Abstract
Background
In 2013–2014, an outbreak of serogroup B meningococcal disease occurred among persons linked to a New Jersey university (University A). In the absence of a licensed serogroup B meningococcal (MenB) vaccine in the US, the Food and Drug Administration authorized use of an investigational MenB vaccine to control the outbreak. An investigation of the outbreak and response was undertaken to determine the population at risk and assess vaccination coverage.
Methods
The epidemiologic investigation relied on compilation and review of case and population data, laboratory typing of meningococcal isolates, and unstructured interviews with university staff. Vaccination coverage data were collected during the vaccination campaign held under an expanded access Investigational New Drug protocol.
Results
Between March 25, 2013 and March 10, 2014, 9 cases of serogroup B meningococcal disease occurred in persons linked to University A. Laboratory typing results were identical for all 8 isolates available. Through May 14, 2014, 89.1% coverage with the two-dose vaccination series was achieved in the target population. From the initiation of MenB vaccination through February 1, 2015, no additional cases of serogroup B meningococcal disease occurred in University A students. However, the 9th case occurred in March 2014 in an unvaccinated close contact of University A students.
Conclusions
No serogroup B meningococcal disease cases occurred in persons who received 1 or more doses of 4CMenB vaccine, suggesting 4CMenB may have protected vaccinated individuals from disease. However, the 9th case demonstrates that carriage of serogroup B Nesisseria meningitidis among vaccinated persons was not eliminated.
Keywords: Meningococcal disease, vaccine, university, epidemiology
Introduction
Between March 25, 2013 and March 10, 2014, 9 cases of serogroup B meningococcal disease were reported in persons linked to a New Jersey university (University A). During this time, options for control of serogroup B meningococcal disease outbreaks were limited by the absence of a licensed serogroup B (MenB) vaccine in the US. However, in 2013 two recombinant MenB vaccines were under pre-licensure review in the US: the three-dose vaccine rLP2086 (Trumenba®, Pfizer) and the two-dose vaccine 4CMenB (Bexsero®, Novartis Vaccines and Diagnostics, Siena, Italy). Because 4CMenB had already been licensed in Europe and Australia in 2013 whereas rLP2086 was not yet licensed in any country, we thought 4CMenB would be more acceptable in the target population. The Centers for Disease Control and Prevention (CDC) therefore submitted an expanded access Investigational New Drug (IND) application to the Food and Drug Administration (FDA) to allow use of 4CMenB to control the outbreak at University A. The CDC, New Jersey Department of Health (NJDOH), Princeton Health Department, and University A collaborated to provide the two-dose vaccination series to the population at risk in the outbreak beginning in December 2013.
Here, we describe the epidemiologic investigation of the outbreak that led to the decision to vaccinate and the implementation of the vaccination campaign with investigational 4CMenB vaccine.
Patients and Methods
Case investigation
Meningococcal disease is nationally notifiable and suspected cases are reported directly to state or local public health authorities. The current Advisory Committee on Immunization Practices guidelines define an organization-based meningococcal disease outbreak as the occurrence of 3 or more cases in 3 months in persons with a common organizational affiliation but without direct close contact and a resulting attack rate of greater than 10 per 100,000 [1]. An outbreak case was defined as a case of serogroup B meningococcal disease with laboratory results consistent with the outbreak strain that occurred in a University A student or close contact of University A students. Cases were reported in New Jersey, Texas, Massachusetts, and Pennsylvania in the US as well as in Greece and were investigated by university and local and state health department staff to identify close contacts for antibiotic chemoprophylaxis. The case-patient who became ill in Greece had been traveling with a group of University A students in Europe for three weeks prior to illness onset; no air travel contacts of this patient required chemoprophylaxis. NJDOH compiled data on all outbreak cases, including those initially reported elsewhere.
Molecular characterization
For eight cases, N. meningitidis serogroup was determined by slide agglutination at the state public health laboratory and confirmed by real-time polymerase chain reaction (rt-PCR) at CDC [2–4]. Serogroup determination and PorA typing for one case was performed in Greece using PCR.
At CDC, isolates were characterized using pulsed-field gel electrophoresis (PFGE), multilocus sequence typing (MLST), and molecular typing of fHbp, NhbA, NadA, and PorA as previously described [5–8]. Novartis assessed whether 4CMenB vaccine was expected to protect against the outbreak strain using human serum bactericidal assay (hSBA) and meningococcal antigen typing system (MATS) [9,10].
