Abstract
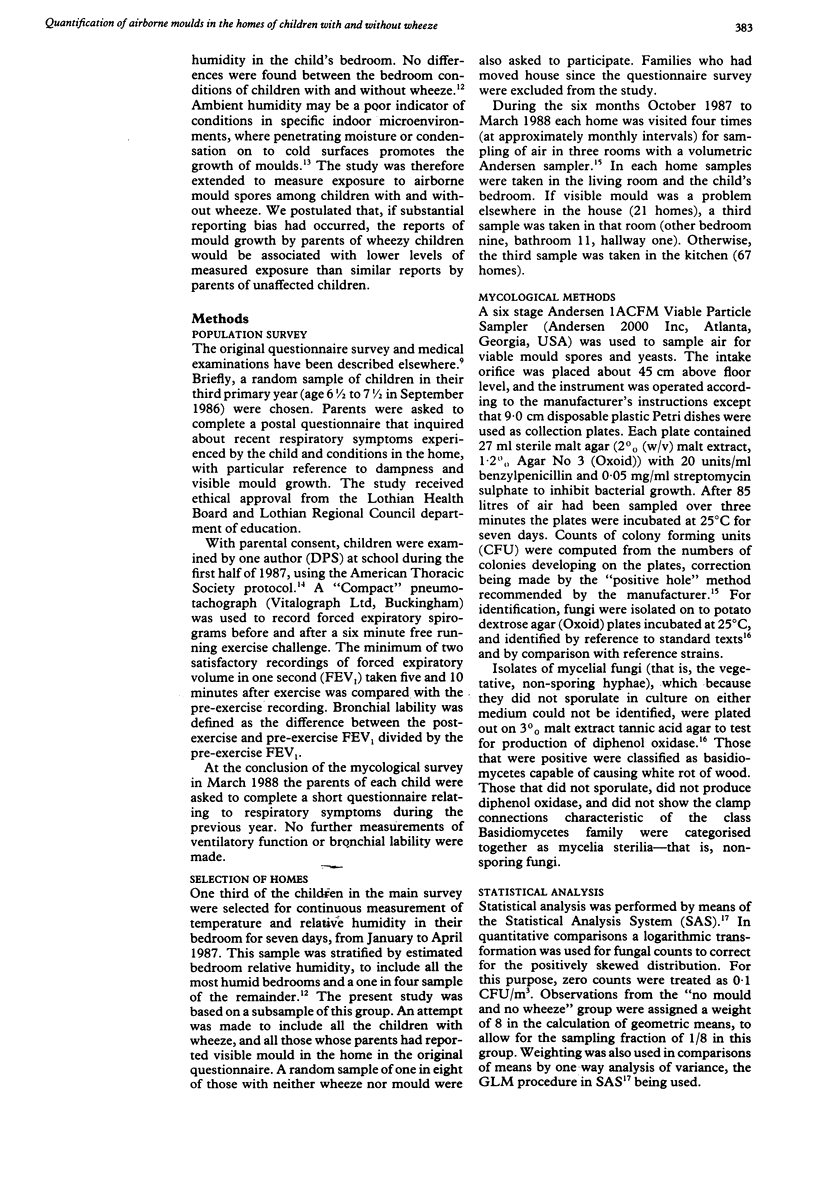
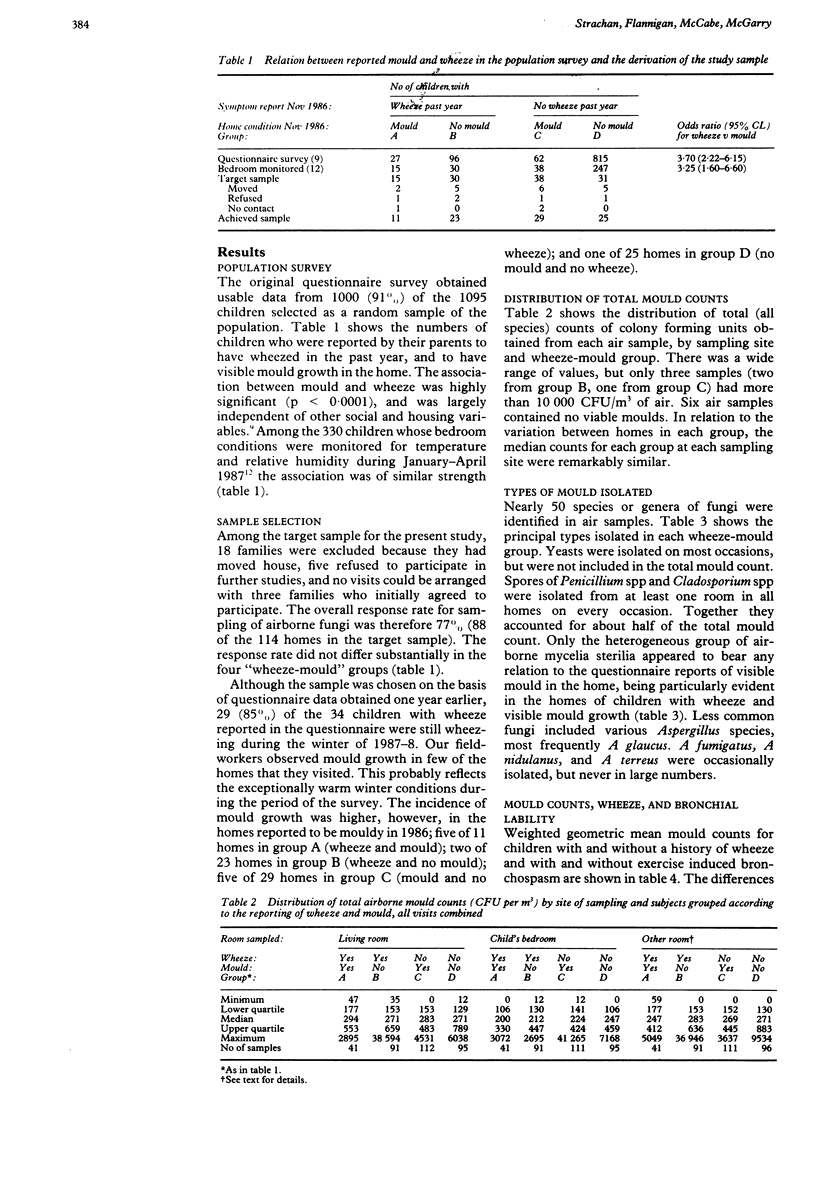
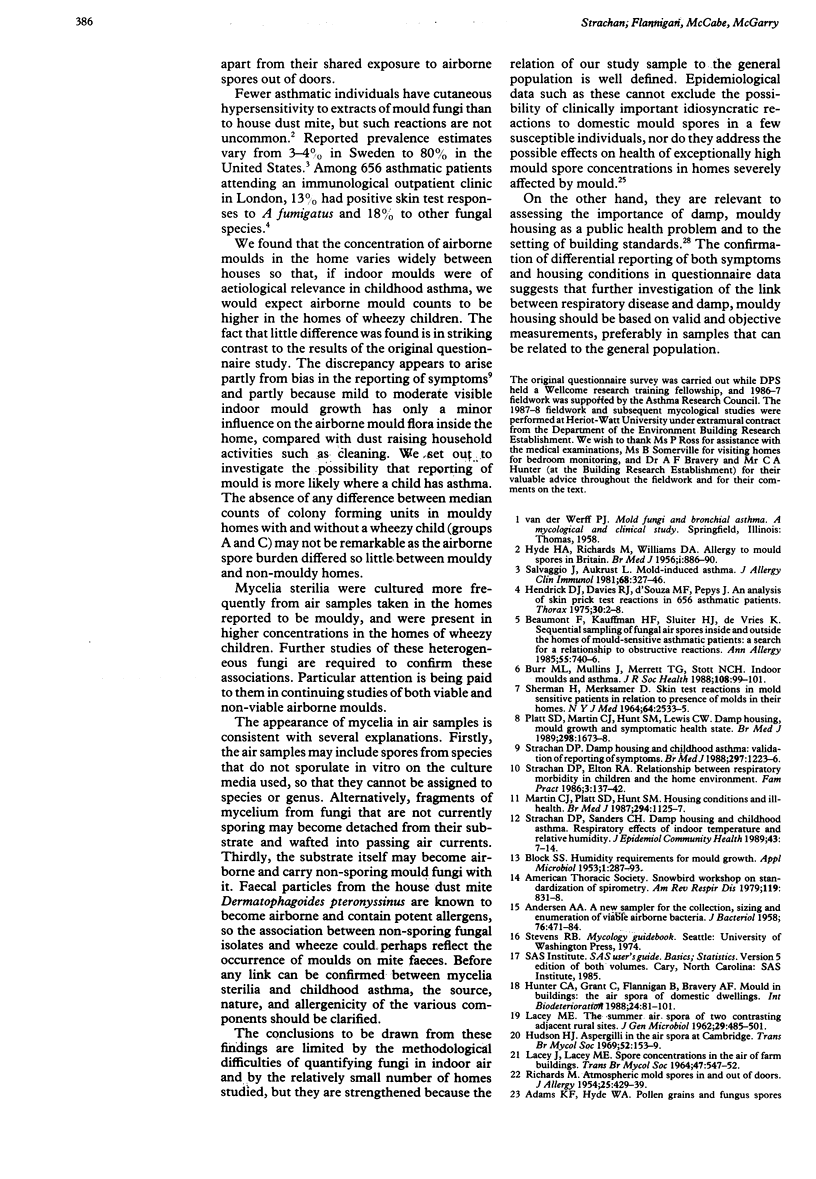
A population survey of 1000 7 year old children found a significant excess of wheeze among children whose homes were reported to be mouldy (odds ratio 3.70, 95% confidence limits 2.22, 6.15). The airborne mould flora was quantified by repeated volumetric sampling during the winter in three rooms of the homes of 88 children. All of these had previously completed spirometric tests before and after a six minute free running exercise challenge. Total airborne mould counts varied from 0 to 41,000 colony forming units (CFU)/m3, but were generally in the range 50-1500 CFU/m3, much lower than the concentrations found outdoors in summer. The principal types of fungi identified are all known to be common out of doors, and most were found on at least one occasion in most of the homes. Median and geometric mean total mould counts were not related to reports of visible mould in the home, or to a history of wheeze in the index child. The heterogeneous group of non-sporing fungi (mycelia sterilia) were the only airborne fungi present at significantly higher concentrations in the homes of wheezy children (geometric mean 2.1 v 0.7 CFU/m3. A non-significant increase in total mould counts was observed in the homes of children with a 10% or greater decline in FEV1 after exercise (geometric mean 354 