Abstract
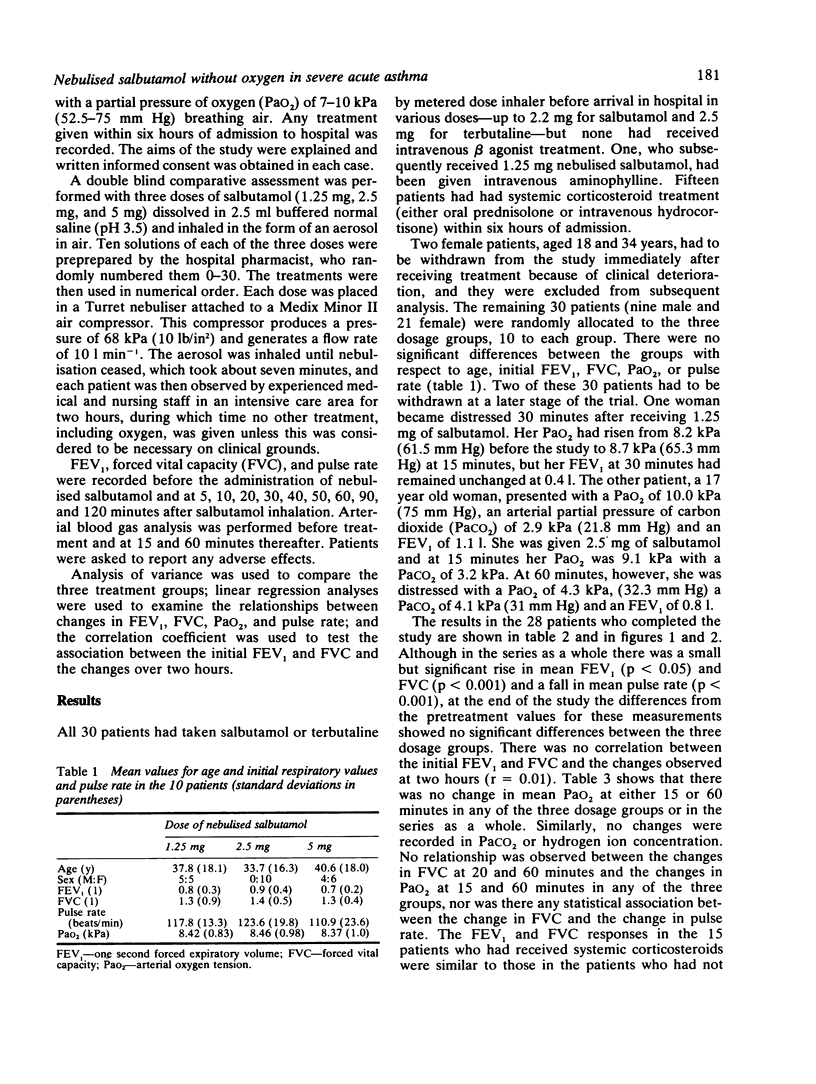
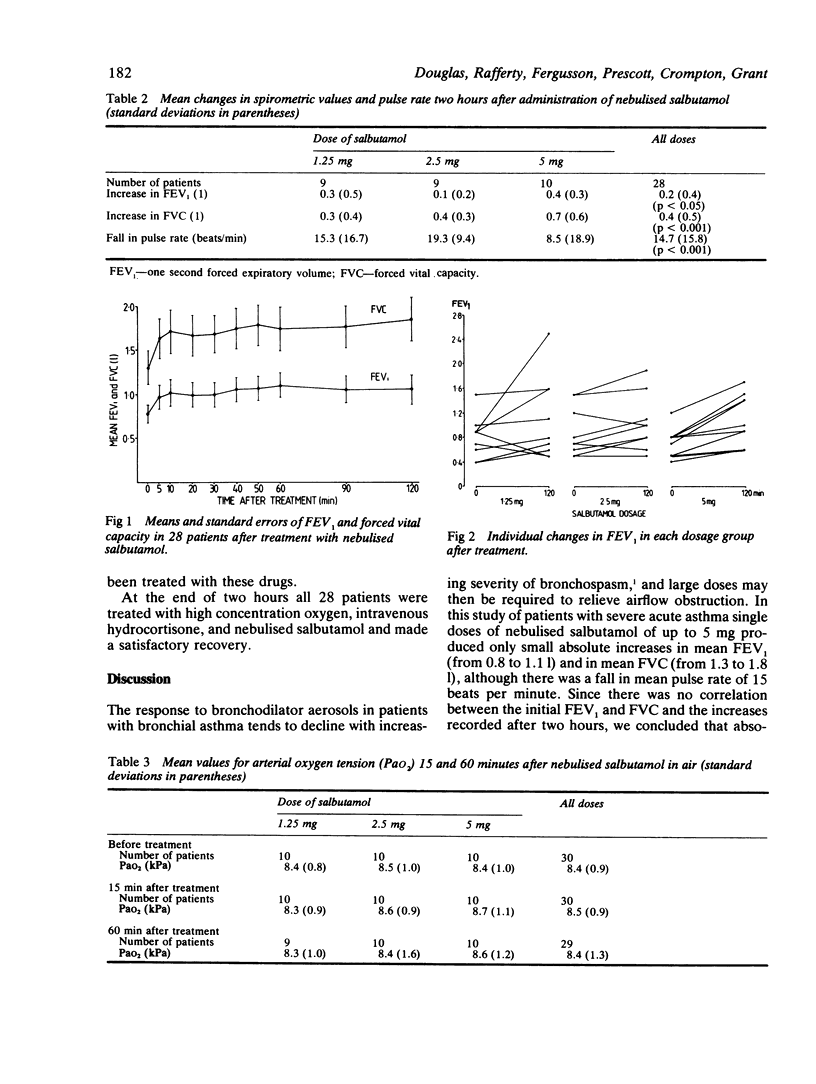
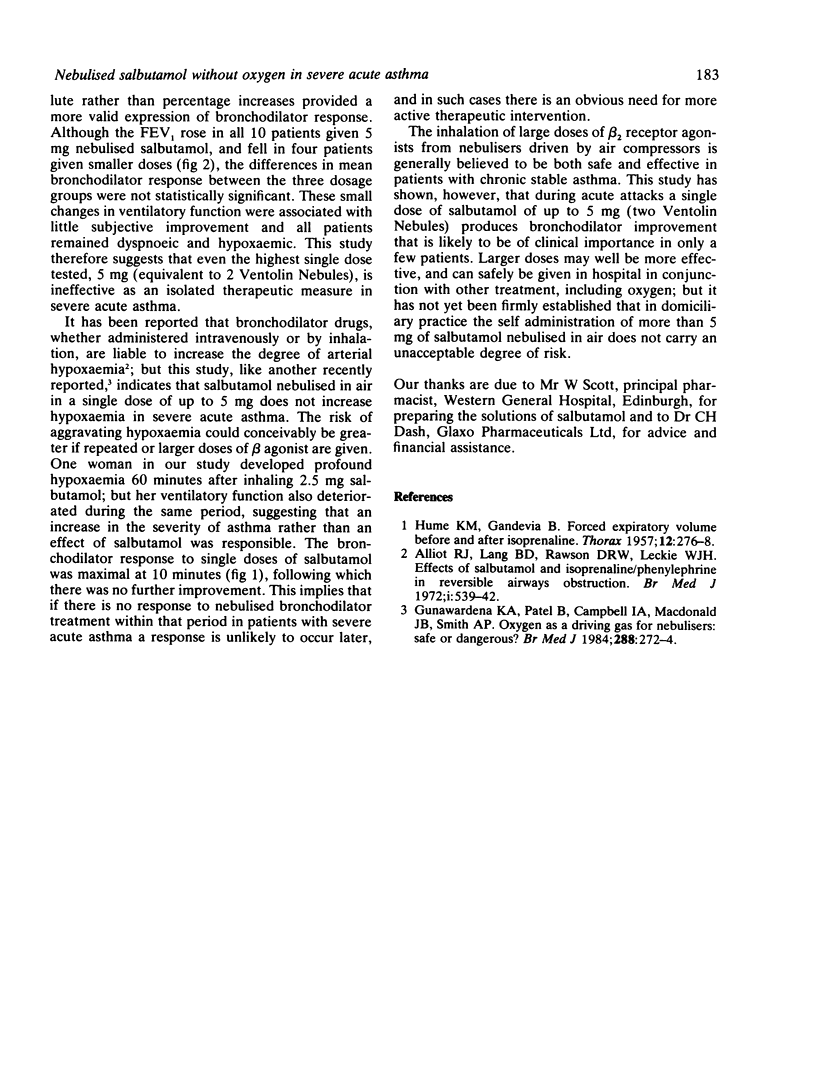
Thirty two patients with severe acute asthma, all of whom were hypoxaemic, entered a double blind comparative assessment of three doses of salbutamol (1.25, 2.5, and 5 mg) nebulised by an electrically operated air compressor. The study lasted for two hours, during which oxygen and corticosteroid treatment were withheld. All patients were observed in an intensive care area during this period. Four patients had to be withdrawn from the study. Two became distressed immediately after receiving salbutamol and were excluded from further analysis. Two other patients were withdrawn, one with persistent respiratory distress and an unchanged one second forced expiratory volume (FEV1) and the other because of the development of profound hypoxaemia and a deteriorating FEV1 within 60 minutes of treatment. No significant differences were observed between the three dosage groups. In the 28 patients completing the study there were only small increases in mean FEV1 (0.8 to 1.1 l) and forced vital capacity (FVC) (1.3 to 1.8 l) over the two hours. There was a fall in the mean pulse rate at 120 minutes of 15 beats per minute (117-102). No significant change in oxygen tension (PaO2) was observed at 15 or 60 minutes after administration of nebulised salbutamol in any of the three groups. Salbutamol nebulised in air, in a single dose of 5 mg, produces only slight relief of airflow obstruction and no worsening of hypoxaemia in severe acute asthma.
