Abstract
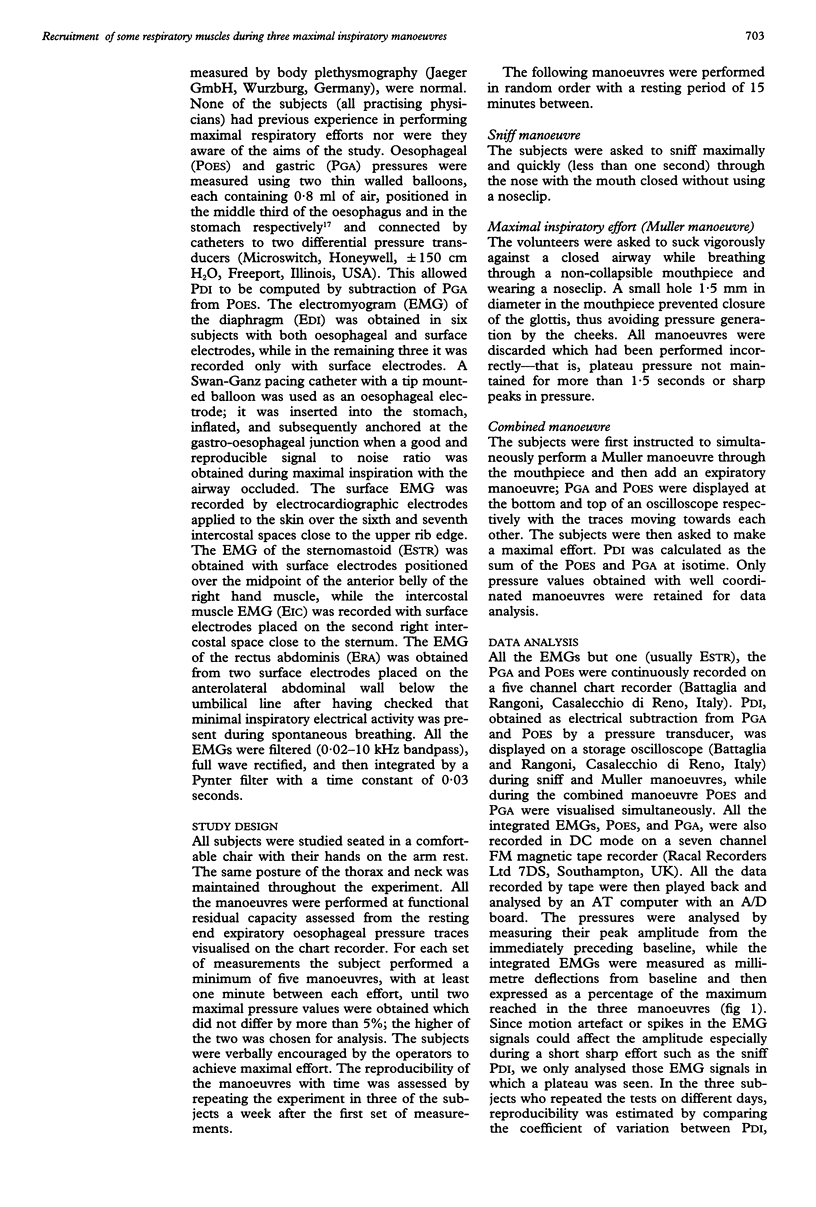
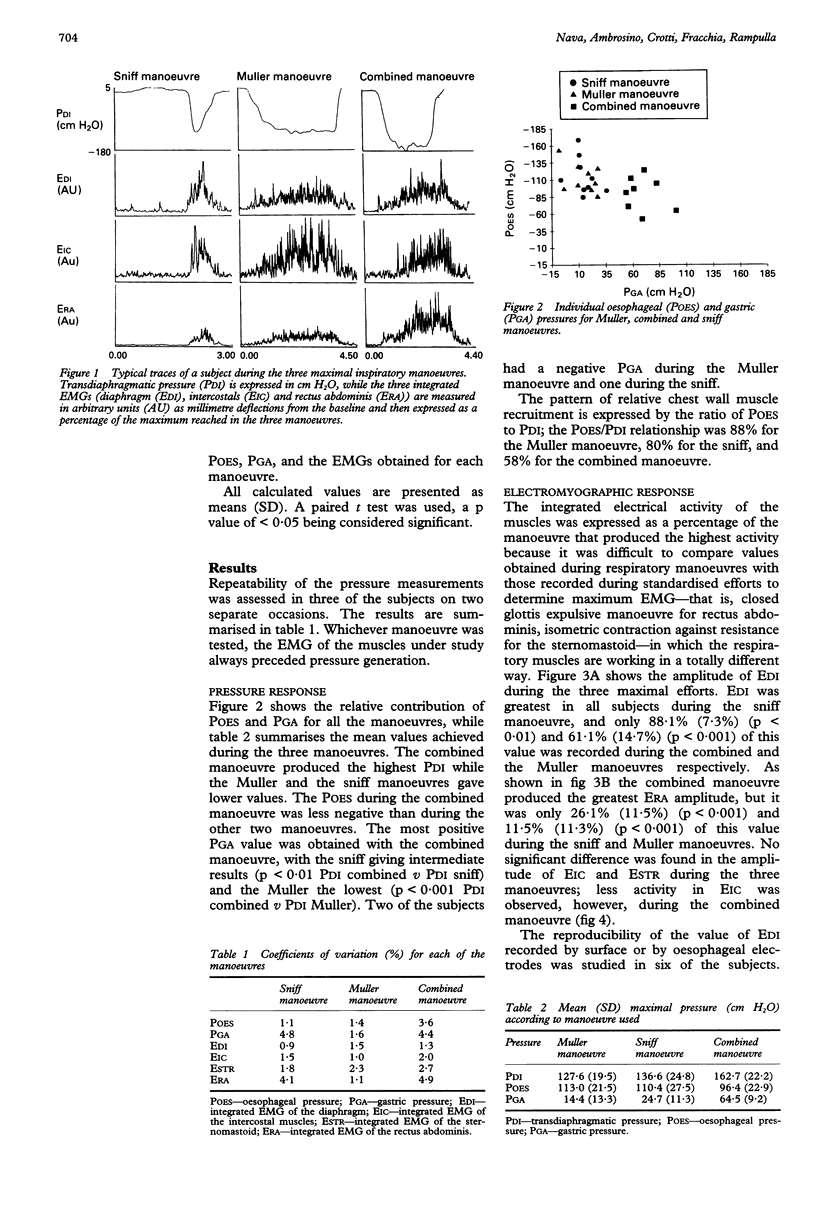
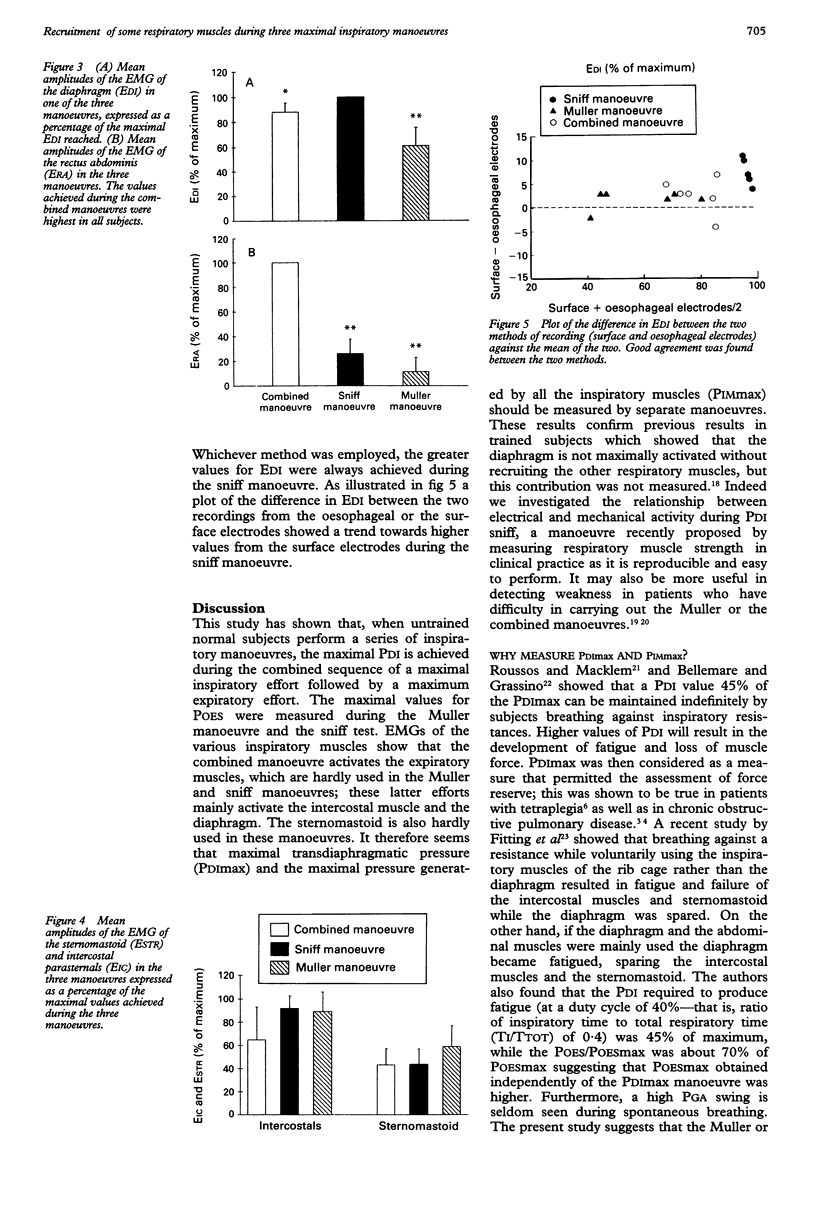
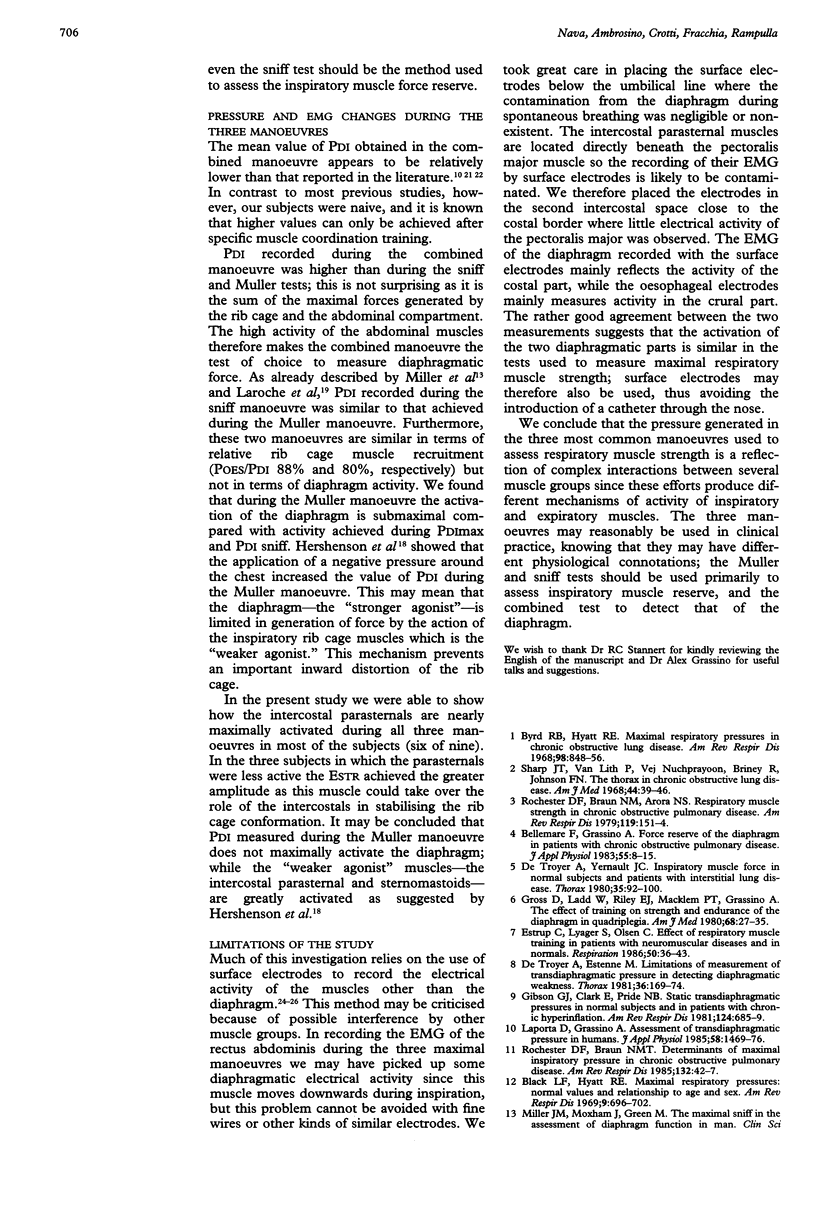
BACKGROUND--A study was undertaken to determine the level of recruitment of the muscles used in the generation of respiratory muscle force, and to ascertain whether maximal diaphragmatic force and maximal inspiratory muscle force need to be measured by separate tests. The level of activity of three inspiratory muscles and one expiratory muscle during three maximal respiratory manoeuvres was studied: (1) maximal inspiration against a closed airway (Muller manoeuvre or maximal inspiratory pressure (MIP)); (2) maximal inspired manoeuvre followed by a maximal expiratory effort (combined manoeuvre); and (3) maximal inspiratory sniff through the nose (sniff manoeuvre). METHODS--All the manoeuvres were performed from functional residual capacity. The gastric (PGA) and oesophageal (POES) pressures and their difference, transdiaphragmatic pressure (PDI), and the integrated EMG activity of the diaphragm (EDI), the sternomastoid (ESTR), the intercostal parasternals (ERIC), and the rectus abdominis muscles (ERA) were recorded. RESULTS--Mean (SD) PDI values for the Muller, combined, and