v 253 CFU/m3). Questionnaire reports of mould in the home may be a poor indicator of exposure to airborne spores. The total burden of inhaled mould spores from indoor sources is probably not an important determinant of wheeze among children in the general population. Although the association with mycelia sterilia could be a chance finding, these non-sporing isolates may include a potent source of allergen.
Full text
PDF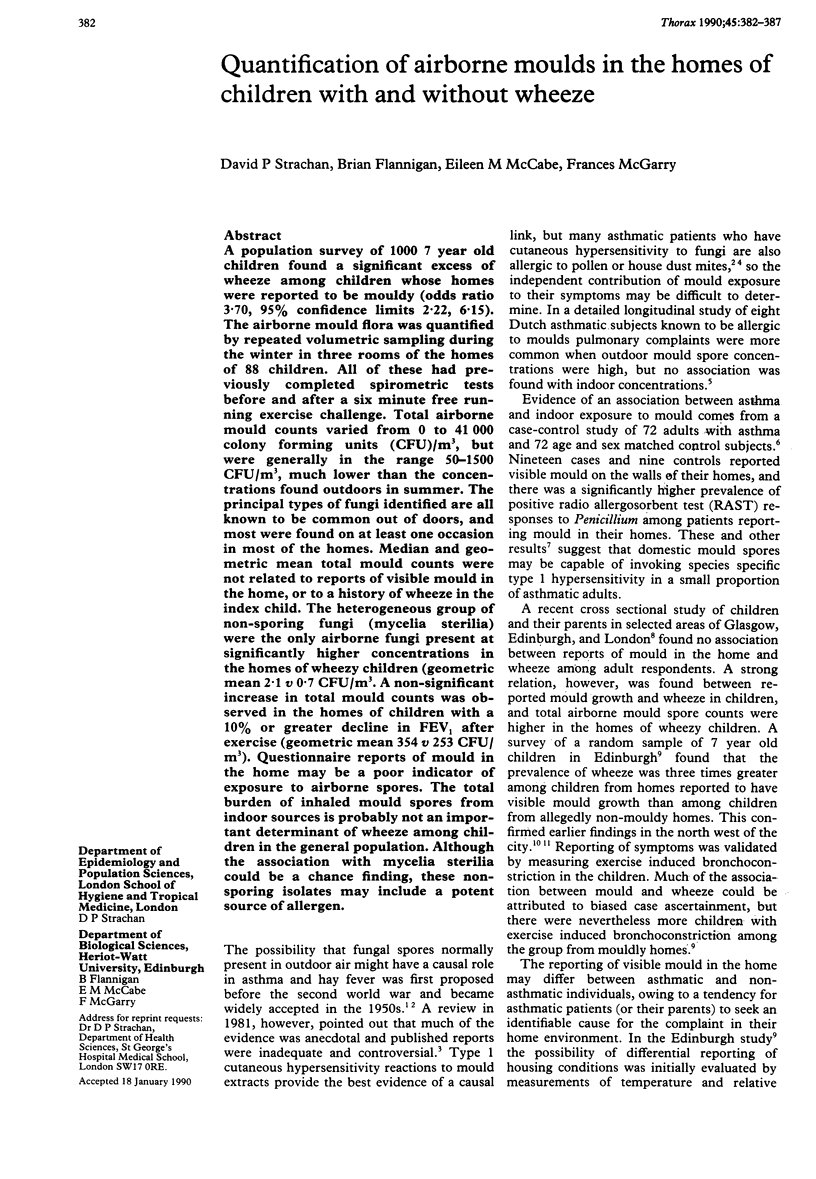


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- ANDERSEN A. A. New sampler for the collection, sizing, and enumeration of viable airborne particles. J Bacteriol. 1958 Nov;76(5):471–484. doi: 10.1128/jb.76.5.471-484.1958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- BLOCK S. S. Humidity requirements for mold growth. Appl Microbiol. 1953 Nov;1(6):287–293. doi: 10.1128/am.1.6.287-293.1953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beaumont F., Kauffman H. F., Sluiter H. J., De Vries K. Sequential sampling of fungal air spores inside and outside the homes of mould-sensitive, asthmatic patients: a search for a relationship to obstructive reactions. Ann Allergy. 1985 Nov;55(5):740–746. [PubMed] [Google Scholar]
- Beaumont F., Kauffman H. F., de Monchy J. G., Sluiter H. J., de Vries K. Volumetric aerobiological survey of conidial fungi in the North-East Netherlands. II. Comparison of aerobiological data and skin tests with mould extracts in an asthmatic population. Allergy. 1985 Apr;40(3):181–186. doi: 10.1111/j.1398-9995.1985.tb00214.x. [DOI] [PubMed] [Google Scholar]
