Abstract
Bone defects can originate from a variety of causes, including trauma, cancer, congenital deformity, and surgical reconstruction. Success of the current “gold standard” treatment (i.e., autologous bone grafts) is greatly influenced by insufficient or inappropriate bone stock. There is thus a critical need for the development of new, engineered materials for bone repair. This review describes the use of natural and synthetic hydrogels as scaffolds for bone tissue engineering. We discuss many of the advantages that hydrogels offer as bone repair materials, including their potential for osteoconductivity, biodegradability, controlled growth factor release, and cell encapsulation. We also discuss the use of hydrogels in composite devices with metals, ceramics, or polymers. These composites are useful because of the low mechanical moduli of hydrogels. Finally, the potential for thermosetting and photo-cross-linked hydrogels as three-dimensionally (3D) printed, patient-specific devices is highlighted. Three-dimensional printing enables controlled spatial distribution of scaffold materials, cells, and growth factors. Hydrogels, especially natural hydrogels present in bone matrix, have great potential to augment existing bone tissue engineering devices for the treatment of critical size bone defects.
Introduction
Bone defects result from a wide variety of pathologies, including osteoporosis, cancer, reconstructive surgery, congenital deformity, and traumatic injury. Bone healing in sub-critical size defects proceeds via a strictly regulated cascade of events (Figure 11) that can be divided into three separate stages: the early inflammatory stage, the repair stage, and the late remodelling stage.2 Early phases are characterized by the formation of a hematoma and infiltration by inflammatory cells. These cells induce migration of osteoblasts to the injury site and stimulate a structurally unorganized cellular response that is not capable of supporting a load or protecting internal organs. This new bone is then remodelled to the final bone structure via osteoclasts and macrophages. Unfortunately, healing can be impaired by a number of factors, including poor blood supply, associated soft-tissue injury, extensive bone loss, and infection.3 In cases of a critical size defect,4, 5 unassisted repair may not be possible.2 As many large bone defects are caused by age related pathologies (i.e., osteoporosis, cancer), demand for methods of large area bone repair will increase as the population ages.
Figure 1.
The Bone Healing Process. Upon the fracturing of a bone (A), blood vessels are severed allowing for the creation of a blood clot, or hematoma, within the bone cavity (B). As the blood clot breaks down (C), granulation tissue forms, allowing angiogenesis to occur within the injured area. Meanwhile, the periosteum of the healthy bone replicates and transforms into chondroblasts, creating a cartilaginous scaffold within the cavity (D). The next phase begins as the process known as endochondral ossification transforms the cartilaginous tissue into trabecular bone matrix (E). Once the cartilage callus has been transformed into laminar bone (F), the bone remodelling process begins to transform the outer laminar bone into compact bone. Image modified, with permissions, from Lissenberg-Thunnissen, S. N. et al., Int Orthop, 2011, 1271.
The current gold standard for large bone defect repair is an autologous graft from a donor site, such as the iliac crest of the pelvis. Allogeneic bone grafting is now rare because it can result in disease transmission or rejection, while autologous grafts have several limitations. Bone graft harvesting procedures can result in donor site morbidity (i.e., in up to 15% of patients6), and there are limitations to the size and shape of donor material. Not all autografts are suitable for targeted repair sites, especially in the case of irregularly shaped defects, such as in the pelvis, spine, head, and neck. Further, the distribution of cortical bone in donor material is not always optimal for the transplant site.7, 8 Autologous grafting is associated with the risks of pain at the donor site and resorption of the graft. The supply of allograft bone is often limited, such as in the traumatically wounded, amputees, and those with bone pathologies (e.g., bone formation deficit, bone cancer, or congenital malformations). Alternative strategies to enhance treatment of large area bone defects are thus needed. Promising strategies have been developed that use engineered materials, including hard and soft biomaterials for bone tissue engineering.
Bone Matrix Mimetics
Bone matrix mimetics are designed to support bone regeneration when autologous graft materials are not available or not suitable. Mimetic scaffolds should ideally be biocompatible, osteogenic, osteoinductive, and/or osteo-conductive, meaning that they should support differentiation of cells into osteoblasts that can form bone, induce progenitor cells to form bone, or support ingrowth of existing osteoblasts that can form new bone needed to repair the injury site and allow vascularization.9 Scaffold porosity is critical to support these functions.10 The presence of interconnected pores allows for endogenous cells, such as bone progenitor or endothelial cells, to migrate into the scaffold, permit transport of nutrients, waste removal, and the ingrowth of blood vessels and nerve.11-14 More specifically, a minimum pore size of ~ 100-150 microns is required for bone formation,11, 15 whereas vascularization requires pore sizes of at least 300 microns.15-17 Extracellular matrix (ECM) production of cell-seeded solid scaffolds is also affected by pore size, with larger pores (~400 microns in a PDLLA scaffold) leading to a well-organized collagen network.18 High pore volumes also increase permeability of nutrients throughout the scaffold; increasing bone regeneration and blood vessel infiltration.13 However, balancing the percent of void volume available for cell infiltration with the mechanical integrity of the scaffold can be challenging.
In addition, bone tissue engineering scaffolds are usually expected to be resorbable and to guide incoming progenitor and vascular cells until neotissue has formed.19 Tuning the degradation rate of the matrix may be the most crucial variable in the development of bone tissue engineering scaffolds. There is substantial disagreement over the appropriate rate of scaffold resorption with suggested values between 2-3 weeks, after initial development of neobone, to suggestions that resorption should be delayed until regeneration is complete (i.e., ~ 3-6 months).9 However, there is general agreement that a degradation rate faster than the rate of cellular infiltration will cause union failure. Similarly, a degradation rate slower than the rate of infiltration may prove antagonistic to new bone formation, increasing the risk of graft failure. Furthermore, it may be desirable to tailor degradation rates to allow for controlled release of growth factors and/or drugs.20 Optimizing these properties to obtain scaffolds that can mechanically and biologically support regeneration until they are no longer needed is the great challenge of bone tissue engineering.
Materials Used as Bone Mimetics
Various materials have been explored as bone tissue matrices, including metals, ceramics, polymers, and their combination. Metals such as titanium, stainless steel, and cobalt-chromium provide both biocompatibility and strength. However, metals usually have a much higher modulus than native bone, which can cause stress shielding (i.e., mechanical bypass of loads around the implant) and can result in bone resorption. Metals also do not generally biodegrade, which may necessitate additional surgery and potentially impede reparative tissue growth, especially in children whose bones have not yet reached mature size.21, 22 Ceramic implants are mainly comprised of calcium phosphates (CaPs) because of their prevalence in native bone tissue,23, 24 with hydroxyapatite (HA) and tricalcium phosphate (TCP), as well as a composite comprised of both substances and known as biphasic calcium phosphate (BCP), being the most commonly employed. Unfortunately, ceramic implants are prone to brittleness and may display inappropriate degradation rates. One of the greatest challenges with both metals and ceramics is tuning the resorption rate.
Polymeric scaffolds have also been of great interest because of their biocompatibility and biodegradability. Amongst the most common natural polymeric scaffolds investigated are collagen, fibrin, alginate, and hyaluronic acid, which are typically employed in hydrogel form. However, naturally-derived polymers may exhibit pathogenic impurities, limiting their clinical application.19 Synthetic polymers, such as poly(propylene fumarate) (PPF), poly(lactic acid) (PLA), poly(glycolic acid) (PGA), poly(caprolactone) (PCL), and poly(ethylene glycol) (PEG) have also been employed in both hydrogel and solid-cured scaffold forms. These polymers are widely used, have been employed in FDA approved devices,25, 26 and can be designed to degrade via non-enzymatic hydrolysis. Synthetic scaffolds can be created with a variety of programmable features (i.e., porosity, pore size, degradation rate, and mechanical properties) that can be tailored to intended application sites.27-31 However, polymers generally have a lower modulus than either metals or ceramics,32 and thus have been limited in application to areas of low mechanical stress.33 Given the need to precisely design bone tissue engineering scaffold properties, including morphology, resorption rate, osteoconductivity, and osteoinduction, attention has increasingly focused on the development of composites to tune these properties. Composites most closely reflect the natural structure of the bone matrices, which are a combination of organic and inorganic material.
Hydrogels
One promising class of candidate materials that could be used to form such composites are hydrogels, which have been shown to increase angiogenesis and osteoconductivity in bone repair models.34-36 Hydrogels are networked, hydrophilic polymers, typically formed via cross-linking or chain entanglement, that absorb significant amounts of water.37 As such, hydrogels potentially provide a substrate that functions like the collagen component of newly forming bone ECM. As previously mentioned, hydrogels can be derived from either natural (e.g., collagen, gelatin, fibrin, hyaluronic acid, alginate, agarose, and chitosan38) or synthetic (e.g., poly(ethylene oxide), poly(vinyl alcohol), poly(acrylic acid), poly(propylene fumarate-co-ethylene glycol), and polypeptide) materials. Natural polymers offer the advantages of low toxicity and high biocompatibility, and are often derived from components of the mammalian extracellular matrix (e.g., collagen, hyaluronic acid, and fibrin) or marine algae sources (e.g., alginate and agarose). Natural materials are typically cross-linked via chain entanglement, but can be chemically modified to promote crosslinking. Synthetic polymers are chemically synthesized and are usually cross-linked via chemical methods (Figure 239-41), including photo- and thermally-initiated polymerization. In comparison to natural hydrogels, synthetic hydrogels allow for improved control over physical properties, such as cross-linking density, mechanical strength, and enhanced tailoring of chemical and biological responses.42 However, unmodified synthetic materials often lack biological activity.
