Abstract
This case report illustrates the improvement of an acupuncture-treated patient who incurred a severe traumatic brain injury (TBI) from a snowboarding accident. Over 4 years, the patient progressed from initially not being able to walk, having difficulty with speech, and suffering from poor eyesight to where he has now regained significant motor function, speech, and vision and has returned to snowboarding. A core acupuncture protocol plus specific points added to address the patient's ongoing concerns was used. This case adds to the medical literature by demonstrating the potential role of acupuncture in TBI treatment.
Key Words: Case report, traumatic brain injury, hemiplegia, acupuncture, diplopia
摘要
本病例报告显示一位因滑雪意外 遭 受 重 度 创 伤 性 脑 损 伤 (Traumatic Brain Injury,TBI) 的针灸治疗患者状况改善。历经 4 年,该患者从起初不能行走、言 语困难和视力不良进展到如今重 获明显的运动功能、言语能力及 视力,并且已经恢复滑雪。使用 了一项核心针灸方案连同为解决 该患者持续顾虑所添加的特定穴 位。通过展示针灸治疗 TBI 的潜 在作用,本病例丰富了医学文献。
SINOPSIS
Este caso clínico pone de manifiesto la mejoría de un paciente tratado con acupuntura que sufrió una lesión cerebral traumática (LCT) grave en un accidente mientras practicaba snowboard. Durante el transcurso de 4 años, el paciente progresó desde ser incapaz de caminar, tener trastornos del habla y problemas de visión hasta alcanzar una recuperación importante de la función motora, el habla y la vista, además de haber vuelto a practicar el snowboard. Se empleó un protocolo de acupuntura en el tronco (core) junto con otros puntos específicos para abordar los problemas continuos del paciente. Este caso amplía la bibliografía médica al demostrar el potencial de la acupuntura en el tratamiento de las LCT.
INTRODUCTION
The leading cause of death for people under 45 years of age in North America is traumatic brain injury (TBI).1 With slightly higher prevalence in men and an increase in frequency before the age of 30, TBI is a significant cause of morbidity. Ranging in scale of severity, TBI can include mild traumatic brain injury (mTBI) including concussion up to severe TBI with loss of consciousness greater than 6 hours.2 TBI that occurs during adolescence and early adulthood can lead to increased challenges with physical, emotional, and mental function during recovery.3 Long-term management of severe TBI typically relies on interventions from many professionals including speech therapists, physical and occupational therapists, and physicians and the support of friends and family.3
Acupuncture and traditional Chinese medicine (TCM) have been used for millennia to address acute and chronic medical concerns. The system has a basis in energy known as qi and its flow in the body through meridians. In TBI and other acute injuries, TCM considers qi to be blocked and energy flow disrupted to different systems in the body. Acupuncture has been shown to be effective in improving short-term outcomes and in managing symptoms within the first year after injury and has been examined in a longitudinal cohort study looking at the entire diagnostic range of TBI.4 In this case report, we describe the significant improvement of a patient with a severe TBI from a snowboarding accident through subsequent acupuncture therapy over a 4-year period.
CLINICAL FINDINGS
At the time of the accident, a brain magnetic resonance imaging (MRI), magnetic resonance angiogram (MRA), neck MRA, and head computerized tomography (CT) scan without contrast were performed. The results indicated diffuse axonal injury as indicated by abnormal signaling in the right splenium of the corpus collosum, the right dorsolateral brainstem and the right frontal and parietal regions. There were also small foci of diffusion weighted signal abnormality high in the right frontoparietal region. There were subtle signal abnormalities in the left basal ganglia and no midline shift of the brain. Numerous skull base fractures were present but no interventricular hemorrhages. A right pulmonary contusion and a small apical thorax were observed in chest imaging. There were also 3 posterior right rib fractures (9, 10, 11) with a small pneumatocele in the right lower lobe. The neck CT scan revealed a non-displaced C6 vertebral body fracture and a non-displaced fracture of the left occipital condyle. The right sphenoid sinus and the medial wall of the right maxillary sinus both had slight fractures. Imaging on day 11 post injury confirmed extensive diffuse axonal injury with stable changes. At week 6 post injury the patient underwent a neuropsychology consultation, and he was described as confused and disoriented with impairments in memory, apraxia, slowed processing speed and mild expressive aphasia.
PATIENT INFORMATION
The patient began his acupuncture treatment at the age of 22 approximately 3.5 months post injury. Before his accident, he was living in Colorado and working for a ski resort.
