Abstract
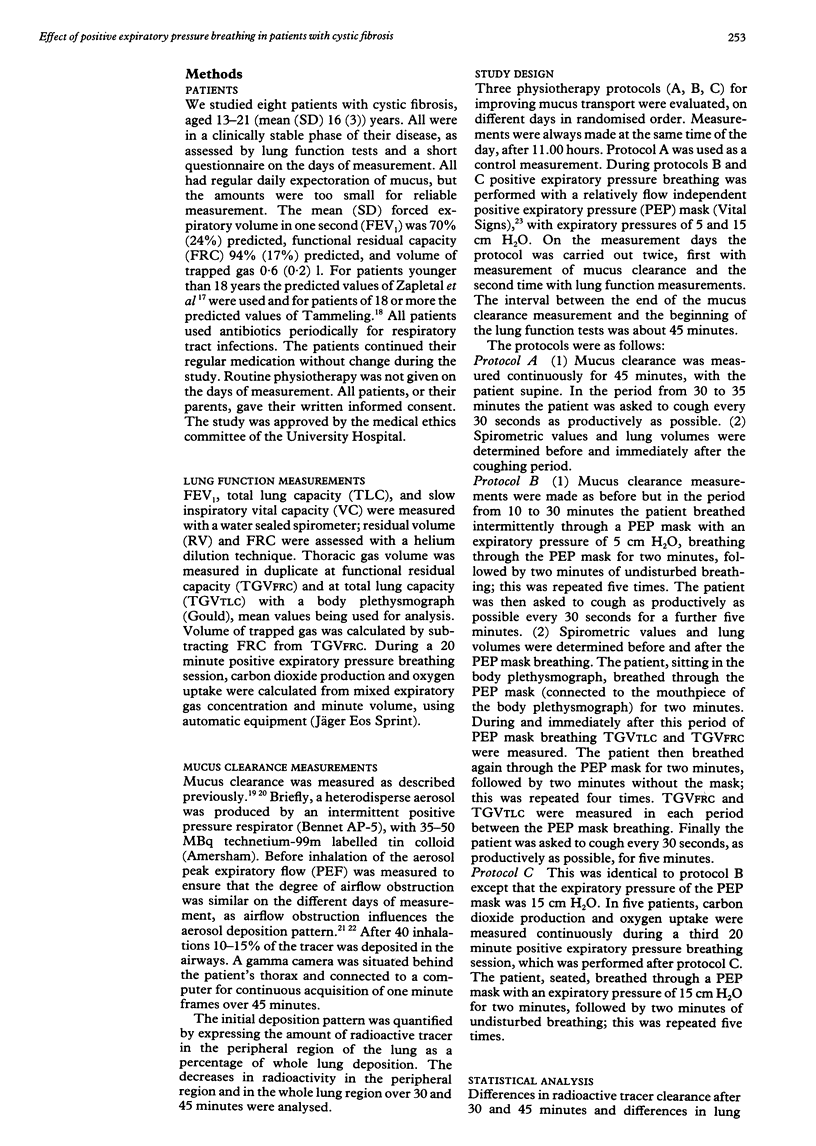
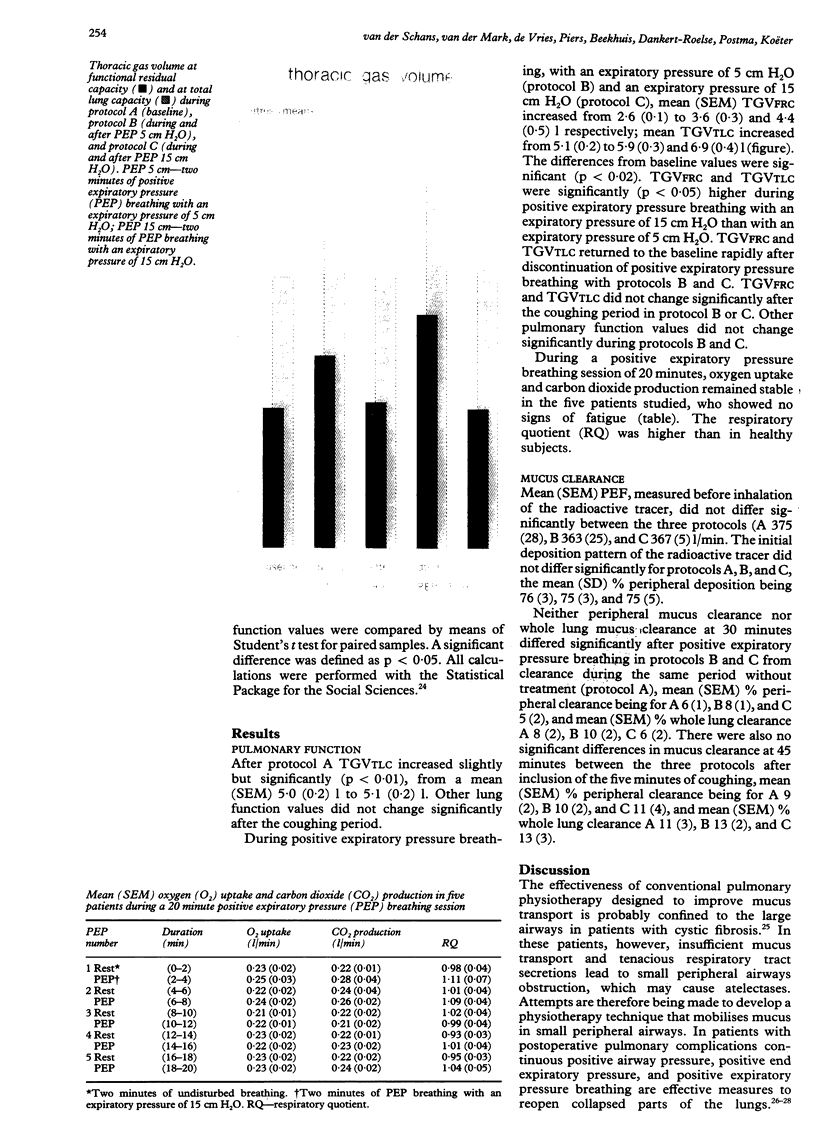
The effect of positive expiratory pressure breathing, alone and in combination with coughing, was investigated in eight patients with cystic fibrosis. Functional residual capacity and total lung capacity was measured with a body plethysmograph before, during, and immediately after breathing with expiratory pressure of 5 and 15 cm H2O, and after a coughing period. The positive expiratory pressure breathing was carried out five times for two minutes with a two minute interval between each period. Mucus transport was measured in a peripheral lung region and over the whole lung by a radioactive aerosol tracer technique. Clearance measurements were carried out continuously during positive expiratory pressure breathing and during a control period. Two minutes' breathing with an expiratory pressure of 5 and 15 cm H2O caused an increase in mean (SEM) functional residual capacity from 2.6 (0.1) to 3.6 (0.3) and 4.4 (0.5) 1 and an increase in total lung capacity from 5.1 (0.2) to 5.9 (0.3) and 6.9 (0.4) 1. Lung volumes were higher during breathing with an expiratory pressure of 15 cm H2O than with 5 cm H2O; both returned to baseline values immediately after positive expiratory pressure breathing. Spontaneous mucus clearance and mucus clearance by coughing were not influenced by positive expiratory pressure breathing at either expiratory pressure. Thus in patients with cystic fibrosis positive expiratory pressure breathing increases lung volumes in relation to the expiratory pressure imposed; these changes in lung volume did not, however, lead to an improvement of mucus transport.
Full text
PDF

Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Andersen J. B., Qvist J., Kann T. Recruiting collapsed lung through collateral channels with positive end-expiratory pressure. Scand J Respir Dis. 1979 Oct;60(5):260–266. [PubMed] [Google Scholar]
- Barach A. L. Physiologic advantages of grunting, groaning, and pursed-lip breathing: adaptive symptoms related to the development of continuous positive pressure breathing. Bull N Y Acad Med. 1973 Aug;49(8):666–673. [PMC free article] [PubMed] [Google Scholar]
- Delaunois L. Anatomy and physiology of collateral respiratory pathways. Eur Respir J. 1989 Oct;2(9):893–904. [PubMed] [Google Scholar]
