Abstract
Objective
Low rates of alcohol treatment seeking has been shown to be associated with perceived barriers to treatment, yet heterogeneity in patterns of perceived barriers have not been explored. We used data from a population-based sample of adults with alcohol abuse and dependence to: describe latent classes of perceived barriers to seeking alcohol treatment and identify characteristics associated with class membership.
Methods
Data are from the National Epidemiologic Survey on Alcohol and Related Conditions (2001-02). Analyses were restricted to treatment-naive adults with alcohol abuse or dependence with a perceived treatment need (N=1,053). Latent class analysis was performed to identify subgroups with respect to barriers to treatment; latent class regression was performed to identify variables associated with each subgroup.
Results
Two subgroups emerged: the low barriers class (87%), characterized primarily by attitudinal barriers, and the high barriers class (13%), characterized by significant attitudinal, financial, stigma and readiness for change barriers. In both classes, the most frequently endorsed barrier was the attitudinal belief that they should be “strong enough” to handle it on their own. Univariate analyses showed strong associations between membership in the high barriers class and comorbid psychiatric disorders, alcohol dependence (relative to abuse), and family history of alcohol problems; multivariate analyses found significant associations with lifetime anxiety disorder and education level.
Conclusions
Findings show that attitudinal barriers are most prevalent, and highlight the existence of a notable subgroup with multiple barriers, including financial and stigma-related barriers, who may require additional resources and support in order to enter treatment.
Alcohol use disorders are common and characterized by a low occurrence of treatment seeking among affected individuals (1-6). Only 7.9% of 2013 National Survey on Drug Use and Health participants with a past-year alcohol disorder received treatment (7). Although some individuals successfully recover from an alcohol disorder without formal treatment (8), treatment has been shown to improve outcomes (9-13).
Factors related to treatment utilization for alcohol problems are multifaceted and complex. In the current study, we draw on Andersen’s model of health service use, which identifies predisposing characteristics (i.e., social and demographic factors, personal health attitudes), enabling factors (e.g., financial and structural resources), and need as predictive of service utilization (14). Predisposing characteristics are the most distal predictors of service use, followed by enabling factors, with need (perceived or real) being most proximal. As we review below, previous alcohol treatment studies have established associations between many of Andersen’s factors and treatment utilization, and found perceived treatment need to be one of the strongest predictors. However, many individuals who perceive a treatment need also perceive barriers to treatment; these perceived barriers are an important impediment to treatment (4,7,15-18).
Andersen’s predisposing characteristics show the least robust associations with treatment utilization. Several studies have found that unmarried individuals are more likely to receive substance treatment (1,2). Numerous studies have found that men are more likely to receive treatment (1,2,19-25), while others have found higher treatment rates among women (26,27). Similarly, studies have reported that racial/ethnic minorities are more likely (4,20,23,28), as likely (1,21,29), or less likely to receive treatment (30,31) compared with non-Hispanic whites. Finally, studies have reported higher treatment rates among both older (1,3,25) and younger individuals (20,23).
With regard to Andersen’s enabling factors, studies have found that individuals with higher income and education levels were less likely to receive substance treatment (1,2,19,20,28). It is possible these individuals may perceive greater stigma towards treatment, consider themselves as having “more to lose,” or have less severe drinking behaviors and consequences (1). Individuals who are uninsured have also been found to have lower rates of treatment (20,30,32), likely as a result of decreased access to or increased cost of services.
Treatment need, comprised of both actual and perceived need, is identified by Andersen as one of the most proximal determinants of treatment (14). Yet, the overwhelming majority of individuals with an alcohol disorder (approximately 90-95%) do not perceive a need for treatment (4,7,33); this hallmark of alcohol disorders may be the most pervasive impediment to treatment (18,33). For those individuals with a perceived treatment need, this perceived need has been shown to be one of the strongest predictors of treatment utilization (4,5,32,34,35). Factors associated with perceived need include age, marital status, family history of alcohol problems, severity of alcohol problems, and comorbid psychiatric problems (5,17,33,35). Disorder severity is another component of need: individuals are more likely to receive treatment if they experience alcohol dependence than abuse (1-3,36) or if they experience greater consequences of drinking (23,28,37). Comorbid psychiatric conditions are also strongly associated with treatment utilization (1,3,5,17,19,20), potentially because comorbidity increases treatment need or because individuals are being referred for alcohol treatment when receiving psychiatric treatment.
Despite perceived need being a strong proximal factor for treatment utilization, only 15-30% of individuals with a perceived treatment need receive treatment (1,2,7,34). Perceived barriers to treatment help explain this treatment gap, given that non-treatment seekers typically report more barriers than treatment seekers (15,16). Attitudinal barriers, such as the belief that one should be “strong enough” to handle alcohol problems on one’s own, have consistently been found to be the most prevalent barriers (4,15-17,34). Previous studies have primarily examined prevalence and correlates of barriers; little work has examined heterogeneity among individuals with respect to perceived barriers. It is likely that non-treatment seeking individuals are comprised of subgroups characterized by distinct sets of perceived barriers.
In this study, we use data from a large, population-based survey of US adults to identify subgroups of non-treatment-seeking individuals with a lifetime alcohol disorder and a perceived treatment need using latent class analysis. Additionally, we examine the associations between subgroup membership and factors previously shown to be associated with perceived need and treatment seeking. This study is one of the first to examine heterogeneity in barriers among treatment-naive individuals with a recognized treatment need. Identifying subgroups among non-treatment seekers can inform screening and treatment outreach efforts, and represents an important step towards increasing alcohol treatment.
