Abstract
Genomic technologies including microarrays and next-generation sequencing have enabled the generation of molecular signatures of prostate cancer. Lists of differentially expressed genes between malignant and non-malignant states are thought to be fertile sources of putative prostate cancer biomarkers. However such lists of differentially expressed genes can be highly variable for multiple reasons. As such, looking at differential expression in the context of gene sets and pathways has been more robust. Using next-generation genome sequencing data from The Cancer Genome Atlas, differential gene expression between age- and stage- matched human prostate tumors and non-malignant samples was assessed and used to craft a pathway signature of prostate cancer. Up- and down-regulated genes were assigned to pathways composed of curated groups of related genes from multiple databases. The significance of these pathways was then evaluated according to the number of differentially expressed genes found in the pathway and their position within the pathway using Gene Set Enrichment Analysis and Signaling Pathway Impact Analysis. The “transforming growth factor-beta signaling” and “Ran regulation of mitotic spindle formation” pathways were strongly associated with prostate cancer. Several other significant pathways confirm reported findings from microarray data that suggest actin cytoskeleton regulation, cell cycle, mitogen-activated protein kinase signaling, and calcium signaling are also altered in prostate cancer. Thus we have demonstrated feasibility of pathway analysis and identified an underexplored area (Ran) for investigation in prostate cancer pathogenesis.
Introduction
Prostate cancer is the second most diagnosed cancer among American men, with over 220,000 new cases predicted in 2015 [1]. Prostate-specific antigen (PSA) has been the cornerstone of prostate cancer screening for decades. However PSA is not an ideal biomarker and widespread use of PSA-screening is falling out of favor [2–4]. Reliance on PSA screening is problematic because false positives result from benign prostatic hyperplasia or prostatitis and because PSA fails to discriminate indolent disease, leading to overdiagnosis. The expansion of genomic and proteomic technology and methodology has improved the characterization of tumor biology, driving the search for more accurate cancer biomarkers. Gene and protein expression differences between normal and malignant prostate tissues have been well documented and serve as a pool for putative diagnostic, prognostic, and risk stratification biomarkers [5–24]. Gene mutations, epigenetic changes, and microRNA expression changes that occur in cancer initiation and progression have also been studied with the goal of biomarker discovery [25–29]. Yet there remain several substantial obstacles in biomarker implementation. Low reproducibility across laboratories, differences in experimental platforms and techniques, the inherent heterogeneity of prostate cancer, and insignificant clinical utility or small gains in sensitivity and specificity beyond PSA hampers the identification, validation, and implementation of biomarkers [30–35].
Previous work has focused on the selection and validation of individual genes as biomarkers. Yet the heterogeneity of prostate cancer makes it extremely unlikely to find a single gene that is a representative marker [36]. Screening panels formed by the combination of multiple genes have been used to increase predictive power for cancer detection, recurrence, relapse, and survival beyond the use of PSA or Gleason score alone [37–40]. The success of the biomarker panel approach is evidenced by the commercial launch of several screening tests which have found clinical usefulness: ProMark [41], Oncotype DX [42], Prolaris [43], and Decipher [44]. These panels may be pulled from molecular classifications studies that use differential expression to craft a signature for cancer.
However molecular classifications and gene signatures are not always stable in the sense that multiple signatures can be found for cancers. Large discrepancies between lists of differentially expressed genes (DEGs) from microarray data have been highlighted [45]. In some cases the overlap between microarray datasets was as low as 5% [46]. So for each set of DEGs, a different signature could be found. Thus biomarkers selected from these lists would perform with varying degrees of success. Taking the list of DEGs and correlating them to a prognostic marker may generate a more useful putative biomarker pool because then only genes correlated with prognosis would comprise the molecular signature. However, Ein-Dor et al. showed that in breast cancer, there was no single, unique set of genes that predicted survival because altering the patient population could produce multiple sets of genes of equal prognostic ability in predicting survival [33]. Furthermore, correlation with survival was not required for prognostic ability [33]. So it is likely that many panels exclude a number of other genes that could be potential biomarkers because the panel was derived from one body of samples (although it may be large) and considered only strongest correlations.
An alternative approach is pathway-based analysis. In pathway analysis, a collection of related genes from the same pathway or network of interaction is assessed instead of examining a group of potentially unrelated genes that optimize sensitivity and selectivity of diagnosis or prognosis. There is increased overlap between data at the pathway level compared to overlap between lists of DEGs [46, 47]. Pathway analysis does not neglect the cooperative nature of genes and considers that oftentimes genes involved in the same process are often deregulated together. By looking at the pathway, minor variations in instrumentation or method are less likely to impact results, leading to more consistent results across different sets of data [48]. Thus the pathway approach yields more robust results, improves disease classification, and may reveal novel insights about a disease [49–51]. One type of pathway analysis starts with a differentially expressed gene and correlates the expression of genes involved in the same pathway or similar process with a particular diagnostic or prognostic outcome [52–54]. A similar iteration starts with a pathway of known importance in cancer initiation or progression and evaluates the prognostic power of its individual components. This has been done for the mitogen-activated protein kinase (MAPK) pathway [55], Akt [56], mTOR pathway [57, 58], Toll-like receptor signaling pathway [59], and other oncogene signatures [60].
In this paper, comprehensive gene expression in human prostate cancer was characterized using an unbiased pathway approach. Next generation sequencing was used to obtain a profile of the differences in RNA expression between human tumors and non-malignant tissue from patients. Pathway analysis included Gene Set Enrichment Analysis and Signaling Pathway Impact Analysis. Two pathways were significantly associated with human prostate tumors—“Ran regulation of mitotic spindle formation” pathway and “transforming growth factor-beta (TGF-β) signaling” pathway.
Materials and Methods
RNA sequencing data
Level 3 de-identified data for prostate cancer samples and all available non-malignant samples from these prostate cancer patients was downloaded from The Cancer Genome Atlas (TCGA) data portal (https://tcga-data.nci.nih.gov). Level 3 describes data that has been processed and aggregated to give gene expression signals for a sample. For each sample, the data contains expression counts for up to 20,531 coding and non-coding RNA transcripts plus clinical information such as age, stage, Gleason score, PSA level, and race/ethnicity. Before analysis, tumor and non-malignant samples were randomly pulled to achieve an age- and stage-matched pool of 225 samples (S1 Table). A total of 173 prostate cancer samples and 52 non-malignant samples from 204 unique patients were analyzed. The patient clinical information is presented in Table 1.
Table 1. Prostate cancer patient clinical information from TCGA.
| Characteristics | Samples (n = 225) | Tumor (n = 173) | Non-Malignant (n = 52) | Fisher’s Exact Test P-value |
|---|---|---|---|---|
| Age | ||||
| < 65 | 155 | 121 | 34 | 0.609 |
| ≥ 65 | 70 | 52 | 18 | |
| Pathological T stage | ||||
| T1 | 0 | 0 | 0 | 0.649 |
| T2 | 113 | 84 | 29 | |
| T3 | 103 | 82 | 21 | |
| T4 | 8 | 6 | 2 | |
| Unspecified | 1 | 1 | 0 | |
| Race | ||||
| White | 92 | 50 | 42 | 0.701 |
| Black | 7 | 3 | 4 | |
| Unspecified | 126 | 120 | 6 | |
| Ethnicity | ||||
| Not Hispanic | 96 | 51 | 45 | |
| Unspecified | 129 | 122 | 7 | |
| Gleason Score | ||||
| ≤ 6 | 24 | 19 | 5 | 0.00168 |
| 7 | 129 | 89 | 40 | |
| 8–10 | 72 | 65 | 7 |
Differential Gene Expression
The R programming environment (version 3.1.2) [61] was used to process raw data, perform statistical calculations, and perform differential expression analysis. After age- and stage-matching, 393 transcripts were removed because they lacked expression in the 225 samples comprising the dataset. The RNA counts for the remaining 20,138 transcripts were rounded to the nearest whole number and compiled into a matrix to build the dataset. The magnitude of expression changes relative to non-malignant samples was also calculated by taking the base 2 logarithm of the tumor/non-malignant mean expression ratio. For genes with no expression in either the tumor or non-malignant samples, the log2 fold changes were adjusted by adding one to each mean and then calculating the ratio. All log2 values quoted are values after any such adjustments. Negative fold changes indicated down-regulation in tumor samples whereas positive values indicated up-regulation. The R package DESeq2 (version 1.6.3) [62] was used to identify DEGs in the TCGA patient RNA data. The computing was done on the Florida State University High Performance Computing Cluster. DESeq2 returned a P-value determined by Wald statistics and an adjusted P-value (Q-value) to correct for multiple comparisons testing using the Benjamini-Hochberg method to determine the false discovery rate (FDR). DEGs were defined as genes different with a FDR less than 1% (Q < 0.01).
To evaluate the significance of the identified DEGs, analyses were conducted to search for overrepresented pathways, gene set enrichment, and signaling pathway impact. First, overrepresented elements were identified among the DEGs. The Protein ANalysis THrough Evolutionary Relationships (PANTHER) Classification System and analysis tools were used to categorize DEGs by PANTHER protein class, Gene Ontology (GO) Molecular Function, and GO Biological Process to then determine if any of these classes or GO terms were overrepresented [63]. The PANTHER Overrepresentation Test (release 20150430) was used to search the data against the PANTHER database (PANTHER version 10.0 Released 2015-05-15) and the GO database (Released 2015-05-09) to identify either protein classes or GO annotations overrepresented in our data when compared to a reference human genome. P-values were adjusted using a Bonferroni correction.
Pathway Analysis
Gene Set Enrichment Analysis (GSEA) [64] was used to identify groups of genes enriched in either the tumor or non-malignant condition. The GSEA analysis tool (version 2.2.0) was downloaded from the Broad Institute website (http://www.broadinstitute.org/gsea/index.jsp). Curated gene sets of BioCarta and Reactome pathways were downloaded from the Broad Institute’s Molecular Signatures Database. An additional gene set was constructed from Kyoto Encyclopedia of Genes and Genomes (KEGG) pathways [65]. Pathways with the least relevance to prostate cancer were excluded. The KEGG pathways included in the analysis are listed in the Supporting Information (S2 Table). The entire RNA expression count matrix was loaded into the GSEA application without limiting the input to only DEGs. Both small (< 5 genes) and large (> 500 genes) gene sets were excluded from the analysis.
Signaling Pathway Impact Analysis (SPIA) was used to assess the importance of enriched pathways in terms of their impact and ability to activate or inhibit a pathway [66]. SPIA analysis was accomplished using the R package “SPIA” (version 2.18.0) [67]. Entrez IDs, log2 fold changes, and Q-values for all genes were compiled. The differential expression cut-off used in the SPIA algorithm was based on the FDR-adjusted Q-value. The analysis was run using the same tailored list of pathways as used in GSEA (S2 Table) and updated versions of these pathways were download prior to running the analysis (accessed 7/29/2015).
Results
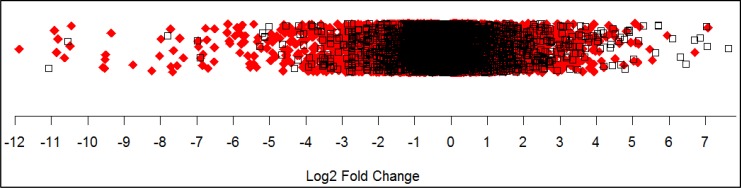
Using a 1% FDR (Q <0.01), DESeq2 analysis marked 11,115 genes and transcripts as statistically different between tumor samples and non-malignant samples in our TCGA dataset (S3 and S4 Tables). This covers 55% of the genes and transcripts sequenced. The number of down-regulated genes and transcripts totaled 5,379 and the number of up-regulated genes and transcripts totaled 5,736. Overall the largest changes observed were in the down-regulation of genes and transcripts (Fig 1). The magnitude of the up-regulation of genes and transcripts was smaller than the magnitude of down-regulated genes and the range of expression was also smaller. The twenty most down-regulated and the twenty most up-regulated genes are presented in Table 2 and Table 3.
Fig 1. Magnitude of gene expression differences between tumor and non-malignant human prostate cancer samples.
In this one-dimensional scatter plot the magnitude of gene expression changes represented by log2 fold ratios are shown. Each point represents a gene or transcript. Significantly differentially expressed genes and transcripts are shown as solid red diamonds.