The patient was injured during a high-speed snowboarding accident resulting in head trauma. His Glasgow Coma Scale (GCS) at the scene was a 3T. The GCS is graded from 3 to 15, with 3 being the worst. The GCS is based on 3 parameters: motor, voice, and eye response. The addition of the modifier “T” indicates that the patient had a tracheal tube in place during assessment.5 Later, when the patient was admitted to the hospital, his GCS was rated as a 5T. Following his injury, he remained in a coma for 3 weeks. When he awoke, the patient had retrograde amnesia for a period of 1 year prior to the accident but had no new memory loss other than getting dates and names confused. He had no use of his right side and had a pill-rolling tremor. His reflexes on the left side were normal (+2) with absent (+0) reflexes on his right side. After 1 month, he regained some use of his right side and could feed himself with his right hand. He was diagnosed with severe TBI that resulted in paralysis and then spastic hemiplegia of the dominant side. His left side was stiff, and his right side was more flaccid with tremors.
The patient initially presented to our facility 3.5 months post injury and was extremely fatigued and weighed 160 lbs with a body mass index of 19.5. His main concerns were his decreased cognitive ability, inability to walk, slurred speech, double vision, parasthesias, numbness, motor control, and tone of his right arm and leg. He was forgetful of dates, names, and numbers at his initial visit. His current prescriptions included amantadine (100 mg), sertraline (50 mg), armodafinil (150 mg), and baclofen (100 mg). He wore a cervical collar at all times until he could have surgery to stabilize his cervical vertebrae including fusion with a spacer of C5-C7 that occurred 5 months after the injury. His tongue was crimson with a white coating and sublingual engorgement. His pulses were slightly wiry, slippery, and rapid. His initial TCM diagnosis was Qi and Blood stagnation with Liver Yang rising resulting in wind and phlegm retention due to Spleen dysfunction caused by Liver attacking Spleen. He expressed optimism about his recovery, even though on a scale of 1 to 10 he was extremely worried about his health, circling 10 (highest value) on the intake form. His vitals at initial presentation were as follows: blood pressure, 120/82; heart rate, 92; respiratory rate, 16; temperature, 99.4 degrees; height, 6 ft, 4 in; weight, 160 lbs. His family medical history was noncontributory.
Prior to presentation to our facility, the patient had been doing occupational and speech therapy. He also had been involved in physical therapy: 2 hours per day for motor control and rehabilitation of his right side. Therapies included transfer training, neuromuscular re-education, pre-gait activities, concentration skill, communication skill retraining, daily life activities retraining, strengthening exercises, balance training, gait training, compensatory strategies for memory, and adjustments to disability training.
DIAGNOSTIC ASSESSMENT
The patient was initially diagnosed at the time of incident with a diffuse axonal injury following a high-speed impact with a tree while snowboarding. Initial evaluation was in Telluride, Colorado. He was subsequently transported to facilities in Arizona for further care and monitoring. The patient had no specific diagnostic challenges at the time of the initial accident. Neuropsychiatric evaluation confirmed mild visual deficits during testing. Although no rating based on the Glasgow Outcome Scale (GOS) or other standard TBI outcome assessment were performed near onset of injury, the patient would likely have been rated as having severe disability.6
INTERVENTION
Following comprehensive inpatient care post injury, the patient was released from the hospital for ongoing rehab and long-term care. The patient remained in inpatient care for less than 30 days. After initial assessment at our teaching clinic, acupuncture was performed by third- and fourth-year naturopathic medical students supervised by a licensed acupuncturist and traditional Chinese medical doctor (OMD) trained at the Chengdu University of Traditional Chinese Medicine in China and a resident naturopathic physician. A core protocol was started to address the presenting pattern of Qi and Blood stagnation with Liver Yang rising resulting in wind and phlegm retention due to Spleen dysfunction caused by Liver attacking Spleen. The initial injury lead to the stagnation of Qi and Blood. The patient had an underlying condition of Kidney Yin deficiency, noted from his pulses and his body size, which can result in relative heat pattern.
The core acupuncture points selected initially (Table 1a) were chosen to regulate and move Qi and Blood and clear Wind with points added to guide the Qi to certain areas such as the shoulder and face.7,8 After the initial series of acupuncture treatments, the patient expressed additional desires and specific areas for which he would like to regain function. As an ongoing adaptation to the patient protocol, supplemental acupuncture points were added as needed to address the range of concerns including acute upper respiratory infection, constipation, insomnia, diplopia, and balance (Table 1b).
