Abstract
To identify trajectories of posttraumatic stress (PTS) and depression symptom groups after deployment and determine the effect of alcohol use disorder on these trajectories, PTS symptoms were modeled using the PTSD Checklist in 472 Ohio National Guard members, and depression symptoms were modeled using the 9-item Patient Health Questionnaire in 727 Ohio National Guard members. There were 42% of participants who were resistant to PTS symptoms across the 4 years of study and 55.9% were resistant to depression symptoms. There were 19% and 42.2% of participants who showed resilience (experiencing slightly elevated symptoms followed by a decline, according to Bonanno et al., 2004) to depression and PTS symptoms, respectively. Mild and chronic dysfunction constituted the smallest trajectory groups across disorders. Marital status, deployment to an area of conflict, and number of lifetime stressors were associated with membership into different latent groups for depression (unstandardized beta estimates range: 0.69 to 1.37). Deployment to an area of conflict, number of lifetime potentially traumatic events and education predicted membership into different latent groups for PTS (unstandardized beta estimate range: 0.83 to 3.17). Alcohol use disorder was associated with an increase in both symptom outcomes (unstandardized beta estimate range: 0.20 to 9.45). These results suggest that alcohol use disorder may have contributed substantially to trajectories of psychopathology in this population.
It is well established that posttraumatic stress (PTS) and depression are more prevalent in military (Thomas et al., 2010) compared to civilian (Kessler et al., 2005) populations. Posttraumatic stress disorder (PTSD) prevalence estimates among Operation Enduring Freedom (OEF) and Operation Iraqi Freedom (OIF) veterans range from about 5% to 20% (Kok, Herrell, Thomas, & Hoge, 2012; Ramchand et al., 2010; Smith et al., 2008); depression prevalence estimates range from about 2–16% (RAND, 2008; Wells et al., 2010). The experiences of OEF/OIF veterans suggest that the trajectories of these disorders may reflect lifecourse civilian and combat experiences that depart from those of previous generations (Bonanno et al., 2012). Trajectories of mental health over time, however, have been predominately studied in civilian populations following specific traumatic event (TE) experiences (Lowe, Galea, Uddin, & Koenen, 2014; Nandi, Tracy, Beard, Vlahov, & Galea, 2009; Pietrzak, Van Ness, Fried, Galea, & Norris, 2013). Generally these trajectory groups include resilient (initial symptomology followed by recovery), resistant (consistently low symptomology), and chronic dysfunction groups (consistently high symptomology), together with more variable relapsing/remitting groups (Bonanno et al., 2012; Norris, Tracy, & Galea, 2009). For example… or “usually one other group”
We also know that alcohol use disorder (AUD) is prevalent among military personnel (Bray et al., 2010; Cohen, Fink, Sampson, & Galea, 2015), potentially due to efforts to self-medicate existing mental illness symptoms (Schumm & Chard, 2012). Although AUD frequently co-exists with psychopathology in military populations (Thomas et al., 2010), we don’t know how it interacts with trajectories of depression and PTS over time. There is a lack of longitudinal follow-up research among OEF/OIF veterans in general (Hoge, Auchterlonie, & Milliken, 2006), with few exceptions (Duma, Reger, Canning, McNeil, & Gahm, 2010; Milliken, Auchterlonie, & Hoge, 2007; Schaller et al., 2014; Seal et al., 2009; Thomas et al., 2010). Further, we are not aware of any published work that has documented trajectories of both depression and PTS in OEF/OIF personnel in one U.S. study. We aimed to document trajectories of symptoms after deployment among OEF/OIF personnel, and estimate how time-stable risk factors and time-varying covariates, including AUD, affect these trajectories across four waves of cohort data.
Method
Participants
Participants were drawn from the Ohio Army National Guard, using a simple random sample as part of the Ohio Army National Guard Mental Health Initiative (OHARNG MHI), drawn from all serving members between 2008 and 2009. After eliminating members without a valid telephone number listed, who wished not to participate, or who were deemed ineligible due to age, retirement status, or language, the official enrollment at baseline was 2,616, with a cooperation rate of 67.5% and a response rate of 43.2%. Detailed information on sampling methods are described elsewhere (Calabrese et al., 2011).
Respondents were interviewed from 2008–2012, approximately 12 months apart. A second round of baseline interviews for new participants (n = 578) was also initiated in 2010–2011 in order to replenish the sample after loss to follow-up. Every respondent included in this analysis participated in at least two waves. The final analytic samples consisted of 727 respondents for depression (those who completed two or more study waves, were deployed within 2 years of baseline assessment, and were non-missing on all risk factors), and 472 respondents for PTS (those who completed two or more study waves, were non-missing on all risk factors, had a TE during a deployment within two years of baseline assessment, and chose that same event as their “worst” event throughout all follow-up interviews, in order to consistently follow symptoms from one single event).
Table 1 presents prevalence of risk factors for both analytical samples, as well as the percent of respondents who completed each wave. The demographics of our analytical samples largely match those of our entire OHARNG MHI sample, with the exception of a lower prevalence of female respondents in both of our analytical samples (not shown), which reflects the fact that we subset to those who had been deployed within two years, and women tend to be deployed less frequently (RAND, 2008). Additionally, the OHARNG MHI study population reflected the overall target population of Ohio National Guard service members (Calabrese et al., 2011).
Table 1.