Table 2. Twenty largest decreases in RNA expression between prostate tumor and non-malignant TCGA samples.
| Gene Symbol | Name | Log2 Fold Change | P-value | Q-value |
|---|---|---|---|---|
| WFDC9 | Protein WFDC9 | -11.89 | 1.98E-04 | 4.30E-04 |
| DEFB125 | Beta-defensin 125 | -10.91 | 4.30E-04 | 8.89E-04 |
| EDDM3B | Epididymal secretory protein E3-beta | -10.85 | 4.64E-09 | 1.96E-08 |
| PAEP | Glycodelin | -10.82 | 3.47E-16 | 3.78E-15 |
| SEMG2 | Semenogelin-2 | -10.64 | 1.98E-63 | 2.36E-60 |
| PATE4 | Prostate and testis expressed protein 4 | -10.48 | 2.26E-55 | 1.54E-52 |
| EDDM3A | Epididymal secretory protein E3-alpha | -10.45 | 5.77E-13 | 4.05E-12 |
| CRISP1 | Cysteine-rich secretory protein 1 | -9.58 | 1.17E-25 | 5.02E-24 |
| PATE1 | Prostate and testis expressed protein 1 | -9.53 | 3.27E-27 | 1.76E-25 |
| DEFB127 | Beta-defensin 127 | -9.52 | 1.06E-04 | 2.41E-04 |
| AQP2 | Aquaporin-2 | -9.50 | 1.94E-57 | 1.69E-54 |
| TMEM114 | Transmembrane protein 114 | -9.35 | 1.19E-15 | 1.21E-14 |
| GRXCR1 | Glutaredoxin domain-containing cysteine-rich protein 1 | -8.75 | 5.95E-19 | 9.64E-18 |
| SPINT3 | Kunitz-type protease inhibitor 3 | -8.23 | 2.11E-24 | 7.48E-23 |
| CLDN2 | Claudin-2 | -8.02 | 2.11E-75 | 6.72E-72 |
| SULT2A1 | Bile salt sulfotransferase | -7.98 | 9.41E-20 | 1.70E-18 |
| SPINK2 | Serine protease inhibitor Kazal-type 2 | -7.71 | 5.75E-71 | 8.46E-68 |
| POU3F3 | POU domain, class 3, transcription factor 3 | -7.70 | 4.68E-17 | 5.77E-16 |
| LCN1 | Lipocalin-1 | -7.66 | 4.18E-08 | 1.56E-07 |
| PATE3 | Prostate and testis expressed protein 3 | -7.63 | 3.33E-25 | 1.32E-23 |
Log2 fold change describes malignant expression relative to non-malignant expression. P-value is determined by DESeq2 using Wald Statistics and Q-value is the false discovery rate-adjusted P-value.
Table 3. Twenty largest increases in RNA expression between prostate tumor and non-malignant TCGA samples.
| Gene Symbol | Name | Log2 Fold Change | P-value | Q-value |
|---|---|---|---|---|
| ANKRD30A | Ankyrin repeat domain-containing protein 30A | 7.08 | 5.95E-10 | 2.82E-09 |
| FEZF2 | Fez family zinc finger protein 2 | 6.71 | 1.89E-06 | 5.59E-06 |
| C6orf10 | Uncharacterized protein C6orf10 | 5.96 | 2.59E-06 | 7.52E-06 |
| FOXG1 | Forkhead box protein G1 | 5.54 | 2.53E-04 | 5.41E-04 |
| GC | Vitamin D-binding protein | 5.47 | 4.70E-04 | 9.67E-04 |
| VAX1 | Ventral anterior homeobox 1 | 5.19 | 3.83E-12 | 2.41E-11 |
| SSX2 | Protein SSX2 | 5.16 | 4.52E-03 | 7.92E-03 |
| FGB | Fibrinogen beta chain | 5.14 | 1.52E-03 | 2.88E-03 |
| SLC45A2 | Membrane-associated transporter protein | 5.09 | 1.10E-51 | 5.99E-49 |
| SPINK1 | Pancreatic secretory trypsin inhibitor | 5.07 | 3.29E-12 | 2.08E-11 |
| HOXC12 | Homeobox protein Hox-C12 | 5.03 | 1.44E-07 | 4.96E-07 |
| SCN1A | Sodium channel protein type 1 subunit alpha | 4.96 | 5.38E-03 | 9.31E-03 |
| LOC284661 | Uncharacterized non-coding RNA | 4.84 | 4.89E-06 | 1.36E-05 |
| TFDP3 | Transcription factor Dp family member 3 | 4.76 | 2.00E-03 | 3.72E-03 |
| B3GNT6 | UDP-GlcNAc:betaGal beta-1,3-N-acetylglucosaminyltransferase 6 | 4.64 | 5.49E-22 | 1.40E-20 |
| FOXB2 | Forkhead box protein B2 | 4.52 | 2.14E-18 | 3.19E-17 |
| NR2E1 | Nuclear receptor subfamily 2 group E member 1 | 4.51 | 1.21E-15 | 1.23E-14 |
| XAGE1E | X antigen family, member 1E | 4.51 | 4.00E-03 | 7.07E-03 |
| TBX10 | T-box transcription factor TBX10 | 4.43 | 6.47E-17 | 7.81E-16 |
Log2 fold change describes malignant expression relative to non-malignant expression. P-value is determined by DESeq2 using Wald Statistics and Q-value is the false discovery rate-adjusted P-value.
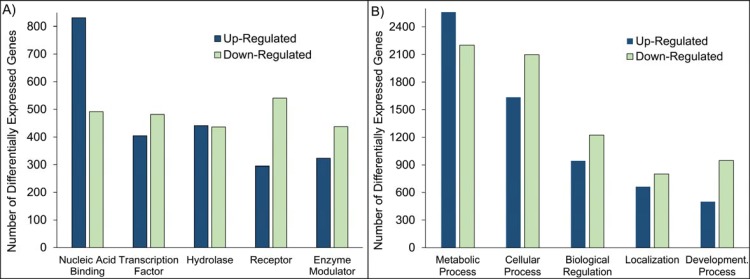
Classification and Overrepresentation Analysis
The 11,115 DEGs were grouped according to PANTHER protein class, GO Molecular Function and GO Biological Process annotations. A total of 6,254 DEGs had either PANTHER protein class, GO Biological Process, or GO Molecular Function annotations and were further classified. Grouping by protein class and GO Biological Process categories proved to be the most informative (Fig 2). The complete classifications can be found in the Supporting Information (S5 Table). The DEGs represent a wide spectrum of protein classes involved in a broad array of processes. The “Nucleic Acid Binding” PANTHER protein class includes both RNA and DNA binding proteins, nucleases, and helicases. The “Transcription Factor” protein class is sub-categorized by structural motif and also contains cofactors and nuclear hormone receptors. Proteases and phosphatases are found within the “Hydrolase” protein class. The types of “Receptor” included are protein kinase receptors, nuclear hormone receptors, cytokine receptors, ligand-gated ion channels, and G-protein coupled receptors. The “Enzyme Modulator” category features G protein, kinase, phosphatase, and protease modulators. Interestingly, the categories were generally not predominantly populated by down-regulated or up-regulated genes or transcripts. For all protein classes except the “Nucleic Acid Binding” class, DEGs were evenly distributed across tumor and non-malignant samples. In the “Nucleic Acid Binding” protein class, there were nearly one and half times as many up-regulated genes as down-regulated. The abundance of nucleic acid binding genes suggests altered transcriptional activity in tumor samples.
Fig 2. Functional Classification of Differentially Expressed Genes in Human Prostate Cancer According to PANTHER Protein Class (A) and Biological Process Gene Ontology Terms (B).
(A) “Nucleic Acid Binding” includes RNA and DNA binding, nucleases, and helicases. “Transcription Factor” includes zinc finger, helix-turn-helix, high mobility group box, basic helix-loop-helix, and basic leucine zipper transcription factors; cofactors; and nuclear hormone receptors. “Hydrolase” refers to proteases, phosphatases, esterases, lipases, deaminases, phosphodiesterases, glycosidases, deacetylases, pyrophosphatases, glucosidases, galactosidases, and amylases. “Receptor” includes protein kinase receptors, nuclear hormone receptors, cytokine receptors, ligand-gated ion channels, and G-protein coupled receptors. “Enzyme Modulator” includes G protein, kinase, phosphatase, and protease modulators. (B) “Metabolic Process” features carbohydrate, cellular amino acid, lipid, protein, and nucleobase-containing compound metabolism; and the tricarboxylic acid cycle. “Cellular Process” categories are cell-cell signaling, cell cycle, growth and proliferation, cell component movement, and cytokinesis. “Biological Regulation” includes the regulation of apoptosis, metabolism, cell cycle, translation, catalytic activity, and homeostasis. “Developmental Process” categories are system, ectoderm, mesoderm, and endoderm development; cell differentiation; death; anatomical structure morphogenesis; embryo development; sex determination; and pattern specification processes. “Localization” includes transport proteins, protein and RNA localization processes.
The two most abundant GO Biological Process groups—“Metabolic Process” and “Cellular Process”—are not surprising because these contains genes are involved in the most basic of life processes. In fact, metabolic changes have been widely documented in tumors [68–70]. The increased energetic and biosynthetic needs of proliferating cancer cells are often met through metabolic dysregulation [71–73]. The heading “Metabolic Process” includes carbohydrate metabolism, cellular amino acid metabolism, lipid metabolism, nucleobase-containing compound metabolism, protein metabolism, and the tricarboxylic acid cycle. “Cellular Process” includes cell-cell signaling, cell cycle, growth and proliferation, cell component movement, and cytokinesis. “Biological Regulation” includes the regulation of apoptosis, metabolism, cell cycle, translation, catalytic activity, and homeostasis. The category “Developmental Process” incorporates system, ectoderm, mesoderm, and endoderm development, as well as cell differentiation, death, anatomical structure morphogenesis, embryo development, sex determination, and pattern specification processes. “Localization” refers to general transport proteins and specific protein and RNA localization processes.
PANTHER’s overrepresentation statistic was used to calculate the probability that the highly populated protein classes and GO groupings among the DEGs would occur by random chance. Indeed, many of the most abundant categories are overrepresented in the data when compared to a reference genome (Table 4). The three most abundant protein classes—“Nucleic Acid Binding”, “Transcription Factor”, and “Hydrolase”—were enriched along with the classes “Transferase” and “Transporter”. The five most populated GO Biological Processes were also enriched: “Metabolic Process”, “Cellular Process”, “Biological Regulation”, “Localization”, and “Developmental Process”. The “Multicellular Organism Process”, “Biological Adhesion”, “Cellular Component Organization or Biogenesis”, and “Immune System Process” GO Biological Processes were also enriched. Finally, five of the top six GO Molecular Functions were enriched: “Binding”, “Catalytic Activity”, “Nucleic Acid Binding Transcription Factor Activity”, “Transporter Activity”, and “Structural Molecule Activity”.
Table 4. Overrepresented PANTHER protein class and GO ontology categories in TCGA data from malignant and non-malignant prostate.
| P-value | |
|---|---|
| PANTHER Protein Class | |
| RNA binding protein (Nucleic Acid Binding) | 9.08E-05 |
| Ribosomal protein (Nucleic Acid Binding) | 4.67E-04 |
| Transcription factor | 2.04E-02 |
| Transferase | 3.41E-04 |
| Hydrolase | 5.75E-04 |
| Transporter | 3.65E-03 |
| GO-Biological Process | |
| Sensory perception of chemical stimulus (Multicellular Organism Process) | 2.96E-10 |
| Protein metabolic process (Metabolic Process) | 6.82E-09 |
| Nucleobase-containing compound metabolic process (Metabolic Process) | 1.64E-08 |
| RNA metabolic process (Metabolic Process) | 6.87E-06 |
| Nervous system development (Developmental Process) | 1.48E-03 |
| Cellular protein modification process (Metabolic Process) | 1.90E-03 |
| Translation (Metabolic Process) | 2.81E-03 |
| Natural killer cell activation (Immune System Process) | 4.06E-03 |
| DNA-dependent transcription (Metabolic Process) | 7.61E-03 |
| Ion transport (Localization) | 1.81E-02 |
| Protein phosphorylation (Metabolic Process) | 3.31E-02 |
| Cellular component morphogenesis (Cellular Component Organization or Biogenesis) | 3.85E-02 |
| Cellular component organization (Cellular Component Organization or Biogenesis) | 7.58E-04 |
| Cell communication (Cellular Process) | 2.57E-02 |
| Biological regulation | 3.03E-05 |
| Biological adhesion | 4.67E-02 |
| GO-Molecular Function | |
| Transferase activity (Catalytic Activity) | 1.67E-06 |
| Hydrolase activity (Catalytic Activity) | 2.87E-04 |
| Kinase activity (Catalytic Activity) | 7.73E-03 |
| Protein binding (Binding) | 2.99E-03 |
| DNA binding (Binding) | 4.19E-03 |
| Transmembrane transporter activity (Transporter Activity) | 3.37E-03 |
| Sequence-specific DNA binding transcription factor activity (Nucleic Acid Binding Transcription Factor Activity) | 1.52E-02 |
| Structural constituent of ribosome (Structural Molecule Activity) | 3.59E-02 |
Overrepresentation was determined by calculating the probability that the number of differentially expressed genes belonging to a particular category is larger or smaller than what would be expected based on a reference human genome. P-values are adjusted using a Bonferroni correction.
Gene Set Enrichment Analysis
One limitation of a class or pathway overrepresentation analysis is that it does not indicate which condition is associated with the overrepresentation; GSEA does. Expressed genes were ranked by their correlation with the malignant phenotype and then this list was compared to sets of genes in a pathway, linking pathway enrichment to a phenotype. The more highly-correlated genes in a gene set, the higher the significance of that gene set. The gene sets with the highest normalized enrichment scores are presented in Table 5 and other results are listed in the Supporting Information (S7 Table). The FDR cutoff was set at 25% to maximize hypothesis generation. Only one pathway was enriched in the tumor samples, the “RanMS pathway” which includes the genes that regulate the formation of the mitotic spindle during cell division. Ten genes in our list of DEGs belonged to this pathway, each contributing to its enrichment in the malignant phenotype (Table 6). All ten were differentially expressed and up-regulated in the malignant samples. The remaining pathways were enriched in the non-malignant phenotype. The most significant pathway enriched in the non-malignant phenotype was the “calcium signaling” pathway. Enrichment of the calcium signaling pathway was due to 81 DEGs and 19 other genes or transcripts (S8 Table). Also enriched in the non-malignant phenotype were several other signaling pathways (oxytocin, prolactin, cAMP, MAPK, cGMP-PKG, TGF-β, Hippo, and Ras) and pathways related to cell-cell and cell-matrix adhesion (extracellular matrix-receptor interaction, actin cytoskeleton regulation, proteoglycans, and focal adhesion).
