Abstract
In 2010, global immunization partners posed the question, “Do new vaccine introductions (NVIs) have positive or negative impacts on immunization and health systems of countries?” An Ad-hoc Working Group was formed for WHO’s Strategic Advisory Group of Experts on immunization (SAGE) to examine this question through five approaches: a published literature review, a grey literature review, in-depth interviews with regional and country immunization staff, in-depth studies of recent NVIs in 3 countries, and a statistical analysis of the impact of NVI on DTP3 coverage in 176 countries. The WHO Health System Framework of building blocks was used to organize the analysis of these data to assess potential areas of impact of NVI on health systems. In April 2012, the Ad-hoc Working Group presented its findings to SAGE. While reductions in disease burden and improvements in disease and adverse events surveillance, training, cold chain and logistics capacity and injection safety were commonly documented as beneficial impacts, opportunities for strengthening the broader health system were consistently missed during NVI. Weaknesses in planning for human and financial resource needs were highlighted as a concern. Where positive impacts on health systems following NVI occurred, these were often in areas where detailed technical guidance or tools and adequate financing were available. SAGE supported the Ad-hoc Working Group’s conclusion that future NVI should explicitly plan to optimize and document the impact of NVI on broader health systems. Furthermore, opportunities for improving integration of delivery of immunization services, commodities, and messages with other parts of the health system should be actively sought with the recognition that integration is a bidirectional process. To avoid the gaps in planning for NVI that can compromise existing immunization and health systems, donors and partners should provide sufficient and timely support to facilitate country planning. Areas for future research were also identified. Finally, to support countries in using NVI as an opportunity to strengthen immunization and health systems, the WHO guidance for countries on new vaccine introduction is being updated to reflect ways this might be accomplished.
Keywords: Vaccine introduction, Health systems, Immunization programmes, Health planning, Systems integration, Human resources
1. Introduction
The introduction of new vaccines into national immunization programmes expands opportunities to prevent substantial morbidity and mortality from an increasing number of diseases. The Expanded Programme on Immunization (EPI) was originally established by the World Health Assembly in 1974 to target “some or all of the following diseases: diphtheria, pertussis, tetanus, measles, poliomyelitis, tuberculosis, smallpox and others, where applicable, according to the epidemiological situation in their respective countries” [1]. Following the establishment of EPI, the six EPI vaccines in wide use remained fairly stable for 20–30 years. However, during the past decade, scientific advancements and renewed global commitment to immunization have made an array of additional vaccines available to countries, including to low-income countries. As a consequence, new vaccine introductions (NVIs) have dramatically accelerated.
Successful introductions of new vaccines depend on well-functioning routine immunization and health systems [2]. Because NVIs require these systems to expand their scope, they can also pose challenges to those systems. Weaknesses in NVIs identified during post-introduction evaluations are commonly found to be related to underlying gaps in immunization or health systems, attesting to this correlation between the robustness of a country’s immunization and health systems and the success of a NVI. Concern has been expressed that NVIs could overburden health systems in low- and middle-income countries. On the other hand, introduction of new vaccines could exert a positive effect and offer important opportunities to strengthen health systems.
In June 2009, the WHO Maximizing Positive Synergies Collaborative Group reported on its assessment of the interactions between global health initiatives (GHIs) and country health systems [3]. Recognizing that both positive and negative impacts on health systems have been attributed to GHIs for polio, HIV/AIDS, malaria, and other major initiatives, global immunization partners posed the question, “Do NVIs have positive or negative impacts on immunization and health systems of countries?”.
