Abstract
Context
This systematic review evaluated the evidence on the impact of contraceptive counseling provided in clinical settings on reproductive health outcomes to provide information to guide national recommendations on quality family planning services.
Evidence acquisition
Multiple databases were searched during 2010–2011 for peer-reviewed articles published in English from January 1985 through February 2011 describing studies that evaluated contraceptive counseling interventions in clinical settings. Studies were excluded if they focused primarily on prevention of HIV or sexually transmitted infections, focused solely on men, or were conducted outside the U.S., Canada, Europe, Australia, or New Zealand.
Evidence synthesis
The initial search identified 12,327 articles, of which 22 studies (from 23 articles) met the inclusion criteria. Six studies examined the impact of contraceptive counseling among adolescents, with four finding a significant positive impact on at least one outcome of interest. Sixteen studies examined the impact of counseling among adults or mixed populations (adults and adolescents), with 11 finding a significant positive impact on at least one outcome of interest.
Conclusions
Promising components of contraceptive counseling were identified despite the diversity of interventions and inability to compare the relative effectiveness of one approach versus another. The evidence base would be strengthened by improved documentation of counseling procedures; assessment of intervention implementation and fidelity to put study findings into context; and development and inclusion of more RCTs, studies conducted among general samples of women, and studies with sample sizes sufficient to detect important behavioral outcomes at least 12 months post-intervention.
Context
Unintended pregnancy rates in the U.S. remain high despite the wide variety of available contraceptive methods.1,2 Approximately 49% of pregnancies each year are unintended, with higher rates among women aged <25 years, members of some racial or ethnic minority groups, and those with lower incomes.1 Unintended pregnancy is preventable with correct and continued contraceptive use. An estimated 95% of unintended pregnancies occur among the one third of women at risk who did not use contraceptives at all during the month of conception or who used a method inconsistently or improperly.3 Contraceptive method choice also influences the likelihood of an unintended pregnancy, as some methods are more effective than others. Some of the most effective contraceptives, based on rates of pregnancy with typical use, are sterilization, intrauterine devices (IUDs), and implants (Tier 1 methods); and injectables, oral contraceptives, contraceptive patches, vaginal rings, and diaphragms (Tier 2 methods).4
Contraceptive counseling provided by trained health-care professionals may reduce unintended pregnancy rates by encouraging women, men, and couples to choose a method concordant with their goals and preferences, and use the chosen method correctly. Although provision of contraceptive counseling is considered a core women’s health competency for primary care providers,5,6 barriers to its provision have been reported. Examples include lack of knowledge, training, and comfort with contraceptive counseling; misguided assumptions about a patient’s pregnancy risk; reliance on patients to initiate discussions; limited time; and competing medical priorities.7 Providers and researchers also do not have clear guidance on what constitutes contraceptive counseling—for example, is provision of information alone sufficient, and what topics must be included?
The U.S. Preventive Services Task Force (USPSTF) defines behavioral counseling interventions in clinical care as those activities delivered by primary care clinicians and related healthcare staff that assist patients in adopting, changing, or maintaining behaviors proven to affect health outcomes and health status.8 However, specific activities that can facilitate effective contraceptive behaviors have not been described, nor is there clear evidence from past systematic reviews9,10 to formulate key components of effective contraceptive counseling interventions.
The objective of this systematic review was to summarize the evidence on the impact of contraceptive counseling provided in clinical settings on reproductive health outcomes including contraceptive behaviors to guide national recommendations on quality family planning services. The information was presented to an expert technical panel in May 2011 at a meeting convened by the Office of Population Affairs and CDC.
Evidence Acquisition
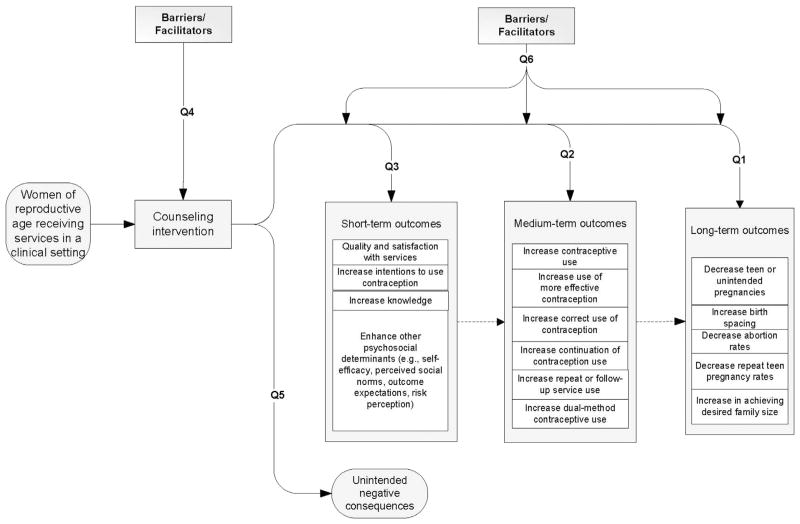
The methods for conducting this systematic review have been described elsewhere.11 In summary, six key questions were developed (Table 1) and an analytic framework was applied to show the relationships among the population of interest (women of reproductive age receiving services in a clinical setting); the intervention of interest (contraceptive counseling); and the short-, medium-, and long-term outcomes of interest (Figure 1). Search terms were identified (Appendix A), which were used to search multiple electronic databases during 2010–2011 to identify potential articles published from January 1985 through February 2011. A targeted search was rerun in March 2015 to identify newly published articles since the initial search. Studies were not considered if they focused primarily on prevention of HIV or sexually transmitted infections (STIs); focused solely on men; or were conducted outside the U.S., Europe, Australia, or New Zealand.
Table 1.
Key Questions for Systematic Review on Impact of Contraceptive Counseling in Clinical Settings
| Key question no. | Question |
|---|---|
| 1 | Is there a relationship between counseling and improved long-term outcomes of family planning services (e.g., decreased teen or unintended pregnancies, increased birth spacing, decreased abortion rates, decreased repeat teen pregnancy rates, or unintended pregnancy rates)? |
| 2 | Is there a relationship between counseling and improved medium-term outcomes of family planning services (e.g., increased contraceptive use, increased use of more effective contraception, increased correct use of contraception, increased continuation of contraception use, increased repeat or follow-up service use)? |
| 3 | Is there a relationship between counseling and improved short-term outcomes of family planning services (e.g., improved quality and satisfaction with service, strengthened social norms, improved intentions to use contraception, increased knowledge, enhanced other psychosocial determinants of contraceptive use)? |
| 4 | What are the barriers and facilitators for clinics to offering counseling in the family planning setting? |
| 5 | Are there any unintended negative consequences associated with counseling when used in the family planning setting? |
| 6 | What are the barriers and facilitators for clients to achieving positive outcomes after receiving counseling in the family planning setting? |
Note: Questions are put into context by the analytic framework presented in Figure 1.
Figure 1.
Analytic framework for systematic review on the impact of contraceptive counseling in clinical settings.
Note: Numbered lines map to key questions (Q). Dashed lines show logical relationships between outcomes, but these relationships were not assessed in this systematic review.
Selection of Studies
Retrieval and inclusion criteria identical across reviews in this series have been described elsewhere.11 Articles also must have evaluated a family planning counseling intervention in a clinic-based setting excluding school-based clinics. For the purpose of this review, we defined contraceptive counseling as an interactive process between provider and client intended to help the client achieve a reproductive health goal. This definition was developed after considering other counseling definitions from the USPSTF,8 the American Counseling Association,12 and a dictionary of public health terms and concepts.13
Some inclusion criteria were specific to key questions. For Questions 1–3, which sought to examine the relationships between contraceptive counseling and improved long-, medium-, and short-term outcomes, studies had to include a comparison group. Articles that described a multicomponent program (e.g., counseling in addition to a noncounseling component) had to report the impact of the counseling component independent of the noncounseling component. For Questions 4–6, which sought to examine unintended negative consequences and barriers and facilitators, articles had to describe a study that examined the impact of counseling on at least one outcome of interest and met the inclusion criteria for Key Questions 1–3.
