Abstract
Background
The World Health Organization (WHO) recommends at least four antenatal care (ANC) visits for all pregnant women. Almost half of pregnant women worldwide, and especially in developing countries do not receive this amount of care. Poor attendance of ANC is associated with delivery of low birthweight babies and more neonatal deaths. ANC may include education on nutrition, potential problems with pregnancy or childbirth, child care and prevention or detection of disease during pregnancy.
This review focused on community‐based interventions and health systems‐related interventions.
Objectives
To assess the effects of health system and community interventions for improving coverage of antenatal care and other perinatal health outcomes.
Search methods
We searched the Cochrane Pregnancy and Childbirth Group's Trials Register (7 June 2015) and reference lists of retrieved studies.
Selection criteria
We included randomised controlled trials (RCTs), quasi‐randomised trials and cluster‐randomised trials. Trials of any interventions to improve ANC coverage were eligible for inclusion. Trials were also eligible if they targeted specific and related outcomes, such as maternal or perinatal death, but also reported ANC coverage.
Data collection and analysis
Two review authors independently assessed trials for inclusion and risk of bias, extracted data and checked them for accuracy.
Main results
We included 34 trials involving approximately 400,000 women. Some trials tested community‐based interventions to improve uptake of antenatal care (media campaigns, education or financial incentives for pregnant women), while other trials looked at health systems interventions (home visits for pregnant women or equipment for clinics). Most trials took place in low‐ and middle‐income countries, and 29 of the 34 trials used a cluster‐randomised design. We assessed 30 of the 34 trials as of low or unclear overall risk of bias.
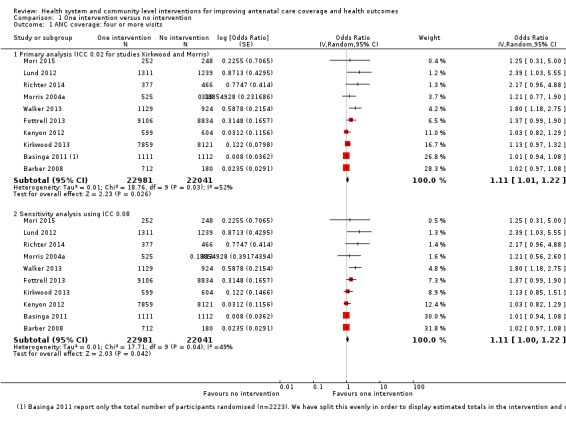
Comparison 1: One intervention versus no intervention
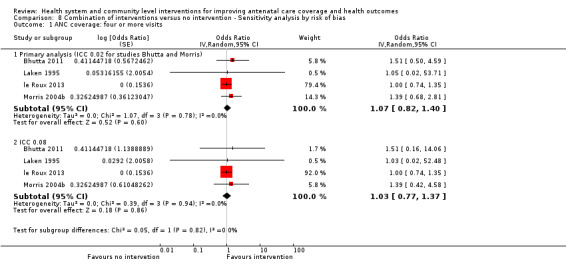
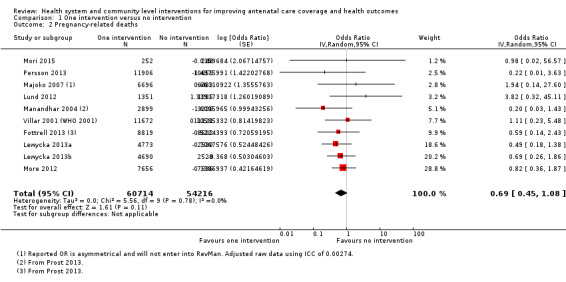
We found marginal improvements in ANC coverage of at least four visits (average odds ratio (OR) 1.11, 95% confidence interval (CI) 1.01 to 1.22; participants = 45,022; studies = 10; Heterogeneity: Tau² = 0.01; I² = 52%; high quality evidence). Sensitivity analysis with a more conservative intra‐cluster correlation co‐efficient (ICC) gave similar marginal results. Excluding one study at high risk of bias shifted the marginal pooled estimate towards no effect. There was no effect on pregnancy‐related deaths (average OR 0.69, 95% CI 0.45 to 1.08; participants = 114,930; studies = 10; Heterogeneity: Tau² = 0.00; I² = 0%; low quality evidence), perinatal mortality (average OR 0.96, 95% CI 0.89 to 1.03; studies = 15; Heterogeneity: Tau² = 0.01; I² = 45%; moderate quality evidence) or low birthweight (average OR 0.94, 95% CI 0.82 to 1.06; studies = five; Heterogeneity: Tau² = 0.00; I² = 5%; high quality evidence). Single interventions led to marginal improvements in the number of women who delivered in health facilities (average OR 1.08, 95% CI 1.02 to 1.15; studies = 10; Heterogeneity: Tau² = 0.00; I² = 0%; high quality evidence), and in the proportion of women who had at least one ANC visit (average OR 1.68, 95% CI 1.02 to 2.79; studies = six; Heterogeneity: Tau² = 0.24; I² = 76%; moderate quality evidence). Results for ANC coverage (at least four and at least one visit) and for perinatal mortality had substantial statistical heterogeneity. Single interventions did not improve the proportion of women receiving tetanus protection (average OR 1.03, 95% CI 0.92 to 1.15; studies = 8; Heterogeneity: Tau² = 0.01; I² = 57%). No study reported onintermittent prophylactic treatment for malaria.
Comparison 2: Two or more interventions versus no intervention
We found no improvements in ANC coverage of four or more visits (average OR 1.48, 95% CI 0.99 to 2.21; participants = 7840; studies = six; Heterogeneity: Tau² = 0.10; I² = 48%; low quality evidence) or pregnancy‐related deaths (average OR 0.70, 95% CI 0.39 to 1.26; participants = 13,756; studies = three; Heterogeneity: Tau² = 0.00; I² = 0%; moderate quality evidence). However, combined interventions led to improvements in ANC coverage of at least one visit (average OR 1.79, 95% CI 1.47 to 2.17; studies = five; Heterogeneity: Tau² = 0.00; I² = 0%; moderate quality evidence), perinatal mortality (average OR 0.74, 95% CI 0.57 to 0.95; studies = five; Heterogeneity: Tau² = 0.06; I² = 83%; moderate quality evidence) and low birthweight (average OR 0.61, 95% CI 0.46 to 0.80; studies = two; Heterogeneity: Tau² = 0.00; I² = 0%; moderate quality evidence). Meta‐analyses for both ANC coverage four or more visits and perinatal mortality had substantial statistical heterogeneity. Combined interventions improved the proportion of women who had tetanus protection (average OR 1.48, 95% CI 1.18 to 1.87; studies = 3; Heterogeneity: Tau² = 0.01; I² = 33%). No trial in this comparison reported on intermittent prophylactic treatment for malaria.
Comparison 3: Two interventions compared head to head. No trials found.
Comparison 4: One intervention versus a combination of interventions
There was no difference in ANC coverage (four or more visits and at least one visit), pregnancy‐related deaths, deliveries in a health facility or perinatal mortality. No trials in this comparison reported on low birthweight orintermittent prophylactic treatment of malaria.
Authors' conclusions
Implications for practice ‐ Single interventions may improve ANC coverage (at least one visit and four or more visits) and deliveries in health facilities. Combined interventions may improve ANC coverage (at least one visit), reduce perinatal mortality and reduce the occurrence of low birthweight. The effects of the interventions are unrelated to whether they are community or health system interventions.
Implications for research ‐ More details should be provided in reporting numbers of events, group totals and the ICCs used to adjust for cluster effects. Outcomes should be reported uniformly so that they are comparable to commonly‐used population indicators. We recommend further cluster‐RCTs of pregnant women and women in their reproductive years, using combinations of interventions and looking at outcomes that are important to pregnant women, such as maternal and perinatal morbidity and mortality, alongside the explanatory outcomes along the pathway of care: ANC coverage, the services provided during ANC and deliveries in health facilities.
Plain language summary
Health system and community level interventions for improving antenatal care coverage and health outcomes
What is the issue?
The World Health Organization recommends at least four antenatal visits for all pregnant women. Almost half of pregnant women worldwide miss out on this level of care, and this is more problematic in low‐ and middle‐income countries.
Why is this important?
Healthcare during pregnancy is a priority because poor antenatal attendance is associated with delivery of low birthweight babies and more newborn deaths. Antenatal care also provides opportunity for nutritional and health checks, such as whether a woman has a disease like malaria or has been exposed to infectious diseases such as HIV (human immunodeficiency virus) or syphilis.
What evidence did we find?
We reviewed randomised controlled trials that tested ways to improve the uptake of antenatal care during pregnancy. Some trials tested community‐based interventions (media campaigns, education on self and infant care or financial incentives for pregnant women to attend antenatal care), while other trials looked at health systems interventions (home visits for pregnant women or provision of equipment for clinics). We included 34 trials with approximately 400,000 women. Most trials took place in low‐ and middle‐income countries, and most trials were conducted in a way that made us feel confident about trusting the published reports. We assessed 30 of the 34 trials as of low or unclear overall risk of bias. The quality rating (high, moderate or low) shows our level of confidence that the result is robust and meaningful.
Trials comparing one intervention with no intervention
Single interventions only marginally improved the numbers of women attending four antenatal visits (high quality). Interventions did not improve rates of maternal death (low quality), baby deaths (moderate quality) or low birthweight (high quality). Even so, interventions led to modest improvements in the number of women who had at least one antenatal visit (moderate quality) and who delivered in a health facility (high quality). The number of women who received intermittent preventive treatment for malaria was not reported.
Trials comparing two or more interventions with no intervention
Combined interventions did not improve the number of women with four or more visits (low quality), or reduce maternal deaths (moderate quality). Nor did it increase the number of women who delivered in a health facility (moderate quality). However, more women who received combined interventions had one or more antenatal visits (moderate quality); there were also fewer baby deaths (moderate quality) and fewer low birthweight babies (moderate quality). The number of women who received intermittent preventive treatment for malaria was not reported.
We found no evidence that trials of community interventions worked differently from trials of health systems interventions.
Trials comparing one intervention with another intervention ‐ there were no trials for this comparison.
Trials comparing one intervention with a combination of interventions ‐ There was no difference in the number of women attending four or more antenatal visits (and at least one visit), maternal deaths, baby deaths, the number of deliveries in a health facility or the number of women who received intermittent preventive treatment for malaria.
What does this mean?
Single interventions may improve antenatal care coverage (women attending at least one visit and women attending four or more visits) and encourage women to give birth to their babies in health facilities. Combined interventions may also improve antenatal care coverage (at least one visit), reduce baby deaths and reduce the number of babies born with low birthweight.
We recommend that further studies of pregnant women and women in their reproductive years use combinations of interventions to maximise impact and look at outcomes that are important to the women themselves, such as maternal and baby deaths or ill health and the use of healthcare services.
Summary of findings
Background
In 2010, about 287,000 maternal deaths occurred worldwide (WHO 2013a). Despite considerable efforts to curb maternal mortality, close to 800 women continue to die every day due to complications of pregnancy and childbirth, and about 99% of these deaths occur in low‐ and middle‐income countries (WHO 2012c). In these settings, neonatal mortality rates are also high, despite the availability of evidence‐based interventions that could avert up to 72% of neonatal deaths (Darmstadt 2005). Interventions such as maternal immunisation against tetanus and skilled care at delivery can reduce both maternal and neonatal deaths (Lassi 2015).
Interventions to reduce maternal mortality may focus on three periods. The first is during pregnancy (antenatal care; ANC), the second is the intrapartum period, (i.e. during labour and delivery) and the third is in the postpartum period (after delivery). The intrapartum period is much shorter and less predictable than the longer more stable pregnancy period (Mbuagbaw 2011). It is also more challenging to provide adequate care in this period, especially in low‐ and middle‐income countries where human resource shortages and other health system weaknesses limit the availability of emergency obstetric care (Dogba 2009). ANC, on the other hand, is less resource‐intensive and its provision can be spread throughout the pregnancy period.
ANC generally comprises the following interventions (Kinzie 2004).
Health promotion: ANC is an opportunity to educate the woman about her health, pregnancy and childbirth, recognising danger signs, the benefits of good nutrition and exclusive breastfeeding, the harms of alcohol, tobacco and drugs, and other relevant issues.
Disease prevention: immunisation against tetanus, prophylactic treatment against malaria, and protection against iron‐deficiency anaemia are some conditions that can de addressed during ANC visits.
Early detection and treatment for complications and diseases: pregnant women can be screened for syphilis, human immunodeficiency virus (HIV) and other sexually transmitted infections. Complications of pregnancy such as pre‐eclampsia and eclampsia, infection and vaginal bleeding among others can be addressed.
Birth preparedness: the pregnant woman is counselled on her decision about where to deliver, choice of a skilled birth attendant and a caregiver (for herself or her other children at home). The ANC visit may cover planning for transportation to the hospital, costs of care and supplies for delivery.
Complication readiness: women are encouraged to have an emergency plan for complicated deliveries. This plan should include money for extra medical or surgical care and potential blood donors.
ANC may not address all the causes of maternal deaths; however, it is positively associated with receiving professional assistance at delivery (Bloom 1999; Mbuagbaw 2011; Mishra 2006; Oakley 2009) and improved pregnancy outcomes such as normal birthweight (Mbuagbaw 2011). In different regions, the effects of ANC on enhancing rates of delivery in a health facility are disparate (Mbuagbaw 2011; Raatikainen 2007).
Description of the condition
The World Health Organization (WHO) recommends at least four ANC visits for all pregnant women (WHO 2013).The first visit should take place during the first trimester (before the 12th week but no later than the 16th week), the second visit between the 24th and 28th week, and the third and fourth visits at 32 weeks and 36 weeks, respectively. Reports indicate that only 53% of pregnant women worldwide receive this amount of care (WHO 2013). Coverage is lower in low‐ and middle‐income countries where the use of maternal health care in general is limited and varies widely within and between countries (Say 2007). Poor attendance of ANC is associated with delivery of low birthweight infants (Mbuagbaw 2011; Raatikainen 2007; Showstack 1984; Siza 2008), and more neonatal deaths (Raatikainen 2007). ANC models with reduced visits may also be linked to higher perinatal mortality (Dowswell 2015; Vogel 2013).
Measuring antenatal care
Even though the WHO recommends four ANC visits during pregnancy, this is not a very informative measure (WHO 2013), as it gives no indication of the quality or timing of the visits. Furthermore, there is no measure of access. A comprehensive measure of ANC should include a measure of personal health‐seeking behaviour and also a measure of the availability of ANC services, as both are integral to effective ANC. More comprehensive measures have been proposed, which include the number and timing of visits, the provider of care and the adequacy of care provided (Delgado‐Rodriguez 1996; Mbuagbaw 2011). Well‐timed ANC visits are critical to the success of some interventions, as a systematic review has shown that adverse outcomes from syphilis can best be prevented by intervening in the first two trimesters (Hawkes 2013). The content of each ANC visit is also important, as some ANC interventions may not be beneficial, such as high does concomitant supplementation with vitamin C and vitamin E to prevent pre‐eclampsia in high‐risk women (Poston 2006). Irrespective of how it is measured, ANC is beneficial and represents an important point of contact with the health system for communication and pregnancy preparedness (Lassi 2015).
For the purposes of this review, coverage will be considered as the proportion of pregnant women who attend at least four ANC visits.
Description of the intervention
The fifth United Nations' Millenium Development Goal (MDG5) targets maternal health and explicitly calls for more ANC (United Nations 2013). The WHO now recommends a package of reduced visits with evidence‐based interventions through goal‐oriented clinic visits (WHO 2011). A variety of interventions can be used to increase the number of women who receive ANC. A systematic review on the effectiveness of interventions to improve early initiation of ANC in vulnerable populations identified two broad categories of interventions: outreach/community‐based interventions and alternative models of clinic‐based ANC. The former included the use of lay health workers and mobile health clinics, while the latter included adaptations of clinic‐based ANC to be more collaborative and comprehensive, and also to accommodate teens (Oakley 2009).
Community‐based interventions such as community support, mobilisation, education and home visits by trained community health workers can lead to significant reductions in maternal morbidity and neonatal mortality, and an increase in referrals to a health facility (Lassi 2015). In underserved areas, a community health van may improve access to adequate ANC (Edgerley 2007).
Other interventions, such as mass media campaigns, social mobilisation, information‐education‐communication (IEC) interventions, financial incentives, behaviour change interventions and policy interventions targeting health workers or pregnant women will also be investigated.
How the intervention might work
Interventions targeting the factors that reduce antenatal care coverage may be beneficial.
Health policy is a critical component of any health system and guides how resources (man power, money and material) are used. Policy can be applied at any level of the health system. Regional health managers are capable of making policy changes that influence the use of ANC services. Recent papers suggest that the effects of policy change in health outcomes should be explored in more detail (Dettrick 2013). Such policy changes may include capacity building in ANC to improve quality of care (Lassi 2015; Say 2007; van Eijk 2006), re‐organisation of services to include more midwives providing ANC (Dowswell 2015; Khan‐Neelofur 1998), and reduction of user fees to eliminate financial barriers (Lassi 2015; Mbuagbaw 2011; Say 2007; Titaley 2010; van Eijk 2006). Where coverage is better in the private sector (Cesar 2012), adopting their (private sector) model of care may be beneficial. Switching to individual counselling sessions may also improve the number of high‐risk women delivering in hospitals (Ballard 2013).
Mass media campaigns can be used to improve the utilisation of health services (Grilli 2002), and may also help to improve the use of ANC services. Social mobilisation ‐ engaging multiple stakeholders ‐ is an important way of bringing change in communities. If pregnant women receive the same consistent message on the benefits of ANC from health workers, community health workers and in other social gatherings, they may be more likely to take heed. Lack of awareness (Lassi 2015; Titaley 2010) and misconceptions (Agus 2012; Say 2007) about ANC can be addressed using IEC sessions. Financial incentives can be used to encourage pregnant women to attend ANC and cover costs including user fees and transportation costs where these problems exist (Lassi 2015; Mbuagbaw 2011; Say 2007; Titaley 2010; van Eijk 2006). They are most effective in the short term, and in resource‐limited settings (Marteau 2009). Behaviour change interventions are interventions derived from a specific model or theory of behaviour change and can play a role in improving health outcomes (Marteau 2006). Such interventions could play an important role in encouraging women to attend ANC.
Why it is important to do this review
Regions of the world with low ANC coverage can benefit from a comprehensive synthesis of the evidence surrounding the ways in which ANC coverage can be improved. In these places, low ANC coverage comes with low rates of deliveries in health facilities and assistance by skilled birth attendants. The latter two factors are associated with high materno‐fetal morbidity. This review will have important implications for reproductive health policy, the provision of services to women in reproductive ages and may highlight gaps in current evidence or openings for further research.
Objectives
To assess the effects of health system and community interventions for improving coverage of antenatal care and other outcomes.
Methods
Criteria for considering studies for this review
Types of studies
We included randomised controlled trials (RCTs), quasi‐randomised trials and cluster‐randomised trials. Trials of cross‐over design were not eligible. Trials reported in abstract form were eligible for inclusion in the review; however, we did not include any trial based on an abstract report alone.
Types of participants
This review included studies of stakeholders, providers of care and beneficiaries, including but not limited to:
professional health workers;
lay health workers;
community members;
pregnant women;
women of reproductive age.
Types of interventions
All interventions susceptible to improve coverage of ANC were eligible for inclusion in this review. These interventions could be aimed at the health system, the population or both. Owing to the potentially wide variety of interventions, there were no restrictions to duration or frequency of the intervention. For the purposes of this review, we classified these interventions into the following two main categories.
Interventions aimed at the health system
Policy changes.
Health worker education.
Re‐organisation of health services.
Interventions aimed at the community
Mass media campaigns.
Social mobilisation.
Information‐education‐communication (IEC).
Financial incentives.
Behaviour change interventions.
Types of outcome measures
Primary outcomes
Coverage of ANC: the proportion of pregnant women who attend at least four ANC visits during pregnancy.
Pregnancy‐related deaths: the proportion of women who die during pregnancy or 42 days after, irrespective of cause (WHO 2004).
Secondary outcomes
Coverage of ANC: the proportion of pregnant women who attend at least one ANC visit during pregnancy.
The proportion of pregnant women who initiate ANC in the first trimester.
The proportion of pregnant women who receive ANC from professional health workers.
The proportion of deliveries in health facilities.
The proportion of pregnant women with a written birth and emergency plan by 37 weeks of pregnancy.
The proportion of pregnant women who receive Intermittent Prophylactic Treatment (IPT) for malaria as per recommended guidelines (WHO 2012b).
The proportion of women with tetanus protection at birth.
The proportion of pregnant women who screen for syphilis.
The proportion of women who screen for asymptomatic bacteriuria.
The proportion of women who screen for HIV.
The proportion of women with HIV who receive a complete antiretroviral course for prevention of mother‐to‐child transmission of HIV.
Maternal near miss, defined as: "a woman who nearly died but survived a complication that occurred during pregnancy, childbirth or within 42 days of termination of pregnancy" (Pattinson 2009).
The proportion of women with preterm labour or delivery.
The proportion of low‐birthweight infants born.
The incidence of perinatal mortality.
We also considered combinations of the above outcomes if the data were not dissociable. For example, the proportion of women who have at least four well‐spaced ANC visits attended by a professional health worker (Mbuagbaw 2011).
Search methods for identification of studies
The following methods section of this review is based on a standard template used by the Cochrane Pregnancy and Childbirth Group.
Electronic searches
We searched the Cochrane Pregnancy and Childbirth Group’s Trials Register by contacting the Trials Search Co‐ordinator (7 June 2015).
The Cochrane Pregnancy and Childbirth Group’s Trials Register is maintained by the Trials Search Co‐ordinator and contains trials identified from:
monthly searches of the Cochrane Central Register of Controlled Trials (CENTRAL);
weekly searches of MEDLINE (Ovid);
weekly searches of Embase (Ovid);
monthly searches of CINAHL (EBSCO);
handsearches of 30 journals and the proceedings of major conferences;
weekly current awareness alerts for a further 44 journals plus monthly BioMed Central email alerts.
Details of the search strategies for CENTRAL, MEDLINE, Embase and CINAHL, the list of handsearched journals and conference proceedings, and the list of journals reviewed via the current awareness service can be found in the ‘Specialized Register’ section within the editorial information about the Cochrane Pregnancy and Childbirth Group.
Trials identified through the searching activities described above are each assigned to a review topic (or topics). The Trials Search Co‐ordinator searches the register for each review using the topic list rather than keywords.
Searching other resources
We searched the reference lists of retrieved studies and contacted authors and experts in the field. We did not apply any language or date restrictions.
Data collection and analysis
The following methods section of this review is based on a standard template used by the Cochrane Pregnancy and Childbirth Group.
Selection of studies
Two review authors (L Mbuagbaw (LM) and N Medley (NM)) independently assessed all the potential studies we identified for inclusion. We resolved any disagreement through discussion or, if required, by consulting a third author (P Ongolo‐Zogo (POZ)). Agreement on the inclusion of studies was estimated using the Kappa statistic (Viera 2005).
A Preferred Reporting Items for Systematic Reviews and Meta‐analyses (PRISMA) study flow diagram was created to map out the number of records identified, included and excluded (Liberati 2009).
Data extraction and management
We designed and tested a form to extract data. For eligible studies (abstract or full text), LM, AD and NM extracted the data using the agreed form. We resolved discrepancies through discussion or, if required, we consulted a third review author (POZ). We entered data into Review Manager software (RevMan 2014) and checked for accuracy.
When information regarding any of the above was unclear, we attempted to contact authors of the original reports to provide further details.
Assessment of risk of bias in included studies
Review authors LM and NM independently assessed risk of bias for each study using the criteria outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). We resolved any disagreement by discussion or by involving a third assessor (POZ).
(1) Random sequence generation (checking for possible selection bias)
We described for each included study the method used to generate the allocation sequence in sufficient detail to allow an assessment of whether it should produce comparable groups.
We assessed the method as:
low risk of bias (any truly random process, e.g. random number table; computer random number generator);
high risk of bias (any non‐random process, e.g. odd or even date of birth; hospital or clinic record number);
unclear risk of bias.
(2) Allocation concealment (checking for possible selection bias)
We described for each included study the method used to conceal allocation to interventions prior to assignment and assessed whether intervention allocation could have been foreseen in advance of, or during recruitment, or changed after assignment.
We assessed the methods as:
low risk of bias (e.g. telephone or central randomisation; consecutively numbered sealed opaque envelopes);
high risk of bias (open random allocation; unsealed or non‐opaque envelopes, alternation; date of birth);
unclear risk of bias (cluster‐RCTs that reported no allocation concealment and RCTs that made no mention of allocation concealment).
(3.1) Blinding of participants and personnel (checking for possible performance bias)
We described for each included study the methods used, if any, to blind study participants and personnel from knowledge of which intervention a participant received. We considered that studies were at low risk of bias if they were blinded, or if we judged that the lack of blinding would be unlikely to affect results. We assessed blinding separately for different outcomes or classes of outcomes.
We assessed the methods as:
low, high or unclear risk of bias for participants;
low, high or unclear risk of bias for personnel.
(3.2) Blinding of outcome assessment (checking for possible detection bias)
We described for each included study the methods used, if any, to blind outcome assessors from knowledge of which intervention a participant received. We assessed blinding separately for different outcomes or classes of outcomes.
We assessed methods used to blind outcome assessment as:
low, high or unclear risk of bias. We entered "unclear risk" for studies that were not blinded for participants/personnel, or where blinding was not described, as most often blinding was not possible due to the nature of the intervention. It is unclear whether a lack of blinding presented a serious risk of bias in cluster‐RCTs with mortality outcomes.
(4) Incomplete outcome data (checking for possible attrition bias due to the amount, nature and handling of incomplete outcome data)
We described for each included study, and for each outcome or class of outcomes, the completeness of data including attrition and exclusions from the analysis. We stated whether attrition and exclusions were reported and the numbers included in the analysis at each stage (compared with the total randomised participants), reasons for attrition or exclusion where reported, and whether missing data were balanced across groups or were related to outcomes. Where sufficient information was reported, or was supplied by the trial authors, we re‐included missing data in the analyses which we undertook.
We assessed methods as:
low risk of bias (e.g. no missing outcome data; missing outcome data balanced across groups);
high risk of bias (e.g. numbers or reasons for missing data imbalanced across groups; ‘as treated’ analysis done with substantial departure of intervention received from that assigned at randomisation);
unclear risk of bias.
Attrition of 20% or more was considered as high risk of bias.
(5) Selective reporting (checking for reporting bias)
We described for each included study how we investigated the possibility of selective outcome reporting bias and what we found.
We assessed the methods as:
low risk of bias (where it is clear that all of the study’s pre‐specified outcomes and all expected outcomes of interest to the review have been reported);
high risk of bias (where not all the study’s pre‐specified outcomes have been reported; one or more reported primary outcomes were not pre‐specified; outcomes of interest are reported incompletely and so cannot be used; study fails to include results of a key outcome that would have been expected to have been reported);
unclear risk of bias.
(6) Other bias (checking for bias due to problems not covered by (1) to (5) above)
We described for each included study any important concerns we had about other possible sources of bias.
We assessed whether each study was free of other problems that could put it at risk of bias:
low risk of other bias;
high risk of other bias;
unclear whether there is risk of other bias.
(7) Overall risk of bias
We made explicit judgements about whether studies were at high risk of bias, according to the criteria given in the Handbook (Higgins 2011). With reference to (1) to (6) above, we assessed the likely magnitude and direction of the bias and whether we considered it was likely to impact on the findings. We explored the impact of the level of bias by undertaking sensitivity analyses ‐ seeSensitivity analysis.
For the cluster‐randomised trials we included, additional sources bias were considered (Higgins 2011), such as:
recruitment bias: whether individuals were recruited into the trial after the clusters had been formed;
baseline imbalances: due to the small numbers of clusters;
attrition of entire clusters;
analysis bias: methods of analysis ignoring the correlation between members of the same cluster;
their comparability with individually‐randomised trials.
Assessing the quality of the body of evidence using the GRADE approach
The quality of the evidence was assessed using the GRADE approach as outlined in the GRADE Handbook in order to assess the quality of the body of evidence relating to the following outcomes.
Coverage of ANC: the proportion of pregnant women who attend at least four ANC visits during pregnancy.
Pregnancy‐related deaths: the proportion of women who die during pregnancy or 42 days after, irrespective of cause (WHO 2004).
Coverage of ANC: the proportion of pregnant women who attend at least one ANC visit during pregnancy.
The proportion of deliveries in health facilities.
The incidence of perinatal mortality.
The proportion of low‐birthweight infants born.
The proportion of pregnant women who receive Intermittent Prophylactic Treatment (IPT) for malaria as per recommended guidelines (WHO 2012b).
The comparisons used to assess the quality of evidence were: Comparison 1: one intervention versus no intervention, and Comparison 2: multiple interventions versus no intervention.
We used the GRADEpro Guideline Development Tool to import data from Review Manager 5.3 (RevMan 2014) in order to create 'Summary of findings' tables. A summary of the intervention effect and a measure of quality for each of the above outcomes was produced using the GRADE approach. The GRADE approach uses five considerations (study limitations, consistency of effect, imprecision, indirectness and publication bias) to assess the quality of the body of evidence for each outcome. The evidence can be downgraded from 'high quality' by one level for serious (or by two levels for very serious) limitations, depending on assessments for risk of bias, indirectness of evidence, serious inconsistency, imprecision of effect estimates or potential publication bias.
We downgraded outcomes for substantial heterogeneity where the I2 > 60%. Because lack of blinding of participants and personnel was nearly universal and would have been prohibitive to the implementation of our included trials, we did not downgrade evidence for lack of blinding during our GRADE assessments. Where we downgraded outcome evidence for risk of bias concerns, these design limitations had to do with the trials' problems with other bias domains, not lack of blinding.
Measures of treatment effect
Dichotomous data
For dichotomous data, we planned to present results as summary risk ratio with 95% confidence intervals. However, the trials in our review reported several different summary effect measures, and the majority presented cluster‐adjusted odds ratios. To make use of these trial data and retain the specific adjustments made by trial statisticians, we have presented our results as odds ratios, with 95% confidence intervals.
Continuous data
For continuous data, we planned to use the mean difference if outcomes were measured in the same way between trials. We would have used the standardised mean difference to combine trials that measured the same outcome, but used different methods.
Unit of analysis issues
Cluster‐randomised trials
We included cluster‐randomised trials in the analyses along with individually‐randomised trials. The review statistician (M Richardson) made appropriate adjustments according to the type of data available from trial reports and through correspondence with authors. Where possible, we adjusted a trials' sample sizes using the methods described in the Handbook using an estimate of the intracluster correlation co‐efficient (ICC) derived from the trial, from a similar trial or from a study of a similar population. We consulted Piaggio 2001, Pagel 2011, Prost 2013, Kidney 2009 and Souza 2013. Professor Souza further provided an ICC for maternal mortality via email. We conducted sensitivity analyses using two extreme values of ICC to investigate the effect of variation in the ICC for the primary outcome only. We have provided details of the specific ICCs used and of any additional methods required to analyse trial data in the additional tables. There is one table of adjustments made for each outcome relevant to the 'Summary of findings' table. Similar details of adjustments made for the analyses of other review outcomes are freely available upon request from the review team.
For cluster‐ and individually‐randomised trials, we considered it reasonable to combine the results from both, if there was little heterogeneity between the study designs and the interaction between the effect of intervention and the choice of randomisation unit was considered to be unlikely. We acknowledged heterogeneity in the randomisation unit, but we have not conducted sensitivity analysis by randomisation unit because all but five of the included trials are cluster‐randomised. Per outcome, there are not sufficient individually‐randomised trials for a subgroup (often just one or no individually‐randomised trial contributed). If in future updates we include several more individually‐randomised trials, we will perform sensitivity analysis, though at present all of the trials in ongoing studies are of cluster‐randomised design.
Other unit of analysis issues
No included trial specifically recruited multiple pregnancies. However, several if not most of the review's trials likely included women with multiple pregnancies. Where this information was provided in trial reports, we have noted this in the Characteristics of included studies table. Results were not reported separately for twins in any included trial. The proportion of twin pregnancies per trial was assumed to be low, and we have not made any adjustments to outcome data for their inclusion.
Some of the included studies had more than one intervention arm. Where appropriate, two intervention arms were combined, and pair‐wise comparisons conducted. Where necessary, we have also split trials. For example, we divided trials if trials had multiple arms and interventions and those interventions were relevant to separate review comparisons. Finally, we have split the control group when necessary to avoid double counting. Please see the included studies tables for Lewycka 2013a and Morris 2004a for specific details.
For quasi‐randomised studies, we planned to use estimates adjusted for baseline imbalances and other confounders.
Dealing with missing data
For included studies, we noted levels of attrition and explored the impact of including studies with high levels of missing data in the overall assessment of treatment effect by using sensitivity analysis.
For all outcomes, we carried out analyses, as far as possible, on an intention‐to‐treat basis, i.e. we attempted to include all participants randomised to each group in the analyses, and all participants were analysed in the group to which they were allocated, regardless of whether or not they received the allocated intervention. The denominator for each outcome in each trial was the number randomised minus any participants whose outcomes were known to be missing.
Assessment of heterogeneity
We assessed statistical heterogeneity in each meta‐analysis using the I², T² and Chi² statistics. We regarded heterogeneity as substantial if an I² was greater than 30% and either a T² was greater than zero, or there was a low P value (less than 0.10) in the Chi² test for heterogeneity. We have left the overall totals turned off only if the effect estimates of different trials were so disparate that it made little clinical sense to combine the trials (for example, if effect estimates fell on opposite sides of the line of no difference and the trials' confidence intervals do not overlap). Overall, even with high heterogeneity in several outcomes, the effect estimates were reasonably similar, and confidence intervals always overlapped. We have not turned off the totals for any outcome listed below.
Assessment of reporting biases
We investigated reporting biases (such as publication bias) using funnel plots. We assessed funnel plot asymmetry visually. If asymmetry was suggested by a visual assessment, we performed exploratory analyses to investigate it.
Data synthesis
We carried out statistical analysis using the Review Manager software (RevMan 2014). We planned to use fixed‐effect meta‐analysis for combining data where it was reasonable to assume that studies were estimating the same underlying treatment effect: i.e. where trials were examining the same intervention, and the trials’ populations and methods were judged sufficiently similar. In practice, we found considerable clinical heterogeneity between the included studies in the review and expected high statistical heterogeneity as a consequence. Therefore, we used random‐effects models to conduct all meta‐analyses. Where high heterogeneity in the overall summary was found, we left analyses pooled and advised readers to interpret the results with caution.
The random‐effects summary was treated as the average range of possible treatment effects and was reported as such, with 95% confidence intervals, and the estimates of T² and I².
We considered the following comparisons.
One intervention versus no intervention.
Two interventions compared.
One intervention versus a combination of interventions.
Combination of interventions versus no intervention.
Different combinations of interventions.
Subgroup analysis and investigation of heterogeneity
We planned to carry out the following subgroup analyses.
Urban versus rural settings.
High‐income versus lower‐income settings.
Interventions targeting the health system versus interventions targeting the population.
These subgroup analyses were limited to the primary outcomes of the review.
We were not able to conduct analyses for urban versus rural settings because our trials were overwhelmingly rural. For example, 14 of 19 trials contributing data for the primary outcome of ANC coverage (at least four visits) took place in rural settings, with just three in urban settings (one trial had mixed settings and one trial report was unclear).
We conducted subgroup analyses comparing trials in upper‐middle and high‐income countries with trials set in low‐ and lower‐middle‐income countries for the outcome of ANC coverage (at least four visits) only (World Bank 2015); there were insufficient data for this analysis for the primary outcome of maternal mortality, because just three of 10 trials contributing data were conducted in higher‐income settings.
We conducted subgroup analysis with trials targeting the health system versus trials targeting the population. All subgroup analyses will be re‐assessed when more trials are added during future updates of the review.
We assessed subgroup differences by interaction tests available within RevMan (RevMan 2014). We reported the results of subgroup analyses quoting the χ2 statistic and P value, and the interaction test I² value.
Sensitivity analysis
Sensitivity analyses were conducted to explore the effects of trial quality and trial design on the outcomes. In the first instance, we compared the results from the studies with high risk of bias with those at low risk of bias, and secondly we investigated the effect of the unit of randomisation (individual versus cluster) on the outcomes. Likewise, we also explored the effects of fixed‐effect or random‐effects analyses for outcomes with statistical heterogeneity and the effects of any assumptions made such as the value of the ICC used for cluster‐randomised trials.
Results
Description of studies
Results of the search
The search of the Cochrane Pregnancy and Childbirth Group's Trials Register retrieved 148 reports; we found three further reports during our own searches (see: Figure 1). We included 34 trials (79 reports) and excluded 30 trials (59 reports). Thirteen studies (13 reports) are ongoing (see Characteristics of ongoing studies), and we await trial completion or the publication of results. We have been unable to locate published data for any of the trials in ‘ongoing studies,’ as of 1 Sept, 2015. Two trials with multiple arms were divided for analyses (Lewycka 2014; Morris 2004), brining the total number of tables for included studies and risk of bias to 36.
1.
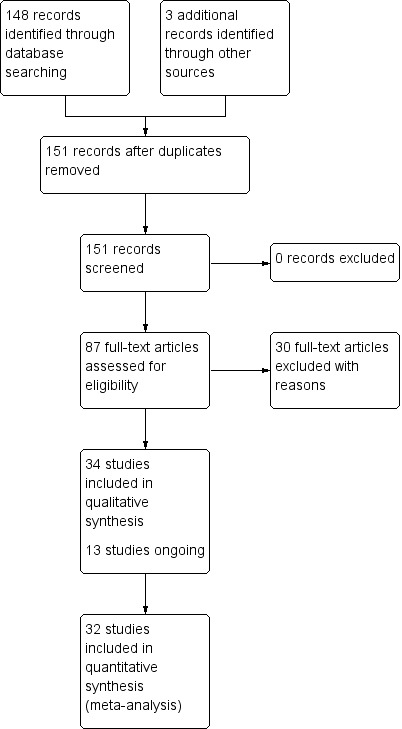
Study flow diagram.
Included studies
A total of 34 trials were identified as eligible for inclusion in this review. Trials involved approximately 400,000 women who were either of reproductive age or pregnant. Ten of the included trials aimed to evaluate health system interventions only (Basinga 2011; Darmstadt 2010; Kenyon 2012; Lund 2012; Majoko 2007; Penfold 2014; Persson 2013; Richter 2014; Villar 2001 (WHO 2001); Walker 2013). One trial with multiple arms aimed to evaluate health system and community interventions separately and together (Morris 2004a). Ten trials evaluated community interventions alone (Barber 2008; Fottrell 2013; Laken 1995; Lewycka 2013a; Manandhar 2004; Melnikow 1997; More 2012; Mori 2015; Mullany 2007; Tripathy 2010). The rest of the trials (13) aimed to evaluate a combination of health system and community interventions (Azad 2010; Baqui 2008; Bhutta 2011; Kirkwood 2013; Klerman 2001; Kumar 2008; le Roux 2013; Midhet 2010; Omer 2008; Villar 1992; Wahlstrom 2011; Waiswa 2015; Wu 2011).
Included trials took place in: Argentina (2), Bangladesh (4), Brazil, Cuba (2), Eastern China, Ghana, Honduras, India (3), Laos, Malawi, Mexico (3), Mongolia, Nepal (2), Pakistan (3), Rwanda, Saudi Arabia, South Africa (2), Southern Tanzania, Thailand, Uganda, United Kingdom, USA (3), Vietnam, Zanzibar and Zimbabwe. Two trials, Villar 1992 and Villar 2001 (WHO 2001), recruited clusters in multiple countries. Five trials were conducted in upper‐middle‐ or high‐income countries (Kenyon 2012; Klerman 2001; Laken 1995; Melnikow 1997; Villar 1992); the remaining trials took place in low‐ or lower‐middle‐income countries. Trials were overwhelmingly rural (22/34), with seven trials in mixed settings and four trials in urban settings; the setting of a final trial was unclear.
All trials were of cluster‐randomised design, apart from five (Kenyon 2012; Klerman 2001; Laken 1995; Melnikow 1997; Mullany 2007). Sample sizes ranged from a few hundred to more than 50,000, while cluster numbers ranged from eight to 506. Follow‐up times ranged from six to 72 months.
Interventions
Ten trials evaluated health system interventions (Basinga 2011; Darmstadt 2010; Kenyon 2012; Lund 2012; Majoko 2007; Penfold 2014; Persson 2013; Richter 2014; Villar 2001 (WHO 2001); Walker 2013). Three of the nine trials included interventions aimed at policy change (Basinga 2011; Lund 2012; Persson 2013). One trial provided financial support to the clusters (Basinga 2011); one trial sent text reminders and mobile credit vouchers (Lund 2012), and one trial held regular stakeholder problem‐solving meetings with generated actions (Persson 2013). Seven trials aimed for reorganisation of the health services (Darmstadt 2010; Kenyon 2012; Majoko 2007; Penfold 2014; Richter 2014; Villar 2001 (WHO 2001); Walker 2013). Four trials added home visits (Darmstadt 2010; Kenyon 2012; Penfold 2014; Richter 2014); two trials restructured the visits (Majoko 2007; Villar 2001 (WHO 2001)), and one trial added an obstetric nurse to rural clinics (Walker 2013).