With several groups interested in this question – including the World Health Organization (WHO), the United States Centers for Disease Control and Prevention (CDC), PATH, the London School of Hygiene and Tropical Medicine (LSHTM), the Maternal and Child Health Integrated Program (MCHIP), the Bill & Melinda Gates Foundation (BMGF), the World Bank, UNICEF, Johns Hopkins Bloomberg School of Public Health, and the GAVI Alliance – there developed an interest in coordinating and collaborating on the various streams of investigation. Early in 2010, an Ad-hoc Working Group, including members from each of the interested groups, was created to examine this issue for WHO’s Strategic Advisory Group of Experts on immunization (SAGE) [4]. The Ad-hoc Working Group embarked on a multi-component examination of the impact of NVIs on immunization and health systems, followed by a joint analysis of the findings, identification of knowledge gaps, and initiation of next steps to translate the findings into practical considerations for programme implementation. In April 2012, the Ad-hoc Working Group presented its findings to SAGE. This paper reviews the Ad-hoc Working Group’s body of completed work, the implications of findings, and next steps.
2. Methods
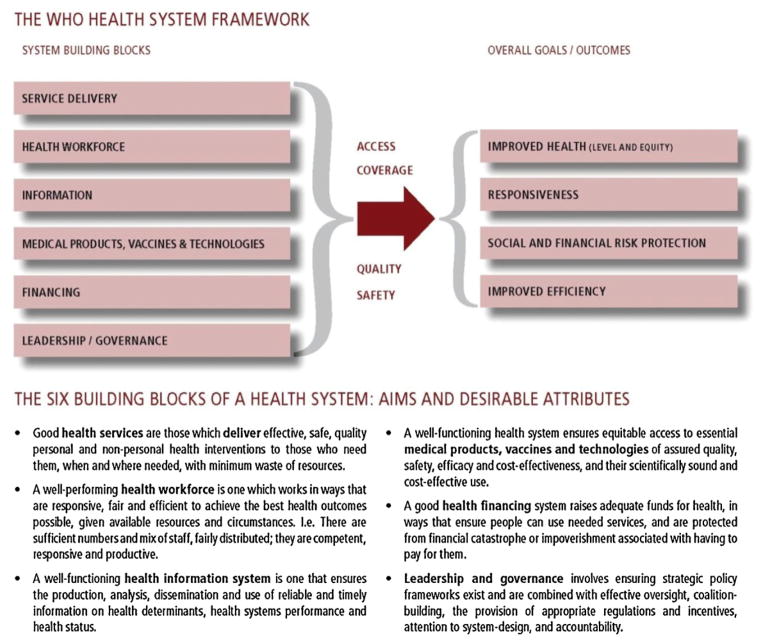
NVI was defined as the introduction of any vaccine beyond the original six EPI vaccines against diphtheria, pertussis, tetanus, measles, poliomyelitis, and tuberculosis. The WHO Health System Framework building blocks [5] was used to organize the analysis of potential areas of impact of NVI on immunization and health systems (Fig. 1). Health systems may be characterized by a set of activities encompassing: service delivery; health workforce; information; medical products, vaccines and technologies; financing and sustainability; and leadership and governance.
Fig. 1.
The WHO Health System Framework.*
*From: WHO. Everybody’s business: strengthening health systems to improve health outcomes – WHO’s framework for action. Geneva: World Health Organization, 2007.
The range of methods used to investigate impacts included: (1) a review of published literature; (2) a review of grey literature; (3) in-depth case studies in three countries; (4) interviews with key informants from countries and WHO Regional Offices; and (5) a multivariable analysis examining impact of NVI on coverage for 3rd dose of diphtheria–tetanus–pertussis vaccine (DTP3). Although five different methods were used, consistent application of the WHO Health System Framework building blocks to organize data allowed for coherent analysis. Table 1 provides an overview of the data sources and their characteristics.
Table 1.
