Abstract
Platelets are small anucleate cells generated from megakaryocytes in the bone marrow. Although platelet generation, maturation, and clearance are still not fully understood, significant progress has been made in the last 1-2 decades. In blood circulation, platelets can quickly adhere and aggregate at sites of vascular injury, forming the platelet plug (i.e. the first wave of hemostasis). Activated platelets can also provide negatively charged phosphatidylserine-rich membrane surface that enhances cell-based thrombin generation, which facilitates blood coagulation (i.e. the second wave of hemostasis). Platelets therefore play central roles in hemostasis. However, the same process of hemostasis may also cause thrombosis and vessel occlusion, which are the most common mechanisms leading to heart attack and stroke following ruptured atherosclerotic lesions. In this review, we will introduce the classical mechanisms and newly discovered pathways of platelets in hemostasis and thrombosis, including fibrinogen-independent platelet aggregation and thrombosis, and the plasma fibronectin-mediated “protein wave” of hemostasis that precedes the classical first wave of hemostasis. Furthermore, we briefly discuss the roles of platelets in inflammation and atherosclerosis and the potential strategies to control atherothrombosis.
Keywords: platelets, thrombosis and hemostasis, integrin αIIbβ3, fibrinogen, fibronectin
Platelets: evolution, generation, and clearance
Platelets are small anucleate cells in the circulation, with a diameter of approximately 1-2 μm. They were first identified in 1874 by Osler[1]; however, it was the Italian physician, Bizzozero, who in 1881 established the role of platelets in hemostasis and thrombosis in his seminal publications[2,3]. By staining the granules of platelets (Wright stain), it was later demonstrated that these anucleate cells are generated from megakaryocytes in the bone marrow[4]. In the following century, intensive investigation of the cellular and molecular mechanisms of platelets and megakaryocytes[5-7] enabled the development of a number of therapeutic agents for the treatment and prevention of thrombotic disorders[8-11].
In non-mammalian vertebrates, hemostasis is mediated by nucleated cells called thrombocytes[12]. Anucleated platelets evolved only in mammals, and to the best of our knowledge, there is no animal species that have been found thus far to have an intermediate state between thrombocytes and platelets. In addition, platelets are more effective than thrombocytes in forming occlusive thrombi under arterial shear stress[13]. Since platelets have an average life span of only 8-10 days in humans and approximately 5 days in mice, they are constantly being produced from megakaryocytes in the bone marrow. During maturation, megakaryocytes undergo DNA replications without cell division (a process called endomitosis), leading to generation of polyploid megakaryocytes. The abundant genomic DNA in the polyploid megakaryocytes enhances their ability to synthesize proteins and package them into specific platelet granules[7,14].
The exact mechanism of platelet release from megakaryocytes is still under debate. In vitro studies demonstrated that platelet formation begins at one pole of megakaryocytes, then the whole cell is disintegrated, resulting in the generation of numerous proplatelets[15]. However, a recent intravital microscopy study revealed that megakaryocytes extend long protrusions into bone marrow sinusoids and release proplatelets from the tip of the protrusions under shear stress, suggesting that platelet generation in vivo is drastically different from in vitro cell culture conditions[16]. Proplatelets then undergo further division to generate mature platelets in vivo[17]. In addition to bone marrow, new discoveries suggest that megakaryocytes can also mature in the lung and shed platelets into the pulmonary vasculature[18,19]. Interestingly, a recent study suggested that platelets are capable of cell division and progeny generation even without a nucleus[20], although more evidence is required to confirm this finding.
The process and mechanism of platelet clearance is also not well understood, but it is assumed that this occurs in the reticuloendothelial system by macrophages. Aged platelets may express more phosphatidylserine (PS), which may attract macrophages for clearance[21-23]. During red blood cell clearance, older cells may induce more autoantibody binding[24]; however, whether this occurs in aged platelets and whether the Fc portion of the autoantibody interacts with Fc receptors on macrophages leading to phagocytosis still remains to be determined. A more recent study demonstrated that antibody opsonization can activate platelets, leading to platelet desialylation[25,26], a mechanism also involved in clearance of chilled platelets[27-29]. These desialylated platelets can then be destroyed in the liver via hepatocyte Ashwell-Morell receptors[21,25]. Whether this novel platelet clearance pathway[25,30] plays a role in the clearance of aged platelets has yet to be investigated.
Platelets in hemostasis and thrombosis
Hemostasis is a critical physiological process to stop bleeding. Platelet accumulation at the site of injury is considered the first wave of hemostasis and the second wave of hemostasis is mediated by the blood coagulation pathway[31]. Platelets play a central role in a series of sequential events during the platelet accumulation (i.e. platelet adhesion, activation, and aggregation) and are also actively involved in cell-based thrombin generation, which markedly amplifies the blood coagulation cascade. Thus, platelets contribute to both the first and the second waves of hemostasis[6,7,32-35].
Platelet adhesion
Platelet adhesion to the injured vessel wall can occur at both low and high shear conditions but are mediated through distinct mechanisms. Low shear rates (20-200/s) are observed in the venous system whilst higher shear rates are found in arteries (300-800/s) and stenotic vessels (800-10,000/s)[36,37]. Following vascular injury, subendothelial matrix proteins such as collagens are exposed to the blood components. Plasma von Willebrand Factor (VWF), originated from endothelial cells, megakaryocytes, and platelets, can then anchor onto the collagen. The VWF receptor on platelets [glycoprotein (GP)Ibα], via interaction with the immobilized VWF, subsequently initiates platelet tethering to the site of injury[38,39]. This binding is essential for platelet adhesion at high shear (e.g. coronary arteries), although the GPIbα-VWF interaction may also contribute to platelet adhesion at low shear[40,41]. Following platelet tethering, GPVI and integrin α2β1 may interact with collagen and deliver activation signals to platelets[38,42,43]. Stable adhesion is subsequently mediated by binding of several integrins to their ligands on the vessel wall (e.g. integrin αIIbβ3 to fibrinogen/fibrin and fibronectin, α5β1 to fibronectin or collagen, and α2β1 to collagen, etc.)[6,42,44-46]. At low shear (e.g. veins) the interactions between platelet integrins and their ligands (e.g. αIIbβ3 to fibrinogen/fibrin or fibronectin etc.) may directly initiate platelet adhesion[6,47].