Assessment of Study Quality and Synthesis of Data
The quality of each piece of evidence identified by the initial search was assessed using the grading system developed by the USPSTF.14 Each counseling intervention was also evaluated on its level of intensity using a definition developed for this review. Findings are reported separately for studies conducted among adolescents and those conducted among adults or mixed populations (adults and adolescents). Findings are also stratified by long-, medium-, and short-term outcomes. As a result, studies that examined multiple outcomes may be discussed more than once. Although short-term outcomes are fully described in the evidence table, they are not discussed in detail in the text. Summary measures of association were not computed across studies because of the diversity of the interventions, study designs, and populations. Articles published since the initial search were not incorporated into the evidence table because we wanted to only include information considered during the May 2011 expert technical panel to guide national recommendations on quality family planning services.
Evidence Synthesis
The initial search strategy identified 12,327 articles (Appendix B). After applying the retrieval criteria, 1,152 articles were reviewed more closely. Of these, 23 articles15–37 met the inclusion criteria and are summarized in detail in the evidence table (Appendix C). Findings from two studies29,30 are described together because they used the same sample of women. Excluded studies included review articles, those not relevant to the key questions, those conducted in developing nations, and those focusing primarily on HIV/AIDs or STI prevention. Of the 22 studies included in this review, six17,19,20,23,24,36 examined the impact of contraceptive counseling among adolescents, and 1615,16,18,21,22,25–35,37 (from 17 articles) examined the impact among adults or mixed populations (adults and adolescents). Although many studies were conducted among the general population of women seeking contraceptive services, five16,25,28,32,37 were conducted among postabortion samples, two22,31 were conducted among postpartum samples, and one33 was conducted among women seeking services at an STI clinic.
Adolescents
Of the six studies that examined the impact of contraceptive counseling among adolescents, two23,24 were RCTs rated as having moderate risk for bias, one36 was a prospective, nonrandomized controlled trial rated as having high risk for bias, and three17,19,20 were pre–post studies rated as having high risk for bias.
A variety of outcomes were examined, ranging from reducing unintended pregnancy to enhancing psychosocial determinants of contraceptive use (e.g., perceived benefits of contraception). Four studies19,20,24,36 examined long-term outcomes, six17,19,20,23,24,36 examined medium-term outcomes, and three23,24,36 examined short-term outcomes. Five19,20,23,24,36 of the six studies examined multiple outcomes. None of the studies reported barriers or facilitators for clinics or clients, but two studies17,19 reported on unintended negative consequences.
Sample sizes in the six studies ranged from 3920 to 1,59019 and all participants were aged 11–18 years. Four studies19,20,24,36 recruited participants from health clinics; the recruitment sites of the other two studies17,23 were not reported. A different model or approach to counseling was used in each of the six studies. Examples included use of peer providers,19 motivational interviewing and narrative therapy,20,24 a model based on a theory of goal achievement,23 and extensive follow-up telephone calls.24 Counseling interventions also varied in intensity; four17,19,24,36 were rated as moderate intensity, whereas two20,23 were rated as low intensity. Appendix C describes the details of each study; Table 2 summarizes findings by outcome of interest.
Table 2.
Summary of Impact of Contraceptive Counseling in Clinical Settings for Adolescents
| Reference | Quality | Intensity | Outcomes
|
Total outcomes with positive impact for study† |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Long-term
|
Medium-term
|
Short-term
|
||||||||||
| Decreased teen pregnancy rate |
Increased contraceptive use |
Increased use of more effective contraceptives |
Increased correct use of contraceptives |
Increased continuation of contraceptive use |
Increased repeat and follow-up service use |
Increased quality and satisfaction with service |
Increased knowledge |
Enhanced other psychosocial determinants of contraceptive use |
||||
| Berger (1987)17 | Level II-3; high risk for bias | Moderate | NA | ↑ | NA | NA | NA | NA | NA | NA | NA | 1/1 |
|
| ||||||||||||
| Brindis (2005)19 | Level II-3; high risk for bias | Moderate | ↑ | ↑ | ↑ | NA | NA | ↑ | NA | NA | NA | 4/4 |
|
| ||||||||||||
| Cowley (2002)20 | Level II-3; high risk for bias | Low | NA | * | * | NA | NA | NA | NA | NA | NA | 0/0 |
|
| ||||||||||||
| Hanna (1993)23 | Level I; moderate risk for bias | Low | NA | NA | NA | ↑ | NA | NA | NA | NA | ↔ | 1/2 |
|
| ||||||||||||
| Kirby (2010)24 | Level I; moderate risk for bias | Moderate | ↔ | ↔ | NA | ↔ | NA | ↔ | ↔ | NA | NA | 0/5 |
|
| ||||||||||||
| Winter (1991)36 | Level II-1; high risk for bias | Moderate | ↔ | ↑ | NA | NA | ↑ | NA | ↔ | ↑ | ↑ | 4/6 |
|
| ||||||||||||
| Total studies with positive impact† | 1/3 | 3/5 | 1/2 | 1/2 | 1/1 | 1/2 | 0/2 | 1/1 | 1/2 | |||
Note: Intensity of intervention defined as low (intervention took place during a single visit); moderate (intervention took place during more than one visit, but less frequently than weekly); or high (intervention took place weekly).
↑Statistically significant positive impact; ↓statistically significant negative impact; ↔ no evidence of a statistically significant impact.
No statistical testing conducted, but improvement observed.
Statistically significant.
NA, not assessed; UIP, unintended pregnancy.
Of the three adolescent studies19,24,36 that examined the impact of contraceptive counseling on long-term outcomes, one19 found a statistically significant positive impact of counseling on decreasing teen pregnancy. In this pre–post study of 1,590 sexually active youth recruited from one of five reproductive health clinics in California, female adolescents were followed for up to 36 months after receiving counseling from a peer provider at intake. Peer providers were used to enhance the quality of the provider–client relationship. Participants also received quarterly follow-up telephone calls to reinforce messages and answer questions. Female adolescents that received both the clinic and telephone counseling components had significantly (p<0.05) lower odds (OR=0.9, CI not reported) of a positive pregnancy test at any follow-up clinic visit than those who received only the clinic counseling component.19 The other two studies24,36 found no statistically significant effect of counseling on unintended pregnancy rates.
The six adolescent studies that examined the impact of contraceptive counseling on medium-term outcomes investigated a variety of outcomes. Of the five studies17,19,20,24,36 that examined contraceptive use (i.e., use of some method at a given point in time), three17,19,36 found a statistically significant impact of moderate-intensity counseling interventions. In one36 of these studies, a prospective, nonrandomized controlled trial of 1,256 female adolescents, significantly (p<0.05) more of those in the intervention group (who received a psychosocial counseling intervention that addressed peer pressure, parental involvement, and confidential services) were using some method of contraception at 6 months (97%) than those in the control group (92%) who received the standard of care. However, use at 12 months did not significantly differ between intervention (96%) and control (92%) participants. In the second study,17 which used a pre–post design, contraceptive use among 383 unmarried youth was examined before and after receiving a counseling intervention that included discussions on establishing sexual values, ability and right to refuse sexual activity, abstinence and alternative forms of intimacy, contraceptive methods, and consequences of unprotected sex. Among sexually active participants, contraceptive use at last intercourse significantly (p<0.001) increased from 22% (baseline) to 70% (follow-up) for female adolescents and from 34% to 85% for male adolescents; average follow-up was 7.8 months. The third study,19 which also used a pre–post design, found a significant impact of a peer provider counseling model in which intervention participants received quarterly follow-up telephone calls after receiving counseling from a peer provider at intake. Contraceptive use at last intercourse significantly (p<0.01) increased for female participants from first (61%) to last (74%) clinic visit, but no significant differences were found for male participants. The remaining two studies either found no statistically significant effect of counseling on contraceptive use24 or observed some uptake in contraceptive use but did not conduct statistical testing.20
Of two studies19,20 that examined use of more effective contraceptives (either shifting from using less effective to more effective methods or initiating methods with higher rates of typical use effectiveness), one19 found a statistically significant impact. In this pre–post study of peer provider counseling, female adolescents demonstrated significant (p<0.01) changes from first (10%) to last (49%) clinic visit in their use of effective contraceptives, defined as methods with <5% of women experiencing a contraceptive failure during the first year of typical use.19 The other study20 observed some uptake in the use of more-effective methods, but statistical testing was not conducted.
