Abstract
Background
Long-term survival after lung transplantation remains poor, yet modifiable risk factors for late-term morbidity and mortality have yet to be identified. Because psychiatric disorders increase risk for poor health outcomes in many non-transplant chronic disease populations, lung recipients with depression or anxiety before or early post-transplant may be at heightened risk for late-term transplant-related morbidity and mortality.
Methods
Among 178 patients from a prospective study of mental health after lung transplantation, we identified 1-year survivors and examined whether they experienced major depression or anxiety disorders during that year as well as before transplantation. We used multivariable Cox regression to examine the relationship between these disorders and risk for subsequent bronchiolitis obliterans syndrome (BOS), mortality and graft loss for up to 15 years post-transplant, controlling for other known risk factors for the outcomes.
Results
155 recipients were studied. Recipients with post-transplant depression had an elevated risk of BOS (HR, 1.91; 95%CI, 1.10,3.31), patient death (HR, 1.65; 95%CI, 1.01,2.71) and graft loss (HR, 1.75; 95%CI, 1.06,2.88). A trend toward reduced risk of BOS was observed in recipients with post-transplant anxiety (HR, 0.61; 95%CI, .37,1.00). Neither pre-transplant disorder was related to risk for any outcome.
Conclusions
Early post-transplant depression increases risk for long-term transplant-related morbidity and mortality. Screening to identify depression should therefore be routine in post-transplant care. Although anxiety was not significantly associated with poor outcomes, screening for post-transplant anxiety should also be routine, to reduce patient distress. Research is needed to better understand mechanisms underlying depression-outcome associations.
Keywords: lung transplantation, survival, BOS, depression, anxiety
Introduction
Despite improvements in long-term survival after lung transplantation, lung recipients continue to have the highest morbidity and mortality of all solid organ recipients (1). Only half of lung recipients survive to 5 years post-transplant; by 10 years, this rate drops to 31% (1,2). Chronic rejection, manifested as bronchiolitis obliterans syndrome (BOS), is prevalent and remains the major obstacle to long-term survival (2-4). Identifying reliable risk factors for BOS is thus a necessary step toward optimizing patient survival. Although clinical predictors of BOS as well as long-term survival have been identified (5-7), few of those identified to date are currently preventable or modifiable.
Psychosocial risk factors – which are often modifiable through preventive interventions and treatment – may also have key roles in predicting these outcomes in lung recipients. Among such factors, psychiatric characteristics, in particular, warrant investigation as potential predictors given their association with poor outcomes in a range of non-transplant general medical illness and chronic disease populations (8-15). Moreover, the high prevalence of depression and anxiety disorders among lung recipients during the first several years post-transplant (occurring in up to 30% of recipients) (16-19) underscores their potential importance as risk factors for poor outcomes.
However, psychiatric disorders have often only been considered as outcomes rather than risk factors for health and survival in transplant recipients. The scant evidence from existing studies that explore the role of psychiatric disorders as risk factors for medical outcomes in transplant populations is mixed and inconsistent (20-36). In lung transplant populations, the evidence is especially slim and appears inconsistent depending on whether morbidity or mortality outcomes are considered (32-37). Furthermore, lung recipient studies have generally focused on the first few years post-transplant. To date, no studies have examined the specific impact of psychiatric disorders on morbidity and mortality over a long-term follow-up period.
We sought to determine whether depression or anxiety disorders occurring before or during the first year after transplant increased subsequent risk for transplant-related morbidity and mortality during the period up to 15 years after lung transplantation. We considered not only psychiatric history before transplant, but also disorders present during the first year after transplant because this latter period is the time during which post-transplant depression and anxiety are most likely to emerge (19,38). The outcomes we examined – time to BOS onset, patient mortality and graft loss – are common metrics used to determine transplant success.
Materials and Methods
Study Population
We prospectively enrolled 178 adults (aged ≥18 years) receiving their first lung transplant between November 1999 and August 2004 in the Cardiothoracic Transplantation Program, University of Pittsburgh Medical Center. The cohort has been described previously (19). Ninety-five percent of all individuals transplanted during this timeframe agreed to enroll. The eligibility criterion was survival beyond the post-transplant surgical recovery period (defined as the first 6 weeks after surgery). Ten recipients (5.6%) died within 1 year of transplantation and were excluded from the present analyses because a goal was to ascertain whether psychiatric disorders during the first year post-transplant predicted subsequent outcomes. Three of these recipients endorsed post-transplant depression at a study interview before their death; 8 and 3, respectively, had depression and anxiety, pre-transplant. Thirteen recipients (7.3%) did not complete the psychiatric assessments because they were too ill (n=2) or refused (n=11); all 13 survived the first year. There were no differences in demographic or transplant-related characteristics between this group of 13 recipients and those who completed study assessments. Our final cohort consisted of 155 lung transplant recipients whom we then followed prospectively for up to 15 years to ascertain study outcomes.
Data Collection
The University of Pittsburgh Institutional Review Board approved the prospective collection of both psychiatric interview and medical records data. Participants provided written informed consent. During the first year post-transplant, participants were interviewed at 2, 7 and 12 months to assess the history and presence of mood and anxiety disorders, as described below. Trained clinicians with advanced degrees in behavioral medicine fields conducted the interviews. Transplant-related medical characteristics and information on post-transplant clinical outcomes were obtained in annual reviews from recipients' medical records, with censoring at patient death or at the end date of August 15, 2014.
Demographic characteristics, transplant-related characteristics and medical comorbidities
Demographic characteristics (i.e., gender, age, race/ethnicity, education, income) were assessed at the initial interview. Transplant-related characteristics were ascertained from the medical record, including: transplant indication; single v. bilateral transplant; ischemia time of the donor graft; recipient/donor CMV mismatch; type of induction immunosuppression received; length of hospital stay for transplant surgery; and both acute cellular rejection (ACR) and airway inflammation (lymphocytic bronchiolitis, LB) occurring during the first year post-transplant, diagnosed by histologic examination of transbronchial or open lung biopsy specimens according to internationally established criteria (39). Other medical comorbidities were also ascertained from the medical record, including: insulin-dependent Type 2 diabetes; dialysis-dependent chronic kidney disease; and congestive heart failure. Whether each of these comorbidities occurred pre- or during the first year post-transplant was recorded.