Methods
Sample
Data are from wave 1 of the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC), a nationally representative survey of U.S. adults conducted by the National Institute on Alcohol Abuse and Alcoholism (38,39). Face-to-face interviews assessed present and past alcohol consumption, utilization of alcohol treatment services, and an extensive diagnostic battery of substance use and psychiatric disorders. Wave 1 of the NESARC (N=43,093) was conducted in 2001-2002.
In total, 11,843 (28%) of wave 1 NESARC participants met DSM-IV criteria for a lifetime alcohol use disorder (lifetime alcohol abuse and/or dependence), the majority of whom had never received treatment (N=10,004). Of these treatment-naive individuals, only 10.5% (N=1,053) perceived a need for treatment as assessed by the following question: “Was there ever a time when you thought you should see a doctor, counselor, or other health professional or seek any other help for your drinking, but you didn’t go?” Items regarding specific treatment barriers were asked only to individuals who reported a perceived treatment need; thus, our study sample consisted of the 1,053 treatment-naive individuals with a lifetime alcohol disorder and a perceived treatment need (see Online Appendix).
Assessment
Individuals who reported a perceived need were asked to identify reasons for not seeking treatment from a list of 26 barriers. In this analysis, a subset of 15 items was used due to infrequency of responses and content overlap of the remaining items.
Alcohol abuse and dependence, non-alcohol substance use disorders, and psychiatric conditions were assessed with the Alcohol Use Disorder and Associated Disabilities Interview Schedule (AUDADIS-IV; 40) based on DSM-IV diagnostic criteria. Individuals were classified as having a lifetime history of abuse (only) or dependence with or without abuse. Mood disorders included in the current analyses were major depressive disorder, dysthymia, and bipolar disorder. Anxiety disorders included generalized anxiety disorder, panic disorder, specific phobia, social phobia, and agoraphobia. Substance use disorders included abuse of and/or dependence on marijuana, stimulants, sedatives, tranquilizers, cocaine, heroin, opioids, inhalants, hallucinogens, and other drugs. Individuals were classified as having a lifetime history of a mood, anxiety, or non-alcohol substance use disorder if they met lifetime criteria for at least one mood, anxiety, or substance use disorder, respectively.
Other variables included in the analyses were sex, age (18-29 years, 30-49 years, 50 years or older), race/ethnicity (non-Hispanic white, non-Hispanic black, Hispanic, other), education (less than high school, high school, greater than high school), household income (less than $15,000, $15,000-$29,999, $30,000-$59,999, $60,000 or greater), insurance status (none, public, private), whether the individual lived with a partner, and parental history of alcohol problems.
Statistical Analysis
Latent class analysis (LCA) empirically identifies the structure of an underlying categorical latent variable based on observed patterns in latent class indicators (41). Using 15 NESARC items addressing specific barriers to treatment, we conducted LCA to identify subgroups of individuals with similar barrier patterns. To determine the optimal number of latent classes, we implemented LCA models with 1 to 5 classes and considered the following fit statistics: Akaike Information Criterion (AIC), Bayesian Information Criterion (BIC), adjusted BIC, Lo-Mendell-Rubin likelihood ratio test (LMR LRT), and entropy (42-46). Lower values of AIC, BIC and adjusted BIC indicate better fit; yet these statistics often marginally decrease with each additional class. To avoid over-fitting the LCA model, we selected the class size associated with the last substantial decrease (47,48). As a sensitivity analysis, we also fit LCA models with all 26 items; the resulting class structures were highly similar, so we present the results from the 15 item LCA for parsimony.
Latent class regression (LCR) was implemented to estimate the associations between covariates and latent class membership. Covariates that had previously been shown to be associated with perceived treatment need or treatment utilization were selected for inclusion in the LCR. Univariate (unadjusted) regressions were considered first; all variables significant at the .20 level were included in the final multivariate (adjusted) LCR model. LCA and LCR were performed in Mplus version 7.11, which uses maximum likelihood estimation to obtain estimates of model parameters (49). All analyses were accounted for NESARC survey weights, clustering, and stratification.
Results
Characteristics of the Sample
In our sample of 1,053 treatment-naive adults with a lifetime alcohol disorder and a perceived treatment need, the mean age was 43.8 years; 68% were male; 76% were non-Hispanic white, 9% Hispanic, 8% non-Hispanic black, and 7% from other racial/ethnic groups. Eighty-three percent met lifetime criteria for alcohol dependence and the remaining 17% met criteria for alcohol abuse. A parental history of alcohol problems was common: 52% reported paternal drinking problems and 20% reported maternal drinking problems. Lifetime psychiatric disorders were prevalent: 56% had a lifetime history of a mood disorder, 40% an anxiety disorder, and 52% a non-alcohol substance use disorder (Table 1).
Table 1.