Figure 2.
Chemical schemes for hydrogel synthesis. (A) Radical polymerization utilizes a radical initiating agent and ultraviolet light to initiate polymerization. In this example, poly(ethylene glycol)-dimethacrylate (PEG-DMA) utilizes a radical producing curing agent to polymerize the hydrogel via methacrylate groups. (B) Polymerization through “click” mechanisms allows for dipolar cycloaddition, or Huisgen reaction, to occur between azido and alkyne groups in aqueous solutions. In this example, hyaluronic acid (HA) was modified using (1-ethyl-3-(3-dimethylaminopropyl)carbodiimide hydrochloride) (EDC) to attach either an azide or alkyne functional group. Addition of the modified HA to a CuCl solution allows for polymerization to occur. (C) Michael addition reactions occur in the presence of a carbanion and an unsaturated carbonyl to create C-C bonds. In this example, poly(ethylene glycol) vinyl sulfone was reacted with free thiol groups located on purified peptides to create functionalized hydrogels. Images modified, with permissions, from Backstrom, S. et al., Materials Sciences and Applications, 2012, 425; Crescenzi, V. et al., Biomacromolecules, 2007, 1844; Lutolf, M. P. et al., Biomacromolecules, 2003, 713.
With regards to natural hydrogel materials in particular, it should be noted that collagen comprises approximately 90% of organic matrix in the bone. Post-translational modification of natural collagen creates extensive crosslinking within the matrix, and assists in the mineralization process; providing much of the structural and mechanical properties of bone.43 Alternatively, hyaluronic acid is another major component of connective tissue, though less prominent in bone. Whereas its function in bone ECM is not well understood, hyaluronic acid plays a role in wound healing and cell migration.44 Thus, these two materials are potential candidates for bone tissue engineering.
Hydrogels can be manufactured with a range of mechanical properties tailored to the healing process for specific tissue types45, and can be used to support cell culture both within the gel and on the gel surface.46 Additionally, hydrogels can be patterned using several approaches to more closely mimic tissue microanatomy.47, 48 As such; hydrogels have been used extensively in tissue engineering. However, most hydrogels are soft materials, with elastic moduli ranging from ~kPa to MPa, whereas native bone has moduli of ~ 1-27 GPa.49 Thus, hydrogel implementation in bone tissue engineering has been limited compared to other tissues.42 Mechanical properties of hydrogels can be modified for use in bone regrowth by adjusting the number of cross-links, type of monomer, and the local environment (e.g., swelling).50 However, the formation of composites that combine hydrogels with stronger materials already used in bone tissue engineering, such as bone cements, is more commonly performed51. (For more detailed synthetic approaches to such materials please see D’Este et al.52 and Geffers et al.53 These materials are commonly composited with collagen, hyaluronic acid, or polysaccharide hydrogels, whose syntheses and composite formation are described in more detail in Ferreira et al.54, Xu et al.55, and Khan et al.56, respectively.)
In addition to cell culture and tissue engineering, hydrogels are attractive candidates for bone tissue engineering because of their capability for controlled release of drugs and soluble factors.57 Hydrogel drug release can be controlled by hydrolytic degradation,58 degradation by native enzymes produced in the microenvironment59 (e.g., matrix metalloproteases or MMPs), or through release in response to a rapid physiological change. The latter type of hydrogels, are known as “smart” hydrogels. Smart hydrogels include thermo-responsive materials (e.g., poly-(N-isopropyl acrylamide) (pNIPAAm)60) that collapse at a temperature near physiological,61 altering release at temperatures near the lower critical solution temperature (LCST), and pH-sensitive materials (e.g., poly(acrylic acid) (PAA))62 that swell and contract in response to changes in the local charge environment.
Hydrogel Scaffolds for Bone Tissue Engineering
Some of the earliest work using hydrogels for bone tissue engineering examined chitosans, linear polysaccharides that can form hydrogels through chain entanglement or chemical cross-linking.63 This was followed by work in other natural systems, such as collagen, hyaluronic acid,64-66 and synthetic polymers67-69 that could be modified to improve controlled release and cytocompatibility. These initial systems demonstrated good biocompatibility and ability to induce bone formation. To improve osteogenic and osteoinductive properties, hydrogels have been modified with peptides, most notable the arginine-glycine-aspartic acid (RGD) motif, which is the primary peptide sequence involved in integrin-extracellular matrix binding.70 For example, alginate hydrogels modified with the RGD peptide demonstrated increased osteoblast adhesion and spreading compared to control, unmodified hydrogels (Figure 371). There was also a direct correlation between ligand density and cell proliferation, and improved in vivo bone formation was observed in a mouse model. Similarly, the RGD sequence was also used to modify oligo(poly(ethylene glycol) fumurate) (OPF) hydrogels, which contain repeating units of PEG and fumaric acid.72 PEG and poly(propylene fumarate) (PPF), a fumaric acid analog, have been individually used as bone tissue engineering scaffolds, and hydrogel composites of these materials are degradable through ester hydrolysis of the PEG-fumaric acid bond. However, this study showed limited efficacy of peptide modfication in vivo. Given that peptide density and spacing all likely contribute to tissue response, these variables must be optimized in any modification approach. There have also been attempts to modify hydrogels with mineralizing agents.73, 74 For example, poly(2-hydroxy etheyl methacrylate) (pHEMA) was modified with alkaline phosphatase via a copolymerization technique to yield composites that permitted mineral deposition within ~ 2 weeks.73 These materials had biomimetic properties that mimic features of matrix vesicles in bone and cartilage that participate in bone mineralization.
Figure 3.
Osteoblasts demonstrate little attachment to unmodified alginate hydrogels (A), but preferentially attach to alginate hydrogels modified with the RGD peptide (B). Image modified, with permissions, from Alsberg, E. et al., Journal of Dental Research, 2001, 2025.
Whereas hydrogel scaffolds demonstrate success in vitro, in terms of promoting adhesion and differentiation of bone cells, most hydrogels do not maintain sufficient mechanical integrity for independent use in load bearing sites. Therefore, there has been substantial interest in forming composites of hydrogels with other materials. An obvious first approach is to composite hydrogel materials with each other, such as early work examining collagen-hyaluronate composites.64 These materials demonstrate the synergy that composites can provide in terms of chemical properties, as composites of collagen-hyaluronate showed greater osteoconductivity than either material independently. Complexation with other, more rigid polymeric constructs, such as electrospun fiber meshes, can be used to provide a template for tissue regeneration and improve structural rigidity.75, 76
However, to enhance mechanical properties, the most popular approach has been complexation with ceramics. Hydrogels have been complexed with calcium phosphates,77 fumed silica nanoparticles,78 bioactive glass nanoparticles,79 and nano-hydroxyapatite.80-85 Hydroxyapatite (HA), a naturally occuring calcium mineral found in bone, is by far the most popular complexing ceramic agent. Complexation of hydrogels, such as collagen with HA, has been shown to promote bone growth and resorbtion by osteoclasts, similar to autografted bone.84 Hydrogel-HA complexes also demonstrate improved mechanical properites, as well as processability over that of individual materials.84, 86-88 For example, PEG-PCL-PEG/collagen/HA “smart” hydrogel composites can be created that are injectible at room temperature, yet thermoset near physiological temperature.88 Other nano-ceramics, such as bioactive glasses,79 show similar benefits when complexed with hydrogels (Figure 479). Hydrogels provide an injectable carrier that permits targeted delivery, whereas ceramics provide bioactivity and mineralization promoting properties.
Figure 4.
Scanning electron microscopy shows that bioactive glass nanoparticles incorporated into chitosan hydrogels support the formation of apatite over time: (a) 0 days (control), (b) 3 days, (c) 7 days and (d) 14 days. Image modified, with permissions, from Couto, D. S. et al., Acta Biomaterialia, 2009, 115.
In addition to mechanical properties, complexation can influence the nanostructure of the hydrogel, with concomittant changes in cell response. For example, the addition of fumed silica nanoparticles to pHEMA composites yielded an increase in cell proliferation that was not observed with a similar concentration doping of microparticles.78 Osteoblasts cultured on the composites also exhibited a spread morphology, similar to that found in vivo, as opposed to the rounded morphology observed on pHEMA alone (Figure 578). Similarly, Zhang et al., in a series of papers,89, 90 demonstrated the importance of nanostructure in composites containing rosette nanotubes based on DNA based pairing interactions that self-assemble in solution to form three-dimensional (3D) structures. Nanotubes modified to display the RGD cell binding sequence and complexed with pHEMA demonstrated increased osteoblast adhesion and proliferation compared to controls without nanostructure. This material was then further modified with nano-hydroxyapatite, which further enhanced cell adhesion.
Figure 5.
Human osteoblasts show increased adhesion and spreading on pHEMA surfaces modified with fumed silica, as seen under scanning electron microscopy 24 h after osteoblast plating: (A) pHEMA, (B) pHEMA + 10% fumed silica, (C) pHEMA + 23% fumed silica (Mag: 12,000X). Image modified with permissions from Schiraldi, C. et al., Biomaterials, 2004, 3645.
