Abstract
Objective
To evaluate the impact of an MBSR program in patients with chronic bothersome tinnitus on the 1) severity of symptoms of tinnitus and 2) functional connectivity in neural attention networks.
Study Design
Open-label interventional pilot study.
Setting
Outpatient academic medical center.
Subjects
A total of 13 adult participants with a median age of 55 years, suffering from bothersome tinnitus.
Methods
An 8-week MBSR program was conducted by a trained MBSR instructor. The primary outcome measure was the difference in patient-reported tinnitus symptoms using the Tinnitus Handicap Index (THI) and Tinnitus Functional Index (TFI) between pre-intervention, post-MBSR, and 4-week post-MBSR assessments. Secondary outcomes included change in measurements of depression, anxiety, mindfulness and cognitive abilities. Functional connectivity MRI was performed at pre- and post- MBSR intervention time points to serve as a neuroimaging biomarker of critical cortical networks.
Results
Scores on the THI and TFI showed statistically significant and clinically meaningful improvement over the course of the study with a median ΔTHI of −16 and median ΔTFI of −14.8 between baseline and 4-week follow-up scores. Except for depression, there was no significant change in any of the secondary outcome measures. Analysis of the rs-fcMRI data showed increased connectivity in the post-MBSR group in attention networks but not the default network.
Conclusion
Participation in an MBSR program is associated with decreased severity in tinnitus symptoms and depression, and connectivity changes in neural attention networks. MBSR is a promising treatment option for chronic bothersome tinnitus that is both noninvasive and inexpensive.
Keywords: tinnitus, functional connectivity MRI, neuroplasticity
INTRODUCTION
Subjective, idiopathic, non-pulsatile tinnitus is the perceived sensation of sound without acoustic stimulation. In the clinical setting, physicians see a striking division between bothered and nonbothered tinnitus patients that is unrelated to perceived loudness of the tinnitus.2 Bothersome tinnitus creates problems with activities of daily living, difficulty functioning, and an inability to relax.3 Tinnitus sufferers present with high rates of depression due to insomnia, and problems with concentration and emotion.1 There is no reliable cure for idiopathic non-pulsatile tinnitus and few effective treatments exist for those with bothersome tinnitus.
A major limiting factor in identifying effective therapy is the lack of understanding of the neurobiology of tinnitus. Although discussion of central hypotheses began long ago,4 most of the early work in tinnitus research focused primarily on the cochlea. Recently, interest has shifted in a new direction to study cortical contributions to tinnitus bother.5 This research has been informed by resting state functional connectivity MRI (rs-fcMRI),5,6 which indirectly measures functional neural connectivity. Recent work has used rs-fcMRI to measure connectivity differences between nonbothered tinnitus patients, bothered tinnitus patients, and healthy controls.7,8 Patients with bothersome tinnitus display altered patterns of neural connectivity, including key cortical attention networks, as compared to healthy controls.9 Nonbothered patients revealed connectivity networks consistent with healthy controls, suggesting that altered network connectivity may play a role in tinnitus bother.10
Mindfulness Based Stress Reduction (MBSR) is a meditation and yoga program11 with a focus on mindfulness, a method for facing, exploring and alleviating suffering by relating to present experiences. MBSR treatment reduces stress levels, improves immune function, and lowers depression and anxiety in numerous clinical settings.12 A recent study by Gans et al. provided preliminary behavioral evidence that MBSR may be an effective intervention for patients with tinnitus.13 Our study expands on previous work by including more participants, a follow-up test, and neuroimaging to explore the impact of MBSR on the cortical contributions of attention networks to bothersome tinnitus. We hypothesized that MBSR would improve patient symptoms by reducing level of tinnitus bother and that MBSR therapy would be associated with modulation of functional connectivity in cortical attention networks.
METHODS
Design and Setting
This was an open-label, prospective, interventional trial conducted at Washington University in Saint Louis to evaluate the feasibility and effectiveness of MBSR as a treatment for patients with chronic bothersome tinnitus. A certified MBSR instructor conducted eight weekly two-hour MBSR sessions and one three-hour retreat based on the Mindfulness-Based Stress Reduction Workbook.14 Content included instruction in mindfulness meditation, mindful movements, and exercises to enhance mindfulness in everyday activity. Participants were given weekly homework assignments, readings, and CDs to follow during daily practice. Participants were asked to practice 30–45 minutes per day, and daily mindfulness logs were collected on a weekly basis. Resting-state functional MRI scans were obtained at pre- and post- MBSR intervention. Questionnaire data was collected in person at pre- and post- MBSR therapy visits and electronically at 1-month following MBSR treatment using REDCap Software (Version 5.11.1). Institutional Review Board approval from the Human Research Protection Office at Washington University in St. Louis was obtained prior to recruitment.
