Abstract
Modern medical management of comorbid conditions has resulted in escalating use of multiple medications and the emergence of the twin phenomena of multimorbidity and polypharmacy. Current understanding of how the polypharmacy in conjunction with multimorbidity influences trauma outcomes is limited, although it is known that trauma patients are at increased risk for medication-related adverse events. The comorbidity-polypharmacy score (CPS) is a simple clinical tool that quantifies the overall severity of comorbidities using the polypharmacy as a surrogate for the “intensity” of treatment necessary to adequately control chronic medical conditions. Easy to calculate, CPS is derived by counting all known pre-injury comorbid conditions and medications. CPS has been independently associated with mortality, increased risk for complications, lower functional outcomes, readmissions, and longer hospital stays. In addition, CPS may help identify older trauma patients at risk of post-emergency department undertriage. The goal of this article was to review and refine the rationale for CPS and to provide an evidence-based outline of its potential clinical applications.
Keywords: Comorbidity-polypharmacy score, elderly trauma patient, estimation of frailty, multimorbidity, physiologic age, public health, world demographics
INTRODUCTION
As powerful megatrends rapidly alter the world's demographics, the number of older (≥45 years) patients in the global population is increasing, as is the proportion of patients from this age group seen at trauma centers.[1,2] Continuously evolving sophistication of modern management of chronic medical conditions has resulted in escalating simultaneous use of multiple medications and the emergence of the phenomenon of polypharmacy.[3,4] Current understanding of how polypharmacy in conjunction with comorbidities may influence trauma outcomes is limited, but there is a growing body of evidence suggesting that older trauma patients are at increased risk for medication-related adverse events,[5,6,7,8] increased overall complications,[3,4,8,9] hospital readmission,[10] and mortality.[3,11]
In the era of medication reconciliation,[3,12] the comorbidity-polypharmacy score (CPS) can easily be calculated and has been proposed as an adjunct for outcome prediction, triage, and discharge planning in the injured patient population.[3,8,9,13] CPS may function as an objective measure of the “cumulative severity” of all comorbid conditions, and thus, a reflection of the patient's “physiologic age.” Early evidence suggests that triage strategies focusing solely on patient chronologic age are imperfect, and adding surrogates of “physiologic age” to the existing models may improve their overall predictive accuracy.[14] Retrospective studies have shown that CPS may help in identification of older trauma patients at risk for poor outcomes and those who are more likely to require additional resources at discharge;[8,9] however, data currently have not yet been published that prospectively validate the utility of CPS and its proposed benefits in enhancing patient outcomes or resource allocation, as consistent with the value-based healthcare paradigm.[15]
THE OLDER TRAUMA PATIENT
Life expectancy in most regions of the world has steadily risen over the past decades (76.2 years for men and 81.1 years for women in 2010), and there is a parallel increase in the size of older population segments (ages 45 years and older).[16,17] Between 2030 and 2051, the proportion of adults ages 40-64 will increase to over 30% of the total population, with the segment including those ≥65 years growing to represent nearly 20% of the population.[17,18,19] These population trends are the direct result of successful innovation and progress in medicine, better access to high-quality care, and availability of ever more effective drugs and pharmaceutical regimens for the management of chronic medical conditions.[3,4,20,21,22] With increasing life expectancy, the prevalence of commonly encountered chronic medical conditions such as hypertension, heart disease, cancer, and diabetes mellitus will likely follow suit.[23,24] As the life expectancy of patients with “multi-comorbidities” increases, the severity (and complexity) of the disease burden increases and patients tend to require co-administration of additional drugs.[22] Traumatic injury is currently among the top five causes of mortality in the US, and seems to disproportionately affect those over age 65.[16] Chronic conditions such as morbid obesity, osteoarthritis, and osteoporosis act synergistically with the phenomena of progressive loss of vision and hearing, impaired balance, and impaired reflexes to cumulatively elevate the risk of injury following seemingly minor traumatic mechanisms in the older patient.[25,26,27,28,29] As general survival in elderly population improves, we are witnessing a trend toward more trauma-related deaths in this population segment.
It has been observed that the contemporary aging individual is much more likely to remain both physically active and productive within the society.[30,31] As these trends converge, it is assumed that active older adults with more comorbidities are bound to visit trauma centers in increasing numbers.[32] There are numerous opinions with respect to the effects of age as an independent predictor of trauma outcomes.[33,34,35,36] Various authors have observed that older trauma patients may succumb to relatively minor injuries that would not be considered life threatening in younger patients, and age itself continues to be an independent predictor of trauma mortality.[3,37,38] Since “chronological age” may not correlate well with “physiological age,”[39,40] it is not surprising that the definitions of older adult use lower bounds ranging from 45 to 75 years of age.[41,42] Based on previously published observations,[4,5,9,13,22] our multi-center group studying the CPS elected to include patients aged 45 years and older. Although some may object to age 45 being considered “older,”[42] that particular age threshold represents the closest estimate of the youngest patient group with an evident increase in the number of chronic health conditions requiring long-term “maintenance” pharmacologic therapy.[22,43] CPS has not been the only attempt at estimating “physiologic age;” the Charlson comorbidity index, the Elixhauser Scoring System, and various other combinations of clinical and lab parameters have been used to attempt predict outcomes in trauma patients.[11,44,45,46,47] While quantification of functional status in geriatric patients has been shown to be effective in predicting outcomes in elective surgery, its utility in trauma patients remains limited.[48]
COMORBIDITIES IN THE OLDER PATIENT
Knowledge of pre-existing comorbid conditions can facilitate assessment of the overall health status of an older trauma patient or the so-called “physiologic age.”[49,50,51] More than half of the geriatric trauma population experience hypertension or some other form of “cardiovascular disease”.[52,53,54,55] Physiologic and functional differences among older adults combined with the overall severity of co-morbid conditions may contribute, directly or indirectly, to complications during the treatment and recovery phases following traumatic injury.[35,51,56] The effect of comorbid conditions on outcomes has been examined extensively in the trauma literature.[35,39,40,57] In fact, the presence of just one comorbidity was associated with greater mortality risk in trauma patients aged 65 years and older.[58] There are also data pointing toward preexisting cardiac disease as a risk factor for posttraumatic mortality.[5,59,60] Interestingly, obesity may be a risk factor for trauma mortality among older trauma patients in some studies but not in others.[27,28] Intimately related to the presence of “multi-comorbidities” is the associated phenomenon of polypharmacy.[3,4,22]
POLYPHARMACY
Polypharmacy has generally been defined as concurrent administration of more than 5 medications, but this definition is not standardized, and various iterations of it are observed in the literature.[22,61] The above inconsistency may be a reflection of the lack of evidence for any specific number of co-administered drugs correlating with any particular risks and/or adverse drug events.[62] Nevertheless, polypharmacy literature describes many potential hazards related to the simultaneous use of multiple medications in the middle age and elderly populations.[5,63,64] Some of the major risks related to polypharmacy include adverse drug reactions and interactions, occurrence of syndromic manifestations (e.g., delirium, falls, vertigo), underprescribing of recommended drugs (e.g., the “treatment risk paradox”), unintended medication errors, poor patient adherence, cognitive and functional decline, and increased need for healthcare utilization with associated greater costs and higher mortality.[63,65] For example, combinations of narcotics and benzodiazepines have been associated with worse patient outcomes.[66]
Some evidence suggests that there is an association between combined comorbidities and polypharmacy and worse trauma outcomes, despite poor correlations between mortality, and polypharmacy or comorbidities in isolation.[4] As stated above, this may be a reflection of the observation that increasing levels of polypharmacy may be reflective of the overall severity of the underlying comorbid conditions,[8,67] yet the combined effect of comorbidities with polypharmacy on trauma outcomes has not been studied to the same extent that each of its individual sub-components has been scrutinized.
