ABSTRACT
Human infections with avian influenza viruses are a serious public health concern. The neuraminidase (NA) inhibitors (NAIs) are the frontline anti-influenza drugs and are the major option for treatment of newly emerging influenza. Therefore, it is essential to identify the molecular markers of NAI resistance among specific NA subtypes of avian influenza viruses to help guide clinical management. NAI-resistant substitutions in NA subtypes other than N1 and N2 have been poorly studied. Here, we identified NA amino acid substitutions associated with NAI resistance among influenza viruses of N3, N7, and N9 subtypes which have been associated with zoonotic transmission. We applied random mutagenesis and generated recombinant influenza viruses carrying single or double NA substitution(s) with seven internal genes from A/Puerto Rico/8/1934 (H1N1) virus. In a fluorescence-based NA inhibition assay, we identified three categories of NA substitutions associated with reduced inhibition by NAIs (oseltamivir, zanamivir, and peramivir): (i) novel subtype-specific substitutions in or near the enzyme catalytic site (R152W, A246T, and D293N, N2 numbering), (ii) subtype-independent substitutions (E119G/V and/or D and R292K), and (iii) substitutions previously reported in other subtypes (Q136K, I222M, and E276D). Our data show that although some markers of resistance are present across NA subtypes, other subtype-specific markers can only be determined empirically.
IMPORTANCE The number of humans infected with avian influenza viruses is increasing, raising concerns of the emergence of avian influenza viruses resistant to neuraminidase (NA) inhibitors (NAIs). Since most studies have focused on NAI-resistance in human influenza viruses, we investigated the molecular changes in NA that could confer NAI resistance in avian viruses grown in immortalized monolayer cells, especially those of the N3, N7, and N9 subtypes, which have caused human infections. We identified not only numerous NAI-resistant substitutions previously reported in other NA subtypes but also several novel changes conferring reduced susceptibility to NAIs, which are subtype specific. The findings indicate that some resistance markers are common across NA subtypes, but other markers need to be determined empirically for each subtype. The study also implies that antiviral surveillance monitoring could play a critical role in the clinical management of influenza virus infection and an essential component of pandemic preparedness.
INTRODUCTION
Vaccination is the primary measure to control the spread of influenza virus infection in humans. However, because of the relatively long time required to prepare conventional influenza vaccine, antiviral drugs are essential as prophylaxis and therapeutics to cope with newly emerging influenza viruses during the early stage of an outbreak. Neuraminidase (NA) inhibitors (NAIs) are the only anti-influenza therapeutics recommended by the World Health Organization because of the wide spread of matrix (M) 2 blocker-resistant variants (1, 2). Four NAIs—oseltamivir (OS), zanamivir (ZA), peramivir (PER), and laninamivir—are commercially available (3).
NA, together with hemagglutinin (HA), comprises a high proportion of the surface protein in the influenza virion, and its catalytic activity cleaves the terminal N-acetyl neuraminic acid (Neu5Ac) on α-2,3- and α-2,6-linked sialic acid moieties, facilitating the release of progeny virions from the host cell and their spread throughout the infected host. This catalytic activity is governed by the following residues conserved among influenza A and B viruses: 8 catalytic residues (R118, D151, R152, R224, E276, R292, R371, and Y406, N2 numbering throughout the manuscript) and 11 framework residues (E119, R156, W178, S179, D198, I222, E227, H274, E277, N294, and E425) (4). The essential role of the NA in influenza virus replication and highly conserved functional residues of NA have made the protein an attractive target for antiviral drugs. The NAIs have been developed to mimic NA's natural substrate, sialic acid (5), thereby preventing the cleavage function of NA by competition and resulting in the aggregation of progeny virions on the cell surface.
Since the increased use of NAIs for clinical treatment, the OS-resistant variants associated with the H274Y mutation have rapidly emerged and spread worldwide and have been detected in up to 100% of seasonal H1N1 viruses from 2007 to 2009 (6). The OS-resistant variant was replaced by the pandemic H1N1 2009 virus (pH1N1), which is generally sensitive to OS, and OS-resistant pH1N1 have been detected at an approximate 1% presence globally (7–11), although some limited spread of OS-resistant pH1N1 has been reported (12). Apart from the H274Y-associated OS-resistant variants, other NA substitutions conferring reduced or highly reduced sensitivity to NAIs have been reported to be clinically relevant. These substitutions conferred distinctive levels of susceptibility to NAIs and have been found to be NA subtype specific: in human H1N1 (Q136K, S246N, and I222R/V), H3N2 (E119V, Q136K, and N294S), H5N1 (N294S), and type B (E105K, R152K, D198N, I222T, N294S, and R371K) viruses (10, 13–26).
Although NAI-resistant mutations have been well studied and profiled in human influenza A viruses of N1 and N2 subtypes and in influenza B viruses, they are poorly understood in avian NA subtypes despite the fact that many avian viruses of the H5, H6, H7, H9, and H10 subtypes and the N1, N2, N3, N7, N8, and N9 subtypes cause human infection (27–31). NA subtypes are classified into two phylogenetically and structurally distinctive groups: group 1 containing N1, N4, N5, and N8 and group 2 containing N2, N3, N6, N7, and N9 (32, 33). Except viruses of the N1 and N8 subtypes in group 1, all NA subtypes that have infected humans belong to group 2. Of note, N2, N3, N7, and N9 were first found in combination with the H7 subtype in humans and caused mild to severe conjunctive and respiratory symptoms (27, 34, 35). Most cases of human infection with H7N2, H7N3, and H7N7 viruses have been related to poultry exposure, with limited evidence of sustained human-to-human transmission, and nearly all patients have recovered after antiviral treatment (35). However, H7N9 is emerging in China, with more than 70% of infected people having influenza-like illness and rapidly progressive respiratory disorders (34, 36). Moreover, the virus has caused more than 30% case fatality rates (37) with sporadic family clusters (38, 39) and detection of NAI-resistance (primarily due to the NA R292K mutation) (40, 41). Nevertheless, limited information associated with NAI resistance is available for avian NA subtypes, and the molecular markers altering NAI susceptibility are often undetermined (42, 43).
Due to the sporadic detection of various avian influenza viruses in humans and the NA subtype specificity of NAI-resistant mutations, it has become essential to identify molecular markers of NAI resistance and to profile NAI-associated resistance in avian influenza viruses. Therefore, we screened for mutations conferring reduced susceptibility to NAIs among avian-origin N3, N7, and N9 influenza virus subtypes. Furthermore, we established an NA gene-fragmented random mutagenesis method facilitating the selection of NAI-resistant substitutions, allowing us to discover novel substitutions. The random-mutant virus libraries generated were processed to select variants resistant to OS and ZA in the genetic background of PR8 virus. We found novel and common substitutions potentially associated with resistance to OS, ZA, and/or PER in avian influenza viruses of N3, N7, and N9 NA subtypes grown in immortalized monolayer cells and offer clues to potential resistance mechanisms in vivo.
MATERIALS AND METHODS
Cells, viruses, plasmids, and neuraminidase inhibitors.
Madin-Darby canine kidney (MDCK) cells were grown at 37°C in 5% CO2 in minimum essential medium (Corning) containing 5% fetal bovine serum (FBS) and vitamins (Gibco). Human embryonic kidney-293T (HEK-293T) cells were grown at 37°C in 5% CO2 in Opti-MEM (Gibco) containing 10% FBS. A/Turkey/Minnesota/916/1980 (H7N3), A/Duck/Potsdam/62-4/1981 (H7N7), and A/Duck/Memphis/546/1974 (H11N9) viruses were propagated in 10-day-old embryonated chicken eggs, and RNA from viruses was extracted to clone the NA gene into the pHW2000 plasmid for virus generation (44). In addition, seven plasmid genes of A/Puerto Rico/8/1934 (H1N1, PR8) virus were also used as part of the genetic background of the variants. The NAIs, oseltamivir carboxylate (ethyl [3R,4R,5S]-4-acetamido-5-amino-3-[1-ethylpropoxy]-1-cyclohexene-1-carboxylate) and zanamivir (2,4-dideoxy-2,3-didehydro-4-guanidineosialic acid), were provided by Hoffmann-La Roche (Nutley, NJ), and peramivir ([1S,2S,3R,4R,1S]-3-[1-acetylamino-2-ethyl] butyl-4-[(aminoimino)-methyl]amino-2-hydroxycyclopentane-1-carboxylic acid) was provided by BioCryst Pharmaceuticals, Inc. (Birmingham, AL). Compounds were dissolved in sterile distilled water and stored in aliquots at −20°C until use.
Gene-fragmented random mutagenesis.
Random mutations were introduced into the catalytic domain of N3, N7, and N9 genes from avian influenza viruses by using a GeneMorph II EZClone domain mutagenesis kit (Stratagene) according to the manufacturer's instructions. The catalytic domains were cleaved into six regions (range, 110 to 470 nucleotide bases) with overlapping fragments by using gene-specific primers (primer sequences are available from the corresponding author upon request). Random mutations of the plasmid libraries were confirmed by sequence analysis of 24 individual clones. Generally, the mutation rate was 1 to 5 amino acid substitutions per kilobase, and two independent library sets per region were generated in each NA gene to increase variations.
