Abstract
Background
Reduced muscle strength is an independent risk factor for falls and related to postural instability in individuals with Parkinson’s disease. The ability of resistance training to improve postural control still remains unclear.
Objective
To compare resistance training with balance training to improve postural control in people with Parkinson’s disease.
Methods
40 patients with idiopathic Parkinson’s disease (Hoehn&Yahr: 2.5–3.0) were randomly assigned into resistance or balance training (2x/week for 7 weeks). Assessments were performed at baseline, 8- and 12-weeks follow-up: primary outcome: Fullerton Advanced Balance (FAB) scale; secondary outcomes: center of mass analysis during surface perturbations, Timed-up-and-go-test, Unified Parkinson’s Disease Rating Scale, Clinical Global Impression, gait analysis, maximal isometric leg strength, PDQ-39, Beck Depression Inventory. Clinical tests were videotaped and analysed by a second rater, blind to group allocation and assessment time.
Results
32 participants (resistance training: n = 17, balance training: n = 15; 8 drop-outs) were analyzed at 8-weeks follow-up. No significant difference was found in the FAB scale when comparing the effects of the two training types (p = 0.14; effect size (Cohen’s d) = -0.59). Participants from the resistance training group, but not from the balance training group significantly improved on the FAB scale (resistance training: +2.4 points, Cohen’s d = -0.46; balance training: +0.3 points, Cohen’s d = -0.08). Within the resistance training group, improvements of the FAB scale were significantly correlated with improvements of rate of force development and stride time variability. No significant differences were found in the secondary outcome measures when comparing the training effects of both training types.
Conclusions
The difference between resistance and balance training to improve postural control in people with Parkinson’s disease was small and not significant with this sample size. There was weak evidence that freely coordinated resistance training might be more effective than balance training. Our results indicate a relationship between the enhancement of rate of force development and the improvement of postural control.
Trial Registration
ClinicalTrials.gov ID: NCT02253563
Introduction
Postural Instability is one of the major motor symptoms of individuals with Parkinson’s disease (PD) and is generally not improved by medication or Deep Brain Stimulation [1–3]. Postural disturbances are one of the independent risk factors for falling [4–6] and fall rates range from 39 to 68% in patients suffering from PD [7,8]. Moderate evidence exists that exercise can improve postural control [9–11]. A study conducted by Canning et al. [12] showed that a combined training targeting balance, strengths and freezing of gait was effective to enhance postural control. Studies have shown that balance training (BT) alone can be effective to improve postural control in people with PD [13,14].
Resistance training (RT) is an effective treatment to improve motor symptoms [15] and strength in PD [16–19]. Reduced muscle strength coincides with an increased risk for falls in PD [4] and is associated with postural impairments [20,21]. Compensatory mechanisms play an important role in PD and the improvement of strength due to resistance training might facilitate the activation of balance related muscle-groups. Accordingly RT might lead to enhanced postural control. Two recently published meta-analysis showed no significant improvement of postural control due to RT in PD [16,17]. The authors report to interpret this result with caution as only 3 studies were analyzed having the assessment of postural control as secondary outcome [22–24]. Furthermore, none of these studies used clinical balance scales to reflect the various dimensions of postural control and the control groups did not received any intervention. Only one study had blinded rating but this study analyzed a combination of training of resistance and balance training [22]. Due to these various limitations, the effect of isolated RT on postural control still remains unclear. Interestingly, a recently published study with healthy elderly showed that RT might be efficacious, as the authors showed better improvement in postural control due to RT in comparison to classical BT [25].
In order to create the most effective exercises, studies often use multidimensional training programs [23,26,27]. These physical therapy techniques are difficult to compare and more specific trials are needed to give further information about which exercise program might be more effective and about the underlying processes leading to the results [9,28].
The aim of the present study was to compare the efficacy of RT with BT to improve postural control in people with PD. BT was chosen because classical BT is widely used in physical therapy to treat individuals with postural instability and further we wanted to pit two typical exercise interventions against each other. In addition, we intended to relate the effects on postural control with changes of several disease associated conditions in order to gain insight which mechanisms play an important role for the improvement of postural control.
Methods
We designed a randomized rater blinded controlled trial to compare the effects of RT with the effects of BT for people with idiopathic PD. The study was registered online at ClinicalTrials.gov (ID: NCT02253563). Registration of the trial was delayed after the enrollment of the first patient due to an administrative error. The authors confirm that all ongoing and related trials for this intervention are registered.
Participants
People were included if they met the following inclusion criteria: (1) diagnosed with idiopathic PD as defined by the UK Brain Bank criteria [29] and by a neurologist specializing in movement disorders, (2) postural instability (Fullerton Advanced Balance (FAB) scale ≤ 25 points) [30], (3) able to follow exercise instructions (assessed during a pre-examination during which the FAB scale was performed (see below)). Exclusion criteria were: (1) deep brain stimulation, (2) other diseases that could influence stance- and gait performance, (3) participation in a specific RT or BT program (beside usual physical therapy) during the last 6 months, (4) participation in any other medical, behavioral or exercise treatment (additionally to the usual received therapeutic treatment) during the study period, (5) unstable medication and (6) cardiopulmonary/metabolic diseases that could interfere with the safe conduct of the study protocol. Cognitive impairments (assessed with the Mini-Mental State Examination (MMSE)) were not defined as exclusion criteria so that a representative sample of affected patients could be included.
The study protocol was approved by the local ethics committee (Ethik-Kommission, Universitätsklinikum Schleswig-Holstein, Campus Kiel, Arnold-Heller-Straße 3, 24105 Kiel, Germany, ref. A 146/11) in September 2011 and all participants gave written informed consent prior to participating. All participants had legal capacity to make decisions and patients having a MMSE score<25 gave written informed consent together with their spouse, if applicable. The person of the images in S1 File and S2 File gave written consent to publication.
Screening and Randomization
Participants were screened with a pre-examination prior to inclusion in the study. The FAB scale was performed to determine the level of postural instability. Patients were stratified by gender and level of postural instability and randomized in matched pairs using computer generated random number sequences in a ratio of 1:1. Participants were reassessed for baseline analysis at another day.
Intervention
Participants were randomly assigned into RT or BT (2x/week for 7 weeks). Each session lasted 60 minutes (4–5 participants/group), and consisted of 10 minutes to warm-up followed by 50 minutes RT or BT. Each session was guided by a movement disorders experienced sport scientist who had experience in neurological rehabilitation and with the help of a sport student (student of kinesiology).
Resistance Training
RT was performed with the aim to improve muscle strength of the lower limbs. The trained muscle groups were hip flexors, extensors and abductors, knee flexors and extensors, ankle dorsiflexors and plantarflexors, as these are muscle groups primary involved in postural control mechanisms [20,21]. The participants’ own weight, cuff weights and elasticated bands were used as resistance [31]. Squats, knee extensions, toe/calf raises, hip abductions and other exercises were performed (see S1 File, which shows the performed exercises). In line with training recommendations based on previous studies (e.g. Hass et al. [32]) participants completed three sets of 15–20 repetitions to volitional fatigue of each exercise. With respect to the age of the participants and the stage of disease, exercise intensity was kept on a moderate level in order to avoid injuries. Once participants could complete more than 20 consecutive repetitions of an exercise, they were asked to increase the resistance to a point where they could only complete between 15–20 repetitions in order to keep the training intensity on a consistent level. Resistance was increased by cuff weights, elasticated bands or by the trainer who gave additional resistance. Participants rested for 2 minutes between exercise sets.