Descriptive statistics for individuals with a lifetime alcohol use disorder who report perceiving a need for treatment but not seeking treatment; data from the National Epidemiologic Survey on Alcohol and Related Conditions, 2001-2002 (N=1,053).
| Variable | N | Weighted % |
|---|---|---|
| Demographics | ||
| Age | ||
| 18-29 | 164 | 17.6 |
| 30-49 | 556 | 54.1 |
| 50+ | 333 | 28.4 |
| Male | 681 | 68.0 |
| Race/Ethnicity | ||
| White | 663 | 76.2 |
| Black | 172 | 7.7 |
| Hispanic | 153 | 8.7 |
| Other | 65 | 7.4 |
| Living with partner | 466 | 56.1 |
| Education | ||
| < High school | 198 | 17.5 |
| High school | 327 | 31.8 |
| > High school | 528 | 50.7 |
| Household income | ||
| <15,000 | 232 | 16.7 |
| 15,000-29,999 | 251 | 20.1 |
| 30,000-59,999 | 323 | 34.5 |
| 60,000+ | 247 | 28.7 |
| Insurance status | ||
| Private | 516 | 52.5 |
| Public (Medicare, Medicaid, VA) | 284 | 22.4 |
| None | 253 | 25.0 |
| Alcohol risk & severity | ||
| Lifetime alcohol disorder | ||
| Abuse only | 195 | 16.8 |
| Dependence (with or without abuse) | 858 | 83.2 |
| Mother was a problem drinker | 225 | 20.4 |
| Father was a problem drinker | 547 | 52.0 |
| Comorbid psychiatric conditions | ||
| Lifetime (non-alcohol) substance use disorder | ||
| Any | 535 | 52.1 |
| Marijuana | 423 | 41.5 |
| Cocaine | 264 | 24.9 |
| Stimulants | 193 | 18.6 |
| Hallucinogens | 151 | 13.6 |
| Opioids | 143 | 14.2 |
| Sedative | 124 | 12.5 |
| Tranquilizers | 114 | 10.5 |
| Heroin | 41 | 2.8 |
| Inhalants | 40 | 3.0 |
| Other drugs | 14 | 1.4 |
| Lifetime mood disorder | 609 | 55.7 |
| Lifetime anxiety disorder | 411 | 40.0 |
|
| ||
| Perceived barriers (Latent class indicators) | ||
|
| ||
| Financial | ||
| Wanted to go, but health insurance didn’t cover | 88 | 7.9 |
| Couldn’t afford to pay the bill | 148 | 14.2 |
| Structural | ||
| Didn’t know any place to go for help | 78 | 7.4 |
| Didn’t have any way to get there | 45 | 3.8 |
| Didn’t have time | 90 | 8.6 |
| Stigma | ||
| Was too embarrassed to discuss it with anyone | 200 | 18.5 |
| Afraid of what boss, friends, family, or others would think | 94 | 8.2 |
| Was afraid I would lose my job | 31 | 2.7 |
| Attitudinal | ||
| Didn’t think anyone could help | 157 | 14.1 |
| Thought the problem would get better by itself | 343 | 32.9 |
| Thought should be strong enough to handle alone | 428 | 41.5 |
| Was afraid they would put me into the hospital | 83 | 8.9 |
| Readiness for change | ||
| Wanted to keep drinking or got drunk | 171 | 16.2 |
| Didn’t think drinking problem was serious enough | 205 | 20.6 |
| Stopped drinking on my own | 198 | 19.6 |
Note: Question stem for Perceived Barrier items was “I did not seek help because…”
Consistent with previous studies (4,15-17,34), individuals primarily reported attitudinal barriers to treatment (Table 1). Most frequently reported was the belief that “I should be strong enough to handle [it] alone” (42%), followed by the belief that “the problem would get better by itself” (33%). Additionally, 21% reported that their drinking problem “was not serious enough” to seek treatment. The most common stigma-related barrier was that an individual was “too embarrassed to discuss it with anyone” (19%); the most common financial barrier was that the individual “couldn’t afford to pay the bill” (14%). Structural barriers (“didn’t know any place to go for help,” “didn’t have any way to get there,” and “didn’t have time”) were the least frequently reported: each was endorsed by less than 10% of participants.
Latent class analysis results
A 2-class model was determined to be optimal based on the information criteria statistics and the LMR LRT test (Table 2). This model had an estimated entropy of .89, indicating good class differentiation (44). We characterized the two classes as the high barriers and low barriers classes, with the majority of individuals (87%) belonging to the low barriers class. The low barriers class exhibited moderate endorsement probabilities for several attitudinal barriers and relatively low endorsement probabilities for all of the remaining items (Figure 2). The most commonly endorsed item for the low barriers class was “I should be strong enough to handle on my own” (36%), followed by “the problem will get better by itself” (27%), and “I stopped drinking on my own” (16%). In contrast, 13% of individuals were estimated to belong to the high barriers class, characterized by moderate to high item probabilities across all items. Indeed, for every individual item, the endorsement probability was higher for the high barriers class than the low barriers class. As in the low barriers class, the most commonly endorsed items were “should be strong enough to handle [it] on my own” (77%) and “the problem will get better by itself” (71%). However, the high barriers class additionally reported stigma, lack of readiness for change, and financial and structural barriers. For example, 62% of individuals in the high barriers class were “too embarrassed to discuss it with anyone” compared to 12% in the low barriers class; 59% “wanted to keep drinking or get drunk” compared to 10% in the low barriers class; 45% were “afraid of what boss, friend, family, or others would think” compared to 3% in the low barriers class; and 43% “couldn’t afford to pay the bill” compared to 10% in the low barriers class. In summary, the classes were similar in that the most common barrier for both classes was attitudinal; yet the high barriers class faced notably more barriers across multiple domains.
