Abstract
Clinical outcomes after a hospital discharge are poorly defined for patients receiving maintenance in-center (outpatient) hemodialysis. To describe the proportion and characteristics of these patients who are rehospitalized, visit an emergency department, or die within 30 days after discharge from an acute hospitalization, we conducted a population-based study of all adult patients receiving maintenance in-center hemodialysis who were discharged between January 1, 2003, and December 31, 2011, from 157 acute care hospitals in Ontario, Canada. For patients with more than one hospitalization, we randomly selected a single hospitalization as the index hospitalization. Of the 11,177 patients included in the final cohort, 1926 (17%) were rehospitalized, 2971 (27%) were treated in the emergency department, and 840 (7.5%) died within 30 days of discharge. Complications of type 2 diabetes mellitus were the most common reason for rehospitalization, whereas heart failure was the most common reason for an emergency department visit. In multivariable analysis using a cause-specific Cox proportional hazards model, the following characteristics were associated with 30-day rehospitalization: older age, the number of hospital admissions in the preceding 6 months, the number of emergency department visits in the preceding 6 months, higher Charlson comorbidity index score, and the receipt of mechanical ventilation during the index hospitalization. Thus, a large proportion of patients receiving maintenance in-center hemodialysis will be readmitted or visit an emergency room within 30 days of an acute hospitalization. A focus on improving care transitions from the inpatient setting to the outpatient dialysis unit may improve outcomes and reduce healthcare costs.
Keywords: clinical epidemiology, hemodialysis, hospitalization
Reducing hospital readmissions and emergency department visits after hospital discharge has become a key priority for policymakers, healthcare leaders, and clinicians.1 The unnecessary use of these resources is increasingly considered to be a marker of the quality of care provided to patients and the effectiveness of the discharge process.2
Patients receiving maintenance in-center (outpatient) hemodialysis are frequently hospitalized and account for 5%–7% of healthcare expenditures in developed countries despite comprising a very small percentage of the general adult population.3–5 These patients possess several characteristics that make them vulnerable to rehospitalization and emergency department use after discharge, including multimorbidity, complex medication regimens, and frequently a distinct care team in the hospital and outpatient setting that may lead to disjointed care.4,6 Despite this, relatively little is known about discharge outcomes after hospitalization for patients receiving maintenance in-center hemodialysis.4,7 Consequently, clinicians and policy makers do not have a fully accurate representation of healthcare resource use of this vulnerable patient group in the period after hospital discharge. Without a clear understanding of the barriers to care transition and the costs thereof, policymakers are less able to develop policies aiming to improve outcomes while controlling costs.
The universal healthcare system in Ontario, Canada, with well recorded health service information, provided a unique opportunity to study the acute care resource use of patients receiving maintenance hemodialysis across 35 outpatient dialysis centers in the 30 days after hospital discharge. Accordingly, we used population-based, linked healthcare databases to identify patients who were discharged from acute care hospitals to determine the proportion of discharges that are followed by a rehospitalization and emergency department visit within 30 days of hospital discharge. We also aimed to determine the clinical diagnoses leading to rehospitalization and emergency department visits, and to identify predictors of rehospitalization within 30 days.
Results
Patient Characteristics
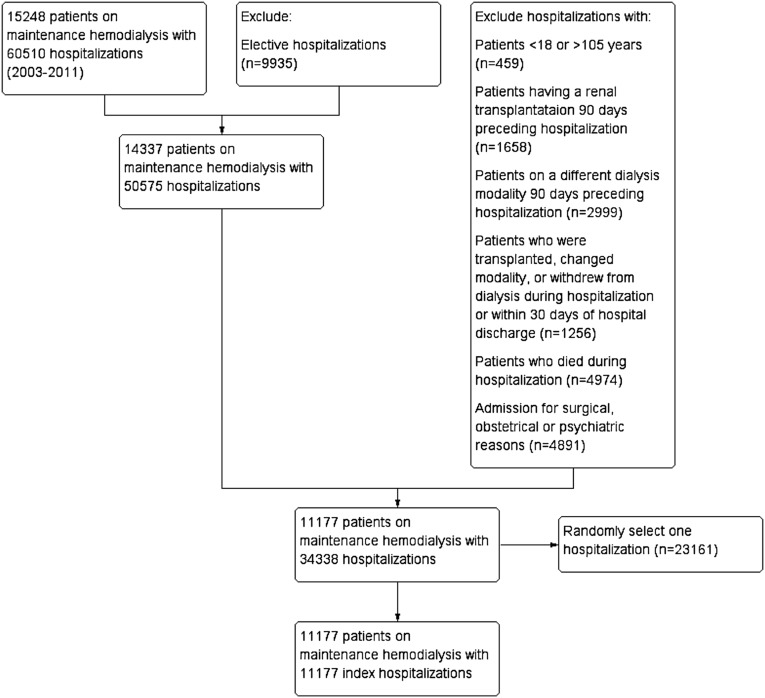
Between 2003 and 2011, 15,248 patients receiving maintenance in-center hemodialysis were hospitalized 60,510 times. Of these 15,248 patients, 11,177 (78%) patients were included in the final cohort (only one hospitalization was counted per patient) (Figure 1).
Figure 1.
Cohort selection.
The mean age of the cohort was 66 years, approximately 42% of patients were women, and 93% lived in the community (as opposed to a chronic care facility, rehabilitation facility, or nursing home). More than one half of patients (54%) had at least one hospitalization in the 6 months before their index hospitalization, whereas 92% had visited the emergency department during this period. Over 90% of patients had hypertension, 68% had coronary artery disease, and 62% had diabetes. The median Charlson index score for the cohort was 4 (interquartile range [IQR], 3–6). The mean time on dialysis for the cohort was 3.2 (SD 4.3) years.
The median length of stay for the index hospitalization was 5 days (IQR, 2–10 days) and 5% of patients received mechanical ventilation during the index hospitalization. Sixty percent of patients were admitted to the same hospital as their dialysis unit. Almost 85% of patients were discharged to their home after the index hospitalization, and almost 7% were discharged to nursing homes (Table 1).
