Abstract
Purpose
The ideal thyroid-stimulating hormone (TSH) range for infertile women attempting conception has not been determined. Current recommendations include optimizing the preconception TSH value to ≤2.5 mIU/L, which is the established goal for pregnant women. The aim of this study was to determine if there is a distinct range of TSH ≤2.5 mIU/L for infertile women undergoing in vitro fertilization (IVF) that improves reproductive outcomes.
Methods
One thousand five hundred ninety-nine euploid blastocyst transfer cycles were evaluated in which TSH measurements were obtained 8 days after embryo transfer. Only euploid embryo transfers were included in an effort to control for embryo quality. Patients were separated into TSH groups utilizing 0.5 mIU/L increments. Implantation, live birth, and miscarriage rates among the TSH groups were compared. Outcomes for individuals on thyroid hormone supplementation and those not requiring supplementation were evaluated.
Results
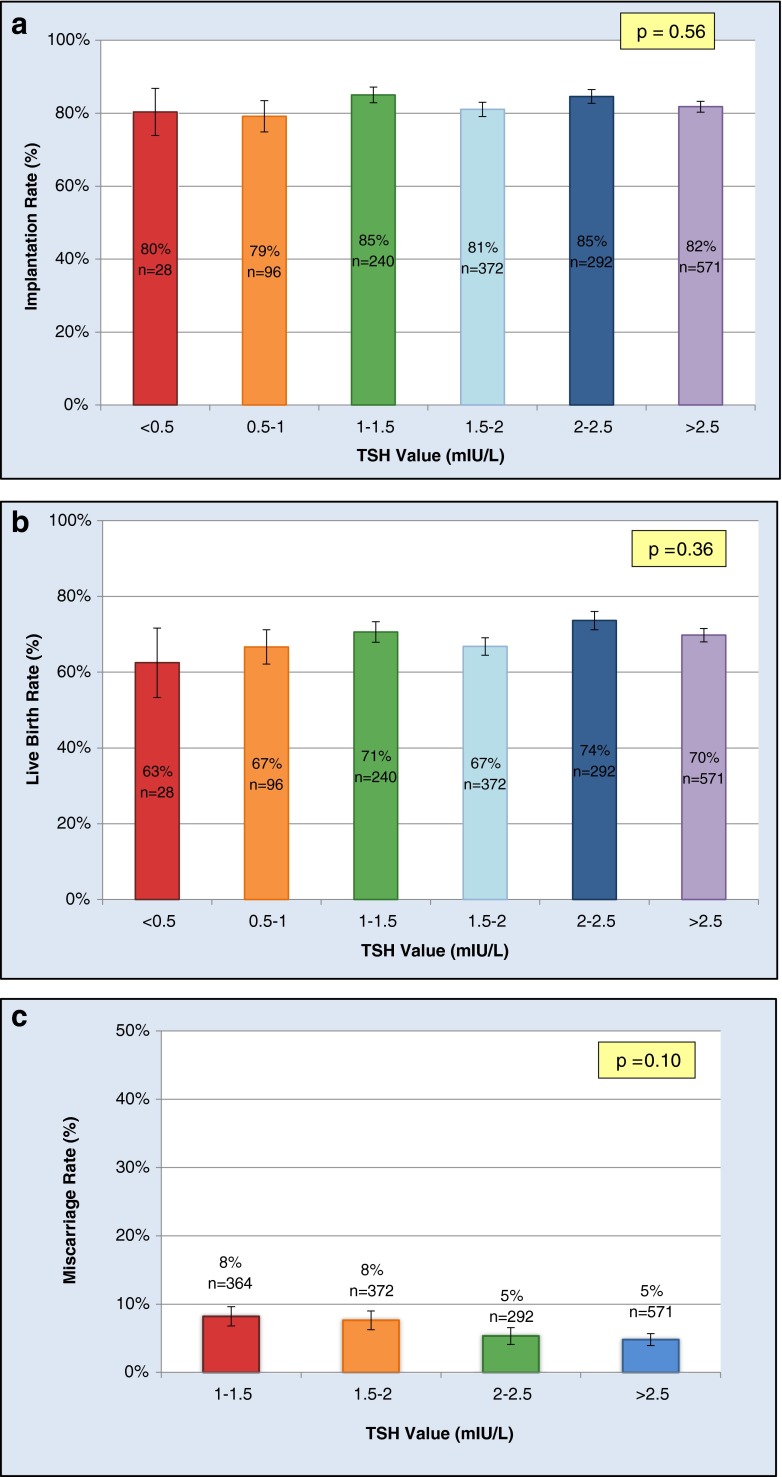
There was no difference in implantation (p = 0.56), live birth (p = 0.36), or miscarriage rates (p = 0.10) between TSH groups. Receiver operating characteristic (ROC) curves for implantation, live birth, and miscarriage approached the line of no discrimination, signifying that there is no value of TSH within the recommended range for pregnancy (≤2.5 mIU/L) that predicts IVF outcomes better than other values in this range. Live birth rates for patients requiring thyroid hormone supplementation and those not on medication were similar (p = 0.86).