Participants
Eighteen adult, MBSR-naïve participants with chronic bothersome tinnitus were consented for the study between October and November 2012. Participants were recruited through advertisements and referral from the Washington University in Saint Louis Otolaryngology clinic. Of the initial 18 participants, two failed screening and were excluded from the study and three participants withdrew from the study for various reasons, including non-compliance with the MBSR program. The remaining 13 participants met inclusion criteria of non-pulsatile subjective unilateral or bilateral tinnitus for at least six months duration. In order to qualify for this study, participants needed to report global tinnitus bother as “bothered more than a little but not a lot,” “bothered a lot”, or “extremely bothered” when asked about the bothersome level of their tinnitus. Exclusion criteria included (1) history of head trauma, seizure, or stroke, (2) active depression or other DSM IV axis I disorder, or moderate or severe depression as evidenced by a score of 15 or higher on the Patient Health Questionnaire (PHQ-9) depression assessment,15 (3) retrocochlear lesion or anatomic/structural lesion of the brain, skull base, temporal bone or ear, (4) current use of medication for depression or anxiety, or (5) active alcohol or drug dependence.
Medical history and behavioral measures
Participants completed questionnaires regarding their health information, hearing history, occupational noise exposure, and tinnitus. All participants were screened for depression, anxiety, mindfulness, and cognitive abilities at the pre- and post- MBSR time points using the PHQ-9,15 Patient-Reported Outcomes Measurement Information System-Anxiety (PROMIS-Anxiety)16 evaluation, Cognitive and Affective Mindfulness Scale-Revised (CAMS-R)17 form, and Cognitive Failures Questionnaire (CFQ).18 Overall degree of tinnitus bother was assessed through the Tinnitus Global Bothersome Scale, a 5-point Likert scale ranging from a score of “Not Bothered” to “Extremely Bothered.” Self-reported measures regarding tinnitus symptoms were obtained from all participants prior to the intervention, immediately following MBSR therapy and at 4-weeks post-intervention. These measures included the Tinnitus Handicap Inventory (THI)19 and the Tinnitus Functional Index (TFI).20 The THI is a 25 item self-report measure with items grouped into functional, emotional and catastropic subscales. The TFI is also a 25 item questionnaire with comprehensive coverage of a wide variety of tinnitus-related complaints. It has been shown to be highly responsive to treatment-related changes in tinnitus.
Resting State Functional Connectivity MRI
Imaging data were collected on a Siemens 3T Trio scanner. Participants were asked to relax with their eyes closed, but remain awake, in the scanner. Blood oxygenation level-dependent (BOLD) signal was captured using an echo-planar imaging (EPI) sequence (Repetition time [TR] = 2200 ms, echo time [TE] = 27 ms, flip angle = 90°, 4 mm isotropic voxels). Three runs of 164 volumes each were acquired for each participant. A T1-weighted structural image was also acquired (MPRAGE sequence: TR = 2100 ms, TE = 3.93ms, flip angle = 7°, 1 × 1 × 1.25 mm voxels).
Statistical Analyses
Behavioral data were analyzed using IBM SPSS Statistics version 20.0 (IBM SPSS Inc, Chicago). The primary behavioral outcome measure was the change in tinnitus symptoms using pre- and post- MSBR differences in TFI and THI scores. Secondary behavioral outcome measures included changes in cognitive function, mindfulness, anxiety levels, and depression. As the data were not normally distributed, a Friedman test was used to assess for overall differences between the three paired time points. Wilcoxon signed-rank tests were conducted for post hoc analysis with the alpha level adjusted using a Bonferroni correction.
Neuroimaging Analyses
Pairs of pre- and post- MBSR intervention scans were available and usable for further data analysis for 12 subjects (an error during data preprocessing occurred for one participant’s images). SPM8 software (Wellcome Trust Centre for Neuroimaging, London, UK) and the Automatic Analysis processing environment (version 4.1; http://github.com/rhodricusack/automaticanalysis) were used to process the MRI data. The variance between successive EPI volumes was computed and then all EPI scans were aligned. Variance and motion parameters were used to identify scans exceeding 0.5mm translation, 0.3° rotation, or a variance of ≥ 5 standard deviations from the mean scaled variance, which were modeled out in timeseries analysis to limit the potential impact of participant motion on connectivity measures.21 EPI images for each participant were coregistered to that participant’s structural image and normalized to Montreal Neurological Institute (MNI) space.22 The data were spatially smoothed with a 9 mm full-width half maximum isotropic Gaussian kernel. Next, a timeseries model was constructed that included discrete cosine basis functions to bandpass filter the data from 0.01–0.1 Hz and the 6 movement parameters obtained from realignment, along with their squares and volterra expansions. A singular value decomposition was performed to reduce these confounds to a smaller number of regressors that explained at least 99% of the variance in the original set. Following model estimation, the residuals from the model were used as estimates of the timeseries of interest.