Table 1a.
Core Protocol
| Acupuncture Point | Action8 |
|---|---|
| Scalp: Motor and Sensory | Motor and sensory disorders of the contralateral side9 |
| LI15: Jianyu | Dispels wind-damp, alleviates pain and benefits the shoulder joint, eliminates wind and regulates qi and blood |
| LI14: Binao | Pain, numbness, and painful obstruction of the upper arm and shoulder, wasting and weakness of the upper arm, inability to raise the arm, contraction and stiffness of the neck |
| LI11: Quchi | Regulates qi and blood, activates the channel, and alleviates pain |
| LI4: Hegu | Regulates the face, eyes, nose, mouth, and ears; activates the channel and alleviates pain; command point of head and face |
| SJ5: Waiguan | Benefits the head and ears, opens the Yang-inking vessel, activates the channel, and alleviates pain |
| ST36: Zusanli | Supports the correct qi and fosters the original qi, tonifies qi and nourishes blood and yin, calms the spirit, activates the channel and alleviates pain |
| ST38: Tiaokou | Expels wind-damp and alleviates pain, benefits the shoulder |
| ST41: Jiexi | Calms the spirit, invigorates blood, activates the channel, and alleviates pain |
| SP6: Sanyinjiao | Meeting point of the spleen, liver, and kidney channels |
| KI3: Taixi | Nourishes kidney yin and clears deficiency heat, tonifies kidney yang, anchors the qi and benefits the lung, strengthens the lumbar spine |
| GB34: Yanglinquan | Command point of sinews and tendons |
Table 1b.
Supplemental Points
| Therapeutic Categories | Acupuncture Points |
|---|---|
| Constipation points | ST25, SP15, ST37 |
| Core and balancing points | Ren 17, Ren6, Scalp Hip, Ling Gu, Da Bai, Zhong Bai, Ba Feng |
| Ear points | 3 needles along the spine region, Shen men, liver, kidney, ankle, cerebellum, brainstem |
| Eye points | GB1, UB2, GB37, Tai yang, ST2 |
| Facial stiffness and speech points | ST4, ST6, LI20 |
| Miscellaneous points | LR3 (soother liver, support tendons), ST40 (clear phlegm) |
| Sleeping points | H7, An Mian, prick SP1, Yin Tang |
| Upper respiratory infection points | UB2 threaded to GB1, Bi Tong, LI20, and LU7 |
The patient took a break from treatment from weeks 72 to 168 to focus on improving his vision and speech therapy. Upon returning, the patient experienced only mild improvement in speech with moderate improvements in vision due to a corrective procedure for diplopia. After resuming treatment, a combined protocol including the core acupuncture points (Table 1a) and supplemental points based on the current presentation (Table 1b). After following this treatment protocol for many sessions, the patient demonstrated significant progress in speech clarity, balance, and convergence of vision. Balance and vision became a primary concern and the acupuncture protocol was altered to a have a focus on the Urinary Bladder (UB) channel on the back (Table 1c). This UB protocol was alternated with an anterior (front) treatment to provide a more comprehensive treatment (Table 1c).
Table 1c.
| Therapy Modification | Acupuncture Points |
|---|---|
| Protocol updated to focus on UB channel | Du 20, UB11-25, ST34, ST36, ST37, ST40, GB34, GB39, SP6, K3 |
| Changed protocol to fewer needles per patient request | Scalp sensory and motor for lower limbs |
| Auricular: cerebellum, brainstem Face: UB2 to UB1, ST2, GB1 Arm bilaterally: LI15, GB21 Hand bilaterally: LI4, Ling Gu, Da Bai; Leg bilaterally: GB 34, GB37, ST34, ST36, ST38, SP6, K3, LR3 |
OUTCOMES
The patient was very adamant in expressing his desired outcomes and goals following treatment. Upon arrival at our facility, he stated that he would like to be able to lose his tremors, regain his vision, and regain his motor control and balance enough to snowboard once again. His acupuncture therapy covered 2 separate treatment periods of 57 weeks and 38 weeks. Overall, following his treatment, his vision had improved, tremors had decreased, and fine motor skills had increased (Table 2). In addition, he was subsequently able to snowboard a number of times during the last year of treatment (Table 2).
Table 2.