In the last decade there have been significant advances in in vivo models of platelet adhesion and thrombus formation using intravital microscopy. VWF knockout (-/-) mice demonstrate decreased platelet adhesion[39,48], a phenotype that, interestingly, is not as severe as the GPIbα-/- mice, suggesting that GPIbα has additional hemostatic function[49]. Mice lacking GPVI present with prolonged bleeding times[50] and similarly, mice deficient in α2 or β1 integrins also have delayed thrombus formation, although these deficiencies are mild compared to GPIbα-/- mice[51].
Platelet activation and granule secretion
The primary interactions between platelet surface receptors (e.g. GPIbα, integrins) and their ligands (e.g. VWF, collagen, fibrinogen/fibrin, fibronectin, etc.), can lead to platelet activation[7,38,52,53]. In addition, following vascular injury, the coagulation system is activated[11,54,55], which generates the most potent platelet activation factor, thrombin. Through cleavage of protease-activated receptors (PARs) and binding to GPIbα, thrombin activates platelets[56-59].
Platelet activation exposes PS on the membrane surface that drives the cell-based thrombin generation[34,35] and facilitates further platelet activation[53,60-61]. Activation signals induced by thrombin, collagen, or ligands of adhesion receptors with the addition of shear stress, can lead to platelet granule release. Platelet adhesion molecules, P-selectin[62], integrins, VWF, fibrinogen, fibronectin[63,64], vitronectin[65], multimerin[60], platelet factor 4, and approximately 300 other proteins are contained within the α-granules[66]. Dense granules release adenosine di-phosphate (ADP), which supports the second wave of platelet aggregation following integrin activation[67]. The release of Ca2+ from the endoplasmic reticulum and the dense granules via the Ca2+ sensor, stromal interaction molecule (STIM)1, and the Ca2+ channel, Orai, is also a significant contributor to platelet activation[68,69]. There are many positive feedback loops during platelet activation/granule release. Notably, ADP, likely via interaction with its receptors on platelets, initiates cell-based thrombin generation and further platelet activation/granule release[61]. These secretion events act as secondary messengers and, in combination with the generation of thromboxane (Tx) A2 and reactive oxygen species, amplify the activation process and integrin αIIbβ3 inside-out signaling, which in turn recruits more platelets for aggregation[70-74].
Platelet aggregation: fibrinogen-dependent and -independent aggregation
Following platelet activation, integrin αIIbβ3 binds fibrinogen and other ligands (i.e. fibrinogen-dependent and -independent pathways[31,39,61,75,76]), which leads to platelet aggregation. It is notable that following the engagement of ligands, integrin αIIbβ3 can deliver outside-in signals, which further enhance platelet activation, cytoskeleton rearrangement, and granule secretion. These signal events facilitate hemostatic plug and thrombus formation.
For more than half a century, fibrinogen was considered required for platelet aggregation[61]. Through interaction with αIIbβ3 via its γ chain C-terminus, fibrinogen bridges adjacent activated platelets[22,77]. However, data from Ni et al. demonstrated that thrombus formation still occurred in fibrinogen-/- mice and in VWF and fibrinogen double knock-out (DKO) mice[39], indicating that fibrinogen was not indispensable for this process. Further studies demonstrated that DKO platelet aggregation occurred in vitro in platelet-rich plasma and gel-filtered platelets without anti-coagulant treatment (i.e. in a more physiological condition compared to anti-coagulated blood used in clinic and research). In contrast, integrin β3-/- mice exhibit no significant platelet aggregation, which indicates an essential role for αIIbβ3 in platelet aggregation and suggests the existence of other unidentified αIIbβ3 ligand(s)[61].
In VWF-fibrinogen DKO mice, fibrinogen-/- mice, and fibrinogen C-terminal γ chain mutant mice[77], as well as in afibrinogenemic patients[22,78], platelet fibronectin (an αIIbβ3 ligand) content was increased 3-5 fold due to enhanced internalization of plasma fibronectin (pFn) by integrin αIIbβ3. Conditional pFn-/- mice have impaired thrombus growth at arterial shear[79], implying that fibronectin may be a compensatory αIIbβ3 ligand that supports platelet aggregation. Unexpectedly, however, further depletion of pFn in VWF-fibrinogen DKO mice enhanced, instead of abolishing, platelet aggregation[31,75]. These results suggest that pFn can switch between supporting and inhibiting platelet aggregation, depending on the presence of fibrinogen/fibrin[31,79].
Another αIIbβ3 ligand, vitronectin, plays a dual role; aggregation is enhanced by granule-released vitronectin but is inhibited by plasma vitronectin[65]. These studies suggested that likely neither fibronectin nor vitronectin are the αIIbβ3 ligand that mediates fibrinogen-independent platelet aggregation. Cadherin 6 contains a canonical "RGD" (arginine-glycine-aspartic acid) integrin-binding motif and increases its expression on platelets after platelet activation[76]. Whilst cadherin 6 contributes to platelet aggregation, clearly other plasma and platelet proteins exist that can also mediate and facilitate fibrinogen-independent platelet aggregation[61]. However, what they are and how they contribute to thrombosis and hemostasis in different pathophysiological conditions requires further study.
Platelet-mediated cell-based thrombin generation and blood coagulation
In addition to their central roles in the platelet adhesion, activation, and aggregation (the first wave of hemostasis), platelets also contribute to coagulation pathway (the second wave of hemostasis). The blood coagulation cascade can be activated by either the extrinsic (tissue factor) or the intrinsic (contact activation) pathways in thrombosis[54,80]. Thrombin, a vital product of the coagulation cascade, converts fibrinogen to fibrin, the end product of the coagulation cascade.
