Abstract
Francisella tularensis LVS (Live Vaccine Strain) is an attenuated bacterium that has been used as a live vaccine. Patients immunized with this organism show a very long-term memory response (over 30 years post vaccination) evidenced by the presence of indicators of robust cell-mediated immunity. Because F. tularensis LVS is such a potent vaccine, we hypothesized that this organism would be an effective vaccine platform. First, we sought to determine if we could genetically modify this strain to produce protective antigens of a heterologous pathogen. Currently, there is not a licensed vaccine against the important opportunistic bacterial pathogen, Pseudomonas aeruginosa. Because many P. aeruginosa strains are also drug resistant, the need for effective vaccines is magnified. Here, F. tularensis LVS was genetically modified to express surface proteins PilAPa, OprFPa, and FliCPa of P. aeruginosa. Immunization of mice with LVS expressing the recombinant FliCPa led to a significant production of antibodies specific for P. aeruginosa. However, mice that had been immunized with LVS expressing PilAPa or OprFPa did not produce high levels of antibodies specific for P. aerugionsa. Therefore, the recombinant LVS strain engineered to produce FliCPa may be able to provide immune protection against a P. aeruginosa challenge. However for future use of this vaccine platform, selection of the appropriate recombinant antigen is critical as not all recombinant antigens expressed in this strain were immunogenic.
Keywords: flagellum, FliC, Francisella, OprF, PilA, pilus, Pseudomonas, recombinant DNA, vaccine
Introduction
The Francisella tularensis live vaccine strain (LVS) has been used to safely vaccinate millions of people worldwide and thousands of at-risk personnel in the US.1 However, even though this vaccine was used safely for over 50 years, immunization with LVS was discontinued as this vaccine has not been licensed by the FDA due to a number of regulatory issues.2 As many of these issues have been resolved, the LVS vaccine is nearing licensure evidenced by the completion of Phase II clinical trials (ClinicalTrials.gov identifier NCT01150695).3 Patients that had been immunized with F. tularensis LVS prior to this strain being deemed unavailable for human use, exhibited robust, long-term immunological memory (over 30 years post vaccination) indicated by a strong cell-mediated immune response.4 Given the long-term cell-mediated memory responses associated with LVS vaccination, and the safety of this vaccine strain, LVS is a superb candidate for use as a vaccine platform to deliver antigens that protect against pathogenic organisms.
Currently, there is not a licensed vaccine against the important opportunistic bacterial pathogen, Pseudomonas aeruginosa.5 P. aeruginosa is a leading cause of nosocomial and burn wound infections, and chronically infects those afflicted with cystic fibrosis.6 Treating these infections therapeutically is challenging, as many strains of P. aeruginosa are drug resistant. This magnifies the need for an effective vaccine. Although a vaccine targeting P. aeruginosa is not available for use in humans, various attempts at vaccine development have identified protective antigens.7 However, corresponding long-term immunity has been diminutive.7 Our objective here is to engineer F. tularensis LVS—a vaccine strain that elicits long term memory and cell mediated immunity—to encode protective antigens of P. aeruginosa. This recombinant strain may provide adequate protection against P. aeruginosa infections.
Results
For use as a potential vaccine platform, encoding heterologous genes in the chromosome of F. tularensis LVS would be most ideal. However, a plasmid-based expression system is more practical to provide proof of concept. Therefore, we modified a stable Francisella plasmid, pFNLTP88 to encode the robust groE promoter of F. tularensis9 (Fig. 1A). This plasmid, pABST was further modified to encode the P. aeruginosa genes pilA, oprF, and fliC (Fig. 1A). pilA encodes the major pilin protein subunit of the type IV pilus, oprF encodes an outer membrane porin protein, and fliC encodes the monomeric flagellin subunit protein of the flagellum.10-12 These genes were selected because they encode protective antigens13-15 and because the expression of these recombinant proteins could be tested using specific antibodies we had in our possession. We therefore generated the plasmids pBR, pOPRF, and pFLI, which encoded P. aeruginosa pilA, oprF, and fliC respectively, under the control of the F. tularensis groE promoter (Fig. 1). After mobilizing these plasmids into F. tularensis LVS, we tested their expression by Western blotting. This analysis indicated that F. tularensis LVS/ pBR produced PilA of P. aeruginosa (PilAPa) (Fig. 2A). In addition, OprF of P. aeruginsa (OprFPa) was produced by LVS / pOPRF (Fig. 2B). These recombinant proteins produced doublet bands (PilAPa) or a band at a slightly higher molecular weight than the endogenous version (OprFPa), likely due to the incompatibility between leader peptidases of LVS and the signal peptides (Fig. 2A and B).16 Moreover, the level of OprFPa protein expression in F. tularensis LVS appeared to be substantially diminished compared to those observed naturally by P. aeruginosa (Fig. 2B). Upon mobilization of pFLI into F. tularensis LVS, we observed very few transformants (data not shown). We hypothesized that perhaps expression of FliC of P. aeruginosa (FliCPa) in LVS is detrimental to this bacterium. Since groE is an especially robust promoter,9 we reasoned using a weaker promoter to drive expression of fliC may reduce the apparent unfavorable effect that overexpression of this heterologous gene was having on LVS. Therefore, we cloned fliC into pGRP so that this P. aeruginosa gene was under the control of the FTL_0580 (FGRp) promoter17 which produces substantially fewer transcripts than the groE promoter18 (Fig. 3). The resulting plasmid, pGFLI, was mobilized into F. tularensis LVS and expression of FliCPa was determined by Western blotting. This Western blot indicated that F. tularensis LVS / pGFLI produced FliCPa at levels seemingly comparable to the parent P. aeruginosa strain (Fig. 2C). However, as we observed for PilAPa and OprFPa, the recombinant FliCPa appeared to be of a higher molecular weight, indicating that this protein is likely processed differently when expressed in F. tularensis LVS.