Two studies23,24 examined the impact of counseling interventions on correct use of contraceptives (e.g., taking all oral contraceptives on time), with one23 finding a statistically significant impact. In this RCT, 51 female adolescents seeking oral contraceptives for the first time were randomized to either receive a low-intensity counseling intervention based on a theory of goal achievement (n=26) or regular counseling services (n=25). Intervention participants demonstrated significantly (p<0.05) increased correct use of oral contraceptives (i.e., less frequently missed pills) at 3-month follow-up versus control group participants.23 The other study24 found no statistically significant effect of the counseling intervention on correct use of condoms, oral contraceptives, injectables, or patches.
One study36 examined continuation of contraceptive use (i.e., continued use of a selected method over time) and found a statistically significant impact. In this prospective, nonrandomized controlled trial that tested a counseling intervention that addressed peer pressure, parental involvement, and confidential services, significantly (p<0.05) more female adolescents in the intervention group were using their chosen method at 6 (92%) and 12 (90%) months versus the control group (85% and 83%, respectively), which received the standard of care.36
Two studies19,24 examined use of repeat or follow-up services, with one19 finding a statistically significant impact. In the first study, which was a pre–post study of peer provider counseling, female adolescents that received both clinic counseling and telephone counseling had significantly (p<0.05) higher odds (OR=1.4, CI not reported) of returning for an annual exam than those who received only clinic counseling.19 The second study24 found no statistically significant effect of the counseling intervention on the number of clinic visits made by the client.
Of the three adolescent studies23,24,36 that examined the impact of contraceptive counseling on short-term outcomes, two24,36 examined quality and satisfaction with services, one36 examined changes in participant knowledge, and two23,36 examined psychosocial determinants of contraceptive use. One controlled trial36 of a psychosocial model found significantly (p<0.05) improved knowledge at 12-month follow-up and more ease coping with contraceptive problems at 6-month follow-up among the intervention group compared with the control group. No other statistically significant effects of counseling on short-term outcomes were found.
Two studies17,19 examined unintended negative consequences associated with contraceptive counseling in family planning settings. The first17—a pre–post study conducted among a sample of 383 unmarried youth, 65% of which were not yet sexually active—investigated whether receipt of counseling promoted sexual debut. Findings suggested that exposure to counseling did not promote entry into sexual activity among non–sexually active youth, as only 3% of those not sexually active at baseline had initiated sexual activity at follow-up, which ranged from 2 to 12 months (average of 7.8 months). In the second study,19 which sought primarily to understand the impact of a peer provider counseling model on contraceptive use behaviors and teen pregnancy, female participants reported significantly (p<0.01) lower odds (OR=0.65, CI not reported) of condom use from first (35%) to last (27%) visit, which was an unexpected and undesirable finding. The authors concluded that the reduction in condom use may have occurred because of the increase in female participants’ use of more-effective methods (a change that was observed in the study), but no tests of association were conducted to support this hypothesis.
Adults or Mixed Populations (Adults and Adolescents)
Of the 16 studies15,16,18,21,22,25–35,37 (from 17 articles) that examined the impact of contraceptive counseling among adults or mixed populations (adults and adolescents), nine16,21,22,25,28,29,31–33 were RCTs. Of these nine studies, eight were rated as having moderate risk for bias and one31 was rated as having high risk for bias. One27 was a prospective, nonrandomized controlled trial, one15 was a prospective cohort study, two18,34 were pre–post studies, and three26,35,37 were cross-sectional surveys. All of the non-RCT studies were rated as having high risk for bias.
A variety of outcomes were examined, ranging from reducing unintended pregnancy to enhancing psychosocial determinants of contraceptive use (e.g., intentions to use contraception the following year). Six studies21,22,27,29,32,33 examined long-term outcomes, 1515,16,18,21,22,25–29,31–33,35,37 examined medium-term outcomes, and five22,28,31,34,35 examined short-term outcomes. Thirteen16,18,21,22,25,27–29,31–33,35,37 of the 16 studies examined multiple outcomes. None of the studies reported barriers or facilitators for clinics or clients or reported on unintended negative consequences.
Sample sizes in the 16 studies ranged from 3322 to 89835; all participants were aged 14–50 years and were recruited from some type of clinical setting. A different counseling model or approach was used in each of the 16 studies. Examples included motivational interviewing,15,18,29 use of specific provider tools (e.g., WHO Decision-Making Tool),21,25 development and use of individualized action plans,15,22,27 consideration of barriers to use or self-efficacy,18,22,27,28 and follow-up telephone calls to reinforce messages.15,18 Counseling interventions also varied in intensity: Three15,16,18 were rated as moderate intensity, 1221,22,25–29,31–34,37 were rated as low intensity, and the intensity was not reported for one study.35 Appendix C describes details of each study; Table 3 summarizes findings by outcome of interest.
Table 3.
Summary of Impact of Contraceptive Counseling in Clinical Settings for Adults or Mixed Populations
| Reference | Quality | Intensity | Outcomes | Total outcomes with positive impact for study† |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Long-term | Medium-term | Short-term | |||||||||||
| Decreased teen or UIP rate |
Increased contraceptive use |
Increased use of more effective contraceptives |
Increased correct use of contraceptives |
Increased continuation of contraceptive use |
Increased repeat or follow-up service use |
Increased dual-method contraceptive use |
Increased quality and satisfaction with service |
Increased knowledge |
Enhanced other psychosocial determinants of contraceptive use |
||||
| Adams-Skinner (2009)15 | Level II-2; high risk for bias | Moderate | NA | ↑/↔ | NA | NA | NA | NA | NA | NA | NA | NA | 1/1 |
| Bender (2004)16 | Level I; moderate risk for bias | Moderate | NA | ↔ | ↔ | NA | NA | NA | NA | NA | NA | NA | 0/2 |
| Boise (2003)18 | Level II-3; high risk for bias | Moderate | NA | * | NA | * | NA | NA | NA | NA | NA | NA | 0/0 |
| Custo (1987)21 | Level I; moderate risk for bias | Low | ↔ | NA | ↑ | NA | NA | NA | NA | NA | NA | NA | 1/2 |
| Gilliam (2004)22 | Level I; moderate risk for bias | Low | ↔ | NA | NA | NA | ↔ | NA | NA | NA | ↑ | NA | 1/3 |
| Langston (2010)25 | Level I; moderate risk for bias | Low | NA | NA | ↔ | NA | ↔ | NA | NA | NA | NA | NA | 0/2 |
| Lee (2011)26 | Level II-3; high risk for bias | Low | NA | ↑ | NA | NA | NA | NA | NA | NA | NA | NA | 1/1 |
| Namerow (1989)27 | Level II-1; high risk for bias | Low | ↔ | NA | NA | ↑ | NA | ↔ | NA | NA | NA | NA | 1/3 |
| Nobili (2007)28 | Level I; moderate risk for bias | Low | NA | NA | ↑ | NA | NA | NA | NA | NA | ↑ | ↑ | 3/3 |
| Petersen (2007)29,30 | Level I; moderate risk for bias | Low | ↔ | NA | NA | ↔ | NA | NA | NA | NA | NA | NA | 0/2 |
| Proctor (2006)31 | Level I; high risk for bias | Low | NA | NA | ↔ | NA | NA | NA | NA | ↑ | NA | NA | 1/2 |
| Schunmann (2006)32 | Level I; moderate risk for bias | Low | ↔ | ↔ | ↑ | NA | ↔ | NA | NA | NA | NA | NA | 1/4 |
| Shlay (2003)33 | Level I; moderate risk for bias | Low | ↔ | NA | ↑/↔ | NA | NA | ↔ | ↑/↔ | NA | NA | NA | 2/4 |
| Todres (1990)34 | Level II-3; high risk for bias | Low | NA | NA | NA | NA | NA | NA | NA | NA | ↑ | NA | 1/1 |
| Weisman (2002)35 | Level II-3; high risk for bias | NR | NA | ↑ | NA | NA | NA | NA | NA | ↑ | NA | ↑/↔ | 3/3 |
| Yassin (2005)37 | Level II-3; high risk for bias | Low | NA | * | * | NA | NA | NA | NA | NA | NA | NA | 0/0 |
| Total studies with positive impact † | 0/6 | 4/7 | 4/8 | 1/3 | 0/3 | 0/2 | 1/1 | 2/2 | 3/3 | 2/2 | |||
Note: Intensity of intervention defined as low (intervention took place during a single visit); moderate (intervention took place during more than one visit, but less frequently than weekly); or high (intervention took place weekly).
