miR-301a/miR-454, which targets the 3′-UTR of ET-1 and PAI-1, are located in the intron of the SKA2 gene. These miRNAs are transcriptionally regulated by PPAR-α. Fenofibrate, a PPAR-α agonist increases levels of miR-301a/miR-454, with potential for amelioration of pulmonary hypertension.
Keywords: endothelin-1 (ET-1), micro ribonucleic acid (miRNA), peroxisome proliferator-activated receptor-α (PPAR-α), plasminogen activator inhibitor-1 (PAI-1), sickle cell disease (SCD), spindle and kinetochore-associated protein-2 (SKA2)
Abstract
Endothelin-1 (ET-1) and plasminogen activator inhibitor-1 (PAI-1) play important roles in pulmonary hypertension (PH) in sickle cell disease (SCD). Our previous studies show higher levels of placenta growth factor (PlGF) in SCD correlate with increased plasma levels of ET-1, PAI-1, and other physiological markers of PH. PlGF-mediated ET-1 and PAI-1 expression occurs via activation of hypoxia-inducible factor-1α (HIF-1α). However, relatively little is understood regarding post-transcriptional regulation of PlGF-mediated expression of ET-1 and PAI-1. Herein, we show PlGF treatment of endothelial cells reduced levels of miR-301a and miR-454 from basal levels. In addition, both miRNAs targeted the 3′-UTRs of ET-1 and PAI-1 mRNAs. These results were corroborated in the mouse model of SCD [Berkeley sickle mice (BK-SS)] and in SCD subjects. Plasma levels of miR-454 in SCD subjects were significantly lower compared with unaffected controls, which correlated with higher plasma levels of both ET-1 and PAI-1. Moreover, lung tissues from BK-SS mice showed significantly reduced levels of pre-miR-301a and concomitantly higher levels of ET-1 and PAI-1. Furthermore, we show that miR-301a/miR-454 located in the spindle and kinetochore-associated protein-2 (SKA2) transcription unit was co-transcriptionally regulated by both HIF-1α and peroxisome proliferator-activated receptor-α (PPAR-α) as demonstrated by SKA2 promoter mutational analysis and ChIP. Finally we show that fenofibrate, a PPAR-α agonist, increased the expression of miR-301a/miR-454 and SKA2 in human microvascular endothelial cell line (HMEC) cells; the former were responsible for reduced expression of ET-1 and PAI-1. Our studies provide a potential therapeutic approach whereby fenofibrate-induced miR-301a/miR-454 expression can ameliorate PH and lung fibrosis by reduction in ET-1 and PAI-1 levels in SCD.
INTRODUCTION
Pulmonary disease, both acute and chronic, is the second most common cause of hospitalization and a leading cause of both morbidity and mortality in adults with sickle cell disease (SCD) [1,2]. Factors implicated in pulmonary hypertension (PH) in SCD include endothelial dysfunction, pulmonary vasoconstriction and vascular remodelling [3–6].
Endothelin-1 (ET-1) and nitric oxide (NO) are opposing pulmonary vasoactive factors that regulate pulmonary vascular tone [4,6–8]. Studies have shown that there is a clinical syndrome of haemolysis-associated PH in SCD [4]. Haemolysis leads to NO quenching by free haemoglobin in plasma, thereby reducing the bioavailability of this NO-synthase product [1,5,9]. ET-1 is a potent pulmonary vasoconstrictor and its levels are elevated in SCD patients with PH [10]. ET-1 is normally induced in endothelial cells in response to hypoxic activation of hypoxia-inducible factor-1 (HIF-1) [11,12]. Abrogation of this linkage by use of ET-1 receptor antagonists has been shown to be beneficial for treatment of primary PH [13]. This treatment has been found to be beneficial for PH treatment in sickle-Antilles-haemoglobin D mice [13], thus indicating the important role of ET-1 in PH in SCD. Other studies show that SCD patients have elevated steady state plasma levels of circulating tissue factor [14] and plasminogen activator inhibitor-1 (PAI-1), both of which increase further during sickle vaso-occlusive crises [15]. The prothrombic state thus predisposes patients to PH and stroke [16,17]. In addition to the role of PAI-1 in coagulation, it is responsible for development of lung injury/fibrosis; its expression is also modulated by other physiological stimuli such as hypoxia, transforming growth factor-β (TGF-β) and lipopolysaccharide (LPS) [18–20].
We have previously reported high circulating levels of placenta growth factor (PlGF) in SCD, compared with healthy control subjects, correlates with increased incidence of vaso-occlusive crises [21]. We also demonstrated the specific contribution of elevated PlGF to PH by ectopic, erythroid PlGF expression from a transduced, lentivirus vector, in normal mice to abnormally high levels also seen in Berkeley-SS mice [6]. These mice showed increased production of ET-1 with increased right ventricular pressures and right ventricle hypertrophy, both markers of PH [6]. These findings were corroborated in patients (n=123) with SCD, in whom plasma PlGF levels were associated with anaemia, an increase in ET-1 levels and increased tricuspid regurgitant velocity (TRV); the latter a marker of peak pulmonary artery pressure [6]. Studies by Brittain et al. [22] of 74 SCD patients found a positive correlation between high PlGF levels, haemolysis and inflammation. Moreover, we showed PlGF increased the expression of ET-1 and PAI-1 in human pulmonary microvascular endothelial cells (HPMVEC) and monocytes via activation of HIF-1α, independently of hypoxia [8,23]. Indeed, PlGF-mediated induction of PAI-1 was achieved by a transcriptional mechanism involving HIF-1α [23] and post-transcriptionally by specific miRNAs (miR-30c and miR-301a) that bind to the 3′-UTR of PAI-1 mRNA [24]. Our recent studies show miR-199a2 targets the 3′-UTR of HIF-1α mRNA and concomitantly attenuates expression of HIF-1α and its downstream target genes, e.g. ET-1 [25].
In the present study, we examined the role of miRNAs in the post-transcriptional regulation of ET-1 and PAI-1. Our studies showed that miR-301a and miR-454, target the 3′-UTRs of ET-1 and PAI-1 mRNAs. A physiological relationship between miR-301a and miR-454 was demonstrated in vitro, as both miRNAs attenuated PlGF-mediated secretion, in human microvascular endothelial cell line (HMEC-1), of both ET-1 and PAI-1. Moreover, these miRNAs co-located in an intron of the spindle and kinetochore-associated protein-2 (SKA2) gene were co-transcriptionally regulated by peroxisome proliferator-activated receptor-α (PPAR-α) and HIF-1α. The participation of PPAR-α in SKA2 transcription was corroborated by employing the PPAR-α agonist, fenofibrate. Furthermore, the expression of pre-miR-301a was significantly reduced in lung tissues harvested from sickle mouse model [Berkeley sickle mice (BK-SS)] animals compared with C57BK/6NJ controls. A similar relationship was observed in the plasma levels of miR-454 of sickle cell anaemia (SCA) patients compared with healthy matched controls, where elevated ET-1 and PAI-1 levels are observed. The present study, to the best of our knowledge, is the first demonstration that PPAR-α co-regulates the transcription of SKA2, miR-301a and miR-454; the ET-1 mRNA has complementary sites in the 3′-UTR for the seed sequences of these miRNAs.
MATERIALS AND METHODS
Cell culture and reagents
HPMVECs, at passage two and growth media were obtained from Cell Applications Inc. These cells were cultured in growth media containing 10% FBS on 1% gelatin-coated tissue culture flasks or dishes according to manufacturer's instructions. These primary cells maintained characteristics of endothelial cell morphology and cell phenotype up to passage 6–7 and thus were not used beyond the 7th passage [26]. Immortalized HMEC-1, grown in culture, were not used beyond 20 passages [26]. These were cultured in RPMI-1640, supplemented with 10% FBS, sodium heparin, HEPES buffer, sodium pyruvate, non-essential amino acids and penicillin–streptomycin. Unless otherwise indicated, endothelial cells were cultured overnight in complete medium containing 2% serum, followed by incubation for 3 h in serum-free medium (SFM) prior to treatment with either PlGF (250 ng/ml) or other experimental conditions as indicated.
Recombinant human PlGF (Peprotech), primary antibodies against HIF-1α, ET-1, PAI-1, PPAR-α and secondary antibodies conjugated to horseradish-peroxidase (HRP) were obtained from Santa Cruz Biotechnology. Antibodies against β-actin were obtained from Sigma Chemical Company. Hsa-miR mimics and hsa-miR-inhibitors were purchased from Shanghai Gene Pharma Co. Ltd and Applied Biosystems. shRNAs for PPAR-α were generously provided by Dr Jae Jung (USC). siRNA for HIF-1α was obtained from Santa Cruz Biotechnology.
Human subjects
All blood samples were obtained from children with homozygous SCA at steady state during their elective clinic appointments with routine clinical blood draws provided through the Hematology Repository at Cincinnati Children's Hospital Medical Center, Cincinnati, OH. All samples were obtained with the informed consent of the patient/legal guardian using Institutional Review Board approved-protocols at Cincinnati Children's Hospital. The plasma samples were obtained from the SCA patients and unaffected sibling as controls. Blood samples were analysed from patients who had no acute sickle events, fevers or infections 3 weeks before or 3 weeks after the blood draw, and were not transfused within the last 90 days.
