Abstract
A meta-analysis of cross-sectional studies found that shorter-time sleep was correlated with increased risk of obesity in children. However, findings from prospective cohort studies were inconsistent. PubMed and other data resources were searched through May 2015. Twenty-five eligible studies were identified including 56,584 children and adolescents with an average 3.4-year follow-up. Compared with children having the longest sleep duration (~12.2 hours), kids with the shortest sleep duration (~10.0 hours) were 76% more likely to be overweight/obese (pooled odds ratio [OR]: 1.76; 95% confidence interval [CI]: 1.39, 2.23); and had relatively larger annual BMI gain (pooled β coefficient: 0.13; 95% CI: 0.01, 0.25 kg/m2). With every 1 hour/day increment in sleep duration, the risk of overweight/obesity was reduced by 21% (OR: 0.79; 95% CI: 0.70, 0.89); and the annual BMI gain declined by 0.05 kg/m2 (β = −0.05; 95% CI: −0.09, −0.01). The observed associations were not appreciably modified by region, baseline age or the length of follow-up. Accumulated literature indicates a modest inverse association between sleep duration and the risk of childhood overweight/obesity. Further research is needed to determine the age and gender specified optimal hours of sleep and ideal sleep pattern with respect to obesity prevention in children.
A number of epidemiological studies have suggested that childhood obesity is an independent risk factor of chronic diseases later in life1,2,3,4. Thus, identifying modifiable risk factors of obesity in childhood is of great public health significance.
Sleep duration, a modifiable factor, was suggested to play an important role in the development of childhood obesity. A meta-analysis that summarized data from 12 cross-sectional studies found that shorter-time sleep was correlated with an increased risk of obesity in children5. Findings from prospective cohort studies were inconsistent. One recent systematic review assessed the longitudinal studies in children and adolescents and concluded that the majority of the studies supported an inverse association between sleep duration and the risk of childhood overweight/obesity6. However, that review did not quantitatively estimate the overall association, particularly the dose-response relationship. Therefore, we aimed to examine the longitudinal association between habitual sleep duration and the risk of childhood overweight/obesity as well as the related anthropometric parameters by quantitatively summarizing data from prospective cohort studies.
Methods
The present meta-analysis was conducted following the guidelines of the Meta-analysis Of Observational Studies in Epidemiology (MOOSE)7. We systematically reviewed the literature in PubMed and EMBASE through May 2015 to identify prospective cohort studies published in English on the association between sleep duration and the risk of overweight/obesity in children and adolescents. We used the key words “sleep” and “obesity”, “adiposity’, “body mass index”, “body weight”, “waist circumference”, or “skinfold thickness”, and “follow-up studies”, “longitudinal studies”, or “prospective studies” and “children” or “adolescents”. In addition, we searched Google Scholar and manually reviewed the reference lists from the relevant articles.
Eligible studies were prospective cohort studies conducted in children and/or adolescents, and reported results on the association between sleep duration and the risk of overweight/obesity and/or anthropometric measures. The primary outcomes included the risk of overweight/obesity and annual body mass index (BMI) gain. The secondary outcomes included BMI, BMI z-score [created from BMI (kg/m2) according to the 2000 Centers for Disease Control (CDC) growth reference], weight, waist circumference (WC), percent body fat (PBF), fat free mass index (FFMI), fat mass (FM), fat mass index (FMI), and sum of skin-folds (SSF). For multiple publications using data from the same cohort, the one with the longest follow-up period or the largest sample size was selected for this meta-analysis.
Data extraction
Two authors reviewed the literature independently and extracted the information for the meta-analysis following a formal protocol written in advance that clearly stated the objectives, the hypotheses to be tested, the subgroups of interest, and the proposed methods and criteria for identifying and selecting relevant studies and extracting and analyzing information8. Data extraction covered 1) general information of the study: first author’s name, study name (if applicable), year of publication, and country where the study was conducted; 2) characteristics of study population: age, total number of participants, and percent of boys; 3) assessment and categorization of exposure; 4) ascertainment of outcome; 5) covariates adjusted in the analysis; and 6) measures of the association, e.g., odds ratio (ORs) and β coefficients and corresponding 95% confidence intervals (CIs). Discrepancies on literature review and data extraction were resolved by group discussion.
Statistical Analysis
According to the recommendation of the World Health Organization (WHO), overweight was defined as an age and gender specific BMI between the 85th and 95th percentile and obesity was defined as a BMI above the 95th percentile9. The average follow-up time was calculated as the sum of person-years divided by the total number of participants.
To estimate the overall association between sleep duration and risk of overweight/obesity, we used the inverse of variance as the weight to calculate the pooled ORs and 95% CIs comparing the shortest to the longest category of sleep duration. Standard errors (SEs) were derived from the fully adjusted ORs and 95% CIs in the primary studies, which were transformed to natural logarithms (ln). To estimate the association between sleep duration and the continuous outcomes (e.g. annual BMI gain), we pooled the β regression coefficients weighted by the inverse of their variances considering that both exposure (i.e. sleep duration) and outcomes (e. g. annual BMI gain) were measured similarly in the primary studies10. If the information on linear association was not available in the primary study, it would be derived from generalized least-squares for trend test if the number of data points was ≥311, or calculated directly under a linear assumption if the number of data points was <3. If the extreme sleep duration category was open-ended (e.g. ≥12 hours/day), its lower/upper limit was estimated by assuming the range equivalent to its adjacent close-ended category.
To assess heterogeneity among the original studies, we inspected forest plots and conducted a Cochran’s Q test with a P ≤ 0.10 considered as significant heterogeneity. We also computed the I2 statistic to measure the magnitude of heterogeneity. The low, moderate, and high levels of heterogeneity were defined as <30%, 30–50%, and >50%, respectively. Sources of heterogeneity were explored using meta-regression and subgroup analyses with pre-defined factors including age (<3, 3- < 5, ≥5 years), gender, follow-up time (above or below median) and study region (USA vs. non-USA).
Small-study effects or publication bias was assessed by funnel plot asymmetry followed by Egger’s regression asymmetry test (when the number of studies was ≥3) or Begg’s adjusted rank correlation test (when the number of studies was <3). The Duval and Tweedie nonparametric “trim and fill” method was used to adjust for publication bias, if needed12.
Results from a random-effects model were presented as our main findings because we found that there were moderate/high heterogeneities in most of the pooled analyses and publication bias existed in some analyses13. Sensitivity analyses were performed to evaluate the robustness of the findings. Specifically, we determined the effects of a single study on the pooled results by removing one study at a time in the meta-analysis. Also, we explored the possible changes if replacing a random-effects model with a fixed-effects model.
All analyses were performed using STATA statistical software (Version 13.0; STATA Corporation LP, College Station, Texas, USA). A two-sided P value ≤0.05 was considered significant if not specified.
