Abstract
Background
Anterior cruciate ligament (ACL) re-injury results in worse outcomes and increases risk of post-traumatic osteoarthritis.
Objectives
To identify the risk factors for both ipsilateral and contralateral ACL tears after primary ACL reconstruction (ACLR).
Study Design
Cohort study; Level of evidence, 3.
Methods
Data from the Multicenter Orthopaedic Outcomes Network (MOON), a prospective longitudinal cohort, were used to identify risk factors for ACL retear. Subjects with primary ACLR, no history of contralateral knee surgery, and a minimum of 2-year follow-up data were included. Age, sex, Marx activity score, graft type, lateral meniscus tear, medial meniscus tear, sport played at index injury, and surgical facility were evaluated to determine their contribution to both ipsilateral retear and contralateral ACL tear.
Results
A total of 2683 subjects with average age of 27 ± 11 years (1498 men; 56%) met all study inclusion/exclusion criteria. Overall there were 4.4% ipsilateral graft tears and 3.5% contralateral ACL tears. The odds of ipsilateral retear were 5.2 times greater for an allograft (p<0.01) compared with a bone-patellar tendon-bone (BTB) autograft; the odds of retear were not significantly different between BTB autograft and hamstring autograft (p=0.12). The odds of an ipsilateral ACL retear decreased by 0.09 for every yearly increase in age (p<0.01) and increased by 0.11 for every increased point on the Marx score (p< 0.01). The odds were not significantly influenced by sex, smoking status, sport played, medial or lateral meniscus tear, or consortium site (p>0.05). The odds of a contralateral ACL tear decreased by 0.04 for every yearly increase in age (p=0.04) and increased by 0.12 for every increased point on the Marx score (p<0.01); these odds were not significantly different between sex, smoking status, sport played, graft type, medial meniscal tear, and lateral meniscal tear (p>0.05).
Conclusions
Younger age, higher activity level, and allograft graft type were predictors of increased odds of ipsilateral graft failure. Higher activity and younger age were found to be risk factors in contralateral ACL tears.
Keywords: anterior cruciate ligament, ACL reconstruction, outcomes, autograft, allograft, failure, retear
INTRODUCTION
Tears of the anterior cruciate ligament (ACL) are common in the active population. The ACL deficient knee has significant risk of functional instability, future meniscus tears and subsequent osteoarthritis (56). Reconstruction of a torn ACL is often performed with the goal of restoring stability to the knee and decreasing risk of subsequent injury to the knee. It is estimated that 200,000 ACL reconstructions (ACLR) are performed annually in the United Stated alone (9). Excellent results of ACLR restoring functional knee stability have been widely reported in the literature (7,56,61). During the 6- to 12-month recovery from an ACLR there is a significant investment of time, discomfort, money and effort by the patient. For the ACL graft to tear after a successful surgery and rehabilitation is a devastating event for the patient as well as the family, coach, and surgeon. Further, it has also been demonstrated that revision ACLRs have inferior results compared to primary ACLRs (12,40,64). Unfortunately, it also is not uncommon to recover from an ACLR of one knee and then tear the native ACL of the contralateral knee (63). This then places the contralateral knee at increased risk of premature osteoarthritis as well.
Risk factors for the tearing of a native ACL have been studied and several have been identified. Female sex and participating in cutting sports have been widely reported as risk factors for tearing a native ACL (1,5,22). Other reported risk factors include posterior tibial slope, narrow notch width, decreased ACL size, limb alignment, and multiple neuromuscular factors (4,42,43,50). However, the risk factors for tearing the contralateral ACL after ACL reconstruction on the opposite knee have not been widely evaluated (3).
The risk for ACL graft tears has been defined but the risk factors for these tears are less well studied (13,20,27,32,34,35,48,52,60,63). Recently both the Swedish (2) and Norwegian (46) ACLR registries have reported multivariable analyses controlling for factors such as sex, age, and surgical characteristics, including autograft type for ACLR graft injury. Unique features of this U.S.-based MOON cohort are collecting and controlling for body mass index (BMI), activity level, and allograft usage, as well as historically obtaining high patient follow-up (>80%) on both knees, which are not available in other well-conducted ACLR registries. A previous analysis of ACLR re-injury (defined as revision ACLR) at 2 years for this cohort included only 2 enrollment years (n=984 ACLR) (26). At the time, this was the first prospective cohort study to demonstrate age as a major risk factor for retear as well as allograft use in younger patients. But the previous study lacked power to report risk of a contralateral ACL tear subsequent to ACLR. The field should continually strive to more comprehensively identify the risk factors, especially those that are modifiable, for both graft retear and contralateral ACL injury for several reasons. First, this information can better educate patients on the expected outcomes of an ACLR. Second, patients can be counseled on reducing the risks of re-injury. Third, this information can be used to develop strategies to reduce re-injury by altering the modifiable risk factors (10,16,23,24,41). Thus, objectives for the current study were two-fold: 1) to identify the risk factors for subsequent ACLR retears; and, 2) to identify the risk factors for a tear of the contralateral native ACL in a large prospective cohort who underwent primary ACLR with minimum two-year follow-up.
METHODS
Subject Population
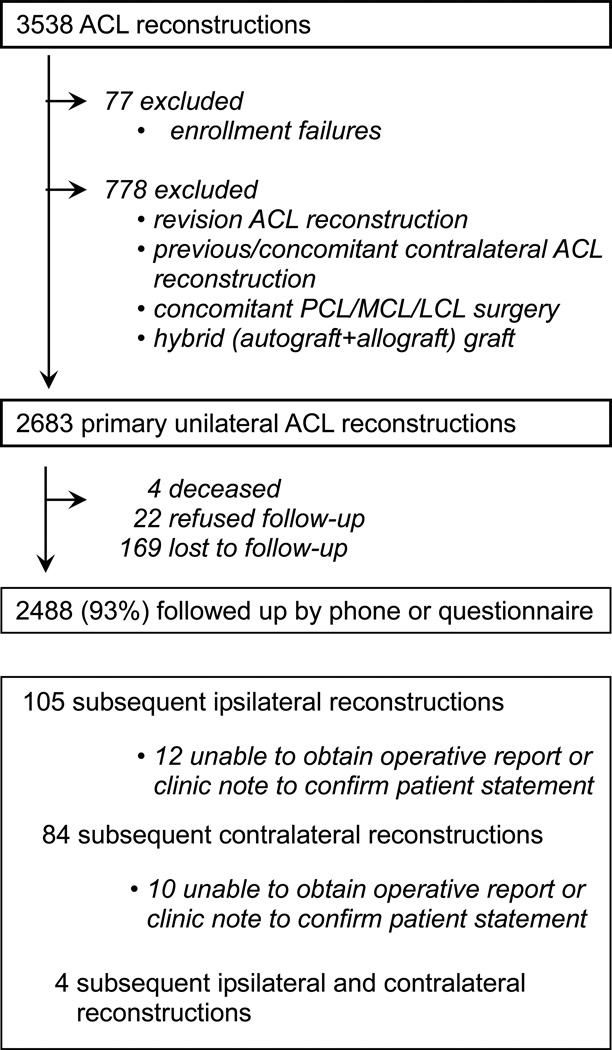
Data from this 2002–2008 cohort database were used to identify risk factors for ACL retear. This study was reviewed and approved by each participating site’s respective institutional review board, and all subjects provided written informed consent prior to data collection. Subjects were selected from an ongoing prospective cohort study, enrolled between 2002 and 2008, which was designed to identify risk factors for patient outcomes and risk of ACL retear. Subjects who had a primary ACLR with no history of contralateral knee surgery with 2-year follow-up data were included in the cohort (Figure 1). Subjects who underwent a multiligament reconstruction or had a hybrid autograft + allograft ACLR were excluded from the analysis. Patient age, sex, BMI, smoking status, Marx activity score (37) at time of index surgery, graft type (bone- patellar tendon-bone [BTB] autograft, hamstring autograft, allograft), sport played after ACLR, full thickness lateral meniscus tear at the time of ACLR, full thickness medial meniscus tear at the time of ACLR, and consortium site were evaluated to determine their contribution to both ipsilateral retear and contralateral ACL tear.