In a four‐armed trial Morris 2004a tested a policy change, financial support and a combination of the two interventions against no intervention.
Ten trials evaluated community interventions (Barber 2008; Fottrell 2013; Laken 1995; Lewycka 2013a; Manandhar 2004; Melnikow 1997; More 2012; Mori 2015; Mullany 2007; Tripathy 2010). The majority of trials (7/10) were based on Information‐education‐communication (IEC) interventions (Fottrell 2013; Lewycka 2013a; Manandhar 2004; More 2012; Mori 2015; Mullany 2007; Tripathy 2010). Of the seven trials, five held participatory women’s groups (Fottrell 2013; Lewycka 2013a; Manandhar 2004; More 2012; Tripathy 2010); one trial had private education sessions (Mullany 2007), and one trial provided women with their own case notes to carry to antenatal visits (Mori 2015). The other four trials gave financial incentives (Barber 2008; Laken 1995; Melnikow 1997; Morris 2004a).
Thirteen trials were based on combined health system and community interventions (Azad 2010; Baqui 2008; Bhutta 2011; Kirkwood 2013; Klerman 2001; Kumar 2008; le Roux 2013; Midhet 2010; Omer 2008; Villar 1992; Wahlstrom 2011; Waiswa 2015; Wu 2011). Several trials provided IEC as a community intervention. These included: participatory women’s groups (Azad 2010), community awareness meetings (Baqui 2008; Bhutta 2011; Klerman 2001; Kumar 2008; Wahlstrom 2011); the provision of information booklets and cassettes and mass media campaigns (Midhet 2010; Villar 1992; Wu 2011); and home education sessions (Kirkwood 2013; le Roux 2013; Omer 2008). Azad 2010, Bhutta 2011, Kirkwood 2013, Midhet 2010, Waiswa 2015, and Wu 2011 provided healthcare worker training as a health system package to the intervention group. Baqui 2008 offered surveillance and home visits (two ANC, three perinatal mortality rate (PNC)) by community health workers (CHWs) and the provision of iron and folic acid supplements. Four other trials also added home visits as a health system intervention (Kumar 2008; le Roux 2013; Villar 1992; Waiswa 2015), while Klerman 2001 added additional clinic visits and extended time with clinicians. Kumar 2008 provided home visits with thermo‐spot and home visits without thermo‐spot as health system interventions. Wu 2011, Wahlstrom 2011 and Waiswa 2015 each also provided equipment and/or medicines for health centres.
Outcomes
Apart from the trial primary outcome, the outcomes listed in the Characteristics of included studies tables refer to this review's prespecified primary and secondary outcomes. All trials reported additional outcomes not relevant to our review beyond those listed in the Characteristics of included studies tables.
Many trials had multiple primary outcomes including different combinations of the following priorities: neonatal and perinatal mortality, antenatal care coverage, healthcare utilisation, newborn care practices (including exclusive breastfeeding), maternal physical and mental health (including postpartum anaemia, treated urinary tract infection, indicators of social support, maternal depression, use of folic acid during pregnancy, tetanus immunisation, birth preparedness and satisfaction with care) and delivery practices (including assisted delivery, hospital delivery). Our 34 included trials had 23 different primary outcomes. Even with this diversity, our included trials most commonly targeted antenatal care coverage and neonatal mortality. Sixteen trials had primary outcomes with a specific antenatal care coverage component (Basinga 2011; Darmstadt 2010; Laken 1995;, Majoko 2007; Melnikow 1997; Midhet 2010; More 2012; Mori 2015; Morris 2004, Mullany 2007; Omer 2008; Richter 2014; Wahlstrom 2011; Waiswa 2015; Walker 2013; Wu 2011), and 12 trials targeted neonatal or perinatal mortality (Azad 2010; Baqui 2008; Bhutta 2011; Fottrell 2013; Kirkwood 2013; Kumar 2008; Lewycka 2013; Manandhar 2004; Midhet 2010; More 2012; Persson 2013; Tripathy 2010).
One trial was included based on unpublished data only (Wahlstrom 2011). Two included trials contributed no usable outcome data to the review (Melnikow 1997; Omer 2008). The trial statistician for Mori 2015 provided unpublished, cluster‐adjusted odds ratios for our use. See the Included studies tables for further details.
Excluded studies
Thirty trials were excluded from the review. Briefly, 27 trials did not assess an increase in antenatal care coverage as a central objective of the trial (Baqui 2009; Bhutta 2008; Colbourn 2013; Dance 1987; Doyle 2014; Ellard 2012; Ford 2001; Gokcay 1993; Homer 2001; Ickovics 2007; Jennings 2010; Kafatos 1989; Koniak‐Griffin 1991; Koniak‐Griffin 2000; Kusulasai 1993; Leung 2012; Miller 2012; Munjanja 1996; Olds 1986; Olds 1995a; Rodriguez‐Angulo 2012; Schellenberg 2011; Srinivasan 1995; Tomlinson 2014; Tough 2006; Tough 2007; Turan 2001). Three studies were excluded for being of observational study design (Alisjahbana 1995; Foord 1995; Magriples 2008). See the Characteristics of excluded studies table for more details.
Risk of bias in included studies
Because two included trials with multiple arms have been divided (Lewycka 2013 and Morris 2004), the total number of studies assessed for bias below is 36, rather than 34.
For the most part, risk of bias was low or unclear. See Figure 2 and Figure 3. In our overall risk assessment only four studies were at high risk of bias: Omer 2008 (data not reported according to randomisation, unclear denominators); Walker 2013 (all data based on provider recall); Wu 2011 (unclear denominators, other interventions in trial area and poor implementation) and Wahlstrom 2011 (unpublished data, unclear analyses). In 16 trials, overall risk of bias was unclear (Basinga 2011; Darmstadt 2010; Fottrell 2013; Laken 1995; le Roux 2013; Lewycka 2013b; Lewycka 2013a; Melnikow 1997; Midhet 2010; More 2012; Morris 2004b; Morris 2004a; Persson 2013; Richter 2014; Tripathy 2010; Waiswa 2015), and it was low in 16 trials (Azad 2010; Baqui 2008; Barber 2008; Bhutta 2011; Kenyon 2012; Kirkwood 2013; Klerman 2001; Kumar 2008; Lund 2012; Majoko 2007; Manandhar 2004; Mori 2015; Mullany 2007; Penfold 2014; Villar 1992; Villar 2001 (WHO 2001)).
2.
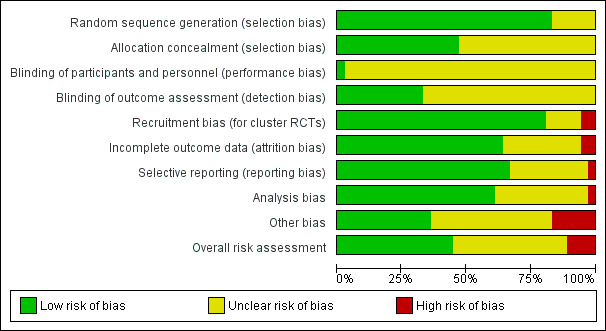
'Risk of bias' graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
3.
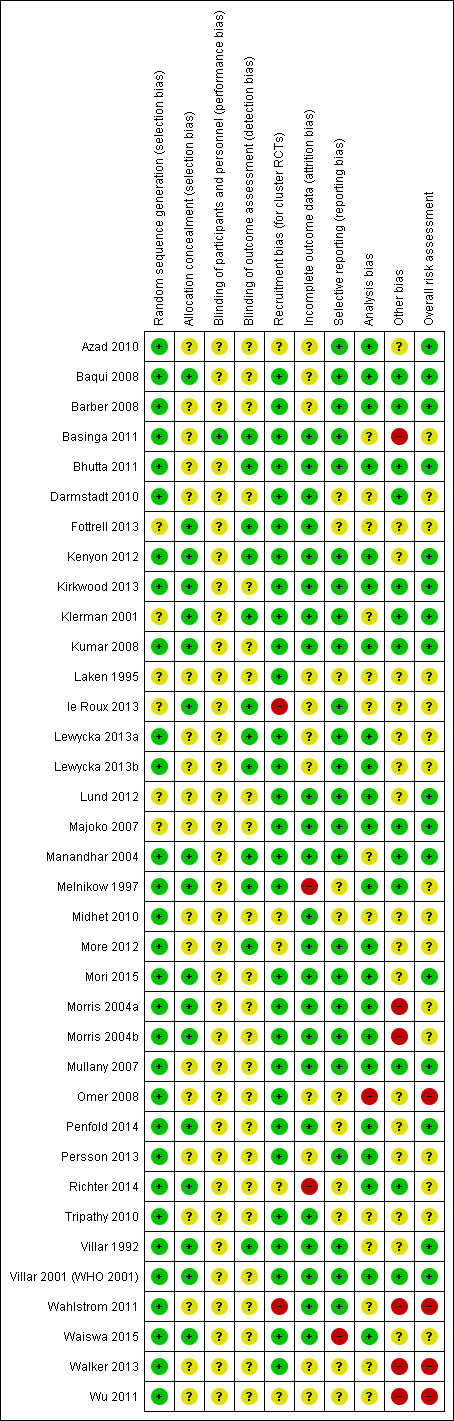
'Risk of bias' summary: review authors' judgements about each risk of bias item for each included study.
Allocation
Random sequence generation
Random sequence generation was adequate (low risk of bias) in 30 trials (Azad 2010; Baqui 2008; Barber 2008; Basinga 2011; Bhutta 2011; Darmstadt 2010; Kenyon 2012; Kirkwood 2013; Kumar 2008; Lewycka 2013a; Lewycka 2013b; Manandhar 2004; Melnikow 1997; Midhet 2010; More 2012; Mori 2015; Morris 2004a; Morris 2004b; Mullany 2007; Omer 2008; Penfold 2014; Persson 2013; Richter 2014; Tripathy 2010; Villar 1992; Villar 2001 (WHO 2001); Wahlstrom 2011; Waiswa 2015; Walker 2013; Wu 2011), and unclear in six trials (Fottrell 2013; Klerman 2001; Laken 1995; le Roux 2013; Lund 2012; Majoko 2007).
Allocation concealment
Seventeen trials were at low risk of bias for allocation concealment (Baqui 2008; Fottrell 2013; Kenyon 2012; Kirkwood 2013; Klerman 2001; Kumar 2008; le Roux 2013; Manandhar 2004; Melnikow 1997; Mori 2015; Morris 2004a; Morris 2004b; Penfold 2014; Richter 2014; Villar 1992; Villar 2001 (WHO 2001); Waiswa 2015). Risk of bias was unclear in 19 trials, where allocation concealment was unclear or not described at all (Azad 2010; Barber 2008; Basinga 2011; Bhutta 2011; Darmstadt 2010; Laken 1995; Lewycka 2013a; Lewycka 2013b; Lund 2012; Majoko 2007; Midhet 2010; More 2012; Mullany 2007; Omer 2008; Persson 2013; Tripathy 2010; Wahlstrom 2011; Walker 2013; Wu 2011).
Blinding
Generally, blinding was not feasible in the trials included in this review. Large cluster‐randomised trials with community or health‐system relevant interventions will not achieve adequate blinding of women and staff. Most trials did make an attempt to prevent contamination between clusters, though. Where trial authors have reported lack of blinding, we have judged this to be of unclear risk of bias because we do not know for certain what kinds of bias may or may not have been introduced. We determined that it was unfair to judge studies that reported a lack of blinding as having a high risk of bias and studies that did not report at all as unclear risk of bias, when blinding might not have been feasible. The risk of bias in all trials due to lack of blinding will differ per outcome, and the impact of no blinding in cluster trials measuring mortality outcomes is also unclear. Where trials did not report blinding at all in published reports, we judged the trial as of unclear risk of bias due to lack of information. Overall, included trials did a much better job of attempting to blind outcomes assessors than participants and personnel.
Blinding of participants and personnel
Only one trial had adequate blinding of participants and low risk of bias (Basinga 2011). Thirty‐five trials had unclear risk of bias; these trials were either not blinded or the blinding of participants was not reported. (Azad 2010; Barber 2008; Baqui 2008; Bhutta 2011; Darmstadt 2010; Fottrell 2013; Kenyon 2012; Kirkwood 2013; Klerman 2001; Kumar 2008; Laken 1995; le Roux 2013; Lewycka 2013a; Lewycka 2013b; Lund 2012; Majoko 2007; Manandhar 2004; Melnikow 1997; Midhet 2010; More 2012; Mori 2015; Morris 2004a; Morris 2004b; Mullany 2007; Omer 2008; Penfold 2014; Persson 2013; Richter 2014; Tripathy 2010; Villar 1992; Villar 2001 (WHO 2001); Walker 2013; Wahlstrom 2011; Waiswa 2015; Wu 2011).
Blinding of outcome assessors
Twelve trials were at low risk of bias due to explicit blinding of data collectors and interviewers (Basinga 2011; Bhutta 2011; Fottrell 2013; Kenyon 2012; Klerman 2001; le Roux 2013; Lewycka 2013a; Lewycka 2013b; Manandhar 2004; Melnikow 1997; More 2012; Villar 1992). Twenty‐four trials were judged to have unclear risk of bias due to either no mention of blinding or lack of blinding of those collecting data (Azad 2010; Baqui 2008; Barber 2008; Darmstadt 2010; Kirkwood 2013; Kumar 2008; Laken 1995; Lund 2012; Majoko 2007; Midhet 2010; Mori 2015; Morris 2004a; Morris 2004b; Mullany 2007; Omer 2008; Penfold 2014; Persson 2013; Richter 2014; Tripathy 2010; Villar 2001 (WHO 2001); Wahlstrom 2011; Waiswa 2015; Walker 2013; Wu 2011).
Incomplete outcome data
Twenty‐three trials were at low risk of bias with clear reporting of losses to follow‐up (Basinga 2011; Bhutta 2011; Darmstadt 2010; Fottrell 2013; Kenyon 2012; Kirkwood 2013; Klerman 2001; Kumar 2008; Lund 2012; Majoko 2007; Manandhar 2004; Midhet 2010; More 2012; Mori 2015, Morris 2004a; Morris 2004b; Mullany 2007; Penfold 2014, Tripathy 2010; Villar 1992; Villar 2001 (WHO 2001), Wahlstrom 2011; Waiswa 2015). Risk of bias was unclear in 11 trials due to confusing reporting or lack of reporting of follow‐up (Azad 2010; Baqui 2008; Barber 2008; Laken 1995; le Roux 2013; Lewycka 2013a; Lewycka 2013b; Omer 2008; Persson 2013; Walker 2013; Wu 2011). One small trial was at high risk of bias due to 32% attrition (22/69) in the intervention arm lost to follow‐up and excluded (Melnikow 1997). Another trial (Richter 2014) also had poor follow‐up and was assessed as of high risk of bias (follow‐up: 70% at post‐birth interview; 57% at six months; 24% at 12 months).
Selective reporting
Twenty‐four studies were at low risk of bias (Azad 2010; Baqui 2008; Barber 2008; Basinga 2011; Bhutta 2011; Kenyon 2012; Kirkwood 2013; Klerman 2001; Kumar 2008; le Roux 2013; Lewycka 2013a; Lewycka 2013b; Lund 2012; Majoko 2007; Manandhar 2004; More 2012; Mori 2015, Morris 2004a; Morris 2004b; Mullany 2007; Persson 2013; Villar 1992; Villar 2001 (WHO 2001); Wahlstrom 2011), and in 11, risk of bias was unclear (Darmstadt 2010; Fottrell 2013; Laken 1995; Melnikow 1997; Midhet 2010; Omer 2008; Penfold 2014; Richter 2014; Tripathy 2010; Walker 2013; Wu 2011). One trial (Waiswa 2015) was assessed as of high risk because the authors have not yet published mortality data; preterm birth was also mentioned in the publication but no data reported; finally, data for low birthweight were not reported according to intervention arm in Waiswa 2015.
Other potential sources of bias
Recruitment bias
Twenty‐six trials were at low risk of bias (Baqui 2008; Barber 2008; Basinga 2011; Bhutta 2011; Darmstadt 2010; Fottrell 2013; Kenyon 2012; Kirkwood 2013; Klerman 2001; Kumar 2008; Laken 1995; Lewycka 2013a; Lund 2012; Majoko 2007; Manandhar 2004; Melnikow 1997; Morris 2004a; Mullany 2007; Omer 2008; Penfold 2014; Persson 2013; Tripathy 2010; Villar 1992; Villar 2001 (WHO 2001); Waiswa 2015; Walker 2013). Risk of bias was unclear for six trials (Azad 2010; Midhet 2010; More 2012; Mori 2015; Richter 2014; Wu 2011) and high for two trials: le Roux 2013 (recruiters were redeployed to control clusters due to 22% fewer women in standard care) and Wahlstrom 2011 (authors reported problems with recruitment in the intervention clusters for the post‐intervention survey).
Analysis bias
Twenty‐two trials were at low risk of bias with clear reporting of methods used for adjustments and analysis (Azad 2010; Baqui 2008; Barber 2008; Bhutta 2011; Kenyon 2012; Kirkwood 2013; Kumar 2008; Lewycka 2013a; Lewycka 2013b; Lund 2012; Majoko 2007; Melnikow 1997; More 2012; Mori 2015; Morris 2004a; Morris 2004b: Mullany 2007; Penfold 2014; Persson 2013; Richter 2014; Villar 2001 (WHO 2001); Waiswa 2015). Risk of bias was unclear in 13 trials, largely due to missing ICCs and unclear methods of adjusting for clustering (Basinga 2011; Darmstadt 2010; Fottrell 2013; Klerman 2001; Laken 1995; le Roux 2013; Manandhar 2004; Midhet 2010; Tripathy 2010; Villar 1992; Wahlstrom 2011; Walker 2013; Wu 2011), and high in one trial, where results were not reported according to the randomisation group (Omer 2008).
Other bias
In this section we assessed the trials for issues such as baseline imbalances, respect of allocation assignment, similarities between clusters, information bias, parallel non‐trial interventions, changes in general living conditions and implementation of the intervention. Thirteen trials did not seem to have any other sources of bias (Baqui 2008; Barber 2008; Bhutta 2011; Darmstadt 2010; Kirkwood 2013; Klerman 2001; Kumar 2008; Majoko 2007; Manandhar 2004; Melnikow 1997; Mullany 2007; Richter 2014; Villar 2001 (WHO 2001)). In 17 trials it was unclear how these issues might have introduced bias (Azad 2010; Fottrell 2013; Kenyon 2012; Laken 1995; le Roux 2013; Lewycka 2013a; Lewycka 2013b; Lund 2012; Midhet 2010; More 2012; Mori 2015; Omer 2008; Penfold 2014; Persson 2013; Tripathy 2010; Villar 1992; Waiswa 2015). Five trials were at high risk of bias from one or more of these sources: Basinga 2011 (allocation assignment was not respected due to government restructuring); Morris 2004a and Morris 2004b (unsuccessful implementation of service‐level package in relevant clusters); Wahlstrom 2011 (baseline differences and recall bias for ANC visits outcome); Walker 2013 (baseline differences, recall and reporting bias); and Wu 2011 (baseline differences, unclear implementation)
Effects of interventions
Summary of findings for the main comparison. One intervention versus no intervention.
| Comparison 1: One intervention versus no intervention | ||||||
| Patient or population: improving antenatal care coverage and health outcomes among pregnant women Setting: Argentina, Bangladesh, Brazil, Cuba, Ghana, Honduras, India, Malawi, Mexico, Mongolia, Nepal, Rwanda, South Africa, Tanzania, UK, Vietnam, Zanzibar, Zimbabwe Intervention: One intervention Comparison: No intervention | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Risk with no intervention | Risk with One intervention | |||||
| ANC coverage: four or more visits | Moderate | Average OR 1.11 (1.01 to 1.22) | 45022 (10 RCTs) | ⊕⊕⊕⊕ HIGH1 | This is the primary analysis, ICC 0.02. | |
| 529 per 1000 | 555 per 1000 (531 to 578) | |||||
| Pregnancy‐related deaths | Moderate | Average OR 0.69 (0.45 to 1.08) | 114930 (10 RCTs) | ⊕⊕⊝⊝ LOW 2 3 | ||
| 700 per 1000000 | 483 per 1000000 (315 to 756) | |||||
| ANC coverage: one or more visits | Moderate | Average OR 1.68 (1.02 to 2.79) | 19281 (6 RCTs) | ⊕⊕⊕⊝ MODERATE 4 | ||
| 490 per 1000 | 617 per 1000 (495 to 728) | |||||
| Deliveries in a health facility | Moderate | Average OR 1.08 (1.02 to 1.15) | 74299 (10 RCTs) | ⊕⊕⊕⊕ HIGH | ||
| 645 per 1000 | 662 per 1000 (650 to 676) | |||||
| Perinatal mortality | Moderate | Average OR 0.96 (0.89 to 1.03) | 189164 (15 RCTs) | ⊕⊕⊕⊝ MODERATE 2 5 | ||
| 40 per 1000 | 38 per 1000 (36 to 41) | |||||
| Low birthweight | Moderate | Average OR 0.94 (0.82 to 1.06) | 27154 (5 RCTs) | ⊕⊕⊕⊕ HIGH | ||
| 125 per 1000 | 118 per 1000 (105 to 132) | |||||
| Intermittent Prophylactic Treatment for malaria | Study population | not pooled | 00 (0 study) | No trial included in this review reported this outcome. | ||
| not pooled | not pooled | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio; OR: Odds ratio. Denominators for the calculation of the absolute comparative effects have been taken from individual trial reports or from Prost 2013. Where different denominators are stated in different reports, we have taken the larger. The median control group risk has been calculated from event and participant raw data, where this was available. If we found no raw event and participant data in published reports, these trials were not included in the calculation of the median control group risk. Both the participant totals and the median control group risk are for illustrative purposes only. In the majority of the trials in this review, the final odds ratio presented will not correspond with raw event and participant data due to adjustments made for the effects of cluster design. We have designated the control risk as moderate because it is based on the median of a wide range of baseline rates in control groups. | ||||||
| GRADE Working Group grades of evidence High quality: We are very confident that the true effect lies close to that of the estimate of the effect Moderate quality: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low quality: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low quality: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | ||||||
1 Statistical heterogeneity, I2 = 52%; we did not downgrade for heterogeneity unless the I2 > 60%.
2 Downgraded one level due to serious risk of bias. Most weight from trials with design limitations (‐1).
3 Downgraded one level due to serious imprecision. Wide confidence interval crossing the line of no effect (‐1).
4 Downgraded one level due to serious inconsistency. Statistical heterogeneity, I2= 76% (‐1).
5 Statistical heterogeneity, I2= 58%; we did not downgrade for heterogeneity unless the I2 > 60%.
Summary of findings 2. Combination of interventions versus no intervention.
| Comparison 2: Combination of interventions versus no intervention | ||||||
| Patient or population: improving antenatal care coverage and health outcomes among pregnant women Setting: Eastern China, Honduras, India, Laos, Malawi, Pakistan, South Africa, USA Intervention: Combination of interventions Comparison: No intervention | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Risk with no intervention | Risk with Combination of interventions | |||||
| ANC coverage: four or more visits | Moderate | Average OR 1.48 (0.99 to 2.21) | 7840 (6 RCTs) | ⊕⊕⊝⊝ LOW 1 2 3 | This is the primary analysis, ICC 0.02. | |
| 430 per 1000 | 528 per 1000 (428 to 625) | |||||
| Pregnancy‐related deaths | Moderate | Average OR 0.70 (0.39 to 1.26) | 13756 (3 RCTs) | ⊕⊕⊕⊝ MODERATE 3 | ||
| 600 per 100000 | 421 per 100000 (235 to 755) | |||||
| ANC coverage: one or more visits | Moderate | Average OR 1.79 (1.47 to 2.17) | 12426 (5 RCTs) | ⊕⊕⊕⊝ MODERATE 3 | ||
| 580 per 1000 | 712 per 1000 (670 to 750) | |||||
| Deliveries in a health facility | Moderate | Average 1.53 (0.96 to 2.43) | 12314 (5 RCTs) | ⊕⊕⊕⊝ MODERATE 3 | ||
| 165 per 1000 | 252 per 1000 (158 to 401) | |||||
| Perinatal mortality | Moderate | Average 0.74 (0.57 to 0.95) | 39130 (5 RCTs) | ⊕⊕⊕⊝ MODERATE 4 | ||
| 90 per 1000 | 67 per 1000 (51 to 58) | |||||
| Low birthweight | Moderate | Average 0.61 (0.46 to 0.80) | 2084 (2 RCTs) | ⊕⊕⊕⊝ MODERATE 1 | ||
| 165 per 1000 | 101 per 1000 (76 to 132) | |||||
| Intermittent Prophylactic Treatment for malaria | Study population | not pooled | 00 (0 study) | No trial eligible for this comparison reported this outcome | ||
| not pooled | not pooled | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI).CI: Confidence interval; RR: Risk ratio; OR: Odds ratio. Denominators for the calculation of the absolute comparative effects have been taken from individual trial reports or from Prost 2013. Where different denominators are stated in different reports, we have taken the larger. The median control group risk has been calculated from event and participant raw data, where this was available. If we found no raw event and participant data in published reports, these trials were not included in the calculation of the median control group risk. Both the participant totals and the median control group risk are for illustrative purposes only. In the majority of the trials in this review, the final odds ratio presented will not correspond with raw event and participant data due to adjustments made for the effects of cluster design. We have designated the control risk as moderate because it is based on the median of a wide range of baseline rates in control groups. | ||||||
| GRADE Working Group grades of evidence High quality: We are very confident that the true effect lies close to that of the estimate of the effect Moderate quality: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low quality: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low quality: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | ||||||
1 Most weight from trials with design limitations (‐1).
2 Statistical heterogeneity, I2 = 48% ; we did not downgrade for heterogeneity unless the I2 > 60%.
3 Wide confidence interval crossing the line of no effect (‐1).
4 Statistical heterogeneity, I2 = 83% (‐1).
All analyses below were conducted with a random‐effects model, because we expected and have found high heterogeneity due to differences in the interventions and targets of individual trials. We have reported the pooled effect estimates below and explained substantial heterogeneity findings where they occur, noting especially if the exclusion of trials of high risk of bias improved heterogeneity. In all analyses below we have combined cluster‐randomised with individually‐randomised trials. Most analysis have few, if any, individually‐randomised trials. We have specifically noted where individually‐randomised trials contribute outcome data.
We have included group totals on the forest plots for the review primary outcomes, for the first two comparisons. These numbers are for illustrative purposes only.
We have also included additional tables with event and participant totals for the outcomes relevant to our 'Summary of findings' tables.
GRADE assessments are found in parenthesis following estimates for 'Summary of findings' outcomes. We did not downgrade outcomes for heterogeneity if the I2 was not greater than 60%.
Comparison 1: One intervention versus no intervention
All trials contributing data to the meta‐analyses for this comparison were of cluster design, apart from one trial Kenyon 2012 (n = 1324; contributing data to outcomes for the main analyses Analysis 1.1; Analysis 1.11, and Analysis 1.13; and for subgroup and sensitivity analyses Analysis 6.1; Analysis 7.1; and Analysis 8.1.
1.1. Analysis.
Comparison 1 One intervention versus no intervention, Outcome 1 ANC coverage: four or more visits.
1.11. Analysis.
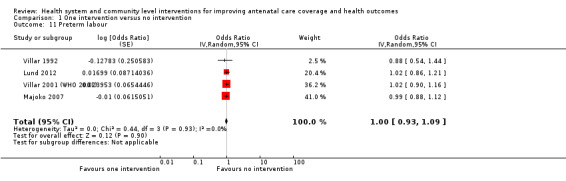
Comparison 1 One intervention versus no intervention, Outcome 11 Preterm labour.
1.13. Analysis.
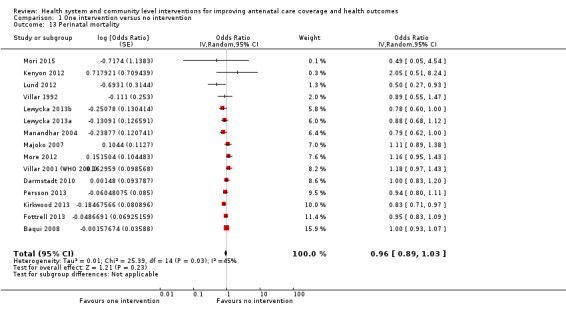
Comparison 1 One intervention versus no intervention, Outcome 13 Perinatal mortality.
6.1. Analysis.
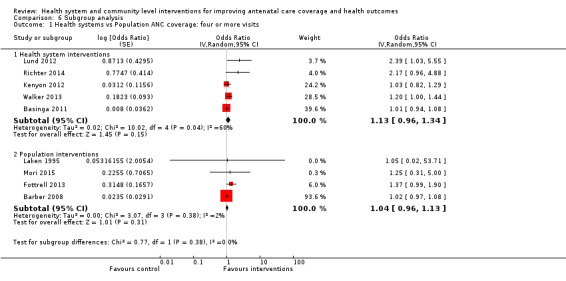
Comparison 6 Subgroup analysis, Outcome 1 Health systems vs Population ANC coverage: four or more visits.
7.1. Analysis.
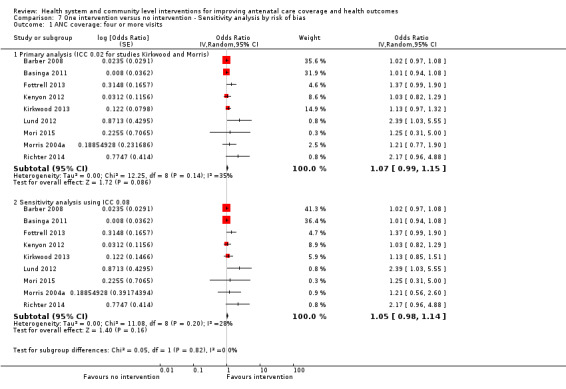
Comparison 7 One intervention versus no intervention ‐ Sensitivity analysis by risk of bias, Outcome 1 ANC coverage: four or more visits.
8.1. Analysis.
Comparison 8 Combination of interventions versus no intervention ‐ Sensitivity analysis by risk of bias, Outcome 1 ANC coverage: four or more visits.
Overall, meta‐analyses identified modest effects for single interventions on two review outcomes. More women in intervention groups received at least four antenatal care visits (high quality evidence) and delivered their babies in health facilities (high quality evidence).
Primary outcomes
Antenatal care (ANC) coverage: four or more visits ‐ results for this outcome had high heterogeneity, as would be expected due to differences among the trials' interventions and targets. Using an intra‐cluster correlation co‐efficient (ICC) of 0.02 showed marginal results favouring the interventions and substantial heterogeneity (average odds ratio (OR) 1.11, 95% confidence interval (CI) 1.01 to 1.22; studies = 10; 45,022 women; Heterogeneity: Tau² = 0.01; (P = 0.03); I² = 52%; GRADE assessment = high quality evidence). The pooled effect using a more conservative ICC of 0.08 showed a similar marginal result in ANC coverage between treatment arms and substantial heterogeneity (average OR 1.11, 95% CI 1.00 to 1.22; studies = 10; Heterogeneity: Tau² = 0.01; (P = 0.04); I² = 49%). See Analysis 1.1. See also Table 3.
1. Primary outcome 1.1 Proportion of women with at least 4 ANC visits.
| Study | Measure of effect | Statistical approach1 | Intervention | Control |
| Barber 2008 | Beta coefficient: 0.0235 (Cash transfer, instrumental variable model; p. 1411, Barber 2008) | Calculate exp(beta) to get OR and CI | 712 | 180 |
| Basinga 2011 | Beta (95% CI): 0.008 (‐0.063 to 0.079) | Calculate exp(beta) to get OR and CI | Reported only the total n, stated as = 2223 | |
| Fottrell 2013 | Adjusted Odds Ratio (95%CI) 1.37 (0.99 to 1.88) | Cluster adjusted, straight into RevMan | 9106 | 8834 |
| Kenyon 2012 | RR = 1.01 (95% CI 0.91 to 1.13) | Non‐cluster trial, calculated OR | 322/599 | 320/604 |
| Kirkwood 2013 | RR 1·02 (0·96 to 1·09) | Adjusted using ICC 0.02 | 5975/7859 | 5988/8121 |
| Lund 2012 | Adjusted OR 2.39 (1.03 to 5.55) adjusted for cluster effect and significant variables | Cluster adjusted, straight into RevMan | 574/1311 | 385/1239 |
| Mori 2015 | Adjusted OR 1.25 (0.31 to 5.00) trial statistician (H Noma) calculated unpublished OR for this systematic review. OR adjusted for cluster effect and significant variables. | Cluster adjusted, straight into RevMan | 243/252 | 237/248 |
| Morris 2004 (Household package arm and service package arm added together) | Calculated from change scores, Table 2 Program effects p. 2034 of main report. | Adjusted using ICC 0.02 | 166/293 + 112/232 | 151/313 |
| Walker 2013 | Adjusted OR 95% CI 1.8(1.2 to 2.8). OR adjusted various characteristics and cluster ('in accordance with WHO standards' from Table 3, p. 1203 Walker 2013) | Cluster adjusted, straight into RevMan | 78/1129 | 39/924 |
1Main analysis with ICC of 0.02. We decided to use the same ICC for this outcome as for Proportion of women with one ANC visit. ICC of 0.02 provided in Manandhar 2004 and Wu 2011. We performed sensitivity analyses with the ICC of 0.08, a midrange of the ICC values in Pagel 2011.
Pregnancy‐related deaths ‐ pooled results showed no clear benefits for women receiving an intervention (average OR 0.69, 95% CI 0.45 to 1.08; studies = 11; 114,930 women; GRADE assessment = low quality evidence, due to design limitations of trials and wide CIs crossing the line of no effect; Analysis 1.2). See also Table 4. We split the control group between Lewycka 2013a and Lewycka 2013b for analysis, so no results have been double counted.
1.2. Analysis.
Comparison 1 One intervention versus no intervention, Outcome 2 Pregnancy‐related deaths.
2. Primary outcome 1.2 Pregnancy related deaths.
| Study | Measure of effect | Statistical approach1 | Intervention | Control |
| Lewycka 20132 women's groups only | Adjusted | 14/4773 | 15/2530 | |
| Lewycka 2013a peer counselling only | Adjusted | 18/4690 | 14/2529 | |
| Lund 2014 | Adjusted | 4/1351 | 1/1286 | |
| Majoko 2007 | OR 1.94 (0.31‐15.2) | Adjusted raw data because the reported OR is asymmetrical. No reply from trial authors regarding our query. | 4/6696 | 2/6483 |
| Manandhar 2004 | Adjusted | 2/2899 | 11/3226 | |
| More 2012 | Adjusted | 20/7656 | 24/7536 | |
| Mori 2015 | Continuity correction for no events in either treatment arm. Unpublished data provided by trial author | 0/252 | 0/248 | |
| Persson 2013 | Adjusted | 1/11,906 | 4/10655 | |
| Fottrell 2013 | Adjusted | 14/8819 | 23/8602 | |
| Villar 2001 | Adjusted | 7/11672 | 6/11121 |
1All data adjusted using an ICC of 0.00247 as suggested by Professor J P Souza by email.
2Mortality data from Trial Profile (Lewycka 2013, p. 1724). Control group (n = 5059) split for this analysis.
Sensitivity analyses
We performed sensitivity analysis for the review primary outcomes of ANC coverage: four or more visits and pregnancy‐related deaths by excluding trials with an overall assessment of high risk of bias. ANC coverage: four or more visits was recalculated without Walker 2013. Results are shown in Analysis 7.1. Heterogeneity was reduced from 52% and 49% (using two ICCs) with Walker 2013 to 35% and 28% without. The pooled result shows no group differences in rates of ANC coverage, whether using an ICC of 0.02 (average OR 1.07, 95% CI 0.99 to 1.15; studies = nine; Heterogeneity: Tau² = 0.00; (P = 0.14); I² = 35%) or an ICC of 0.08 (average OR 1.05, 95% CI 0.98 to 1.14; studies = nine; Heterogeneity: Tau² = 0.00; (P = 0.20); I² = 28%). These two ICCs were obtained from reports of other studies (Manandhar 2004; Wu 2011; Pagel 2011) and were used to determine the robustness of our findings to assumptions about the correct ICC.
Secondary outcomes
ANC coverage: one or more visits ‐ pooled results show marginal improvement in coverage in the intervention arms; however, due to high levels of heterogeneity we would question whether this result is meaningful (average OR 1.68, 95% CI 1.02 to 2.79; studies = six; Heterogeneity: Tau² = 0.24;(P = 0.0009); I² = 76%; GRADE assessment = moderate quality evidence, downgraded once for high statistical heterogeneity; Analysis 1.3). See also Table 5.
1.3. Analysis.
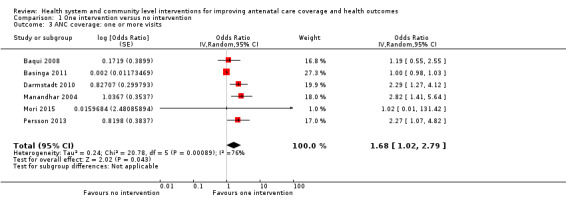
Comparison 1 One intervention versus no intervention, Outcome 3 ANC coverage: one or more visits.
3. SOF outcome 1.3 ANC coverage: one or more visits.
| Study | Measure of effect | Statistical approach1 | Intervention | Control |
| Basinga 2011 | beta (95% CI): 0.002 (‐0.021 to 0.025); | Calculated ln (OR) and se (ln OR) | Reported only the total n = 2309 | |
| Baqui 2008 | Adjusted | 2297/3421 | 828/1689 | |
| Darmstadt 2010 | Adjusted | 1192/1732 | 864/1759 | |
| Manandhar 2004 | Adjusted OR 2.82 (1.41 to 5.62) | Straight into RevMan. Worked out what ICC they used to adjust for clustering | 1747/3190 | 1051/3524 |
| Mori 2015 | Adjusted OR 1.02 (0.01 to 131.42) trial statistician provided unpublished OR adjusted for clustering and significant variables | Straight into RevMan | 252/252 | 248/248 |
| Persson 2013 | Adjusted OR 2.27 95% CI 1.07 to 4.80. For years 1‐3. | Straight into RevMan | 596/656 | 482/587 |
1ICC of 0.02 provided in Manandhar 2004 and Wu 2011.
Pregnant women initiating ANC in the first trimester ‐ one trial reported this outcome with similar rates of ANC in treatment arms (average OR 1.20, 95% CI 0.99 to 1.45; studies = one; Analysis 1.4).
1.4. Analysis.
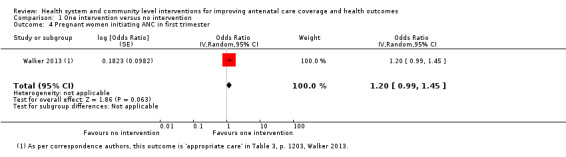
Comparison 1 One intervention versus no intervention, Outcome 4 Pregnant women initiating ANC in first trimester.
Pregnant women receiving ANC from a health professional ‐ one trial reported this outcome with no evidence of benefit for the intervention arm (average OR 1.13, 95% CI 0.84 to 1.52; studies = one; Analysis 1.5).
1.5. Analysis.
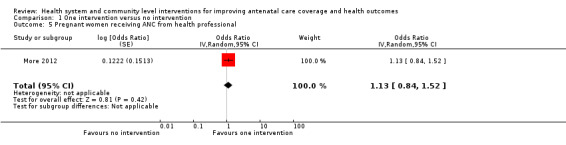
Comparison 1 One intervention versus no intervention, Outcome 5 Pregnant women receiving ANC from health professional.
Deliveries in a health facility ‐ marginally more women in the intervention groups delivered their babies in a health facility (average OR 1.08, 95% CI 1.02 to 1.15; participants = 510; studies = 10); Heterogeneity: Tau² = 0.00; P = 0.58; I² = 0%; GRADE assessment = high quality evidence; Analysis 1.6). See also Table 6.
1.6. Analysis.
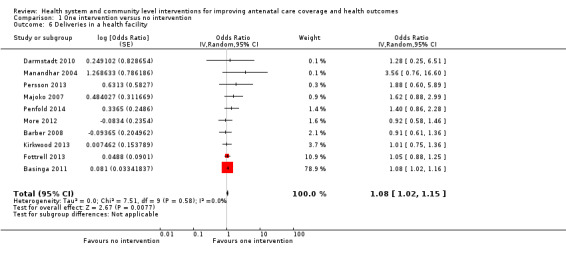
Comparison 1 One intervention versus no intervention, Outcome 6 Deliveries in a health facility.
4. SOF outcome 1.6 Deliveries in health facilities.
| Study | Measure of effect | Statistical approach1 | Intervention | Control |
| Barber 2008 | Adjusted | 480/776 | 130/203 | |
| Basinga 2011 | beta (95% CI): 0.081 (0.015 to 0.146) | Calculated ln (OR) and se (ln OR) | Reported only total n = 2108 | |
| Darmstadt 2010 | Adjusted | 350/1732 | 290/1759 | |
| Fottrell 2013 | Adjusted Odds Ratio (95%CI) 1.05 (0.88 to 1.25) | Straight into RevMan | ||
| Kirkwood 2013 | Adjusted | 5373/7859 | 5539/8121 | |
| Mojoko 2007 | Adjusted OR for delivery at health centre 1.7 (0.88 to 3.0) ICC used 0.103 | Decided to use delivery at health centre outcome rather than hospital outcome. The OR is asymmetrical so will not go in RevMan ‐ have adjusted the data using the reported ICC 0.103 | Health centre 2660/5261 | 1986/5137 |
| Manandhar 2004 | Adjusted | 201/2945 | 66/3270 | |
| More 2012 | Adjusted OR 0.92 (0.58 to 1.47) | Straight into RevMan | 6602 / 7656 | 6573/ 7536 |
| Penfold 2014 | Adjusted | 187/256 | 166/254 | |
| Persson 2013 | Adjusted OR 1.88 95% CI 0.60 to 5.87. For years 1‐3. | Straight into RevMan | 594/656 | 510/587 |
1Data adjusted using ICC 0.103 from Majoko 2007.