Epidemiologic investigation
Following the 6th outbreak case in October 2013, NJDOH invited CDC to assist with an on-site investigation to determine the target population for potential vaccination. To understand whether cases shared epidemiologic links, case information gathered by NJDOH, the Princeton Health Department, and University A was compiled and reviewed. The population at risk [1] was characterized through interviews with University A staff and students and review of university data on student ages, living arrangements, and social interactions.
Vaccination clinic
In November 2013, use of 4CMenB vaccine was authorized per FDA under the expanded access IND regulations (21 CFR 312.320). The primary goal of the expanded access IND was to make vaccine available to the population at risk for serogroup B meningococcal disease during the outbreak given the lack of an adequate, approved alternative for prevention of this potentially life-threatening condition in the US. The primary purpose of an expanded access IND is to provide access to a vaccine or treatment; it is not intended to establish safety and efficacy of the product.
CDC’s Institutional Review Board (IRB) served as the IRB for this IND protocol; the university’s IRB deferred to CDC. Written informed consent was obtained from all vaccine recipients and parental consent and written assent were obtained for recipients under age 18 years.
University A and CDC collaborated to provide students, parents, faculty, and staff with accurate and timely information about the 4CMenB vaccination program; implement the vaccination campaign; and monitor adverse events following vaccination. Potential vaccine recipients were notified of the clinic through multiple mechanisms, including email, posters, and text messages. At the clinic, precautions and contraindications for vaccination were assessed through a screening questionnaire for each recipient; those with questions about the vaccine or medical conditions received further evaluation from a clinical team composed of medical doctors from CDC and University A. Vaccination coverage was monitored through real-time entry of vaccination into recipients’ electronic health records or, for non-students, by collecting copies of the informed consent paperwork. Reports of adverse events following vaccination are being collected passively via phone and student health clinic visits and actively via surveys administered at the time of second dose administration and 30 days after receipt of the second dose.
Results
Case ascertainment
Between March and November 2013, seven cases occurred in University A undergraduates and one additional case occurred in a high school student who became ill after staying in an undergraduate dormitory at University A. Excluding the one case that occurred during the university’s summer break, case-patients lived or stayed in 6 out of the 50 undergraduate dormitories at University A immediately prior to disease onset. No cases occurred in graduate students, faculty, staff, local community members, or family members of case-patients. The median time between cases was 26 days (range 12–94).
All 8 of these case-patients experienced headache and fever and 7 of the 8 developed a rash. Seven case-patients had meningitis while one had bloodstream infection only. All case-patients were hospitalized; the median length of stay was 7 days (range 5–10 days). None of these 8 cases was fatal, but three case-patients had long-term sequelae (unilateral hearing loss (n=1), neurocognitive deficits (n=1), and chronic headaches (n=1)).
The 9th case occurred in March 2014, after the 4CMenB vaccination campaigns and 109 days after the 8th case. This case occurred in a student at a different university who had close contact with University A undergraduates at an off-campus social event 8 days prior to disease onset. The 9th case-patient exhibited a petechial rash but did not have evidence of meningitis. The ninth case was fatal, bringing the overall outbreak case-fatality ratio to 11%.