↑Statistically significant positive effect; ↓statistically significant negative effect; ↔ no evidence of a statistically significant effect.
No statistical testing conducted, but improvement observed.
Statistically significant.
NA, not assessed; NR, not reported; UIP, unintended pregnancy.
Of the six studies21,22,27,29,32,33 among adults or mixed populations that examined the impact of contraceptive counseling on long-term outcomes, none found a statistically significant impact of counseling on decreasing teen or unintended pregnancy. One prospective, nonrandomized controlled trial27 that compared 412 female participants who received a contingency plan counseling intervention with 411 who received the standard of care found a significantly (p<0.05) reduced likelihood of unintended pregnancy at 6-month follow-up among previously pregnant intervention participants than among previously pregnant control participants (subgroup sample sizes not stated); however, these differences dissipated by 12 months.
Of the 15 studies among adults or mixed populations that examined the impact of contraceptive counseling on medium-term outcomes, a variety of outcomes were investigated. Seven studies15,16,18,26,32,35,37 examined contraceptive use, with three15,26,35 finding a statistically significant impact of counseling. One prospective cohort study15 followed 78 sexually active female participants for 6 months and compared those who received a counseling intervention grounded in motivational interviewing and relapse prevention that promoted dual-method contraceptive use (n=36) with control group participants who received the standard of care (n=42). Counseling sessions for both groups were audiotaped and coded to measure three components of interest: promotion of dual protection, relapse prevention counseling, and quality of nurse–client interaction. For the total sample (intervention and control groups combined), the quality of the nurse–client interaction was significantly (p<0.05) associated with condom use at 6-month follow-up, after adjustment for study group. Promotion of dual protection and relapse prevention techniques were not significantly associated with condom use at 6-month follow-up. The second study,35 cross-sectional in design, examined patient-reported contraceptive counseling received in the past 2 years from managed care providers in a 16-county commercial provider network on three components: exposure, content, and personalization. Among women considered at risk of unintended pregnancy (i.e., fertile, non-pregnant, heterosexually active, not seeking pregnancy, with a non-sterilized partner), receiving personalized counseling and information was significantly (p<0.05) associated with increased odds of current contraceptive use (AOR=4.97, CI not reported) compared with those who received no counseling. The third study26 that found a significant impact of counseling on contraceptive use was a cross-sectional survey conducted among 770 women recruited from four primary care clinics. This study asked women about the contraceptive counseling they received from their primary care physician 7–30 days after their visit. Participants who received counseling from a physician on any method had significantly (p<0.05) increased odds of reporting use of a hormonal method at last intercourse (OR=2.68, 95% CI=1.48, 4.87) compared with those who did not receive any counseling. In addition, those who received counseling on a specific method had higher odds of reporting use of that method (OR=4.78, 95% CI=3.70, 11.37, for hormonal methods and OR=18.45, 95% CI=4.88, 69.84, for long-acting, reversible methods). Of the remaining four studies that examined contraceptive use, two16,32 found no statistically significant effect of counseling on contraceptive use, and two18,37 reported an improvement but did not conduct tests of statistical significance.
Eight studies16,21,25,28,31–33,37 examined use of more-effective contraceptives, with four21,28,32,33 finding a statistically significant impact of counseling. One RCT21 examined 100 female participants who received standard counseling and a counseling intervention that used a standardized provider tool intended to help women select the most appropriate behavioral or barrier contraceptive method and increase satisfaction with their chosen method. This group was compared with 100 female participants who received only standard counseling to examine changes in method selection from baseline to 12–15-month follow-up. Diaphragm use (the most effective contraceptive method examined in the study) significantly (p<0.05) increased among intervention participants from baseline (9%) to follow-up (26%), whereas no significant differences from baseline to follow-up were detected among controls (11% vs 16%, respectively). In addition, the rate of diaphragm use among intervention participants at follow-up (26%) was significantly (p<0.05) higher than the rate among control participants (16%). In the second study,28 another RCT of 43 women undergoing pregnancy termination, women who received a patient-centered counseling intervention that explored past and present contraceptive experiences, barriers to use, perceptions of risk, and future plans (n=21) were compared with those who received the standard of care (n=22). The intervention group demonstrated a significant (p<0.005) increase in the proportion of women using an effective contraceptive method (defined by the authors as IUDs, oral contraceptives, vaginal rings, contraceptive patches, condoms, or emergency contraception; 65% and 80% at 1 and 3 months, respectively) versus baseline (20%), whereas no significant changes between follow-up (32% and 38% at 1 and 3 months, respectively) and baseline (19%) were found in the control group. The authors did not compare the change from baseline to follow-up between the intervention and control groups. In the third study,32 another RCT of 613 female participants seeking pregnancy termination, the intervention group received brief individual counseling to discuss future contraceptive needs during an initial consultation and a posttermination interview with a specialist trained in contraception (n=316). These women were compared with women in the control group who received the standard of care (n=297). At 4-month follow-up, significantly (p<0.05) more women in the intervention group (37%) than the control group (26%) were using a longer-acting method (i.e., IUD, implant, or injectable). In the fourth study,33 also an RCT, 877 women seeking services at an STI clinic were randomized into two groups, both of which received condoms with spermicide and a referral list of primary care providers for ongoing reproductive health care. The intervention group (n=437) received enhanced contraceptive care that included individual counseling, initial provision of contraception, and a facilitated referral to a primary care provider. Significantly (p<0.0001) more intervention than control participants reported use of effective contraceptives (defined by the authors as sterilization; use of IUDs, implants, injectables, oral contraceptives, or spermicide with condoms for > 75% of coital acts; and sexual abstinence) at 4 months (50% and 22%, respectively) and 8 months (44% and 26%, respectively). Differences were not significant at 12-month follow-up. Of the remaining four studies, three16,25,31 found no statistically significant effect of counseling on effective contraceptive use, and one37 observed an improvement but did not conduct tests of statistical significance.
Three studies18,27,29 examined the impact of counseling on correct use of contraceptives (e.g., taking oral contraceptives appropriately every day), with one27 finding a statistically significant positive impact. In this study, a prospective, nonrandomized controlled trial of 823 women, intervention participants (n=412) received contingency plan counseling that included asking participants to articulate a pregnancy goal; assess their perceived probability of pregnancy; list contingencies that might arise and interfere with correct use of their chosen method (e.g., not having the method available at time of intercourse); and develop detailed plans for dealing with each contingency.27 Intervention participants were compared with control group participants who received the standard of care (n=411). Among oral contraceptive users (n=319), a significantly (p<0.05) higher proportion of those in the intervention group (53%) versus those in the control group (43%) reported correct use (i.e., taking oral contraceptives every day). In addition, among users of oral contraceptives who had missed pills (n=166), significantly more women in the intervention versus control group reported taking the forgotten pills appropriately (89% and 68%, respectively, p<0.01). Of the remaining two studies, one29 did not find a statistically significant impact of counseling on increasing correct use, and the other18 observed an improvement in correct use but did not conduct tests of statistical significance.