COMORBIDITY-POLYPHARMACY SCORE
The CPS was designed to be an easy-to-use assessment of the synergistic impact of a patient's comorbidities and the intensity of medical treatment required to manage these respective comorbidities.[4] Defined as the simple sum of the number of pre-injury medications (prescription and over-the-counter) and all known comorbidities (including medical, psychiatric, and substance abuse), the CPS assigns 1 point to each prehospital medication and each prehospital comorbidity.[3,9,13] Severity of CPS has been traditionally stratified as mild (CPS 0-7), moderate (8-14),[8,9,10,11,12,13,14] severe (15-21),[15,16,17,18,19,20,21] and morbid (≥22 points).[3]
Outcomes research examining CPS as an independent predictor of mortality and morbidity has utilized multivariate models with CPS, ISS, and age as independent variables.[3,8,9,11] Older trauma patients with a CPS >15 appear at greater risk for mortality, complications, and longer hospital and ICU stays [Table 1 and Figure 1].[3,11] Greater CPS “severity” has also been associated with increased need for transfusion during the first 24 h following injury and lower functional outcomes at discharge.[3] The latter finding closely relates to the fact that the discharge to a nursing or rehabilitation facility instead of home was also significantly more likely among patients with higher CPS scores [Table 1].[3,11] Finally, the independent association between CPS and 30-day hospital readmission carries important implications in the new paradigm of value-based healthcare,[10] where prediction and avoidance of complications and hospital readmissions will be increasingly rewarded over the traditional “high volume, high revenue” paradigm.[68] Overall, the current understanding of how the polypharmacy and multi-morbidity affect trauma outcomes continues to be limited despite the fact that trauma patients may be more likely to experience adverse consequences related to medications than non-trauma patients.[69,70] Recently published evidence also points to the possibility that previously undefined interactions between common medication classes may have the ability to modulate outcomes in older trauma patients.[5] Many of these medication-related side effects and previously unknown synergistic drug-drug interactions are more likely to come to light as research in this important area advances thanks to greater awareness as well as a number of patient safety initiatives such as the requirement for medication reconciliation, as mandated by the Joint Commission.[3]
Table 1.
Composite of patient characteristics and key clinical outcomes grouped according to CPS severity; data presented as corresponding ranges for two major published studies (Evans, et al. J Am Geriatr Soc 2012;60:1465. Holmes, et al. J Am Coll Surg 2014;219:631)
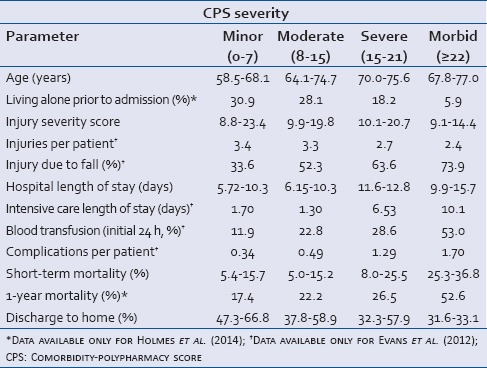
Figure 1.