Intermittent prophylactic treatment for malaria ‐ one trial, Darmstadt 2010, reported this outcome, but we have excluded these data due to a national vaccine shortage during the study period. GRADE assessment not possible.
Proportion of women with tetanus protection at birth ‐ high heterogeneity compromises our confidence in this finding, which shows no group differences for women receiving tetanus protection (average OR 1.03, 95% CI 0.92 to 1.15; studies = eight; Heterogeneity: Tau² = 0.01; (P = 0.02); I² = 57%; Analysis 1.8).
1.8. Analysis.
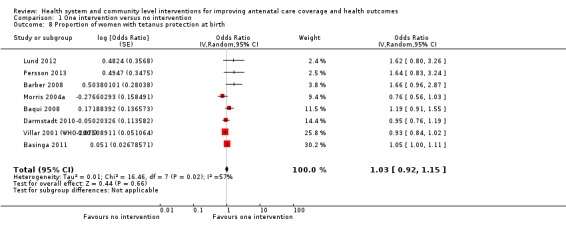
Comparison 1 One intervention versus no intervention, Outcome 8 Proportion of women with tetanus protection at birth.
Proportion of women receiving treatment for syphilis ‐ two trials measured this outcome, with similar numbers of women in both groups receiving treatment (average OR 1.46, 95% CI 0.94 to 2.26; studies = two; Analysis 1.9).
1.9. Analysis.
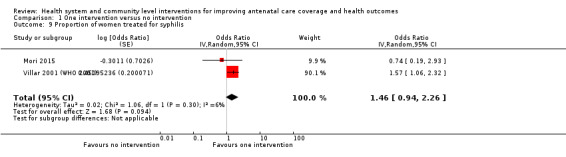
Comparison 1 One intervention versus no intervention, Outcome 9 Proportion of women treated for syphilis.
Proportion of women with HIV who receive a complete antiretroviral course ‐ just one trial (Richter 2014; n = 1200) reported more women in control groups had the complete antiretroviral course (OR 0.44, 95% CI 0.26 to 0.74; studies = one; Analysis 1.10); trial authors were not able to explain this finding.
1.10. Analysis.
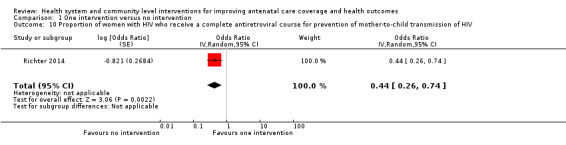
Comparison 1 One intervention versus no intervention, Outcome 10 Proportion of women with HIV who receive a complete antiretroviral course for prevention of mother‐to‐child transmission of HIV.
Preterm labour ‐ there was no measurable effect of interventions on rates of preterm labour (average OR 1.00, 95% CI 0.93 to 1.09; studies = four; Heterogeneity: Tau² = 0.00; (P = 0.93); I² = 0%; Analysis 1.11).
Low birthweight ‐ there is no evidence that interventions were able to impact rates of low birthweight among trial participants (average OR 0.94, 95% CI 0.82 to 1.06; studies = five; Heterogeneity: Tau² = 0.00; (P = 0.38); I² = 5%; GRADE assessment = high quality evidence; Analysis 1.12). See also Table 7.
1.12. Analysis.
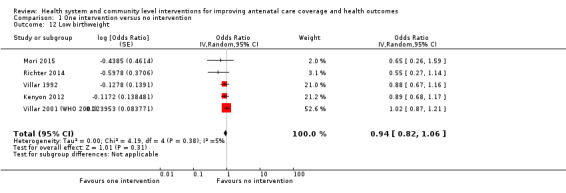
Comparison 1 One intervention versus no intervention, Outcome 12 Low birthweight.
5. SOF outcome 1.12 Low birth weight.
| Trial | Measure of effect | Statistical approach1 | Intervention | Control |
| Kenyon 2012 | RR 0.92 (0.74, 1.14) P = 0.43 | Not cluster trial ‐ calculated OR | 127/605 | 141/613 |
| Mori 2015 | Adjusted OR 0.65 (0.26 to 1.59) trial statistician (H Noma) calculated unpublished OR adjusted for cluster effects and significant variables | Straight into RevMan | 8/251 | 12/247 |
| Richter 2014 | Adjusted | 67/377 | 52/414 | |
| Villar 1992 | OR 0.88 (95% CI 0.67 to 1.16) | Straight into RevMan | 115/1033 | 130/1040 |
| Villar 2001 | Adjusted | 910/11534 | 852/11040 |
1ICC from Piaggio 2001 paper of 0.0004 for ANC trial with average cluster size 426.
Perinatal mortality ‐ trials had mixed results for improving rates of perinatal deaths, contributing to substantial heterogeneity for this outcome. The pooled result shows similar numbers of deaths in intervention and control study arms (average OR 0.96, 95% CI 0.89 to 1.03; studies = 15; Heterogeneity: Tau² = 0.01; (P = 0.003) I² = 45%; GRADE assessment = moderate quality evidence, downgraded once for design limitations in contributing trials; Analysis 1.13). Just two of 15 trials showed positive results for interventions (Kirkwood 2013; Lund 2012). No trial contributing to this outcome was assessed as of high risk of bias overall, but several trials reported perinatal mortality calculated with different definitions of neonatal death. Lund 2012 included deaths up to 42 days; Baqui 2008 and Kirkwood 2013 included neonatal deaths to 28 days. Removing these trials from the analysis reduced the heterogeneity from 45% to 34% but made no difference to the pooled effect estimate. See also Table 8.
6. SOF outcome 1.13 Perinatal mortality.
| Trial | Effect Measure | Statistical approach1 | Intervention | Control |
| Baqui 2008 | Adjusted | 2552/32279 | 1260/15914 | |
| Darmstadt 2010 | Adjusted | 224/4800 | 255/5472 | |
| Fottrell 2013 | Risk Ratio (95% CI) adjusted without Tea‐garden residents 0.87 (0.62 to 1.22) | Calculated OR | 474/9106 | 503/8834 |
| Kenyon 2012 | RR 2.04 (0.51 to 8.12) P = 0.30 | Not a cluster trial. Calculated adjusted OR |
6/604 | 3/616 |
| Kirkwood 2013 | Adjusted | 288/8035 | 355/8294 | |
| Lewycka 2013a peer counselling only | Adjusted | 150/4690 | 103/2529 | |
| Lewycka 2013 women's groups only | Adjusted | 173/4773 | 104/2530 | |
| Lund 2012 | Adjusted OR 0.50 (0.27 to 0.93) adjusted for clustering and covariates associated with perinatal mortality | Straight into RevMman | 25/1300 | 44/1236 |
| Majoko 2007 | OR 1.11 (0.89 to 1.39) | 185/6614 | 161/6384 | |
| Manandhar 2004 | Adjusted as below | 123/2972 | 147/3303 | |
| More 2012 | Adjusted | 205/8017 | 173/7844 | |
| Mori 2015 | Unpublished OR 0.49 (0.05 to 4.54) provided by trial statistician (H Noma) adjusted for cluster effect and significant variables | Straight into RevMan | 1/253 | 2/248 |
| Persson 2013 | Adjusted | 283/11906 | 290/10655 | |
| Villar 1992 | OR 0.89 (95% CI 0.55 to 1.47) | Straight into RevMan | 3.6% of 1033 | 4% of 1040 |
| Villar 2001 (WHO 2001) | From Vogel 2013 Adjusted RR 1.18 (1.01 to 1.37). Adjusted for clustering and for risk strata, smoking, education less than primary, hospital admission in last pregnancy, previous surgery on reproductive tract, late booking, vaginal bleeding in the first trimester, age, previous low birth weight, parity. | Calculated adjusted OR | 234/11672 | 190/11121 |
1Piaggio 2001 reports ICC for perinatal mortality of 0.
Outcomes not reported in the included studies ‐ No trial included in this comparison reported the outcomes: pregnant women with a written birth and emergency plan by 37 weeks; pregnant women screened for asymptomatic bacteriuria; pregnant women screened for HIV; and maternal near miss defined as: "a woman who nearly died but survived a complication that occurred during pregnancy, childbirth or within 42 days of termination of pregnancy" (Pattinson 2009).
Exploration of publication bias
Four outcomes had 10 or more trials contributing data: 1.1 ANC: four or more visits (Figure 4), 1.2 pregnancy‐related deaths (Figure 5), 1.6 deliveries in a health facility (Figure 6) and 1.13 perinatal mortality (Figure 7). We visually inspected funnel plots for these outcomes and found no conclusive evidence of asymmetry suggesting publication bias. Though two funnel plots displayed apparent asymmetry (1.1 (Figure 4), and 1.6 (Figure 6)), we did not downgrade evidence when assessing these outcomes with GRADE. Just one of the outlier trials in question had a significant result, and the weight that each these trials contributed to the pooled effect estimate was extremely low (< 1.5%). Finally, each of these outcomes had just the 10 trials required for the analysis, not more. For these reasons we do not feel that the apparent asymmetry should be interpreted as evidence of publication bias. We will reassess this interpretation when more trials are added in future updates of this review.
4.
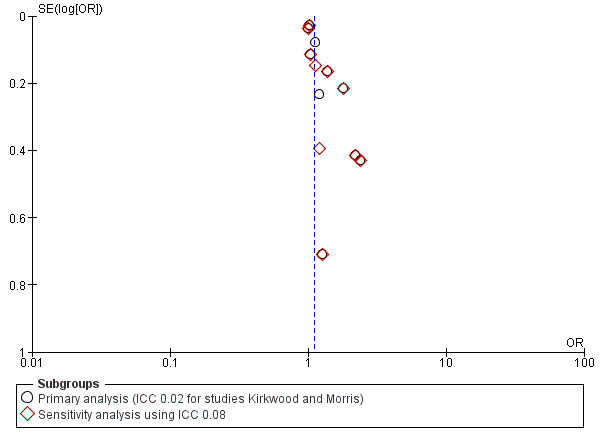
Funnel plot of comparison: 1 One intervention versus no intervention, outcome: 1.1 ANC coverage: four or more visits.
5.
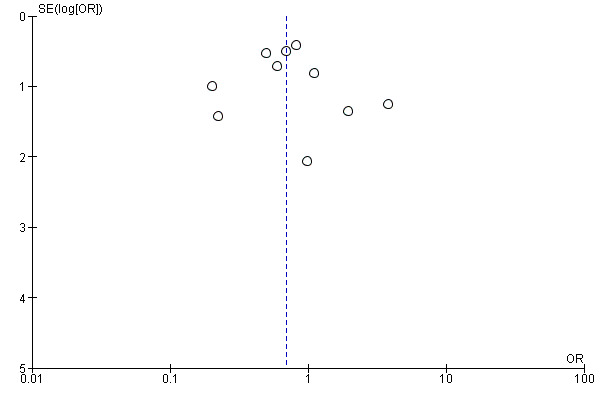
Funnel plot of comparison: 1 One intervention versus no intervention, outcome: 1.2 Pregnancy‐related deaths.
6.
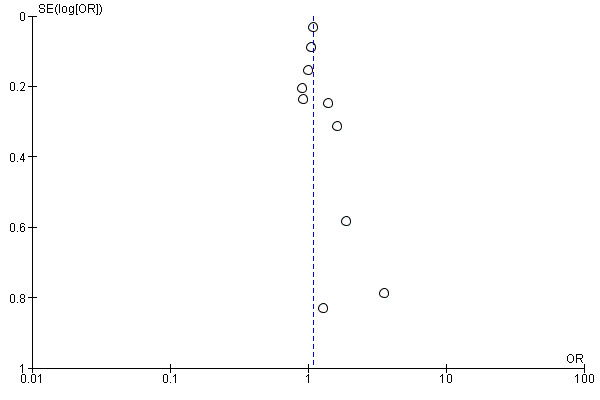
Funnel plot of comparison: 1 One intervention versus no intervention, outcome: 1.6 Deliveries in a health facility.
7.
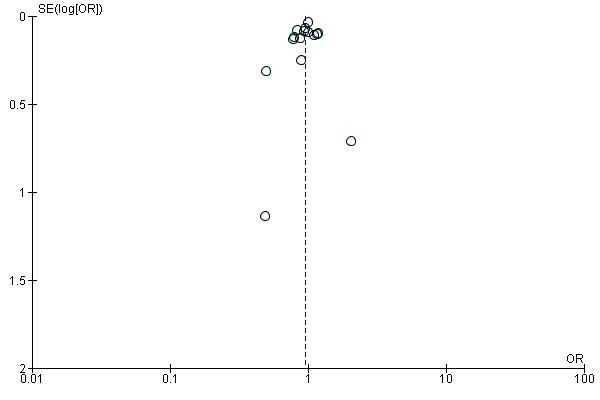
Funnel plot of comparison: 1 One intervention versus no intervention, outcome: 1.13 Perinatal mortality.
Comparison 2: A combination of interventions versus no intervention
All trials contributing data to the meta‐analyses for this comparison were of cluster design, apart from Klerman 2001 (outcomes 2.10 and 2.11) and Laken 1995 (2.1, 2.2, 2.6, and 2.13).
There were clear benefits of the combined interventions with respect to antenatal care: far more women received at least one antenatal care visit in the intervention arms. Women were also far more likely to receive any ANC from a health professional and to receive tetanus protection at birth. Infants also benefited from combined interventions; they were less likely to be born of low birthweight and less likely to die during pregnancy or during the first seven days of life.
Primary outcomes
ANC coverage: four or more visits ‐ there was no clear difference between groups with respect to ANC coverage with either ICC used (0.02 or 0.08). Results are: ICC 0.02 (average OR 1.48, 95% CI 0.99 to 2.21; studies = six; 7840 women; Heterogeneity: Tau² = 0.10; (P = 0.09); I² = 48%; GRADE assessment = low quality evidence due to design limitations in contributing trials and wide CI crossing the line of no effect) and ICC 0.08 (average OR 1.45, 95% CI 0.95 to 2.23; studies = six; Heterogeneity: Tau² = 0.09; (P = 0.17); I² = 35%); Analysis 2.1. One trial (Wahlstrom 2011) had a considerably larger effect size than the others, but we considered this trial to be of high risk of bias due to questions about analysis methods in the trial. The data were unpublished and provided by the authors. (See Included Studies tables). Removal of Wahlstrom 2011 from the analysis 2.1 cancels out all of the heterogeneity but doesn't change the results. See also Table 9.
2.1. Analysis.
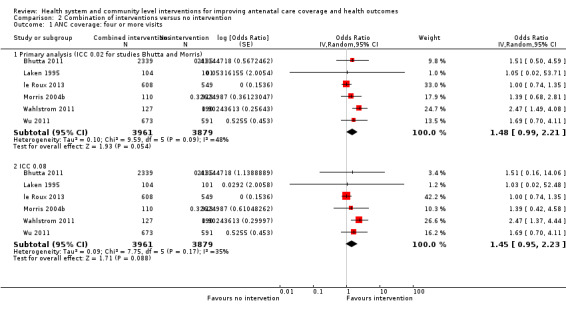
Comparison 2 Combination of interventions versus no intervention, Outcome 1 ANC coverage: four or more visits.
7. Primary outcome 2.1: Proportion of women with at least 4 ANC visits.
| Study | Measure of effect | Statistical approach1 | Intervention | Control |
| Bhutta 2011 | Adjusted | 302/2339 | 191/2135 | |
| Laken 1995 | Not cluster trial – two intervention arms added together. calculated ln (OR) and se (Ln OR) | 104/194 | 101/101 | |
| Le Roux 2013 | 1.00 (0.74, 1.34) OR Random effects logistic regression, adjusted for neighbourhood clustering. Models for outcomes among HIV‐positive mothers control for baseline employment. | Straight into RevMan | 474/608 | 439/549 |
| Morris 2004 both packages | Calculated from change scores, Table 2 Program effects p. 2034 of main report. Intervention 38.1% + 18.4% = 56.5% of the final sample size in this group which is 110; 48.9% ‐ 0.7% = 48.2 % in the control group (n = 313). Adjusted as below | 62/110 | 151/313 | |
| Manthip 2015 | Adjusted | 62/127 | 53/190 | |
| Wu 2011 | Calculated adjusted SE from P value 0.246 | 376/673 | 253/591 |
1Primary analysis using ICC of 0.02.
Pregnancy‐related deaths ‐ no trial was able to improve women's chances of survival (average OR 0.70, 95% CI 0.39 to 1.26; studies = three; 13756 women; Heterogeneity: Tau² = 0.00; (P = 0.65); I² = 0%; GRADE assessment = moderate quality evidence, downgraded once due to wide CI crossing the line of no effect; Analysis 2.2). See also Table 10.
2.2. Analysis.
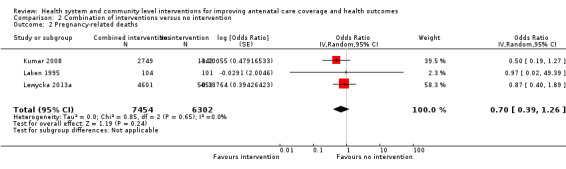
Comparison 2 Combination of interventions versus no intervention, Outcome 2 Pregnancy‐related deaths.
8. Primary outcome 2.2: Pregnancy related deaths.
| Study | Measure of effect | Statistical approach | Intervention | Control |
| Kumar 2008 | Adjusted | 12/2749 | 10/1142 | |
| Laken 1995 | 0.9713 (0.0191 to 49.4211) | Straight into RevMan | 0/104 | 0/101 |
| Lewycka 2013 | Adjusted | 23/4601 | 29/5059 |
1All data adjusted using an ICC of 0.00247 as suggested by Professor J P Souza by email.
Sensitivity analyses
One primary outcome with substantial heterogeneity above included trials assessed as of high risk of bias.
ANC coverage: four or more visits (Analysis 2.1) ‐ one trial (Wahlstrom 2011) had a considerably larger effect size than the others, and we considered this trial to be of high risk of bias due to questions about analysis methods in the trial. The data were unpublished and provided by the authors. A second trial Wu 2011 was also assessed as of high risk of bias due to multiple bias concerns. (See Included studies tables). Removal of Wahlstrom 2011 from the analysis reduced the heterogeneity found for the ICC of 0.02 (originally I² = 48%). Removing both trials of high risk of bias likewise eliminates all heterogeneity for the ICC of 0.08 (I² = 35%). Both sensitivity analyses shift the overall estimates toward the line of no difference (ICC 0.02 average OR 1.07, 95% CI 0.82 to 1.40; studies = four) and ICC 0.08 (average OR 1.03, 95% CI 0.77 to 1.37; studies = four; Analysis 8.1).
Secondary outcomes
ANC coverage: one or more visits ‐ women in intervention arms were much more likely to attend at least one antenatal care session (average OR 1.79, 95% CI 1.47 to 2.17; studies = five; Heterogeneity: Tau² = 0.00; (P = 0.84); I² = 0%; GRADE assessment = moderate quality evidence, downgraded once due to wide CI crossing the line of no effect; Analysis 2.3). See also Table 11.
2.3. Analysis.
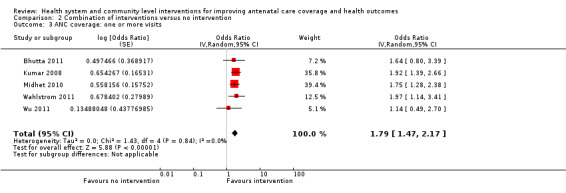
Comparison 2 Combination of interventions versus no intervention, Outcome 3 ANC coverage: one or more visits.
9. SOF outcome 2.3 ANC coverage: one or more ANC visits.
| Study | Measure of effect | Statistical approach1 | Intervention | Control |
| Bhutta 2011 | Adjusted | 1616/2339 | 1230/2135 | |
| Kumar 2008 | 24.5% of 2681 intervention and 14.4% of 1129 controls: RR (95%CI); 1.67 (1.47 to 1.91) | Calculated adjusted OR | 657/2681 | 163/1129 |
| Wahlstrom 2011 | Adjusted | 99/127 | 122/190 | |
| Midhet 2010 | Adjusted | Womens group 254/836 couples group 187/703 women + couples = 441/1539 | 191/1022 | |
| Wu 2011 | Calculated the ICC that they used to adjust the results using the reported P = 0.758 | 85/88 | 74/77 |
1As for first comparison, ICC of 0.02 used for this outcome. Both Manandhar 2004 and Wu 2011 use ICCS of approximately 0.02
Pregnant women initiating ANC in the first trimester ‐ for just one trial, a combined intervention did not encourage more women to attend ANC earlier in pregnancy (OR 0.83, 95% CI 0.47 to 1.47; studies = one; Analysis 2.4).
2.4. Analysis.
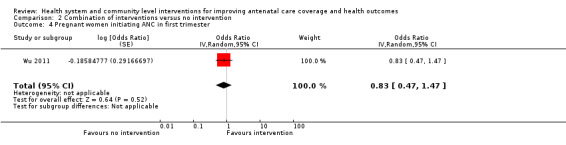
Comparison 2 Combination of interventions versus no intervention, Outcome 4 Pregnant women initiating ANC in first trimester.
Pregnany women receiving ANC from health professionals ‐ women in intervention arms in two trials were much more likely to receive antenatal care from health professionals, though the analysis had high heterogeneity (average OR 2.97, 95% CI 1.67 to 5.30; studies = two; Heterogeneity: Tau² = 0.11; Chi² = 2.70, df = 1 (P = 0.10); I² = 63%; Analysis 2.5). We assessed one trial contributing data to this outcome as of high risk of bias (Wahlstrom 2011). Both trials contributing data had interventions that combined education for pregnant women with provision of equipment/resources for health services (such as clean delivery kits); Wahlstrom 2011 also provided education for healthcare staff.
2.5. Analysis.
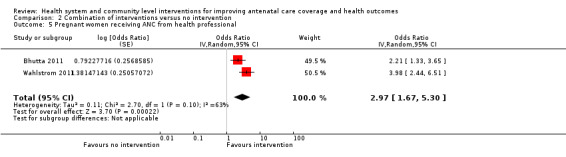
Comparison 2 Combination of interventions versus no intervention, Outcome 5 Pregnant women receiving ANC from health professional.
Deliveries in a health facility ‐ women in intervention arms seemed to get more antenatal care (as above) and to deliver in health facilities more often than did women in control arms, though this difference in place of deliveries was not statistically significant (average OR 1.53, 95% CI 0.96 to 2.43; studies = five; Heterogeneity: Tau² = 0.00; (P = 0.99); I² = 0%; GRADE assessment = moderate quality evidence, downgraded once due to wide CI crossing the line of no effect; Analysis 2.6). See also Table 12.
2.6. Analysis.
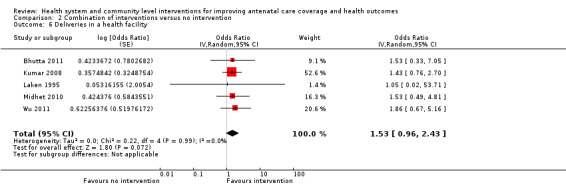
Comparison 2 Combination of interventions versus no intervention, Outcome 6 Deliveries in a health facility.
10. SOF outcome 2.6 Deliveries in health facilities.
| Study | Measure of effect | Statistical approach1 | Intervention | Control |
| Bhutta 2011 | Adjusted as below | 1272/2339 | 936/2135 | |
| Kumar 2008 | RR (95%CI); 1.35 (0.88 to 2.07) | Calculated adjusted OR | 507/2681 | 158/1129 |
| Laken 1995 | NOT A CLUSTER TRIAL ‐ calculated OR and confidence interval | 104/104 | 101/101 | |
| Midhet 2010 | Adjusted as below | 46/ 836 in women's group 42/703 in couple's group Combined intervention arms: 88/1539 | 39/1022 | |
| Wu 2011 | Calculated what the ICC would have been using the reported adjusted p‐value (P = 0.231) | 625/673 | 517/591 |
1ICC from Wu (0.099).
Intermittent prophylactic treatment for malaria ‐ no trial included in this comparison reported this outcome. GRADE assessment not possible.
Proportion of women with tetanus protection at birth ‐ far more women in the combined intervention arms received tetanus protection at birth (average OR 1.48, 95% CI 1.18 to 1.87; studies = three; Heterogeneity: Tau² = 0.01; (P = 0.23); I² = 33%; Analysis 2.8), though there was moderate heterogeneity for this outcome. None of the trials included in this analysis was assessed as of high risk of bias, so the finding of heterogeneity will most likely be due to differences in interventions. Kumar 2008 and Midhet 2010 both had cultural components to their combined interventions, while Morris 2004b tested financial incentives for women and for health systems. In fact, removing Morris 2004b from the meta‐analysis eliminated all of the heterogeneity found without changing the overall result (i.e. there is still a clear difference between groups).
2.8. Analysis.
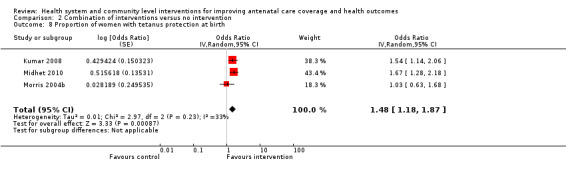
Comparison 2 Combination of interventions versus no intervention, Outcome 8 Proportion of women with tetanus protection at birth.
Preterm labour ‐ just one individual randomised trial (Klerman 2001) reported this outcome, with no clear benefit for women in the intervention arm (OR 0.74, 95% CI 0.45 to 1.20; participants = 607; studies = one; Analysis 2.9).
2.9. Analysis.
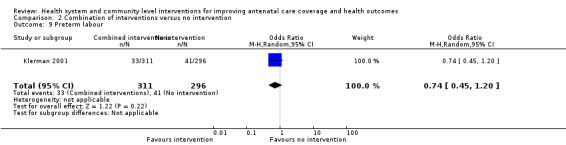
Comparison 2 Combination of interventions versus no intervention, Outcome 9 Preterm labour.
Low birthweight ‐ two trials (Klerman 2001; le Roux 2013) found clear benefits of combined interventions of education and augmented antenatal care; women were far less likely to give birth to infants of low birthweight (average OR 0.61, 95% CI 0.46 to 0.80; studies = two; Heterogeneity: Tau² = 0.00; (P = 0.68); I² = 0%; GRADE assessment = moderate quality evidence, downgraded once due to design limitations in contributing trials; Analysis 2.10). See also Table 13.
2.10. Analysis.
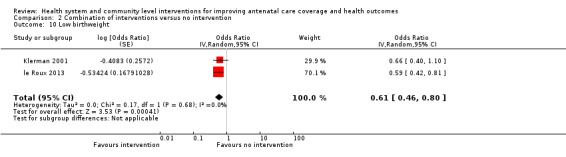
Comparison 2 Combination of interventions versus no intervention, Outcome 10 Low birthweight.
11. SOF outcome 2.10 Low birthweight.
| Trial | Statistical approach1 | Intervention | Control |
| Klerman 2001 | Straight into RevMan ‐ not cluster trial | 39/311 | 33/296 |
| Le roux 2013 | Calculated adjusted OR | 88/608 | 123/549 |
ICC from Piaggio paper of 0.0004 for ANC trial with average cluster size 426
Perinatal mortality ‐ more babies survived when born to women in combined intervention arms (average OR 0.74, 95% CI 0.57 to 0.95; studies = five; Heterogeneity: Tau² = 0.06; (P = 0.0001); I² = 83%; GRADE assessment = moderate quality evidence, downgraded once due to high statistical heterogeneity; Analysis 2.11). Extremely high heterogeneity for this analysis cannot be explained due to trials of high risk of bias. Heterogeneity is most likely explained by the different interventions in the contributing trials and the considerable differences in effect sizes; three large trials in India and Pakistan found highly significant effects (Bhutta 2011; Kumar 2008; Midhet 2010) while, other trials found no group differences. We must advise caution when interpreting this result due to the high heterogeneity found. We excluded the perinatal mortality data from one trial relevant to this analysis (Wu 2011) due to multiple risk of bias concerns, including unclear group denominators. See also Table 14.
2.11. Analysis.
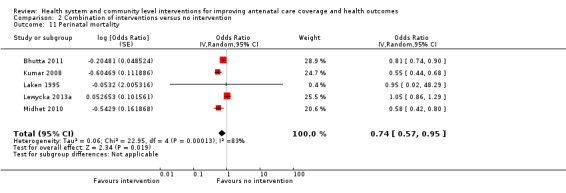
Comparison 2 Combination of interventions versus no intervention, Outcome 11 Perinatal mortality.
12. SOF outcome 2.11 Perinatal deaths.
| Trial | Statistical approach1 | Intervention | Control |
| Bhutta 2011 | Calculated OR | 880/12028 | 972/11005 |
| Laken 1995 | Calculated OR | 0/96 | 0/91 |
| Lewycka 2013 | Calculated OR | 198/4601 | 207/5059 |
| Midhet 2010 | Calculated OR | Women's group 36/836 plus couple's group 42/703 | Control 86/1022 |
| Kumar 2008 | Calculated OR | 219/ 2609 | 155/ 1079 |
1Piaggio 2001 reports and ICC of 0 for perinatal deaths.
Outcomes not reported in the included studies: pregnant women with a written birth and emergency plan by 37 weeks; pregnant women screened for syphilis; pregnant women screened for asymptomatic bacteriuria; pregnant women screened for HIV; pregnant women receiving a complete antiretroviral course for prevention of HIV transmission; and maternal near miss defined as: "a woman who nearly died but survived a complication that occurred during pregnancy, childbirth or within 42 days of termination of pregnancy" (Pattinson 2009).
Exploration of publication bias
No outcome in this comparison had the required 10 trials contributing data.
Comparison 3: Two interventions compared
No included trial tested different single interventions head to head.
Comparison 4: Combined interventions versus one intervention
All trials contributing to this comparison were of cluster‐randomised design.
Primary outcomes
ANC coverage: four or more visits ‐ there was no evidence of a difference between single or combined interventions using an ICC of 0.02 (average OR 0.99, 95% CI 0.70 to 1.40; studies = two; Heterogeneity: Tau² = 0.04; (P = 0.12); I² = 60%; Analysis 4.1). Neither trial was assessed as of high risk of bias. The interventions in both trials involved a community education intervention for pregnant women and a facility strengthening component for health systems. Azad 2010 (Bangladesh) was a much larger trial than Waiswa 2015 (Uganda), with a higher proportion of women receiving four ANC visits.
4.1. Analysis.
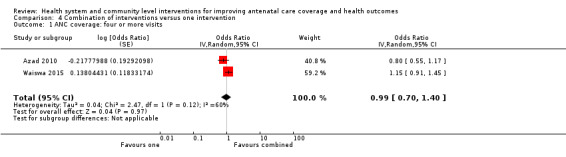
Comparison 4 Combination of interventions versus one intervention, Outcome 1 ANC coverage: four or more visits.
Pregnancy‐related deaths ‐ there was no evidence that interventions could reduce pregnancy‐related deaths (average OR 1.00, 95% CI 0.52 to 1.96; studies = two; Heterogeneity: Tau² = 0.12; (P = 0.19); I² = 43%; Analysis 4.2). Different effect sizes as well as differences in interventions likely contributed to the heterogeneity found in this analysis. Tripathy 2010 (India) was three times larger than the Azad 2010 (Bangladesh) trial and had no facility strengthening component, as in Azad 2010.
4.2. Analysis.
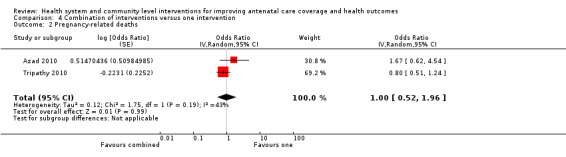
Comparison 4 Combination of interventions versus one intervention, Outcome 2 Pregnancy‐related deaths.
Sensitivity analysis
No trial contributing to the primary outcomes for this comparison was judged to be of high risk of bias.
Secondary outcomes
ANC coverage: one or more visits ‐ there was no evidence that combined interventions were more effective than single interventions in three trials (average OR 0.86, 95% CI 0.61 to 1.20; studies = three; Heterogeneity: Tau² = 0.02; (P = 0.33); I² = 11%; Analysis 4.3).
4.3. Analysis.
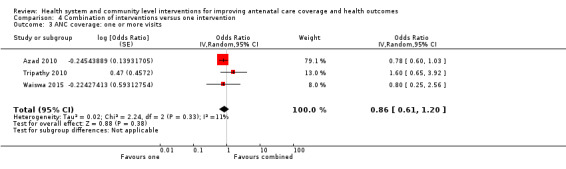
Comparison 4 Combination of interventions versus one intervention, Outcome 3 ANC coverage: one or more visits.
Deliveries in a health facility ‐ similar proportions of pregnant women delivered in health facilities (average OR 0.95, 95% CI 0.69 to 1.30; studies = three; Heterogeneity: Tau² = 0.00; (P = 0.92); I² = 0%; Analysis 4.4).
4.4. Analysis.
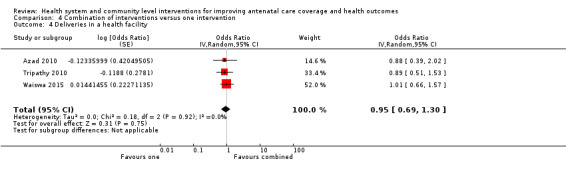
Comparison 4 Combination of interventions versus one intervention, Outcome 4 Deliveries in a health facility.
Perinatal mortality ‐ two trials found mixed results for perinatal mortality. Tripathy 2010 found a reduction in perinatal mortality, though Azad 2010 did not (average OR 0.88, 95% CI 0.72 to 1.07; studies = two; Heterogeneity: Tau² = 0.02; (P = 0.02); I² = 83%; Analysis 4.5). Very high heterogeneity makes us doubt whether this pooled result is meaningful.
4.5. Analysis.
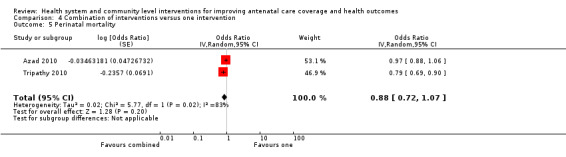
Comparison 4 Combination of interventions versus one intervention, Outcome 5 Perinatal mortality.
Proportion of women with tetanus protection at birth ‐ there was no evidence of group differences for women who received tetanus protection (average OR 1.07, 95% CI 0.80 to 1.43; studies = two; Heterogeneity: Tau² = 0.03; (P = 0.18); I² = 44%; Analysis 4.6). Again, substantial heterogeneity likely has to do with differences between the interventions between the Tripathy 2010 (India) and Azad 2010 (Bangladesh) trials, as above.
4.6. Analysis.
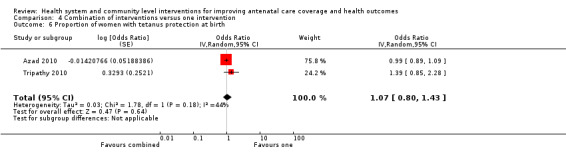
Comparison 4 Combination of interventions versus one intervention, Outcome 6 Proportion of women with tetanus protection at birth.
Outcomes not reported in the included studies: low birthweight; preterm labour; intermittent prophylactic treatment for malaria; proportion of women who received ANC from professional health workers; pregnant women with a written birth and emergency plan by 37 weeks; pregnant women screened for syphilis; pregnant women screened for asymptomatic bacteriuria; pregnant women screened for HIV; pregnant women receiving a complete antiretroviral course for prevention of HIV transmission; and maternal near miss defined as: "a woman who nearly died but survived a complication that occurred during pregnancy, childbirth or within 42 days of termination of pregnancy" (Pattinson 2009).
Exploration of publication bias
No outcome in this comparison had 10 trials contributing data.
Comparison 5: Different combinations of interventions
One individually‐randomised trial was included in this comparison. Mullany 2007 (n = 383) compared three groups: in one arm women attended education sessions alone and received health education flyers; in a second arm women attended education sessions with their husbands and received education health flyers; a third arm received health educational flyers. All pregnant women received standard antenatal care. For this analysis, we have combined the arms receiving education sessions and flyers and compared these with the control arm receiving only flyers.
Primary outcomes
ANC coverage: four or more antenatal visits ‐ there were no group differences in women's attendance of antenatal care (average OR 0.77, 95% CI 0.41 to 1.43; studies = one; Analysis 5.1).
5.1. Analysis.
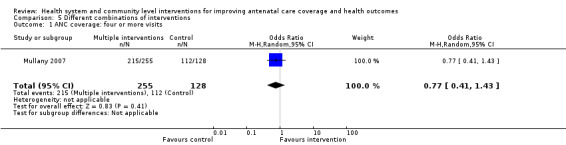
Comparison 5 Different combinations of interventions, Outcome 1 ANC coverage: four or more visits.
Pregnancy‐related deaths ‐ Mullany 2007 did not report this outcome.
Sensitivity analysis
Only one trial was included these analyses.
Secondary outcomes
One or more ANC visits ‐ this outcome was not reported in Mullany 2007.
Deliveries in a health facility ‐ there was no evidence of a difference in rates of women who delivered in health facilities (average OR 1.55, 95% CI 0.71 to 3.37; studies = one; Analysis 5.4).
5.4. Analysis.
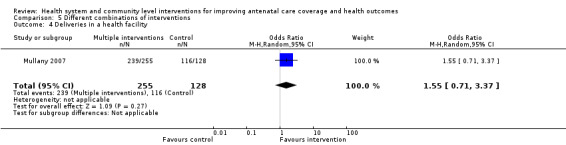
Comparison 5 Different combinations of interventions, Outcome 4 Deliveries in a health facility.
Outcomes not reported in the included study under this comparison: the trial did not report any of the following review secondary outcomes: pregnant women initiating ANC in first trimester, pregnant women receiving ANC from health professional, intermittent prophylactic treatment for malaria, proportion of women with tetanus protection, proportion of women treated for syphilis, proportion of women with HIV who received a complete anti‐retroviral course for the prevention of transmission of HIV from mother to child, preterm labour, low birthweight, perinatal mortality.
Exploration of publication bias
Only one trial was included in these analyses.
Analysis 6: Subgroup analysis
The subgroup analyses were limited to the two primary outcomes of the review: ANC (at least four visits) and maternal deaths. We compared any interventions or combinations of interventions with no intervention or single interventions.
We were not able to conduct analyses for urban versus rural settings because our trials were overwhelmingly rural. For example, 13 of 18 trials contributing data for the primary outcome of ANC coverage (at least four visits) took place in rural settings, with just three in urban settings (one trial had mixed settings and one trial report was unclear).
We conducted subgroup analysis with trials targeting the health system versus trials targeting the population. Becasue several trials included both types of interventions, though, the number of trials included in subgroup analysis is not representative of the included studies overall.
We conducted subgroup analyses comparing trials set in upper‐middle‐ and high‐income countries versus trials set in low‐ or lower‐middle‐income countries, for the outcome of ANC coverage (at least four visits) only. There were insufficient data for this analysis for the primary outcome of maternal mortality, because just three of 13 trials contributing data were conducted in higher‐income settings.
For the review primary outcomes of ANC coverage: at least four visits and pregnancy‐related deaths, there were no clear differences between treatment arms in any subgroup reported below.
Health Systems versus Population ANC coverage: four or more visits ‐ there was no evidence of subgroup differences between trials classed as health systems interventions and trials targeting populations (test for subgroup differences: Chi² = 0.77, df = 1 (P = 0.38), I² = 0%). There were no discernable effects of the interventions on coverage, either, and there was substantial heterogeneity in the health systems subgroup (See Analysis 6.1). The pooled result for health systems interventions was (average OR 1.13, 95% CI 0.96 to 1.34; studies = five; Heterogeneity: Tau² = 0.02; (P = 0.04); I² = 60%), and for population interventions was (average OR 1.04, 95% CI 0.96 to 1.13; studies = four; Heterogeneity: Tau² = 0.00; (P = 0.38); I² = 2%).
Health Systems versus Population Pregnancy‐related deaths ‐ there was no evidence of subgroup differences between trial types for maternal deaths (test for subgroup differences: Chi² = 0.91, df = 1 (P = 0.34), I² = 0%; See Analysis 6.2). There was no evidence of heterogeneity in either subgroup, and no evidence that trials had any impact to reduce mortality in intervention arms. The pooled effect for health systems trials was (average OR 1.22, 95% CI 0.41 to 3.65; studies = four; Heterogeneity: Tau² = 0.00; (P = 0.50); I² = 0%), while for trials targeting populations the result was (average OR 0.69, 95% CI 0.46 to 1.03; studies = eight; Heterogeneity: Tau² = 0.00; (P = 0.92); I² = 0%). Population interventions look more promising for women in this instance, but all trials were underpowered to show a statistically significant impact on rates of maternal mortality. We split the control group between Lewycka 2013a and Lewycka 2013b for analysis, so no results have been double counted.