- Desmond K. J., Schwenk W. F., Thomas E., Beaudry P. H., Coates A. L. Immediate and long-term effects of chest physiotherapy in patients with cystic fibrosis. J Pediatr. 1983 Oct;103(4):538–542. doi: 10.1016/s0022-3476(83)80579-4. [DOI] [PubMed] [Google Scholar]
- Dolovich M. B., Sanchis J., Rossman C., Newhouse M. T. Aerosol penetrance: a sensitive index of peripheral airways obstruction. J Appl Physiol. 1976 Mar;40(3):468–471. doi: 10.1152/jappl.1976.40.3.468. [DOI] [PubMed] [Google Scholar]
- Fick R. B., Jr, Stillwell P. C. Controversies in the management of pulmonary disease due to cystic fibrosis. Chest. 1989 Jun;95(6):1319–1327. doi: 10.1378/chest.95.6.1319. [DOI] [PubMed] [Google Scholar]
- Garrard C. S., Gerrity T. R., Schreiner J. F., Yeates D. B. The characterization of radioaerosol deposition in the healthy lung by histogram distribution analysis. Chest. 1981 Dec;80(6 Suppl):840–842. doi: 10.1378/chest.80.6.840. [DOI] [PubMed] [Google Scholar]
- Groth S., Stafanger G., Dirksen H., Andersen J. B., Falk M., Kelstrup M. Positive expiratory pressure (PEP-mask) physiotherapy improves ventilation and reduces volume of trapped gas in cystic fibrosis. Bull Eur Physiopathol Respir. 1985 Jul-Aug;21(4):339–343. [PubMed] [Google Scholar]
- Herala M., Gislason T. Chest physiotherapy. Evaluation by transcutaneous blood gas monitoring. Chest. 1988 Apr;93(4):800–802. doi: 10.1378/chest.93.4.800. [DOI] [PubMed] [Google Scholar]
- Hofmeyr J. L., Webber B. A., Hodson M. E. Evaluation of positive expiratory pressure as an adjunct to chest physiotherapy in the treatment of cystic fibrosis. Thorax. 1986 Dec;41(12):951–954. doi: 10.1136/thx.41.12.951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Menkes H. A., Traystman R. J. Collateral ventilation. Am Rev Respir Dis. 1977 Aug;116(2):287–309. doi: 10.1164/arrd.1977.116.2.287. [DOI] [PubMed] [Google Scholar]
- Mueller R. E., Petty T. L., Filley G. F. Ventilation and arterial blood gas changes induced by pursed lips breathing. J Appl Physiol. 1970 Jun;28(6):784–789. doi: 10.1152/jappl.1970.28.6.784. [DOI] [PubMed] [Google Scholar]
- Oberwaldner B., Evans J. C., Zach M. S. Forced expirations against a variable resistance: a new chest physiotherapy method in cystic fibrosis. Pediatr Pulmonol. 1986 Nov-Dec;2(6):358–367. doi: 10.1002/ppul.1950020608. [DOI] [PubMed] [Google Scholar]
- Peters R. M. Pulmonary physiologic studies of the perioperative period. Chest. 1979 Nov;76(5):576–584. doi: 10.1378/chest.76.5.576. [DOI] [PubMed] [Google Scholar]