Table 2.
Model fit indices for models with one to five classes in the latent class analysis.
| Number of classes | Number of free parameters | AIC | BIC | Adjusted BIC | Entropy | LMR LRT p-value |
|---|---|---|---|---|---|---|
| 1 | 15 | 11988.37 | 12062.56 | 12014.92 | NA | NA |
| 2 | 31 | 11174.34 | 11327.67 | 11229.21 | .89 | .00 |
| 3 | 47 | 11104.03 | 11336.49 | 11187.22 | .67 | .56 |
| 4 | 63 | 11047.19 | 11358.78 | 11158.69 | .73 | .58 |
| 5 | 79 | 10979.49 | 11370.22 | 11119.31 | .78 | .37 |
Note: AIC = Akaike Information Criterion; BIC = Bayesian Information Criterion; Adjusted BIC = adjusted Bayesian Information Criterion; LMR LRT = Lo-Mendel-Rubin likelihood ratio test.
Figure 2.
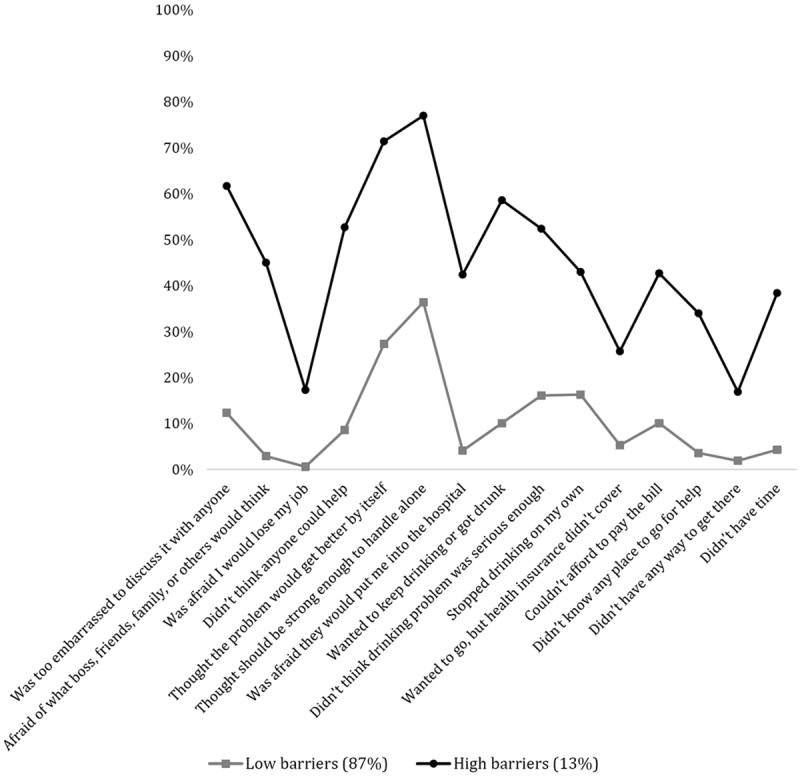
Weighted probability of endorsing perceived barriers conditional on membership in the latent class; data from the National Epidemiologic Survey on Alcohol and Related Conditions 2001-2002 (N=1,053).
Latent class regression results
Latent class regression was conducted to estimate the unadjusted and adjusted associations between class membership and factors related to demographics, alcohol risk and severity, and comorbid conditions. We present the estimated odds ratios (OR) for being in the high barriers class relative to the low barriers class for each covariate (Table 3). In the univariate analyses, all variables except race/ethnicity, insurance status, and partner status were associated with class membership at the p<.20 level; these three variables were not included in the multivariate analysis. Alcohol dependence was significantly associated with the high barriers class, relative to alcohol abuse (OR=2.63, p=.02). Family history of alcohol problems was also predictive of the high barriers class (mother OR=1.91, p=.02; father OR=1.61, p=.08). A lifetime mood disorder, anxiety disorder, and non-alcohol substance use disorder were each significantly associated with the high barriers class (OR=2.36, OR=2.81, and OR=2.07, respectively; all p<.05).
Table 3.
Latent class regression: Odds of high barriers class membership, relative to the low barriers class. OR reflects unadjusted (univariate) associations; AOR reflects adjusted (multivariate) associations.
