Abstract
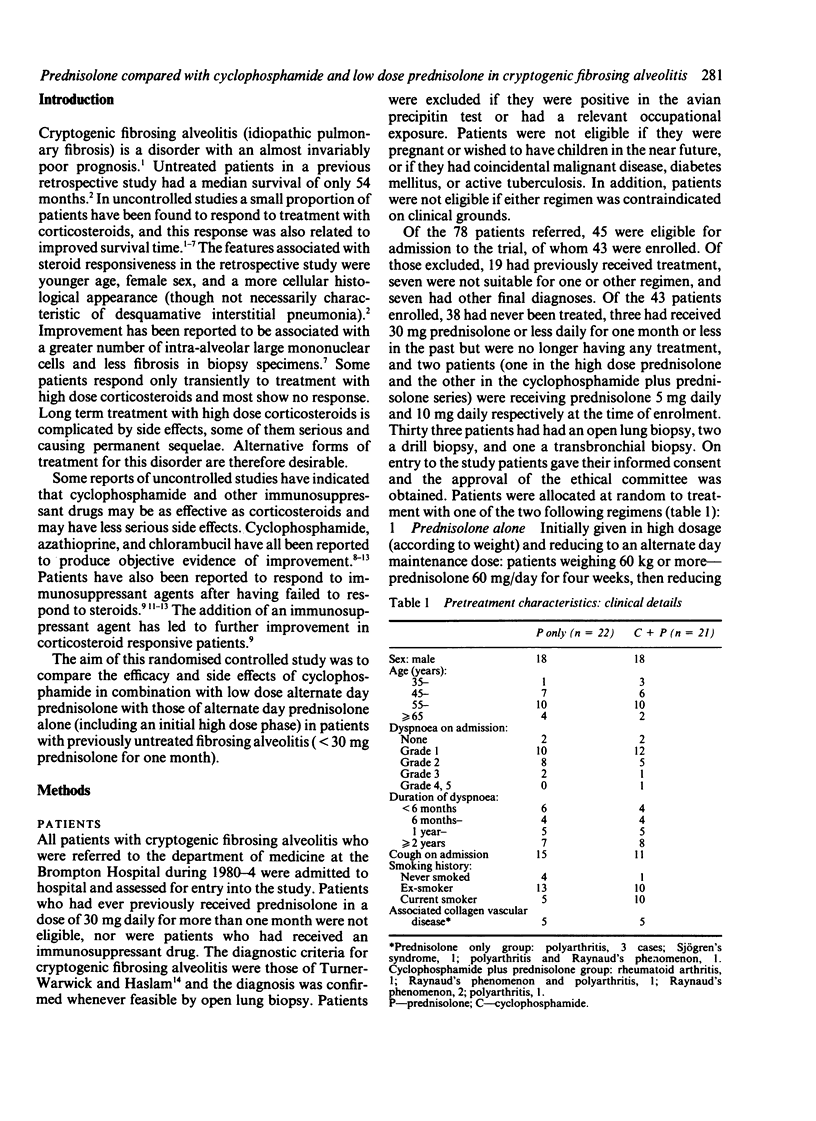
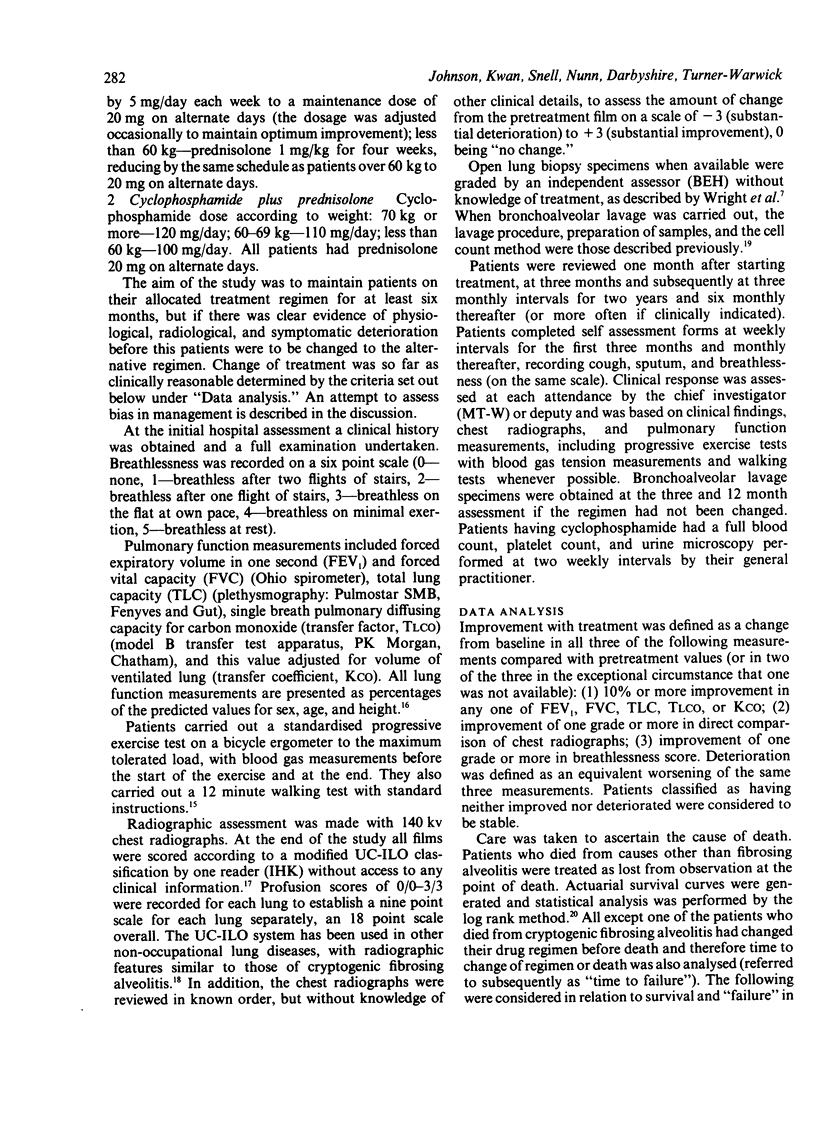
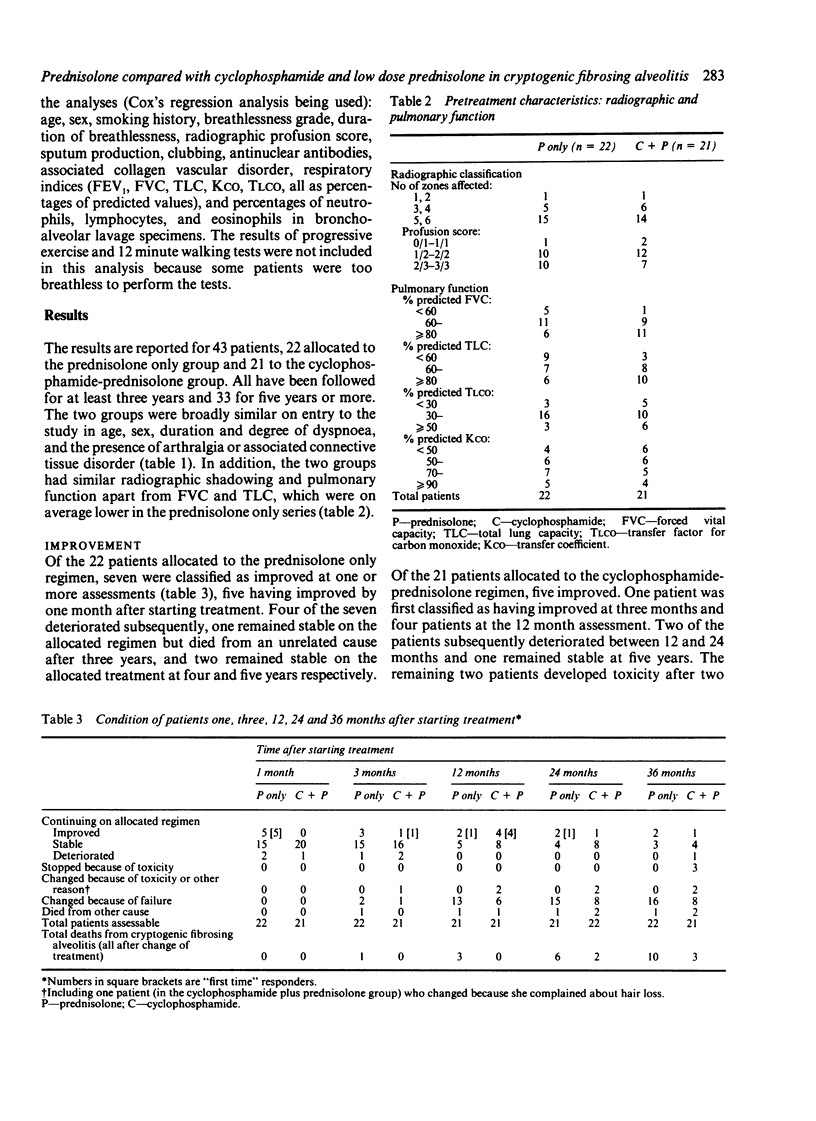
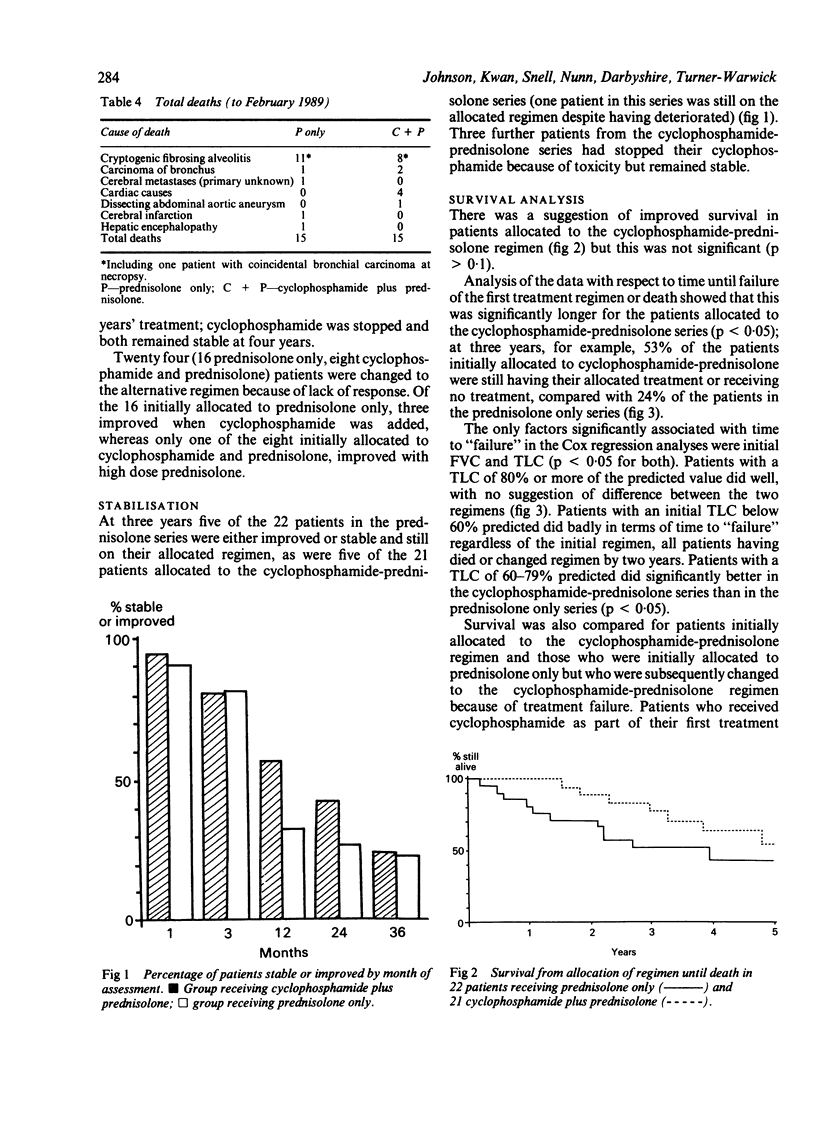
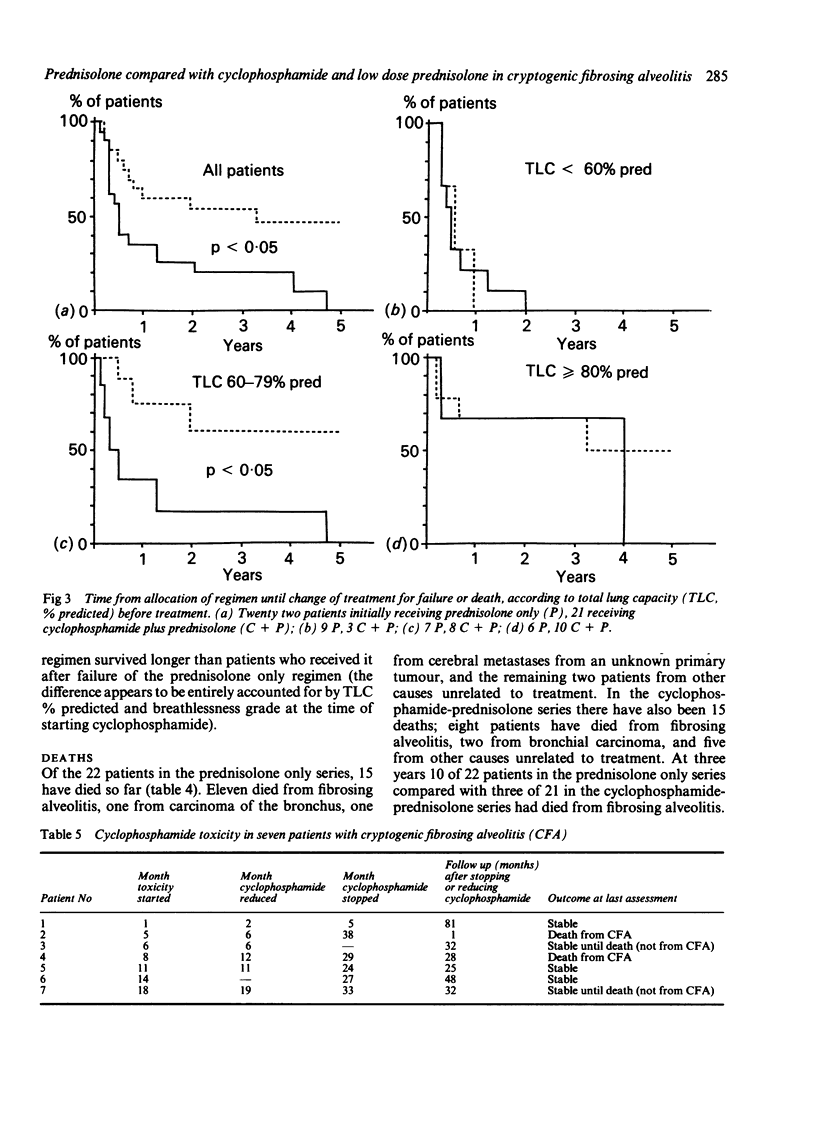
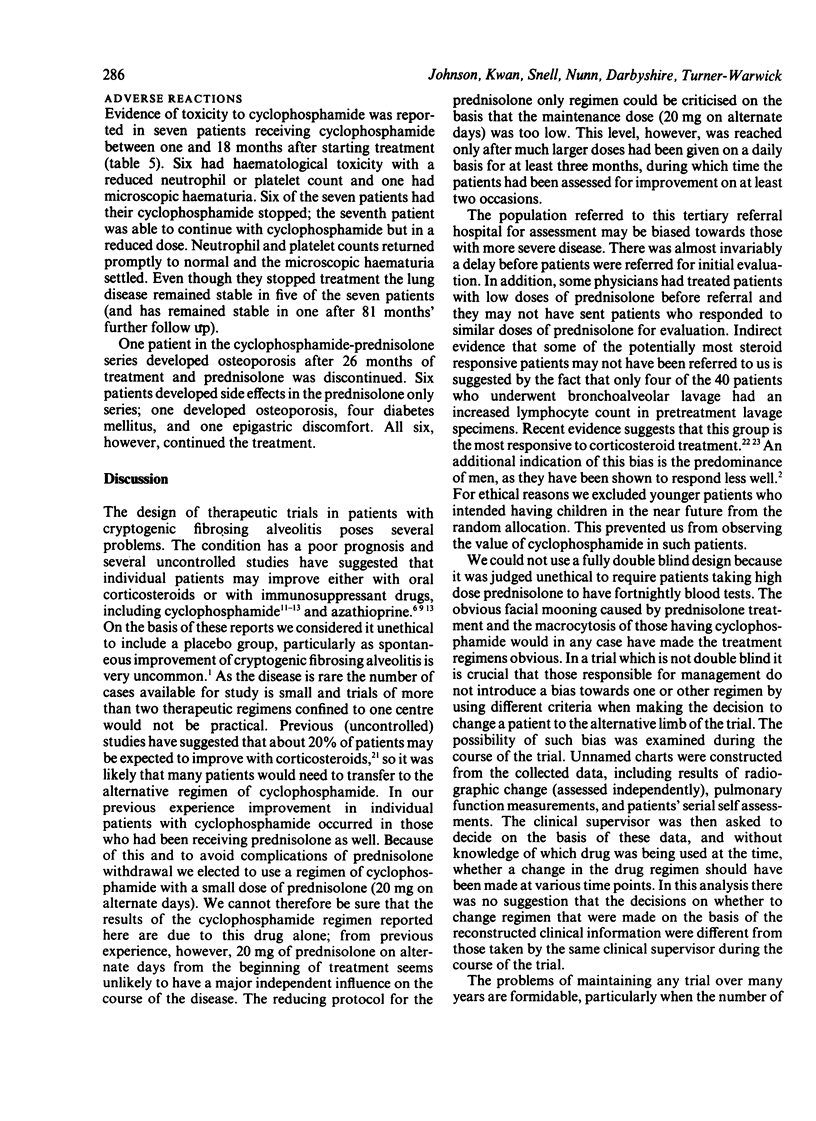
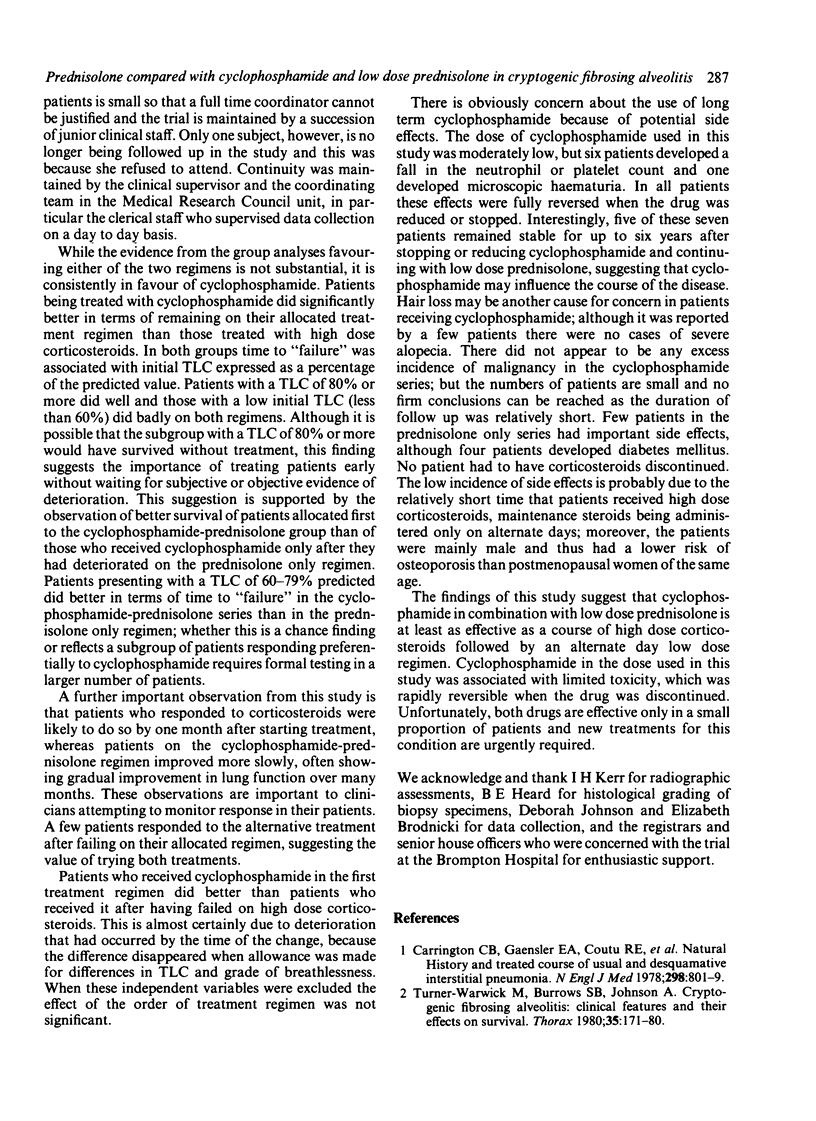
In a randomised, controlled study alternate day prednisolone with an initial high dose phase ("prednisolone only series") has been compared with cyclophosphamide plus alternate day low dose prednisolone ("cyclophosphamide-prednisolone