Hydrogels for controlled release
In addition to their properties as 3D scaffolds, another attractive advantage of using hydrogels in tissue engineering constructs is their wide spread use as drug delivery vehicles. Drug delivery via hydrogel can be tailored to occur instantaneously (i.e., triggered by an external signal) or over long time periods, in contrast to intravenous or direct injection. Since the pivotal studies of Urist in 1965,91 several growth factors have been identified as important contributors to the bone regeneration process that would be logical candidates for drug release via hydrogel, including bone morphogenetic proteins (BMPs), transforming growth factor-beta-1 (TGF-β1), and fibroblast growth factor (FGF). BMPs, members of the TGF-β super family, are the most extensively studied factors for delivery. BMPs have been linked to bone healing, with BMP-2, 4, and 7 demonstrating the ability to differentiate progenitor cells toward an osteoblast lineage.92 Native BMPs are produced by osteoprogenitor and osteoblast cells. TGF-β1 is expressed in both mature and regenerating bone, and its expression is increased by mechanical loading.93 In the bone regrowth process, TGF-β1 is believed to be released by clot forming platelets and to stimulate cell proliferation.92 However, its role in osteoinduction is uncertain, potentially requiring high doses. FGF encourages cell proliferation and also angiogenesis, important components of the bone healing process, and is expressed by osteoblasts. In addition to these growth factors, there has been interest in controlled release of other molecules, such as anti-inflammatory drugs to combat the foreign body response to bone implants94-96 and to modulate the critically important inflammation phase of the regeneration process.97
Early work in the area of bone tissue engineering controlled release focused primarily on gelatin/collagen composites. Gelatin is a hydrolyzed form of the collagen protein, and the popularity of both materials stems from the fact that collagen nanofibers comprise portions of native bone.89 Gelatin/collagen composites have been used to release BMPs98, 99, FGF100 (Figure 6100), and TGF-β1101, as well as anti-inflammatory compounds102. These constructs demonstrated improved bone formation in vivo compared to hydrogels not releasing factors or factor addition alone,98-101 with drastically improved pharmacokinetic profiles compared to injected factors. For example, BMP was present in hydrogels even after 30 days, whereas injected solution was cleared from the body within 24 hours.99
Figure 6.
After 12 weeks, 6 mm rabbit, cranial defects were analysed via histology after treatment with: (A) PBS, (B) gelatin hydrogel, (C,D) 100 μg of free β-FGF, (E,F) β-FGF-incorporating gelatin hydrogel. Incorporation of a β-FGF gelatin hydrogel shows an increase of infiltrative osteoblasts, as well as new bone formation. B=bone, DM=duramater, C=connective tissue, NB=new bone, OB=osteoblast. (A, B, C and D; ×40, E and F; ×400) Image modified, with permissions, from Tabata, Y. et al., Biomaterials, 1998, p.807.
In addition to gelatin/collagen, hyaluronic acid, a native component of bone and tissues44, has been used as a carrier for factors. Unmodified hyaluronic acid hydrogels are generally non-permissive to cell adhesion, but combination with released growth factors can encourage bone matrix formation.103, 104 Hyaluronic acid can also be complexed with other polymers, such as poly(vinyl alcohol) to yield injectable systems, with the potential to fill non-uniform gaps.105 Other materials investigated for controlled release include peptide amphiphiles,106 non-native peptide sequences that self-assemble in solution, and thus can be designed in injectable form, and synthetic hydrogels, such as photo-cross-linked PEG.68 Like hyaluronic acid, PEG is generally not supportive of cell adhesion, but combination with growth factor delivery can increase bone formation and mineralization. Importantly, photo-encapsulated growth factors maintain viability throughout the photo-encapsulation process.68
One of the most critical elements in the design of hydrogels for controlled release in bone tissue engineering is the balance between the rate of factor elution and the rate of gel degradation.100 Most hydrogels release factors via controlled degradation, typically via ester hydrolysis,58 the rate of which can be tuned to offer factor elution over days to months. However, the ideal degradation rates for scaffold dissolution and factor release often differ. Scaffolds that degrade too quickly fail to provide adequate support for bone growth; scaffolds that degrade too slowly prevent proper infiltration of regenerating bone. Degradation rates of up to 12 weeks have shown little influence on bone infiltration.107
Degradation rate can be influenced by the local environment, particularly for natural hydrogels.101 For example, 95 wt% gelatin hydrogels containing TGF-β1 and implanted in a rabbit cranial defect degraded completely within six weeks compared to control hydrogels containing no TGF-β1, which were still intact. This most likely resulted from the production of proteases released by the activated cells surrounding the implant. It was also observed that intermediate degradation rates were ideal for bone regrowth, consistent with the needs for prolonged factor delivery and scaffold degradation rates rapid enough to permit bone regrowth. However, factors themselves may modulate healing rates, with increased factor release accelerating healing and reducing the time of scaffold integrity needed. For example, Patterson et al.108 showed that hydrogels that degraded rapidly, and therefore released factors at higher initial doses, showed good bone regrowth despite rapid loss of scaffold integrity. Control of degradation can be enhanced using mechanisms other than ester hydrolysis for gel degradation. For example, in an attempt to match physiological regrowth, MMP-cleavable substrates have been incorporated directly into the hydrogel matrix.109 MMPs are naturally secreted enzymes that degrade proteins, such as collagen, to permit tissue regeneration and remodeling. Thus, MMP-cleavable substrates should degrade according to the rate of tissue regeneration, permitting biological control of scaffold degradation.
Another approach is to decouple degradation and drug release rates through the use of a two-material system. For example, incorporation of drug-eluting microspheres within hydrogel composites permits independent modulation of release rates through the choice of microsphere carrier, while permitting separate tuning of the degradation of the scaffold material.110, 111 Further, there is some evidence that encapsulation may preserve factor biological activity over solution phase, most likely by protecting factors from degraditory stimuli in the environment.110 Release from these systems can occur through diffusion across both material phases or be dynamically altered through the use of smart hydrogels. For example, dextran/gelatin hydrogels containing Dextran/PEG microspheres permitted optimization of the LCST in the physiological range.112 Collapsed gels exhibited much slower BMP release than gels at room temperature, suggesting that drug release could be tuned by altering material LCST.
Cellularized Hydrogel Scaffolds for Bone Repair
Hydrogels have been widely used to encapsulate and deliver cells that support natural tissue regeneration. For bone tissue engineering, implanted cells should promote initial stages of bone repair, when the patient is most likely to be deficient in osteogenic growth factors.20 In addition, cells should differentiate into osteoblasts and promote the initial formation of vascular tissue. Stem cells are thus an obvious candidate for bone repair because of their ability to differentiate, and the most commonly investigated cell type is mesenchymal stem cells (MSCs). MSCs are most frequently isolated from bone marrow,113 although adipose-derived stem cells (ADSCs) isolated from collagenase-digested lipo-aspirates114 are also employed. MSCs can differentiate into osteoblasts and other osteogenic cells; however, bone-forming ability decreases significantly as the age of the host increases.32 MSCs can also be expanded in culture; however, this process often takes several weeks, delaying prospective treatment. Finally, most MSCs are cultured in the presence of fetal bovine serum, which poses the risk of an immunologic response. Thus, MSCs have yet to achieve widespread clinical use.9
Initial efforts to deliver cells using hydrogel supports primarily focused on infiltration of cells into existing scaffolds, rather than true encapsulation.65, 115 Encapsulation approaches for bone tissue engineering were introduced by the Anseth group through a series of papers in 2000 and 200267, 116 demonstrating a photo-encapsulation method in acrylated PEG hydrogels. A key finding in this work was that encapsulation did not significantly alter cell viability. Other papers from this group describe the limits of this approach in more detail,117 for example potential cytotoxicity of the cross-linking agent. In addition, the use of additives such as ceramics, common in hydrogel scaffolds, can interfere with the photo-cross-linking process.82
Natural cross-linking approaches have also been employed, for example mesenchymal progenitor cells were encapsulated in fibrinogen hydrogels generated by the addition of thrombin.118 These materials were then introduced to PCL and PCL-HA materials created by fused deposition modeling, a form of 3D printing. Similarly, beta-glycerophosphate, which has osteogenic properties, was used to initiate gelation of chitosan, collagen, and their composite to encapsulate bone marrow derived stem cells.119 Chain entanglement approaches are also popular for natural materials, such as collagen120 and alginate, and can be used to encapsulate cells, as well as ceramic additives.121, 122 Synthetic polyethylene oxide “smart” hydrogels have also been formed via a similar thermo-setting approach and used to encapsulate MSCs, which formed bone upon injection into mice.123 In many of these cases, hydrogels are used to fill solid-cured scaffolds to facilitate bone progenitor or endothelial cell proliferation, migration, attachment, and/or differentiation.