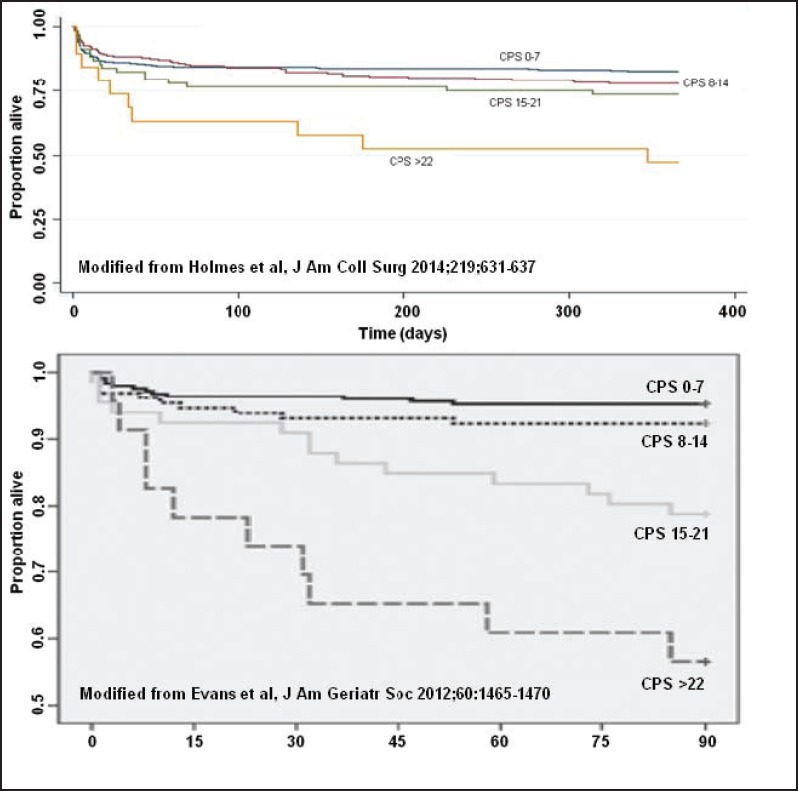
Survival plots for older trauma patients based on comorbidity-polypharmacy score (CPS) severity: (Top) Data from Holmes et al. demonstrates survival differences based on CPS strata up to 1-year post-injury. (Bottom) Similarly, stratified data from Evans et al. show survival differences during the first 90 days post-injury
CHARLSON SCORING SYSTEM
The Charlson Scoring System (CSS) and a number of associated modifications have also been used in assessing the role of comorbid conditions in predicting patient outcomes.[71,72,73,74] The calculation of CSS involves a procedure that requires the identification of several specific comorbid conditions, scoring each according to pre-determined point weights, and adding additional predefined points for the patient's age group.[72,73] More importantly, the Charlson score does not take into account the individualized disease severity for the patient's many comorbidities. For example, a patient with advanced rheumatoid arthritis, whose mobility (and thus post-injury recovery) is severely limited by that condition, would receive a score of “1” under the Charlson category of “Connective Tissue Disease.”[46,71,73] The same can be said for essentially every condition included in the CSS – the quantification of disease severity is limited. In addition, as Holmes et al.[11] properly describe in their article, the Charlson index's categorization of relative disease severity is dated. For example HIV/AIDS, devastating and rightly deserving of a “6” weighting when Charlson's paper was first published in 1987, is now a very manageable, chronic condition that very likely does not deserve the “most severe” designation as long as it is medically controlled.[75,76] Similarly, the weighting provided for different ages in the Charlson index is fixed, while it may be argued that patients considered “very old” as recently as 20 years ago are more commonly healthy and active now than at any other time in human history. Furthermore, the Charlson index was originally intended for predicting mortality in a narrowly defined, relatively small cohort of patients.[77] Despite the bias associated with its early development, the CSS has since been successfully applied to claims data, in-hospital mortality, use of blood products, lengths of hospital stay, discharges, and to predict short-term outcomes.[74,78,79,80] The CSS incorporates “age range” within its overall modeling, contributing to somewhat “muddy” results, especially when the CSS itself is included in further multivariable analyses that introduce age as another variable. Sound statistical principles dictate that multivariate analyses should not include an independent variable that is also “embedded” within another variable. In comparative analyses, both CPS and CSS are very close in their estimation of outcome prediction.[11] Predictive differences between the CPS and CSS are small and each of the two scores can be fairly said to be able to stand on its own. Regarding the applicability of this in an acute trauma setting, Figure 2 demonstrates how a simple bivariate model incorporating only ISS and CPS outperforms a model containing CSS, ISS, patient age, and the presence of hypotension on the initial Emergency Department (ED) evaluation.
Figure 2.
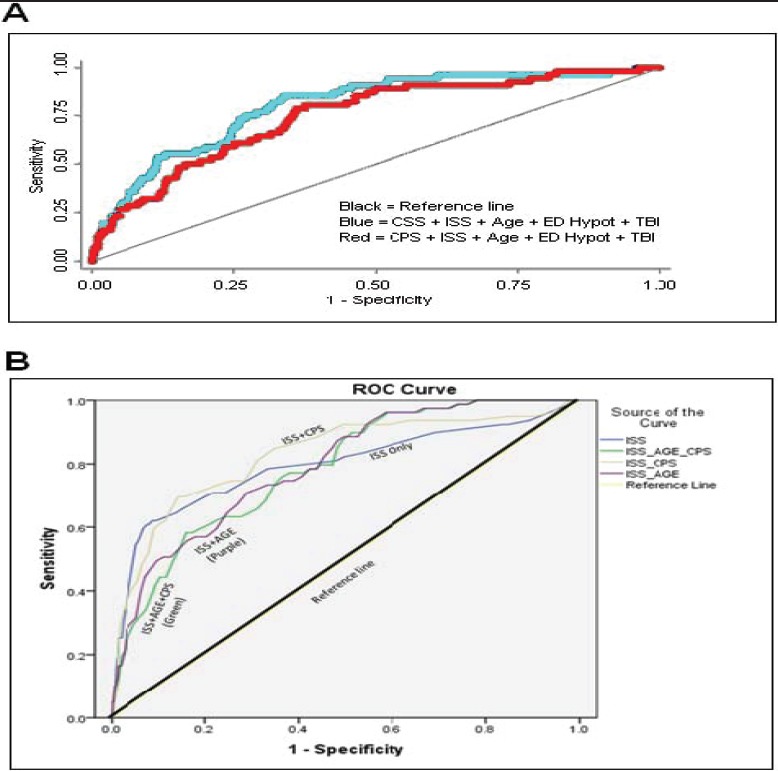
Comparison of receiver operating characteristic (ROC) curves from two independent studies of the comorbidity-polypharmacy score (CPS). Part (A) shows the comparison of ROC curves for models incorporating CPS (red) versus Charlson Scoring System (blue) for in-hospital mortality area under curve (AUC = 0.75 vs. 0.80, respectively; P = 0.02, modified from Holmes et al., J Am Coll Surg, 2014;219(4):631). Part (B) shows the comparison of ROC curves for in-hospital mortality from a post hoc, previously unpublished, secondary analysis of 5,580 older trauma patients for ISS alone (AUC = 0.79), ISS+CPS (AUC = 0.83), ISS + AGE (AUC = 0.79), and ISS + AGE + CPS (AUC = 0.78, all, P < 0.01). As evident from the above comparisons, ISS in combination with CPS provides the best predictive model for in-hospital mortality among older trauma patients
ELIXHAUSER SCORING SYSTEM
Elixhauser et al.[77] developed an approach to use comorbidity data in conjunction with administrative data to aid in outcome prediction. This group pioneered an approach that started by identifying five key concepts related to a patient's hospitalization:
The primary reason for hospitalization,
The severity of the principal diagnosis,
Complications of care,
Unimportant or unrelated comorbidities that are present on admission, but do not impact resources, and
Important comorbidities/conditions not related to the reason for admission, but which may impact resources or cause a poor outcome.[77]
Elixhauser's team was subsequently able to identify and develop 30 comorbidity measures that were significantly associated with greater hospital lengths of stay, higher hospital charges, and elevated mortality.[77] The group's argument was based on assumptions that:
Complications and comorbidities may be difficult to differentiate;
Better outcome prediction can be achieved when certain additional comorbidities (not considered in the CSS) are incorporated into the model; and
Certain conditions or comorbidities considered to be unrelated to outcome are eliminated from the model.[77]
Consequently, both the CSS and the Elixhauser methodologies may contain difficult-to-quantify biases, leading to both significant controversy and long-standing academic discussions.