| Covariates | High barriers class
|
|||
|---|---|---|---|---|
| OR | 95% CI | AOR | 95% CI | |
| Demographics | ||||
| Age | ||||
| 18-29 | 1.75† | .79-3.92 | 1.13 | .40-3.16 |
| 30-49 | .85 | .48-1.51 | .71 | .35-1.44 |
| 50+ | ref. | ref. | ||
| Male | .67† | .39-1.14 | 1.15 | .59-2.24 |
| Race/Ethnicity | ||||
| White | ref. | |||
| Black | .75 | .32-1.78 | ||
| Hispanic | .89 | .42-1.92 | ||
| Other | .79 | .28-2.22 | ||
| Living with partner | .73 | .45-1.19 | ||
| Education | ||||
| < High school | ref. | ref. | ||
| High school | 1.56 | .67-3.61 | 1.95 | .71-5.40 |
| > High school | 1.96† | .82-4.70 | 2.70** | 1.08-6.72 |
| Household income | ||||
| <15,000 | 1.75† | .78-3.96 | 2.07* | .93-4.60 |
| 15,000-29,999 | 1.51 | .66-3.46 | 1.46 | .65-3.25 |
| 30,000-59,999 | 1.69 | .76-3.75 | 1.60 | .68-3.76 |
| 60,000+ | ref. | ref. | ||
| Insurance | ||||
| None | 1.08 | .55-2.12 | ||
| Public | 1.26 | .66-2.39 | ||
| Private | ref. | |||
| Alcohol risk & severity | ||||
| Lifetime alcohol disorder | ||||
| Abuse only | ref. | ref. | ||
| Dependence (with or without abuse) | 2.63** | 1.16-5.94 | 1.52 | .58-4.03 |
| Mother was a problem drinker | 1.91** | 1.12-3.23 | 1.79* | .98-3.30 |
| Father was a problem drinker | 1.61* | .94-2.75 | 1.22 | .73-2.03 |
| Comorbid psychiatric conditions | ||||
| Lifetime (non-alcohol) substance disorder | 2.07** | 1.08-3.96 | 1.66 | .80-3.42 |
| Lifetime mood disorder | 2.36** | 1.19-4.67 | 1.76 | .77-4.04 |
| Lifetime anxiety disorder | 2.81** | 1.58-4.97 | 1.93** | 1.06-3.53 |
Note: OR = odds ratio, AOR = adjusted OR, CI = confidence interval, ref. = reference group.
p < .20,
p< .10, and
p < .05
In the adjusted model, a lifetime anxiety disorder was significantly associated with the high barriers class (AOR=1.93, p=.03). The association with maternal history of alcohol problems was attenuated and significant at the trend level (AOR=1.79, p=.06), but the association with alcohol dependence was no longer significant (AOR=1.52, p=.40). Higher education level was significantly associated with the high barriers class (AOR = 2.70 for greater than high school relative to less than high school, p=.03). Finally, lower income was associated with the high barriers class at the trend level (AOR=2.07 for less than $15,000 relative to $60,000 or greater, p=.08).
Discussion
We conducted a novel analysis that identified heterogeneous subgroups with respect to perceived alcohol treatment barriers among treatment-naive adults with a lifetime alcohol disorder and a perceived treatment need. In this population-based sample, individuals were best characterized as belonging to one of two distinct groups, characterized as the low barriers and high barriers classes. The vast majority of individuals (87%) were in the low barriers class and faced primarily attitudinal barriers to alcohol treatment. Individuals in the high barriers class (13%) represented a small but important subgroup that faced a complex set of attitudinal, readiness to change, structural, financial, and stigma barriers.
Attitudinal barriers were the most commonly reported barriers across both classes, consistent with previous studies (4,15-17,34). Furthermore, for a majority of individuals, the only perceived barriers were attitudinal. Given that attitudinal barriers may be the most modifiable, our findings suggest that interventions to reduce the stigma of alcohol treatment and to increase motivation for behavior change may be effective and sufficient for the majority of individuals with perceived treatment barriers. To this end, we endorse the use of Screening, Brief Intervention, and Referral to Treatment (SBIRT) in primary care (50). SBIRT’s screening component may be particularly beneficial to individuals with no perceived treatment need, who comprise the majority of individuals with alcohol problem. The Brief Intervention component could include Motivational Interviewing (51), which may be beneficial to individuals with attitudinal barriers. Routine screening may encourage discussion with healthcare providers; similar screening campaigns for depression have been successful at increasing awareness, reducing stigma, and increasing treatment uptake (29). Although physicians are increasingly implementing such evidence-based practices, many still report feeling uncomfortable asking patients about alcohol and substance use. Medical education should seek to improve clinician self-efficacy in discussing alcohol and substance use problems with patients. Furthermore, we believe that alcohol screening could be augmented to include several screening items regarding treatment barriers. This would help clinicians identify whether individuals primarily face attitudinal barriers or a more complex set of barriers, which could aid in decisions regarding treatment and supportive services.
Our results also highlight independent associations with the high barriers class for alcohol dependence, family history of alcohol problems, and comorbid psychiatric disorders; these factors have previously been found to be associated with treatment seeking and perceived barriers (1,3,5,19,20,33,36). The observed attenuations in the adjusted model may be due to the co-occurrence of these factors: for example, 88% of those with a maternal and 86% of those with a paternal history of alcohol problems met criteria for alcohol dependence rather than abuse. Overall, our results indicate that lifetime psychiatric disorders, particularly anxiety, are associated with belonging to the high barriers class. Increasing integration of substance use and mental health services may promote treatment uptake among this population.
This analysis is a cross-sectional description of class membership; membership may change over the course of one’s alcohol use disorder due to shifts in readiness for change, attitudes, or life circumstances. These classes may reflect individuals at different stages of change as described by the Transtheoretical Model of Change (52) –individuals who are farther from the Action stage may belong to the high barriers class and transition to the low barriers class as they near the Action stage. Alternatively, changes in employment, financial circumstances or relationship status may affect barriers and shift individuals between classes.