Table 1.
Characteristics of the cohort
| Characteristic | Overall Cohort (N=11,177) | Hospitalization in Prior 6 mo | Standardized Difference (%) | |
|---|---|---|---|---|
| Yes (n=6075) | No (n=5102) | |||
| Demographic | ||||
| Age (yr), mean (SD) | 66.4 (15.1) | 66.3 (14.9) | 66.6 (15.4) | 2 |
| Women, n (%) | 4668 (41.8) | 2544 (41.9) | 2124 (41.6) | 1 |
| Place of residence before index hospitalization, n (%) | ||||
| Home | 10433 (93.3) | 5620 (92.5) | 4813 (94.3) | 7 |
| Rehabilitation facility | 115 (1.0) | a | a | a |
| Nursing home | 625 (5.6) | 338 (5.6) | 287 (5.6) | 0 |
| Complex continuing care | a | a | a | a |
| Healthcare utilization in prior 6 mo | ||||
| Number of emergency department visits, mean (SD) | 2.4 (2.4) | 3.0 (2.7) | 1.6 (1.6) | 64 |
| Clinical, n (%) | ||||
| Diabetes | 6931 (62.0) | 3884 (63.9) | 3047 (59.7) | 9 |
| Congestive heart failure | 6133 (54.9) | 3664 (60.3) | 2469 (48.4) | 24 |
| Coronary artery disease | 7598 (68.0) | 4351 (71.6) | 3247 (63.6) | 17 |
| Hypertension | 10168 (91.0) | 5627 (92.6) | 4541 (89.0) | 13 |
| Chronic obstructive pulmonary disease | 5272 (47.2) | 3092 (50.9) | 2180 (42.7) | 16 |
| Cerebrovascular disease | 888 (7.9) | 589 (9.7) | 299 (5.9) | 14 |
| Cancer | 283 (2.5) | 199 (3.3) | 84 (1.6) | 11 |
| Chronic liver disease | 1579 (14.1) | 965 (15.9) | 614 (12.0) | 11 |
| Peripheral vascular disease | 2126 (19.0) | 1255 (20.7) | 871 (17.1) | 9 |
| Charlson index, median (IQR) | 4 (2–6) | 5 (3–6) | 4 (2–5) | 50 |
| Time on dialysis (d), mean (SD) | 1164 (1555) | 1041 (1536) | 1311 (1565) | 17 |
| Hospital | ||||
| Teaching hospital, n (%) | 3894 (34.8) | 2127 (35.0) | 1767 (34.6) | 1 |
| Index admission | ||||
| Length of stay (d), median (IQR) | 5 (2–10) | 5 (2–11) | 5 (2–9) | 1 |
| Mechanical ventilation, n (%) | 514 (4.6) | 326 (5.4) | 188 (3.7) | 8 |
| Patient receiving in-center dialysis at index hospital, n (%) | 6645 (59.5) | 3528 (58.1) | 3117 (61.1) | 6 |
| Site of care after discharge, n (%) | ||||
| Home | 9338 (83.5) | 4960 (81.6) | 4378 (85.8) | 11 |
| Rehabilitation facility | 428 (3.8) | 248 (4.1) | 180 (3.5) | 3 |
| Nursing home | 766 (6.9) | 422 (7.0) | 344 (6.7) | 1 |
| Complex continuing care | 645 (5.8) | 445 (7.3) | 200 (3.9) | 15 |
Suppressed because of small cell count (<5).
Patients who were hospitalized within 6 months of their index hospitalization had a higher mean number of emergency department visits (3.0 versus 1.6) in the 6 months before their index hospitalization compared with those who were not hospitalized. They also had a higher proportion of congestive heart failure (60.3% versus 48.4%), coronary artery disease (71.6% versus 63.6%), and a higher median Charlson score (5 versus 4) (Table 1).
Thirty-Day Emergency Department Visits, Rehospitalizations, and Deaths
More than one in four (27%) patients receiving maintenance in-center hemodialysis visited an emergency department in the 30 days after their index hospitalization. Of these visits, 46% resulted in a rehospitalization and 52% resulted in discharge from the emergency department (treat-and-release visit), with the other 2% having died in the emergency department. The median number of days between the date of discharge and the emergency department visit was 11 days (IQR, 5–19 days). Seventy-four percent of patients receiving maintenance in-center hemodialysis visited the emergency department at the same hospital from which they were discharged, and almost 50% visited the emergency department of the hospital where they regularly received dialysis. Approximately 8% of emergency department visits were for the same reason as the index hospitalization. The most common diagnoses for a visit to the emergency department were heart failure (4.4%), followed by throat and chest pain (4.2%), and abdominal pain (3.7%) (Table 2).
Table 2.
Characteristics of index hospitalization, rehospitalization, and emergency department visits among chronic hemodialysis recipients rehospitalized or visiting the emergency department after discharge from a hospital stay for a medical indication
| Characteristic | Value |
|---|---|
| No. of chronic hemodialysis recipients with at least one acute medical hospitalization (2003–2011)a | 11,177 |
| Hemodialysis recipient outcomes (30 d after index hospitalization) | |
| Rehospitalization | 1926 (17.2) |
| Emergency department visit | 2971 (26.6) |
| Death | 840 (7.5) |
| Features of the index hospitalization (N=11,177) | |
| Length of stay (d) | 5 (2–10) |
| Five most common diagnosesb | Complications of cardiac and vascular prosthetic devices, implants, and grafts; complications of type 2 diabetes mellitus; heart failure; pneumonia, organism unspecified; and acute myocardial infarction |
| Features of the rehospitalization (n=1 926) | |
| No. of days between index hospitalization discharge and rehospitalization | 11 (15–19) |
| Rehospitalization at the same institution as the index hospitalization | 1567 (81.4) |
| Most responsible diagnosis for rehospitalization the same as for the index hospitalization | 343 (17.8) |
| Five most common diagnosesb | Complications of type 2 diabetes mellitus; heart failure; other septicemia; acute myocardial infarction; and complications of cardiac and vascular prosthetic devices, implants, and grafts |
| Features of the emergency department visit (n=2971) | |
| No. of days between index hospitalization discharge and emergency department visit | 11 (5–19) |
| Emergency department visit to same hospital as discharging hospital | 2203 (74.2) |
| Emergency department visit to same hospital as dialysis unit | 1467 (49.4) |
| Discharge disposition | |
| Discharged (i.e., treat-and-release visit) | 1540 (51.8) |
| Admitted to hospital | 1378 (46.4) |
| Died | 53 (1.8) |
| Most responsible diagnosis for emergency department visit the same as for the index hospitalization | 246 (8.3) |
| Five most common diagnosesb | Heart failure; pain in throat and chest; abdominal and pelvic pain; abnormalities of breathing; and pneumonia, organism unspecified |
Data are presented as n (%) or median (IQR). ICD-10, International Classification of Diseases, 10th Revision.