A number of studies during the past decade were undertaken in order to better understand and to resolve the differences between the CSS and the Elixhauser method. Some authors have indicated that any kind of scoring system performs well if used with “local coding and diagnostic practices,” with both CSS and the Elixhauser index performing comparably well.[81] Austin et al.[44] concluded that summary comorbidity measures as opposed to individual measures are more effective, but are only as good as the variables used to create the index. Southern et al.[46] found that the Elixhauser score performed better than CSS when looking at acute myocardial infarctions in Canada, likely due to the Elixhauser formula's ability to better focus on individual contributing variables and the lack of reliance on weighted scoring. Finally, modified or combined scoring systems or indices may be helpful, especially in the elderly.[45,82]
TRIAGE AND EVALUATION OF THE OLDER TRAUMA PATIENT
Risk stratification of older injured patients begins with pre-hospital triage to appropriately equipped trauma hospitals and continues during the initial patient evaluation that takes place after the patient arrives to the trauma resuscitation area.[83,84] Older trauma patients currently account for approximately one-fourth of trauma fatalities but are less likely to be appropriately triaged to trauma centers.[85] Even after their arrival at the ED, post-ED triage of older trauma patients continues to be challenging, as morbidity and mortality associated with any given level of injury severity tend to escalate with age.[86] Given equivalent injury severity, mortality in elderly patients is known to be substantially greater than in younger patients.[33] In spite of this, older patients are known to be more likely undertriaged compared with other trauma victims.[87,88,89] Undertriage predisposes patients to critical delays in diagnostic, resuscitative, and therapeutic measures.[90] A recent study of over 700 older trauma patients demonstrated that there was a significant association between CPS levels and the likelihood of undertriage based on lack of recognition of the patient frailty.[13] In fact, CPS was significantly higher in patients that were undertriaged, as defined by the need for unanticipated transfer to a higher level of care within 24 h of admission, even after adjusting for ISS scores.[13] The study by Justiniano et al.[13] was consistent with previous reporting that undertriage was significantly associated with greater morbidity, mortality, and the likelihood of discharge to a facility.[91] One noticeable limitation of the study by Justiniano et al.[13] is that it could not prove that CPS predicted undertriage independently of age; however, given that unconscious age bias by receiving trauma teams has been previously identified as a possible cause of undertriage,[91] CPS could function as a more objective decision-guiding tool than some of the currently utilized criteria.
LIMITATIONS, CONTROVERSIES, AND FUTURE DIRECTIONS
The CSS, the CPS, and the Elixhauser score all are subject to important biases in the acute trauma setting. Perhaps the greatest challenge to “frailty score” implementation is the reporting bias regarding comorbidities and pre-injury medications. Although wider implementation of electronic medical records (EMR) may help in this domain, it would not be surprising that the initial estimation of such scores must be taken with some skepticism due to the high probability of incomplete initial information. Yet, despite the lack of initial knowledge of every patient's comorbid conditions and/or medications, both assessment systems demonstrate reasonably accurate prediction of outcomes.[11] Consequently, the authors propose that these tools can be combined with other strategies such as modified geriatric trauma criteria to achieve the optimum predictive power and thus have the potential to positively affect and enhance care for the older injured patient.[14]
Recent work by Austin et al.[44] presents a good argument as to why comorbidity measures are utilitarian by presenting a mathematical model using SEER-Medicare data, suggesting that CPS-like models are necessary and in fact work. This is on the heels of work by Gangne et al.[45] indicating that a combination of comorbidity scoring systems, in this case, Charlson and Elixhauser, fares better in predicting mortality in the elderly than either score alone. Indeed, the authors’ argument is that CPS does just that. It provides the equivalent level of prediction through an innovative and simple approach. Further research in this area is clearly warranted, including current scientific efforts evaluating the applicability of CPS as a measure of frailty across all age groups. The CPS's independence of chronologic age as an included variable, simplicity of calculation, and ability to adapt to changing medical care by avoidance of fixed scoring systems may allow it to offer better insight into a patient's true “physiologic age” than the Charlson index or the Elixhauser score. A readily calculated and objective tool like CPS can help with early identification of older trauma patients who may be at risk for poorer outcomes and undertriage.[3,9,10,13] When properly validated and applied, such instrument could not only affect patient outcomes, but could also aid hospital staff in more appropriately deploying resources needed for effective discharge planning and readmission reduction.[9,10]
Our group continues related work and research in this critically important area of public health. Investigation is ongoing regarding the utilization of more advanced modeling approaches to predict patient outcomes. In this work, our team is using “intelligent” computational models and neural network methodologies that utilize readily available patient data from established electronic medical records (EMR) resources and turn this information into actionable, clinically useful information. In today's healthcare environment, there is great pressure to identify whether patients should receive inpatient or outpatient care (e.g., the “two-midnight rule”). The ultimate outcome of our work will be the development of an intelligent and automated system implementing these advanced modeling techniques to significantly improve allocation of healthcare resources, and to ensure that patients receive the appropriate level of safe, high-quality care.