Several limitations deserve mention. First, this analysis was not designed to identify causal associations; due to the cross-sectional nature of the data, we cannot establish temporal ordering of covariates and class membership. For example, we were not able to establish whether psychiatric disorders were present during the period of perceived treatment need. Second, social and temporal trends regarding stigma and treatment accessibility over the past decade may somewhat limit the generalizability of our findings. While national surveys indicate that rates of alcohol treatment seeking have remained essentially flat since the NESARC was collected (7), there is little data regarding temporal trends in perceived barriers. Third, although the use of LCA does account for measurement error with regard to barriers to treatment (41,53), our analysis may still be subject to misclassification bias. Furthermore, all NESARC data are self-reported and thus may be subject to recall bias or social desirability bias. Finally, NESARC data were limited to barriers from the participants’ perspectives and did not include information regarding barriers at the provider, state, or national level.
Conclusions
In summary, this study identified two distinct subgroups among treatment-naive adults with a lifetime alcohol disorder and a perceived treatment need. Our results highlight that the majority of individuals face few, and primarily attitudinal, barriers, while a notable subset faces a complex set of barriers. Routine screening may help identify non-treatment seeking individuals; individuals in the low barriers class may benefit from motivation interviewing while individuals in the high barriers class may require more innovative and comprehensive treatment strategies.
Supplementary Material
Acknowledgments
This work was funded by grant AA016346 from the National Institute on Alcohol Abuse and Alcoholism, grant DA030460, P50DA010075 and T32DA017629 from the National Institute on Drug Abuse, as well as the Sommer Scholar program at Johns Hopkins Bloomberg School of Public Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute on Alcohol Abuse and Alcoholism, the National Institute on Drug Abuse, or the National Institutes of Health.
Footnotes
Disclosures of Conflicts of Interest:
No authors have any disclosures.
Contributor Information
Megan S. Schuler, Johns Hopkins University Bloomberg School of Public Health, Department of Mental Health, Baltimore, MD
Savitha Puttaiah, Department of Psychiatry, Sinai Hospital, Baltimore, MD.
Ramin Mojtabai, Johns Hopkins University Bloomberg School of Public Health, Department of Mental Health, Johns Hopkins School of Medicine, Department of Psychiatry & Behavioral Sciences, Baltimore, MD.
Rosa M. Crum, Johns Hopkins Bloomberg School of Public Health, Department of Epidemiology, Department of Mental Health, Johns Hopkins Bloomberg School of Public Health, Johns Hopkins School of Medicine, Department of Psychiatry & Behavioral Sciences, Baltimore MD
References
- 1.Cohen E, Feinn R, Arias A, et al. Alcohol treatment utilization: findings from the National Epidemiologic Survey on Alcohol and Related Conditions. Drug and Alcohol Dependence. 2007;86:214–221. doi: 10.1016/j.drugalcdep.2006.06.008. [DOI] [PubMed] [Google Scholar]
- 2.Hasin DS, Stinson FS, Ogburn E, et al. Prevalence, Correlates, Disability, and Comorbidity of DSM-IV Alcohol Abuse and Dependence in the United States. Archives of General Psychiatry. 2007;64:830–842. doi: 10.1001/archpsyc.64.7.830. [DOI] [PubMed] [Google Scholar]
- 3.Grella C, Karno M, Warda U, et al. Perceptions of need and help received for substance dependence in a national probability survey. Psychiatric Services. 2009;60:1068–1074. doi: 10.1176/appi.ps.60.8.1068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Oleski J, Mota N, Cox BJ, et al. Perceived need for care, help seeking, and perceived barriers to care for alcohol use disorders in a national sample. Psychiatric Services. 2010;61:1223–1231. doi: 10.1176/ps.2010.61.12.1223. [DOI] [PubMed] [Google Scholar]
- 5.Mojtabai R, Olfson M, Mechanic D. Perceived need and help-seeking in adults with mood, anxiety, or substance use disorders. Archives of General Psychiatry. 2002;59:77–84. doi: 10.1001/archpsyc.59.1.77. [DOI] [PubMed] [Google Scholar]
- 6.Regier DA, Narrow WE, Rae DS, et al. The de facto US mental and addictive disorders service system. Epidemiologic catchment area prospective 1-year prevalence rates of disorders and services. Archives of General Psychiatry. 1993;50:85–94. doi: 10.1001/archpsyc.1993.01820140007001. [DOI] [PubMed] [Google Scholar]
- 7.Results from the 2013 National Survey on Drug Use and Health Summary of National Findings. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2014. NSDUH series H-48, HHS pub no SMA 14-4863. [Google Scholar]
- 8.Dawson DA, Grant BF, Stinson FS, et al. Recovery from DSM-IV alcohol dependence: United States, 2001–2002. Addiction. 2005;100:281–292. doi: 10.1111/j.1360-0443.2004.00964.x. [DOI] [PubMed] [Google Scholar]