Animal studies
Animal protocols were approved by the Institutional Animal Care and Use Committee at Cincinnati Children's Hospital Medical Center. BK-SS originally obtained from Jackson Laboratories were bred up to the 6th generation against a C57BL/6NJ background. The BK-SS mice carry deletions for the mouse α- and β-globin genes, and carry a transgene expressing the human α-globin and a mini β-globin cluster, including the β-sickle globin as described [25,27]. Six male BK-SS mice at 10–12 weeks of age were used for these experiments. Five female and one male, in-house bred C57BL/6NJ animals (10–12 weeks old) served as controls. Mice were exsanguinated and lungs were removed for analysis; all tissues were stored at −80°C and later assayed for miRNAs, ET-1 and PAI-1.
Isolation of RNA and expression of mRNA and miRNA by qRT-PCR
Endothelial cells were treated with PlGF for indicated time periods followed by total RNA extraction using TriZOL reagent (Invitrogen) as per manufacturer's protocol. mRNA and pre-miRNA expression were determined and quantified using specific primers (Table 1). Quantitative real-time PCR (qRT-PCR) of mRNA and pre-miRNA templates was performed using the iScript One-Step RT-PCR Kit with SYBR Green detection (Bio-Rad) in an ABI Prism 7900 HT sequence detection system (Applied Biosystems, Foster City, CA). Briefly, PCR amplification of 100 ng of total RNA was performed for 40 cycles under the following conditions: cDNA synthesis at 42°C for 10 min, iScript reverse transcriptase inactivation at 95°C for 10 s and PCR cycling and detection at 95°C for 5 s, followed by 60°C for 34 s. Values are expressed as relative expression of mRNAs or pre-miRNAs, normalized to endogenous GAPDH mRNA levels [24,28]. Mature miRNAs were isolated using mirVana isolation kit (Applied Biosystems) and miRNA expression levels were determined using the TaqMan MicroRNA Assay Kits for indicated miRNAs (Applied Biosystems), as previously described [24].
Table 1. Oligonucleotide primers used in the present study.
Abbreviations: qRT-PCR, quantitative real-time PCR; SDM, site directed mutagenesis.
| Gene | Method | Forward primer | Reverse primer |
|---|---|---|---|
| SKA2 mRNA | qRT-PCR | GTTCCAGAAAGCTGAGTCTGA | TTGCTGAATCAGGATGATTAGTCT |
| GAPDH mRNA | qRT-PCR | AACCTGCCAAGTACGATGACATC | GTAGCCCAGGATGCCCTTGA |
| Pre-miR-301a RNA | qRT-PCR | CTGCTAACGAATGCTCTGAC | CCTGCTTTCAGATGCTTTGAC |
| Pre-miR-454 RNA | qRT-PCR | GATCCTAGAACCCTATCAATATTG | CCCATTGTTCTTTCCAAACACC |
| mPAI-1 | qRT-PCR | GTA TGA CGT CGT GGA ACT GC | TTTCTCAAAGGGTGC AGC GA |
| mET-1 | qRT-PCR | TGCCTCTGAAGTTAGCCGTG | AGTTCTCCGCCGCCTTTTTA |
| mGAPDH | qRT-PCR | TTGCAGTGGCAAAGTGGAGA | GTCTCGCTCCTGGAAGATGG |
| mpremiR-301a | qRT-PCR | GCTAACGGCTGCTCTGACTT | CTCGCGGATGCTTTGACAAT |
| SKA2 HRE1M (−193/−189) | SDM | TTGTGATTGGCTGAGATagatcAGAGCTC- CAGCCAATCAG | CTGATTGGCTGGAGCTCTgatcTATCTCA- GCCAATCACAA |
| SKA2 HRE2M (−223/−219) | SDM | CGGATGGTGTAGGAgatcAGCCCGGCTTG- TGA | TCACAAGCCGGGCTgatcTCCTACACCAT- CCG |
| SKA2 del PPAR-α | SDM | GATATGAAGAAGTAAAAACCTCCCAAG- AGAATTTGACAATATTAGAATATATTCC | GGAATATATTCTAATATTGTCAAATTC- TCTTGGGAGGTTTTTACTTCTTCATATC |
| SKA2 promoter (PPRE at −1671/−1653) | ChIP | GCTAAGTGTTAGCTAGCAAGTGT | GCCAACTCCTGCAAAAGACT |
| ET-1 miR-301a/454 site 1 mutant | SDM | TGGCCGACTCcatcCTCTCCACCCTGG | CAGGGCTCTCCGTGGAGG |
| ET-1 miR-301a/454 site 2 mutant | SDM | TCACCTATATcatcCTCTGGCAGAAGTATTTC | GGTAGACTCATATTCATGAAAC |
| PAI-1 miR-301a/454 site 1 mutant | SDM | ATGGATGTAAcatcCTTTGGGAGGCCAAGGC | CTTTGTGCCCTACCCTCTG |
| PAI-1 miR-301a/454 site 2 mutant | SDM | TTTTTGATTTcatcCTGGACGGTGACG | AGAAAGAAAGAAAAACCCCAAAG |
Generation of SKA2 promoter luciferase constructs and 3′-UTR reporter luciferase constructs for ET-1 and PAI-1
The SKA2 promoter luciferase construct was generated using the Infusion Cloning kit. Briefly, the 5′-flanking region of SKA2 spanning nts −2000 to +12 was PCR amplified from human BAC clone RP11-626H11 (BACPAC Resources Center) with the Phusion PCR kit (New England Biolabs), and amplified product was inserted into the pGL3-Basic vector. The 3′-UTR for ET-1 was PCR amplified from human BAC clone RP11-353G10 and inserted into the unique XbaI site, 3′ to the reporter gene in the pGL3-Control vector. PAI-1 3′-UTRs were PCR amplified from BAC clone RP11-213E22 and inserted into the pMIR vector using the Infusion cloning kit (Clontech) and primers listed in Table 1. Deletions of the PPAR-α site and mutation of the HIF-1α-binding site, within the SKA2 promoter, mutations within the miR-301a/miR-454-binding sites in the ET-1 and PAI-1 3′-UTRs were all carried out using the Q5 site-directed mutagenesis kit (New England Biolabs) in the corresponding parental vectors using primers listed in Table 1. All constructs and mutations were verified by sequencing.
Transient transfections
Transient transfections of endothelial cells were performed using the Amaxa Nucleofector [25]. Briefly, 1×106 cells per transfection were collected by centrifugation and resuspended in 100 μl of RPMI-1640, along with the indicated plasmids. Cells were then electroporated using the Y-001 transfection protocol. Transfected cells were incubated for 24 h in complete media, followed by serum deprivation for 12 h prior to treatment with PlGF. For luciferase reporter experiments, 1 μg each of the luciferase plasmid and Renilla luciferase plasmid was used. For RNAi experiments, 1 μg of the shRNA plasmid, 90 pmol of the miRNA mimics and miRNA inhibitors, as indicated, were used for transfections.
Luciferase assays
Luciferase assays were conducted using the Dual-luciferase assay kit (Promega), as per the manufacturer's protocol. Briefly, cells were centrifuged and lysed in 1× passive lysis buffer; 20 μl of the lysates were used for the luciferase assays. Luciferase values were normalized to Renilla luciferase values. Data are expressed relative to the parent vector or promoterless vector, as appropriate.
Western blot analysis
Whole cell lysates were prepared from cells as previously described [25]. Extracts were subjected to electrophoresis on a 12% SDS/PAGE gel followed by electrophoretic transfer to a PVDF membrane. Membranes were probed for HIF-1α, ET-1 and PAI-1 proteins utilizing antibodies to HIF-1α (1:250), ET-1 (1:500) and PAI-1 (1:500), respectively. Blots were stripped and reprobed with a β-actin antibody to monitor protein loading. The immunoreactive protein bands were detected using the Clarity Western ECL Solution (Bio-Rad). The quantitation of band intensities was performed on scanned images utilizing ImageJ Software.
ChIP assays
HMEC-1 cells in serum free media were treated with PlGF (250 ng/ml). ChIP analysis was performed using an antibody to HIF-1α and PPAR-α (Santa Cruz Biotechnology) as previously described [25]. DNA was subjected to PCR amplification for 30 cycles using the following conditions: 95°C for 45 s, 63°C for 30 s, 72°C for 120 s, using primers listed in Table 1. The PCR products were analysed by electrophoresis on a 2% agarose gel, visualized by ethidium bromide staining and quantified using the ImageJ analysis software [25].
Quantification of secreted ET-1 and PAI-1
HMEC-1 (1×105 cells) were transfected with indicated miRNA mimic or negative controls (NC mimic or inhibitors; 90 pmol) as described above and incubated in complete media at 37°C for 24 h. Cells were washed with SFM and incubated for 3 h in SFM (2 ml) treatments were begun by replacement with fresh SFM (1 ml) and additions, as indicated. Cells were treated with either PlGF (250 ng/ml) or fenofibrate (0.1 mM) overnight. The culture supernatant was collected and an aliquot (0.1 ml) was assayed for ET-1 (R&D Systems) and PAI-1 (Peprotech) release using an ELISA kit. The cells were collected by scraping and the pellet was assayed for protein content utilizing the Bradford method.