Resistance mutation screening and generation of variants.
A total of 18 NA random mutant plasmids libraries (6 libraries per each NA gene) and 3 wild-type NA genes were used to generate a random-mutant virus library. First, 2 μg of each NA plasmid was mixed with 1 μg of seven remaining plasmids of PR8 virus and transfected into a HEK-293T/MDCK cell mixture (3:1) prepared in six-well plates by using TransIT-LT1 reagent (Mirus Bio). At 18 h posttransfection, the medium was replaced with 1 ml of serum-free Opti-MEM with antibiotics. At 40 h posttransfection, 1 ml of Opti-MEM with TPCK (l-tosylamido 2-phenylethyl chloromethyl ketone)-trypsin (final concentration, 1 μg/ml) was added. At 4 days posttransfection, half of each supernatant sample was used to select resistant variants to OS and ZA, and the remaining half of each was used to confirm the sequence of viruses recovered by plaque assay in MDCK cells. After two to four serial passages of rescued viruses in increased dose (10 to 40 μM) of OS and ZA, NA genes of the passaged samples were fully sequenced, and the mutations were verified. All screening procedures were performed three times in each subtype. Any mutations found in NA genes (including mixed population) were introduced into the corresponding subtype in which the mutation was identified by using site-directed mutagenesis (Stratagene) and then recovered by performing reverse genetics according to the general protocol for influenza rescue (44). All rescued viruses were sequenced to confirm that no unwanted mutations were present.
Susceptibility to neuraminidase inhibitors.
A modified fluorometric assay using the fluorogenic substrate 2′-(4-methylumberlliferyl)-α-d-N-acetylneuraminic acid (MUNANA; Sigma-Aldrich, St. Louis, MO) was performed to determine viral NA activity (45). Influenza viruses were standardized to NA activity equivalent to 10 μM 4-methylumbelliferone and incubated with NAIs (concentration range, 5 × 10−7 to 50 μM). The fluorescence of the released 4-methylumbelliferone was measured in a Synergy 2 microplate reader (Biotek, Winooski, VT) at excitation and emission wavelengths of 360 and 460 nM, respectively. The drug concentration that inhibited 50% of the NA enzymatic activity (IC50) was determined from the dose-response curve by using GraphPad Prism 5.0 software (La Jolla, CA). The results are representative of two independent tests. The susceptibility of the mutant viruses was categorized by the criteria recommended by the World Health Organization Antiviral Working Group for interpreting data for the influenza A virus with reduced inhibition by NAIs. These criteria are based on the fold change in IC50 compared to the susceptible virus: normal inhibition, <10-fold; reduced inhibition, 10- to 100-fold; and highly reduced inhibition, >100-fold (46).
Plaque assay.
MDCK cells in six-well plates were prepared to determine the number of PFU per milliliter of recovered, single or double point-mutated viruses. After 48 h of incubation at 37°C in 5% CO2, the plates were chilled at 4°C for 10 min, and the 0.9% agarose overlay (SeaPlqaue; Lonza) was removed and stained with a 1% (wt/vol) crystal violet solution containing 10% formaldehyde. After the plates were washed and dried, the number of plaques in each well that contained between 20 and 100 plaques was counted, and the average size of 20 plaques was calculated after using ImageJ software to measure the size of individual plaques (ImageJ, 1.46r; National Institutes of Health).
Illumina sequencing to determine the genetic proportion of specific mutations.
Viral RNA was extracted by using MagMAX viral isolation kit (Ambion), and one-step reverse transcription-PCR (RT-PCR) was performed with NA gene–specific primers. PCR products were then extracted from 1% agarose gel and purified by using the QIAquick 96 PCR purification kit (Qiagen). Library preparation was performed by using Illumina's Nextera XT DNA sample preparation kit according to the manufacturer's protocol. Amplicons were sequenced on Illumina's MiSeq platform using the paired-end approach. Sequencing reads were then demultiplexed, quality-trimmed, and filtered by using either the NCBI/Sanger or Illumina Pipeline version 1.8 or later format on the CLC Genomics Workbench 7 (CLC Bio). Reads were aligned to the wild-type virus' sequence, and the mapped reads were put through the Quality-Based Variant Detection pipeline. The variants are called if they meet the predefined quality scores and present in both forward and reverse reads at equal ratios. In addition, the minimum variant read frequency was set at 5%, and variants had to be supported by a minimum of 10 reads.
Molecular modeling.
The mutant structures were generated by using the Molecular Operating Environment molecular modeling program (ChemCorp), with the following crystal structures of neuraminidase in complex with inhibitors used as the templates: PDB ID 4MWQ for the OS complex, PDB ID 4MWR for the ZA complex, and PDB ID 4MWV for the PER complex.
RESULTS
Neuraminidase inhibitor resistance screening in avian N3 NAs.
Human infection with avian H7N3 influenza virus was first reported in Italy in 2003 (47) and has caused mostly mild illness in exposed patients (48, 49). Although no evidence of NAI resistance among N3 influenza viruses was reported, several studies demonstrated efficient transmissibility of H7N3 strains in a ferret model (50, 51), indicating potential transmission in humans. We introduced random mutations throughout the catalytic domain of the NA gene of A/Turkey/Minnesota/916/1980 (H7N3) virus and generated a random-mutant virus library in the background of PR8 virus. After subsequent passages (two to four times) in the presence of OS or ZA, NA genes were sequenced. The mutations selected by OS and ZA were directly introduced into the attenuated N3 virus to generate point-mutated viruses for further study. In N3 NA, one amino acid substitution, R292K, was found by OS selection, and seven amino acid substitutions were found by ZA selection (Table 1). Two mutations, R292K and E119G, reduced susceptibility to all 3 NAIs tested as determined by results of a NA inhibition assay with MUNANA substrate, but viruses with the other mutations remained susceptible to the inhibitors. R292K, which was selected by OS, highly reduced inhibition by OS (17,959.7-fold), and reduced inhibition by ZA (22.5-fold) and PER (41.1-fold) compared to that of the parental N3 virus. The E119G mutation, which was selected by ZA, reduced inhibition by ZA (523.2-fold), OS (24.5-fold), and PER (13.6-fold) compared to that of the parental N3 virus. Interestingly, both NA mutations conferred multidrug resistance to N3 viruses (i.e., reduced inhibition by both OS and ZA regardless of PER). For comparison, the H274Y mutation, which reduces susceptibility to OS in N1 subtype (25, 26), was also introduced into NA of N3 virus, and the variant was resistant to OS but remained susceptible to ZA and PER. Although E119G and R292K mutant viruses formed smaller plaques and replicated to lower virus titers in MDCK cells than did the parental N3 virus, the selected mutations are genetically stable in N3 gene in the background of PR8 virus after 3 sequential passages in MDCK cells (Table 1). However, virus with the H274Y NA substitution characterized by highly impaired viral growth and reduced plaque size in MDCK cells, as well as the presence of a high proportion of reverse substitutions after three passages (Table 1).
TABLE 1.
Susceptibility to NAIs and viral properties caused by the selected substitutions in NA of avian N3 influenza virusesa
| NA amino acid change (N2 numbering) | Location within NA active siteb | Selection NAIc | Oseltamivir |
Zanamivir |
Peramivir |
Mean infectivity (log10 PFU/ml ± SD) | Mean plaque size ± SD (mm) | Genetic stabilityd (% read) | |||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean IC50 ± SD (nM) | Fold change | Mean IC50 ± SD (nM) | Fold change | Mean IC50 ± SD (nM) | Fold change | ||||||
| WT N3 | na | na | 0.18 ± 0.02 | 1.0 | 0.50 ± 0.04 | 1.0 | 0.27 ± 0.09 | 1.0 | 8.6 ± 0.1 | 1.78 ± 0.41 | na |
| E119G | Framework | ZA | 4.41 ± 0.62 | 24.5 | 261.59 ± 200.47 | 523.2 | 3.68 ± 1.12 | 13.6 | 5.8 ± 0.3* | 1.31 ± 0.36* | G (100) |
| D125A | – | ZA | 0.15 ± 0.01 | 0.8 | 0.32 ± 0.04 | 0.6 | 0.14 ± 0.00 | 0.5 | 8.5 ± 0.2 | 1.70 ± 0.59 | ND |
| Q136L | – | ZA | 0.15 ± 0.01 | 0.8 | 0.32 ± 0.04 | 0.6 | 0.14 ± 0.00 | 0.5 | 8.2 ± 0.0 | 1.34 ± 0.48* | ND |
| I149F | – | ZA | 0.17 ± 0.01 | 1.0 | 0.49 ± 0.05 | 1.0 | 0.20 ± 0.02 | 0.8 | 8.6 ± 0.1 | 1.65 ± 0.48 | ND |
| N268Y | – | ZA | 0.21 ± 0.01 | 1.1 | 0.58 ± 0.06 | 1.2 | 0.21 ± 0.03 | 0.8 | 8.5 ± 0.2 | 1.68 ± 0.46 | ND |
| H274Y | Framework | Inducede | 2,201.25 ± 429.5 | 12,229.2 | 1.01 ± 0.46 | 2.0 | 0.20 ± 0.05 | 0.7 | 5.6 ± 0.1* | 1.08 ± 0.22* | H (59), Y (41) |
| R292K | Catalytic | OS | 3,232.75 ± 1,192.36 | 17,959.7 | 11.24 ± 1.14 | 22.5 | 11.11 ± 3.20 | 41.1 | 7.6 ± 0.1* | 0.51 ± 0.16* | K (100) |
| A329V | – | ZA | 0.22 ± 0.07 | 1.2 | 0.58 ± 0.11 | 1.2 | 0.20 ± 0.02 | 0.7 | 8.5 ± 0.1 | 1.48 ± 0.40* | ND |
| I427L | – | ZA | 0.13 ± 0.03 | 0.7 | 0.50 ± 0.06 | 1.0 | 0.13 ± 0.01 | 0.5 | 8.6 ± 0.2 | 1.48 ± 0.45* | ND |
Mean values are means from two independent experiments. Fold changes are expressed respective to replication of the WT virus.WT, wild type; na, not applicable; ND, not determined due to insignificant alteration of NAI-susceptibility of the indicated mutant virus; –, located outside NA enzyme active site; ZA, zanamivir; OS, oseltamivir; *, P < 0.05, compared to the corresponding infectivity or plaque size of WT virus.