Full text
PDF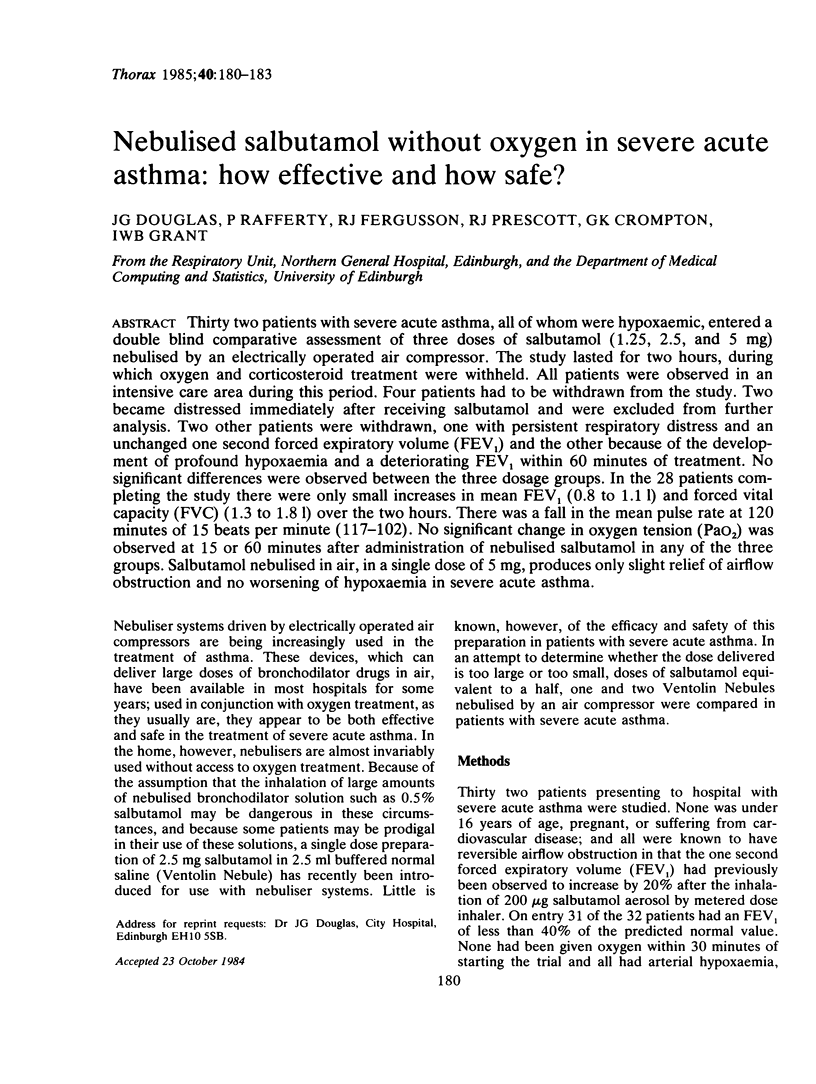
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Alliott R. J., Lang B. D., Rawson D. R., Leckie W. J. Effects of salbutamol and isoprenaline-phenylephrine in reversible airways obstruction. Br Med J. 1972 Feb 26;1(5799):539–542. doi: 10.1136/bmj.1.5799.539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gunawardena K. A., Patel B., Campbell I. A., MacDonald J. B., Smith A. P. Oxygen as a driving gas for nebulisers: safe or dangerous? Br Med J (Clin Res Ed) 1984 Jan 28;288(6413):272–274. doi: 10.1136/bmj.288.6413.272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- HUME K. M., GANDEVIA B. Forced expiratory volume before and after isoprenaline. Thorax. 1957 Sep;12(3):276–278. doi: 10.1136/thx.12.3.276. [DOI] [PMC free article] [PubMed] [Google Scholar]