Statistical analysis
Data are presented as means±S.D. One-way ANOVA, followed by Tukey–Kramer test were used for multiple comparisons using the Instat-2 software (Graph Pad). P values of less than 0.05 were considered significant.
RESULTS
miR-301a and miR-454, located in the first intron of host gene SKA2, are co-transcriptionally regulated by PPAR-α and HIF-1α
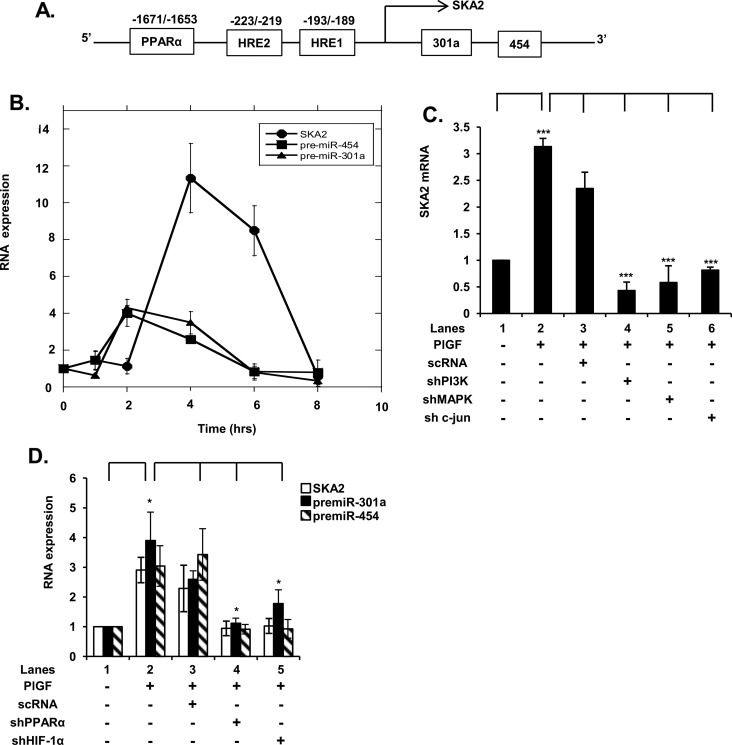
Our previous studies show PlGF treatment of HPMVECs attenuates expression of miR-30c and miR-301a, which target the 3′-UTR of PAI-1 mRNA and thus affect its turnover [24]. In silico analysis showed miR-301a is located in the first intron of the SKA2 gene and is co-localized with miR-454 as shown in the gene schematic (Figure 1A). Further analysis predicted that miR-454 also could interact with the 3′-UTRs of ET-1 and PAI-1. We began by examining the time course of expression of SKA2, pre-miR-301a and pre-miR-454 mRNA by qRT PCR, in response to PlGF in HMEC-1. We observed that PlGF treatment of HMEC resulted in a time-dependent increase in SKA2 mRNA expression with maximal increase of ∼10-fold at 4 h (Figure 1B). The expression of pre-miR-301a and pre-miR-454 mRNA showed a maximal increase in ∼4-fold at 2 h, followed by a gradual decline after 4 h to almost basal level by 8 h (Figure 1B). Moreover, PlGF-mediated SKA2 expression was attenuated by shRNA for phosphoinositide 3-kinase (PI3K), shRNAs for mitogen-activated protein kinase (MAP kinase) and c-Jun (Figure 1C), indicating the roles of PI3K, MAP kinase and c-Jun in the transcription of SKA2. Furthermore, these results indicated that pri-miRNA synthesis and pre-miRNA processing preceded SKA2 transcription and splicing, as expected from the 5′-proximal location of the miRNA genes within SKA2. Alternatively an independent promoter for pri-miRNA transcription could be operative. In an effort to distinguish between these two possibilities further analysis of SKA2 and miRNA transcription was performed.
Figure 1. PlGF up-regulates the expression of miR-301a and miR-454 located in an intron of host gene SKA2 by activation of HIF-1α and PPAR-α.
(A) Schematic of 5′ end of SKA2 gene showing locations of miR-301a and miR-454 in the first intron of SKA2 and positions of cis-binding elements for HIF-1α and PPAR-α. (B) Time-dependent (1–8 h) expression of SKA2, pre-miR-301a and pre-miR-454 RNA. (C) Effect of transfection of shRNAs for PI3K, MAPK and c-Jun on SKA2 mRNA expression. HMEC cells were transfected with shRNAs for 24 h, followed by treatment with PlGF for 4 h. (D) Effect of transfection of shRNAs for HIF-1α and PPAR-α on PlGF-mediated SKA2 transcription following 2 h incubation. Data are means±S.D. of three independent experiments. ***P<0.001, **P<0.01, *P<0.05, nsP>0.05.
In silico analysis of the 5′-flanking ∼2 kb region of SKA2 revealed the presence of cis-binding elements for PPAR-α and binding sites for HIF-1α (HRE, hypoxia response element), as shown in Figure 1(A). The presence of these transcription factor-binding sites within the SKA2 promoter guided our decision to perform a gene knockdown approach. As shown in Figure 1(D), transfection of HMEC with PPAR-α shRNA and HIF-1α shRNA attenuated PlGF-mediated induction of SKA2 mRNA to the basal level (Figure 1D, lanes 4 and 5 compared with lane 2). Moreover, the knockdown of PPAR-α and HIF-1α also reduced >90% the expression of pre-miR-301a and pre-miR-454 (Figure 1D). Taken together these data showed that pre-miR-301a and pre-miR-454 were co-transcribed with the SKA2 primary transcript, induced by PlGF, and were not products of a secondary transcription unit within the SKA2 intron.
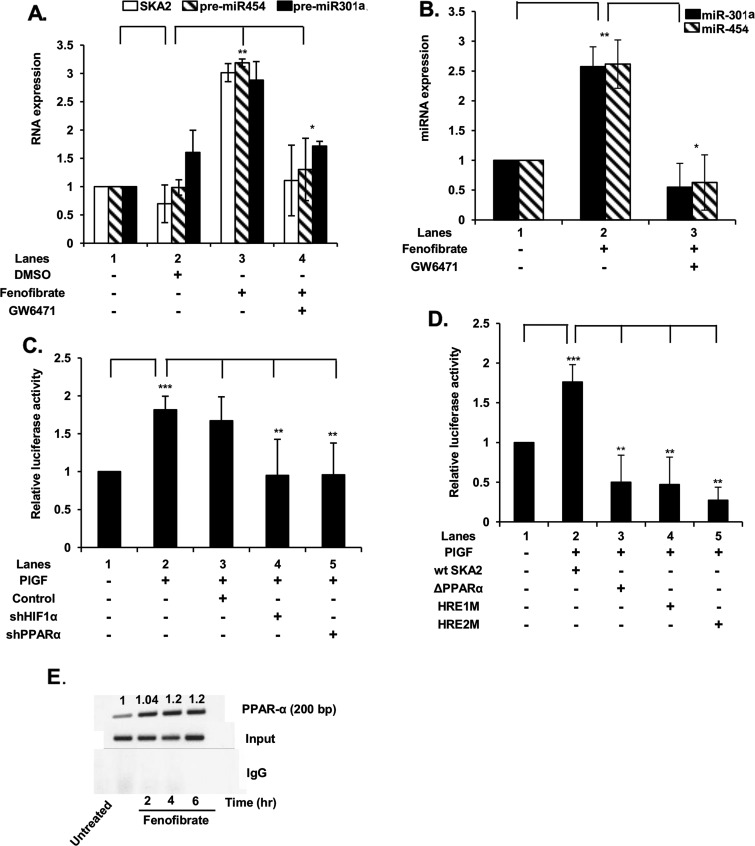
PlGF-mediated transcription of SKA2 involves PPAR-α as demonstrated by PPAR-α agonist, promoter analysis and ChIP
In order to further extend our observation regarding the participation of PPAR-α in SKA2 transcription, we employed the synthetic PPAR-α agonist fenofibrate and the PPAR-α antagonist GW6471 for their effects on SKA2 transcription. Treatment of HMEC with fenofibrate resulted in a ∼3-fold increase in SKA2 mRNA, pre-miR-301a and pre-miR-454. Moreover, the induction of SKA2 mRNA, pre-miR-301a and pre-miR-454 was reduced by >80% by GW6471 (Figure 2A). In addition, fenofibrate addition also augmented by 3-fold the expression of mature miR-301a and miR-454, both of which were attenuated by GW6471 (Figure 2B). These results clearly showed by a functional approach that synthesis of the latter miRNAs was linked to the initiation of transcription of SKA2.
Figure 2. PlGF-mediated expression of SKA2 transcription unit is regulated by PPAR-α and HIF-1α as demonstrated by SKA2 promoter analysis and ChIP.