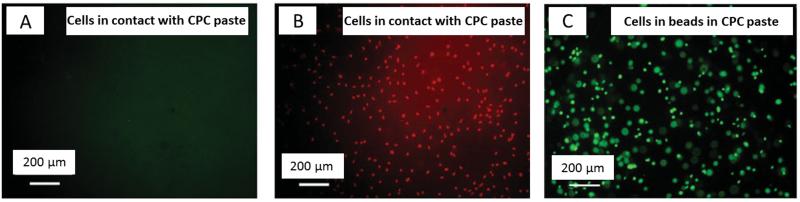
Another common presentation for hydrogels in bone tissue engineering composites is in microstructure form, usually as a bead. Many ceramic materials are not conducive to live cell encapsulation, and the incorporation of cell encapsulating hydrogel microbeads provides a potential solution to this issue. For example, cells cultured in alginate beads were able to sustain osteoblasts in culture, whereas nearly all cells exposed to calcium phosphate cement alone died (Figure 7124). Presentation in bead form also provides a potential means of injectability, permitting conformal filling of the defect shape.125 Culture in microstructure form also takes advantage of the ability of hydrogels to support 3D culture. For example, 3D nanotubes display much more extensive cell proliferation than essentially flat alginate disks, despite being composed of the same concentration alginate solution.126 Similarly, cells embedded in 3D collagen beads demonstrate increased calcium and bone protein deposition compared to cells cultured on the same materials in 2D.127
Figure 7.
Live/Dead staining of MC3T3-E1 cells cultured in the presence of calcium phosphate cement (CPC) show no living cells, in green (A) and extensive cell death, in red (B). Whereas, cells encapsulated within alginate hydrogel beads (C) show a significant increase in cell survival, green. Image modified, with permissions, from Weir, M.D. et al., Journal of Biomedical Materials Research Part A, 2006, 487.
It should be noted that mechanical characteristics of hydrogels, both static45 and dynamic128, can contribute to cell response within the hydrogel, including proliferation, differentiation, and bone forming potential. For example, MSCs subjected to cyclic compression, potentially mimicking natural loading strains experienced during bone repair, increased markers related to bone forming potential over cells cultured in gels without compression.128 Thus, mechanics of the hydrogel support, as well as ability to survive pre-implantation culture, should be considered in designing bone tissue engineering scaffolds.
Combined Delivery Systems
The combination of factor delivery with cell encapsulation in hydrogel supports has yielded some of the most promising data, especially in hydrogels that do not typically support cell culture. For example, alginate scaffolds encapsulating bone marrow stromal cells demonstrated little in growth in a mouse model; however, bone formation was observed in as little as six weeks when cells were delivered with a combination of TGF-β3 and BMP-2.129 Similarly, hyaluronic acid hydrogels cultured with BMP-2 and MSCs demonstrated significantly more bone ingrowth than unmodified hyaluronic acid and either BMP-2 or MSCs alone.34 Importantly, both alginate and hyaluoronic acid demonstrate little cell permissibilty in their unmodified form. Similar results have been seen in non-permissive synthetic hydrogels, such as PEGs. PEG-PCL composites encapsulating MSCs130 and ADSCs131 together with dexamethasone demonstrated greater osteoinductive and osteogenic behavior than gels without factors.
Three-Dimensional Printed Constructs for Bone Tissue Engineering
As with most types of tissue engineering, generating vasculature remains a major challenge in clinical implementation. Successful angiogenesis has been directly linked with enhanced quality of newly formed bone.132 One potential technology to address vascularization, as well as provide the porosity necessary for cell infiltration and bone growth, is the use of 3D printing to create scaffolds with intrinsic, multiplexed structures (Figure 8133). Because of these advantages, and the fact that 3D printed scaffolds can generally be produced and replicated at low cost,134 they have been applied for large gap bone repair.135
Figure 8.
Three-dimensional printing offers great potential for the creation of cell favourable, multiplexed constructs for tissue engineering. (A) Represents a modified stereolithographic printer adapted for multiple materials, while still achieving layer-by-layer deposition through the bottom-up approach. Insets depict a representation of the geometric shapes being created. Fluorescence staining of the encapsulated cells within a PEG-dimethacrylate hydrogel confirms that the multiplexed geometries are maintained during printing: Top-down view (B) and the cross-sectional view (C). Image modified, with permissions, from Chan, V. et al., Lab Chip, 2010, 2062.
Three-dimensional printing was developed in the early 1980’s.136, 137 Though various modalities exist, there are four main printing methods currently employed. Fused deposition modelling,138 utilizes an extruding device to sequentially eject the solid polymer feedstock at high temperature (i.e., above melting temperature) while scanning over the printing surface. Within this subfield, microextrusion printing, which employs a head moving in the x-y-z planes, is the most commonly used. This method generates beads instead of droplets and is therefore able to print high viscosity materials. However, pressures required for extrusion can negatively impact cell viability.139 Stereolithography,140 uses a an external stimulus to initiate polymerization (i.e., ultraviolet light (UV) or a laser) in conjunction with a reaction initiator. This method can create scaffolds with high resolution and can be used across a wide range of polymer viscosities because polymerization is tightly controlled, but the addition of polymerization-initiating chemicals may negatively impact cell viability.117 Bioprinting, or inkjet printing, is commonly used with cells and hydrogel carriers. However, bioprinting requires deposition of multiple layers with registration.141 Additionally, cells must survive potential shear forces encountered during the printing process. Finally, laser sintering uses a laser, rastered across the sample, to locally heat powered ceramics, metals, and polymers to their melting temperature to yield the final scaffold.141 Laser sintering is generally used in a layer-by-layer assembly approach and may require multiple passes. In addition, resolution is significantly lower than that of stereolithography.
Hydrogels in 3D Printing for Bone Tissue Engineering
Several materials have been investigated for 3D printing in bone repair, the most common of which are ceramics, such as calcium phosphates and hydroxyapatite,142 polymers such as PPF, PCL, PLGA, and poly(vinyl alcohol),141 and metals including NiTi.143 Hydrogels are primarily used as cell carriers in bioprinting or stereolithography. In both cases, the hydrogel must be extruded from a nozzle onto the printing surface where polymerization is initiated by a specific trigger, such as ultraviolet (UV) light, temperature, or pH changes. Hydrogels are ideal candidates for 3D printing via these approaches because their formation can be initiated through a variety of chemistries, including chain polymerization, Michael addition144, physical entanglement, click chemistry145, and radical polymerization146, 147 reactions (Figure 2). Cross-linking methods involving chain polymerization and Michael addition generally demonstrate poor control over the final structure, and therefore, these methods are less frequently used in 3D printing. However, cross-linking initiated via radicals has several advantages in 3D printing applications. Because polymerization is initiated through chemical- or photo-generated radicals, the area of cross-linking can be precisely controlled and the speed is generally rapid. Chain entanglement via thermal setting is also commonly used, provided that the time to set can be tuned to permit rapid polymerization following the deposition phase.
In addition to cross-linking speed, viscosity of the hydrogel is also crucial. Ideally, the hydrogel would demonstrate shear thinning to allow extrusion through the printer nozzle, with immediate cessation of flow to maintain the resolution of the plotted shape. Highly viscous materials will hold their shape throughout the printing and polymerization processes, lending integrity to the final printed structure. Low viscosity materials do not retain shape over long time periods and can only be used in combination with rapid polymerization methods. In addition, feature resolution is diminished by rapid flow of the material before polymerization to the final form. Hydrogel viscosity is affected by multiple material properties, such as the molecular, monomer, and cross-linking densities, cell concentration, bioactive molecule concentration, and ECM protein concentration.148
Early attempts to employ hydrogels in 3D printed structures for bone tissue engineering fabricated chitosan-HA composites using a robotic dispensing system.149 Chitosan polymerization was initiated by the addition of base; chitosan is not water soluble at high pH. Osteoblasts cultured on these scaffolds in the presence of fibrin glue survived and proliferated over the four weeks of observation. As an alternative to direct printing, hydrogels have also been incorporated as fillers that infiltrated pre-formed polymer118 or ceramic150 scaffolds. The primary purpose of hydrogels in these materials is to serve as a cell carrier, whereas the polymer scaffold provided mechanical rigidity. The combination of hydrogels with 3D printed polymers has led to significant formation of cell-cell and cell-ECM interactions. In addition to cells, 3D printing approaches can be used to print microbeads encapsulating growth factors. For example, BMP-2 loaded gelatin microparticles were printed in alignate scaffolds using CaCl2 ionic cross-linking.151
A signficant advantage of 3D printing approaches is the ability to spatially pattern cells, ligands, and factors. The principal limitation in engineered bone grafts is believed to be the inability of vascular networks to penetrate graft materials, resulting in an insufficient supply of oxygen and nutrients throughout the construct, and therefore, the death of regenerating or seeded cells. However, porosity can be controlled directly by 3D printing to enhance ingrowth of regenerating tissue and oxygenation of encapsulated cells, which is difficult through traditional hydrogel formation methods.152 In the case of photo-cross-linked entities, the concentration can also be controlled.153 For example, bone marrow stromal cells and endothelial cells were co-printed in alginate, Matrigel, Lutrol F127, and methylcellulose hydrogels.154 Three-dimensional printing permitted both cell types to be precisely patterned within the gel, simulating potential in vivo presentation. When combined with growth factor printing as described in Poldervaart et al., it would be possible to create tailored environments for the growth of separate cell populations, such as bone and vascular cells. Although current approaches are not capable of creating complex vascularized constructs, 3D printing shows promise in resolving this critical limitation.155 Current printing techniques have been applied successfully to create vasculature consisting of single and branched channels,155, 156 as well as a functional, perfusable network of capillaries.157
Conclusion
Tissue engineered bone constructs provide an alternative to autograft and allograft procedures; however, clinical implementation will require scaffolds that demonstrate good biocompatibility, biodegradability, vascularization potential, mechanical properties, osteoconductive, osteoinductive, and osteogenic potential. Individual materials investigated, including metals, ceramics, and polymers, have yet to meet all of these goals, and thus composites that offer the potential to tune overall scaffold properties by controlling the ratio of optimized constituents are desired. Hydrogels have much to offer as bone tissue engineering materials, especially in composite form where their mechanical properties can be increased by addition of other materials. Among these, natural hydrogels, including collagen and hyaluronic acid, which already form part of the native bone matrix, and PEG, which provides a blank slate that can be investigator modified, offer the most potential as bone tissue engineering materials. Hydrogels can be used to provide degradability, native chemical signals (e.g., for example collagen or hyaluronic acid), controlled release of encapsulated factors, and delivery of cells encapsulated within their matrices. In addition, their thermosetting and radical-initiated cross-linking properties permit their use in 3D printing, which can be employed to generate scaffolds that conform to specific target sites, incorporate spatially patterned cells and growth factors, and to add porosity to enhance tissue ingrowth and vascularization. In addition, many hydrogel constituents are already used in FDA-approved devices, making them attractive for rapid clinical translation. Thus, hydrogel composites, particularly with collagen, hyaluronic acid and PEG, show great promise for future application in bone tissue engineering.