Table 5. Significant gene sets enriched in malignant and non-malignant prostate with the largest normalized enrichment scores.
| Gene Set | ES | NES | P-value | Q-value |
|---|---|---|---|---|
| BioCarta: RanMS pathway | 0.827 | 1.652 | 4.02E-03 | 2.05E-01 |
| KEGG: Calcium signaling pathway | -0.456 | -1.714 | 4.89E-03 | 5.75E-02 |
| KEGG: Basal cell carcinoma | -0.482 | -1.647 | 6.59E-03 | 6.10E-02 |
| KEGG: Oxytocin signaling pathway | -0.443 | -1.603 | 1.66E-02 | 6.26E-02 |
| KEGG: Thyroid hormone synthesis | -0.466 | -1.652 | 1.19E-02 | 6.34E-02 |
| KEGG: Signaling pathways regulating pluripotency of stem cells | -0.432 | -1.596 | 4.56E-03 | 6.35E-02 |
| KEGG: Prolactin signaling pathway | -0.461 | -1.605 | 4.52E-03 | 6.44E-02 |
| KEGG: Pathways in cancer | -0.433 | -1.624 | 8.77E-03 | 6.49E-02 |
| KEGG: ECM-receptor interaction | -0.517 | -1.633 | 3.76E-02 | 6.52E-02 |
| KEGG: cAMP signaling pathway | -0.434 | -1.719 | 0.00E+00 | 6.63E-02 |
| KEGG: MAPK signaling pathway | -0.417 | -1.614 | 2.28E-03 | 6.78E-02 |
| KEGG: Regulation of actin cytoskeleton | -0.449 | -1.606 | 8.99E-03 | 6.84E-02 |
| KEGG: Phosphatidylinositol signaling pathway | -0.517 | -1.653 | 4.38E-03 | 6.93E-02 |
| KEGG: cGMP-PKG signaling pathway | -0.469 | -1.677 | 1.43E-02 | 7.12E-02 |
| KEGG: TGF-beta signaling pathway | -0.513 | -1.654 | 1.11E-02 | 7.73E-02 |
| KEGG: Focal adhesion | -0.517 | -1.725 | 1.61E-02 | 7.87E-02 |
| KEGG: Hippo signaling pathway | -0.482 | -1.733 | 0.00E+00 | 9.65E-02 |
| KEGG: Proteoglycans in cancer | -0.492 | -1.740 | 0.00E+00 | 1.38E-01 |
| KEGG: Ras signaling pathway | -0.460 | -1.760 | 2.23E-03 | 2.13E-01 |
| BioCarta: p38 MAPK pathway | -0.527 | -1.584 | 8.15E-03 | 2.48E-01 |
ES = enrichment score, NES = normalized enrichment score, Q-value = false discovery rate-adjusted P-value. Positive enrichment scores correspond to enrichment in the malignant samples. Negative enrichment scores correspond to enrichment in the non-malignant samples.
Table 6. Differentially Expressed Ran-Mitotic Spindle Pathway Components in Human Prostate Cancer.
| Ran regulation of mitotic spindle formation pathway | |||
|---|---|---|---|
| Gene Name | Symbol | Expression | Role |
| GTP-binding nuclear protein Ran | RAN | ↑ | GTPase; nuclear transport; formation of mitotic spindle [74] |
| Regulator of chromosome condensation | RCC1 | ↑ | Guanine nucleotide exchange factor of Ran, produces a RanGTP gradient around chromosomes. [75] |
| Ran GTPase-activating protein 1 | RANGAP1 | ↑ | Accelerates RanGTP hydrolysis, helps maintain RanGTP gradient around chromosomes. [75] |
| Ran binding protein 1 | RANBP1 | ↑ | Regulates activity of RCC1 and RANGAP [76, 77] |
| Importin subunit alpha-1 | KPNA2 | ↑ | Nuclear import; KPNB1 adapter protein [78] |
| Importin subunit beta-1 | KPNB1 | ↑ | Nuclear import; docking platform [79, 80] |
| Targeting protein for Xklp2 | TPX2 | ↑ | Spindle assembly factor; microtubule nucleation, separation of bipolar mitotic spindle [81, 82] |
| Nuclear mitotic apparatus protein 1 | NUMA1 | ↑ | Spindle assembly factor; Establishes, maintains mitotic spindle poles. [83] |
| Kinesin-like protein KIF15 | KIF15 | ↑ | Spindle assembly factor; Bipolar spindle maintenance, elongation [82] |
| Aurora kinase A | AURKA | ↑ | Centrosome maturation, separation, and centrosomal microtubule stabilization and nucleation. [84] |
↑ = up-regulated expression, ↓ = down-regulated expression
Signaling Pathway Impact Analysis
SPIA considers whether or not the DEGs found in a pathway have a meaningful impact within that pathway and thus addresses the topology of DEGs in pathways [66]. In other words, pathway significance is partly dependent on if the number of DEGs observed in a pathway is larger than that observed by random chance. This is captured in the probability of overrepresentation. Pathway significance is also partly based on whether DEGs in a particular pathway are at crucial junctions and can thus perturb the pathway. This is the probability of perturbation. These two probabilities are combined into a global probability which is adjusted by the false discovery rate. This adjusted metric was used to rank the impact of the pathways. Many of the same pathways were identified as significant in both GSEA and SPIA analysis (Table 7). In fact, the 8 most significant pathway results from SPIA were all significantly enriched in GSEA. However, only the “calcium signaling” pathway was highly ranked in both analyses. The only pathway activated in the malignant condition was the “TGF-β signaling” pathway (Table 8). The other pathways were all inhibited in the malignant condition. Similar to GSEA results, several signaling pathways (oxytocin, cAMP, MAPK, cGMP-PKG, TGF-β, Hippo, Rap1, ErbB, and Ras) and pathways related to cell-cell and cell-matrix adhesion (proteoglycans, focal adhesion, and actin cytoskeleton regulation) were impacted. Images of the pathways with DEGs highlighted can be accessed in the Supporting Information (S9 Table).
Table 7. Significantly impacted pathways in human prostate cancer as determined by SPIA.
| Name | NDE/pSize | pNDE | pPERT | pG | pGFdr |
|---|---|---|---|---|---|
| Proteoglycans in cancer | 140/201 | 1.75E-05 | 5.00E-06 | 2.11E-09 | 1.86E-07 |
| Hippo signaling pathway | 112/153 | 3.12E-06 | 1.60E-02 | 8.90E-07 | 3.91E-05 |
| Pathways in cancer | 257/398 | 7.77E-05 | 2.00E-03 | 2.59E-06 | 7.60E-05 |
| Focal adhesion | 144/207 | 1.48E-05 | 2.10E-02 | 4.97E-06 | 1.09E-04 |
| cGMP-PKG signaling pathway | 118/167 | 2.80E-05 | 3.07E-01 | 1.09E-04 | 1.92E-03 |
| Calcium signaling pathway | 115/180 | 1.08E-02 | 4.00E-03 | 4.78E-04 | 7.01E-03 |
| Ras signaling pathway | 144/225 | 4.36E-03 | 2.90E-02 | 1.26E-03 | 1.59E-02 |
| TGF-β signaling pathway | 60/80 | 1.95E-04 | 8.54E-01 | 1.62E-03 | 1.78E-02 |
| Chronic myeloid leukemia | 55/73 | 2.93E-04 | 8.74E-01 | 2.37E-03 | 2.32E-02 |
| Basal cell carcinoma | 36/55 | 8.03E-02 | 6.00E-03 | 4.16E-03 | 3.59E-02 |
| Regulation of actin cytoskeleton | 135/213 | 9.11E-03 | 6.80E-02 | 5.20E-03 | 3.59E-02 |
| ErbB signaling pathway | 60/87 | 5.98E-03 | 1.07E-01 | 5.34E-03 | 3.59E-02 |
| Glioma | 48/65 | 1.50E-03 | 4.51E-01 | 5.60E-03 | 3.59E-02 |
| Small cell lung cancer | 58/86 | 1.38E-02 | 5.00E-02 | 5.71E-03 | 3.59E-02 |
| Oxytocin signaling pathway | 105/157 | 1.82E-03 | 4.53E-01 | 6.69E-03 | 3.87E-02 |
| MAPK signaling pathway | 152/254 | 7.51E-02 | 1.30E-02 | 7.75E-03 | 3.87E-02 |
| Cell cycle | 85/124 | 1.60E-03 | 6.41E-01 | 8.07E-03 | 3.87E-02 |
| MicroRNAs in cancer | 97/149 | 8.72E-03 | NA | 8.72E-03 | 3.87E-02 |
| cAMP signaling pathway | 132/200 | 1.15E-03 | 9.75E-01 | 8.76E-03 | 3.87E-02 |
| Rap1 signaling pathway | 130/211 | 3.42E-02 | 3.30E-02 | 8.80E-03 | 3.87E-02 |
NDE = number of differentially expressed elements, pSize = pathway size, pNDE = overrepresentation probability, pPERT = perturbation probability, pG = global probability, pGFdr = false discovery rate-adjusted global probability. Bold pathways were also significant by Gene Set Enrichment Analysis.
Table 8. Components of the TGF-β Signaling Pathway Differentially Expressed in Human Prostate Cancer.
| TGF-β Signaling Pathway | |||
|---|---|---|---|
| Gene Name | Symbol | Expression | Role |
| Transforming growth factor β-2 | TGF-β2 | ↓ | Cytokine growth factor [85] |
| Transforming growth factor β-3 | TGF-β3 | ↓ | Cytokine growth factor [85] |
| TGF-β receptor type I | TGFBR1 | ↓ | transmembrane serine/threonine kinase [86] |
| TGF-β receptor type II | TGFBR2 | ↓ | transmembrane serine/threonine kinase [86] |
| TGF-β receptor type III | TGFBR3 | ↓ | non-signaling receptor, presents TGF-β ligands to TGFBR2 [86] |
| Latent-transforming growth factor β-binding protein 1 | LTBP1 | ↓ | maintains latency of TGF-β [87] |
| Mothers against decapentaplegic homolog 2 | SMAD2 | ↓ | receptor SMAD for TGFBR1 [88] |
| Mothers against decapentaplegic homolog 3 | SMAD3 | ↓ | receptor SMAD for TGFBR1 [88] |
| Mothers against decapentaplegic homolog 4 | SMAD4 | ↓ | complexes with receptor SMADs before nuclear translocation [88] |
| Mothers against decapentaplegic homolog 7 | SMAD7 | ↓ | blocks phosphorylation of SMAD 2/3 [89] |
| E3 ubiquitin-protein ligase RBX1 | RBX1 | ↑ | In complex with CUL1 degrades SMAD2/3 [90] |
| Cullin-1 | CUL1 | ↓ | In complex with RBX1 degrades SMAD2/3 [90] |
| Retinoblastoma-like protein 1 | RBL1 | ↓ | E2F4/5 corepressor of myc [91] |
| Transcription factor E2F4 | E2F4 | ↓ | myc transcription factor [91] |
| Transcription factor E2F5 | E2F5 | ↑ | myc transcription factor [91] |
| Myc proto-oncogene protein | MYC | ↑ | Influences cell growth, cell cycle, apoptosis, metabolism, energy production, DNA replication and RNA stability and splicing [92] |
| Sp1 Transcription factor | SP1 | ↓ | Transcription factor regulating growth factors, DNA synthesis regulators, and cell cycle genes including CDKN2B [93, 94] |
| Cyclin-dependent kinase 4 inhibitor B | CDKN2B | ↓ | Mediates cell cycle arrest at G1 [95] |
↑ = up-regulated, ↓ = down-regulated
Discussion
Global expression studies have documented many differentially expressed genes in human prostate cancer [7, 9, 13–15, 96–102]. Lucas and Heath compiled a list of differentially expressed genes with reported prognostic significance in prostate cancer [30]. Of the 22 genes listed, 19 were differentially expressed in our TCGA dataset and there was agreement in expression pattern between 12 genes. PTEN, TMPRSS2, MYC, SMAD4, EZH2, p53, BCL2, NPY, PLA2G7, Ki-67, p16, and BAX expression in our findings matched what was presented in the literature. PTEN, a tumor suppressor, was down-regulated in malignant samples. The deletion of PTEN correlates with higher Gleason grade, risk of progression, and recurrence after therapy, and advanced localized or metastatic disease and death [103, 104]. SMAD4 was down-regulated in our TCGA prostate cancer data and has also been found to be down-regulated in prostate cancers, including advanced tumors [105, 106]. The deletion of this gene has led to invasive, metastatic, and lethal prostate cancers in a mouse model [39]. TMPRSS2 was up-regulated and this is in agreement with reports of it being more highly expressed in prostate carcinoma compared to normal prostate epithelium [107, 108]. TMPRSS2 contributes to the invasion and metastasis of prostate cancer [109]. Further, TMPRSS2-ERG gene fusion holds promise as a potential prostate cancer biomarker [110]. MYC was also up-regulated in this dataset and the overexpression (gene amplification, mRNA, and protein increase) of MYC in prostate cancer is well-documented [111–115]. MYC gene amplification was found more often in metastases [116, 117] and also correlated with poor prognostic factors like higher Gleason and histopathological scores [118], or greater chance of PSA recurrence [114]. EZH2 up-regulation is reported here and in the literature where such overexpression led to increased proliferation in prostate cells and is associated with aggressive disease and increased risk of recurrence [119]. The expression of p53 mRNA was increased in malignant samples in our TCGA data. In a study of prostate cancer patients, p53 positive expression was seen in the majority (69.1%) of patients with the number of positive patients increasing as stage and Gleason score increased. P53 was also an independent predictor of recurrence [120]. BCL2 mRNA expression was decreased in TCGA tumor samples. The absence of BCL-2 protein expression is reported in prostate cancer [120, 121]. Furthermore, BCL-2 expression is negative in androgen-dependent, but increased in hormone insensitive prostate cancers [122–124] and correlated with poor prognosis [125]. Pro-neuropeptide Y was up-regulated in this study and in the literature [126, 127]. Pro-neuropeptide Y up-regulation is associated with non-aggressive tumors [128] and regulates proliferation in prostate cancer cell lines [129]. PLA2G7 was up-regulated in our data. It is reported to be more highly expressed in prostate cancer compared to benign samples [130, 131] and the TCGA samples studied here. Levels of Ki-67 mRNA were increased in tumor versus non-malignant samples from our TCGA data and in the literature compared to normal tissue [132]. Furthermore Ki-67 protein is increased in prostate cancer [133–136], prostate cancer metastases [137, 138] and is a useful prognostic marker [139]. In our list of DEGs, p16 was up-regulated. Recently, p16 expression was found in a large majority of prostate tissues [140]. BAX mRNA expression was increased in this TCGA dataset and BAX protein had increased expression in prostate cancer [141].