(A) Effect of PPAR-α agonist (fenofibrate) and its antagonist (GW6471) on SKA2, pre-miR-301a and pre-miR-454 RNA expression. HMEC cells were pre-treated with GW6471 (15 μM) for 30 min, where indicated, followed by treatment with fenofibrate (100 μM) for 2 h. (B) Effect of fenofibrate on induction of mature miR-301a and miR-454. (C) Effect of shRNA for HIF-1α and PPAR-α on PlGF-mediated transcription of SKA2, as demonstrated utilizing wt SKA2 promoter-luciferase reporter. HMEC were co-transfected overnight with wt SKA2-luc and indicated shRNAs along with Renilla luciferase plasmid, followed by treatment with PlGF for 4 h. Cell lysates were assayed for luciferase activity and data normalized for Renilla luciferase activity. (D) Effect of mutation of HRE sites and deletion of PPAR-α sites in wt SKA2 promoter of SKA2-luc reporter. HMEC cells were transfected with the wt SKA2 promoter-luc or SKA2-luc reporters with mutations in either HRE site 1 or HRE site 2 or deletion of PPAR-α cis-binding element. Cells were co-transfected with Renilla luciferase plasmid for 24 h and were treated with PlGF for 4 h. Luciferase activity was normalized to Renilla luciferase activity to correct for transfection efficiency and the data are expressed as relative expression compared with the luciferase activity of wt construct, as indicated in the figure. Data are means±S.D. of three independent experiments. ***P<0.001, **P<0.01, *P<0.05, nsP>0.05. (E) ChIP analysis of HMEC cells treated with fenofibrate for 2–6 h, for assay of PPAR-α binding to the SKA2 promoter. PPAR-α antibody (top row) or control rabbit IgG (bottom row) were used for immunoprecipitation of soluble chromatin. The middle panel represents the amplification of input DNA before immunoprecipitation. Densitometric analysis, showing relative intensity of PPAR-α PCR product normalized to input DNA are indicated above each lane. Data are representative of two independent experiments.
Since PlGF induced SKA2 mRNA expression in HMEC, we utilized a SKA2 promoter luciferase reporter gene construct to further delineate the roles of PPAR-α and HIF-1α in this promoter. The wt SKA2-luc plasmid (∼2 kb) has provisionally identified PPAR-α and HIF-1α cis-binding promoter elements as depicted in the schematic diagram in Figure 1(A). HMEC transfected with the wt SKA2 luc reporter plasmid followed by treatment with PlGF showed a ∼1.8-fold increase in luciferase activity (Figure 2C, lane 2 compared with lane 1). The promoter construct was functionally the same as the endogenous promoter as shown by the effect of shRNA for PPAR-α and HIF-1α, both of which attenuated PlGF induced luciferase activity (Figure 2C).
Next, we determined cis-binding element regions for PPAR-α in the SKA2 promoter, which were responsible for SKA2 transcription. HMEC were transfected with the wt promoter (∼2000 bp) luciferase reporter and a promoter construct deleting the PPAR-α site located at nts −1671 to −1673. Expression of this PPAR-α deleted SKA2 promoter in HMEC, following PlGF treatment resulted in reduction in luciferase activity below the basal level when compared with the intact wt SKA2 promoter (Figure 2D, lane 3 compared with lane 2). Similarly, mutation of either HRE-1 or HRE-2 sites in the SKA2 promoter completely abrogated PlGF induction of luciferase activity (Figure 2D, lanes 4 and 5 compared with lane 2). These results confirmed the predicted transcription factor utilization in the initiation of SKA2 transcription, showing that both PPAR-α and HIF-1α were actively involved in transcription.
An assessment of binding of PPAR-α to the SKA2 promoter was confirmed by analysis of native chromatin in HMEC using the ChIP assay. For this analysis, we utilized chromatin from HMEC cells treated with a PPAR-α agonist, fenofibrate. HMEC were incubated with fenofibrate up to 8 h followed by ChIP with PPAR-α antibody or control rabbit IgG. Fenofibrate treatment of HMEC showed ∼3-fold increase in an expected 200 bp PCR product that corresponds to nt −1736 to −1537 of the SKA2 promoter region containing the PPAR-α site (Figure 2E). The recovery of the expected PCR product reached a maximum after 4 h and remained constant through 8 h, post fenofibrate addition (Figure 2E). As shown, amplification of the input DNA prior to immunoprecipitation was equivalent in all the samples (Figure 2E, middle panel) and the absence of signal in the control IgG immunoprecipitate confirmed the specificity of the anti-PPAR-α immunoprecipitation. The combination of these promoter studies clearly established that PPAR-α participates in SKA2 transcription.
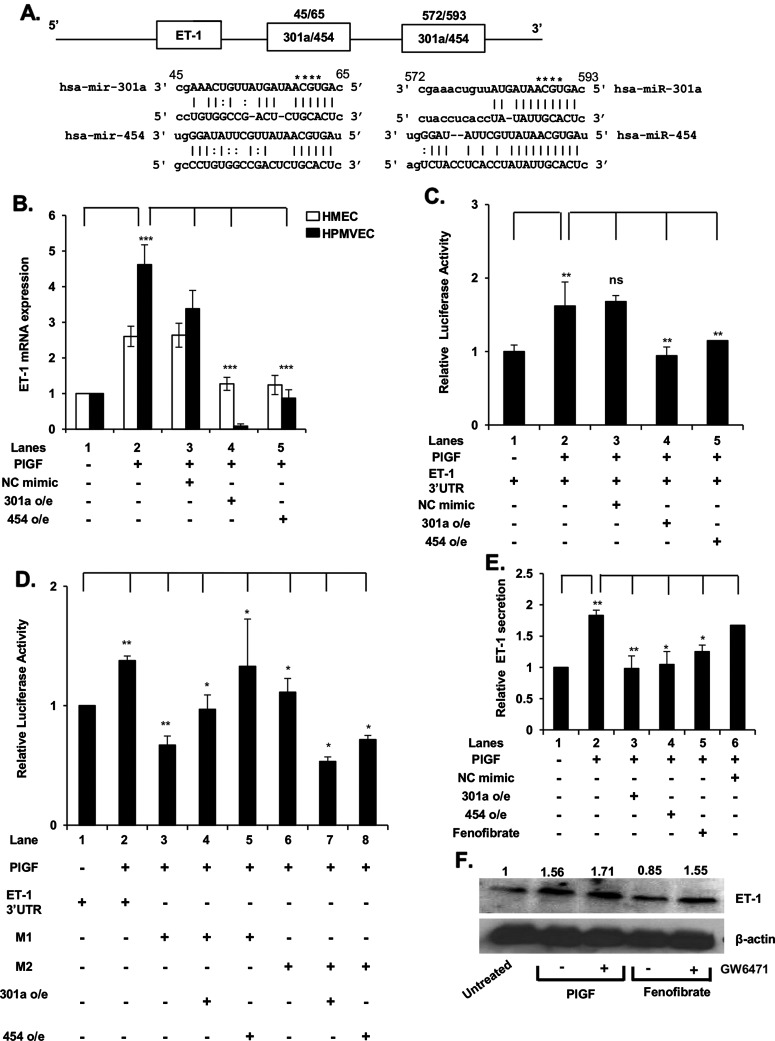
miR-301a and miR-454 target 3′-UTR of ET-1 and attenuate ET-1 mRNA and protein levels
In silico analysis of the 3′-UTR of ET-1 mRNA predicted miR-301a/miR-454 miRNA recognition element (MRE) sequences at nucleotides +45/+65 and +572/+593, as depicted in the schematic of Figure 3(A). Although the 3′ complementary regions of these miRNAs are different, the 5′-domains of each are capable of base pairing to the same MRE in the ET-1 3′-UTR. We tested this prediction by examining the effects of synthetic miR-301a and miR-454 on PlGF induced ET-1 mRNA expression in both HMEC and HPMVEC. As shown in Figure 3B, transfection with both miR-301a and miR-454 mimics reduced PlGF-mediated ET-1 mRNA to basal levels. We next examined the role of the ET-1 3′-UTR as the sole determinant of miR-301a and miR-454 targeting in a luciferase translation reporter, in response to PlGF. Upon co-transfection of pGL3-ET-1 3′-UTR-luc with exogenous miR-301a or miR-454 mimics, we observed ∼90% decrease in luciferase activity, compared with PlGF treated cells (Figure 3C, lanes 4 and 5 compared with lane 2). These data showed that both miR-301a and miR-454 target the 3′-UTR of ET-1 mRNA to attenuate ET-1 synthesis.
Figure 3. miR-301a and miR-454 target the 3′-UTR of ET-1 mRNA.
(A) Schematic of 3′-UTR of ET-1 mRNA showing locations of MRE for miR-301a and miR-454. (B) Effects of miR-301a and miR-454 synthetic mimics on PlGF-mediated ET-1 mRNA expression. HMEC and HPMVEC cells were transfected with miR-301a mimic (90 pmol), miR-454 mimic (90 pmol) or control (NC mimic) overnight, followed by treatment with PlGF for 6 h. (C) Effect of miR-301a and miR-454 synthetic mimics on 3′-UTR-ET-1-luciferase activity. HMEC cells were transfected with wt pGL3-3′-UTR-ET-1 luc reporter along with indicated miRNA mimics, followed by PlGF treatment for 6 h. (D) Effect of mutation of MRE sites for miR-301a/miR-454 in wt 3′-UTR-ET-1 luc. The sequences of predicted miR-301a-/miR-454-binding sites within ET-1 3′-UTR are shown in panel A. The bases in bold font indicate seed sequences of miR-301a/miR-454 and the base substitutions created in the corresponding MRE sequences are indicated by asterisks in panel A. HMEC were transfected with wild type ET-1 3′-UTR-luc or the indicated ET-1 3′-UTR mutant constructs (M1 or M2) along with either synthetic miR-301a or miR-454. At 24 h post-transfection, cells were treated with PlGF for 6 h. Cells were lysed in reporter assay buffer for assay of luciferase activity and data were normalized for Renilla activity. Results shown are means±S.D. of three independent experiments. ***P<0.001, **P<0.01, *P<0.05, nsP>0.05. (E) Effect of synthetic miR-301a and miR-454 mimics on PlGF-induced secretion of ET-1 from HMEC. HMEC were transfected with synthetic miR mimics (90 pmol). At 24 h post-transfection, mimic treated and control cells were treated with either PlGF or fenofibrate for 24 h, as indicated. The cell culture media were assayed for secreted ET-1 by ELISA and total protein content of cell lysates was determined. The data are expressed as relative release of ET-1 from HMEC cells. Data are means±S.D. of three independent experiments. (F) Effects of PPAR-α agonist (fenofibrate) and antagonist (GW6471) on ET-1 protein expression in HMEC cells. Densitometric analysis showing relative density values of ET-1 protein normalized to β-actin protein as a loading control, are indicated above each lane. Data are representative of two independent experiments.