sniff manoeuvres were: 127.6 (19.4), 162.7 (22.2), and 136.6 (24.8) cm H2O, respectively. The pattern of rib cage muscle recruitment (POES/PDI) was similar for the Muller and sniff manoeuvres (88% and 80% respectively), and was 58% in the combined manoeuvre, confirming data previously reported in the literature. Peak EDI amplitude was greater during the sniff manoeuvre in all subjects (100%) than during the combined (88.1%) and Muller (61.1%) manoeuvres. ESTR and EIC were more active in the Muller and the sniff manoeuvres. The contribution of the expiratory muscle (ERA) to the three manoeuvres was 100% in the combined, 26.1% for the sniff, and 11.5% for the Muller manoeuvre. CONCLUSIONS--Each of these three manoeuvres results in different mechanisms of inspiratory and expiratory muscle activation and the intrathoracic and intra-abdominal pressures generated are a reflection of the interaction between the various muscle groups. The Muller and sniff manoeuvres reflect mainly the force of the inspiratory muscles and the combined manoeuvre that of the diaphragm.
Full text
PDF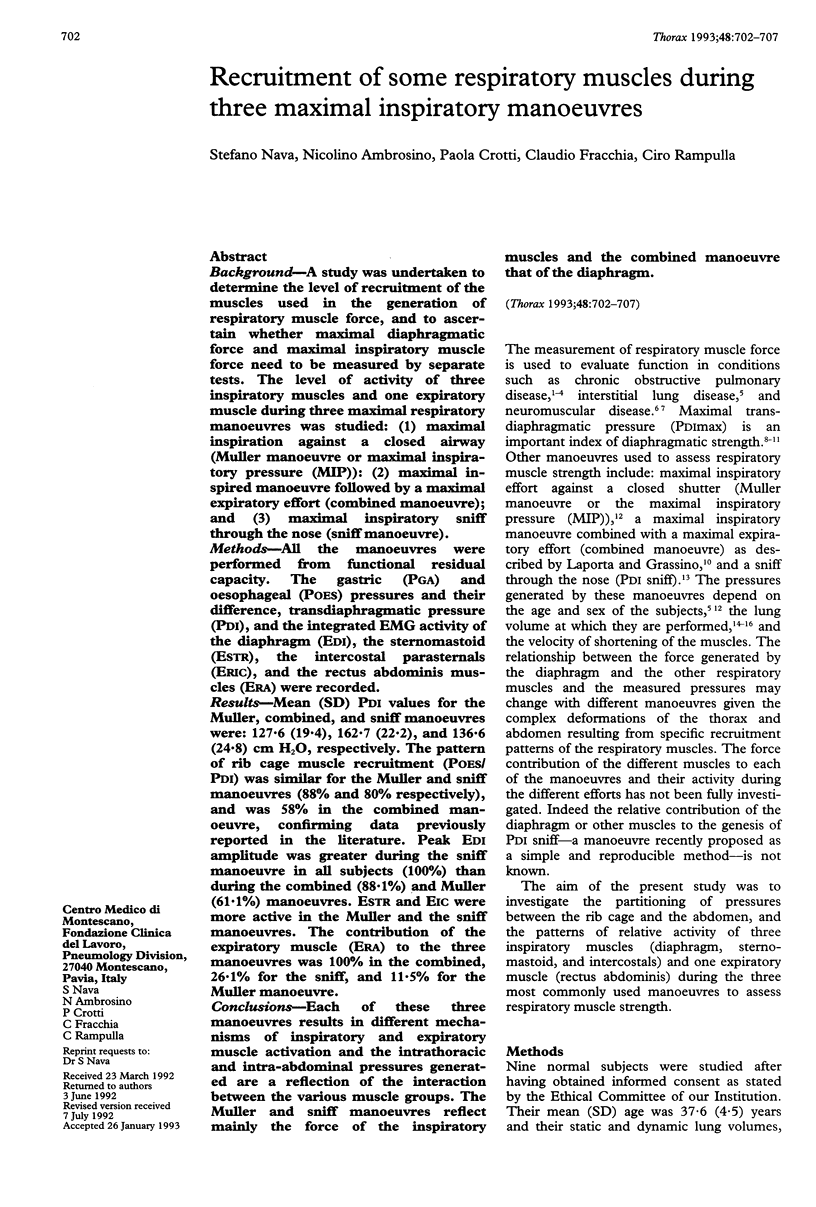

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- AGOSTONI E., RAHN H. Abdominal and thoracic pressures at different lung volumes. J Appl Physiol. 1960 Nov;15:1087–1092. doi: 10.1152/jappl.1960.15.6.1087. [DOI] [PubMed] [Google Scholar]