In seed-based functional connectivity analyses the timecourse of brain activation is extracted from one region (the seed region), and the activity of all other parts of the brain are compared to this seed region to evaluate the neural connectivity. For our seed-based analyses, we chose canonical regions of interest (ROIs)23 in the frontoparietal (left inferior frontal gyrus: [−42 38 21], right inferior frontal gyrus: [48 25 27]), cingulo-opercular (left anterior frontal operculum: [−51 8 −2], right anterior frontal operculum: [36 10 1]), and default (posterior cingulate: [8 −48 31], anterior cingulate: [12 36 20]) networks. Our choice of seeds in the frontoparietal attention network was motivated by the importance of these regions to task performance (Duncan ref) and implication in previous tinnitus studies (Burton?), and our choice of seeds in the default mode network by frequent reports of MBSR-related changes in this network (REFS). Around each coordinate we extracted the mean timeseries data from a sphere with radius 5 mm. These data were then entered in a timeseries model as above to identify regions of the brain in which activity was related to that of the seed region. The resulting parameter estimate maps for all participants were then entered into second-level group analyses to look at the activity for the pre-MBSR scans, post-MBSR scans, and their comparison (using a paired-samples t-test). For all analyses, we used a cluster-forming voxelwise threshold of p < .001, corrected for whole-brain significance at the cluster level (p < .05) using random field theory.24 Results were plotted on an inflated cortical surface using Connectome Workbench (v0.85; http://www.humanconnectome.org/software/connectome-workbench.html) and slices using MRIcron (http://www.mccauslandcenter.sc.edu/mricro/mricron/).25
RESULTS
Participants
The 13 participants who completed the study were derived from an initial group of 70 patients who were pre-screened for the study; 52 of these were excluded due to inclusion criteria or refusal to participate. Eighteen patients were consented and screened and two of these patients failed screening due to medication regimens and claustrophobia. Ultimately, 16 patients enrolled in the study with 3 patients withdrawing due to personal reasons. The 13 patients who completed the study had a median age of 55 years (range = 32–65) and 9 of them (69%) were female. The median duration of tinnitus among the group was 4 years, with a median duration of bothersome tinnitus of 1.8 years (range 0.6 to 10 years). Five patients reported that they did not have difficulty hearing speech, 7 felt that they sometimes did, and 1 reported that speech was often hard to hear. Only 1 patient reported using a hearing aid.
All 13 participants attended at least 6 MBSR sessions and 10 participants attended the retreat. Review of meditation logs indicated that participants completed an average of 35 hours of mindfulness practice during the course of the MBSR program. Three participants failed to turn in more than two weekly logs, so the amount of participation in mindfulness activities for these participants is unknown.
Self-Reported Tinnitus Scores
TFI scores are shown in Figure 1a. At baseline, the median TFI score was 39 (range of 24–61), at the immediate post-intervention visit 27 (range of 6–60), and at the 4-week follow-up assessment 23 (range of 4–48). At the 4-week assessment, scores were reduced as compared to baseline with a median ΔTFI of −14.8 and 8 patients (62%) had achieved a clinically meaningful reduction20 of 13 points or more. Friedman’s test revealed that there was a significant difference in the median ΔTFI scores, X2 (2df) = 8.77, p = 0.012. Wilcoxon signed-rank tests revealed significant differences in TFI between pre- and post- MBSR data points (Z = −2.517, p = 0.012) and pre-MBSR and 4-week follow-up assessment values (Z = −2.587, p = 0.010). There was no significant difference between TFI values measured at the post-MBSR visit and the 4-week follow-up assessment (Z = −1.15, p = 0.249).
Figure 1.