6.2. Analysis.
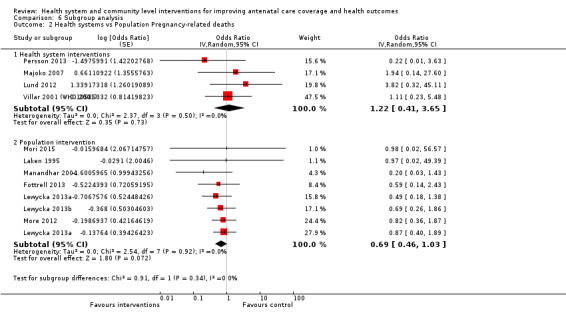
Comparison 6 Subgroup analysis, Outcome 2 Health systems vs Population Pregnancy‐related deaths.
Country Income Low versus High ANC coverage: four or more visits ‐ there was no evidence that interventions worked differently in high‐ or low‐income countries (test for subgroup differences: Chi² = 0.43, df = 1 (P = 0.51), I² = 0%; See Analysis 6.3). Interventions made a marginal difference in the proportion of women receiving at least four antenatal visits in low‐ and lower middle‐income countries, with moderate heterogeneity observed (average (OR 1.21, 95% CI 1.04 to 1.40; participants = 46009; studies = 11; Heterogeneity: Tau² = 0.03; I² = 58%). Treatment groups had similar rates of ANC coverage in upper‐middle‐income or high‐income countries, with moderate heterogeneity between trials (average OR 1.12, 95% CI 0.95 to 1.32; studies = 7; Heterogeneity: Tau² = 0.01; I² = 40%). We calculated estimates for Morris 2004a and Morris 2004b using a split control group so no women were counted twice.
6.3. Analysis.
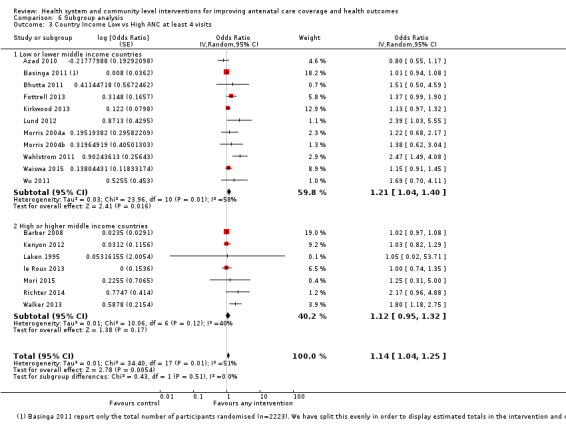
Comparison 6 Subgroup analysis, Outcome 3 Country Income Low vs High ANC at least 4 visits.
Discussion
In this review, we synthesised evidence relating to interventions with the potential to improve antenatal care (ANC) coverage and other outcomes. We included 34 trials involving approximately 400,000 women. Despite our attempts to categorise the trials in a meaningful way (health system versus community), we found very disparate results, with very few interventions improving ANC coverage. Most of the trials were similar in design and choice of participants and were in run in low‐resource rural settings ‐ where ANC coverage is low. However, the interventions were varied and complex, with different levels of compliance and implementation. We noted specific instances where health system changes impeded the conduct of trial (Morris 2004a; Wu 2011). In most instances, the control group received some form of care. With regards to the outcomes, some studies did not explicitly target improvements in ANC, but reported them as an outcome. This raises questions as to whether these trials were sufficiently powered to detect differences in ANC coverage. Most of the studies were cluster trials, but their sizes differed greatly. Follow‐up time also differed substantially. Our findings suggest that it is unlikely that one type of intervention is substantially better than another, but a combination of interventions may yield stronger effect.
Despite these issues some interventions proved to be beneficial. These findings should be interpreted in the light of substantial heterogeneity and the pragmatic nature of the trials. In addition, subtleties in how interventions are combined must be considered. From this systematic review, we can draw a general picture of the effects of health system and community level interventions on ANC coverage and other materno‐fetal outcomes. Our pooled estimates should respond to the question of whether interventions aimed at improving ANC coverage and other outcomes actually work. Our results could not identify which specific interventions were most effective.
Summary of main results
One intervention versus no intervention
When one intervention was compared to none, we found marginal improvements in ANC (at least four visits). This finding was not robust to sensitivity analysis with a more conservative intra‐cluster correlation co‐efficient (ICC) and excluding studies at high risk of bias and shifted the estimate towards no effect (GRADE assessment = high quality evidence).There was no effect on pregnancy‐related deaths (low quality evidence), perinatal mortality (moderate quality evidence) or low birthweight (high quality evidence). No studies reported on receiving intermittent prophylactic treatment for malaria in this comparison. The interventions led to modest improvements in the number of deliveries in health facilities (high quality evidence) and in the proportion of women having at least one ANC visit (moderate quality evidence).
Two or more interventions versus no intervention
When two or more interventions were combined in comparison to none, we found no improvements in ANC coverage (four or more visits; low quality evidence) or pregnancy‐related deaths (moderate quality evidence). However, the interventions led to improvements in ANC coverage (at least one visit; moderate quality evidence), perinatal mortality (moderate quality evidence) and low birthweight (moderate quality evidence). No trials in this comparison reported on intermittent prophylactic treatment for malaria.
One intervention versus a combination of interventions
When one intervention was compared to a combination of other interventions, there was no improvement in ANC coverage (four or more visits and least one visit), pregnancy‐related deaths, deliveries in a health facility or perinatal mortality. No trials in this comparison reported on low birthweight or intermittent prophylactic treatment of malaria.
Subgroups
There were no discernable differences in effect when health system interventions were compared to community interventions. With respect to the proportion of women receiving at least four antenatal visits, all interventions had a more positive impact in low‐ and lower‐middle‐income countries, but this difference did not reach statistical significance.
Overall completeness and applicability of evidence
Completeness of evidence
We applied standard Cochrane methods our searches and screening procedures. We also contacted study authors to provide incomplete or missing information. We are confident that this review is a comprehensive representation of the existing body of literature. A considerable number of trials have been conducted with interventions that may improve ANC or other materno‐fetal outcomes. As expected, most of the trials were of cluster design and conducted in rural settings, in many low‐ and middle‐income countries. There were little to no data on outcomes such as: pregnant women with a written birth and emergency plan by 37 weeks; pregnant women screened for asymptomatic bacteriuria; pregnant women screened for syphilis; pregnant women screened for HIV; pregnant women receiving a complete antiretroviral course for prevention of HIV transmission and maternal near miss. These outcomes are important for determining the mechanism by which ANC improves materno‐fetal outcomes.
Applicability of evidence
The trials included in this review targeted the right participants (women in their reproductive years or pregnant women) and were conducted mostly in the regions of the world with low ANC coverage and high maternal mortality. For the most part, the interventions included in this review built upon existing health system or community resources and should be applicable in similar settings. However, local health system realities should be considered, particularly for interventions that target policies and other components of the health system.
Quality of the evidence
The evidence for the comparison of one intervention versus none was generally high to moderate, with low quality for one outcome (pregnancy‐related deaths) in which many of the studies contributing to the data had design limitations.
The evidence for the comparison of two or more interventions to no intervention was moderate to low, due to design limitations in trials, statistical heterogeneity and wide confidence intervals crossing the line of no effect (imprecision).
We have not downgraded the following outcomes: four or more ANC visits and deliveries in a health facility, for apparent asymmetry in funnel plots. The trials that appear on the plots as outliers are mostly small studies, contributing very little (< 5%) to the overall effect estimate. These studies also have confidence intervals crossing the line of no effect. We were therefore not convinced that these trials contributed to inflated effect estimates due to publication bias. In addition, we sought and included unpublished data in our analysis.
Potential biases in the review process
We conducted a comprehensive search of the literature and have no reason to believe any relevant trials were left out. We completed study selection, appraisal and data extraction in duplicate. However, some systematic error (precision of pooled estimates) might have been introduced in our choice of ICC. We conducted sensitivity analyses with different ICCs to mitigate this potential bias. There was considerable clinical and statistical heterogeneity in most of the analyses, for which we present only random‐effects pooled estimates to embrace this heterogeneity. However, for readers interested in the effects of specific interventions, such aggregation might be questioned.
Agreements and disagreements with other studies or reviews
Other systematic reviews have evaluated the effects of specific interventions on materno‐fetal outcomes and reported similar results. For example, in a systematic review of participatory women’s groups only one study showed an improvement in ANC coverage, despite a general improvement in other maternal and neonatal outcomes (Prost 2013). Community‐based intervention packages were demonstrated to improve maternal and fetal outcomes (Kidney 2009; Lassi 2015). Multiple micronutrients were shown to reduce low birthweight (Haider 2012). Antenatal nutritional advice reduced risk of preterm birth, increased head circumference at birth and increased protein intake (Ota 2015). A multi‐country survey of facility deliveries in 29 countries found that substantial reductions in maternal mortality require improvements in maternal care and the availability of comprehensive emergency care (Souza 2013). These reports suggest that some interventions at the health system level or community level improve materno‐fetal outcomes. In addition, an economic evaluation of strategies to improve healthcare practice and healthcare seeking for maternal and neonatal health found them to be cost effective (Mangham‐Jefferies 2014). To the best of our knowledge, this review is the first to focus on all interventions that may improve ANC coverage. The review's broad scope limits its comparability to other published reviews.
Authors' conclusions
Implications for practice.
Single interventions may improve ANC coverage (at least one visit and four or more visits) and deliveries in health facilities.
Combined interventions may improve ANC coverage (at least one visit), reduce perinatal mortality and reduce the occurrence of low birthweight.
The effects of the interventions are unrelated to whether they are community of health system interventions.
Implications for research.
For cluster‐randomised trials, more details should be provided in reporting numerators and denominators. The ICCs used to adjust for cluster effects should be reported routinely. There is a need for uniform reporting of outcomes so that they are comparable to commonly used population indicators. Given that combinations of interventions seem to have a superior effect to single interventions, further research is required on the most appropriate combinations that would maximise impact. As such, we recommend further cluster‐randomised trials of pregnant women and women in their reproductive years, using combinations of interventions and looking at patient important outcomes like maternal and perinatal morbidity and mortality, alongside the explanatory outcomes along the pathway of care: ANC coverage, the services provided during ANC and deliveries in health facilities.
What's new
| Date | Event | Description |
|---|---|---|
| 22 February 2016 | Amended | Data for the outcome perinatal mortality for the Persson 2013 trial were entered incorrectly; the data have been corrected and the review edited to reflect the change. These edits do not change the overall results and conclusions of the review. |
Acknowledgements
We acknowledge the assistance of the Centre for the Development of Best Practices in Health (CDBPH) and the South African Cochrane Centre (SACC). This review is written within the scope of activities of the Effective Health Care Research Consortium (EHCRC).
Nancy Medley's work was financially supported by the UNDP/UNFPA/UNICEF/WHO/World Bank Special Programme of Research, Development and Research Training in Human Reproduction (HRP), Department of Reproductive Health and Research (RHR), World Health Organization. The named authors alone are responsible for the views expressed in this publication.
We are grateful to Tess Lawrie for her help in preparing the tables of included studies and conducting 'Risk of bias' assessments; she also contributed text for the descriptions of included studies.
This project was supported by the National Institute for Health Research, via Cochrane Infrastructure funding to Cochrane Pregnancy and Childbirth. The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR, NHS or the Department of Health.
As part of the pre‐publication editorial process, this review has been commented on by three peers (an editor and two referees who are external to the editorial team), members of the Pregnancy and Childbirth Group's international panel of consumers and the Group's Statistical Adviser.
Data and analyses
Comparison 1. One intervention versus no intervention.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 ANC coverage: four or more visits | 10 | Odds Ratio (Random, 95% CI) | Subtotals only | |
| 1.1 Primary analysis (ICC 0.02 for studies Kirkwood and Morris) | 10 | 45022 | Odds Ratio (Random, 95% CI) | 1.11 [1.01, 1.22] |
| 1.2 Sensitivity analysis using ICC 0.08 | 10 | 45022 | Odds Ratio (Random, 95% CI) | 1.11 [1.00, 1.22] |
| 2 Pregnancy‐related deaths | 10 | 114930 | Odds Ratio (Random, 95% CI) | 0.69 [0.45, 1.08] |
| 3 ANC coverage: one or more visits | 6 | Odds Ratio (Random, 95% CI) | 1.68 [1.02, 2.79] | |
| 4 Pregnant women initiating ANC in first trimester | 1 | Odds Ratio (Random, 95% CI) | 1.20 [0.99, 1.45] | |
| 5 Pregnant women receiving ANC from health professional | 1 | Odds Ratio (Random, 95% CI) | 1.13 [0.84, 1.52] | |
| 6 Deliveries in a health facility | 10 | Odds Ratio (Random, 95% CI) | 1.08 [1.02, 1.15] | |
| 7 Intermittent Prophylactic Treatment for malaria | 0 | 0 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 8 Proportion of women with tetanus protection at birth | 8 | Odds Ratio (Random, 95% CI) | 1.03 [0.92, 1.15] | |
| 9 Proportion of women treated for syphilis | 2 | Odds Ratio (Random, 95% CI) | 1.46 [0.94, 2.26] | |
| 10 Proportion of women with HIV who receive a complete antiretroviral course for prevention of mother‐to‐child transmission of HIV | 1 | Odds Ratio (Random, 95% CI) | 0.44 [0.26, 0.74] | |
| 11 Preterm labour | 4 | Odds Ratio (Random, 95% CI) | 1.00 [0.93, 1.09] | |
| 12 Low birthweight | 5 | Odds Ratio (Random, 95% CI) | 0.94 [0.82, 1.06] | |
| 13 Perinatal mortality | 15 | Odds Ratio (Random, 95% CI) | 0.96 [0.89, 1.03] |
Comparison 2. Combination of interventions versus no intervention.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 ANC coverage: four or more visits | 6 | Odds Ratio (Random, 95% CI) | Subtotals only | |
| 1.1 Primary analysis (ICC 0.02 for studies Bhutta and Morris) | 6 | 7840 | Odds Ratio (Random, 95% CI) | 1.48 [0.99, 2.21] |
| 1.2 ICC 0.08 | 6 | 7840 | Odds Ratio (Random, 95% CI) | 1.45 [0.95, 2.23] |
| 2 Pregnancy‐related deaths | 3 | 13756 | Odds Ratio (Random, 95% CI) | 0.70 [0.39, 1.26] |
| 3 ANC coverage: one or more visits | 5 | Odds Ratio (Random, 95% CI) | 1.79 [1.47, 2.17] | |
| 4 Pregnant women initiating ANC in first trimester | 1 | Odds Ratio (Random, 95% CI) | 0.83 [0.47, 1.47] | |
| 5 Pregnant women receiving ANC from health professional | 2 | Odds Ratio (Random, 95% CI) | 2.97 [1.67, 5.30] | |
| 6 Deliveries in a health facility | 5 | Odds Ratio (Random, 95% CI) | 1.53 [0.96, 2.43] | |
| 7 Intermittent Prophylactic Treatment for malaria | 0 | 0 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 8 Proportion of women with tetanus protection at birth | 3 | Odds Ratio (Random, 95% CI) | 1.48 [1.18, 1.87] | |
| 9 Preterm labour | 1 | 607 | Odds Ratio (M‐H, Random, 95% CI) | 0.74 [0.45, 1.20] |
| 10 Low birthweight | 2 | Odds Ratio (Random, 95% CI) | 0.61 [0.46, 0.80] | |
| 11 Perinatal mortality | 5 | Odds Ratio (Random, 95% CI) | 0.74 [0.57, 0.95] |
Comparison 3. Two interventions compared.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 ANC coverage: four or more visits | 0 | 0 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 2 Pregnancy‐related deaths | 0 | 0 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 3 ANC coverage: one or more visits | 0 | 0 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Deliveries in a health facility | 0 | 0 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5 Perinatal mortality | 0 | 0 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6 Low birthweight | 0 | 0 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7 Intermittent Prophylactic Treatment for malaria | 0 | 0 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
Comparison 4. Combination of interventions versus one intervention.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 ANC coverage: four or more visits | 2 | Odds Ratio (Random, 95% CI) | 0.99 [0.70, 1.40] | |
| 2 Pregnancy‐related deaths | 2 | Odds Ratio (Random, 95% CI) | 1.00 [0.52, 1.96] | |
| 3 ANC coverage: one or more visits | 3 | Odds Ratio (Random, 95% CI) | 0.86 [0.61, 1.20] | |
| 4 Deliveries in a health facility | 3 | Odds Ratio (Random, 95% CI) | 0.95 [0.69, 1.30] | |
| 5 Perinatal mortality | 2 | Odds Ratio (Random, 95% CI) | 0.88 [0.72, 1.07] | |
| 6 Proportion of women with tetanus protection at birth | 2 | Odds Ratio (Random, 95% CI) | 1.07 [0.80, 1.43] | |
| 7 Low birthweight | 0 | 0 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 8 Intermittent Prophylactic Treatment for malaria | 0 | 0 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
Comparison 5. Different combinations of interventions.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 ANC coverage: four or more visits | 1 | 383 | Odds Ratio (M‐H, Random, 95% CI) | 0.77 [0.41, 1.43] |
| 2 Pregnancy‐related deaths | 0 | 0 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 3 ANC coverage: one or more visits | 0 | 0 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Deliveries in a health facility | 1 | 383 | Odds Ratio (M‐H, Random, 95% CI) | 1.55 [0.71, 3.37] |
| 5 Perinatal mortality | 0 | 0 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6 Low birthweight | 0 | 0 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7 Intermittent Prophylactic Treatment for malaria | 0 | 0 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
Comparison 6. Subgroup analysis.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Health systems vs Population ANC coverage: four or more visits | 9 | Odds Ratio (Random, 95% CI) | Subtotals only | |
| 1.1 Health system interventions | 5 | Odds Ratio (Random, 95% CI) | 1.13 [0.96, 1.34] | |
| 1.2 Population interventions | 4 | Odds Ratio (Random, 95% CI) | 1.04 [0.96, 1.13] | |
| 2 Health systems vs Population Pregnancy‐related deaths | 11 | Odds Ratio (Random, 95% CI) | Subtotals only | |
| 2.1 Health system interventions | 4 | Odds Ratio (Random, 95% CI) | 1.22 [0.41, 3.65] | |
| 2.2 Population intervention | 7 | Odds Ratio (Random, 95% CI) | 0.69 [0.46, 1.03] | |
| 3 Country Income Low vs High ANC at least 4 visits | 18 | Odds Ratio (Random, 95% CI) | 1.14 [1.04, 1.25] | |
| 3.1 Low or lower middle income countries | 11 | Odds Ratio (Random, 95% CI) | 1.21 [1.04, 1.40] | |
| 3.2 High or higher middle income countries | 7 | Odds Ratio (Random, 95% CI) | 1.12 [0.95, 1.32] |
Comparison 7. One intervention versus no intervention ‐ Sensitivity analysis by risk of bias.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 ANC coverage: four or more visits | 9 | Odds Ratio (Random, 95% CI) | Subtotals only | |
| 1.1 Primary analysis (ICC 0.02 for studies Kirkwood and Morris) | 9 | Odds Ratio (Random, 95% CI) | 1.07 [0.99, 1.15] | |
| 1.2 Sensitivity analysis using ICC 0.08 | 9 | Odds Ratio (Random, 95% CI) | 1.05 [0.98, 1.14] |
Comparison 8. Combination of interventions versus no intervention ‐ Sensitivity analysis by risk of bias.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 ANC coverage: four or more visits | 4 | Odds Ratio (Random, 95% CI) | Subtotals only | |
| 1.1 Primary analysis (ICC 0.02 for studies Bhutta and Morris) | 4 | Odds Ratio (Random, 95% CI) | 1.07 [0.82, 1.40] | |
| 1.2 ICC 0.08 | 4 | Odds Ratio (Random, 95% CI) | 1.03 [0.77, 1.37] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Azad 2010.
| Methods | Parallel arm cluster‐RCT conducted at 18 sites in Bangladesh between Feb 2005 and Dec 2008. | |
| Participants |
Sample size: 18 clusters (6389 women). Clusters: purposive sampling was performed in 3 different divisions in Bangladesh on the basis of the districts having active Diabetic Association of Bangladesh (BADAS) offices. Within these districts, sub districts (upazilas) and unions (the lowest level administrative units in rural Bangladesh) were also purposefully sampled by use of recommendations from BADAS representatives, the main criteria being perceived limited access to perinatal health care in those unions, and a feasible travelling distance from BADAS district headquarters. Individuals: women were eligible to participate in the study if they were aged 15–49 years, residing in the project area, and had given birth during the study period. |
|
| Interventions |
Target: health system (re‐organisation of health services intervention) and community (education or IEC intervention). Arm 1 (9 clusters, 17,514 births ITT): in intervention clusters, a facilitator convened 18 groups every month to support participatory action and learning for women, and to develop and implement strategies to address maternal and neonatal health problems. 5 of the 9 clusters became TBA intervention clusters and 4 became controls. 482 TBAs were given basic training in undertaking clean and safe deliveries, providing safe delivery kits, recognising danger signs in mothers and infants, making emergency preparedness plans, accompanying women to facilities, and undertaking mouth‐to‐mouth resuscitation. They also received additional training in neonatal resuscitation with bag valve‐mask. Arm 2 (9 clusters, 18,599 births ITT): health services strengthening intervention and basic training of TBAs. |
|
| Outcomes |
Trial primary outcome: neonatal mortality rate. Review outcomes reported: Primary: ANC coverage (at least 4 visits), maternal mortality. Secondary: health facility deliveries, tetanus protection, perinatal mortality, neonatal mortality. Follow‐up: outcomes measured at 1, 2, and 3 years. We have used mortality data from Table 2 (Azad 2010 p. 1197). We used Years 1‐3 combined, excluding the "temporary and tea garden residents" who may not have received the full intervention. We calculated our own cluster adjusted ORs for antenatal care outcomes using the percentages from Table 4, p. 1200 and the denominators from years 1‐3 in Table 2, p. 1197 (all births: intervention n = 15,696 and control n = 15,257). |
|
| Notes | Funders: Women and Children First, the UK Big Lottery Fund, Saving Newborn Lives, and the UK Department for International Development. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "The allocation sequence was decided upon by the project team before drawing" pg 1194 "and was based on clusters rather than individuals." |
| Allocation concealment (selection bias) | Unclear risk | Not clear how allocation was concealed. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not reported. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported. |
| Recruitment bias (for cluster RCTs) | Unclear risk | "Additionally, about 10% of mothers in our study area were temporary residents and mainly came into the cluster areas to give birth, since the tradition is for women to go to their mothers’ home just before delivery. These temporary residents were not exposed to the women’s group intervention, and often had returned to their marital homes outside the study area before the postnatal interview." Presumably this would have affected all clusters. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not reported. |
| Selective reporting (reporting bias) | Low risk | Most relevant outcomes reported. |
| Analysis bias | Low risk | Analysis appropriate for clusters; ICC reported; ITT analysis performed. |
| Other bias | Unclear risk | Baseline imbalances not reported. |
| Overall risk assessment | Low risk | No serious risk of bias concerns. |
Baqui 2008.
| Methods | Parallel 3‐arm cluster‐RCT conducted at 24 sites in Bangladesh (Sylhet district) between Jul 2003 and Dec 2005. | |
| Participants |
Sample size: 24 clusters (113816 women; 46,444 live births analysed). Clusters: 24 clusters (with a population of about 20,000 each) in Sylhet district, a district with poor access to health care, about 15,000 livebirths per year, and the presence of non‐government organisations with the ability to scale‐up the intervention. The area also has the highest neonatal mortality in Bangladesh. Individuals: ever‐married women of reproductive age (15–49 years old). |
|
| Interventions |
Target: health system (addition of home visits) and community (IEC). Arm 1 (8 clusters, 36,059 women): (Home care) the CHWs identified pregnancies through routine surveillance during visits to each household once every 2 months; promoted birth and newborn care preparedness through 2 scheduled antenatal and 3 early postnatal home visits; and provided iron and folic acid supplements during birth and newborn‐care preparedness visits. Arm 2 (8 clusters, 40,159 women): (Community care) in the community‐care arm, female volunteers called community resource people were recruited in each village to identify pregnant women, encourage them to attend community meetings held by the community mobilisers, receive routine ANC, and seek care for signs of serious illness in mothers or newborns. Arm 3 (8 clusters, 37,598 women): (Usual care) families received the usual health services provided by the government, non‐government organisations, and private providers. Refresher training sessions for management of maternal and newborn complications were provided for government health workers in all 3 study arms. |
|
| Outcomes |
Trial primary outcome: reduction in neonatal mortality. Review outcomes reported: Primary: not reported. Secondary: tetanus protection, at least 1 ANC visit, neonatal mortality. Follow‐up: 9, 16, and 24 months. We have analysed these data by combining the 2 arms with individual interventions (home care or community care) compared to the control arm of standard care. Outcome data are included in our Comparison 1. |
|
| Notes | Funders: United States Agency for International Development and saving newborn lives programme by Save the Children (US) with a grant from Bill and Melinda Gates Foundation. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "computer generated pseudo random number sequence." |
| Allocation concealment (selection bias) | Low risk | "The computer‐generated randomisation was implemented by a study investigator who had no role in the implementation of the study." |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | "nature of the intervention meant masking was unachievable." |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported. |
| Recruitment bias (for cluster RCTs) | Low risk | None noted. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Missing data described in study flow chart. |
| Selective reporting (reporting bias) | Low risk | Most relevant outcomes reported. |
| Analysis bias | Low risk | Analysis appropriate for clusters; ICC reported; ITT analysis performed. |
| Other bias | Low risk | No baseline imbalances. |
| Overall risk assessment | Low risk | No serious risk of bias concerns. |
Barber 2008.
| Methods | Parallel‐arm cluster‐RCT conducted at 506 sites in Mexico between 1997 and 2003. | |
| Participants |
Sample size: 506 clusters randomised (individuals not reported), 173 clusters analysed. Clusters: "The rural programme established eligibility in two stages: poor communities were first identified, and low‐income households were identified within those communities". Communities and households were randomly selected based on a probability sample proportionate to the number of women of reproductive age women (15–49 years). Individuals: the sample included women who experienced a singleton live birth between 1997 and 2003, were designated as poor and eligible for Oportunidades, and lived in the original treatment and control communities |
|
| Interventions |
Target: community (financial incentive intervention). Arm 1 (97 clusters, 810 women): Progresa or Opportunidades is a conditional cash transfer program established in 1997 in Mexico, with the dual aim of immediate poverty relief and long‐term impact on the generational transfer of poverty. Every 2 months intervention families received a cash transfer representing approximately a 25% increase in household income (Gertler 2000, p. 3). The cash transfer required specific health behaviours of all members of households. Pregnant women were required to have 5 prenatal visits beginning in the first trimester of pregnancy. Beneficiary births are those births that occurred after the household received their first cash transfer. Households in intervention areas began receiving benefits during the summer of 1998. Arm 2 (61 communities, 215 women): non‐beneficiary births are those that occurred among eligible women prior to receiving the first cash transfer. Households in control clusters began receiving benefits in November 1999. |
|
| Outcomes |
Trial primary outcome: birthweight. Review outcomes reported: Primary: ANC coverage (at least 4 visits). Secondary: at least 1 ANC visit, health facility deliveries, tetanus protection, low birthweight infants. Follow‐up: once. |
|
| Notes | The Mexican social welfare program Oportunidades (now Prospera) has multiple citations. We have incorporated data from a specific analysis conducted on a small sample of women in households involved in this large poverty relief program (Barber 2008). Funders: National Institutes of Health Fogarty International Center TW006084 and National Institute of Child Health and Human Development. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | For the initial cluster‐randomisation, "random assignment was generated at the community level without weighting by use of the randomisation commands in Stata version 2.0" (Fernald 2008). For the survey, areas were randomly assigned "based on a probability sample proportionate to the number of women of reproductive age". p. 20 Barber 2009. |
| Allocation concealment (selection bias) | Unclear risk | Not reported. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Due to the nature of the intervention participants could not be blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported. |
| Recruitment bias (for cluster RCTs) | Low risk | None noted. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Loss to follow‐up described but sample sizes vary in the different reports. |
| Selective reporting (reporting bias) | Low risk | Most relevant outcomes reported. |
| Analysis bias | Low risk | Analysis appropriate for clusters; ITT analysis performed. |
| Other bias | Low risk | No baseline imbalances. |
| Overall risk assessment | Low risk | No serious risk of bias concerns. |
Basinga 2011.
| Methods | Parallel‐arm cluster‐RCT conducted at 166 sites in Rwanda between June 2006 and Oct 2006. | |
| Participants |
Sample size: 166 clusters (2563 women). Clusters: districts without pre‐existing P4P schemes managed by non‐governmental organisations. Individuals: not described. |
|
| Interventions |
Target: health system (financial intervention). Arm 1 (80 clusters, 1242 women): P4P scheme to supplement primary health centres’ input‐based budgets. In this P4P scheme, payments are made directly to facilities and are used at each facility’s discretion. Arm 2 (86 clusters, 1321 women): control facilities would continue to receive traditional input‐based financing for an additional 23 months until the rollout of the scheme was complete. |
|
| Outcomes |
Trial primary outcomes: prenatal care visits and institutional deliveries. Review outcomes reported: Primary: ANC coverage (at least 4 visits). Secondary: ANC coverage (at least 1 visit), health facility deliveries, tetanus protection, use of child preventative care. Follow‐up: baseline and 25 months. |
|
| Notes | Funders: World Bank’s Bank‐Netherlands Partnership Program, the British Economic and Social Research Council, the Government of Rwanda, and the World Bank’s Spanish Impact Evaluation Fund; Global Development Network and the MacNamara Foundation. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "The remaining districts were then grouped into eight blocks based on rainfall, population density, and livelihood data from the 2002 Census.15 Blocks covered between two and 4 districts, depending on district characteristics and size. The blocks were then divided into two sides, and one side of each block was randomly assigned to either the intervention or control group. Randomisation was done by coin toss." |
| Allocation concealment (selection bias) | Unclear risk | Not reported. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Women interviewed in households would not have been aware of their local facility's group assignment. Women attending facilities should also not have been aware of the funding scheme in operation at her local health clinic. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | "All surveys were done by trained enumerators hired by external firms specialised in data collection who were masked to whether they were interviewing in an intervention or control area." |
| Recruitment bias (for cluster RCTs) | Low risk | None noted. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 2.1 % of intervention and 1.9% of control households refused to participate. 12% loss to follow‐up between baseline and end of trial surveys. 11.8% attrition in each treatment arm between first and second interviews. Incomplete household surveys were dropped from the sample after each round. |
| Selective reporting (reporting bias) | Low risk | Most relevant outcomes are reported. |
| Analysis bias | Unclear risk | Analysis appropriate for clusters, ICC and ITT not reported. |
| Other bias | High risk | Allocation assignment not respected due to government restructuring. |
| Overall risk assessment | Unclear risk | Due to uncertainties raised above. |
Bhutta 2011.
| Methods | Parallel‐arm cluster‐RCT conducted at 16 sites in Pakistan (Hala and Matiari sub districts) between Feb 2006 and Mar 2008. | |
| Participants |
Sample size: 16 clusters (51409 individuals). Clusters: catchment areas of primary care facilities with adequate numbers of LHWs. Individuals: not described. Exclusion criteria: areas with low numbers of LHWs and areas with poor access were excluded. |
|
| Interventions |
Target: health system (health worker education) and community (IEC intervention). Arm 1: the intervention package was delivered by trained LHWs through group sessions consisted of promotion of ANC and maternal health education, use of clean delivery kits, facility births, immediate newborn care, identification of danger signs, and promotion of care seeking. Arm 2: in the control clusters, the LHW programme continued to function as usual and no additional attempt was made to link LHWs with the Dais or communities. |
|
| Outcomes |
Trial primary outcome: perinatal and all‐cause neonatal mortality. Review outcomes reported: Primary: ANC coverage (at least 4 visits). Secondary: ANC coverage (at least 1 visit), professional ANC, health facility deliveries, perinatal mortality, stillbirth, neonatal mortality. Follow‐up: every 3 months for 2 years. |
|
| Notes | Funders: grants from the WHO and the Saving Newborn Lives programme funded by the Bill & Melinda Gates Foundation. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "From this list of balanced allocations, we selected one scheme using a computer generated random number." |
| Allocation concealment (selection bias) | Unclear risk | Not reported. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not reported. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Data collectors and their supervisors were masked to cluster allocation p. 406 Bhutta 2011. |
| Recruitment bias (for cluster RCTs) | Low risk | None noted. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Only 414 lost to follow‐up (less than 1%). |
| Selective reporting (reporting bias) | Low risk | Most relevant outcomes reported. |
| Analysis bias | Low risk | Analysis appropriate for clusters; ICC reported; ITT analysis performed. |
| Other bias | Low risk | No baseline imbalances. |
| Overall risk assessment | Low risk | No serious risk of bias concerns. |
Darmstadt 2010.
| Methods | Parallel arm cluster‐RCT conducted in Mirzapur, Bangladesh, between Dec 2003 and Dec 2006. | |
| Participants |
Sample size: 12 clusters (21,140 individuals randomised, 10,700 women with at least 1 pregnancy during 10 preceding months analysed). Clusters: rural unions surrounding an urban central union (excluded from the study) served by a 750 bed private referral‐level hospital. Individuals: all married women of reproductive age (i.e. 15–49 years) in the intervention arm were eligible for enrolment. Women in the survey were eligible if they had had a pregnancy outcome in the last 3 years. |
|
| Interventions |
Target: health system (addition of home visits). Arm 1: 2 home visits (12‐16 and 32‐34 weeks); they were given a labour card for women to present upon arrival at hospital for delivery and 3 postnatal visits on days 2, 5 and 8. CHWs facilitated free‐of‐charge transfer of ill neonates to hospital.The purpose of the antenatal component of the intervention was to increase uptake of ANC (3 visits taking place at home or at a health centre or satellite clinic ‐ distinct from the 2 antenatal CHW home visits), tetanus toxoid vaccination, general pregnancy and newborn care education, and birth preparedness (including delivery at a health facility). Arm 2: standard ANC. |
|
| Outcomes |
Trial primary outcomes: antenatal and immediate newborn care behaviours, knowledge of danger signs, care seeking for neonatal complications, and neonatal mortality. Review outcomes reported: Primary: not reported. Secondary: ANC coverage (at least 1 visit), health facility delivery, IPT for malaria, neonatal mortality. Follow‐up: data collection at delivery and during pre and postnatal home visits. Endline survey Jan ‐ May 2006, before the end of the trial. |
|
| Notes | Funders: The Wellcome Trust: Burroughs Wellcome Fund Infectious Disease Initiative 2000 and the Office of Health, Infectious Diseases and Nutrition, Global Health Bureau, United States Agency for International Development (USAID) through the Global Research Activity Cooperative agreement with the Johns Hopkins Bloomberg School of Public Health (award HRN‐A‐00‐96‐90006‐00). Support for data analysis and manuscript preparation was provided by the Saving Newborn Lives program through a grant by the Bill & Melinda Gates Foundation to Save the Children‐US. The study was registered at clinicaltrials.gov, No. NCT00198627. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation of clusters with a computer‐generated randomisation sequence. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not blinded. |
| Recruitment bias (for cluster RCTs) | Low risk | None noted. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Study flow chart with details of exclusions. Response rate for the endline survey reported as 87.8% (11731/16771). |
| Selective reporting (reporting bias) | Unclear risk | Data for proportion of women who received 2 tetanus toxoid immunisations were not reported. The authors report falling rates during the trial and attribute this to a national shortage of vaccine. |
| Analysis bias | Unclear risk | Method of analysing clusters not clearly described apart from stating ITT analysis performed. |
| Other bias | Low risk | Baseline characteristics similar between arms. |
| Overall risk assessment | Unclear risk | Due to uncertainties raised above. |
Fottrell 2013.
| Methods | Parallel‐arm cluster‐RCT conducted at 18 sites/unions in Bangladesh between Jan 2009 and June 2011. | |
| Participants |
Sample size: 18 clusters (532,996 population). Clusters: purposeful selection of the 3 districts on the basis of having active Diabetic Association of Bangladesh offices and somewhat representing the social and geographical diversity of Bangladesh..basis of perceived limited access to perinatal health care and feasible accessibility from Diabetic Association of Bangladesh district headquarters. Individuals: women whose childbirths or deaths were recorded in the study areas. |
|
| Interventions |
Target: community (IEC intervention). Arm 1 (9 clusters, 12,135 women/births): women's participation groups; effect of monthly participatory learning and action cycle focus on maternal and newborn health. Arm 2 (9 clusters, 13,459 women/births): control not described (presumably no women's participation groups). |
|
| Outcomes |
Trial primary outcome: neonatal mortality rate. Review outcomes reported: Primary: ANC coverage (at least 4 visits). Secondary: health facility deliveries, perinatal and neonatal mortality. Follow‐up: data collected monthly for 24 months. 1 of the control areas (with 3 clusters) included "tea‐garden estates". Residents on these estates were described as having more social and economic disadvantage, and separate analyses were carried out including and excluding these areas. For the analyses in this review, we have used the outcome data that excludes these tea garden residents. |
|
| Notes |
Funders: Big Lottery Fund International Strategic Grant, Wellcome Trust Strategic Award. For the outcome of perinatal mortality we have used stillbirths plus early neonatal deaths. We calculated our own OR using an ICC because the adjusted perinatal deaths OR (without Tea Garden residents) is asymmetrical and would not go into RevMan. See Fottrell 2013 (Table 3, p. 823). |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Paper stated that the sequence "had been decided before drawing the papers" (containing the allocation). |
| Allocation concealment (selection bias) | Low risk | Allocated "by blindly pulling pieces of paper, each representing 1 union from a bottle". |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | The intervention was not masked, it is not clear how lack of blinding might affect outcomes reported. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | The implementation and in‐country monitoring and evaluation teams were blind to the allocation arms" during interim analysis (June 2011). |
| Recruitment bias (for cluster RCTs) | Low risk | None noted. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Study flow chart included displaying reasons for exclusions. Missing data described as 13% on home delivery practice and 0.8% on other secondary outcomes. |
| Selective reporting (reporting bias) | Unclear risk | Relevant outcomes reported although separate analyses for some control group births meant that results were more difficult to interpret. |
| Analysis bias | Unclear risk | Analysis appropriate for clusters but ICC not reported and ITT analysis only performed for primary outcomes. |
| Other bias | Unclear risk | 1 of the control areas (with 3 clusters) included "tea‐garden estates"; residents on these estates were described as having more social and economic disadvantage and separate analyses were carried out including and excluding these areas. For the analyses in this review, we have used the outcome data that excludes these tea garden residents. |
| Overall risk assessment | Unclear risk | We were uncertain whether some of the above might have significantly biased the results. |
Kenyon 2012.
| Methods | Parallel‐arm individual‐randomised RCT conducted at 3 primary care trusts in Birmingham, UK between Jul 2010 and Oct 2011. Trial name: ELSIPS. | |
| Participants |
Sample size: 1324 women. Inclusion criteria: nulliparous women < 28 weeks' gestation assessed by a midwife as having specific social risk. (Risk factors included housing problems, lack of social support, smoking, low maternal weight or obesity, teenage, late booking for ANC.) Exclusion criteria: women under 16 years of age, or teenage mothers recruited to another national trial of additional support during pregnancy. |
|
| Interventions |
Target: health system (re‐organisation of health services: home visits). Arm 1 (662 women): POW provided support, including home visits, in addition to standard ANC and PNC. The POW organised antenatal visits and advised on lifestyle changes. In addition to emotional and health‐related support, the POW helped with financial, legal or benefits problems and with housing. The POW also provided support with care of the newborn, including breastfeeding. Arm 2 (662 women): women in the control group received standard ANC and PNC. |
|
| Outcomes |
Trial primary outcome: Edinburgh Postnatal Depression Scale1 (EPDS) 8–12 weeks postpartum and antenatal visits attended. Review outcomes reported: Primary: ANC coverage (at least 10 contacts). Secondary: preterm birth (< 34 weeks), low birthweight infants, perinatal mortality. Other: depression scores. Follow‐up: intervention involved individual support during pregnancy and follow‐up to 8‐12 weeks postpartum. We did not include data for preterm birth < 34 weeks because our review's definition of preterm birth < 37 weeks. Outcome data from unpublished paper obtained from author: SL Kenyon, s.kenyon@bham.ac.uk. |
|
| Notes | Funders: this work was funded by the National Institute for Health Research (NIHR) through the Collaborations for Leadership in Applied Health Research and Care for Birmingham and Black Country (CLAHRC‐BBC) programme. The views expressed in this publication are not necessarily those of the NIHR, the Department of Health. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation generated by the trial statistician using computer‐generated lists with random block sizes stratified by area. |
| Allocation concealment (selection bias) | Low risk | Telephone randomisation using a registered trial unit ensured allocation concealment. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Inadequate ‐ blinding not possible. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Outcomes were recorded in maternity care notes by staff providing care. Those who collected and entered data were blind to group assignment. |
| Recruitment bias (for cluster RCTs) | Low risk | Not applicable. Not a cluster‐randomised trial. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data on antenatal outcomes available for 100% and 99%. Data for the EPDS at 8‐12 weeks postpartum were available for 82% and 85% of the intervention and control arms. respectively. |
| Selective reporting (reporting bias) | Low risk | All outcomes stated in protocol are reported in the unpublished paper, with the exception of "engagement with other services, as required (e.g. smoking cessation services)". |
| Analysis bias | Low risk | ITT analysis performed. |
| Other bias | Unclear risk | Baseline characteristics similar between treatment groups. |
| Overall risk assessment | Low risk | No serious risk of bias concerns for primary outcomes. |
Kirkwood 2013.