Figure 1.
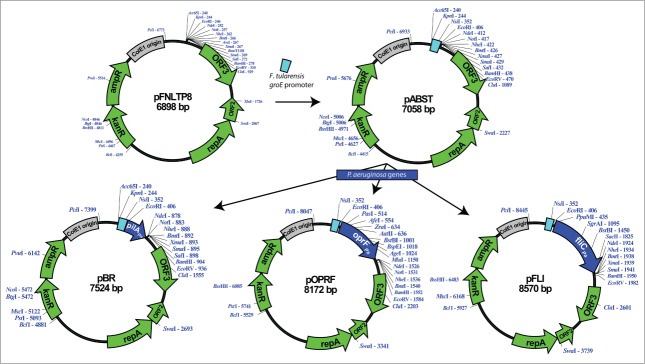
Construction of the plasmids pABST, pBR, pOPRF, and pFLI. The F. tularensis LVS groE promoter was PCR-amplified and the amplicon generated was digested with KpnI and EcoRI, gel-purified, and ligated with pFNLTP8 that had been digested with these same enzymes to generate pABST. Primers were used to PCR-amplify pilA (P. aeruginosa 1244), oprF, or fliC (both of P. aerugionosa PA14). The amplicons generated were digested with EcoRI and NdeI, gel purified, and ligated with pABST that had been digested with these same enzymes to generate pBR, pOPRF, or pFLI respectively.
Figure 2.
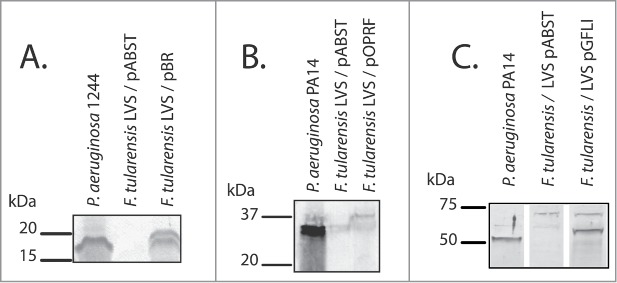
Western blotting of recombinant F. tularensis LVS strains expressing proteins of P. aeruginosa. Prior to SDS-PAGE, bacterial cells were normalized to the same density. SDS-PAGE gels were electroblotted onto nitrocellulose paper. After the membrane was blocked, the nitrocellulose paper was probed with mouse monoclonal 5.44 specific for PilA (A), serum specific for OprF (B), or serum specific for FliC (C). Bands were visualized by using alkaline phosphatase-labeled secondary antibodies and naphthol as-mx phosphate with fast red tr salt zinc chloride.
Figure 3.
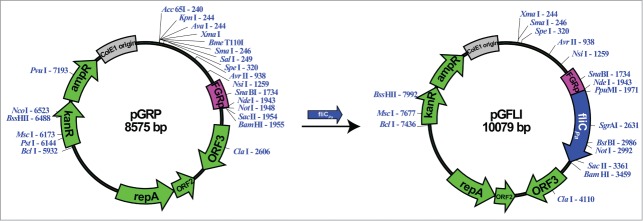
Construction of the plasmid, pGFLI. Primers were used to amplify fliC of P. aeruginosa PA14. This amplicon was digested with NdeI and BamHI, gel purified, and ligated with pGRP that had been digested with these same enzymes.