CONCLUSION
As the global population ages, patients transported to trauma centers will be increasingly more likely to present with pre-injury multimorbidity and polypharmacy. The CPS, CSS, and the Elixhauser index are tools that trauma and emergency practitioners may employ to more accurately characterize the “frailty” or “physiological age” of a patient. The concurrent assessment of chronic health conditions and the associated “pre-existing disease burden” will become a necessity and will complement the traditional anatomic and physiologic assessment of the routine trauma patient evaluation. Prospective studies of CPS score as a tool to guide prehospital and Emergency Department triage, disposition planning, and other interventional strategies are warranted. There also may be a role for the implementation of CPS and other assessments of polypharmacy in injury prevention efforts, both within the community as a primary prevention strategy and in the hospital setting where major improvements in secondary prevention can be achieved to reduce the incidence of post-discharge deterioration or re-injury, and avoid readmissions. Eventually, computerized systems based on “intelligent algorithms” and neural network-based methodologies will be able to prospectively identify “at-risk” older trauma patients, recommend early intervention, and help formulate appropriate preventive strategies based on the associated level of frailty.
Footnotes
Source of Support: Nil.
Conflicts of Interest: None declared.
REFERENCES
- 1.High-tech approach to medication reconciliation saves time, bolsters safety at hospital in northern Virginia. ED Manag. 2011;23:117–9. [PubMed] [Google Scholar]
- 2.Lutz W, Sanderson W, Scherbov S. The coming acceleration of global population ageing. Nature. 2008;451:716–9. doi: 10.1038/nature06516. [DOI] [PubMed] [Google Scholar]
- 3.Evans DC, Cook CH, Christy JM, Murphy CV, Gerlach AT, Eiferman D, et al. Comorbidity-polypharmacy scoring facilitates outcome prediction in older trauma patients. J Am Geriatr Soc. 2012;60:1465–70. doi: 10.1111/j.1532-5415.2012.04075.x. [DOI] [PubMed] [Google Scholar]
- 4.Evans DC, Gerlach AT, Christy JM, Jarvis AM, Lindsey DE, Whitmill ML, et al. Pre-injury polypharmacy as a predictor of outcomes in trauma patients. Int J Crit Illn Inj Sci. 2011;1:104–9. doi: 10.4103/2229-5151.84793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wisler JR, Springer AN, Hateley K, Mo XM, Evans DC, Cook CH, et al. Pre-injury neuro-psychiatric medication use, alone or in combination with cardiac medications, may affect outcomes in trauma patients. J Postgrad Med. 2014;60:366–71. doi: 10.4103/0022-3859.143957. [DOI] [PubMed] [Google Scholar]
- 6.Hohl CM, Dankoff J, Colacone A, Afilalo M. Polypharmacy, adverse drug-related events, and potential adverse drug interactions in elderly patients presenting to an emergency department. Ann Emerg Med. 2001;38:666–71. doi: 10.1067/mem.2001.119456. [DOI] [PubMed] [Google Scholar]
- 7.Veehof LJ, Stewart RE, Meyboom-de Jong B, Haaijer-Ruskamp FM. Adverse drug reactions and polypharmacy in the elderly in general practice. Eur J Clin Pharmacol. 1999;55:533–6. doi: 10.1007/s002280050669. [DOI] [PubMed] [Google Scholar]
- 8.Mubang RN, Stoltzfus JC, Hoey BA, Stehly CD, Evans DC, Jones C, et al. Validation of comorbidity-polypharmacy score as predictor of outcomes in older trauma patients. 2013 May 23; doi: 10.1007/s00268-015-3041-5. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 9.Justiniano CF, Coffey RA, Evans DC, Jones LM, Jones CD, Bailey JK, et al. Comorbidity-polypharmacy score predicts in-hospital complications and the need for discharge to extended care facility in older burn patients. J Burn Care Res. 2015;36:193–6. doi: 10.1097/BCR.0000000000000094. [DOI] [PubMed] [Google Scholar]
- 10.Housley BC, Kelly NJ, Baky FJ, Stawicki SP, Evans DC, Jones CD. Comorbidity-Polypharmacy Score Predicts Readmission in Older Trauma Patients. 2015 doi: 10.1016/j.jss.2015.05.014. [DOI] [PubMed] [Google Scholar]
- 11.Holmes M, Garver M, Albrecht L, Arbabi S, Pham TN. Comparison of two comorbidity scoring systems for older adults with traumatic injuries. J Am Coll Surg. 2014;219:631–7. doi: 10.1016/j.jamcollsurg.2014.05.014. [DOI] [PubMed] [Google Scholar]
- 12.Barnsteiner JH. Hughes RG, editor. Medication reconciliation. Patient Safety and Quality: An Evidence-Based Handbook for Nurses. Agency for Healthcare Research and Quality, Rockville, Maryland. 2008 [PubMed] [Google Scholar]
- 13.Justiniano CF, Evans DC, Cook CH, Eiferman DS, Gerlach AT, Beery PR, Jr, et al. Comorbidity-polypharmacy score: A novel adjunct in post-emergency department trauma triage. J Surg Res. 2013;181:16–9. doi: 10.1016/j.jss.2012.05.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ichwan B, Darbha S, Shah MN, Thompson L, Evans DC, Boulger CT, et al. Geriatric-specific triage criteria are more sensitive than standard adult criteria in identifying need for trauma center care in injured older adults. Ann Emerg Med. 2015;65:92–1003. doi: 10.1016/j.annemergmed.2014.04.019. [DOI] [PubMed] [Google Scholar]
- 15.MacStravic S. Value-based operation for healthcare organizations: Are you ready? (48).Healthc Financ Manage. 2007;61:44–6. [PubMed] [Google Scholar]
- 16.Murphy SL, Xu J, Kochanek KD. Deaths: Final data for 2010. Natl Vital Stat Rep. 2013;61:1–117. [PubMed] [Google Scholar]