Summary of 5 data sources and their key characteristics.
| Study | Published literature review | Grey literature review | In-depth study of 3 countries | Interviews with country and regional informants | Analysis of impact on DTP3 coverage |
|---|---|---|---|---|---|
| Methodology | Systematic review | Review | Mixed methods | Qualitative | Quantitative |
| Time frame | 1911 to Sept 2010 | Jan 2000–Oct 2010 | July 2011–Jan 2012 | June 2011 | 1999–2009 |
| Methodology description | Search of 7 publication databases using 104terms encompassing immunization and health systems | Search of 7 data sources for documents that were not peer-reviewed or published commercially | Semi-structured interviews and questionnaires | Semi- structured interviews | Multivariate, cross-national,mixed-effect longitudinal model to evaluate new vaccine introduction on DTP3coverage |
| Data sources | Medline, Embase, Nursing Update, West African Journal of Nursing, CINAHL, Web of Science and Global Health | Popline, PubMED, Cochrane Library, ELDIS, System for Information on Grey Literature in Europe, CAB Abstracts, and WHO regional offices | Guatemala – rotavirus vaccine introduction in 2010; Kenya – 10 valent pneumococcal conjugate vaccine introduction in 2011; Mali – Meningococcal A vaccine introduction in 2010/11 | National immunization and health officials of WHO regional offices | WHO/UNICEF Coverage Estimates |
| Scope | 130 articles included in the analysis (of 24,767 articles identified through search terms) | 61 documents included | 116 interviews conducted with national, regional and district staff; 87 health facilities responded to questionnaires | Interviews conducted with 9 senior country immunization programme staff and 7 WHO regional staff | 152 new vaccine introductions included |
| Notable features | 75% of articles from high-income countries; majority of studies not designed to address the research question | Focus on low and middle-income countries; majority of studies not designed to address the research question | Middle and low-income countries with diverse health systems; 3 different vaccines considered | Mostly introduction of pentavalent DTP-hepatitis B-Haemophilus influenzae type b (Hib) or hepatitis B vaccines | Many countries but primarily introduction of pentavalent DTP-hepatitis B-Hib or hepatitis B vaccines |
2.1. Published literature review
Seven publication databases (Medline, Embase, Nursing Update, West African Journal of Nursing, CINAHL, Web of Science and Global Health) were searched for the published literature review [6], using 104 terms encompassing vaccines, immunization systems, and health systems themes. The search, completed on September 29, 2010 and not limited to a beginning year, yielded 24,768 articles. After a standardized review process in which titles and abstracts were screened using set inclusion and exclusion criteria, 130 relevant articles were selected for inclusion in the analysis. A standard abstraction form was developed to systematically abstract information on the study setting, methodology, relevance and impact on immunization and health system. Most of the articles analyzed in the review pertained to experiences in high-income countries.
2.2. Grey literature review
A systematic search of the grey literature [7] included documents that were not peer-reviewed or published commercially, and were written between January 2000 and October 2010. Popline, PubMED, Cochrane Library, ELDIS, System for Information on Grey Literature in Europe, CAB Abstracts, and WHO regional office databases were searched using a combination of free text and MESH terms. In addition, websites of agencies working on immunization and NVI were searched, and additional documents were identified through networking. From among a total of approximately 300 documents, 61 were identified that contained information on the impact of NVI on immunization programmes and, in a few cases, on the broader health system. Most of the 61 documents were Post-Introduction Evaluations (PIEs), PIE summaries, meeting reports and presentations, and consultant reports. These documents focused on low- and middle-income countries.
2.3. In-depth study of three countries
Three low- and middle-income case countries were selected to reflect a variety of vaccines and health systems contexts. Field work was conducted in Guatemala to evaluate a February 2010 introduction of rotavirus vaccine, in Kenya to examine a February 2011 introduction of 10 valent pneumococcal conjugate vaccine (PCV10), and in Mali to assess the introduction of Meningococcal A vaccine through campaigns conducted between September 2010 and November 2011 [8]. Semi-structured interviews were conducted with key informants to assess the impact of NVIs on the health systems of the countries. One hundred-sixteen interviews were conducted with national, regional and district staff. In addition, questionnaires were completed with staff from 87 facilities in selected districts. Interviewees were identified through snowball sampling and field locations were selected to reflect various levels of vaccination coverage, as a proxy for health system strength. In each country, selected routine data were collected at health facility level, including number vaccinated and number receiving antenatal care services before and after the new vaccine was introduced.
