Abstract
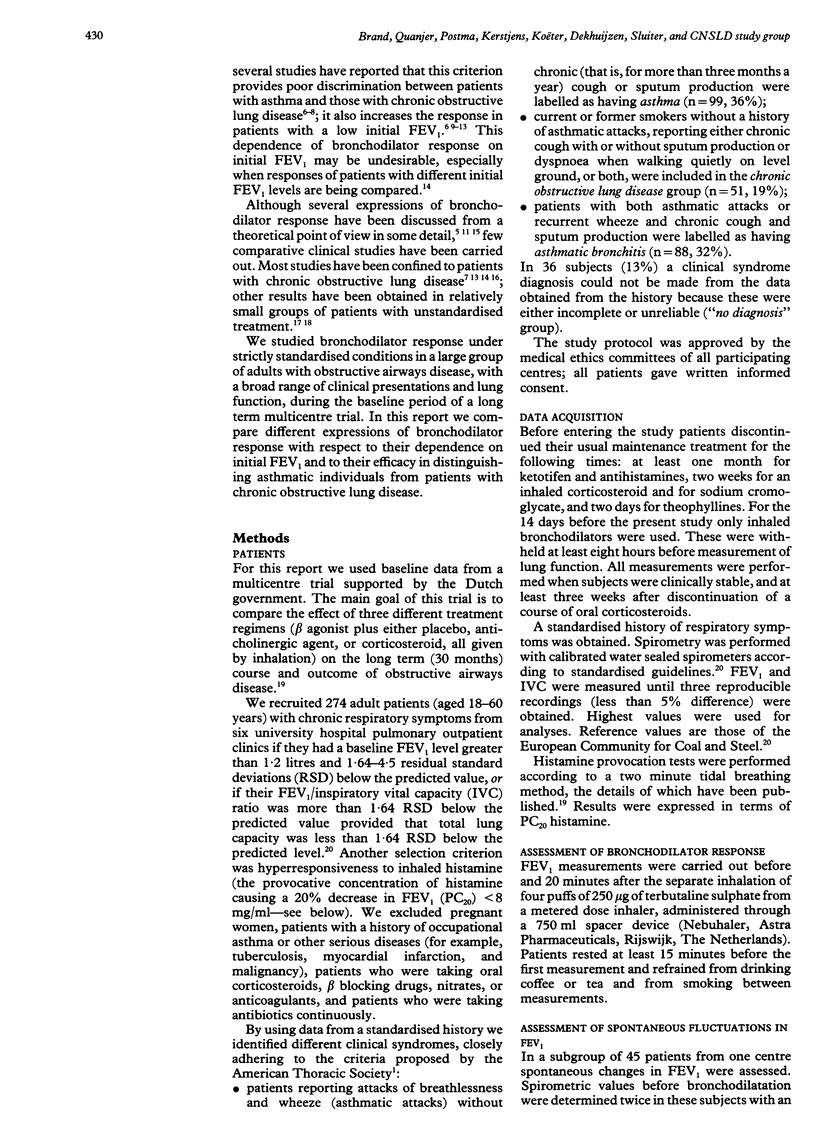
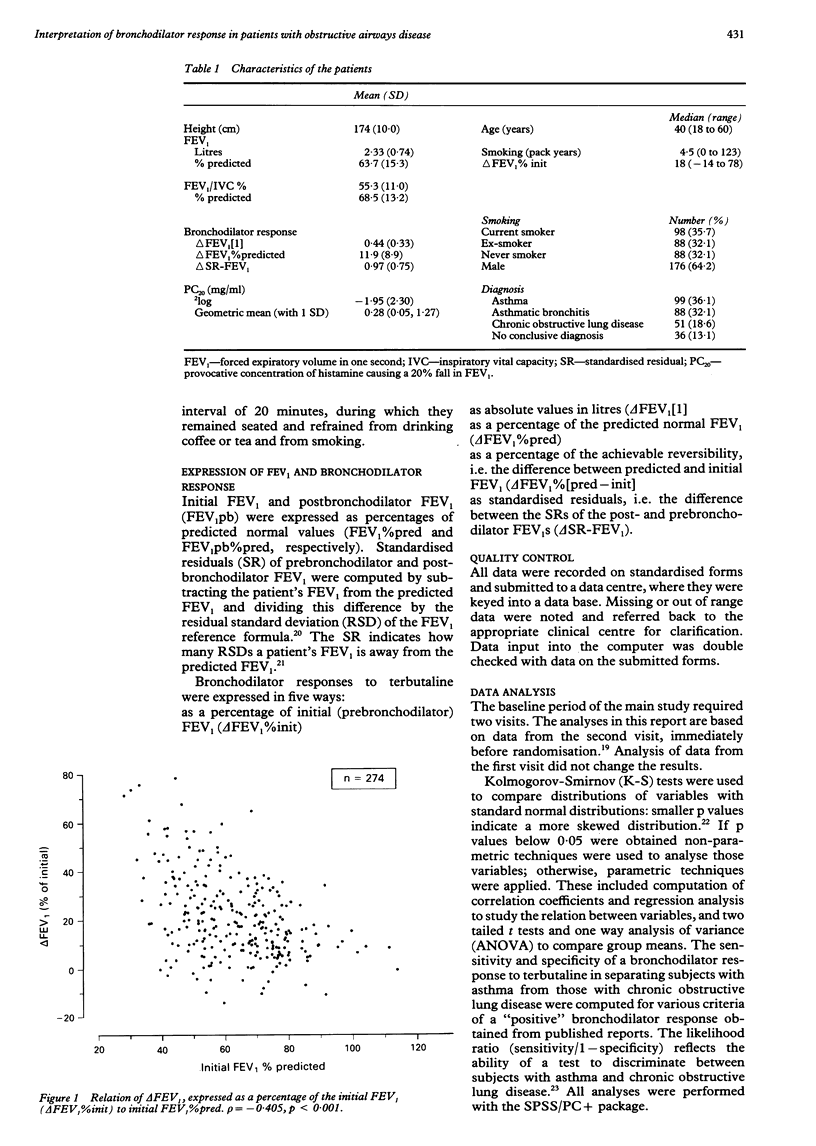
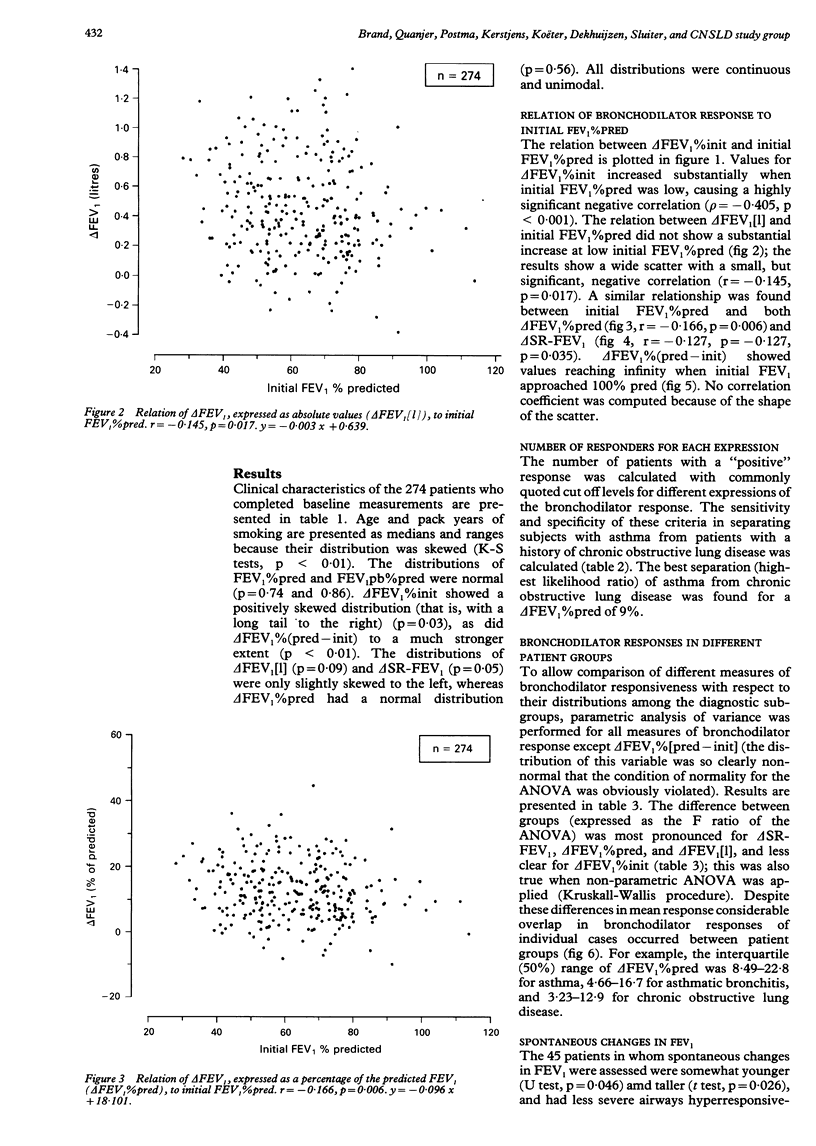
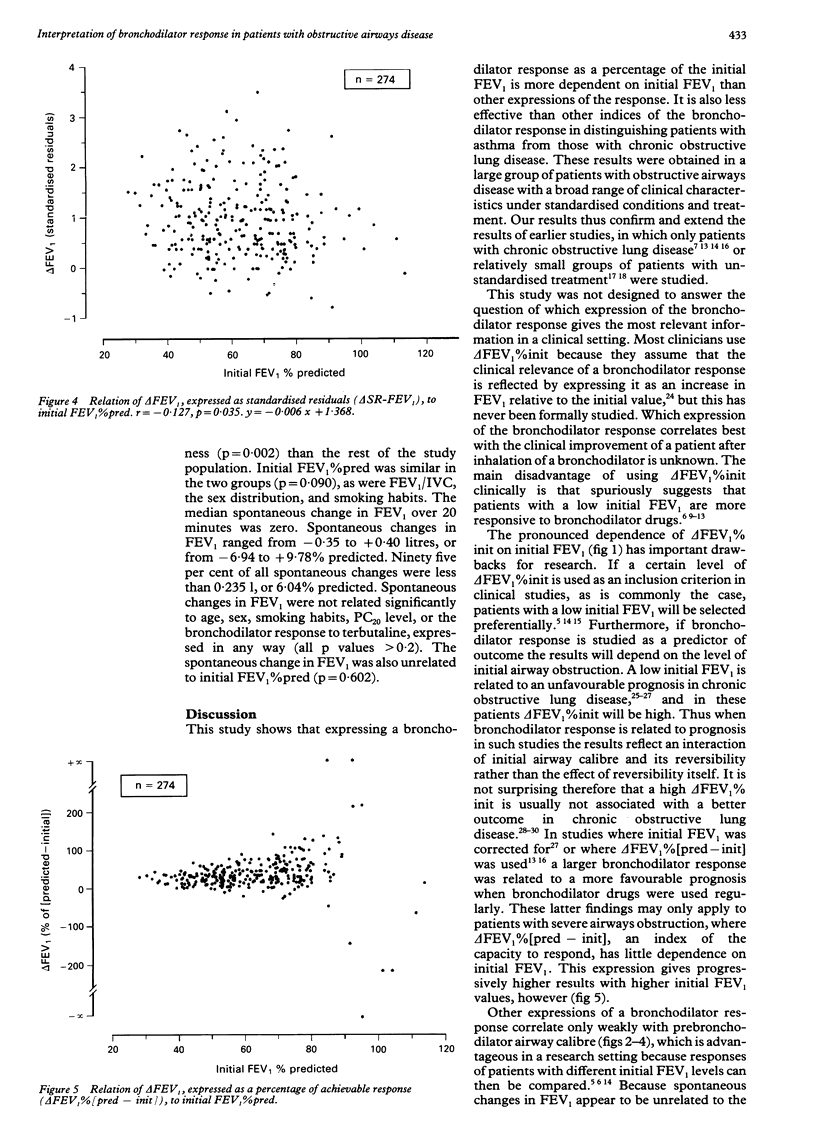
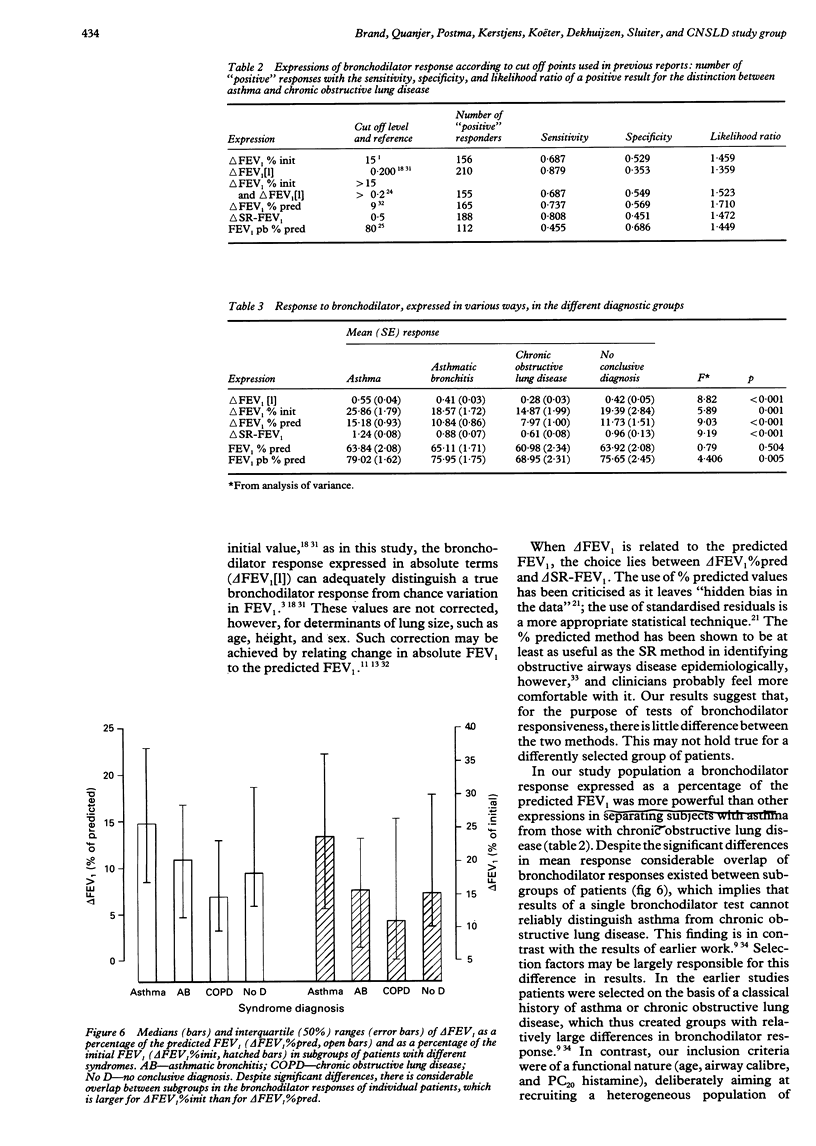
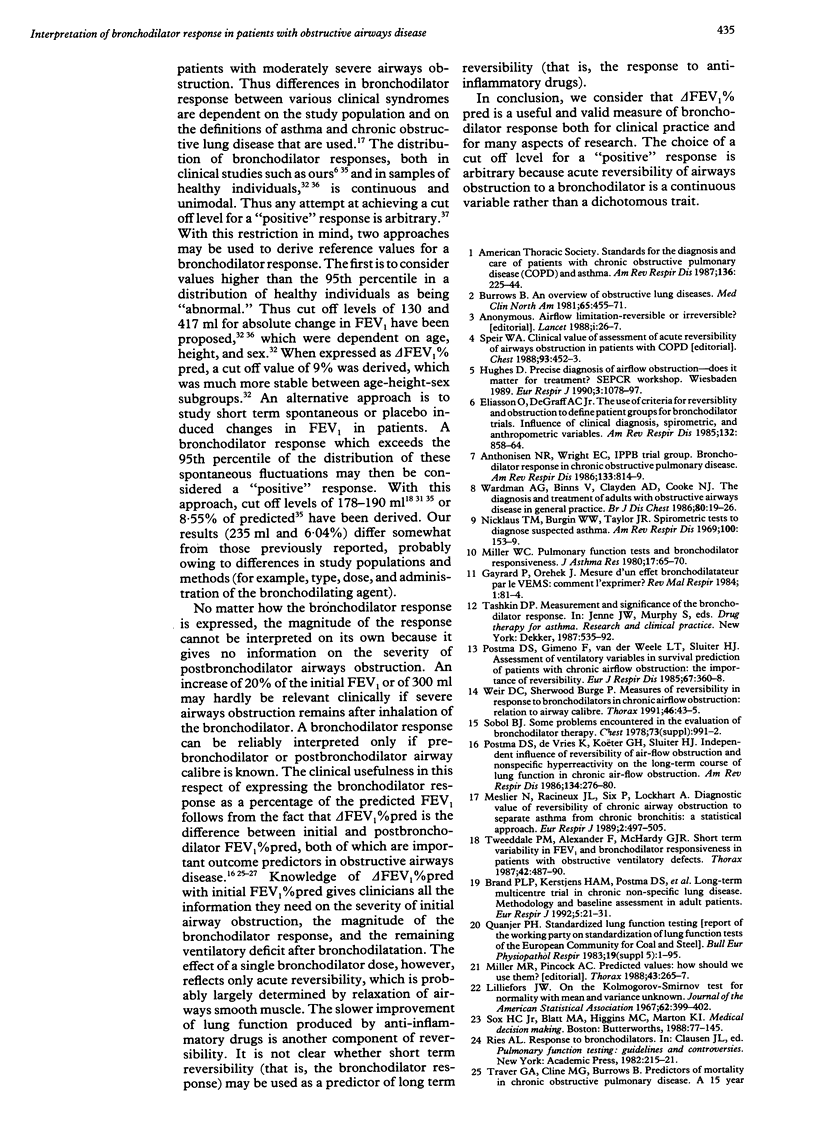
BACKGROUND: There is no agreement on how a bronchodilator response should be expressed. Ideally, the index used should be able to distinguish asthma from chronic obstructive lung disease and be independent of initial FEV1. METHODS: Two hundred and seventy four adults (aged 18-60 years) outpatients with obstructive airways disease were studied. Patients were divided into syndrome groups on the basis of a standardised history: asthma (n = 99), asthmatic bronchitis (n = 88), and chronic obstructive lung disease (n = 51); 36 subjects could not be attributed to any subgroup. FEV1 was measured before and 20 minutes after inhalation of 1000 micrograms terbutaline. Different expressions of bronchodilator response (delta FEV1) were compared with respect to their dependence on initial FEV1 and their efficacy in separating subjects with asthma from those with chronic obstructive lung disease. delta FEV1 was expressed as a percentage of initial FEV1 (delta FEV1%init), absolute value (delta FEV1[1]), percentage of predicted FEV1 (delta FEV1%pred), standardised residual (delta