Balance Training
BT involved stance- and gait tasks which require feedforward and feedback postural control [13]. Feedforward postural control for example was trained by letting the participants lean forward, backward or sideward, thus letting them control their center of pressure inside the boundaries of their base of support. To practice feedback control one exercise was to perturb the participants by shoulder pulls from the trainer. Training progression during the intervention period was reached by reducing or manipulating sensory information, necessary to obtain balance and by adding movement to make the activity more dynamic. Visual information for example was disturbed by closing the eyes or looking up to the ceiling. Proprioceptive feedback was manipulated by standing on different unstable surfaces instead of normal overground. Each exercise lasted for 45 sec and was performed 3 times, followed by a break of 2 minutes (see S2 File, which shows the performed exercises).
Outcome Measures
Assessments were performed at baseline, 8- and 12-weeks follow-up. Primary outcome measure was the FAB scale [33]. The FAB scale is a 10-item clinical balance scale with a 5-point ordinal scale (0–4) for each item and a maximal score of 40 points (higher values indicate better performance). The FAB scale is validated for individuals with Parkinson’s disease with excellent interrater and test-retest reliability [30]. We chose the FAB scale instead of the often used Berg Balance Scale because in contrast to the Berg Balance Scale the FAB scale has less ceiling effect and includes the assessment of reactive postural control [30]. We decided against the frequently used Mini-BESTest as the FAB scale’s items are more detailed and it takes less time to perform the FAB scale [30].
Secondary outcome measures: Center of mass (COM) displacement was analyzed during surface perturbations. Participants were asked to maintain their balance without doing steps while standing on a movable platform which shifted unexpectedly towards the anterior or posterior direction (20cm with a velocity of 0.1m/s and an acceleration of 10m/s2). Participants were aware neither when the platform would move nor in which direction the surface would change.COM was assessed with an infrared movement analysis system (Qualisys, Gothenburg, Sweden) consisting of six infrared cameras (240 Hz sampling rate). 17 infrared light emitting diodes were placed on anatomic landmarks as described in detail elsewhere [2] and the COM was calculated as the weighted sum of all segments, as adapted from Winter et al. [34]. According to Visser et al. [2] the vector length of three-dimensional COM displacement was calculated. In order to adapt to different biomechanical requirements due to different sizes of participants, the vector length was normalized to COM height. The average normalized vector length over all backward and forward pulls was calculated, respectively. The area under the curve of the normalized vector length from the beginning until 1 sec after the perturbation was defined as an instability outcome measure (see S3 File, which gives further details about the analysis of the surface perturbations) [2].
The following tests were used additionally: Timed-up-and-go-test (TUG) [35], Clinical Global Impression—Improvement (CGI-I) [36], Unified PD Rating Scale (UPDRS) [37], PD Questionnaire (PDQ-39) [38], Beck Depression Inventory (BDI) [39] and Physical Activity Scale for the Elderly (PASE) [40].
Gait velocity of participants was measured during uninterrupted ground level walking, recorded by light barriers placed at the beginning and at the end of a 5m pathway, which the participants had to cross 5 times. Afterwards, participants were asked to walk 2 min. on a treadmill (Woodway, Weil am Rhein, Germany) with their overground gait velocity. The treadmill comprised two separate belts, each with 4 force transducers (Kistler, Winterthur, Switzerland) (960Hz sampling rate). Contact times (heel strike, toe off) were measured by the force transducers to calculate the following spatio-temporal variables: stride length, double support time, stride time variability, bilateral coordination (Phase Coordination Index (PCI)) [41] and gait asymmetry [41] (see S4 File, which describes in detail the gait analysis).
Maximal isometric leg strength was measured on a custom designed leg press equipped with a force platform (Kistler, Winterthur, Switzerland) (1000Hz sampling rate). Maximal voluntary contraction (MVC) and rate of force development (RFD) was assessed. Results were analyzed for both legs separately according to the less- (LAS) and more (MAS) affected PD side—defined by comparing the sums of the UPDRS items 20–26 for the left and right side separately [42,43] (see S5 File, which describes in detail the strength testing).
All clinical tests were carried out by a rater who was blind to the participant’s group allocation. The FAB scale and UPDRS were videotaped and rated by a second rater, blind to participant’s group allocation and assessment time.
Testing Procedure
Assessments were performed on two separate days. Participants were tested in the medication ON-state (1 hour after the last intake of antiparkinsonian medication). Each participant performed the baseline, 8- and 12-weeks follow-up measurements at the exact same time of day.
Statistical Analysis
Sample size calculation was performed for the FAB scale as the main outcome. A sample size of 18 participants per group was found to be required to detect a between-group difference of 2 points at the FAB scale from baseline to 8-weeks follow-up (power = 0.9, alpha = 0.05) (G*Power, version 3.1.9 [44]). This predicted difference equate to a large effect size of 0.6 or greater. With an expected 10% drop-out rate we included 20 participants per group.
Between-group differences in demographic and baseline variables were tested using the Mann-Whitney-U-Test. Within group differences were analysed with the Wilcoxon signed rank test.
To compare the effect of treatment between the two training groups, the difference between 8-weeks follow-up and baseline performance was computed for each participant. Both groups were then compared with the Mann-Whitney-U-Test.
Non-parametric statistical tests were used for the demographic, within and between group analyses as some of the outcome variables are ordinal scaled and not all of the variables were normally distributed.
The Mann-Whitney-U-Test was used to compare CGI-I between the groups.
Interrater reliability between the blinded rater and the blinded video rater were analysed by calculating two-way mixed single measure intraclass correlation coefficients (ICC (3,1)).
Cohen’s d was calculated to evaluate effect sizes.
To analyze the relationship between the magnitude of change in the different outcome variables, Spearman’s rank correlation coefficients (Spearman’s Rho) were calculated. Those variables which significantly correlated with the changes in the FAB scale were included as independent variables in a multiple linear regression analysis. To analyze the risk of multicollinearity variance inflation factors were calculated for each independent variable. A variance inflation factor > 10 indicates high multicollinearity [45].
Data were analyzed on a per-protocol basis. Participants were excluded if they missed more than two training sessions, if medication was changed or if any other injury which could influence stance- and gait performance occurred during the study period.
Statistical tests were performed with SPSS (version 19, IBM), the α level for significance was set at P < 0.05 and all tests were two-sided. Bonferroni correction was used for multiple comparisons for the variables of the gait analysis and strength testing separately.
The study protocol and supporting CONSORT checklist are available as supporting information (S1 Protocol, S2 Protocol, and S1 CONSORT Checklist).