- Bellemare F., Grassino A. Force reserve of the diaphragm in patients with chronic obstructive pulmonary disease. J Appl Physiol Respir Environ Exerc Physiol. 1983 Jul;55(1 Pt 1):8–15. doi: 10.1152/jappl.1983.55.1.8. [DOI] [PubMed] [Google Scholar]
- Black L. F., Hyatt R. E. Maximal respiratory pressures: normal values and relationship to age and sex. Am Rev Respir Dis. 1969 May;99(5):696–702. doi: 10.1164/arrd.1969.99.5.696. [DOI] [PubMed] [Google Scholar]
- Braun N. M., Arora N. S., Rochester D. F. Force-length relationship of the normal human diaphragm. J Appl Physiol Respir Environ Exerc Physiol. 1982 Aug;53(2):405–412. doi: 10.1152/jappl.1982.53.2.405. [DOI] [PubMed] [Google Scholar]
- Byrd R. B., Hyatt R. E. Maximal respiratory pressures in chronic obstructive lung disease. Am Rev Respir Dis. 1968 Nov;98(5):848–856. doi: 10.1164/arrd.1968.98.5.848. [DOI] [PubMed] [Google Scholar]
- De Troyer A., Estenne M. Limitations of measurement of transdiaphragmatic pressure in detecting diaphragmatic weakness. Thorax. 