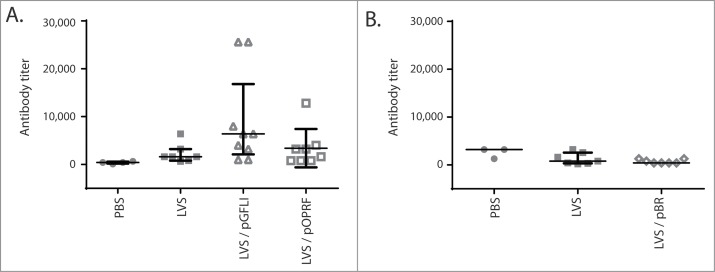
Since these recombinant F. tularensis LVS strains were capable of producing PilAPa, OprFPa, and FliCPa, we wanted to test their ability to elicit production of specific antibodies. Antibodies specific for surface antigens of P. aeruginosa are important for opsonin-mediated phagocytosis of this pathogen, a phenomenon associated with protective immunity.19 Mice were immunized by intranasal (i.n.) administration with individual recombinant F. tularensis LVS strains (LVS / pBR, LVS / pOPRF, or LVS / pGFLI), LVS alone, or phosphate buffered saline (PBS). This immunization route was selected because previous studies showed robust mucosal and systemic antibody production in response to alternative Pseudomonas vaccines.20,21 Serum was collected from mice 42 days post-immunization. Mice that had been immunized with LVS / pGFLI produced robust levels of antibodies specific for P. aerugionsa (P < 0.05) compared to animals treated with PBS (Fig. 4A). However, immunization with LVS / pOPRF or LVS / pBR did not result in high levels of antibodies specific for P. aeruginosa (Fig. 4A and B). Therefore, even though LVS elicits a robust adaptive immune response,4 not all recombinant antigens expressed in this strain may be equally immunogenic. In the case of OprF, it is also possible that the lower level of expression relative to P. aeruginosa was not sufficient to elicit a robust response.
Figure 4.
Antibody levels from mice immunized with recombinant F. tularensis LVS expressing P. aeruginosa proteins. Antibody levels from mice immunized with F. tularensis LVS, F. tularensis LVS / pBR, F. tularensis LVS / pGFLI, F. tularensis LVS / pOPRF, or PBS was determined by ELISA. Data points represent antibody titers from individual mice. Serum was extracted from mice on day 42 post-immunization. ELISA plates were coated with P. aeruginosa PA14 (A) or 1244 (B). Lines and error bars represent the medians and quartiles respectively. Antibody levels from mice immunized with LVS / pGFLI produced significant levels of antibodies specific for P. aerugionsa (P < 0.05) compared to mice treated with PBS.
Discussion
In this study, F. tularensis LVS was engineered to express P. aeruginosa proteins. This strategy employed the use of a stable Francisella shuttle vector in which the exogenous genes were under the control of either the groE or FGRp promoter.9,17 These recombinant F. tularensis LVS strains were used to immunize mice to determine if the heterologously-expressed proteins could generate a robust adaptive immune response against P. aeruginosa. Mice that were immunized with recombinant LVS expressing FliC of P. aeruginosa produced a significant level of antibodies specific for P. aeruginosa relative to mock-immunized mice. This study establishes that F. tularensis LVS could potentially be used as a vaccine platform to deliver antigens that stimulate an immune response against heterologous bacteria. A recent study indicated that a mutant of F. novicida U112 expressing flagellin of Salmonella typhimurium could activate TLR5 resulting in increased inflammation, and therefore, this strain may be a potent tularemia vaccine candidate.22 The possibility exists that F. tularensis LVS / pGFLI may also provide increased protection against F. tularensis for similarly stimulating TLR5, however this remains to be determined.
Mice immunized with LVS expressing either PilA or OprF of P. aerugionsa did not stimulate robust antibody production from mice. This could be due to the meager protein levels produced by the recombinant LVS expressing these proteins (Figs. 2 and 3). Future efforts will focus on determining whether optimizing codon selection or utilizing a more robust promoter9 will lead to increased expression and enhanced ability to stimulate antibody production. Two candidate promoters would be those of bfr or FTL_1138.9 Zaide et al showed these 2 promoters, along with groE, are the most potent of F. tularensis.9 An alternative strategy to achieve greater protein expression could be to utilize tandem promoters to maximize transcript levels.23 However, the possibility exists that excessive expression of exogenous proteins could be deleterious to the host bacterium—a plausible explanation for the poor transformation efficiency we observed for pFLI into F. tularensis LVS. In support of this interpretation, utilization of a weaker promoter (FGRp) resulted in multiple viable transformants capable of expressing FliCPa. To control heterologous gene expression, future studies could take advantage of tetracycline-regulated promoter systems that allow for both induction and repression of downstream genes. Such systems have been developed for Francisella species.24,25 However, whether or not the tetracycline-regulation for Francisella is effective inside an animal host remains to be determined. Another potential pitfall of the current study is that, for ease of manipulation, the genes encoding the exogenous proteins were harbored on plasmids. Although stable, these plasmids could have been lost in vivo, diminishing exposure of the animals to the antigens. Future studies should focus on utilizing existing molecular tools to generate stable recombinant F. tularensis LVS bacteria encoding chromosomal copies of selected heterologous genes.26-30 Aside from adjusting expression levels by F. tularensis LVS, more robust immune responses may be attained by altering the route of immunization or utilizing a boost following vaccination.31 It is also possible that lack of pre-protein processing may have altered the antigenicity of the recombinant proteins. Future experiments should focus on recombinantly expressing coding sequence for mature heterologous proteins in F. tularensis LVS and determining whether the resulting strains induce a more robust immune response.