Hemodialysis recipients with more than one hospitalization had a single hospitalization randomly selected and designated the index hospitalization.
Using the first three digits of the most responsible ICD-10 code.
In the 30 days after the index hospitalization, 1926 (17.2%) patients receiving maintenance in-center hemodialysis were rehospitalized. The median number of days between the discharge date and the rehospitalization date was 11 (IQR, 5–19). More than four in five (1567 patients or 81%) who were rehospitalized were admitted to the same hospital as their index hospitalization. The five most common rehospitalization diagnoses included complications related to type 2 diabetes mellitus (6.3%), heart failure (5.6%), septicemia (5.2%), acute myocardial infarction (3.6%), and complications related to cardiac and vascular prosthetic devices (3.4%). Interestingly, >80% of rehospitalizations were in a distinct diagnostic category compared with the initial hospitalization (Table 2).
In the 30 days after hospital discharge, 840 (7.5%) patients died.
Predictors of Rehospitalization
In multivariable analysis using a cause-specific hazard model, older age (adjusted hazard ratio [aHR], 1.07; 95% confidence interval [95% CI], 1.04 to 1.11 per decade), the number of prior hospital admissions in the preceding 6 months (aHR, 1.13; 95% CI, 1.09 to 1.17 per hospitalization), the number of prior emergency department visits in the past 6 months (aHR, 1.03; 95% CI, 1.02 to 1.04 per visit), higher Charlson comorbidity index score (aHR, 1.08; 95% CI, 1.06 to 1.11 per unit), and the receipt of mechanical ventilation during the index hospitalization (aHR, 1.33; 95% CI, 1.09 to 1.61) were significantly associated with an increase in the rate of 30-day rehospitalization (single hospitalization, randomly chosen). Being discharged to complex continuing care after the index hospitalization (aHR, 0.56; 95% CI, 0.44 to 0.72) was significantly associated with a lower risk for 30-day rehospitalization (Table 3).
Table 3.
Association of patient and hospital characteristics with 30-day rehospitalization compared with no 30-day rehospitalization (randomly chosen, single hospitalization)
| Characteristic | Cause-Specific Hazard Ratio (95% Confidence Interval) |
|---|---|
| Demographic | |
| Age, per decade | 1.07 (1.04 to 1.11) |
| Female sex | 1.01 (0.92 to 1.11) |
| Healthcare utilization | |
| Prior hospital admissions within the past 6 mo, per hospital admission | 1.13 (1.09 to 1.17) |
| Number of emergency department visits within the past 6 mo, per emergency room visit | 1.03 (1.02 to 1.04) |
| Charlson index, per unit | 1.08 (1.06 to 1.11) |
| Dialysis characteristics | |
| Time on dialysis, per year | 1.01 (0.99 to 1.02) |
| Hospital | |
| Teaching (versus community) hospital | 1.05 (0.96 to 1.15) |
| Index admission | |
| Length of stay, per day | 1.00 (1.00 to 1.00) |
| Admission to same hospital as dialysis unit | 0.97 (0.88 to 1.06) |
| Mechanical ventilation | 1.33 (1.09 to 1.61) |
| Site of care after discharge | |
| Community | 1.00 (referent) |
| Rehabilitation facility | 0.82 (0.64 to 1.05) |
| Nursing home | 0.94 (0.78 to 1.12) |
| Complex continuing care | 0.56 (0.44 to 0.72) |
When repeat hospitalization events were accounted for, the number of prior hospital admissions in the preceding 6 months (aHR, 1.13; 95% CI, 1.12 to 1.15 per hospitalization), the number of prior emergency department visits in the past 6 months (aHR, 1.03; 95% CI, 1.02 to 1.04 per visit), and a higher Charlson comorbidity index score (aHR, 1.06; 95% CI, 1.04 to 1.07 per unit) were associated with an increased risk of 30-day rehospitalization. Discharge to complex continuing care (aHR, 0.62; 95% CI, 0.53 to 0.73) was significantly associated with a lower risk for 30-day rehospitalization (Table 4).
Table 4.