Baseline Prevalence of Risk Factors by Subsample
| Variable | Depression subsample (n = 727) | PTS subsample (n = 472) | ||
|---|---|---|---|---|
| n | % | n | % | |
| Completed Wave 2 | 628 | 86.4 | 412 | 87.3 |
| Completed Wave 3 | 478 | 65.8 | 304 | 64.4 |
| Completed Wave 4 | 395 | 54.3 | 252 | 53.4 |
| Not married | 395 | 54.3 | 260 | 55.1 |
| High school/GED or less | 173 | 23.8 | 109 | 23.1 |
| 10+ lifetime TEs | 335 | 46.1 | 284 | 60.2 |
| 4+ lifetime stressful events | 343 | 47.2 | 233 | 49.4 |
Note. GED = General Education Development (degree); TE = Traumatic Event
We ran additional analyses comparing respondents who completed all four waves with those who were lost to follow-up on risk factors, covariates, and outcomes. For the depression analytic sample, we found that married soldiers were more likely to have completed all waves (p = .016). The mean number of depression symptoms at baseline, however, was not associated with follow-up completion, so we were not concerned about potential respondent bias. For the PTS analytic sample, complete follow-up was not associated with any risk factors, time-varying covariates, or PTS symptoms at baseline (results not shown).
Procedure
An alert letter with an opt-out was sent to all listed participants, and verbal informed consent was obtained from all participants prior to participation. Interviews (about 60 minutes in length) were administered via a computer-assisted telephone survey.
The Ohio National Guard and the institutional review boards of University Hospitals Case Medical Center, University of Toledo, University of Michigan, Ann Arbor Veterans Administration Medical Center, Columbia University, Boston University, and the Office of Human Research Protections of the US Army Medical Research and Materiel Command approved this study protocol.
Measures
Past-year depression symptoms were modeled assuming a zero-inflated Poisson distribution (ideal for a highly skewed outcome), using a symptom count (0–9) from the Patient Health Questionnaire (PHQ-9; Kroenke, Spitzer, & Williams, 2001); symptoms present during the last 30 days for period of at least 2 weeks were counted as positive. PTS symptoms were modeled assuming a censored normal distribution (considered appropriate for psychiatric scale data; Jones, Nagin, & Roeder, 2001; Nagin & Tremblay, 1999) using the PTSD Check List – Civilian version (PCL) symptom scale (range: 17–85) (Blanchard, Jones-Alexander, Buckley, & Forneris, 1996). PTS symptoms had a Cronbach’s α of .94 at baseline in our analytic sample.
Time-stable risk factors (assessed only at baseline) and time-varying covariates (collected at each time point) were selected for inclusion based on theoretical considerations, significance of terms when entered into models, and model convergence.
PTEs were assessed with the Life Events Checklist – Civilian Version (Gray, Litz, Hsu, & Lombardo, 2004), the Deployment Risk and Resilience Inventory items (King, King, Vogt, Knight, & Samper, 2006), and events used by Breslau et al (Breslau et al., 1998). Events could have occurred either during or outside of the most recent deployment. These were all events that met Criterion A1 for the DSM-IV (Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition [DSM-IV], 4th ed., text rev., American Psychiatric Association [APA], 2000) definition of a PTE, the full list of which are presented in the first part of Supplemental Table 1. A binary variable for high level of TEs was created using the median (10) of the count of total PTEs in the sample. Stressors were events from the above stated instruments that did not qualify for Criterion A1, and are presented in the second half of Supplemental Table 1. A binary variable for high level of stressors was also created using the median (4) of the count in the sample.
Being deployed to an Area of Conflict (AOC) was defined as deployment to either Iraq or Afghanistan during the most recent deployment at baseline. Considering everyone in this sample was deployed within 2 years of baseline, these deployments were to OEF/OIF. Low education was defined as having a high school diploma, GED, or less.
AUD was defined as having either past-year abuse or dependence according to the DSM-IV, as assessed by the Mini-International Neuropsychiatric Interview (Sheehan et al., 1998). Alcohol abuse and dependence were both validated among a random sample of 500 soldiers from the original baseline sample assessed by trained clinicians (Calabrese et al., 2011).
PTSD as a time-varying covariate (for TEs that occurred both in and outside of deployment) was defined as meeting criteria for past-year PTSD, according to the DSM-IV-TR using the PCL (Blanchard et al., 1996), which was validated using the Clinician-Administered PTSD Scale in the clinical sample described above and found to have high sensitivity (.92) and moderate specificity (.54; Prescott et al., 2014).
Past-year depression as a time-varying covariate was defined as reporting a period of at least two weeks with two or more co-occurring symptoms on the PHQ-9 (Kroenke et al., 2001), with one symptom being depressed mood or anhedonia. This definition included, but was not limited to, the DSM-IV diagnosis of Major Depressive Disorder. This inclusive definition was chosen due to higher sensitivity relative to Major Depressive Disorder by itself (.51 compared to .35; both had specificity greater than .82) when validated against the Structured Clinical Interview for DSM-IV-TR (SCID; First, Spitzer, Gibbon, & Williams, 2002) in the clinical sample (Prescott et al., 2014).
Cumulative PTEs were defined as reporting at least one TE (from deployment or not) since last study wave. For all participants, cumulative TEs at baseline were coded as zero, in order to avoid co-linearity with the time-stable measure of baseline TE count.