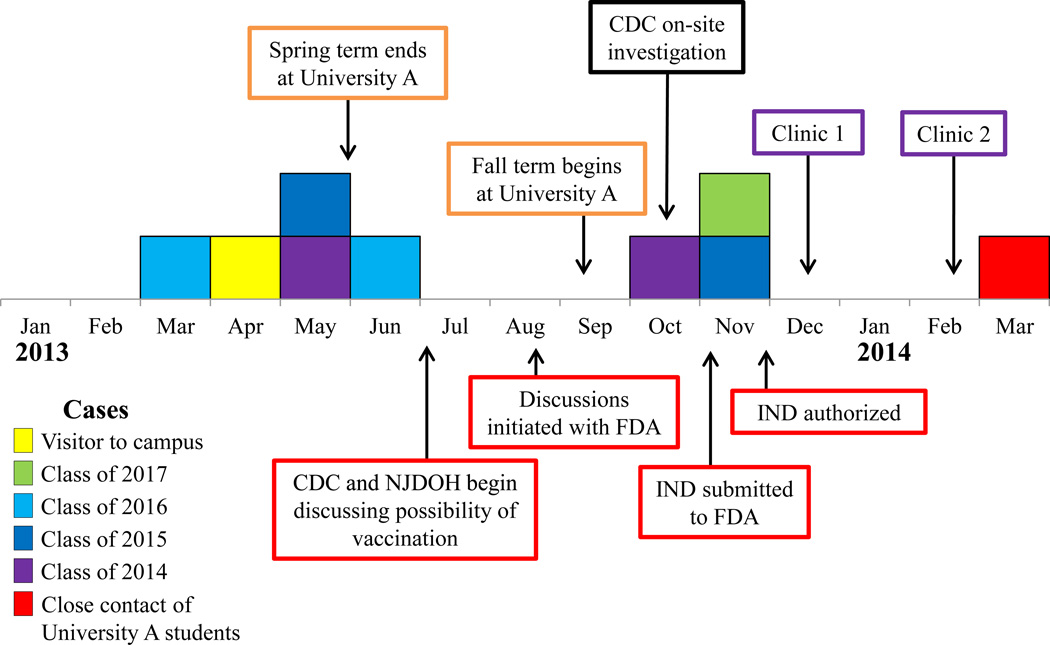
Outbreak case-patient ages ranged from 17 to 21 years (median 19); cases occurred in both males (56%) and females and across four undergraduate classes (Figure 1). No case-patients had a prior diagnosis of a medical condition that increases risk of meningococcal disease (i.e., functional or anatomic asplenia or persistent complement component deficiency) [1]. The annualized attack rate of serogroup B meningococcal disease among University A undergraduates was 134 per 100,000.
Figure 1.
Timeline of outbreak cases and response activities.
Immediately upon identification of each case, close contacts of case-patients were identified by University A, NJDOH, the Princeton Health Department, and other state and local health departments and were recommended antibiotic chemoprophylaxis. Close contacts include household contacts (including roommates), child care center contacts, and anyone else with a direct exposure to a case-patient’s oral secretions [1]. No secondary cases occurred in close contacts of case-patients. In addition to chemoprophylaxis for close contacts, in May 2013 the university issued recommendations for students to reduce sharing of eating and drinking materials and other activities that could result in contact with oral secretions.
Molecular characterization
All cases were confirmed as serogroup B meningococcal disease and had the same PorA type (P1.5-1,2-2). Isolates from the eight cases identified in the US were characterized further; all were sequence type 409 (ST-409) of clonal complex 41/44/Lineage 3 and had the same PFGE pattern (429) and antigen types (fHbp 1.276, NhbA p0002, and NadA negative by Novartis nomenclature). The fHbp and NhbA antigens in the outbreak strain demonstrated cross-reactivity with 4CMenB vaccine antigens by MATS; hSBA testing showed that serum from people vaccinated with 4CMenB was able to kill the outbreak strain.
Epidemiologic investigation
The outbreak spanned two academic years. Only one person was identified as a close contact of more than one case (cases 4 and 7); however, these cases occurred nearly 6 months apart and the contact in question received chemoprophylaxis immediately following the identification of each case. No case-patients were found to share common extracurricular activities and no cases occurred in the same dormitory within an academic year.
In the 2013–2014 academic year, 5,241 undergraduate and 2,666 graduate students were enrolled at University A. More than 98% of undergraduates and 20% of graduate students lived in on-campus dormitories. For undergraduates, the mean age was 21 years (range 16–31) and vaccination coverage with quadrivalent meningococcal conjugate vaccine (MenACWY) was >99.9%. Graduate students living in the graduate student dormitory were significantly younger than graduate students living in university-owned apartments, with mean ages of 24.1 and 26.4 years, respectively (t-test, t=13, p<0.0001). Social mixing between undergraduate and graduate students was reported to be uncommon but extant; however, the degree of social mixing could not be quantified.
Based on this investigation, the target population for vaccination included: University A undergraduate students (n = 5,241), graduate students living in undergraduate and graduate student dormitories (n = 541), graduate students, faculty, and staff with a medical condition that increases risk of meningococcal disease (n = 11), and spouses and care-givers of undergraduate and graduate students living in a dormitory with the students (n = 6).
Vaccination Campaign
The first-dose vaccination clinic was held December 9–12, 2013 and the second-dose clinic was held February 17–20, 2014. Additional small clinics were held for persons unable to attend the larger clinics. Through May 14, 2014, 94.9% of the target population had received at least 1 dose of the vaccine and 89.1% had received both doses (Table 1). Within this target population, coverage was highest among undergraduate students, of whom 96.6% received the first dose and 91.4% received both doses (Table 1). As of February 1, 2015, one serious adverse event was deemed possibly related to the vaccine (a case of rhabdomyolysis with onset 1 day after the second dose), but no concerning patterns of adverse events following vaccination have been observed. Monitoring for adverse events is ongoing.