Association of patient and hospital characteristics with 30-day rehospitalization compared with no 30-day rehospitalization (all eligible hospitalizations).
| Characteristic | Cause-Specific Hazard Ratio (95% Confidence Interval) |
|---|---|
| Demographic | |
| Age, per decade | 1.00 (0.98 to 1.02) |
| Female sex | 1.00 (0.95 to 1.05) |
| Healthcare utilization | |
| Prior hospital admissions within the past 6 mo, per hospital admission | 1.13 (1.12 to 1.15) |
| Number of emergency department visits within the past 6 mo, per emergency room visit | 1.03 (1.02 to 1.04) |
| Charlson index, per unit | 1.06 (1.04 to 1.07) |
| Dialysis characteristics | |
| Time on dialysis, per year | 1.00 (1.00 to 1.01) |
| Hospital | |
| Teaching (versus community) hospital | 1.04 (0.98 to 1.09) |
| Index admission | |
| Length of stay, per day | 1.00 (1.00 to 1.00) |
| Admission to same hospital as dialysis unit | 1.03 (0.98 to 1.08) |
| Mechanical ventilation | 1.08 (0.96 to 1.21) |
| Site of care after discharge | |
| Community | 1.00 (referent) |
| Rehabilitation facility | 0.78 (0.68 to 0.91) |
| Nursing home | 1.04 (0.94 to 1.14) |
| Complex continuing care | 0.62 (0.53 to 0.73) |
Discussion
Almost one half of patients receiving maintenance in-center hemodialysis who survive an acute medical hospitalization visit the emergency department or are rehospitalized in the 30-day period after discharge. This proportion is almost twice that of the general Canadian population and reflects the disease burden of patients receiving hemodialysis, and their vulnerability to recurrent illness.8 A minority of rehospitalizations and emergency department visits were for similar reasons as the initial hospitalization, suggesting that other, less immediate medical issues might have been inadequately addressed on the initial hospital stay (e.g., subclinical heart failure in a patient hospitalized for vascular access infection).
Investigators in the United States have previously studied the acute care resource use of patients receiving hemodialysis in the period after hospital discharge, focusing solely on 30-day rehospitalizations.4 Our study extends the knowledge of posthospitalization healthcare use in patients receiving maintenance in-center hemodialysis by also considering emergency department visits.
The US Renal Data System (USRDS) reported that 36% of discharges from an all-cause hospitalization were followed by a rehospitalization within 30 days in hemodialysis recipients.4 By contrast, our study found that in Ontario, Canada, patients receiving maintenance in-center hemodialysis are roughly one half as likely to be rehospitalized relative to patients in the United States. This difference may be attributable to variation in the provision of dialysis care and reimbursement policies between units in Ontario and the United States, as well as differences in the study cohorts. Specifically, in Ontario, dialysis units are not-for-profit units and are mostly located within a hospital setting. They are also staffed primarily by registered nurses, and consistently dialyze patients for a fixed amount of time. By contrast, the majority of dialysis units included in the USRDS data are for-profit satellite dialysis units, which employ fewer personnel per dialysis run, generally employ less highly skilled personnel (e.g., technicians, compared with registered nurses), and have historically offered shorter dialysis treatments.9,10 Indeed, a recent study demonstrated a lower rate of rehospitalization in not-for-profit units compared with for-profit dialysis units, which may represent differences in the quality of care.11
On a similar note, the affiliation of dialysis units with hospitals may be an important factor in the lower rehospitalization rates in Canadian dialysis units compared with those in the United States. This may occur through a number of mechanisms, including the improved transmission of discharge information via shared informatics, hospital-physician continuity of care, and improved access to healthcare resources including specialists in the outpatient dialysis unit. Unfettered access to hospitalization information by way of shared information technology and timely communication of discharge summaries has been demonstrated to improve clinical outcomes primarily by eliminating an important lag time in which lapses in care may occur.12–14 Similarly, hospital-physician continuity of care has been demonstrated to reduce rehospitalizations.15 Familiarity with the hospital course allows follow-up physicians to determine therapeutic effectiveness and identify complications of hospital therapies or procedures. Because patients are often discharged from the hospital with problems that are improving but not yet resolved, if a physician knows that a particular patient was worse when he or she was admitted to hospital, they would be less apt to interpret a patient’s current clinical conditions as a deterioration, thereby possibly preventing rehospitalization. Finally, the close proximity of the outpatient dialysis unit to the hospital may permit greater access to healthcare resources such as specialist consultation during outpatient hemodialysis treatment, which may allow more timely institution of therapies, thereby potentially preventing clinical deterioration and subsequent rehospitalization.
Despite the potential benefits of hospital-dialysis unit affiliations in Ontario, rehospitalization rates among patients receiving maintenance dialysis are still almost twice as high as in the general population (8.5%), which may hint at a broader failure of the discharge process owing to lapses in communication between the discharging hospital and the receiving hemodialysis unit.16 In our study, 40% of hemodialysis recipients had their index hospitalization in the same facility as their dialysis unit. This may have led to discontinuity in the timely transmission of important discharge information from the hospital to the dialysis unit. Because patients generally require dialysis three times per week, they often visit their dialysis facility within 1–2 days after hospital discharge. Failure to provide timely access to information concerning changes to the patients’ dialysis prescription, medications, and underlying healthcare issues may impede the ability of the dialysis unit to provide high-quality and appropriate care.
The high rehospitalization rates among patients receiving maintenance dialysis in our study is also surprising considering that patients on maintenance dialysis are observed for several hours, typically thrice weekly. Indeed, early and sustained follow-up after hospitalization has been shown to decrease rehospitalization rates across a spectrum of conditions.17,18 This benefit is hypothesized to manifest primarily through the improvement of the transition of care from the inpatient to outpatient setting. Specifically, early follow-up should improve the level of attention to pressing health conditions that prompted hospitalization—a potential benefit if problems are few, but a potential problem where problems are many and more than one or two of these problems require coordinated care with non-nephrologists. Early follow-up also allows for the detection of signs and symptoms of disease and timely intervention in an outpatient setting before rehospitalization is required. Indeed, a few small studies have demonstrated that early interventions such as hemoglobin monitoring and erythropoietin dosing changes for patients receiving maintenance dialysis after hospital discharge are associated with a decreased risk for rehospitalization.19,20
Although early follow-up may represent one piece of the puzzle in mitigating rehospitalization, the most effective strategy is likely for the hemodialysis unit to possess the capability to deal with intercurrent illnesses in the unit itself. This is challenging in light of the large burden of comorbid disease experienced by patients on dialysis, compounded by their heightened susceptibility to developing new impairments during hospitalization, their increased vulnerability to illness after discharge, and the setup of modern dialysis units. It is plausible that a combination of these factors may negate the benefits of early and sustained follow-up. As such, the dialysis healthcare team may not possess the resources, expertise, or ability to manage all of the medical issues of their patients receiving maintenance hemodialysis in an outpatient setting, which may necessitate an emergency department referral and/or hospitalization.