Results
Literature search
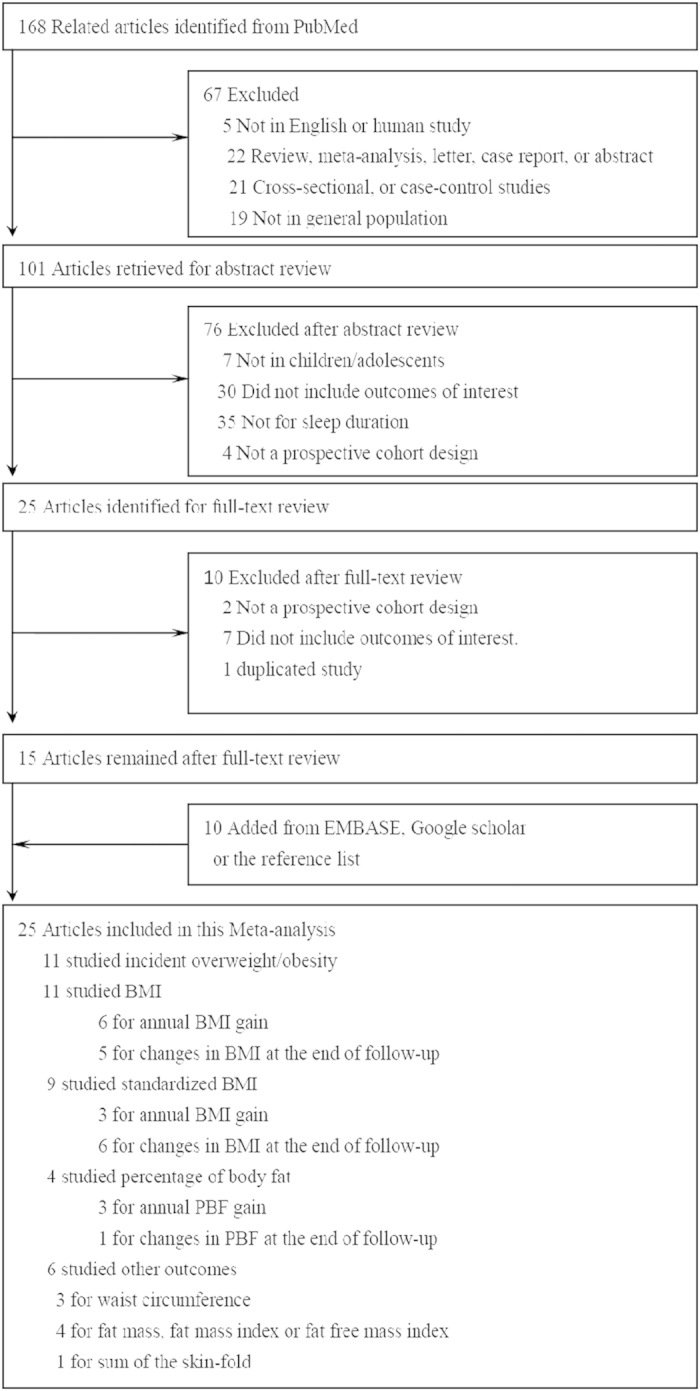
As shown in Figure 1, 168 relevant articles were retrieved from PubMed. Of them, 145 were excluded for one of the following reasons: 1) not in English (n = 5); 2) not original studies (e.g., letter to editor) (n = 22); 3) not prospective cohort studies (n = 26); 4) not in children/adolescents (n = 26); 5) not on sleep duration or no outcome of interest (n = 72); 6) no sufficient information on measures of the association of interest (n = 1). In addition, 10 studies were identified from EMBASE, Google Scholar, or the reference lists of the relevant articles, for a total of 25 eligible studies in the meta-analysis14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38.
Figure 1. Flowchart of study screening and selection.
Characteristics of included studies
Table 1 presents characteristics of the 25 included studies. Eleven studies were conducted in the USA15,16,17,19,20,25,29,31,33,37,38, four in Australia23,28,32,35, two in Canada18,24, two in Denmark30,34, and one in each of the following countries: UK14, Germany22, New Zealand21, Portugal26, Korea27, and Belgium36. Some studies reported results separately based on two19,23,27,30 or three different age groups38, or separately by genders29. We treated them as independent cohorts. In the final dataset, 56,584 children and adolescents from 25 studies (32 independent cohorts), with an average 3.4-year follow-up, were included.
Table 1. Characteristics of the Studies Included in the Meta-analysis.
| Source | Age at baseline | Boys, % | Follow-up, year | No. of Individuals/events | Exposure categories | Exposure assessment | Outcome and its assessment | Adjusted variables | Main results |
|---|---|---|---|---|---|---|---|---|---|
| Reilly, the ALSPC, 2005, UK | 4 months to 5 years | 50.7 | ~5 | 7,758/671 | Quartiles of night sleep duration (hour/day): <10.5; 10.5–10.9; 11–11.9; ≥12.0. | Sleep duration in children aged 30 months was reported by parents. | Obesity: defined as BMI ≥ its 95th percentile. | Maternal education, smoking during pregnancy, age of mother at delivery, gender, birth weight, parity, season of birth, gestational age, no of fetuses, infant feeding, parent obesity, no of siblings, energy intake at 3 years, ethnicity, television watching, time in car per day, and dietary patterns. | Obesity at age 7 [OR (95% CI)]:Q1: 1.45(1.10, 1.89);Q2: 1.35(1.02, 1.79);Q3: 1.04(0.76, 1.42);Q4: 1.00(Referent). |
| Lumeng, the NICHD-SECCYD study, 2007, USA | 9 years | 50.0 | ~3 | 785/139 | Sleep time (hour/day) Sleep time in tertiles | Sleep duration was obtained by maternal report on CSHQ in the 3rd and 6th grades. | Obesity: defined as a BMI of ≥95th percentile. | Gender, race, maternal education, change in sleep duration between 3rd and 6th grades, and the child’s weight status in the 3rd grade. | Obesity in 6th grade [OR (95% CI)]: 0.60(0.36, 0.99).T1: 3.48(1.09, 11.12);T2: 1.00(Referent);T3: 0.75(0.25, 2.30). |
| Snell, the PSID-CDS study, 2007, USA | 3–12 years | 50.0 | ~5 | 2,281/821 | Sleep time(hour/day);Sleep time (hour/day):< 8; 8–8.9; 9–9.9; 10–10.9; ≥11. | The PSID-CDS time diaries were used to measure sleep time. | Standardized BMI by child’s age, gender and adjusted for skew. Overweight: following international guidelines (Cole, 2000). | BMI/overweight at time 1, gender, child’s age at time 1, child’s age at time 2, family income, average parental education in years, and race. | Subsequent age- and gender- standardized BMI (β±SE): −0.115±0.036.0.108±0.165;0.033±0.109;0(Referent);−0.164±0.086;−0.257±0.122.Overweight (β±SE):−0.053±0.017.−0.009±0.073;0.014±0.054;0(Referent);−0.070±0.044;−0.171±0.063. |
| Taveras, the Project Viva, 2008, USA | 6 months to 2 years | 50.0 | 1.75 | 915/82 | Sleep duration (hour/day): <12;≥12. | Sleep duration at children’s age 6 months, 1 year and 2 years were reported by the mothers and weighted to get the average sleep time (hours/day). | BMI z-score; The sum of SS and TR skinfold thicknesses; Obesity: a BMI of ≥95th age- and gender-specific percentile. | Maternal education, income, pre-pregnancy BMI, marital status, prenatal smoking history, breast feeding duration and child’s race/ethnicity, birth weight, 6-month weight-for-length z-score, daily television viewing, and daily active play. | Measures at end of follow-up:BMI z-score [β(95% CI)]:0.16(0.02, 0.29);0(Referent).Sum of SS and TR skinfold thicknesses:0.79(0.18, 1.40);0(Referent).Obesity[OR (95% CI)]:2.04 (1.07, 3.91);1.00(Referent). |
| Touchette, the QLSCD, 2008, Canada | 29 months | 46.8 | ~3.75 | 1,138/159 | Sleep duration patterns: short persistent; short increasing; 10-hour persistent; 11-hour persistent. | Sleep duration was reported at 2.5, 3.5, 4, 5, and 6 years based on the last month by an open question from the sleep-administered questionnaire for mother. | Overweight and obesity were defined according to international standard definitions taking gender and age into account. | Birth weight, prematurity, low birth weight, gender of the child, maternal smoking during pregnancy, weight at 5 months, low parental education, modified family structure, late cereal introduction, not breast-fed, immigrant mother, naptime at 2.5 years, watching television at 6 years, playing video games at 6 years, doing physical activities, overeating at 6 years, snacking at 6 years, eating sweets at 6 years, snoring at 6 years, and low income status at 6 years. | Overweight/obesity at age 6 [OR (95% CI)]:short persistent:4.2(1.6, 11.1);short increasing:2.4(0.9, 6.4);10-hour persistent:1.8(1.1, 2.9);11-hour persistent:1.0 (Referent). |
| Bell, the PSID-CDS study,2010, USA | 0–4 years | 52 | ~5 | 822/271 | Age-specific percentile of sleep duration: <25th ; ≥25th. | The CDS questionnaire | Overweight: BMI>85th and <95th percentile. Obesity: BMI of ≥95th percentile. | Age, gender, birth weight, father present, hours per day of television viewing, birth order, urban residence, child BMI z-score at baseline, race, family income, maternal education, parents’ BMI in 1999, and physical activity. | Overweight/obesity at end of follow-up [OR (95% CI)]:1.80(1.16, 2.80);1.00(Referent). |
| 5–13 years | 50 | ~5 | 1,108/399 | Age-specific percentile of sleep duration: <25th ; ≥25th. | The CDS questionnaire | Overweight: BMI>85th and <95th percentile. Obesity: BMI of ≥95th percentile. | Age, gender, birth weight, father present, hours per day of television viewing, birth order, urban residence, child BMI z-score at baseline, race, family income, maternal education, parents’ BMI in 1999, and physical activity. | Overweight/obesity at end of follow-up [OR (95% CI)]:1.21(0.85, 1.73);1.00(Referent) | |
| Calamaro, the ADD health study, 2010, USA | 16 years | 50.3 | ~2 | 13,568/1,455 | Duration of night sleep (hour/day): <6; 6~; 8~; 11-<14. | Adolescents were asked about the sleep duration during the in-home interview in both waves I and II. | Obesity, defined as BMI> 95th age-specific percentile | Obesity at Wave I, age, gender, race, and parental income. | Obesity at wave II [OR (95% CI)]:1.41(0.87, 2.37);0.86(0.65, 1.14);1.00(Referent);1.15(0.56, 2.33). |
| Diethelm, the DONALD Study, 2010, Germany | ~2 years | 50.3 | ~5 | 481/NA | Sleep duration (hour/day): Consistently short; Inconsistent; Consistently long. | Sleep duration in children was reported by parents. | BMI gain; PBF gain; FFMI gain. | Gender, birth year, birth weight (<3000g) and rapid weight gain (0–18months). | Gains in outcomes of interest from age 2 to 7 (β±SE):BMI:0.12±0.11;−0.03±0.11; 0(Referent).FMI:0.15±0.07;−0.03±0.07; 0(Referent).FFMI:0.02±0.07;0.04±0.07; 0(Referent). |