| Methods | Parallel‐arm cluster‐RCT conducted in Ghana between Nov 2008 and Dec 2009. | |
| Participants |
Sample size: 98 clusters (18,609 individuals). Clusters: residential zones. Individuals: all pregnant women and newborn babies living in the Newhints zones, where pregnancies ended between November 2008 and December 2009. |
|
| Interventions |
Target: health system (added home visits by community‐based surveillance volunteers) and community (IEC). Arm 1 (49 clusters, 9174 women): training of community‐based surveillance volunteers to identify pregnant women in their community and to undertake 2 home visits during pregnancy and 3 visits after birth on days 1, 3, and 7, to promote essential newborn‐care practices, and to assess and refer sick newborn babies. Arm 2 (49 clusters, 9435 women): control (no intervention). |
|
| Outcomes |
Trial primary outcome: neonatal mortality rate and coverage of key essential newborn‐care practices. Review outcomes reported: Primary: ANC coverage (at least 4 visits). Secondary: health facility deliveries, neonatal mortality. Other: coverage of key essential newborn care practices. Follow‐up: 2 home visits during pregnancy and 3 visits after birth on days 1, 3, and 7. |
|
| Notes | Funders: WHO, Save the Children’s Saving Newborn Lives Programme from the Bill & Melinda Gates Foundation, and the UK Department for International Development. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "computer generated randomisation." |
| Allocation concealment (selection bias) | Low risk | An independent epidemiologist conducted the randomisation. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not described. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described. |
| Recruitment bias (for cluster RCTs) | Low risk | None noted. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 3 groups of pregnancies were not included in the analysis of NMR: 908 (5%) women were lost to follow‐up during pregnancy; 1216 (7%) had pregnancies that ended early and did not result in a livebirth or stillbirth; and 156 (< 1%) women moved, resulting in a change of treatment groups. |
| Selective reporting (reporting bias) | Low risk | Most relevant outcomes reported. |
| Analysis bias | Low risk | Analysis appropriate for clusters; ICC reported; ITT analysis performed. |
| Other bias | Low risk | No baseline imbalances noted. |
| Overall risk assessment | Low risk | No serious risk of bias concerns. |
Klerman 2001.
| Methods | Parallel‐arm individually‐randomised RCT conducted in the USA between Mar 94 and Jun 98. | |
| Participants |
Sample size: 656 women. Inclusion criteria: African American, eligible for Medicaid, less than 26 weeks' gestation, at least 16 years old, score of 10 or higher on a risk assessment scale. Exclusion criteria: alcoholism and substance abuse, asthma, cancer, diabetes, epilepsy, high blood pressure, sickle cell disease and HIV/AIDS. |
|
| Interventions |
Target: health system (additional and longer appointments) and community (IEC). Arm 1: educational intervention informing women about their risk conditions and what behaviours might improve their pregnancy outcome. Augmented care included educationally oriented peer groups, additional appointments, extended time with clinicians, and other supports. Arm 2: control (no intervention). |
|
| Outcomes |
Trial primary outcomes: pregnancy outcomes, women's knowledge of risks, satisfaction with care. Review outcomes reported: Primary: not reported. Secondary: preterm birth, low birthweight infants. Other: average no. of ANC visits. Follow‐up: every 2 weeks, until the last month of pregnancy then every week. |
|
| Notes | Funders: Federal Agency for Health Care Policy and Research to the University of Alabama at Birmingham, USA. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Sequence generation not described. |
| Allocation concealment (selection bias) | Low risk | "sealed envelopes." |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not described. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | "interviewers blinded" to treatment allocation. Additional outcome data taken from clinic records, data collection forms and a computerised database. |
| Recruitment bias (for cluster RCTs) | Low risk | Not applicable. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Missing data < 10%. 656 women enrolled, but data available for 619; 12 women with fetal deaths excluded from analysis (intervention group: 3 before 20 weeks and 4 after; controls: 3 before 20 weeks and 2 after). |
| Selective reporting (reporting bias) | Low risk | Relevant outcomes reported. |
| Analysis bias | Unclear risk | ITT not stated. |
| Other bias | Low risk | No baseline imbalances. |
| Overall risk assessment | Low risk | No serious risk of bias concerns. |
Kumar 2008.
| Methods | Parallel 3‐arm cluster‐RCT conducted in India between Jan 2004 and May 2005. | |
| Participants |
Sample size: 39 clusters (3891 individuals analysed). Clusters: administrative units. Individuals: all mothers who had delivered during the study period and were available for interview. |
|
| Interventions |
Target: health system (home visits) and community (IEC). Arm 1 (13 clusters): a preventive package of interventions for essential newborn care (birth preparedness, clean delivery and cord care, thermal care [including skin‐to‐skin care], breastfeeding promotion, and danger sign recognition). The strategy included 2 prenatal (60 days and 30 days before expected date of delivery) and 2 postnatal (day 0 and day 3) home visits, community meetings and folk‐song meetings, maternal and newborn health stakeholder meetings, and meetings for community volunteers. Arm 2 (13 clusters): received same package of essential newborn care plus use of a liquid crystal hypothermia indicator (ThermoSpot; a sticker that indicates hypothermia in the newborn by changing colour). Arm 3 (13 clusters): received the standard care available from government and NGO providers in the area. |
|
| Outcomes |
Trial primary outcome: newborn care practices and neonatal mortality rate. Review outcomes reported: Primary: not reported. Secondary: maternal mortality (up to 6 weeks postpartum), ANC coverage (at least 1 visit), health facility deliveries, tetanus protection, stillbirths, neonatal mortality. Other: essential newborn care measures, breastfeeding. Follow‐up: 2 prenatal assessments at 60 days and 30 days before expected date of delivery; 2 postnatal assessments at day 0 and day 3. |
|
| Notes |
Funders: The United States Agency for International Development, Delhi Mission, and the Saving Newborn Lives program of Save the Children US through a grant from the Bill and Melinda Gates Foundation. Perinatal mortality included neonatal deaths up to 28 days after birth. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Stratified cluster‐randomisation conducted at Johns Hopkins University using a computer program. |
| Allocation concealment (selection bias) | Low risk | Allocation performed remotely. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Blinding not possible. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Preliminary analysis (2005) of neonatal mortality rate was said to be masked. |
| Recruitment bias (for cluster RCTs) | Low risk | None noted. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Loss to follow‐up described in study flow diagram with missing data < 20%. |
| Selective reporting (reporting bias) | Low risk | Relevant outcomes reported. |
| Analysis bias | Low risk | Analysis appropriate for clusters; no ICC reported; ITT analysis performed. |
| Other bias | Low risk | No baseline imbalances. |
| Overall risk assessment | Low risk | No serious risk of bias concerns. |
Laken 1995.
| Methods | 3‐arm, individually‐randomised RCT conducted in Detroit, USA; recruitment dates not reported. | |
| Participants |
Sample size: 205 individuals. Inclusion criteria: low‐income women who entered prenatal care at a local clinic before 32 weeks' gestation and who delivered at a tertiary‐level hospital. Exclusion criteria: not reported. |
|
| Interventions |
Target: community (financial incentive intervention). Arm 1 (51 women): women received gift certificates for each prenatal appointment. Arm 2 (53 women): women received gift certificates and a chance to win in a $100 raffle. Arm 2 (101 women): no financial incentive. Women in all 3 groups were offered $10 for the postnatal interview. |
|
| Outcomes |
Triap Primary Outcome: kept appointments for antenatal care and postpartum care Review outcomes reported: Primary: ANC coverage (at least 4 visits). Secondary: maternal mortality, health facility deliveries, perinatal mortality. Follow‐up: 6‐8 weeks postpartum. |
|
| Notes |
Funders: Michigan Health Care Education and Research Foundation. Authors provided unpublished data for coverage, mortality and health facility deliveries by email on 16/1/15. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "random numbers were used" for group assignment. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Clinic staff members were blind to assignment, but women would have been aware of their own assignment. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported. |
| Recruitment bias (for cluster RCTs) | Low risk | Not applicable. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Missing data < 20% for birth outcomes (low risk) but high loss to follow‐up at the postnatal interview (45%). |
| Selective reporting (reporting bias) | Unclear risk | Relevant outcomes reported, but insufficient data provided. |
| Analysis bias | Unclear risk | Methods not reported in sufficient detail. |
| Other bias | Unclear risk | Insufficient information to make a judgement. |
| Overall risk assessment | Unclear risk | Insufficient information to make a judgement. |
le Roux 2013.
| Methods | Parallel‐arm cluster RCT conducted at 26 sites in South Africa between May 2009 and Sept 2010. | |
| Participants |
Sample size: 26 clusters (24 clusters and 1238 individuals analysed). Clusters: neighbourhoods were matched. Eligible neighbourhoods had 450‐600 households, with formal and informal housing, that were within 5 km of health clinics; had 5 to 7 alcohol bars; were noncontiguous or separated by natural barriers; had similar numbers of child care centres, informal shops, and schools; and had households with similar length of residence. Individuals: pregnant women were recruited at an average 26 weeks of pregnancy (range, 3–40 weeks). 94 women in 10 of the 12 standard care neighbourhoods were enrolled post‐birth. Approximately 25% of women in each treatment arm were living with HIV. |
|
| Interventions |
Target: health system (added home visits) and community (IEC). Arm 1 (12 clusters, 644 women): Philani Intervention Program, home visits by CHWs in addition to standard care. Arm 2 (12 clusters, 594 women): standard care, comprehensive healthcare at clinics. |
|
| Outcomes |
Trial primary outcomes: composite of maternal and child health and well being measures. Review outcomes reported: Primary: ANC coverage (at least 4 visits). Secondary: HIV screening, complete antiretroviral course, low birthweight infants. Follow‐up: once during pregnancy and twice after birth: at 1 week, 6 months; additional trial report for 18 months follow‐up. Mortality data for women and infants are reported in the primary trial report. However, these data represent all deaths within the particular time frame of data collection (e.g. all deaths to 6 months post birth, p. 1464 of the 2013 trial report). We consulted with trial authors, but we cannot recalculate the mortality data to fit standard definitions for pregnancy‐related deaths or perinatal deaths. We were particularly concerned that maternal deaths may have been unrelated to pregnancy. We were therefore unable to use mortality data in meta‐analysis. |
|
| Notes | Funders: NIAAA Grant # 1R01AA017104 and supported by NIH grants MH58107, 5P30AI028697, and UL1TR000124. M.T. is supported by the National Research Foundation (South Africa). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Sequence generation not described. Method described as simple randomisation. |
| Allocation concealment (selection bias) | Low risk | Neighbourhoods were randomised in matched pairs using simple randomisation. Randomisation conducted by an independent research team (UCLA). |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | "interviewers were blinded but may have known from participants about CHWs." |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | A driver transported all participants to a central assessment site, allowing interviewers to be blind to group allocation. |
| Recruitment bias (for cluster RCTs) | High risk | "Initially, however, we identified 22% fewer pregnant women in standard care. By redeploying recruiters, we identified an additional 94 women in 10 of the 12 standard care neighbourhoods who were pregnant during the recruitment period (median of 7 late‐entry participants per neighbourhood; range, 3–24). These women were enrolled post‐birth when their infants were a mean age of 9 months old (range, 1–18 months). The final sample (n = 1238) consisted of a median of 51 pregnant women per neighbourhood (range, 23–72)." Analyses were conducted with and without late‐entry participants and results were similar. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 1 matched cluster pair was excluded after 6 months due to poor recruitment. |
| Selective reporting (reporting bias) | Low risk | Relevant outcomes were reported. |
| Analysis bias | Unclear risk | Analysis appropriate for clusters; no ICC reported; ITT analysis not performed. |
| Other bias | Unclear risk | Not reported. |
| Overall risk assessment | Unclear risk | We were uncertain what impact potential biases mentioned above had on results. |
Lewycka 2013a.
| Methods | 2 by 2 factorial cluster‐RCT conducted in Malawi between 2005 and 2009. | |
| Participants |
Sample size: 42 clusters (18960 pregnancies, 18,744 livebirths analysed). Clusters: the unit of randomisation was a cluster of villages and not an individual village. Cluster design was based on census enumeration areas with population of approximately 3000, surrounded by a buffer zone to reduce contamination. The target population was rural communities; the urban administrative centre of the district was excluded. Individuals: all women aged 10‐49 who were willing to participate were enrolled. Women who had a terminal family planning procedure were excluded from the final sample, but not from participating in the intervention. |
|
| Interventions |
Target: community (IEC). Arm 1 (12 clusters, 4557 pregnancies): facilitator initiated women's groups to discuss issues of pregnancy, childbirth and newborn and infant health, as well as peer counselling (infant feeding and care counselling via 5 home visits during and after pregnancy (3rd trimester, week after birth, at 1, 3 and 5 months). Arm 2 (12 clusters, 4722 pregnancies): facilitated women's groups. Arm 3 (12 clusters, 4660 pregnancies): peer counselling via home visits. Arm 4 (12 clusters, 5021 pregnancies): no intervention. All clusters benefited from training of staff in health facilities in essential newborn care. |
|
| Outcomes |
Trial primary outcomes: maternal, perinatal, neonatal and infant mortality rates, and exclusive breastfeeding. Review outcomes reported: Primary: ANC coverage (at least 4 visits), maternal mortality. Secondary: ANC coverage (at least 1 visit), health facility deliveries, IPT for malaria, tetanus protection, HIV screening, perinatal mortality, neonatal mortality. Follow‐up: data were gathered monthly between December 2004 and December 2010. All pregnancies, births and deaths were identified, and surviving mothers and infants were followed for up to 1 year. |
|
| Notes |
Funders: Saving Newborn Lives, UK Department for International Development, Wellcome Trust, Institute of Child Health, and UNICEF Malawi. The primary trial report presents several different analyses, including 1 where Interventions were combined, in order to evaluate the effect of women's groups (arm 1 + 2 combined versus arm 3 + 4 combined) and the effect of peer counselling (arm 1 + 3 combined versus arm 2 + 4 combined) separately. For the analysis in our review's Comparison 1: Lewycka 2013a refers to the women's group intervention only. Lewycka 2013b refers to the peer counselling intervention only. These 2 single‐intervention arms are compared to the arm with no intervention. For the analysis in our review's Comparison 2: Lewycka 2013a refers to the trial arm that received both women's groups and peer counselling. This arm is compared to the arm with no intervention. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation done with computer program Stata. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Group assignment was masked for data analysis. Data collection was conducted independently of program implementation and was not fed back to inform the intervention. |
| Recruitment bias (for cluster RCTs) | Low risk | None noted. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Women with miscarriages were excluded from analysis. Loss to follow‐up about 20%. Miscarriage rates varied across study arms and were more frequent in the combined intervention cluster. |
| Selective reporting (reporting bias) | Low risk | Relevant outcomes reported. |
| Analysis bias | Low risk | Analysis appropriate for clusters; no ICC reported; ITT analysis performed. |
| Other bias | Unclear risk | The authors discuss an interaction between the 2 interventions and baseline imbalances after randomisation across several outcomes. |
| Overall risk assessment | Unclear risk | We were concerned that the exclusion of women with miscarriages might bias maternal death rates. |
Lewycka 2013b.
| Methods | 2 by 2 factorial cluster RCT conducted in Malawi between 2005 and 2009. Lewycka 2013b describes the same trial as Lewycka 2013a above, and all of the descriptions and risk of bias are identical to that above. We have had to duplicate the 'Risk of bias' judgements below due to RevMan requirements. |
|
| Participants | For the analysis in our review's Comparison 1: Lewycka 2013a refers to the women's group intervention only. Lewycka 2013b refers to the peer counselling intervention only. These 2 single‐intervention arms are compared to the arm with no intervention. | |
| Interventions | See Lewycka 2013a. | |
| Outcomes | See Lewycka 2013a. | |
| Notes | See Lewycka 2013a. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation done with computer program Stata. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Group assignment was masked for data analysis. Data collection was conducted independently of program implementation and was not fed back to inform the intervention. |
| Recruitment bias (for cluster RCTs) | Low risk | None noted. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Women with miscarriages were excluded from analysis. Loss to follow‐up about 20%. Miscarriage rates varied across study arms and were more frequent in the combined intervention cluster. |
| Selective reporting (reporting bias) | Low risk | Relevant outcomes reported. |
| Analysis bias | Low risk | Analysis appropriate for clusters; no ICC reported; ITT analysis performed. |
| Other bias | Unclear risk | The authors discuss an interaction between the 2 interventions and baseline imbalances after randomisation across several outcomes. |
| Overall risk assessment | Unclear risk | We were concerned that the exclusion of women with miscarriages might bias maternal death rates. |
Lund 2012.
| Methods | A parallel arm cluster‐RCT conducted on the island of Unguja, Zanzibar, Tanzania between Mar 2009 and Mar 2010. | |
| Participants |
Sample size: 24 clusters (2367 individuals randomised, 2550 analysed). Clusters: government‐run primary healthcare facilities, 4 per district, were selected, based on 2 inclusion criteria: highest number of ANC clients in 2008 and the availability of at least 1 midwife in the facility. All included facilities had mobile phone network coverage. Individuals: women who attended ANC at 1 of the 24 selected healthcare facilities were included on their first ANC visit and followed until 42 days after delivery. Women were eligible for study participation irrespective of their mobile phone and literacy status. Exclusion criteria: PIH, anaemia, multiple pregnancy and malpresentation. |
|
| Interventions |
Target: health system (policy/practice change). Arm 1 (12 clusters, 1351 women): women received an automated text messaging service for health information and appointment reminders, mobile phone vouchers to enable women to contact health services. The content of messages depended upon gestational age. Women received 2 messages/month < 36 weeks and then 2 per week. Only women with registered phone numbers received text messages; women without received only vouchers with mobile credit. Arm 2 (12 clusters 1286 women): women attending control health facilities received standard ANC, with the goal of at least 4 ANC visits. |
|
| Outcomes |
Trial primary outcome: skilled delivery attendance. Review outcomes reported: Primary: ANC coverage (at least 4 visits), maternal mortality. Secondary: tetanus protection, perinatal mortality, neonatal mortality. Other: skilled birth attendant (midwife/doctor/nurse) at delivery. Follow‐up: women were offered at least 4 antenatal visits and a postnatal home visit within 48 hours after delivery. Women were interviewed for demographics at trial entry at 6 weeks after delivery. The trial definition of perinatal mortality is non‐standard, stated as stillbirth and death of the infant up to 42 days. |
|
| Notes | Funders: Danish International Development Cooperation. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomisation described as 'simple randomisation' but sequence generation not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Clusters and study participants were not masked due to the nature of the intervention requiring overt participation. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described. |
| Recruitment bias (for cluster RCTs) | Low risk | None noted. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Exclusions/withdrawals < 20% were due to exclusion criteria (development of complications) or loss to follow‐up. |
| Selective reporting (reporting bias) | Low risk | Relevant outcomes reported. |
| Analysis bias | Low risk | Analysis appropriate for clusters, ITT analysis was performed. No ICC reported. |
| Other bias | Unclear risk | No baseline imbalances noted. The trial definition of perinatal mortality is non‐standard, stated as stillbirth and death of the infant up to 42 days. |
| Overall risk assessment | Low risk | No serious risk of bias concerns. |
Majoko 2007.
| Methods | Parallel arm cluster‐RCT conducted in a rural setting in Zimbabwe between Jan 1995 and Oct 1997. | |
| Participants |
Sample size: 23 clusters (13517 individuals). Clusters: health centres in a rural setting. Gutu district was chosen as the study area because the utilisation of maternity services and reproductive health status of the community had been previously studied.The district had 25 health facilities, comprising a district hospital and 24 rural health centres (RHCs) serving a population of 195 000. Individuals: all mothers booking for ANC since 01/12/94. |
|
| Interventions |
Target: health system (re‐organisation of ANC). Arm 1: an experimental package of ANC with reduced procedures, clear goals and symphysio‐fundal height measurements. Visits scheduled according to a 5 visit program with reduced routine procedures at these visits. First visit: risk assessment, health education and delivery plan, Hb, rapid plasma reagin, tetanus vaccination and do urinalysis. Visit 2 at 24–28 weeks: exclude multiple pregnancy, check for hypertensive disorders, and do urinalysis. Visit 3 at 32–34 weeks: Exclude anaemia, check fetal growth and review delivery plans, check Hb and do urinalysis. Visit 4 at 36–38 weeks: check fetal growth, exclude abnormal presentation, discuss labour and do urinalysis. Visit 5 at 40–41 weeks: check fetal well being, referral for post‐term induction at 42 weeks and do urinalysis. Arm 2: the control arm followed the standard schedule with a visit every 4 weeks from booking until 28 weeks, every 2 weeks between 28 and 36 weeks and weekly after 36 weeks until delivery. Risk assessment was performed at the booking and subsequent visits, and referral for hospital delivery was made using a list of risk markers recommended by the Zimbabwe Ministry of Health and Child Welfare. Blood pressure, body weight and urinalysis were measured at each visit, while Hb and syphilis test (RPR) were performed at the first visit. Women who tested positive for syphilis had treatment initiated at the booking visit. Oral iron supplementation was provided to all women in both models. |
|
| Outcomes |
Trial primary outcomes: number of antenatal visits, referrals for antenatal, intrapartum or postpartum problems, place of delivery and low birthweight infant (< 2500 g). Review outcomes reported: Primary: maternal mortality. Secondary: health facility deliveries, preterm birth, perinatal mortality, neonatal mortality. Follow‐up: women were followed up at ANC visits. |
|
| Notes | Funders: Swedish International Development Cooperation Agency (Sida/SAREC) through the Sida–University of Zimbabwe Reproductive Health Research Programme. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Sequence generation not described. Randomisation described as stratified according to the availability of telecommunication for referrals. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not blinded. |
| Recruitment bias (for cluster RCTs) | Low risk | None noted. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 13,517 women randomised. Full records were available for 78% of women with curtailed follow‐up for an additional 20%. Communication with the authors has clarified the numbers used for perinatal deaths, adding back in many women whose records were not retrieved. |
| Selective reporting (reporting bias) | Low risk | Relevant outcomes reported. The authors were contacted to clarify the numbers used to calculate perinatal death. |
| Analysis bias | Low risk | Analysis appropriate for clusters; no ICC reported; ITT analysis performed. |
| Other bias | Low risk | No baseline imbalances. |
| Overall risk assessment | Low risk | No serious risk of bias concerns after contacting authors with data queries. |
Manandhar 2004.
| Methods | Parallel arm cluster‐RCT conducted in a rural setting in Nepal between Sept 1999 and Nov 2003. | |
| Participants |
Sample size: 24 clusters (28931 individuals). Clusters: Rural Village Development Committees were matched for geography, population and ethnicity; 12 pairs were randomised. Individuals: married women aged 15‐49 residing within the study area who could potentially conceive within the period of the study. Exclusion criteria: unmarried women, permanently separated or widowed women; women under the age of 15 or older than 49. |
|
| Interventions |
Target: community (IEC intervention). Arm 1 (12 clusters, 14,884 women): participatory women's groups facilitated by a female facilitator who convened 9 women's group meetings every month. The facilitator supported groups through an action learning cycle in which they identified local perinatal problems and formulated strategies to address them. Arm 2 (12 clusters, 14,047 women): health service strengthening activities were undertaken in both intervention and control areas. These improvements included provision of equipment. |
|
| Outcomes |
Trial primary outcome: neonatal mortality rate. Review outcomes reported: Primary: not reported. Secondary: ANC coverage (at least 1 visit), health facility deliveries, perinatal mortality, neonatal mortality. Follow‐up: 2 interviews for each pregnancy, at 7 months and at 1 month postpartum. The adjusted OR for maternal mortality was taken directly from the systematic review Prost 2013. |
|
| Notes | Funders: DFID, with important support from the Division of Child and Adolescent Health, WHO, the United Nations Children's Fund, and the United Nations Fund for Population Activities. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Sequence to randomised pairs was from a random numbers list; to randomise within pairs a coin toss was used. |
| Allocation concealment (selection bias) | Low risk | Allocation sequence was generated centrally (Kathmandu) before enrolment of participants in relevant clusters. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Outcome assessor was blinded to group allocation. |
| Recruitment bias (for cluster RCTs) | Low risk | None noted. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All clusters analysed. |
| Selective reporting (reporting bias) | Low risk | Relevant outcomes reported. |
| Analysis bias | Unclear risk | Analysis appropriate for clusters; ITT analysis performed; ICC not reported. |
| Other bias | Low risk | No baseline imbalances noted. |
| Overall risk assessment | Low risk | No serious risk of bias concerns. |
Melnikow 1997.
| Methods | Parallel arm, individually‐randomised RCT conducted at 5 sites in the USA between Jan 94 and Dec 95. | |
| Participants |
Sample size: 104 women. Inclusion criteria: all pregnant women planning to attend prenatal care at 1 of 5 participating family planning and women's health clinics. All randomised women were eligible for the state of California's Medicaid program (assistance with healthcare costs). Exclusion criteria: women planning prenatal care at another location or women considering abortion. |
|
| Interventions |
Target: community (financial incentive). Arm 1: 34 women were randomised to receive at taxi voucher and 35 received a coupon for a baby blanket. Arm 2: the control group received no incentive to attend the first antenatal appointment. |
|
| Outcomes |
Trial primary outcome: compliance with the first prenatal appointment. Review outcomes reported: Primary: not reported. Secondary: not reported. Follow‐up: the primary study outcome was compliance with the first prenatal appointment. It appears that additional outcomes were not collected. |
|
| Notes |
Funders: funded in part by a grant from the American Academy of Family Physicians' Foundation. No usable data. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Sequence from a table of random numbers. |
| Allocation concealment (selection bias) | Low risk | Sealed envelopes were prepared remotely from clinics. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Women were not told that the study had to do with appointment compliance. It is not clear if staff were aware of group assignment. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Outcomes assessors for the primary outcome were blind to group assignment. |
| Recruitment bias (for cluster RCTs) | Low risk | Not applicable. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 22/69 (32%) in the intervention group lost to follow‐up and excluded; 8/35 in controls. |
| Selective reporting (reporting bias) | Unclear risk | No review outcomes reported. |
| Analysis bias | Low risk | ITT analysis performed. |
| Other bias | Low risk | No baseline imbalances noted. |
| Overall risk assessment | Unclear risk | High loss to follow‐up with no relevant review outcomes. |
Midhet 2010.
| Methods | Parallel arm cluster‐RCT conducted in Balochistan, Pakistan. A baseline survey took place in Aug‐Sept 1998. Intervention package in place by March 2000; follow‐up survey was conducted between March and April 2002. | |
| Participants |
Sample size: 32 clusters (2561 individuals analysed). Clusters: Balochistan is an underdeveloped and poor region of Packistan with the highest maternal mortality rate. Each eligible village cluster had between 5‐15 villages. The project area was divided into 3 zones based on distance from the district hospital. Randomisation took place within each zone. Individuals: women who had had a pregnancy in the last 12 months. |
|
| Interventions |
Target: health system (health worker education and re‐organisation of services ‐ transport) community (IEC intervention). Arm 1: women were provided information on safe motherhood through pictorial booklets and audiocassettes; TBAs were trained in clean delivery and recognition of obstetric and newborn complications; and emergency transportation systems were set up. The intervention was delivered to women only in 1 group and to both women and husbands in another. Arm 2: the project provided training for health professionals at the district hospital, who provided care for women from both intervention and control clusters. Government healthcare providers also trained staff in primary health facilities throughout the study area. |
|
| Outcomes |
Trial primary outcomes: perinatal or neonatal death; use of iron‐folic acid.
during pregnancy; prenatal care; tetanus immunisation; and delivery in the district hospital Review outcomes reported: Primary: not reported. Secondary: ANC coverage (at least 1 visit), health facility deliveries, tetanus protection, perinatal mortality, neonatal mortality. Follow‐up: household survey was conducted 2 years after intervention. The perinatal death outcome seems to have been calculated with live births rather than all births. For our analyses, we have used data from the 2002 follow‐up survey only. |
|
| Notes |
Funders: NICHD, USAID, UNICEF, World Health Organization, British Council, Government of Japan and The Asia Foundation, and implemented by The Asia Foundation’s Islamabad office. Residual impact survey conducted 2 years after project ended, in 2004; on a sample of 900 women randomly selected from immunisation records at the district health office. We have used data from the original cluster‐randomised trial only. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation by "blindly drawing village cluster names written on folded chits". |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described. |
| Recruitment bias (for cluster RCTs) | Unclear risk | At the 2002 follow‐up survey, intervention clusters were expanded, resulting in 47% increase in size of the control arm. At the 2004 follow‐up survey, refusals or locked households in a selected cluster were replaced by the nearest available household. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The follow‐up survey interviews were completed for 95.2% of visited households. |
| Selective reporting (reporting bias) | Unclear risk | Relevant outcomes were reported. |
| Analysis bias | Unclear risk | Analysis appropriate for clusters; ICC reported; ITT not stated. |
| Other bias | Unclear risk | Information bias. Most of the results are from the 2002 follow‐up survey, but authors state that some data are from the 2004 survey. |
| Overall risk assessment | Unclear risk | We were uncertain whether the risk of bias concerns above might have impacted the results. |
More 2012.
| Methods | A parallel arm cluster‐RCT conducted in India between Oct 2006 and Sept 2009. | |
| Participants |
Sample size: 48 clusters (18,197 individuals). Clusters: eligible clusters were communities in urban slums in Mumbai for which a perinatal vital registration was set up as part of the City Initiative for Newborn Health in 2005. The wards were selected purposively for the 2005 Initiative based on accessibility and relative infant mortality rates. Communities with transient populations and areas where resettlement was being negotiated were both excluded. Individuals: women of all ages residing in intervention clusters, whether pregnant or not pregnant, were invited to attend women's groups. |
|
| Interventions |
Target: community (IEC intervention). Arm 1: women were invited to weekly meetings that emphasized knowledge of local health services, perinatal health care, and negotiating optimal care with family and health providers. Arm 2: no weekly meetings. Surveillance data were collected in both intervention and control areas. 12 interviewers collected these data at 6 weeks postpartum. Unwell mothers or infants in either arm were referred and treatment expedited. |
|
| Outcomes |
Trial primary outcome: perinatal care, maternal morbidity, and extended perinatal mortality. Review outcomes reported: Primary: maternal mortality. Secondary: professional ANC, health facility delivery, perinatal mortality, neonatal mortality. Follow‐up: weekly women's group meetings and attendance records. Interviews took place 6 weeks postpartum. Retrospective census at end of trial to pick up any missed births in all 48 clusters. |
|
| Notes | Funders: ICICI Foundation for Inclusive Growth – Centre for Child Health and Nutrition, and the Wellcome Trust. DO was funded by a Wellcome Trust Fellowship (081052/Z/06/Z). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation by "drawing of lots". |
| Allocation concealment (selection bias) | Unclear risk | Allocation not concealed. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Interviewers may have been aware of the assignment of their particular area, but the authors argue that they "were focused on their task (surveillance) and did not dwell on the comparative nature of the trial." Data analysts were blinded. |
| Recruitment bias (for cluster RCTs) | Unclear risk | 9 clusters were expanded for insufficient births, and 2 clusters reduced for excess births. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition was less than 20% in each arm, and authors have provided a study flow diagram with documented reasons for loss to follow‐up. |
| Selective reporting (reporting bias) | Low risk | Relevant outcomes were reported. |
| Analysis bias | Low risk | Analysis appropriate for clusters; ITT analysis performed; ICC not reported. |
| Other bias | Unclear risk | Other initiatives during the trial period include outreach services by health volunteers, birth registration and pulse polio campaigns and infectious disease surveillance. Conditions in slums improved over the trial period. |
| Overall risk assessment | Unclear risk | We were uncertain whether the risk of bias concerns above might have impacted the results. |
Mori 2015.
| Methods | Cluster‐RCT in Bulgan, Mongolia. | |
| Participants |
Sample size: 501 women randomised. Clusters: the unit of randomisation was the Soum and bag, small geographic areas in Mongolia. Each Soum has a healthcare facility where women must register their newborn. 18 geographic areas were randomised, after selection for administrative convenience and to avoid contamination. Individuals: pregnant women living in Bulgan, Mongolia. |
|
| Interventions |
Target: community. Arm 1: distribution of maternal and child health handbooks during pregnancy. The MCH handbook logged maternal health and personal information, pregnancy, delivery and postpartum health and weight, dental health, parenting classes, child developmental milestones from 0‐6 years, immunisation records and height and weight charts for children. Arm 2: women received standard care. |
|
| Outcomes |
Trial primary outcome: number of antenatal visits; proportion of women attending 6 or more antenatal visits. (The national standard for ANC in Mongolia is 6 visits.) Review outcomes reported: Primary: ANC coverage of at least 4 visits, maternal mortality Secondary: maternal outcomes: morbidity during pregnancy, mode of delivery, breastfeeding initiation, maternal depression and health (EPDS and GHQ). Infant outcomes: birthweight, Apgar score, NICU admission, neonatal mortality at discharge. Maternal healthy behaviours. Follow‐up: data collection at 1 month postpartum. |
|
| Notes |
Funders: this study was funded by the National Center for Global Health and Medicine, Tokyo, Japan. Significant group differences noted for distances travelled to nearest health centre (greater in the intervention group) and for wealth index (the control group was poorer). The authors report that travel time did not function as an effect modifier; however, women from a higher socioeconomic background attended more ANC visits. Trial authors provided unpublished outcome data upon request. The trial statistician (HN) calculated ORs and 95% confidence intervals using the generalised estimating equations (GEE) method to adjust for cluster design and baseline differences, including wealth. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Sequence according to the shuffling of sealed envelopes. |
| Allocation concealment (selection bias) | Low risk | Allocation was concealed in sealed envelopes at time of randomisation. All areas were randomised at the same time. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Masking was not possible for this intervention. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Masking was not possible for this intervention. |
| Recruitment bias (for cluster RCTs) | Low risk | No problems with recruitment are reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 3 randomised areas were excluded; 1 was the subject of a pilot study, and 2 areas were included in another health study. 9 clusters each received the intervention or the control. Missing outcome data for individual women is reported and minimal. |
| Selective reporting (reporting bias) | Low risk | Prespecified outcomes have been reported. Addtional analyses were obtained from the authors upon request. The trial data file has been published online with the trial report. |
| Analysis bias | Low risk | Analyses were undertaken with methods appropriate for cluster trials; the authors used GEE methods to adjust for the effects of cluster design and baseline variables. A sample size calculation was undertaken and met. |
| Other bias | Unclear risk | The authors reported baseline imbalances between clusters for travel time to health centre and wealth. The authors reported that recall bias may exist due to data collection at 1 month after birth. |
| Overall risk assessment | Low risk | Overall the trial was well planned and conducted. |
Morris 2004a.
| Methods | Parallel arm cluster‐RCT conducted in Honduras between Aug 2000 and Oct 2002. | |
| Participants |
Sample size: 70 clusters (˜5600 households). Clusters: municipalities, which were selected because they had the highest prevalence of malnutrition in the country. Individuals: women were eligible who had been pregnant during the previous 12 months but were not pregnant on the day of the interview. |
|
| Interventions |
Target: health system (financial resources to health team and training) and community (financial incentive and IEC). Arm 1: 1 (20 clusters): a household‐level package consisted of monetary vouchers paid to women in households whose residence in the beneficiary municipalities had been recorded in a special census done in mid‐2000. 3 (20 clusters): financial resources to local health teams combined with a community‐based nutrition intervention involving the training of lay nutrition promoters. 2 (10 clusters): both packages. Arm 2 (20 clusters): neither package. |
|
| Outcomes |
Trial primary outcome: use of health services. Review outcomes reported: Primary: ANC coverage (at least 4 visits). Secondary: tetanus protection. Follow‐up: monthly for 10 months. |
|
| Notes |
Funders: Government of Honduras. We have calculated a final score by adding the change scores to the baseline scores presented in the trial report, Table 2 Program Effects, p. 2034. For our review's Comparison 1: Morris 2004a is the 2 single intervention trial arms added together and compared with the control group. For our review's Comparison 2: Morris 2004b is the 'both packages' trial arm compared with the control group. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Within each stratum, random allocation was achieved by a child drawing coloured balls from a box, without replacement. Thus, the randomisation was both stratified and blocked." |
| Allocation concealment (selection bias) | Low risk | "The aperture of the box was sufficiently small that once the child had inserted his or her arm, it was impossible for him or her to see the coloured balls. From the day of the randomisation onwards, there was no attempt to conceal the allocation." |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Surveys were conducted by an independent data collection company. Not clear if individual interviewers would have been aware of cluster assignment. |
| Recruitment bias (for cluster RCTs) | Low risk | None noted. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Study flow chart included. Loss to follow‐up less than 5% in all arms. |
| Selective reporting (reporting bias) | Low risk | Relevant outcomes reported. |
| Analysis bias | Low risk | Analysis appropriate for clusters (no ICC reported); ITT analysis performed. |
| Other bias | High risk | The intervention involving direct transfer of resources to health teams and part of the service‐level package was not successfully implemented in the relevant clusters. Non baseline imbalances noted. |
| Overall risk assessment | Unclear risk | We were uncertain whether the risk of bias concerns relating to poor implementation impacted the results. |
Morris 2004b.
| Methods | This trial is the same as that described in Morris 2004a above. Due to RevMan requirements, we have replicated the 'Risk of bias' assessments below. However, Morris 2004b describes a specific 'both packages' arm of Morris 2004a and not a different study. | |
| Participants | For our review's Comparison 2, Morris 2004b is the 'both packages' trial arm compared with the control group. | |
| Interventions | See Morris 2004a. | |
| Outcomes | See Morris 2004a. | |
| Notes | See Morris 2004a. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Within each stratum, random allocation was achieved by a child drawing coloured balls from a box, without replacement. Thus, the randomisation was both stratified and blocked." |
| Allocation concealment (selection bias) | Low risk | "The aperture of the box was sufficiently small that once the child had inserted his or her arm, it was impossible for him or her to see the coloured balls. From the day of the randomisation onwards, there was no attempt to conceal the allocation." |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Surveys were conducted by an independent data collection company. Not clear if individual interviewers would have been aware of cluster assignment. |
| Recruitment bias (for cluster RCTs) | Low risk | None noted. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Study flow chart included. Loss to follow‐up less than 5% in all arms. |
| Selective reporting (reporting bias) | Low risk | Relevant outcomes reported. |
| Analysis bias | Low risk | Analysis appropriate for clusters (no ICC reported); ITT analysis performed. |
| Other bias | High risk | The intervention involving direct transfer of resources to health teams and part of the service‐level package was not successfully implemented in the relevant clusters. Non baseline imbalances noted. |
| Overall risk assessment | Unclear risk | We were uncertain whether the risk of bias concerns relating to poor implementation impacted the results. |
Mullany 2007.
| Methods | A parallel, 3‐arm RCT conducted at 1 site in Nepal between Aug 2003 and Jan 2004. | |
| Participants |
Sample size: 299 women and 145 couples. Inclusion criteria: currently married women attending their first ANC visit at PGMH (gestational age 16–28 weeks) whose husbands were present at the hospital compound were eligible. Exclusion criteria: women were excluded if they were < 18 years of age or lived > 90 min away from the PGM Hospital. |
|
| Interventions |
Target: Community (IEC). Arm 1: 2 35 minute health education sessions administered in a private room, for women only, 4‐6 weeks apart, plus a detailed health education flier. Arm 2: 2 35 minute health education sessions administered in a private room, for women and their husbands, 4‐6 weeks apart, plus the detailed health education flier. Arm 3: a brief flier with standardised health messages. Women in the control groups received standard ANC. |
|
| Outcomes |
Trial primary outcomes: maternal health care utilisation and birth preparedness. Review outcomes reported: Primary: ANC coverage (at least 4 visits). Secondary: health facility deliveries. Follow‐up: baseline or initial visit and questionnaire, 36‐week ANC visit, questionnaire 2 weeks postpartum. |
|
| Notes | Funders: Hopkins Population Center Dissertation Fieldwork Grant, awarded by the Andrew Mellon Foundation, and a grant awarded by the Bill and Melinda Gates Institute for Population and Reproductive Health. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Using the statistical software program Stata 8.0 (Stata Corp., College Station, TX, USA), a list was generated randomizing the sequence of recruitment of study groups for each day of the recruitment period." |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not described. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Blinding of research assistants administering questionnaires not described. Data entry and coding described as blinded. |
| Recruitment bias (for cluster RCTs) | Low risk | Not applicable. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data for all women (442) for final ANC visit; data for 386 (87%) for postnatal questionnaire. |
| Selective reporting (reporting bias) | Low risk | Relevant outcomes reported. |
| Analysis bias | Low risk | ITT analysis performed. |
| Other bias | Low risk | No baseline imbalances noted. |
| Overall risk assessment | Low risk | No serious risk of bias concerns noted. |
Omer 2008.