Conclusions
The recommended TSH range for pregnancy (≤2.5 mIU/L) may be applied to infertile patients attempting conception without a need for further adjustment.
Keywords: Thyroid-stimulating hormone, Infertility, In vitro fertilization, Implantation, Live birth, Miscarriage
Introduction
Thyroid function varies throughout life and is dependent on particular developmental and physiologic states. Certain medical conditions are associated with altered thyroid function, including diabetes and adrenal insufficiency [1]; however, variations in thyroid function, as determined by thyroid-stimulating hormone (TSH) levels, do not always represent pathology. In utero, increased levels of fetal TSH and thyroid hormones have been observed with increasing gestation, likely due to fetal brain and thyroid maturation, respectively [2]. Thus, in some cases, TSH fluctuations may simply reflect different biological functions of and requirements for thyroid hormones at various life stages.
It is well established that there are separate TSH goals for pregnant and non-pregnant adults [3]. The recommended range for pregnancy is based on data associating TSH levels >2.5 mIU/L with pregnancy complications, such as miscarriage, preterm delivery, and potential impaired fetal neurologic development [3, 4]. Furthermore, it has been demonstrated that clinical outcomes are improved when TSH is kept ≤2.5 mIU/L during early pregnancy [5], which is a notably stricter TSH goal than that of non-pregnant individuals (<4.12 mIU/L) [1].
Given that the recommended TSH ranges for pregnant and non-pregnant adults differ, it is possible that there is a specific TSH range for women attempting conception that may have an impact on reproductive efficiency and success. Defining normal TSH parameters for this population is particularly important, as 100 % of infertile patients are at risk for thyroid dysfunction and should undergo screening [3]. Presently, if high-risk women are identified in the preconception period to have a TSH value above the recommended range for pregnancy (>2.5 mIU/L), they are treated with medication to reach the established TSH goal [3, 6–8]. However, it may be incorrect to assume that the recommended upper limit of TSH for pregnant women is sufficient for infertile women attempting pregnancy. It has not previously been investigated if there is a cutoff below 2.5 mIU/L that optimizes pregnancy outcomes in the infertile population.
When investigating the optimal TSH range for infertile women, only values ≤2.5 mIU/L should be considered, due to the adverse pregnancy outcomes associated with TSH values above this cutoff [3, 4]. The concern that clinical outcomes may be affected by variations within the ≤2.5 mIU/L range is based on previous literature demonstrating that subtle variations of TSH may impact reproductive outcomes. A prospective cohort study of 2497 spontaneous conceptions demonstrated that the incidence of pregnancy loss increased by 60 % for every doubling of TSH (OR = 1.6, 95 % CI 1.04–2.47; p = 0.033) [9]. The findings demonstrate a linear relationship between increasing TSH and risk for pregnancy loss, even within the recommended TSH range [9]. Whether variations of TSH in the recommended range for pregnancy (≤2.5 mIU/L) affect in vitro fertilization (IVF) outcomes in the infertile population is unknown.