Results
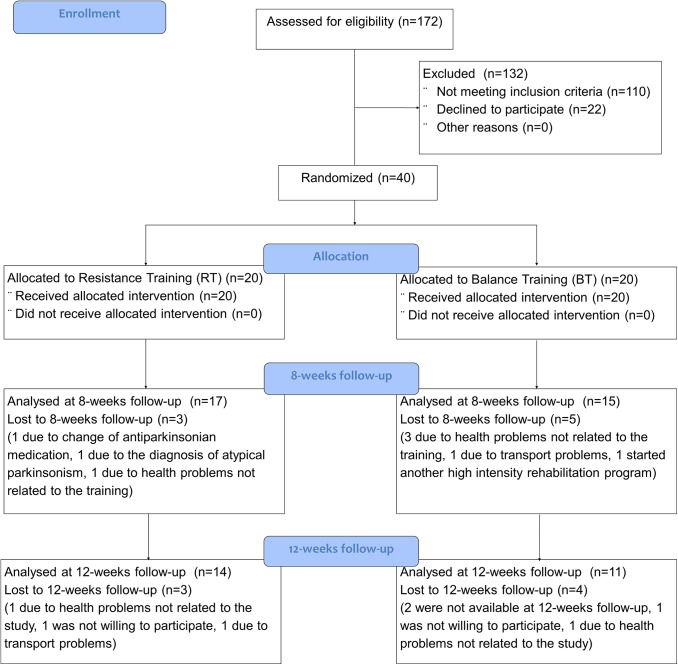
From September 2011 till August 2013 a total of 172 persons were screened for eligibility at the department of Neurology, University Hospital Schleswig-Holstein, Kiel, Germany, among which 40 patients met the inclusion criteria and underwent randomization. Final data collection was February 2014. 8 participants (20%; 3 RT; 5 BT) did not complete the training protocol. For drop-out reasons see Fig 1 which shows the CONSORT flow diagram. All patients were able to follow the instructions during the training sessions.
Fig 1. The CONSORT flow diagram for this study.
Baseline data
No significant differences were found in the demographic or baseline variables between the two groups except for the outcome forward pull (Tables 1 and 2).
Table 1. Participant characteristics.
| Variable | Resistance (n = 17) | Balance (n = 15) | p-value a |
|---|---|---|---|
| Age (yr) | 75.7 ± 5.5 | 75.7 ± 7.2 | 0.882 |
| No. of female subjects | 5 (29.4%) | 6 (40%) | 0.529 b |
| Duration of Disease (yr) | 10.1 ± 6.0 | 9.3 ± 7.9 | 0.455 |
| BMI (kg/m2) | 27.9 ± 5.5 | 25.5 ± 4.4 | 0.142 |
| H&Y | 2.8 ± 0.26 | 2.7 ± 0.4 | 0.216 |
| H&Y (Range) | 2.5–3.0 | 2.5–3.0 | n/a |
| UPDRS total (ON) | 40.2 ± 12.5 | 37.7 ± 13.1 | 0.455 |
| UPDRS part II (ON) | 13.4 ± 5.1 | 11.1 ± 6.0 | 0.105 |
| UPDRS part III (ON) | 23.6 ± 9.5 | 22.3 ± 6.1 | 0.941 |
| FAB scale | 22.2 ± 4.8 | 24.5 ± 4.6 | 0.123 |
| MMSE | 27.3 ± 3.6 | 27.7 ± 3.0 | 0.891 |
| MMSE (Range) | 17–30 | 20–30 | n/a |
| PASE score | 104.6 ± 87.3 | 77.2 ± 63.1 | 0.576 |
| LEDD (mg/day) | 817.4 ± 468.0 | 674.7 ± 294.9 | 0.318 |
If not indicated differently, values are either mean ± SD or number and percentage. BMI, Body-Mass-Index; FAB, Fullerton Advanced Balance; H&Y, Hoehn & Yahr; LEDD, levodopa equivalent daily dose; MMSE, Mini-Mental State Examination; PASE, Physical Activity Scale for the Elderly; UPDRS, Unified Parkinson’s Disease Rating Scale
a unless otherwise indicated P-value of independent samples Mann-Whitney-U-Test
b P-value of Chi-Square Test.
Table 2. Comparison within- and between the two training groups from baseline to 8-weeks follow-up.
| Variable | Baseline | 8-wk follow-up | Mean change (95% CI) from baseline to 8-wk follow-up | p-value a (within group comparison) | p-value b (between group comparison) | Effect size c (within group) | Effect size c (between group) | |
|---|---|---|---|---|---|---|---|---|
| FAB scale d | RT | 22.2 ± 4.8 | 24.5 ± 5.4 | 2.4 (0.1; 4.6) | 0.04* | 0.143 | -0.46 | -0.59 |
| BT | 24.5 ± 4.6 | 24.9 ± 5.3 | 0.3 (-0.8; 1.5) | 0.526 | -0.08 | |||
| Forward pull e | RT | 2270.3 ± 375.1 | 2336.7 ± 274.0 | 66.4 (-138.2; 270.9) | 0.311 | 0.769 | -0.20 | -0.17 |
| BT | 1807.4 ± 351.8 | 1836.6 ± 360.9 | 29.2 (-66.4; 124.9) | 0.239 | -0.08 | |||
| Backward pull e | RT | 1882.3 ± 326.9 | 1782.1 ± 373.4 | -100.2 (-311.5; 111.0) | 0.286 | 0.332 | 0.29 | 0.42 |
| BT | 1844.6 ± 411.4 | 1917.4 ± 362.7 | 72.8 (-261.4; 407.0) | 0.657 | -0.19 | |||
| TUG (sec) | RT | 11.2 ± 3.2 | 9.5 ± 2.4 | -1.7 (-3.3; -0.1) | 0.033* | 0.139 | 0.60 | 0.69 |
| BT | 9.2 ± 3.0 | 9.0 ± 1.8 | -0.2 (-1.3; 0.9) | 0.929 | 0.08 | |||
| UPDRS total score | RT | 40.2 ± 12.5 | 38.5 ± 12.3 | -1.7 (-5.1; 1.8) | 0.347 | 0.272 | 0.14 | -0.38 |
| BT | 37.7 ± 13.1 | 33.6 ± 12.3 | -4.1 (-7.3; -0.9) | 0.033* | 0.32 | |||
| UPDRS motor score f | RT | 22.6 ± 8.8 | 22.2 ± 8.9 | -0.4 (-2.0; 1.2) | 0.568 | 0.911 | 0.04 | -0.51 |
| BT | 20.3 ± 4.9 | 19.4 ± 6.7 | -0.9 (-3.0; 1.1) | 0.821 | 0.49 | |||
| gait velocity (cm/sec) | RT | 104.3 ± 15.3 | 106.1 ± 15.0 | 1.8 (-5.2; 8.7) | 0.619 | 0.692 | -0.12 | -0.14 |
| BT | 106.9 ± 18.3 | 106.8 ± 17.7 | -0.1 (-7.4; 7.4) | 0.776 | 0.01 | |||
| stride length (cm) | RT | 80.6 ± 13.0 | 80.3 ± 11.7 | -0.4 (-4.5; 3.7) | 0.865 | 0.097 | 0.02 | 0.50 |
| BT | 88.8 ± 15.7 | 91.5 ± 16.1 | 2.7 (-0.4; 5.9) | 0.131 | -0.17 | |||
| double support time (msec) | RT | 156.6 ± 31.7 | 156.3 ± 35.5 | -0.3 (-8.4; 7.8) | 0.532 | 0.134 | 0.01 | 0.45 |