- 9.Dawson DA, Grant BF, Stinson FS, et al. Estimating the effect of help-seeking on achieving recovery from alcohol dependence. Addiction. 2006;101:824–834. doi: 10.1111/j.1360-0443.2006.01433.x. [DOI] [PubMed] [Google Scholar]
- 10.Miller WR, Brown J, Simpson T, et al. What works? A methodological analysis of the alcohol treatment outcome literature. In: Hester R, Miller WR, editors. Handbook of Alcoholism Treatment Approaches: Effective Alternatives. Boston, MA: Allyn and Bacon; 1995. [Google Scholar]
- 11.Miller WR, Wilbourne PL. Mesa Grande: a methodological analysis of clinical trials of treatments for alcohol use disorders. Addiction. 2002;97:265–277. doi: 10.1046/j.1360-0443.2002.00019.x. [DOI] [PubMed] [Google Scholar]
- 12.Moos RH, Moos BS. Rates and predictors of relapse after natural and treated remission from alcohol use disorders. Addiction. 2006;101:212–222. doi: 10.1111/j.1360-0443.2006.01310.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Timko C, DeBenedetti A, Billow R. Intensive referral to 12-step self-help groups and 6 month substance use disorder outcomes. Addiction. 2006;101:678–688. doi: 10.1111/j.1360-0443.2006.01391.x. [DOI] [PubMed] [Google Scholar]
- 14.Andersen RM. Revisiting the behavioral model and access to medical care: Does it matter? Journal of Health and Social Behavior. 1995;36:1–10. [PubMed] [Google Scholar]
- 15.Saunders SM, Zygowicz KM, D’Angelo BR. Person-related and treatment-related barriers to alcohol treatment. Journal of Substance Abuse Treatment. 2006;30:261–270. doi: 10.1016/j.jsat.2006.01.003. [DOI] [PubMed] [Google Scholar]
- 16.Cunningham JA, Sobell LC, Sobell MB, et al. Barriers to treatment: why alcohol and drug abusers delay or never seek treatment. Addictive Behaviors. 1993;18:347–353. doi: 10.1016/0306-4603(93)90036-9. [DOI] [PubMed] [Google Scholar]
- 17.Kaufman CN, Chen LY, Crum RM, et al. Treatment seeking and barriers to treatment for alcohol use in persons with alcohol use disorders and comorbid mood or anxiety disorders. Social Psychiatry and Psychiatric Epidemiology. 2014 doi: 10.1007/s00127-013-0740-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mojtabai R, Chen LY, Kaufmann CN, et al. Comparing barriers to mental health treatment and substance use disorder treatment among individuals with comorbid major depression and substance use disorders. Journal of Substance Abuse Treatment. 2014;46:268–73. doi: 10.1016/j.jsat.2013.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wu LT, Ringwalt CL, Williams CE. Use of substance abuse treatment services by persons with mental health and substance use problems. Psychiatric Services. 2003;54:363–369. doi: 10.1176/appi.ps.54.3.363. [DOI] [PubMed] [Google Scholar]
- 20.Ilgen MA, Price AM, Burnett-Zeigler I, et al. Longitudinal predictors of addictions treatment utilization in treatment naive adults with alcohol use disorders. Drug and Alcohol Dependence. 2011;113:215–221. doi: 10.1016/j.drugalcdep.2010.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Alvanzo AAH, Storr CL, Mojtabai R, et al. Gender and race/ethnicity differences for initiation of alcohol-related service use among persons with alcohol dependence. Drug and Alcohol Dependence. 2014;140:48–55. doi: 10.1016/j.drugalcdep.2014.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dawson DA. Correlates of past-year status among treated and untreated persons with former alcohol dependence: United States, 1992. Alcoholism: Clinical and Experimental Research. 1996;20:771–779. doi: 10.1111/j.1530-0277.1996.tb01685.x. [DOI] [PubMed] [Google Scholar]
- 23.Kaskutas L, Weisner C, Caetana R. Predictors of help seeking among a longitudinal sample of the general population, 1984–1992. Journal of Studies on Alcohol and Drugs. 1997;58:155–161. doi: 10.15288/jsa.1997.58.155. [DOI] [PubMed] [Google Scholar]
- 24.Raimo EB, Daeppen JB, Smith TL, et al. Clinical characteristics of alcoholism in alcohol-dependent subjects with and without a history of alcohol treatment. Alcoholism: Clinical and Experimental Research. 1999;23:1605–1613. [PubMed] [Google Scholar]
- 25.Tighe E, Saxe L. Community-based substance abuse reduction and the gaps between treatment need and treatment utilization: Analysis of data from the “Fighting Back” general population survey. Journal of Drug Issues. 2006;36:295–312. [Google Scholar]
- 26.Harris AHS, Bowe T. Predictors of initiation and engagement in VA substance use disorder treatment. Psychological Services. 2008;5:228–238. [Google Scholar]
- 27.Weisner C, Mertens J, Tam T, et al. Factors affecting the initiation of substance abuse treatment in managed care. Addiction. 2001;96:705–716. doi: 10.1046/j.1360-0443.2001.9657056.x. [DOI] [PubMed] [Google Scholar]
- 28.Weisner C, Matzger H, Tam T, et al. Who goes to alcohol and drug treatment? Understanding utilization within the context of insurance. Journal of Studies of Alcohol and Drugs. 2002;63:673–682. doi: 10.15288/jsa.2002.63.673. [DOI] [PubMed] [Google Scholar]