Previously defined residues were divided into two groups of active residues: catalytic and framework residues.
That is, the NAI used to select the corresponding mutations.
Sequence variation was analyzed by Illumina sequencing.
Introduced mutation for comparison.
Neuraminidase inhibitor resistance screening in avian N7 NAs.
The first report of human infection with low-pathogenicity avian influenza H7N7 virus was published in the United Kingdom in 1996 (52). However, the first reported outbreak of human infection with highly pathogenic avian influenza (HPAI) H7N7 virus was in the Netherlands in 2003 and involved 86 poultry workers, one of whom died of pneumonia and acute respiratory distress syndrome (53, 54). Therefore, we also assessed avian N7 originating from A/Duck/Potsdam/62-4/1981 (H7N7) virus to identify any NA substitutions that reduce susceptibility to NAIs. The entire catalytic domain of the NA gene was screened by using random mutagenesis as mentioned above. Six amino acid substitutions were found in NA protein after passaging in MDCK cells under OS pressure. Three NA mutations at either framework (E119V) or catalytic (R152W and R292K) residues conferred reduced susceptibility to NAIs (Table 2). Viruses with the E119V mutation were associated with reduced inhibition by OS (55.3-fold increase) but remained susceptible to ZA and PER. Notably, R292K conferred highly reduced inhibition to both OS (44,326.4-fold) and PER (414.8-fold) and reduced inhibition to ZA (21.1-fold). An Arg (R)-to-Trp (W) substitution at position 152 is a novel NA mutation that conferred reduced NAI susceptibility, and the mutation is associated with resistance to both OS (14.1-fold) and ZA (11.4-fold), with susceptibility to PER unaltered. Nine NA mutations were found after ZA selection; four of these were associated with reduced susceptibility to NAIs: E119G/D, E276D, and D293N (Table 2). Both E119D and E119G conferred either reduced or highly reduced sensitivity to ZA (67.3- and 116-fold, respectively) but did not affect susceptibility to OS and PER. E119D was identified together with the S111N mutation, but the S111N-E119D double mutant had an IC50 similar to that of the E119D single mutant. Both E276D and D293N are novel mutations found by selective drug pressure and are located in or near catalytic residues. E276D is associated with reduced inhibition by ZA (13.6- to 25.9-fold) but normal inhibition by OS and PER (4.8- to 6.7-fold). D293N conferred reduced inhibition by OS (13.5-fold) and ZA (57.3-fold) without affecting susceptibility to PER (5.4-fold). Although the N198Y/K mutation is in a framework residue in NA, mutants containing this alteration remained susceptible to all NAIs tested. The addition of the H274Y mutation reduced inhibition by OS (17.4-fold) in N7 virus. Although three mutations, R152W, E276D, and D293N, resulted in plaque sizes smaller than those of the parental N7 virus, the virus titers of all N7 mutants in PR8 background were comparable to that of their parental N7 virus, and all mutants maintained the given NA changes after three sequential passages in MDCK cells (Table 2).
TABLE 2.
Susceptibility to NAIs and viral properties caused by the selected substitutions in NA of avian N7 influenza virusesa
| NA amino acid change (N2 numbering) | Location within NA active siteb | Selection NAIc | Oseltamivir |
Zanamivir |
Peramivir |
Mean infectivity (log10 PFU/ml ± SD) | Mean plaque size ± SD (mm) | Genetic stabilityd (% read) | |||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean IC50 ± SD (nM) | Fold change | Mean IC50 ± SD (nM) | Fold change | Mean IC50 ± SD (nM) | Fold change | ||||||
| WT N7 | na | na | 0.36 ± 0.01 | 1.0 | 1.32 ± 0.11 | 1.0 | 0.25 ± 0.04 | 1.0 | 7.4 ± 0.1 | 1.51 ± 0.48 | na |
| E119V | Framework | OS | 19.90 ± 0.82 | 55.3 | 1.61 ± 0.36 | 1.2 | 0.41 ± 0.03 | 1.6 | 7.9 ± 0.1 | 1.44 ± 0.42 | V (100) |
| E119G | Framework | ZA | 0.43 ± 0.07 | 1.2 | 88.90 ± 17.27 | 67.3 | 0.29 ± 0.00 | 1.1 | 7.9 ± 0.0 | 1.46 ± 0.42 | G (99) |
| S111N-E119D | –/Framework | ZA | 1.28 ± 0.10 | 3.6 | 153.53 ± 30.54 | 116.3 | 0.31 ± 0.00 | 1.2 | 8.8 ± 0.2 | 1.45 ± 0.42 | N (100), D (100) |
| E119D | Framework | ZA | 1.22 ± 0.08 | 3.4 | 132.83 ± 9.35 | 100.6 | 0.28 ± 0.02 | 1.1 | 8.2 ± 0.1 | 1.50 ± 0.34 | D (100) |
| R152W | Catalytic | OS | 5.08 ± 0.20 | 14.1 | 15.01 ± 0.64 | 11.4 | 0.19 ± 0.04 | 0.8 | 7.5 ± 0.3 | 1.06 ± 0.38* | W (100) |
| T153S | – | OS | 0.37 ± 0.03 | 1.0 | 1.14 ± 0.06 | 0.9 | 0.27 ± 0.10 | 1.1 | 8.1 ± 0.1 | 1.39 ± 0.35 | ND |
| L163M | – | ZA | 0.31 ± 0.03 | 0.9 | 1.23 ± 0.15 | 0.9 | 0.28 ± 0.04 | 1.1 | 8.2 ± 0.1 | 1.62 ± 0.45 | ND |
| R189S | – | ZA | 0.32 ± 0.05 | 0.9 | 1.01 ± 0.12 | 0.8 | 0.41 ± 0.20 | 1.7 | 7.9 ± 0.1 | 1.60 ± 0.48 | ND |
| N198Y | Framework | OS | 0.60 ± 0.02 | 1.7 | 1.36 ± 0.22 | 1.0 | 0.18 ± 0.03 | 0.7 | 7.3 ± 0.1 | 1.47 ± 0.45 | ND |
| N198K | Framework | ZA | 0.69 ± 0.08 | 1.9 | 1.70 ± 0.12 | 1.3 | 0.27 ± 0.12 | 1.1 | 7.8 ± 0.1 | 1.43 ± 0.29 | ND |
| K216R | – | OS | 0.34 ± 0.01 | 0.9 | 1.30 ± 0.14 | 1.0 | 0.28 ± 0.06 | 1.1 | 7.6 ± 0.1 | 1.56 ± 0.46 | ND |
| H274Y | Framework | Inducede | 6.28 ± 0.33 | 17.4 | 2.34 ± 0.24 | 1.8 | 0.50 ± 0.12 | 2.0 | 7.5 ± 0.2 | 1.32 ± 0.36 | Y (100) |
| I275T-E276D | –/Catalytic | ZA | 2.23 ± 0.09 | 6.2 | 17.93 ± 1.94 | 13.6 | 1.21 ± 0.18 | 4.8 | 7.5 ± 0.2 | 0.81 ± 0.13* | T (100), D (100) |
| I275T | – | ZA | 0.16 ± 0.01 | 0.5 | 1.18 ± 0.18 | 0.9 | 0.21 ± 0.02 | 0.8 | 7.5 ± 0.1 | 1.73 ± 0.44 | ND |
| E276D | Catalytic | ZA | 2.42 ± 0.04 | 6.7 | 34.18 ± 2.91 | 25.9 | 1.30 ± 0.07 | 5.2 | 7.6 ± 0.4 | 0.79 ± 0.20* | D (100) |
| R292K | Catalytic | OS | 15,957.50 ± 2,375.48 | 44,326.4 | 27.86 ± 2.21 | 21.1 | 103.71 ± 12.89 | 414.8 | 7.6 ± 0.4 | 1.37 ± 0.39 | K (100) |
| D293N | – | ZA | 4.86 ± 2.00 | 13.5 | 75.65 ± 3.97 | 57.3 | 1.36 ± 0.04 | 5.4 | 8.0 ± 0.2 | 1.06 ± 0.32* | N (100) |
See Table 1, footnote a.