The remaining 7 DEGs in common with Lucas and Heath’s list displayed a discrepancy in expression pattern between our results and the literature. TGF-β1 was not differentially expressed but TGF-β2 was down-regulated. Expression of TGF-β1 and TGF-β2 was increased in prostate cancer compared to normal or non-malignant tissues [142–147]. However, TGF-β3 was down-regulated in agreement with other reports of TGF-β3 expression in prostate cancer [97, 148]. Both α and β isoforms of IL-1 and IL-6 were down-regulated in this TCGA dataset. IL-1α and IL-6 were up-regulated in prostate cancer samples [149–153]. IL-6 stimulated growth of LNCaP cells [154] and elevated IL-6 was also associated with poor prognosis in prostate cancer [149, 155–162]. IL-1β has been reported both up- and down-regulated in the literature. Protein expression in patient samples was down-regulated [163] but elevated gene and protein expression in human cancer cells and tumors has also been reported [164]. In our list of DEGs, p21 was down-regulated. Aaltomaa et al. reported p21 protein expression in the majority of prostate tumors but not in normal prostate epithelial cells [165] but other studies reported p21 immunostaining in only 20%-35% of cancer samples [166, 167]. Both p21 and p16 inhibited growth in prostate cancer cell lines [168]. Vascular endothelial growth factor A (VEGF-A) was down-regulated in our data. High expression of VEGF correlated with poor prognosis [169], but some studies reported that the higher expression of VEGF-A correlated with better clinical outcome [170]. TRAIL/TNFSF10 was up-regulated in our TCGA data. While epithelial expression of TRAIL protein was stronger in tumors, stromal expression of TRAIL was decreased or absent in tumors [171, 172]. Only stromal TRAIL expression correlated with recurrence-free survival [171]. NFKB1 was down-regulated in our data. However, NFKB1 protein expression progressively increased in normal, benign prostatic hyperplasia and prostate cancer tissues [173]. The other DEGs with prognostic significance in prostate cancer that were not differentially expressed in our list of DEGs include IL-7, CCL-2, and CDH1.
Comparisons between the DEGs presented herein and DEGs listed in other studies highlight variance from experiment to experiment. Despite such variance a strong underlying correlation between datasets may still sometimes be seen [174]. These correlations would most likely be captured in a pathway approach. Thus our TCGA data was subject to pathway analysis. We found the “Ran regulation of mitotic spindle formation” pathway to be most significant in prostate cancer and the “TGF-β signaling” pathway to be activated in prostate cancer. Additionally, the following pathways were significant across both GSEA and SPIA methods and were associated with the non-malignant samples and were inhibited in the tumor samples: “proteoglycans in cancer”, “Hippo signaling pathway”, “cGMP-PKG signaling pathway”, “Ras signaling pathway”, “MAPK signaling pathway”, “Focal adhesion”, “Regulation of actin cytoskeleton”, “Oxytocin signaling pathway”, and “Pathways in cancer”.
Ran regulation of mitotic spindle formation pathway
Ran is a small GTPase of the Ras family known to function in directing nucleocytoplasmic transport, in cell cycle control through regulation of transition to S-phase and mitosis, and in regulating the mitotic spindle during mitosis and the reassembly of the nuclear envelope after mitosis [175]. Ran’s control over the mitotic spindle is the pathway that was shown to be significant in prostate cancer in our data. Proper functioning of this pathway assembles spindle microtubules for chromosome alignment and segregation in a way that ensures a single copy of each chromosome is distributed to the daughter cells, thus avoiding aneuploidy [74, 75, 176]. Each of the genes in this pathway, which include Ran, its regulators, accessory proteins, spindle assembly factors, and import/export factors, was up-regulated (Table 6). Ran’s function in mitotic spindle assembly is reviewed by Clarke and Zhang [176]. Ran-GDP is converted to Ran-GTP by the guanine nucleotide-exchange factor RCC1 and is hydrolyzed back to Ran-GDP with the aid of the GTPase activating protein RanGAP1 and RanBP1/2. The specific localization of RCC1 and RanGAP1/RanBP2 results in the formation of Ran-GTP at precise points along spindle assembly. Importin-α/importin-β complexes carry spindle assembly factors such as TPX2 and NuMA into the nucleus where they are released at chromosomes after interaction with Ran-GTP. Spindle assembly factors then interact with other molecules such as Aurora kinase A to form the spindle.
Ran-GTP overexpression was reported in various human cancers [177–181] and multiple cancer cell lines [181, 182]. Ran proved critical for epithelial ovarian cancer cell survival [183] and its overexpression caused malignant transformation in rat mammary cells [184]. Silencing of Ran in tumor cell lines, but not normal cells, led to cell death after aberrations in mitotic spindle assembly and mitochondrial function [181]. In agreement with our data, other pathway components and Ran-associated genes are also overexpressed in cancer: Aurora kinase A [185], TPX2 [186–188], and HSET [189]. Ran has not been extensively studied in prostate cancer. There are reports of increased Ran expression in prostate tumor tissues [190] and Ran functions as an androgen receptor coactivator [191, 192].
TGF-β Signaling
The TGF-β signaling pathway was activated in the malignant condition in this TCGA prostate cancer dataset. In general, TGF-β signaling regulates cell proliferation, migration, differentiation, epithelial-mesenchymal transition, immune-suppression, and apoptosis [85, 193]. Several components of the TGF-β signaling pathway were differentially expressed (Table 8). The binding of active TGF-β to its receptors begins a phosphorylation cascade that activates Smad transcription factors which translocate to the nucleus. In the nucleus, the Smad complex binds various transcription factors, coactivators, co-repressors, and chromatin remodeling factors to regulate gene expression [194, 195]. Ultimately, TGF-β signaling promotes expression of inhibitors of cell cycle progression and suppresses proliferative genes [195, 196]. Tumor cells can subvert the suppressive effect of TGF-β signaling seen in normal cells to promote tumorigenesis [194, 195].
Several studies have reported the increase of TGF-β isoforms in prostate cancer [142, 145–147, 197, 198], however our study shows a significant decrease in TGF-β2 and TGF-β3 gene expression and no differential expression of TGF-β1. Our results are, however, corroborated by the work of Dallas et al. which showed both latent and active forms of TGF-β2 were decreased in malignant prostate cells compared to normal prostate epithelial cells cultured from the same patient [199]. Our results are also corroborated by studies showing lost or decreased expression of TGF-β3 [143, 148]. In our TCGA dataset, all three TGF-β receptors were down-regulated. Loss of TGF-β receptors is consistent with literature [146, 200–204] and represents a mechanism through which tumors avoid growth suppression by TGF-β, thus facilitating the development of cancer after oncogenic triggers [195]. Additionally, down-regulation of TGF-β1, β2, and β3 is associated with androgen-stimulated growth of prostate cancer cells [205].
Although TGF-β signaling typically operates through Smad proteins, the pathway signal may also be diverted through other Smad-independent pathways like PI3K/AKT, ERK/MAPK, JNK/p38 MAPK and Rho-like GTPase signaling pathways [151, 206]. Since Smad genes were down-regulated, we looked at other effectors and found serine/threonine-protein phosphatase 2A 65 kDa regulatory subunit A alpha and beta isoforms (PPP2R1A, PPP2R1B) to be up-regulated along with the targets ribosomal protein S6 kinase β-1 and β-2 (RPS6KB1, RPS6KB2), the serine/threonine-protein phosphatase 2A catalytic subunit β isoform (PPP2CB) was down-regulated, both RhoA and ROCK1 were down-regulated and MAPK1 and MAPK3 were also down-regulated. In our TCGA data, MAPK signaling pathway was significantly different between tumor and non-malignant samples, however it was more associated with non-malignant samples whereas TGF-β was more associated with tumor samples. Erk signaling alters the expression of genes controlling cell motility, and cell-matrix adhesion and interactions [207]. Cell motility and cell-matrix adhesion-related gene sets were also significantly enriched in the non-malignant samples of our TCGA prostate cancer data (Table 5).
Pathway Comparison
There were a few surprising results from GSEA analysis—namely, the significance of prolactin and oxytocin signaling pathways and thyroid hormone synthesis pathway. The genes contributing to the enrichment of these pathways in non-malignant samples were not the namesake hormones themselves, but the multiple kinases, phosphatases, and calcium or potassium channel proteins that participate in hormone signaling (S10–S12 Tables). In the case of oxytocin signaling, the pathway operates through both calcium signaling and MAPK signaling (S1 Fig), which were also found to be significant. For the prolactin pathway (S2 Fig), the enrichment of MAPK kinases and PI3K kinases is abundant however prolactin itself is not enriched (S11 Table). Finally, for thyroid synthesis pathway (S3 Fig), none of the hormones or receptors are present but other components through which they operate are (S12 Table). Thus it appears these pathways could have been flagged due to substantial overlap with the signaling of other pathways since neither oxytocin, prolactin, or thyroid stimulating hormone nor their receptors were differentially expressed. These results demonstrate the limitation of GSEA discussed previously, the topology of genes in the pathways is unaccounted for. SPIA is a complementary pathway method that does consider the position of genes in the pathway. It is noteworthy that SPIA analysis was able to filter prolactin and thyroid hormone synthesis pathways from significant results.
Comparison to previous pathway studies which used microarray data or single nucleotide polymorphisms from genome-wide association studies showed that several pathways were identified across experimental platforms. Savli et al. looked at gene networks and pathway analysis in prostate cancer [208]. However, that study used microarray to measure gene expression and found 738 up-regulated genes and 515 down-regulated genes. This study used RNA sequencing data and found 5,736 up-regulated genes and 5,379 down-regulated genes. Some advantages of a sequencing method over microarray approach include more extensive transcript identification beyond the coverage of sequence libraries although correlation between some sequencing approaches and microarray platforms has been demonstrated [34]. Additionally, our patient pool was much larger (173 versus 21 tumor and 52 versus 10 non-malignant). The methods for identifying pathways was also different. Savli et al. used Ingenuity Pathway Analysis to identify pathways and construct gene networks. “Axonal guidance signaling” (down-regulated) and “acute phase response” (up-regulated) were the most significant pathways among the up- and down-regulated canonical pathways reported by Savli et al. but were not found in this study’s results. However other important pathways in prostate cancer were found in both studies including “actin cytoskeleton” (down-regulated in both), “calcium signaling” (up-regulated in Savli et al., down-regulated in ours), and “MAPK signaling” (down-regulated in both). Jia et al. used a combination of GSEA and Plink set-based tests on microarray data and genome-wide association studies to identify thirteen KEGG pathways involved in prostate cancer [209]. In this study, we found five of these KEGG pathways to be important in prostate cancer: regulation of actin cytoskeleton, small cell lung cancer, cell cycle, chronic myeloid leukemia, and TGF-β signaling pathway.
Conclusion
This work presents a comprehensive gene expression profile of human prostate cancer. Differential gene expression was analyzed in the context of gene sets and pathways to identify signature pathways associated with prostate cancer. “TGF-β signaling” and “Ran regulation of mitotic spindle formation” pathways were strongly associated with prostate cancer. Since it is an underexplored area in prostate cancer, we suggest Ran pathway components for further investigation in prostate cancer pathogenesis. Several other significant pathways confirm reported findings from microarray data that suggest actin cytoskeleton regulation, cell cycle, MAPK signaling, and calcium signaling are also altered in prostate cancer. We further observed that none of the most highly altered genes with the largest increases or decreases in expression appeared in the significant pathways. Thus we have demonstrated that both differential expression and pathway analysis are important in extracting meaningful information.
Supporting Information
Differentially expressed genes are highlighted in red.
(PNG)
Differentially expressed genes are highlighted in red.
(PNG)
Differentially expressed genes are highlighted in red.
(PNG)
This file includes the RNAseq expression data for the 225 age- and stage-matched prostate cancer non-malignant and tumor samples downloaded from The Cancer Genome Atlas and used for the analyses presented in this work.