| Carter, the FLAME study, 2011, New Zealand | 3~5 years | 56.0 | ~3 | 244/60 | Sleep duration (hour/day) | Sleep duration were measured with Mini-Mitter omnidirectional Actical accelerometers attached by belts to the waist for five consecutive days, including two weekend days. | BMI; FMI; FFMI; Overweight (BMI≥85th percentile). | Gender, maternal education, income, BMI, smoking during pregnancy, and income and child’s birth weight, ethnicity, physical activity, television viewing, non-core food intake, fruit and vegetable intake, and outcome of interest at baseline. | BMI at age 7:−0.39(−0.72, −0.06).FMI at age 7:−0.48(−0.86, −0.10).FFMI at age 7;−0.11(−0.29, 0.07).Overweight at age 7:0.44 (0.29, 0.67). |
| Hiscock, the LSAC, 2011, Australia | 0–1 years | 51.0 | 2 | 3,857/NA | Sleep duration (minute/day) | Sleep duration was measured using time-use diary reported by parents after each interview at wave 1 and 2. | BMI z-score: BMI was transferred to BMI z-score using the 2000 CDC growth reference. | Wave 1 gender and weight-for-age z-score. | BMI z-score at wave 2 [β(95%CI)]:−0.0002(−0.0005, 0.0001). |
| 4–5 years | 51.7 | 2 | 3,844/NA | Sleep duration (minute/day) | Sleep duration was measured using time-use diary reported by parents after each interview at wave 1 and 2. | BMI z-score: BMI was transferred to BMI z-score using the 2000 CDC growth reference. | Wave 1 gender and BMI z-score. | BMI z-score at wave 2 [β (95%CI)]:−0.0002 (−0.0005, 0.0001). | |
| Seeger, the QLSCD, 2011, Canada | 10 years | 50.1 | 3 | 1,916/194 | TIB at 10 (continuous); TIB trajectory: Short sleepers; 10.5-hour sleepers; 11-hour sleepers. | Using open-ended questions, mothers were asked about their preadolescents’ bedtimes and waking times on weekdays at 10, 11, 12 and 13 years of age. Sleep duration was estimated as the TIB between bedtime and waking time. | BMI; The international definitions of overweight and obesity for preadolescents were based on BMI curves as a function of gender and age, as defined by Cole et al. | Gender, maternal immigrant status, familial income, birth weight, maternal and paternal educational levels, pubertal status, time spent watching television, and frequency of physical activity. | BMI at age 13 [β(95% CI)]:−0.71(−1.28, −0.14).1.24(0.38, 2.09);0.62(−0.01, 1.26);1.00 (Referent).Overweight at 13 [OR(95%CI)]:1.51(1.28, 1.76);1.99(1.67, 2.37);1.56(1.22, 1.99);1.00(Referent).Obesity [OR(95%CI)]:2.07(1.51, 2.84);2.23(2.18, 2.27);1.26(1.23, 1.29);1.00(Referent). |
| Silva, the TuCASA study, 2011, USA | 6–12 years | 51.0 | 4.8 | 304/106 | Sleep duration (hour/night): ≥9; 7.5–9; <7.5. | Parents were asked to complete SHQs that inquired their children’s sleep history and sleep characteristics. | BMI; Overweight/obesity: BMI ≥85th percentile; Obesity: BMI ≥95th percentiles. | Ethnicity, baseline BMI, anxious/depressed, and learning problems, and age, SDB, and caffeine use at follow-up. | BMI gains [β(95% CI)]:0(Referent);1.06(−0.20, 2.10);1.70(0.40, 3.10).Overweight [OR(95%CI)]:1.0(Referent);1.5(0.69, 3.15);2.2(0.95, 5.09).Obesity [OR(95%CI)]:1.0(Referent);2.0(0.73, 5.64);3.3(1.09, 9.66). |
| Araújo, the EPITeen cohort study, 2012, Portugal | 13 years | 46.5 | ~4 | 1,171/NA | Sleep duration (hour/day) | Sleep duration was estimated by self-reported bedtimes and wake-up times at 17 years. | Change in BMI z-score from age 13 to 17; Change in PBF from age 13 to 17. | Parental education, KIDMED index, BMI z-score at age 13y, and PBF at age 13y. | β(95% CI) of change in BMI z-scores:Girls: 0.039(−0.006, 0.084)Boys: 0.010(−0.044, 0.065)β(95% CI) of change in PBF:Girls: 0.039(−0.139, 0.820)Boys: −0.334(−0.814, 0.146) |
| Klingenberg, the SKOT cohort study, 2012, Denmark | 9 months | 47.6 | 2.25 | 311/NA* | Sleep duration (hour/day) | Sleep duration including daytime napping from questionnaire data (TSD-Q) was based on parental report of time at age 9 months. | BMI z-score; SSF; PBF; FM. | Birth weight, gestational age, duration of breastfeeding, maternal smoking during pregnancy, maternal BMI at 9 months of examination, household income at time of investigation, and educational levels of both parents at time of investigation. | Adiposity at age 3 [β(95% CI)]: BMI z-score:−0.008(−0.13, 0.12).SSF: 0.289(−0.16, 0.73).PBF: −0.001(−0.003, 0.001).FM: −0.140(−0.35, 0.073). |
| 18 months | 47.6 | 1.5 | 311/NA* | Sleep duration (hour/day) | Sleep duration including daytime napping from questionnaire data (TSD-Q) was based on parental report of time at age 18 months. | BMI z-score; SSF; PBF; FM. | Birth weight, gestational age, duration of breastfeeding, maternal smoking during pregnancy and maternal BMI at 9 months of examination, household income at time of investigation, and educational levels of both parents at time of investigation. | Adiposity at age 3 [β(95% CI)]:BMI z-score:−0.010(−0.07, 0.05).SSF: −0.039(−0.24, 0.16).PBF: 0.00005(−0.001, 0.001).FM: 0.024(−0.05, 0.09). | |
| Lee, the Obesity and Metabolic Disorders Cohort in Childhood study, 2012, Korea | 7 years | 47.4 | 2 | 474/NA | Sleep duration (hours/day): <8.5; 8.5–9.5; ≥9.5. | Children and their parents were asked to fill out the questionnaires together about the sleep duration. | BMI gains during 2 year follow-up. | Age, gender, sexual maturation at 6th year follow-up, baseline BMI, exercise, weekly screen time per an hour, household income, maternal BMI, paternal BMI, maternal education, paternal education, maternal job, family structure, energy intake, % of energy intake from fat, meal skipping during a week, and snacking status. | BMI gains[β(95% CI)]:0(Referent);−0.192(−0.543, 0.159);−0.463(−0.871, −0.054). |
| 10 years | 49.3 | 2 | 1,030/NA | Sleep duration (hour/day): <8; 8–9; ≥9. | Children and their parents were asked to fill out the questionnaires together about the sleep duration. | BMI gains during 2 year follow-up. | Age, gender, sexual maturation at 6th year follow-up, baseline BMI exercise, weekly screen time per an hour, household income, maternal BMI, paternal BMI, maternal education, paternal education, maternal job, family structure, energy intake, % of energy intake from fat, meal skipping during a week, and snacking status. | BMI gains[β(95% CI)]:0(Referent);−0.079(−0.321, 0.162);−0.024(−0.236, 0.285). | |
| Lytle_male, The IDEA study and the ECHO study, 2012, USA | 14.7 years | 100 | 2 | 352/NA | Sleep duration (hour/day) | Total sleep duration was assessed via self-report. | BMI gains; PBF gains. | Race, grade, parental education, school lunch, puberty, study, screen time/sedentary behavior, depression, activity, and energy intake. | Gain in Adiposity(β±SE):BMI: −0.091±0.110.PBF: 0.105±0.306. |
| Lytle_female, The IDEA study and the ECHO study, 2012, USA | 14.7 years | 0 | 2 | 371/NA | Sleep duration (hour/day) | Total sleep duration was assessed via self-report. | BMI gains; PBF gains. | Race, grade, parental education, school lunch, puberty, study, screen time/sedentary behavior, depression, activity, and energy intake. | Gain in Adiposity(β±SE):BMI: 0.030±0.094.PBF: 0.259±0.226. |
| O’Dea, 2012, Australia | 7–12 years | 50.8 | 4 | 939/NA | Sleep duration during 4 years of follow-up: Consistently low; Intermediate; Consistently high. | Children and their mother completed an annual questionnaire (telephone interview) to assess usual amount of sleep. | BMI gains. | Age, birth weight, age of mother, maternal BMI, SES, mother smokes, father’s education, ethnicity, and physical activity. | The difference in BMI gains between children with consistently low and high sleep times was 1.00±0.45 kg/m2. |