See Table 1, footnote b.
See Table 1, footnote c.
See Table 1, footnote d.
See Table 1, footnote e.
Neuraminidase inhibitor resistance screening in avian N9 NAs.
Since the first human outbreak of avian H7N9 virus in China in 2013, the virus has been causing serious influenza-like illness with a case fatality rate of ∼30% and has rapidly acquired NAI-resistant substitutions. Thus, we also used random mutagenesis to screen for mutations conferring reduced susceptibility to NAIs in avian N9 originating from A/Duck/Memphis/546/1974 (H11N9) virus when assessed in immortalized monolayer cells. Four and five amino acid substitutions in the NA protein were found by OS and ZA selection, respectively (Table 3). Of the OS-selected mutations, E119V, I222M, and R292K were associated with reduced susceptibility to NAIs. E119V and I222M, which are located in framework residues, reduced susceptibility to OS (49.5- and 18.3-fold, respectively) but did not alter susceptibility to either ZA or PER. However, the R292K mutation conferred resistance to all NAIs tested (68,891.1-fold to OS, 51.3-fold to ZA, and 2,067.9-fold to PER). Of the ZA-selected mutations, Q136K and A246T mutations, which are not in functional or framework residues, resulted in reduced susceptibility to NAI(s) (Table 3). Q136K was associated with highly reduced inhibition to ZA (121.1-fold) and reduced inhibition to PER (53.9-fold). A246T, a novel NAI resistance mutation, reduced sensitivity to ZA (25.4-fold) but did not affect inhibition by OS (6.2-fold) and PER (7.2-fold). When the H274Y mutation was added for comparison, the N9 virus had reduced inhibition by OS (90.3-fold) and PER (11.2-fold). Although most of the N9 mutants in PR8 background with reduced susceptibility to NAI(s) formed smaller plaques than did the parental N9 virus, their virus titers were comparable to those of the parental N9 virus, and all mutants maintained the given mutations after three sequential passages in MDCK cells (Table 3).
TABLE 3.
Susceptibility to NAIs and viral properties caused by the selected substitutions in NA of avian N9 influenza virusesa
| NA amino acid change (N2 numbering) | Location within NA active siteb | Selection NAIc | Oseltamivir |
Zanamivir |
Peramivir |
Mean infectivity (log10 PFU/ml ± SD) | Mean plaque size ± SD (mm) | Genetic stabilityd (% read) | |||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean IC50 ± SD (nM) | Fold change | Mean IC50 ± SD (nM) | Fold change | Mean IC50 ± SD (nM) | Fold change | ||||||
| WT N9 | na | na | 0.40 ± 0.02 | 1.0 | 0.59 ± 0.03 | 1.0 | 0.06 ± 0.03 | 1.0 | 8.1 ± 0.2 | 1.51 ± 0.40 | na |
| E119V | Framework | OS | 20.01 ± 1.35 | 49.5 | 1.79 ± 0.13 | 3.0 | 0.08 ± 0.02 | 1.4 | 8.6 ± 0.2 | 1.23 ± 0.16* | V (100) |
| P120S | – | ZA | 0.40 ± 0.01 | 1.0 | 0.73 ± 0.03 | 1.2 | 0.06 ± 0.04 | 1.0 | 8.5 ± 0.2 | 1.35 ± 0.36 | ND |
| Q136K | – | ZA | 0.20 ± 0.04 | 0.5 | 71.48 ± 4.47 | 121.1 | 3.23 ± 0.89 | 53.9 | 7.6 ± 0.2 | 0.74 ± 0.21* | K (100) |
| G147R | – | ZA | 0.26 ± 0.02 | 0.6 | 1.03 ± 0.07 | 1.7 | 0.08 ± 0.04 | 1.5 | 8.3 ± 0.5 | 1.28 ± 0.23* | ND |
| I222M | Framework | OS | 7.32 ± 0.27 | 18.3 | 2.37 ± 0.74 | 4.0 | 0.24 ± 0.02 | 4.0 | 8.1 ± 0.3 | 1.05 ± 0.22* | M (100) |
| A246T | – | ZA | 2.47 ± 0.72 | 6.2 | 15.01 ± 1.93 | 25.4 | 0.43 ± 0.07 | 7.2 | 7.5 ± 0.1 | 1.51 ± 0.31 | T (100) |
| E259D | – | OS | 0.41 ± 0.02 | 1.0 | 0.75 ± 0.09 | 1.3 | 0.13 ± 0.02 | 2.2 | 8.0 ± 0.0 | 1.54 ± 0.26 | ND |
| H274Y | Framework | Inducede | 36.13 ± 12.53 | 90.3 | 1.41 ± 0.18 | 2.4 | 0.67 ± 0.19 | 11.2 | 7.7 ± 0.1 | 0.89 ± 0.22* | Y (100) |
| R292K | Catalytic | OS | 27,832.00 ± 31,020.67 | 68,891.1 | 30.27 ± 5.49 | 51.3 | 116.43 ± 6.65 | 2,067.9 | 8.5 ± 0.1 | 1.00 ± 0.16* | K (100) |
| D339G | – | ZA | 0.38 ± 0.02 | 0.9 | 0.63 ± 0.10 | 1.1 | 0.10 ± 0.01 | 1.7 | 8.4 ± 0.2 | 1.62 ± 0.44 | ND |
See Table 1, footnote a.
See Table 1, footnote b.
See Table 1, footnote c.
See Table 1, footnote d.
See Table 1, footnote e.
Structural modeling of H7N9 NA protein with the identified substitutions in N9 virus.
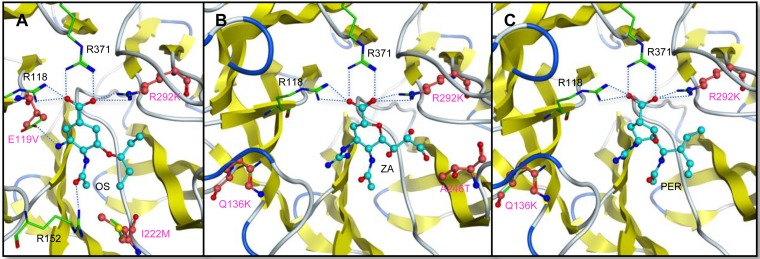
During the avian H7N9 outbreak in China, R292K and E119V changes in the NA gene that are associated with resistance to NAIs were identified (40, 55). The N9 structure of A/Anhui/1/2013 (H7N9) virus has been determined in complex with various NAIs (56). We modeled the R292K, E119V, I222M, Q136K, and A246T mutations by using the known NA structure of H7N9 virus (Fig. 1). In the case of all three NAIs, the R292K substitution potentially leads to loss of two hydrogen bond interactions between the protein and the inhibitor (Fig. 1). The E119V substitution may also causes loss of a hydrogen bond with the inhibitor, reducing affinity for OS (Fig. 1A). The I222M substitution potentially causes a steric clash with R152, possibly pushing it away from OS and causing the loss of another hydrogen bond that this arginine makes with OS (Fig. 1A). Although the lysine in the Q136K mutation does not seem to make any direct contact with the inhibitor, its interaction with other surrounding residues may lead to local changes that eventually reduce affinity for ZA and PER (Fig. 1B and C). A246T mutation potentially leads to steric clashes with the inhibitor, reducing affinity for ZA (Fig. 1B).
FIG 1.
Structural modeling of H7N9 NA protein bounded NAIs with the identified substitutions in N9 virus. NA protein mutations conferring resistance to oseltamivir (OS) (A), zanamivir (ZA) (B), and peramivir (PER) (C). The indicated drug molecule bound to NA is depicted in ball and stick model: wild-type residues are depicted in sticks with green carbon atoms, and mutated residues (including position number) are indicated in pink. H-bond interactions are depicted by dotted lines. The respective Protein Data Bank accession numbers of the cocrystal structures used to model A, B, and C are 4MWQ, 4MWR, and 4MWV.
DISCUSSION
Sequence-based NAI susceptibility screening of human influenza viruses is a rapid component of epidemic and pandemic response. The sequence data obtained during antiviral surveillance monitoring could play an important role in the clinical management of influenza virus infection. The rationale for the present study was therefore to identify NAI resistance-associated substitution in the NA protein of avian influenza viruses utilizing immortalized monolayer cells as an essential component of pandemic preparedness. To address biosafety issues associated with induction of NA substitution to clinically relevant antivirals (such as NAIs), we used an attenuated viral backbone with limited replication capacity in humans and NAs from viruses not associated with zoonotic infection. Because it is well documented that the balanced activity of HA and NA is essential for influenza virus growth, our approach did not, however, allow us to evaluate the fitness characteristics of N3, N7, and N9 viruses carrying NAI resistance mutations. In addition, the NAI resistance mutations were identified in avian viruses grown in the specific cultured monolayer cell setting, which may or may not translate into NAI resistance in vivo.