Besides these two classical coagulation pathways, the exposure of PS on platelets, following platelet activation, markedly potentiates thrombin generation by inducing a negatively charged surface that harbors the coagulation factors[34]. Interestingly, in a study of platelet aggregation in fibrinogen and VWF DKO mice, Yang et al. found that ADP can induce thrombin generation that is required for platelet aggregation in the DKO mice[61]. Recently, GPVI was also identified as a novel fibrin receptor involved in potentiating thrombin generation[81]. Thrombin initiates robust downstream signaling, through PAR1, PAR4[82] and GPIbα, leading to platelet activation and further PS exposure, a positive feedback loop for thrombin generation and blood coagulation[57,83,84]. Thus, there are many interactions between the first wave (platelet accumulation) and the second wave (blood coagulation) of hemostasis, which synergistically contribute to the arrest of bleeding.
Platelets and the "protein wave" of hemostasis: new discoveries
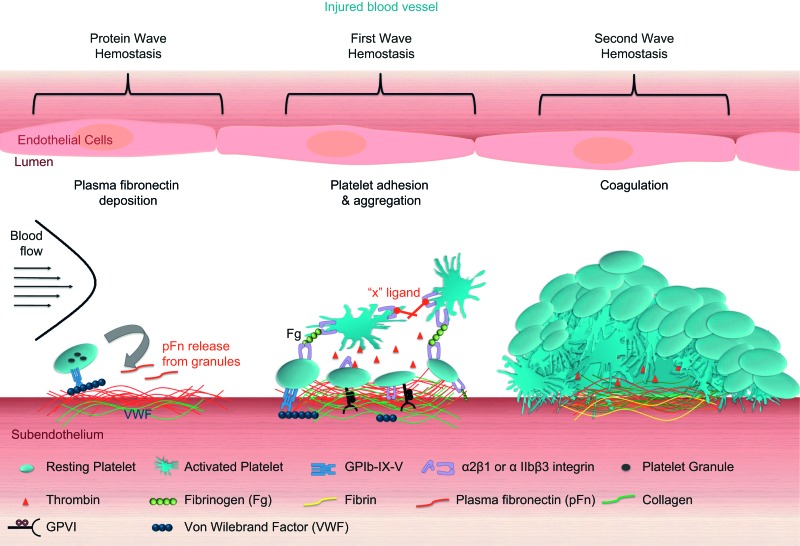
One of the most recent studies revealed a novel concept of a ′protein wave′ of hemostasis, where pFn deposition on the injured vessel wall occurs prior to platelet accumulation (the first wave of hemostasis) and contributes to hemostasis[31,85]. In mice lacking fibrinogen, further depletion of pFn markedly increased the mortality rate due to uncontrolled bleeding. Increased bleeding time was also observed in pFn conditional -/- mice, treated with heparin and other anti-coagulants, suggesting that pFn is important for hemostasis in both genetic and drug-induced deficiencies of blood coagulation. We observed that the pFn deposition onto the injured vessel wall can occur independently of fibrinogen, VWF, β3 integrin, and platelets. It seems that the pFn-collagen interaction may play an important role in this process[31,85]. pFn, likely via the covalent binding to fibrin, increases the diameter of fibrin fibers and enhances the mechanical strength of the clot and this mechanism likely contributes to the pFn deposition onto the injured vessel walls of normal individuals where fibrin exists. Interestingly, in the absence of fibrin (a product of fibrinogen), pFn switches its function from promoting to inhibiting platelet aggregation. As fibrin is mainly formed at the bottom of the hemostatic plug close to the vessel wall, pFn may support hemostasis at the base of the thrombi (likely through the formation of a pFn-fibrin complex) and switch to inhibiting excessive thrombus growth at the apical surface of thrombi. Through this mechanism, pFn serves to control bleeding, while preventing excessive thrombus growth and vessel occlusion. Further investigation of the interaction between platelets and circulating/deposited pFn may reveal novel therapeutic targets for thrombotic disorders, as well as usage of pFn for transfusion to control bleeding disorders, particularly those patients in association with anti-coagulant therapy. It would also be interesting to investigate whether the markedly increased platelet fibronectin content in fibrinogen-/- mice and afibrinogenemic patients can be released onto the injured vessel wall and contribute to the protein wave of hemostasis (Fig. 1).
Fig. 1. At the site of vascular injury plasma fibronectin deposition occurs even before platelets adhere.
Platelets may release their internalized plasma fibronectin from intracellular granules. Platelet receptors then bind physiological ligands, such as VWF and collagen, activating integrin αIIbβ3 and resulting in fibrinogen binding and subsequent platelet aggregation. Thrombin is generated on the negatively charged platelet surface and further activates platelets and contributes to the coagulation cascade. In a growing hemostatic plug/thrombus, the fibrin and fibronectin matrix is usually formed at the interface between the injured vessel wall and the platelet plug.
Conclusion and future directions
The primary physiological function of platelets is to stop bleeding upon vascular injury. Platelets, via their contributions to the "protein wave" and to the classical first and second waves of hemostasis, play key roles in the arrest of bleeding[31]. Thrombocytopenias caused by either genetic deficiencies[86] or autoimmune[87-89] and alloimmune responses lead to bleeding disorders[21,32,33,90-96]. However, the same platelet accumulation and coagulation may lead to thrombosis. Thrombotic events occur at the site of a ruptured atherosclerotic plaque and can result in heart attack or stroke, the leading causes of mortality and morbidity worldwide.
In addition to thrombosis, the late stage of atherothrombosis, recent studies demonstrated that platelets are actively involved in the initiation of atherosclerosis[97,98]. Platelets are sensitive to environmental changes, such as food products[99-101], lipids[102], and advanced glycation end products in diabetes[103,104], which may affect atherosclerosis. Furthermore, as we demonstrated, platelets can respond to fibrinogen level changes. Through interaction with integrin αIIbβ3, platelets can use their residual mRNA to de novo synthesize P-selectin and other proteins[62,105], which may also affect inflammation and directly or indirectly affect atherosclerosis and the stability of atherosclerotic plugs[106-108].
In this review, we described the concept of fibrinogen/VWF-independent platelet aggregation, which was first noted in the early 2000s[61], and provided insight into multiple and diverse interactions between platelets and their environment. Despite considerable efforts[62,76], the 'x' ligand(s) of integrin αIIbβ3 has yet to be uncovered. These concepts are an example of how diverse platelets can be and demonstrate the need for further investigation into platelet interactions. Furthermore, whilst platelets play a pivotal role in hemostasis and thrombosis, they are also versatile cells and are involved in multiple functions, including inflammation, immune responses, lymphatic vessel development, angiogenesis, tumor metastasis, as well as atherosclerosis[106-109]. Further elucidations of platelet versatilities will provide insights into development of new methods to control not only thrombosis and hemostasis but also inflammation, cancer, and immunological disorders.