Data Analysis
Proc Traj, a SAS-callable add-on package which estimates discrete mixture models for longitudinal data (Jones et al., 2001; Jung & Wickrama, 2008), was used to estimate trajectories in SAS version 9.4 (“SAS 9.4 Software,” 2013). Proc Traj is used for group-based latent class growth analysis, which fixes within-group variance to zero in order to more clearly identify latent classes and therefore serves as a more hypothesis-generating method compared to more conventional growth modeling approaches (Jung & Wickrama, 2008). Proc Traj drops respondents who are missing any baseline risk factors from the analysis; consequently, our analytic samples only included participants with non-missing risk factors. Respondents missing time-varying variables, including outcomes and covariates, are kept in the model, and are estimated using other data points under the assumption that they are missing at random Nagin, 2009). Since we had loss to follow-up across the four waves (see Table 1), these missing data points were estimated under this assumption.
Our first step in the analysis was to determine the ideal number of latent groups for each outcome, using the Bayesian Information Criterion (BIC; an approximation of the Bayes factor) and mean posterior probability (greater than or equal to.80 on average for each group; Andruff, Thompson, Gaudreau, & Louvet, 2009). BIC indices suggested that a model with four groups was most appropriate for both outcomes, and all probabilities for these models were greater than or equal to .79 for depression (Supplemental Table 2) and .84 for PTS (Supplemental Table 4), showing a high predictive probability. The order and shape of each trajectory was then determined by iteratively assessing the significance of each term. Covariates and risk factors were added to each model one at a time. Finally, predicted symptoms were graphed in order to specify the difference in predicted trajectory paths based on fixed values of each time-varying covariate (Jones et al., 2001).
Results
Depression
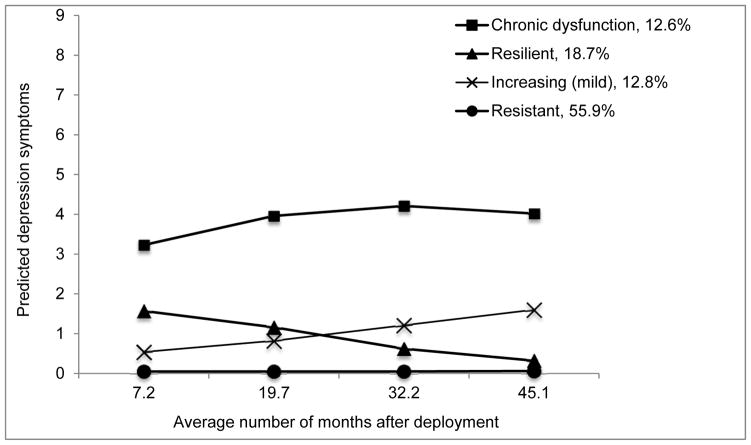
Most participants had low levels of depression symptoms throughout the time period. The means and standard deviations of the number of symptoms at each wave were as follows: 1.04(1.88), 1.07(2.02), 0.91(1.77), and 1.03(2.09). 406 respondents (55.9% of the depression sample) were resistant to symptoms; 136(18.7%) were resilient; 93(12.8%) had a steady increase in symptoms throughout the study period; and 92(12.7%) had a fairly stable high level of symptomatology throughout (referred to as the “chronic dysfunction” group). Figure 1 shows a graph of predicted symptoms across the four time points (Supplemental Table 2 presents data points).
Figure 1. Predicted Trajectories of Depression Symptoms from the PHQ-9 in the Depression Subsample.
Note. PHQ-9 = Nine-Item Patient Health Questionnaire
Table 2 presents risk factors and time-varying covariates that were significant in the final model, along with their corresponding beta estimates. Past-year AUD and PTSD both significantly contributed to a change in shape for all four trajectory groups. Baseline risk factors associated with group membership included marital status, AOC deployment, and lifetime stressors. Having four or more lifetime stressors made respondents more likely to fall into the chronic dysfunction (unstandardized beta = 1.37, p < .001) and increasing (unstandardized beta = 0.69, p = .018) groups. AOC deployment was significantly associated with membership in the chronic dysfunction (unstandardized beta = 1.02, p < .001) and resilient (unstandardized beta = 0.92, p < .001) groups. Being nonmarried was significantly associated with membership in the resilient group (b = 0.80, p = .004). All of these comparisons are with reference to the resistant group.
Table 2.
Unstandardized Beta Estimates of Risk Factors by Subsample
| Latent group | Depression subsample (n = 727) | PTS subsample (n = 472) | |||
|---|---|---|---|---|---|
| Risk factor | Estimate | Risk factor | Estimate | ||
| Resistant group (n = 406) | Referent group | Resistant group (n = | Referent group | ||
| Resilient group (n = 136) | Not married | 0.80* | Resilient group (n = 199) | Deployed to AOC | 0.52 |
| Deployed to AOC | 0.92* | 10+ lifetime TEs | 1.54* | ||
| 4+ lifetime stressors | 0.51 | Low education | 0.83* | ||
| Increasing group (n = 93) | Not married | −0.16 | Constant (mild) group (n=55) | Deployed to AOC | 1.59* |
| Deployed to AOC | 0.13 | 10+ lifetime TEs | 2.04* | ||
| 4+ lifetime stressors | 0.69* | Low education | 0.78 | ||
| Chronic dysfunction group (n = 92) | Not married | −0.15 | Chronic dysfunction group (n = 22) | Deployed to AOC | 1.24 |
| Deployed to AOC | 1.02* | 10+ lifetime TEs | 3.17* | ||
| 4+ lifetime stressors | 1.37* | Low education | 1.01 | ||
Note.
