparities in cardiovascular health in the United States. Circulation. 2005;111:1233–1241. doi: 10.1161/01.CIR.0000158136.76824.04. [DOI] [PubMed] [Google Scholar]
- Fang J, Yang Q, Hong Y, Loustalot F. Status of cardiovascular health among adult Americans in the 50 states and the District of Columbia, 2009. J Am Heart Assoc. 2012;1:e005371. doi: 10.1161/JAHA.112.005371. doi: 10.1161/JAHA.112.005371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. 2014. Behavioral Risk Factor Surveillance System survey data and documentation.
- Centers for Disease Control and Prevention. Methodologic changes in the Behavioral Risk Factor Surveillance System in 2011 and potential effects on prevalence estimates. MMWR Morb Mortal Wkly Rep. 2012;61:410. [PubMed] [Google Scholar]
- Klein RJ, Schoenborn CA. Healthy People 2010 statistical notes: age adjustment using the 2000 projected US population. Healthy People Stat Notes. 2001;20:1–12. [PubMed] [Google Scholar]
- StataCorp. Stata 13 Base Reference Manual: Contrast. College Station, TX: Stata Press; 2013. [Google Scholar]
- Pierannunzi C, Hu SS, Balluz L. A systematic review of publications assessing reliability and validity of the Behavioral Risk Factor Surveillance System (BRFSS), 2004–2011. BMC Med Res Methodol. 2013;13:49. doi: 10.1186/1471-2288-13-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li C, Balluz LS, Ford ES, Okoro CA, Zhao G, Pierannunzi C. A comparison of prevalence estimates for selected health indicators and chronic diseases or conditions from the Behavioral Risk Factor Surveillance System, the National Health Interview Survey, and the National Health and Nutrition Examination Survey, 2007–2008. Prev Med. 2012;54:381–387. doi: 10.1016/j.ypmed.2012.04.003. [DOI] [PubMed] [Google Scholar]
- Jones DS, Greene JA. The contributions of prevention and treatment to the decline in cardiovascular mortality: lessons from a forty-year debate. Health Aff. 2012;31:2250–2258. doi: 10.1377/hlthaff.2011.0639. [DOI] [PubMed] [Google Scholar]
- Fries JF, Bruce B, Chakravarty E. Compression of morbidity 1980–2011: a focused review of paradigms and progress. J Aging Res. 2011;2011:1–10. doi: 10.4061/2011/261702. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Age-Standardized Mean Overall CVHI and Percent of Population With “poor” and “ideal” CVHI Stratified by State and Year, 2003–2011