Table 1.
4CMenB vaccine Vaccination Coverage in Targeted Populations at University A, December 9, 2013–May 14, 2014
| Constituency | # in Target Population |
# First Doses Given |
Coverage with First Dose (%) |
# Second Doses Given |
Coverage with Two-Dose Series (%) |
|---|---|---|---|---|---|
| Undergraduate students | 5241 | 5062 | 96.6 | 4791 | 91.4 |
| Class of 2017 | 1292 | 1260 | 97.5 | 1214 | 94.0 |
| Class of 2016 | 1349 | 1296 | 96.1 | 1232 | 91.3 |
| Class of 2015 | 1320 | 1274 | 96.5 | 1178 | 89.2 |
| Class of 2014 | 1280 | 1232 | 96.3 | 1167 | 91.2 |
| Graduate students | 541 | 424 | 78.4 | 361 | 66.7 |
| Other1 | 17 | 16 | 94.1 | 13 | 76.5 |
| Total | 5799 | 5502 | 94.9 | 5165 | 89.1 |
Category includes faculty, staff, and graduate students with medical conditions that increase risk of meningococcal disease, and spouses and care-givers of graduate and undergraduate students living in a dormitory with the students.
Through February 1, 2015, no cases of serogroup B meningococcal disease have been reported in individuals who received the 4CMenB vaccine. However, as noted above, the 9th case did occur after the vaccination campaigns. The 9th case-patient was a student at another university who had close contact with several University A students, most of whom had received 2 doses of 4CMenB, prior to disease onset. The student body of the second university was not considered to be at increased risk for meningococcal disease due to this incident.
Discussion
In this report, we describe the first time an expanded access IND program for an investigational vaccine has been implemented in response to a serogroup B meningococcal disease outbreak in the US. The attack rate among undergraduate students at University A, 134 per 100,000, was more than 1,400 times greater than the national incidence in this age group [1, CDC unpublished data]. Prior to routine MenACWY vaccination, most meningococcal disease outbreaks on college campuses were caused by serogroup C [11,12]. However, serogroup C outbreaks have declined with high MenACWY coverage in adolescents [13], leaving serogroup B as the cause of recent meningococcal outbreaks on college campuses.
The sequence type of the bacterial strain isolated in this outbreak, ST-409, is uncommon in the US. Aside from the samples received from this outbreak, CDC has received only 9 (0.25%) serogroup B ST-409 isolates out of 3,595 unique case isolates that have been characterized by MLST (isolates collected 1911–2014). None of these other ST-409 isolates had the same antigen profile as the University A outbreak strain. To our knowledge, no other outbreaks associated with ST-409 have been reported in the US or elsewhere. Little is known about the clinical presentation of meningococcal disease caused by ST-409, but in this outbreak the case-fatality ratio and proportion of case-patients with meningitis were consistent with those from meningococcal disease surveillance data for the US [14].
It is not clear why this strain caused an outbreak at University A. This strain might be more invasive than other N. meningitidis sequence types and indeed it is part of the ST-41/44 clonal complex, which is thought to be hypervirulent [15]. Alternatively, the undergraduate population may have had low baseline immunity to this novel bacterial strain, leading to a high attack rate once it was introduced into the student population.
Defining the population at risk in meningococcal disease outbreaks can be challenging. In this outbreak, cases occurred in students of four undergraduate class years, and therefore the entire undergraduate population was targeted for vaccination. While no cases occurred in graduate students, graduate students living in on-campus dormitories were targeted for vaccination because the increased risk of meningococcal disease for college freshmen living in dormitories [16–19] raised concerns that dormitory living might also increase risk for other populations. Furthermore, most outbreak-associated cases of meningococcal disease in the US occur in persons aged <25 years and the mean age of the graduate students living in dormitories was <25 years [11, CDC unpublished data]. While the population at risk must be determined separately for each outbreak of meningococcal disease, we hope the process used to define the population at risk at University A can inform this determination in future outbreaks.