Psychiatric disorders
Depression and anxiety disorders were diagnosed according to standard criteria from the Diagnostic and Statistical Manual of Mental Disorders, 4th Edition, Text Revision (DSM-IV-TR) (40). We used the Structured Clinical Interview for DSM-IV-TR (SCID) (41) to determine the presence of major depressive disorder and several anxiety disorders (panic disorder, post-traumatic stress disorder related to transplant [PTSD-T] and generalized anxiety disorder). The 2-month interview assessed disorders since the time of transplant, and the 7- and 12-month interviews covered the period since the previous assessment. The present study examined whether or not each disorder occurred at any time during the first year post-transplant. At the initial (2-month) interview, we also determined with the SCID whether recipients had a pre-transplant lifetime history of major depressive disorder, panic disorder or generalized anxiety disorder.
Outcomes
Three outcomes were considered: (1) onset of BOS, (2) patient survival and (3) graft survival. Medical record abstractors and outcome adjudicators were blinded to recipients' psychiatric status. The earliest date at which each outcome was present was recorded. The outcomes were defined as follows. The presence of BOS at grade ≥1 was determined according to internationally established criteria (39). Determinations were based on consensus decisions by 2 study investigators and a transplant pulmonologist using pulmonary function tests (PFTs) and medical records of clinical encounters. All recipients received PFTs and clinical follow-up according to the transplant center's standard post-transplant care protocol, including surveillance bronchoscopy with transbronchial biopsy and bronchoalveolar lavage, spirometry, physical examination and bloodwork. The surveillance protocol included follow-up (including PFTs) every 3-4 months during the first 2 years post-transplant. Beyond 2 years, all recipients received follow-up every 4-6 months, with PFTs and additional testing performed as clinically indicated. The date of the incidence of BOS was recorded. Patient survival was defined as time to patient death, with death date ascertained from the medical record. Graft survival was defined as time to graft loss by patient death or retransplantation.
Statistical Analysis
We used descriptive statistics to characterize the sample's demographic, transplant-related, and medical characteristics. To determine the impact of pre- and post-transplant psychiatric disorders on each outcome, we used multivariable Cox regression with data censoring due to patient death (for the BOS outcome) or end of follow-up. This approach allowed us to examine the unique impact of each psychiatric disorder while controlling for demographic, transplant-related and medical comorbidity covariates known to be associated with morbidity and mortality (2,42). This is important because, without controlling such covariates, any observed associations of psychiatric status with outcomes might be spurious, i.e., due to factors leading to both the psychiatric conditions and the outcomes of interest (43). For each outcome, one analysis was done to assess the impact of pre- and post-transplant major depression, and a separate analysis was done to assess the impact of pre- and post-transplant anxiety disorders. We performed separate analyses to examine depression history and anxiety history so that we could maintain an adequate ratio of respondents:predictors of at least 15:1 in the analyses (43), and because the rate of comorbid depression and anxiety was generally low, as discussed below. We assessed regression model assumptions for all models as appropriate (43). For all analyses, we required a p level <.05 to declare that a finding was statistically significant.
Results
Description of Study Sample
Demographic and transplant-related characteristics of our sample of 155 lung recipients are shown in Table 1. Our sample is similar to the international population of lung recipients transplanted during the same period in terms of gender, age, transplant indication and transplant type (2). Most patients received tacrolimus-based immunosuppression. Nearly half of all unilateral transplants were performed in recipients with chronic obstructive pulmonary disease/emphysema, and—mirroring the pattern of associations in ISHLT registry data during the years of transplant encompassed by our study (2)—indication for transplant and type of transplant were significantly associated (χ2(3)=45.9;p<.001). Median follow-up time was 12.1 years (range:10-14.7 years).
Table 1. Demographic, Transplant-Related and Psychiatric Characteristics of the Sample, n=155.
| Characteristic | % | (No.) |
|---|---|---|
| Demographic | ||
| Age, years, mean (SD) | 51.8 | (12.0) |
| Male | 49.0 | (76) |
| Caucasian | 94.8 | (147) |
| Less than high school education | 49.0 | (76) |
| Transplant-related | ||
| Years since transplant, median (IQR) | 12.1 | (10.8-13.2) |
| Indication for transplant | ||
| COPD/emphysema | 43.2 | (67) |
| Pulmonary fibrosis (including sarcoidosis and scleroderma) | 31.0 | (48) |
| Cystic fibrosis | 15.5 | (24) |
| Other | 10.3 | (16) |
| Bilateral lung transplanta | 45.2 | (70) |
| Total length of stay for transplant, days, median (IQR) | 21 | (12-35) |
| Ischemia time of donor graft, minutes, mean (SD) | 308.7 | (95.6) |
| Induction immunosuppression | ||
| Alemtuzumab | 30.3 | (47) |
| Daclizumab | 29.7 | (46) |
| Rabbit antithymocyte globulin | 18.7 | (29) |
| None | 21.3 | (33) |
| Maintenance immunosuppression | ||
| Tacrolimus | 87.1 | (135) |
| Cyclosporine | 12.9 | (50) |
| CMV mismatch (Recipient-/Donor+)b | 27.4 | (42) |
| Acute cellular rejection during first year post-transplant | 65.8 | (102) |
| Lymphocytic bronchiolitis during first year post-transplant | 25.8 | (40) |
| Medical comorbidities | ||
| Insulin-dependent Type 2 diabetes pre-transplant | 5.8 | (9) |
| Insulin-dependent Type 2 diabetes during first year post-transplant | 18.1 | (28) |
| Dialysis-dependent chronic kidney disease pre- or during the first year post-transplant | 0.0 | (0) |
| Congestive heart failure pre- or during the first year post-transplant | 0.0 | (0) |
| Psychiatric | ||
| Major depressive disorder | ||
| Pre-transplantc | 40.9 | (63) |
| Received pharmacologic treatment | 44.4 | (28) |
| During first year post-transplantd | 19.9 | (30) |
| Received pharmacologic treatment | 70.0 | (21) |
| Anxiety disordere | ||
| Pre-transplantc | 25.3 | (39) |
| Received pharmacologic treatment | 41.0 | (16) |
| During first year post-transplante | 26.5 | (40) |
| Received pharmacologic treatment | 57.6 | (23) |
Includes 4 heart-lung recipients
n=153 because there was missing information on 2 donors
n=154 because there was insufficient information to determine whether 1 recipient had pre-transplant disorders
n=151 because there was insufficient information to determine whether 3 recipients had post-transplant disorders
Pre-transplant, 6 recipients had panic disorder only, 9 had GAD only and 7 had both disorders. Post-transplant, 14 recipients had panic only, 1 had GAD only, 19 had PTSD-T only, 3 had panic and GAD, and 3 had panic and PTSD-T
Abbreviations: IQR, interquartile range; COPD, chronic obstructive pulmonary disease; A1AT, α-1-antitrypsin deficiency
Description of Psychiatric Disorders
Table 1 also shows the distribution of pre- and post-transplant depression and anxiety disorders in the sample. Over 40% (n=63) of the sample had a pre-transplant history of depression, and nearly 20% (n=30) had depression during the first year post-transplant. Of those with a pre-transplant history of depression, 36% experienced diagnosable depression during the first year post-transplant. Of those with depression post-transplant, 27% of cases were incident cases (i.e., occurring in individuals with no previous history of depression).