series") in 43 patients with previously untreated fibrosing alveolitis (five patients had received prednisolone in minimal dosage). In the prednisolone only series prednisolone 60 mg daily was given for one month and then reduced by 5 mg a week to 20 mg on alternate days or the minimum dose to maintain early improvement. Patients in the cyclophosphamide-prednisolone series received 100, 110, or 120 mg cyclophosphamide daily (depending on body weight) plus 20 mg prednisolone on alternate days. Treatment was continued indefinitely, or changed to the alternative regimen if the patient deteriorated, failed to improve, or developed drug toxicity. For response to treatment (as judged by change in breathlessness score, radiographic appearance, and lung function) patients were classified as improved, stable, or deteriorating. Deaths from cryptogenic fibrosing alveolitis were also analysed. Improvement had occurred at one or more assessments in seven of the 22 patients in the prednisolone only series and in five of the 21 patients in the cyclophosphamide-prednisolone series. At three years, however, only two of the 22 patients in the prednisolone only series were still improved and three stable, compared with one and seven of the 21 patients in the cyclophosphamide-prednisolone series (three of the seven had stopped treatment because of toxicity). Life table analysis suggested better survival in patients in the cyclophosphamide-prednisolone series but this was not significant. At three years 10 of 22 patients in the prednisolone only series had died compared with three of 21 patients in the cyclophosphamide-prednisolone series. With death or failure of first treatment regimen as outcome there was a significant advantage to the patients having cyclophosphamide-prednisolone. This advantage was explained in part by the better lung volumes in this group on admission. After allowance had been made for total lung capacity (TLC), no other factor was predictive of outcome. Analyses of subgroups according to TLC on admission showed that patients with a TLC below 60% predicted did badly and those with a TLC of 80% or more predicted did well with both regimens. Patients with an initial TLC of 60-79% predicted did better with the cyclophosphamide-prednisolone regimen. Side effects were uncommon in both series and those due to cyclophosphamide resolved when treatment was stopped. The combination of cyclophosphamide with prednisolone may be an alternative to prednisolone alone with an initial high dose phase. Many patients, however, failed to respond to either treatment.