1981 Mar;36(3):169–174. doi: 10.1136/thx.36.3.169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Estrup C., Lyager S., Noeraa N., Olsen C. Effect of respiratory muscle training in patients with neuromuscular diseases and in normals. Respiration. 1986;50(1):36–43. doi: 10.1159/000194904. [DOI] [PubMed] [Google Scholar]
- Fitting J. W., Bradley T. D., Easton P. A., Lincoln M. J., Goldman M. D., Grassino A. Dissociation between diaphragmatic and rib cage muscle fatigue. J Appl Physiol (1985) 1988 Mar;64(3):959–965. doi: 10.1152/jappl.1988.64.3.959. [DOI] [PubMed] [Google Scholar]
- Gallagher C. G., Hof V. I., Younes M. Effect of inspiratory muscle fatigue on breathing pattern. J Appl Physiol (1985) 1985 Oct;59(4):1152–1158. doi: 10.1152/jappl.1985.59.4.1152. [DOI] [PubMed] [Google Scholar]
- Gibson G. J., Clark E., Pride N. B. Static transdiaphragmatic pressures in normal subjects and in patients with chronic hyperinflation. Am Rev Respir Dis. 1981 Dec;124(6):685–689. doi: 10.1164/arrd.1981.124.6.685. [DOI] [PubMed] [Google Scholar]
- Gross D., Grassino A., Ross W. R., Macklem P. T. Electromyogram pattern of diaphragmatic fatigue. J Appl Physiol Respir Environ Exerc Physiol. 1979 Jan;46(1):1–7. doi: 10.1152/jappl.1979.46.1.1. [DOI] [PubMed] [Google Scholar]