p < .05
AOC= Area of Conflict; TE = Traumatic Event
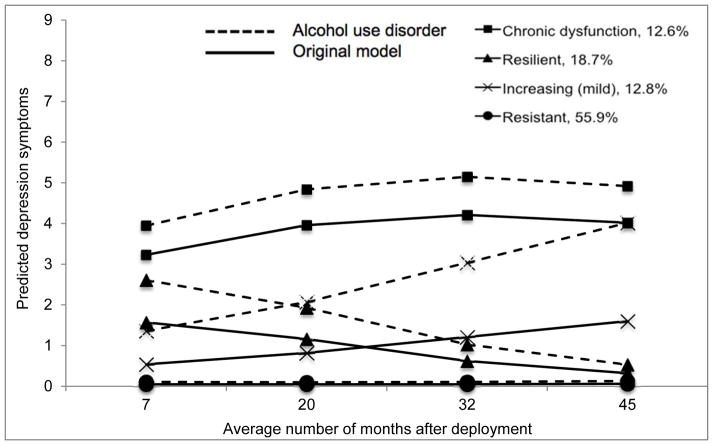
Figure 2 shows the potential effect of AUD on each trajectory (data points presented in Supplemental Table 3). The solid lines represent predicted trajectories of symptoms as they are in Figure 1. The dotted lines represent predicted trajectories of symptoms where past-year PTSD was set to a constant 0 but past-year AUD was set to 1 at every time point. AUD at each point resulted in an increase of the number of symptoms of depression overall. The group affected most by AUD was the mild increasing group (b = 0.92, p < .001). The gap between the predicted trajectories of the increasing group widened with time, while the resilient group showed a smaller gap between the two potential shapes as more time since deployment passed. The chronic dysfunction and resistant groups both showed the same general shape across time, with a small increase in symptoms.
Figure 2. Potential effect of AUD on depression symptoms from the PHQ-9 in the Depression Subsample.
Note. AUD = Alcohol Use Disorder; PHQ-9 = Nine-Item Patient Health Questionnaire
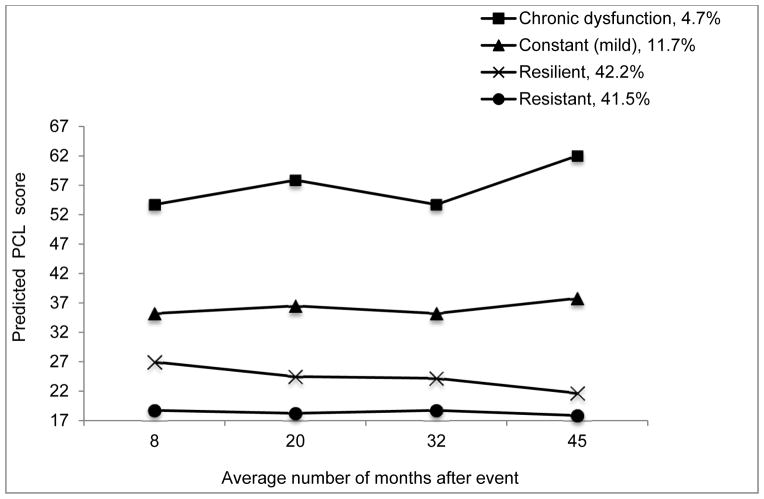
The means and standard deviations of the PCL at each eave were as follows: 28.92(13.68), 25.35(12.11), 24.44(12.42), and 24.93(13.93). We observed a resistant group (n = 196; 41.5%), a resilient group (n = 199; 42.2%), a mild constant group (n = 52; 11.7%), and a chronic dysfunction group (n = 22; 4.7%) for PTS. Figure 3 shows a graph of these predicted symptoms across the four time points (data points specified in Supplemental Table 4).
Figure 3. Predicted trajectories of PTS symptoms using PCL score.
Note. PTS = Posttraumatic Stress; PCL = Posttraumatic Stress Checklist
Table 3 presents covariates that were significant in the final PTS model, along with their corresponding beta estimates. Risk factors at baseline that were associated with group membership included education, PTEs, and AOC deployment. Reporting high lifetime PTEs was significantly associated with membership in the chronic dysfunction (unstandardized beta = 3.17, p = .003) and constant mild (unstandardized beta = 2.04, p < .001) groups. AOC deployment was significantly associated with membership in the mild constant group (unstandardized beta = 1.59, p = .001). Having low education was associated with membership into the resilient group (unstandardized beta = 0.83, p = .032). All of these comparisons are with reference to the resistant group.
Table 3.