Figure 1.
Flow diagram showing inclusion/exclusion and follow-up. ACL, anterior cruciate ligament; PCL, posterior cruciate ligament; MCL, medial collateral ligament; LCL, lateral collateral ligament.
Patient Follow-up
At 2 years after surgery, patients were contacted by email, telephone, and/or questionnaire and asked if they had undergone any subsequent surgery (on either knee) following their index ACLR. If the patient indicated that he or she had had a subsequent surgery, when available, the operative report was reviewed for verification. The study cohort is summarized in a flow chart. (Figure 1)
Statistical Analyses
Multivariable logistic regression via the statistical software package STATA 9.0 (StataCorp LP, College Station, TX) was used to determine if the chosen variables were associated with the primary outcome, ACL graft tear. Odds ratios and confidence intervals were reported for the variables associated with outcome. A separate multivariable logistic regression was performed to evaluate the variable’s effect on contralateral ACL tear.
RESULTS
A total of 2683 subjects with a mean ± SD age of 27 ± 11 (1498 men; 56%) met all study inclusion criteria. Two-year follow-up was obtained on 2488 of the 2683 participants (92.7%). From the 2488 subjects, 109 (4.4%) ipsilateral graft retears and 88 (3.5%) contralateral ACL tears were identified and confirmed by operative report at the two-year follow-up. The number of subjects and percentage of ipsilateral graft retears are summarized for the variables tested in Table 1.
Table 1.
Patient Demographics
| Entire Cohort | ||
| N | % Retear | |
| Graft type | ||
| BTB autograft | 1131 | 3.2 |
| Hamstring autograft | 891 | 4.6 |
| Allograft | 466 | 6.9 |
| Sex | ||
| Male | 1365 | 4.6 |
| Female | 1123 | 4.1 |
| Smoking Status | ||
| No | 1962 | 5.1 |
| Quit | 254 | 1.2 |
| Current | 207 | 2.4 |
| Sport played at ACLR | ||
| None | 198 | 1.0 |
| Football | 269 | 8.9 |
| Basketball | 505 | 4.0 |
| Soccer | 365 | 7.1 |
| Other | 1151 | 3.2 |
| Medial Meniscus | ||
| No tear | 1722 | 4.9 |
| Tear | 766 | 3.3 |
| Lateral Meniscus | ||
| No tear | 1615 | 4.5 |
| Tear | 873 | 4.1 |
| Entire Cohort | ||
| No Tear, mean ± SD |
Tear, mean ± SD |
|
| Age, years | 27.4 ± 11.4 | 19.6 ± 6.6 |
| BMI | 25.5 ± 4.8 | 23.8 ± 4.0 |
| Marx score | 11.3 ± 5.3 | 14.4 ± 3.6 |
Key:
ACLR, anterior cruciate ligament reconstruction; BMI, body mass index; BTB, bone-patellar tendon-bon
Risk Factors of Ipsilateral ACL Graft Retear
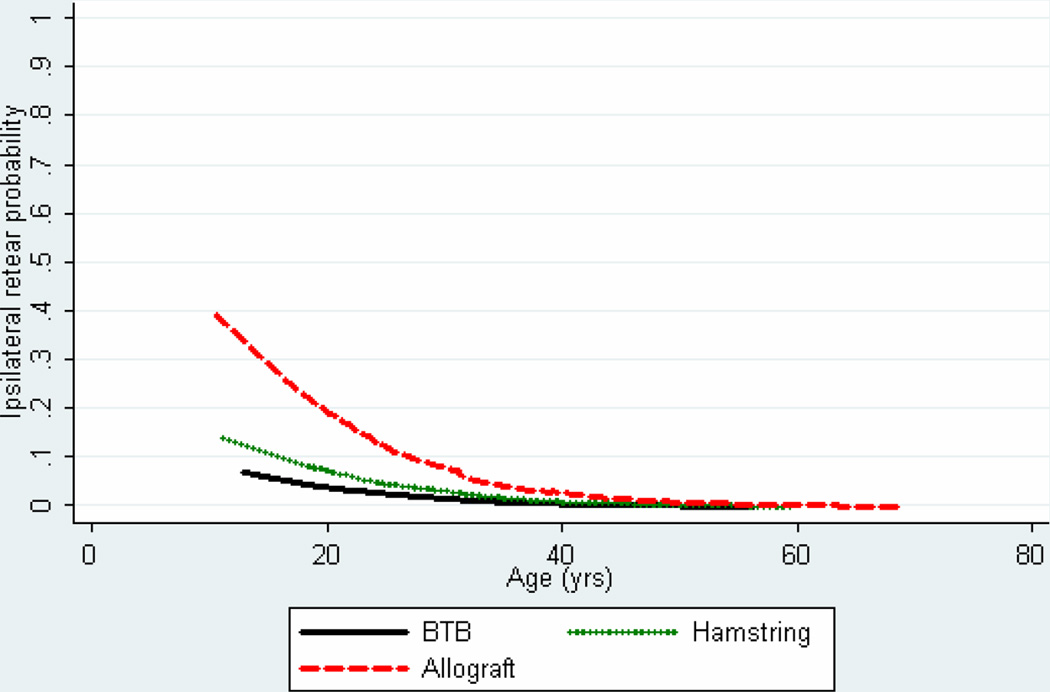
Odds ratios for the tested variables are summarized in Table 2. The odds of an ipsilateral retear were not significantly different for hamstring autograft (odds ratio [OR]=1.60; 95% CI: 0.89–2.90; p=0.12), but were 5.2 times greater for an allograft (OR=5.20; 95% CI: 2.60–10.44; p<0.01) compared with a BTB autograft (reference group). The odds of an ipsilateral retear decreased by 0.09 for every yearly increase in age (OR=0.91; 95% CI: 0.87–0.94; p<0.01) and increased by 0.11 for every increased point on the Marx activity score (OR=1.11; 95% CI: 1.03–1.20; p< 0.01). The odds of retear were not significantly different between sex, smoking status, sport played, medial or lateral meniscus tear status, or site (p>0.05). Figure 2 shows the probability of a graft tear by graft type as age increases.
