We thank Martina Sester and colleagues for their careful reading of our paper [1] and for their support to the prospect of tuberculosis (TB) elimination in low-incidence countries in a foreseeable future. While we respect the views of the authors that the targets may appear too ambitious, we believe that, if the scientific community stay focussed on innovative approaches that can translate into scalable and effective interventions, we could reap the benefits of such interventions within the space of the next two decades [2]. Figure 1 shows the trend in TB incidence into the future, should current efforts to control TB – including the treatment of latent Mycobacterium tuberculosis infection (LTBI) – be intensified and boosted by new techniques and approaches.
Short abstract
Continued research is crucial to reach elimination targets, which will be unattainable unless new tools are developed http://ow.ly/TFYNi
From the authors:
We thank Martina Sester and colleagues for their careful reading of our paper [1] and for their support to the prospect of tuberculosis (TB) elimination in low-incidence countries in a foreseeable future. While we respect the views of the authors that the targets may appear too ambitious, we believe that, if the scientific community stay focussed on innovative approaches that can translate into scalable and effective interventions, we could reap the benefits of such interventions within the space of the next two decades [2]. Figure 1 shows the trend in TB incidence into the future, should current efforts to control TB – including the treatment of latent Mycobacterium tuberculosis infection (LTBI) – be intensified and boosted by new techniques and approaches.
FIGURE 1.
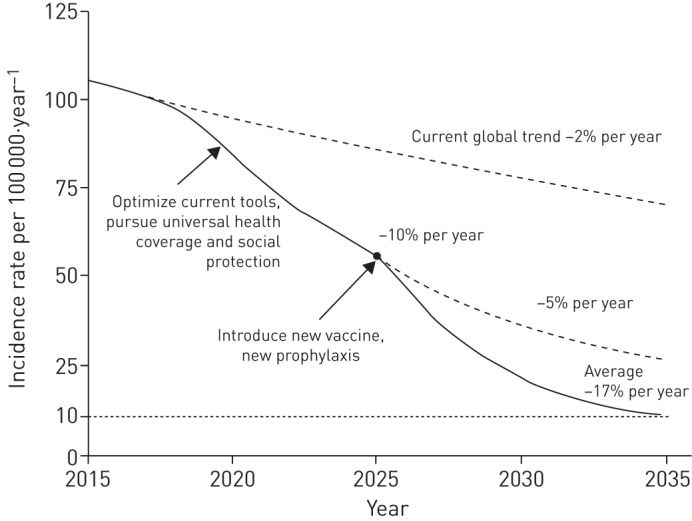
Projected trend in the decline of global tuberculosis incidence, from 110 cases per 100 000 in 2015 to 10 cases per 100 000 or less by 2035. Reproduced from [3] with permission from the publisher.
When discussing the importance of preventive chemotherapy for LTBI in the context of TB elimination, the authors point out two critical issues: the limitations of diagnostic tests for LTBI, and the importance of appropriately defining target populations for systematic LTBI testing. To provide guidance in this area, the World Health Organization (WHO) has recently issued guidelines on LTBI management [4].
Both tuberculin skin testing (TST) and interferon-γ release assays (IGRAs) have a poor positive predictive value to determine which individuals with presumed latent infection are more likely to develop active TB, implying that a high proportion of treated individuals would receive medication unnecessarily. Nonetheless, these tests still have a role in helping clinicians improve the health outcomes of their patients and to progress towards TB elimination. Conversely, the negative predictive value of TST and IGRAs is high enough to exclude most individuals who would not benefit from LTBI treatment [5]. Contrary to what Martina Sester and colleagues maintain, the number of active TB cases that will continue to occur among those testing negative is thus unlikely to have a significant public health impact.