Unstandardized Beta Estimates of Parameters and Time-varying Covariates by Subsample
| Latent group | Depression subsample (n = 727) | PTS subsample (n = 472) | |||
|---|---|---|---|---|---|
| Parameter | Estimate | Parameter | Estimate | ||
| Resistant group (n = 406) | Linear | −0.03 | Resistant group (n = 196) | Alcohol use disorder | 6.11* |
| Quadratic | 0.00* | Depression | 3.57* | ||
| Alcohol use disorder | 0.75* | Cumulative TE | −1.86 | ||
| PTSD | 3.74* | ||||
| Resilient group (n = 136) | Linear | 0.01 | Resilient group (n = 199) | Linear | −0.15* |
| Quadratic | 0.00* | Alcohol use disorder | 5.28* | ||
| Alcohol use disorder | 0.51* | Depression | 8.32* | ||
| PTSD | 1.41* | Cumulative TE | −1.30 | ||
| Increasing group (n = 93) | Linear | 0.03* | Constant (mild) group (n=55) | Alcohol use disorder | 9.45* |
| Alcohol use disorder | 0.92* | Depression | 14.02* | ||
| PTSD | −1.99* | Cumulative TE | 1.30 | ||
| Chronic dysfunction group (n = 92) | Linear | 0.03 | Chronic dysfunction group (n = 22) | Alcohol use disorder | 5.72 |
| Quadratic | 0.00 | Depression | 9.65* | ||
| Cubic | 0.00 | Cumulative TE | 4.17* | ||
| Alcohol use disorder | 0.20* | 4+ lifetime stressors | 1.37* | ||
| PTSD | 0.40* | ||||
Note.
p < .05
PTSD = Posttraumatic Stress Disorder; TE = Traumatic Event(s)
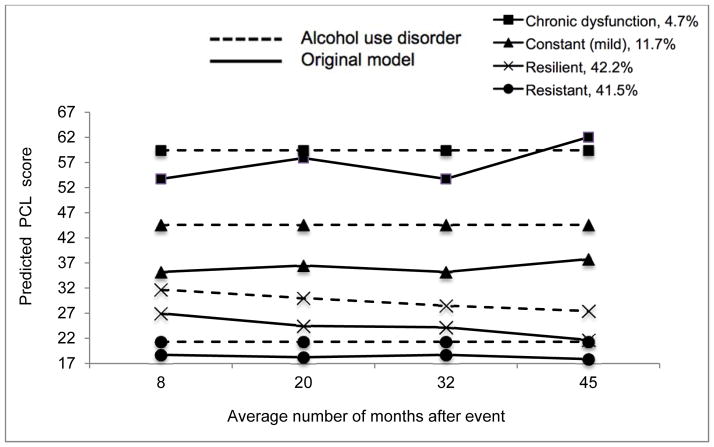
AUD, cumulative P=TEs, and past-year depression were all significantly associated with trajectory shape. Figure 4 shows the potential effect of AUD on PTS trajectories (data points are specified in Supplemental Table 5). Holding other time-varying covariates constant and setting AUD as positive at each time point flattened out the slope of all trajectory groups and produced elevated symptoms for all groups. The mild constant group showed the largest increase (b = 9.45, p < .001 for AUD).
Figure 4. Potential effect of AUD on PTS symptoms using PCL score.
Note. AUD = Alcohol Use Disorder; PTS = Posttraumatic Stress; PCL = Posttraumatic Stress Checklist
Discussion
Using data from a sample of National Guard service members followed across four years after deployment, discrete mixture modeling documented four trajectory groups of both depression and PTS. For both outcomes, the majority of respondents fell into one of the two lowest-symptom groups, supporting previous studies that people are modally resistant to trauma (Bonanno, 2004; Bonanno et al., 2012; Lowe et al., 2014; Nandi et al., 2009). Both Lowe (Lowe et al., 2014) and Bonanno (Bonanno et al., 2012), using non-military samples exposed to PTE experiences, estimated four groups for PTS as well, including a consistently low-level symptom group and a chronically high group with similar proportions of respondents in each group compared with our findings. Our study is the first, as far as we are aware, to have shown similar findings in a sample of U.S. military personnel.
We found that a high number of lifetime stressful events was associated with higher-symptom trajectory group membership for depression. Stressful events have been widely known to contribute to poor mental health symptoms in the military (Nash et al., 2010). Our finding that being nonmarried was associated with resilience might be explained by a lack of relationship/family stress, which has been shown to contribute to depression outcomes, particularly in military populations (Gibbs, Clinton-Sherrod, & Johnson, 2012; Martin et al., 2013).
For both trajectory outcomes, we found that soldiers deployed to an AOC were more likely to be in the chronic dysfunction groups. This is consistent with Hoge’s findings that service members returning from Iraq or Afghanistan were more likely to have mental health problems compared to those deployed to other locations (Hoge et al., 2006).
For PTS, we found that experiencing more lifetime TEs was associated with membership in higher-symptom trajectory groups, which agrees with civilian trajectories research (Lowe et al., 2014; Nandi et al., 2009), as was low education.
AUD at all time points was associated with an increase in both depression and PTS symptoms, with the largest effect seen on the already higher-symptom trajectory groups. For the increasing depression symptom group, the gap between the original predicted trajectory and that with AUD present increased over time, suggesting that the addition of AUD contributed to a steeper increase in symptoms among those with increasing symptoms as more time passed since their initial deployment. In contrast, the depression-resilient group actually showed a smaller gap between the two potential shapes as more time from their deployment passed, suggesting that resilience toward depression symptoms after a deployment experience may put individuals in a better position to be resilient to the effect of AUD on depression as well. Similarly, AUD had the smallest effect on the resistant group for PTS, suggesting that if a respondent reports consistently low PTS symptoms after a potentially traumatic event, the addition of AUD is not likely to change this outcome. In contrast, respondents who are already affected by PTS symptoms are more likely to worsen even more with co-occurring AUD.