| Methods | Parallel arm cluster‐RCT conducted at 10 sites in Pakistan (Sindh province) between Jun 2000 and April 2001. | |
| Participants |
Sample size: 10 clusters (1070 women interviewed, 969 households visited). Clusters: 10 enumeration areas from 3 districts in the Sindh province of Pakistan were chosen. 8 of the 10 areas were rural. Individuals: women who were pregnant or had delivered in the past 3 years were eligible. |
|
| Interventions |
Target: health system (change in health worker practice) and community (IEC). Arm 1 (5 clusters, 529 women): a LHW showed an evidence‐based tool and embroidered cloth that depicted 3 important maternal practices, viz. attending antenatal check‐ups, giving colostrum after birth and avoiding heavy work. Arm 2 (5 clusters, 541 women): the LHW delivered standard care. |
|
| Outcomes |
Trial primary outcome: health practices during pregnancy, including ANC. Review outcomes reported: Primary: not reported. Secondary: ANC coverage (at least 1 visit), professional (LHW) ANC. Other: giving colostrum at birth, stopping heavy work, exclusive breastfeeding for 4 months. Follow‐up: after the intervention had been in use for 10 months, field workers completed data collection in 1 week. Fieldworkers also conducted a household survey of pregnant women or those who had delivered in the past 3 years. |
|
| Notes |
Funders: Canadian International Development Agency International Development Agency’s (CIDA) Canada Fund for Local Initiatives in Pakistan. Data for ANC visits were not reported by randomisation group and not usable. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Sequence from computerised random numbers generator. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Blinding not possible due to the nature of the intervention. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Fieldworkers collecting data were blinded to the allocation of the community in which they worked but women may have revealed which group they were in if they mentioned the embroideries. |
| Recruitment bias (for cluster RCTs) | Low risk | None noted. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | The total number of women visited by LHW is not stated, only households visited. It is not clear how many households refused the survey or whether there were women approached who refused the interview. There seem to me more women with data for visits than there were households visited or women interviewed. |
| Selective reporting (reporting bias) | Unclear risk | Exclusive breastfeeding for 4 months is mentioned in the abstract, but there are no results for this outcome. |
| Analysis bias | High risk | It is stated that ITT analysis was undertaken but most results were not reported by randomisation group but rather by whether or not women had seen the LHW. There is no evidence of any adjustment made for correlations within or between clusters. The analysis seems to have been done at the individual level. It was stated that baseline imbalance was taken into account in secondary analysis. |
| Other bias | Unclear risk | Baseline imbalances are not clearly stated. |
| Overall risk assessment | High risk | Due to unclear group denominators, attrition and inappropriate analysis methods. |
Penfold 2014.
| Methods | Cluster‐RCT in 6 districts of Southern Tanzania. INSIST (Improving Newborn Survival in Southern Tanzania) community intervention trial. | |
| Participants |
Sample size: 512 women delivering 521 babies completed the final survey (9 pairs of twins). Clusters: 65 intervention and 67 control clusters were randomised. 1 control cluster was lost to follow‐up. Individuals: women were eligible for the survey if they had given birth in the previous year and were aged 13‐49. |
|
| Interventions |
Target: health system Arm 1: the intervention consisted of prenatal (3) and postnatal (2) counselling home visits to support pregnant women and educate women about birth preparation, delivery and recommended newborn care practices. Counselling tools included picture cards and a doll. Arm 2: pregnant women received standard care. |
|
| Outcomes |
Trial primary outcomes: breastfeeding within an hour of delivery, birth attendants for home deliveries washing hands before childbirth or wearing gloves, and babies fed only breast milk in the first 3 days. Review outcomes reported: Primary: not reported Secondary: other behaviours promoted during counselling to maximise newborn health, e.g. skilled attendance for childbirth, birth preparedness (for home deliveries), immediate drying and wrapping of the baby, clean cord care and delayed bathing of the baby. Follow‐up: outcome data are based on a post‐intervention survey conducted by trained interviewers with women who had given birth in the past 12 months. |
|
| Notes |
Funders: the study was funded by the Bill & Melinda Gates Foundation through the Saving Newborn Lives program of Save the Children (www.savethechildren.org/
programs/health/saving‐newborn‐lives/), Unicef, the Laerdal Foundation and the Batchworth Trust. The study was part of INSIST (www.clinicaltrials.gov, NCT01022788), and was approved by the review boards of Ifakara Health Institute, the Medical Research Coordinating Committee of the National Institute for Medical Research, Tanzania Commission for Science and Technology, and the London School of Hygiene and Tropical Medicine, UK. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Sequence by list of random numbers. Wards with baseline data were randomised using stratification (matched pairs according to baseline neonatal mortality and population). |
| Allocation concealment (selection bias) | Low risk | Allocation performed at same time as sequence generation, by central randomisation team. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not blinded. |
| Recruitment bias (for cluster RCTs) | Low risk | Not noted. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 1 cluster (ward). |
| Selective reporting (reporting bias) | Unclear risk | Outcome data on coverage had to do specifically with the home visits offered by the trial; it is not clear whether any other ANC was available to women. Neonatal mortality data are reported, but perinatal mortality data are not. |
| Analysis bias | Low risk | Methods appropriate for cluster trials. ITT analysis. |
| Other bias | Unclear risk | Baseline variables comparable. Authors state that receipt of counselling visits may have been over‐reported; implementation was difficult with just half of women receiving a postnatal visit (p. 10). There may have been some contamination of control clusters due to women living near intervention clusters receiving visits or women in control areas inadvertently moving into intervention areas to be with family during childbirth (p. 10). |
| Overall risk assessment | Low risk | No serious risk of bias noted. |
Persson 2013.
| Methods | A parallel arm cluster‐RCT conducted in 90 sites in Vietnam, Quang Ninh Province between Jul 2008 and Jun 2011. | |
| Participants |
Sample size: 90 clusters (22,561 births; 1243 mother‐newborn pairs randomly selected for secondary outcomes). Clusters : eligible districts had NMR ≥ 15/1000 in 2005. Individuals: all mother–newborn pairs within the study area with births from July 2008 to June 2011 were eligible. There were 22,561 births registered in the study area during the study period. |
|
| Interventions |
Target: health system (policy/practice change). Arm 1 (44 clusters, 11,906 births): the intervention consisted of facilitated work with stakeholder groups (primary care staff, local politicians and women's union representatives) on the commune level and included the identification of local perinatal health problems and use of a problem‐solving cycle. The 44 communes in the intervention group had a total of 1508 maternal and newborn health groups (MNHG) meetings, lasting approximately 2 hours each. The problem‐solving process identified 15‐27 unique problems which resulted in 19‐27 unique actions applied 297‐649 times per year. Arm 2 (46 clusters, 10,655 births): standard health care in control communities. A 6% random sample of all registered live births, surviving the neonatal period, was continuously selected each month in order to represent the entire birth cohort for secondary outcome data. Home visits were performed for families of a deceased newborn in another random sample. |
|
| Outcomes |
Trial primary outcome: neonatal mortality. Review outcomes reported: Primary: maternal mortality. Secondary: ANC coverage (at least 1 visit), health facility deliveries, tetanus protection, perinatal mortality, neonatal mortality. Other: postnatal home visit. Follow‐up: data collection took place monthly for 3 years. |
|
| Notes | Funders: Swedish International Development Cooperation Agency (Sida), Swedish Research Council, and Uppsala University. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation for the cluster assignments is described as by random number lists. Randomisation for the sample of women used to assess secondary outcomes is not described. |
| Allocation concealment (selection bias) | Unclear risk | The sequence was "concealed until the intervention assigned". |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Data collectors had no contact with the facilitation of maternal and newborn health groups. It is not clear that they were blind to what was happening in their area, though. |
| Recruitment bias (for cluster RCTs) | Low risk | None noted. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | There were attempts to ensure a full data set for the primary outcome (neonatal mortality) but denominators used for the secondary outcomes vary. Loss to follow‐up in this population is not described. |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting. |
| Analysis bias | Low risk | Analysis appropriate for clusters; ICC reported; ITT analysis not stated. |
| Other bias | Unclear risk | In the first year it appeared that women in the control communities were more likely to lack education, be from poor households and be from minority ethnic groups. |
| Overall risk assessment | Unclear risk | We were uncertain how potential risks above impacted on findings. |
Richter 2014.
| Methods | Cluster‐randomised trial in KwaZulu‐Natal, South Africa. Clinicaltrials.gov identifier: NCT00972699. | |
| Participants |
Sample size: intervention clusters (4 clinics; n = 544); control clusters (4 clinics; n = 656). Clusters: unit of randomisation was the clinic (n = 8). 1 clinic in the intervention had 2 sites. Overall sites randomised were the 5 intervention and 4 controls. Individuals: potential participants were pregnant women at least 18 years old living in the neighbourhood from May 2009 to September 2010. Only HIV pregnant women were eligible for the intervention. The control group were determined to be at no‐ or low‐risk for contamination of intervention activities. |
|
| Interventions |
Target: health system ‐ addition of peer mentors to antenatal and postnatal care. Arm 1: enhanced intervention (EI). The EI consisted of an initial assessment and 4 antenatal and 4 postnatal small group sessions led by Peer Mentors. The intervention targeted 5 domains: HIV prevention, infant health, healthcare and health monitoring, mental health and parenting tasks (p. 707 Richter). Both treatment arms received standard care: dual therapy to prevent HIV transmission, referral and treatment for women with low CDC count (< 400 or WHO stage 4 illness), a recommended single feeding method for the first week of life, and tinned powdered infant milk. Mobile phones were used to collect data in this study. Transport was also provided. Arm 2: standard care as above: dual therapy to prevent HIV transmission, referral and treatment for women with low CDC count (< 400 or WHO stage 4 illness), a recommended single feeding method for the first week of life, and tinned powdered infant milk. |
|
| Outcomes |
Trial primary outcome: a summary measure of indicators of maternal and infant health, including: child health status, health care and health monitoring, HIV transmission‐related behaviours, mental health and social support. Review outcomes reported: Primary: ANC coverage (at least 4 visits) Secondary: Proportion of women with HIV receiving complete anti‐retroviral course to prevent transmission, low birthweight Follow‐up: 6 days, 6 month and 12 months post birth. |
|
| Notes |
Funders: this work was supported by NIAAA grant R01 AA017104, the Center for HIV Identification, Prevention, and Treatment Services (CHIPTS) NIMH grant P30
MH58107; the UCLA Center for AIDS Research (CFAR) grant P30 AI028697; and the National Center for Advancing Translational Sciences through UCLA CSTI Grant
UL1 TR000124. We have not used mortality data as reported for this trial because numbers reflect the trial's own definition (all deaths within 12 months, for example) rather than the standard definitions of maternal mortality and perinatal mortality required for use in this review. We contacted authors (Mary Jane Rotheram: rotheram@ucla.edu) for clarification, but it was not possible to recalculate the trial deaths with our definitions. We were also concerned that any maternal deaths reported may have been HIV‐related rather than pregnancy‐related. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Clinic were randomised according to matched pairs with a simple randomisation schedule by UCLA. |
| Allocation concealment (selection bias) | Low risk | Not stated, but randomisation and allocation took place remotely (UCLA). |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | All women were invited into the PeerMentor program while in clinic waiting rooms, and all women gave written consent. It is unclear if women would have been aware of the content of the intervention versus standard care. Research and clinical staff would have been aware of allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Female research assistants were trained to interview women at baseline and post‐birth. Because interviewers were assigned by clinic, they were not blinded to condition. |
| Recruitment bias (for cluster RCTs) | Unclear risk | Women were invited into the PeerMentor program from July 2008, but data collection from March 2009. Data available only for the last 602 women recruited. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Follow‐up rates varied: 70% at post‐birth interview; 57% at 6 months; 24% at 12 months. |
| Selective reporting (reporting bias) | Unclear risk | Longer‐term outcomes have been published in multiple reports. Mortality data are not usable due to non‐standard definitions of maternal mortality and perinatal mortality. |
| Analysis bias | Low risk | Adjustments made for cluster‐design. |
| Other bias | Low risk | None noted. |
| Overall risk assessment | Unclear risk | We were uncertain how the above risks, specifically attrition, may have impacted the findings. |
Tripathy 2010.
| Methods | A parallel arm cluster‐RCT conducted at 36 sites in India, Jharkhand and Orissa, between Jul 2005 and Jul 2008. | |
| Participants |
Sample size: 36 clusters (19030 births). Clusters: not clearly stated. The study area had disproportionately high NMR and an underserved population. Individuals: women aged 15‐49 residing in the project area who gave birth during the study (July 31, 2005‐July 30, 2008). Women who migrated out of the region were excluded from some analyses. 2 women from each arm refused the interview and were excluded. |
|
| Interventions |
Target: community (IEC). Arm 1 (18 clusters, 9686 births): monthly facilitator‐convened women's groups monthly for a total of 20 meetings. Groups discussed maternal and newborn health problems and practices using pictures, role‐play and storytelling. In addition, health committees were formed to provide village representatives the chance to learn about health services and comment on their design and management. Arm 2 (18 clusters, 9089 births): in control clusters only health committees were formed. |
|
| Outcomes |
Trial primary outcome: reduction in neonatal mortality rate and maternal depression. Review outcomes reported: Primary: maternal mortality. Secondary: ANC coverage (at least 1 visit), health facility deliveries, tetanus protection, perinatal mortality, neonatal mortality, stillbirth. Follow‐up: data collection took place monthly. |
|
| Notes |
Funders: Health Foundation, UK Department for International Development, Wellcome Trust, and the Big Lottery Fund (UK). Data for years 1‐3 combined excluding migrants were used for our comparison 4 (Table 2, p. 1188). All ORs were taken directly from the published report (Tripathy 2010). The trial authors adjusted data for clustering, stratification, maternal education, assets and any tribal affiliation. Antenatal care outcome data are found in Table 5, p. 1190. It is unclear whether the OR presented for perinatal mortality (excluding migrants) includes infants who died between 0‐6 days or 0‐28 days (Table 3, p. 1188). |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Drawing folded papers with numbers corresponding to clusters from a basket. |
| Allocation concealment (selection bias) | Unclear risk | The first 4 numbers drawn were assigned to the intervention; the next 4 to the control group. Participants in the randomisation process would have been aware of the next assignment but as the process was transparent it would not have been possible to manipulate the process. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not blinded. |
| Recruitment bias (for cluster RCTs) | Low risk | None noted. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition and exclusions outlined in study flow diagram with limited missing data. |
| Selective reporting (reporting bias) | Unclear risk | Analysis was presented fully but there were multiple analyses with various adjustments and multiple testing which made results difficult to interpret. |
| Analysis bias | Unclear risk | Both adjusted and unadjusted data were provided. Adjustment for clustering and other factors did not appear to change the main conclusions. ICC of 0.0005 was mentioned but it's unclear if this was actually used for adjustments of data for neonatal death. Analysis was stated as by ITT. |
| Other bias | Unclear risk | There were baseline differences in household assets, maternal education, literacy and tribal membership; the intervention clusters were generally poorer. Some analyses adjusted for baseline differences. |
| Overall risk assessment | Unclear risk | We were uncertain how potential risks above impacted on findings. |
Villar 1992.
| Methods | Parallel arm RCT conducted in 4 Latin American countries including Argentina (Rosario), Brazil (Pelotas), Cuba (Havana), and Mexico City between Jan 1989 and Mar 1991. | |
| Participants |
Sample size: 2235 individuals. Inclusion criteria: 1 or more risk factor for delivering a low birthweight infant, including: a history of low birthweight, premature birth, fetal death, infant death; mothers less than 17 years of age, weighing less than 50 kg, or under 1.5 m tall; low socioeconomic level; less than 3 years of education; smokers; consumption of alcohol; single mothers; started prenatal care between 15‐22 weeks; singleton pregnancy. Exclusion criteria: chronic renal disease, cardiovascular problems, chronic hypertension, cerclage, Rh negative, mental disorders. |
|
| Interventions |
Target: health system (the addition of home visits to standard ANC package) and community (IEC intervention). Arm 1 (1115 women): 4‐6 home visits from a nurse or social worker during pregnancy, with emphasis on health education, uptake of ANC, improving participants' social networks and individual psychological support. The intervention provided a hotline, a dedicated hospital office, a poster and booklet and a guided tour of the hospital delivery facilities. Arm 2 (1120 women): standard ANC which took place in clinics. |
|
| Outcomes |
Trial primary outcome: low birthweight (for sample size) and indicators of social support. Review outcomes reported: Primary: not reported. Secondary: preterm birth, low birthweight infants, perinatal mortality, neonatal mortality. Other: mean no. ANC visits (these data were not usable for meta‐analysis). Follow‐up: women were followed during their pregnancies (from 15‐22 weeks) and up to 40 days postpartum. |
|
| Notes | Funders: International Development Research Center, Ottawa, Canada. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Sequence from computer‐generated code in blocks of 20, stratified according to centre. |
| Allocation concealment (selection bias) | Low risk | Sealed, opaque envelopes were used for group assignment. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Home visitors and women were aware of group assignment; staff at health clinics were not aware of group assignment unless women themselves disclosed this. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Langer 1993 reports that the outcome assessors at the Mexico City site were blind to group assignment. |
| Recruitment bias (for cluster RCTs) | Low risk | Not applicable. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Missing data < 20%. Loss to follow‐up not described. 83% of women received the planned number of home visits, with 90% visited at least once. Denominators for delivery outcomes were stated as 1033 for intervention and 1040 for control (< 10%). |
| Selective reporting (reporting bias) | Low risk | None noted. |
| Analysis bias | Unclear risk | ITT not stated. |
| Other bias | Unclear risk | Baseline imbalances not described. |
| Overall risk assessment | Low risk | No serious risk of bias concerns. |
Villar 2001 (WHO 2001).
| Methods | Parallel arm cluster‐RCT conducted in 53 clinics in Argentina, Cuba, Saudi Arabia and Thailand between May 1996 and April 1998. | |
| Participants |
Sample size: 53 clusters (24526 individuals). Clusters: clinics serving 300 new patients within 24 months. The clinics had to be part of a public or semi‐public health system and not require direct fee‐for‐services payment. Clinics had to have an ANC system in place with adequate staffing and be able to implement and fund tests or activities required by the protocol. Individuals: all women attending prenatal care for the first time at any participating clinic were eligible. Women later found not to be pregnant were excluded. Multiple births were excluded from some outcomes (specifically low birthweight outcomes). Women had to be traceable at delivery, including women transferred to hospitals as high‐risk. |
|
| Interventions |
Target: health system (reorganisation of services). Arm 1 (27 clusters, 12,568 women): a reduced visits regime of ANC. Women classified as higher risk received standard ANC but were analysed according to ITT. The new model of care included 4 antenatal visits for low‐risk women. The visits were goal‐oriented and focused on scientifically evaluated components of ANC. Arm 2 (26 clusters, 11,958 women): standard ANC. |
|
| Outcomes |
Trial primary outcomes: low birthweight (< 2500 g), pre‐eclampsia/eclampsia, severe postpartum anaemia (< 90 g/L Hb), treated urinary tract infection. Review outcomes reported: Primary: maternal mortality. Secondary: ANC coverage (< 5 visits), tetanus protection, syphilis treatment, preterm birth, low birthweight infants, perinatal mortality, neonatal mortality, stillbirth. Other: median no. of ANC visits, pre‐eclampsia, antepartum haemorrhage, mode of delivery, and others. Follow‐up: schedule of antenatal visits and data collection at delivery. |
|
| Notes | Funders: UNDP/UNFPA/WHO/World Bank Special Programme of Research, Development and Research Training in Human Reproduction of WHO. Additional support from City of Rosario, Argentina, Ministry of Health, Cuba, National Institute of Public Health, Mexico, The Population Council ‐ Regional Office for Latin America and the Caribbean, Ministry of Health, Saudia Arabia, Swedish Agency of Research Cooperation with Developing Countries, Ministry of Public Health and Faculty of Medicine, Khon Kaen University, Thailand, Department for International Development, UK; Mother Care ‐ John Snow, Inc; National Institute for Child Health and Human Development, National Institutes of Health, USA, and The World Bank. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Sequence was computer‐generated. Randomisation was stratified according to study site and clinic characteristics. |
| Allocation concealment (selection bias) | Low risk | Allocation kept centrally until each site had completed the basic introductory training of study personnel, which took place in both intervention and control clinics. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Blinding not possible. Staff recording outcome data after the birth were not aware of group allocation but outcomes were recorded by staff providing ANC (not blinded). |
| Recruitment bias (for cluster RCTs) | Low risk | None noted. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Loss of follow‐up varied for delivery outcomes but was reasonably low and balanced across groups (i.e. loss to follow‐up in reduced visits group was 253/12,568 (2.0%) and standard ANC group was 290/11958 (2.4%). For the low birthweight outcome 138/11672 single births were missing for the new model clinics and 81/11121 in the standard care clinics. |
| Selective reporting (reporting bias) | Low risk | Relevant outcomes were reported. |
| Analysis bias | Low risk | Analysis appropriate for clusters; ICC reported; ITT analysis was performed. |
| Other bias | Low risk | There was some evidence of imbalance at baseline. Women in the new model were less likely to smoke during pregnancy (10.4% versus 12.5%) but it was more likely that women in the new model clinics to have lower levels of education (17.5% education less than primary versus 15.7%). The impact of these differences at baseline are not clear and the differences are taken into account in the adjusted analyses. |
| Overall risk assessment | Low risk | No serious risk of bias concerns. |
Wahlstrom 2011.
| Methods | Cluster‐randomised trial in rural Laos. | |
| Participants |
Sample size: 40 clusters randomised. Post‐intervention survey n = 127 intervention and n = 190 controls. Clusters: 2 provinces were selected, with 2 districts in each province. Eligible districts were selected based on having geographically separate populations with different economic standards and having road access. 10 villages were randomly selected in 2 districts (Champasack and Khammouane): in each district 5 randomised villages had health centres and 5 did not. For the Champasack district, the intervention was implemented in the better‐off villages. This was decided by coin. In the district of Khammouane, poorer villages received the intervention with the better‐off villages serving as controls. Individuals: women aged 15‐49 years and currently pregnant with a reported gestational length of 32 weeks or more, or who had recently given birth (during the last year for the pre‐intervention survey, and during the last 6 months for the post‐intervention survey). |
|
| Interventions |
Tareget: community and health system. Arm 1: 10 community awareness‐raising meetings over 6 months; provision of basic ANC equipment to health centres; a refresher course for healthcare providers. Arm 2: control arm not described and presumed to be standard care. |
|
| Outcomes |
Trial primary outcomes: difference in overall ANC used as reported by interviewed women and checked with the ANC record book. Review outcomes reported: Primary: ANC coverage at least 4 visits Secondary: ANC from health centres Follow‐up: baseline data collected in 2008. Intervention June ‐ November 2010. Intervention lasted 6 months; follow‐up survey in March 2011 (3 months after intervention ended). We obtained unpublished outcome data from the author: Rolf Wahlstrom, rolf.wahlstrom@ki.se. |
|
| Notes | For the review outcome of at least 1 ANC visit, we used the data for the trial outcome 'overall ANC'. Funders: Swedish International Development Cooperation Agency, the Swedish Institute (SI) and the Ministry of Health of Laos. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Sequence described as random. |
| Allocation concealment (selection bias) | Unclear risk | Allocation concealment not described. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Women were not blind to the intervention. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Interviewers were aware of the goals of the study. |
| Recruitment bias (for cluster RCTs) | High risk | Problems with recruitment in the intervention arm for the post‐intervention survey. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Pre‐ and post‐intervention surveys were different populations. Authors report problems in recruitment for the post‐intervention survey but no attrition. |
| Selective reporting (reporting bias) | Low risk | Relevant outcome data reported. |
| Analysis bias | Unclear risk | Authors describe adjustments for clustering and intra‐class correlations as "reduced by combining two districts from different provinces as intervention and control areas". |
| Other bias | High risk | Authors report that baseline differences in education favoured the control group and impacted overall results. Women were recruited after 32 weeks of pregnancy, which limited the intervention's capacity to improve rates of the outcome of ANC at least 4 visits. Recall bias: visits were based on women's reports; responses were validated against ANC booklets for a third of respondents. |
| Overall risk assessment | High risk | We were concerned about the impact of baseline group differences and recruitment problems as noted above. |
Waiswa 2015.
| Methods | Uganda Newborn Study (UNEST) 2 armed cluster‐randomised trial. | |
| Participants |
Sample size: 63 clusters randomised; baseline survey n = 194 intervention and n = 201 controls; endline survey n = 894 intervention and n = 893 control. Clusters: Uganda, Iganga and Mayuge districts in eastern Uganda, predominantly rural with 65 villages and total population of 70,000 at time of the study. Local health services include 1 100 bed hospital and 19 health centres that provide delivery services. 63 villages randomised (31 intervention and 32 control. Individuals: all consenting pregnant women and their newborns residing in the study area between September 2009 and August 2011. women were eligible for the baseline survey if they had a live birth in the last 4 months; women were eligible for the end line survey if they had a live birth in the last 12 months. |
|
| Interventions |
Target: community and health systems. Arm 1: CHWs made 5 home visits (2 prenatal and 3 postnatal) with extra visits for sick or small newborns. Health facility strengthening in all facilities (both arms) to improve quality of care. Facility strengthening included: "6‐day in‐service training, provision of a once‐off catalytic supply of equipment and medicines, as well as collaboration with the district health team to continuously improve the quality of care provided to mothers and newborns" (p. 4). Arm 2: the control arm received standard care as well as facility strengthening. |
|
| Outcomes |
Trial primary outcomes: ANC coverage and services. Birth preparedness, skilled attendance at delivery, and postnatal care, as well as increases in healthy practices including breastfeeding, thermal care, and hygiene. Review outcomes reported: Primary: ANC coverage 4 or more visits; Mortality data were collected but not reported in this publication (authors emailed with no reply 5/15). Secondary: deliveries in a health facility, ANC coverage one visit Follow‐up: baseline survey March‐Aug 2008; Study began 01/09/2009 and ended 01/08/2011; end line survey Sept‐Nov 2011. Home visits were: 2 prenatal (first and third trimesters) and 3 postnatal (days 1, 3 and 7). |
|
| Notes | Funders: this study was supported by the Sida/SAREC‐Makerere University‐ Karolinska Institutet Research collaboration as well as by funds provided by Save the Children through a grant from the Bill & Melinda Gates Foundation. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated restricted randomisation was done in a 1‐to‐1 ratio by an independent epidemiologist from the London School of Hygiene and Tropical Medicine. |
| Allocation concealment (selection bias) | Low risk | Allocation done remotely as above. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Women and staff not blind. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Outcomes assessors not blind. |
| Recruitment bias (for cluster RCTs) | Low risk | No problems with recruitment reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Different populations for pre and post‐intervention surveys. |
| Selective reporting (reporting bias) | High risk | Mortality data not reported yet in published reports; analysis of a household survey to document mortality outcomes is ongoing; low birthweight not reported according to intervention arm; preterm birth mentioned in discussion but unclear if these data were available. |
| Analysis bias | Low risk | ITT analysis. Authors report adjustments made for cluster design. |
| Other bias | Unclear risk | Demographic variables comparable at baseline (age, parity and household wealth); only women with a live birth were eligible; mortality data are not reported; there were no buffer zones between control and intervention villages. |
| Overall risk assessment | Unclear risk | Conduct of the trial is of low risk of bias, though reporting bias is unclear. |
Walker 2013.
| Methods | Parallel arm cluster‐RCT conducted in 2 states in Mexico between Jan 2009 and Dec 2010. | |
| Participants |
Sample size: 27 clusters (2053 individuals). Clusters: health centres located in the study area had to have > 25 registered births in 2007, have basic equipment and supplies to attend deliveries and be located 1‐2 hours from the referral hospital. Study areas were 2 states, Oaxaca or Guerrero, with high maternal mortality. Individuals: birth outcome data were taken from monthly interviews and chart review instead of direct observation. Staff were asked to recall their 3 most recent deliveries. |
|
| Interventions |
Target: health system (addition of obstetric nurse or professional midwife to physician‐based health centre). Arm 1 (12 clusters, 1129 births): the addition of an obstetric nurse or professional midwife to the physician‐based team in rural health clinics. Arm 2 (15 clusters, 924 births): women attending control clinics received standard obstetric care. |
|
| Outcomes |
Trial primary outcome: an index of ANC measures. Primary: ANC coverage (at least 4 visits). Secondary: pregnant women initiating ANC in first trimester Follow‐up: monthly data collection for 18 months. The trial author clarified the ANC outcomes presented in the text and in Table 3 of the primary trial report. Prof Walker replied, "Appropriate care in Table 3 signifies first antenatal visit before 12 weeks gestation." This would be our outcome: 1.4 The proportion of women who initiate ANC in the first trimester. We used "In accordance with WHO standards" from Table 3 for our review's primary outcome 1.1 pregnant women attending at least 4 ANC visits. Dilys Walker: dilys.walker@ucsf.edu. |
|
| Notes | Funders: The National Center for Gender Equity and Reproductive Health,the National Institute of Women, and the Bill and Melinda Gates Foundation. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Sequence was computer‐based. |
| Allocation concealment (selection bias) | Unclear risk | Allocation concealment not described, but it appears that all sites were randomised at the same time through a computer program. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not blinded. |
| Recruitment bias (for cluster RCTs) | Low risk | None noted. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | For delivery outcomes, data are based on provider recall of the most recent 3 deliveries. |
| Selective reporting (reporting bias) | Unclear risk | Few relevant outcomes reported. ANC coverage not clearly reported. Correspondece with author to clarify ANC outcome data for this review. |
| Analysis bias | Unclear risk | Adjusted for clusters but ITT not stated and no ICC reported. |
| Other bias | High risk | Recall bias may have distorted the data for delivery outcomes in both the intervention and control sites. These data have not been reported in usable form. Some outcomes were composites, e.g. care meeting WHO standards, resulting in very low numbers in either group appearing to receive adequate care. Baseline differences were present in the proportion of literate women in each group, with control clusters having significantly less literate women (1021/1259 intervention versus 705/995 control, P < 0.001). It was more likely that information on baseline characteristics was recorded for intervention group women, so it is possible that there were further differences between I and C groups at baseline. |
| Overall risk assessment | High risk | For above reasons. |
Wu 2011.
| Methods | A parallel arm cluster‐RCT conducted in Anhui province, Eastern China, between Aug 2000 to Jul 2002. | |
| Participants |
Sample size: 20 clusters (1264 individuals). Clusters: townships were selected and paired according to: place of birth (hospital, family planning centre or other); per capital income; average number of prenatal care visits; and location. Population, proportion of farmers, infant death rate, number of midwives and number of hospital beds were also taken into account. Townships were required to have an existing health facility and the staff necessary to implement the trial. Individuals: women who had given birth in the past year were eligible for the interview. |
|
| Interventions |
Target: health system (health worker education and equipment provision) and community (IEC). Arm 1 (10 clusters, 673 women): the intervention had 3 health system components: training of community midwives, a public awareness campaign with posters and leaflets about prenatal care, and provision of equipment to health centres. Arm 2 (10 clusters, 591 women): usual health system. |
|
| Outcomes |
Trial primary outcomes: prenatal care utilisation and perinatal outcomes. Primary: ANC coverage (at least 4 visits). Secondary: ANC initiation in first trimester, health facility deliveries, stillbirths, perinatal mortality, neonatal mortality. Follow‐up: data were collected from health centre records monthly. Observation in intervention hospitals monthly. Training of midwives involved initial sessions over 2 days and meetings every 3 months. Poster and leaflets in the community throughout trial. Interviews with pregnant women conducted after delivery (mothers of dead infants were not approached for interviews). |
|
| Notes |
Funders: Academy of Finland, Finnish Ministry of Education (DPPH‐program), European Commission INCO Programme "Structural hinders to and promoters of good maternal care in rural China ‐ C HIMACA (015396). Results of a hospital‐based survey are not included in this trial report. We have excluded the perinatal mortality data reported for this trial due to multiple risk of bias concerns, including unclear denominators. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Sequence generated from a coin toss. |
| Allocation concealment (selection bias) | Unclear risk | 1 township in each matched pair was assigned to intervention or control by a coin toss. Allocation concealment was not described. Matching was checked after randomisation for matching. It was not clear if allocation could be changed. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not blinded. |
| Recruitment bias (for cluster RCTs) | Unclear risk | None noted. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | The denominators for perinatal outcomes were not clear (results expressed at percentages) so it was not possible to assess attrition bias for these outcomes. 1306 women were eligible for the survey, and data were reported for 1264 (missing data ˜ 3%). 42 mothers were described as missing; 2 refused; 27 were out of the village; and 13 cases were missing for "other reasons". |
| Selective reporting (reporting bias) | Unclear risk | Denominators not clearly reported. Mortality stats after the intervention were compared with those before the intervention with major differences reported. |
| Analysis bias | Unclear risk | Adjustments made for clusters, but no information on ICC or what difference adjustment made. ITT not stated. |
| Other bias | High risk | The perinatal data are difficult to interpret due to differences between clusters before the intervention. Data from the community based survey showed group differences for parity, but similarities on other demographic traits. Mortality data were taken from township family planning records. The early neonatal death rate for girls' is much higher than that for boys', causing the authors to doubt the utility of mortality outcomes for the intervention. They wrote, "If the impact of the family planning policy is larger on perinatal mortality than maternal care, then it is hard for any health care intervention to have an effect on perinatal health outcomes". Authors state that the Provincial Health Board implemented a program of ANC in control and intervention townships just 8 months after the trial had begun. 2 intervention districts and 4 control districts also had a prepayment scheme for maternal care implemented during this period. These health initiatives likely contaminated the controls and diluted the effects of the intervention. Furthermore, trialists failed to distribute posters and leaflets because of poor co‐operation between family planning and health sectors, and so this component of the intervention was not completed. |
| Overall risk assessment | High risk | Due to multiple risk of bias concerns above. |
ANC: antenatal care CHW: community health worker Hb: haemoglobin IEC: information, education and communication intervention ICC: intra‐cluster correlation coefficient IPT: intermittent prophylactic treatment ITT: intention‐to‐treat LHW: lady healthcare worker NGO: non‐governmental organisations NICU: neonatal intensive care unit NMR: neonatal mortality rate OR: odds ratio P4P: payment for performance POW: pregnancy outreach worker RCT: randomised controlled trial TBA: traditional birth attendant
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Alisjahbana 1995 | Not randomised. This study was a 15‐month longitudinal, observational study of 2 treatment areas. Women in the intervention area received integrated a maternity services, and women in the control area women received standard care. |
| Baqui 2009 | Intervention does not target ANC. This study compares neonatal assessment by community health workers with assessment carried out by physicians. |
| Bhutta 2008 | This study was a pilot study for the cluster‐randomised trial reported in Bhutta 2011. This study was not randomised. |
| Colbourn 2013 | This study examined the effects of community mobilisation and quality improvement on maternal, neonatal and perinatal mortality. The objective of the trial was not improved ANC coverage. Percentage of women attending women's groups was a secondary outcome. |
| Dance 1987 | This trial investigated whether additional care for women who had 1 previous low birthweight baby would effect birthweight and other pregnancy outcomes. An increase of ANC coverage was not an objective of the trial. |
| Doyle 2014 | The intervention in this trial involved prenatal education and support, with the objective of improved perinatal outcomes among disadvantaged women. An increase in ANC coverage was not an aim of this trial. |
| Ellard 2012 | Protocol. This trial will investigate whether increased training of healthcare workers of has an impact on perinatal and maternal mortality rates. Availability of resources, resource use, and a process evaluation are also planned. Improved coverage of ANC is not an objective of the trial. |
| Foord 1995 | This report describes an observational study to evaluate improved ANC and is not a randomised trial. |
| Ford 2001 | This is a trial of an intervention to improve the self‐efficacy of teenage mothers. The intervention does not have the goal of increased ANC coverage. |
| Gokcay 1993 | This trial looked at the possible differences between care delivered by midwives versus lady home visitors. Increased antenatal coverage was not an objective of the trial. |
| Homer 2001 | The intention of this trial was to compare community based and standard ANC in order to improve clinical outcomes, especially rate of caesarean birth. Improved ANC coverage was not the objective of the trial. |
| Ickovics 2007 | This trial investigated group versus standard ANC in young pregnant women (aged 18‐25) with a view to improved pregnancy outcomes, psychosocial function, costs and patient satisfaction. Improved coverage of ANC was not an objective of the trial. |
| Jennings 2010 | This trial investigated group versus standard ANC in young pregnant women (aged 18‐25) with a view to improved pregnancy outcomes, psychosocial function, costs and patient satisfaction. Improved coverage of ANC was not an objective of the trial. |
| Kafatos 1989 | This study examined the effects of a nutrition education program for pregnant women. Improved ANC coverage was not part of the objective of the trial. |
| Koniak‐Griffin 1991 | The purpose of this intervention was to improve the maternal skills of adolescent mothers. An improved coverage of ANC was not an objective of the trial. |
| Koniak‐Griffin 2000 | This trial compared an augmented and a standard form of prenatal and follow‐up care for at‐risk pregnant women. Increased coverage of ANC was not an objective of the trial. |
| Kusulasai 1993 | This is a quasi‐randomised trial (alternate allocation by odd or even hospital number) with no allocation concealment. The study compares a reduced‐visits regimen of ANC with standard care. An increase in ANC coverage was not an objective of the trial. |
| Leung 2012 | The intervention for this trial involved group psychotherapy with the aim of reducing depression and stress in new mothers. Increased ANC coverage was not an objective of the trial. |
| Magriples 2008 | This study is not a randomised trial but an analysis of patterns of prenatal care utilization for women enrolled in a randomised trial. Data were retrieved from computerised databases and patterns of care were evaluated using the Kotelchuck index. Predictors of visits were explored, and structured interviews with participants were conducted. |
| Miller 2012 | This cluster‐randomised trial examined the effects of training for traditional birth attendants in the Dera Ghazi Khan District of Punjab, Pakistan. The objective of the trial was improved birth attendant performance and reduced perinatal mortality. |
| Munjanja 1996 | This trial looked at a program of reduced ANC visits and considered the impact of this change on maternal and infant outcomes. An increase in ANC coverage was not an objective of the trial. |
| Olds 1986 | The intervention in this trial of home visitation had the objective of reducing and preventing child abuse and neglect. Outcomes included number of substantiated reports of child abuse from state records and level of domestic violence in the home as measured in the Conflict Tactics Scale. Increased ANC was not an objective of the trial. |
| Olds 1995a | This trial investigated the effects of prenatal and postnatal home visits on the maternal life course and on children's longer‐term functioning. Increased ANC coverage was not an objective of this trial. |
| Rodriguez‐Angulo 2012 | This trial examined the impact of an intervention to educate women about serious pregnancy complications. Increased ANC coverage was not an objective of the trial. |
| Schellenberg 2011 | This trial examined the impact of a community‐based intervention to improve the care of newborn infants. Increased ANC coverage was not an objective of the trial. |
| Srinivasan 1995 | This trial compared an augmented and a standard form of prenatal and follow‐up care for at‐risk pregnant women. Increased coverage of ANC was not an objective of the trial. |
| Tomlinson 2014 | The intervention in this trial involved 2 prenatal and 5 postnatal visits with the aim of improving neonatal outcomes, including breastfeeding at 12 weeks and decreasing transmission of HIV. Increased coverage of ANC was not an objective of the trial. Data for coverage of antenatal HIV testing were collected. |
| Tough 2006 | This trial compared augmented prenatal care with standard care in the Canadian health system, where there is universal coverage. Increased ANC coverage was not an objective of this trial. |
| Tough 2007 | This trial compares group with individual prenatal care. Increased coverage of ANC is not an objective of the trial. |
| Turan 2001 | Three studies are described in this report. One is a randomised trial of antenatal education sessions for couples, women‐only or control. Increased ANC coverage was not an objective of the trial. |
ANC: antenatal care RCT: randomised controlled trial
Characteristics of ongoing studies [ordered by study ID]
Bhandari 2014.
| Trial name or title | Overcoming barriers to scaling SBA utilization in improving maternal, neonatal and child health in Nepal. Location: Nepal. Trial Registration: ISRCTN78892490. |
| Methods | Cluster‐randomised trial in 3 districts in Nepal, 36 clusters selected for study. Clusters were not eligible if they had already achieved the target coverage of SBAs. |
| Participants | All pregnant women. |
| Interventions |
Arm 1: the intervention has 5 components to strengthen the capacity of the existing health system. The intervention is implemented through training community health volunteers, training of health personnel, organisation of community leaders and reorganisation of emergency services. The intervention targets: family support for transport to health facility for childbirth, emergency funding for transport, availability of transport, women‐friendly environment in health facilities, mechanisms to improve security at health facilities. The fifth component of measuring the impact of the intervention will be a survey of process indicators. Arm 2: standard care |
| Outcomes |
Target: health system strengthening. Primary outcome: utilisation of SBAs. Secondary outcome: at least 4 ANC visits, postnatal care, availability of transport, functional operation of emergency fund, security of SBA, family support, women‐friendly environment at health facility. |
| Starting date | May 2013‐Aug 2014 intervention; May 2014‐Oct 2014 evaluation. Mid‐term data monitoring in Oct 2013. |
| Contact information | G Bhandari ‐ gpbhandari@gmail.com |
| Notes |
Chavane 2014.