Table 2.
Odds Ratios for Ipsilateral Graft Tear
| Odds Ratio |
SE | P value |
95% Conf. Interval |
||
|---|---|---|---|---|---|
| Graft type | |||||
| BTB autograft | Reference | ||||
| Hamstring autograft | 1.60 | 0.48 | 0.12 | 0.89 | 2.90 |
| Allograft | 5.20 | 1.84 | <0.01 | 2.60 | 10.44 |
| Age (years) | 0.91 | 0.02 | <0.01 | 0.87 | 0.94 |
| Marx activity score (time zero) | 1.11 | 0.04 | <0.01 | 1.03 | 1.20 |
| Sport played | |||||
| Did not return to sport | Reference | ||||
| Football | 2.34 | 2.53 | 0.43 | 0.28 | 19.37 |
| Basketball | 1.37 | 1.47 | 0.77 | 0.17 | 11.11 |
| Soccer | 2.29 | 2.43 | 0.44 | 0.28 | 18.40 |
| Other | 1.81 | 1.90 | 0.57 | 0.23 | 14.13 |
| Sex | |||||
| Male | Reference | ||||
| Female | 0.79 | 0.18 | 0.31 | 0.50 | 1.25 |
| Smoking status | |||||
| Never smoked | Reference | ||||
| Quit | 0.55 | 0.34 | 0.33 | 0.17 | 1.83 |
| Current smoker | 1.25 | 0.62 | 0.65 | 0.47 | 3.31 |
| Meniscal tear status | |||||
| No medial meniscus tear | Reference | ||||
| Medial meniscus tear | 1.03 | 0.25 | 0.89 | 0.64 | 1.67 |
| No lateral meniscus tear | Reference | ||||
| Lateral meniscus tear | 0.74 | 0.16 | 0.17 | 0.48 | 1.14 |
| Consortium site | |||||
| Site 1 | Reference | ||||
| Site 2 | 0.78 | 0.26 | 0.45 | 0.40 | 1.50 |
| Site 3 | 1.00 | 0.31 | 0.99 | 0.55 | 1.82 |
| Site 4 | 0.25 | 0.26 | 0.19 | 0.03 | 1.93 |
| Site 5 | 0.50 | 0.23 | 0.13 | 0.20 | 1.22 |
| Site 6 | 0.96 | 0.48 | 0.94 | 0.37 | 2.53 |
| Site 7 | 1.10 | 0.59 | 0.85 | 0.39 | 3.12 |
Key: Bolded values indicate statistical significance.
ACL, anterior cruciate ligament; BTB, bone-patellar tendon-bone.
Figure 2.
Probability of retear as age increases by graft type.
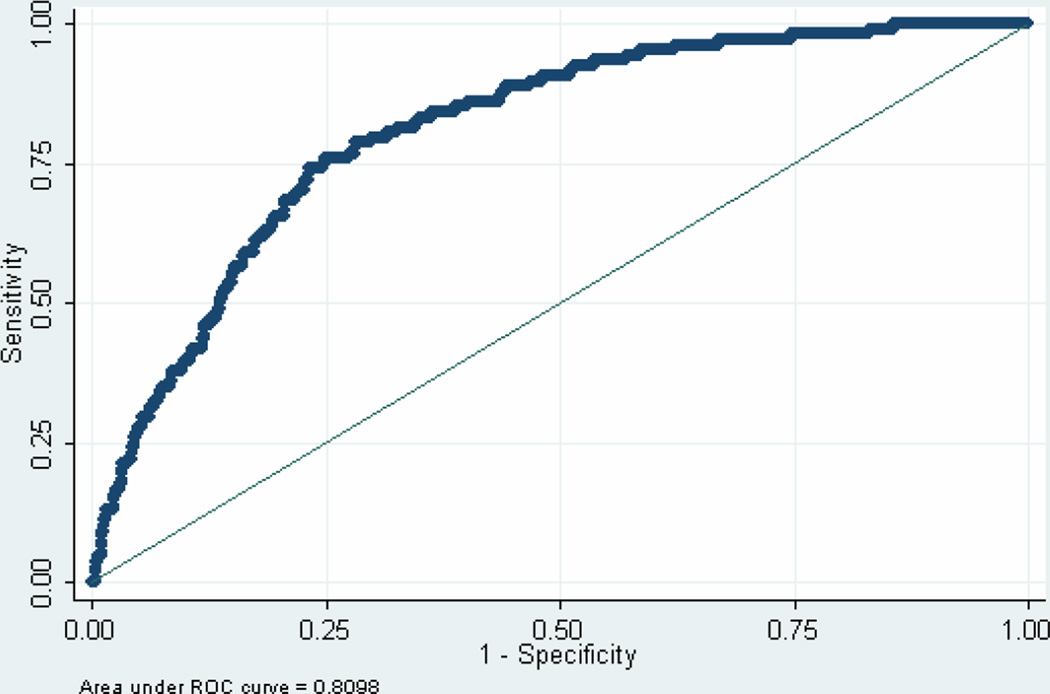
The fit of the model was deemed adequate both graphically, by evaluating the area under the receiver operating characteristic (ROC) curve (0.81; Figure 3), and statistically, by the Hosmer-Lemeshow goodness-of-fit test (p=0.82).
Figure 3.
ROC curve for ipsilateral graft tear logistic regression model.
Risk Factors of Contralateral ACL Tear
Odds ratios for the tested variables are summarized in Table 3. Lower age and higher activity level were found to be significant risk factors for tearing the contralateral ACL. The odds of a contralateral ACL tear decreased by 0.04 for every yearly increase in age (OR=0.96; 95% CI: 0.93–0.99; p=0.04) and increased by 0.12 for every increased point on the Marx activity score (OR=1.12; 95% CI: 1.04–1.22; p<0.01). The odds of a contralateral ACL tear were not significantly different as a function of sex, smoking status, sport played, graft type, or medial or lateral meniscal tear status (p>0.05).
Table 3.