SR-FEV1), and percentage of maximal possible increase (delta FEV1%[pred-init]). RESULTS: delta FEV1%init was more dependent on initial FEV1 (p = -0.405) than delta FEV1[1] (r = -0.145), delta FEV1%pred (r = -0.166), and delta SR-FEV1 (r = -0.127). delta FEV1%[pred-init] reached infinity when initial FEV1 approached predicted levels. delta FEV1%pred had a higher likelihood ratio (1.71) for separating patients with asthma from those with chronic obstructive lung disease than other expressions of bronchodilator response. Asthmatic patients had larger mean bronchodilator responses than patients in other subgroups; this difference was largest for delta SR-FEV1 (F = 9.19) and delta FEV1%pred (F = 9.03); it was much smaller for delta FEV1%init (F = 5.89). Despite significant differences in mean response, there was a large overlap of individual responses between diagnostic subgroups. The bronchodilator response was continuously and unimodally distributed for all expressions. CONCLUSIONS: delta FEV1%pred appears to be the most useful method of expressing bronchodilator response, both for clinical and for research purposes. Reversibility of airways obstruction in response to a bronchodilator is a continuous variable and not a dichotomous triat. Any cut off level of a "positive" bronchodilator response is therefore arbitrary.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Anthonisen N. R., Wright E. C. Bronchodilator response in chronic obstructive pulmonary disease. Am Rev Respir Dis. 1986 May;133(5):814–819. [PubMed] [Google Scholar]
- Anthonisen N. R., Wright E. C., Hodgkin J. E. Prognosis in chronic obstructive pulmonary disease. Am Rev Respir Dis. 1986 Jan;133(1):14–20. doi: 10.1164/arrd.1986.133.1.14. [DOI] [PubMed] [Google Scholar]
- Brand P. L., Kerstjens H. A., Postma D. S., Sterk P. J., Quanjer P. H., Sluiter H. J., Dijkman J. H., van Herwaarden C. L., Hilvering C., Jansen H. M. Long-term multicentre trial in chronic nonspecific lung disease: methodology and baseline assessment in adult patients. Dutch CNSLD Study Group. Eur Respir J. 1992 Jan;5(1):21–31. [PubMed] [Google Scholar]
- Burrows B. An overview of obstructive lung diseases. Med Clin North Am. 1981 May;65(3):455–471. doi: 10.1016/s0025-7125(16)31509-7. [DOI] [PubMed] [Google Scholar]
- Burrows B., Earle R. H. Course and prognosis of chronic obstructive lung disease. A prospective study of 200 patients. N Engl J Med. 1969 Feb 20;280(8):397–404. doi: 10.1056/NEJM196902202800801. [DOI] [PubMed] [Google Scholar]
- Dales R. E., Spitzer W. O., Tousignant P., Schechter M., Suissa S. Clinical interpretation of airway response to a bronchodilator. Epidemiologic considerations. Am Rev Respir Dis. 1988 Aug;138(2):317–320. doi: 10.1164/ajrccm/138.2.317. [DOI] [PubMed] [Google Scholar]