Because recombinant F. tularensis LVS is capable of directing an immune response against heterologous proteins, and since immunization with this bacterium leads to over 30 years of cell-mediated immunity4, this bacterium has potential for use as a universal vaccine platform against a number of bacterial and viral infections. Genetic tools have been developed that could allow for stable, safe, and effective vaccine strains.26-30 However, viral proteins requiring glycosylation by eukaryotic host machinery may not be compatible for use with this system. Nevertheless, there is immense potential for F. tularensis LVS to express heterologous bacterial toxoids, surface proteins, and enzymes for lipid or carbohydrate biosynthetic pathways to direct the immune response against the cognate pathogens. In the more immediate future, studies should investigate whether immunization with F. tularensis / pGFLI protects against a lethal P. aeruginosa infection using the appropriate animal model such as the murine cystic fibrosis model or the burn mouse model.21,32
Materials and Methods
Bacterial strains and media
Bacterial strains utilized in this study are listed in Table 1. F. tularensis LVS frozen stock cultures were used to inoculate chocolate II agar plates which were incubated at 37°C with 5% CO2 for 2–4 days. P. aeruginosa bacteria were cultivated overnight at 37°C on trypticase soy agar or in trypticase soy broth with agitation. Escherichia coli 5-α (New England Biolabs) bacteria were cultivated using LB agar incubated at 37°C for 14–24 hours. E. coli was also cultivated using LB broth incubated at 37°C with shaking. When necessary, the following antibiotics were supplemented into the media: ampicillin (100 μg/ml), kanamycin (35 μg/ml for E. coli; 10 μg/ml for F. tularensis).
Table 1.
Strains, plasmids, and primers used in this study. Primer sequences are written 5′→3′
| Description | Source or Reference | |
|---|---|---|
| Strains | ||
| F. tularensis | ||
| LVS | F. tularensis subsp. holarctica live vaccine strain | Karen Elkins |
| E. coli | ||
| 5-α | fhuA2 Δ(argF-lacZ)U169 phoA glnV44 Φ80 Δ(lacZ)M15 gyrA96 recA1 relA1 endA1 thi-1 hsdR17 | New England Biolabs |
| P. aeruginosa | ||
| 1244 | Wild type | Peter Castric |
| PA14 | Wild type | Costi Sifri |
| Plasmids | ||
| pFNLTP8 | Francisella shuttle plasmid, Kmr | Ref.8 |
| pABST | pFNLTP8 with F. tularensis LVS groE promoter | This study |
| pBR | pABST with P. aeruginosa 1244 pilA under the control of the F. tularensis LVS groE promoter | This study |
| pOPRF | pABST with P. aeruginosa PA14 oprF under the control of the F. tularensis LVS groE promoter | This study |
| pFLI | pABST with P. aeruginosa PA14 fliC under the control of the F. tularensis LVS groE promoter | This study |
| pGRP | Francisella shuttle vector containing the promoter of FTL_0581 | Ref.17 |
| pGFLI | pGRP under the control of the F. tularensis LVS FTL_0581 promoter | This study |
| Primers | ||
| groE1 | ACGTGGTACCCGAGAGCTTGTTTGACAAAAAAAC | This study |
| groE2 | CATGGAATTCAACAATCTTACTCCTTTGTTAAATTATTTTTG | This study |
| pilA1 | ACGTGAATTCATGAAAGCTCAGAAGGGTTTTAC | This study |
| pilA2 | CATGCATATGTTAGGATTTCGGGCAATTAGC | This study |
| oprFfwd | CATGGAATTCCTAACTGACCATCAAGATGGG | This study |
| oprF2rev | CATGCATATGGCCGGGTTTTTCCTTAGAG | This study |
| fliCfwd | CATGGAATTCCGCAAGCTCAGGTAACCGAAATAGGTCCTTTGGAGGAAATC | This study |
| fliCrev | CATGCATATGTTAGCGCAGCAGGCTCAGGACCGCC | This study |
| fliCfwdnde | CATGCATATGCGCAAGCTCAGGTAACCGAAATAGG | This study |
| fliCrevbam | CATGGGATCCTTAGCGCAGCAGGCTCAGGACCGCC | This study |
Generation of recombinant vaccine strains
Plasmids and oligonucleotide primers used in the study are listed in Table 1. All general cloning was conducted using E. coli 5-α (New England Biolabs). Bacterial chromosomal DNA that had been extracted from stationary-phase broth cultures using a standard phenol-chloroform procedure was used as a template for PCR amplifications. Primers groE1 and groE2 were used to PCR-amplify the F. tularensis LVS groE promoter.9 This amplicon was digested with KpnI and EcoRI, gel-purified, and ligated with pFNLTP8 that had been digested with these same enzymes yielding pABST.