Significant Milestones as Reported by the Patient
| Week | Milestone |
|---|---|
| 0 | Snowboard accident |
| 11 | Rehab intake |
| 14 | Initial acupuncture treatment |
| 15 | Neuropsychiatric evaluation |
| 20 | Increased mobility, improved range of motion in shoulder |
| 23 | Eye prescription decreased, patient using walker |
| 27 | Patient starts physical therapy |
| 38 | Eye points added to acupuncture protocol |
| 51 | Eye prescription change |
| 66 | Patient goes snowboarding with modified board |
| 67 | Eye prescription change |
| 71 | Eye prescription change |
| 72-168 | Patient stops acupuncture treatment; week 141: eye surgery to help diplopia |
| 179 | Patient wins swimming competition |
| 180 | Ear needles added for balance |
| 181 | Vision converges to single vs double vision |
| 188 | Patient uses cane for balance |
| 198 | Patient able to snap fingers on right hand |
| 201 | Patient able to watch 3D movies |
| 207 | Patient goes snowboarding 5 times |
The patient attended treatment sessions 1 to 2 times per week for the duration of his treatment with mean number of sessions per week of 1.3, ranging from 0 to 3. He tolerated the treatment well and “pushed” himself when it came to electrical-stimulation (e-stim) and number of acupuncture needles per visit. He continued with his physical therapy at home and included swimming and eye exercises to help with convergence. He demonstrated discipline to maintain all therapies suggested. The patient was questioned on any changes he noticed during the acupuncture treatment, and significant progress was noted regularly. Major milestones included beginning improvements in vision as well as a transition to using a walker 9 weeks after initiating acupuncture treatment (Table 2). On week 24 of treatment (38 weeks after the injury), a focus on eye acupuncture treatment including points near the eyes and distal points on the arms and legs. Subsequently, he had notable glasses prescription changes at 13, 29, and 33 weeks after modifying the treatment (Table 2). The patient elected to stop treatment for 96 weeks during which he had a surgical procedure to help further correct his vision. After returning to treatment, gross and fine motor control continued to improve with a change to walking with a cane, ability to snap his fingers, and a return to swimming (Table 2).
During the first 41 weeks of acupuncture treatment, the patient was largely tracked via subjective measures. The classic “10 questions” for acupuncture diagnosis provided a framework for assessment from session to session.9 These included questions on digestion, bowel movements, urination, eyesight, hearing, thirst, appetite, overall temperature, sleep, energy, emotional state, vertigo, and headaches. Responses to the questions were reviewed and graded on a scale of –2 to 2 corresponding to much worse, worse, same, better, and much better (Figure 1) in comparison to the previous visit. Due to the length of the patient's treatment course, results were combined into approximate 2-week groupings to show the general trend over time. As shown in Figure 1, the patient reported improved performance 71% of the time from visit to visit. At no point did the patient report a decrease in performance between visits, and only 29% of the time did the patient report no change in performance between visits (Figure 2). The number of visits per grouping was also tracked to assess for level of improvement compared to visit frequency (Figure 2). As shown in comparison between Figures 1 and 2, the patient improved most rapidly with increased frequency of visits. This can be seen between weeks 20 and 25 when the patient had very frequent visits (Figure 2) and reported performance improvement 100% of the time between visits (Figure 1).
Figure 1.
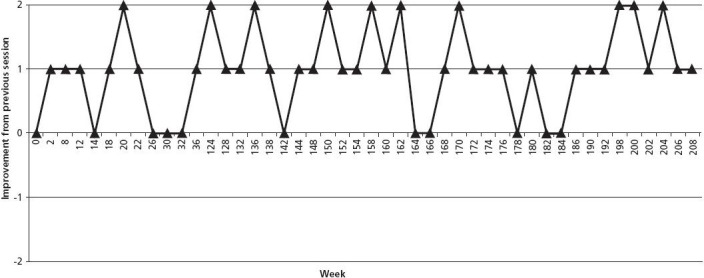
Patient reported progression between visitations. Subjective scale based on patient's report of symptom change between visits. Scale ranges from –2 to +2 with increments corresponding to much worse (–2), worse (–1), same (0), better (+1), much better (+2). Scale is broken into approximately 2-week sessions.
Figure 2.
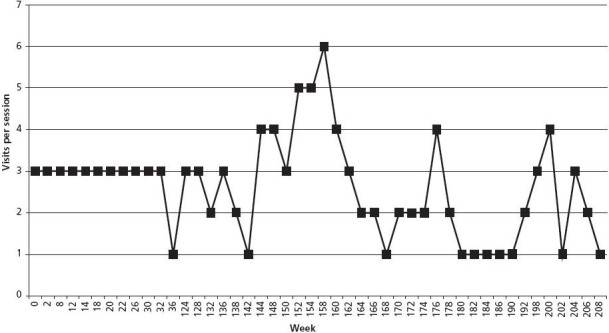
Frequency of patient visits per 2-week session. Graph illustrates the frequency of clinic visits patient had during 2-week intervals.