Over 5,000 students received 4CMenB vaccine during the 4-day first-dose vaccination campaign. Several factors likely contributed to the campaign’s success. First, the university provided information about meningitis and the vaccination clinics to students and parents through multiple mechanisms, including emails, posters, text messages, a student-created video, and town hall meetings featuring University A and CDC staff. In addition, efficient clinic management and short wait times for participants resulted in high throughput. Finally, the high attack rate of meningococcal disease and the occurrence of cases shortly before the vaccination campaign likely motivated students to receive the vaccine. This highly successful vaccination campaign provides a model for future vaccination campaigns in response to outbreaks on college campuses.
As of February 1, 2015, no additional serogroup B meningococcal disease cases occurred at University A. While two doses of the vaccine are critical for a sustained immune response [20], one study demonstrated that adolescents also have a strong initial immune response after a single dose [21]. This fact might have contributed to the absence of cases between the first and second vaccination campaigns. However, a case did occur in a close contact of University A students in March 2014. Most of the students with whom the last case-patient had contact had received two doses of 4CMenB vaccine. The occurrence of this case demonstrates that the vaccination campaign had not eliminated carriage from the University A population by this time and that transmission of the outbreak strain was ongoing. This finding is consistent with a recent study demonstrating that 4CMenB has at most a modest impact on prevalence of meningococcal carriage in vaccinated people [22]. Ultimately, it is unknown whether additional cases would have occurred in University A students in the absence of the vaccination campaign, but the lack of cases in vaccinated persons combined with the evidence of ongoing transmission in the population suggests the campaign did succeed in providing primary protection to the student population.
The first vaccine for serogroup B meningococcal disease, rLP2086 (Trumenba®, Pfizer) was licensed for use in individuals 10–25 years old on October 29, 2014, and 4CMenB was approved for use in the same age group on January 23, 2015. Although the Advisory Committee on Immunization Practices has not yet developed recommendations for the use of either vaccine, CDC formed a meningitis outbreak working group to provide interim guidance for responding to outbreaks of serogroup B meningococcal disease. These guidelines are available online at http://www.cdc.gov/meningococcal/outbreaks/vaccine-serogroupb.html. While the number of sporadic cases of serogroup B meningococcal disease occurring in adolescents each year is at historic lows, the potential impact of MenB vaccines on both sporadic disease and outbreaks will be important to consider in the development of recommendations for use of licensed MenB vaccines in the US.
Conclusions
No serogroup B meningococcal disease cases occurred in students who had received 1 or more doses of 4CMenB vaccine, suggesting 4CMenB was effective in protecting vaccinated individuals from disease. However, the 9th case demonstrates that carriage of serogroup B Nesisseria meningitidis among vaccinated persons was not eliminated. The outbreak investigation and highly successful vaccination campaign described here can serve as a model for how to approach similar outbreaks in the future.
What’s Known on This Subject
Outbreaks of serogroup B meningococcal disease occur at universities and other organizations. However, until October 2014 options for control of serogroup B outbreaks were limited by the absence of a licensed vaccine for serogroup B meningococcal disease in the US.
What This Study Adds
This report describes a serogroup B outbreak at a university in 2013 and the campaign with investigational serogroup B vaccine held in response. This was the first use of a serogroup B vaccine as an outbreak response in the US.
Acknowledgements
Dr. Peter Johnsen was invited by Pfizer (manufacturer of rLP2086, Trumenba®) to speak to their vaccine group and at three national conferences. Pfizer paid for Dr. Johnsen's airfare and lodging to attend these events; he did not receive an honorarium or other reimbursements. Dr. Johnsen was also invited by The National Meningitis Association to participate in a round table at another conference. The National Meningitis Association paid for Dr. Johnsen's lodging but did not provide any honorarium or other reimbursements.
We thank Evangeline Reynolds and Wendy Chung of Dallas County Health and Human Services, Dallas; Tamara Baldwin and Grace Kubin, Texas Department of State Health Services, Austin; Johanna Vostok, Massachusetts Department of Public Health, Boston; Ami Patel, Office of Public Health Preparedness and Response, Centers for Disease Control and Prevention, Atlanta and Philadelphia Department of Public Health; Lauren Finn, Philadelphia Department of Public Health; Lisa Dettinger and Christina Russell, Pennsylvania Department of Health, Exton; Maria Orsini and Howard Sarubin, New Jersey Department of Health, Trenton; and the staff of the Princeton Health Department, Princeton, the Mercer County Division of Public Health, Trenton, Papageorgiou General Hospital, Thessaloniki, the American Hospital of Paris, Neuilly-sur-Seine, Drexel University, and the Presbyterian University Hospital for assistance with case investigations, contact tracing, and meningococcal testing. We are grateful to the staff of Novartis Vaccines and Diagnostics, Siena, Italy for coordinating MATS and hSBA testing of patient isolates and vaccine procurement as well as for providing information about the 4CMenB vaccine. We thank Chad Myers and the New Jersey staff of Maxim Healthcare Services, Columbia, MD; Sarah Meyer and Tejpratap Tiwari, Division of Bacterial Diseases, National Center for Immunization and Respiratory Diseases, Centers for Disease Control and Prevention, Atlanta; Natalie Kratz, CDC/CSTE Applied Epidemiology Fellow assigned to the New Jersey Department of Health, Trenton; and the staff and students of University A for their work implementing and supporting the vaccination campaigns.