The NA substitutions identified in this study belong to three categories: (i) novel subtype specific substitutions (R152W and D293N in N7 and A246T in N9), (ii) common substitutions (E119D/G or V and R292K), and (iii) substitutions previously reported in other subtypes (Q136K, I222M, and E276D).
R152 is a catalytic residue that directly interacts with the sialic acid moiety, and the resistant mutation R152K has been found only in influenza B virus-infected patient after treatment with ZA (19, 57). Unlike highly reduced susceptibility to multiple NAIs that is conferred by R152K in influenza B virus, the R152W mutation was selected by OS and reduced inhibition by only OS and ZA in N7 virus. The D293 residue is located between catalytic residue R292 and the framework residue N294, potentially affecting the conformation of the binding moieties. However, D293N does not seem to directly interact with the inhibitors when modeled into the N9 structure, likely affecting the affinity in some indirect manner or the N7 subtype may have a conformation differing from that of the other subtypes.
The A246T change may be a group 2 NA-specific resistance substitution. Group 1 NAs possess serine instead of alanine at position 246 (58), and the S246N mutation has been reported to reduce susceptibility to NAIs in N1 viruses (14, 59). A246 was found to be highly conserved among the group 2 NAs in sequence variation analysis, and T246 was found in only human N2 viruses but not in the other avian group 2 NAs (Table 4 and data not shown). In addition, deletion of amino acids between 245 and 248 residues in human N2 virus conferred resistance to NAIs (60), suggesting that evaluating the effect of the mutation in human H3N2 virus may be beneficial. Furthermore, A246 is structurally colocated with the S246 residue of group 1 NA, supporting the hypothesis that A246T mutation is a group 2 NA-specific NAI resistance mutation (data not shown). Moreover, when we superimposed the mutation on the N2's structure, it similarly altered the binding moiety with ZA, suggesting that it may confer ZA resistance to N2 viruses. The reason these novel mutations have not been found in the previous studies is unclear. Several possible explanations exist: (i) NAI resistance-associated substitutions are NA subtype specific, so the identified novel substitution may be specific to avian N7 and N9 viruses; (ii) relatively low IC50 levels of resistance may not be easily selected by NAIs, with their highest levels of reduction to corresponding NAIs ranging from 14- to 57-fold; and (iii) less frequent use of ZA (two of three mutations were selected by using ZA, which is not as frequently prescribed as OS).
TABLE 4.
NA sequence variations of the NAI resistance-associated substitution identified in N3, N7, and N9 subtypes and in the human N2 subtype
| NA residuea | Consensus | Identified substitution | Sequence variation in human N2 subtype (no. identified)b | No. of sequences analyzed |
|---|---|---|---|---|
| 119 | E | D/G/V | E (8,937), V (26), D (4), G (2), I (2), N (1) | 8,972 |
| 136 | Q | K | Q (8,986), K (7), R (6), H (2), P (2) | 9,003 |
| 152 | R | W | R (9,027), G (1) | 9,028 |
| 222 | I | M | I (9,055), V (16), T (11), N (2), F (1) | 9,085 |
| 246 | A | T | A (9,078), T (2), V (2), S (1) | 9,083 |
| 276 | E | D | E (9,079), K (1) | 9,080 |
| 292 | R | K | R (9,067), K (7), I (1) | 9,075 |
| 293 | D | N | D (9,075), A (1) | 9,076 |
N2 numbering.
Searched in the Influenza Research Database.
We identified common resistance mutations in avian N3, N7, and N9 viruses in this study. Only two substitutions, those at residues E119 and R292, were found in all three avian NA subtypes investigated and conferred some level of NAI resistance. The E119V NA mutation, found in both N7 and N9 subtypes in the present study, is a clinically relevant mutation in human N2 viruses of group 2 NAs by OS treatment and is associated with highly reduced inhibition by OS (18, 19). The mutation also confers resistance to multiple NAIs in N1 subtype of group 1 NAs but significantly impairs their viral fitness (61, 62). In addition to E119V, the E119G/D mutations were identified in N7 and/or N3 subtypes in the present study and tended to have more effect on ZA susceptibility than on the other NAIs. As in other reports (13, 62–64), we observed that mutations at E119 also showed NAI-specific susceptibility in avian N3, N7, and N9 subtypes. Interestingly, all reported NAI resistance mutations at residue E119 (D, G, and V) were found in N7 subtype, suggesting that the residue in this subtype has more flexibility to switch amino acid sequence by OS- or ZA-selective pressure than do the other subtypes. The R292K mutation has frequently been identified in group 2 NAs because of the structural distinction from group 1 NAs (19, 25, 33, 40, 65). Although the PER susceptibility levels of the N3 virus with R292K (41-fold) was higher than that of N7 and N9 viruses (415- to 2,068-fold), the mutation was seen after OS selection in all three NAs of group 2 in our study and showed comparable patterns of reduced inhibition by multiple NAIs, similar to the findings of previous studies (61, 63, 66, 67).
Amino acid changes that have been reported in N1, N2, and B viruses were also identified in avian N3, N7, and N9 viruses in our study. The Q136K mutation found by ZA selection in N9 subtype here was reported in both N1 and N2 subtypes in antiviral surveillance and showed effects similar to those we report in the present study (15, 21, 64). The Q136L mutation, which was reported to increase resistance to OS and ZA in HPAI H5N1 virus (68) was found in N3 subtype in the present study but did not affect susceptibility to all NAIs. Mutations at the I222 residue have been abundantly reported to confer drug resistance in N1, N2, and B viruses (25, 58). We found here that the I222M mutation found in N9 subtype conferred reduced sensitivity to OS: the mutation was also found in HPAI H5N1 and produced synergistic effects when combined with the H274Y mutation (13). The effect of the E276D mutation on NAI susceptibility was previously evaluated after being experimentally introduced (67, 69). Although the mutation showed few effects on N1 virus of group 1 NAs, E276D-possessing N7 and N2 viruses, which belong to group 2 NAs, had reduced inhibition by ZA (67, 69).
We did not identify an H274Y mutation in any avian N3, N7, and N9 viruses. The mutation generally confers high resistance to OS in N1 subtype, which belongs to group 1 NAs, but has little effect on group 2 NAs (33, 70). Consistent with previous results, we found that the H274Y mutation in N7 and N9 subtypes did not confer resistance to OS to the extent as it does in N1 subtypes (62, 71). Although the H274Y substitution had a large effect on the OS resistance of the N3 virus in our study, it also impaired virus growth (5.2 × 105 versus 4.8 × 108 PFU/ml in N3 H274Y mutant and parental N3 virus, respectively) and was unstable upon passage, suggesting that other compensatory changes would be needed for fixation of this resistance marker in N3 subtype.
Because OS and ZA are the predominant NAIs for influenza prophylaxis and therapeutics (PER and laninamivir are still in limited use in most countries), it is critical to investigate whether any mutations confer resistance to both drugs. The appearance of multidrug resistance has been common when a substitution occurs in catalytic residues, such as R152K in influenza B virus or R292K in N2 viruses (25, 26, 58). However, these variants generally possess impaired viral fitness due to altered NA enzymatic activity/affinity and stability. However, several pH1N1 variants associated with mutations in I222 (a framework residue) were recently reported to reduce inhibition to multiple drugs without diminishing viral fitness (16, 72, 73). During our screening, we found that several mutations associated with multidrug resistance. R292K in all three subtypes and E119G in N3 conferred resistance to all NAIs tested. Of note, R152W and D293N, newly identified in N7 subtype, also reduce inhibition to multiple drugs without decreasing virus titer and are genetically stable even though D293N is not located in any catalytic or framework regions.
We demonstrated that random mutagenesis is a suitable approach to identify novel and known NA substitutions associated with NAI resistance among influenza viruses. However, additional efforts must be undertaken to improve the strategy used in the present study and to improve its capacity to predict optimal treatment of emerging viruses. One limitation of our study is the use of the laboratory-adapted PR8 influenza virus backbone to support our mutated NAs. We chose this approach primarily for issues related to biosafety since PR8 has a strong safety record in relation to human infection. The downside of this approach is that we were unable to assess the fitness of viruses carrying such NAs. Any resistance mutation that is associated with a fitness cost for the virus may have limited clinical impact. The ability to accurately predict field NAI resistance would require introduction of the identified NA substitutions into naturally occurring viruses. As such, the mutations that we have identified here can only be considered possible mutations that can confer resistance during virus growth in immortalized monolayer cell cultures, and we can make no inference regarding their resistance phenotype in the field or the likelihood of their emergence and/or spread under field conditions. Although NA subtypes are divided into two structurally distinct groups and each group shares similar NAI-susceptibility profiles, our data show that there are clearly subtle differences between subtypes within group 2 NAs. Therefore, drug resistance markers must be empirically determined for each NA subtype and data from one cannot necessarily be extrapolated to others. Although there are many factors that contribute to the emergence and stability of NAI resistant influenza viruses, the monopoly of NAIs in our ability to treat influenza urges the documentation of resistance imparting mutations in other NA subtypes circulating in nature.