- 17.Pink B. National Population Projections 2004 (base) to 2051. In The Government of New Zealand. 2004 [Google Scholar]
- 18.Purcell P. Pension Sponsorship and Participation: Summary of Recent Trends. 2009 [Google Scholar]
- 19.Day JC. Population Projections of the United States, by Age, Sex, Race, and Hispanic Origin: 1992-2050. US Department of Commerce, Economics and Statistics Administration, Bureau of the Census. 1992 [Google Scholar]
- 20.Epping-Jordan JE, Pruitt SD, Bengoa R, Wagner EH. Improving the quality of health care for chronic conditions. Qual Saf Health Care. 2004;13:299–305. doi: 10.1136/qshc.2004.010744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Oliver A, Mossialos E. Equity of access to health care: Outlining the foundations for action. J Epidemiol Community Health. 2004;58:655–8. doi: 10.1136/jech.2003.017731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Stawicki S, Gerlach A. Polypharmacy and medication errors: Stop, listen, look, and analyze. OPUS. 2009;12:6–10. [Google Scholar]
- 23.Fortin M, Hudon C, Haggerty J, Akker Mv, Almirall J. Prevalence estimates of multimorbidity: A comparative study of two sources. BMC Health Serv Res. 2010;10:111. doi: 10.1186/1472-6963-10-111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fortin M, Bravo G, Hudon C, Vanasse A, Lapointe L. Prevalence of multimorbidity among adults seen in family practice. Ann Fam Med. 2005;3:223–8. doi: 10.1370/afm.272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Melton LJ, 3rd, Riggs BL. Risk factors for injury after a fall. Clin Geriatr Med. 1985;1:525–39. [PubMed] [Google Scholar]
- 26.Arden NK, Nevitt MC, Lane NE, Gore LR, Hochberg MC, Scott JC, et al. Osteoarthritis and risk of falls, rates of bone loss, and osteoporotic fractures. Study of Osteoporotic Fractures Research Group. Arthritis Rheum. 1999;42:1378–85. doi: 10.1002/1529-0131(199907)42:7<1378::AID-ANR11>3.0.CO;2-I. [DOI] [PubMed] [Google Scholar]
- 27.Neville AL, Brown CV, Weng J, Demetriades D, Velmahos GC. Obesity is an independent risk factor of mortality in severely injured blunt trauma patients. Arch Surg. 2004;139:983–7. doi: 10.1001/archsurg.139.9.983. [DOI] [PubMed] [Google Scholar]
- 28.Evans DC, Stawicki SP, Davido HT, Eiferman D. Obesity in trauma patients: Correlations of body mass index with outcomes, injury patterns, and complications. Am Surg. 2011;77:1003–8. doi: 10.1177/000313481107700818. [DOI] [PubMed] [Google Scholar]
- 29.Sturnieks DL, St George R, Lord SR. Balance disorders in the elderly. Neurophysiol Clin. 2008;38:467–78. doi: 10.1016/j.neucli.2008.09.001. [DOI] [PubMed] [Google Scholar]
- 30.Kerschner H, Pegues JA. Productive aging: A quality of life agenda. J Am Diet Assoc. 1998;98:1445–8. doi: 10.1016/S0002-8223(98)00327-7. [DOI] [PubMed] [Google Scholar]
- 31.Bass SA. New Haven: Yale University Press; 1995. Americans Over 55 at Work Program (Commonwealth Fund) Older and Active: How Americans Over 55 are Contributing to Society. [Google Scholar]
- 32.Fantus RJ. NTDB® data points. Older and thinner. Bull Am Coll Surg. 2010;95:59–60. [PubMed] [Google Scholar]
- 33.Perdue PW, Watts DD, Kaufmann CR, Trask AL. Differences in mortality between elderly and younger adult trauma patients: Geriatric status increases risk of delayed death. J Trauma. 1998;45:805–10. doi: 10.1097/00005373-199810000-00034. [DOI] [PubMed] [Google Scholar]
- 34.Knudson MM, Lieberman J, Morris JA, Jr, Cushing BM, Stubbs HA. Mortality factors in geriatric blunt trauma patients. Arch Surg. 1994;129:448–53. doi: 10.1001/archsurg.1994.01420280126017. [DOI] [PubMed] [Google Scholar]
- 35.Grossman MD, Miller D, Scaff DW, Arcona S. When is an elder old?. Effect of preexisting conditions on mortality in geriatric trauma. J Trauma. 2002;52:242–6. doi: 10.1097/00005373-200202000-00007. [DOI] [PubMed] [Google Scholar]
- 36.Osler T, Hales K, Baack B, Bear K, Hsi K, Pathak D, et al. Trauma in the elderly. Am J Surg. 1988;156:537–43. doi: 10.1016/s0002-9610(88)80548-8. [DOI] [PubMed] [Google Scholar]
- 37.Stawicki SP, Grossman MD, Hoey BA, Miller DL, Reed JF., 3rd Rib fractures in the elderly: A marker of injury severity. J Am Geriatr Soc. 2004;52:805–8. doi: 10.1111/j.1532-5415.2004.52223.x. [DOI] [PubMed] [Google Scholar]
- 38.McCoy GF, Johnston RA, Duthie RB. Injury to the elderly in road traffic accidents. J Trauma. 1989;29:494–7. doi: 10.1097/00005373-198904000-00013. [DOI] [PubMed] [Google Scholar]
- 39.Kauder D. The geriatric puzzle. Assessment challenges of elderly trauma patients. (68).JEMS. 2000;25:64–6. [PubMed] [Google Scholar]
- 40.Schwab CW, Kauder DR. Trauma in the geriatric patient. Arch Surg. 1992;127:701–6. doi: 10.1001/archsurg.1992.01420060077011. [DOI] [PubMed] [Google Scholar]
- 41.Seymour JF, Fenaux P, Silverman LR, Mufti GJ, Hellström-Lindberg E, Santini V, et al. Effects of azacitidine compared with conventional care regimens in elderly (≥75 years) patients with higher-risk myelodysplastic syndromes. Crit Rev Oncol Hematol. 2010;76:218–27. doi: 10.1016/j.critrevonc.2010.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.O’Mara MS. Is 45 the new 65: The rising role of geriatrics in traumatic injury. J Surg Res. 2013;185:531–2. doi: 10.1016/j.jss.2012.06.073. [DOI] [PubMed] [Google Scholar]