Full text
PDF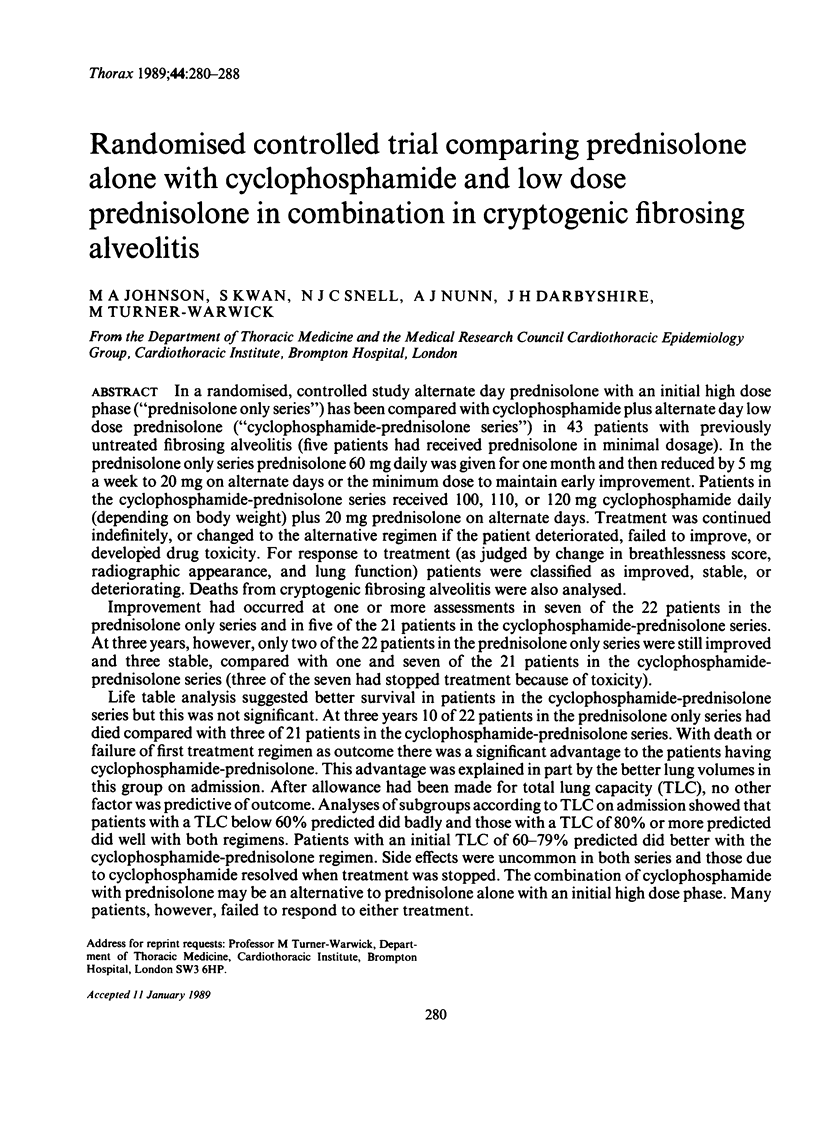
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Brown C. H., Turner-Warwick M. The treatment of cryptogenic fibrosing alveolitis with immunosuppressant drugs. Q J Med. 1971 Apr;40(158):289–302. doi: 10.1093/oxfordjournals.qjmed.a067271. [DOI] [PubMed] [Google Scholar]
- Carrington C. B., Gaensler E. A., Coutu R. E., FitzGerald M. X., Gupta R. G. Natural history and treated course of usual and desquamative interstitial pneumonia. N Engl J Med. 1978 Apr 13;298(15):801–809. doi: 10.1056/NEJM197804132981501. [DOI] [PubMed] [Google Scholar]
- Crystal R. G., Fulmer J. D., Roberts W. C., Moss M. L., Line B. R., Reynolds H. Y. Idiopathic pulmonary fibrosis. Clinical, histologic, radiographic, physiologic, scintigraphic, cytologic, and biochemical aspects. Ann Intern Med. 1976 Dec;85(6):769–788. doi: 10.7326/0003-4819-85-6-769. [DOI] [PubMed] [Google Scholar]
- Ferris B. G. Epidemiology Standardization Project (American Thoracic Society). Am Rev Respir Dis. 1978 Dec;118(6 Pt 2):1–120. [PubMed] [Google Scholar]
- Haslam P. L., Turton C. W., Lukoszek A., Salsbury A. J., Dewar A., Collins J. V., Turner-Warwick M. Bronchoalveolar lavage fluid cell counts in cryptogenic fibrosing alveolitis and their relation to therapy. Thorax. 1980 May;35(5):328–339. doi: 10.1136/thx.35.5.328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGavin C. R., Artvinli M., Naoe H., McHardy G. J. Dyspnoea, disability, and distance walked: comparison of estimates of exercise performance in respiratory disease. Br Med J. 1978 Jul 22;2(6132):241–243. doi: 10.1136/bmj.2.6132.241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meier-Sydow J., Rust M., Kronenberger H., Thiel C., Amthor M., Riemann H. Langzeitbeobachtung von Lungenfunktionsparametern bei idiopathischen Lungenfibrosen unter Prednison und Azathioprin oder D-Penicillamin. Prax Klin Pneumol. 1979 Apr;33 (Suppl 1):680–688. [PubMed] [Google Scholar]
- Meuret G., Fueter R., Gloor F. Early stage of fulminant idiopathic pulmonary fibrosis cured by intense combination therapy using cyclophosphamide, vincristine, and prednisone. Respiration. 1978;36(4):228–233. doi: 10.1159/000193955. [DOI] [PubMed] [Google Scholar]