2.4. Interviews with country and regional informants
During the annual Global New and Under-utilized Vaccine Implementation meeting in Montreux, Switzerland in June 2011, semi-structured interviews were conducted with nine senior national immunization and health officials and seven WHO regional office staff to gain their perspectives on the impact of recent NVIs on immunization and health systems [9]. Informants were also asked about their views on possible tools to develop for countries to provide guidance on minimizing potential negative effects and maximizing positive impacts on systems when introducing a new vaccine.
2.5. Analysis of impact on DTP3 coverage
Multivariable, cross-national, longitudinal models were developed to evaluate the effect of NVI on DTP3 coverage in 176 countries during 1999–2009 [10]. DTP3 coverage data from the WHO-UNICEF Coverage Estimates [11] were regressed on variables representing the introduction of new vaccines to determine whether NVI significantly contributed to changes in DTP3 coverage in the birth cohort born in the year of NVI. The models controlled for underlying determinants of DTP3 coverage, including national income, access to health services and population health.
3. Results
Findings based on the information available from reviewing the five data sources are described below by WHO health system building block. Available data on impact of NVI on immunization and health systems from the data sources were qualitative, rather than quantitative. It was not possible to establish pre-set indicators for assessment of impact for each building block; whatever findings could be gleaned from the five data sources on any aspect of impact for each building block were extracted. Further details and findings for each data source may be found by reviewing documents located under “Session: Impact of introduction of new vaccines on the strengthening of immunization and health systems” and particularly “Summary of main themes and findings from review of 5 data sources by WHO health system building blocks” [12], located at http://www.who.int/immunization/sage/meetings/2012/april/presentationsbackgrounddocs/en/index.html.
3.1. Service delivery
NVIs appeared to have mixed effects on immunization programmes. Although senior immunization respondents commonly described short-term improvement in coverage for routine vaccines, particularly when introducing new vaccines that targeted highly visible diseases, the analysis of impact of NVI on DTP3 coverage using the multivariable, longitudinal model found no association between the introduction of a new vaccine, either positive or negative, when controlling for other possible determinants of coverage. Short-term negative effects on coverage for routine vaccines as well as for other health services were observed during vaccine campaigns conducted for NVI examined through the in-depth country study. Generally, new vaccines increased community acceptance of immunization programme activities and were viewed positively by health workers; the occasional exceptions to this were related to activity by anti-vaccination movements. There was a generally reported positive impact because of increased use of safe injection equipment and improvements in safe immunization practices. It was not possible to ascertain the impact of NVI on overall non-immunization health service delivery.
3.2. Health workforce
NVIs appeared to have mixed effects on the health work-force who conducted immunization activities. There were positive impacts on health worker immunization skills associated with the training and the short-term enhanced supervision that accompanied NVI. In a number of countries, the ability to offer clients an additional effective health intervention increased health worker motivation. There was at least a short-term increase in staff workload during vaccine introductions. However, countries did not expand their workforces except briefly in the case of specific delivery strategies such as delivery through vaccination campaigns or schools. It was not possible to ascertain impact of NVI on non-immunization activities of the health workforce.
3.3. Information
NVI appeared to have mostly positive effects on information related to immunization systems. Disease surveillance systems at health facility and laboratory levels improved in several countries with enhanced surveillance of diseases prevented by new vaccines. Improved awareness and reporting of Adverse Events Following Immunization (AEFIs) occurred as a result of NVIs in a number of countries. Improvements in surveillance of vaccine preventable diseases led to some improvements in surveillance for other diseases but there were no data on impact of NVI on other health system information systems.