| Storfer-isser, the CCSHS, 2012, USA | 8–11 years | 100 | ~8 | 157/NA | Sleep duration (hour/day) | Sleep duration was reported by the parents (ages 8–15) or the adolescent (ages 16–19). | Gender- and age-adjusted BMI z-score. | Age, race, low birth weight, low SES, and BMI z-score at baseline. | Subsequent BMI z-score (β±SE):Age 12–15:−0.08±0.08.Age 16–19:−0.06±0.08. |
| 0 | ~8 | 156/NA | Sleep duration (hour/day) | Sleep duration was reported by the parents (ages 8—15) or the adolescent (ages 16–19). | Gender- and age-adjusted BMI z-score. | Age, race, low birth weight, low SES, and BMI z-score at baseline. | Subsequent BMI z-score (β±SE):Age 12–15:0.01±0.07.Age 16–19:0.03±0.07. | ||
| Magee, the LSAC, 2013, Australia | Aged 0–1 years and 4–5 years | 51.1 | 10 | 1,079/NA | Sleep duration (hour/day) | In waves 1, 2, and 3, sleep duration was assessed via time use diaries completed by one of the child’s parents. | BMI | Weekly household income, breastfed or not, the age the child stopped being breastfed completely, birth weight, mother/father education, and gender. | Shorter sleep duration are primarily associated with BMI in children with early onset obesity(a subgroup): Sleep duration at age 6 to 7 was inversely associated with BMI at age 8 to 9 years (β = −0.68, P = 0.017); and sleep duration at age 8 to 9 was inversely associated with BMI at age 10 to 11 years (β = −1.21, P = 0.003). |
| Mitchell, 2013, USA | 14 years | 50 | 3.4 (3–4) | 1,390/NA | Sleep duration (hour/day) | Typical duration of sleep on a school night and on a weekend night was self-reported by the participants. | BMI gains | Gender, race, maternal education, MVPA, and screen time. | 50th percentile of BMI [β(95% CI)]:−0.15(−0.24,−0.06). |
| Hjorth, the OPUS school meal study, 2014, Denmark | 8–11 years | 51.7 | 0.55 | 723/NA | Sleep duration (hour/day) | The parents and children were instructed to keep logs for bedtime (“lights off” and trying to sleep) and waking time (“lights on”) during the week in which the monitor was worn. | Change in WC | Baseline age, gender, pubertal status, gender-pubertal status interaction, days of follow up and baseline WC. | β(95% CI):−0.10(−0.67, 0.46). |
| Magee, the LSAC, 2014, Australia | 4–5 years | 52.4 | 4 | 2,984/NA | Sleep duration (hour/day) | Sleep duration was reported by parents by self-report questionnaires and time use diaries. | BMI | Gender, sleep problems, household income, maternal education, and maternal weight status. | Short sleep duration at age 4 to 5 years was significantly associated with higher BMI at age 8 to 9 years (β = −0.07, P = 0.044), which was slightly attenuated by television viewing at age 6 (β = −0.06, P = 0.076). |
| Michels, Belgian longitudinal ChiBS study, 2014, Belgium. | 6–12 years | 52 | ~2 | 193/NA | Sleep duration (hour/day) | Sleep duration in children was reported by parents using a sleep diary | BMI z-score gains; PBF gains;WC gains. | Age, gender, parental education, physical activity and reported snacking frequency. | Adiposity evolution over 2 years: BMI z-score[β (p-value)]: −0.381(0.030);PBF [β(p-value)]: −2.348 (0.002); WC[β(p-value)]: −1.666(0.016). |
| Scharf, the ECLS-B, 2014, USA | 9 months | 50.9 | 5 | 8,950/NA | Sleep time (hour/day) | The primary care giver (most often the mother) completed a computer-assisted interview at home by trained assessors. | Increases in BMI z-score. | Gender, race/ethnicity, socioeconomic status, and television viewing. | Increases in BMI z-score (beta±SE):−0.0287±0.0127 |
| Taveras, the Project Viva, 2014, USA | 6 months to 2 years | 49.7 | 7.2 | 1,046/116* | Curtailed sleep (hour/day): <12; ≥12. | Mothers reported their baby’s sleep duration in a usual 24-hour period at 6 months and 1 year old. | BMI z-score; FMI; WC; Obesity: BMI for age and gender ≥95th percentiles. | Child’s age and gender, maternal age, education, and parity, household income and child’s race and television viewing at mid-childhood. | BMI z-score[β (95%CI)]:0.15(0.02, 0.28);0(Referent).FMI[β (95%CI)]:0.19(−0.05, 0.43);0(Referent).WC[β (95%CI)]:1.02(0.03, 2.01);0(Referent).Obesity[OR (95% CI)]:1.36(0.84, 2.21);1.00(Referent). |
| 3–4 years | 49.7 | 4.4 | 1,046/116* | Curtailed sleep (hour/day): <10; 10- < 11; ≥11. | Parents reported their children’s sleep duration in a usual 24-hour period on average weekday and weekend day in the past month. | BMI z-score; FMI; WC; Obesity: BMI for age and gender ≥95th percentiles. | Child’s age and gender, maternal age, education, and parity, household income and child’s race and television viewing at mid-childhood. | BMI z-score[β (95%CI)]:0.20(−0.01, 0.40);0.07(−0.07, 0.20);0(Referent).FMI[β (95%CI)]:0.15(−0.25, 0.54);0.07(−0.17, 0.32);0(Referent).WC[β (95%CI)]:0.99(−0.64, 2.62);0.46(−0.57, 1.48);0(Referent).Obesity[OR (95% CI)]:1.27(0.64, 2.52);0.98(0.58, 1.66);1.00(Referent). | |
| 5–7 years | 49.7 | 1.7 | 1,046/116* | Curtailed sleep (hour/day): <9; 9-<10; ≥10. | Mothers reported their children’s sleep duration in a usual 24-hour period on average weekday and weekend day in the past month. | BMI z-score; FMI; WC; Obesity: BMI for age and gender ≥95th percentiles. | Child’s age and gender, maternal age, education, and parity, household income and child’s race and television viewing at mid-childhood. | BMI z-score[β (95%CI)]:0.24(−0.08, 0.56);0.01(−0.15, 0.18);0(Referent).FMI[β (95%CI)]:0.33(−0.32, 0.98);0.05(−0.26, 0.36);0(Referent).WC[β (95%CI)]:1.92(−0.72, 4.56);0.36(−0.94, 1.67);0(Referent).Obesity[OR (95% CI)]:2.12(0.90, 4.98);1.09(0.60, 2.00);1.00(Referent). |
ADD: the National Longitudinal Study of Adolescent Health; ALSPAC : Avon Longitudinal Study of Parents And Children; BMI: body mass index; CCSHS: Cleveland Children’s Sleep and Health Study; CDC: Center of Disease Control; CDS: Child Development Supplement; ChiBS: Children’s Body composition and Stress; CI: confidence interval; CSHQ: Children’s Sleep Habits Questionnaire; DONALD: Dortmund Nutritional and Anthropometric Longitudinally Designed; ECHO: Etiology of ChildHood Obesity; ECLS-B: the Early Childhood Longitudinal Study-Birth Cohort; EPITeen: Epidemiological Investigation of Teenagers Health in Porto; FFMI: fat free mass index; FM: fat mass; FMI: fat mass index; FLAME: Family Lifestyle, Activity, Movement and Eating study; IDEA: International Day for the Evaluation of Abdominal Obesity; IOTF: International Obesity Task Force; KIDMED: Mediterranean Diet Quality Index in Children and Adolescents; LSAC: Longitudinal Study of Australian Children; MVPA: moderate-to-vigorous physical activity; NA: not applicable; NICHD-SECCYD: National Institute of Child Health and Human Development Study of Early Child Care and Youth Development; OPUS: Optimal well-being, development and health for Danish children through a healthy New Nordic Diet; OR: odds ratio; PBF: Percentage body fat; PIAMA: Prevention and Incidence of Asthma and Mite Allergy study; PSID: the Panel Survey of Income Dynamics; QLSCD: Quebec Longitudinal Study of Child Development; SDB: sleep disordered breathing; SES: social economic status; SHQ: sleep habits questionnaire; SKOT: Småbørns Kost Og Trivsel (in Danish, which means “Toddlers Diet And Welfare” in English); SS: subscapular; SSF: sum of the skin-fold; TIB: time in bed; TR: triceps; TuCASA: Tucson Children’s Assessment of Sleep Apnea Study; UK: the United Kingdom; USA: the United States of America; WC: waist circumference.