| BT | 149.4 ± 24.9 | 155.0 ± 32.1 | 5.6 (-2.1; 13.3) | 0.11 | -0.19 | |||
| stride time variability (%) | RT | 3.8 ± 1.0 | 3.7 ± 1.7 | -0.1 (-0.8; 0.6) | 0.334 | 0.413 | 0.07 | -0.53 |
| BT | 3.9 ± 1.8 | 3.0 ± 0.8 | -0.9 (-2.0; 0.3) | 0.182 | 0.65 | |||
| PCI (%) | RT | 6.6 ± 1.5 | 6.1 ± 1.8 | -0.5 (-1.1; 0.1) | 0.061 | 0.077 | 0.30 | 0.75 |
| BT | 6.1 ± 1.4 | 6.9 ± 2.1 | 0.8 (-0.7; 2.3) | 0.286 | -0.45 | |||
| Asymmetry Index | RT | 5.1 ± 4.1 | 6.0 ± 4.3 | 0.9 (-1.1; 0.1) | 0.82 | 0.959 | -0.21 | -0.22 |
| BT | 4.9 ± 3.7 | 5.0 ± 5.3 | 0.1 (-1.6; 1.8) | 0.99 | -0.02 | |||
| leg strength (MVC), LES (N) | RT | 393.8 ± 113.5 | 416.9 ± 91.0 | 23.0 (-15.5; 61.6) | 0.279 | 0.458 | -0.22 | -0.43 |
| BT | 416.5 ± 129.6 | 408.8 ± 138.5 | -7.7 (-53.3; 37.8) | 0.925 | 0.06 | |||
| leg strength (MVC), MAS (N) | RT | 401.8 ± 130.0 | 399.8 ± 85.7 | -2.0 (-48.2; 44.2) | 0.807 | 0.287 | 0.02 | 0.33 |
| BT | 407.9 ± 134.4 | 426.2 ± 131.6 | 18.3 (-4.4; 41.1) | 0.133 | -0.14 | |||
| peak RFD, LAS (N/msec) | RT | 1.5 ± 0.7 | 1.6 ± 0.8 | 0.1 (-0.4; 0.4) | 0.753 | 0.223 | -0.13 | 0.50 |
| BT | 1.6 ± 1.0 | 1.8 ± 0.9 | 0.3 (0.0; 0.5) | 0.028** | -0.21 | |||
| peak RFD, MAS (N/msec) | RT | 1.5 ± 1.0 | 1.5 ± 0.7 | 0.0 (-0.6; 0.5) | 0.972 | 0.503 | 0.00 | 0.40 |
| BT | 1.4 ± 0.7 | 1.7 ± 0.9 | 0.3 (-0.2; 0.8) | 0.308 | -0.37 | |||
| RFD, LAS (N/msec) | RT | 0.8 ± 0.6 | 0.9 ± 0.6 | 0.1 (-0.2; 0.5) | 0.249 | 0.627 | -0.17 | 0.31 |
| BT | 0.7 ± 0.5 | 1.0 ± 0.6 | 0.3 (0.0; 0.5) | 0.056 | -0.54 | |||
| RFD, MAS (N/msec) | RT | 0.8 ± 0.7 | 0.9 ± 0.6 | 0.1 (-0.3; 0.5) | 0.600 | 0.939 | -0.15 | -0.14 |
| BT | 0.9 ± 0.7 | 0.9 ± 0.7 | 0.0 (-0.4; 0.4) | 0.507 | 0.00 |
FAB, Fullerton Advanced Balance; TUG, Timed-Up-and-Go-Test; LAS, less affected side; MAS, more affected side; MVC, maximal voluntary contraction; PCI, Phase Coordination Index; RFD, rate of force development (0-100ms); UPDRS, Unified Parkinson’s Disease Rating Scale
a p-value of Wilcoxon test
b p-value of independent samples Mann-Whitney-U-Test
c Cohen’s d was calculated as effect size
d blinded video rating
e values represent the area under the curve of the normalized vector length from 0–3 sec after the surface perturbation
f blinded video rating, without item 22 (rigidity)
RT, resistance training (n = 17); BT, balance training (n = 15)
*significant different (p<0.05)
**after Bonferroni-adjustment not significant.
Agreement between the two blinded raters
The agreement between the blinded rater and the blinded video rater was high with ICCs >0.80 for baseline and 8-weeks follow-up. Since the blinded video rater (the person who rated by videos) not only was blind to group allocation but also to assessment time, results are analysed and interpreted with priority to the blinded video rater.
Effect of intervention from baseline to 8-weeks follow-up
The RT-group significantly improved from baseline to week 8 on average by 2.4 points on the FAB scale (p = 0.04; Cohen’s d = -0.46), whereas the score of the BT-group only increased on average by 0.3 points and that was statistically not significant (p = 0.526; Cohen’s d = -0.08) (Table 2). The higher intervention effect of the RT-group did not differ significantly from the training effect of the BT-group (p = 0.143, Cohen’s d = -0.59).
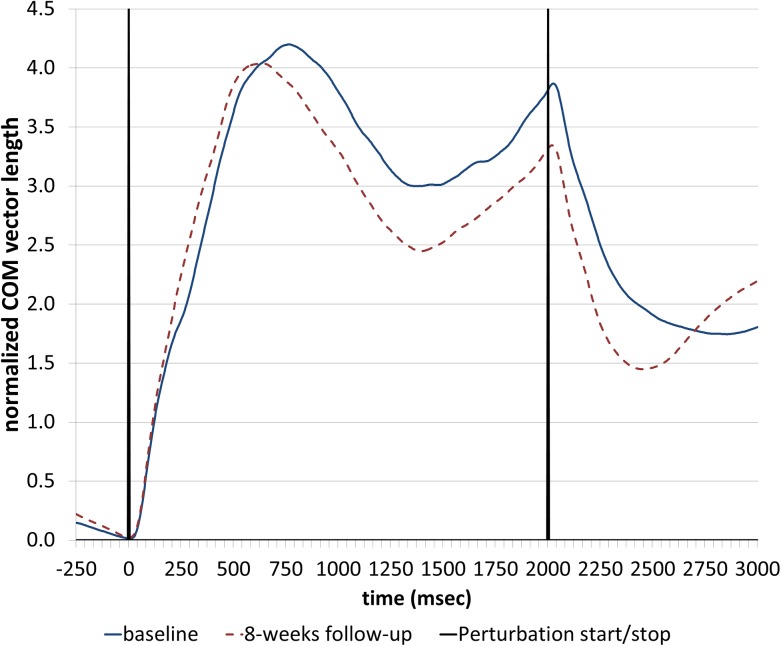
No significant differences were found when analysing the COM displacement during surface perturbations (an example of the average normalized COM vector length during backward perturbations is shown in Fig 2).
Fig 2. Average normalized center of mass (COM) vector length of one participant during backward perturbations at baseline and 8-weeks follow-up.
The RT-group but not the BT-group performed the TUG significantly quicker at 8-weeks follow-up in comparison to baseline (on average -1.7sec, p = 0.033) but the difference between the training types was not significant (p = 0.139).