A follow-up neurological exam was performed in week 228 which showed visual acuity to be 20/40 right-eye, left-eye, and both eyes. Although no initial screening neurological exam was performed at onset of acupuncture, significant advances were seen in comparison to the discharge report from the rehabilitation center. Specific areas of highest improvement based on observation included vision, left lower leg motor control, coordination, right shoulder and arm strength, and motor speech. In an interview with the patient and his mother, his mother noted that at onset of treatment with acupuncture “He could barely lift his arm and now he's swimming! His vision is almost back to perfect; he used to have double vision and trouble with depth perception.” She also noted his progression from wheelchair to walker and then the use of a cane, indicating his significant progress with balance and motor control. Her need for continual oversight had decreased as the patient began to ambulate safely on his own.
DISCUSSION
The strength of this case is related to the profound improvements the patient made during the 4 years of acupuncture treatment. Previous evidence supports that acupuncture, along with traditional therapies, is useful for recovering from TBI, spastic hemiplegia, and diplopia.6,10,11 These improvements are above and beyond the typical improvement observed with standard therapies alone for similar TBIs.10 While limited studies exist looking at outcomes past the initial year post injury, patients with severe TBI have the poorest outcomes and highest rate of mortality.12 The limitations on this case include the fact that the patient was not able to undergo a final outpatient rehabilitation examination. Therefore, at this time, we do not have objective measurements of his progress other than the improvement in his eyesight and observational changes in motor skills and speech. In addition, we have a limited ability to accurately assess the role of acupuncture in his healing vs the roles of pharmacology, occupational therapy, and physical therapy. However, based on historically similar TBIs, the patient's improvements with the inclusion of acupuncture therapy appeared to be dramatically more rapid and successful as compared to conventional treatments alone.
Qi and Blood stagnation is a common symptom pattern following acute trauma. Most often associated with pain, a stagnation pattern can result from any decrease in energy flow in the body. In TCM, Qi and Blood work together. The Chinese philosophy states that “Blood is the mother of Qi” and “Qi governs the Blood.” Deficiencies or excesses in either can compromise function of the TCM organ pairs. The result of this is malnourishment of the tendons and muscles. The liver helps maintain both structure and function of all the tendons in the body by maintaining proper blood and Qi flow. When there is Qi and Blood stagnation, the liver is not able to support all the tendons, which can lead to symptoms including flaccidity, paralysis, myalgia, and other muscular conditions. When Qi and Blood flow are significantly disturbed along with underlying Yin deficiency pattern, the result can be liver Wind. The emotional stress surrounding acute injury and recovery can also increase liver qi stagnation and heat. This results in the signs of muscular tremors, abnormal muscular movements, and paralysis and stiffness. The phlegm retention, manifesting as heavy limbs, mental status changes, and thick coating on the tongue, is a result of the compromised Liver function affecting the Spleen. This process results in decreased Spleen function leading to accumulation of dampness and phlegm.
There is no clear endpoint for people who suffer from TBI. A similar 22-year-old patient diagnosed with a GCS=3 who was treated with physiotherapy without the addition of acupuncture over a course of 3 years, only progressed to the point of being able to eat soup by himself and to take 5 consecutive steps unaided.13 Studies have established that there is no direct correlation with GCS rating and recovery.10 Variables, including age, play a more important role. Studies also show that it is impossible for 1 healing modality to address all the problems TBI patients encounter. Additionally, rehabilitation programs after a TBI lead to better outcomes when most patients attended programs for 3 months.12 In the case presented, the patient was only in the inpatient rehabilitation unit for less than 30 days. The patient initially pursued many different treatment modalities, with acupuncture being the most consistent. Although it is difficult to confirm that acupuncture caused the majority of the positive changes in this case, it is clear that the patient progressed significantly after initiating this treatment regime. Studies have also shown that the addition of acupuncture to patients post-TBI can help reduce long-term emergency care and hospitalizations.4 Additionally, acupuncture used for acute management and rehabilitation of patients with TBI shows success in outcome measures as well as speech and motor assessments and often outperforms conventional therapy alone.11 However, many of these studies are limited to short-term views and do not assess outcomes multiple years post injury. Throughout the course of the acupuncture treatment with this patient, there was slow but continual progress in motor, visual, and speech deficits. Based on the patient's report, his most drastic improvements were with the addition of the eye acupuncture points. In this patient, acupuncture functioned well as an additive and synergistic treatment method along with other ongoing multimodality care for TBI. Long-term speech, physical and occupational therapy were also important to long-term return of function. Overall the patient felt that acupuncture therapy played a key role in the progress of his recovery.