We agree with Martina Sester and colleagues that to optimise the allocation of available resources, appropriate selection of risk groups for systematic LTBI testing and treatment is crucial. WHO recommends that individuals with a positive TST or IGRA should be treated for LTBI if they have the following risks: HIV infection, are contacts of pulmonary TB cases, initiate anti-tumour necrosis factor treatment, receive dialysis, prepare for transplantation, or have silicosis. The WHO guidelines group – composed of leading world experts using the GRADE (Grading of Recommendations Assessment, Development and Evaluation) approach [6] – made a strong recommendation for LTBI treatment in these groups, on the premise of both direct and surrogate evidence for an increased risk of progression from infection to disease when compared with the general population, and much less upon a positive LTBI test. Martina Sester and colleagues argue that the number of individuals who need to take prophylactic medication in order to prevent one active case (number needed to treat (NNT)) would have been a better outcome measure to select at-risk populations. While this appears to be a logical approach, it also has limitations. The values tabulated for NNT are likely to have a very wide confidence interval (data not shown), limiting their use in public health planning. Even if the point estimates of NNT are comparable in similar groups, it is likely that, in practice, these will vary because of setting-specific factors, such as the programmatic effectiveness of prophylaxis measures given, background levels of drug resistance, multiple risks in the same individuals and so on.
Regardless of the approach, Martina Sester and colleagues come to the conclusion that contacts should be prioritised for systematic testing and treatment, and we could not agree more. Indeed, in low-incidence countries, outbreaks contribute importantly to TB dynamics and hence contact-tracing activities are crucial for TB elimination [7, 8]. As cases become rarer in such settings contact tracing becomes more important.
The suggestion that, among people living with HIV, there should be a focus primarily on those with active viral replication remains speculative until more comprehensive evidence is available.
Martina Sester and colleagues suggest that even in patients, such as those preparing for stem cell or solid organ transplant testing (and treatment) should only be done if additional risk factors are present, an opinion based on very limited data.
We agree that health care workers may not represent a high risk population in low incidence countries, and the decision to screen should be based on local epidemiology, needs, and resources. In fact, the WHO 2014 guidelines only make a conditional recommendation for testing and treatment in this group.
In conclusion, continued research will remain crucial to reach the elimination targets, which will be unattainable unless new tools are developed, particularly better prognostic tests for LTBI diagnosis and shorter, safer, and effective prophylactic treatment. In addition, we need effective ways at implementing such interventions at scale and addressing the upstream determinants of TB as laid out by WHO's End TB Strategy for the post 2015 horizon [9].
Acknowledgments
This article is one of a selection of articles published as ERJ Open papers, as part of an initiative agreed between the European Respiratory Society and the World Health Organization.
Footnotes
Conflict of interest: None declared.
References
- 1.Lönnroth K, Migliori GB, Abubakar I, et al. . Towards tuberculosis elimination: an action framework for low-incidence countries. Eur Respir J 2015; 45:928–952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Diel R, Loddenkemper R, Zellweger J-P, et al. . Old ideas to innovate tuberculosis control: preventive treatment to achieve elimination. Eur Respir J 2013; 42: 785–801. [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization. Draft global strategy and targets for tuberculosis prevention, care and control after 2015. Report by the Secretariat. A67/11 Geneva, World Health Organization, 2014. Available from: apps.who.int/gb/ebwha/pdf_files/WHA67/A67_11-en.pdf [Google Scholar]
- 4.Guidelines on the Management of Latent Tuberculosis Infection (WHO/HTM/TB/2015.01) Geneva, World Health Organization, 2014. Available from: http://apps.who.int/iris/bitstream/10665/136471/1/9789241548908_eng.pdf [Google Scholar]
- 5.Diel R, Loddenkemper R, Niemann S, et al. . Negative and positive predictive value of a whole-blood interferon-γ release assay for developing active tuberculosis: an update. Am J Respir Crit Care Med 2011; 183: 88–95. [DOI] [PubMed] [Google Scholar]
- 6.Guyatt GH, Oxman AD, Vist GE, et al. . GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008; 336: 924–926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Codecasa LR, Ciconali G, Mazzola E, et al. . Managing an extensively drug-resistant tuberculosis outbreak: the public health face of the medal. Eur Respir J 2015; 45: 292–294. [DOI] [PubMed] [Google Scholar]
- 8.Esposito S, D'Ambrosio L, Tadolini M, et al. . ERS/WHO Tuberculosis Consilium assistance with extensively drug-resistant tuberculosis management in a child: case study of compassionate delamanid use. Eur Respir J 2014; 44: 811–815. [DOI] [PubMed] [Google Scholar]
- 9.Uplekar M, Weil D, Lonnroth K, et al. . WHO's new end TB strategy. Lancet 2015; 385: 1799–1801. [DOI] [PubMed] [Google Scholar]