This study was devised to determine the optimal range of TSH ≤2.5 mIU/L for infertile women attempting pregnancy through IVF. Infertile patients can be challenging to study as they may have one or more risk factors for pregnancy complications [10–15]. Previous studies investigating the effect of TSH on IVF outcomes have not accounted for the confounding variable of embryonic competence and aneuploidy. This is potentially the largest risk factor for infertility, and recent literature suggests that the prevalence of embryonic aneuploidy may be higher than expected, particularly in young women (>40 % aneuploidy rate in women ≤23 years of age) [16]. In an attempt to control for this significant cause of implantation failure and isolate the effect of TSH on reproductive outcomes, only euploid blastocyst transfers were evaluated in this analysis.
Materials and methods
Study design
This retrospective analysis included all women undergoing their first cycle of IVF with intracytoplasmic sperm injection (ICSI) and comprehensive chromosome screening (CCS) from February 2012 through August 2014. All clinical treatment and embryology procedures were performed at a single academic institution. Institutional review board approval was obtained.
Population
Women with a preexisting diagnosis of thyroid disease, as documented by history, were excluded. Patients found to have a basal TSH value >2.5 mIU/L at their initial visit were started on levothyroxine. Euthyroid status was confirmed prior to embryo transfer (ET) in accordance with current practice standards (TSH ≤2.5 mIU/L within 1 year prior to ET). As such, the timing of basal TSH measurements in relation to ET varied between patients. In order to analyze TSH values drawn at a consistent time between all patients and to most accurately reflect thyroid function at the time of implantation, TSH values drawn 8 days after ET were used in the analysis, as this is obtained for all patients at this center. To control for embryonic aneuploidy, only cycles in which CCS was performed were considered in the analysis.
Stimulation protocols
This study was inclusive of all eligible patients regardless of the specific stimulation protocol. Ovarian stimulation was achieved using purified or recombinant gonadotropins. Protocols consisted of microdose leuprolide flare, pituitary downregulation with leuprolide, or gonadotropin-releasing hormone (GnRH) antagonist cycles. ICSI was performed in all cases, as this is routine practice for all CCS cases at our facility. Viable blastocysts underwent trophectoderm biopsy on day 5 or 6 for CCS.
Patients had either a fresh or frozen ET based on cycle-specific criteria. Fresh ETs were performed on the morning of day 6. A single-embryo transfer (SET) or double-embryo transfer (DET) was performed in accordance with the American Society for Reproductive Medicine (ASRM) guidelines [17].
Laboratory analysis
Basal TSH values were measured on the date of the initial visit, and elevated levels (>2.5 mIU/L) were corrected with levothyroxine. Euthyroid status was confirmed by documentation of a normal TSH value within 1 year prior to embryo transfer. Eight days after ET, routine blood work included serum beta-human chorionic gonadotropin (hCG) and TSH measurements. Patients with a TSH value >2.5 mIU/L were started on levothyroxine therapy, or dosages were adjusted if patients had previously been started on this medication. Patients with a positive pregnancy test (>5 IU/L) and subsequent appropriate rise in beta-hCG had a transvaginal ultrasound performed 15 days after ET. Pregnancies were following until approximately 9 weeks of gestation, and fetal cardiac activity was documented.
Data analysis
TSH values drawn 8 days after embryo transfer were empirically grouped using 0.5 mIU/L increments. These increments were chosen to facilitate the detection of the impact of subtle variations of TSH in the ≤2.5 mIU/L range. TSH values are reported as mean ± standard error. The implantation rate (IR) was calculated by dividing the number of gestational sacs by the number of embryos transferred. Live birth was defined as the delivery of a viable fetus after 24 weeks of gestation. The live birth rate (LBR) was calculated by dividing the number of live births by the number of embryos transferred. The miscarriage rate was calculated by dividing the number of fetal heartbeats at discharge by the maximum number of gestational sacs visualized and subtracting this value from 1.