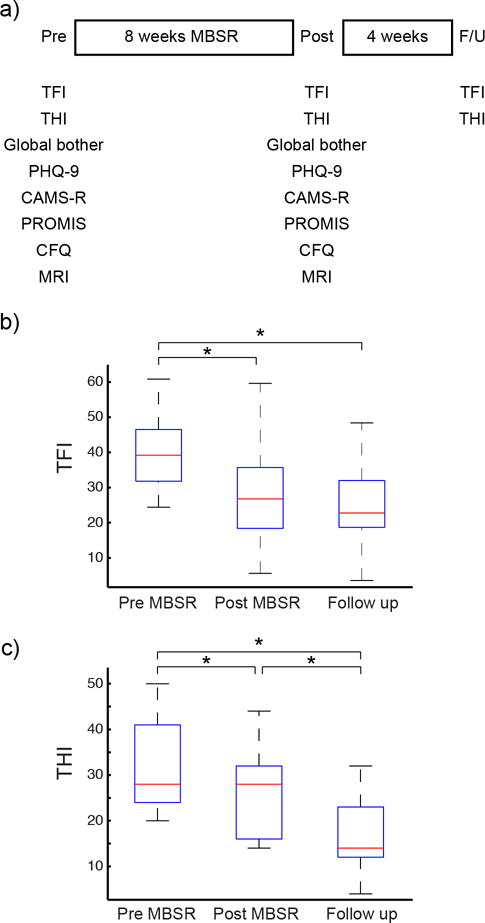
Self reported tinnitus health status. (A) Boxplot indicating median tinnitus functional index (TFI). (B) Boxplot indicating median tinnitus handicap inventory (THI). * indicates p < .05
THI scores are shown in Figure 1b. The median THI score at baseline was 28 (range of 20–50), at the immediate post-intervention visit 28 (range of 14–44), and at the four-week follow up assessment 14 (range of 4–32). The median change in THI score at the 4-week follow-up was −16 points from baseline. At the 4-week follow-up assessment, 10 patients (77%) had achieved a clinically meaningful difference defined by 7 points or greater reduction in THI scores.26 Friedman’s test revealed that there was an overall significant difference in the ΔTHI, X2 (2df) = 18.12, p < 0.001. Individual Wilcoxon signed-rank tests, corrected for 3 samples, revealed significant differences in THI between pre- and post- MBSR values (Z = −2.635, p = 0.008), post-MBSR and 4-week follow up assessment time points (Z = −2.635, p = 0.008) and pre-MBSR and 4 week follow-up assessment values (Z = −3.066, p= 0.002).
There was no significant difference in the degree of global bother assessed at both the pre- and post-MBSR visits (p=0.368).
Neurocognitive Measures
Scores on the PROMIS-Anxiety, CAMS-R, and CFQ did not reveal any statistically significant change between pre- and post- intervention time points. Although not clinically significant, the responses on the PHQ-9 assessed at the end of MBSR intervention changed from the baseline PHQ-9 scores with a median of −1 points and range from 3 points reduction to 1 point increase (p=0.03).
Functional connectivity MRI
Seed-based functional connectivity analyses were performed on regions from two executive attention networks23,27 previously implicated in tinnitus bother9,10 and the default network. Functional connectivity analyses started with the left and right inferior frontal gyrus (IFG), part of the frontoparietal attention network (Figure 2). Connectivity with the left IFG was significantly increased following MBSR in three clusters: left superior temporal gyrus (peak [−58 −6 −2], peak Z = 4.41, 518 voxels), posterior cingulate (peak [−12 −50 20], peak Z = 4.15, 194 voxels), and visual cortex (peak [8 −84 −14], peak Z = 3.83, 179 voxels). Connectivity was increased with the right IFG to a cluster in the posterior cingulate cortex (peak [−12 −50 22], peak Z = 4.14, 283 voxels). There were no regions showing significant decreases in connectivity.
Figure 2.
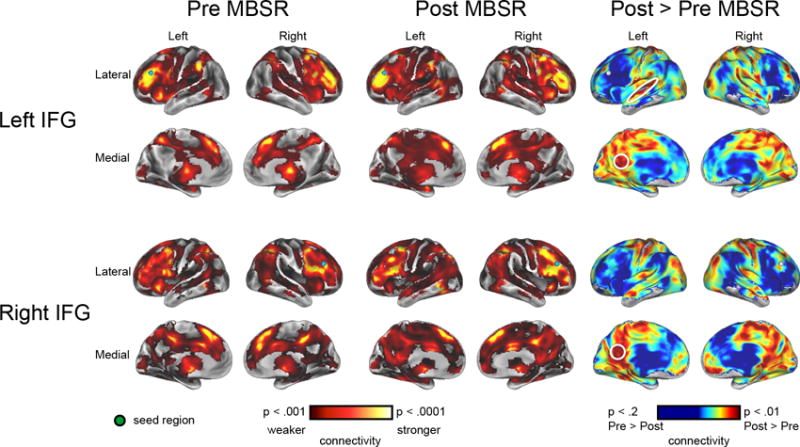
Functional connectivity for inferior frontal gyrus regions of interest pre- and post- MBSR. For each analysis, the seed region is displayed as a green sphere. Warm colors indicate brain regions that show significant connectivity with the seed region, with the colormap corresponding to the t statistic. The right column shows post > pre functional connectivity data with significant clusters circled in white.