ACKNOWLEDGMENTS
M.-S.S. is partly supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by Ministry of Science, ICT, and Future Planning (NRF-2007-0054930).
We especially thank Cherise Guess for carefully editing the manuscript.
M.-S.S. and R.J.W. designed research. M.-S.S., B.M.M., G.K., S.-S.W., A.R., and M.Z. performed experiments. M.-S.S., Y.-K.C., R.G.W., E.A.G., and R.J.W. analyzed data. M.-S.S., E.A.G., and R.J.W. wrote the paper.
REFERENCES
- 1.CDC. 2006. High levels of adamantane resistance among influenza A (H3N2) viruses and interim guidelines for use of antiviral agents–United States, 2005-06 influenza season. MMWR Morb Mortal Wkly Rep 55:44–46. [PubMed] [Google Scholar]
- 2.Pizzorno A, Abed Y, Boivin G. 2011. Influenza drug resistance. Semin Respir Crit Care Med 32:409–422. doi: 10.1055/s-0031-1283281. [DOI] [PubMed] [Google Scholar]
- 3.Webster RG, Govorkova EA. 2014. Continuing challenges in influenza. Ann N Y Acad Sci 1323:115–139. doi: 10.1111/nyas.12462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Colman PM. 1994. Influenza virus neuraminidase: structure, antibodies, and inhibitors. Protein Sci 3:1687–1696. doi: 10.1002/pro.5560031007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kim CU, Lew W, Williams MA, Wu H, Zhang L, Chen X, Escarpe PA, Mendel DB, Laver WG, Stevens RC. 1998. Structure-activity relationship studies of novel carbocyclic influenza neuraminidase inhibitors. J Med Chem 41:2451–2460. doi: 10.1021/jm980162u. [DOI] [PubMed] [Google Scholar]
- 6.CDC. 2009. Update: influenza activity: United States, September 28, 2008–January 31, 2009. MMWR Morb Mortal Wkly Rep 58:115–119. [PubMed] [Google Scholar]
- 7.Wolfe C, Greenwald I, Chen L. 2010. Pandemic (H1N1) 2009 and oseltamivir resistance in hematology/oncology patients. Emerg Infect Dis 16:1809–1811. doi: 10.3201/eid1611.101053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Moore C, Galiano M, Lackenby A, Abdelrahman T, Barnes R, Evans MR, Fegan C, Froude S, Hastings M, Knapper S, Litt E, Price N, Salmon R, Temple M, Davies E. 2011. Evidence of person-to-person transmission of oseltamivir-resistant pandemic influenza A (H1N1) 2009 virus in a hematology unit. J Infect Dis 203:18–24. doi: 10.1093/infdis/jiq007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chen LF, Dailey NJ, Rao AK, Fleischauer AT, Greenwald I, Deyde VM, Moore ZS, Anderson DJ, Duffy J, Gubareva LV, Sexton DJ, Fry AM, Srinivasan A, Wolfe CR. 2011. Cluster of oseltamivir-resistant 2009 pandemic influenza A (H1N1) virus infections on a hospital ward among immunocompromised patients–North Carolina, 2009. J Infect Dis 203:838–846. doi: 10.1093/infdis/jiq124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.CDC. 2009. Oseltamivir-resistant 2009 pandemic influenza A (H1N1) virus infection in two summer campers receiving prophylaxis–North Carolina, 2009. MMWR Morb Mortal Wkly Rep 58:969–972. [PubMed] [Google Scholar]
- 11.Le QM, Wertheim HF, Tran ND, van Doorn HR, Nguyen TH, Horby P. 2010. A community cluster of oseltamivir-resistant cases of 2009 H1N1 influenza. N Engl J Med 362:86–87. doi: 10.1056/NEJMc0910448. [DOI] [PubMed] [Google Scholar]
- 12.Hurt AC, Hardie K, Wilson NJ, Deng YM, Osbourn M, Leang SK, Lee RT, Iannello P, Gehrig N, Shaw R, Wark P, Caldwell N, Givney RC, Xue L, Maurer-Stroh S, Dwyer DE, Wang B, Smith DW, Levy A, Booy R, Dixit R, Merritt T, Kelso A, Dalton C, Durrheim D, Barr IG. 2012. Characteristics of a widespread community cluster of H275Y oseltamivir-resistant A(H1N1)pdm09 influenza in Australia. J Infect Dis 206:148–157. doi: 10.1093/infdis/jis337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hurt AC, Holien JK, Barr IG. 2009. In vitro generation of neuraminidase inhibitor resistance in A(H5N1) influenza viruses. Antimicrob Agents Chemother 53:4433–4440. doi: 10.1128/AAC.00334-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hurt AC, Lee RT, Leang SK, Cui L, Deng YM, Phuah SP, Caldwell N, Freeman K, Komadina N, Smith D, Speers D, Kelso A, Lin RT, Maurer-Stroh S, Barr IG. 2011. Increased detection in Australia and Singapore of a novel influenza A(H1N1)2009 variant with reduced oseltamivir and zanamivir sensitivity due to a S247N neuraminidase mutation. Euro Surveill 16:pii–19884. [PubMed] [Google Scholar]
- 15.Hurt AC, Holien JK, Parker M, Kelso A, Barr IG. 2009. Zanamivir-resistant influenza viruses with a novel neuraminidase mutation. J Virol 83:10366–10373. doi: 10.1128/JVI.01200-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nguyen HT, Fry AM, Loveless PA, Klimov AI, Gubareva LV. 2010. Recovery of a multidrug-resistant strain of pandemic influenza A 2009 (H1N1) virus carrying a dual H275Y/I223R mutation from a child after prolonged treatment with oseltamivir. Clin Infect Dis 51:983–984. doi: 10.1086/656439. [DOI] [PubMed] [Google Scholar]
- 17.Le QM, Kiso M, Someya K, Sakai YT, Nguyen TH, Nguyen KH, Pham ND, Ngyen HH, Yamada S, Muramoto Y, Horimoto T, Takada A, Goto H, Suzuki T, Suzuki Y, Kawaoka Y. 2005. Avian flu: isolation of drug-resistant H5N1 virus. Nature 437:1108. doi: 10.1038/4371108a. [DOI] [PubMed] [Google Scholar]
- 18.Baz M, Abed Y, McDonald J, Boivin G. 2006. Characterization of multidrug-resistant influenza A/H3N2 viruses shed during 1 year by an immunocompromised child. Clin Infect Dis 43:1555–1561. doi: 10.1086/508777. [DOI] [PubMed] [Google Scholar]
- 19.Mishin VP, Hayden FG, Gubareva LV. 2005. Susceptibilities of antiviral-resistant influenza viruses to novel neuraminidase inhibitors. Antimicrob Agents Chemother 49:4515–4520. doi: 10.1128/AAC.49.11.4515-4520.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wang D, Sleeman K, Huang W, Nguyen HT, Levine M, Cheng Y, Li X, Tan M, Xing X, Xu X, Klimov AI, Gubareva LV, Shu Y. 2013. Neuraminidase inhibitor susceptibility testing of influenza type B viruses in China during 2010 and 2011 identifies viruses with reduced susceptibility to oseltamivir and zanamivir. Antivir Res 97:240–244. doi: 10.1016/j.antiviral.2012.12.013. [DOI] [PubMed] [Google Scholar]
- 21.Dapat C, Suzuki Y, Saito R, Kyaw Y, Myint YY, Lin N, Oo HN, Oo KY, Win N, Naito M, Hasegawa G, Dapat IC, Zaraket H, Baranovich T, Nishikawa M, Saito T, Suzuki H. 2010. Rare influenza A (H3N2) variants with reduced sensitivity to antiviral drugs. Emerg Infect Dis 16:493–496. doi: 10.3201/eid1603.091321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fujisaki S, Takashita E, Yokoyama M, Taniwaki T, Xu H, Kishida N, Sato H, Tashiro M, Imai M, Odagiri T. 2012. A single E105K mutation far from the active site of influenza B virus neuraminidase contributes to reduced susceptibility to multiple neuraminidase-inhibitor drugs. Biochem Biophys Res Commun 429:51–56. doi: 10.1016/j.bbrc.2012.10.095. [DOI] [PubMed] [Google Scholar]
- 23.Sheu TG, Deyde VM, Okomo-Adhiambo M, Garten RJ, Xu X, Bright RA, Butler EN, Wallis TR, Klimov AI, Gubareva LV. 2008. Surveillance for neuraminidase inhibitor resistance among human influenza A and B viruses circulating worldwide from 2004 to 2008. Antimicrob Agents Chemother 52:3284–3292. doi: 10.1128/AAC.00555-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Carr S, Ilyushina NA, Franks J, Adderson EE, Caniza M, Govorkova EA, Webster RG. 2011. Oseltamivir-resistant influenza A and B viruses pre- and postantiviral therapy in children and young adults with cancer. Pediatr Infect Dis J 30:284–288. doi: 10.1097/INF.0b013e3181ff863b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Samson M, Pizzorno A, Abed Y, Boivin G. 2013. Influenza virus resistance to neuraminidase inhibitors. Antivir Res 98:174–185. doi: 10.1016/j.antiviral.2013.03.014. [DOI] [PubMed] [Google Scholar]