These findings that AUD exacerbates both depression and PTS symptom trajectories build on previous literature that comorbidity can substantially, adversely affect outcomes in already vulnerable populations (Campbell et al., 2007; Guadiano & Zimmerman, 2010; J. P. Smith, 2012). Our findings also illustrate how the cumulative effect of AUD may manifest in a higher burden of psychopathology at multiple time points across the study period. This is especially important considering that AUD has been documented as a modifiable risk factor in U.S. service members (Pemberton et al., 2011).
Two principal limitations must be considered in interpreting our findings. First, although this is a longitudinal study and we have estimates of AUD, depression and PTS at every time point, we cannot make any statements about direction or causation; it is possible that high depression/PTS symptoms lead to AUD, not the reverse.
Second, there was loss to follow-up across the four years of our study, requiring additional recruitment. However, this concern is mitigated by a few observations: (a) attrition is a problem in most large-scale military cohorts like ours (Littman et al., 2010), including in another trajectory study (Boasso, Steenkamp, Nash, Larson, & Litz, 2015), particularly due to the fact that the military is a young and mobile population (Bush, Sheppard, Fantelli, Bell, & Reger, 2013); (b) the Proc Traj SAS procedure estimates missing data points using available data (Jones et al., 2001; Nagin, 2009); and (c) loss to follow-up in our samples was not associated with PTS or depression at baseline. Future longitudinal studies should aim to minimize attrition, as there are so few long-term military studies that keep participation rates constant across time. Additionally, longitudinal military studies should employ latent class analysis in order to allow for more comparison between studies. One direction could be to model AUD as an outcome, or to investigate other outcomes such as generalized anxiety. If a study has a large enough sample, it may be illuminating to observe the differences between male and female service members’ trajectories.
Despite limitations, our findings suggest a longitudinal perspective is critical when investigating psychopathology in service members. This is particularly important currently given that a greater proportion of service members are returning home with mental health burdens compared with past conflicts (Institute of Medicine Committee on the Initial Assessment of Readjustment Needs of Military Personnel & Their, 2010). Finally, the role of AUD is of utmost importance in understanding longer-term psychopathology, as it modifies trajectories of depression and PTS.
Supplementary Material
Acknowledgments
This work was supported by the Office of the Assistant Secretary of Defense for Health Affairs through the Joint Warfighter Medical Research Program under Award No. W81XWH-15-1-0080. Opinions, interpretations, conclusions and recommendations are those of the author and are not necessarily endorsed by the Department of Defense. The U.S. Army Medical Research Acquisition Activity, 820 Chandler Street, Fort Detrick MD 21702-5014 is the awarding and administering acquisition office.
We would also like to acknowledge the following funding: Department of Defense Congressionally Directed Medical Research Program W81XWH-07-1-0409, the “Combat Mental Health Initiative.”
David S. Fink would like to acknowledge the following funding: National Institute of Drug Abuse (NIDA) (D.S.F., grant number T32DA031099)
References
- Andruff N, Thompson A, Gaudreau PBL. Latent class growth modelling: a tutorial. Tutorials in Quantitative Methods for Psychology. 2009;51(1):11–24. [Google Scholar]
- Blanchard EB, Jones-Alexander J, Buckley TC, Forneris CA. Psychometric properties of the PTSD Checklist (PCL) Behav Res Ther. 1996;34(8):669–673. doi: 10.1016/0005-7967(96)00033-2. [DOI] [PubMed] [Google Scholar]
- Boasso AM, Steenkamp MM, Nash WP, Larson JL, Litz BT. The Relationship Between Course of PTSD Symptoms in Deployed U.S. Marines and Degree of Combat Exposure. J Trauma Stress. 2015;28(1):73–78. doi: 10.1002/jts.21988. [DOI] [PubMed] [Google Scholar]
- Bonanno GA. Loss, Trauma, and Human Resilience: Have We Underestimated the Human Capacity to Thrive After Extremely Aversive Events? American Psychologist. 2004;59(1):20–28. doi: 10.1037/0003-066X.59.1.20. [DOI] [PubMed] [Google Scholar]
- Bonanno GA, Mancini AD, Horton JL, Powell TM, Leardmann CA, Boyko EJ, Smith TC. Trajectories of trauma symptoms and resilience in deployed U.S. military service members: prospective cohort study. Br J Psychiatry. 2012;200(4):317–323. doi: 10.1192/bjp.bp.111.096552. [DOI] [PubMed] [Google Scholar]
- Bray RM, Pemberton MR, Lane ME, Hourani LL, Mattiko MJ, Babeu LA. Substance use and mental health trends among U.S. military active duty personnel: key findings from the 2008 DoD Health Behavior Survey. Mil Med. 2010;175(6):390–399. doi: 10.7205/MILMED-D-09-00132. [DOI] [PubMed] [Google Scholar]