The plasmid pBR encoding pilA of P. aeruginosa 1244 under the control of the F. tularensis LVS groE promoter was generated using the following procedures. The primers pilA1 and pilA2 were used to PCR-amplify pilA of P. aeruginosa 1244. This amplicon was digested with EcoRI and NdeI, gel purified, and ligated with pABST that had been digested with these same enzymes.
The plasmid pOPRF encoding oprF of P. aeruginosa PA14 under the control of the F. tularensis LVS groE promoter was constructed as follows. The primers oprFfwd and oprF2rev were used to amplify oprF of P. aeruginosa PA14. This amplicon was digested with EcoRI and NdeI, gel purified, and ligated with pABST that had been digested with these same enzymes.
The plasmid pFLI encoding fliC of P. aeruginosa PA14 under the control of the F. tularensis LVS groE promoter was constructed using the following procedures. The primers fliCfwd and fliCrev were used to amplify fliC of P. aeruginosa PA14. This amplicon was digested with EcoRI and NdeI, gel purified, and ligated with pABST that had been digested with these same enzymes.
The plasmid pGFLI encoding fliC of P. aeruginosa PA14 under the control of the F. tularensis LVS FGRp promoter17 was generated as follows. The primers fliCfwdnde and fliCrevbam were used to amplify fliC of P. aeruginosa PA14. This amplicon was digested with NdeI and BamHI, gel purified, and ligated with pGRP17 that had been digested with these same enzymes.
Plasmid maps
Plasmid maps were generated using pDRAW32.
Electroporation
Plasmids were mobilized into F. tularensis LVS by electroporation as previously described.17 Briefly, F. tularensis LVS bacteria grown on chocolate agar plates were used to inoculate trypticase soy broth supplemented with 0.1% Cysteine HCl (TSBc). This culture was incubated overnight at 37°C with shaking until bacteria reached stationary phase. This starter culture was diluted 1:10 in fresh TSBc and incubated at 37°C with shaking until bacteria reached double their optical density (about 3-4 hours). For each electroporation, 1 ml of culture was washed 3 times in 500 mM sucrose. Subsequently, pellets were suspended in 50 μl of 500 mM sucrose, plasmid DNA was added (approximately 1-3 μg DNA in 2.5 μl), and then this suspension was transferred to a 0.2 cm gap electrocuvette. Electrocuvettes were pulsed at 2.5 kV, 150 Ω, and 25 μF. Cells were then recovered in 1 ml of TSBc and incubated at 37°C with shaking for at least 1 hour before plating on chocolate II agar containing kanamycin.
Western blotting
Western blotting was conducted in a similar fashion as described previously.10 Bacterial cells were normalized to the same density (optical density at 600 nm), pelleted, and suspended in Laemmli buffer with 2.5% β-mercaptoethanol. This material was sonicated, subjected to SDS-PAGE, and then electroblotted onto nitrocellulose paper. After the membrane was blocked (phosphate buffered saline containing 0.5% casein, 0.5% Bovine serum albumin, 100 mg/L Phenol Red, and 0.2% Sodium Azide, pH 7.4), the blot was probed with mouse monoclonal 5.44 specific for PilA of P. aeruginosa 1244 (a gift from Peter Castric), or rabbit serum specific for OprF (a gift from Hiroshi Nikaido), or FliC (a gift from Reuben Ramphal). Alkaline phosphatase-labeled secondary antibodies (Pierce) were used, and bands were visualized after adding naphthol as-mx phosphate (Sigma-Aldrich) and fast red tr salt zinc chloride (MP Biomedicals, LLC).
Animal immunizations
All experiments involving mice were conducted at the University of South Carolina and were approved by this institution's animal care and use committee. Female 5-6 week old Balb/c mice (Jackson labs) were immunized (i.n.) using F. tularensis LVS, F. tularensis LVS / pBR, F. tularensis LVS / pGFLI, F. tularensis LVS / pOPRF, or PBS as a control in a similar fashion to previously conducted studies.33 Blood was extracted from the tail vein of mice on day 42 post-immunization.34 The blood was allowed to clot at room temperature, and serum was extracted following centrifugation.