Supplementary Material
Acknowledgements
The authors gratefully acknowledge the support of the Ohio State University Women in Philanthropy, The Ohio State Metro High School Fellowship (to A.R.S.), The Ohio State Howard Hughes Medical Institute Med into Grad Scholars Program (to M.C.), and partial support from NIH grant R01-AR061460 and the Army, Navy, NIH, Air Force, VA, and Health Affairs to support the AFIRM II effort under award No. W81XWH-14–2-0004. The US Army Medical Research Acquisition Activity is the awarding and administering acquisition office for award No. W81XWH-14–2-0004. Opinions, interpretations, conclusions, and recommendations are those of the authors and are not necessarily endorsed by the US Department of Defense.
References
- 1.Lissenberg-Thunnissen SN, de Gorter DJ, Sier CF, Schipper IB. Int Orthop. 2011;35:1271–1280. doi: 10.1007/s00264-011-1301-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Doblaré M, García JM, Gómez MJ. Engineering Fracture Mechanics. 2004;71:1809–1840. [Google Scholar]
- 3.Praemer A, Furner S, Rice DP, S. American Academy of Orthopaedic . Musculoskeletal conditions in the United States. American Academy of Orthopaedic Surgeons, Park Ridge, Ill.; 1992. [Google Scholar]
- 4.Durham SR, McComb JG, Levy ML. Neurosurgery. 2003;52:842–845. doi: 10.1227/01.neu.0000054220.01290.8e. [DOI] [PubMed] [Google Scholar]
- 5.Schmitz JP, Hollinger JO. Clin. Orthop. 1986:299–308. [PubMed] [Google Scholar]
- 6.Arrington ED, Smith WJ, Chambers HG, Bucknell AL, Davino NA. Clin. Orthop. 1996:300–309. doi: 10.1097/00003086-199608000-00037. [DOI] [PubMed] [Google Scholar]
- 7.Goulet JA, Senunas LE, DeSilva GL, Greenfield ML. Clinical Orthopaedics and Related Research. 1997:76–81. doi: 10.1097/00003086-199706000-00011. [DOI] [PubMed] [Google Scholar]
- 8.Younger EM, Chapman MW. J. Orthop. Trauma. 1989;3:192–195. doi: 10.1097/00005131-198909000-00002. [DOI] [PubMed] [Google Scholar]
- 9.Willie BM, Petersen A, Schmidt-Bleek K, Cipitria A, Mehta M, Strube P, Lienau J, Wildemann B, Fratzl P, Duda G. Soft Matter. 2010;6:4976–4987. [Google Scholar]
- 10.Puppi D, Chiellini F, Piras AM, Chiellini E. Prog. Polym. Sci. 2010;35:403–440. [Google Scholar]
- 11.Guldberg RE, Duvall CL, Peister A, Oest ME, Lin AS, Palmer AW, Levenston ME. Biomaterials. 2008;29:3757–3761. doi: 10.1016/j.biomaterials.2008.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.D. H, Muller B, Fierz VC, Irsen SH, Yoon JY, Mushkolaj S, Boss O, Vorndran E, Gbureck U, Degistirici O, Thie M, Leukers B, Beckmann F, Witte F. Proc. SPIE. 2009;7401 [Google Scholar]
- 13.Mitsak AG, Kemppainen JM, Harris MT, Hollister SJ. Tissue engineering. Part A. 2011;17:1831–1839. doi: 10.1089/ten.tea.2010.0560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yang F, Murugan R, Ramakrishna S, Wang X, Ma YX, Wang S. Biomaterials. 2004;25:1891–1900. doi: 10.1016/j.biomaterials.2003.08.062. [DOI] [PubMed] [Google Scholar]
- 15.Karageorgiou V, Kaplan D. Biomaterials. 2005;26:5474–5491. doi: 10.1016/j.biomaterials.2005.02.002. [DOI] [PubMed] [Google Scholar]
- 16.Xue W, Krishna BV, Bandyopadhyay A, Bose S. Acta biomaterialia. 2007;3:1007–1018. doi: 10.1016/j.actbio.2007.05.009. [DOI] [PubMed] [Google Scholar]
- 17.Otsuki B, Takemoto M, Fujibayashi S, Neo M, Kokubo T, Nakamura T. Biomaterials. 2006;27:5892–5900. doi: 10.1016/j.biomaterials.2006.08.013. [DOI] [PubMed] [Google Scholar]
- 18.Stoppato M, Carletti E, Sidarovich V, Quattrone A, Unger RE, Kirkpatrick CJ, Migliaresi C, Motta A. J. Bioact. Compat. Polym. 2013;28:16–32. [Google Scholar]
- 19.Liu X, Ma PX. Annals of biomedical engineering. 2004;32:477–486. doi: 10.1023/b:abme.0000017544.36001.8e. [DOI] [PubMed] [Google Scholar]
- 20.Hutmacher DW. Biomaterials. 2000;21:2529–2543. doi: 10.1016/s0142-9612(00)00121-6. [DOI] [PubMed] [Google Scholar]
- 21.Lopez-Heredia MA, Sohier J, Gaillard C, Quillard S, Dorget M, Layrolle P. Biomaterials. 2008;29:2608–2615. doi: 10.1016/j.biomaterials.2008.02.021. [DOI] [PubMed] [Google Scholar]
- 22.Hughes TB. Clin. Orthop. 2006:169–174. doi: 10.1097/01.blo.0000205884.81328.cc. DOI: 10.1097/01.blo.0000205884.81328.cc. [DOI] [PubMed] [Google Scholar]
- 23.Burg KJ, Porter S, Kellam JF. Biomaterials. 2000;21:2347–2359. doi: 10.1016/s0142-9612(00)00102-2. [DOI] [PubMed] [Google Scholar]
- 24.Damien E, Hing K, Saeed S, Revell PA. J. Biomed. Mater. Res. Part A. 2003;66A:241–246. doi: 10.1002/jbm.a.10564. [DOI] [PubMed] [Google Scholar]
- 25.Makadia HK, Siegel SJ. Polymers. 2011;3:1377–1397. doi: 10.3390/polym3031377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Veronese FM, Pasut G. Drug Discov. Today. 2005;10:1451–1458. doi: 10.1016/S1359-6446(05)03575-0. [DOI] [PubMed] [Google Scholar]
- 27.Sheikh FA, Ju HW, Moon BM, Lee OJ, Kim JH, Park HJ, Kim DW, Kim DK, Jang JE, Khang G, Park CH. Journal of tissue engineering and regenerative medicine. 2015 doi: 10.1002/term.1989. DOI: 10.1002/term.1989. [DOI] [PubMed] [Google Scholar]
- 28.Yaszemski MJ, Payne RG, Hayes WC, Langer R, Mikos AG. Biomaterials. 1996;17:2127–2130. doi: 10.1016/0142-9612(96)00008-7. [DOI] [PubMed] [Google Scholar]
- 29.Hu YH, Grainger DW, Winn SR, Hollinger JO. J. Biomed. Mater. Res. 2002;59:563–572. doi: 10.1002/jbm.1269. [DOI] [PubMed] [Google Scholar]
- 30.Oh SH, Kang SG, Kim ES, Cho SH, Lee JH. Biomaterials. 2003;24:4011–4021. doi: 10.1016/s0142-9612(03)00284-9. [DOI] [PubMed] [Google Scholar]
- 31.Schaefer D, Martin I, Shastri P, Padera RF, Langer R, Freed LE, Vunjak-Novakovic G. Biomaterials. 2000;21:2599–2606. doi: 10.1016/s0142-9612(00)00127-7. [DOI] [PubMed] [Google Scholar]
- 32.Porter JR, Ruckh TT, Popat KC. Biotechnology progress. 2009;25:1539–1560. doi: 10.1002/btpr.246. [DOI] [PubMed] [Google Scholar]
- 33.An YH, Woolf SK, Friedman RJ. Biomaterials. 2000;21:2635–2652. doi: 10.1016/s0142-9612(00)00132-0. [DOI] [PubMed] [Google Scholar]
- 34.Kim J, Kim IS, Cho TH, Lee KB, Hwang SJ, Tae G, Noh I, Lee SH, Park Y, Sun K. Biomaterials. 2007;28:1830–1837. doi: 10.1016/j.biomaterials.2006.11.050. [DOI] [PubMed] [Google Scholar]
- 35.Maus U, Andereya S, Gravius S, Siebert CH, Ohnsorge JAK, Niedhart C. Arch. Orthop. Trauma Surg. 2008;128:1461–1466. doi: 10.1007/s00402-008-0608-8. [DOI] [PubMed] [Google Scholar]