| Trial name or title | Implementation of evidence‐based ANC in Mozambique. Location: antenatal clinics in3 regions of Mozambique. Trial Registration: Pan African Clinical Trial Registry database. Identification number: PACTR201306000550192. |
| Methods | Cluster‐randomised trial. |
| Participants | "Clinics were eligible if (1) they were not already implementing the proposed ANC model; (2) they served at least 200 new pregnant women per year; (3) they had midwives or nurses midwives among their personnel; and (4) they were willing to participate. All women attending ANC visits at the participating clinics will be eligible to receive the ANC package." |
| Interventions | Target: health system. "The aim of this study is to determine the effect of an intervention designed to increase the use of evidence‐based practices included in the ANC package by midwives (and other health professionals) in prenatal clinics in Mozambique. Specifically, we will assess the effect of the intervention on practices related to the detection, treatment and prevention of major health‐related conditions (e.g., anaemia, and infectious diseases such as HIV/AIDS, malaria, and congenital syphilis)." Arm 1: the intervention has 4 components: ANC kits for clinics, storage for ANC kits, tracking system, training for staff. Arm 2: standard care. |
| Outcomes |
Primary outcome: administration of a set of practices during first ANC visit Secondary outcome: composite of several practices. • Frequency of women receiving screening for syphilis. • Frequency of women receiving screening for HIV. • Frequency of women receiving screening for anaemia. • Frequency of women receiving screening for hypertension. • Frequency of women receiving tetanus toxoid. • Frequency of women receiving intermittent preventive malaria treatment. • Frequency of women receiving iron supplementation. • Frequency of women receiving anti‐parasitic treatment (de‐worming). • Frequency of syphilis sero‐positive women receiving the administration of syphilis treatment. • Frequency of HIV sero‐positive women receiving administration of antiretroviral treatment. |
| Starting date | July 2013‐March 2015. |
| Contact information | Leonardo Chavane ‐ leochavane@gmail.com |
| Notes | Funding ‐ World Health Organization, Department of Reproductive Health and Research. |
Kestler 2013.
| Trial name or title | A matched pair cluster‐randomised implementation trial to measure the effectiveness of an intervention package aiming to decrease perinatal mortality and increase institution‐based obstetric care among indigenous women in Guatemala. Location: Guatemala. Trial Registration: ClinicalTrial.gov NCT01653626. |
| Methods | Matched pair cluster‐randomised implementation trial (30 matched pairs randomised evenly). |
| Participants | All women in study areas, aged 10‐49. |
| Interventions |
Target: community and health system. Arm 1: intervention involves 3 components: PRONTO a training program for management of emergency obstetric care, social campaign to increase use of health facilities for birth, strengthening lings between trained birth assistants and professional midwives. Arm 2: standard care. |
| Outcomes |
Primary outcome: perinatal mortality. Secondary outcome: process indicators, deliveries in a health facility. |
| Starting date | July 2012‐Dec 2013. |
| Contact information | Edgar Kestler ‐ ekestler@ciesar.or.gt |
| Notes | Funding: This study is funded by the Alliance/WHO grant file register: H9‐TSA‐224. We are also grateful for the support of the Guatemalan Reproductive Health Observatory and National Reproductive Health Program, the Guatemalan Ministry of Health and its Department of Nursing and the National Society of Gynecologists and Obstetricians of Guatemala. |
Khan 2012.
| Trial name or title | Making birth safe for Pakistan women: a cluster‐randomised trial. Location: Jhang, Chiniot and Khanewal districts of Punjab, Pakistan. Trial Registration: Current Controlled Trials ISRCTN86264432. |
| Methods | Cluster‐randomised trial with 3 arms (7 clusters per arm). A costing study and exploratory qualitative study are also proposed. |
| Participants | All pregnant women in the catchment areas. |
| Interventions |
Arm 1: structured birth planning and travel facilitation. Arm 2: structured birth planning. Arm 3: control (routine care by Lady Health Workers, as available to all pregnant women). |
| Outcomes |
Primary outcome: neonatal mortality and service utilisation. Secondary outcome: maternal mortality. |
| Starting date | February 2011‐May 2013. |
| Contact information | Shirin Mirza, shirin.mirza.ebo806@student.aku.edu |
| Notes | This trial appears to be completed. |
Kikuchi 2015.
| Trial name or title | Ghana’s Ensure Mothers and Babies Regular Access to Care (EMBRACE) program. Location: Dodowa, Kintampo, and Navrongo, Ghana. Trial registration: Current Controlled Trials ISRCTN90618993. |
| Methods | Cluster‐randomised trial using an effectiveness‐implementation hybrid design. |
| Participants | Women of reproductive age between the ages of 15 and 49 years living in the study areas. |
| Interventions |
Arm 1: the package includes: 1) use of a new continuum of care card, 2) continuum of care orientation for health workers, 3) 24‐hour health facility retention of mothers and newborns after delivery, and 4) postnatal care by home visits. Arm 2: standard ANC. |
| Outcomes |
Primary outcome: continuum of care completion rate of mothers and infants Secondary outcome: PNC rate within 48 hours, the complication rate requiring mothers’ and newborns' hospitalisations, and the PMR and NMR. The PMR is defined as fetal deaths during any period of pregnancy and newborn deaths within 7 completed days after birth. The NMR includes early neonatal deaths occurring during the first 7 days of life and late neonatal deaths occurring after 7 days but before 28 completed days of life. |
| Starting date | The expected recruitment period will be from August to September 2014 for the baseline survey, from October 2014 to September 2015 for the intervention, and from October to November 2015 for the follow‐up survey. |
| Contact information | Masamine Jimba ‐ mjimba@m.u‐tokyo.ac.jp |
| Notes | The Ghana EMBRACE Implementation Research Project is conducted by the Government of the Republic of Ghana, Japan International Cooperation Agency (JICA) Human Development Department, and JICA Research Institute. |
Morrison 2011.
| Trial name or title | Community mobilisation and health management committee strengthening to increase birth attendance by trained health workers in rural Makwanpur, Nepal. Trial registration: ISRCTN99834806. |
| Methods | Cluster‐randomised trial to test the effect on institutional deliveries and home deliveries by trained health workers of a combination of community mobilisation through women’s groups and strengthening of health management committees. |
| Participants | Women of reproductive age, family members, health service cadres, health management committee members, and communities. |
| Interventions |
Intervention arm: community mobilisation through women’s groups, and health management committee strengthening. Control arm: no intervention. We stratified clusters into 4 groups. Group 1 included control clusters from 2002‐2005, and intervention clusters from 2005 to 2008. Group 2 included intervention clusters from 2001‐2008. In group 3 we monitored birth outcomes from 2005‐2008. In group 4, we had not previously conducted any intervention or monitoring activities. There were equal numbers of clusters from each group allocated to intervention and control clusters. |
| Outcomes | Primary outcome measures: 1. Deliveries conducted by trained health workers. 2. Institutional deliveries. Secondary outcome measures: 1. ANC uptake. 2. Postnatal care uptake. 3. Neonatal deaths per 1000 live births. 4. Stillbirths per 1000 births. 5. Maternal morbidities. |
| Starting date | Overall trial start date: 01/10/2010. Overall trial end date: 30/09/2012. |
| Contact information | Anthony Costello: a.costello@ich.ucl.ac.uk |
| Notes | The Wellcome Trust funded this study. |
Owen‐Jones 2013.
| Trial name or title | Building Blocks: Family Nurse Partnership in England trial. 18 study sites around England. Location: England, United Kingdom. Trial registration: ISRCTN23019866. |
| Methods | Individually‐randomised parallel controlled trial with a parallel economic modelling study. |
| Participants | Nulliparous pregnant women aged 19 or under, recruited by 24 weeks' gestation and followed until child is aged 2 are eligible. Women who require a translator or sign interpreter, who plan to move from the trial area, or who plan to have their children adopted are excluded from the trial. |
| Interventions |
Arm 1: Family Nurse Partnership and usual care. The Family Nurse Partnership programme is a "structured, intensive programme of home visits delivered by specially trained nurses, provided from early pregnancy until the child is 2 years old. ...Visits cover core content areas of personal and environmental health, life course development, maternal role, family and friends and access to health and social services" (p. 2). Arm 2: usual care. Usual care women receive local maternity services as standard in the UK, including pre and postnatal visits and an assigned Health Visitor after the birth of the baby. |
| Outcomes |
Primary outcomes: birthweight, changes in prenatal tobacco use, emergency attendances and hospital admissions for the child within 2 years, proportion of women with a second pregnancy within 2 years. Secondary outcomes: multiple outcomes for mothers and infants, including use of ANC and other services, maternal health and well being, health behaviours, social support, parenting beliefs, behaviours and experience, and for infants/children: Apgar, neonatal intensive care unit admissions, head circumference, feeding and development outcomes, child health and use of services, emergency attendances and admissions. |
| Starting date | 06/04/2009‐19/09/2014. |
| Contact information | Owen‐JonesCE@cardiff.ac.uk |
| Notes | Michael Robling also an author. The trial appears to be finished. |
Ramsey 2013.
| Trial name or title | The Tanzania Connect Project: a cluster‐randomised trial of the child survival impact of adding paid community health workers to an existing facility‐focused health system. Location: 3 rural districts in Tanzania, with a population of roughly 360,000 ( Kilombero, Rufiji, and Ulanga). Trial Registration: ISRCTN96819844. |
| Methods | Cluster‐randomised trial with the following objectives.
|
| Participants | 1. Women who reside within the catchment population of the Ifakara and Rufiji HDSS. 2. The household survey will include roughly 3000 households. Households can be included only if: 2.1. have women of reproductive age (15‐49 years of age), or be the primary care takers of at least 1 under 5‐year old child for women more than 49 years old; 2.2. the population to be enrolled as participants in the household survey will, in most cases, be non‐English speaking, educationally‐ and economically‐disadvantaged. Kiswahili is the national language of Tanzania and residents of rural villages are typically impoverished and with limited means to adequate schooling. No children under the age of 15 will be enrolled. All women of reproductive age will be enrolled as participants; 3. Health workers – any Community Health Agents (CHAs) and government health employees within the study districts. |
| Interventions |
Intervention: integrated community health services strengthening (addition of community health agents or CHA, and emergency health services); health service and facility strengthening (health workforce training, communications and information systems improvement, facility and medicines/supplies strengthening, financial and social protection including reducing emergency transport costs, improvements in local planning and referral). Controls: no CHAs. |
| Outcomes | Several maternal, newborn and child health outcomes. Sample size based on child, infant and newborn mortality. |
| Starting date | Overall trial start date: 01/07/2010. Overall trial end date: 31/07/2014. |
| Contact information | Primary contact: Dr James Phillips 60 Haven Ave B‐2 New York 10032 United States of America |
| Notes | Funder: Doris Duke Charitable Foundation DDCF 2009058 (USA). |
Richter 2013.
| Trial name or title | PROCOMIDA ‐ Strengthening and Evaluating the Preventing Malnutrition in Children under 2 Approach in Guatemala: Report of the Enrollment Survey. Location: Guatemala. Trial Registration: ClinicalTrials.gov Identifier:NCT01072279. |
| Methods | Cluster‐randomised trial ‐ enrolment survey component of the impact evaluation. |
| Participants | "Women can enrol in PROCOMIDA at any stage during pregnancy or lactation if the lactating woman has a child under 6 months of age or can enrol her child between the ages of 6 and 18 months. Children graduate from the program when they are 23 months of age." Participants in the enrolment survey, undertaken to establish a baseline for the trial, were between 3 and 7 months pregnant. |
| Interventions | Target: health systems. The trial "aims to lower the prevalence of child malnutrition by targeting all pregnant women, mothers of children 0–23 months, and children under 2 in food‐insecure areas with a package of health and nutrition interventions. PROCOMIDA is implemented by Mercy Corps in Alta Verapaz, Guatemala." There are 6 study arms: Group A: full family ration (rice, pinto beans, and oil), individual ration (corn‐soy blend [CSB]), BCC, and required health visits. Group B: reduced family ration (rice, pinto beans, and oil), individual ration (CSB), BCC, and required health visits. Group C: no family ration, individual ration (CSB), BCC, and required health visits. Group D: full family ration (rice, pinto beans, and oil), lipid‐based nutrient supplement (LNS) as the individual ration, BCC, and required health visits. Group E: full family ration (rice, pinto beans, and oil), micronutrient powder (MNP) supplement as the individual ration, BCC, and required health visits. Group F: control group: does not receive PROCOMIDA (i.e. does not receive family or individual rations or BCC messages) and is not required to attend health visits; however, families in the control group do have access to standard MOH health services. |
| Outcomes |
Primary outcome: child nutritional status. Secondary outcome: multiple outcomes to do with women's and children's health, process indicators. |
| Starting date | April 2010‐Dec 2015. |
| Contact information | Marie Ruel, IFPRI. |
| Notes | Funding ‐ International Food Policy Research Institute, Food and Nutrition Technical Assistance Project 2 of the Academy of Educational Development, United States Agency for International Development (USAID), Catholic Relieve Services‐Burundi, Mercy Corps‐Guatemala, Guatemal Ministry of Health. This 2013 report provides the results of the first round of a longitudinal study, undertaken to establish baseline values and confirm randomisation. |
Sando 2014.
| Trial name or title |
Familia Salama: a cluster‐randomised health systems implementation study. Location: Dar es Salaam, Tanzania. Trial registration: ClinicalTrials.gov: EJF22802. |
| Methods | A 2 by 2 factorial cluster‐randomised trial to test the effectiveness, cost‐effectiveness, feasibility, and acceptability of a community health worker intervention in improving ANC and PMTCT outcomes. |
| Participants | All pregnant women in the study areas. |
| Interventions | 2 by 2 factorial design. The 2 urban districts of Kinondoni and Ilala districts in which the trial takes place have 60 wards. These wards were randomly allocated to either the community health worker intervention (36 wards) or the normal standard of care in Dar es Salaam (24 wards). The 2 arms were then randomised again to receiving either WHO Option A or Option B for prevention of mother‐to‐child transmission of HIV (PMTCT). The number of clusters in the arms varies to reflect the difference in the population sizes in each ward. The community health workers: (1) identify pregnant women through home visits and refer them to ANC; (2) provide education to pregnant women on ANC, PMTCT, birth, and postnatal care; (3) routinely follow up on all pregnant women to ascertain whether they have attended ANC; and (4) follow up on women who have missed ANC or PMTCT appointments. Under the standard of care, facility‐based health workers follow up on patients who have missed scheduled appointments for PMTCT, first through a telephone call and then with a home visit. |
| Outcomes |
Primary outcomes: (1) the percentage of pregnant women making at least 4 antenatal clinic visits (as recommended by WHO); (2) the percentage of pregnant women delivering at a healthcare facility;
(3) the percentage of HIV‐infected women receiving PMTCT; (4) the percentage of HIV‐exposed infants who received a confirmatory HIV test by 6 weeks after the cessation of breastfeeding; and (5) the percentage of infants born to HIV‐infected mothers who have acquired HIV by 6 weeks after the complete cessation of breastfeeding. Secondary outcomes: (1) the percentage of pregnant women who were tested for HIV during pregnancy or labour and delivery; (2) the number of weeks of gestation at which pregnant women attend ANC for the first time; (3) the percentage of HIVinfected pregnant women who completed PMTCT; and (4) the percentage of HIV‐exposed infants who received PMTCT. |
| Starting date | The trial is being carried out over a period of 17 months from January 2013 to May 2014. |
| Contact information | Till W Bärnighausen: tbaernig@hsph.harvard.edu |
| Notes | The study is carried out by Management and Development for Health (MDH, Tanzania). The Harvard School of Public Health provides technical assistance for the trial of the CHW intervention. MDH is a Tanzanian organisation based in Dar es Salaam, which works in partnership with Tanzania’s Ministry of Health and Social Welfare. It provides technical and financial support to 50 HIV treatment sites, 17 tuberculosis clinics, and 180 PMTCT outlets across Dar es Salaam. |
Shepard 2014.
| Trial name or title | Impact Evaluation of the Pilot SMS Mother Reminder System. Location: Uganda. Trial Registration: ClinicalTrials.gov Identifier: NCT02121821. |
| Methods | Randomised trial. |
| Participants | All pregnant women attending ANC. Estimated enrolment: 11,454. |
| Interventions |
Target: health systems. Arm 1: village health teams and SMS reminder system. Arm 2: Standard care. |
| Outcomes |
Primary outcome: ANC visits: pregnant women attend 4 ANC visits. Secondary outcome: sulfadoxine‐pyrimethamine (SP) doses: pregnant women receive at least 2 doses of intermittent preventive treatment of malaria in pregnancy using SP. Other maternal health outcomes and process outcomes. |
| Starting date | May 2014‐May 2015 (preliminary data). |
| Contact information | Lungi Okoko: lokoko@as4h.org. PI ‐ Donald Shepard, Brandeis University (Massachussetts, USA). |
| Notes | Funding: African Strategies for Health, United States Agency for International Development (USAID). |
Shrestha 2011.
| Trial name or title |
MIRA Dhanusha: Community interventions to reduce child mortality in Dhanusha, Nepal. Trial Registration: ISRCTN87820538. |
| Methods | Cluster‐randomised trial. |
| Participants | Pregnant women and infants up to 1 year of age. |
| Interventions |
Arm 1: women's groups, female community health volunteers trained to care for vulnerable infants. Arm 2: standard care. |
| Outcomes |
Primary outcome: neonatal mortality. Secondary outcome: MIRA Dhanusha community group: stillbirth, infant and under‐2 mortality rates, care practices and healthcare‐seeking behaviour, maternal diet, breastfeeding and complementary feeding practices, maternal and under‐2 anthropometric status. MIRA Dhanusha sepsis management: identification and treatment of neonatal sepsis by community health volunteers, infection‐specific neonatal mortality. |
| Starting date | Jan 2008‐Jan 2010. |
| Contact information | Naomi Saville: n.saville@ich.ucl.ac.uk |
| Notes | Funding: UBS Optimus Foundation (Switzerland). This trial has finished, but we have not located published data. |
Vos 2015.
| Trial name or title | Effectiveness of score card‐based antenatal risk selection, care pathways, and multidisciplinary consultation in the Healthy Pregnancy 4 All study (HP4ALL). Location: The Netherlands. Trial Registration: Dutch Trial Registry (NTR‐3367). |
| Methods | Cluster‐randomised trial. |
| Participants | All midwives and gynaecologists providing care to women living in these zip codes will be invited to participate in the Healthy Pregnancy 4 All study. All pregnant women living in these selected areas are eligible for this trial. All municipalities deal with an above‐average perinatal mortality rate and many disadvantaged neighbourhoods. Exclusion criteria include an acute obstetric situation during the booking visit (for example, ectopic pregnancy) and women in labour during this initial visit. |
| Interventions |
Intervention: use of the R4U scorecard, corresponding care pathways, and multidisciplinary consultation. Control: standard ANC. The follow‐up period consists of 6 weeks. Details of pregnancy, delivery, and maternal follow‐up will be recorded after 6 weeks in a case record form. If necessary, medical records of newborns will be requested (if consent is provided). |
| Outcomes | Primary outcome: small for gestational age (< 10th percentile) and preterm birth (gestational age below 37 weeks). Secondary outcome: |
| Starting date | Randomisation took place January 2011; Recruitment began August 2012. |
| Contact information | Amber A Vos (a.a.vos@erasmusmc.nl) |
| Notes | This study is funded by the Dutch government, Ministry of Welfare and Sports (VWS), grant 318804. |
ANC: antenatal care CHA: Community Health Agents NMR: neonatal mortality rate PMTCT: prevention of mother‐to‐child transmission PNC: perinatal mortality rate SBA: skilled birth attendants
Differences between protocol and review
The are some differences between our published protocol (Mbuagbaw 2014) and the full review.
We have deleted the subgroup of single versus combined interventions because this analysis has been captured at the comparison level.
Three new co‐authors have joined the review team: N Medley, A J Darzi, M Richardson and T Lawrie.
We have used the GRADE approach as outlined in the GRADE Handbook to assess the quality of the body of evidence and we have included 'Summary of findings' tables.
Methods/Assessment of Risk of bias: ‐ due to the inclusion of cluster‐randomised trials in the review, we have added several recommended 'Risk of bias' domains, including recruitment bias and analysis bias
Methods/Measures of treatment effect/Dichotomous data ‐ we have presented these results as summary odds ratios not summary risk ratios as stated in our protocol.
Methods/Assessment of heterogeneity ‐ we have added the following text: "We have left the overall totals turned off only if the effect estimates of different trials were so disparate that it made little clinical sense to combine the trials (for example, if effect estimates fell on opposite sides of the line of no difference and the trials' confidence intervals do not overlap). Overall, even with high heterogeneity in several outcomes, the effect estimates were reasonably similar, and confidence intervals always overlapped. We have not turned off the totals for any outcome below".
Methods/Unit of analysis issues ‐ we have expanded this section. We have provided more details about how we handled cluster‐randomised trials. We have expanded the methods for 'other unit of analysis issues' relating to studies with multiple treatment arms. We have also discussed issues relating to studies involving multiple pregnancies.
Methods/subgroup analysis and investigation of heterogeneity ‐ we have removed 'single versus combined interventions' from our list of planned subgroup analyses since this is a comparison rather than a subgroup analysis.
We did not measure agreement during the screening and data extraction processes.
Methods/types of studies ‐ in our protocol we did not specify whether studies published in abstract form were eligible for inclusion. In the full review we have clarified that "Trials reported in abstract form were eligible for inclusion in the review; however, we did not include any trial based on an abstract report alone."
Contributions of authors
LM is the guarantor for this review. He contributed to the background and methods section of the protocol. LM, HG and POZ jointly conceived the idea for the review as a response to policy debates in Cameroon. All authors worked on the protocol and approved the final manuscript.
LM and NM assessed trials for inclusion. LM, AD and NM extracted data. AD contributed to the text describing included studies. MR is the review statistician; she adjusted data from cluster trials and prepared all of the meta‐analyses. LM and NM completed the text of the review.
Sources of support
Internal sources
Centre for Development of Best Practices in Health, Cameroon.
South African Cochrane Centre, Medical Research Council, South Africa.
External sources
Effective Health Care Research Consortium, UK.
UNDP/UNFPA/UNICEF/WHO/World Bank Special Programme of Research, Development and Research Training in Human Reproduction (HRP), Department of Reproductive Health and Research (RHR), World Health Organization, Switzerland.
Declarations of interest
Lawrence Mbuagbaw ‐ none known.
Nancy Medley ‐ none known.
Andrea J Darzi ‐ none known.
Marty Richardson ‐ none known.
Theresa A Lawrie ‐ none known.
Kesso Habiba Garga ‐ none known.
Pierre Ongolo‐Zogo ‐ the Centre for the Development of Best Practices receives funding from UKaid through the Effective Health Care Research Consortium, UK to promote and support evidence based health care.
Edited (no change to conclusions)
References
References to studies included in this review
Azad 2010 {published data only}
- Azad K, Barnett S, Banerjee B, Shaha S, Khan K, Rego AR, et al. Effect of scaling up women's groups on birth outcomes in three rural districts in Bangladesh: a cluster‐randomised controlled trial. Lancet 2010;375(9721):1193‐202. [DOI] [PubMed] [Google Scholar]
Baqui 2008 {published data only}
- Baqui AH, El‐Arifeen S, Darmstadt GL, Ahmed S, Williams EK, Seraji HR, et al. Effect of community‐based newborn‐care intervention package implemented through two service‐delivery strategies in Sylhet district, Bangladesh: a cluster‐randomised controlled trial. Lancet 2008;371(9628):1936‐44. [DOI] [PubMed] [Google Scholar]
Barber 2008 {published data only}
- Barber SL. Mexico's conditional cash transfer programme increases cesarean section rates among the rural poor. European Journal of Public Health 2010;20(4):383‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barber SL, Gertler PJ. Empowering women to obtain high quality care: evidence from an evaluation of Mexico's conditional cash transfer programme. Health Policy and Planning 2009;24(1):18‐25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barber SL, Gertler PJ. The impact of Mexico's conditional cash transfer programme, Oportunidades, on birthweight. Tropical Medicine and International Health 2008;13(11):1405‐14. [DOI] [PMC free article] [PubMed] [Google Scholar]
Basinga 2011 {published data only}
- Basinga P, Gertler PJ, Binagwaho A, Soucat AL, Sturdy J, Vermeersch CM. Effect on maternal and child health services in Rwanda of payment to primary health‐care providers for performance: an impact evaluation. Lancet 2011;377(9775):1421‐8. [DOI] [PubMed] [Google Scholar]
- Priedeman Skiles M. An equity analysis of performance‐based financing in Rwanda [thesis]. Chapel Hill: University of North Carolina, 2012. [Google Scholar]
- Priedeman Skiles M, Curtis SL, Basinga P, Angeles G. An equity analysis of performance‐based financing in Rwanda: are services reaching the poorest women?. Health Policy and Planning 2013;28(8):825‐37. [DOI] [PubMed] [Google Scholar]
Bhutta 2011 {published data only}
- Bhutta Z, Soofi SB, Memon ZA, Mohammad S, Khan A, Cousens, et al. Impact of community mobilization and education and training of primary health care workers in newborn care in reducing neonatal mortality in rural district of Pakistan: an effectiveness cluster‐randomized controlled trial. Pediatric Academic Societies Annual Meeting; 2009 May 2‐5; Baltimore, Maryland, USA. 2009.
- Bhutta ZA, Memon Z, Soofi S, Muhammad S, Raza F, for the Hala project team. Hala project: a cluster‐randomized effectiveness trial in rural Pakistan. Personal communication 2010.
- Bhutta ZA, Soofi S, Cousens S, Mohammad S, Memon ZA, Ali I, et al. Improvement of perinatal and newborn care in rural Pakistan through community‐based strategies: a cluster‐randomised effectiveness trial. Lancet 2011;377(9763):403‐12. [DOI] [PubMed] [Google Scholar]
- Soofi SB. Impact of an intervention package on perinatal and neonatal mortality delivered through lady health workers (LHWs) and traditional birth attendants (Dais) in rural Pakistan. Pediatric Academic Societies Annual Meeting; 2010 May 1‐4; Vancouver, Canada. 2010.
Darmstadt 2010 {published data only}
- Darmstadt GL, Choi Y, Arifeen SE, Bari S, Rahman SM, Mannan I, et al. Evaluation of a cluster‐randomized controlled trial of a package of community‐based maternal and newborn interventions in Mirzapur, Bangladesh. PloS One 2010;5(3):e9696. [DOI] [PMC free article] [PubMed] [Google Scholar]
Fottrell 2013 {published data only}
- Clarke K, Azad K, Kuddus A, Shaha S, Nahar T, Aumon BH, et al. Impact of a participatory intervention with women's groups on psychological distress among mothers in rural Bangladesh: secondary analysis of a cluster‐randomised controlled trial. Plos One 2014;9(10):e110697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fottrell E, Azad K, Kuddus A, Younes L, Shaha S, Nahar T, et al. The effect of increased coverage of participatory women's groups on neonatal mortality in Bangladesh: A cluster randomized trial. JAMA Pediatrics 2013;167(9):816‐25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Houweling TAJ, Azad K, Younes L, Kuddus A, Shaha S, Haq B, et al. The effect of participatory women's groups on birth outcomes in Bangladesh: does coverage matter? Study protocol for a randomized controlled trial. Trials 2011;12:208. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kenyon 2012 {published data only}
- Kenyon S, Jolly K, Hemming K, Ingram L, Blissett J, Dann S, et al. Effects of additional lay support for pregnant women with social risk factors on antenatal attendance and maternal psychological health: a randomised controlled trial (ELSIPS). Archives of Disease in Childhood. Fetal and Neonatal Edition 2014;99(Suppl 1):A18. [Google Scholar]
- Kenyon S, Jolly K, Hemming K, Ingram L, Gale N, Dann SA, et al. Evaluation of Lay Support in Pregnant women with Social risk (ELSIPS): a randomised controlled trial. BMC Pregnancy and Childbirth 2012;12:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kirkwood 2013 {published data only}
- Kirkwood BR, Manu A, Tawiah‐Agyemang C, Asbroek G, Gyan T, Weobong B, et al. NEWHINTS cluster randomised trial to evaluate the impact on neonatal mortality in rural Ghana of routine home visits to provide a package of essential newborn care interventions in the third trimester of pregnancy and the first week of life: trial protocol. Trials 2010;11:58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirkwood BR, Manu A, Asbroek AH, Soremekun S, Weobong B, Gyan T, et al. Effect of the Newhints home‐visits intervention on neonatal mortality rate and care practices in Ghana: a cluster randomised controlled trial. Lancet 2013;381(9884):2184‐92. [DOI] [PubMed] [Google Scholar]
Klerman 2001 {published data only}
- Klerman LV, Ramey SL, Goldenberg RL, Marbury S, Hou J, Cliver SP. A randomized trial of augmented prenatal care for multiple‐risk, Medicaid‐eligible African American women. American Journal of Public Health 2001;91(1):105‐11. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kumar 2008 {published data only}
- Keating EM, Kumar A, Kumar V, Darmstadt G, Naz A, Belur G, et al. Designing for change: How an effectively designed community‐based behavior change intervention substantially improved newborn survival in Shivgarh, India. American Journal of Tropical Medicine and Hygiene 2011;85(6 Suppl 1):171. [Google Scholar]
- Kumar V, Kumar A, Das V, Srivastava NM, Baqui AH, Santosham M, et al. Community‐driven impact of a newborn‐focused behavioral intervention on maternal health in Shivgarh, India. International Journal of Gynecology and Obstetrics 2012;117(1):48‐55. [DOI] [PubMed] [Google Scholar]
- Kumar V, Mohanty S, Kumar A, Misra RP, Santosham M, Awasthi S, et al. Effect of community‐based behavior change management on neonatal mortality in Shivgarh, Uttar Pradesh, India: a cluster‐randomised controlled trial. Lancet 2008;372(9644):1151‐62. [DOI] [PubMed] [Google Scholar]
Laken 1995 {published data only}
- Laken MP, Ager J. Using incentives to increase participation in prenatal care. Obstetrics & Gynecology 1995;85:326‐9. [DOI] [PubMed] [Google Scholar]
le Roux 2013 {published data only}
- Rotheram‐Borus MJ, Tomlinson M, Roux IM, Harwood JM, Comulada S, O'Connor MJ, et al. A cluster randomised controlled effectiveness trial evaluating perinatal home visiting among South African mothers/infants. Plos One 2014;9(10):e105934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rotheram‐Borus MJ, Roux IM, Tomlinson M, Mbewu N, Comulada WS, Roux K, et al. Philani Plus (+): a Mentor Mother community health worker home visiting program to improve maternal and infants' outcomes. Prevention Science 2011;12(4):372‐88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roux IM, Rotheram‐Borus MJ, Stein J, Tomlinson M. The impact of paraprofessional home visitors on infants' growth and health at 18 months. Vulnerable Children and Youth Studies 2014;9(4):291‐304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roux IM, Tomlinson M, Harwood JM, O'Connor MJ, Worthman CM, Mbewu N. Outcomes of home visits for pregnant township mothers and their infants in South Africa: a cluster randomised controlled trial. AIDS (London, England) 2013;27:1461‐71. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lewycka 2013a {published data only}
- Lewycka S, Mwansambo C, Kazembe P, Phiri T, Mganga A, Rosato M, et al. A cluster randomised controlled trial of the community effectiveness of two interventions in rural Malawi to improve health care and to reduce maternal, newborn and infant mortality. Trials 2010;11:88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewycka S, Mwansambo C, Rosato M, Kazembe P, Phiri T, Mganga A, et al. Effect of women's groups and volunteer peer counselling on rates of mortality, morbidity, and health behaviours in mothers and children in rural Malawi (MaiMwana): a factorial, cluster‐randomised controlled trial. Lancet 2013;381(9879):1721‐35. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lewycka 2013b {published data only}
- Lewycka S, Mwansambo C, Kazembe P, Phiri T, Mganga A, Rosato M, et al. A cluster randomised controlled trial of the community effectiveness of two interventions in rural Malawi to improve health care and to reduce maternal, newborn and infant mortality. Trials 2010;11:88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewycka S, Mwansambo C, Rosato M, Kazembe P, Phiri T, Mganga A, et al. Effect of women's groups and volunteer peer counselling on rates of mortality, morbidity, and health behaviours in mothers and children in rural Malawi (MaiMwana): a factorial, cluster‐randomised controlled trial. Lancet 2013;381(9879):1721‐35. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lund 2012 {published data only}
- Lund S, Hemed M, Nielsen BB, Said A, Said K, Makungu MH, et al. Mobile phones as a health communication tool to improve skilled attendance at delivery in Zanzibar: a cluster‐randomised controlled trial. BJOG: an international journal of obstetrics and gynaecology 2012;119:1256‐64. [DOI] [PubMed] [Google Scholar]
- Lund S, Nielsen BB, Hemed M, Boas IM, Said A, Said K, et al. Mobile phones improve antenatal care attendance in Zanzibar: a cluster randomized controlled trial. BMC Pregnancy and Childbirth 2014;14(1):29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lund S, Nielsen BB, Hemed M, Said A, Said K, Makungu MH, et al. Mobile phones as a health communication tool to improve maternal and perinatal health in Zanzibar: A cluster randomised controlled trial. Tropical Medicine & International Health 2013;18(Suppl 1):22. [DOI] [PubMed] [Google Scholar]
- Lund S, Rasch V, Hemed M, Boas IM, Said A, Said K, et al. Mobile phone intervention reduces perinatal mortality in Zanzibar: secondary outcomes of a cluster randomized controlled trial. JMIR mHealth and uHealth 2014;2(1):e15. [DOI] [PMC free article] [PubMed] [Google Scholar]
Majoko 2007 {published data only}
- Majoko F, Munjanja SP, Lindmark G, Nystrom L, Mason E. A comparison of two antenatal packages in a rural area in Zimbabwe. Women's Health ‐ into the new millennium. Proceedings of the 4th International Scientific Meeting of the Royal College of Obstetricians and Gynaecologists; 1999 October 3‐6; Cape Town South Africa. RCOG, 1999:2.
- Majoko F, Munjanja SP, Lindmark G, Nystrom L, Mason E. A study of two antenatal care models in a rural setting in Zimbabwe. Acta Obstetricia et Gynecologica Scandinavica 1997;76(167):87. [Google Scholar]
- Majoko F, Munjanja SP, Nystrom L, Mason E, Lindmark G. Randomised controlled trial of two antenatal care models in rural Zimbabwe. BJOG: an international journal of obstetrics and gynaecology 2007;114(7):802‐11. [DOI] [PubMed] [Google Scholar]
Manandhar 2004 {published data only}
- Borghi J, Thapa B, Osrin D, Jan S, Morrison J, Tamang S, et al. Economic assessment of a women's group intervention to improve birth outcomes in rural Nepal. Lancet 2005;366(9500):1882‐4. [DOI] [PubMed] [Google Scholar]
- MIRA (Mother Infant Research Unit). The MIRA Makwanpur Study. Personal communication 2002.
- Manandhar DS, Osrin D, Shrestha BP, Mesko N, Morrison J, Tumbahangphe KM, et al. Effect of a participatory intervention with women's groups on birth outcomes in Nepal: cluster‐randomised controlled trial. Lancet 2004;364:970‐9. [DOI] [PubMed] [Google Scholar]
- Osrin D, Mesko N, Shrestha BP, Shrestha D, Tamang S, Thapa S, et al. Implementing a community‐based participatory intervention to improve essential newborn care in rural Nepal. Transactions of the Royal Society of Tropical Medicine & Hygiene 2003;97:18‐21. [DOI] [PubMed] [Google Scholar]
- Wade A, Osrin D, Shrestha BP, Sen A, Morrison J, Tumbahangphe KM, et al. Behaviour change in perinatal care practices among rural women exposed to a women's group intervention in Nepal [ISRCTN31137309]. BMC Pregnancy and Childbirth 2006;6:20. [DOI] [PMC free article] [PubMed] [Google Scholar]
Melnikow 1997 {published data only}
- Melnikow J, Paliescheskey M, Stewart GK. Effect of a transportation incentive on compliance with the first prenatal appointment: a randomized trial. Obstetrics & Gynecology 1997;89:1023‐7. [DOI] [PubMed] [Google Scholar]
Midhet 2010 {published data only}
- Midhet F, Becker S. Impact of community‐based intervention on maternal and neonatal health indicators: results from a community randomized trial in rural Balochistan, Pakistan. Reproductive Health 2010;7:30. [DOI] [PMC free article] [PubMed] [Google Scholar]
More 2012 {published data only}
- More NS, Bapat U, Das S, Alcock G, Patil S, Porel M, et al. Community mobilization in Mumbai slums to improve perinatal care and outcomes: a cluster randomized controlled trial. PLoS Medicine 2012;9(7):e1001257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- More NS, Bapat U, Das S, Patil S, Porel M, Vaidya L, et al. Cluster‐randomised controlled trial of community mobilisation in Mumbai slums to improve care during pregnancy, delivery, postpartum and for the newborn. Trials 2008;9:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mori 2015 {published data only}
- Mori R, Yonemoto N, Noma H, Ochirbat T, Barber E, Soyolgerel G, et al. The Maternal and Child Health (MCH) handbook in Mongolia: A cluster‐randomized, controlled trial. Plos One 2015;10(4):e0119772. [DOI] [PMC free article] [PubMed] [Google Scholar]
Morris 2004a {published data only}
- Morris SS, Flores R, Olinto P, Medina JM. Monetary incentives in primary health care and effects on use and coverage of preventive health care interventions in rural Honduras: cluster randomised trial. Lancet 2004;364(9450):2030‐7. [DOI] [PubMed] [Google Scholar]
Morris 2004b {published data only}
- Morris SS, Flores R, Olinto P, Medina JM. Monetary incentives in primary health care and effects on use and coverage of preventive health care interventions in rural Honduras: cluster randomised trial. Lancet 2004;364(9450):2030‐7. [DOI] [PubMed] [Google Scholar]
Mullany 2007 {published data only}
- Mullany BC, Becker S, Hindin MJ. The impact of including husbands in antenatal health education services on maternal health practices in urban Nepal: results from a randomized controlled trial. Health Education Research 2007;22(2):166‐76. [DOI] [PubMed] [Google Scholar]
- Mullany BC, Lakhey B, Shrestha D, Hindin MJ, Becker S, Mullany BC, et al. Impact of husbands' participation in antenatal health education services on maternal health knowledge: Impact of husbands' participation in antenatal health education services on maternal health knowledge. Journal of the Nepal Medical Association 2009;48(173):28‐34. [PubMed] [Google Scholar]
Omer 2008 {published data only}
- Omer K, Mhatre S, Ansari N, Laucirica J, Andersson N. Evidence‐based training of frontline health workers for door‐to‐door health promotion: a pilot randomized controlled cluster trial with lady health workers in Sindh Province, Pakistan. Patient Education and Counseling 2008;72(2):178‐85. [DOI] [PubMed] [Google Scholar]
Penfold 2014 {published data only}
- Penfold S, Manzi F, Mkumbo E, Temu S, Jaribu J, Shamba DD, et al. Effect of home‐based counselling on newborn care practices in southern Tanzania one year after implementation: a cluster‐randomised controlled trial. BMC Pediatrics 2014;14(1):187. [DOI] [PMC free article] [PubMed] [Google Scholar]
Persson 2013 {published data only}
- Persson LA, Nga NT, Malqvist M, Thi Phuong Hoa D, Eriksson L, Wallin L, et al. Effect of facilitation of local maternal‐and‐newborn stakeholder groups on neonatal mortality: cluster‐randomized controlled trial. PLoS Medicine 2013;10(5):e1001445. [DOI] [PMC free article] [PubMed] [Google Scholar]
Richter 2014 {published data only}
- Richter L, Rotheram‐Borus M, Heerden A, Stein A, Tomlinson M, Harwood J, et al. Pregnant women living with HIV (WLH) supported at clinics by peer WLH: a cluster randomized controlled trial. AIDS Behaviour 2014;18:706‐15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rotheram‐Borus M, Roux IM, Tomlinson M, Mbewu N, Comulada WS, Roux K, et al. Philani Plus (+): a mentor mother community health worker home visiting program to improve maternal and infants’ outcomes. Prevention Science 2011;12:372‐88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rotheram‐Borus MJ, Richter L, Rooyen H, Heerden A, Tomlinson M, Stein A, et al. Project Masihambisane: a cluster randomised controlled trial with peer mentors to improve outcomes for pregnant mothers living with HIV. Trials 2011;12:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Tripathy 2010 {published data only}
- Rath S, Nair N, Tripathy PK, Barnett S, Mahapatra R, Gope R, et al. Explaining the impact of a women's group led community mobilisation intervention on maternal and newborn health outcomes: The Ekjut trial process evaluation. BMC International Health and Human Rights 2010;10(1):25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roy SS, Mahapatra R, Rath S, Bajpai A, Singh V, Rath S, et al. Improved neonatal survival after participatory learning and action with women's groups: a prospective study in rural eastern India. Bulletin of the World Health Organization 2013;91(6):426‐33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tripathy P, Nair N, Barnett S, Mahapatra R, Borghi J, Rath S, et al. Effect of a participatory intervention with women's groups on birth outcomes and maternal depression in Jharkhand and Orissa, India: a cluster‐randomised controlled trial. Lancet 2010;375(9721):1182‐92. [DOI] [PubMed] [Google Scholar]
- Tripathy P, Nair N, Mahapatra R, Gope RK, Rath S, Bajpai A, et al. Community mobilisation with women's groups facilitated by Accredited Social Health Activists (ASHAs) to improve maternal and newborn health in underserved areas of Jharkhand and Orissa: study protocol for a cluster‐randomised controlled trial. Trials 2011;12:182. [DOI] [PMC free article] [PubMed] [Google Scholar]
Villar 1992 {published data only}
- Belizan JM, Barros F, Langer A, Farnot U, Victora C, Villar J, et al. Impact of health education during pregnancy on behavior and utilization of health resources. American Journal of Obstetrics and Gynecology 1995;173:894‐9. [DOI] [PubMed] [Google Scholar]
- Langer A, Farnot U, Garcia C, Barros F, Victora C, Belizan JM, et al. The Latin American trial of psychosocial support during pregnancy: effects on mother's wellbeing and satisfaction Latin American Network For Perinatal and Reproductive Research (LANPER). Social Sciences and Medicine 1996;42(11):1589‐97. [DOI] [PubMed] [Google Scholar]
- Langer A, Garcia C, Leis T, Reynoso S, Hernandez B. Pyschosocial support as a strategy to promote the health of the newborn. Revista de Investigacion Clinica 1993;45:317‐28. [PubMed] [Google Scholar]
- Langer A, Victora C, Victora M, Barros F, Farnot U, Belizan J, et al. The Latin American trial of psychosocial support during pregnancy: a social intervention evaluated through an experimental design. Social Sciences and Medicine 1993;36:495‐507. [DOI] [PubMed] [Google Scholar]
- Victora CG, Langer A, Barros F, Belizan J, Farnot U, Villar J, et al. The Latin American multicenter trial on psychosocial support during pregnancy: methodology and baseline comparability. Controlled Clinical Trials 1994;15:379‐94. [DOI] [PubMed] [Google Scholar]
- Villar J, Farnot U, Barros F, Victoria C, Langer A, Belizan J. A randomized trial of psychosocial support during high‐risk pregnancies. New England Journal of Medicine 1992;327:1266‐71. [DOI] [PubMed] [Google Scholar]
Villar 2001 (WHO 2001) {published data only}
- Villar J, Ba'aqeel H, Piaggio G, Lumbiganon P, Belizan JM, Farnot U, et al. Who antenatal care randomised trial for the evaluation of a new model of routine antenatal care. The WHO Antenatal Care Trial Research group. Lancet 2001;357(9268):1551‐64. [DOI] [PubMed] [Google Scholar]
- Villar J, Bakketeig L, Donner A, Al‐Mazrou Y, Ba'aqeel H, Belizan M, et al. The WHO Antenatal Care Randomised Controlled Trial: rationale and study design. Paediatric and Perinatal Epidemiology 1998;12(Suppl 2):27‐58. [DOI] [PubMed] [Google Scholar]
- Villar J, Merialdi M, Ba'aqeel H, Piaggio G, Lumbiganon P, Belizan JM, et al. Developments in antenatal care [abstract]. XVIIIth European Congress of Obstetrics and Gynaecology; 2004 May 12‐15; Athens, Greece. 2004:82.