3.4. Supply management (medical products, vaccines, and technologies)
NVI had mixed effects on supply management for immunization systems. Assessment and expansion of cold chain infrastructure often occurred at the national or central level but cold chain infrastructure often remained inadequate at the local or peripheral levels. Even some middle-income countries experienced significant short-term stress on cold storage and transportation capacity for vaccines and other health commodities with NVI. Introductions of combination vaccines placed less stress on immunization systems than introductions of single antigen vaccines. The supply and use of safe injection equipment (auto-disable syringes and safety boxes) was noted to have greatly increased due to NVIs. However, existing weaknesses in vaccine forecasting and stock management were sometimes amplified with NVIs. There was generally no significant improvement in immunization waste disposal, despite increased needs. For health systems generally, there was some limited evidence of positive impact on supply management. In several countries, use of auto-disable syringes and safety boxes for newly introduced vaccines led to their use for other health services. In addition, for a few countries, planning of cold chain expansion for vaccines took cold chain expansion for other medical products into consideration.
3.5. Financing and sustainability
NVIs appeared to have mixed effects on financing and sustainability of immunization programmes. There were substantial increases in programme costs as new vaccines were more expensive than traditional vaccines and collateral expenses related to NVIs were often not adequately anticipated or budgeted. NVIs led to diversification of financing mechanisms and funding sources, including greater government co-financing in some countries and the development of innovative global financing mechanisms. Vaccine introductions also raised concerns of countries being overly dependent on donors and of uncertainty about long-term sustainability of financing for the new vaccines. However, in the short term, most countries successfully managed to mobilize vaccine co-financing and to sustain funding for safe injection equipment. There was some evidence of reduced expenditures for the health system since NVIs contributed to a reduced need for outpatient visits and hospitalizations, with associated reductions in the costs of treating diseases and of responding to disease outbreaks.
3.6. Leadership and governance
NVIs appeared to have positive effects on leadership and governance of immunization programmes. Prompted by activities related to NVI, national immunization technical advisory groups were established or strengthened in a number of countries, and there was increased recognition of the importance of national regulatory authorities. There was some evidence of positive impact on leadership and governance for the overall health system since NVIs led to improved coordination between ministries of health and other government ministries, especially with expansion of vaccination to new target age groups such as school-age children and adults.
4. Discussion
Characterization of the impact of a NVI arguably varies depending not only on the strength of the immunization programme and the health system, but also depending on the vaccine characteristics, the target population, and the delivery mode. Findings from an assessment of impact on an immunization programme or health system can also vary depending on the effect being measured and the timing of the assessment (e.g., 6 weeks, 6 months, 12 months or 2 years after NVI). For these reasons, it was challenging to compare and contrast findings from a multitude of introductions with an array of different vaccines, populations, delivery strategies, timelines, immunization programmes, health systems, and country contexts.
The WHO Health System Framework of building blocks provided a useful structure for comparing data across this array of studies (for details, please see Annex, pages 8–14 [12]). Despite different methodological approaches, the major findings and themes were remarkably consistent across the 5 evaluations, suggesting robustness of the findings.
NVI was associated with positive health system effects. New vaccines resulted in reduced disease incidence that contributed to decline in use of curative services. NVIs brought new technologies such as auto-disable syringes and combination vaccines, enhancements to cold chain, emphasis on training and education of health workers, and increased social mobilization. Technical capacity was increased through strengthened national immunization technical advisory groups, more robust systems for disease surveillance, improvements in injection safety, and more emphasis on AEFI monitoring. Furthermore, communities and health workers generally welcomed the introduction of new vaccines, particularly for diseases with well-recognized and substantial health burdens.
Negative effects associated with NVI appeared to arise when planning was inadequate. For example, at the time of NVI, the peripheral cold chain was not always sufficient and the workload for health workers was sometimes quite heavy. Diversion of efforts toward NVI and away from other aspects of the routine immunization programme was highlighted as a concern. Collateral operational costs of NVI were not always adequately considered or funded and social mobilization and communication were not always sufficiently implemented to adequately educate communities. Different vaccine delivery strategies were noted to have collateral effects – for example, although vaccination campaigns can be highly effective in quickly vaccinating large populations, they could potentially harm routine vaccine coverage and reduce short-term availability of other primary health services. However, this is a characteristic of the delivery strategy rather than whether the vaccine is new to the country and thus can also be seen with other public health service delivery campaigns.