ELISA
Serum antibody concentrations were determined by ELISA in a similar manner as previously described.34 Approximately 2 × 108 CFU P. aeruginosa bacteria suspended in 200 μl phosphate buffered saline were distributed into each well of a microtitre plate (96-well). Plates were covered and stored overnight at 4°C to allow bacteria to adhere. After this incubation, the remaining liquid was discarded and the wells were washed twice with PBS containing 0.05% Tween-20 (PBSt). Each well was blocked with 200 μl of PBS containing 1% bovine serum albumin (PBSb) at room temperature for 1 hour. After 2 washes with PBSt, plates were covered and stored at 4°C until needed.
To determine serum antibody concentrations, prepared ELISA plates were washed twice with PBSt and subsequently serially diluted mouse serum samples (diluted in PBSb) were added to the wells. Control wells were treated similarly but did not contain diluted mouse serum. After an overnight incubation at 4°C, this plate was washed twice with PBSt. The secondary antibody (goat anti-mouse Ig [heavy and light chain, HRP-conjugated; Southern Biotech]) was diluted (10−4) in PBSb and was added to each well. After a 90 minute incubation at 37°C, the plate was washed 3 times with PBSt and subsequently 200 μl of 3,3′,5,5′-tetramethylbenzidine was added to each well. The plate was incubated in the dark, and the reaction was stopped by adding 50 μl of 1 M HCl to each well. The absorbance of each well at 450 nm (OD450) was measured using an Eppendorf PlateReader AF2200. The mean OD450 of control wells plus 3 standard deviations was used to calculate the cutoff for antibody concentrations. The antibody concentration was determined to be the inverse of the lowest dilution of serum producing a higher OD450 than the cutoff. Samples in which the antibody concentration was below the limit of detection were assigned a value of the inverse of the lowest dilution assayed minus 1.
A statistical analysis of the antibody titers was conducted using GraphPad Prism software. Data were analyzed using a Kruskal-Wallis with a Dunn's multiple comparisons test to determine statistically significant differences.
Disclosure of Potential Conflicts of Interest
No potential conflicts of interest were disclosed.
Acknowledgments
The authors thank Hiroshi Nikaido, Reuben Ramphal, and Peter Castric for providing antibodies used in this study.
Funding
This work was funded by a grant through the NASA WV Space Grant Consortium (NNX10AK62H), an Institutional Development Award (IDeA) from the National Institute of General Medical Sciences of the National Institutes of Health (P20GM103434), and a grant from the National Institutes of Health, National Institute of Allergy and Infectious Diseases (5K22AI087703).
References
- 1. Ellis J, Oyston PC, Green M, Titball RW. Tularemia. Clin Microbiol Rev 2002; 15(4):631-46; PMID:12364373; http://dx.doi.org/ 10.1128/CMR.15.4.631-646.2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Wayne Conlan J, Oyston PC. Vaccines against Francisella tularensis. Ann N Y Acad Sci 2007; 1105:325-50; PMID:17395730; http://dx.doi.org/ 10.1196/annals.1409.012 [DOI] [PubMed] [Google Scholar]
- 3. El Sahly HM, Atmar RL, Patel SM, Wells JM, Cate T, Ho M, Guo K, Pasetti MF, Lewis DE, Sztein MB, et al . Safety, reactogenicity and immunogenicity of Francisella tularensis live vaccine strain in humans. Vaccine 2009; 27(36):4905-11; PMID:19567246; http://dx.doi.org/ 10.1016/j.vaccine.2009.06.036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Eneslätt K, Rietz C, Rydén P, Stöven S, House RV, Wolfraim LA, Tärnvik A, Sjöstedt A. Persistence of cell-mediated immunity three decades after vaccination with the live vaccine strain of Francisella tularensis. Eur J Immunol 2011; 41(4):974-80; http://dx.doi.org/ 10.1002/eji.201040923 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Sharma A, Krause A, Worgall S. Recent developments for Pseudomonas vaccines. Hum Vaccin 2011; 7(10):999-1011; PMID:21941090; http://dx.doi.org/ 10.4161/hv.7.10.16369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Driscoll JA, Brody SL, Kollef MH. The epidemiology, pathogenesis and treatment of Pseudomonas aeruginosa infections. Drugs 2007; 67(3):351-68; PMID:17335295; http://dx.doi.org/ 10.2165/00003495-200767030-00003 [DOI] [PubMed] [Google Scholar]