- Vogel JP, Ndema HA, Souza JP, Gulmezoglu MA, Dowswell T, Carroli G, et al. Antenatal care packages with reduced visits and perinatal mortality: a secondary analysis of the WHO Antenatal Care Trial. Reproductive Health 2013;10(1):19. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wahlstrom 2011 {published data only}
- Wahlstrom R. Improving antenatal care utilization through a low cost community intervention which includes community participation combined with the provision of basic ANC equipment to health centers and a refresher course for healthcare providers: a pragmatic randomized trial in two provinces in rural Laos People's Democratic Republic. Current Controlled Trials (www.controlled‐trials.com/) [accessed 11 November 2013] 2011.
Waiswa 2015 {published data only}
- Pariyo G. Improving newborn health and survival through a community based intervention linked to health facilities: a randomised controlled cluster trial. Current Controlled Trials (www.controlled‐trials.com/) (accessed 12 May 2010) 2010.
- Waiswa P, Namazzi G, Kerber K, Peterson S. Designing for action: adapting and implementing a community‐based newborn care package to affect national change in Uganda. Global Health Action 2015;8:24250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waiswa P, Pariyo G, Kallander K, Akuze J, Namazzi G, Ekirapa‐Kiracho E, et al. Effect of the Uganda Newborn Study on care‐seeking and care practices: a cluster‐randomised controlled trial. Global Health Action 2015; Vol. 8:24584. [DOI] [PMC free article] [PubMed]
- Waiswa P, Peterson SS, Namazzi G, Ekirapa EK, Naikoba S, Byaruhanga R, et al. The Uganda Newborn Study (UNEST): an effectiveness study on improving newborn health and survival in rural Uganda through a community‐based intervention linked to health facilities ‐ study protocol for a cluster randomized controlled trial. Trials 2012;13(1):213. [DOI] [PMC free article] [PubMed] [Google Scholar]
Walker 2013 {published data only}
- Walker D, Demaria L, Gonzalez‐Hernandez D, Padron‐Salas A, Romero‐Alvarez M, Suarez L. Are all skilled birth attendants created equal? A cluster randomised controlled study of non‐physician based obstetric care in primary health care clinics in Mexico. Midwifery 2013;29(10):1199‐205. [DOI] [PubMed] [Google Scholar]
- Walker DM, DeMaria L, Suarez L, Gonzales D, Romero M, Padron A. Are all skilled birth attendants created equal? evidence from Mexico. International Journal of Gynecology and Obstetrics 2012;119(Suppl 3):S516‐S517. [Google Scholar]
Wu 2011 {published data only}
- Wu Z, Viisainen K, Wang Y, Hemminki E. Evaluation of a community‐based randomized controlled prenatal care trial in rural China. BMC Health Services Research 2011;11:92. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to studies excluded from this review
Alisjahbana 1995 {published data only}
- Alisjahbana A, Williams C, Dharmayanti R, Hermawan D, Kwast BE, Koblinsky M. An integrated village maternity service to improve referral patterns in a rural area in West‐Java. International Journal of Gynecology & Obstetrics 1995;48 Suppl:S83‐S94. [DOI] [PubMed] [Google Scholar]
Baqui 2009 {published data only}
- Baqui AH, Arifeen SE, Rosen HE, Mannan I, Rahman SM, Al‐Mahmud AB, et al. Community‐based validation of assessment of newborn illnesses by trained community health workers in Sylhet district of Bangladesh. Tropical Medicine and International Health 2009;14(12):1448‐56. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bhutta 2008 {published data only}
- Bhutta ZA, Memon ZA, Soofi S, Salat MS, Cousens S, Martines J. Implementing community‐based perinatal care: results from a pilot study in rural Pakistan. Bulletin of the World Health Organization 2008;86(6):452‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Colbourn 2013 {published data only}
- Colbourn T, Nambiar B, Bondo A, Makwenda C, Tsetekani E, Makonda‐Ridley A, et al. Effects of quality improvement in health facilities and community mobilization through women's groups on maternal, neonatal and perinatal mortality in three districts of Malawi: MaiKhanda, a cluster randomized controlled effectiveness trial. International Health 2013;5(3):180‐95. [DOI] [PMC free article] [PubMed] [Google Scholar]
Dance 1987 {published data only}
- Dance J. A social intervention by linkworkers to Pakistani women and pregnancy outcome [MA thesis]. Warwick: University of Warwick, 1987. [Google Scholar]
Doyle 2014 {published data only}
- Doyle O, McGlanaghy E, Palamaro‐Munsell E, McAuliffe F. Home based educational intervention to improve perinatal outcomes for a disadvantaged community: a randomised control trial. European Journal of Obstetrics, Gynecology, and Reproductive Biology 2014;180:162‐7. [DOI] [PubMed] [Google Scholar]
Ellard 2012 {published data only}
- Ellard D, Simkiss D, Quenby S, Davies D, Kandala NB, Kamwendo F, et al. The impact of training non‐physician clinicians in Malawi on maternal and perinatal mortality: a cluster randomised controlled evaluation of the enhancing training and appropriate technologies for mothers and babies in Africa (ETATMBA) project. BMC Pregnancy and Childbirth 2012;12:116. [DOI] [PMC free article] [PubMed] [Google Scholar]
Foord 1995 {published data only}
- Foord F. Gambia: evaluation of the mobile health care service in West Kiang district. World Health Statistics Quarterly 1995;48(1):18‐22. [PubMed] [Google Scholar]
Ford 2001 {published data only}
- Ford K, Hoyer P, Weglicki L, Kershaw T, Schram C, Jacobson M. Effects of a prenatal care intervention on the self‐concept and self‐efficacy of adolescent mothers. Journal of Perinatal Education 2001;10(2):15‐22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ford K, Weglicki L, Kershaw T, Schram C, Hoyer PJ, Jacobson ML. Effects of a prenatal care intervention for adolescent mothers on birth weight, repeat pregnancy, and educational outcomes at one year postpartum. Journal of Perinatal Education 2002;11(1):35‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gokcay 1993 {published data only}
- Gokcay G, Bulut A, Neyzi O. Paraprofessional women as health care facilitators in mother and child health. Tropical Doctor 1993;23:79‐81. [DOI] [PubMed] [Google Scholar]
Homer 2001 {published data only}
- Homer C. Incorporating cultural diversity in randomised controlled trials in midwifery. Midwifery 2000;16:252‐9. [DOI] [PubMed] [Google Scholar]
- Homer CS, Davis GK, Brodie PM. What do women feel about community‐based antenatal care?. Australian & New Zealand Journal of Public Health 2000;24:590‐5. [DOI] [PubMed] [Google Scholar]
- Homer CS, Davis GK, Cooke M, Barclay LM. Women's experiences of continuity of midwifery care in a randomised controlled trial in Australia. Midwifery 2002;18(2):102‐12. [DOI] [PubMed] [Google Scholar]
- Homer CS, Matha DV, Jordan LG, Wills J, Davis GK. Community‐based continuity of midwifery care versus standard hospital care: a cost analysis. Australian Health Review 2001;24(1):85‐93. [DOI] [PubMed] [Google Scholar]
- Homer CSE, Davis GK, Brodie PM, Sheehan A, Barclay LM, Wills J, et al. Collaboration in maternity care: a randomised controlled trial comparing community‐based continuity of care with standard hospital care. BJOG: an international journal of obstetrics and gynaecology 2001;108:16‐22. [DOI] [PubMed] [Google Scholar]
Ickovics 2007 {published data only}
- Ickovics JR, Kershaw TS, Westdahl C, Magriples U, Massey Z, Reynolds H, et al. Group prenatal care and perinatal outcomes: a randomized controlled trial. Obstetrics & Gynecology 2007;110(2 Pt 1):330‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Novick G, Reid E, Lewis J, Kershaw S, Rising SS, Ickovics R. Group prenatal care: model fidelity and outcomes. American Journal of Obstetrics and Gynecology 2013;209(2):112.e1‐112.e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Novick G, Reid E, Lewis J, Kershaw T, Rising S, Ickovics R. Group prenatal care: model fidelity and outcomes. Journal of Midwifery & Women's Health 2013;58(5):586‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Jennings 2010 {published data only}
- Jennings L, Yebadokpo AS, Affo J, Agbogbe M. Antenatal counseling in maternal and newborn care: use of job aids to improve health worker performance and maternal understanding in Benin. BMC Pregnancy and Childbirth 2010;10:75. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kafatos 1989 {published data only}
- Kafatos AG, Tsitoura S, Pantelakis SN, Doxiadis SA. Maternal and infant health education in a rural Greek community. Hygie 1991;10(1):32‐7. [PubMed] [Google Scholar]
- Kafatos AG, Vlachonikolis IG, Codrington CA. Nutrition during pregnancy: the effects of an educational intervention program in Greece. American Journal of Clinical Nutrition 1989;50:970‐9. [DOI] [PubMed] [Google Scholar]
Koniak‐Griffin 1991 {published data only}
- Koniak‐Griffin D, Verzemnieks I. Effects of nursing intervention on adolescents' maternal role attainment. Issues in Comprehensive Pediatric Nursing 1991;14:121‐38. [DOI] [PubMed] [Google Scholar]
Koniak‐Griffin 2000 {published data only}
- Koniak‐Griffin D, Anderson NL, Brecht ML, Verzemnieks I, Lesser J, Kim S. Public health nursing care for adolescent mothers: impact on infant health and selected maternal outcomes at 1 year postbirth. Journal of Adolescent Health 2002;30(1):44‐54. [DOI] [PubMed] [Google Scholar]
- Koniak‐Griffin D, Anderson NL, Verzemnieks I, Brecht ML. A public health nursing early intervention program for adolescent mothers: outcomes from pregnancy through 6 weeks postpartum. Nursing Research 2000;49(3):130‐8. [DOI] [PubMed] [Google Scholar]
- Koniak‐Griffin D, Verzemnieks IL, Anderson NL, Brecht ML, Lesser J, Kim S, et al. Nurse visitation for adolescent mothers: two‐year infant health and maternal outcomes. Nursing Research 2003;52(2):127‐36. [DOI] [PubMed] [Google Scholar]
Kusulasai 1993 {published data only}
- Kusulasai K, Somrit N. A comparative study of new antenatal care schedule versus conventional one in detection of pregnancy complications in Chon Buri Hospital. Chon Buri Hospital Journal 1993;18(2):17‐31. [Google Scholar]
Leung 2012 {published data only}
- Leung SSK, Lam TH. Group antenatal intervention to reduce perinatal stress and depressive symptoms related to intergenerational conflicts: a randomized controlled trial. International Journal of Nursing Studies 2012;49(11):1391‐402. [DOI] [PubMed] [Google Scholar]
Magriples 2008 {published data only}
- Magriples U, Kershaw TS, Rising SS, Massey Z, Ickovics JR. Prenatal health care beyond the obstetrics service: utilization and predictors of unscheduled care. American Journal of Obstetrics and Gynecology 2008;198(1):75.e1‐75.e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Miller 2012 {published data only}
- Miller PC, Rashida G, Tasneem Z, Haque MU. The effect of traditional birth attendant training on maternal and neonatal care. International Journal of Gynecology and Obstetrics 2012;117(2):148‐52. [DOI] [PubMed] [Google Scholar]
Munjanja 1996 {published data only}
- Munjanja SP. A randomized controlled trial of two programmes of antenatal care in Harare, Zimbabwe. International Journal of Gynecology & Obstetrics 1994;46:31. [Google Scholar]
- Munjanja SP, Lindmark G, Nystrom L. Randomised controlled trial of a reduced‐visits programme of antenatal care in Harare, Zimbabwe. Lancet 1996;348:364‐9. [DOI] [PubMed] [Google Scholar]
- Murira N, Munjanja SP, Zhanda I, Nystrom L, Lindmark G. Effect of a new antenatal care programme on the attitudes of pregnant women and midwives towards antenatal care in Harare. Central African Journal of Medicine 1997;43(5):131‐5. [PubMed] [Google Scholar]
Olds 1986 {published data only}
- Eckenrode J, Ganzel B, Henderson CRJ, Smith E, Olds DL, Powers J, et al. Preventing child abuse and neglect with a program of nurse home visitation: the limiting effects of domestic violence [See comments]. JAMA 2000;284(11):1385‐91. [DOI] [PubMed] [Google Scholar]
- Olds D, Henderson CRJ, Kitzman H, Cole R. Effects of prenatal and infancy nurse home visitation on surveillance of child maltreatment. Pediatrics 1995;95(3):365‐72. [PubMed] [Google Scholar]
- Olds DL. Home visitation for pregnant women and parents of young children. American Journal of Diseases of Children 1992;146:704‐8. [DOI] [PubMed] [Google Scholar]
- Olds DL, Eckenrode J, Henderson CRJ, Kitzman H, Powers J, Cole R, et al. Long‐term effects of home visitation on maternal life course and child abuse and neglect. Fifteen‐year follow‐up of a randomized trial. JAMA: Journal of the American Medical Association 1997;278(8):637‐43. [PubMed] [Google Scholar]
- Olds DL, Henderson CR, Chamberlin R, Tatelbaum R. Preventing child abuse and neglect: a randomized trial of nurse home visitation. Pediatrics 1986;78:65‐78. [PubMed] [Google Scholar]
- Olds DL, Henderson CR, Phelps C, Kitzman H, Hanks C. Effect of prenatal and infancy nurse home visitation on government spending. Medical Care 1993;31:155‐74. [DOI] [PubMed] [Google Scholar]
- Olds DL, Henderson CR, Tatelbaum R. Intellectual impairment in children of women who smoke cigarettes during pregnancy. Pediatrics 1994;93:221‐7. [PubMed] [Google Scholar]
- Olds DL, Henderson CR, Tatelbaum R, Chamberlin R. Improving the delivery of prenatal care and outcomes of pregnancy: a randomized trial of nurse home visitation. Pediatrics 1986;77:16‐28. [PubMed] [Google Scholar]
- Olds DL, Henderson CR, Tatelbaum R, Chamberlin R. Improving the life‐course development of socially disadvantaged mothers: a randomized trial of nurse home visitation. American Journal of Public Health 1988;78:1436‐45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olds DL, Henderson CRJ, Kitzman H. Does prenatal and infancy nurse home visitation have enduring effects on qualities of parental caregiving and child health at 25 to 50 months of life?. Pediatrics 1994;93(1):89‐98. [PubMed] [Google Scholar]
Olds 1995a {published data only}
- Olds DL, Kitzman H, Cole R, Robinson J, Sidora K, Luckey DW, et al. Effects of nurse home‐visiting on maternal life course and child development: age 6 follow‐up results of a randomized trial. Pediatrics 2004;114(6):1550‐9. [DOI] [PubMed] [Google Scholar]
- Olds DL, Kitzman H, Hanks C, Cole R, Anson E, Sidora‐Arcoleo K, et al. Effects of nurse home visiting on maternal and child functioning: age‐9 follow‐up of a randomized trial. Pediatrics 2007;120(4):e832‐45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olds DL, Kitzman HJ, Cole RE. Effect of home visitation by nurses on caregiving and maternal life‐course. Archives of Pediatrics and Adolescent Medicine 1995;149:P76. [Google Scholar]
- Olds DL, Kitzman HJ, Cole RE, Hanks CA, Arcoleo KJ, Anson EA, et al. Enduring effects of prenatal and infancy home visiting by nurses on maternal life course and government spending: follow‐up of a randomized trial among children at age 12 years. Archives of Pediatrics & Adolescent Medicine 2010;164(5):419‐24. [DOI] [PMC free article] [PubMed] [Google Scholar]
Rodriguez‐Angulo 2012 {published data only}
- Rodriguez‐Angulo E, Andueza‐Pech G, Rosado‐Alcocer L, Ortiz‐Panozo E, Hernandez‐Prado B. Effect of a community‐based intervention to improve the knowledge on the warning signs of maternal complications among Mayan women from Yucatan randomized controlled trial [Spanish] [Efecto de una intervencion comunitaria para mejorar conocimientos sobre signos de alarma de complicaciones maternas en mujeres mayas de Yucatan, ensayo controlado, aleatorizado]. Revista de Investigacion Clinica 2012;64(2):154‐63. [PubMed] [Google Scholar]
Schellenberg 2011 {published data only}
- Schellenberg D, Mshinda H, Tanner M. Improving newborn survival in rural southern Tanzania: a study to evaluate the impact and cost of a scaleable package of interventions at community level with health system strengthening. http://clinicaltrials.gov/ct2/show/record/NCT01022788 (accessed 25 November 2011) 2011.
Srinivasan 1995 {published data only}
- Srinivasan V, Radhakrishna S, Sudha R, Malathi MV, Jabbar S, Ramakrishnan R, et al. Randomised controlled field trial of two antenatal care packages in rural south India. Indian Journal of Medical Research 1995;102:86‐94. [PubMed] [Google Scholar]
Tomlinson 2014 {published data only}
- Tomlinson M. An effectiveness study of an integrated, community based package for maternal, newborn, child and HIV care in a disadvantaged community in South Africa. Current Controlled Trials (www.controlled‐trials.com) (accessed 12 May 2010) 2010. [DOI] [PMC free article] [PubMed]
- Tomlinson M, Doherty T, Ijumba P, Jackson D, Lawn J, Persson LA, et al. Goodstart: a cluster randomised effectiveness trial of an integrated, community‐based package for maternal and newborn care, with prevention of mother‐to‐child transmission of HIV in a South African township. Tropical Medicine & International Health 2014;19(3):256‐66. [DOI] [PubMed] [Google Scholar]
- Tomlinson M, Doherty T, Jackson D, Lawn JE, Ijumba P, Colvin M, et al. An effectiveness study of an integrated, community‐based package for maternal, newborn, child and HIV care in South Africa: study protocol for a randomized controlled trial. Trials 2011;12:236. [DOI] [PMC free article] [PubMed] [Google Scholar]
Tough 2006 {published data only}
- Johnston D, Tough S, Siever J. The Community Perinatal Care Study: home visiting and nursing support for pregnant women. Zero to Three 2006;27(2):11‐7. [Google Scholar]
- Tough SC, Johnston DW, Siever JE, Jorgenson G, Slocombe L, Lane C, et al. Does supplementary prenatal nursing and home visitation support improve resource use in a universal health care system? A randomized controlled trial in Canada. Birth 2006;33(3):183‐94. [DOI] [PubMed] [Google Scholar]
- Tough SC, Johnston DW, Siever JE, Jorgenson G, Slocombe L, Lane C, et al. Does supplementary prenatal nursing and home visitation support improved resource utilization in a system of univeral health care? Results from a randomized controlled trial in Canada [abstract]. Pediatric Academic Societies Annual Meeting; 2006 April 29‐May 2; San Fransisco, CA, USA. 2006. [DOI] [PubMed]
- Tough SC, Siever JE, Johnston DW. Retaining women in a prenatal care randomized controlled trial in Canada: implications for program planning. BMC Public Health 2007;7:148. [DOI] [PMC free article] [PubMed] [Google Scholar]
Tough 2007 {published data only}
- Tough S. A randomised controlled trial comparing group to individual prenatal care. Current Controlled Trials (www.controlled‐trials.com/) (accessed 30 October 2007) 2007.
Turan 2001 {published data only}
- Turan JM, Nalbant H, Bulut A, Sahip Y. Including expectant fathers in antenatal education programmes in Istanbul, Turkey. Reproductive Health Matters 2001;9(18):114‐25. [DOI] [PubMed] [Google Scholar]
References to ongoing studies
Bhandari 2014 {published data only}
- Bhandari GP, Subedi N, Thapa J, Choulagai B, Maskey MK, Onta SR. A cluster randomized implementation trial to measure the effectiveness of an intervention package aiming to increase the utilization of skilled birth attendants by women for childbirth: study protocol. BMC Pregnancy and Childbirth 2014;14(1):109. [DOI] [PMC free article] [PubMed] [Google Scholar]
Chavane 2014 {published data only}
- Chavane L, Merialdi M, Betran AP, Requejo‐Harris J, Bergel E, Aleman A, et al. Implementation of evidence‐based antenatal care in Mozambique: a cluster randomized controlled trial: study protocol. BMC Health Services Research 2014;14(1):228. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kestler 2013 {published data only}
- Kestler E, Walker D, Bonvecchio A, Saenz de Tejada S, Donner A. A matched pair cluster randomized implementation trial to measure the effectiveness of an intervention package aiming to decrease perinatal mortality and increase institution‐based obstetric care among indigenous women in Guatemala: study protocol. BMC Pregnancy and Childbirth 2013;13(1):73. [DOI] [PMC free article] [PubMed] [Google Scholar]
Khan 2012 {published data only}
- Khan MA, Mirza S, Ahmed M, Rasheed A, Khan A, Walley J, et al. Making birthing safe for Pakistan women: A cluster randomized trial. BMC Pregnancy and Childbirth 2012;12:67. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kikuchi 2015 {published data only}
- Kikuchi K, Ansah E, Okawa S, Shibanuma A, Gyapong M, Owusu‐Agyei S, et al. Ghana's Ensure Mothers and Babies Regular Access to Care (EMBRACE) program: study protocol for a cluster randomized controlled trial. Trials 2015;16:22. [DOI] [PMC free article] [PubMed] [Google Scholar]
Morrison 2011 {published data only}
- Morrison J, Tumbahangphe KM, Budhathoki B, Neupane R, Sen A, Dahal K, et al. Community mobilisation and health management committee strengthening to increase birth attendance by trained health workers in rural Makwanpur, Nepal: Study protocol for a cluster randomised controlled trial. Trials 2011;12:128. [DOI] [PMC free article] [PubMed] [Google Scholar]
Owen‐Jones 2013 {published data only}
- Owen‐Jones E, Bekkers MJ, Butler CC, Cannings‐John R, Channon S, Hood K, et al. The effectiveness and cost‐effectiveness of the Family Nurse Partnership home visiting programme for first time teenage mothers in England: a protocol for the Building Blocks randomised controlled trial. BMC Pediatrics 2013;13:114. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ramsey 2013 {published data only}
- Ramsey K, Hingora A, Kante M, Jackson E, Exavery A, Pemba S, et al. The Tanzania Connect Project: a cluster‐randomized trial of the child survival impact of adding paid community health workers to an existing facility‐focused health system. BMC Health Services Research 2013;13(Suppl 2):S6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Richter 2013 {published data only}
- Richter SM, Leroy JL, Olney D, Quinones E, Ruel M. Strengthening and evaluating the preventing malnutrition in children under 2 approach in Guatemala: Report of the enrollment survey. Strengthening and Evaluating the Preventing Malnutrition in Children under 2 Approach in Guatemala: Report of the Enrollment Survey. Washington DC: FHI 360, 2013. [Google Scholar]
Sando 2014 {published data only}
- Sando D, Geldsetzer P, Magesa L, Andrew I, Machumi L, Mwanyika‐Sando M, et al. Evaluation of a community health worker intervention and the World Health Organization's option B versus option A to improve antenatal care and PMTCT outcomes in Dar es Salaam, Tanzania: study protocol for a cluster‐randomized controlled health systems implementation trial. Trials 2014;15(1):359. [DOI] [PMC free article] [PubMed] [Google Scholar]
Shepard 2014 {published data only}
- Shepard D. Impact evaluation of the pilot SMS mother reminder system. ClinicalTrials.gov (http://clinicaltrials.gov/) [accessed 2 September 2014] 2014.
Shrestha 2011 {published data only}
- Shrestha BP, Bhandari B, Manandhar DS, Osrin D, Costello A, Saville N. Community interventions to reduce child mortality in Dhanusha, Nepal: study protocol for a cluster randomized controlled trial. Trials 2011;12:136. [DOI] [PMC free article] [PubMed] [Google Scholar]
Vos 2015 {published data only}
- Vos AA, Voorst SF, Waelput AJ, Jong‐Potjer LC, Bonsel GJ, Steegers EA, et al. Effectiveness of score card‐based antenatal risk selection, care pathways, and multidisciplinary consultation in the Healthy Pregnancy 4 All study (HP4ALL): study protocol for a cluster randomized controlled trial. Trials 2015;16(1):8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Additional references
Agus 2012
- Agus Y, Horiuchi S, Porter SE. Rural Indonesia women's traditional beliefs about antenatal care. BMC Research Notes 2012;5:589. [PUBMED: 23106915] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ballard 2013
- Ballard K, Gari L, Mosisa H, Wright J. Provision of individualised obstetric risk advice to increase health facility usage by women at risk of a complicated delivery: a cohort study of women in the rural highlands of West Ethiopia. BJOG: an international journal of obstetrics and gynaecology 6 March 2013;120(8):971‐978. [DOI: 10.1111/1471-0528.12190; PUBMED: 23464619] [DOI] [PubMed] [Google Scholar]
Barber 2009
- Barber SL, Gertler PJ. Empowering women to obtain high quality care: evidence from an evaluation of Mexico's conditional cash transfer programme. Health Policy and Planning 2009;24(1):18‐25. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bloom 1999
- Bloom SS, Lippeveld T, Wypij D. Does antenatal care make a difference to safe delivery? A study in urban Uttar Pradesh, India. Health Policy and Planning 1999;14(1):38‐48. [PUBMED: 10351468] [DOI] [PubMed] [Google Scholar]
Cesar 2012
- Cesar JA, Sutil AT, Santos GB, Cunha CF, Mendoza‐Sassi RA. Prenatal care in public and private health services: a population‐based survey in Rio Grande, Rio Grande do Sul State, Brazil [Assistencia pre‐natal nos servicos publicos e privados de saude: estudo transversal de base populacional em Rio Grande, Rio Grande do Sul, Brasil]. Cadernos de Saude Publica 2012;28(11):2106‐14. [PUBMED: 23147952] [DOI] [PubMed] [Google Scholar]
Darmstadt 2005
- Darmstadt GL, Bhutta ZA, Cousens S, Adam T, Walker N, Bernis L. Evidence‐based, cost‐effective interventions: how many newborn babies can we save?. Lancet 2005;365(9463):977‐88. [PUBMED: 15767001] [DOI] [PubMed] [Google Scholar]
Delgado‐Rodriguez 1996
- Delgado‐Rodriguez M, Gomez‐Olmedo M, Bueno‐Cavanillas A, Galvez‐Vargas R. A comparison of two indices of adequacy of prenatal care utilization. Epidemiology 1996;7(6):648‐50. [DOI] [PubMed] [Google Scholar]
Dettrick 2013
- Dettrick Z, Firth S, Jimenez Soto E. Do strategies to improve quality of maternal and child health care in lower and middle income countries lead to improved outcomes? A review of the evidence. PloS One 2013;8(12):e83070. [PUBMED: 24349435] [DOI] [PMC free article] [PubMed] [Google Scholar]
Dogba 2009
- Dogba M, Fournier P. Human resources and the quality of emergency obstetric care in developing countries: a systematic review of the literature. Human Resources for Health 2009;7:7. [PUBMED: 19200353] [DOI] [PMC free article] [PubMed] [Google Scholar]
Dowswell 2015
- Dowswell T, Carroli G, Duley L, Gates S, Gulmezoglu AM, Khan‐Neelofur D, Piaggio G. Alternative versus standard packages of antenatal care for low‐risk pregnancy. Cochrane Database of Systematic Reviews 2015, Issue 7. [DOI: 10.1002/14651858.CD000934.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Edgerley 2007
- Edgerley L. Use of a community mobile health van to increase early access to prenatal care. Maternal and Child Health Journal 2007;11(3):235‐9. [DOI: 10.1007/s10995-006-0174-z] [DOI] [PubMed] [Google Scholar]
Gertler 2000
- Gertler, Paul. Final report: The impact of Progressa on health. International Food Policy Research Institute Nov 2000. [Google Scholar]
Grilli 2002
- Grilli R, Ramsay C, Minozzi S. Mass media interventions: effects on health services utilisation. Cochrane Database of Systematic Reviews 2002, Issue 1. [DOI: 10.1002/14651858.CD000389] [DOI] [PubMed] [Google Scholar]
Haider 2012
- Haider BA, Bhutta ZA. Multiple‐micronutrient supplementation for women during pregnancy. Cochrane Database of Systematic Reviews 2012, Issue 11. [DOI: 10.1002/14651858.CD004905.pub3] [DOI] [PubMed] [Google Scholar]
Hawkes 2013
- Hawkes SJ, Gomez GB, Broutet N. Early antenatal care: does it make a difference to outcomes of pregnancy associated with syphilis? A systematic review and meta‐analysis. PloS One 2013;8(2):e56713. [PUBMED: 23468875] [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Khan‐Neelofur 1998
- Khan‐Neelofur D, Gulmezoglu M, Villar J. Who should provide routine antenatal care for low‐risk women, and how often? A systematic review of randomised controlled trials. WHO Antenatal Care Trial Research Group. Paediatric and Perinatal Epidemiology 1998;12(Suppl 2):7‐26. [PUBMED: 9805721] [DOI] [PubMed] [Google Scholar]
Kidney 2009
- Kidney E, Winter HR, Khan KS, Gulmezoglu AM, Meads CA, Deeks JJ, et al. Systematic review of effect of community‐level interventions to reduce maternal mortality. BMC Pregnancy and Childbirth 2009;9:2. [PUBMED: 19154588] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kinzie 2004
- Kinzie B, Gomez P. Basic maternal and newborn care: a guide for skilled providers. http://www.jhpiego.org/files/BMNCrevmanEN.pdf (JHPIEGO/MNH Program: Baltimore, MD) 2004.
Langer 1993
- Langer A, Victora C, Victora M, Barros F, Farnot U, Belizan J, et al. The Latin American trial of psychosocial support during pregnancy: a social intervention evaluated through an experimental design. Social Sciences and Medicine 1993;36:495‐507. [DOI] [PubMed] [Google Scholar]
Lassi 2015
- Lassi ZS, Bhutta ZA. Community‐based intervention packages for reducing maternal and neonatal morbidity and mortality and improving neonatal outcomes. Cochrane Database of Systematic Reviews 2015, Issue 3. [DOI: 10.1002/14651858.CD007754.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Liberati 2009
- Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta‐analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ (Clinical Research ed.) 2009;339:b2700. [PUBMED: 19622552] [DOI] [PMC free article] [PubMed] [Google Scholar]
Mangham‐Jefferies 2014
- Mangham‐Jefferies L, Pitt C, Cousens S, Mills A, Schellenberg J. Cost‐effectiveness of strategies to improve the utilization and provision of maternal and newborn health care in low‐income and lower‐middle‐income countries: a systematic review. BMC Pregnancy and Childbirth 2014;14:243. [PUBMED: 25052536] [DOI] [PMC free article] [PubMed] [Google Scholar]
Marteau 2006
- Marteau T, Dieppe P, Foy R, Kinmonth A, Schneiderman N. Behavioural medicine: changing our behaviour. BMJ 2006;332(7539):437‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Marteau 2009
- Marteau TM, Ashcroft RE, Oliver A. Using financial incentives to achieve healthy behaviour. BMJ 2009;338:b1415. [DOI] [PubMed] [Google Scholar]
Mbuagbaw 2011
- Mbuagbaw LC, Gofin R. A new measurement for optimal antenatal care: determinants and outcomes in Cameroon. Maternal and Child Health Journal 2011;15(8):1427‐34. [PUBMED: 21057862] [DOI] [PubMed] [Google Scholar]
Mishra 2006
- Mishra V, Retherford RD. The effect of neonatal care on professional assistance at delivery in rural India. Demographic and Health Research 2006; Vol. 28.
Oakley 2009
- Oakley L, Gray R, Kurinczuk JJ, Brocklehurst P, Hollowell J. A systematic review of the effectiveness of interventions to increase the early initiation of antenatal care in socially disadvantaged and vulnerable women. https://www.npeu.ox.ac.uk/files/downloads/infant‐mortality/Infant‐Mortality‐ANC‐Uptake‐Review.pdf 2009. [DOI] [PMC free article] [PubMed]
Ota 2015
- Ota E, Hori H, Mori R, Tobe‐Gai R, Farrar D. Antenatal dietary education and supplementation to increase energy and protein intake. Cochrane Database of Systematic Reviews 2015, Issue 6. [DOI: 10.1002/14651858.CD000032.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Pagel 2011
- Pagel C, Prost A, Lewycka S, Das S, Colbourn T, Mahapatra R, et al. Intracluster correlation coefficients and coefficients of variation for perinatal outcomes from five cluster‐randomised controlled trials in low and middle‐income countries: results and methodological implications. Trials 2011;12:151‐62. [DOI] [PMC free article] [PubMed] [Google Scholar]
Pattinson 2009
- Pattinson R, Say L, Souza JP, Broek N, Rooney C. WHO maternal death and near‐miss classifications. Bulletin of the World Health Organization 2009; Vol. 87, issue 10:734. [PUBMED: 19876533] [DOI] [PMC free article] [PubMed]
Piaggio 2001
- Piaggio G, Carroli G, Villar J, Pinol A, Bakketeig L, Lumbiganon P, et al. Methodological considerations on the design and analysis of an equivalence stratified cluster randomization trial. Statistics in Medicine 2001;20(40):401‐16. [DOI] [PubMed] [Google Scholar]
Poston 2006
- Poston L, Briley AL, Seed PT, Kelly FJ, Shennan AH. Vitamin C and vitamin E in pregnant women at risk for pre‐eclampsia (VIP trial): randomised placebo‐controlled trial. Lancet (London, England) 2006;367(9517):1145‐54. [PUBMED: 16616557] [DOI] [PubMed] [Google Scholar]
Prost 2013
- Prost A, Colbourn T, Seward N, Azad K, Coomarasamy A, Copas A, et al. Women's groups practising participatory learning and action to improve maternal and newborn health in low‐resource settings: a systematic review and meta‐analysis. Lancet 2013;381(9879):1736‐46. [PUBMED: 23683640] [DOI] [PMC free article] [PubMed] [Google Scholar]
Raatikainen 2007
- Raatikainen K, Heiskanen N, Heinonen S. Under‐attending free antenatal care is associated with adverse pregnancy outcomes. BMC Public Health 2007;7:268. [PUBMED: 17900359] [DOI] [PMC free article] [PubMed] [Google Scholar]
RevMan 2014 [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan). Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Say 2007
- Say L, Raine R. A systematic review of inequalities in the use of maternal health care in developing countries: examining the scale of the problem and the importance of context. Bulletin of the World Health Organization 2007;85:812–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Showstack 1984
- Showstack JA, Budetti PP, Minkler D. Factors associated with birthweight: an exploration of the roles of prenatal care and length of gestation. American Journal of Public Health 1984;74(9):1003‐8. [PUBMED: 6465400] [DOI] [PMC free article] [PubMed] [Google Scholar]
Siza 2008
- Siza JE. Risk factors associated with low birth weight of neonates among pregnant women attending a referral hospital in northern Tanzania. Tanzania Journal of Health Research 2008;10(1):1‐8. [PUBMED: 18680958] [DOI] [PubMed] [Google Scholar]
Souza 2013
- Souza JP, Gulmezoglu AM, Vogel J, Carroli G, Lumbiganon P, Qureshi Z, et al. Moving beyond essential interventions for reduction of maternal mortality (the WHO Multicountry Survey on Maternal and Newborn Health): a cross‐sectional study. Lancet 2013;381:1747‐55. [DOI] [PubMed] [Google Scholar]
Titaley 2010
- Titaley CR, Hunter CL, Heywood P, Dibley MJ. Why don't some women attend antenatal and postnatal care services?: a qualitative study of community members' perspectives in Garut, Sukabumi and Ciamis districts of West Java Province, Indonesia. BMC Pregnancy and Childbirth 2010;10:61. [PUBMED: 20937146] [DOI] [PMC free article] [PubMed] [Google Scholar]
United Nations 2013
- United Nations. United Nations' Millenium Development Goals. http://www.un.org/millenniumgoals/ [accessed 1 Sept 2015] 2013.
van Eijk 2006
- Eijk AM, Bles HM, Odhiambo F, Ayisi JG, Blokland IE, Rosen DH, et al. Use of antenatal services and delivery care among women in rural western Kenya: a community based survey. Reproductive Health 2006;3:2. [PUBMED: 16597344] [DOI] [PMC free article] [PubMed] [Google Scholar]
Viera 2005
- Viera AJ, Garrett JM. Understanding interobserver agreement: the kappa statistic. Family Medicine 2005;37(5):360‐3. [PubMed] [Google Scholar]
Vogel 2013
- Vogel JP, Ndema HA, Souza JP, Gulmezoglu MA, Dowswell T, Carroli G, et al. Antenatal care packages with reduced visits and perinatal mortality: a secondary analysis of the WHO Antenatal Care Trial. Reproductive Health 2013;10(1):19. [PUBMED: 23577700] [DOI] [PMC free article] [PubMed] [Google Scholar]
WHO 2004
- WHO. International Classification of Diseases (ICD) 10th Revision. http://www.who.int/healthinfo/statistics/indmaternalmortality/en/ [accessed 1 Sept 2015]. Geneva: World Health Organization, 2004.
WHO 2011
- WHO. Statement on antenatal care. http://www.who.int/reproductivehealth/publications/maternal_perinatal_health/rhr_11_12/en/ [accessed 1 Sept 2015] 2011.
WHO 2012b
- WHO. WHO Evidence Review Group: Intermittent Preventive Treatment of malaria in pregnancy (IPTp) with Sulfadoxine‐Pyrimethamine (SP). http://www.who.int/malaria/mpac/sep2012/iptp_sp_erg_meeting_report_july2012.pdf [accessed 1 Sept 2015] 2012.
WHO 2012c
- WHO. Maternal mortality. http://www.who.int/mediacentre/factsheets/fs348/en/ [accessed 1 Sept 2015] 2012.
WHO 2013
- WHO. Antenatal care. http://www.who.int/gho/maternal_health/reproductive_health/antenatal_care_text/en/ [accessed 1 Sept 2015] 2013.
WHO 2013a
- WHO, UNICEF, UNFPA, The World Bank, the United Nations Population Division. Trends in Maternal Mortality: 1990 to 2013. http://www.who.int/reproductivehealth/publications/monitoring/maternal‐mortality‐2013/en/ [accessed 1 Sept 2015] 2013.
World Bank 2015
- World Bank. Country and Lending Groups. http://data.worldbank.org/about/country‐and‐lending‐groups [accessed 1 Sept 2015] 2015.
References to other published versions of this review
Mbuagbaw 2014
- Mbuagbaw L, Habiba Garga K, Ongolo‐Zogo P. Health system and community level interventions for improving antenatal care coverage and health outcomes. Cochrane Database of Systematic Reviews 2014, Issue 2. [DOI: 10.1002/14651858.CD010994] [DOI] [PMC free article] [PubMed] [Google Scholar]