Three studies22,25,32 examined continuation of contraceptive use, and two studies27,33 examined use of repeat or follow-up services, with none finding a statistically significant positive impact of counseling. One study33 examined the impact of counseling on dual-method contraceptive use (i.e., use of an effective method to prevent pregnancy plus a condom). In this RCT of 877 women seeking services at an STI clinic, all participants received condoms with spermicide and a referral list of primary care providers for ongoing reproductive health care. Those in the intervention group also received enhanced contraceptive care that included individual counseling, initial provision of contraception, and a facilitated referral to a primary care provider. Significantly (p<0.01) more intervention than control participants reported dual-method use at 4 months (29% and 14%, respectively) and 8 months (23% and 14%, respectively), but differences were not significant at 12-month follow-up.
Of the five studies22,28,31,34,35 among adults or mixed populations that examined the impact of contraceptive counseling on short-term outcomes, two31,35 examined quality and satisfaction with services, three22,28,34 examined changes in participant knowledge, and two28,35 examined psychosocial determinants of contraceptive use. Among these studies, two31,35 found positive impacts for satisfaction with services, three22,28,34 for participant knowledge, and two28,35 for psychosocial determinants.
Discussion
This systematic review identified 22 studies that examined the impact of contraceptive counseling in clinical settings and met the inclusion criteria. Of these, six studies17,19,20,23,24,36 examined the impact of counseling among adolescents, with four finding a statistically significant positive impact of low-intensity23 or moderate-intensity17,19,36 counseling interventions on at least one outcome of interest. Three19,24,36 of the six adolescent studies examined long-term outcomes, with one19 finding a statistically significant positive impact of counseling. This study found that youth who received clinic-based contraceptive counseling from a peer provider and follow-up telephone calls had lower odds of teen pregnancy than those who received only clinic-based counseling. All six studies examined medium-term outcomes, of which four17,19,23,36 found a statistically significant positive impact on at least one outcome of interest. Finally, one36 of three studies23,24,36 that examined short-term outcomes found a statistically significant positive impact on at least one outcome of interest.
Of the 16 studies15,16,18,21,22,25–29,31–35,37 that focused on adults or mixed populations (adolescents and adults), 11 found a statistically significant positive impact of counseling interventions with low,21,22,26–28,31–34 moderate,15 or unrated35 intensity on at least one outcome of interest. Six21,22,27,29,32,33 of the 16 adult or mixed population studies examined long-term outcomes. None found a statistically significant positive impact of counseling on decreasing teen or unintended pregnancy. Of the 15 studies that examined medium-term outcomes, eight15,21,26–28,32,33,35 found a statistically significant positive impact on at least one outcome of interest. Finally, all five studies22,28,31,34,35 that examined short-term outcomes found a statistically significant positive impact on at least one outcome of interest.
No studies that examined the impact of counseling for adolescents, adults, or mixed populations reported information on barriers or facilitators for clinics offering counseling or clients achieving positive outcomes after receiving counseling in family planning settings. Two studies on adolescents examined unintended negative consequences, with one17 finding that counseling did not promote sexual debut among non–sexually active participants, and the other19 finding decreased use of condoms among female participants, possibly because of an increase in use of more-effective methods at preventing pregnancy.
Because each study examined a different counseling intervention—some of which incorporated multiple approaches—this review was unable to assess the impact of a single counseling component separate from the others or to compare the relative effectiveness of one approach versus another. Nevertheless, components of counseling approaches that resulted in some statistically significant positive change in long-, medium-, or short-term outcomes can be considered when developing counseling guidelines for family planning clients.
Promising components that emerged from the studies in this systematic review include an emphasis on the quality of interaction between counselor and client (e.g., developing rapport)15,19,28,31; personalizing discussions to meet clients’ individual needs23,28,32,33,35; and addressing psychosocial determinants of contraceptive use behaviors (e.g., perceived benefits and barriers, outcome expectations).22,23,28,32,36 Other promising components include setting goals; discussing possible difficulties with achieving goals (e.g., side effects, difficulty obtaining the method); developing action plans to deal with potential difficulties15,22,23,27; and multiple contacts with clients.15,17,19,33,36
When examining the number of outcomes positively impacted by a single counseling intervention in studies included in this systematic review (Tables 2 and 3), it is not surprising that all five19,28,33,35,36 interventions for which a significant impact on multiple outcomes was detected included one,35 two,19,33,36 or three28 of the promising components. For example, one study19 that found positive impacts on both long- and medium-term outcomes (including decreased odds of pregnancy) used peer providers to enhance the quality of the provider–client relationship and quarterly telephone calls by peer providers to reinforce counseling messages and answer questions.
Evidence from other fields, including chronic disease management and psychotherapy, support the importance of the provider–client relationship.38–40 Previous research has suggested that 30% of a client’s improvement after counseling is attributed to the provider’s empathy, warmth, acceptance, and encouragement.38 Qualitative evidence on women’s preferences for contraceptive counseling suggests that women prefer caring interpersonal relationships with providers and want their values and preferences emphasized.41 Client-centered health techniques, such as motivational interviewing and shared decision making,42–46 may be one way to promote the quality of provider–client interaction and personalize counseling messages. Core components of client-centered care have been developed and described elsewhere.47 Specific to contraceptive counseling and drawn from the health communications literature, best practices to promote quality provider–client communication, both relational and exchange of essential information, have also been described.48
The chronic disease literature has also suggested that goal setting can be used as a behavior change strategy in health education,49,50 and other areas of behavioral counseling (related to nutrition, smoking cessation, and physical activity) have suggested the need for repeated counseling sessions to support positive behavior change.51–53 Additionally, several of the promising components identified in this systematic review were recommended as part of 12 principles for providing contraceptive counseling to adolescents, based on reviews of scientific literature on decision making and contraceptive behavior.54
Limitations
This body of evidence has several limitations. Of the 22 studies in this review, none were determined to have a low risk for bias, and more than half17–20,26,27,31,34–37 were determined to have a high risk for bias. Studies were considered to be at risk for bias because of selection bias, recall bias, self-report bias, attrition bias, or short follow-up times for behavioral outcomes. Among the examined RCTs, primary weaknesses included lack of21,25,29,32 or no reporting of23,24,31,33 blinding; no reporting of allocation procedures, including concealment,16,21,23,24,28,33 and no concealment of allocation.32 Some studies15,18,20,22,23,28,34 were conducted among small samples (<100) and may have been underpowered to detect meaningful differences in outcomes. Other studies24,35,36 did not state clearly how outcomes of interest were measured or they used instruments with questionable validity. For studies that examined use of more-effective contraceptives, some21,28,33 included methods with lower rates of typical use effectiveness4 in their categorization of effective methods (e.g., diaphragm, condoms). Some studies16,32,34,36,37 failed to adequately establish comparability between study groups, limiting the ability to definitively attribute outcomes to the counseling intervention. Two studies20,29 included participants who either desired pregnancy at enrollment or had ambivalent pregnancy intentions, which may have biased findings related to contraceptive use behaviors and pregnancy rates. As previously mentioned, some studies were conducted among samples of women receiving postpartum care,22,31 postpregnancy termination care,16,25,28,32,37 or services at an STI clinic.33 Although these are important subpopulations for interventions, these participants may not best represent the general population of people seeking family planning services. Finally, 1115,19,21–25,27,28,32,36 of 1815,16,19,21–29,31–33,35–37 studies that included a comparison group in the design or analysis compared intervention participants with participants who received standard of care contraceptive counseling. The estimated effects of the interventions in these studies would likely be less than comparable estimates had the comparison group received no contraceptive counseling.