- Gayrard P., Orehek J. Mesure d'un effet bronchodilatateur par le VEMS: comment l'exprimer? Rev Mal Respir. 1984;1(2):81–84. [PubMed] [Google Scholar]
- Kanner R. E. The relationship between airways responsiveness and chronic airflow limitation. Chest. 1984 Jul;86(1):54–57. doi: 10.1378/chest.86.1.54. [DOI] [PubMed] [Google Scholar]
- Kawakami Y., Kishi F., Dohsaka K., Nishiura Y., Suzuki A. Reversibility of airway obstruction in relation to prognosis in chronic obstructive pulmonary disease. Chest. 1988 Jan;93(1):49–53. doi: 10.1378/chest.93.1.49. [DOI] [PubMed] [Google Scholar]
- Lorber D. B., Kaltenborn W., Burrows B. Responses to isoproterenol in a general population sample. Am Rev Respir Dis. 1978 Nov;118(5):855–861. doi: 10.1164/arrd.1978.118.5.855. [DOI] [PubMed] [Google Scholar]
- Meslier N., Racineux J. L., Six P., Lockhart A. Diagnostic value of reversibility of chronic airway obstruction to separate asthma from chronic bronchitis: a statistical approach. Eur Respir J. 1989 Jun;2(6):497–505. [PubMed] [Google Scholar]