Acknowledgments
This work was supported in part by Canadian Institutes of Health Research(MOP 119540), National Natural Science Foundation of China-Canadian Institutes of Health Research (China-Canada Joint Health Research Initiative Program), Heart and Stroke Foundation of Canada (Ontario). This work was also supported by equipment Funds from St. Michael's Hospital, Canadian Blood Services, and Canada Foundation for Innovation. Naadiya Carrim is a recipient of a Postdoctoral Fellowship from Canadian Blood Services and Health Canada. Yiming Wang is a recipient of a Ph.D. Graduate Student Fellowship from Canadian Blood Services and Meredith & Malcolm Silver Scholarship in Cardiovascular Studies, University of Toronto. Yan Hou is a recipient of a State Scholarship Fund from the China Scholarship Council.
References
- [1].Osler W. An account of certain organisms occurring in the liquor sanguinis[J] Proc R Soc Lond. 1874:391–398. [Google Scholar]
- [2].Bizzozero G. Su di un nuovo elemento morfologico del sangue dei mammiferi e della sua importanza nella trombosi e nella coagulazione[J] L’Osservatore. 1881:785–787. [Google Scholar]
- [3].Bizzozero G. Uber einen neuen Formbestandteil des Blutes und dessen Rolle bei der Thrombose und Blutgrinnung[J] Virchows Archiv. 1882:261–332. [Google Scholar]
- [4].Wright J. The origin and nature of blood platelets[J] Boston Med Surg J. 1906:643–645. [Google Scholar]
- [5].Ruggeri ZM. Platelets in atherothrombosis[J] Nat Med. 2002;8:1227–1234. doi: 10.1038/nm1102-1227. [DOI] [PubMed] [Google Scholar]
- [6].Ni H, Freedman J. Platelets in hemostasis and thrombosis: role of integrins and their ligands[J] Transfus Apher Sci. 2003;28:257–264. doi: 10.1016/S1473-0502(03)00044-2. [DOI] [PubMed] [Google Scholar]
- [7].Wang Y, Andrews M, Yang Y, et al. Platelets in thrombosis and hemostasis: old topic with new mechanisms[J] Cardiovasc Hematol Disord Drug Targets. 2012;12:126–132. doi: 10.2174/1871529x11202020126. [DOI] [PubMed] [Google Scholar]
- [8].Coller BS. Historical perspective and future directions in platelet research[J] J Thromb Haemost. 2011;9 Suppl 1:374–395. doi: 10.1111/j.1538-7836.2011.04356.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Jackson SP, Schoenwaelder SM. Antiplatelet therapy: in search of the 'magic bullet'[J] Nat Rev Drug Discov. 2003;2:775–789. doi: 10.1038/nrd1198. [DOI] [PubMed] [Google Scholar]
- [10].Gachet C. Antiplatelet drugs: which targets for which treatments?[J] J Thromb Haemost. 2015;13:S313–322. doi: 10.1111/jth.12947. [DOI] [PubMed] [Google Scholar]
- [11].Mackman N. Triggers, targets and treatments for thrombosis[J] Nature. 2008;451:914–918. doi: 10.1038/nature06797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Michelson AD. Platelets. 3rd edition 2013. [Google Scholar]
- [13].Schmaier AA, Stalker TJ, Runge JJ, et al. Occlusive thrombi arise in mammals but not birds in response to arterial injury: evolutionary insight into human cardiovascular disease[J] Blood. 2011;118:3661–3669. doi: 10.1182/blood-2011-02-338244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Machlus KR, Italiano JE., Jr The incredible journey: From megakaryocyte development to platelet formation[J] J Cell Biol. 2013;201:785–796. doi: 10.1083/jcb.201304054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Italiano JE, Jr, Lecine P, Shivdasani RA, et al. Blood platelets are assembled principally at the ends of proplatelet processes produced by differentiated megakaryocytes[J] J Cell Biol. 1999;147:1299–1312. doi: 10.1083/jcb.147.6.1299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Junt T, Schulze H, Chen Z, et al. Dynamic visualization of thrombopoiesis within bone marrow[J] Science. 2007;317:1767–1770. doi: 10.1126/science.1146304. [DOI] [PubMed] [Google Scholar]
- [17].Thon JN, Montalvo A, Patel-Hett S, et al. Cytoskeletal mechanics of proplatelet maturation and platelet release[J] J Cell Biol. 2010;191:861–874. doi: 10.1083/jcb.201006102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Fuentes R, Wang Y, Hirsch J, et al. Infusion of mature megakaryocytes into mice yields functional platelets[J] J Clin Invest. 2010;120:3917–3922. doi: 10.1172/JCI43326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Wang Y, Hayes V, Jarocha D, et al. Comparative analysis of human ex vivo-generated platelets vs megakaryocyte-generated platelets in mice: a cautionary tale[J] Blood. 2015;125:3627–3636. doi: 10.1182/blood-2014-08-593053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Schwertz H, Koster S, Kahr WH, et al. Anucleate platelets generate progeny[J] Blood. 2010;115:3801–3809. doi: 10.1182/blood-2009-08-239558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Li J, van der Wal DE, Zhu L, et al. Fc-independent phagocytosis: implications for IVIG and other therapies in immune-mediated thrombocytopenia[J] Cardiovasc Hematol Disord Drug Targets. 2013;13:50–58. doi: 10.2174/1871529x11313010006. [DOI] [PubMed] [Google Scholar]
- [22].Xu X, Wu J, Zhai Z, et al. A novel fibrinogen Bbeta chain frameshift mutation in a patient with severe congenital hypofibrinogenaemia[J] Thromb Haemost. 2006;95:931–935. doi: 10.1160/TH06-01-0020. [DOI] [PubMed] [Google Scholar]