- Burr M. L., Mullins J., Merrett T. G., Stott N. C. Indoor moulds and asthma. J R Soc Health. 1988 Jun;108(3):99–101. doi: 10.1177/146642408810800311. [DOI] [PubMed] [Google Scholar]
- HYDE H. A., RICHARDS M., WILLIAMS D. A. Allergy to mould spores in Britain. Br Med J. 1956 Apr 21;1(4972):886–890. doi: 10.1136/bmj.1.4972.886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hendrick D. J., Davies R. J., D'Souza M. F., Pepys J. An analysis of skin prick test reactions in 656 asthmatic patients. Thorax. 1975 Feb;30(1):2–8. doi: 10.1136/thx.30.1.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LACEY M. E. The summer air-spora of two contrasting adjacent rural sites. J Gen Microbiol. 1962 Nov;29:485–501. doi: 10.1099/00221287-29-3-485. [DOI] [PubMed] [Google Scholar]
- Martin C. J., Platt S. D., Hunt S. M. Housing conditions and ill health. Br Med J (Clin Res Ed) 1987 May 2;294(6580):1125–1127. doi: 10.1136/bmj.294.6580.1125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palmgren U., Ström G., Blomquist G., Malmberg P. Collection of airborne micro-organisms on Nuclepore filters, estimation and analysis--CAMNEA method. J Appl Bacteriol. 1986 Nov;61(5):401–406. doi: 10.1111/j.1365-2672.1986.tb04303.x. [DOI] [PubMed] [Google Scholar]