This study/report was supported in part by an appointment to the Applied Epidemiology Fellowship Program administered by the Council of State and Territorial Epidemiologists (CSTE) and funded by the Centers for Disease Control and Prevention (CDC) Cooperative Agreement Number 5U38HM000414-5.
Abbreviations
- CDC
US Centers for Disease Control and Prevention
- hSBA
human serum bactericidal assay
- FDA
US Food and Drug Administration
- IND
Investigational New Drug
- IRB
Institutional Review Board
- MATS
Meningococcal Antigen Typing System
- MenACWY
quadrivalent meningococcal conjugate vaccine
- MenB
serogroup B meningococcal
- NJDOH
New Jersey Department of Health
- ST-409
Sequence type 409
Footnotes
Financial Disclosure: The authors have no financial relationships relevant to this article to disclose.
Potential Conflict of Interest:The other authors have no potential conflicts to disclose.
Contributor’s Statements:
Lucy McNamara: participated in collection and analysis of epidemiologic data on the cases and population at risk, contributed to the conception and design of the epidemiologic investigation and analysis, contributed to the conception and design of the vaccination campaign and vaccination coverage and safety data collection, contributed to collection and analysis of vaccination coverage and safety data, drafted the initial manuscript, and approved the final manuscript as submitted.
Alice Shumate: participated in collection and analysis of epidemiologic data on the cases and population at risk, contributed to the conception and design of the epidemiologic investigation and analysis, contributed to the conception and design of the vaccination campaign and vaccination coverage and safety data collection, contributed to collection of vaccination coverage and safety data, critically reviewed the manuscript, and approved the final manuscript as submitted.
Peter Johnsen: participated in collection of epidemiologic data on the cases and population at risk, contributed to the conception and design of the vaccination campaign and vaccination coverage and safety data collection, contributed to collection of vaccination coverage and safety data, critically reviewed the manuscript, and approved the final manuscript as submitted.
Jessica MacNeil: participated in collection and analysis of epidemiologic data on the cases and population at risk, contributed to the conception and design of the epidemiologic investigation and analysis, contributed to the conception and design of the vaccination campaign and vaccination coverage and safety data collection, critically reviewed the manuscript, and approved the final manuscript as submitted.
Manisha Patel: contributed to the conception and design of the vaccination campaign and vaccination coverage and safety data collection, contributed to collection and analysis of vaccination coverage and safety data, critically reviewed the manuscript, and approved the final manuscript as submitted.
Tina Bhavsar: contributed to the conception and design of the vaccination campaign and vaccination coverage and safety data collection, critically reviewed the manuscript, and approved the final manuscript as submitted.
Amanda Cohn: contributed to the conception and design of the epidemiologic investigation and analysis, critically reviewed the manuscript, and approved the final manuscript as submitted.
Jill Dinitz-Sklar: participated in collection of epidemiologic data on the cases and population at risk, critically reviewed the manuscript, and approved the final manuscript as submitted.
Jonathan Duffy: contributed to the conception and design of the vaccination campaign and vaccination coverage and safety data collection, contributed to collection and analysis of vaccination safety data, critically reviewed the manuscript, and approved the final manuscript as submitted.
Janet Finnie: contributed to the conception and design of the vaccination campaign and vaccination coverage and safety data collection, critically reviewed the manuscript, and approved the final manuscript as submitted.
Denise Garon: participated in collection of epidemiologic data on the cases and population at risk, critically reviewed the manuscript, and approved the final manuscript as submitted.
Robert Hary: participated in collection of epidemiologic data on the cases and population at risk, critically reviewed the manuscript, and approved the final manuscript as submitted.