- 36.Fellah BH, Weiss P, Gauthier O, Rouillon T, Pilet P, Daculsi G, Layrolle P. J. Orthop. Res. 2006;24:628–635. doi: 10.1002/jor.20125. [DOI] [PubMed] [Google Scholar]
- 37.Peppas NA, Bures P, Leobandung W, Ichikawa H. Eur. J. Pharm. Biopharm. 2000;50:27–46. doi: 10.1016/s0939-6411(00)00090-4. [DOI] [PubMed] [Google Scholar]
- 38.Lee KY, Mooney DJ. Chem. Rev. 2001;101:1869–1879. doi: 10.1021/cr000108x. [DOI] [PubMed] [Google Scholar]
- 39.Backstrom S, Benavente J, Berg RW, Stibius K, Larsen M, Bohr H, Helix-Nielsen C. Materials Sciences and Applications. 2012;3:425–431. [Google Scholar]
- 40.Crescenzi V, Cornelio L, Di Meo C, Nardecchia S, Lamanna R. Biomacromolecules. 2007;8:1844–1850. doi: 10.1021/bm0700800. [DOI] [PubMed] [Google Scholar]
- 41.Lutolf MP, Hubbell JA. Biomacromolecules. 2003;4:713–722. doi: 10.1021/bm025744e. [DOI] [PubMed] [Google Scholar]
- 42.Drury JL, Mooney DJ. Biomaterials. 2003;24:4337–4351. doi: 10.1016/s0142-9612(03)00340-5. [DOI] [PubMed] [Google Scholar]
- 43.Knott L, Bailey AJ. Bone. 1998;22:181–187. doi: 10.1016/s8756-3282(97)00279-2. [DOI] [PubMed] [Google Scholar]
- 44.Laurent TC, Fraser JR. FASEB Journal. 1992;6:2397–2404. [PubMed] [Google Scholar]
- 45.Engler AJ, Sen S, Sweeney HL, Discher DE. Cell. 2006;126:677–689. doi: 10.1016/j.cell.2006.06.044. [DOI] [PubMed] [Google Scholar]
- 46.Elisseeff J, McIntosh W, Anseth K, Riley S, Ragan P, Langer R. J. Biomed. Mater. Res. 2000;51:164–171. doi: 10.1002/(sici)1097-4636(200008)51:2<164::aid-jbm4>3.0.co;2-w. [DOI] [PubMed] [Google Scholar]
- 47.Schanen BC, De Groot AS, Moise L, Ardito M, McClaine E, Martin W, Wittman V, Warren WL, Drake DR. Vaccine. 2011;29:3299–3309. doi: 10.1016/j.vaccine.2011.02.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kloxin AM, Kasko AM, Salinas CN, Anseth KS. Science. 2009;324:59–63. doi: 10.1126/science.1169494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wu SL, Liu XM, Yeung KWK, Liu CS, Yang XJ. Mater. Sci. Eng. R-Rep. 2014;80:1–36. [Google Scholar]
- 50.Anseth KS, Bowman CN, BrannonPeppas L. Biomaterials. 1996;17:1647–1657. doi: 10.1016/0142-9612(96)87644-7. [DOI] [PubMed] [Google Scholar]
- 51.Vo TN, Kasper FK, Mikos AG. Adv. Drug Delivery. Rev. 2012;64:1292–1309. doi: 10.1016/j.addr.2012.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.D’Este M, Eglin D. Acta Biomater. 2013;9:5421–5430. doi: 10.1016/j.actbio.2012.11.022. [DOI] [PubMed] [Google Scholar]
- 53.Geffers M, Groll J, Gbureck U. Materials. 2015;8:2700–2717. [Google Scholar]
- 54.Ferreira AM, Gentile P, Chiono V, Ciardelli G. Acta Biomater. 2012;8:3191–3200. doi: 10.1016/j.actbio.2012.06.014. [DOI] [PubMed] [Google Scholar]
- 55.Xu X, Jha AK, Harrington DA, Farach-Carson MC, Jia XQ. Soft Matter. 2012;8:3280–3294. doi: 10.1039/C2SM06463D. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Khan F, Ahmad SR. Macromol. Biosci. 2013;13:395–421. doi: 10.1002/mabi.201200409. [DOI] [PubMed] [Google Scholar]
- 57.Korsmeyer RW, Peppas NA. J. Membr. Sci. 1981;9:211–227. [Google Scholar]
- 58.Sawhney AS, Pathak CP, Hubbell JA. Macromolecules. 1993;26:581–587. [Google Scholar]
- 59.Mann BK, Gobin AS, Tsai AT, Schmedlen RH, West JL. Biomaterials. 2001;22:3045–3051. doi: 10.1016/s0142-9612(01)00051-5. [DOI] [PubMed] [Google Scholar]
- 60.Huffman AS, Afrassiabi A, Dong LC. J. Control. Release. 1986;4:213–222. [Google Scholar]
- 61.Yoshida R, Uchida K, Kaneko Y, Sakai K, Kikuchi A, Sakurai Y, Okano T. Nature. 1995;374:240–242. [Google Scholar]
- 62.Brannonpeppas L, Peppas NA. J. Control. Release. 1991;16:319–330. [Google Scholar]
- 63.Muzzarelli RA, Zucchini C, Ilari P, Pugnaloni A, Mattioli Belmonte M, Biagini G, Castaldini C. Biomaterials. 1993;14:925–929. doi: 10.1016/0142-9612(93)90134-n. [DOI] [PubMed] [Google Scholar]
- 64.Liu LS, Thompson AY, Heidaran MA, Poser JW, Spiro RC. Biomaterials. 1999;20:1097–1108. doi: 10.1016/s0142-9612(99)00006-x. [DOI] [PubMed] [Google Scholar]
- 65.Winn SR, Schmitt JM, Buck D, Hu Y, Grainger D, Hollinger JO. J. Biomed. Mater. Res. 1999;45:414–421. doi: 10.1002/(sici)1097-4636(19990615)45:4<414::aid-jbm17>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 66.Radice M, Brun P, Cortivo R, Scapinelli R, Battaliard C, Abatangelo G. J. Biomed. Mater. Res. 2000;50:101–109. doi: 10.1002/(sici)1097-4636(200005)50:2<101::aid-jbm2>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- 67.Burdick JA, Anseth KS. Biomaterials. 2002;23:4315–4323. doi: 10.1016/s0142-9612(02)00176-x. [DOI] [PubMed] [Google Scholar]
- 68.Burdick JA, Mason MN, Hinman AD, Thorne K, Anseth KS. J. Control. Release. 2002;83:53–63. doi: 10.1016/s0168-3659(02)00181-5. [DOI] [PubMed] [Google Scholar]
- 69.Lee KY, Alsberg E, Mooney DJ. J. Biomed. Mater. Res. 2001;56:228–233. doi: 10.1002/1097-4636(200108)56:2<228::aid-jbm1089>3.0.co;2-9. [DOI] [PubMed] [Google Scholar]
- 70.Pierschbacher MD, Ruoslahti E. Nature. 1984;309:30–33. doi: 10.1038/309030a0. [DOI] [PubMed] [Google Scholar]
- 71.Alsberg E, Anderson KW, Albeiruti A, Franceschi RT, Mooney DJ. J. Dent. Res. 2001;80:2025–2029. doi: 10.1177/00220345010800111501. [DOI] [PubMed] [Google Scholar]
- 72.Shin H, Ruhe PQ, Mikos AG, Jansen JA. Biomaterials. 2003;24:3201–3211. doi: 10.1016/s0142-9612(03)00168-6. [DOI] [PubMed] [Google Scholar]
- 73.Filmon R, Basle MF, Barbier A, Chappard D. J. Biomater. Sci.-Polym. Ed. 2000;11:849–868. doi: 10.1163/156856200744057. [DOI] [PubMed] [Google Scholar]
- 74.Beertsen W, van den Bos T. J. Clin. Investig. 1992;89:1974–1980. doi: 10.1172/JCI115805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Kolambkar YM, Dupont KM, Boerckel JD, Huebsch N, Mooney DJ, Hutmacher DW, Guldberg RE. Biomaterials. 2011;32:65–74. doi: 10.1016/j.biomaterials.2010.08.074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Xu W, Ma J, Jabbari E. Acta Biomater. 2010;6:1992–2002. doi: 10.1016/j.actbio.2009.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Daculsi G, Weiss P, Bouler JM, Gauthier O, Millot F, Aguado E. Bone. 1999;25:59S–61S. doi: 10.1016/s8756-3282(99)00135-0. [DOI] [PubMed] [Google Scholar]
- 78.Schiraldi C, D’Agostino A, Oliva A, Flamma F, De Rosa A, Apicella A, Aversa R, De Rosa M. Biomaterials. 2004;25:3645–3653. doi: 10.1016/j.biomaterials.2003.10.059. [DOI] [PubMed] [Google Scholar]