Odds Ratios for Contralateral ACL Tear
| Odds Ratio |
SE | P value |
95% Conf. Interval |
||
|---|---|---|---|---|---|
| Graft type | |||||
| BTB autograft | Reference | ||||
| Hamstring autograft | 0.99 | 0.35 | 0.98 | 0.50 | 1.97 |
| Allograft | 0.53 | 0.27 | 0.22 | 0.19 | 1.45 |
| Age (years) | 0.96 | 0.02 | 0.04 | 0.93 | 0.99 |
| Marx activity score (time zero) | 1.12 | 0.05 | <0.01 | 1.04 | 1.22 |
| Sport played | |||||
| Did not return to sport | Reference | ||||
| Football | 1.15 | 0.97 | 0.87 | 0.22 | 5.96 |
| Basketball | 1.19 | 0.94 | 0.82 | 0.25 | 5.61 |
| Soccer | 0.98 | 0.79 | 0.98 | 0.20 | 4.72 |
| Other | 0.68 | 0.53 | 0.62 | 0.15 | 3.14 |
| Sex | |||||
| Male | Reference | ||||
| Female | 1.52 | 0.40 | 0.11 | 0.91 | 2.54 |
| Smoking status | |||||
| Never smoked | Reference | ||||
| Quit | 0.92 | 0.50 | 0.88 | 0.32 | 2.67 |
| Current smoker | 0.80 | 0.49 | 0.71 | 0.24 | 2.67 |
| Meniscal tear status | |||||
| No medial meniscus tear | Reference | ||||
| Medial meniscus tear | 1.14 | 0.29 | 0.60 | 0.70 | 1.87 |
| No lateral meniscus tear | Reference | ||||
| Lateral meniscus tear | 0.86 | 0.20 | 0.54 | 0.54 | 1.37 |
| Consortium site | |||||
| Site 1 | Reference | ||||
| Site 2 | 1.29 | 0.44 | 0.45 | 0.67 | 2.50 |
| Site 3 | 1.45 | 0.53 | 0.31 | 0.71 | 2.98 |
| Site 4 | 0.40 | 0.42 | 0.38 | 0.05 | 3.08 |
| Site 5 | 0.56 | 0.26 | 0.21 | 0.22 | 1.40 |
| Site 6 | 1.24 | 0.65 | 0.69 | 0.44 | 3.49 |
| Site 7 | 0.42 | 0.43 | 0.40 | 0.05 | 3.20 |
Key: Bolded values indicate statistical significance.
ACL, anterior cruciate ligament; BTB, bone-patellar tendon-bone.
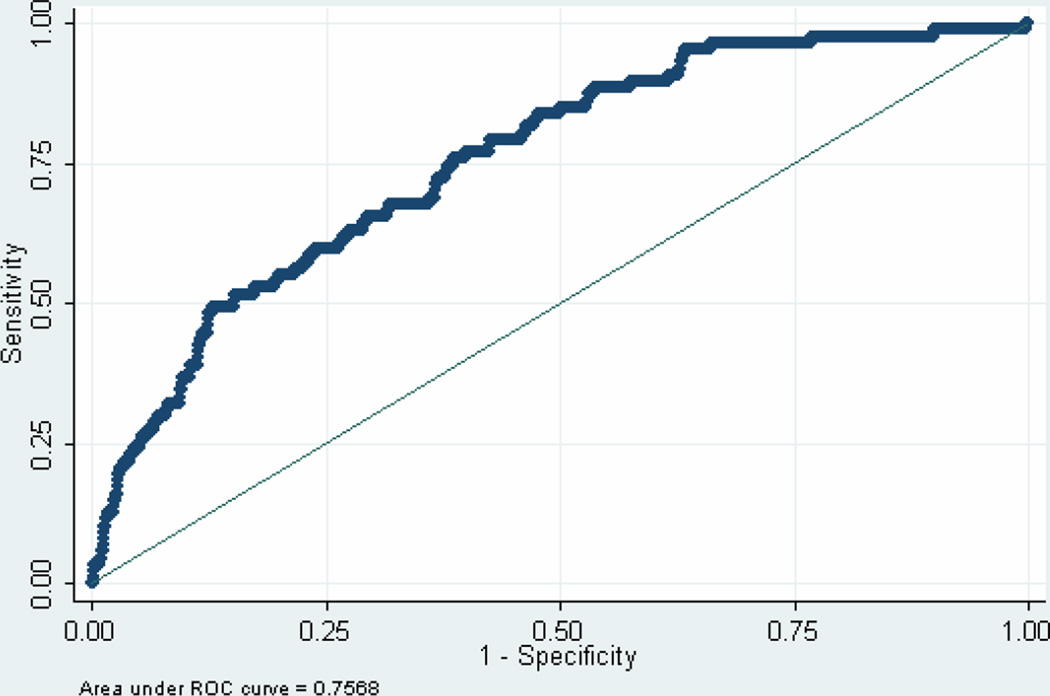
The fit of the model was deemed adequate both graphically, by evaluating the area under the ROC curve (0.76; Figure 4), and statistically, by the Hosmer-Lemeshow goodness-of-fit test (p=0.37).
Figure 4.
ROC curve for contralateral ACL tear logistic regression model.
DISCUSSION
Controlling for multiple patient and surgical-related factors, this study found that the risk of tearing a primary ACLR within 2 years was significantly influenced by younger age, higher activity level, and allograft use. Similarly, younger age and high activity level were found to be significant risk factors for tearing a contralateral native ACL within 2 years of surgically repairing the other one. A tear of an otherwise successful ACLR is not only frustrating to all parties involved, but often necessitates a revision ACLR, which subjects the patient to additional expense, surgical risk, physical therapy and time away from athletic activity. It has also been demonstrated that revision ACLRs have inferior results to primary reconstructions (12,40,64). Understanding the risk of reinjury is important in order to appropriately counsel patients regarding expected long-term results as well as potential reduction of risk by modifying one or more risk factors (10,16).
Ipsilateral ACL
Allograft versus Autograft
In this study, 3.2% of BTB autografts tore, 4.6% of hamstring autografts tore, and 6.9% of allografts tore. When controlling for other risk factors (i.e., age, sex, Marx activity) allograft use (compared with BTB autograft) was a significant predictor for ACL graft tears within 2 years of follow-up. This was most clinically relevant in the younger age group. A review of Figure 2 demonstrates that with increasing age, the clinical significance of allograft versus autograft tear risk decreases such that by the mid-30s it appears there is no clinically significant difference between the grafts. Allograft use in ACLR has been reported to be a reasonable option (11,47,54,62). It has been reported by others that allograft ACLRs have a high retear risk (8,9,11,15,26,28,44,49,55,57). More recently, several studies have reported that non-irradiated / non-chemically treated allografts can have similar results to those of autograft (21,29–31,38,39). In this cohort, the use of allograft tissue (as well as youth and high activity) was a predictor of graft tear in the early time frame. Many of the grafts in this cohort had low-dose irradiation with the goal of sterilizing surface contaminants. The level of irradiation to achieve surface sterilization is much lower than that required to sterilize the entire graft of possible donor prion/viral infection. The clinical significance of low-dose irradiation versus no irradiation has not been well studied. Studies have demonstrated in animal models that allografts biologically incorporate into the joint less readily than autografts (45,53). The clinical significance of this is unclear. Other studies have shown that fresh-frozen, non-irradiated allografts have a retear risk similar to that of autografts (25,29,36,58,59). However, these studies did not have large numbers of young highly active patients in the allograft group. A limitation of our paper is that we did not control for the allograft variables of donor age, donor sex, anatomic location, irradiation status, processing type, storage length, or storage method. Thus, our results cannot be extrapolated to all allografts. Further research into the influence of donor characteristics, processing techniques, tissue type and recipient characteristics on allograft ACLR outcomes is needed.