The primary outcome was defined as the IR of euploid blastocysts compared among the different TSH groups. Secondary outcomes included the live birth and miscarriage rates between TSH groups. The LBR based on thyroid hormone supplementation was also evaluated to determine if outcomes for patients with normal TSH values on thyroid supplementation differed from those not requiring medication.
Statistical analyses were performed using OpenEpi Version 3.03 and AnalyzeIt version 2.30. Demographic data were assessed for normality and analysis of variance (ANOVA) tests were used to compare normally distributed data. Nonparametric data (estradiol levels) were compared using a Kruskal-Wallis test. Chi-Squared tests were used to compare categorical variables. Receiver operating characteristic (ROC) analyses were performed to determine if there is a discriminatory value of TSH within the recommended range for pregnancy for predicting implantation, live birth, or miscarriage. The ROC curves were generated by plotting the sensitivity and 1-specificity of all TSH values for the given outcome variable. ANOVA was used to compare the means of the IR, LBR, and miscarriage rate between TSH groups. For the analysis of miscarriage, the lowest three TSH groups were grouped together due to the small number of patients in each of these three groups. A t test was used to compare TSH values between fresh and frozen cycles.
Results
One thousand five hundred ninety-nine transfer cycles were included for analysis. Women were similar with regards to age, follicle-stimulating hormone (FSH), basal antral follicle count (BAFC), peak estradiol (E2), endometrial thickness, and the number of embryos transferred (Table 1). Causes of infertility were categorized according to the Society for Assisted Reproductive Technology (SART) diagnoses and included the following: male factor (35.1 %), ovulatory dysfunction (17.7 %), diminished ovarian reserve (7.8 %), tubal factor (6.3 %), endometriosis (3.1 %), uterine factor (1.3 %), unknown (13.8 %), and others (14.9 %). Of the 1599 cycles, 1191 were frozen ETs and 408 were fresh ETs. There were 1009 single-embryo transfers and 590 double-embryo transfers.
Table 1.
Demographics of TSH groups
| TSH (mIU/L) | N | Age (years) | FSH (mIU/mL) | BAFC (n) | Peak E2 on day of hCG (pg/mL) | Endometrial thickness (mm) | Number of embryos transferred (n) |
|---|---|---|---|---|---|---|---|
| <0.5 | 28 | 35.8 ± 4.5 | 7.2 ± 2.1 | 13.1 ± 7 | 2333 (1347-2794) | 9.7 ± 2.7 | 1.5 ± 0.5 |
| 0.5 to <1 | 96 | 35.7 ± 3.7 | 6.7 ± 2.7 | 16.5 ± 9.7 | 2509 (1596-3684) | 9 ± 2 | 1.4 ± 0.5 |
| 1 to <1.5 | 240 | 35.1 ± 4.3 | 7.1 ± 2.8 | 16.7 ± 9.7 | 2241 (1333-3056) | 8.9 ± 1.7 | 1.3 ± 0.5 |
| 1.5 to <2 | 372 | 35.3 ± 4.2 | 6.7 ± 2.3 | 16.9 ± 10.7 | 2157 (1432-3025) | 9 ± 1.9 | 1.4 ± 0.5 |
| 2 to ≤2.5 | 292 | 35.3 ± 4 | 7.2 ± 2.6 | 17 ± 8.8 | 2185 (1551-2904) | 8.8 ± 1.9 | 1.4 ± 0.5 |
| >2.5 | 571 | 34.9 ± 4.3 | 7.3 ± 4.4 | 16 ± 8.9 | 2099 (1397-2863) | 8.9 ± 1.9 | 1.4 ± 0.5 |
| p value | 0.38 | 0.11 | 0.24 | 0.09 | 0.23 | 0.14 |
Values are reported as mean ± standard deviation or median (interquartile range) if data are nonparametric (peak E2)
The mean TSH value for the study population was 2.37 ± 0.03 mIU/L. For patients not requiring thyroid hormone supplementation (n = 1015), the mean TSH value was 2.18 ± 0.03 mIU/L. The mean TSH value among patients requiring levothyroxine treatment (n = 584) was 2.69 ± 0.06 mIU/L.