*The numbers of participants and events, i.e. 1,046/116, are for the whole study across three age groups.
Information on sleep duration and the risk of overweight/obesity were available in 11 studies (14 cohorts)14,15,16,17,18,19,20,21,24,25,38, including 31,185 participants and 4,473 cases with a follow-up range from 21 months to 5 years. Data on sleep duration and annual BMI gain were available in six studies (8 cohorts)22,25,27,28,31,33 including 5,341 participants with a follow-up range from 2 to 5 years.
Sleep duration and risk of overweight/obesity
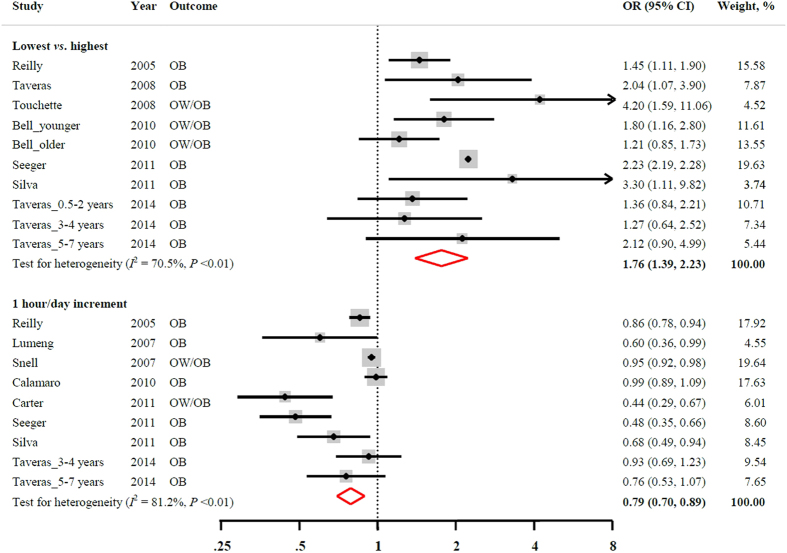
Figure 2 shows the association between sleep duration and the risk of overweight/obesity. By combining data from seven studies (10 independent cohorts), the pooled OR (95% CIs) was 1.76 (95% CI: 1.39, 2.23) for participants in the shortest sleep duration group as compared with those who were in the longest sleep duration group. The heterogeneity was high among studies (I2 = 70.5%, P < 0.01). No strong evidence of publication bias was observed (Egger’s test, P = 0.10).
Figure 2. Multivariable-adjusted OR and 95% CI of overweight/obesity in relation to sleep duration.
The overall estimates are obtained by using a random-effects model. The dots indicate the adjusted ORs comparing the lowest to the highest levels of sleep duration or every 1 hour/day increment in sleep duration. The size of the shaded square is proportional to the weight of each study. The horizontal lines represent 95% CIs. The diamond indicates the pooled OR. CI: confidence interval; OB: obesity; OR: odds ratio; OW: overweight.
For the dose-response relationship, after pooling available data from 8 studies (9 independent cohorts), the risk of overweight/obesity was 21% lower with every 1 hour/day sleep duration increment (combined OR: 0.79; 95% CI: 0.70, 0.89). A high heterogeneity among studies was observed (I2 = 81.2%, P < 0.01). Because Egger’s test indicated a significant publication bias (P = 0.01), the “trim and fill” method was used to adjust for the publication bias. With this adjustment, the pooled linear association was somewhat attenuated and became statistically non-significant (pooled OR: 0.92; 95% CI: 0.81, 1.05).
Sleep duration and annual BMI gain
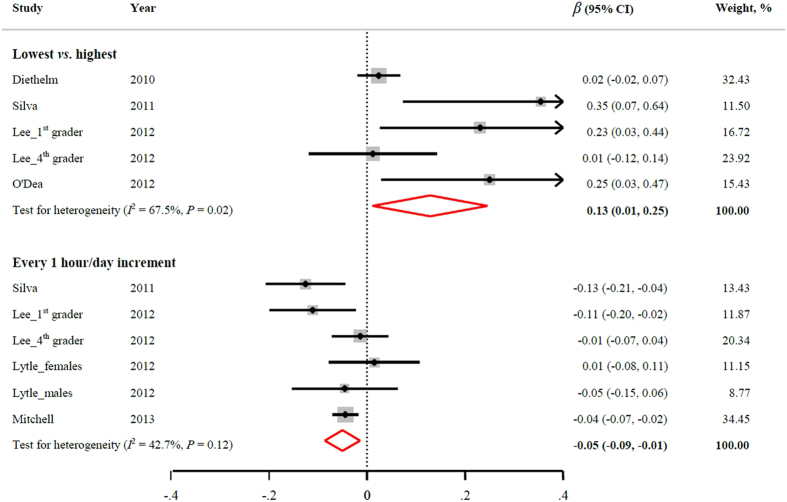
Figure 3 demonstrates the relation between sleep duration and annual BMI gain. Four studies (5 independent cohorts) provided data on the multivariable-adjusted β coefficient (95% CIs) comparing children with the shortest to the longest sleep duration. The pooled results indicated that participants with the shortest sleep duration had significantly more annual BMI gain (β coefficient: 0.13; 95% CI: 0.01, 0.25). High heterogeneity among studies existed (I2 = 67.5%, P = 0.02). The test for publication bias approached significance (Egger’s test, P = 0.054).
Figure 3. Multivariable-adjusted β coefficient and 95% CI of annual BMI gain in relation to sleep duration.
The overall estimates are obtained by using a random-effects model. The dots indicate the adjusted β coefficients comparing the lowest to the highest levels of sleep duration or every 1 hour/day increment in sleep duration. The size of the shaded square is proportional to the weight of each study. The horizontal lines represent 95% CIs. The diamond indicates the pooled β coefficient. BMI: body mass index; CI: confidence interval.
For the dose-response relationship, 4 studies (6 independent cohorts) had data available. Every 1 hour/day sleep duration increment would decrease annual BMI gain by 0.05 kg/m2 (β = −0.05; 95% CI: −0.09, −0.01). A moderate heterogeneity was observed (I2 = 42.7, P = 0.12). There was no evidence indicating publication bias (Egger’s test, P = 0.70).