(XLSX)
This is the set of KEGG pathways used in Gene Set Enrichment Analysis and Signaling Pathway Impact Analysis. Pathways likely to have little relevance to prostate cancer (e.g. parasitic, bacterial, and viral infectious diseases, substance dependencies, and specific immune, neurodegenerative, and cardiovascular diseases) have been excluded.
(XLSX)
A total of 11,115 genes and transcripts were differentially expressed according to DESeq2 analysis using Wald statistics. All statistical parameters plus the calculated log2 fold change are presented.
(XLSX)
Complete results of DESeq2 analysis with statistical parameters and calculated log2 fold change.
(XLSX)
Complete classification based on PANTHER protein class, GO Molecular Function and GO Biological Process terms.
(XLSX)
This is the full pathway overrepresentation analysis of protein class and GO Biological Process categories among DEGs from the dataset.
(XLSX)
(XLSX)
These genes and transcripts from the evaluated TCGA dataset contribute to the enrichment of the KEGG Calcium Signaling Pathway in non-malignant samples.
(XLSX)
(XLSX)
These genes and transcripts from the evaluated TCGA dataset contribute to the enrichment of the KEGG Calcium Signaling Pathway in non-malignant samples.
(XLSX)
These genes and transcripts from the evaluated TCGA dataset contribute to the enrichment of the KEGG Calcium Signaling Pathway in non-malignant samples.
(XLSX)
These genes and transcripts from the evaluated TCGA dataset contribute to the enrichment of the KEGG Calcium Signaling Pathway in non-malignant samples.
(XLSX)
Acknowledgments
The authors thank Dr. Jinfeng Zhang and Mr. Kaixian Yu in the Departments of Statistics at Florida State University for helpful discussions. This work was in part supported by the Leslie N. Wilson-Delores Auzenne Graduate Assistantship for Minorities awarded to JSM by the Florida State University Graduate School, the Research Experience Program of Women in Math, Science, and Engineering of Florida State University to AKVL, and grants from the Florida State University and an Endowed Chair Professorship in Cancer Research from anonymous donors to QXAS. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Abbreviations
- PSA
prostate-specific antigen
- DEGs
differentially expressed genes
- MAPK
mitogen activated protein kinase
- TGF-β
transforming growth factor-beta
- TCGA
The Cancer Genome Atlas
- FDR
false discovery rate
- PANTHER
Protein ANalysis THrough Evolutionary Relationships
- GO
Gene Ontology
- GSEA
Gene Set Enrichment Analysis
- KEGG
Kyoto Encyclopedia of Genes and Genomes
- SPIA
Signaling Pathway Impact Analysis
- ES
enrichment score
- NES
normalized enrichment score
- pNDE
probability of overrepresentation
- pPERT
probability of perturbation
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This work was in part supported by the Leslie N. Wilson-Delores Auzenne Graduate Assistantship for Minorities awarded to JSM by the Florida State University Graduate School, the Research Experience Program of Women in Math, Science, and Engineering of Florida State University to AKVL, and grants from the Florida State University and an Endowed Chair Professorship in Cancer Research from anonymous donors to QXAS. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Siegel RL, Miller KD, Jemal A. Cancer statistics, 2015. 2015; 65(1): 5–29. [DOI] [PubMed]
- 2. Draisma G, Etzioni R, Tsodikov A, Mariotto A, Wever E, Gulati R, et al. Lead time and overdiagnosis in prostate-specific antigen screening: importance of methods and context. J Natl Cancer Inst. 2009; 101(6): 374–383. 10.1093/jnci/djp001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Hoffman RM. Screening for Prostate Cancer. N Engl J Med. 2011; 365(21): 2013–2019. 10.1056/NEJMcp1103642 [DOI] [PubMed] [Google Scholar]
- 4. Moyer VA, U.S. Preventive Services Task Force. Screening for prostate cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2012; 157(2): 120–134. 10.7326/0003-4819-157-2-201207170-00459 [DOI] [PubMed] [Google Scholar]
- 5. Cazares LH, Adam BL, Ward MD, Nasim S, Schellhammer PF, Semmes OJ, et al. Normal, benign, preneoplastic, and malignant prostate cells have distinct protein expression profiles resolved by surface enhanced laser desorption/ionization mass spectrometry. Clin Cancer Res. 2002; 8(8): 2541–2552. [PubMed] [Google Scholar]
- 6. Dhanasekaran SM, Barrette TR, Ghosh D, Shah R, Varambally S, Kurachi K, et al. Delineation of prognostic biomarkers in prostate cancer. Nature. 2001; 412(6849): 822–826. 10.1038/35090585 [DOI] [PubMed] [Google Scholar]
- 7. Ernst T, Hergenhahn M, Kenzelmann M, Cohen CD, Bonrouhi M, Weninger A, et al. Decrease and gain of gene expression are equally discriminatory markers for prostate carcinoma: a gene expression analysis on total and microdissected prostate tissue. Am J Pathol. 2002; 160(6): 2169–2180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Lapointe J, Li C, Higgins JP, van de Rijn M, Bair E, Montgomery K, et al. Gene expression profiling identifies clinically relevant subtypes of prostate cancer. Proc Natl Acad Sci U S A. 2004; 101(3): 811–816. 10.1073/pnas.0304146101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Luo J, Duggan DJ, Chen Y, Sauvageot J, Ewing CM, Bittner ML, et al. Human prostate cancer and benign prostatic hyperplasia: molecular dissection by gene expression profiling. Cancer Res. 2001; 61(12): 4683–4688. [PubMed] [Google Scholar]
- 10. Qian DZ, Huang CY, O'Brien CA, Coleman IM, Garzotto M, True LD, et al. Prostate cancer-associated gene expression alterations determined from needle biopsies. Clin Cancer Res. 2009; 15(9): 3135–3142. 10.1158/1078-0432.CCR-08-1982 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Stamey TA, Warrington JA, Caldwell MC, Chen Z, Fan Z, Mahadevappa M, et al. Molecular genetic profiling of Gleason grade 4/5 prostate cancers compared to benign prostatic hyperplasia. J Urol. 2001; 166(6): 2171–2177. [PubMed] [Google Scholar]
- 12. Yu YP, Landsittel D, Jing L, Nelson J, Ren B, Liu L, et al. Gene expression alterations in prostate cancer predicting tumor aggression and preceding development of malignancy. J Clin Oncol. 2004; 22(14): 2790–2799. 10.1200/JCO.2004.05.158 [DOI] [PubMed] [Google Scholar]
- 13. Welsh JB, Sapinoso LM, Su AI, Kern SG, Wang-Rodriguez J, Moskaluk CA, et al. Analysis of gene expression identifies candidate markers and pharmacological targets in prostate cancer. Cancer Res. 2001; 61(16): 5974–5978. [PubMed] [Google Scholar]
- 14. Singh D, Febbo PG, Ross K, Jackson DG, Manola J, Ladd C, et al. Gene expression correlates of clinical prostate cancer behavior. Cancer Cell. 2002; 1(2): 203–209. [DOI] [PubMed] [Google Scholar]
- 15. LaTulippe E, Satagopan J, Smith A, Scher H, Scardino P, Reuter V, et al. Comprehensive gene expression analysis of prostate cancer reveals distinct transcriptional programs associated with metastatic disease. Cancer Res. 2002; 62(15): 4499–4506. [PubMed] [Google Scholar]
- 16. Khan AP, Poisson LM, Bhat VB, Fermin D, Zhao R, Kalyana-Sundaram S, et al. Quantitative proteomic profiling of prostate cancer reveals a role for miR-128 in prostate cancer. Mol Cell Proteomics. 2010; 9(2): 298–312. 10.1074/mcp.M900159-MCP200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Varambally S, Yu J, Laxman B, Rhodes DR, Mehra R, Tomlins SA, et al. Integrative genomic and proteomic analysis of prostate cancer reveals signatures of metastatic progression. Cancer Cell. 2005; 8(5): 393–406. [DOI] [PubMed] [Google Scholar]
- 18.Lin J, Xu J, Tian H, Gao X, Chen Q, Gu Q, et al. Identification of candidate prostate cancer biomarkers in prostate needle biopsy specimens using proteomic analysis. 2007; 121(12): 2596–2605. [DOI] [PubMed]
- 19. Alaiya AA, Al-Mohanna M, Aslam M, Shinwari Z, Al-Mansouri L, Al-Rodayan M, et al. Proteomics-based signature for human benign prostate hyperplasia and prostate adenocarcinoma. Int J Oncol. 2011; 38(4): 1047–1057. 10.3892/ijo.2011.937 [DOI] [PubMed] [Google Scholar]
- 20. Ahram M, Best CJM, Flaig MJ, Gillespie JW, Leiva IM, Chuaqui RF, et al. Proteomic analysis of human prostate cancer. Mol Carcinog. 2002; 33(1): 9–15. 10.1002/mc.10019 [DOI] [PubMed] [Google Scholar]
- 21. Meehan KL, Holland JW, Dawkins HJS. Proteomic analysis of normal and malignant prostate tissue to identify novel proteins lost in cancer. Prostate. 2002; 50(1): 54–63. 10.1002/pros.10032 [DOI] [PubMed] [Google Scholar]
- 22. Kiprijanovska S, Stavridis S, Stankov O, Komina S, Petrusevska G, Polenakovic M, et al. Mapping and Identification of the Urine Proteome of Prostate Cancer Patients by 2D PAGE/MS. Int J Proteomics. 2014; 2014: 594761 10.1155/2014/594761 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Davalieva K, Kostovska IM, Kiprijanovska S, Markoska K, Kubelka-Sabit K, Filipovski V, et al. Proteomics analysis of malignant and benign prostate tissue by 2D DIGE/MS reveals new insights into proteins involved in prostate cancer. Prostate. 2015; 75(14): 1586–1600. 10.1002/pros.23034 [DOI] [PubMed] [Google Scholar]
- 24. Glinsky GV, Glinskii AB, Stephenson AJ, Hoffman RM, Gerald WL. Gene expression profiling predicts clinical outcome of prostate cancer. J Clin Invest. 2004; 113(6): 913–923. 10.1172/JCI20032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Song C, Chen H, Wang T, Zhang W, Ru G, Lang J. Expression profile analysis of microRNAs in prostate cancer by next-generation sequencing. Prostate. 2015; 75(5): 500–516. 10.1002/pros.22936 [DOI] [PubMed] [Google Scholar]
- 26. Gordanpour A, Nam RK, Sugar L, Seth A. MicroRNAs in prostate cancer: from biomarkers to molecularly-based therapeutics. Prostate Cancer Prostatic Dis. 2012; 15(4): 314–319. 10.1038/pcan.2012.3 [DOI] [PubMed] [Google Scholar]
- 27. Mahapatra S, Klee EW, Young CY, Sun Z, Jimenez RE, Klee GG, et al. Global methylation profiling for risk prediction of prostate cancer. Clin Cancer Res. 2012; 18(10): 2882–2895. 10.1158/1078-0432.CCR-11-2090 [DOI] [PubMed] [Google Scholar]
- 28. Hoque MO, Topaloglu O, Begum S, Henrique R, Rosenbaum E, Van Criekinge W, et al. Quantitative methylation-specific polymerase chain reaction gene patterns in urine sediment distinguish prostate cancer patients from control subjects. J Clin Oncol. 2005; 23(27): 6569–6575. [DOI] [PubMed] [Google Scholar]
- 29. Ozen M, Creighton CJ, Ozdemir M, Ittmann M. Widespread deregulation of microRNA expression in human prostate cancer. Oncogene. 2008; 27(12): 1788–1793. [DOI] [PubMed] [Google Scholar]
- 30. Lucas SM, Heath EI. Current challenges in development of differentially expressed and prognostic prostate cancer biomarkers. Prostate Cancer. 2012; 2012: 640968 10.1155/2012/640968 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Coppola V, De Maria R, Bonci D. MicroRNAs and prostate cancer. 2010; 17(1): F1-F17. [DOI] [PubMed]
- 32. Arora R, Koch MO, Eble JN, Ulbright TM, Li L, Cheng L. Heterogeneity of Gleason grade in multifocal adenocarcinoma of the prostate. Cancer. 2004; 100(11): 2362–2366. 10.1002/cncr.20243 [DOI] [PubMed] [Google Scholar]
- 33. Ein-Dor L, Kela I, Getz G, Givol D, Domany E. Outcome signature genes in breast cancer: is there a unique set? Bioinformatics. 2005; 21(2): 171–178. 10.1093/bioinformatics/bth469 [DOI] [PubMed] [Google Scholar]
- 34. Liu F, Jenssen T, Trimarchi J, Punzo C, Cepko CL, Ohno-Machado L, et al. Comparison of hybridization-based and sequencing-based gene expression technologies on biological replicates. BMC Genomics. 2007; 8(1): 153 10.1186/1471-2164-8-153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Diamandis EP. The failure of protein cancer biomarkers to reach the clinic: why, and what can be done to address the problem? BMC Med. 2012; 10: 87-7015-10-87. 10.1186/1741-7015-10-87 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Diamandis EP. Present and future of cancer biomarkers. Clin Chem Lab Med. 2014; 52(6): 791–794. 10.1515/cclm-2014-0317 [DOI] [PubMed] [Google Scholar]