In order to clearly establish the relationship between the putative miRNA recognition sites in the ET-1 3′-UTR and miR-301a and miR-454, we mutated both MREs for miR-301a/miR-454 in pGL3-ET-1 3′-UTR-luc. As shown in Figure 3(D), PlGF augmented luciferase activity in the reporter plasmid containing the wt ET-1 3′-UTR (Figure 3D, lane 2 compared with lane 1). However, mutation of the MRE site denoted M1 (nt +60/+63) of the ET-1 3′-UTR (shown in Figure 3A), prevented the inhibitory effects of exogenous miR-301a and miR-454 on luciferase activity. Similarly, mutation of the MRE site denoted M2 (nt +584/+588) of the ET-1 3′-UTR, resulted in attenuation of PlGF-induced luciferase activity (Figure 3D, lanes 7 and 8 compared with lane 6). These data showed that both MREs in the 3′-UTR of ET-1 mRNA were required for functional effects of miR-301a and miR-454.
To determine whether miR-301a and miR-454 reduced ET-1 protein synthesis via interaction with the 3′-UTR of ET-1 mRNA, we measured the secretion of ET-1 protein from HMEC cells. As shown in Figure 3(E), PlGF treatment of HMEC resulted in ∼2-fold increase in the secretion of ET-1 protein. Transfection of HMEC with exogenous miR-301a or miR-454 mimic reduced PlGF-mediated ET-1 secretion to the basal level (Figure 3E, lanes 3 and 4 compared with lane 2).
As shown above, fenofibrate increased the expression of miR-301a and miR-454 by inducing transcription of SKA2, accordingly we examined its effect on ET-1 secretion. Fenofibrate treatment of HMEC reduced PlGF-induced ET-1 secretion by ∼80% (Figure 3E). The effect of fenofibrate on ET-1 synthesis was due to reduced mRNA translation as demonstrated by Western blot. The effect of fenofibrate on ET-1 synthesis was reversed by GW6471, a PPAR-α antagonist (Figure 3F). Taken together these data showed that increased levels of miR-301a and miR-454 decreased expression of ET-1, induced by PlGF.
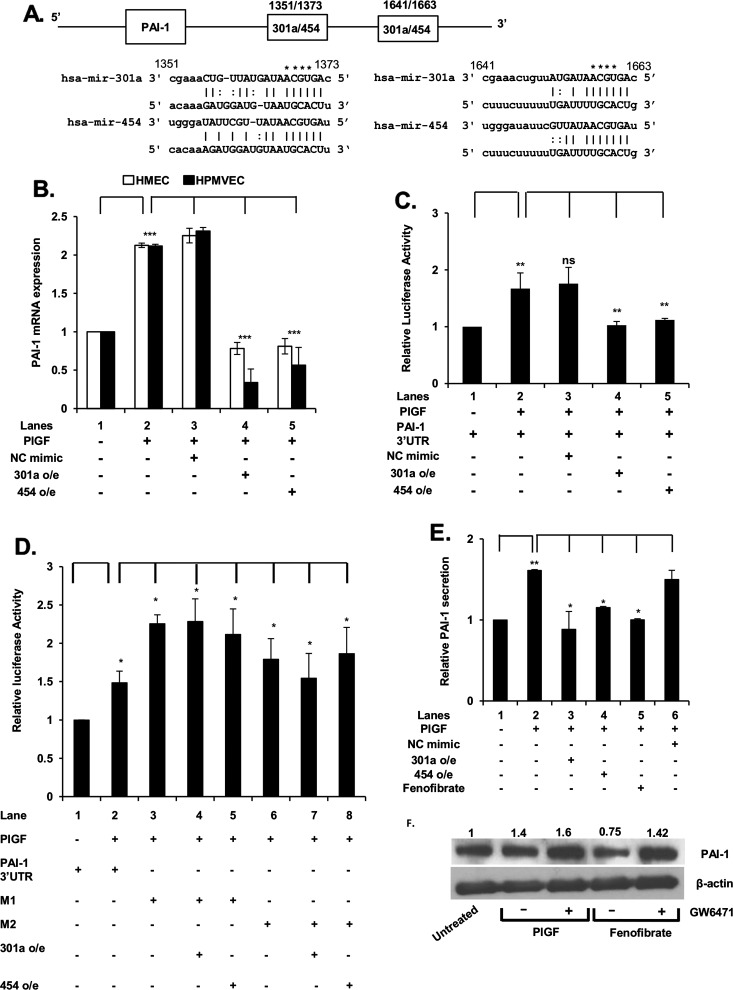
miR-301a and miR-454 target the 3′-UTR of PAI-1 and effect a decrease in PAI-1 mRNA and protein levels
In silico analysis of the 3′-UTR of PAI-1 mRNA showed the presence of miR-301a/miR-454 recognition elements at nt +1351/+1373 and at nt +1641/+1663 as depicted in the schematic of Figure 4(A). Thus, we examined the effects of exogenous miR-301a and miR-454 on PlGF-induced PAI-1 mRNA levels in both HMEC and HPMVEC. As shown in Figure 4(B), transfection with miR-301a and miR-454 mimics in HMEC and HPMVEC reduced PlGF-induced PAI-1 mRNA to basal level and below basal level, respectively. Transfection with control NC mimic had no effect on PlGF-mediated PAI-1 mRNA levels (Figure 4B, lane 3 compared with lane 2). Next, we examined binding of miR-301a and miR-454 to their target sequences in the PAI-1 3′-UTR of pGL3-PAI-1-3′-UTR reporter in response to PlGF. Upon co-transfection of pGL3-PAI-1-3′-UTR- with exogenous miR-301a or miR-454 mimics, there was ∼90% decrease in luciferase activity, compared with PlGF-treated cells (Figure 4C, lanes 4 and 5 compared with lane 2). These data showed that both miR-301a and miR-454 target the 3′-UTR of PAI-1 mRNA to attenuate PAI-1 translation.
Figure 4. miR-301a and miR-454 target the 3′-UTR of PAI-1 mRNA.
(A) Schematic of 3′-UTR of PAI-1 mRNA showing locations of MRE for miR-301a and miR-454. (B) Effect of miR-301a and miR-454 synthetic mimics on PlGF-mediated PAI-1 mRNA expression. HMEC and HPMVEC cells were transfected with synthetic miR-301a mimic (90 pmol), miR-454 mimic (90 pmol) or control (NC mimic) as described in Figure 3 legend. (C) Effect of miR-301a and miR-454 synthetic mimics on 3′-UTR-PAI-1-luciferase activity. (D) Effect of mutation of MRE sites for miR-301a/miR-454 in wt 3′-UTR-PAI-1 luc. The sequences of predicted miR-301a-/miR-454-binding sites within PAI-1 3′-UTR are shown. The bases in bold font indicate seed sequences of miR-301a/miR-454 and the base substitutions in the MRE sequences are indicated by asterisks in panel A. HMEC were transfected with wild type PAI-1 3′-UTR-luc or the indicated PAI-1 3′-UTR mutant constructs (M1 or M2) along with either miR-301a or miR-454. Cells were lysed in reporter assay buffer for assay of luciferase activity and data are normalized for Renilla activity. Results are means±S.D. of three independent experiments. ***P<0.001, **P<0.01, *P<0.05, nsP>0.05. (E) Effect of synthetic miR-301a and miR-454 mimics on PlGF-induced secretion of PAI-1 from HMEC. The data are expressed as relative secretion of PAI-1 from HMEC cells. Results are means±S.D. of three independent experiments. (F) Effects of PPAR-α agonist (fenofibrate) and antagonist (GW6471) on PAI-1 protein expression in HMEC cells. Densitometric analysis of PAI-1 protein expression with values normalized to β-actin as a loading control are indicated above each lane. Data are representative of two independent experiments.
Next, we examined whether mutation of MRE sites for miR-301a/miR-454 in pGL3-PAI-3′-UTR affected reporter activity with exogenous miR-301a and miR-454. As shown in Figure 4(D), exogenous PlGF augmented wt PAI-1 3′-UTR reporter luciferase activity (Figure 3D, lane 2 compared with lane 1). However, mutation of the MRE sites located at nt +1367/+1370 (M1) and at positions +1657/+1660 (M2) of the PAI-1 3′-UTR (see schematic in Figure 4A) in the luciferase reporter gene, prevented either exogenous miR-301a or miR-454 from negatively affecting luciferase activity (Figure 4D). These data showed that both MRE sites were effective functional targets in the 3′-UTR of PAI-1 mRNA for miR-301a and miR-454.