As noted in Table 1 (footnote e), the numbers of cases of individual anxiety disorders were relatively small; thus, we focus on whether recipients met criteria for any anxiety disorder. Table 1 shows that 25% (n=39) of the sample had a pre-transplant history of an anxiety disorder and 26% (n=40) had an anxiety disorder during the first year post-transplant. Of those with a pre-transplant history of anxiety, 44% experienced diagnosable anxiety during the first year post-transplant. Of those with anxiety post-transplant, 58% of cases were incident cases.
Comorbidity between depression and anxiety was relatively infrequent. Pre-transplant, 16% of the sample had histories of both types of disorders, and post-transplant, 7% met criteria for both types of disorders.
Prediction of Study Outcomes
BOS
For the BOS analysis, the sample excluded 3 recipients whose BOS preceded the depression and anxiety diagnoses during the first year post-transplant; this ensured that we examined the prospective impact of each psychiatric disorder. There were 106 cases of BOS. Risk of BOS was nearly doubled if recipients experienced post-transplant major depression (hazard ratio [HR], 1.91; 95% confidence interval [CI], 1.10,3.31; p=.021; see first column, Table 2), whereas risk of BOS was not reliably associated with pre-transplant depression (p>.05; Table 2). Fig. 1a depicts the association of post-transplant depression with BOS risk.
Table 2. Results from Cox Regression Analyses of Psychiatric Predictors of Outcomes.
| Outcome | |||||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| BOSa | Patient survival | Graft survival | |||||||
| Predictorsb | HR | 95% CI | p | HR | 95% CI | p | HR | 95% CI | p |
| Regression model including major depressive disorder | |||||||||
| Older age at tx | .99 | .97,1.02 | .656 | 1.02 | .98,1.04 | .463 | 1.00 | .97,1.03 | .950 |
| Unilateral tx | .77 | .44,1.34 | .350 | .66 | .36,1.19 | .165 | .64 | .36,1.15 | .135 |
| Indication for tx: COPDc | 1.34 | .86,2.01 | .196 | .94 | .60,1.47 | .797 | 1.07 | .69,1.64 | .772 |
| Ischemia time of graft | 1.00 | 1.00,1.01 | .557 | 1.00 | 1.00,1.01 | .737 | 1.00 | 1.00,1.01 | .475 |
| Induction with alemtuzumab | .63 | .39,1.03 | .064 | 1.00 | .61,1.63 | .992 | .82 | .51,1.33 | .424 |
| CMV mismatch (R–/D+) | – | – | – | .89 | .55,1.43 | .636 | .85 | .53,1.34 | .478 |
| Longer length of stay for tx | – | – | – | 1.01 | 1.01,1.01 | .014* | 1.01 | 1.01,1.01 | .006* |
| Acute cellular rejection in first year | 1.04 | .64,1.68 | .887 | – | – | – | – | – | – |
| Lymphocytic bronchiolitis in first year | .96 | .59,1.57 | .880 | – | – | – | – | – | – |
| Diabetes pre-tx or during first year | – | – | – | .57 | .34,.98 | .042* | .50 | .29,.85 | .010* |
| Pre-tx depression v. none | .83 | .53,1.30 | .427 | .82 | .52,1.29 | .388 | .78 | .51,1.22 | .277 |
| Post-tx depression v. none | 1.91 | 1.10,3.31 | .021* | 1.65 | 1.01,2.71 | .048* | 1.75 | 1.06,2.88 | .028* |
|
| |||||||||
| Regression model including anxiety disorders | |||||||||
| Older age at tx | .99 | .97,1.02 | .647 | 1.02 | .99,1.05 | .264 | 1.01 | .98,1.03 | .722 |
| Unilateral tx | .77 | .45,1.34 | .362 | .66 | .37,1.18 | .164 | .62 | .35,1.10 | .103 |
| Indication for tx: COPDc | 1.14 | .73,1.79 | .567 | .89 | .57,1.39 | .599 | .99 | .64,1.54 | .975 |
| Ischemia time of graft | 1.00 | 1.00,1.01 | .601 | 1.00 | 1.00,1.01 | .547 | 1.00 | 1.00,1.01 | .440 |
| Induction with alemtuzumab | .64 | .40,1.03 | .064 | .81 | .50,1.34 | .424 | .70 | .43,1.14 | .151 |
| CMV mismatch (R-/D+) | – | – | – | .88 | .55,1.40 | .583 | .86 | .54,1.35 | .507 |
| Longer length of stay for tx | – | – | – | 1.01 | 1.01,1.01 | .004* | 1.01 | 1.01,1.01 | .002** |
| Acute cellular rejection in first year | 1.13 | .70,1.82 | .616 | – | – | – | – | – | – |
| Lymphocytic bronchiolitis in first year | 1.10 | .68,1.80 | .689 | – | – | – | – | – | – |
| Diabetes pre-tx or during first year | – | – | – | .54 | .32,.93 | .026* | .48 | .28,.82 | .007** |
| Pre-tx anxiety | .99 | .63,1.58 | .975 | 1.17 | .74,1.84 | .495 | 1.05 | .67,1.65 | .818 |
| Post-tx anxiety | .61 | .37,1.00 | .050 | .96 | .60,1.53 | .854 | .84 | .53,1.34 | .471 |
p<.05,
p<.01
Excludes 3 recipients whose BOS preceded the depression or anxiety diagnosis during the first year post-transplant.