- 79.Couto DS, Hong Z, Mano JF. Acta Biomater. 2009;5:115–123. doi: 10.1016/j.actbio.2008.08.006. [DOI] [PubMed] [Google Scholar]
- 80.Tan R, Feng Q, She Z, Wang M, Jin H, Li J, Yu X. Polym. Degrad. Stab. 2010;95:1736–1742. [Google Scholar]
- 81.Zhang SM, Cui FZ, Liao SS, Zhu Y, Han L. J. Mater. Sci.: Mater. Med. 2003;14:641–645. doi: 10.1023/a:1024083309982. [DOI] [PubMed] [Google Scholar]
- 82.Gaharwar AK, Dammu SA, Canter JM, Wu CJ, Schmidt G. Biomacromolecules. 2011;12:1641–1650. doi: 10.1021/bm200027z. [DOI] [PubMed] [Google Scholar]
- 83.Serre CM, Papillard M, Chavassieux P, Boivin G. Biomaterials. 1993;14:97–106. doi: 10.1016/0142-9612(93)90217-p. [DOI] [PubMed] [Google Scholar]
- 84.Kikuchi M, Itoh S, Ichinose S, Shinomiya K, Tanaka J. Biomaterials. 2001;22:1705–1711. doi: 10.1016/s0142-9612(00)00305-7. [DOI] [PubMed] [Google Scholar]
- 85.Du C, Cui FZ, Zhu XD, de Groot K. J. Biomed. Mater. Res. 1999;44:407–415. doi: 10.1002/(sici)1097-4636(19990315)44:4<407::aid-jbm6>3.0.co;2-t. [DOI] [PubMed] [Google Scholar]
- 86.Miyamoto Y, Ishikawa K, Takechi M, Toh T, Yuasa T, Nagayama M, Suzuki K. Biomaterials. 1998;19:707–715. doi: 10.1016/s0142-9612(97)00186-5. [DOI] [PubMed] [Google Scholar]
- 87.Zhang QQ, Ren L, Wang C, Liu LR, Wen XJ, Liu YH, Zhang XD. Artif. Cells Blood Substit. Immobil. Biotechnol. 1996;24:693–702. doi: 10.3109/10731199609118892. [DOI] [PubMed] [Google Scholar]
- 88.Fu SZ, Ni PY, Wang BY, Chu BY, Zheng L, Luo F, Luo JC, Qian ZY. Biomaterials. 2012;33:4801–4809. doi: 10.1016/j.biomaterials.2012.03.040. [DOI] [PubMed] [Google Scholar]
- 89.Zhang L, Rakotondradany F, Myles AJ, Fenniri H, Webster TJ. Biomaterials. 2009;30:1309–1320. doi: 10.1016/j.biomaterials.2008.11.020. [DOI] [PubMed] [Google Scholar]
- 90.Zhang LJ, Rodriguez J, Raez J, Myles AJ, Fenniri H, Webster TJ. Nanotechnology. 2009;20 doi: 10.1088/0957-4484/20/17/175101. [DOI] [PubMed] [Google Scholar]
- 91.Urist MR. Science. 1965;150:893. doi: 10.1126/science.150.3698.893. &. [DOI] [PubMed] [Google Scholar]
- 92.Lieberman JR, Daluiski A, Einhorn TA. J. Bone Joint Surg.-Am. Vol. 2002;84A:1032–1044. doi: 10.2106/00004623-200206000-00022. [DOI] [PubMed] [Google Scholar]
- 93.Linkhart TA, Mohan S, Baylink DJ. Bone. 1996;19:S1–S12. doi: 10.1016/s8756-3282(96)00138-x. [DOI] [PubMed] [Google Scholar]
- 94.Urist MR, Mazet R., Jr. The Journal of bone and joint surgery. American volume. 1959;41-A:409–416. [PubMed] [Google Scholar]
- 95.Moshaverinia A, Chen C, Xu XT, Ansari S, Zadeh HH, Schricker SR, Paine ML, Moradian-Oldak J, Khademhosseini A, Snead ML, Shi ST. Adv. Funct. Mater. 2015;25:2296–2307. doi: 10.1002/adfm.201500055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Wang W, Sun L, Zhang PF, Song JF, Liu WG. Acta Biomater. 2014;10:4983–4995. doi: 10.1016/j.actbio.2014.08.022. [DOI] [PubMed] [Google Scholar]
- 97.Ratanavaraporn J, Furuya H, Tabata Y. Biomaterials. 2012;33:304–316. doi: 10.1016/j.biomaterials.2011.09.050. [DOI] [PubMed] [Google Scholar]
- 98.Asahina I, Watanabe M, Sakurai N, Mori M, Enomoto S. J. Med. Dent. Sci. 1997;44:63–70. [PubMed] [Google Scholar]
- 99.Yamamoto M, Tabata Y, Ikada Y. Journal of biomaterials science. Polymer edition. 1998;9:439–458. doi: 10.1163/156856298x00550. [DOI] [PubMed] [Google Scholar]
- 100.Tabata Y, Yamada K, Miyamoto S, Nagata I, Kikuchi H, Aoyama I, Tamura M, Ikada Y. Biomaterials. 1998;19:807–815. doi: 10.1016/s0142-9612(98)00233-6. [DOI] [PubMed] [Google Scholar]
- 101.Hong L, Tabata Y, Miyamoto S, Yamamoto M, Yamada K, Hashimoto N, Ikada Y. J. Neurosurg. 2000;92:315–325. doi: 10.3171/jns.2000.92.2.0315. [DOI] [PubMed] [Google Scholar]
- 102.Amaro Martins VC, Goissis G. Artif. Organs. 2000;24:224–230. doi: 10.1046/j.1525-1594.2000.06517.x. [DOI] [PubMed] [Google Scholar]
- 103.Bulpitt P, Aeschlimann D. J. Biomed. Mater. Res. 1999;47:152–169. doi: 10.1002/(sici)1097-4636(199911)47:2<152::aid-jbm5>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- 104.Hunt DR, Jovanovic SA, Wikesjo UM, Wozney JM, Bernard GW. J. Periodontol. 2001;72:651–658. doi: 10.1902/jop.2001.72.5.651. [DOI] [PubMed] [Google Scholar]
- 105.Bergman K, Engstrand T, Hilborn J, Ossipov D, Piskounova S, Bowden T. J. Biomed. Mater. Res. Part A. 2009;91A:1111–1118. doi: 10.1002/jbm.a.32289. [DOI] [PubMed] [Google Scholar]
- 106.Hosseinkhani H, Hosseinkhani M, Khademhosseini A, Kobayashi H. J. Control. Release. 2007;117:380–386. doi: 10.1016/j.jconrel.2006.11.018. [DOI] [PubMed] [Google Scholar]
- 107.Hokugo A, Saito T, Li A, Sato K, Tabata Y, Jarrahy R. Biomaterials. 2014;35:5565–5571. doi: 10.1016/j.biomaterials.2014.03.018. [DOI] [PubMed] [Google Scholar]
- 108.Patterson J, Siew R, Herring SW, Lin ASP, Guldberg R, Stayton PS. Biomaterials. 2010;31:6772–6781. doi: 10.1016/j.biomaterials.2010.05.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Lutolf MR, Weber FE, Schmoekel HG, Schense JC, Kohler T, Muller R, Hubbell JA. Nat. Biotechnol. 2003;21:513–518. doi: 10.1038/nbt818. [DOI] [PubMed] [Google Scholar]
- 110.Kempen DHR, Lu L, Hefferan TE, Creemers LB, Maran A, Classic KL, Dhert WJA, Yaszemski MJ. Biomaterials. 2008;29:3245–3252. doi: 10.1016/j.biomaterials.2008.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Niu XF, Feng QL, Wang MB, Guo XD, Zheng QX. J. Control. Release. 2009;134:111–117. doi: 10.1016/j.jconrel.2008.11.020. [DOI] [PubMed] [Google Scholar]
- 112.Chen FM, Zhao YM, Sun HH, Jin T, Wang QT, Zhou W, Wu ZF, Jin Y. J. Control. Release. 2007;118:65–77. doi: 10.1016/j.jconrel.2006.11.016. [DOI] [PubMed] [Google Scholar]
- 113.Watson L, Elliman S, Coleman C. Stem Cell Research & Therapy. 2014;5:51. doi: 10.1186/scrt439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Guilak F, Estes BT, Diekman BO, Moutos FT, Gimble JM. Clinical Orthopaedics and Related Research. 2010;468:2530–2540. doi: 10.1007/s11999-010-1410-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Weng YL, Cao YL, Silva CA, Vacanti MP, Vacanti CA. J. Oral Maxillofac. Surg. 2001;59:185–190. doi: 10.1053/joms.2001.20491. [DOI] [PubMed] [Google Scholar]
- 116.Burkoth AK, Burdick JA, Anseth KS. J. Biomed. Mater. Res. 2000;51:352–359. doi: 10.1002/1097-4636(20000905)51:3<352::aid-jbm8>3.0.co;2-c. [DOI] [PubMed] [Google Scholar]