We extended our study of miRNA effects on PAI-1 synthesis to determine whether miR-301a and miR-454 affected PlGF-induced PAI-1 protein expression, as reflected by changes in PAI-1 secretion from HMEC. As shown in Figure 4(E), PlGF treatment of HMEC resulted in ∼1.8-fold increase in the secretion of PAI-1 protein. Transfection of HMEC with exogenous miR-301a or miR-454 mimic attenuated PlGF-mediated PAI-1 protein release to the basal level (Figure 4E, lanes 3 and 4 compared with lane 2).
In an effort to induce endogenous miR-301a and miR-454, fenofibrate treatment of HMEC augmented the endogenous expression of miR-301a and miR-454 and subsequently reduced the secretion of PlGF-induced, endogenous PAI-1 by ∼90% (Figure 4E). This effect was not due to inhibition of secretion but was indeed due to decreased PAI-1 synthesis as shown by Western blot analysis of whole cell lysates. Fenofibrate attenuated PAI-1 protein expression whereas GW6471, a PPAR-α antagonist, reversed the effect of fenofibrate on PAI-1 protein synthesis (Figure 4F). The sum of these studies showed that miR-301a and miR-454 could be induced in situ by fenofibrate to antagonize PlGF-induction of PAI-1 synthesis and secretion. The effect of these miRNAs was elaborated through their interaction with the 3′-UTR of PAI-1 mRNA.
miR-454 expression in vivo
We previously demonstrated miR-301a levels are depressed in SCD subjects compared with matching controls [24]. As we show in this report, miR-454 is also functional as a post-transcriptional regulator of PAI-1 synthesis and co-synthesized with miR-301a, consequently it was necessary to establish that miR-454 levels paralleled miR-301a in both normal and in SCD.
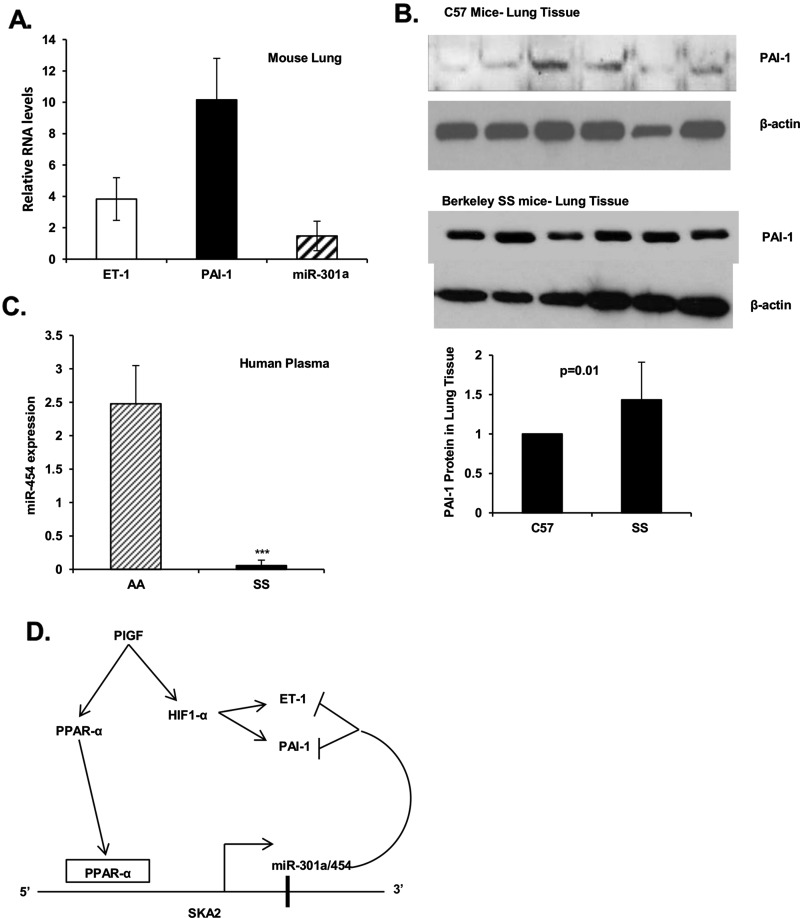
We examined miR-301a expression in lungs from BK-SS sickle mice and control C57BL/6NJ mice. Mice do not have an orthologue for human miR-454, although the location of miR-301a is syntenic between human and mouse. We previously showed that miR-301a is depressed in plasma from BK-SS mice [24]. We extended this observation by examining the expression of PAI-1 and miR-301a in mouse lung. As shown in Figure 5(A), miR-301a expression in lung tissue from BK-SS mice compared with control mice was not significantly different. As a model for PH, the BK-SS mice also expressed higher levels of ET-1 and PAI-1 mRNAs and proteins as shown in Figures 5(A) and 5(B), respectively. These results were further extended in human subjects, wherein miR-454 in plasma of SCD patients was also reduced significantly in comparison with levels determined in control subjects (Figure 5C). These results extended our previous observation that plasma from SCD patients showed decreased expression of miR-301a with correspondingly higher levels of PAI-1. Furthermore, these results demonstrated that miR-301a and miR-454 are indeed co-regulated in SCD and undergo down regulation by an as yet unidentified process. Thus co-regulated reduction in miR-301a and miR-454 appears to significantly contribute to the observed increase in ET-1 and PAI-1 seen in SCD.
Figure 5. Expression of miR-301a and miR-454 in lung tissues of BK-SS and SCD human subjects.
(A and B) Frozen lung tissue samples (−80°C storage) from BK-SS mice (n=6) and control C57BL/6NJ mice (n=6) were sliced and homogenized directly in RNA extraction buffer or protein cell lysate buffer. (A) Extracted RNA was analysed for ET-1 and PAI-1 mRNA expression by qRT-PCR utilizing primers indicated in Table 1. The data were normalized to GAPDH as internal control. miRNA was isolated from lung tissues using miRNA isolation kit, followed by PCR analysis. miRNA levels were normalized to internal reference 5S rRNA. The data are expressed as relative RNA levels in BK-SS mice compared with control mice. (B) Western blots of cell lysates of lung tissue from BK-SS and control C57BL/6NJ mice utilizing ET-1 and PAI-1 antibodies. Gel lanes correspond to individual animals. Lower panel, combined densitometric quantitation of PAI-1 expression in sickle (BK-SS) compared with control animals (C57). (C) miR-454 expression in plasma of SCD subjects compared with sibling controls (n=10). (D) Working model of PlGF induced transcription of SKA2 transcription unit, encompassing intronic miR-301a/miR-454, by activation of PPAR-α and binding to the 5′-flanking region of the SKA 2 promoter. miR-301a/miR-454 target the 3′-UTR of ET-1 mRNA and the 3′-UTR of PAI-1 mRNAs leading to reduction in corresponding ET-1 and PAI-1 levels. The reduced expression of miR-454 in SCD will lead to increased ET-1 and PAI-1 expression.
DISCUSSION
Our previous studies show higher circulatory levels of PlGF in the BK-SS model and SCD patients are associated with increased levels of plasma ET-1 and other markers of PH, including PAI-1 [6]. We previously showed that expression of ET-1 and PAI-1 was transcriptionally regulated by HIF-1α, independent of hypoxia [8,23]. Our studies also show PlGF attenuates the expression of miR-30c and miR-301a in cultured endothelial cells, both of which target the 3′-UTR of PAI-1 under basal conditions [24]. Although extensive biochemical reagents and computational tools based on public data sets are available for identification of specific mRNA gene targets by miRNAs, there is a dearth of information describing transcriptional regulation of miRNA genes in the scheme of post-transcriptional regulation of gene expression [29–31].
The transcription factor Twist-1 regulates expression of the miR-199a2/miR-214 cluster during development of specific neural cell populations in mouse embryogenesis [32]. Recently, we showed this miRNA cluster is also transcriptionally regulated by PPAR-α [25]. miR-199a2 targets the 3′-UTR of HIF-1α mRNA; increased expression of the former reduces transcription of hypoxia and stress-related genes. We demonstrated that PPAR-α agonists induced transcription of the miR-199a2/miR-214 cluster leading to down-regulation of HIF-1α levels, manifested by significant decreases in HIF-1α-dependent gene transcription. Together this work clearly demonstrated that this miRNA cluster is subject to differential regulation in response to changes in physiological conditions.
In the present study, we extended our prior report regarding the regulatory activity of miR-301a on PAI-1. The transcriptional regulation of miR-301a was previously examined in the context of PAI-1 synthesis. Additionally a re-analysis of the PAI-1 mRNA showed two additional miR-301a sites in its 3′-UTR. The search algorithm used previously (Microcosm: http://www.ebi.ac.uk/enright-srv/microcosm/cgi-bin/targets/v5/search.pl) predicted the site at nt +422 to +444 [24], but not the miR-301a sites at nt+1351/+1373 and nt +1641/+1663. The latter sites have complementarity to the seed region of miR-301a and were also identified as potential miR-454-binding sites (www.microrna.org). Thus miR-301a and miR-454 comprised a miRNA set which potentially interacted with PAI-1 mRNA. This became of interest because both miR-301a and miR-454 are co-synthesized from the SKA2 transcription unit.