In conclusion, the results presented support that acupuncture therapy should be considered as a viable treatment addition for patients with TBI. A patient-specific treatment protocol focusing on the individual's deficits appears to provide beneficial results in the long-term. An important lesson learned from this case is that future studies would benefit from obtaining more specific baseline measures at the start of acupuncture treatment including neurological screening and vision screening. Additionally, frequent objective measures of progress will enhance the strength of future case studies on acupuncture and TBI. As mentioned, TBI is best treated by a combination of therapies. Beyond conventional pharmacological, occupational, and physical therapies; alternative therapies, including acupuncture, may provide positive synergistic effects when used together.
Disclosures The authors completed the ICMJE Form for Disclosure of Potential Conflicts of Interest and had no conflicts to disclose.
Contributor Information
Jacob Wolf, Southwest College of Naturopathic Medicine, Tempe, Arizona (Dr Wolf), United States.
Linda Sparks, Southwest College of Naturopathic Medicine, Tempe, Arizona (Dr Sparks), United States.
Yong Deng, Southwest College of Naturopathic Medicine, Tempe, Arizona (Dr Deng), United States.
Jeffrey Langland, Southwest College of Naturopathic Medicine, Tempe, Arizona (Dr Langland), United States; Arizona State University, Biodesign Institute, Tempe (Dr Langland), United States.
REFERENCES
- 1.Hemphill JC, III, Phan N. Traumatic brain injury: epidemiology, classification, and pathophysiology. UpToDate. UpToDate, 21 September. [Google Scholar]
- 2.Pangilinan P. Classification and complications of traumatic brain injury: measures of severity. Medscape. http://emedicine.medscape.com/article/326643-overview#aw2aab6b5. Accessed September 29, 2015.
- 3.Katz DI, Zasler ND, Zafonte RD. editors Brain injury medicine: principles and practice. 2nd Ed New York: Demos Medical Publishing, LLC; 2013. [Google Scholar]
- 4.Shih CC, Lee HH, Chen TL. et al. Reduced use of emergency care and hospitalization in patients with traumatic brain injury receiving acupuncture treatment. Evid Based Complement Alternat Med. 2013;2013:262039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Neurological assessment using the Glasgow Coma Scale. http://www.sign.ac.uk/pdf/sign110_annex3.pdf. Accessed September 29, 2015.
- 6.Andruszkow H, Deniz E, Urner J. et al. Physical and psychological long-term outcome after traumatic brain injury in children and adult patients. Health Qual Life Outcomes. 2014. February 26;12:26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Deadman P, Al-Khafaji M, Baker K. A manual of acupuncture. Hove, East Sussex, England: Journal of Chinese Medicine Publications; 2007. [Google Scholar]
- 8.Kuoch DJ. Acupuncture desk reference: your guide to complete knowledge. San Francisco, CA: Acumedwest; 2011. [Google Scholar]
- 9.Maciocia G. Diagnosis by interrogation. : The foundations of Chinese medicine: a comprehensive text for acupuncturists and herbalists. 2nd ed Edinburgh: Elsevier Churchill Livingstone; 2005:320–50. [Google Scholar]
- 10.Gupta A, Taly AB. Functional outcome following rehabilitation in chronic severe traumatic brain injury patients: a prospective study. Ann Indian Acad Neurol. 2012. April;15(2):120–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wong V, Cheuk DK, Lee S, Chu V. Acupuncture for acute management and rehabilitation of traumatic brain injury. Cochrane Database Syst Rev. 2013. March 28;3:CD007700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Catroppa C, Anderson VA, Morse SA, Haritou F, Rosenfeld JV. Outcome and predictors of functional recovery 5 years following pediatric traumatic brain injury (TBI). J Pediatr Psychol. 2008. August;33(7):707–18. [DOI] [PubMed] [Google Scholar]
- 13.Keren O, Reznik J, Groswasser Z. Combined motor disturbances following severe traumatic brain injury: an integrative long-term treatment approach. Brain Inj. 2001. July;15(7):633–8. [DOI] [PubMed] [Google Scholar]