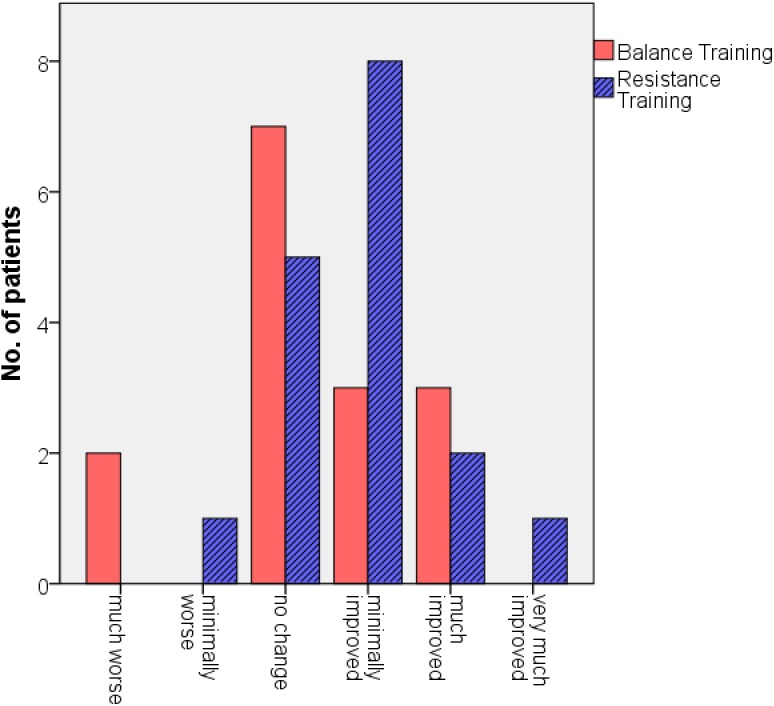
Fig 3 shows the results of the CGI-I. 65% of the participants from the RT-group reported a clinical global improvement whereas only 40% of the participants from the BT-group indicated amelioration. However, the difference between both groups was not significant (p = 0.295).
Fig 3. Results of the Clinical Global Impression–Improvement scale (CGI-I).
In contrast to the RT-group, a significant improvement was found for the BT-group at the UPDRS total score (on average -4.1 points, p = 0.033) without any significant difference between the training types (p = 0.272). No significant differences were found for the UPDRS motor score.
The BT-group slightly improved the peak rate of force development of the less affected side from baseline to week 8, but this improvement was statistically not significant after Bonferroni-correction.
No significant differences were found for the PDQ-39 (baseline: RT: 28.5 ±12.7, BT: 28.5 ±17.7; 8-weeks follow-up: RT: 26.5 ±12.0, BT: 30.2 ±17.8) and the BDI (baseline: RT: 9.9 ±5.6, BT: 14.0 ±9.1; 8-weeks follow-up: RT: 8.4 ±5.3, BT: 10.8 ±5.9) for the between group comparison (baseline and differences from baseline to 8-weeks follow-up) and within group comparison (p<0.05).
Effect of intervention from baseline to 12-weeks follow-up
Table 3 shows the results of the baseline, 8- and 12 weeks follow-up assessments. The differences within one group from baseline to week 12 and the comparison of changes between the two training groups were statistically not significant.
Table 3. Comparison of baseline, 8- and 12-weeks follow-up.
| Variable | Group | Baseline | 8-wk follow-up | 12-wk follow-up | Mean change (baseline to 12-wk follow-up) (95% CI) | p-value a (within group comparison, baseline to 12-wk follow-up) | p-value b (between group comparison, baseline to 12-wk follow-up) |
|---|---|---|---|---|---|---|---|
| FAB scale c | RT | 22.2 ± 5.3 | 24.4 ± 5.7 | 22.5 ± 5.1 | 0.3 (-2.2; 2.8) | 0.370 | 0.767 |
| BT | 24.8 ± 4.2 | 25.3 ± 4.4 | 24.0 ± 4.6 | -0.8 (-2.6; 1.0) | 0.900 | ||
| TUG (sec) | RT | 11.4 ± 3.6 | 9.4 ± 2.5 | 10.0 ± 2.1 | -1.4 (-3.2; 0.4) | 0.686 | 0.699 |
| BT | 9.2 ± 3.8 | 9.0 ± 2.4 | 8.4 ± 1.9 | -0.8 (-3.5; 1.9) | 0.139 | ||
| UPDRS total score | RT | 40.7 ± 15.0 | 40.7 ± 13.1 | 39.4 ± 12.0 | -1.4 (-9.8; 7.1) | 0.183 | 0.797 |
| BT | 38.8 ± 14.7 | 32.8 ± 13.5 | 36.4 ± 15.9 | -2.5 (-9.0; 4.1) | 0.286 | ||
| UPDRS motor score d | RT | 23.7 ± 10.4 | 23.4 ± 10.5 | 22.5 ± 10.2 | -1.2 (-3.3; 0.9) | 0.183 | 0.833 |
| BT | 20.8 ± 4.1 | 19.3 ± 6.6 | 19.6 ± 5.5 | -1.3 (-3.4; 0.9) | 0.052 |
FAB, Fullerton Advanced Balance; TUG, Timed-Up-and-Go-Test; UPDRS, Unified Parkinson’s Disease Rating Scale
a p-value of Wilcoxon test
b p-value of independent samples Mann-Whitney-U-Test
c blinded video rating
d blinded video rating, without item 22 (rigidity)
RT, resistance training (n = 14); BT, balance training (n = 11).
Correlation between different outcome variables
When correlating the differences from baseline to week 8 of the FAB scale (∆-FAB scale) with the magnitude of changes of the other test variables, we found significant correlations between ∆-FAB scale and ∆-stride time variability (Spearman’s Rho: -0.649, p = 0.009) and ∆-RFD (LES) (Spearman’s Rho: 0.643, p = 0.018) within the RT-group (Table 4). A multiple linear regression analysis showed that 71.6% (adjusted R2) of the variance of ∆-FAB scale (as dependent variable) can be explained by ∆-stride time variability and ∆-RFD (LES) (as independent variables) and this model was statistically significant (F = 14.9, p = 0.001). Stride time variability and average RFD equally contributed to the model (stride time variability: Beta = 0.517, T = 2.98, p = 0.015; RFD: Beta = -0.54, T = -3.114, p = 0.012).
Table 4. Correlation between the differences from baseline to 8-weeks follow-up of the FAB scale with the differences from baseline to 8-weeks follow-up of other outcomes.
| Resistance | Balance | |||
|---|---|---|---|---|
| Variable | Rho a | p | Rho a | p |
| Forward pull b | -0.318 | 0.289 | -0.366 | 0.241 |
| Backward pull b | -0.217 | 0.420 | 0.019 | 0.956 |
| TUG | -0.097 | 0.754 | 0.230 | 0.497 |
| UPDRS total score | -0.413 | 0.100 | 0.003 | 0.992 |
| UPDRS motor score c | -0.397 | 0.115 | 0.030 | 0.915 |
| gait velocity | 0.148 | 0.572 | 0.058 | 0.837 |
| stride length | 0.319 | 0.246 | -0.074 | 0.828 |
| double support time | 0.310 | 0.260 | -0.357 | 0.281 |
| stride time variability | -0.649 | 0.009 | 0.260 | 0.440 |
| PCI | -0.152 | 0.587 | -0.608 | 0.047 |
| Asymmetry Index | 0.215 | 0.441 | -0.153 | 0.653 |
| Leg Strength (MVC), LAS | 0.014 | 0.964 | 0.343 | 0.230 |
| Leg Strength (MVC), MAS | -0.510 | 0.075 | -0.140 | 0.647 |
| peak RFD, LAS | 0.114 | 0.712 | -0.003 | 0.993 |
| peak RFD, MAS | 0.263 | 0.385 | -0.119 | 0.713 |
| average RFD (0-100ms), LAS | 0.643 | 0.018 | 0.276 | 0.340 |
| average RFD (0-100ms), MAS | 0.355 | 0.235 | -0.174 | 0.569 |
| PDQ-39 | 0.017 | 0.948 | 0.053 | 0.852 |
| BDI | 0.337 | 0.186 | 0.718 | 0.003 |
BDI, Beck Depression Inventory; FAB, Fullerton Advanced Balance; TUG, Timed-Up-and-Go-Test; LAS, less affected side; MAS, more affected side; MVC, maximal voluntary contraction; PCI, Phase Coordination Index; PDQ-39, Parkinson’s Disease Questionnaire; RFD, rate of force development; UPDRS, Unified Parkinson’s Disease Rating Scale
a Spearman’s rank correlation coefficient
b value represents the area under the curve of the normalized vector length from 0–3 sec after the surface perturbation (see Fig 2 and S3 File)
c blinded video rating, without item 22 (rigidity).