The functional consequence of binding miR-301a and miR-454 to target gene mRNAs ET-1 and PAI-1 was demonstrated by use of synthetic miR-301a and miR-454 mimics. Both miRNAs attenuated PlGF-induced ET-1 and PAI-1 expression in HMEC. The specificity of the interaction between miR-301a and miR-454 and their respective MREs in the 3′-UTR of ET-1 mRNA was established by inclusion of the ET-1 3′-UTR in a luciferase translation reporter. This reporter responded to synthetic miR-301a and miR-454 mimics like endogenous ET-1 mRNA. Mutation of the miR-301a- and miR-454-binding sites in the luciferase translation reporter confirmed the functional interaction between these miRNAs and the 3′-UTR of ET-1 mRNA.
The first intron of SKA2 gene includes genes for miR-301a and miR-454. Ska2 participates in mitotic spindle formation and function during metaphase; it is also important for monitoring aberrant kinetochore assembly during the spindle check point step of mitosis [33]. Although the miRNA genes are in the correct polarity to be part of the SKA2 transcription unit, it was still conceivable that a smaller transcription unit within the intron was responsible for miR-301a/miR-454 synthesis. Our studies showed PlGF coordinately induced the expression of pre-miR-301a, pre-miR-454 and SKA2 mRNA, which was maximal at 4 h followed by complete return to basal level by 8 h. These expression kinetics would be expected for normal expression of this locus from a common promoter. The importance of this level of post-transcriptional regulation is consistent with our previous demonstration that PlGF leads to a reduction in miR-301a and miR-454 expression, thus providing a permissive cell state enhancing the PlGF induction of ET-1 and PAI-1 expression in SCD [6,23].
As further validation of miRNA coexpression with SKA2, we showed that cis-binding elements for PPAR-α and HIF-1α associated with the SKA2 promoter were functionally important for PlGF-induced transcription of the SKA2 gene. This was demonstrated using shRNAs specific for PPAR-α and HIF-1α, which antagonized production of SKA2 mRNA as well as both miR-301a and miR-454. The SKA2 promoter was further examined in a luciferase reporter construct where we showed mutation of the HRE and deletion of the PPAR-α cis-elements rendered the promoter insensitive to induction by PlGF. These transcription factor cis-elements were found to be functional for SKA2 in native chromatin as demonstrated by ChIP assay probes specific for the factor-binding sites in the SKA2 promoter.
The participation of PPAR-α in SKA2 transcription was of particular interest to us because PPAR-α agonists could be useful for induction of the latter gene. We found that fenofibrate treatment of HMEC induced the co-expression of SKA2, the precursors of miR-301a and miR-454 and their mature forms. The effect of this agonist was specific since co-incubation of fenofibrate-treated cells with the PPAR-α antagonist GW6471 prevented induction as reflected by the absence of any increase in SKA2 or miRNA transcription.
The fenofibrate induction of SKA2 and miR-301a/miR-454, leading to attenuation of ET-1 expression in HMEC, may in fact also be assisted by fenofibrate-dependent reduction in HIF-1α expression. Our laboratory previously showed fenofibrate induces transcription of miR-199a2 from the DNM3os locus [25]. The latter gene produces a long noncoding RNA, serving as pri-miRNA for miR-199a2 and miR-214, the transcription of which is subject to trans-activation by PPAR-α. We demonstrated that miR-199a2 targets the 3′-UTR of HIF-1α mRNA for down-regulation, leading to decreased transcription of the ET-1 and PAI-1 genes [25].
The data presented in the present study may explain the physiological effect of chronically high PlGF levels in SCD. PlGF transiently induced miR-301a and miR-454 in HMEC after 4 h, however expression quickly returned to basal levels by 6 h. In other words, SKA2 transcription became refractory to PlGF induction after 6 h by an unknown process preventing sustained transcription of the SKA2 gene. Indeed, SCD patients exhibit abnormally high plasma levels of PlGF and were observed to express lower plasma levels of miR-301a and miR-454. This physiological phenomenon is also observed in the BK-SS model, which exhibits higher plasma levels of PlGF and abnormal levels of ET-1 with other functional markers of PH. Our studies showed that lung tissues from BK-SS mice displayed reduced levels of miR-301a consistent with the observation in human SCD patients. We propose that increased levels of ET-1 and PAI-1, as previously shown, [6] arises from the SKA2 gene becoming transcriptionally inactive upon chronic PlGF exposure. Loss of miR-301a and miR-454 expression would therefore render ineffective a proposed feedback loop controlling ET-1 and PAI-1 levels (Figure 5D).
In conclusion, our studies provided further mechanistic insight into the co-regulation of miR-301a and miR-454 and their relationship to ET-1 mRNA and its translation. The present study, to the best of our knowledge, is the first demonstration that PPAR-α co-regulates the transcription of SKA2, miR-301a and miR-454; the ET-1 mRNA has complementary sites in the 3′-UTR for the seed sequences of these miRNAs. Our studies on the PlGF responsiveness of SKA2 transcription may explain how chronic PlGF expression as observed in human SCD subjects and in the mouse SCD model results in abnormal expression of ET-1 and PAI-1. High level expression of the latter physiological mediators is a significant causal factor in PH [6,23]. These studies also revealed that fenofibrate, a PPAR-α agonist, approved by the Food and Drug Administration for the treatment of dyslipidemia [34] may increase the expression of both miR-301a and miR-454 leading to decreased ET-1 and PAI-1. In fact, fenofibrate has a secondary effect of reducing HIF-1α levels by inducing transcription of miR-199a2, which post-transcriptionally suppresses HIF-1α synthesis [25]. Thus our studies provide a mechanistic basis for fenofibrate-mediated transcriptional regulation of miR-301a and miR-454 in the present study and miR-199a2 [25] as a rational therapeutic approach to attenuate elevated levels of ET-1 and PAI-1 observed in PH of SCD.
Acknowledgments
The content is solely the responsibility of the authors and does not necessarily represent the official views of NHLBI or National Institutes of Health.
Abbreviations
- BK-SS
Berkeley sickle mice
- ET-1
endothelin-1
- HIF-1α
hypoxia-inducible factor-1α
- HMEC
human microvascular endothelial cell line
- HPMVEC
human pulmonary microvascular endothelial cells
- HRE
hypoxia response element
- MAP kinase
mitogen-activated protein kinase
- MRE
miRNA recognition element
- NC
negative control
- NO
nitric oxide
- PAI-1
plasminogen activator inhibitor-1
- PH
pulmonary hypertension
- PI3K
phosphoinositide 3-kinase
- PlGF
placenta growth factor
- PPAR-α
peroxisome proliferator-activated receptor-α
- qRT-PCR
quantitative real-time PCR
- SCA
sickle cell anaemia
- SCD
sickle cell disease
- SFM
serum-free medium
- SKA2
spindle and kinetochore-associated protein-2
AUTHOR CONTRIBUTION
Caryn Gonsalves performed all in vitro experiments. Chen Li performed analysis of human plasma and mouse lung RNA levels. Punam Malik designed human and mouse experiments. Vijay Kalra and Stanley Tahara designed experiments, supervised analysis and interpreted data. Caryn Gonsalves, Stanley Tahara and Vijay Kalra wrote and reviewed the manuscript.
FUNDING
This work was supported by the National Heart, Lung and Blood Institute [grant number R01-HL111372]; and the Analytical–Metabolic Instrumentation Core, University of Southern California Research Center for Liver Disease [grant number P30-DK048522].