CMV mismatch, longer length of stay for tx and diabetes were not controlled in the BOS models because they have not been shown to impact risk of BOS, whereas they have been shown todirectly increase risk of mortality (2,53). Acute cellular rejection and lymphocytic bronchiolitis were controlled in the BOS models because they have been shown to increase risk of BOS, not risk of late-term mortality (2,5,7).
We could not examine each indication separately because there were too few cases in some subgroups. We report effects comparing the largest patient group (COPD/emphysema) to all other patients because inclusion of this dichotomous variable, along with all other predictors in the Cox models, allowed us to maintain a ratio of respondents: predictors of at least 15:1. As noted in the text, there was no interaction effect between indication for transplant and psychiatric disorders on risk for the outcomes. However, in an additional exploratory analysis, we included variables comparing (a) pulmonary fibrosis, (b) cystic fibrosis and (c) all other indications for transplant to a COPD/emphysema referent group in order to determine whether any interaction effects might then emerge. There was no evidence of any such effects.
Abbreviations: BOS, bronchiolitis obliterans syndrome; tx, transplant; COPD, chronic obstructive pulmonary disorder; CMV, cytomegalovirus; R, recipient; D, donor
Figure 1.
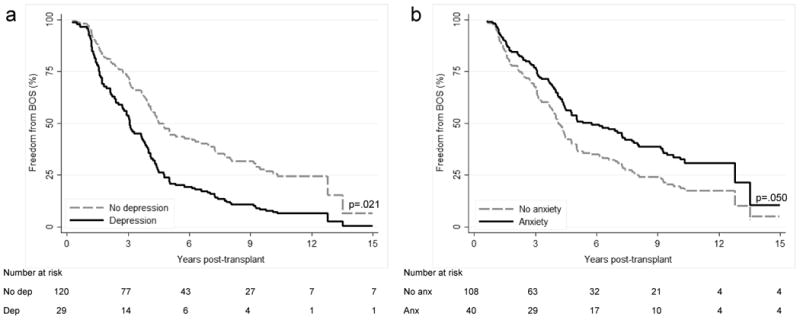
Cox regression curves depicting freedom from BOS in lung transplant recipients with and without (a) depression and (b) anxiety during the first year after transplant. p values refer to tests of significance between recipients with and without the psychiatric disorder. Abbreviations: dep, depression; anx, anxiety
There was a trend toward reduced risk of BOS in recipients with post-transplant anxiety (HR, 0.61; 95%CI, .37,1.00; p=.050) (Fig. 1b and Table 2, first column). Risk did not reliably vary between recipients with and without pre-transplant anxiety (p>.05, Table 2).
Patient survival
There were 107 deaths. The most common causes of death were graft failure (25%), infection (24%) and malignancy (21%), followed by pulmonary (11%), cardiovascular (3%) and cerebrovascular (3%) causes. The distribution of causes of death did not differ by psychiatric diagnosis (depression: χ2(6)=6.07, p=.414; anxiety: χ2(6)=3.70, p=.717). Risk of patient death was higher for recipients with post-transplant major depression than recipients without (HR, 1.65; 95%CI, 1.01,2.71; p=.048) (Fig. 2a), whereas risk of patient death did not differ between recipients with and without pre-transplant depression (p>.05, see second column, Table 2).
Figure 2.
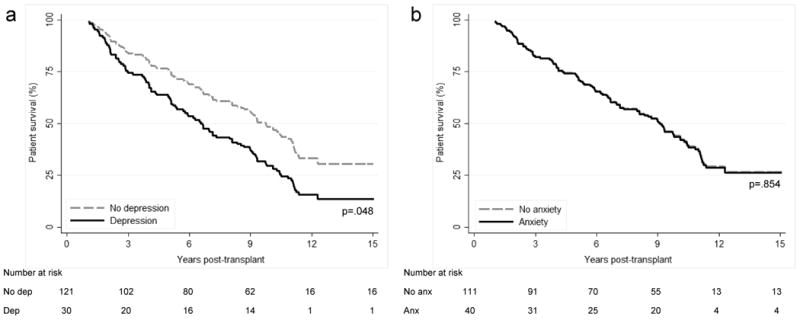
Cox regression curves depicting patient survival in lung transplant recipients with and without (a) depression and (b) anxiety during the first year after transplant. p values refer to tests of significance between recipients with and without the psychiatric disorder. Abbreviations: dep, depression; anx, anxiety
Risk of patient death was not related to post-transplant anxiety (HR, 0.96; 95%CI, 0.60,1.53; p=.854) (Fig. 2b and Table 2). Risk was also unrelated to pre-transplant anxiety (p>.05, Table 2).
Graft survival
There were 112 cases of graft loss. Risk of graft death was higher for recipients with post-transplant major depression than recipients without (HR, 1.75; 95%CI, 1.06,2.88; p=.028) (Fig 3a), whereas risk of graft loss did not differ as a function of pre-transplant depression history (p>.05, see third column, Table 2). Risk of graft loss also was not reliably related to post-transplant anxiety (HR, 0.84; 95%CI, 0.53,1.34; p=.471) (Fig. 3b). Pre-transplant anxiety did not affect risk of graft loss (p>.05, Table 2).
Figure 3.
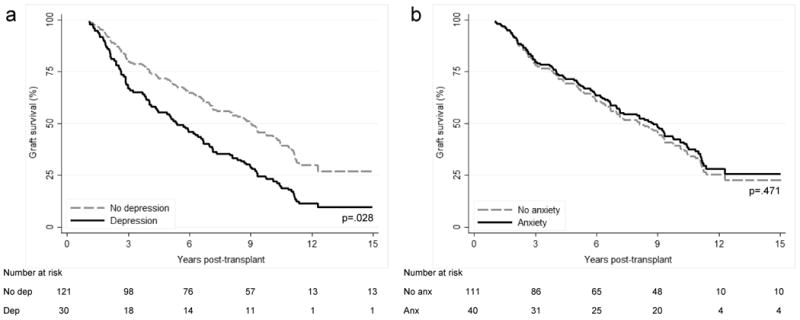
Cox regression curves depicting graft survival in lung transplant recipients with and without (a) depression and (b) anxiety during the first year after transplant. p values refer to tests of significance between recipients with and without the psychiatric disorder. Abbreviations: dep, depression; anx, anxiety
Of interest is whether the impact of either depression or anxiety varied depending on recipients' native lung disease. However, adding the interaction term for indication for transplant with each psychiatric predictor to the models for each outcome yielded consistently small and nonsigificant effects (see also Table 2, footnote c).