To promote dissemination and adoption of promising contraceptive counseling interventions to other populations and settings, interventions should be clearly and fully described and well documented in a manual or protocol that can be referenced or shared with others. Documentation of procedures also allows assessment of program fidelity (or examination of intervention implementation), which is important to consider when examining the impact of an intervention (e.g., is the intervention being implemented as conceptualized and consistently by different counselors?) Of the 22 studies in this review, only three15,24,25 referenced a manual that was used to guide the counseling interventions, and only one24 of the three discussed study findings in the context of intervention fidelity. In this RCT, intervention participants were to receive regular counseling and nine follow-up telephone calls over 12 months. Although the study found no evidence that the intervention impacted the outcomes of interest, the intervention had poor completion rates, with counselors completing, on average, only 2.7 of nine follow-up telephone calls. To facilitate assessment of intervention implementation for prevention counseling, the HIV/STI counseling literature has proposed quality assurance measures, including the development of standard tools, standard training, frequent observation and feedback to counselors, and process evaluations.55 Documentation of procedures is also needed to evaluate an intervention’s intensity, which has been suggested as a critical predictor of an intervention’s effectiveness in the HIV/STI counseling literature.56,57 Although this systematic review described interventions by intensity, the definition developed for this review was crude because of incomplete intervention descriptions (e.g., lack of information on total amount of time to complete interventions).
Despite these limitations, the evidence base for contraceptive counseling also has several strengths. Half of the studies (11 of 22) in this review were RCTs,16,21–25,28,29,33 and many used random number tables for group allocation,16,22,24,25,29,31,32 concealed group allocation,22,25,29,31 and used blinding.16,22,28 Several studies followed participants for at least 12 months.21,22,24,27,29,32,33,36 Other strengths included high participation rates,23,27,29,37 high completion rates,29,31,33,37 small differences in follow-up rates between study groups,16,21,25,27,29,31,32 and study groups with similar baseline characteristics.15,21,23–25,27,29,31–33 Two studies also used instruments with psychometric evidence of validity or reliability to measure constructs of interest,15,36 and at least two measured pregnancy by using urine tests versus self-report.19,27 Many studies17–20,23–25,36 directly acknowledged training study staff, and two20,21 reported using standardized provider tools to improve intervention implementation.
Additional articles58–63 meeting the inclusion criteria for this systematic review have been published since our initial search of the literature. Three cross-sectional studies59,61,63 did not provide details about the contraceptive counseling received by women. One cohort study62 supported the importance of provider–patient interaction, personalized discussions, and addressing psychosocial determinants of contraceptive use behaviors during counseling. Another cohort study60 found no increased uptake of long-acting reversible contraceptives among women receiving structured, comprehensive contraceptive counseling versus the standard of care in settings where financial barriers to contraception were removed, but uptake was high in both groups (>70%). Last, one RCT58 provided mixed support on the usefulness of developing action plans and multiple client contacts.
Conclusions
Despite the diversity of interventions examined in this systematic review and the inability to compare the relative effectiveness of one approach versus another, promising counseling components emerged. Along with expert feedback and findings from two other complementary systematic reviews on the impact of education and reminder systems in family planning programs,64,65 the information was used to develop recommendations for providing quality contraceptive counseling in the 2014 “Providing Quality Family Planning Services.”66 The evidence base on the impact of contraceptive counseling in clinical settings would be strengthened by improved documentation of counseling procedures; assessment of intervention implementation and fidelity to put study findings into context; and the development and inclusion of more RCTs, studies conducted among general samples of women (e.g., from primary care settings), and studies with sample sizes that are large enough to detect important behavioral outcomes at least 12 months post-intervention. Continued efforts to develop and test effective contraceptive counseling interventions are needed and might consider incorporating promising components identified in this review and drawing on literature from other health fields.
Supplementary Material
Acknowledgments
Publication of this article was supported by the U.S. Centers for Disease Control and Prevention (CDC) and the Office of Population Affairs (OPA).
Appendix. Supplementary data
Supplementary data associated with this article can be found at http://dx.doi.org/10.1016/j.amepre.2015.03.023.
Footnotes
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of CDC or the Office of Population Affairs.
No financial disclosures were reported by the authors of this paper.
References
- 1.Finer LB, Zolna MR. Unintended pregnancy in the United States: incidence and disparities, 2006. Contraception. 2011;84(5):478–485. doi: 10.1016/j.contraception.2011.07.013. http://dx.doi.org/10.1016/j.contraception.2011.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mosher WD, Jones J. Use of contraception in the United States: 1982–2008. Vital Health Stat 23. 2010;29:1–44. [PubMed] [Google Scholar]
- 3.Gold RB, Sonfield A, Richards CL, Frost JJ. Next Steps for America’s Family Planning Program: Leveraging the Potential of Medicaid and Title X in an Evolving Health Care System. New York: Guttmacher Institute; 2009. [Google Scholar]
- 4.Trussell J. Contraceptive failure in the United States. Contraception. 2011;83(5):397–404. doi: 10.1016/j.contraception.2011.01.021. http://dx.doi.org/10.1016/j.contraception.2011.01.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cassel C, Blank L, Braunstein G, Burke W, Fryhofer SA, Pinn V. What internists need to know: core competencies in women’s health. ABIM Subcommittee on Clinical Competence in Women’s Health. Am J Med. 1997;102(6):507–512. doi: 10.1016/s0002-9343(97)00227-1. [DOI] [PubMed] [Google Scholar]
- 6.Accreditation Council for Graduate Medical Education (ACGME) ACGME Program Requirements for Graduate Medical Education in Family Medicine. 2013:1–32. www.acgme.org/acgmeweb/Portals/0/PFAssets/ProgramRequirements/120_family_medicine_07012014.pdf.
- 7.Akers AY, Gold MA, Borrero S, Santucci A, Schwarz EB. Providers’ perspectives on challenges to contraceptive counseling in primary care settings. J Womens Health (Larchmt) 2010;19(6):1163–1170. doi: 10.1089/jwh.2009.1735. http://dx.doi.org/10.1089/jwh.2009.1735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Whitlock EP, Orleans CT, Pender N, Allan J. Evaluating primary care behavioral counseling interventions: an evidence-based approach. Am J Prev Med. 2002;22(4):267–284. doi: 10.1016/s0749-3797(02)00415-4. http://dx.doi.org/10.1016/S0749-3797(02)00415-4. [DOI] [PubMed] [Google Scholar]
- 9.Moos MK, Bartholomew NE, Lohr KN. Counseling in the clinical setting to prevent unintended pregnancy: an evidence-based research agenda. Contraception. 2003;67(2):115–132. doi: 10.1016/s0010-7824(02)00472-9. http://dx.doi.org/10.1016/S0010-7824(02)00472-9. [DOI] [PubMed] [Google Scholar]
- 10.Lopez LM, Tolley EE, Grimes DA, Chen M, Stockton LL. Theory-based interventions for contraception. Cochrane Database Syst Rev. 2013;8:CD007249. doi: 10.1002/14651858.CD007249.pub4. http://dx.doi.org/10.1002/14651858.CD007249.pub4. [DOI] [PubMed] [Google Scholar]
- 11.Tregear SJ, Gavin LE, Williams JR. Systematic review evidence methodology: providing quality family planning services. Am J Prev Med. 2015;49(2S1):S23–S30. doi: 10.1016/j.amepre.2015.03.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.American Counseling Association. 20/20: consensus definition of counseling. www.counseling.org/knowledge-center/20-20-a-vision-forthe-future-of-counseling/consensus-definition-of-counseling.