- 7. Döring G, Pier GB. Vaccines and immunotherapy against Pseudomonas aeruginosa. Vaccine 2008; 26(8):1011-24; PMID:18242792; http://dx.doi.org/ 10.1016/j.vaccine.2007.12.007 [DOI] [PubMed] [Google Scholar]
- 8. Maier TM, Havig A, Casey M, Nano FE, Frank DW, Zahrt TC. Construction and characterization of a highly efficient Francisella shuttle plasmid. Appl Environ Microbiol 2004; 70(12):7511-9; PMID:15574954; http://dx.doi.org/ 10.1128/AEM.70.12.7511-7519.2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Zaide G, Grosfeld H, Ehrlich S, Zvi A, Cohen O, Shafferman A. Identification and characterization of novel and potent transcription promoters of Francisella tularensis. Appl Environ Microbiol 2011; 77(5):1608-18; PMID:21193666; http://dx.doi.org/ 10.1128/AEM.01862-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Castric PA, Sidberry HF, Sadoff JC. Cloning and sequencing of the Pseudomonas aeruginosa 1244 pilin structural gene. Mol Gen Genet 1989; 216(1):75-80; PMID:2499765; http://dx.doi.org/ 10.1007/BF00332233 [DOI] [PubMed] [Google Scholar]
- 11. Sugawara E, Nestorovich EM, Bezrukov SM, Nikaido H. Pseudomonas aeruginosa porin OprF exists in two different conformations. J Biol Chem 2006; 281(24):16220-9; PMID:16595653; http://dx.doi.org/ 10.1074/jbc.M600680200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Verma A, Arora SK, Kuravi SK, Ramphal R. Roles of specific amino acids in the N terminus of Pseudomonas aeruginosa flagellin and of flagellin glycosylation in the innate immune response. Infect Immun 2005; 73(12):8237-46; PMID:16299320; http://dx.doi.org/ 10.1128/IAI.73.12.8237-8246.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Krause A, Whu WZ, Xu Y, Joh J, Crystal RG, Worgall S. Protective anti-Pseudomonas aeruginosa humoral and cellular mucosal immunity by AdC7-mediated expression of the P. aeruginosa protein OprF. Vaccine 2011; 29(11):2131-9; PMID:21215829; http://dx.doi.org/ 10.1016/j.vaccine.2010.12.087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Kao DJ, Churchill ME, Irvin RT, Hodges RS. Animal protection and structural studies of a consensus sequence vaccine targeting the receptor binding domain of the type IV pilus of Pseudomonas aeruginosa. J Mol Biol 2007; 374(2):426-42; PMID:17936788; http://dx.doi.org/ 10.1016/j.jmb.2007.09.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Faezi S, Safarloo M, Amirmozafari N, Nikokar I, Siadat SD, Holder IA, Mahdavi M. Protective efficacy of Pseudomonas aeruginosa type-A flagellin in the murine burn wound model of infection. APMIS 2014; 122(2):115-27; PMID:23758581; http://dx.doi.org/ 10.1111/apm.12101 [DOI] [PubMed] [Google Scholar]
- 16. Faridmoayer A, Fentabil MA, Mills DC, Klassen JS, Feldman MF. Functional characterization of bacterial oligosaccharyltransferases involved in O-linked protein glycosylation. J Bacteriol 2007; 189(22):8088-98; PMID:17890310; http://dx.doi.org/ 10.1128/JB.01318-07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Horzempa J, Tarwacki DM, Carlson PE, Robinson CM, Nau GJ. Characterization and application of a glucose-repressible promoter in Francisella tularensis. Appl Environ Microbiol 2008; 74(7):2161-70; PMID:18245238; http://dx.doi.org/ 10.1128/AEM.02360-07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Horzempa J, Carlson PE, O'Dee DM, Shanks RM, Nau GJ. Global transcriptional response to mammalian temperature provides new insight into Francisella tularensis pathogenesis. BMC Microbiol 2008; 8:172; PMID:18842136; http://dx.doi.org/ 10.1186/1471-2180-8-172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. DiGiandomenico A, Warrener P, Hamilton M, Guillard S, Ravn P, Minter R, Camara MM, Venkatraman V, Macgill RS, Lin J, et al. Identification of broadly protective human antibodies to Pseudomonas aeruginosa exopolysaccharide Psl by phenotypic screening. J Exp Med 2012; 209(7):1273-87; PMID:22734046; http://dx.doi.org/ 10.1084/jem.20120033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. DiGiandomenico A, Rao J, Harcher K, Zaidi TS, Gardner J, Neely AN, Pier GB, Goldberg JB. Intranasal immunization with heterologously expressed polysaccharide protects against multiple Pseudomonas aeruginosa infections. Proc Natl Acad Sci U S A 2007; 104(11):4624-9; PMID:17360574; http://dx.doi.org/ 10.1073/pnas.0608657104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Horzempa J, Held TK, Cross AS, Furst D, Qutyan M, Neely AN, Castric P. Immunization with a Pseudomonas aeruginosa 1244 pilin provides O-antigen-specific protection. Clin