Similar analyses were conducted using seed regions from the left and right anterior operculum (aO), part of the cingulo-opercular network associated with task set maintenance (Figure 3). Significant increases from left aO were found to a cluster extending into the left cingulate cortex (peak [−16 −6 40], peak Z = 4.15, 253 voxels); increases from right aO were found to a cluster spanning left temporal and parietal cortex (peak [−36 −42 22], peak Z = 5.00, 432 voxels), right frontal regions bordering anterior cingulate and middle frontal gyrus (peak [20 20 24], peak Z = 4.25, 192 voxels), and left superior temporal gyrus (peak [−54 −2 −4], peak Z = 3.85, 151 voxels). There were no regions showing significant decreases in connectivity.
Figure 3.
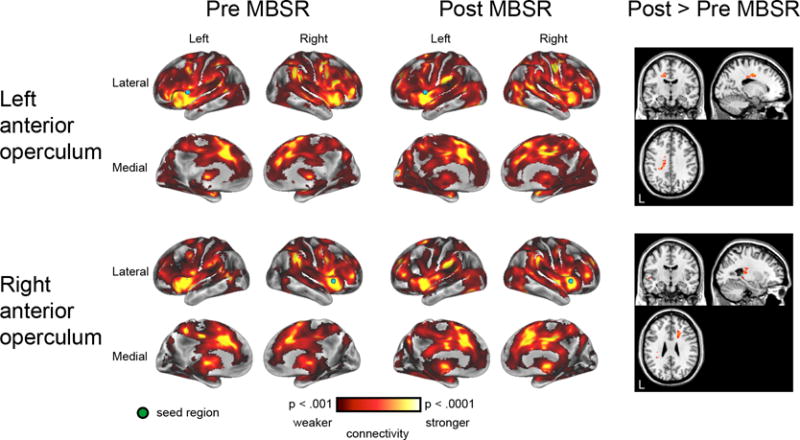
Functional connectivity for left and right anterior operculum regions of interest pre- and post- MBSR. The right panel illustrates significant clusters showing increased connectivity for post-MBSR relative to pre-MBSR.
Lastly, the default network was investigated using seeds in posterior cingulate cortex (PCC) and anterior cingulate cortex (ACC) (Figure 4). Although connectivity with both seeds revealed a stereotypical pattern of default network connectivity, there were no statistically significant differences between pre- and post-MBSR connectivity with these seeds.
Figure 4.
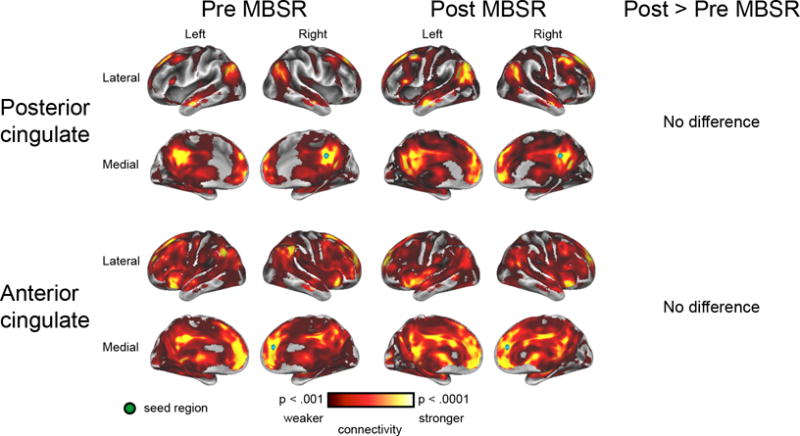
Functional connectivity for posterior and anterior cingulate regions of interest pre- and post- MBSR. There were no significant differences between pre- and post- MBSR scans.
DISCUSSION
This study examined changes in symptoms and neural connectivity after MBSR in patients with bothersome tinnitus. A significant and clinically meaningful reduction in tinnitus bother was observed following MBSR using both THI and TFI assessment measures. Measures of depression, anxiety, mindfulness, and cognitive abilities did not show clinically meaningful changes after MBSR, although there was a statistically significant change in pre-post depression scores. A seed-based analysis performed on rs-fcMRI scans obtained before and after MBSR treatment revealed changes in functional connectivity within regions associated with known attention networks. Together these results suggest that the subjective improvement associated with participation in an MBSR program may be related to altered neural connectivity.