- Miller M. R., Pincock A. C. Predicted values: how should we use them? Thorax. 1988 Apr;43(4):265–267. doi: 10.1136/thx.43.4.265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller W. C. Pulmonary function tests and bronchodilator responsiveness. J Asthma Res. 1980 Jan;17(2):65–70. doi: 10.3109/02770908009105682. [DOI] [PubMed] [Google Scholar]
- Nicklaus T. M., Burgin W. W., Jr, Taylor J. R. Spirometric tests to diagnose suspected asthma. Am Rev Respir Dis. 1969 Aug;100(2):153–159. doi: 10.1164/arrd.1969.100.2.153. [DOI] [PubMed] [Google Scholar]
- Oliver L. C., Eisen E. A., Sprince N. L. A comparison of two definitions of abnormality on pulmonary outcome in epidemiologic studies. Am Rev Respir Dis. 1986 May;133(5):825–829. [PubMed] [Google Scholar]
- Petrie G. R., Palmer K. N. Comparison of aerosol ipratropium bromide and salbutamol in chronic bronchitis and asthma. Br Med J. 1975 Feb 22;1(5955):430–432. doi: 10.1136/bmj.1.5955.430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Postma D. S., Gimeno F., van der Weele L. T., Sluiter H. J. Assessment of ventilatory variables in survival prediction of patients with chronic airflow obstruction: the importance of reversibility. Eur J Respir Dis. 1985 Nov;67(5):360–368. [PubMed] [Google Scholar]
- Postma D. S., de Vries K., Koëter G. H., Sluiter H. J. Independent influence of reversibility of air-flow obstruction and nonspecific hyperreactivity on the long-term course of lung function in chronic air-flow obstruction. Am Rev Respir Dis. 1986 Aug;134(2):276–280. doi: 10.1164/arrd.1986.134.2.276. [DOI] [PubMed] [Google Scholar]