- 37.Schroten C, Dits NF, Steyerberg EW, Kranse R, van Leenders AGJLH, Bangma CH, et al. The additional value of TGFß1 and IL-7 to predict the course of prostate cancer progression. 2011; 61(6): 905–910. [DOI] [PMC free article] [PubMed]
- 38. Latil A, Bieche I, Chene L, Laurendeau I, Berthon P, Cussenot O, et al. Gene expression profiling in clinically localized prostate cancer: a four-gene expression model predicts clinical behavior. Clin Cancer Res. 2003; 9(15): 5477–5485. [PubMed] [Google Scholar]
- 39. Ding Z, Wu C, Chu GC, Xiao Y, Ho D, Zhang J, et al. SMAD4-dependent barrier constrains prostate cancer growth and metastatic progression. Nature. 2011; 470(7333): 269–273. 10.1038/nature09677 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Bibikova M, Chudin E, Arsanjani A, Zhou L, Garcia EW, Modder J, et al. Expression signatures that correlated with Gleason score and relapse in prostate cancer. Genomics. 2007; 89(6): 666–672. 10.1016/j.ygeno.2007.02.005 [DOI] [PubMed] [Google Scholar]
- 41. Blume-Jensen P, Berman DM, Rimm DL, Shipitsin M, Putzi M, Nifong TP, et al. Development and clinical validation of an in situ biopsy-based multimarker assay for risk stratification in prostate cancer. Clin Cancer Res. 2015; 21(11): 2591–2600. 10.1158/1078-0432.CCR-14-2603 [DOI] [PubMed] [Google Scholar]
- 42. Knezevic D, Goddard AD, Natraj N, Cherbavaz DB, Clark-Langone KM, Snable J, et al. Analytical validation of the Oncotype DX prostate cancer assay—a clinical RT-PCR assay optimized for prostate needle biopsies. BMC Genomics. 2013; 14: 690 10.1186/1471-2164-14-690 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Cuzick J, Swanson GP, Fisher G, Brothman AR, Berney DM, Reid JE, et al. Prognostic value of an RNA expression signature derived from cell cycle proliferation genes in patients with prostate cancer: a retrospective study. Lancet Oncol. 2011; 12(3): 245–255. 10.1016/S1470-2045(10)70295-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Karnes RJ, Bergstralh EJ, Davicioni E, Ghadessi M, Buerki C, Mitra AP, et al. Validation of a genomic classifier that predicts metastasis following radical prostatectomy in an at risk patient population. J Urol. 2013; 190(6): 2047–2053. 10.1016/j.juro.2013.06.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Zhang M, Yao C, Guo Z, Zou J, Zhang L, Xiao H, et al. Apparently low reproducibility of true differential expression discoveries in microarray studies. Bioinformatics. 2008; 24(18): 2057–2063. 10.1093/bioinformatics/btn365 [DOI] [PubMed] [Google Scholar]
- 46. Chen J, Wang Y, Shen B, Zhang D. Molecular signature of cancer at gene level or pathway level? Case studies of colorectal cancer and prostate cancer microarray data. Comput Math Methods Med. 2013; 2013: 909525 10.1155/2013/909525 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Wang Y, Chen J, Li Q, Wang H, Liu G, Jing Q, et al. Identifying novel prostate cancer associated pathways based on integrative microarray data analysis. Comput Biol Chem. 2011; 35(3): 151–158. 10.1016/j.compbiolchem.2011.04.003 [DOI] [PubMed] [Google Scholar]
- 48. Abraham G, Kowalczyk A, Loi S, Haviv I, Zobel J. Prediction of breast cancer prognosis using gene set statistics provides signature stability and biological context. BMC Bioinformatics. 2010; 11(1): 277 10.1186/1471-2105-11-277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Tian L, Greenberg SA, Kong SW, Altschuler J, Kohane IS, Park PJ. Discovering statistically significant pathways in expression profiling studies. Proc Natl Acad Sci U S A. 2005; 102(38): 13544–13549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Lee E, Chuang HY, Kim JW, Ideker T, Lee D. Inferring pathway activity toward precise disease classification. PLoS Comput Biol. 2008; 4(11): e1000217 10.1371/journal.pcbi.1000217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Chuang H, Lee E, Liu Y, Lee D, Ideker T. Network-based classification of breast cancer metastasis. Mol Syst Biol. 2007; 3: 140 10.1038/msb4100180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Basu A, Drame A, Munoz R, Gijsbers R, Debyser Z, De Leon M, et al. Pathway specific gene expression profiling reveals oxidative stress genes potentially regulated by transcription co-activator LEDGF/p75 in prostate cancer cells. Prostate. 2012; 72(6): 597–611. 10.1002/pros.21463 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Bettuzzi S, Davalli P, Astancolle S, Carani C, Madeo B, Tampieri A, et al. Tumor progression is accompanied by significant changes in the levels of expression of polyamine metabolism regulatory genes and clusterin (sulfated glycoprotein 2) in human prostate cancer specimens. Cancer Res. 2000; 60(1): 28–34. [PubMed] [Google Scholar]
- 54. Bettuzzi S, Scaltriti M, Caporali A, Brausi M, D'Arca D, Astancolle S, et al. Successful prediction of prostate cancer recurrence by gene profiling in combination with clinical data: a 5-year follow-up study. Cancer Res. 2003; 63(13): 3469–3472. [PubMed] [Google Scholar]
- 55. Mukherjee R, McGuinness DH, McCall P, Underwood MA, Seywright M, Orange C, et al. Upregulation of MAPK pathway is associated with survival in castrate-resistant prostate cancer. Br J Cancer. 2011; 104(12): 1920–1928. 10.1038/bjc.2011.163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Waalkes S, Simon P, Hennenlotter J, Knapp J, Tezval H, Serth J, et al. Altered expression of Akt signaling pathway parameters in prostate needle biopsies derived from benign, adjacent and cancerous tissue. Oncol Rep. 2010; 23(5): 1257–1260. [DOI] [PubMed] [Google Scholar]
- 57. Campa D, Husing A, Stein A, Dostal L, Boeing H, Pischon T, et al. Genetic variability of the mTOR pathway and prostate cancer risk in the European Prospective Investigation on Cancer (EPIC). PLoS One. 2011; 6(2): e16914 10.1371/journal.pone.0016914 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Kremer CL, Klein RR, Mendelson J, Browne W, Samadzedeh LK, Vanpatten K, et al. Expression of mTOR signaling pathway markers in prostate cancer progression. Prostate. 2006; 66(11): 1203–1212. 10.1002/pros.20410 [DOI] [PubMed] [Google Scholar]
- 59. Xu J, Lowey J, Wiklund F, Sun J, Lindmark F, Hsu FC, et al. The interaction of four genes in the inflammation pathway significantly predicts prostate cancer risk. Cancer Epidemiol Biomarkers Prev. 2005; 14(11 Pt 1): 2563–2568. [DOI] [PubMed] [Google Scholar]
- 60. Creighton CJ. Multiple oncogenic pathway signatures show coordinate expression patterns in human prostate tumors. PLoS One. 2008; 3(3): e1816 10.1371/journal.pone.0001816 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. R Core Team. R: A language and environment for statistical computing Vienna, Austria:R Foundation for Statistical Computing;2014. [Google Scholar]
- 62. Love MI, Huber W, Anders S. Moderated estimation of fold change and dispersion for RNA-seq data with DESeq2. Genome Biol. 2014; 15(12): 550–558. 10.1186/s13059-014-0550-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Mi H, Muruganujan A, Thomas PD. PANTHER in 2013: modeling the evolution of gene function, and other gene attributes, in the context of phylogenetic trees. Nucleic Acids Research. 2013; 41(D1): 08/05/2015-D377-D386. 10.1093/nar/gks1118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Subramanian A, Tamayo P, Mootha VK, Mukherjee S, Ebert BL, Gillette MA, et al. Gene set enrichment analysis: A knowledge-based approach for interpreting genome-wide expression profiles. PNAS. 2005; 102(43): 15545–15550. 10.1073/pnas.0506580102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Kanehisa M, Goto S, Furumichi M, Tanabe M, Hirakawa M. KEGG for representation and analysis of molecular networks involving diseases and drugs. Nucleic Acids Res. 2010; 38(Database issue): D355–60. 10.1093/nar/gkp896 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Tarca AL, Draghici S, Khatri P, Hassan SS, Mittal P, Kim JS, et al. A novel signaling pathway impact analysis. Bioinformatics. 2009; 25(1): 75–82. 10.1093/bioinformatics/btn577 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Tarca AL, Kathri P and Draghici S. SPIA: Signaling Pathway Impact Analysis (SPIA) using combined evidence of pathway over-representation and unusual signaling perturbations. 2013.
- 68. Furuta E, Okuda H, Kobayashi A, Watabe K. Metabolic genes in cancer: their roles in tumor progression and clinical implications. Biochim Biophys Acta. 2010; 1805(2): 141–152. 10.1016/j.bbcan.2010.01.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Robey RB, Weisz J, Kuemmerle NB, Salzberg AC, Berg A, Brown DG, et al. Metabolic reprogramming and dysregulated metabolism: cause, consequence and/or enabler of environmental carcinogenesis? Carcinogenesis. 2015; 36(Suppl 1): S203–S231. 10.1093/carcin/bgv037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Dang CV. Links between metabolism and cancer. Genes Dev. 2012; 26(9): 877–890. 10.1101/gad.189365.112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. DeBerardinis RJ, Lum JJ, Hatzivassiliou G, Thompson CB. The biology of cancer: metabolic reprogramming fuels cell growth and proliferation. Cell Metab. 2008; 7(1): 11–20. 10.1016/j.cmet.2007.10.002 [DOI] [PubMed] [Google Scholar]
- 72. Vander Heiden MG, Cantley LC, Thompson CB. Understanding the Warburg effect: the metabolic requirements of cell proliferation. Science. 2009; 324(5930): 1029–1033. 10.1126/science.1160809 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Hu J, Locasale JW, Bielas JH, O'Sullivan J, Sheahan K, Cantley LC, et al. Heterogeneity of tumor-induced gene expression changes in the human metabolic network. Nat Biotechnol. 2013; 31(6): 522–529. 10.1038/nbt.2530 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Gruss OJ, Vernos I. The mechanism of spindle assembly: functions of Ran and its target TPX2. J Cell Biol. 2004; 166(7): 949–955. 10.1083/jcb.200312112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Kalab P, Heald R. The RanGTP gradient—a GPS for the mitotic spindle. J Cell Sci. 2008; 121(Pt 10): 1577–1586. 10.1242/jcs.005959 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Bischoff FR, Krebber H, Smirnova E, Dong W, Ponstingl H. Co-activation of RanGTPase and inhibition of GTP dissociation by Ran-GTP binding protein RanBP1. EMBO J. 1995; 14(4): 705–715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Zhang MS, Arnaoutov A, Dasso M. RanBP1 governs spindle assembly by defining mitotic Ran-GTP production. Dev Cell. 2014; 31(4): 393–404. 10.1016/j.devcel.2014.10.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Ems-McClung SC, Zheng Y, Walczak CE. Importin alpha/beta and Ran-GTP regulate XCTK2 microtubule binding through a bipartite nuclear localization signal. Mol Biol Cell. 2004; 15(1): 46–57. 10.1091/mbc.E03-07-0454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Nachury MV, Maresca TJ, Salmon WC, Waterman-Storer CM, Heald R, Weis K. Importin ß Is a Mitotic Target of the Small GTPase Ran in Spindle Assembly. Cell. 2001; 104(1): 95–106. 10.1016/S0092-8674(01)00194-5 [DOI] [PubMed] [Google Scholar]
- 80. Wiese C, Wilde A, Moore MS, Adam SA, Merdes A, Zheng Y. Role of importin-beta in coupling Ran to downstream targets in microtubule assembly. Science. 2001; 291(5504): 653–656. [DOI] [PubMed] [Google Scholar]
- 81. Trieselmann N, Armstrong S, Rauw J, Wilde A. Ran modulates spindle assembly by regulating a subset of TPX2 and Kid activities including Aurora A activation. J Cell Sci. 2003; 116(Pt 23): 4791–4798. 10.1242/jcs.00798 [DOI] [PubMed] [Google Scholar]