In line with previous studies, approximately 80% of rehospitalizations in our cohort were for reasons different from those responsible for the index hospitalization.2,21,22 This finding has been ascribed, in part, to the development of a “posthospitalization syndrome,” which is a generalized vulnerability to illness among recently discharged patients, many of whom have developed new physiologic and psychologic impairments both during and after hospitalization.23 Given hemodialysis patients’ multiple comorbid conditions and complex healthcare needs, they are particularly vulnerable to the posthospitalization syndrome.
Indeed, studies have demonstrated that a multifaceted, coordinated approach between the inpatient service and outpatient specialists reduces rehospitalizations by addressing not only the acute illness leading to the initial hospitalization but also risk factors for the posthospitalization syndrome.24,25 As such, close coordination between the inpatient team, dialysis unit, and nephrologist is paramount. For example, during the initial hospitalization, the inpatient team should not only focus on the urgencies of the acute illness, but should also seek to promote health actively by strengthening patients and contributing to their physiologic reserve. Once the transition is made to the outpatient setting, the dialysis unit and nephrologist should frequently assess patients for changes in their clinical condition as well as apply interventions aimed at promoting practices that reduce the risk of delirium and confusion, emphasizing physical activity and strength maintenance or improvement, and enhancing cognitive and physical function, all of which may decrease the risk for rehospitalization.
Novel to our study is that we also assessed the use of emergency department resources after hospital discharge and found that almost one-quarter of hospital discharges resulted in an emergency department visit within 30 days of discharge, the majority of which were treat-and-release types of visits. There are a few reasons to explain our findings. First, dialysis units may be using the “path of least resistance” and referring patients with acute and subacute or chronic illnesses to the emergency department, even if the medical issue at hand can potentially be dealt with in the dialysis unit. However, a minority of emergency department visits (<10%) were for conditions that could be realistically managed in the dialysis unit (e.g., hyperkalemia, heart failure, or vascular access issues). Second, the high rate of treat-and-release emergency department visits may be representative of the complexity of dialysis patients and the inability of the dialysis unit to provide monitoring and management of a number of acute conditions such as chest pain or an acute abdomen, which require specialized monitoring and testing that may be beyond the capability of an outpatient unit. Third, the quality of care in the dialysis unit may be poor in the period after hospital discharge, thus contributing to lapses in care, medical errors, and higher emergency department usage. Studies have demonstrated that nephrologist visits occurring in the days and early weeks after hospital discharge may be of particular benefit in reducing rehospitalization.26 Despite this, a recent study of variation in visit frequency found that patients who were recently hospitalized were 2% less likely to be seen four or more times than patients without a recent hospitalization.27 Moreover, the depth of interaction may also be important, as demonstrated by data from the Dialysis Outcomes and Practice Patterns Study, which found that patients experienced improved survival when their providers spent more time conducting face-to-face visits at the outpatient hemodialysis unit.28 Fourth, given the time constraints of dialysis, patients may be using the emergency department as a surrogate for their primary care provider. Finally, some dialysis shifts occur during the evenings or on weekends, when access to medical support staff may be limited, thereby necessitating referral to the emergency department. Indeed, studies have demonstrated the “weekend/after-hours effect” and its negative effect on timeliness of care and mortality.29,30 Nevertheless, further work is necessary to determine the optimal role of the emergency department in the care of patients receiving dialysis.
Our multivariable model demonstrated several patient characteristics that were associated with an increased likelihood of a 30-day acute care event, including increasing age, greater number of hospitalizations and emergency department visits in the 6 months before admission, greater comorbidity, and intensive care unit admission during the index hospitalization. These variables are markers of more complex disease and their association with rehospitalization and emergency department visits is well described among different patient populations.31,32 Practically, our confirmation of predictors of rehospitalization may allow for the derivation and validation of a predictive model or decision rule. Such a model could not only be used for gauging the quality of care, but could also help discharging hospitals and dialysis units “flag” patients at high risk of rehospitalization. This would help facilitate the implementation of important predischarge planning protocols and support arrangements, including patient and family education, provider continuity, and home visits, all of which have been demonstrated to decrease rehospitalization. Moreover, alerting the home dialysis unit to patients at high risk of rehospitalization would allow dialysis providers to focus more resources on these patients, including conducting more frequent physician assessments. Indeed, a recent study demonstrated that additional provider visits in the dialysis unit in the month after hospital discharge reduces 30-day rehospitalization and improves survival time.26,28
Our study should be viewed in the context of some limitations. First, the study sample was limited to Ontario and nonprofit, in-center dialysis units. Although there are some aspects of the healthcare system that are unique to Ontario, our findings are still generalizable to other jurisdictions, because patients on maintenance hemodialysis possess a number of similar health-related issues that transcend geographic boundaries. Second, we focused only on acute care hospital episodes. As such, we did not include visits to urgent care centers or walk-in clinics, which may have underestimated the use of healthcare resources after hospital discharge. Third, although we were able to identify the principal causes for rehospitalization and emergency department visits, we were unable to determine the processes that led to these events; therefore, it is unclear whether these events were the consequence of lapses in care in the dialysis unit, were attributable to the discharge process, or were because of the complexity of the patient and were unrelated to quality of care. Finally, as with any large healthcare database analysis, limitations related to the use of claims-based data have the potential for errors in misclassification of conditions and encounters. However, the databases used in our studies are highly accurate and have been used in a number of studies.33–35
Our findings have important implications. First, by highlighting the magnitude of the problem, we provide a rationale for further study on the determinants of rehospitalizations and the optimal role of the emergency department in the care of chronic hemodialysis recipients. This is paramount, given the renewed interest in performance measures for dialysis patients and the financial implications that will accrue with implementation of such measures in funding formulas. Second, aside from the development of predictive models for risk stratification, our findings also highlight provider and systems issues that may be optimized to mitigate the high rehospitalization rate among patients receiving maintenance hemodialysis. For example, improvement in the coordination between inpatient and outpatient care through physician continuity, a greater emphasis on mitigating risk factors for posthospitalization syndrome during the inpatient stay and after discharge in the dialysis unit, and an increased emphasis on the sharing of information technology between hospitals and dialysis units may all contribute to improving the quality of care of dialysis patients. Finally, the high 30-day mortality in our cohort highlights the fact that many hospitalizations may herald impending death. Although efforts should be made to identify potentially avoidable postdischarge deaths, the hospital stay may be the appropriate venue to discuss end-of-life issues and revisit the patient’s philosophy of care.