The overall implantation and live birth rates were 82.4 and 69.6 %, respectively. The overall miscarriage rate was 6.3 %. The areas under the ROC curves for implantation, live birth, and miscarriage were 0.519 (95 % CI 0.475–0.563), 0.530 (95 % CI 0.497–0.563), and 0.563 (95 % CI 0.497–0.629), respectively (Fig. 1a–c). All three ROC curves approached the line of no discrimination, indicating that there is no value of TSH within the recommended range for pregnancy that predicts implantation, live birth, or miscarriage in the infertile population better than other values in this range.
Fig. 1.
ROC plots representing the sensitivity and 1-specificity of each TSH value for predicting the outcomes of a implantation, b live birth, and c miscarriage
As there was no cutoff value of TSH identified in the ROC analysis, the IR, LBR, and miscarriage rates among patients stratified by TSH were compared. Outcomes were evaluated among the following TSH groups: <0.5, 0.5 to <1.0, 1.0 to <1.5, 1.5 to <2, 2 to ≤2.5, and >2.5 mIU/L. There was no difference in the implantation or live birth rate between the different TSH groups (p = 0.56 and p = 0.36, respectively) (Fig. 2a, b). The miscarriage rates among the various TSH groups were also similar (p = 0.10) (Fig. 2c).
Fig. 2.
a Implantation, b live birth, and c miscarriage rates between TSH groups are not statistically different. Error bars represent standard error
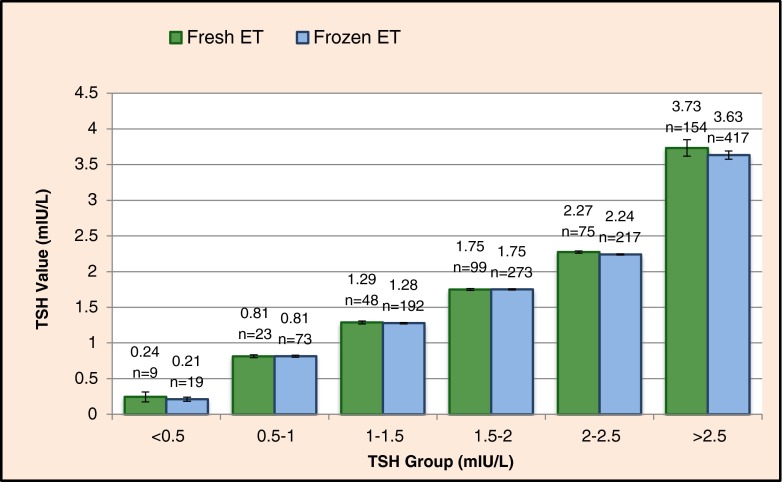
There was no difference in the live birth rate between women taking levothyroxine and those not on levothyroxine (69.9 vs. 69.5 %, respectively; p = 0.86) (Fig. 3). The overall live birth rates for fresh and frozen ET cycles were 66.5 and 70.7 %, respectively (p = 0.09). The mean TSH values between fresh and frozen ET cycles within each TSH group were not significantly different (p = 0.08–0.97) (Fig. 4). The p value of 0.08 corresponds to the fresh and frozen TSH values (2.27 and 2.24 mIU/L, respectively) in the TSH of 2–2.5 mIU/L group. These TSH values are clearly quite similar, and it is likely that the p value approaches statistical significance due to the large population size and is not of clinical significance.
Fig. 3.
Live birth rate for women taking levothyroxine and those not taking levothyroxine. Error bars represent standard error
Fig. 4.
TSH values between fresh and frozen ETs within each TSH group. Data labels represent TSH mean (mIU/L) and sample size. Error bars represent standard error. All p values are non-significant (range 0.08–0.97)
Discussion
In this large cohort of infertile patients, the optimal TSH range for patients attempting conception through IVF was investigated. In particular, the impact of variations of TSH within the recommended range for pregnancy (≤2.5 mIU/L) on IVF outcomes was evaluated. No association between varying TSH values and implantation, live birth, or miscarriage rates was detected.