- 13.Modeste N. Dictionary of Public Health Promotion and Education: Terms and Concepts. Thousand Oaks, CA: SAGE Publications; 1996. [Google Scholar]
- 14.Harris RP, Helfand M, Woolf SH, et al. Current methods of the U.S. Preventive Services Task Force: a review of the process. Am J Prev Med. 2001;20(3 suppl):21–35. doi: 10.1016/s0749-3797(01)00261-6. http://dx.doi.org/10.1016/S0749-3797(01)00261-6. [DOI] [PubMed] [Google Scholar]
- 15.Adams-Skinner J, Exner T, Pili C, Wallace B, Hoffman S, Leu CS. The development and validation of a tool to assess nurse performance in dual protection counseling. Patient Educ Couns. 2009;76(2):265–271. doi: 10.1016/j.pec.2008.12.024. http://dx.doi.org/10.1016/j.pec.2008.12.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bender SS, Geirsson RT. Effectiveness of preabortion counseling on postabortion contraceptive use. Contraception. 2004;69(6):481–487. doi: 10.1016/j.contraception.2003.12.014. http://dx.doi.org/10.1016/j.contraception.2003.12.014. [DOI] [PubMed] [Google Scholar]
- 17.Berger DK, Perez G, Kyman W, et al. Influence of family planning counseling in an adolescent clinic on sexual activity and contraceptive use. J Adolesc Health Care. 1987;8(5):436–440. doi: 10.1016/0197-0070(87)90233-6. http://dx.doi.org/10.1016/0197-0070(87)90233-6. [DOI] [PubMed] [Google Scholar]
- 18.Boise R, Petersen R, Curtis KM, et al. Reproductive health counseling at pregnancy testing: a pilot study. Contraception. 2003;68(5):377–383. doi: 10.1016/j.contraception.2003.08.002. http://dx.doi.org/10.1016/j.contraception.2003.08.002. [DOI] [PubMed] [Google Scholar]
- 19.Brindis CD, Geierstanger SP, Wilcox N, McCarter V, Hubbard A. Evaluation of a peer provider reproductive health service model for adolescents. Perspect Sex Reprod Health. 2005;37(2):85–91. doi: 10.1363/psrh.37.085.05. http://dx.doi.org/10.1363/3708505. [DOI] [PubMed] [Google Scholar]
- 20.Cowley CB, Farley T, Beamis K. “Well, maybe I’ll try the pill for just a few months…”: Brief motivational and narrative-based interventions to encourage contraceptive use among adolescents at high risk for early childbearing. Fam Syst Health. 2002;20(2):183–204. http://dx.doi.org/10.1037/h0089493. [Google Scholar]
- 21.Custo G, Saitto C, Cerza S, Sertoli G. The adjusted contraceptive score (ACS) improves the overall performance of behavioural and barrier contraceptive methods. Adv Contracept Deliv Syst. 1987;3(4):367–373. [PubMed] [Google Scholar]
- 22.Gilliam M, Knight S, McCarthy Success with oral contraceptives: a pilot study. Contraception. 2004;69(5):413–418. doi: 10.1016/j.contraception.2003.12.006. http://dx.doi.org/10.1016/j.contraception.2003.12.006. [DOI] [PubMed] [Google Scholar]
- 23.Hanna KM. Effect of nurse-client transaction on female adolescents’ oral contraceptive adherence. Image J Nurs Sch. 1993;25(4):285–290. doi: 10.1111/j.1547-5069.1993.tb00261.x. http://dx.doi.org/10.1111/j.1547-5069.1993.tb00261.x. [DOI] [PubMed] [Google Scholar]
- 24.Kirby D, Raine T, Thrush G, Yuen C, Sokoloff A, Potter SC. Impact of an intervention to improve contraceptive use through follow-up phone calls to female adolescent clinic patients. Perspect Sex Reprod Health. 2010;42(4):251–257. doi: 10.1363/4225110. http://dx.doi.org/10.1363/4225110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Langston AM, Rosario L, Westhoff CL. Structured contraceptive counseling—a randomized controlled trial. Patient Educ Couns. 2010;81(3):362–367. doi: 10.1016/j.pec.2010.08.006. http://dx.doi.org/10.1016/j.pec.2010.08.006. [DOI] [PubMed] [Google Scholar]
- 26.Lee JK, Parisi SM, Akers AY, Borrero S, Schwarz EB. The impact of contraceptive counseling in primary care on contraceptive use. J Gen Intern Med. 2011;26(7):731–736. doi: 10.1007/s11606-011-1647-3. http://dx.doi.org/10.1007/s11606-011-1647-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Namerow PB, Weatherby N, Williams-Kaye J. The effectiveness of contingency-planning counseling. Fam Plann Perspect. 1989;21(3):115–119. http://dx.doi.org/10.2307/2135661. [PubMed] [Google Scholar]
- 28.Nobili MP, Piergrossi S, Brusati V, Moja EA. The effect of patient-centered contraceptive counseling in women who undergo a voluntary termination of pregnancy. Patient Educ Couns. 2007;65(3):361–368. doi: 10.1016/j.pec.2006.09.004. http://dx.doi.org/10.1016/j.pec.2006.09.004. [DOI] [PubMed] [Google Scholar]
- 29.Petersen R, Albright J, Garrett JM, Curtis KM. Pregnancy and STD prevention counseling using an adaptation of motivational interviewing: a randomized controlled trial. Perspect Sex Reprod Health. 2007;39(1):21–28. doi: 10.1363/3902107. http://dx.doi.org/10.1363/3902107. [DOI] [PubMed] [Google Scholar]
- 30.Petersen R, Albright JB, Garrett JM, Curtis KM. Acceptance and use of emergency contraception with standardized counseling intervention: results of a randomized controlled trial. Contraception. 2007;75(2):119–125. doi: 10.1016/j.contraception.2006.08.009. http://dx.doi.org/10.1016/j.contraception.2006.08.009. [DOI] [PubMed] [Google Scholar]
- 31.Proctor A, Jenkins TR, Loeb T, Elliot M, Ryan A. Patient satisfaction with 3 methods of postpartum contraceptive counseling: a randomized, prospective trial. J Reprod Med. 2006;51(5):377–382. [PubMed] [Google Scholar]
- 32.Schunmann C, Glasier A. Specialist contraceptive counselling and provision after termination of pregnancy improves uptake of long-acting methods but does not prevent repeat abortion: a randomized trial. Hum Reprod. 2006;21(9):2296–2303. doi: 10.1093/humrep/del168. http://dx.doi.org/10.1093/humrep/del168. [DOI] [PubMed] [Google Scholar]
- 33.Shlay JC, Mayhugh B, Foster M, Maravi ME, Baron AE, Douglas Initiating contraception in sexually transmitted disease clinic setting: a randomized trial. Am J Obstet Gynecol. 2003;189(2):473–481. doi: 10.1067/s0002-9378(03)00493-9. http://dx.doi.org/10.1067/S0002-9378(03)00493-9. [DOI] [PubMed] [Google Scholar]
- 34.Todres R. Effectiveness of counseling in the transmission of family planning and sexuality knowledge. J Sex Educ Ther. 1990;16(4):279–285. [Google Scholar]
- 35.Weisman CS, Maccannon DS, Henderson JT, Shortridge E, Orso CL. Contraceptive counseling in managed care: preventing unintended pregnancy in adults. Womens Health Issues. 2002;12(2):79–95. doi: 10.1016/s1049-3867(01)00147-5. http://dx.doi.org/10.1016/S1049-3867(01)00147-5. [DOI] [PubMed] [Google Scholar]
- 36.Winter L, Breckenmaker LC. Tailoring family planning services to the special needs of adolescents. Fam Plann Perspect. 1991;23(1):24–30. http://dx.doi.org/10.2307/2135397. [PubMed] [Google Scholar]
- 37.Yassin AS, Cordwell D. Does dedicated pre-abortion contraception counselling help to improve post-abortion contraception uptake? J Fam Plann Reprod Health Care. 2005;31(2):115–116. doi: 10.1783/1471189053629347. http://dx.doi.org/10.1783/1471189053629347. [DOI] [PubMed] [Google Scholar]
- 38.Lambert MJ. Psychotherapy outcome research: implications for integrative and eclectic therapists. In: Norcross JC, Goldfried MR, editors. Handbook of Psychotherapy Integration. New York, NY: Basic Books; 1992. pp. 96–97. [Google Scholar]
- 39.Feinberg J. The effect of patient-practitioner interaction on compliance: a review of the literature and application in rheumatoid arthritis. Patient Educ Couns. 1988;11(3):171–187. doi: 10.1016/0738-3991(88)90018-3. http://dx.doi.org/10.1016/0738-3991(88)90018-3. [DOI] [PubMed] [Google Scholar]