- Peto R., Pike M. C., Armitage P., Breslow N. E., Cox D. R., Howard S. V., Mantel N., McPherson K., Peto J., Smith P. G. Design and analysis of randomized clinical trials requiring prolonged observation of each patient. II. analysis and examples. Br J Cancer. 1977 Jan;35(1):1–39. doi: 10.1038/bjc.1977.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stack B. H., Choo-Kang Y. F., Heard B. E. The prognosis of cryptogenic fibrosing alveolitis. Thorax. 1972 Sep;27(5):535–542. doi: 10.1136/thx.27.5.535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner-Warwick M., Burrows B., Johnson A. Cryptogenic fibrosing alveolitis: clinical features and their influence on survival. Thorax. 1980 Mar;35(3):171–180. doi: 10.1136/thx.35.3.171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner-Warwick M., Haslam P. L. The value of serial bronchoalveolar lavages in assessing the clinical progress of patients with cryptogenic fibrosing alveolitis. Am Rev Respir Dis. 1987 Jan;135(1):26–34. doi: 10.1164/arrd.1987.135.1.26. [DOI] [PubMed] [Google Scholar]
- Turner-Warwick M., Haslam P. Antibodies in some chronic fibrosing lung diseases. I. Non organ-specific autoantibodies. Clin Allergy. 1971 Mar;1(1):83–95. doi: 10.1111/j.1365-2222.1971.tb02450.x. [DOI] [PubMed] [Google Scholar]
- Watters L. C., Schwarz M. I., Cherniack R. M., Waldron J. A., Dunn T. L., Stanford R. E., King T. E. Idiopathic pulmonary fibrosis. Pretreatment bronchoalveolar lavage cellular constituents and their relationships with lung histopathology and clinical response to therapy. Am Rev Respir Dis. 1987 Mar;135(3):696–704. doi: 10.1164/arrd.1987.135.3.696. [DOI] [PubMed] [Google Scholar]
- Weese W. C., Levine B. W., Kazemi H. Interstitial lung disease resistant to corticosteroid therapy. Report of three cases treated with azathioprine or cyclophosphamide. Chest. 1975 Jan;67(1):57–60. doi: 10.1378/chest.67.1.57. [DOI] [PubMed] [Google Scholar]
- Winterbauer R. H., Hammar S. P., Hallman K. O., Hays J. E., Pardee N. E., Morgan E. H., Allen J. D., Moores K. D., Bush W., Walker J. H. Diffuse interstitial pneumonitis. Clinicopathologic correlations in 20 patients treated with prednisone/azathioprine. Am J Med. 1978 Oct;65(4):661–672. doi: 10.1016/0002-9343(78)90855-0. [DOI] [PubMed] [Google Scholar]
- Wright P. H., Heard B. E., Steel S. J., Turner-Warwick M. Cryptogenic fibrosing alveolitis: assessment by graded trephine lung biopsy histology compared with clinical, radiographic, and physiological features. Br J Dis Chest. 1981 Jan;75(1):61–70. doi: 10.1016/s0007-0971(81)80008-3. [DOI] [PubMed] [Google Scholar]