The mean TSH value for all patients was below 2.5 mIU/L; however, as demonstrated in the figures, there were patients with TSH values over 2.5 mIU/L 8 days after embryo transfer. One possible explanation for this finding is that elevations of TSH may be a direct effect of ovarian stimulation, as it has been demonstrated that up to one third of euthyroid women may experience elevations of TSH over 2.5 mIU/L after undergoing IVF [18]. Second, patients had documentation of euthyroid status within 1 year prior to embryo transfer. Therefore, it is possible that TSH values at the time of actual embryo transfer were at or above 2.5 mIU/L in select patients. Regardless of the potential etiologies of TSH elevations in a portion of the study population, the objective of the study was to evaluate outcomes based on TSH values. The findings demonstrate that variations of TSH, particularly within the ≤2.5 mIU/L range, do not differentially impact IVF outcomes.
The live birth rate was similar for women on levothyroxine and those not taking levothyroxine, suggesting that equivalent IVF outcomes may be expected after providing thyroid hormone supplementation to patients with elevated TSH levels. Another important clinical application of this study is that the TSH range for early pregnancy is sufficient for infertile women attempting conception through IVF. We did not evaluate for an upper limit of TSH >2.5 mIU/L, as values above this cutoff have been associated with adverse pregnancy outcomes and would not be appropriate for women attempting pregnancy [3, 4]. Within the recommended TSH range for pregnancy, there was no TSH value more predictive of IVF success than other values in this range.
A notable strength of this study is that we eliminated the variable of embryonic competence by only evaluating euploid blastocyst transfers. To our knowledge, this is the first study to evaluate such a population, which facilitated a more specific evaluation of the TSH effect on IVF outcomes. Additional strengths of this study are the consistent timing of the TSH measurements among the study population and the fact that TSH was evaluated during the interval that may best reflect peri-implantation thyroid status. Limitations of the study include its retrospective design and lack of data on embryologic outcomes or on the presence of antithyroid antibodies.
TSH values drawn 8 days after embryo transfer were utilized in this analysis as there were no standardized preimplantation TSH values available for the study population. However, preimplantation TSH values may provide information regarding expected ovarian stimulation response and IVF outcomes. Previous analyses have exhibited significant inter- and intra-study variability with regards to the timing of TSH measurements in relation to the IVF cycle [18–22]. If IVF outcomes based on preimplantation TSH values are to be evaluated, TSH levels should be drawn at a standardized time near the start of an IVF cycle. One such retrospective cohort study evaluated outcomes based on TSH values measured within 6 weeks prior to cycle start [21]. This analysis detected no difference in the number of oocytes retrieved, fertilization rates, or pregnancy outcomes when comparing women with a TSH value above and below 2.5 mIU/L [21]. The consistent timing of TSH measurements and the proximity of these measurements to cycle start are commendable strengths of this study. It is important to note, however, that thyroid hormone supplementation was initiated in patients found to have elevated TSH levels within 6 weeks prior to IVF. American Thyroid Association recommendations include repeating TSH measurements 4–6 weeks after the initiation of medication in case dose adjustments are required [23]. Thus, it is possible that the actual TSH value at the time of IVF differed from the value used in the analysis. It would be beneficial for future analyses to evaluate the impact of preimplantation TSH measured at the time of cycle start. These studies may clarify what impact, if any, preimplantation TSH values have on cycle response and embryo development.
Despite evidence of a linear relationship between lower TSH values and improved outcomes in spontaneous conceptions [9], no such association was detected in this infertile population attempting conception through IVF. Variations of TSH within the recommended range for pregnancy (≤2.5 mIU/L) have no effect on outcomes after euploid blastocyst transfer.
Footnotes
Capsule
The TSH goal for pregnancy (≤ 2.5 mIU/L) is appropriate for infertile patients attempting conception, and variations within this range do not impact IVF outcomes.