- 82. Tanenbaum ME, Macurek L, Janssen A, Geers EF, Alvarez-Fernandez M, Medema RH. Kif15 cooperates with eg5 to promote bipolar spindle assembly. Curr Biol. 2009; 19(20): 1703–1711. 10.1016/j.cub.2009.08.027 [DOI] [PubMed] [Google Scholar]
- 83. Silk AD, Holland AJ, Cleveland DW. Requirements for NuMA in maintenance and establishment of mammalian spindle poles. J Cell Biol. 2009; 184(5): 677–690. 10.1083/jcb.200810091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Katayama H, Sasai K, Kloc M, Brinkley BR, Sen S. Aurora kinase-A regulates kinetochore/chromatin associated microtubule assembly in human cells. 2008; 7(17): 2691–2704. [DOI] [PubMed]
- 85. Akhurst RJ, Hata A. Targeting the TGFbeta signalling pathway in disease. Nat Rev Drug Discov. 2012; 11(10): 790–811. 10.1038/nrd3810 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Wrana JL, Attisano L, Wieser R, Ventura F, Massague J. Mechanism of activation of the TGF-beta receptor. Nature. 1994; 370(6488): 341–347. 10.1038/370341a0 [DOI] [PubMed] [Google Scholar]
- 87. Hyytiainen M, Penttinen C, Keski-Oja J. Latent TGF-beta binding proteins: extracellular matrix association and roles in TGF-beta activation. Crit Rev Clin Lab Sci. 2004; 41(3): 233–264. 10.1080/10408360490460933 [DOI] [PubMed] [Google Scholar]
- 88. Nakao A, Imamura T, Souchelnytskyi S, Kawabata M, Ishisaki A, Oeda E, et al. TGF-beta receptor-mediated signalling through Smad2, Smad3 and Smad4. EMBO J. 1997; 16(17): 5353–5362. 10.1093/emboj/16.17.5353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Hayashi H, Abdollah S, Qiu Y, Cai J, Xu YY, Grinnell BW, et al. The MAD-related protein Smad7 associates with the TGFbeta receptor and functions as an antagonist of TGFbeta signaling. Cell. 1997; 89(7): 1165–1173. [DOI] [PubMed] [Google Scholar]
- 90. Fukuchi M, Imamura T, Chiba T, Ebisawa T, Kawabata M, Tanaka K, et al. Ligand-dependent degradation of Smad3 by a ubiquitin ligase complex of ROC1 and associated proteins. Mol Biol Cell. 2001; 12(5): 1431–1443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Chen CR, Kang Y, Siegel PM, Massague J. E2F4/5 and p107 as Smad cofactors linking the TGFbeta receptor to c-myc repression. Cell. 2002; 110(1): 19–32. [DOI] [PubMed] [Google Scholar]
- 92. Kress TR, Sabo A, Amati B. MYC: connecting selective transcriptional control to global RNA production. Nat Rev Cancer. 2015; 15(10): 593–607. 10.1038/nrc3984 [DOI] [PubMed] [Google Scholar]
- 93. Feng XH, Lin X, Derynck R. Smad2, Smad3 and Smad4 cooperate with Sp1 to induce p15(Ink4B) transcription in response to TGF-beta. EMBO J. 2000; 19(19): 5178–5193. 10.1093/emboj/19.19.5178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Black AR, Black JD, Azizkhan-Clifford J. Sp1 and kruppel-like factor family of transcription factors in cell growth regulation and cancer. J Cell Physiol. 2001; 188(2): 143–160. 10.1002/jcp.1111 [DOI] [PubMed] [Google Scholar]
- 95. Kim WY, Sharpless NE. The Regulation of INK4/ARF in Cancer and Aging. Cell. 2006; 127(2): 265–275. 10.1016/j.cell.2006.10.003 [DOI] [PubMed] [Google Scholar]
- 96. Luo J, Yu YP, Cieply K, Lin F, Deflavia P, Dhir R, et al. Gene expression analysis of prostate cancers. Mol Carcinog. 2002; 33(1): 25–35. 10.1002/mc.10018 [DOI] [PubMed] [Google Scholar]
- 97. Chetcuti A, Margan S, Mann S, Russell P, Handelsman D, Rogers J, et al. Identification of differentially expressed genes in organ-confined prostate cancer by gene expression array. Prostate. 2001; 47(2): 132–140. 10.1002/pros.1056 [DOI] [PubMed] [Google Scholar]
- 98. Zhao H, Ramos CF, Brooks JD, Peehl DM. Distinctive gene expression of prostatic stromal cells cultured from diseased versus normal tissues. J Cell Physiol. 2007; 210(1): 111–121. 10.1002/jcp.20828 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Xu J, Stolk JA, Zhang X, Silva SJ, Houghton RL, Matsumura M, et al. Identification of differentially expressed genes in human prostate cancer using subtraction and microarray. Cancer Res. 2000; 60(6): 1677–1682. [PubMed] [Google Scholar]
- 100. Golub TR, Slonim DK, Tamayo P, Huard C, Gaasenbeek M, Mesirov JP, et al. Molecular classification of cancer: class discovery and class prediction by gene expression monitoring. Science. 1999; 286(5439): 531–537. [DOI] [PubMed] [Google Scholar]
- 101. Ramaswamy S, Tamayo P, Rifkin R, Mukherjee S, Yeang CH, Angelo M, et al. Multiclass cancer diagnosis using tumor gene expression signatures. Proc Natl Acad Sci U S A. 2001; 98(26): 15149–15154. 10.1073/pnas.211566398 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Gregg JL, Brown KE, Mintz EM, Piontkivska H, Fraizer GC. Analysis of gene expression in prostate cancer epithelial and interstitial stromal cells using laser capture microdissection. BMC Cancer. 2010; 10: 165-2407-10-165. 10.1186/1471-2407-10-165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Lotan TL, Gurel B, Sutcliffe S, Esopi D, Liu W, Xu J, et al. PTEN protein loss by immunostaining: analytic validation and prognostic indicator for a high risk surgical cohort of prostate cancer patients. Clin Cancer Res. 2011; 17(20): 6563–6573. 10.1158/1078-0432.CCR-11-1244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Chaux A, Peskoe SB, Gonzalez-Roibon N, Schultz L, Albadine R, Hicks J, et al. Loss of PTEN expression is associated with increased risk of recurrence after prostatectomy for clinically localized prostate cancer. Mod Pathol. 2012; 25(11): 1543–1549. 10.1038/modpathol.2012.104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Zeng L, Rowland RG, Lele SM, Kyprianou N. Apoptosis incidence and protein expression of p53, TGF-ß receptor II, p27Kip1, and Smad4 in benign, premalignant, and malignant human prostate1 1Accepted for publication 0, 2003. Hum Pathol. 2004; 35(3): 290–297. 10.1016/j.humpath.2003.11.001 [DOI] [PubMed] [Google Scholar]
- 106. Aitchison AA, Veerakumarasivam A, Vias M, Kumar R, Hamdy FC, Neal DE, et al. Promoter methylation correlates with reduced Smad4 expression in advanced prostate cancer. Prostate. 2008; 68(6): 661–674. 10.1002/pros.20730 [DOI] [PubMed] [Google Scholar]
- 107. Lin B, Ferguson C, White JT, Wang S, Vessella R, True LD, et al. Prostate-localized and androgen-regulated expression of the membrane-bound serine protease TMPRSS2. Cancer Res. 1999; 59(17): 4180–4184. [PubMed] [Google Scholar]
- 108. Vaarala MH, Porvari K, Kyllonen A, Lukkarinen O, Vihko P. The TMPRSS2 gene encoding transmembrane serine protease is overexpressed in a majority of prostate cancer patients: detection of mutated TMPRSS2 form in a case of aggressive disease. Int J Cancer. 2001; 94(5): 705–710. 10.1002/ijc.1526 [DOI] [PubMed] [Google Scholar]
- 109. Lucas JM, Heinlein C, Kim T, Hernandez SA, Malik MS, True LD, et al. The androgen-regulated protease TMPRSS2 activates a proteolytic cascade involving components of the tumor microenvironment and promotes prostate cancer metastasis. Cancer Discov. 2014; 4(11): 1310–1325. 10.1158/2159-8290.CD-13-1010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Dijkstra S, Mulders PF, Schalken JA. Clinical use of novel urine and blood based prostate cancer biomarkers: a review. Clin Biochem. 2014; 47(10–11): 889–896. 10.1016/j.clinbiochem.2013.10.023 [DOI] [PubMed] [Google Scholar]
- 111. Fleming WH, Hamel A, MacDonald R, Ramsey E, Pettigrew NM, Johnston B, et al. Expression of the c-Myc protooncogene in human prostate hyperplasia. Cancer research. 1986; 46(3): 1535–1538. [PubMed] [Google Scholar]
- 112. Buttyan R, Sawczuk IS, Benson MC, Siegal JD, Olsson CA. Enhanced expression of the c-myc protooncogene in high-grade human prostate cancers. Prostate. 1987; 11(4): 327–337. [DOI] [PubMed] [Google Scholar]
- 113. Koh CM, Bieberich CJ, Dang CV, Nelson WG, Yegnasubramanian S, De Marzo AM. MYC and Prostate Cancer. Genes Cancer. 2010; 1(6): 617–628. 10.1177/1947601910379132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114. Hawksworth D, Ravindranath L, Chen Y, Furusato B, Sesterhenn IA, McLeod DG, et al. Overexpression of C-MYC oncogene in prostate cancer predicts biochemical recurrence. Prostate Cancer Prostatic Dis. 2010; 13(4): 311–315. 10.1038/pcan.2010.31 [DOI] [PubMed] [Google Scholar]
- 115. Gurel B, Iwata T, Koh CM, Jenkins RB, Lan F, Van Dang C, et al. Nuclear MYC protein overexpression is an early alteration in human prostate carcinogenesis. Mod Pathol. 2008; 21(9): 1156–1167. 10.1038/modpathol.2008.111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116. Bubendorf L, Kononen J, Koivisto P, Schraml P, Moch H, Gasser TC, et al. Survey of gene amplifications during prostate cancer progression by high-throughout fluorescence in situ hybridization on tissue microarrays. Cancer Res. 1999; 59(4): 803–806. [PubMed] [Google Scholar]
- 117. Jenkins RB, Qian J, Lieber MM, Bostwick DG. Detection of c-myc oncogene amplification and chromosomal anomalies in metastatic prostatic carcinoma by fluorescence in situ hybridization. Cancer Res. 1997; 57(3): 524–531. [PubMed] [Google Scholar]
- 118. Sato H, Minei S, Hachiya T, Yoshida T, Takimoto Y. Fluorescence in situ hybridization analysis of c-myc amplification in stage TNM prostate cancer in Japanese patients. Int J Urol. 2006; 13(6): 761–766. [DOI] [PubMed] [Google Scholar]
- 119. Yang YA, Yu J. EZH2, an epigenetic driver of prostate cancer. Protein Cell. 2013; 4(5): 331–341. 10.1007/s13238-013-2093-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120. Moul JW, Bettencourt M, Sesterhenn IA, Mostofi FK, McLeod DG, Srivastava S, et al. Protein expression of p53, bcl-2, and KI-67 (MIB-1) as prognostic biomarkers in patients with surgically treated, clinically localized prostate cancer. Surgery. 1996; 120(2): 159–167. 10.1016/S0039-6060(96)80283-2 [DOI] [PubMed] [Google Scholar]
- 121. Johnson MI, Robinson MC, Marsh C, Robson CN, Neal DE, Hamdy FC. Expression of Bcl-2, Bax, and p53 in high-grade prostatic intraepithelial neoplasia and localized prostate cancer: relationship with apoptosis and proliferation. Prostate. 1998; 37(4): 223–229. [DOI] [PubMed] [Google Scholar]
- 122. McDonnell TJ, Troncoso P, Brisbay SM, Logothetis C, Chung LW, Hsieh JT, et al. Expression of the protooncogene bcl-2 in the prostate and its association with emergence of androgen-independent prostate cancer. Cancer Res. 1992; 52(24): 6940–6944. [PubMed] [Google Scholar]
- 123. Apakama I, Robinson M, Walter N, Charlton R, Royds J, Fuller C, et al. bcl-2 overexpression combined with p53 protein accumulation correlates with hormone-refractory prostate cancer. Br J Cancer. 1996; 74(8): 1258–1262. 10.1038/bjc.1996.526 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124. Colombel M, Symmans F, Gil S, O'Toole KM, Chopin D, Benson M, et al. Detection of the apoptosis-suppressing oncoprotein bc1-2 in hormone-refractory human prostate cancers. Am J Pathol. 1993; 143(2): 390–400. [PMC free article] [PubMed] [Google Scholar]
- 125. Bubendorf L, Sauter G, Moch H, Jordan P, Blochlinger A, Gasser TC, et al. Prognostic significance of Bcl-2 in clinically localized prostate cancer. Am J Pathol. 1996; 148(5): 1557–1565. [PMC free article] [PubMed] [Google Scholar]
- 126. Mack D, Hacker GW, Hauser-Kronberger G, Frick J, Dietze O. Vasoactive Intestinal Polypeptide (VIP) and Neuropeptide Tyrosine (NPY) in Prostate Carcinoma. Eur J Cancer. 1997; 33(2): 317–318. 10.1016/S0959-8049(96)00402-9 [DOI] [PubMed] [Google Scholar]
- 127. Ueda K, Tatsuguchi A, Saichi N, Toyama A, Tamura K, Furihata M, et al. Plasma low-molecular-weight proteome profiling identified neuropeptide-Y as a prostate cancer biomarker polypeptide. J Proteome Res. 2013; 12(10): 4497–4506. 10.1021/pr400547s [DOI] [PubMed] [Google Scholar]
- 128.Liu A, Furusato B, Ravindranath L, Chen Y, Srikantan V, Mcleod DG, et al. Quantitative analysis of a panel of gene expression in prostate cancer—with emphasis on NPY expression analysis. 2007; 8(12): 853–859. [DOI] [PMC free article] [PubMed]