Discussion
Identifying modifiable predictors of poor outcomes is an important step toward reducing long-term morbidity and mortality in lung recipients. Although the link between psychiatric distress and mortality (and to a lesser extent, morbidity) has been studied in recipients of other solid organs, this issue has received little attention in lung recipients. The handful of existing studies in lung recipients have examined transplant-related morbidities as predictors of psychiatric distress (16,17,32), or pre-transplant or early post-transplant psychiatric symptoms as predictors of health outcomes mainly in the early years post-transplant (33-37). Findings from the latter studies have been inconsistent. Moreover, the vast majority examined relatively short follow-up periods post-transplant. Our study is the first to prospectively examine the impact of post-transplant psychiatric disorders on long-term morbidity and mortality in lung recipients, and its nearly 15-year follow-up is the longest follow-up period in studies of these risk factors to date. Studying the prospective impact of psychiatric disorders on transplant-related outcomes is a distinct and important question given that depression and anxiety are prevalent in lung recipients and are largely modifiable through medical and behavioral intervention.
Our main finding is that major depression during the first year post-transplant reliably increases risk for long-term morbidity and mortality. This is consistent with a large body of work in general medical illness and chronic disease populations (8-12). In transplant populations, studies have reported mixed findings on the link between depression in the early aftermath of transplant and mortality (20-25,29,37). However, our findings are consistent with the only other study to examine the impact of post-transplant depression among lung recipients (37): although Smith et al. focused on depressive symptom levels rather than diagnosable depressive disorder, they found that a greater depressive symptom level at 18 months post-transplant was associated with increased mortality risk during the next decade of follow-up.
The literature on the impact of depression on risk for morbidity in transplant recipients is even smaller and equally mixed (22,29-31). To our knowledge, only one study has examined the impact of post-transplant depression on subsequent morbidity in lung recipients, showing an association between depression and the development of BOS over the following year (33). Our finding thus adds an important sample to the growing body of literature suggesting that depression, particularly when present post-transplant, increases risk for morbidity and mortality.
Although the literature on anxiety and medical outcomes is smaller than that which focuses on depression, existing evidence suggests that anxiety also has a clinically important and harmful role in a range of non-transplant medical illnesses (13-15). However, the few studies in transplant populations have reported mixed findings: one relatively large study of heart recipients found strong links between post-transplant PTSD-T and mortality (31), whereas 3 other studies of heart recipients have not shown similar associations (24-26). As the first study to examine anxiety's impact in lung recipients, our findings are an important first step toward understanding whether post-transplant anxiety should be considered a risk factor for subsequent poor outcomes. Although we did not find a statistically significant (p<.05) relationship between post-transplant anxiety and patient or graft mortality, we observed a trend toward reduced risk of BOS in recipients with post-transplant anxiety. More work in this population is needed to reliably determine the direction and strength of any link between anxiety and medical outcomes.
It is notable that neither pre-transplant depression nor anxiety was associated with morbidity or mortality across our 15-year follow-up. The majority of recipients in our sample who had pre-transplant histories of psychiatric disorders did not experience episodes of these disorders during the first year post-transplant. Moreover, we observed cases of depression and anxiety post-transplant in individuals with no pre-transplant histories of such disorders. Taken together, all of these findings suggest that pre-transplant psychiatric status does not necessarily portend risk for poor medical outcomes or poor psychiatric functioning. Two (34,35) of three previous studies in lung recipients similarly observed no predictive impact of pre-transplant psychiatric status on post-transplant health, although their follow-up periods were considerably shorter (34-36). One explanation for why depression after but not before transplant in our cohort might have an impact on outcomes is that post-transplant depression is more proximal to the outcome and thus more likely to have a stronger effect. Another possible explanation is that recipients with depression pre-transplant may have sought mental health treatment before transplant and were therefore better prepared to cope with the stresses of transplantation. In any case, these findings suggest that a history of a psychiatric disorder before transplantation does not necessarily portend poorer post-transplant outcomes, which is an important consideration for candidate selection.
The question of whether psychiatric treatment can attenuate the risk of poor outcomes in recipients with depression is important. It is especially pertinent in light of evidence from liver recipients suggesting that adequate treatment of depression may improve outcomes (44). We have already described our cohort's patterns of help-seeking for psychiatric conditions (19): the majority of recipients with post-transplant depression and anxiety, 70% and 58%, respectively, had received pharmacologic treatment, whereas less than half of those with pre-transplant disorders had received such medications. Our sample size precludes definitive analyses of the impact of treatment receipt, but stratifying the sample with post-transplant depression by whether or not they received pharmacologic treatment does not suggest that receipt of medication was associated with improved survival. Similarly, we discerned no evidence of medication effects in recipients with anxiety disorders (although, again, our sample is underpowered for reliable interpretation). More broadly, although the high proportion of patients who received treatment for psychiatric disorders indicates that these disorders were often recognized by clinicians, we cannot discern whether untreated cases were actually undetected, or whether other clinical issues may have precluded or made pharmacologic treatment for these individuals more difficult.
Although our study was not designed to address the mechanisms underlying the links between post-transplant depression and subsequent morbidity and mortality (or the trend associating post-transplant anxiety with reduced risk of BOS), we were able to examine several behavioral elements that may have had a role in these pathways. Some evidence suggests that transplant recipients with psychiatric disorders, particularly depression, have poor medical adherence after transplant (45). However, previous analyses with the present cohort did not find evidence that recipients' pre- or post-transplant psychiatric status was associated with adherence levels, at least through the first 2 years post-transplant (adherence was not monitored beyond this time point) (46). Another possibility is that recipients with depression were less likely to request and subsequently undergo pulmonary biopsies and PFTs, which might have delayed detection and treatment of complications. Alternatively, those with anxiety may have been more vigilant regarding these issues. However, upon additional medical record reviews, we found that recipients' likelihood of undergoing these procedures was the same regardless of whether they experienced depression, anxiety or neither disorder. Furthermore, we have previously reported that recipients with and without psychiatric disorders did not differ in their number of missed clinic visits (46), suggesting that psychiatric status did not impact the consistency of post-transplant clinical follow-up in the first 2 years post-transplant.