In general, positive effects that occurred following NVI were often in areas for which detailed technical guidance or tools and adequate financing were available (e.g., cold chain, training, surveillance). Importantly, NVI did not commonly occur in tandem with greater integration, coordination, or synergies with other health services. Thus, opportunities for strengthening the broader health system were often missed during NVIs. There was minimal evidence that NVI led to deliberate strategies to use the introduction to strengthen routine immunization or other health services. This finding is consistent with other findings on the evaluation of interactions between disease control programmes and wider health systems [13,14].
To tackle the disconnect between NVI and health system strengthening, future efforts will need to address the specific knowledge gaps identified by this analysis of 5 data sources (Box 1) so that progress can be made to better understand the impact of NVIs on immunization programmes and health systems and how to make that impact beneficial. While this body of work attempted to examine the impact on immunization and health systems from a variety of perspectives, the published and grey literature reviews highlighted the lack of research designed to evaluate this essential question.
Box 1. Knowledge gaps deserving further evaluation.
Areas for future evaluation to better understand impact of vaccine introduction on health systems
Health system: How can the success of a vaccine introduction on the immunization and health systems be appropriately measured? What are the health system determinants of successful vaccine introduction? What aspects of vaccine introduction are key determinants for negative or positive impacts on health systems? How can the success of a vaccine introduction be appropriately measured from a broad health system perspective?
Integrated service delivery: Which health interventions are most appropriate for integration with vaccine delivery? Under what circumstances? What additional resources or conditions are needed? How can planning be improved to enhance integration?
Costs and financing: What are the actual costs of new vaccine introduction, including collateral costs? Is there re-direction of resources from other health programmes to finance vaccine introductions?
Equity: What can be done to improve equity of access and health benefits when a vaccine is being introduced?
Another way to address the absence of an adequate link between NVI and health systems strengthening is by systematically considering and developing plans to optimize the impact of vaccine introduction on broader health systems, and by monitoring and evaluating those efforts. As an initial step in this direction, the Ad-hoc Working Group translated the findings from this data analysis into more practical information for countries by developing Principles for Adding a Vaccine to a National Immunization Programme. In January 2012, the Principles were shared for review, comments, and endorsement by global immunization partners. The Principles were further finalized and endorsed at the April 2012 SAGE meeting (Box 2) [15].
Box 2. Principles for adding a vaccine to a national immunization programme while strengthening the immunization and health systems.
Optimal new vaccine introduction that strengthens health systems benefits from:
A strong, country-led, evidence-based decision-making, planning, and prioritization process that is accountable and coordinated with other components of the health system.
A well-performing or improving and responsive immunization programme.
-
Seizing the opportunity to achieve:
A well-trained and motivated workforce
Quality education and communication about the new vaccine for the health workforce and community
Functional cold storage, logistics and vaccine management systems
Safe immunization practices and monitoring of adverse events
High-quality monitoring and evaluation, including disease surveillance and immunization coverage monitoring
Resource, performance, and management accountability.
Maximizing opportunities to deliver vaccines as integral components of comprehensive health promotion and disease prevention and control efforts so that vaccines are delivered as part of a package of effective, feasible, and affordable interventions based on national contexts.
Sufficient allocation of human and financial resources to introduce the new vaccine and sustain its use without adversely affecting other programmes and services.
A safe and efficacious vaccine that is appropriate for local use and is available with an uninterrupted, sufficient supply.