Subgroup and sensitivity analysis
According to the available data, we examined potential effect modification by study region (USA vs. Non-USA), age (<3, 3 < 5, ≥5 year), or follow-up duration (above or below the median). None of these factors materially modified the observed associations (Table 2). A few studies26,29,31 examined gender difference between sleep duration and BMI z-score or PBF. Although the number of studies is not sufficient for us to pool the results, none of these studies found a significant gender difference.
Table 2. Stratified analyses of the association between sleep duration and risk of overweight/obesity or annual BMI gain.
| Outcome | Sleep duration | Potential modifiers | No of cohorts | No of participants/events | Heterogeneity test | OR/β (95% CI) | Pfor interaction | |
|---|---|---|---|---|---|---|---|---|
| Overweight/Obesity | lowest vs. highest | Baseline age, year | <3 | 5 | 11,679/1,299 | I2 = 28.1%,P = 0.23 | 1.68 (1.30, 2.16) | 0.61 |
| 3~<5 | 1 | 1,046/116 | NA | 1.27 (0.64, 2.52) | ||||
| ≥5 | 4 | 4,374/815 | I2 = 28.1%,P = 0.23 | 1.90 (1.24, 2.91) | ||||
| Follow-up period, year | <3.4 | 3 | 3,877/392 | I2 = 51.0%,P = 0.13 | 1.95 (1.44, 2.65) | 0.34 | ||
| ≥3.4 | 7 | 12,176/1722 | I2 = 35.3%,P = 0.16 | 1.62 (1.26, 2.09) | ||||
| Study location | USA | 7 | 4,195/974 | I2 = 0.0%,P = 0.43 | 1.52 (1.24, 1.86) | 0.29 | ||
| Non-USA | 3 | 10,812/1024 | I2 = 82.3%, P < 0.01 | 2.03 (1.37,3.01) | ||||
| Overweight/Obesity | ↑ 1 hour/day | Baseline age, year | <3 | 1 | 7,758/671 | NA | 0.86 (0.78, 0.94) | 0.74 |
| 3 ~ <5 | 2 | 1,290/176 | I2 = 82.3%,P < 0.01 | 0.65 (0.31, 1.34) | ||||
| ≥5 | 6 | 20,815/2,913 | I2 = 82.3%,P < 0.01 | 0.79 (0.67, 0.92) | ||||
| Follow-up period, year | <3.4 | 4 | 11,389/1,714 | I2 = 87.6%, P < 0.01 | 0.64 (0.44, 0.93) | 0.20 | ||
| ≥3.4 | 5 | 17,559/1,964 | I2 = 63.1%, P < 0.01 | 0.89 (0.80, 0.98) | ||||
| Study location | USA | 6 | 17,984/2,637 | I2 = 89.8%, P < 0.01 | 0.91 (0.83, 0.998) | 0.13 | ||
| Non-USA | 3 | 9,918/925 | I2 = 47.5%,P = 0.09 | 0.58 (0.36, 0.95) | ||||
| Annual BMI gain | lowest vs. highest | Baseline age, year | <3 | 1 | 481/NA | NA | 0.02 (−0.02, 0.07) | 0.51 |
| 3~<5 | 0 | — | — | — | ||||
| ≥5 | 4 | 2,747/NA | I2 = 47.5%,P = 0.09 | 0.19 (0.13, 0.35) | ||||
| Follow-up period, year | <3.4 | 2 | 1,504/NA | I2 = 68.1%,P = 0.08 | 0.11 (−0.11, 0.32) | 0.72 | ||
| ≥3.4 | 3 | 1,724/NA | I2 = 77.3%,P = 0.01 | 0.18 (−0.04, 0.40) | ||||
| Study location | USA | 1 | 304/NA | NA | 0.35 (0.07, 0.64) | 0.26 | ||
| Non-USA | 4 | 2,924/NA | I2 = 60.2%,P = 0.06 | 0.09 (−0.02, 0.19) | ||||
| Annual BMI gain | ↑ 1 hour/day | Baseline age, year | <3 | 0 | — | — | — | — |
| 3 ~ <5 | 0 | — | — | — | ||||
| ≥5 | 6 | 3,921/NA | I2 = 42.7%,P = 0.21 | −0.05 (−0.09, −0.01) | ||||
| Follow-up period, year | <3.4 | 4 | 2,227/NA | I2 = 33.6%,P = 0.21 | −0.04 (−0.09, 0.02) | 0.46 | ||
| ≥3.4 | 2 | 1,694/NA | I2 = 71.6%,P = 0.06 | −0.08 (−0.15, 0.00) | ||||
| Study location | USA | 4 | 2,417/NA | I2 = 44.5%,P = 0.14 | −0.05 (−0.10, −0.00) | 0.97 | ||
| Non-USA | 2 | 1,504/NA | I2 = 69.5%,P = 0.07 | −0.06 (−0.15, 0.04) |
BMI: body mass index; CI: confidence interval; NA: not applicable; OR: odds ratio; USA: the United States of America.
In addition, the results were not appreciably changed when replacing random-effects models with fixed-effects models (data not shown). No single study substantially influenced the pooled results on sleep duration and the risk of overweight/obesity when omitting one study each time in the meta-analysis (Supplemental Table). However, the association between sleep duration and annual BMI gain was substantially attenuated when removing one of three independent cohorts (Silva, 201125, Lee, 201227, or O’Dea, 201228) at a time (Supplemental Table).
Sleep duration and secondary outcomes
Table 3 shows the association between sleep duration and secondary outcomes. Sleep duration was inversely associated with BMI, BMI z-score and WC, and positively related to FMI.
Table 3. The association of sleep duration with secondary outcomes.
| Outcome | Exposure | No. of cohorts | No of participants | β (95% CI) | Heterogeneity test |
|---|---|---|---|---|---|
| BMI, kg/m2 | |||||
| End of follow-up | Lowest vs. highest | 1 | 1,916 | 1.24 (0.39, 2.09) | — |
| End of follow-up | ↑ 1 hour/day | 5 | 5,814 | −0.51 (−0.88, −0.14) | I2 = 83.8%; P < 0.01 |
| BMI (standardized), kg/m2 | |||||
| Annual gain | ↑ 1 hour/day | 3 | 3,438 | −0.02 (−0.06, 0.02) | I2 = 82.8%; P < 0.01 |
| End of follow-up | Lowest vs. highest | 4 | 1,961 | 0.17 (0.08, 0.25) | I2 = 49.6%; P = 0.03 |
| End of follow-up | ↑ 1 hour/day | 11 | 11,652 | −0.04 (−0.07, −0.02) | I2 = 0.0%; P = 0.95 |
| WC, cm | 2 | ||||
| Annual gain | ↑ 1 hour/day | 2 | 916 | −0.40 (−0.06, 0.02) | I2 = 61.5%; P = 0.11 |
| End of follow-up | Lowest vs. highest | 3 | 1,046 | 1.10 (0.29, 1.90) | I2 = 0.0%; P = 0.81 |
| End of follow-up | ↑ 1 hour/day | 2 | 1,046 | −0.54 (−1.06, −0.01) | I2 = 0.0%; P = 0.76 |
| PBF, % | |||||
| Annual gain | ↑ 1 hour/day | 4 | 2,087 | −0.06 (−0.30, 0.18) | I2 = 73.5%; P = 0.01 |
| End of follow-up | ↑ 1 hour/day | 2 | 311 | −0.00 (−0.00, 0.00) | I2 = 0.0%; P = 0.35 |
| FFMI | |||||
| Annual gain | Lowest vs. highest | 1 | 481 | 0.00 (−0.02, 0.03) | — |
| End of follow-up | ↑ 1 hour/day | 1 | 244 | −0.11 (−0.29, 0.07) | — |
| FM | |||||
| End of follow-up | ↑ 1 hour/day | 2 | 311 | −0.03 (−0.17, 0.12) | I2 = 51.8%; P = 0.15 |
| FMI | |||||
| Annual gain | Lowest vs. highest | 1 | 481 | 0.03 (0.003,0.06) | — |
| End of follow-up | Lowest vs. highest | 3 | 1,046 | −0.16 (−0.34, 0.03) | I2 = 47.7%; P = 0.15 |
| End of follow-up | ↑ 1 hour/day | 3 | 1,290 | 0.19 (−0.00, 0.39)* | I2 = 0.0%; P = 0.90 |
| SSF | |||||
| End of follow-up | ↑ 1 hour/day | 2 | 311 | 0.06 (−0.23, 0.36) | I2 = 42.4%; P = 0.19 |
BMI: body mass index; FFMI: fat free mass index; FM: fat mass; FMI: fat mass index; PBF: Percentage body fat; SSF: sum of the skin-fold; WC: waist circumference.