- 43.Christy JM, Stawicki SP, Jarvis AM, Evans DC, Gerlach AT, Lindsey DE, et al. The impact of antiplatelet therapy on pelvic fracture outcomes. J Emerg Trauma Shock. 2011;4:64–9. doi: 10.4103/0974-2700.76841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Austin SR, Wong YN, Uzzo RG, Beck JR, Egleston BL. Why summary comorbidity measures such as the Charlson comorbidity index and elixhauser score work. Med Care. 2013 May 23; doi: 10.1097/MLR.0b013e318297429c. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Gagne JJ, Glynn RJ, Avorn J, Levin R, Schneeweiss S. A combined comorbidity score predicted mortality in elderly patients better than existing scores. J Clin Epidemiol. 2011;64:749–59. doi: 10.1016/j.jclinepi.2010.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Southern DA, Quan H, Ghali WA. Comparison of the Elixhauser and Charlson/Deyo methods of comorbidity measurement in administrative data. Med Care. 2004;42:355–60. doi: 10.1097/01.mlr.0000118861.56848.ee. [DOI] [PubMed] [Google Scholar]
- 47.Leskovan JJ, Justiniano CF, Bach JA, Cook CH, Lindsey DE, Eiferman DS, et al. Anion gap as a predictor of trauma outcomes in the older trauma population: Correlations with injury severity and mortality. Am Surg. 2013;79:1203–6. [PubMed] [Google Scholar]
- 48.Jones TS, Dunn CL, Wu DS, Cleveland JC, Jr, Kile D, Robinson TN. Relationship between asking an older adult about falls and surgical outcomes. JAMA Surg. 2013;148:1132–8. doi: 10.1001/jamasurg.2013.2741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hollingsworth JW, Hashizume A, Jablon S. Correlations between tests of aging in Hiroshima subjects: An attempt to define “physiologic age”. Yale J Biol Med. 1965;38:11–26. [PMC free article] [PubMed] [Google Scholar]
- 50.Murray IM. Assessment of physiologic age by combination of several criteria; vision, hearing, blood pressure, and muscle force. J Gerontol. 1951;6:120–6. doi: 10.1093/geronj/6.2.120. [DOI] [PubMed] [Google Scholar]
- 51.Papadimos TJ, Stawicki SP. The aging paradox: How old is old and all that jazz? J Am Geriatr Soc. 2011;59:1987–8. doi: 10.1111/j.1532-5415.2011.03610_18.x. [DOI] [PubMed] [Google Scholar]
- 52.Thompson HJ, McCormick WC, Kagan SH. Traumatic brain injury in older adults: Epidemiology, outcomes, and future implications. J Am Geriatr Soc. 2006;54:1590–5. doi: 10.1111/j.1532-5415.2006.00894.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Vokonas PS, Kannel WB, Cupples LA. Epidemiology and risk of hypertension in the elderly: The Framingham Study. J Hypertens Suppl. 1988;6:S3–9. [PubMed] [Google Scholar]
- 54.Roger VL, Go AS, Lloyd-Jones DM, Adams RJ, Berry JD, Brown TM, et al. Heart disease and stroke statistics-2011 update: A report from the American Heart Association. Circulation. 2011;123:e18–209. doi: 10.1161/CIR.0b013e3182009701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Writing Group Members. Lloyd-Jones D, Adams RJ, Brown TM, Carnethon M, Dai S, et al. Heart disease and stroke statistics – 2010 update: A report from the American Heart Association. Circulation. 2010;121:e46–215. doi: 10.1161/CIRCULATIONAHA.109.192667. [DOI] [PubMed] [Google Scholar]
- 56.Bonne S, Schuerer DJ. Trauma in the older adult: Epidemiology and evolving geriatric trauma principles. Clin Geriatr Med. 2013;29:137–50. doi: 10.1016/j.cger.2012.10.008. [DOI] [PubMed] [Google Scholar]
- 57.Kennedy RL, Grant PT, Blackwell D. Low-impact falls: Demands on a system of trauma management, prediction of outcome, and influence of comorbidities. J Trauma. 2001;51:717–24. doi: 10.1097/00005373-200110000-00016. [DOI] [PubMed] [Google Scholar]
- 58.McGwin G, Jr, MacLennan PA, Fife JB, Davis GG, Rue LW., 3rd Preexisting conditions and mortality in older trauma patients. J Trauma. 2004;56:1291–6. doi: 10.1097/01.ta.0000089354.02065.d0. [DOI] [PubMed] [Google Scholar]
- 59.Milzman DP, Boulanger BR, Rodriguez A, Soderstrom CA, Mitchell KA, Magnant CM. Pre-existing disease in trauma patients: A predictor of fate independent of age and injury severity score. J Trauma. 1992;32:236–43. [PubMed] [Google Scholar]
- 60.Evans DC, Khoo KM, Radulescu A, Cook CH, Gerlach AT, Papadimos TJ, et al. Pre-injury beta blocker use does not affect the hyperdynamic response in older trauma patients. J Emerg Trauma Shock. 2014;7:305–9. doi: 10.4103/0974-2700.142766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Hippisley-Cox J, Pringle M, Ryan R. Polypharmacy in the Elderly: Analysis of QRESEARCH Data. In QRESEARCH; 2007 [Google Scholar]
- 62.Viktil KK, Blix HS, Moger TA, Reikvam A. Polypharmacy as commonly defined is an indicator of limited value in the assessment of drug-related problems. Br J Clin Pharmacol. 2007;63:187–95. doi: 10.1111/j.1365-2125.2006.02744.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Ziere G, Dieleman JP, Hofman A, Pols HA, van der Cammen TJ, Stricker BH. Polypharmacy and falls in the middle age and elderly population. Br J Clin Pharmacol. 2006;61:218–23. doi: 10.1111/j.1365-2125.2005.02543.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Baranzini F, Diurni M, Ceccon F, Poloni N, Cazzamalli S, Costantini C, et al. Fall-related injuries in a nursing home setting: Is polypharmacy a risk factor? BMC Health Serv Res. 2009;9:228. doi: 10.1186/1472-6963-9-228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Shoair OA, Nyandege AN, Slattum PW. Medication-related dizziness in the older adult. (x).Otolaryngol Clin North Am. 2011;44:455–71. doi: 10.1016/j.otc.2011.01.014. [DOI] [PubMed] [Google Scholar]