Previous behavioral studies done at other institutions have reported preliminary evidence for the efficacy of MBSR in reducing bother associated with chronic tinnitus.13,28 Our current findings expand on previous studies through the use of a larger sample size and the incorporation of advanced neuroimaging to study the functional connectivity within cortical attention networks. The interpretation of prior studies investigating the effects of MBSR using rs-fcMRI is limited by variability in methodology and analysis approach.
Our findings agree with past studies, which are largely consistent in reporting changes in neural connectivity following MBSR. However, studies using rs-fcMRI to investigate the effects of MBSR show considerable heterogeneity in the populations studied, seed regions, and analysis approach, making direct comparisons of specific neural changes difficult. Several studies have focused exclusively on the default mode network.29–31 Hasenkamp and Barsalou32 found that participants with more meditation experience exhibited increased connectivity within attention networks, as well as between attentional regions and the default mode network. In another study examining the use of MBSR in healthy adults, differences in functional connectivity between the MBSR and control groups were found in the auditory/salience and medial visual networks, but there were no noted changes in the default mode network or attention networks.33 Thus, although there is agreement that MBSR results in changed neural connectivity, the consistency of MBSR effects on specific attention networks across populations from prior studies is difficult to evaluate.
The functional connectivity results of this study suggest multiple changes and increased activation between networks responsible for attention and focus. Our previous work9 suggests that patients with bothersome tinnitus have abnormal functional connectivity in networks responsible for attention, decision-making, and somatosensory input. The functional connectivity observations in the current study suggest that participation in an MBSR program can result in neuroplastic changes in attention networks. These changes coincided with self-reported improvement in symptoms.
There are several limitations to this study. First, this was a pilot study and we did not use a control group. An appropriate control group would be matched in regards to age, gender and tinnitus bother and would undergo an intervention that does not incorporate the techniques of MBSR but does control for the attention provided to the participant during MBSR. A health education program (HEP)34 has been suggested as an appropriate active control condition for MBSR: while HEP improves chronic disease management, it does not teach mindfulness techniques or address worry and rumination, and is thus a credible behavioral intervention that has none of the posited active ingredients of MBSR.35 A second limitation of our study was the small sample size, (n=13). The participants represented a wide range of ages, variability in pre- and post- MBSR tinnitus symptom scores, amount of time spent using the MBSR program at home, and attendance at weekly sessions. Due to our limited sample size, we were not able to adequately control for these factors or conduct cogent subgroup analyses. Future studies including both an active control group and a larger sample size will be beneficial.
Conclusion
This research identified a reduction in tinnitus symptoms and neuroimaging changes in functional connectivity in cortical attention networks, coinciding with clinical improvement of symptoms. MBSR appears to be a beneficial technique for tinnitus patients: MBSR is inexpensive, non-invasive, and takes advantage of the neuroplasticity of the brain to potentially create lasting benefits.
Acknowledgments
This research and publication was supported, in part, by the Washington University Institute of Clinical and Translational Sciences grant UL1 TR000448 from the National Center for Advancing Translational Sciences, the “Development Of Clinician/Researchers In Academic ENT” T32 DC00022 from the National Institutes of Deafness and Other Communication Disorders, and grant AT007064 from the National Center for Complementary and Alternative Medicine. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
This project was also supported, in part, with funding from the Mallinckrodt Institute of Radiology at the Washington University School of Medicine. The use of REDCap software was supported by Clinical and Translational Science Award (CTSA) Grant UL1TR00048 and Siteman Comprehensive Cancer Center and NCI Cancer Center Support Grant P30 CA091842.