- Gross D., Ladd H. W., Riley E. J., Macklem P. T., Grassino A. The effect of training on strength and endurance of the diaphragm in quadriplegia. Am J Med. 1980 Jan;68(1):27–35. doi: 10.1016/0002-9343(80)90157-6. [DOI] [PubMed] [Google Scholar]
- Hershenson M. B., Kikuchi Y., Loring S. H. Relative strengths of the chest wall muscles. J Appl Physiol (1985) 1988 Aug;65(2):852–862. doi: 10.1152/jappl.1988.65.2.852. [DOI] [PubMed] [Google Scholar]
- King R. J. Pulmonary surfactant. J Appl Physiol Respir Environ Exerc Physiol. 1982 Jul;53(1):1–8. doi: 10.1152/jappl.1982.53.1.1. [DOI] [PubMed] [Google Scholar]
- Laporta D., Grassino A. Assessment of transdiaphragmatic pressure in humans. J Appl Physiol (1985) 1985 May;58(5):1469–1476. doi: 10.1152/jappl.1985.58.5.1469. [DOI] [PubMed] [Google Scholar]
- Laroche C. M., Mier A. K., Moxham J., Green M. The value of sniff esophageal pressures in the assessment of global inspiratory muscle strength. Am Rev Respir Dis. 1988 Sep;138(3):598–603. doi: 10.1164/ajrccm/138.3.598. [DOI] [PubMed] [Google Scholar]
- MILIC-EMILI J., MEAD J., TURNER J. M., GLAUSER E. M. IMPROVED TECHNIQUE FOR ESTIMATING PLEURAL PRESSURE FROM ESOPHAGEAL BALLOONS. J Appl Physiol. 1964 Mar;19:207–211. doi: 10.1152/jappl.1964.19.2.207. [DOI] [PubMed] [Google Scholar]