To further support countries to explicitly consider and plan to optimize the impact of NVI on immunization programmes and the broader health systems, the 2005 WHO Vaccine Introduction Guidelines [16] are being updated to assist decision-makers, country immunization programme managers, and global partners with identifying and taking opportunities to strengthen the health system throughout the process of NVI, from decision-making through planning, implementation, and evaluation. The forthcoming WHO guidance, entitled “Principles and considerations for adding a vaccine into a national immunization programme,” outlines considerations to be addressed for strengthening the health system that are intended to be flexibly applied to suit local contexts; these considerations are not intended as requirements or obstacles to NVI.
Viewing health service delivery in a holistic and integrated manner rather than as independent, disparate programmes is recognized as necessary in order to achieve efficiencies and avoid fragmentation. Opportunities for improving integration of delivery of services, commodities, and messages with other parts of the health system should be actively sought with the recognition that integration is a bi-directional process, so success will take time, effort, and mutual collaboration.
For the donor and partner community, this analysis highlights the need to avoid the gaps in planning and resourcing for NVI that can compromise or burden existing immunization and health systems. Where financial and technical resources are being offered, donors and partners should provide such support in a timely and sufficient manner to facilitate country planning and to support evaluation of impact of NVI on health systems.
All six of the strategic objectives of the Global Vaccine Action Plan (GVAP), endorsed by the World Health Assembly in May 2012 [2], are essential for NVIs and for continuous improvement of immunization and health systems. In particular, the Ad-hoc Working Group’s analysis underscores the importance of the elements (e.g., information, health workforce, management, infrastructure, logistics, vaccine supply, leadership, financing, and delivery of vaccines with complementary services) outlined in Strategic objective 4: strong immunization systems are an integral part of a well-functioning health system. By proposing a more integrated approach to service delivery and a comprehensive approach to disease control, as well as more effective planning of NVI that strengthens immunization and health systems, the Ad-hoc Working Group’s findings give an additional impetus to the GVAP. It is now up to countries and the international community to ensure that we are all accountable for giving life to these principles and for building effective evaluation mechanisms into the process of NVIs.
Acknowledgments
For their contributions to the collection and analysis of data, the authors wish to acknowledge and thank Helen Burchett (London School of Hygiene and Tropical Medicine), Denise DeRoeck (Consultant to WHO), Robert Steinglass (MCHIP), Denis Porignon (WHO), and Maritel Costales (UNICEF).
Footnotes
Conflict of interest
None of the authors have conflicts of interest.
Contributor Information
Susan A. Wang, Email: wangsu@who.int.
Terri B. Hyde, Email: thyde@cdc.gov.
Sandra Mounier-Jack, Email: Sandra.Mounier-Jack@lshtm.ac.uk.
Logan Brenzel, Email: loganbrenzel@gmail.com.
Michael Favin, Email: mfavin@manoffgroup.com.
W. Scott Gordon, Email: sgordon@path.org.
Jessica C. Shearer, Email: shearejc@mcmaster.ca.
Carsten F. Mantel, Email: mantelc@who.int.
Narendra Arora, Email: nkarora@inclentrust.org.
David Durrheim, Email: David.Durrheim@newcastle.edu.au.