References
- 1.Gladwin M.T., Barst R.J., Castro O.L., Gordeuk V.R., Hillery C.A., Kato G.J., Kim-Shapiro D.B., Machado R., Morris C.R., Steinberg M.H., Vichinsky E.P. Pulmonary hypertension and NO in sickle cell. Blood. 2010;116:852–854. doi: 10.1182/blood-2010-04-282095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Machado R.F., Gladwin M.T. Pulmonary hypertension in hemolytic disorders: pulmonary vascular disease: the global perspective. Chest. 2010;137:30S–38S. doi: 10.1378/chest.09-3057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gladwin M.T., Sachdev V., Jison M.L., Shizukuda Y., Plehn J.F., Minter K., Brown B., Coles W.A., Nichols J.S., Ernst I., et al. Pulmonary hypertension as a risk factor for death in patients with sickle cell disease. N. Engl. J. Med. 2004;350:886–895. doi: 10.1056/NEJMoa035477. [DOI] [PubMed] [Google Scholar]
- 4.Hsu L.L., Champion H.C., Campbell-Lee S.A., Bivalacqua T.J., Manci E.A., Diwan B.A., Schimel D.M., Cochard A.E., Wang X., Schechter A.N., et al. Hemolysis in sickle cell mice causes pulmonary hypertension due to global impairment in nitric oxide bioavailability. Blood. 2007;109:3088–3098. doi: 10.1182/blood-2006-06-029173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bunn H.F., Nathan D.G., Dover G.J., Hebbel R.P., Platt O.S., Rosse W.F., Ware R.E. Pulmonary hypertension and nitric oxide depletion in sickle cell disease. Blood. 2010;116:687–692. doi: 10.1182/blood-2010-02-268193. [DOI] [PubMed] [Google Scholar]
- 6.Sundaram N., Tailor A., Mendelsohn L., Wansapura J., Wang X., Higashimoto T., Pauciulo M.W., Gottliebson W., Kalra V.K., Nichols W.C., et al. High levels of placenta growth factor in sickle cell disease promote pulmonary hypertension. Blood. 2010;116:109–112. doi: 10.1182/blood-2009-09-244830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Phelan M.W., Faller D.V. Hypoxia decreases constitutive nitric oxide synthase transcript and protein in cultured endothelial cells. J. Cell. Physiol. 1996;167:469–476. doi: 10.1002/(SICI)1097-4652(199606)167:3<469::AID-JCP11>3.0.CO;2-#. [DOI] [PubMed] [Google Scholar]
- 8.Patel N., Gonsalves C.S., Malik P., Kalra V.K. Placenta growth factor augments endothelin-1 and endothelin-B receptor expression via hypoxia-inducible factor-1 alpha. Blood. 2008;112:856–865. doi: 10.1182/blood-2007-12-130567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Reiter C.D., Wang X., Tanus-Santos J.E., Hogg N., Cannon R.O., Schechter A.N., Gladwin M.T. Cell-free hemoglobin limits nitric oxide bioavailability in sickle-cell disease. Nat. Med. 2002;8:1383–1389. doi: 10.1038/nm1202-799. [DOI] [PubMed] [Google Scholar]
- 10.Rybicki A.C., Benjamin L.J. Increased levels of endothelin-1 in plasma of sickle cell anemia patients. Blood. 1998;92:2594–2596. [PubMed] [Google Scholar]
- 11.Hu J., Discher D.J., Bishopric N.H., Webster K.A. Hypoxia regulates expression of the endothelin-1 gene through a proximal hypoxia-inducible factor-1 binding site on the antisense strand. Biochem. Biophys. Res. Commun. 1998;245:894–899. doi: 10.1006/bbrc.1998.8543. [DOI] [PubMed] [Google Scholar]
- 12.Kourembanas S., Marsden P.A., McQuillan L.P., Faller D.V. Hypoxia induces endothelin gene expression and secretion in cultured human endothelium. J. Clin. Invest. 1991;88:1054–1057. doi: 10.1172/JCI115367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sabaa N., de Franceschi L., Bonnin P., Castier Y., Malpeli G., Debbabi H., Galaup A., Maier-Redelsperger M., Vandermeersch S., Scarpa A., et al. Endothelin receptor antagonism prevents hypoxia-induced mortality and morbidity in a mouse model of sickle-cell disease. J. Clin. Invest. 2008;118:1924–1933. doi: 10.1172/JCI33308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Key N.S., Slungaard A., Dandelet L., Nelson S.C., Moertel C., Styles L.A., Kuypers F.A., Bach R.R. Whole blood tissue factor procoagulant activity is elevated in patients with sickle cell disease. Blood. 1998;91:4216–4223. [PubMed] [Google Scholar]
- 15.Nsiri B., Gritli N., Mazigh C., Ghazouani E., Fattoum S., Machghoul S. Fibrinolytic response to venous occlusion in patients with homozygous sickle cell disease. Hematol. Cell. Ther. 1997;39:229–232. doi: 10.1007/s00282-997-0229-7. [DOI] [PubMed] [Google Scholar]
- 16.Ataga K.I., Moore C.G., Hillery C.A., Jones S., Whinna H.C., Strayhorn D., Sohier C., Hinderliter A., Praise L.V., Oringer E.P. Coagulation activation and inflammation in sickle cell disease-associated pulmonary hypertension. Hematologica. 2008;93:20–2617. doi: 10.3324/haematol.11763. [DOI] [PubMed] [Google Scholar]
- 17.Hillery C.A., Panepinto J.A. Pathophysiology of stroke in sickle cell disease. Microcirculation. 2004;11:195–208. doi: 10.1080/10739680490278600. [DOI] [PubMed] [Google Scholar]
- 18.Keeton M.R., Curriden S.A., van Zonneveld A.J., Loskutoff D.J. Identification of regulatory sequences in the type 1 plasminogen activator inhibitor gene responsive to transforming growth factor beta. J. Biol. Chem. 1991;266:23048–23052. [PubMed] [Google Scholar]
- 19.Fink T., Kazlauskas A., Poellinger L., Ebbesen P., Zachar V. Identification of a tightly regulated hypoxia-response element in the promoter of human plasminogen activator inhibitor-1. Blood. 2002;99:2077–2083. doi: 10.1182/blood.V99.6.2077. [DOI] [PubMed] [Google Scholar]
- 20.Arndt P.G., Young S.K., Worthen G.S. Regulation of lipopolysaccharide-induced lung inflammation by plasminogen activator inhibitor-1 through a JNK-mediated pathway. J. Immunol. 2005;175:4049–4059. doi: 10.4049/jimmunol.175.6.4049. [DOI] [PubMed] [Google Scholar]
- 21.Perelman N., Selvaraj S.K., Batra S., Luck L.R., Erdreich-Epstein A., Coates T.D., Kalra V.K., Malik P. Placenta growth factor activates monocytes and correlates with sickle cell disease severity. Blood. 2003;102:1506–1514. doi: 10.1182/blood-2002-11-3422. [DOI] [PubMed] [Google Scholar]
- 22.Brittain J.E., Hulkower B., Jones S.K., Strayhorn D., De Castro L., Telen M.J., Orringer E.P., Hinderliter A., Ataga K.I. Placenta growth factor in sickle cell disease: association with hemolysis and inflammation. Blood. 2010;115:2014–2020. doi: 10.1182/blood-2009-04-217950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Patel N., Sundaram N., Yang M., Madigan C., Kalra V.K., Malik P. Placenta growth factor (PlGF), a novel inducer of plasminogen activator inhibitor-1 (PAI-1) in sickle cell disease (SCD) J. Biol. Chem. 2010;285:16713–16722. doi: 10.1074/jbc.M110.101691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Patel N., Tahara S.M., Malik P., Kalra V.K. Involvement of miR-30c and miR-301a in immediate induction of plasminogen activator inhibitor-1 by placenta growth factor in human pulmonary endothelial cells. Biochem. J. 2011;434:473–482. doi: 10.1042/BJ20101585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Li C., Mpollo M.-S.E.M., Gonsalves C.S., Tahara S.M., Malik P., Kalra V.K. Peroxisome proliferator-activated receptor-α-mediated transcription of miR-199a2 attenuates endothelin-1 expression via hypoxia-inducible factor-1α. J. Biol. Chem. 2014;289:36031–36047. doi: 10.1074/jbc.M114.600775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kim K.S., Rajagopal V., Gonsalves C., Johnson C., Kalra V.K. A novel role of hypoxia-inducible factor in cobalt chloride- and hypoxia-mediated expression of IL-8 chemokine in human endothelial cells. J. Immunol. 2006;177:7211–7224. doi: 10.4049/jimmunol.177.10.7211. [DOI] [PubMed] [Google Scholar]
- 27.Pászty C., Brion C.M., Manci E., Witkowska H.E., Stevens M.E., Mohandas N., Rubin E.M. Transgenic knockout mice with exclusively human sickle hemoglobin and sickle cell disease. Science. 1997;278:876–878. doi: 10.1126/science.278.5339.876. [DOI] [PubMed] [Google Scholar]
- 28.Patel N., Gonsalves C.S., Yang M., Malik P., Kalra V.K. Placenta growth factor induces 5-lipoxygenase-activating protein to increase leukotriene formation in sickle cell disease. Blood. 2009;113:1129–1138. doi: 10.1182/blood-2008-07-169821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Schanen B.C., Li X. Transcriptional regulation of mammalian miRNA genes. Genomics. 2011;97:1–6. doi: 10.1016/j.ygeno.2010.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Xiao Z.-D., Diao L.-T., Yang J.-H., Xu H., Huang M.-B., Deng Y.-J., Zhou H., Qu L.-H. Deciphering the transcriptional regulation of microRNA genes in humans with ACTLocater. Nucleic Acids Res. 2013;41:e5. doi: 10.1093/nar/gks821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Guo Z., Maki M., Ding R., Yang Y., zhang B., Xiong L. Genome-wide survey of tissue-specific microRNA and transcription factor regulatory networks in 12 tissues. Sci. Rep. 2014;4:5150. doi: 10.1038/srep05150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lee Y.-B., Bantounas I., Lee D.-Y., Phylactou L., Caldwell M.A., Uney J.B. Twist-1 regulates the miR-199a/214 cluster during development. Nucleic Acids Res. 2009;37:123–128. doi: 10.1093/nar/gkn920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cao G., Huang B., Liu Z., Zhang J., Xu H., Xia W., Li J., Li S., Chen L., Ding H., et al. Intronic miR-301 feedback regulates its host gene, ska2, in A549 cells by targeting MEOX2 to affect ERK/CREB pathways. Biochem. Biophys. Res. Commun. 2010;396:978–982. doi: 10.1016/j.bbrc.2010.05.037. [DOI] [PubMed] [Google Scholar]
- 34.Lalloyer F., Staels B. Fibrates, glitazones, and peroxisome proliferator-activated receptors. Atertio. Thromb. Vasc. Biol. 2010;30:894–899. doi: 10.1161/ATVBAHA.108.179689. [DOI] [PMC free article] [PubMed] [Google Scholar]