Age and Activity
Younger age and higher activity at index ACLR were highly significant predictors of graft tear. The odds of retear decreased by 9% for each year increase in age and increased by 11% for each increase of a point on the Marx activity scale, which has a range of 0 to 16. We suspect that return to activity is the driver of both these findings. This study utilized the Marx activity level at the index ACLR, which has been shown to be the most powerful predictor of activity level at two years (14). These findings are consistent with those reported by Kamien et al (27). These findings indicate that any future analysis of predictors of graft tear should control level of activity to which the subject returned (6,19). The Swedish (2) and Norwegian (46) registries did control for age within their analyses, and the Norwegian registry likewise confirmed younger age as a major risk factor for retear. Neither registry included activity level in its model.
Sex
Although a strong predictor of native ACL injury, female sex was not found to be a risk factor for tear of an ACL graft in this cohort. This matches findings in other reports, (7,17,52) including both Swedish and Norwegian registries (2,46). A potential confounder of this analysis is that if return to activity is the strongest predictor of graft tear and women return to a lower level of activity, this may mask an inherent sex risk factor. Very few studies control for differences in return to activity levels between the sexes when evaluating risk of retear after ACLR. In many studies, women have an absolute higher risk of retear, but this typically does not reach statistical significance (7,17,51). In multivariable analysis, activity level was controlled for and sex was not a risk factor for re-injury of either knee. The findings of the current study, along with the Swedish and Norwegian registries, have shown through multivariable analysis in over 25,000 ACLR patients that sex is not a risk factor for ACLR re-injury.
Sport Played
We attempted to identify whether the sport played at index injury was a risk factor for graft retear. As seen in Table 1, the percent of retear in the no-sport group was 1%, whereas patients who played American football, soccer, and basketball had retears of 8.9%, 7.1%, and 4.0%, respectively. This corresponds well with reports in the literature that cutting sports such as soccer, basketball, and football have high rates of ACL injuries (1,5). Type of sport was not analyzed in the Swedish and Norwegian registry analyses.
Meniscal Tear Status
In our study we defined meniscal tear as a complete tear and compared these subjects to the partial/no tear group. With these definitions, we found that meniscal status had no effect on the risk of graft retear. We did not separate repaired versus partial meniscectomies within the tear group. Further study into the influence of repairing meniscal tears on the risk of retear would be of interest.
Contralateral ACL Tears
To our knowledge, this is only the second multivariable analysis of risk factors for the contralateral normal ACL tear (3). The finding that age and activity at index ACLR were risk factors for contralateral ACL injury corresponds well with reports in the literature for risk factors for first-time ACL tears (1,3,5). Again, this likely indicates that return to a high Marx activity level is a major risk factor that drives these findings, as both age and activity level at index ACLR likely correlate with returning to a high level of activity after the reconstruction. Unfortunately the study did not identify any modifiable risk factors for athletes of cutting sports. However, further investigation of anatomic and neuromuscular risk factors is required.
Comparison with Scandinavian Registries
There are many similarities between the current study and studies based on the Scandinavian registries (2,3,18,46), including prospective data collection, overlapping time periods of enrollment, near-equivalent sex distribution, definition of re-injury as revision ACLR, and most important, the use of multivariable analysis in order to control for confounding factors. Two results are consistent among all three studies: that younger age is a primary risk factor for revision ACLR and that gender is not a risk factor. Whether a hamstring autograft has a higher risk of re-injury in the younger population is discordant between the Swedish (no difference) versus Norwegian (hamstring higher risk) registries. A recent study showed a significantly lower risk of graft tear for BTB autografts; 4.2% of hamstring autografts were expected to need a revision compared with 2.8% of BTB autografts (18). These percentages were similar to those found in the present study; however, similar to the Swedish registry, this study failed to find a higher risk of re-injury using a hamstring autograft (compared with a BTB autograft). A possible explanation of differing results regarding hamstring retear risk may be the size of the hamstring construct used. Two recent studies have shown that size of the graft may be a risk factor for retear (33,35). Further investigation into factors influencing retears of hamstring grafts is warranted.
There are also unique aspects of each study, as the risk factors explored between studies were different. The Swedish registry uniquely evaluated graft width (no difference), single versus double bundle (no difference), femoral fixation (no difference), and time from initial injury to primary ACLR (no difference). They found that tibial fixation and articular cartilage injury significantly influenced the risk of early revision ACLR. Both BMI and meniscus injury were evaluated by both registries and shown not to be a risk factor. Unique factors that were controlled for in the current study included sport played, consortium site, and smoking status. Activity level was measured and accounted for in this study, while activity level was not evaluated in the two other studies. In this study we found that the higher the baseline activity level, the greater the risk of revision ACLR.
CONCLUSIONS
Age and activity at index ACLR were predictors of graft tear as well as contralateral native ACL injury. Allograft use was a predictor of subsequent graft failure after ACLR. This was most clinically significant in younger patients. Female sex, sport played, and meniscal injury were not risk factors for graft tear or contralateral ACL tear. Future studies reporting ACLR failure must control for age and, if possible, activity level, since three prospective multicenter studies with over 25,000 ACLR all agree age is the major risk factor. Previous literature not controlling for age should be viewed cautiously.
What is known about this subject?
Anterior cruciate ligament (ACL) re-injury results in worse outcomes and increases risk of post-traumatic osteoarthritis.
What this study adds to existing knowledge
Younger age, higher activity level, and allograft graft type were predictors of increased odds of ipsilateral graft failure. Higher activity and younger age were found to be risk factors in contralateral ACL tears.