References
- 1.Garber JR, Cobin RH, Gharib H, Hennessey JV, Klein I, Mechanick JI, et al. Clinical practice guidelines for hypothyroidism in adults: cosponsored by the American Association of Clinical Endocrinologists and the American Thyroid Association. Endocr Pract. 2012;18(6):988–1028. doi: 10.4158/EP12280.GL. [DOI] [PubMed] [Google Scholar]
- 2.Thorpe-Beeston JG, Nicolaides KH, Felton CV, Butler J, McGregor AM. Maturation of the secretion of thyroid hormone and thyroid-stimulating hormone in the fetus. N Engl J Med. 1991;324(8):532–536. doi: 10.1056/NEJM199102213240805. [DOI] [PubMed] [Google Scholar]
- 3.Stagnaro-Green A, Abalovich M, Alexander E, Azizi F, Mestman J, Negro R, et al. Guidelines of the American Thyroid Association for the diagnosis and management of thyroid disease during pregnancy and postpartum. American Thyroid Association Taskforce on Thyroid Disease During Pregnancy and Postpartum. Thyroid. 2011;21(10):1081–1125. doi: 10.1089/thy.2011.0087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Casey BM, Dashe JS, Wells CE, McIntire DD, Byrd W, Leveno KJ, et al. Subclinical hypothyroidism and pregnancy outcomes. Obstet Gynecol. 2005;105(2):239–245. doi: 10.1097/01.AOG.0000152345.99421.22. [DOI] [PubMed] [Google Scholar]
- 5.Negro R, Schwartz A, Gismondi R, Tinelli A, Mangieri T, Stagnaro-Green A. Universal screening versus case finding for detection and treatment of thyroid hormonal dysfunction during pregnancy. J Clin Endocrinol Metab. 2010;95(4):1699–1707. doi: 10.1210/jc.2009-2009. [DOI] [PubMed] [Google Scholar]
- 6.De Groot L, Abalovich M, Alexander EK, Amino N, Barbour L, Cobin RH, et al. Management of thyroid dysfunction during pregnancy and postpartum: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2012;97(8):2543–2565. doi: 10.1210/jc.2011-2803. [DOI] [PubMed] [Google Scholar]
- 7.Abalovich M, Gutierrez S, Alcaraz G, Maccallini G, Garcia A, Levalle O. Overt and subclinical hypothyroidism complicating pregnancy. Thyroid. 2002;12(1):63–68. doi: 10.1089/105072502753451986. [DOI] [PubMed] [Google Scholar]
- 8.Kim CH, Ahn JW, Kang SP, Kim SH, Chae HD, Kang BM. Effect of levothyroxine treatment on in vitro fertilization and pregnancy outcome in infertile women with subclinical hypothyroidism undergoing in vitro fertilization/intracytoplasmic sperm injection. Fertil Steril. 2011;95(5):1650–1654. doi: 10.1016/j.fertnstert.2010.12.004. [DOI] [PubMed] [Google Scholar]
- 9.Benhadi N, Wiersinga WM, Reitsma JB, Vrijkotte TG, Bonsel GJ. Higher maternal TSH levels in pregnancy are associated with increased risk for miscarriage, fetal or neonatal death. Eur J Endocrinol. 2009;160(6):985–991. doi: 10.1530/EJE-08-0953. [DOI] [PubMed] [Google Scholar]
- 10.Krassas GE, Poppe K, Glinoer D. Thyroid function and human reproductive health. Endocr Rev. 2010;31(5):702–755. doi: 10.1210/er.2009-0041. [DOI] [PubMed] [Google Scholar]
- 11.Gleicher N, Kushnir VA, Weghofer A, Barad DH. The “graying” of infertility services: an impending revolution nobody is ready for. Reprod Biol Endocrinol. 2014;12:63. doi: 10.1186/1477-7827-12-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hodes-Wertz B, Grifo J, Ghadir S, Kaplan B, Laskin CA, Glassner M, et al. Idiopathic recurrent miscarriage is caused mostly by aneuploid embryos. Fertil Steril. 2012;98(3):675–680. doi: 10.1016/j.fertnstert.2012.05.025. [DOI] [PubMed] [Google Scholar]