- Pride N. B., Vermeire P., Allegra L. Diagnostic labels applied to model case histories of chronic airflow obstruction. Responses to a questionnaire in 11 North American and Western European countries. Eur Respir J. 1989 Sep;2(8):702–709. [PubMed] [Google Scholar]
- Sobol B. J. Some problems encountered in the evaluation of bronchodilator therapy. Chest. 1978 Jun;73(6 Suppl):991–992. [PubMed] [Google Scholar]
- Sourk R. L., Nugent K. M. Bronchodilator testing: confidence intervals derived from placebo inhalations. Am Rev Respir Dis. 1983 Jul;128(1):153–157. doi: 10.1164/arrd.1983.128.1.153. [DOI] [PubMed] [Google Scholar]
- Speir W. A., Jr Clinical value of assessment of acute reversibility of airways obstruction in patients with COPD. Chest. 1988 Mar;93(3):452–453. doi: 10.1378/chest.93.3.452. [DOI] [PubMed] [Google Scholar]
- Standardized lung function testing. Report working party. Bull Eur Physiopathol Respir. 1983 Jul;19 (Suppl 5):1–95. [PubMed] [Google Scholar]
- Traver G. A., Cline M. G., Burrows B. Predictors of mortality in chronic obstructive pulmonary disease. A 15-year follow-up study. Am Rev Respir Dis. 1979 Jun;119(6):895–902. doi: 10.1164/arrd.1979.119.6.895. [DOI] [PubMed] [Google Scholar]