Fang Hu: collected and analyzed laboratory data, critically reviewed the manuscript, and approved the final manuscript as submitted.
Hajime Kamiya: participated in collection and analysis of epidemiologic data on the cases and population at risk, contributed to collection of vaccination safety data, critically reviewed the manuscript, and approved the final manuscript as submitted.
Hye-Joo Kim: contributed to the conception and design of the vaccination campaign and vaccination coverage and safety data collection, critically reviewed the manuscript, and approved the final manuscript as submitted.
John Kolligian: contributed to the conception and design of the vaccination campaign and vaccination coverage and safety data collection, critically reviewed the manuscript, and approved the final manuscript as submitted.
Janet Neglia: participated in collection of epidemiologic data on the cases and population at risk, critically reviewed the manuscript, and approved the final manuscript as submitted.
Judith Oakley: contributed to collection and analysis of vaccination coverage data, critically reviewed the manuscript, and approved the final manuscript as submitted.
Jacqueline Wagner: contributed to the conception and design of the vaccination campaign and vaccination coverage and safety data collection, contributed to collection of vaccination coverage data, critically reviewed the manuscript, and approved the final manuscript as submitted.
Kathy Wagner: contributed to the conception and design of the vaccination campaign and vaccination coverage and safety data collection, contributed to collection of vaccination coverage data, critically reviewed the manuscript, and approved the final manuscript as submitted.
Xin Wang: collected and analyzed laboratory data, critically reviewed the manuscript, and approved the final manuscript as submitted.
Yon Yu: contributed to the conception and design of the vaccination campaign and vaccination coverage and safety data collection, critically reviewed the manuscript, and approved the final manuscript as submitted.
Barbara Montana: contributed to the conception and design of the epidemiologic investigation and analysis, critically reviewed the manuscript, and approved the final manuscript as submitted.
Christina Tan: contributed to the conception and design of the epidemiologic investigation and analysis, critically reviewed the manuscript, and approved the final manuscript as submitted.
Robin Izzo: contributed to the conception and design of the epidemiologic investigation and analysis, critically reviewed the manuscript, and approved the final manuscript as submitted.
Thomas Clark: contributed to the conception and design of the epidemiologic investigation and analysis, critically reviewed the manuscript, and approved the final manuscript as submitted.
All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
References
- 1.CDC. Prevention and Control of Meningococcal Disease: Recommendations of the Advisory Committee on Immunization Practices (ACIP) Morbid Mortal Wkly Rep. 2013;62(RR-2):1–28. [PubMed] [Google Scholar]
- 2.Dolan Thomas J, Hatcher CP, Satterfield DA, et al. sodC-Based Real-Time PCR for Detection of Neisseria meningitidis. PLoS one. 2011;6(5):e19361. doi: 10.1371/journal.pone.0019361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mothershed EA, Sacchi CT, Whitney AM, et al. Use of Real-Time PCR To Resolve Slide Agglutination Discrepancies in Serogroup Identification of Neisseria meningitidis. J Clin Microbiol. 2004;42(1):320–328. doi: 10.1128/JCM.42.1.320-328.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wang X, Theodore MJ, Mair R, et al. Clinical Validation of Multiplex Real-Time PCR Assays for Detection of Bacterial Meningitis Pathogens. J Clin Microbiol. 2012;50(3):702–708. doi: 10.1128/JCM.06087-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Maiden MCJ, Bygraves JA, Feil E, et al. Multilocus sequence typing: A portable approach to the identification of clones within populations of pathogenic microorganisms. Proc Natl Acad Sci. 1998;95:3140–3145. doi: 10.1073/pnas.95.6.3140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Popovic T, Schmink S, Rosenstein NA, et al. Evaluation of Pulsed-Field Gel Electrophoresis in Epidemiological Investigations of Meningococcal Disease Outbreaks Caused by Neisseria meningitidis Serogroup C. J Clin Microbiol. 2001;39(1):75. doi: 10.1128/JCM.39.1.75-85.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sacchi CT, Whitney AM, Popovic T, et al. Diversity and Prevalence of PorA Types in Neisseria meningitidis Serogroup B in the United States, 1992–1998. J Infect Dis. 2000;182:1169–1176. doi: 10.1086/315833. [DOI] [PubMed] [Google Scholar]