- 29.Keyes KM, Hatzenbuehler ML, Alberti P, et al. Service utilization differences for Axis I psychiatric and substance use disorders between White and Black adults. Psychiatric Services. 2008;59:893–901. doi: 10.1176/appi.ps.59.8.893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wu LT, Kouzis A, Schlenger W. Substance use, dependence, and service utilization among the US uninsured nonelderly population. American Journal of Public Health. 2003;93:2079–2085. doi: 10.2105/ajph.93.12.2079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Schmidt LA, Ye Y, Greenfield TK, et al. Ethnic disparities in clinical severity and services for alcohol problems: results from the National Alcohol Survey. Alcoholism: Clinical and Experimental Research. 2007;31:48–56. doi: 10.1111/j.1530-0277.2006.00263.x. [DOI] [PubMed] [Google Scholar]
- 32.Katz SJ, Kessler RC, Frank RG, et al. The use of outpatient mental health services in the United States and Ontario: the impact of mental morbidity and perceived need for care. American Journal of Public Health. 1997;87:1136–1143. doi: 10.2105/ajph.87.7.1136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Edlund M, Booth B, Feldman Z. Perceived need for treatment for alcohol use disorders: results from two national surveys. Psychiatric Services. 2009;60:1618–1628. doi: 10.1176/appi.ps.60.12.1618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mojtabai R, Crum RM. Perceived unmet need for alcohol and drug use treatments and future use of services: Results from a longitudinal study. Drug and Alcohol Dependence. 2013;127:59–64. doi: 10.1016/j.drugalcdep.2012.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Edlund MJ, Unutzer J, Curran GM. Perceived need for alcohol, drug, and mental health treatment. Social Psychiatry and Psychiatric Epidemiology. 2006;41:480–487. doi: 10.1007/s00127-006-0047-1. [DOI] [PubMed] [Google Scholar]
- 36.Kessler R, Aguilar-Gaxiola S, Berglund PA, et al. Patterns and predictors of treatment seeking after onset of a substance use disorder. Archives of General Psychiatry. 2001;58:1065–1071. doi: 10.1001/archpsyc.58.11.1065. [DOI] [PubMed] [Google Scholar]
- 37.Finney JW, Moos RH. Entering treatment for alcohol abuse: A stress and coping model. Addiction. 1995;90:1223–1240. doi: 10.1046/j.1360-0443.1995.90912237.x. [DOI] [PubMed] [Google Scholar]
- 38.Grant BF, Stinson FS, Dawson DA, et al. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Archives of General Psychiatry. 2004;61:807–816. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- 39.Grant BF, Dawson DA. Introduction to the National Epidemiologic Survey on Alcohol and Related Conditions. Alcohol Research and Health. 2006;29:74–78. doi: 10.4088/jcp.v67n0305. [DOI] [PubMed] [Google Scholar]
- 40.Grant BF, Dawson DA, Stinson FS, et al. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV (AUDADIS-IV): Reliability of alcohol consumption, tobacco use, family history of depression and psychiatric diagnostic modules in a general population sample. Drug and Alcohol Dependence. 2003;71:7–16. doi: 10.1016/s0376-8716(03)00070-x. [DOI] [PubMed] [Google Scholar]
- 41.Collins LM, Lanza ST. Latent Class and Latent Transition Analysis: With Applications in the Social, Behavioral, and Health Sciences. New York, NY: Wiley; 2010. [Google Scholar]
- 42.Akaike H. A new look at the statistical model identification. IEEE Transactions on Automatic Control. 1974;19:716–723. [Google Scholar]
- 43.Schwartz GE. Estimating the dimension of a model. Annals of Statistics. 1978;6:461–464. [Google Scholar]
- 44.Sclove SL. Application of model-selection criteria to some problems in multivariate analysis. Psychometrika. 1987;52:333–343. [Google Scholar]
- 45.Lo Y, Mendell NR, Rubin DB. Testing the number of components in a normal mixture. Biometrika. 2001;88:767–778. [Google Scholar]
- 46.Celeux G, Soromenho G. An entropy criterion for assessing the number of clusters in a mixture model. Journal of Classification. 1996;13:195–212. [Google Scholar]
- 47.Landa RJ, Gross AL, Stuart EA, et al. Latent class analysis of early developmental trajectory in baby siblings of children with autism. Journal of Child Psychology and Psychiatry. 2012;53:986–996. doi: 10.1111/j.1469-7610.2012.02558.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Petras H, Masyn K. General growth mixture analysis with antecedents and consequences of change. In: Piquero AR, Weisburd D, editors. Handbook of Quantitative Criminology. New York, NY: Springer; 2010. [Google Scholar]
- 49.Muthén LK, Muthén BO. Mplus User’s Guide. 7. Los Angeles, CA: Muthén & Muthén; 1998-2012. [Google Scholar]
- 50.Babor TF, McRee BG, Kassebaum PA, et al. Screening, Brief Intervention, and Referral to Treatment (SBIRT) Substance Abuse. 2007;28:7–30. doi: 10.1300/J465v28n03_03. [DOI] [PubMed] [Google Scholar]
- 51.Miller WR, Rollnick S. Motivational interviewing: Preparing people for change. New York, NY: Guilford Press; 1991. [Google Scholar]
- 52.Prochaska JO, DiClemente CC. Toward a comprehensive model of change. In: Miller WR, Heather N, editors. Treating Addictive Behaviors: Processes of Change. New York, NY: Plenum Press; 1986. [Google Scholar]
- 53.Flaherty BP. Assessing reliability of categorical substance use measures with latent class analysis. Drug and Alcohol Dependence. 2002;68:7–20. doi: 10.1016/s0376-8716(02)00210-7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