Our study has several limitations. First, we report only a single-center experience. However, our findings are potentially generalizable because our cohort's clinical and demographic characteristics are similar to those of the international lung transplant population, and our center's protocol for surveillance biopsies and PFTs is similar to that used in other centers across the United States. Second, our selection of outcomes was limited to BOS, patient death and graft loss. Although these are among the most important outcomes for lung recipients, we were unable to examine two other major post-transplant outcomes: infections, because they are not consistently documented in our transplant center's medical record beyond the first few years post-transplant (i.e., patients may not return to our center for care of every infection), and malignancies, because too few cases occurred over our follow-up. Third, our estimates of depression's impact on risk for BOS were obtained from traditional Cox regression models in which cases without BOS who died before the end of follow-up were considered censored at the point of death. A competing hazards approach, modeling both time to death and time to BOS might have yielded different effects. However, traditional (non-competing hazards) models have been shown to perform well when the competing event (here, death in 29 cases before BOS onset) is infrequent relative to the event of interest (here, BOS observed in 106 cases; there were also 17 cases that did not have BOS and remained alive throughout follow-up) (47). A competing hazards approach was not feasible given our limited sample size, number of outcome events and numbers of cases of the psychiatric disorder (47,48).
A fourth study limitation is that, while our study design followed recipients prospectively after transplant, our assessment of pre-transplant psychiatric disorders was retrospective. Fifth, as noted earlier, we were unable to directly assess the impact of psychiatric treatment because our sample had too few cases of the disorders and our study collected limited information on the range of psychiatric interventions patients may have received (e.g., psychotherapy). Future work should attempt to determine whether treating psychiatric disorders, especially depression, attenuates the risk of poorer outcomes that we observed in recipients with early post-transplant depression. Future work should also strive to recruit large enough samples to examine any differential impact on risk for outcomes associated with depression occurring early v. later during the first year post-transplant, as well as in subsequent years. It would also be important to consider differential effects of depression based on patients' other transplant-related characteristics or medical comorbidities. For example, the combination of multiple medical comorbidities plus depression might have a synergistic effect, leading to poorer outcomes than either set of factors alone. Our study addressed the initial question of whether psychiatric status itself plays a key role in elevating risk but was not designed to address questions regarding complicated patterns of combined effects. Finally, our study was not designed to isolate the causal pathways underlying the link between psychiatric disorders and physical outcomes. It is clear that future exploration of mechanistic hypotheses – both behavioral and pathophysiologic – will be important for understanding this relationship and identifying potential targets for intervention.
In sum, major depression during the first year after transplant appears to be an important risk factor for poor long-term outcomes, nearly doubling the risk of BOS and increasing the risk of patient death and graft loss over 1.5-fold. This underscores the need to screen all recipients for psychiatric disorders after transplant, which is not currently standard practice in most transplant centers. Short and easy-to-administer screening instruments, such as Beck Depression Inventory-II (49), Patient Health Questionnaire-9 (50), Spielberger State-Trait Anxiety Inventory (51) or Generalized Anxiety Disorder-7 Scale (52), may be practical tools for transplant teams to use to identify cases to refer for more in-depth evaluation and treatment. Identifying and treating depression should be a major priority after transplant, not only because effective depression treatments exist but also because treating depression may be a means of preventing long-term morbidity and mortality. Although anxiety during the first year post-transplant does not appear to be associated with increased risk for morbidity and mortality, transplant teams should nonetheless screen for, monitor and treat anxiety as well, since it factors largely into quality of life. The opportunity for mental health screening and intervention during the first post-transplant year should not be missed, as this is when post-transplant psychiatric disorders are most likely to emerge (19,38) and when transplant teams have most contact with recipients. Heightened mental health surveillance during this critical period may yield benefits that ultimately extend beyond quality of life to improved post-transplant health over the long-term.
Acknowledgments
Funding: Preparation of this article was supported in part by Grant R01 MH59229 from the National Institute of Mental Health, Rockville, MD, and Grant TL1TR000145 from the National Center for Advancing Translational Sciences of the National Institutes of Health (NIH), Rockville, MD.
Abbreviations
- BOS
bronchiolitis obliterans syndrome
- DSM-IV-TR
Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision
- PTSD-T
post-traumatic stress disorder related to transplant
- PFTs
pulmonary function tests
Footnotes
Disclosure: The authors declare no conflicts of interest.
Contributor Information
Emily M. Rosenberger, Department of Clinical and Translational Science, University of Pittsburgh.
Andrea F. DiMartini, Departments of Psychiatry and Surgery, University of Pittsburgh.
Annette J. DeVito Dabbs, School of Nursing, University of Pittsburgh.
Christian A. Bermudez, Department of Surgery, University of Pittsburgh, Heart and Vascular Institute, University of Pittsburgh Medical Center.
Joseph M. Pilewski, Department of Medicine, Division of Pulmonary, Allergy, and Critical Care Medicine, University of Pittsburgh.
Yoshiya Toyoda, Department of Surgery, Temple University.
Mary Amanda Dew, Departments of Psychology, Epidemiology, Biostatistics, and Clinical and Translational Science, University of Pittsburgh.