- 26.Ferraris O, Lina B. 2008. Mutations of neuraminidase implicated in neuraminidase inhibitors resistance. J Clin Virol 41:13–19. doi: 10.1016/j.jcv.2007.10.020. [DOI] [PubMed] [Google Scholar]
- 27.Belser JA, Bridges CB, Katz JM, Tumpey TM. 2009. Past, present, and possible future human infection with influenza virus A subtype H7. Emerg Infect Dis 15:859–865. doi: 10.3201/eid1506.090072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Malik Peiris JS. 2009. Avian influenza viruses in humans. Rev Sci Tech 28:161–173. [DOI] [PubMed] [Google Scholar]
- 29.Ip DK, Liao Q, Wu P, Gao Z, Cao B, Feng L, Xu X, Jiang H, Li M, Bao J, Zheng J, Zhang Q, Chang Z, Li Y, Yu J, Liu F, Ni MY, Wu JT, Cowling BJ, Yang W, Leung GM, Yu H. 2013. Detection of mild to moderate influenza A/H7N9 infection by China's national sentinel surveillance system for influenza-like illness: case series. BMJ 346:f3693. doi: 10.1136/bmj.f3693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chen H, Yuan H, Gao R, Zhang J, Wang D, Xiong Y, Fan G, Yang F, Li X, Zhou J, Zou S, Yang L, Chen T, Dong L, Bo H, Zhao X, Zhang Y, Lan Y, Bai T, Dong J, Li Q, Wang S, Zhang Y, Li H, Gong T, Shi Y, Ni X, Li J, Zhou J, Fan J, Wu J, Zhou X, Hu M, Wan J, Yang W, Li D, Wu G, Feng Z, Gao GF, Wang Y, Jin Q, Liu M, Shu Y. 2014. Clinical and epidemiological characteristics of a fatal case of avian influenza A H10N8 virus infection: a descriptive study. Lancet 383:714–721. doi: 10.1016/S0140-6736(14)60111-2. [DOI] [PubMed] [Google Scholar]
- 31.Yuan J, Zhang L, Kan X, Jiang L, Yang J, Guo Z, Ren Q. 2013. Origin and molecular characteristics of a novel 2013 avian influenza A(H6N1) virus causing human infection in Taiwan. Clin Infect Dis 57:1367–1368. doi: 10.1093/cid/cit479. [DOI] [PubMed] [Google Scholar]
- 32.World Health Organization. 1980. A revision of the system of nomenclature for influenza viruses: a WHO memorandum. Bull World Health Organ 58:585–591. [PMC free article] [PubMed] [Google Scholar]
- 33.Russell RJ, Haire LF, Stevens DJ, Collins PJ, Lin YP, Blackburn GM, Hay AJ, Gamblin SJ, Skehel JJ. 2006. The structure of H5N1 avian influenza neuraminidase suggests new opportunities for drug design. Nature 443:45–49. doi: 10.1038/nature05114. [DOI] [PubMed] [Google Scholar]
- 34.Yu H, Cowling BJ, Feng L, Lau EH, Liao Q, Tsang TK, Peng Z, Wu P, Liu F, Fang VJ, Zhang H, Li M, Zeng L, Xu Z, Li Z, Luo H, Li Q, Feng Z, Cao B, Yang W, Wu JT, Wang Y, Leung GM. 2013. Human infection with avian influenza A H7N9 virus: an assessment of clinical severity. Lancet 382:138–145. doi: 10.1016/S0140-6736(13)61207-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Abdelwhab EM, Veits J, Mettenleiter TC. 2014. Prevalence and control of H7 avian influenza viruses in birds and humans. Epidemiol Infect 142:896–920. doi: 10.1017/S0950268813003324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ke Y, Wang Y, Liu S, Guo J, Zhang W, Yuan X, Zhang N, Wang Z, Song H, Huang L, Chen Z. 2013. High severity and fatality of human infections with avian influenza A(H7N9) infection in China. Clin Infect Dis 57:1506–1507. doi: 10.1093/cid/cit371. [DOI] [PubMed] [Google Scholar]
- 37.World Health Organization. 2014. WHO risk assessment: human infections with avian influenza A(H7N9) virus 28 February 2014. World Health Organization, Geneva, Switzerland. [Google Scholar]
- 38.Li Q, Zhou L, Zhou M, Chen Z, Li F, Wu H, Xiang N, Chen E, Tang F, Wang D, Meng L, Hong Z, Tu W, Cao Y, Li L, Ding F, Liu B, Wang M, Xie R, Gao R, Li X, Bai T, Zou S, He J, Hu J, Xu Y, Chai C, Wang S, Gao Y, Jin L, Zhang Y, Luo H, Yu H, He J, Li Q, Wang X, Gao L, Pang X, Liu G, Yan Y, Yuan H, Shu Y, Yang W, Wang Y, Wu F, Uyeki TM, Feng Z. 2014. Epidemiology of human infections with avian influenza A(H7N9) virus in China. N Engl J Med 370:520–532. doi: 10.1056/NEJMoa1304617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Belser JA, Gustin KM, Pearce MB, Maines TR, Zeng H, Pappas C, Sun X, Carney PJ, Villanueva JM, Stevens J, Katz JM, Tumpey TM. 2013. Pathogenesis and transmission of avian influenza A (H7N9) virus in ferrets and mice. Nature 501:556–559. doi: 10.1038/nature12391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hu Y, Lu S, Song Z, Wang W, Hao P, Li J, Zhang X, Yen HL, Shi B, Li T, Guan W, Xu L, Liu Y, Wang S, Zhang X, Tian D, Zhu Z, He J, Huang K, Chen H, Zheng L, Li X, Ping J, Kang B, Xi X, Zha L, Li Y, Zhang Z, Peiris M, Yuan Z. 2013. Association between adverse clinical outcome in human disease caused by novel influenza A H7N9 virus and sustained viral shedding and emergence of antiviral resistance. Lancet 381:2273–2279. doi: 10.1016/S0140-6736(13)61125-3. [DOI] [PubMed] [Google Scholar]
- 41.Hai R, Schmolke M, Leyva-Grado VH, Thangavel RR, Margine I, Jaffe EL, Krammer F, Solorzano A, Garcia-Sastre A, Palese P, Bouvier NM. 2013. Influenza A(H7N9) virus gains neuraminidase inhibitor resistance without loss of in vivo virulence or transmissibility. Nat Commun 4:2854. doi: 10.1038/ncomms3854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Orozovic G, Orozovic K, Jarhult JD, Olsen B. 2014. Study of oseltamivir and zanamivir resistance-related mutations in influenza viruses isolated from wild mallards in Sweden. PLoS One 9:e89306. doi: 10.1371/journal.pone.0089306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Stoner TD, Krauss S, Turner JC, Seiler P, Negovetich NJ, Stallknecht DE, Frase S, Govorkova EA, Webster RG. 2012. Susceptibility of avian influenza viruses of the N6 subtype to the neuraminidase inhibitor oseltamivir. Antivir Res 93:322–329. doi: 10.1016/j.antiviral.2011.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hoffmann E, Neumann G, Kawaoka Y, Hobom G, Webster RG. 2000. A DNA transfection system for generation of influenza A virus from eight plasmids. Proc Natl Acad Sci U S A 97:6108–6113. doi: 10.1073/pnas.100133697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Potier M, Mameli L, Belisle M, Dallaire L, Melancon SB. 1979. Fluorometric assay of neuraminidase with a sodium (4-methylumbelliferyl-alpha-d-N-acetylneuraminate) substrate. Anal Biochem 94:287–296. doi: 10.1016/0003-2697(79)90362-2. [DOI] [PubMed] [Google Scholar]
- 46.Okomo-Adhiambo M, Nguyen HT, Abd EA, Sleeman K, Fry AM, Gubareva LV. 2014. Drug susceptibility surveillance of influenza viruses circulating in the United States in 2011-2012: application of the WHO antiviral working group criteria. Influenza Other Respir Viruses 8:258–265. doi: 10.1111/irv.12215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Puzelli S, Di TL, Fabiani C, Campitelli L, De Marco MA, Capua I, Aguilera JF, Zambon M, Donatelli I. 2005. Serological analysis of serum samples from humans exposed to avian H7 influenza viruses in Italy between 1999 and 2003. J Infect Dis 192:1318–1322. doi: 10.1086/444390. [DOI] [PubMed] [Google Scholar]
- 48.Tweed SA, Skowronski DM, David ST, Larder A, Petric M, Lees W, Li Y, Katz J, Krajden M, Tellier R, Halpert C, Hirst M, Astell C, Lawrence D, Mak A. 2004. Human illness from avian influenza H7N3, British Columbia. Emerg Infect Dis 10:2196–2199. doi: 10.3201/eid1012.040961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Nguyen-Van-Tam JS, Nair P, Acheson P, Baker A, Barker M, Bracebridge S, Croft J, Ellis J, Gelletlie R, Gent N, Ibbotson S, Joseph C, Mahgoub H, Monk P, Reghitt TW, Sundkvist T, Sellwood C, Simpson J, Smith J, Watson JM, Zambon M, Lightfoot N. 2006. Outbreak of low pathogenicity H7N3 avian influenza in the UK, including associated case of human conjunctivitis. Euro Surveill 11:E060504. [DOI] [PubMed] [Google Scholar]