- 13.Clementini E, Palka C, Iezzi I, Stuppia L, Guanciali-Franchi P, Tiboni GM. Prevalence of chromosomal abnormalities in 2078 infertile couples referred for assisted reproductive techniques. Hum Reprod. 2005;20(2):437–442. doi: 10.1093/humrep/deh626. [DOI] [PubMed] [Google Scholar]
- 14.Chan YY, Jayaprakasan K, Zamora J, Thornton JG, Raine-Fenning N, Coomarasamy A. The prevalence of congenital uterine anomalies in unselected and high-risk populations: a systematic review. Hum Reprod Update. 2011;17(6):761–771. doi: 10.1093/humupd/dmr028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chan YY, Jayaprakasan K, Tan A, Thornton JG, Coomarasamy A, Raine-Fenning NJ. Reproductive outcomes in women with congenital uterine anomalies: a systematic review. Ultrasound Obstet Gynecol. 2011;38(4):371–382. doi: 10.1002/uog.10056. [DOI] [PubMed] [Google Scholar]
- 16.Franasiak JM, Forman EJ, Hong KH, Werner MD, Upham KM, Treff NR, et al. The nature of aneuploidy with increasing age of the female partner: a review of 15,169 consecutive trophectoderm biopsies evaluated with comprehensive chromosomal screening. Fertil Steril. 2014;101(3):63.e1. doi: 10.1016/j.fertnstert.2013.11.004. [DOI] [PubMed] [Google Scholar]
- 17.ASRM Practice Committee of the American Society for Reproductive Medicine and the Practice Committee of the Society for Assisted Reproductive Technology. Criteria for number of embryos to transfer: a committee opinion. Fertil Steril. 2013;99(1):44–46. doi: 10.1016/j.fertnstert.2012.09.038. [DOI] [PubMed] [Google Scholar]
- 18.Benaglia L, Busnelli A, Somigliana E, Leonardi M, Vannucchi G, De Leo S, et al. Incidence of elevation of serum thyroid-stimulating hormone during controlled ovarian hyperstimulation for in vitro fertilization. Eur J Obstet Gynecol Reprod Biol. 2014;173:53–57. doi: 10.1016/j.ejogrb.2013.11.003. [DOI] [PubMed] [Google Scholar]
- 19.Reh A, Grifo J, Danoff A. What is a normal thyroid-stimulating hormone (TSH) level? Effects of stricter TSH thresholds on pregnancy outcomes after in vitro fertilization. Fertil Steril. 2010;94(7):2920–2922. doi: 10.1016/j.fertnstert.2010.06.041. [DOI] [PubMed] [Google Scholar]
- 20.Mintziori G, Goulis DG, Gialamas E, Dosopoulos K, Zouzoulas D, Gitas G, et al. Association of TSH concentrations and thyroid autoimmunity with IVF outcome in women with TSH concentrations within normal adult range. Gynecol Obstet Invest. 2014;77(2):84–88. doi: 10.1159/000357193. [DOI] [PubMed] [Google Scholar]
- 21.Michalakis KG, Mesen TB, Brayboy LM, Yu B, Richter KS, Levy M, et al. Subclinical elevations of thyroid-stimulating hormone and assisted reproductive technology outcomes. Fertil Steril. 2011;95(8):2634–2637. doi: 10.1016/j.fertnstert.2011.02.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Abdel Rahman AH, Aly Abbassy H, Abbassy AA. Improved in vitro fertilization outcomes after treatment of subclinical hypothyroidism in infertile women. Endocr Pract. 2010;16(5):792–797. doi: 10.4158/EP09365.OR. [DOI] [PubMed] [Google Scholar]
- 23.Jonklaas J, Bianco AC, Bauer AJ, Burman KD, Cappola AR, Celi FS, et al. Guidelines for the treatment of hypothyroidism: prepared by the American Thyroid Association task force on thyroid hormone replacement. Thyroid. 2014;24(12):1670–1751. doi: 10.1089/thy.2014.0028. [DOI] [PMC free article] [PubMed] [Google Scholar]