References
- 1.Dobie R. Overview: Suffering from tinnitus. In: Snow JBJ, editor. Tinnitus: Theory and Management. Hamilton, Ontario: BC Decker; 2004. [Google Scholar]
- 2.Coles RRA, Hallam RS. Tinnitus and its management. British Medical Bulletin. 1987;43(4):983–998. doi: 10.1093/oxfordjournals.bmb.a072230. [DOI] [PubMed] [Google Scholar]
- 3.Hoffman HJ, Reed GW. Tinnitus: Theory and Management. Ontario: BC Decker; 2004. Epidemiology of Tinnitus. [Google Scholar]
- 4.Tyler RS, Conrad-Armes D. Masking of tinnitus compared to masking of pure tones. Journal of Speech and Hearing Research. 1984;27:106–111. doi: 10.1044/jshr.2701.106. [DOI] [PubMed] [Google Scholar]
- 5.Husain FT, Schmidt SA. Using resting state functional connectivity to unravel networks of tinnitus. Hearing Research. 2014;307:153–162. doi: 10.1016/j.heares.2013.07.010. [DOI] [PubMed] [Google Scholar]
- 6.Buckner RL, Krienen FM, Yeo BTT. Opportunities and limitations of intrinsic functional connectivity MRI. Nat Neurosci. 2013;16:832–837. doi: 10.1038/nn.3423. [DOI] [PubMed] [Google Scholar]
- 7.Maudoux A, Lefebvre P, Cabay JE, Demertzi A, Vanhaudenhuyse A, Laureys S. Soddu A Auditory resting-state network connectivity in tinnitus: a functional MRI study. PLoS One. 2012;7:e36222. doi: 10.1371/journal.pone.0036222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Maudoux A, Lefebvre P, Cabay JE, Demertzi A, Vanhaudenhuyse A, Laureys S. Soddu A Connectivity graph analysis of the auditory resting state network in tinnitus. Brain Res. 2012:10–21. doi: 10.1016/j.brainres.2012.05.006. [DOI] [PubMed] [Google Scholar]
- 9.Burton H, Wineland A, Bhattacharya M, Nicklaus J, Garcia K, Piccirillo J. Altered networks in bothersome tinnitus: a functional connectivity study. BMC Neurosci. 2012;13(3):1–15. doi: 10.1186/1471-2202-13-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wineland AM, Burton H, Piccirillo J. Functional connectivity networks in nonbothersome tinnitus. Otolaryngol Head Neck Surg. 2012;147(5):900–906. doi: 10.1177/0194599812451414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kabat-Zinn J. Mindfulness-Based Interventions in Context: Past, Present, and Future. Clinical Psychology. 2003;10(2):144–156. [Google Scholar]
- 12.Lengacher CA, Johnson-Mallard V, Post-White J, Moscoso MS, Jacobsen PB, Klien TW, Widen RH, Fitzgerald SG, Shelton MM, Barta M, Goodman M, Cox CE, Kip KE. Randomized controlled trial of mindfulness-based stress reduction (MBSR) for survivors of breast cancer. Psycho-Oncology. 2009;18:1261–1272. doi: 10.1002/pon.1529. [DOI] [PubMed] [Google Scholar]
- 13.Gans J, O’Sullivan P, Bircheff V. Mindfulness based tinnitus stress reduction pilot study: a symptom perception shift program. Mindfulness. 2013:1–12. [Google Scholar]
- 14.Stahl B, Goldstein E. Mindfulness-Based Stress Reduction Workbook. Oakland, CA: New Harbinger Publications, Inc; 2010. [Google Scholar]
- 15.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Reeves DL, Winter KP, Bleiberg J, Kane RL. ANAM genogram: historical perspectives, description, and current endeavors. Arch Clin Neuropsychol. 2007;22(Suppl 1):S15–S37. doi: 10.1016/j.acn.2006.10.013. [DOI] [PubMed] [Google Scholar]
- 17.Feldman G. Mindfulness and Emotion Regulation: The Development and Initial Validation of the Cognitive and Affective Mindfulness Scale-Revised (CAMS-R) Psychopathol Behav Assess. 2007;29:177–190. [Google Scholar]
- 18.Broadbent DE, Cooper PF, Fitzgerald P, Parkes KR. The Cognitive Failures Questionnaire (CFQ) and its correlates. Br J Clin Psychol. 1982:1–16. doi: 10.1111/j.2044-8260.1982.tb01421.x. [DOI] [PubMed] [Google Scholar]
- 19.Newman CW, Jacobson GP, Spitzer JB. Development of the Tinnitus Handicap Inventory. Archives of Otolaryngology – Head & Neck Surgery. 1996;122(2):143–148. doi: 10.1001/archotol.1996.01890140029007. [DOI] [PubMed] [Google Scholar]
- 20.Meikle MB, Henry JA, Griest SE, Stewart BJ, Abrams HB, McArdle R, Myers PJ, Newman CW, Sandridge S, Turk DC, Folmer RL, Frederick EJ, House JW, Jacobson GP, Kinney SE, Martin WH, Nagler SM, Reich GE, Searchfield G, Sweetow R, Vernon JA. The tinnitus functional index: development of a new clinical measure for chronic, intrusive tinnitus. Ear Hear. 2012;33(2):153–176. doi: 10.1097/AUD.0b013e31822f67c0. [DOI] [PubMed] [Google Scholar]