Patients receiving maintenance hemodialysis who are discharged from an acute care hospital experience exceptionally high risks of rehospitalization, emergency department use, and death within 30 days. The striking rates of these events demand further efforts to identify the determinants of adverse outcomes during the vulnerable period of transition from inpatient care to the outpatient dialysis unit. Ultimately, by modifying processes of care that contribute to higher rates of rehospitalization, emergency department visits, and death, patients and the medical system will benefit by improving patient care and outcomes (including health-related quality of life) and moderating costs.
Concise Methods
Setting and Study Population
We used population-based linked administrative healthcare databases for all of Ontario to identify patients receiving maintenance in-center hemodialysis, who comprise the vast majority of patients receiving hemodialysis (90%) in Ontario (8522 total in Ontario as of September 2013).36 Ontario is Canada’s most populous province, with >13 million residents. All Ontario citizens are insured for physician services, ambulatory care (including dialysis), and in-hospital care by the Ontario Health Insurance Plan.
We identified all adult patients aged 18–105 years receiving maintenance in-center hemodialysis who were discharged alive after a hospital stay for a medical indication between January 1, 2003, and December 31, 2011. When a patient had a single hospitalization during the period of interest, this became the index hospitalization. When a patient had more than one hospitalization, we randomly selected a single hospitalization and designated it the index hospitalization after applying our exclusionary criteria. We utilized this strategy to abrogate the need to account for dependent observations in the analysis.
We excluded all hospitalizations in which patients withdrew from dialysis or died during the index hospitalization. We also excluded hospitalizations in which patients were on another dialysis modality (e.g., peritoneal dialysis or home hemodialysis) 90 days before the hospitalization or had received a renal transplantation in the 90 days before the hospitalization. Hospitalizations during which patients changed modality (e.g., hemodialysis to peritoneal dialysis), underwent kidney transplantation, or withdrew from hemodialysis in the 30 days after discharge from the hospitalization were also excluded. To ensure that we captured only medical hospitalizations, we excluded hospitalizations in which patients receiving maintenance in-center hemodialysis were admitted for surgical, obstetrical, or psychiatric services. We also excluded all elective index hospitalizations.
This study was approved by the research ethics board at Sunnybrook Hospital in Toronto, Ontario, Canada, which waived the need for patient-level consent.
Databases
We linked Ontario population-based administrative databases held at the Institute for Clinical Evaluative Sciences (ICES) to identify all patients receiving maintenance in-center hemodialysis discharged from Ontario hospitals and to determine postdischarge hospital use, including emergency department visits and rehospitalizations. Prevalent patients were identified using the Canadian Organ Replacement Registry, which captures the incidence, prevalence, and dialysis treatment changes of >99% of patients receiving maintenance dialysis in Canada.34 Information on all hospital admissions was obtained using the Canadian Institute for Health Information Discharge Abstract Database. This database contains the encrypted health card number, date of admission and discharge, and up to16 diagnoses in the International Classification of Diseases, Ninth Revision (before 2002), as well as 25 diagnoses in the International Classification of Diseases, 10th Revision (from 2002 onward). Emergency department visits were identified using the Canadian Institute for Health Information National Ambulatory Care Reporting System, which contains detailed diagnostic and procedural information regarding all emergency department visits in Ontario. The Ontario Health Insurance Plan database contains records of all physician claims for outpatient and inpatient services, including a service date, procedure performed, and a single diagnosis. The Registered Persons Database contains healthcare identifiers for all eligible individuals, age, sex, and date of death. Admissions to long-term care facilities/nursing homes and rehabilitation centers were reported in the Continuing Care Reporting System and National Rehabilitation System databases, respectively.
Descriptive Variables
We assessed demographic characteristics (age and sex), comorbidities (diabetes mellitus, congestive heart failure, coronary artery disease, hypertension, chronic obstructive pulmonary disease, cerebrovascular disease, cancer, chronic liver disease, and peripheral vascular disease) in the 5 years preceding the index admission, the Charlson comorbidity index37 in the 3 years preceding the index admission, and the number of hospitalizations and emergency department visits in the 6 months preceding the index admission. We also determined the length of time that each patient was on hemodialysis before the index admission, as well as the characteristics of the index admission, including the length of stay and the receipt of mechanical ventilation, the latter being a validated marker for intensive care unit admission.38
Outcomes
We followed each eligible patient after discharge from the index hospitalization for 30 days to assess for the frequency of the following: (1) all-cause rehospitalization, (2) emergency department visit (consisting of a visit to the emergency department that resulted in a rehospitalization, or a visit to the emergency department that resulted in a discharge from the emergency department [treat-and-release visit]), and (3) death. Individuals were eligible for multiple outcomes within the 30-day time period (i.e., individuals could be seen in an emergency department and discharged home, then rehospitalized at a later date within the 30-day period).
Reasons for Rehospitalization and Emergency Department Visits
We described the patterns of diagnoses at the index hospitalization, rehospitalization, and treat-and-release emergency department visit by identifying the five diagnoses that accounted for the largest number of index hospitalizations, as well as rehospitalizations and emergency department visits, using the first three digits of the most responsible International Classification of Diseases, 10th Revision, code.