- 8.Wang X, Cohn A, Comanducci M, et al. Prevalence and genetic diversity of candidate vaccine antigens among invasive Neisseria meningitidis isolates in the United States. Vaccine. 2011;29:4739–4744. doi: 10.1016/j.vaccine.2011.04.092. [DOI] [PubMed] [Google Scholar]
- 9.Donnelly J, Medini D, Boccadifuoco G, et al. Qualitative and quantitative assessment of meningococcal antigens to evaluate the potential strain coverage of protein-based vaccines. Proc Natl Acad Sci. 2010;107(45):19490–19495. doi: 10.1073/pnas.1013758107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Giuliani MM, Biolchi A, Serruto D, et al. Measuring antigen-specific bactericidal responses to a multicomponent vaccine against serogroup B meningococcus. Vaccine. 2010;28(31):5023–5030. doi: 10.1016/j.vaccine.2010.05.014. [DOI] [PubMed] [Google Scholar]
- 11.Jackson LA, Schuchat A, Reeves MW, Wenger JD. Serogroup C Meningococcal Outbreaks in the United States. JAMA. 1995;273(5):383–389. [PubMed] [Google Scholar]
- 12.CDC. Meningococcal Disease and College Students: Recommendations of the Advisory Committee on Immunization Practices (ACIP) Morbid Mortal Wkly Rep. 2000;49(RR07):11–20. [PubMed] [Google Scholar]
- 13.Curtis CR, Yankey D, Jeyarajah J, et al. National and State Vaccination Coverage Among Adolescents Aged 13–17 years — United States, 2012. Morbid Mortal Wkly Rep. 2013;62(34):685–693. [PMC free article] [PubMed] [Google Scholar]
- 14.Cohn AC, MacNeil RJ, Harrison LH, et al. Changes in Neisseria meningitidisDisease Epidemiology in the United States, 1998–2007: Implications for Prevention of Meningococcal Disease. Clin Infect Dis. 2010;50:184–191. doi: 10.1086/649209. [DOI] [PubMed] [Google Scholar]
- 15.Climent Y, Yero D, Martinez I, et al. Clonal Distribution of Disease-Associated and Healthy Carrier Isolates of Neisseria meningitidis between 1983 and 2005 in Cuba. J Clin Microbiol. 2010;48(3):802–810. doi: 10.1128/JCM.01653-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bruce MG, Rosenstein NE, Capparella JM, Shutt KA, Perkins BA, Collins M. Risk Factors for Meningococcal Disease in College Students. JAMA. 2001;286(6):688–693. doi: 10.1001/jama.286.6.688. [DOI] [PubMed] [Google Scholar]
- 17.Froeschle JE. Meningococcal Disease in College Students. Clin Infect Dis. 1999;29(1):215–216. doi: 10.1086/520166. [DOI] [PubMed] [Google Scholar]
- 18.Harrison LH, Dwyer DM, Maples CT, Billmann L. Risk of Meningococcal Infection in College Students. JAMA. 1999;281(20):1906–1910. doi: 10.1001/jama.281.20.1906. [DOI] [PubMed] [Google Scholar]
- 19.Neal KR, Nguyen-Van-Tam J, Monk P, O’Brien SJ, Stuart J, Ramsay M. Invasive meningococcal disease among university undergraduates: association with universities providing relatively large amounts of catered hall accommodation. Epidemiol Infect. 1999;122:351–357. doi: 10.1017/s0950268899002368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Santolaya ME, O’Ryan ML, Valenzuela MT, et al. Persistence of antibodies in adolescents 18–24 months after immunization with one, two, or three doses of 4CMenB meningococcal serogroup B vaccine. Hum Vaccin Immunother. 2013;9(11):2304–2310. doi: 10.4161/hv.25505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Santolaya ME, O’Ryan ML, Valenzuela MT, et al. Immunogenicity and tolerability of a multicomponent meningococcal serogroup B (4CMenB) vaccine in healthy adolescents in Chile: a phase 2b/3 randomised, observer-blind, placebo-controlled study. Lancet. 2012;379:617–624. doi: 10.1016/S0140-6736(11)61713-3. [DOI] [PubMed] [Google Scholar]
- 22.Read RC, Baxter D, Chadwick DR, et al. Effect of a quadrivalent meningococcal ACWY glycoconjugate or a serogroup B meningococcal vaccine on meningococcal carriage: an observer-blind, phase 3 randomised clinical trial. Lancet. 2014 doi: 10.1016/S0140-6736(14)60842-4. published online ahead of print: [DOI] [PubMed] [Google Scholar]