- [23].Rand ML, Wang H, Bang KW, et al. Procoagulant surface exposure and apoptosis in rabbit platelets: association with shortened survival and steady-state senescence[J] J Thromb Haemost. 2004;2:651–659. doi: 10.1111/j.1538-7836.2004.00670.x. [DOI] [PubMed] [Google Scholar]
- [24].Webster ML, Zhu G, Li Y, et al. Fc-independent phagocytosis: implications for intravenous IgG therapy in immune thrombocytopenia[J] Cardiovasc Hematol Disord Drug Targets. 2008;8:278–282. doi: 10.2174/187152908786786223. [DOI] [PubMed] [Google Scholar]
- [25].Li J, van der Wal DE, Zhu G, et al. Desialylation is a mechanism of Fc-independent platelet clearance and a therapeutic target in immune thrombocytopenia[J] Nat Commun. 2015;6:7737–7753. doi: 10.1038/ncomms8737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].van Der Wal D, Zhu G, Li J, et al. Desialylation: A Novel Platelet Clearance Mechanism and a Potential New Therapeutic Target in Anti-GPIb Antibody Mediated Thrombocytopenia [J]; 54th ASH Annual Meeting; 2012. (Session: 311. Disorders of Platelet Number or Function: Biology of antibody mediated platelet destruction: HIT, NAIT and mechanisms of ivig) [Google Scholar]
- [27].Sorensen AL, Rumjantseva V, Nayeb-Hashemi S, et al. Role of sialic acid for platelet life span: exposure of beta-galactose results in the rapid clearance of platelets from the circulation by asialoglycoprotein receptor-expressing liver macrophages and hepatocytes[J] Blood. 2009;114:1645–1654. doi: 10.1182/blood-2009-01-199414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Rumjantseva V, Hoffmeister KM. Novel and unexpected clearance mechanisms for cold platelets[J] Transfus Apher Sci. 2010;42:63–70. doi: 10.1016/j.transci.2009.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Jansen AJ, Josefsson EC, Rumjantseva V, et al. Desialylation accelerates platelet clearance after refrigeration and initiates GPIbalpha metalloproteinase-mediated cleavage in mice[J] Blood. 2012;119:1263–1273. doi: 10.1182/blood-2011-05-355628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Jansen AJ, Peng J, Zhao HG, et al. Sialidase inhibition to increase platelet counts: A new treatment option for thrombocytopenia[J] Am J Hematol. 2015;90:E94–95. doi: 10.1002/ajh.23953. [DOI] [PubMed] [Google Scholar]
- [31].Wang Y, Reheman A, Spring CM, et al. Plasma fibronectin supports hemostasis and regulates thrombosis[J] J Clin Invest. 2014;124:4281–4293. doi: 10.1172/JCI74630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Yougbare I, Lang S, Yang H, et al. Maternal anti-platelet beta3 integrins impair angiogenesis and cause intracranial hemorrhage[J] J Clin Invest. 2015;125:1545–1556. doi: 10.1172/JCI77820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Vadasz B, Chen P, Yougbaré I, et al. Platelets and platelet alloantigens: Lessons from human patients and animal models of fetal and neonatal alloimmune thrombocytopenia[J] Gene and Diseases. 2015;2:173–185. doi: 10.1016/j.gendis.2015.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Roberts HR, Hoffman M, Monroe DM. A cell-based model of thrombin generation[J] Semin Thromb Hemost. 2006;32 Suppl 1:32–38. doi: 10.1055/s-2006-939552. [DOI] [PubMed] [Google Scholar]
- [35].Monroe DM, Hoffman M, Roberts HR. Platelets and thrombin generation[J] Arterioscler Thromb Vasc Biol. 2002;22:1381–1389. doi: 10.1161/01.atv.0000031340.68494.34. [DOI] [PubMed] [Google Scholar]
- [36].Dopheide SM, Maxwell MJ, Jackson SP. Shear-dependent tether formation during platelet translocation on von Willebrand factor[J] Blood. 2002;99:159–167. doi: 10.1182/blood.v99.1.159. [DOI] [PubMed] [Google Scholar]
- [37].Goto S, Salomon DR, Ikeda Y, et al. Characterization of the unique mechanism mediating the shear-dependent binding of soluble von Willebrand factor to platelets[J] J Biol Chem. 1995;270:23352–23361. doi: 10.1074/jbc.270.40.23352. [DOI] [PubMed] [Google Scholar]
- [38].Ruggeri ZM. Mechanisms initiating platelet thrombus formation[J] Thromb Haemost. 1997;78:611–616. [PubMed] [Google Scholar]
- [39].Ni H, Denis CV, Subbarao S, et al. Persistence of platelet thrombus formation in arterioles of mice lacking both von Willebrand factor and fibrinogen[J] J Clin Invest. 2000;106:385–392. doi: 10.1172/JCI9896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Andre P, Denis CV, Ware J, et al. Platelets adhere to and translocate on von Willebrand factor presented by endothelium in stimulated veins[J] Blood. 2000;96:3322–3328. [PubMed] [Google Scholar]
- [41].Lei X, Reheman A, Hou Y, et al. Anfibatide, a novel GPIb complex antagonist, inhibits platelet adhesion and thrombus formation in vitro and in vivo in murine models of thrombosis[J] Thromb Haemost. 2014;111:279–289. doi: 10.1160/TH13-06-0490. [DOI] [PubMed] [Google Scholar]
- [42].Savage B, Almus-Jacobs F, Ruggeri ZM. Specific synergy of multiple substrate-receptor interactions in platelet thrombus formation under flow[J] Cell. 1998;94:657–666. doi: 10.1016/s0092-8674(00)81607-4. [DOI] [PubMed] [Google Scholar]
- [43].Nieswandt B, Brakebusch C, Bergmeier W, et al. Glycoprotein VI but not alpha2beta1 integrin is essential for platelet interaction with collagen[J] EMBO J. 2001;20:2120–2130. doi: 10.1093/emboj/20.9.2120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Wilkins JA, Li A, Ni H, et al. Control of beta1 integrin function. Localization of stimulatory epitopes[J] J Biol Chem. 1996;271:3046–3051. [PubMed] [Google Scholar]