REFERENCES
- 1.Agel J, Arendt EA, Bershadsky B. Anterior cruciate ligament injury in national collegiate athletic association basketball and soccer: a 13-year review. Am J Sports Med. 2005;22(4):524–530. doi: 10.1177/0363546504269937. [DOI] [PubMed] [Google Scholar]
- 2.Andernord D, Björnsson H, Petzold M, Eriksson B, Forssblad M, Karlsson J, Samuelsson K. Surgical predictors of early revision surgery after anterior cruciate ligament reconstruction: results from the Swedish National Knee Ligament Register on 13,102 patients. Am J Sports Med. 2014;42(7):1574–1582. doi: 10.1177/0363546514531396. [DOI] [PubMed] [Google Scholar]
- 3.Andernord D, Desai N, Bjornsson H, Gillen S, Karlsson J, Samuelsson K. Predictors of contralateral anterior cruciate ligament reconstruction: a cohort study of 9061 patients with 5-year follow-up. Am J Sports Med. 2015;43(2):295–302. doi: 10.1177/0363546514557245. [DOI] [PubMed] [Google Scholar]
- 4.Anderson AF, Dome DC, Gautam S, et al. Correlation of anthropometric measurements, strength, anterior cruciate ligament size, and intercondylar notch characteristics to sex differences in anterior cruciate ligament tear rates. Am J Sports Med. 2001;29(1):58–66. doi: 10.1177/03635465010290011501. [DOI] [PubMed] [Google Scholar]
- 5.Arendt E, Dick R. Knee injury patterns among men and women in collegiate basketball and soccer. NCAA data and review of literature. Am J Sports Med. 1995;23(6):694–701. doi: 10.1177/036354659502300611. [DOI] [PubMed] [Google Scholar]
- 6.Barber-Westin SD, Noyes FR. Objective criteria for return to athletics after anterior cruciate ligament reconstruction and subsequent reinjury rates: a systematic review. Phys Sportsmed. 2011;39(3):100–110. doi: 10.3810/psm.2011.09.1926. [DOI] [PubMed] [Google Scholar]
- 7.Barber-Westin SD, Noyes RF, Andrews M. A rigorous comparison between the sexes of results and complications after anterior cruciate ligament reconstruction. Am J Sports Med. 1997;25(4):514–526. doi: 10.1177/036354659702500415. [DOI] [PubMed] [Google Scholar]
- 8.Barrett GR, Luber K, Replogle WH, Manley JL. Allograft anterior cruciate ligament reconstruction in the young, active patient: Tegner activity level and failure rate. Arthroscopy. 2010;26(12):1593–1601. doi: 10.1016/j.arthro.2010.05.014. [DOI] [PubMed] [Google Scholar]
- 9.Borchers JR, Pedroza A, Kaeding C. Activity level and graft type as risk factors for anterior cruciate ligament graft failure: a case-control study. Am J Sports Med. 2009;37(12):2362–2367. doi: 10.1177/0363546509340633. [DOI] [PubMed] [Google Scholar]
- 10.Caraffa A, Cerulli G, Projetti M, et al. Prevention of anterior cruciate ligament injuries in soccer. A prospective controlled study of proprioceptive training. Knee Surg Sports Traumatol Arthrosc. 1996;4(1):19–21. doi: 10.1007/BF01565992. [DOI] [PubMed] [Google Scholar]
- 11.Chang SK, Egami DK, Saieb MD, et al. Anterior cruciate ligament reconstruction: allograft versus autograft. Arthroscopy. 2003;19(5):453–462. doi: 10.1053/jars.2003.50103. [DOI] [PubMed] [Google Scholar]
- 12.Chen JL, Allen CR, Stephens TE, Haas AK, Huston LJ, Wright RW, Feeley BT. Multicenter ACL Revision Study (MARS) Group. Differences in mechanisms of failure, intraoperative findings, and surgical characteristics between single- and multiple-revision ACL reconstructions: a MARS cohort study. Am J Sports Med. 2013;41(7):1571–1578. doi: 10.1177/0363546513487980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Crawford SN, Waterman BR, Lubowitz JH. Long-term failure of anterior cruciate ligament reconstruction. Arthroscopy. 2013;29(9):1566–1571. doi: 10.1016/j.arthro.2013.04.014. [DOI] [PubMed] [Google Scholar]
- 14.Dunn WR, Spindler K MOON Consortium. Predictors of activity level two years after ACL reconstruction: a multicenter ACLR cohort study. Am J Sports Med. 2010;38(10):2040–2050. doi: 10.1177/0363546510370280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ellis HB, Matheny LM, Briggs KK, Pennock AT, Steadman JR. Outcomes and revision rate after bone-patellar tendon-bone allograft versus autograft anterior cruciate ligament reconstruction in patients aged 18 years or younger with closed physes. Arthroscopy. 2012;28(12):1819–1825. doi: 10.1016/j.arthro.2012.06.016. [DOI] [PubMed] [Google Scholar]
- 16.Ettlinger CF, Johnson RJ, Shealy JE. A method to help reduce the risk of serious knee sprains incurred in alpine skiing. Am J Sports Med. 1995;23(5):531–537. doi: 10.1177/036354659502300503. [DOI] [PubMed] [Google Scholar]
- 17.Ferrari JD, Back BR, Jr, Bush-Joseph CA, et al. Anterior cruciate ligament reconstruction in men and women: an outcome analysis comparing gender. Arthroscopy. 2001;17(6):588–596. doi: 10.1053/jars.2001.24686. [DOI] [PubMed] [Google Scholar]
- 18.Gifstad T, Foss OA, Engebretsen L, Lind M, Forssblad M, Albrektsen G, Drogset JO. Lower risk of revision with patellar tendon autografts compared with hamstring autografts: a registry study based on 45,998 primary ACL reconstructions in Scandinavia. Am J Sports Med. 2014;42(10):2319–2328. doi: 10.1177/0363546514548164. [DOI] [PubMed] [Google Scholar]
- 19.Gobbi A, Francisco R. Factors affecting return to sports after anterior cruciate ligament reconstruction with patellar tendon and hamstring graft: a prospective clinical investigation. Knee Surg Tramatol Arthrosc. 2006;14(10):1021–1028. doi: 10.1007/s00167-006-0050-9. [DOI] [PubMed] [Google Scholar]
- 20.Goddard M, Salmon L, Waller A, Papapetros E, Pinczewski LA. Incidence of graft rupture 15 years after bilateral anterior cruciate ligament reconstructions: a case-control study. Bone Joint J. 2013;95-B(6):798–802. doi: 10.1302/0301-620X.95B6.30841. [DOI] [PubMed] [Google Scholar]
- 21.Guo L, Yang L, Duan XJ, He R, Chen GX, Wang FY, Zhang Y. Anterior cruciate ligament reconstruction with bone-patellar tendon-bone graft: comparison of autograft, fresh-frozen allograft, and γ-irradiated allograft. Arthroscopy. 2012;28(2):211–217. doi: 10.1016/j.arthro.2011.08.314. [DOI] [PubMed] [Google Scholar]