- 40.Viller F, Guillemin F, Briancon S, Moum T, Suurmeijer T, van den Heuvel W. Compliance to drug treatment of patients with rheumatoid arthritis: a 3 year longitudinal study. J Rheumatol. 1999;26(10):2114–2122. [PubMed] [Google Scholar]
- 41.Dehlendorf C, Levy K, Kelley A, Grumbach K, Steinauer J. Women’s preferences for contraceptive counseling and decision making. Contraception. 2013;88(2):250–256. doi: 10.1016/j.contraception.2012.10.012. http://dx.doi.org/10.1016/j.contraception.2012.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Emmons KM, Rollnick S. Motivational interviewing in health care settings. Opportunities and limitations. Am J Prev Med. 2001;20(1):68–74. doi: 10.1016/s0749-3797(00)00254-3. http://dx.doi.org/10.1016/S0749-3797(00)00254-3. [DOI] [PubMed] [Google Scholar]
- 43.Knight KM, McGowan L, Dickens C, Bundy C. A systematic review of motivational interviewing in physical health care settings. Br J Health Psychol. 2006;11(Pt 2):319–332. doi: 10.1348/135910705X52516. http://dx.doi.org/10.1348/135910705X52516. [DOI] [PubMed] [Google Scholar]
- 44.Leffingwell TR, Neumann CA, Babitzke AC, Leedy MJ. Social psychology and motivational interviewing: a review of relevant principles and recommendations for research and practice. Behav Cogn Psychother. 2007;35:31–45. http://dx.doi.org/10.1017/S1352465806003067. [Google Scholar]
- 45.Britt E, Hudson SM, Blampied NM. Motivational interviewing in health settings: a review. Patient Educ Couns. 2004;53:147–155. doi: 10.1016/S0738-3991(03)00141-1. http://dx.doi.org/10.1016/S0738-3991(03)00141-1. [DOI] [PubMed] [Google Scholar]
- 46.Elwyn G, Dehlendorf C, Epstein RM, Marrin K, White J, Frosch DL. Shared decision making and motivational interviewing: achieving patient-centered care across the spectrum of health care problems. Ann Fam Med. 2014;12(3):270–275. doi: 10.1370/afm.1615. http://dx.doi.org/10.1370/afm.1615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Silow-Carroll S, Alteras T, Stepnick L. Patient-Centered Care for Underserved Populations: Definition and Best Practices. Washington, DC: W.K. Kellogg Foundation; 2006. [Google Scholar]
- 48.Dehlendorf C, Krajewski C, Borrero S. Contraceptive counseling: best practices to ensure quality communication and enable effective contraceptive use. Clin Obstet Gynecol. 2014;57(4):659–673. doi: 10.1097/GRF.0000000000000059. http://dx.doi.org/10.1097/GRF.0000000000000059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Pearson ES. Goal setting as a health behavior change strategy in overweight and obese adults: a systematic literature review examining intervention components. Patient Educ Couns. 2012;87(1):32–42. doi: 10.1016/j.pec.2011.07.018. http://dx.doi.org/10.1016/j.pec.2011.07.018. [DOI] [PubMed] [Google Scholar]
- 50.Hobbs N, Godfrey A, Lara J, et al. Are behavioral interventions effective in increasing physical activity at 12 to 36 months in adults aged 55 to 70 years? A systematic review and meta-analysis. BMC Med. 2013;11(1):75. doi: 10.1186/1741-7015-11-75. http://dx.doi.org/10.1186/1741-7015-11-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lai DT, Cahill K, Qin Y, Tang JL. Motivational interviewing for smoking cessation. Cochrane Database Syst Rev. 2010;(1):CD006936. doi: 10.1002/14651858.CD006936.pub2. http://dx.doi.org/10.1002/14651858.CD006936.pub2. [DOI] [PubMed]
- 52.Pignone MP, Ammerman A, Fernandez L, et al. Counseling to promote a healthy diet in adults: a summary of the evidence for the U.S. Preventive Services Task Force. Am J Prev Med. 2003;24(1):75–92. doi: 10.1016/s0749-3797(02)00580-9. http://dx.doi.org/10.1016/S0749-3797(02)00580-9. [DOI] [PubMed] [Google Scholar]
- 53.Simons-Morton DG, Calfas KJ, Oldenburg B, Burton NW. Effects of interventions in health care settings on physical activity or cardiorespiratory fitness. Am J Prev Med. 1998;15(4):413–430. doi: 10.1016/s0749-3797(98)00078-6. http://dx.doi.org/10.1016/S0749-3797(98)00078-6. [DOI] [PubMed] [Google Scholar]
- 54.Jaccard J, Levitz N. Counseling adolescents about contraception: towards the development of an evidence-based protocol for contraceptive counselors. J Adolesc Health. 2013;52(4 suppl):S6–S13. doi: 10.1016/j.jadohealth.2013.01.018. http://dx.doi.org/10.1016/j.jadohealth.2013.01.018. [DOI] [PubMed] [Google Scholar]
- 55.Kamb ML, Dillon BA, Fishbein M, Willis KL. Quality assurance of HIV prevention counseling in a multi-center randomized controlled trial. Project RESPECT Study Group. Public Health Rep. 1996;111(suppl 1):99–107. [PMC free article] [PubMed] [Google Scholar]
- 56.Lin JS, Whitlock E, O’Connor E, Bauer V. Behavioral counseling to prevent sexually transmitted infections: a systematic review for the U.S. Preventive Services Task Force. Ann Intern Med. 2008;149(7):497–508. W96–W99. doi: 10.7326/0003-4819-149-7-200810070-00011. [DOI] [PubMed] [Google Scholar]
- 57.Lin J, Whitlock E, O’Connor E, Bauer V. Behavioral Counseling to Prevent Sexually Transmitted Infections. Rockville, MD: Agency for Healthcare Research and Quality; 2008. [PubMed] [Google Scholar]
- 58.Berenson AB, Rahman M. A randomized controlled study of two educational interventions on adherence with oral contraceptives and condoms. Contraception. 2012;86(6):716–724. doi: 10.1016/j.contraception.2012.06.007. http://dx.doi.org/10.1016/j.contraception.2012.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Lee JK, Parisi SM, Schwarz EB. Contraceptive counseling and use among women with poorer health. J Womens Health Issues Care. 2013;2(1):103. doi: 10.4172/2325-9795.1000103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Madden T, Mullersman JL, Omvig KJ, Secura GM, Peipert JF. Structured contraceptive counseling provided by the Contraceptive CHOICE Project. Contraception. 2013;88(2):243–249. doi: 10.1016/j.contraception.2012.07.015. http://dx.doi.org/10.1016/j.contraception.2012.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Maslow BS, Morse CB, Schanne A, Loren A, Domchek SM, Gracia CR. Contraceptive use and the role of contraceptive counseling in reproductive-aged women with cancer. Contraception. 2014;90(1):79–85. doi: 10.1016/j.contraception.2014.03.002. http://dx.doi.org/10.1016/j.contraception.2014.03.002. [DOI] [PubMed] [Google Scholar]
- 62.Minnis AM, Mavedzenge SN, Luecke E, Dehlendorf C. Provider counseling to young women seeking family planning services. Perspect Sex Reprod Health. 2014;46(4):223–231. doi: 10.1363/46e1414. http://dx.doi.org/10.1363/46e1414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Zapata LB, Murtaza S, Whiteman MK, et al. Contraceptive counseling and postpartum contraceptive use. Am J Obstet Gynecol. 2015;212(2):171.e1–171.e8. doi: 10.1016/j.ajog.2014.07.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Pazol K, Zapata LB, Tregear SJ, et al. Impact of contraceptive education on contraceptive knowledge and decision making: a systematic review. Am J Prev Med. 2015;49(2S1):S46–S56. doi: 10.1016/j.amepre.2015.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Zapata LB, Tregear SJ, Tiller M, et al. Impact of reminder systems in clinical settings to improve family planning outcomes: a systematic review. Am J Prev Med. 2015;49(2S1):S57–S64. doi: 10.1016/j.amepre.2015.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.CDC. Providing quality family planning services: recommendations of CDC and the U.S. Office of Population Affairs. MMWR Recomm Rep. 2014;63(4):1–54. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.