- [45].Ni H, Li A, Simonsen N, et al. Integrin activation by dithiothreitol or Mn2+ induces a ligand-occupied conformation and exposure of a novel NH2-terminal regulatory site on the beta1 integrin chain[J] J Biol Chem. 1998;273:7981–7987. doi: 10.1074/jbc.273.14.7981. [DOI] [PubMed] [Google Scholar]
- [46].Ni H, Wilkins JA. Localisation of a novel adhesion blocking epitope on the human beta 1 integrin chain[J] Cell Adhes Commun. 1998;5:257–271. doi: 10.3109/15419069809040296. [DOI] [PubMed] [Google Scholar]
- [47].Bledzka K, Smyth SS, Plow EF. Integrin alphaIIbbeta3: from discovery to efficacious therapeutic target[J] Circ Res. 2013;112:1189–1200. doi: 10.1161/CIRCRESAHA.112.300570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48].Denis C, Methia N, Frenette PS, et al. A mouse model of severe von Willebrand disease: defects in hemostasis and thrombosis[J] Proc Natl Acad Sci U S A. 1998;95:9524–9529. doi: 10.1073/pnas.95.16.9524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49].Bergmeier W, Piffath CL, Goerge T, et al. The role of platelet adhesion receptor GPIbalpha far exceeds that of its main ligand, von Willebrand factor, in arterial thrombosis[J] Proc Natl Acad Sci U S A. 2006;103:16900–16905. doi: 10.1073/pnas.0608207103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].Nieswandt B, Schulte V, Bergmeier W, et al. Long-term antithrombotic protection by in vivo depletion of platelet glycoprotein VI in mice[J] J Exp Med. 2001;193:459–469. doi: 10.1084/jem.193.4.459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [51].Nuyttens BP, Thijs T, Deckmyn H, et al. Platelet adhesion to collagen[J] Thromb Res. 2011;127:S26–29. doi: 10.1016/S0049-3848(10)70151-1. [DOI] [PubMed] [Google Scholar]
- [52].Bergmeier W, Hynes RO. Extracellular matrix proteins in hemostasis and thrombosis[J] Cold Spring Harb Perspect Biol. 2012;4 doi: 10.1101/cshperspect.a005132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [53].Berndt MC, Metharom P, Andrews RK. Primary haemostasis: newer insights[J] Haemophilia. 2014;20:15–22. doi: 10.1111/hae.12427. [DOI] [PubMed] [Google Scholar]
- [54].Gui T, Reheman A, Ni H, et al. Abnormal hemostasis in a knock-in mouse carrying a variant of factor IX with impaired binding to collagen type IV[J] J Thromb Haemost. 2009;7:1843–1851. doi: 10.1111/j.1538-7836.2009.03545.x. [DOI] [PubMed] [Google Scholar]
- [55].Gui T, Reheman A, Funkhouser WK, et al. In vivo response to vascular injury in the absence of factor IX: examination in factor IX knockout mice[J] Thromb Res. 2007;121:225–234. doi: 10.1016/j.thromres.2007.03.026. [DOI] [PubMed] [Google Scholar]
- [56].Sambrano GR, Weiss EJ, Zheng YW, et al. Role of thrombin signalling in platelets in haemostasis and thrombosis[J] Nature. 2001;413:74–78. doi: 10.1038/35092573. [DOI] [PubMed] [Google Scholar]
- [57].Celikel R, McClintock RA, Roberts JR, et al. Modulation of alpha-thrombin function by distinct interactions with platelet glycoprotein Ibalpha[J] Science. 2003;301:218–221. doi: 10.1126/science.1084183. [DOI] [PubMed] [Google Scholar]
- [58].Ni H, Ramakrishnan V, Ruggeri ZM, et al. Increased thrombogenesis and embolus formation in mice lacking glycoprotein V[J] Blood. 2001;98:368–373. doi: 10.1182/blood.v98.2.368. [DOI] [PubMed] [Google Scholar]
- [59].Li C, Piran S, Chen P, et al. The maternal immune response to fetal platelet GPIbalpha causes frequent miscarriage in mice that can be prevented by intravenous IgG and anti-FcRn therapies[J] J Clin Invest. 2011;121:4537–4547. doi: 10.1172/JCI57850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [60].Reheman A, Tasneem S, Ni H, et al. Mice with deleted multimerin 1 and alpha-synuclein genes have impaired platelet adhesion and impaired thrombus formation that is corrected by multimerin 1[J] Thromb Res. 2010;125:e177–183. doi: 10.1016/j.thromres.2010.01.009. [DOI] [PubMed] [Google Scholar]
- [61].Yang H, Reheman A, Chen P, et al. Fibrinogen and von Willebrand factor-independent platelet aggregation in vitro and in vivo[J] J Thromb Haemost. 2006;4:2230–2237. doi: 10.1111/j.1538-7836.2006.02116.x. [DOI] [PubMed] [Google Scholar]
- [62].Yang H, Lang S, Zhai Z, et al. Fibrinogen is required for maintenance of platelet intracellular and cell-surface P-selectin expression[J] Blood. 2009;114:425–436. doi: 10.1182/blood-2008-03-145821. [DOI] [PubMed] [Google Scholar]
- [63].Ni H. Unveiling the new face of fibronectin in thrombosis and hemostasis[J] J Thromb Haemost. 2006;4:940–942. doi: 10.1111/j.1538-7836.2006.01899.x. [DOI] [PubMed] [Google Scholar]
- [64].Wang Y, Ni H. Fibronectin: extra domain brings extra risk?[J] Blood. 2015;125:3043–3054. doi: 10.1182/blood-2015-03-630855. [DOI] [PubMed] [Google Scholar]
- [65].Reheman A, Gross P, Yang H, et al. Vitronectin stabilizes thrombi and vessel occlusion but plays a dual role in platelet aggregation[J] J Thromb Haemost. 2005;3:875–883. doi: 10.1111/j.1538-7836.2005.01217.x. [DOI] [PubMed] [Google Scholar]