- 50.Belser JA, Davis CT, Balish A, Edwards LE, Zeng H, Maines TR, Gustin KM, Martinez IL, Fasce R, Cox NJ, Katz JM, Tumpey TM. 2013. Pathogenesis, transmissibility, and ocular tropism of a highly pathogenic avian influenza A (H7N3) virus associated with human conjunctivitis. J Virol 87:5746–5754. doi: 10.1128/JVI.00154-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Belser JA, Blixt O, Chen LM, Pappas C, Maines TR, Van HN, Donis R, Busch J, McBride R, Paulson JC, Katz JM, Tumpey TM. 2008. Contemporary North American influenza H7 viruses possess human receptor specificity: implications for virus transmissibility. Proc Natl Acad Sci U S A 105:7558–7563. doi: 10.1073/pnas.0801259105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kurtz J, Manvell RJ, Banks J. 1996. Avian influenza virus isolated from a woman with conjunctivitis. Lancet 348:901–902. doi: 10.1016/S0140-6736(05)64783-6. [DOI] [PubMed] [Google Scholar]
- 53.Koopmans M, Wilbrink B, Conyn M, Natrop G, van der Nat H, Vennema H, Meijer A, van SJ, Fouchier R, Osterhaus A, Bosman A. 2004. Transmission of H7N7 avian influenza A virus to human beings during a large outbreak in commercial poultry farms in the Netherlands. Lancet 363:587–593. doi: 10.1016/S0140-6736(04)15589-X. [DOI] [PubMed] [Google Scholar]
- 54.Fouchier RA, Schneeberger PM, Rozendaal FW, Broekman JM, Kemink SA, Munster V, Kuiken T, Rimmelzwaan GF, Schutten M, Van Doornum GJ, Koch G, Bosman A, Koopmans M, Osterhaus AD. 2004. Avian influenza A virus (H7N7) associated with human conjunctivitis and a fatal case of acute respiratory distress syndrome. Proc Natl Acad Sci U S A 101:1356–1361. doi: 10.1073/pnas.0308352100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Qi Y, Fan H, Qi X, Zhu Z, Guo X, Chen Y, Ge Y, Zhao K, Wu T, Li Y, Shan Y, Zhou M, Shi Z, Wang H, Cui L. 2014. A novel pyrosequencing assay for the detection of neuraminidase inhibitor resistance-conferring mutations among clinical isolates of avian H7N9 influenza virus. Virus Res 179:119–124. doi: 10.1016/j.virusres.2013.10.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Wu Y, Bi Y, Vavricka CJ, Sun X, Zhang Y, Gao F, Zhao M, Xiao H, Qin C, He J, Liu W, Yan J, Qi J, Gao GF. 2013. Characterization of two distinct neuraminidases from avian-origin human-infecting H7N9 influenza viruses. Cell Res 23:1347–1355. doi: 10.1038/cr.2013.144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Gubareva LV, Matrosovich MN, Brenner MK, Bethell RC, Webster RG. 1998. Evidence for zanamivir resistance in an immunocompromised child infected with influenza B virus. J Infect Dis 178:1257–1262. doi: 10.1086/314440. [DOI] [PubMed] [Google Scholar]
- 58.Nguyen HT, Fry AM, Gubareva LV. 2012. Neuraminidase inhibitor resistance in influenza viruses and laboratory testing methods. Antivir Ther 17:159–173. doi: 10.3851/IMP2067. [DOI] [PubMed] [Google Scholar]
- 59.Boltz DA, Douangngeun B, Phommachanh P, Sinthasak S, Mondry R, Obert C, Seiler P, Keating R, Suzuki Y, Hiramatsu H, Govorkova EA, Webster RG. 2010. Emergence of H5N1 avian influenza viruses with reduced sensitivity to neuraminidase inhibitors and novel reassortants in Lao People's Democratic Republic. J Gen Virol 91:949–959. doi: 10.1099/vir.0.017459-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Abed Y, Baz M, Boivin G. 2009. A novel neuraminidase deletion mutation conferring resistance to oseltamivir in clinical influenza A/H3N2 virus. J Infect Dis 199:180–183. doi: 10.1086/595736. [DOI] [PubMed] [Google Scholar]
- 61.Abed Y, Baz M, Boivin G. 2006. Impact of neuraminidase mutations conferring influenza resistance to neuraminidase inhibitors in the N1 and N2 genetic backgrounds. Antivir Ther 11:971–976. [PubMed] [Google Scholar]
- 62.Pizzorno A, Bouhy X, Abed Y, Boivin G. 2011. Generation and characterization of recombinant pandemic influenza A(H1N1) viruses resistant to neuraminidase inhibitors. J Infect Dis 203:25–31. doi: 10.1093/infdis/jiq010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Zurcher T, Yates PJ, Daly J, Sahasrabudhe A, Walters M, Dash L, Tisdale M, McKimm-Breschkin JL. 2006. Mutations conferring zanamivir resistance in human influenza virus N2 neuraminidases compromise virus fitness and are not stably maintained in vitro. J Antimicrob Chemother 58:723–732. doi: 10.1093/jac/dkl321. [DOI] [PubMed] [Google Scholar]
- 64.Okomo-Adhiambo M, Demmler-Harrison GJ, Deyde VM, Sheu TG, Xu X, Klimov AI, Gubareva LV. 2010. Detection of E119V and E119I mutations in influenza A (H3N2) viruses isolated from an immunocompromised patient: challenges in diagnosis of oseltamivir resistance. Antimicrob Agents Chemother 54:1834–1841. doi: 10.1128/AAC.01608-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Varghese JN, Smith PW, Sollis SL, Blick TJ, Sahasrabudhe A, McKimm-Breschkin JL, Colman PM. 1998. Drug design against a shifting target: a structural basis for resistance to inhibitors in a variant of influenza virus neuraminidase. Structure 6:735–746. doi: 10.1016/S0969-2126(98)00075-6. [DOI] [PubMed] [Google Scholar]
- 66.Yen HL, Herlocher LM, Hoffmann E, Matrosovich MN, Monto AS, Webster RG, Govorkova EA. 2005. Neuraminidase inhibitor-resistant influenza viruses may differ substantially in fitness and transmissibility. Antimicrob Agents Chemother 49:4075–4084. doi: 10.1128/AAC.49.10.4075-4084.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Yen HL, Hoffmann E, Taylor G, Scholtissek C, Monto AS, Webster RG, Govorkova EA. 2006. Importance of neuraminidase active-site residues to the neuraminidase inhibitor resistance of influenza viruses. J Virol 80:8787–8795. doi: 10.1128/JVI.00477-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Hurt AC, Lowther S, Middleton D, Barr IG. 2010. Assessing the development of oseltamivir and zanamivir resistance in A(H5N1) influenza viruses using a ferret model. Antivir Res 87:361–366. doi: 10.1016/j.antiviral.2010.06.009. [DOI] [PubMed] [Google Scholar]
- 69.Ho HT, Hurt AC, Mosse J, Barr I. 2007. Neuraminidase inhibitor drug susceptibility differs between influenza N1 and N2 neuraminidase following mutagenesis of two conserved residues. Antivir Res 76:263–266. doi: 10.1016/j.antiviral.2007.08.002. [DOI] [PubMed] [Google Scholar]
- 70.Wang MZ, Tai CY, Mendel DB. 2002. Mechanism by which mutations at his274 alter sensitivity of influenza a virus n1 neuraminidase to oseltamivir carboxylate and zanamivir. Antimicrob Agents Chemother 46:3809–3816. doi: 10.1128/AAC.46.12.3809-3816.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Nguyen HT, Sheu TG, Mishin VP, Klimov AI, Gubareva LV. 2010. Assessment of pandemic and seasonal influenza A (H1N1) virus susceptibility to neuraminidase inhibitors in three enzyme activity inhibition assays. Antimicrob Agents Chemother 54:3671–3677. doi: 10.1128/AAC.00581-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.van d V, Veldhuis Kroeze EJ, Stittelaar KJ, Linster M, Van der Linden A, Schrauwen EJ, Leijten LM, van AG, Schutten M, Kuiken T, Osterhaus AD, Fouchier RA, Boucher CA, Herfst S. 2011. Multidrug resistant 2009 A/H1N1 influenza clinical isolate with a neuraminidase I223R mutation retains its virulence and transmissibility in ferrets. PLoS Pathog 7:e1002276. doi: 10.1371/journal.ppat.1002276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Eshaghi A, Patel SN, Sarabia A, Higgins RR, Savchenko A, Stojios PJ, Li Y, Bastien N, Alexander DC, Low DE, Gubbay JB. 2011. Multidrug-resistant pandemic (H1N1) 2009 infection in immunocompetent child. Emerg Infect Dis 17:1472–1474. doi: 10.3201/eid1708.102004. [DOI] [PMC free article] [PubMed] [Google Scholar]