- Breslau N, Kessler RC, Chilcoat HD, Schultz LR, Davis GC, Andreski P. Trauma and posttraumatic stress disorder in the community: The 1996 detroit area survey of trauma. Archives of General Psychiatry. 1998;55(7):626–632. doi: 10.1001/archpsyc.55.7.626. [DOI] [PubMed] [Google Scholar]
- Bush NE, Sheppard SC, Fantelli E, Bell KR, Reger MA. Recruitment and attrition issues in military clinical trials and health research studies. Mil Med. 2013;178(11):1157–1163. doi: 10.7205/milmed-d-13-00234. [DOI] [PubMed] [Google Scholar]
- Calabrese JR, Prescott M, Tamburrino M, Liberzon I, Slembarski R, Goldmann E, Galea S. PTSD comorbidity and suicidal ideation associated with PTSD within the Ohio Army National Guard. Journal of Clinical Psychiatry. 2011;72(8):1072–1078. doi: 10.4088/JCP.11m06956. [DOI] [PubMed] [Google Scholar]
- Campbell DG, Felker BL, Liu CF, Yano EM, Kirchner JE, Chan D, Chaney EF. Prevalence of depression-PTSD comorbidity: implications for clinical practice guidelines and primary care-based interventions. J Gen Intern Med. 2007;22(6):711–718. doi: 10.1007/s11606-006-0101-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen GH, Fink DS, Sampson L, Galea S. Mental health among Reserve Component military service members and veterans. Epidemiologic Reviews. 2015 doi: 10.1093/epirev/mxu007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diagnostic and Statistical Manual of Mental Disorders. 4. Washington, DC: American Psychiatric Association; 2000. Fourth Edition (DSM-IV) text rev. [DOI] [Google Scholar]
- Duma SJ, Reger MA, Canning SS, McNeil JD, Gahm GA. Longitudinal mental health screening results among postdeployed U.S. soldiers preparing to deploy again. J Trauma Stress. 2010;23(1):52–58. doi: 10.1002/jts.20484. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Non-patient Edition. (SCID-I/NP) New York, NY: Biometrics Research, New York State Psychiatric Institute; 2002. [Google Scholar]
- Gibbs DA, Clinton-Sherrod AM, Johnson RE. Interpersonal conflict and referrals to counseling among married soldiers following return from deployment. Mil Med. 2012;177(10):1178–1183. doi: 10.7205/MILMED-D-12-00008. [DOI] [PubMed] [Google Scholar]
- Gray MJ, Litz BT, Hsu JL, Lombardo TW. Psychometric properties of the life events checklist. Assessment. 2004;11(4):330–341. doi: 10.1177/1073191104269954. [DOI] [PubMed] [Google Scholar]
- Guadiano BA, Zimmerman M. Does Comorbid Posttraumatic Stress Disorder Affect the Severity and Course of Psychotic Major Depression? J Clin Psychiatry. 2010;71(4):442–450. doi: 10.4088/JCP.08m04794gre. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoge CW, Auchterlonie JL, Milliken CS. Mental health problems, use of mental health services, and attrition from military service after returning from deployment to Iraq or Afghanistan. JAMA. 2006;295(9):1023–1032. doi: 10.1001/jama.295.9.1023. [DOI] [PubMed] [Google Scholar]
- Their F. Institute of Medicine Committee on the Initial Assessment of Readjustment Needs of Military Personnel, V. Returning Home from Iraq and Afghanistan: Preliminary Assessment of Readjustment Needs of Veterans, Service Members, and Their Families. Washington (DC): National Academies Press (US); 2010. Copyright 2010 by the National Academy of Sciences. All rights reserved. [PubMed] [Google Scholar]
- Jones BL, Nagin DS, Roeder K. A SAS procedure based on mixture models for estimating developmental trajectories. Sociological Methods & Research. 2001;29(3):374–393. doi: 10.1177/0049124101029003005. [DOI] [Google Scholar]
- Jung T, Wickrama KAS. An introduction to latent class growth analysis and growth mixture modeling. Social and Personality Psychology Compass. 2008:302–317. doi: 10.1111/j.1751-9004.2007.00054.x. [DOI] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- King LA, King DW, Vogt DS, Knight J, Samper RE. Deployment Risk and Resilience Inventory: A Collection of Measures for Studying Deployment-Related Experiences of Military Personnel and Veterans. Military Psychology. 2006;18(2):89–120. doi: 10.1207/s15327876mp1802_1. [DOI] [Google Scholar]
- Kok BC, Herrell RK, Thomas JL, Hoge CW. Posttraumatic stress disorder associated with combat service in Iraq or Afghanistan: reconciling prevalence differences between studies. J Nerv Ment Dis. 2012;200(5):444–450. doi: 10.1097/NMD.0b013e3182532312. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Littman AJ, Boyko EJ, Jacobson IG, Horton J, Gackstetter GD, Smith B, Smith TC. Assessing nonresponse bias at follow-up in a large prospective cohort of relatively young and mobile military service members. BMC Med Res Methodol. 2010;10:99. doi: 10.1186/1471-2288-10-99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lowe SR, Galea S, Uddin M, Koenen KC. Trajectories of posttraumatic stress among urban residents. Am J Community Psychol. 2014;53(1–2):159–172. doi: 10.1007/s10464-014-9634-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin JS, Ghahramanlou-Holloway M, Englert DR, Bakalar JL, Olsen C, Nademin EM, Branlund S. Marital status, life stressor precipitants, and communications of distress and suicide intent in a sample of United States Air Force suicide decedents. Arch Suicide Res. 2013;17(2):148–160. doi: 10.1080/13811118.2013.776456. [DOI] [PubMed] [Google Scholar]