- [66].Rao AK. Inherited platelet function disorders: overview and disorders of granules, secretion, and signal transduction[J] Hematol Oncol Clin North Am. 2013;27:585–611. doi: 10.1016/j.hoc.2013.02.005. [DOI] [PubMed] [Google Scholar]
- [67].Johnston-Cox HA, Yang D, Ravid K. Physiological implications of adenosine receptor-mediated platelet aggregation[J] J Cell Physiol. 2011;226:46–51. doi: 10.1002/jcp.22379. [DOI] [PubMed] [Google Scholar]
- [68].Bergmeier W, Stefanini L. Novel molecules in calcium signaling in platelets[J] J Thromb Haemost. 2009;7(Suppl 1):187–190. doi: 10.1111/j.1538-7836.2009.03379.x. [DOI] [PubMed] [Google Scholar]
- [69].Varga-Szabo D, Braun A, Nieswandt B. STIM and Orai in platelet function[J] Cell Calcium. 2011;50:270–278. doi: 10.1016/j.ceca.2011.04.002. [DOI] [PubMed] [Google Scholar]
- [70].Jin J, Quinton TM, Zhang J, et al. Adenosine diphosphate (ADP)-induced thromboxane A(2) generation in human platelets requires coordinated signaling through integrin alpha(IIb)beta(3) and ADP receptors[J] Blood. 2002;99:193–198. doi: 10.1182/blood.v99.1.193. [DOI] [PubMed] [Google Scholar]
- [71].Arthur JF, Gardiner EE, Kenny D, et al. Platelet receptor redox regulation[J] Platelets. 2008;19:1–8. doi: 10.1080/09537100701817224. [DOI] [PubMed] [Google Scholar]
- [72].Carrim N, Walsh TG, Consonni A, et al. Role of focal adhesion tyrosine kinases in GPVI-dependent platelet activation and reactive oxygen species formation[J] PLoS One. 2014;9:e113679. doi: 10.1371/journal.pone.0113679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [73].Walsh TG, Berndt MC, Carrim N, et al. The role of Nox1 and Nox2 in GPVI-dependent platelet activation and thrombus formation[J] Redox Biol. 2014;13:178–186. doi: 10.1016/j.redox.2013.12.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [74].Chen W, Thielmann I, Gupta S, et al. Orai1-induced store-operated Ca(2+) entry enhances phospholipase activity and modulates canonical transient receptor potential channel 6 function in murine platelets[J] J Thromb Haemost. 2014;12:528–539. doi: 10.1111/jth.12525. [DOI] [PubMed] [Google Scholar]
- [75].Reheman A, Yang H, Zhu G, et al. Plasma fibronectin depletion enhances platelet aggregation and thrombus formation in mice lacking fibrinogen and von Willebrand factor[J] Blood. 2009;113:1809–1817. doi: 10.1182/blood-2008-04-148361. [DOI] [PubMed] [Google Scholar]
- [76].Dunne E, Spring CM, Reheman A, et al. Cadherin 6 has a functional role in platelet aggregation and thrombus formation[J] Arterioscler Thromb Vasc Biol. 2012;32:1724–1731. doi: 10.1161/ATVBAHA.112.250464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [77].Ni H, Papalia JM, Degen JL, et al. Control of thrombus embolization and fibronectin internalization by integrin alpha IIb beta 3 engagement of the fibrinogen gamma chain[J] Blood. 2003;102:3609–3614. doi: 10.1182/blood-2003-03-0850. [DOI] [PubMed] [Google Scholar]
- [78].Zhai Z, Wu J, Xu X, et al. Fibrinogen controls human platelet fibronectin internalization and cell-surface retention[J] J Thromb Haemost. 2007;5:1740–1746. doi: 10.1111/j.1538-7836.2007.02625.x. [DOI] [PubMed] [Google Scholar]
- [79].Ni H, Yuen PS, Papalia JM, et al. Plasma fibronectin promotes thrombus growth and stability in injured arterioles[J] Proc Natl Acad Sci U S A. 2003;100:2415–2419. doi: 10.1073/pnas.2628067100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [80].Smith SA, Travers RJ, Morrissey JH. How it all starts: Initiation of the clotting cascade[J] Crit Rev Biochem Mol Biol. 2015;50:1–11. doi: 10.3109/10409238.2015.1050550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [81].Mammadova-Bach E, Ollivier V, Loyau S, et al. Platelet glycoprotein VI binds to polymerized fibrin and promotes thrombin generation[J] Blood. 2015;126:683–691. doi: 10.1182/blood-2015-02-629717. [DOI] [PubMed] [Google Scholar]
- [82].Alberelli MA, De Candia E. Functional role of protease activated receptors in vascular biology[J] Vascul Pharmacol. 2014;62:72–81. doi: 10.1016/j.vph.2014.06.001. [DOI] [PubMed] [Google Scholar]
- [83].Dumas JJ, Kumar R, Seehra J, et al. Crystal structure of the GpIbalpha-thrombin complex essential for platelet aggregation[J] Science. 2003;301:222–226. doi: 10.1126/science.1083917. [DOI] [PubMed] [Google Scholar]
- [84].Lechtenberg BC, Freund SM, Huntington JA. GpIbalpha interacts exclusively with exosite II of thrombin[J] J Mol Biol. 2014;426:881–893. doi: 10.1016/j.jmb.2013.11.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [85].Wang Y, Carrim N, Ni H. Fibronectin orchestrates thrombosis and hemostasis[J] Oncotarget Journal. 2015;6:19350–19351. doi: 10.18632/oncotarget.5097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [86].Nurden AT, Freson K, Seligsohn U. Inherited platelet disorders[J] Haemophilia. 2012;18:154–160. doi: 10.1111/j.1365-2516.2012.02856.x. [DOI] [PubMed] [Google Scholar]
- [87].Peng J, Ma SH, Liu J, et al. Association of autoantibody specificity and response to intravenous immunoglobulin G therapy in immune thrombocytopenia: a multicenter cohort study[J] J Thromb Haemost. 2014;12:497–504. doi: 10.1111/jth.12524. [DOI] [PubMed] [Google Scholar]
- [88].Webster ML, Sayeh E, Crow M, et al. Relative efficacy of intravenous immunoglobulin G in ameliorating thrombocytopenia induced by antiplatelet GPIIbIIIa versus GPIbalpha antibodies[J] Blood. 2006;108:943–946. doi: 10.1182/blood-2005-06-009761. [DOI] [PubMed] [Google Scholar]