References
- 1.OPTN/SRTR 2012 Annual Data Report: Lung. Am J Transplant. 2014;14:139. doi: 10.1111/ajt.12584. [DOI] [PubMed] [Google Scholar]
- 2.Yusen RD, Edwards LB, Kucheryavaya AY, et al. The Registry of the International Society for Heart and Lung Transplantation: thirty-first adult lung and heart-lung transplant report—2014; focus theme: retransplantation. J Heart Lung Transplant. 2014;33:1009. doi: 10.1016/j.healun.2014.08.004. [DOI] [PubMed] [Google Scholar]
- 3.Ahmad S, Shlobin OA, Nathan SD. Pulmonary complications of lung transplantation. Chest. 2011;139:402. doi: 10.1378/chest.10-1048. [DOI] [PubMed] [Google Scholar]
- 4.Song MK, DeVito Dabbs AJ, Studer SM, Zangle SE. Course of illness after the onset of chronic rejection in lung transplant recipients. Am J Crit Care. 2008;17:246. [PubMed] [Google Scholar]
- 5.Belperio JA, Weigt SS, Fishbein MC, Lynch JP., III Chronic lung allograft rejection: mechanisms and therapy. Proc Am Thorac Soc. 2009;6:108. doi: 10.1513/pats.200807-073GO. [DOI] [PubMed] [Google Scholar]
- 6.Davis WA, Finlen Copeland CA, Todd JL, Snyder LD, Martissa JA, Palmer SM. Spirometrically significant acute rejection increases the risk for BOS and death after lung transplantation. Am J Transplant. 2012;12:745. doi: 10.1111/j.1600-6143.2011.03849.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fiser SM, Tribble CG, Long SM, et al. Ischemia-reperfusion injury after lung transplantation increases risk of late bronchiolitis obliterans syndrome. Ann Thorac Surg. 2002;73:1041. doi: 10.1016/s0003-4975(01)03606-2. [DOI] [PubMed] [Google Scholar]
- 8.Dew MA, Cyranowski JM, Pilkonis PA. Medical conditions and depression. In: Ingramn RE, editor. The International Encyclopedia of Depression. New York: Springer; 2009. p. 375. [Google Scholar]
- 9.Eaton WW, Fogel J, Armenian HK. The consequences of psychopathology in the Baltimore Epidemiologic Catchment Area follow-up. In: Eaton WW, editor. Medical and Psychiatric Comorbidity Over the Course of Life. Washington, DC: American Psychiatric Publishing; 2006. p. 21. [Google Scholar]
- 10.Katon W, Lin EH, Kroenke K. The association of depression and anxiety with medical symptom burden in patients with chronic medical illness. Gen Hosp Psychiatry. 2007;29:147. doi: 10.1016/j.genhosppsych.2006.11.005. [DOI] [PubMed] [Google Scholar]
- 11.Stein MB, Cox BJ, Afifi TO, Belik SL, Sareen J. Does co-morbid depressive illness magnify the impact of chronic physical illness? A population-based perspective Psychol Med. 2006;36:587. doi: 10.1017/S0033291706007239. [DOI] [PubMed] [Google Scholar]
- 12.Sullivan MD, O'Connor P, Feeney P, et al. Depression predicts all-cause mortality: epidemiological evaluation from the ACCORD HRQL substudy. Diabetes Care. 2012;35:1708. doi: 10.2337/dc11-1791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Roy-Byrne PP, Davidson KW, Kessler RC, et al. Anxiety disorders and comorbid medical illness. Gen Hosp Psychiatry. 2008;30:208. doi: 10.1016/j.genhosppsych.2007.12.006. [DOI] [PubMed] [Google Scholar]
- 14.Sareen J, Cox BJ, Clara I, Asmundson GJ. The relationship between anxiety disorders and physical disorders in the U.S. National Comorbidity Survey. Depress Anxiety. 2005;21:193. doi: 10.1002/da.20072. [DOI] [PubMed] [Google Scholar]
- 15.Harter MC, Conway KP, Merikangas KR. Associations between anxiety disorders and physical illness. Eur Arch Psychiatry Clin Neurosci. 2003;253:313. doi: 10.1007/s00406-003-0449-y. [DOI] [PubMed] [Google Scholar]
- 16.Goetzmann L, Scheuer E, Naef R, et al. Psychosocial situation and physical health in 50 patients > 1 year after lung transplantation. Chest. 2005;127:166. doi: 10.1378/chest.127.1.166. [DOI] [PubMed] [Google Scholar]
- 17.van den Berg J, Geertsma A, van der Bij W, Koeter GH, et al. Bronchiolitis obliterans syndrome after lung transplantation and health-related quality of life. Am J Respir Crit Care Med. 2000;16:1937. doi: 10.1164/ajrccm.161.6.9909092. [DOI] [PubMed] [Google Scholar]
- 18.Corbett C, Armstrong MJ, Parker R, Webb K, Neuberger JM. Mental Health Disorders and Solid-Organ Transplant Recipients. Transplantation. 2013;96:593. doi: 10.1097/TP.0b013e31829584e0. [DOI] [PubMed] [Google Scholar]
- 19.Dew MA, DiMartini AF, DeVito Dabbs AJ, et al. Onset and risk factors for anxiety and depression during the first 2 years after lung transplantation. Gen Hosp Psychiatry. 2012;34:127. doi: 10.1016/j.genhosppsych.2011.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Corruble E, Barry C, Varescon I, Falissard B, Castaing D, Samuel D. Depressive symptoms predict long-term mortality after liver transplantation. J Psychosom Res. 2011;71:32. doi: 10.1016/j.jpsychores.2010.12.008. [DOI] [PubMed] [Google Scholar]
- 21.DiMartini A, Dew MA, Chaiffetz D, Fitzgerald MG, Devera ME, Fontes P. Early trajectories of depressive symptoms after liver transplantation for alcoholic liver disease predicts long-term survival. Am J Transplant. 2011;11:1287. doi: 10.1111/j.1600-6143.2011.03496.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Novak M, Molnar MZ, Szeifert L, et al. Depressive symptoms and mortality in patients after kidney transplantation: a prospective prevalent cohort study. Psychosom Med. 2010;72:527. doi: 10.1097/PSY.0b013e3181dbbb7d. [DOI] [PubMed] [Google Scholar]
- 23.Havik OE, Sivertsen B, Relbo A, et al. Depressive symptoms and all-cause mortality after heart transplantation. Transplantation. 2007;84:97. doi: 10.1097/01.tp.0000268816.90672.a0. [DOI] [PubMed] [Google Scholar]
- 24.Sirri L, Potena L, Masetti M, Tossani E, Magelli C, Grandi S. Psychological predictors of mortality in heart transplanted patients: a prospective, 6-year follow-up study. Transplantation. 2010;89:879. doi: 10.1097/TP.0b013e3181ca9078. [DOI] [PubMed] [Google Scholar]
- 25.Favaro A, Gerosa G, Caforio AL, et al. Posttraumatic stress disorder and depression in heart transplantation recipients: the relationship with outcome and adherence to medical treatment. Gen Hosp Psychiatry. 2011;33:1. doi: 10.1016/j.genhosppsych.2010.10.001. [DOI] [PubMed] [Google Scholar]