References
- 1.World Health Organization. Twenty-seventh World Health Assembly 1974. Geneva: World Health Organization; 1974. Resolution WHA 27.57. WHO Expanded Programme on Immunization. WHA27/1974/REC/1. [Google Scholar]
- 2.Decade of Vaccines Collaboration. Global Vaccine Action Plan. Vaccine. 2013;31:B5–31. doi: 10.1016/j.vaccine.2013.02.015. [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization Maximizing Positive Synergies Collaborative Group. Samb B, Evans T, Dybul M, Atun R, Moatti JP, et al. An assessment of interactions between global health initiatives and country health systems. Lancet. 2009;373(June 9681):2137–69. doi: 10.1016/S0140-6736(09)60919-3. [DOI] [PubMed] [Google Scholar]
- 4.World Health Organization. Meeting of the Strategic Advisory Group of Experts on immunization, April 2010 – conclusions and recommendations. Wkly Epidemiol Rec. 2010;85(May 22):197–212. [PubMed] [Google Scholar]
- 5.World Health Organization. Everybody’s business: strengthening health systems to improve health outcomes – WHO’s framework for action. Geneva: World Health Organization; 2007. [Google Scholar]
- 6.Hyde TB, Dentz H, Wang SA, Burchett H, Mounier-Jack S, Mantel CF, et al. The impact of new vaccine introduction on immunization and health systems: a review of the published literature. Vaccine. 2012;30(Aug 29):6347–58. doi: 10.1016/j.vaccine.2012.08.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Favin M, Macabasco R, Steinglass R. Impact of new vaccine introduction on developing country immunization programs and broader health systems: a review of the grey literature. Prepared for the 10–12 April 2012 Meeting of the WHO Strategic Group of Experts on immunization; Geneva. 2012; Available at: http://www.who.int/immunization/sage/meetings/2012/april/presentationsbackgrounddocs/en/index.html. [Google Scholar]
- 8.Mounier-Jack S, Burchett H, Griffiths U. Impact of vaccine introductions on EPI and health systems: preliminary findings from 3 countries. Prepared for the 10–12 April 2012 Meeting of the WHO Strategic Group of Experts on immunization; Geneva. 2012; Available at: http://www.who.int/immunization/sage/meetings/2012/april/presentationsbackgrounddocs/en/index.html. [Google Scholar]
- 9.DeRoeck D. Impact of vaccine introductions on immunization and health systems: interviews with EPI managers and WHO regional officers held during the 2011 annual NUVI meeting. Prepared for the 10–12 April 2012 Meeting of the WHO Strategic Group of Experts on immunization; Geneva. 2012; Available at: http://www.who.int/immunization/sage/meetings/2012/april/presentationsbackgrounddocs/en/index.html. [Google Scholar]
- 10.Shearer JC, Walker DG, Risko N, Levine OS. The impact of new vaccine introduction on the coverage of existing vaccines: a crossnational, multivariable analysis. Vaccine. 2012 doi: 10.1016/j.vaccine.2012.10.036. http://dx.doi.org/10.1016/j.vaccine.2012.10.036. [DOI] [PubMed]
- 11.World Health Organization and UNICEF. WHO-UNICEF estimates of immunization coverage, 7 October 2009. Geneva: World Health Organization; 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.World Health Organization. Summary of main themes and findings from review of 5 data sources by WHO health system building blocks, Annex, pages 8–14. Prepared for the 10–12 April 2012 Meeting of the WHO Strategic Advisory Group of Experts on immunization; Geneva. 2012; Available at http://www.who.int/immunization/sage/meetings/2012/april/presentationsbackgrounddocs/en/index.html. [Google Scholar]
- 13.Mounier-Jack S, Rudge JW, Phetsouvanh R, Chanthapadith C, Coker R. Critical interactions between Global Fund-supported programmes and health systems: a case study in Lao People’s Democratic Republic. Health Policy Plan. 2010;25(November Suppl 1):i37–42. doi: 10.1093/heapol/czq056. [DOI] [PubMed] [Google Scholar]
- 14.Rudge JW, Phuanakoonon S, Nema KH, Mounier-Jack S, Coker R. Critical interactions between Global Fund-supported programmes and health systems: a case study in Papua New Guinea. Health Policy Plan. 2010;25(November Suppl 1):i48–52. doi: 10.1093/heapol/czq058. [DOI] [PubMed] [Google Scholar]
- 15.World Health Organization. Meeting of the Strategic Advisory Group of Experts on Immunization, April 2012 – conclusions and recommendations. Wkly Epidemiol Rec. 2012;87(May 21):201–16. [PubMed] [Google Scholar]
- 16.WHO. Adding a vaccine to a national immunization programme: decision and implementation. Geneva: World Health Organization; 2005. Vaccine introduction guidelines. WHO/IVB/05.18. [Google Scholar]