Within the BT-group significant correlations were found between ∆-FAB-scale and ∆-PCI (Spearman’s Rho: -0.608, p = 0.047) and ∆-BDI (Spearman’s Rho: 0.718, p = 0.003) (Table 4). With ∆-PCI and ∆-BDI as predictors for ∆-FAB-scale in the multiple linear regression analysis for the BT-group, the model failed to be significant (adjusted R2 = 19.2%; F = 2.191, p = 0.174).
The independent variables of both models did not correlate (Spearman’s Rho<0.6; p<0.05) and the variance inflation factors were below 2.2 indicating a very low risk of mutlicollinearity.
No significant correlation was found when correlating the degree of cognitive impairment (measured by the MMSE) and ∆-FAB scale.
Discussion
No significant differences were found when comparing the effects of RT with the effects of BT to improve postural control in individuals with PD. Within the RT group, participants significantly improved postural control with a medium effect size. The average improvement at the FAB scale of the RT group was beyond the minimal detectable change (MDC) (MDC95 = 2.25 points, calculated according to [30,46]), indicating a true performance change instead of a change due to variability of performance or measurement error. Participants from the BT group only slightly improved on the FAB scale but this amelioration was not significant and the effect size was small. Within the RT group 7 patients improved beyond the MDC of the FAB scale whereas only 2 of the participants of the BT group showed improvements beyond the MDC. The fact, that the difference between the training effects was not significant, may be due to our small sample size. We conclude that there exists only a small difference between RT and BT. With regard to the large effect size when comparing the effects of the two training interventions, a tendency is given that RT might be more effective than BT to improve postural control in this population.
It has been shown that balance training can be effective to improve postural control in PD [13,14]. These studies used higher training frequencies which may explain the different findings in comparison to our trial. Furthermore the aim of these studies was not to compare competing training types but to analyse the efficacy of one training type.
The higher training effects of the RT group in comparison to the BT group on the FAB scale is notable, as—in contrast to RT—the items of the FAB scale are closely related to the exercises of the BT. All participants underwent an examination to assess eligibility before participating meanwhile the FAB scale was carried out the first time. At baseline the participants thus performed the scale the second time. This emphasizes to consider the improvement from baseline to week 8 due to training effects and not based on memory effects due to the repetition of the same test.
It has to be taken into account that participants only trained two times per week. Training frequency therefore was low and maybe not high enough to detect significant differences. The pre-intervention level of physical activity of the participants was relatively low but similar to the activity level of healthy age-matched controls. In the study of Joshua et al. [25] who showed significant stronger improvement in postural control due to RT in comparison to BT in healthy elderly, training intensity was much higher and participants trained 4x/week for 6 months. As our participants were in an advanced stage of disease (H&Y: 2.5–3.0) and all of them reported to have postural impairments, we considered this training frequency practical feasible as most of the participants were not able to come to the training sessions alone and probably may not be able to train more often.
Gait velocity did not improve due to RT. This is in line with a recently published meta-analysis [16]. Furthermore, we have shown that stride lengths, double support time, gait variability, gait asymmetry and bilateral coordination did not improve due to both training types. To our best knowledge, this is the first study analysing the efficacy of RT and BT on more specific gait features than gait velocity.
The relationship between the improvement in postural control and improvement in rate of force development of the less affected PD site highlights the importance of strength with regard to postural control. The ability to generate force in the early onset of muscle contraction seems to play an important role for postural control mechanisms. By contrast, the changes of overall motor and mobility performance (measured by the UPDRS and TUG) did not correlate with the improvements of balance. The fact that especially the RFD of the less- but not the more affected PD side contributed to better postural control is in accordance with a recent study showing that training the less affected side leads to higher improvements in PD than standard exercise [47]. This raises the idea that RT may be an effective compensatory strategy to enhance postural control in this population.
RT was not performed with exercise machines; instead, participants’ body weight, cuff weights and elasticated bands were used as resistance. This was done as we wanted to perform a training type, which is–as BT–easy and cost-effective to perform without the need of exercise machines which are not always present in physical therapy. We are aware that beside the main aim to improve strength, RT with freely coordinated exercises may train sensorimotor integration as well. However, the primary objective of these kinds of exercises is the improvement of muscle strength.
Three participants had MMSE scores below 25 points. As some tests with multi-step instructions (FAB scale and TUG) and some tests with self-report measures (UPDRS, BDI, PDQ-39 and CGI-I) require cognitive capacity, we reanalyzed our data excluding these three patients for the between group comparison. Results did not change except for the PDQ-39 (significant higher improvement of the RT group in comparison to the BT group).
The following limitations exist. First, one major limitation is that training frequency was low and probably under-dosed to detect significant differences between these two competing training types. Second, we had a 20% drop-out rate, which was larger as we anticipated in the sample size calculation. Our sample size therefore might have been underpowered to detect significant differences. Especially as the correlation- and regression analysis were performed with the RT- and BT-group separately, results have to be interpreted with caution with respect to the small sample size. Furthermore, we did not assess fall rates which would be of interest as strength and balance performance are independent risk factors for falls. Finally, we did not include any control group without any intervention which would allow to further interpret the effects of both training types.
Conclusions
This randomized controlled rater blinded trial shows that the difference between RT and BT to improve postural control in individuals with PD was small and not significant with this sample size. There was weak evidence that freely coordinated RT might be more effective than BT. Our results indicate a relationship between the enhancement of rate of force development and the improvement of postural control within the RT group, but this should be verified in future trials. Future studies should include larger sample sizes to further explore the impact of RT to improve postural control in patients with PD. The comparison of competing training interventions should be analyzed furthermore to gain insight into which exercise program might be most effective and about the underlying processes leading to the results. Concerning long-term attendance the assessment of how much the participants like to participate in a specific training type should be included.
Supporting Information
(PDF)
Text and figures which describe the resistance training.
(PDF)
Text and figures which describe the balance training.
(PDF)
Text which gives further details about the surface perturbations.
(PDF)
Text which gives further details about the gait analysis.
(PDF)
Text which gives further details about the strength testing.