- 66.Cannon R, Bozeman M, Miller KR, Smith JW, Harbrecht B, Franklin G, et al. The prevalence and impact of prescription controlled substance use among injured patients at a Level I trauma center. J Trauma Acute Care Surg. 2014;76:172–5. doi: 10.1097/TA.0b013e3182ab10de. [DOI] [PubMed] [Google Scholar]
- 67.Montamat SC, Cusack B. Overcoming problems with polypharmacy and drug misuse in the elderly. Clin Geriatr Med. 1992;8:143–58. [PubMed] [Google Scholar]
- 68.Porter ME, Teisberg EO. Boston, Mass: Harvard Business School Press; 2006. Redefining Health Care: Creating Value-based Competition on Results. [Google Scholar]
- 69.Lazarus HM, Fox J, Evans RS, Lloyd JF, Pombo DJ, Burke JP, et al. Adverse drug events in trauma patients. J Trauma. 2003;54:337–43. doi: 10.1097/01.TA.0000051937.18848.68. [DOI] [PubMed] [Google Scholar]
- 70.Corbett SM, Rebuck JA. Medication-related complications in the trauma patient. J Intensive Care Med. 2008;23:91–108. doi: 10.1177/0885066607312966. [DOI] [PubMed] [Google Scholar]
- 71.Hall WH, Ramachandran R, Narayan S, Jani AB, Vijayakumar S. An electronic application for rapidly calculating Charlson comorbidity score. BMC Cancer. 2004;4:94. doi: 10.1186/1471-2407-4-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Charlson M, Szatrowski TP, Peterson J, Gold J. Validation of a combined comorbidity index. J Clin Epidemiol. 1994;47:1245–51. doi: 10.1016/0895-4356(94)90129-5. [DOI] [PubMed] [Google Scholar]
- 73.Charlson ME, Charlson RE, Peterson JC, Marinopoulos SS, Briggs WM, Hollenberg JP. The Charlson comorbidity index is adapted to predict costs of chronic disease in primary care patients. J Clin Epidemiol. 2008;61:1234–40. doi: 10.1016/j.jclinepi.2008.01.006. [DOI] [PubMed] [Google Scholar]
- 74.D’Hoore W, Sicotte C, Tilquin C. Risk adjustment in outcome assessment: The Charlson comorbidity index. Methods Inf Med. 1993;32:382–7. [PubMed] [Google Scholar]
- 75.Losina E, Freedberg KA. Life expectancy in HIV. BMJ. 2011;343:d6015. doi: 10.1136/bmj.d6015. [DOI] [PubMed] [Google Scholar]
- 76.Harrison KM, Song R, Zhang X. Life expectancy after HIV diagnosis based on national HIV surveillance data from 25 states, United States. J Acquir Immune Defic Syndr. 2010;53:124–30. doi: 10.1097/QAI.0b013e3181b563e7. [DOI] [PubMed] [Google Scholar]
- 77.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36:8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 78.D’Hoore W, Bouckaert A, Tilquin C. Practical considerations on the use of the Charlson comorbidity index with administrative data bases. J Clin Epidemiol. 1996;49:1429–33. doi: 10.1016/s0895-4356(96)00271-5. [DOI] [PubMed] [Google Scholar]
- 79.Hartz AJ, Kuhn EM, Kayser KL, Pryor DP, Green R, Rimm AA. Assessing providers of coronary revascularization: A method for peer review organizations. Am J Public Health. 1992;82:1631–40. doi: 10.2105/ajph.82.12.1631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45:613–9. doi: 10.1016/0895-4356(92)90133-8. [DOI] [PubMed] [Google Scholar]
- 81.Bottle A, Aylin P. Comorbidity scores for administrative data benefited from adaptation to local coding and diagnostic practices. J Clin Epidemiol. 2011;64:1426–33. doi: 10.1016/j.jclinepi.2011.04.004. [DOI] [PubMed] [Google Scholar]
- 82.van Walraven C, Austin PC, Jennings A, Quan H, Forster AJ. A modification of the Elixhauser comorbidity measures into a point system for hospital death using administrative data. Med Care. 2009;47:626–33. doi: 10.1097/MLR.0b013e31819432e5. [DOI] [PubMed] [Google Scholar]
- 83.Stawicki SP. Trends in nonoperative management of traumatic injuries: A synopsis. OPUS 12 Sci. 2007;1:19–35. doi: 10.4103/IJCIIS.IJCIIS_7_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Bach JA, Leskovan JJ, Scharschmidt T, Boulger CT, Papadimos TJ, Russell S, et al. The right team at the right time: Multidisciplinary approach to multi-trauma patient with orthopedic injuries. OPUS 12 Sci. 2012;6:6–10. doi: 10.4103/IJCIIS.IJCIIS_5_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Phillips S, Rond PC, 3rd, Kelly SM, Swartz PD. The failure of triage criteria to identify geriatric patients with trauma: Results from the Florida Trauma Triage Study. J Trauma. 1996;40:278–83. doi: 10.1097/00005373-199602000-00018. [DOI] [PubMed] [Google Scholar]
- 86.Stawicki SP, Guarnaschelli JJ, Dzenitis AJ. Cervical disc disease in geriatric patients: A comparison study. Eur J Gen Med. 2009;6:140–3. [Google Scholar]
- 87.Lossius HM, Langhelle A, Soreide E, Pillgram-Larsen J, Lossius TA, Laake P, et al. Reporting data following major trauma and analysing factors associated with outcome using the new Utstein style recommendations. Resuscitation. 2001;50:263–72. doi: 10.1016/s0300-9572(01)00361-6. [DOI] [PubMed] [Google Scholar]
- 88.Zimmer-Gembeck MJ, Southard PA, Hedges JR, Mullins RJ, Rowland D, Stone JV, et al. Triage in an established trauma system. J Trauma. 1995;39:922–8. doi: 10.1097/00005373-199511000-00017. [DOI] [PubMed] [Google Scholar]
- 89.Ma MH, MacKenzie EJ, Alcorta R, Kelen GD. Compliance with prehospital triage protocols for major trauma patients. J Trauma. 1999;46:168–75. doi: 10.1097/00005373-199901000-00029. [DOI] [PubMed] [Google Scholar]
- 90.Wong K, Petchell J. Trauma teams in Australia: A national survey. ANZ J Surg. 2003;73:819–25. doi: 10.1046/j.1445-2197.2003.02782.x. [DOI] [PubMed] [Google Scholar]
- 91.Chang DC, Bass RR, Cornwell EE, Mackenzie EJ. Undertriage of elderly trauma patients to state-designated trauma centers. Arch Surg. 2008;143:776–81. doi: 10.1001/archsurg.143.8.776. [DOI] [PubMed] [Google Scholar]