- Ricksten S. E., Bengtsson A., Soderberg C., Thorden M., Kvist H. Effects of periodic positive airway pressure by mask on postoperative pulmonary function. Chest. 1986 Jun;89(6):774–781. doi: 10.1378/chest.89.6.774. [DOI] [PubMed] [Google Scholar]
- Thoman R. L., Stoker G. L., Ross J. C. The efficacy of pursed-lips breathing in patients with chronic obstructive pulmonary disease. Am Rev Respir Dis. 1966 Jan;93(1):100–106. doi: 10.1164/arrd.1966.93.1.100. [DOI] [PubMed] [Google Scholar]
- Tyrrell J. C., Hiller E. J., Martin J. Face mask physiotherapy in cystic fibrosis. Arch Dis Child. 1986 Jun;61(6):598–600. doi: 10.1136/adc.61.6.598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tønnesen P., Støvring S. Positive expiratory pressure (PEP) as lung physiotherapy in cystic fibrosis: a pilot study. Eur J Respir Dis. 1984 Aug;65(6):419–422. [PubMed] [Google Scholar]
- Van Asperen P. P., Jackson L., Hennessy P., Brown J. Comparison of a positive expiratory pressure (PEP) mask with postural drainage in patients with cystic fibrosis. Aust Paediatr J. 1987 Oct;23(5):283–284. doi: 10.1111/j.1440-1754.1987.tb00272.x. [DOI] [PubMed] [Google Scholar]
- Weller P. H., Bush E., Preece M. A., Matthew D. J. Short-term effects of chest physiotherapy on pulmonary function in children with cystic fibrosis. Respiration. 1980;40(1):53–56. doi: 10.1159/000194251. [DOI] [PubMed] [Google Scholar]
- Zapletal A., Paul T., Samánek M. Normální hodnoty statických plicních objemů a ventilace u detí a mladistvých. Cesk Pediatr. 1976 Oct;31(10):532–539. [PubMed] [Google Scholar]
- van Hengstum M., Festen J., Beurskens C., Hankel M., van den Broek W., Buijs W., Corstens F. The effect of positive expiratory pressure versus forced expiration technique on tracheobronchial clearance in chronic bronchitics. Scand J Gastroenterol Suppl. 1988;143:114–118. doi: 10.3109/00365528809090229. [DOI] [PubMed] [Google Scholar]
- van der Schans C. P., Piers D. A., Beekhuis H., Koëter G. H., van der Mark T. W., Postma D. S. Effect of forced expirations on mucus clearance in patients with chronic airflow obstruction: effect of lung recoil pressure. Thorax. 1990 Aug;45(8):623–627. doi: 10.1136/thx.45.8.623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van der Schans C. P., Piers D. A., Postma D. S. Effect of manual percussion on tracheobronchial clearance in patients with chronic airflow obstruction and excessive tracheobronchial secretion. Thorax. 1986 Jun;41(6):448–452. doi: 10.1136/thx.41.6.448. [DOI] [PMC free article] [PubMed] [Google Scholar]