(PDF)
(PDF)
(PDF)
Abbreviations:
- BDI
Beck Depression Inventory
- BT
Balance Training
- CGI-I
Clinical Global Impression–Improvement
- FAB
Fullerton Advanced Balance
- ICC
intraclass correlation coefficient
- LAS
less affected Parkinson’s disease side
- LSWT
long swing time
- MAS
more affected Parkinson’s disease side
- MDC
minimal detectable change
- MMSE
Mini-Mental State Examinaion
- MVC
maximal voluntary contraction
- PD
Parkinson’s disease
- PDQ-39
Parkinson’s disease Questionnaire
- PASE
Physical Activity for the Elderly
- RFD
rate of force development
- RT
Resistance Training
- SSWT
short swing time
- TUG
Timed-up-and-go-test
- UPDRS
Unified Parkinson’s Disease Rating Scale
Data Availability
Data availability is restricted by the local ethics committee. Data are available upon request from the corresponding author.
Funding Statement
The project was funded by the Coppenrath-Stiftung, Geeste/Groß-Hesepe, Niedersachsen, Germany and Krumme-Stiftung, Eckernförde, Schleswig-Holstein, Germany. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Nantel J, McDonald JC, Bronte-Stewart H (2012) Effect of medication and STN-DBS on postural control in subjects with Parkinson's disease. Parkinsonism & related disorders 18: 285–289. [DOI] [PubMed] [Google Scholar]
- 2. Visser JE, Allum JH, Carpenter MG, Esselink RA, Speelman JD, Borm GF, et al. (2008) Subthalamic nucleus stimulation and levodopa-resistant postural instability in Parkinson's disease. J Neurol 255: 205–210. 10.1007/s00415-008-0636-x [DOI] [PubMed] [Google Scholar]
- 3. Fasano A, Aquino CC, Krauss JK, Honey CR, Bloem BR (2015) Axial disability and deep brain stimulation in patients with Parkinson disease. Nature reviews Neurology 11: 98–110. 10.1038/nrneurol.2014.252 [DOI] [PubMed] [Google Scholar]
- 4. Latt MD, Lord SR, Morris JG, Fung VS (2009) Clinical and physiological assessments for elucidating falls risk in Parkinson's disease. Mov Disord 24: 1280–1289. 10.1002/mds.22561 [DOI] [PubMed] [Google Scholar]
- 5. Robinson K, Dennison A, Roalf D, Noorigian J, Cianci H, Bunting-Perry L, et al. (2005) Falling risk factors in Parkinson's disease. NeuroRehabilitation 20: 169–182. [PubMed] [Google Scholar]
- 6. Kerr GK, Worringham CJ, Cole MH, Lacherez PF, Wood JM, Silburn PA (2010) Predictors of future falls in Parkinson disease. Neurology 75: 116–124. 10.1212/WNL.0b013e3181e7b688 [DOI] [PubMed] [Google Scholar]
- 7. Ashburn A, Stack E, Pickering RM, Ward CD (2001) Predicting fallers in a community-based sample of people with Parkinson's disease. Gerontology 47: 277–281. [DOI] [PubMed] [Google Scholar]
- 8. Wood BH, Bilclough JA, Bowron A, Walker RW (2002) Incidence and prediction of falls in Parkinson's disease: a prospective multidisciplinary study. J Neurol Neurosurg Psychiatry 72: 721–725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Dibble LE, Addison O, Papa E (2009) The effects of exercise on balance in persons with Parkinson's disease: a systematic review across the disability spectrum. J Neurol Phys Ther 33: 14–26. 10.1097/NPT.0b013e3181990fcc [DOI] [PubMed] [Google Scholar]
- 10. Allen NE, Sherrington C, Suriyarachchi GD, Paul SS, Song J, Canning CG (2012) Exercise and motor training in people with Parkinson's disease: a systematic review of participant characteristics, intervention delivery, retention rates, adherence, and adverse events in clinical trials. Parkinson's disease 2012: 854–869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Goodwin VA, Richards SH, Taylor RS, Taylor AH, Campbell JL (2008) The effectiveness of exercise interventions for people with Parkinson's disease: a systematic review and meta-analysis. Movement Disorders 23: 631–640. 10.1002/mds.21922 [DOI] [PubMed] [Google Scholar]
- 12. Canning CG, Sherrington C, Lord SR, Close JC, Heritier S, Heller GZ, et al. (2015) Exercise for falls prevention in Parkinson disease: A randomized controlled trial. Neurology 84: 304–312. 10.1212/WNL.0000000000001155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Smania N, Corato E, Tinazzi M, Stanzani C, Fiaschi A, Girardi P, et al. (2010) Effect of balance training on postural instability in patients with idiopathic Parkinson's disease. Neurorehabil Neural Repair 24: 826–834. 10.1177/1545968310376057 [DOI] [PubMed] [Google Scholar]
- 14.Conradsson D, Lofgren N, Nero H, Hagstromer M, Stahle A, Lokk J, et al. (2015) The Effects of Highly Challenging Balance Training in Elderly With Parkinson's Disease: A Randomized Controlled Trial. Neurorehabilitation and neural repair. [DOI] [PMC free article] [PubMed]
- 15. Corcos DM, Robichaud JA, David FJ, Leurgans SE, Vaillancourt DE, Poon C, et al. (2013) A two-year randomized controlled trial of progressive resistance exercise for Parkinson's disease. Movement disorders: official journal of the Movement Disorder Society 28: 1230–1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Tillman A, Muthalib M, Hendy AM, Johnson LG, Rantalainen T, Kidgell DJ, et al. (2015) Lower limb progressive resistance training improves leg strength but not gait speed or balance in Parkinson's disease: a systematic review and meta-analysis. Frontiers in aging neuroscience 7: 40 10.3389/fnagi.2015.00040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chung CL, Thilarajah S, Tan D (2015) Effectiveness of resistance training on muscle strength and physical function in people with Parkinson's disease: A systematic review and meta-analysis. Clinical rehabilitation. [DOI] [PubMed]
- 18. Lima LO, Scianni A, Rodrigues-de-Paula F (2013) Progressive resistance exercise improves strength and physical performance in people with mild to moderate Parkinson's disease: a systematic review. Journal of physiotherapy 59: 7–13. 10.1016/S1836-9553(13)70141-3 [DOI] [PubMed] [Google Scholar]
- 19. Brienesse LA, Emerson MN (2013) Effects of resistance training for people with Parkinson's disease: a systematic review. Journal of the American Medical Directors Association 14: 236–241. 10.1016/j.jamda.2012.11.012 [DOI] [PubMed] [Google Scholar]
- 20. Nallegowda M, Singh U, Handa G, Khanna M, Wadhwa S, Yadav SL, et al. (2004) Role of sensory input and muscle strength in maintenance of balance, gait, and posture in Parkinson's disease: a pilot study. American journal of physical medicine & rehabilitation 83: 898–908. [DOI] [PubMed] [Google Scholar]
- 21. Nocera JR, Buckley T, Waddell D, Okun MS, Hass CJ (2010) Knee extensor strength, dynamic stability, and functional ambulation: are they related in Parkinson's disease? Arch Phys Med Rehabil 91: 589–595. 10.1016/j.apmr.2009.11.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Allen NE, Canning CG, Sherrington C, Lord SR, Latt MD, Close JC, et al. (2010) The effects of an exercise program on fall risk factors in people with Parkinson's disease: a randomized controlled trial. Movement disorders: official journal of the Movement Disorder Society 25: 1217–1225. [DOI] [PubMed] [Google Scholar]