*P = 0.053
Discussion
This meta-analysis of prospective cohort studies provides accumulated evidence supporting the hypothesis that sleep duration in children and/or adolescents is inversely associated with the risk of overweight/obesity in a dose-response manner. This inverse association is not appreciably modified by study region, baseline age or the length of follow-up.
Strengths and limitations
This meta-analysis was based on up-to-date literature with the largest synthesis of prospective cohort studies from various populations. The overall sample size was large (n = 56,584) and the average follow-up period was relatively long (~3.4 years) among children and adolescents. Data for the pooled analysis were derived from fully adjusted models in the primary studies, which should reduce the likelihood of confounding. Also, our conclusions were strengthened by the consistent findings in the binary associations (the shortest vs. the longest sleep duration), the dose-response relationships, and the results of other related anthropometric measures such as annual BMI gain and WC.
A few limitations of this meta–analysis should also be considered. First, because sleep duration was parent- or self-reported, misclassification was possible, though it was likely to be non-differential and may attenuate the observed associations. Second, incident cases of overweight/obesity in the primary studies could not be determined. However, this was a common methodological issue in the studies of childhood obesity. Third, sleep durations were classified differently across the original studies, especially the reference groups were somewhat different. This inconsistency could affect our pooled results. Fourth, the findings could be biased by residual confounding or unmeasured confounders in the primary studies. Fifth, results from some sub-group analyses might not be very robust because of the high heterogeneity across the primary studies. Finally, publication bias was found when assessing linear association between sleep duration and the risk of overweight/obesity. However, the conclusion generally remained after controlling for the publication bias using Duval and Tweedie’s “trim and fill” method.
Comparison with previous reviews or meta-analyses
A few previous narrative or systematic reviews found an inverse association between sleep duration and risk of obesity or weight gains among children and adolescents6,39,40,41,42. However, these reviews did not conduct any quantitative analysis. A meta-analysis published in 2008 found that children or adolescents with shorter sleep duration had a 58% higher risk of overweight/obesity43. Of note, nine out of eleven studies included in that meta-analysis were cross-sectional, and only 2 were longitudinal studies. Similar results were reported in the same year in another meta-analysis, which included 12 cross-sectional studies5. A recently published meta-analysis focused on longitudinal studies in children and adolescents44, but this analysis did not examine the dose-response relationship and other related anthropometric parameters. Thus, the present study certainly contributes important additional information to the literature.
Potential mechanisms
The etiology of obesity is multifactorial, in which genetic45, metabolic46, environmental47, behavioral48, and social or cultural factors49,50 are major contributors. Although the exact mechanism remains mysterious, there are several possible pathways that could explain the inverse association between sleep duration and the risk of obesity/overweight. First, sleep has a beneficial effect on the sympathetic nervous system and hypothalamic hormones6. For example, sleep deprivation is associated with low levels of leptin and high levels of ghrelin, which suggests an important role in appetite regulation51,52. Sleep restriction is also associated with an increase in cortisol levels, which promotes increased food intake and the accumulation of visceral fat6. Second, sleep restriction or deprivation may lead to reduced energy expenditure by reducing thyroid-stimulating hormone (TSH), and therefore reducing basal metabolic rate, or by breaking the balance of neural circuits that maintain body weight. Third, sleep restriction can contribute to obesity by promoting waking behavior that causes weight gain. For instance, increased waking hours may provide more opportunities for an individual to eat more energy dense foods53,54. Also, lack of sleep is associated with sedentary activities such as television watching that might lead to weight gain due to increased snacking35. In addition, people with sleep restriction often experience fatigue and sleepiness throughout the day, which may cause a decrease in physical activity53. It is also possible that people with short sleep duration might drink/eat more high-energy drinks/foods to conquer fatigue53.
Summary
In conclusion, this meta-analysis of prospective cohort studies, based on up-to-date literature, provides moderate evidence that sleep duration may be inversely and longitudinally associated with the risk of overweight/obesity in children and adolescents. To prevent childhood obesity and, thereafter, chronic diseases, a certain amount of sleep time for children and adolescents should be recommended. Since a randomized clinical trial on sleep duration may not be feasible due to ethical and practical considerations, further prospective cohort studies with longer follow-up periods, valid objective measures of sleep duration and dynamic sleep quality, as well as multiple measures of body composition, are warranted to further explore age and gender specified optimal sleep duration, and ideal sleep pattern (e.g., sleep timing and chronotype) in terms of weight maintenance.
Additional Information
How to cite this article: Ruan, H. et al. Habitual Sleep Duration and Risk of Childhood Obesity: Systematic Review and Dose-response Meta-analysis of Prospective Cohort Studies. Sci. Rep. 5, 16160; doi: 10.1038/srep16160 (2015).
Supplementary Material
Acknowledgments
The work was supported by grants from the Programs of Shanghai Public Health Promotion (2011–2013). The authors thank all the colleagues for their support on this research.
Footnotes
Author Contributions The authors’ responsibilities were as follows —Q.T. funding and administrative support; K.H. and Q.T. study concept and design; H.R. and P.X.: literature search, study selection, data extraction; P.X. statistical analyses; P.X. and H.R. prepared the tables and figures; H.R., P.X. and K.H. drafting the original manuscript; W.C., K.H. and Q.T. responsible for supervision. All the authors completely consented with all the data in the study, critically received the manuscript for important intellectual content and approved the final manuscript. Q.T. and K.H. had the primary responsibility for final manuscript.
References
- Kahn S. E., Hull R. L. & Utzschneider K. M. Mechanisms linking obesity to insulin resistance and type 2 diabetes. Nature 444, 840–846 (2006). [DOI] [PubMed] [Google Scholar]
- Greenberg A. S. & McDaniel M. L. Identifying the links between obesity, insulin resistance and beta-cell function: potential role of adipocyte-derived cytokines in the pathogenesis of type 2 diabetes. Eur J Clin Invest 32 Suppl 3, 24–34 (2002). [DOI] [PubMed] [Google Scholar]
- Ziyyat A. et al. Epidemiology of hypertension and its relationship with type 2 diabetes and obesity in eastern Morocco. Springerplus 3, 644 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boodai S. A., Cherry L. M., Sattar N. A. & Reilly J. J. Prevalence of cardiometabolic risk factors and metabolic syndrome in obese Kuwaiti adolescents. Diabetes Metab Syndr Obes 7, 505–511 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cappuccio F. P. et al. Meta-analysis of short sleep duration and obesity in children and adults. SLEEP 31, 619–626 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thind H. et al. Does short sleep lead to obesity among children and adolescents?: Current understanding and implications. Am J Lifestyle Med (2014), doi: 10.1177/1559827614533911. [DOI] [Google Scholar]
- Stroup D. F. et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA 283, 2008–2012 (2000). [DOI] [PubMed] [Google Scholar]
- Egger M., Smith G. D. & Phillips A. N. Meta-analysis: principles and procedures. BMJ 315, 1533–1537 (1997). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Must A., Dallal G. E. & Dietz W. H. Reference data for obesity: 85th and 95th percentiles of body mass index (wt/ht2) and triceps skinfold thickness. Am J Clin Nutr 53, 839–846 (1991). [DOI] [PubMed] [Google Scholar]
- Becker B. J. & Wu M. J. The Synthesis of Regression Slopes in Meta-Analysis. Res Synth Methods 22, 414–429 (2007). [Google Scholar]
- Greenland S. & Longnecker M. P. Methods for trend estimation from summarized dose-response data, with applications to meta-analysis. Am J Epidemiol 135, 1301–1309 (1992). [DOI] [PubMed] [Google Scholar]