- Platt S. D., Martin C. J., Hunt S. M., Lewis C. W. Damp housing, mould growth, and symptomatic health state. BMJ. 1989 Jun 24;298(6689):1673–1678. doi: 10.1136/bmj.298.6689.1673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- RICHARDS M. Atmospheric mold spores in and out of doors. J Allergy. 1954 Sep;25(5):429–439. doi: 10.1016/0021-8707(54)90007-6. [DOI] [PubMed] [Google Scholar]
- SHERMAN H., MERKSAMER D. SKIN TEST REACTIONS IN MOLD-SENSITIVE PATIENTS IN RELATION TO PRESENCE OF MOLDS IN THEIR HOMES. N Y State J Med. 1964 Oct 15;64:2533–2535. [PubMed] [Google Scholar]
- Salvaggio J., Aukrust L. Postgraduate course presentations. Mold-induced asthma. J Allergy Clin Immunol. 1981 Nov;68(5):327–346. doi: 10.1016/0091-6749(81)90131-7. [DOI] [PubMed] [Google Scholar]
- Strachan D. P. Damp housing and childhood asthma: validation of reporting of symptoms. BMJ. 1988 Nov 12;297(6658):1223–1226. doi: 10.1136/bmj.297.6658.1223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strachan D. P., Elton R. A. Relationship between respiratory morbidity in children and the home environment. Fam Pract. 1986 Sep;3(3):137–142. doi: 10.1093/fampra/3.3.137. [DOI] [PubMed] [Google Scholar]
- Strachan D. P., Sanders C. H. Damp housing and childhood asthma; respiratory effects of indoor air temperature and relative humidity. J Epidemiol Community Health. 1989 Mar;43(1):7–14. doi: 10.1136/jech.43.1.7. [DOI] [PMC free article] [PubMed] [Google Scholar]