- Tweeddale P. M., Alexander F., McHardy G. J. Short term variability in FEV1 and bronchodilator responsiveness in patients with obstructive ventilatory defects. Thorax. 1987 Jul;42(7):487–490. doi: 10.1136/thx.42.7.487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tweeddale P. M., Merchant S., Leslie M., Alexander F., McHardy G. J. Short term variability in FEV1: relation to pretest activity, level of FEV1, and smoking habits. Thorax. 1984 Dec;39(12):928–932. doi: 10.1136/thx.39.12.928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vollmer W. M., Johnson L. R., Buist A. S. Relationship of response to a bronchodilator and decline in forced expiratory volume in one second in population studies. Am Rev Respir Dis. 1985 Dec;132(6):1186–1193. doi: 10.1164/arrd.1985.132.6.1186. [DOI] [PubMed] [Google Scholar]
- Wardman A. G., Binns V., Clayden A. D., Cooke N. J. The diagnosis and treatment of adults with obstructive airways disease in general practice. Br J Dis Chest. 1986 Jan;80(1):19–26. doi: 10.1016/0007-0971(86)90005-7. [DOI] [PubMed] [Google Scholar]
- Weir D. C., Sherwood Burge P. Measures of reversibility in response to bronchodilators in chronic airflow obstruction: relation to airway calibre. Thorax. 1991 Jan;46(1):43–45. doi: 10.1136/thx.46.1.43. [DOI] [PMC free article] [PubMed] [Google Scholar]