- 23. Hirsch MA, Toole T, Maitland CG, Rider RA (2003) The effects of balance training and high-intensity resistance training on persons with idiopathic Parkinson's disease. Arch Phys Med Rehabil 84: 1109–1117. [DOI] [PubMed] [Google Scholar]
- 24. Schilling BK, Pfeiffer RF, Ledoux MS, Karlage RE, Bloomer RJ, Falvo MJ (2010) Effects of moderate-volume, high-load lower-body resistance training on strength and function in persons with Parkinson's disease: a pilot study. Parkinson's disease 2010: 824734 10.4061/2010/824734 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Joshua AM, D'Souza V, Unnikrishnan B, Mithra P, Kamath A, Acharya V, et al. (2014) Effectiveness of progressive resistance strength training versus traditional balance exercise in improving balance among the elderly—a randomised controlled trial. Journal of clinical and diagnostic research 8: 98–102. 10.7860/JCDR/2014/8217.4119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Gobbi LT, Oliveira-Ferreira MD, Caetano MJ, Lirani-Silva E, Barbieri FA, Stella F, et al. (2009) Exercise programs improve mobility and balance in people with Parkinson's disease. Parkinsonism Relat Disord 15 Suppl 3: 49–52. [DOI] [PubMed] [Google Scholar]
- 27. Toole T, Hirsch MA, Forkink A, Lehman DA, Maitland CG (2000) The effects of a balance and strength training program on equilibrium in Parkinsonism: A preliminary study. NeuroRehabilitation 14: 165–174. [PubMed] [Google Scholar]
- 28. Tomlinson CL, Herd CP, Clarke CE, Meek C, Patel S, Stowe R, et al. (2014) Physiotherapy for Parkinson's disease: a comparison of techniques. The Cochrane database of systematic reviews 6: CD002815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Gelb DJ, Oliver E, Gilman S (1999) Diagnostic criteria for Parkinson disease. Archives of neurology 56: 33–39. [DOI] [PubMed] [Google Scholar]
- 30. Schlenstedt C, Brombacher S, Hartwigsen G, Weisser B, Moller B, Deuschl G (2015) Comparing the Fullerton Advanced Balance Scale With the Mini-BESTest and Berg Balance Scale to Assess Postural Control in Patients With Parkinson Disease. Arch Phys Med Rehabil 96: 218–225. 10.1016/j.apmr.2014.09.002 [DOI] [PubMed] [Google Scholar]
- 31. Martins WR, de Oliveira RJ, Carvalho RS, de Oliveira Damasceno V, da Silva VZ, Silva MS (2013) Elastic resistance training to increase muscle strength in elderly: a systematic review with meta-analysis. Archives of gerontology and geriatrics 57: 8–15. 10.1016/j.archger.2013.03.002 [DOI] [PubMed] [Google Scholar]
- 32. Hass CJ, Buckley TA, Pitsikoulis C, Barthelemy EJ (2012) Progressive resistance training improves gait initiation in individuals with Parkinson's disease. Gait Posture 35: 669–673. 10.1016/j.gaitpost.2011.12.022 [DOI] [PubMed] [Google Scholar]
- 33. Rose DJ, Lucchese N, Wiersma LD (2006) Development of a multidimensional balance scale for use with functionally independent older adults. Arch Phys Med Rehabil 87: 1478–1485. [DOI] [PubMed] [Google Scholar]
- 34. Winter DA, Patla AE, Ishac M, Gage WH (2003) Motor mechanisms of balance during quiet standing. J Electromyogr Kinesiol 13: 49–56. [DOI] [PubMed] [Google Scholar]
- 35. Podsiadlo D, Richardson S (1991) The timed "Up & Go": a test of basic functional mobility for frail elderly persons. Journal of the American Geriatrics Society 39: 142–148. [DOI] [PubMed] [Google Scholar]
- 36.Guy W (1976) ECDEU assessment manual for psychopharmacology; National Institute of Mental Health. Psychopharmacology Research Branch. Division of Extramural Research P, editor. Rockville, Md: U.S. Dept. of Health, Education, and Welfare, Public Health Service, Alcohol, Drug Abuse, and Mental Health Administration, National Institute of Mental Health, Psychopharmacology Research Branch, Division of Extramural Research Programs. 218–222 p.
- 37. Fahn S, Elton RL (1987) Unified Parkinson’s Disease Rating Scale In: Fahn S, Marsden CD, Calne D, Goldstein M, editors. Recent developments in Parkinson’s disease. Florham Park (NJ): MacMillan Health Care Information; pp. 153–163. [Google Scholar]
- 38. Jenkinson C, Fitzpatrick R, Peto V, Greenhall R, Hyman N (1997) The Parkinson's Disease Questionnaire (PDQ-39): development and validation of a Parkinson's disease summary index score. Age Ageing 26: 353–357. [DOI] [PubMed] [Google Scholar]
- 39. Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J (1961) An inventory for measuring depression. Archives of general psychiatry 4: 561–571. [DOI] [PubMed] [Google Scholar]
- 40. Washburn RA, Smith KW, Jette AM, Janney CA (1993) The Physical Activity Scale for the Elderly (PASE): development and evaluation. J Clin Epidemiol 46: 153–162. [DOI] [PubMed] [Google Scholar]
- 41. Plotnik M, Giladi N, Hausdorff JM (2007) A new measure for quantifying the bilateral coordination of human gait: effects of aging and Parkinson's disease. Experimental brain research 181: 561–570. [DOI] [PubMed] [Google Scholar]
- 42. Plotnik M, Hausdorff JM (2008) The role of gait rhythmicity and bilateral coordination of stepping in the pathophysiology of freezing of gait in Parkinson's disease. Mov Disord 23: 444–450. [DOI] [PubMed] [Google Scholar]
- 43. Geurts AC, Boonstra TA, Voermans NC, Diender MG, Weerdesteyn V, Bloem BR (2011) Assessment of postural asymmetry in mild to moderate Parkinson's disease. Gait & Posture 33: 143–145. [DOI] [PubMed] [Google Scholar]
- 44. Faul F, Erdfelder E, Lang AG, Buchner A (2007) G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior research methods 39: 175–191. [DOI] [PubMed] [Google Scholar]
- 45. Slinker BK, Glantz SA (1985) Multiple regression for physiological data analysis: the problem of multicollinearity. The American journal of physiology 249: R1–12. [DOI] [PubMed] [Google Scholar]
- 46. Haley SM, Fragala-Pinkham MA (2006) Interpreting change scores of tests and measures used in physical therapy. Physical therapy 86: 735–743. [PubMed] [Google Scholar]
- 47.Ricciardi L, Ricciardi D, Lena F, Plotnik M, Petracca M, Barricella S, et al. (2015) Working on asymmetry in Parkinson's disease: randomized, controlled pilot study. Neurological sciences: official journal of the Italian Neurological Society and of the Italian Society of Clinical Neurophysiology. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF)
Text and figures which describe the resistance training.
(PDF)
Text and figures which describe the balance training.
(PDF)
Text which gives further details about the surface perturbations.
(PDF)
Text which gives further details about the gait analysis.
(PDF)
Text which gives further details about the strength testing.
(PDF)
(PDF)
(PDF)
Data Availability Statement
Data availability is restricted by the local ethics committee. Data are available upon request from the corresponding author.