- [89].Zeng Q, Zhu L, Tao L, et al. Relative efficacy of steroid therapy in immune thrombocytopenia mediated by anti-platelet GPIIbIIIa versus GPIbalpha antibodies[J] Am J Hematol. 2012;87:206–208. doi: 10.1002/ajh.22211. [DOI] [PubMed] [Google Scholar]
- [90].Semple JW, Italiano JE, Freedman J. Platelets and the immune continuum[J] Nat Rev Immunol. 2011;11:264–274. doi: 10.1038/nri2956. [DOI] [PubMed] [Google Scholar]
- [91].Chen P, Li C, Lang S, et al. Animal model of fetal and neonatal immune thrombocytopenia: role of neonatal Fc receptor in the pathogenesis and therapy[J] Blood. 2010;116:3660–3668. doi: 10.1182/blood-2010-05-284919. [DOI] [PubMed] [Google Scholar]
- [92].Ni H, Chen P, Spring CM, et al. A novel murine model of fetal and neonatal alloimmune thrombocytopenia: response to intravenous IgG therapy[J] Blood. 2006;107:2976–2983. doi: 10.1182/blood-2005-06-2562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [93].Sachs UJ. Fetal/neonatal alloimmune thrombocytopenia[J] Thromb Res. 2013;131(Suppl 1):S42–46. doi: 10.1016/S0049-3848(13)70020-3. [DOI] [PubMed] [Google Scholar]
- [94].Liang Y, Qiu H, Glinka Y, et al. Immunity against a therapeutic xenoprotein/Fc construct delivered by gene transfer is reduced through binding to the inhibitory receptor FcgammaRIIb[J] J Gene Med. 2011;13:470–477. doi: 10.1002/jgm.1598. [DOI] [PubMed] [Google Scholar]
- [95].Tiller H, Killie MK, Chen P, et al. Toward a prophylaxis against fetal and neonatal alloimmune thrombocytopenia: induction of antibody-mediated immune suppression and prevention of severe clinical complications in a murine model[J] Transfusion. 2012;52:1446–1457. doi: 10.1111/j.1537-2995.2011.03480.x. [DOI] [PubMed] [Google Scholar]
- [96].Tiller H, Killie MK, Husebekk A, et al. Platelet antibodies and fetal growth: maternal antibodies against fetal platelet antigen 1a are strongly associated with reduced birthweight in boys[J] Acta Obstet Gynecol Scand. 2012;91:79–86. doi: 10.1111/j.1600-0412.2011.01269.x. [DOI] [PubMed] [Google Scholar]
- [97].Murphy AJ, Bijl N, Yvan-Charvet L, et al. Cholesterol efflux in megakaryocyte progenitors suppresses platelet production and thrombocytosis[J] Nat Med. 2013;19:586–594. doi: 10.1038/nm.3150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [98].Lindemann S, Kramer B, Seizer P, et al. Platelets, inflammation and atherosclerosis[J] J Thromb Haemost. 2007;5(Suppl 1):203–211. doi: 10.1111/j.1538-7836.2007.02517.x. [DOI] [PubMed] [Google Scholar]
- [99].Yang Y, Andrews MC, Hu Y, et al. Anthocyanin extract from black rice significantly ameliorates platelet hyperactivity and hypertriglyceridemia in dyslipidemic rats induced by high fat diets[J] J Agric Food Chem. 2011;59:6759–6764. doi: 10.1021/jf201079h. [DOI] [PubMed] [Google Scholar]
- [100].Yang Y, Shi Z, Reheman A, et al. Plant food delphinidin-3-glucoside significantly inhibits platelet activation and thrombosis: novel protective roles against cardiovascular diseases[J] PLoS One. 2012;7:e37323. doi: 10.1371/journal.pone.0037323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [101].Song F, Zhu Y, Shi Z, et al. Plant food anthocyanins inhibit platelet granule secretion in hypercholesterolaemia: Involving the signalling pathway of PI3K-Akt[J] Thromb Haemost. 2014;112:981–991. doi: 10.1160/TH13-12-1002. [DOI] [PubMed] [Google Scholar]
- [102].Podrez EA, Byzova TV, Febbraio M, et al. Platelet CD36 links hyperlipidemia, oxidant stress and a prothrombotic phenotype[J] Nat Med. 2007;13:1086–1095. doi: 10.1038/nm1626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [103].Ni H. The platelet "sugar high" in diabetes[J] Blood. 2012;119:5949–5951. doi: 10.1182/blood-2012-04-420794. [DOI] [PubMed] [Google Scholar]
- [104].Zhu W, Li W, Silverstein RL. Advanced glycation end products induce a prothrombotic phenotype in mice via interaction with platelet CD36[J] Blood. 2012;119:6136–6144. doi: 10.1182/blood-2011-10-387506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [105].Weyrich AS, Schwertz H, Kraiss LW, et al. Protein synthesis by platelets: historical and new perspectives[J] J Thromb Haemost. 2009;7:241–246. doi: 10.1111/j.1538-7836.2008.03211.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [106].Xu X, Carrim N, Lavalle C, et al. Platelets Are Versatile Cells: Emerging new roles in inflammation, immune response, angiogenesis, and atherosclerosis[J] Critical Reviews in Clinical Laboratory Sciences. In press. [Google Scholar]
- [107].Li C, Li J, Li Y, et al. Crosstalk between Platelets and the Immune System: Old Systems with New Discoveries[J] Adv Hematol. 2012;2012:384685–384699. doi: 10.1155/2012/384685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [108].Nording HM, Seizer P, Langer HF. Platelets in inflammation and atherogenesis[J] Front Immunol. 2015;6:98–109. doi: 10.3389/fimmu.2015.00098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [109].Bertozzi CC, Schmaier AA, Mericko P, et al. Platelets regulate lymphatic vascular development through CLEC-2-SLP-76 signaling[J] Blood. 2010;116:661–670. doi: 10.1182/blood-2010-02-270876. [DOI] [PMC free article] [PubMed] [Google Scholar]