Vaccine Immunol 2008; 15(4):590-7; PMID:18272666; http://dx.doi.org/ 10.1128/CVI.00476-07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Cunningham AL, Dang KM, Yu JJ, Guentzel MN, Heidner HW, Klose KE, Arulanandam BP. Enhancement of vaccine efficacy by expression of a TLR5 ligand in the defined live attenuated Francisella tularensis subsp. novicida strain U112ΔiglB::fljB. Vaccine 2014; 32(40):5234-40; PMID:25050972; http://dx.doi.org/ 10.1016/j.vaccine.2014.07.038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Tani C, Inoue K, Tani Y, Harun-ur-Rashid M, Azuma N, Ueda S, Yoshida K, Maeda I. Sensitive fluorescent microplate bioassay using recombinant Escherichia coli with multiple promoter-reporter units in tandem for detection of arsenic. J Biosci Bioeng 2009; 108(5):414-20; PMID:19804866; http://dx.doi.org/ 10.1016/j.jbiosc.2009.05.014 [DOI] [PubMed] [Google Scholar]
- 24. McWhinnie RL, Nano FE. Synthetic promoters functional in Francisella novicida and Escherichia coli. Appl Environ Microbiol 2014; 80(1):226-34; PMID:24141126; http://dx.doi.org/ 10.1128/AEM.02793-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. LoVullo ED, Miller CN, Pavelka MS, Kawula TH. TetR-based gene regulation systems for Francisella tularensis. Appl Environ Microbiol 2012; 78(19):6883-9; PMID:22820330; http://dx.doi.org/ 10.1128/AEM.01679-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Horzempa J, Shanks RM, Brown MJ, Russo BC, O'Dee DM, Nau GJ. Utilization of an unstable plasmid and the I-SceI endonuclease to generate routine markerless deletion mutants in Francisella tularensis. J Microbiol Methods 2010; 80(1):106-8; PMID:19879904; http://dx.doi.org/ 10.1016/j.mimet.2009.10.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. LoVullo ED, Sherrill LA, Perez LL, Pavelka MS. Genetic tools for highly pathogenic Francisella tularensis subsp. tularensis. Microbiology 2006; 152(Pt 11):3425-35; PMID:17074911; http://dx.doi.org/ 10.1099/mic.0.29121-0 [DOI] [PubMed] [Google Scholar]
- 28. LoVullo ED, Sherrill LA, Pavelka MS. Improved shuttle vectors for Francisella tularensis genetics. FEMS Microbiol Lett 2009; 291(1):95-102; PMID:19067747; http://dx.doi.org/ 10.1111/j.1574-6968.2008.01440.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. LoVullo ED, Molins-Schneekloth CR, Schweizer HP, Pavelka MS. Single-copy chromosomal integration systems for Francisella tularensis. Microbiology 2009; 155(Pt 4):1152-63; PMID:19332817; http://dx.doi.org/ 10.1099/mic.0.022491-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Kalivoda EJ, Horzempa J, Stella NA, Sadaf A, Kowalski RP, Nau GJ, Shanks RM. New vector tools with a hygromycin resistance marker for use with opportunistic pathogens. Mol Biotechnol 2011; 48(1):7-14; PMID:20972648; http://dx.doi.org/ 10.1007/s12033-010-9342-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Jia Q, Bowen R, Sahakian J, Dillon BJ, Horwitz MA. A heterologous prime-boost vaccination strategy comprising the Francisella tularensis live vaccine strain capB mutant and recombinant attenuated Listeria monocytogenes expressing F. tularensis IglC induces potent protective immunity in mice against virulent F. tularensis aerosol challenge. Infect Immun 2013; 81(5):1550-61; PMID:23439306; http://dx.doi.org/ 10.1128/IAI.01013-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Warrener P, Varkey R, Bonnell JC, DiGiandomenico A, Camara M, Cook K, Peng L, Zha J, Chowdury P, Sellman B, et al. A novel anti-PcrV antibody providing enhanced protection against Pseudomonas aeruginosa in multiple animal infection models. Antimicrob Agents Chemother 2014; 58(8):4384-91; PMID:24841258; http://dx.doi.org/ 10.1128/AAC.02643-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Schmitt DM, O'Dee DM, Brown MJ, Horzempa J, Russo BC, Morel PA, Nau GJ. Role of NK cells in host defense against pulmonary type A Francisella tularensis infection. Microbes Infect 2013; 15(3):201-11; PMID:23211929; http://dx.doi.org/ 10.1016/j.micinf.2012.11.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. DiGiandomenico A, Rao J, Goldberg JB. Oral vaccination of BALB/c mice with Salmonella enterica serovar Typhimurium expressing Pseudomonas aeruginosa O antigen promotes increased survival in an acute fatal pneumonia model. Infect Immun 2004; 72(12):7012-21; PMID:15557624; http://dx.doi.org/ 10.1128/IAI.72.12.7012-7021.2004 [DOI] [PMC free article] [PubMed] [Google Scholar]