- Duval S. & Tweedie R. A Nonparametric “Trim and Fill” Method of Accounting for Publication Bias in Meta-Analysis. Journal of the American Statistical Association 95, 89–98 (2000). [Google Scholar]
- Poole C. & Greenland S. Random-effects meta-analyses are not always conservative. Am J Epidemiol 150, 469–475 (1999). [DOI] [PubMed] [Google Scholar]
- Reilly J. J. et al. Early life risk factors for obesity in childhood: cohort study. BMJ 330, 1357 (2005). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lumeng J. C. et al. Shorter sleep duration is associated with increased risk for being overweight at ages 9 to 12 years. Pediatrics 120, 1020–1029 (2007). [DOI] [PubMed] [Google Scholar]
- Snell E. K., Adam E. K. & Duncan G. J. Sleep and the body mass index and overweight status of children and adolescents. Child Dev 78, 309–323 (2007). [DOI] [PubMed] [Google Scholar]
- Taveras E. M., Rifas-Shiman S. L., Oken E., Gunderson E. P. & Gillman M. W. Short sleep duration in infancy and risk of childhood overweight. Arch Pediatr Adolesc Med 162, 305–311 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Touchette E. et al. Associations between sleep duration patterns and overweight/obesity at age 6. SLEEP 31, 1507–1514 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell J. F. & Zimmerman F. J. Shortened nighttime sleep duration in early life and subsequent childhood obesity. Arch Pediatr Adolesc Med 164, 840–845 (2010). [DOI] [PubMed] [Google Scholar]
- Calamaro C. J. et al. Shortened sleep duration does not predict obesity in adolescents. J Sleep Res 19, 559–566 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carter P. J., Taylor B. J., Williams S. M. & Taylor R. W. Longitudinal analysis of sleep in relation to BMI and body fat in children: the FLAME study. BMJ 342, d2712 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diethelm K., Bolzenius K., Cheng G., Remer T. & Buyken A. E. Longitudinal associations between reported sleep duration in early childhood and the development of body mass index, fat mass index and fat free mass index until age 7. Int J Pediatr Obes 6, e114–123 (2011). [DOI] [PubMed] [Google Scholar]
- Hiscock H., Scalzo K., Canterford L. & Wake M. Sleep duration and body mass index in 0–7-year olds. Arch Dis Child 96, 735–739 (2011). [DOI] [PubMed] [Google Scholar]
- Seegers V. et al. Short sleep duration and body mass index: a prospective longitudinal study in preadolescence. Am J Epidemiol 173, 621–629 (2011). [DOI] [PubMed] [Google Scholar]
- Silva G. E. et al. Longitudinal association between short sleep, body weight, and emotional and learning problems in Hispanic and Caucasian children. SLEEP 34, 1197–1205 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Araujo J., Severo M. & Ramos E. Sleep duration and adiposity during adolescence. Pediatrics 130, e1146–1154 (2012). [DOI] [PubMed] [Google Scholar]
- Lee H. H. et al. Factors related to body mass index and body mass index change in korean children: preliminary results from the obesity and metabolic disorders cohort in childhood. Korean J Fam Med 33, 134–143 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Dea J. A., Dibley M. J. & Rankin N. M. Low sleep and low socioeconomic status predict high body mass index: a 4-year longitudinal study of Australian schoolchildren. Pediatr Obes 7, 295–303 (2012). [DOI] [PubMed] [Google Scholar]
- Storfer-Isser A., Patel S. R., Babineau D. C. & Redline S. Relation between sleep duration and BMI varies by age and sex in youth age 8-19. Pediatr Obes 7, 53–64 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klingenberg L. et al. No relation between sleep duration and adiposity indicators in 9–36 months old children: the SKOT cohort. Pediatr Obes 8, e14–18 (2013). [DOI] [PubMed] [Google Scholar]
- Lytle L. A. et al. Examining the longitudinal relationship between change in sleep and obesity risk in adolescents. Health Educ Behav 40, 362–370 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magee C. A., Caputi P. & Iverson D. C. The longitudinal relationship between sleep duration and body mass index in children: a growth mixture modeling approach. J Dev Behav Pediatr 34, 165–173 (2013). [DOI] [PubMed] [Google Scholar]
- Mitchell J. A., Rodriguez D., Schmitz K. H. & Audrain-McGovern J. Sleep duration and adolescent obesity. Pediatrics 131, e1428–1434 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hjorth M. F. et al. Low physical activity level and short sleep duration are associated with an increased cardio-metabolic risk profile: a longitudinal study in 8–11 year old Danish children. PLOS ONE 9, e104677 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magee C., Caputi P. & Iverson D. Lack of sleep could increase obesity in children and too much television could be partly to blame. Acta Paediatr 103, e27–31 (2014). [DOI] [PubMed] [Google Scholar]
- Michels N., Verbeiren A., Ahrens W., De Henauw S. & Sioen I. Children’s sleep quality: relation with sleep duration and adiposity. Public Health 128, 488–490 (2014). [DOI] [PubMed] [Google Scholar]
- Scharf R. J. & DeBoer M. D. Sleep timing and longitudinal weight gain in 4- and 5-year-old children. Pediatr Obes 10, 141–148 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taveras E. M., Gillman M. W., Pena M. M., Redline S. & Rifas-Shiman S. L. Chronic sleep curtailment and adiposity. Pediatrics 133, 1013–1022 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel SRPatel S. R. & Hu F. B. Short sleep duration and weight gain: a systematic review. Obesity (Silver Spring) 16, 643–653 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshall N. S., Glozier N. & Grunstein R. R. Is sleep duration related to obesity? A critical review of the epidemiological evidence. Sleep Med Rev 12, 289–298 (2008). [DOI] [PubMed] [Google Scholar]
- Magee L. & Hale L. Longitudinal associations between sleep duration and subsequent weight gain: a systematic review. Sleep Med Rev 16, 231–241 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guidolin M. & Gradisar M. Is shortened sleep duration a risk factor for overweight and obesity during adolescence? A review of the empirical literature. Sleep Med 13, 779–786 (2012). [DOI] [PubMed] [Google Scholar]
- Chen X., Beydoun M. A. & Wang Y. Is sleep duration associated with childhood obesity? A systematic review and meta-analysis. Obesity (Silver Spring) 16, 265–274 (2008). [DOI] [PubMed] [Google Scholar]
- Fatima Y., Doi S. A. & Mamun A. A. Longitudinal impact of sleep on overweight and obesity in children and adolescents: a systematic review and bias-adjusted meta-analysis. Obes Rev 16, 137–149 (2015). [DOI] [PubMed] [Google Scholar]
- Allison D. B. et al. The heritability of body mass index among an international sample of monozygotic twins reared apart. Int J Obes Relat Metab Disord 20, 501–506 (1996). [PubMed] [Google Scholar]
- Hamilton M. T., Hamilton D. G. & Zderic T. W. Role of low energy expenditure and sitting in obesity, metabolic syndrome, type 2 diabetes, and cardiovascular disease. Diabetes 56, 2655–2667 (2007). [DOI] [PubMed] [Google Scholar]
- Appelhans B. M. et al. The home environment and childhood obesity in low-income households: indirect effects via sleep duration and screen time. BMC Public Health 14, 1160 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birch L. L. & Davison K. K. Family environmental factors influencing the developing behavioral controls of food intake and childhood overweight. Pediatr Clin North Am 48, 893–907 (2001). [DOI] [PubMed] [Google Scholar]
- O’Dea J. A. & Dibley M. J. Prevalence of obesity, overweight and thinness in Australian children and adolescents by socioeconomic status and ethnic/cultural group in 2006 and 2012. Int J Public Health 59, 819–828 (2014). [DOI] [PubMed] [Google Scholar]
- O’Dea J. A. Gender, ethnicity, culture and social class influences on childhood obesity among Australian schoolchildren: implications for treatment, prevention and community education. Health Soc Care Community 16, 282–290 (2008). [DOI] [PubMed] [Google Scholar]
- Chaput J. P., Despres J. P., Bouchard C. & Tremblay A. Short sleep duration is associated with reduced leptin levels and increased adiposity: Results from the Quebec family study. Obesity (Silver Spring) 15, 253–261 (2007). [DOI] [PubMed] [Google Scholar]
- Taheri S., Lin L., Austin D., Young T. & Mignot E. Short sleep duration is associated with reduced leptin, elevated ghrelin, and increased body mass index. PLoS Med 1, e62 (2004). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaput J. P. Short sleep duration promoting overconsumption of food: A reward-driven eating behavior? SLEEP 33, 1135–1136 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nedeltcheva A. V. et al. Sleep curtailment is accompanied by increased intake of calories from snacks. Am J Clin Nutr 89, 126–133 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.