Statistical Analyses
Baseline characteristics of the study participants were summarized using descriptive statistics. Continuous variables were expressed as the mean (SD) or median (IQR) and categorical variables were expressed as a percentage. Covariate balance was measured by the standardized difference, in which an absolute standardized difference >10% represents meaningful imbalance.39
We used cause-specific hazards modeling to estimate the risk of rehospitalization compared with not being rehospitalized within 30 days, censoring for death.40 This model included clinically important variables, including age, sex, number of hospital admissions within the past 6 months (from the index hospitalization admission date), number of emergency department visits within the past 6 months (from the index hospitalization admission date), Charlson score, type of hospital (teaching versus nonteaching), time on hemodialysis, the length of stay of the index admission, the receipt of mechanical ventilation during the index admission (as a surrogate for an intensive care unit admission), index admission to a hospital where the patient undergoes dialysis, and the site of care after discharge (community, nursing home, or rehabilitation facility).
Repeat hospitalization events were examined using Cox regression analysis for recurrent events, accounting for the possibility of multiple rehospitalizations occurring over the study period in the same patient.41
We compared baseline characteristics using SAS software (version 9.3 for UNIX; SAS Institute, Cary, NC). All analyses assumed a two-sided, type I error probability set at 0.05.
Disclosures
None.
Acknowledgments
This study was supported by the Institute for Clinical Evaluative Sciences (ICES), which is funded by an annual grant from the Ontario Ministry of Health and Long-Term Care (MOHLTC). The opinions, results and conclusions reported in this paper are those of the authors and are independent from the funding sources. No endorsement by ICES or the MOHLTC is intended or should be inferred.
This project was conducted with members of the provincial ICES Kidney, Dialysis, and Transplantation Research Program, which receives programmatic grant funding from the Canadian Institutes of Health Research.
Footnotes
Published online ahead of print. Publication date available at www.jasn.org.
References
- 1.Burgess JF, Hockenberry JM: Can all cause readmission policy improve quality or lower expenditures? A historical perspective on current initiatives. Health Econ Policy Law 9: 193–213, 2014 [DOI] [PubMed] [Google Scholar]
- 2.Jencks SF, Williams MV, Coleman EA: Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med 360: 1418–1428, 2009 [DOI] [PubMed] [Google Scholar]
- 3.De Vecchi AF, Dratwa M, Wiedemann ME: Healthcare systems and end-stage renal disease (ESRD) therapies—an international review: costs and reimbursement/funding of ESRD therapies. Nephrol Dial Transplant 14[Suppl 6]: 31–41, 1999 [DOI] [PubMed] [Google Scholar]
- 4.US Renal Data System : 2012 Annual Data Report: Atlas of Chronic Kidney Disease and End-Stage Renal Disease in the United States, Bethesda, MD, National Institutes of Health, 2012 [Google Scholar]
- 5.Manns BJ, Mendelssohn DC, Taub KJ: The economics of end-stage renal disease care in Canada: Incentives and impact on delivery of care. Int J Health Care Finance Econ 7: 149–169, 2007 [DOI] [PubMed] [Google Scholar]
- 6.Seliger SL, Zhan M, Hsu VD, Walker LD, Fink JC: Chronic kidney disease adversely influences patient safety. J Am Soc Nephrol 19: 2414–2419, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Canadian Institute for Health Information : Canadian Organ Replacement Register Annual Report: Treatment of End-Stage Organ Failure in Canada, 2003 to 2012, Ottawa, ON, Canada, Canadian Institute for Health Information, 2014 [Google Scholar]
- 8.Canadian Institute for Health Information : All-Cause Readmission to Acute Care and Return to the Emergency Department, Ottawa, ON, Canada, Canadian Institute for Health Information, 2012 [Google Scholar]
- 9.Saran R, Bragg-Gresham JL, Levin NW, Twardowski ZJ, Wizemann V, Saito A, Kimata N, Gillespie BW, Combe C, Bommer J, Akiba T, Mapes DL, Young EW, Port FK: Longer treatment time and slower ultrafiltration in hemodialysis: Associations with reduced mortality in the DOPPS. Kidney Int 69: 1222–1228, 2006 [DOI] [PubMed] [Google Scholar]
- 10.Foley RN, Hakim RM: Why is the mortality of dialysis patients in the United States much higher than the rest of the world? J Am Soc Nephrol 20: 1432–1435, 2009 [DOI] [PubMed] [Google Scholar]
- 11.Erickson KF, Winkelmayer WC, Chertow GM, Bhattacharya J: Physician visits and 30-day hospital readmissions in patients receiving hemodialysis. J Am Soc Nephrol 25: 2079–2087, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kripalani S, Theobald CN, Anctil B, Vasilevskis EE: Reducing hospital readmission rates: Current strategies and future directions. Annu Rev Med 65: 471–485, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bell CM, Schnipper JL, Auerbach AD, Kaboli PJ, Wetterneck TB, Gonzales DV, Arora VM, Zhang JX, Meltzer DO: Association of communication between hospital-based physicians and primary care providers with patient outcomes. J Gen Intern Med 24: 381–386, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.van Walraven C, Seth R, Austin PC, Laupacis A: Effect of discharge summary availability during post-discharge visits on hospital readmission. J Gen Intern Med 17: 186–192, 2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.van Walraven C, Mamdani M, Fang J, Austin PC: Continuity of care and patient outcomes after hospital discharge. J Gen Intern Med 19: 624–631, 2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Harel Z, Wald R, Perl J, Schwartz D, Bell CM: Evaluation of deficiencies in current discharge summaries for dialysis patients in Canada. J Multidiscip Healthc 5: 77–84, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hernandez AF, Greiner MA, Fonarow GC, Hammill BG, Heidenreich PA, Yancy CW, Peterson ED, Curtis LH: Relationship between early physician follow-up and 30-day readmission among Medicare beneficiaries hospitalized for heart failure. JAMA 303: 1716–1722, 2010 [DOI] [PubMed] [Google Scholar]