- Milliken CS, Auchterlonie JL, Hoge CW. Longitudinal assessment of mental health problems among active and reserve component soldiers returning from the Iraq war. JAMA. 2007;298(18):2141–2148. doi: 10.1001/jama.298.18.2141. [DOI] [PubMed] [Google Scholar]
- Nagin D, Tremblay RE. Trajectories of boys’ physical aggression, opposition, and hyperactivity on the path to physically violent and nonviolent juvenile delinquency. Child Dev. 1999;70(5):1181–1196. doi: 10.1111/1467-8624.00086. [DOI] [PubMed] [Google Scholar]
- Nagin DS. Group-Based Modeling of Development. Cambridge, MA: Harvard University Press; 2009. [Google Scholar]
- Nandi A, Tracy M, Beard JR, Vlahov D, Galea S. Patterns and predictors of trajectories of depression after an urban disaster. Ann Epidemiol. 2009;19(11):761–770. doi: 10.1016/j.annepidem.2009.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nash WP, Vasterling J, Ewing-Cobbs L, Horn S, Gaskin T, Golden J, Baker DG. Consensus recommendations for common data elements for operational stress research and surveillance: report of a federal interagency working group. Arch Phys Med Rehabil. 2010;91(11):1673–1683. doi: 10.1016/j.apmr.2010.06.035. [DOI] [PubMed] [Google Scholar]
- Norris FH, Tracy M, Galea S. Looking for resilience: understanding the longitudinal trajectories of responses to stress. Soc Sci Med. 2009;68(12):2190–2198. doi: 10.1016/j.socscimed.2009.03.043. [DOI] [PubMed] [Google Scholar]
- Pemberton MR, Williams J, Herman-Stahl M, Calvin SL, Bradshaw MR, Bray RM, Mitchell GM. Evaluation of two web-based alcohol interventions in the U.S. military. J Stud Alcohol Drugs. 2011;72(3):480–489. doi: 10.15288/jsad.2011.72.480. [DOI] [PubMed] [Google Scholar]
- Pietrzak RH, Van Ness PH, Fried TR, Galea S, Norris FH. Trajectories of posttraumatic stress symptomatology in older persons affected by a large-magnitude disaster. J Psychiatr Res. 2013;47(4):520–526. doi: 10.1016/j.jpsychires.2012.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prescott MR, Tamburrino M, Calabrese JR, Liberzon I, Slembarski R, Shirley E, Galea S. Validation of lay-administered mental health assessments in a large Army National Guard cohort. Int J Methods Psychiatr Res. 2014;23(1):109–119. doi: 10.1002/mpr.1416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramchand R, Schell TL, Karney BR, Osilla KC, Burns RM, Caldarone LB. Disparate prevalence estimates of PTSD among service members who served in Iraq and Afghanistan: possible explanations. J Trauma Stress. 2010;23(1):59–68. doi: 10.1002/jts.20486. [DOI] [PubMed] [Google Scholar]
- Tanielian T, Jaycox LH, editors. RAND. Invisible wounds of war: Psychological and cognitive injuries, their consequences, and services to assist recovery. Santa Monica, CA: RAND Corporation; 2008. [Google Scholar]
- SAS 9.4 Software (Version 9.4) Cary, North Carolina: SAS Institute Inc; 2013. [Google Scholar]
- Schaller EK, Woodall KA, Lemus H, Proctor SP, Russell DW, Crum-Cianflone NF. A Longitudinal Comparison of Posttraumatic Stress Disorder and Depression Among Military Service Components. Military Psychology. 2014;26(2):77–87. doi: 10.1037/mil0000034. [DOI] [Google Scholar]
- Schumm JA, Chard KM. Alcohol and stress in the military. Alcohol Res. 2012;34(4):401–407. [PMC free article] [PubMed] [Google Scholar]
- Seal KH, Metzler TJ, Gima KS, Bertenthal D, Maguen S, Marmar CR. Trends and risk factors for mental health diagnoses among Iraq and Afghanistan veterans using Department of Veterans Affairs health care, 2002–2008. Am J Public Health. 2009;99(9):1651–1658. doi: 10.2105/ajph.2008.150284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, Dunbar GC. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59(Suppl 20):22–33. quiz 34–57. [PubMed] [Google Scholar]
- Smith JP. Anxiety and Alcohol Use Disorders: Comorbidity and Treatment Considerations. Alcohol Res. 2012;34(4):414–431. [PMC free article] [PubMed] [Google Scholar]
- Smith TC, Ryan MA, Wingard DL, Slymen DJ, Sallis JF, Kritz-Silverstein D. New onset and persistent symptoms of post-traumatic stress disorder self reported after deployment and combat exposures: prospective population based US military cohort study. BMJ. 2008;336(7640):366–371. doi: 10.1136/bmj.39430.638241.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas JL, Wilk JE, Riviere LA, McGurk D, Castro CA, Hoge CW. Prevalence of mental health problems and functional impairment among active component and National Guard soldiers 3 and 12 months following combat in Iraq. Arch Gen Psychiatry. 2010;67(6):614–623. doi: 10.1001/archgenpsychiatry.2010.54. [DOI] [PubMed] [Google Scholar]
- Wells TS, LeardMann CA, Fortuna SO, Smith B, Smith TC, Ryan MA, Blazer D. A prospective study of depression following combat deployment in support of the wars in Iraq and Afghanistan. Am J Public Health. 2010;100(1):90–99. doi: 10.2105/ajph.2008.155432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xue C, Ge Y, Tang B, Liu Y, Kang P, Wang M, Zhang L. A Meta-Analysis of Risk Factors for Combat-Related PTSD among Military Personnel and Veterans. PLoS ONE. 2015;10(3):e0120270. doi: 10.1371/journal.pone.0120270. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.