- Mier-Jedrzejowicz A., Brophy C., Moxham J., Green M. Assessment of diaphragm weakness. Am Rev Respir Dis. 1988 Apr;137(4):877–883. doi: 10.1164/ajrccm/137.4.877. [DOI] [PubMed] [Google Scholar]
- Rochester D. F., Braun N. M., Arora N. S. Respiratory muscle strength in chronic obstructive pulmonary disease. Am Rev Respir Dis. 1979 Feb;119(2 Pt 2):151–154. doi: 10.1164/arrd.1979.119.2P2.151. [DOI] [PubMed] [Google Scholar]
- Rochester D. F., Braun N. M. Determinants of maximal inspiratory pressure in chronic obstructive pulmonary disease. Am Rev Respir Dis. 1985 Jul;132(1):42–47. doi: 10.1164/arrd.1985.132.1.42. [DOI] [PubMed] [Google Scholar]
- Roussos C. S., Macklem P. T. Diaphragmatic fatigue in man. J Appl Physiol Respir Environ Exerc Physiol. 1977 Aug;43(2):189–197. doi: 10.1152/jappl.1977.43.2.189. [DOI] [PubMed] [Google Scholar]
- Wanke T., Schenz G., Zwick H., Popp W., Ritschka L., Flicker M. Dependence of maximal sniff generated mouth and transdiaphragmatic pressures on lung volume. Thorax. 1990 May;45(5):352–355. doi: 10.1136/thx.45.5.352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Troyer A., Yernault J. C. Inspiratory muscle force in normal subjects and patients with interstitial lung disease. Thorax. 1980 Feb;35(2):92–100. doi: 10.1136/thx.35.2.92. [DOI] [PMC free article] [PubMed] [Google Scholar]