- 18.Sharma G, Kuo YF, Freeman JL, Zhang DD, Goodwin JS: Outpatient follow-up visit and 30-day emergency department visit and readmission in patients hospitalized for chronic obstructive pulmonary disease. Arch Intern Med 170: 1664–1670, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chan KE, Lazarus JM, Wingard RL, Hakim RM: Association between repeat hospitalization and early intervention in dialysis patients following hospital discharge. Kidney Int 76: 331–341, 2009 [DOI] [PubMed] [Google Scholar]
- 20.Plantinga LC, Jaar BG: Preventing repeat hospitalizations in dialysis patients: A call for action. Kidney Int 76: 249–251, 2009 [DOI] [PubMed] [Google Scholar]
- 21.Dharmarajan K, Hsieh AF, Lin Z, Bueno H, Ross JS, Horwitz LI, Barreto-Filho JA, Kim N, Bernheim SM, Suter LG, Drye EE, Krumholz HM: Diagnoses and timing of 30-day readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia. JAMA 309: 355–363, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dunlay SM, Weston SA, Killian JM, Bell MR, Jaffe AS, Roger VL: Thirty-day rehospitalizations after acute myocardial infarction: A cohort study. Ann Intern Med 157: 11–18, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Krumholz HM: Post-hospital syndrome—an acquired, transient condition of generalized risk. N Engl J Med 368: 100–102, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jack BW, Chetty VK, Anthony D, Greenwald JL, Sanchez GM, Johnson AE, Forsythe SR, O’Donnell JK, Paasche-Orlow MK, Manasseh C, Martin S, Culpepper L: A reengineered hospital discharge program to decrease rehospitalization: A randomized trial. Ann Intern Med 150: 178–187, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rich MW, Vinson JM, Sperry JC, Shah AS, Spinner LR, Chung MK, Davila-Roman V: Prevention of readmission in elderly patients with congestive heart failure: Results of a prospective, randomized pilot study. J Gen Intern Med 8: 585–590, 1993 [DOI] [PubMed] [Google Scholar]
- 26.Erickson KF, Winkelmayer WC, Chertow GM, Bhattacharya J: Physician visits and 30-day hospital readmissions in patients receiving hemodialysis. J Am Soc Nephrol 25: 2079–2087, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Erickson KF, Tan KB, Winkelmayer WC, Chertow GM, Bhattacharya J: Variation in nephrologist visits to patients on hemodialysis across dialysis facilities and geographic locations. Clin J Am Soc Nephrol 8: 987–994, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kawaguchi T, Karaboyas A, Robinson BM, Li Y, Fukuhara S, Bieber BA, Rayner HC, Andreucci VE, Pisoni RL, Port FK, Morgenstern H, Akizawa T, Saran R: Associations of frequency and duration of patient-doctor contact in hemodialysis facilities with mortality. J Am Soc Nephrol 24: 1493–1502, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bell CM, Redelmeier DA: Waiting for urgent procedures on the weekend among emergently hospitalized patients. Am J Med 117: 175–181, 2004 [DOI] [PubMed] [Google Scholar]
- 30.James MT, Wald R, Bell CM, Tonelli M, Hemmelgarn BR, Waikar SS, Chertow GM: Weekend hospital admission, acute kidney injury, and mortality. J Am Soc Nephrol 21: 845–851, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Krumholz HM, Parent EM, Tu N, Vaccarino V, Wang Y, Radford MJ, Hennen J: Readmission after hospitalization for congestive heart failure among Medicare beneficiaries. Arch Intern Med 157: 99–104, 1997 [PubMed] [Google Scholar]
- 32.van Walraven C, Dhalla IA, Bell C, Etchells E, Stiell IG, Zarnke K, Austin PC, Forster AJ: Derivation and validation of an index to predict early death or unplanned readmission after discharge from hospital to the community. CMAJ 182: 551–557, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Harel Z, Wald R, Bargman JM, Mamdani M, Etchells E, Garg AX, Ray JG, Luo J, Li P, Quinn RR, Forster A, Perl J, Bell CM: Nephrologist follow-up improves all-cause mortality of severe acute kidney injury survivors. Kidney Int 83: 901–908, 2013 [DOI] [PubMed] [Google Scholar]
- 34.Moist LM, Richards HA, Miskulin D, Lok CE, Yeates K, Garg AX, Trpeski L, Chapman A, Amuah J, Hemmelgarn BR: A validation study of the Canadian Organ Replacement Register. Clin J Am Soc Nephrol 6: 813–818, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Juurlink D, Preyra C, Croxford R, Chong A, Austin P, Tu J, Laupacis A: Canadian Institute for Health Information Discharge Abstract Database: A Validation Study, Toronto, ON, Canada, Institute for Clinical Evaluative Sciences, 2006 [Google Scholar]
- 36.Ontario Renal Network: Ontario Renal Reporting System, 2013. Available at: http://www.renalnetwork.on.ca/ontario_renal_plan/accountability_to_patients/ckd_data/prevalence/. Accessed August 20, 2014
- 37.Hemmelgarn BR, Manns BJ, Quan H, Ghali WA: Adapting the Charlson Comorbidity Index for use in patients with ESRD. Am J Kidney Dis 42: 125–132, 2003 [DOI] [PubMed] [Google Scholar]
- 38.Scales DC, Guan J, Martin CM, Redelmeier DA: Administrative data accurately identified intensive care unit admissions in Ontario. J Clin Epidemiol 59: 802–807, 2006 [DOI] [PubMed] [Google Scholar]
- 39.Austin PC: Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat Med 28: 3083–3107, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kalbfleisch J, Prentice R: The Statistical Analysis of Failure Time Data, 2nd Ed., New York, Wiley Interscience, 2002 [Google Scholar]
- 41.Therneau T, Grambsch P: Modeling Survival Data: Extending the Cox Model, New York, Springer Verlag, 2000 [Google Scholar]