- 26.Owen JE, Bonds CL, Wellisch DK. Psychiatric evaluations of heart transplant candidates: predicting post-transplant hospitalizations, rejection episodes, and survival. Psychosomatics. 2006;47:213. doi: 10.1176/appi.psy.47.3.213. [DOI] [PubMed] [Google Scholar]
- 27.Rogal SS, Landsittel D, Surman O, et al. Pretransplant depression, antidepressant use, and outcomes of orthotopic liver transplantation. Liver Transpl. 2011;17:251. doi: 10.1002/lt.22231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Telles-Correia D, Barbosa A, Mega I, et al. Psychiatric and psychosocial predictors of medical outcome after liver transplantation: a prospective, single-center study. Transplant Proc. 2011;43:155. doi: 10.1016/j.transproceed.2010.12.006. [DOI] [PubMed] [Google Scholar]
- 29.Dobbels F, Skeans MA, Snyder JJ, et al. Depressive disorder in renal transplantation: an analysis of Medicare claims. Am J Kidney Dis. 2008;51:819. doi: 10.1053/j.ajkd.2008.01.010. [DOI] [PubMed] [Google Scholar]
- 30.Rocha G, Poli de Figueiredo CE, d'Avila D, Saitovitch D. Depressive symptoms and kidney transplant outcome. Transplant Proc. 2001;33:3424. doi: 10.1016/s0041-1345(01)02476-9. [DOI] [PubMed] [Google Scholar]
- 31.Dew MA, Kormos RL, Roth LH, Murali S, DiMartini A, Griffith BP. Early post-transplant medical compliance and mental health predict physical morbidity and mortality one to three years after heart transplantation. J Heart Lung Transplant. 1999;18:549. doi: 10.1016/s1053-2498(98)00044-8. [DOI] [PubMed] [Google Scholar]
- 32.Gries CJ, Dew MA, Curtis JR, et al. Nature and correlates of post-traumatic stress symptomatology in lung transplant recipients. J Heart Lung Transplant. 2013;32:525. doi: 10.1016/j.healun.2013.01.1046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Goetzmann L, Irani S, Schwegler K, Stamm M, et al. Distress and alexithymia in lung recipients – psychosocial strains and associations with chronic allograft dysfunction. Swiss Med Wkly. 2010;140:382. doi: 10.4414/smw.2010.12770. [DOI] [PubMed] [Google Scholar]
- 34.Vermeulen KM, Ten Vergert EM, Verschuuren EA, Erasmus ME, van der Bij W. Pre-transplant quality of life does not predict survival after lung transplantation. J Heart Lung Transplant. 2008;27:623. doi: 10.1016/j.healun.2008.03.011. [DOI] [PubMed] [Google Scholar]
- 35.Evon DM, Burker EJ, Galanko JA, Dedert E, Egan TM. Depressive symptoms and mortality in lung transplant. Clin Transplant. 2010;24:E201. doi: 10.1111/j.1399-0012.2010.01236.x. [DOI] [PubMed] [Google Scholar]
- 36.Woodman CL, Geist LJ, Vance S, et al. Psychiatric disorders and survival after lung transplantion. Psychosomatics. 1999;40:293. doi: 10.1016/S0033-3182(99)71221-1. [DOI] [PubMed] [Google Scholar]
- 37.Smith PJ, Blumenthal JA, Carney RM, et al. Neurobehavioral functioning and survival following lung transplantation. Chest. 2014;145:604. doi: 10.1378/chest.12-2127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Rosenberger EM, Dew MA, DiMartini AF, DeVito Dabbs AJ, Yusen RD. Psychosocial issues facing lung transplant candidates, recipients and family caregivers. Thorac Surg Clin. 2012;22:517. doi: 10.1016/j.thorsurg.2012.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Estenne M, Maurer JR, Boehler A, et al. Bronchiolitis obliterans syndrome 2001: an update of the diagnostic criteria. J Heart Lung Transplant. 2002;21:297. doi: 10.1016/s1053-2498(02)00398-4. [DOI] [PubMed] [Google Scholar]
- 40.American Psychological Association. Diagnostic and statistical manual of mental disorders. 4th. Washington, DC: American Psychiatric Press, Inc.; 2000. [Google Scholar]
- 41.First MB, Spitzer RL, Gibbon M, Williams JBW. Structured clinical interview for DSM-IV axis I disorders, clinician version (SCID-CV) Washington, DC: American Psychiatric Press, Inc; 1996. revised 2002. [Google Scholar]
- 42.Shyu S, Dew MA, Pilewski JM, et al. Five-year outcomes with alemtuzumab induction after lung transplantation. J Heart Lung Transplant. 2011;30:743. doi: 10.1016/j.healun.2011.01.714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Tabachnick BG, Fidell LS. Using multivariate statistics. 6th. Boston: Pearson; 2012. [Google Scholar]
- 44.Rogal SS, Dew MA, Fontes P, DiMartini AF. Early treatment of depressive symptoms and long-term survival after liver transplantation. Am J Transplant. 2013;13(4):928–35. doi: 10.1111/ajt.12164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Dobbels F, Vanhaecke J, Dupont L, et al. Pretransplant predictors of posttransplant adherence and clinical outcome: an evidence base for pretransplant psychosocial screening. Transplantation. 2009;87:1497. doi: 10.1097/TP.0b013e3181a440ae. [DOI] [PubMed] [Google Scholar]
- 46.Dew MA, DiMartini AF, DeVito Dabbs AJ, et al. Adherence to the medical regimen during the first two years after lung transplantation. Transplantation. 2008;85:193. doi: 10.1097/TP.0b013e318160135f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Dignam JJ, Kocherginsky MN. Choice and interpretation of statistical tests used when competing risks are present. Journal of Clinical Oncology. 2008;26:4027. doi: 10.1200/JCO.2007.12.9866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Tai BC, Wee J, Machin D. Analysis of design of randomised clinical trials involving competing risks endpoints. Trials. 2011;12:127. doi: 10.1186/1745-6215-12-127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Archives of General Psychiatry. 1961;4:561. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 50.Kronke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Spielberger CD, Gorsuch RL, Lushene R, Vagg PR, Jacobs GA. Manual for the State-Trait Anxiety Inventory. Palo Alto, CA: Consulting Psychologists Press; 1983. [Google Scholar]
- 52.Spitzer RL, Kronke K, Williams JB, Lowe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166:1092. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- 53.Hackman KL, Bailey MJ, Snell GI, Bach LA. Diabetes is a major risk factor for mortality after lung transplantation. Am J Transplant. 2014;14:438. doi: 10.1111/ajt.12561. [DOI] [PubMed] [Google Scholar]