- 22.Gwinn DE, Wilckens JH, McDevitt Er, et al. The relative incidence of anterior cruciate ligament injury in men and women at the United States Naval Academy. Am J Sports Med. 2000;28(1):98–102. doi: 10.1177/03635465000280012901. [DOI] [PubMed] [Google Scholar]
- 23.Hewett TE, Di Stasi SL, Myer GD. Current concepts for injury prevention in athletes after anterior cruciate ligament reconstruction. Am J Sports Med. 2013;41(1):216–224. doi: 10.1177/0363546512459638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hewett TE, Lindenfeld TN, Riccobene JV, et al. The effect of neuromuscular training on the incidence of knee injury in female athletes. A prospective study. Am J Sports Med. 1999;27(6):699–706. doi: 10.1177/03635465990270060301. [DOI] [PubMed] [Google Scholar]
- 25.Indelicato PA, Linton RC, Huegel M. The results of fresh-frozen patellar tendon allografts for chronic anterior cruciate ligament deficiency of the knee. Am J Sports Med. 1992;20(2):118–121. doi: 10.1177/036354659202000204. [DOI] [PubMed] [Google Scholar]
- 26.Kaeding CC, Aros B, Pedroza A, Pifel E, Amendola A, Andrish JT, Dunn WR, Marx RG, McCarty EC, Parker RD, Wright RW, Spindler KP. Allograft versus autograft anterior cruciate ligament reconstruction: predictors of failure from a MOON prospective longitudinal cohort. Sports Health. 2011;3(1):73–81. doi: 10.1177/1941738110386185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kamien PM, Hydrick JM, Replogle WH, Go LT, Barrett GR. Age, graft size, and Tegner activity level as predictors of failure in anterior cruciate ligament reconstruction with hamstring autograft. Am J Sports Med. 2013;41(8):1808–1812. doi: 10.1177/0363546513493896. [DOI] [PubMed] [Google Scholar]
- 28.Kraeutler MJ, Bravman JT, McCarty EC. Bone-patellar tendon-bone autograft versus allograft in outcomes of anterior cruciate ligament reconstruction: a meta-analysis of 5182 patients. Am J Sports Med. 2013;41(10):2439–2448. doi: 10.1177/0363546513484127. [DOI] [PubMed] [Google Scholar]
- 29.Krych AJ, Jackson JD, Hoskin TL, et al. A meta-analysis of patellar tendon autograft versus patellar tendon allograft in anterior cruciate ligament reconstruction. Arthroscopy. 2008;24(3):292–298. doi: 10.1016/j.arthro.2007.08.029. [DOI] [PubMed] [Google Scholar]
- 30.Lamblin CJ, Waterman BR, Lubowitz JH. Anterior cruciate ligament reconstruction with autografts compared with non-irradiated, non-chemically treated allografts. Arthroscopy. 2013;29(6):1113–1122. doi: 10.1016/j.arthro.2013.01.022. [DOI] [PubMed] [Google Scholar]
- 31.Lawhorn KW, Howell SM, Traina SM, Gottlieb JE, Meade TD, Freedberg HI. The effect of graft tissue on anterior cruciate ligament outcomes: a multicenter, prospective, randomized controlled trial comparing autograft hamstrings with fresh-frozen anterior tibialis allograft. Arthroscopy. 2012;28(8):1079–1086. doi: 10.1016/j.arthro.2012.05.010. [DOI] [PubMed] [Google Scholar]
- 32.Ma Y, Ao YF, Yu JK, Dai LH, Shao ZX. Failed anterior cruciate ligament reconstruction: analysis of factors leading to instability after primary surgery. Chin Med J (Engl) 2013;126(2):280–285. [PubMed] [Google Scholar]
- 33.Magnussen R, Lawrence J, West R, Toth A, Taylor D, Garrett W. Graft size and patient age are predictors of early revision after anterior cruciate ligament reconstruction with hamstring autograft. Arthroscopy. 2012;28(4):526–531. doi: 10.1016/j.arthro.2011.11.024. [DOI] [PubMed] [Google Scholar]
- 34.Magnussen RA, Taylor DC, Toth AP, Garrett WE. ACL graft failure location differs between allografts and autografts. Sports Med Arthrosc Rehabil Ther Technol. 2012;4(1):22. doi: 10.1186/1758-2555-4-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mariscalco MW, Flanigan DC, Mitchell J, Pedroza AD, Jones MH, Andrish JT, Parker RD, Kaeding CC, Magnussen RA. The influence of hamstring autograft size on patient-reported outcomes and risk of revision after anterior cruciate ligament reconstruction: a Multicenter Orthopaedic Outcomes Network (MOON) cohort study. Arthroscopy. 2013;29(12):1948–1953. doi: 10.1016/j.arthro.2013.08.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mariscalco MW, Magnussen RA, Mehta D, Hewett TE, Flanigan DC, Kaeding CC. Autograft versus nonirradiated allograft tissue for anterior cruciate ligament reconstruction: a systematic review. Am J Sports Med. 2014;42(2):492–499. doi: 10.1177/0363546513497566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Marx RG, Stump TJ, Jones EC, et al. Development and evaluation of an activity rating scale for disorders of the knee. Am J Sports Med. 2001;29(2):213–218. doi: 10.1177/03635465010290021601. [DOI] [PubMed] [Google Scholar]
- 38.Mayr HO, Willkomm D, Stoehr A, Schettle M, Suedkamp NP, Bernstein A, Hube R. Revision of anterior cruciate ligament reconstruction with patellar tendon allograft and autograft: 2- and 5-year results. Arch Orthop Trauma Surg. 2012;132(6):867–874. doi: 10.1007/s00402-012-1481-z. [DOI] [PubMed] [Google Scholar]
- 39.Mehta VM, Mandala C, Foster D, Petsche TS. Comparison of revision rates in bone-patella tendon-bone autograft and allograft anterior cruciate ligament reconstruction. Orthopedics. 2010;33(1):12. doi: 10.3928/01477447-20091124-15. [DOI] [PubMed] [Google Scholar]
- 40.Morgan JA, Dahm D, Levy B, Stuart MJ MARS Study Group. Femoral tunnel malposition in ACL revision reconstruction. J Knee Surg. 2012;25(5):361–368. doi: 10.1055/s-0031-1299662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Myer GD, Martin L, Jr, Ford KR, Paterno MV, Schmitt LC, Heidt RS, Jr, Colosimo A, Hewett TE. No association of time from surgery with functional deficits in athletes after anterior cruciate ligament reconstruction: evidence for objective return-to-sport criteria. Am J Sports Med. 2012;40(10):2256–2263. doi: 10.1177/0363546512454656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Oates KM, Van Eenenaam DP, Briggs K, et al. Comparative injury rates of uninjured, anterior cruciate ligament-deficient, and reconstructed knees in a skiing population. Am J Sports Med. 1999;27(5):606–610. doi: 10.1177/03635465990270051001. [DOI] [PubMed] [Google Scholar]