- 21.Power JD, Barnes KA, Snyder AZ, Schlaggar BL, Petersen SE. Spurious but systematic correlations in functional connectivity MRI networks arise from subject motion. NeuroImage. 2012;59:2142–2154. doi: 10.1016/j.neuroimage.2011.10.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ashburner J, Friston KJ. Unified segmentation. NeuroImage. 2005;26:839–851. doi: 10.1016/j.neuroimage.2005.02.018. [DOI] [PubMed] [Google Scholar]
- 23.Power JD, Cohen AL, Nelson SM, et al. Functional network organization of the human brain. Neuron. 2011;72:665–678. doi: 10.1016/j.neuron.2011.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Worsley KJ, Evans AC, Marrett S, Neelin P. A three-dimensional statistical analysis for CBF activation studies in human brain. J Cereb Blood Flow Metab. 1992 Nov;12(6):900–918. doi: 10.1038/jcbfm.1992.127. [DOI] [PubMed] [Google Scholar]
- 25.Rorden C, Brett M. Stereotaxic display of brain lesions. Behavioural Neurology. 2000;12:191–2000. doi: 10.1155/2000/421719. [DOI] [PubMed] [Google Scholar]
- 26.Zemen F, Koller M, Figueiredo R, Aazevedo A, Rates M, Coelho C, Kleinjung T, de Ridder D, Langguth B, Landgrebe M. Tinnitus handicap inventory for evaluating treatment effects: which changes are clinically relevant? Otolaryngol Head Neck Surg. 2011;145(2):282–287. doi: 10.1177/0194599811403882. [DOI] [PubMed] [Google Scholar]
- 27.Petersen SE, Posner MI. The attention system of the human brain: 20 years after. Annu Rev Neurosci. 2012;35:73–89. doi: 10.1146/annurev-neuro-062111-150525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kreuzer PM, Goetz M, Holl M, Schecklmann M, Landgrebe M, Staudinger S, Langguth B. Mindfulness-and body-psychotherapy-based group treatment of chronic tinnitus: a randomized controlled pilot study. BMC Complementary and Alternative Medicine. 2012;12 doi: 10.1186/1472-6882-12-235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Taylor VA, Daneault V, Grant J, Scavone G, Breton E, Roffe-Vidal S, Courtemanche J, Lavarenne AS, Marrelec G, Benali H, Beuregard M. Impact of meditation training on the default mode network during a restful state. Soc Cogn Affect Neurosi. 2012;8:4–14. doi: 10.1093/scan/nsr087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Brewer JA, Worhunsky PD, Gray JR, Tang YY, Weber J, Kober H. Meditation experience is associated with differences in default mode network activity and connectivity. Proc Natl Acad Sci USA. 2011;108(50) doi: 10.1073/pnas.1112029108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wells RE, Yeh GY, Kerr CE, Wolkin J, Davis RG, Tan Y, Spaeth R, Wall RB, Walsh J, Kaptchuk TJ, Press D, Phillips RS, Kong J. Meditation’s impact on default mode network and hippocampus in mild cognitive impairment: A pilot study. Neuroscience Letters. 2013;556:15–19. doi: 10.1016/j.neulet.2013.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Haskenkamp W, Barsalou LW. Effects of meditation experience on functional connectivity of distributed brain networks. Front Hum Neurosci. 2012;6(38) doi: 10.3389/fnhum.2012.00038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kilpatrick LA, Suyenobu BY, Smith SR, Bueller JA, Goodman T, Creswell JD, Tillisch K, Mayer EA, Naliboff BD. Impact of Mindfulness-Based Stress Reduction Training on Intrinsic Brain Connectivity. Neuroimage. 2011;56:290–298. doi: 10.1016/j.neuroimage.2011.02.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lorig K, Holman H, Sobel D, Laurent D, Gonzalez V. Living a Healthy Life with Chronic Conditions: For Ongoing Physical and Mental Health Conditions. Bull Publishing Company; 2007. [Google Scholar]
- 35.MacCoon DG, Imel ZE, Rosenkranz MA, Sheftel JG, Weng HY, Sullivan JC, Bonus KA, Stoney CM, Salomons TV, Davidson RJ, Lutz A. The validation of an active control intervention for Mindfulness Based Stress Reduction (MBSR) Behav Res Ther. 2012(50):3–12. doi: 10.1016/j.brat.2011.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]