- 117.Bryant SJ, Nuttelman CR, Anseth KS. J. Biomater. Sci.-Polym. Ed. 2000;11:439–457. doi: 10.1163/156856200743805. [DOI] [PubMed] [Google Scholar]
- 118.Endres M, Hutmacher DW, Salgado AJ, Kaps C, Ringe J, Reis RL, Sittinger M, Brandwood A, Schantz JT. Tissue Eng. 2003;9:689–702. doi: 10.1089/107632703768247386. [DOI] [PubMed] [Google Scholar]
- 119.Wang LM, Stegemann JP. Biomaterials. 2010;31:3976–3985. doi: 10.1016/j.biomaterials.2010.01.131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Wiesmann HP, Nazer N, Klatt C, Szuwart T, Meyer U. J. Oral Maxillofac. Surg. 2003;61:1455–1462. doi: 10.1016/j.joms.2003.05.001. [DOI] [PubMed] [Google Scholar]
- 121.Weinand C, Gupta R, Huang AY, Weinberg E, Madisch I, Qudsi RA, Neville CM, Pomerantseva I, Vacanti JP. Tissue Eng. 2007;13:757–765. doi: 10.1089/ten.2006.0083. [DOI] [PubMed] [Google Scholar]
- 122.Marelli B, Ghezzi CE, Mohn D, Stark WJ, Barralet JE, Boccaccini AR, Nazhat SN. Biomaterials. 2011;32:8915–8926. doi: 10.1016/j.biomaterials.2011.08.016. [DOI] [PubMed] [Google Scholar]
- 123.Chen F, Mao T, Tao K, Chen S, Ding G, Gu X. Br. J. Oral Maxillofac. Surg. 2003;41:240–243. doi: 10.1016/s0266-4356(03)00084-6. [DOI] [PubMed] [Google Scholar]
- 124.Weir MD, Xu HHK, Simon CG. J. Biomed. Mater. Res. Part A. 2006;77A:487–496. doi: 10.1002/jbm.a.30626. [DOI] [PubMed] [Google Scholar]
- 125.Zhao LA, Weir MD, Xu HHK. Biomaterials. 2010;31:6502–6510. doi: 10.1016/j.biomaterials.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Barralet JE, Wang L, Lawson M, Triffitt JT, Cooper PR, Shelton RM. J. Mater. Sci. Mater. Med. 2005;16:515–519. doi: 10.1007/s10856-005-0526-z. [DOI] [PubMed] [Google Scholar]
- 127.Lund AW, Bush JA, Plopper GE, Stegemann JP. J. Biomed. Mater. Res. Part B. 2008;87B:213–221. doi: 10.1002/jbm.b.31098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Terraciano V, Hwang N, Moroni L, Park HB, Zhang Z, Mizrahi J, Seliktar D, Elisseeff J. Stem Cells. 2007;25:2730–2738. doi: 10.1634/stemcells.2007-0228. [DOI] [PubMed] [Google Scholar]
- 129.Simmons CA, Alsberg E, Hsiong S, Kim WJ, Mooney DJ. Bone. 2004;35:562–569. doi: 10.1016/j.bone.2004.02.027. [DOI] [PubMed] [Google Scholar]
- 130.Kim MS, Kim SK, Kim SH, Hyun H, Khang G, Lee HB. Tissue Eng. 2006;12:2863–2873. doi: 10.1089/ten.2006.12.2863. [DOI] [PubMed] [Google Scholar]
- 131.Ahn HH, Kim KS, Lee JH, Lee JY, Kim BS, Lee IW, Chun HJ, Kim JH, Lee HB, Kim MS. Tissue Engineering Part A. 2009;15:1821–1832. doi: 10.1089/ten.tea.2008.0386. [DOI] [PubMed] [Google Scholar]
- 132.Gerber HP, Ferrara N. Trends Cardiovasc. Med. 2000;10:223–228. doi: 10.1016/s1050-1738(00)00074-8. [DOI] [PubMed] [Google Scholar]
- 133.Chan V, Zorlutuna P, Jeong JH, Kong H, Bashir R. Lab Chip. 2010;10:2062–2070. doi: 10.1039/c004285d. [DOI] [PubMed] [Google Scholar]
- 134.Bishop G. Innovation in education. Macmillan London: 1986. [Google Scholar]
- 135.Cooke MN, Fisher JP, Dean D, Rimnac C, Mikos AG. J. Biomed. Mater. Res. Part B. 2003;64B:65–69. doi: 10.1002/jbm.b.10485. [DOI] [PubMed] [Google Scholar]
- 136.Kodama H. Rev. Sci. Instrum. 1981;52:1770–1773. [Google Scholar]
- 137.Jacobs PF, Society of Manufacturing Engineers Rapid prototyping and manufacturing: fundamentals of stereolithography. 1992 [Google Scholar]
- 138.Crump SS. Journal. 1992 [Google Scholar]
- 139.Chang R, Nam J, Sun W. Tissue engineering. Part A. 2008;14:41–48. doi: 10.1089/ten.a.2007.0004. [DOI] [PubMed] [Google Scholar]
- 140.Hull CW. Journal. 1986 [Google Scholar]
- 141.Childers EP, Wang MO, Becker ML, Fisher JP, Dean D. MRS Bulletin. 2015;40:119–126. [Google Scholar]
- 142.Chia HN, Wu BM. J. Biol. Eng. 2015;9 doi: 10.1186/s13036-015-0001-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Andani MT, Moghaddam NS, Haberland C, Dean D, Miller MJ, Elahinia M. Acta Biomater. 2014;10:4058–4070. doi: 10.1016/j.actbio.2014.06.025. [DOI] [PubMed] [Google Scholar]
- 144.Metters A, Hubbell J. Biomacromolecules. 2005;6:290–301. doi: 10.1021/bm049607o. [DOI] [PubMed] [Google Scholar]
- 145.Malkoch M, Vestberg R, Gupta N, Mespouille L, Dubois P, Mason AF, Hedrick JL, Liao Q, Frank CW, Kingsbury K, Hawker CJ. Chem. Commun. 2006:2774–2776. doi: 10.1039/b603438a. DOI: 10.1039/b603438a. [DOI] [PubMed] [Google Scholar]
- 146.Xia Y, Yin XC, Burke NAD, Stover HDH. Macromolecules. 2005;38:5937–5943. [Google Scholar]
- 147.Oh JK, Siegwart DJ, Lee HI, Sherwood G, Peteanu L, Hollinger JO, Kataoka K, Matyjaszewski K. J. Am. Chem. Soc. 2007;129:5939–5945. doi: 10.1021/ja069150l. [DOI] [PubMed] [Google Scholar]
- 148.Peppas NA, Hilt JZ, Khademhosseini A, Langer R. Adv. Mater. 2006;18:1345–1360. [Google Scholar]
- 149.Ang TH, Sultana FSA, Hutmacher DW, Wong YS, Fuh JYH, Mo XM, Loh HT, Burdet E, Teoh SH. Materials Science and Engineering: C. 2002;20:35–42. [Google Scholar]
- 150.Weinand C, Pomerantseva I, Neville CM, Gupta R, Weinberg E, Madisch I, Shapiro F, Abukawa H, Troulis MJ, Vacanti JP. Bone. 2006;38:555–563. doi: 10.1016/j.bone.2005.10.016. [DOI] [PubMed] [Google Scholar]
- 151.Poldervaart MT, Wang H, van der Stok J, Weinans H, Leeuwenburgh SCG, Oner FC, Dhert WJA, Alblas J. PLoS One. 2013;8 doi: 10.1371/journal.pone.0072610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Fedorovich NE, Kuipers E, Gawlitta D, Dhert WJA, Alblas J. Tissue Engineering Part A. 2011;17:2473–2486. doi: 10.1089/ten.TEA.2011.0001. [DOI] [PubMed] [Google Scholar]
- 153.Mapili G, Lu Y, Chen SC, Roy K. J. Biomed. Mater. Res. Part B. 2005;75B:414–424. doi: 10.1002/jbm.b.30325. [DOI] [PubMed] [Google Scholar]
- 154.Fedorovich NE, Dewijn JR, Verbout AJ, Alblas J, Dhert WJA. Tissue Engineering Part A. 2008;14:127–133. doi: 10.1089/ten.a.2007.0158. [DOI] [PubMed] [Google Scholar]
- 155.Cui X, Boland T, D’Lima DD, Lotz MK. Recent Pat. Drug Delivery Formulation. 2012;6:149–155. doi: 10.2174/187221112800672949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Ozbolat IT, Yu Y. IEEE Trans. Biomed. Eng. 2013;60:691–699. doi: 10.1109/TBME.2013.2243912. [DOI] [PubMed] [Google Scholar]
- 157.Bertassoni LE, Cecconi M, Manoharan V, Nikkhah M, Hjortnaes J, Cristino AL, Barabaschi G, Demarchi D, Dokmeci MR, Yang Y, Khademhosseini A. Lab on a Chip. 2014;14:2202–2211. doi: 10.1039/c4lc00030g. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.