- 43.Orchard J, Seward H, McGivern J, et al. Intrinsic and extrinsic risk factors for anterior cruciate ligament injury in Australian footballers. Am J Sports Med. 2001;29(2):196–200. doi: 10.1177/03635465010290021301. [DOI] [PubMed] [Google Scholar]
- 44.Pallis M, Svoboda SJ, Cameron KL, Owens BD. Survival comparison of allograft and autograft anterior cruciate ligament reconstruction at the United States Military Academy. Am J Sports Med. 2012;40(6):1242–1246. doi: 10.1177/0363546512443945. [DOI] [PubMed] [Google Scholar]
- 45.Papageorgiou CD, Ma CB, Abramowitch SD, et al. A multidisciplinary study of the healing of an intraarticular anterior cruciate ligament graft in a goat model. Am J Sports Med. 2001;29(5):620–626. doi: 10.1177/03635465010290051501. [DOI] [PubMed] [Google Scholar]
- 46.Persson A, Fjeldsgaard K, Gjertsen J, Kjellsen A, Engebretsen L, Hole R, Fevand J. Increased risk of revision with hamstring tendon grafts compared with patellar tendon grafts after anterior cruciate ligament reconstruction: a study of 12,643 patients from the Norwegian Anterior Cruciate Ligament Registry, 2004 – 2012. Am J Sports Med. 2014;42(2):285–291. doi: 10.1177/0363546513511419. [DOI] [PubMed] [Google Scholar]
- 47.Poehling GG, Curl WW, Lee CA, et al. Analysis of outcomes of anterior cruciate ligament repair with 5-year follow-up: allograft versus autograft. Arthroscopy. 2005;21(7):774–785. doi: 10.1016/j.arthro.2005.04.112. [DOI] [PubMed] [Google Scholar]
- 48.Rahr-Wagner L, Thillemann TM, Pedersen AB, Lind MC. Increased risk of revision after anteromedial compared with transtibial drilling of the femoral tunnel during primary anterior cruciate ligament reconstruction: results from the Danish Knee Ligament Reconstruction. Arthroscopy. 2013;29(1):98–105. doi: 10.1016/j.arthro.2012.09.009. [DOI] [PubMed] [Google Scholar]
- 49.Rappe M, Horodyski M, Meister K, et al. Nonirradiated versus irradiated Achilles allograft: in vivo failure comparison. Am J Sports Med. 2007;35(10):1653–1658. doi: 10.1177/0363546507302926. [DOI] [PubMed] [Google Scholar]
- 50.Rozzi SL, Lephart SM, Gear WS, et al. Knee joint laxity and neuromuscular characteristics of male and female soccer and basketball players. Am J Sport Med. 1999;27(3):312–319. doi: 10.1177/03635465990270030801. [DOI] [PubMed] [Google Scholar]
- 51.Ryan J, Magnussen R, Cox C, Hurbanek J, Flanigan D, Kaeding C. ACL reconstruction: do outcomes differ by sex? J Bone Joint Surg Am. 2014;96(6):507–512. doi: 10.2106/JBJS.M.00299. [DOI] [PubMed] [Google Scholar]
- 52.Salmon L, Russell V, Musgrove T, et al. Incidence and risk factors for graft rupture and contralateral rupture after anterior cruciate ligament reconstruction. Arthroscopy. 2005;21(8):948–957. doi: 10.1016/j.arthro.2005.04.110. [DOI] [PubMed] [Google Scholar]
- 53.Scheffler SU, Schmidt T, Gangey I, et al. Fresh-frozen free-tendon allografts versus autografts in anterior cruciate ligament reconstruction: delayed remodeling and inferior mechanical function during long-term healing in sheep. Arthroscopy. 2008;24(4):448–458. doi: 10.1016/j.arthro.2007.10.011. [DOI] [PubMed] [Google Scholar]
- 54.Shino KIM, Horibe S, Hamada M, Ono K. Reconstruction of the anterior cruciate ligament using allogenic tendon. Long-term follow-up. Am J Sports Med. 1990;18(5):457–465. doi: 10.1177/036354659001800502. [DOI] [PubMed] [Google Scholar]
- 55.Singhal MC, Gardiner JR, Johnson DL. Failure of primary anterior cruciate ligament surgery using anterior tibialis allograft. Arthroscopy. 2007;23(5):469–475. doi: 10.1016/j.arthro.2006.12.010. [DOI] [PubMed] [Google Scholar]
- 56.Spindler KP, Kuhn JE, Freedman KB, et al. Anterior cruciate ligament reconstruction autograft choice: bone-tendon-bone versus hamstring: does it really matter? A systematic review. Am J Sports Med. 2004;32(8):1986–1995. doi: 10.1177/0363546504271211. [DOI] [PubMed] [Google Scholar]
- 57.Stringham DR, Pelmas CJ, Burks RT, et al. Comparison of anterior cruciate ligament reconstructions using patellar tendon autograft or allograft. Arthroscopy. 1996;12(4):414–421. doi: 10.1016/s0749-8063(96)90034-1. [DOI] [PubMed] [Google Scholar]
- 58.Sun K, Zhang J, Wang Y, Xia C, Zhang C, Yu T, Tian S. Arthroscopic anterior cruciate ligament reconstruction with at least 2.5 years’ follow-up comparing hamstring tendon autograft and irradiated allograft. Arthroscopy. 2011;27(9):1195–1202. doi: 10.1016/j.arthro.2011.03.083. [DOI] [PubMed] [Google Scholar]
- 59.Sun K, Zhang J, Wang Y, Xia C, Zhang C, Yu T, Tian S. Arthroscopic reconstruction of the anterior cruciate ligament with hamstring tendon autograft and fresh-frozen allograft: a prospective, randomized controlled study. Am J Sports Med. 2011;39(7):1430–1438. doi: 10.1177/0363546511400384. [DOI] [PubMed] [Google Scholar]
- 60.Swärd P, Kostogiannis I, Roos H. Risk factors for a contralateral anterior cruciate ligament injury. Knee Surg Sports Traumatol Arthrosc. 2010;18(3):277–291. doi: 10.1007/s00167-009-1026-3. [DOI] [PubMed] [Google Scholar]
- 61.Tiamklang T, Sumanont S, Foocharoen T, Laopaiboon M. Double-bundle versus single-bundle reconstruction for anterior cruciate ligament rupture in adults. Cochrane Database Syst Rev. 2012;11:CD008413. doi: 10.1002/14651858.CD008413.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Van Eck CF, Schkrohowsky JG, Working ZM, Irrgang JJ, Fu FH. Prospective analysis of failure rate and predictors of failure after anatomic anterior cruciate ligament reconstruction with allograft. Am J Sports Med. 2012;40(4):800–807. doi: 10.1177/0363546511432545. [DOI] [PubMed] [Google Scholar]
- 63.Wright RW, Dunn WR, Amendola A, et al. Risk of tearing the intact anterior cruciate ligament in the contralateral knee and rupturing the anterior cruciate ligament graft during the first 2 years after anterior cruciate ligament reconstruction: a prospective MOON cohort study. Am J Sports Med. 2007;35(7):1131–1134. doi: 10.1177/0363546507301318. [DOI] [PubMed] [Google Scholar]
- 64.Wright RW, Gill CS, Chen L, Brophy RH, Matava MJ, Smith MV, Mall NA. Outcome of revision anterior cruciate ligament reconstruction: a systematic review. J Bone Joint Surg Am. 2012;94(6):531–536. doi: 10.2106/JBJS.K.00733. [DOI] [PMC free article] [PubMed] [Google Scholar]