- 129. Ruscica M, Dozio E, Boghossian S, Bovo G, Martos Riano V, Motta M, et al. Activation of the Y1 receptor by neuropeptide Y regulates the growth of prostate cancer cells. Endocrinology. 2006; 147(3): 1466–1473. [DOI] [PubMed] [Google Scholar]
- 130. Vainio P, Gupta S, Ketola K, Mirtti T, Mpindi JP, Kohonen P, et al. Arachidonic acid pathway members PLA2G7, HPGD, EPHX2, and CYP4F8 identified as putative novel therapeutic targets in prostate cancer. Am J Pathol. 2011; 178(2): 525–536. 10.1016/j.ajpath.2010.10.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131. Vainio P, Lehtinen L, Mirtti T, Hilvo M, Seppanen-Laakso T, Virtanen J, et al. Phospholipase PLA2G7, associated with aggressive prostate cancer, promotes prostate cancer cell migration and invasion and is inhibited by statins. Oncotarget. 2011; 2(12): 1176–1190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132. Zhong W, Peng J, He H, Wu D, Han Z, Bi X, et al. Ki-67 and PCNA expression in prostate cancer and benign prostatic hyperplasia. Clin Invest Med. 2008; 31(1): E8–E15. [DOI] [PubMed] [Google Scholar]
- 133. Thompson SJ, Mellon K, Charlton RG, Marsh C, Robinson M, Neal DE. P53 and Ki-67 immunoreactivity in human prostate cancer and benign hyperplasia. Br J Urol. 1992; 69(6): 609–613. [DOI] [PubMed] [Google Scholar]
- 134. Mucci NR, Rubin MA, Strawderman MS, Montie JE, Smith DC, Pienta KJ. Expression of nuclear antigen Ki-67 in prostate cancer needle biopsy and radical prostatectomy specimens. J Natl Cancer Inst. 2000; 92(23): 1941–1942. [DOI] [PubMed] [Google Scholar]
- 135. Revelos K, Petraki C, Gregorakis A, Scorilas A, Papanastasiou P, Tenta R, et al. p27(kip1) and Ki-67 (MIB1) immunohistochemical expression in radical prostatectomy specimens of patients with clinically localized prostate cancer. In Vivo. 2005; 19(5): 911–920. [PubMed] [Google Scholar]
- 136. Grover SK, Agarwal S, Gupta S, Wadhwa N, Sharma N. Expression of Estrogen Receptor ß and Ki 67 in Benign & Malignant Human Prostate Lesions by Immunohistochemistry. 2015; 21(3): 651–657. 10.1007/s12253-014-9870-y [DOI] [PubMed] [Google Scholar]
- 137.Reis S, Timoszczuk L, Pontes-Junior J, Viana N, Silva I, Dip N, et al. The role of micro RNAs let7c, 100 and 218 expression and their target RAS, C-MYC, BUB1, RB, SMARCA5, LAMB3 and Ki-67 in prostate cancer. 2013; 68(5): 652–657. [DOI] [PMC free article] [PubMed]
- 138. Tamboli P, Amin MB, Schultz DS, Linden MD, Kubus J. Comparative analysis of the nuclear proliferative index (Ki-67) in benign prostate, prostatic intraepithelial neoplasia, and prostatic carcinoma. Mod Pathol. 1996; 9(10): 1015–1019. [PubMed] [Google Scholar]
- 139. Van der Kwast TH. Prognostic prostate tissue biomarkers of potential clinical use. Virchows Arch. 2014; 464(3): 293–300. 10.1007/s00428-014-1540-7 [DOI] [PubMed] [Google Scholar]
- 140. Remo A, Pancione M, Zanella C, Manfrin E. p16 Expression in Prostate Cancer and Nonmalignant Lesions: Novel Findings and Review of the Literature. Appl Immunohistochem Mol Morphol. 2015; 10.1097/PAI.0000000000000171 [DOI] [PubMed] [Google Scholar]
- 141. Royuela M, De Miguel MP, Bethencourt FR, Fraile B, Arenas MI, Paniagua R. IL-2, its receptors, and bcl-2 and bax genes in normal, hyperplastic and carcinomatous human prostates: immunohistochemical comparative analysis. Growth Factors. 2000; 18(2): 135–146. [DOI] [PubMed] [Google Scholar]
- 142. Royuela M, De Miguel MP, Bethencourt FR, Sanchez-Chapado M, Fraile B, Paniagua R. Transforming growth factor beta 1 and its receptor types I and II. Comparison in human normal prostate, benign prostatic hyperplasia, and prostatic carcinoma. Growth Factors. 1998; 16(2): 101–110. [DOI] [PubMed] [Google Scholar]
- 143. Cardillo MR, Petrangeli E, Perracchio L, Salvatori L, Ravenna L, Di Silverio F. Transforming growth factor-beta expression in prostate neoplasia. Anal Quant Cytol Histol. 2000; 22(1): 1–10. [PubMed] [Google Scholar]
- 144. Shariat SF, Menesses-Diaz A, Kim IY, Muramoto M, Wheeler TM, Slawin KM. Tissue expression of transforming growth factor-beta1 and its receptors: correlation with pathologic features and biochemical progression in patients undergoing radical prostatectomy. Urology. 2004; 63(6): 1191–1197. 10.1016/j.urology.2003.12.015 [DOI] [PubMed] [Google Scholar]
- 145. Perry KT, Anthony CT, Steiner MS. Immunohistochemical localization of TGF beta 1, TGF beta 2, and TGF beta 3 in normal and malignant human prostate. Prostate. 1997; 33(2): 133–140. [DOI] [PubMed] [Google Scholar]
- 146. Gerdes MJ, Larsen M, McBride L, Dang TD, Lu B, Rowley DR. Localization of transforming growth factor-beta1 and type II receptor in developing normal human prostate and carcinoma tissues. J Histochem Cytochem. 1998; 46(3): 379–388. [DOI] [PubMed] [Google Scholar]
- 147. Truong LD, Kadmon D, McCune BK, Flanders KC, Scardino PT, Thompson TC. Association of transforming growth factor-ß1 with prostate cancer: An immunohistochemical study. Hum Pathol. 1993; 24(1): 4–9. 10.1016/0046-8177(93)90055-L [DOI] [PubMed] [Google Scholar]
- 148. Djonov V, Ball RK, Graf S, Mottaz AE, Arnold AM, Flanders K, et al. Transforming growth factor-beta 3 is expressed in nondividing basal epithelial cells in normal human prostate and benign prostatic hyperplasia, and is no longer detectable in prostate carcinoma. Prostate. 1997; 31(2): 103–109. [DOI] [PubMed] [Google Scholar]
- 149. Twillie DA, Eisenberger MA, Carducci MA, Hseih W, Kim WY, Simons JW. Interleukin-6: A candidate mediator of human prostate cancer morbidity. Urology. 1995; 45(3): 542–549. 10.1016/S0090-4295(99)80034-X [DOI] [PubMed] [Google Scholar]
- 150. Hobisch A, Rogatsch H, Hittmair A, Fuchs D, Bartsch G Jr, Klocker H, et al. Immunohistochemical localization of interleukin-6 and its receptor in benign, premalignant and malignant prostate tissue. J Pathol. 2000; 191(3): 239–244. [DOI] [PubMed] [Google Scholar]
- 151. Park JI, Lee MG, Cho K, Park BJ, Chae KS, Byun DS, et al. Transforming growth factor-beta1 activates interleukin-6 expression in prostate cancer cells through the synergistic collaboration of the Smad2, p38-NF-kappaB, JNK, and Ras signaling pathways. Oncogene. 2003; 22(28): 4314–4332. 10.1038/sj.onc.1206478 [DOI] [PubMed] [Google Scholar]
- 152. Bouraoui Y, Ricote M, Garcia-Tunon I, Rodriguez-Berriguete G, Touffehi M, Rais NB, et al. Pro-inflammatory cytokines and prostate-specific antigen in hyperplasia and human prostate cancer. Cancer Detect Prev. 2008; 32(1): 23–32. 10.1016/j.cdp.2008.02.007 [DOI] [PubMed] [Google Scholar]
- 153. Mechergui YB, Ben Jemaa A, Mezigh C, Fraile B, Ben Rais N, Paniagua R, et al. The profile of prostate epithelial cytokines and its impact on sera prostate specific antigen levels. Inflammation. 2009; 32(3): 202–210. 10.1007/s10753-009-9121-7 [DOI] [PubMed] [Google Scholar]
- 154. Lee SO, Lou W, Hou M, de Miguel F, Gerber L, Gao AC. Interleukin-6 promotes androgen-independent growth in LNCaP human prostate cancer cells. Clin Cancer Res. 2003; 9(1): 370–376. [PubMed] [Google Scholar]
- 155. D E Drachenberg A.-A.A. Elgamal,R Rowbotham,M Peterson,G P Murphy. Circulating levels of interleukin-6 in patients with hormone refractory prostate cancer. The Prostate. 1999; 41(2): 127–133. [DOI] [PubMed] [Google Scholar]
- 156. Akimoto S, Okumura A, Fuse H. Relationship between serum levels of interleukin-6, tumor necrosis factor-a and bone turnover markers in prostate cancer patients. Endocrine journal. 1998; 45(2): 183–189. [DOI] [PubMed] [Google Scholar]
- 157. Adler HL, Mccurdy MA, Kattan MW, Timme TL, Scardino PT, Thompson TC. Elevated Levels of Circulating Interleukin-6 and Transforming Growth Factor-Beta 1 in Patients with Metastatic Prostatic Carcinoma. J Urol. 1999; 161(1): 182–187. 10.1016/S0022-5347(01)62092-5 [DOI] [PubMed] [Google Scholar]
- 158. Wise GJ, Marella VK, Talluri G, Shirazian D. Cytokine variations in patients with hormone treated prostate cancer. J Urol. 2000; 164(3 Pt 1): 722–725. [DOI] [PubMed] [Google Scholar]
- 159. Shariat SF, Andrews B, Kattan MW, Kim J, Wheeler TM, Slawin KM. Plasma levels of interleukin-6 and its soluble receptor are associated with prostate cancer progression and metastasis. Urology. 2001; 58(6): 1008–1015. 10.1016/S0090-4295(01)01405-4 [DOI] [PubMed] [Google Scholar]
- 160. Michalaki V, Syrigos K, Charles P, Waxman J. Serum levels of IL-6 and TNF-alpha correlate with clinicopathological features and patient survival in patients with prostate cancer. Br J Cancer. 2004; 90(12): 2312–2316. 10.1038/sj.bjc.6601814 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161. George DJ, Halabi S, Shepard TF, Sanford B, Vogelzang NJ, Small EJ, et al. The prognostic significance of plasma interleukin-6 levels in patients with metastatic hormone-refractory prostate cancer: results from cancer and leukemia group B 9480. Clin Cancer Res. 2005; 11(5): 1815–1820. [DOI] [PubMed] [Google Scholar]
- 162. Nakashima J, Tachibana M, Horiguchi Y, Oya M, Ohigashi T, Asakura H, et al. Serum interleukin 6 as a prognostic factor in patients with prostate cancer. Clin Cancer Res. 2000; 6(7): 2702–2706. [PubMed] [Google Scholar]
- 163. Ricote M, Garcia-Tunon I, Bethencourt FR, Fraile B, Paniagua R, Royuela M. Interleukin-1 (IL-1alpha and IL-1beta) and its receptors (IL-1RI, IL-1RII, and IL-1Ra) in prostate carcinoma. Cancer. 2004; 100(7): 1388–1396. 10.1002/cncr.20142 [DOI] [PubMed] [Google Scholar]
- 164. Liu Q, Russell MR, Shahriari K, Jernigan DL, Lioni MI, Garcia FU, et al. Interleukin-1 Promotes Skeletal Colonization and Progression of Metastatic Prostate Cancer Cells with Neuroendocrine Features. Cancer Res. 2013; 73(11): 3297–3305. 10.1158/0008-5472.CAN-12-3970 [DOI] [PubMed] [Google Scholar]
- 165. Aaltomaa S, Lipponen P, Eskelinen M, Ala-Opas M, Kosma VM. Prognostic value and expression of p21(waf1/cip1) protein in prostate cancer. Prostate. 1999; 39(1): 8–15. [DOI] [PubMed] [Google Scholar]
- 166. Omar EA, Behlouli H, Chevalier S, Aprikian AG. Relationship of p21(WAF-I) protein expression with prognosis in advanced prostate cancer treated by androgen ablation. Prostate. 2001; 49(3): 191–199. 10.1002/pros.1134 [DOI] [PubMed] [Google Scholar]
- 167. Rigaud J, Tiguert R, Decobert M, Hovington H, Latulippe E, Laverdiere J, et al. Expression of p21 cell cycle protein is an independent predictor of response to salvage radiotherapy after radical prostatectomy. Prostate. 2004; 58(3): 269–276. 10.1002/pros.10329 [DOI] [PubMed] [Google Scholar]
- 168. Gotoh A, Kao C, Ko S, Hamada K, Liu T, Chung LWK. Cytotoxic Effects of Recombinant Adenovirus p53 and Cell Cycle Regulator Genes (p21 sup WAF1/CIP1 and p16 sup CDKN4) in Human Prostate Cancers. J Urol. 1997; 158(2): 636–641. 10.1016/S0022-5347(01)64574-9 [DOI] [PubMed] [Google Scholar]
- 169. Green MM, Hiley CT, Shanks JH, Bottomley IC, West CM, Cowan RA, et al. Expression of vascular endothelial growth factor (VEGF) in locally invasive prostate cancer is prognostic for radiotherapy outcome. Int J Radiat Oncol Biol Phys. 2007; 67(1): 84–90. [DOI] [PubMed] [Google Scholar]
- 170. Mori R, Dorff TB, Xiong S, Tarabolous CJ, Ye W, Groshen S, et al. The relationship between proangiogenic gene expression levels in prostate cancer and their prognostic value for clinical outcomes. Prostate. 2010; 70(15): 1692–1700. 10.1002/pros.21204 [DOI] [PubMed] [Google Scholar]
- 171. Anees M, Horak P, El-Gazzar A, Susani M, Heinze G, Perco P, et al. Recurrence-free survival in prostate cancer is related to increased stromal TRAIL expression. Cancer. 2011; 117(6): 1172–1182. 10.1002/cncr.25504 [DOI] [PubMed] [Google Scholar]
- 172. Sanlioglu AD, Koksal IT, Ciftcioglu A, Baykara M, Luleci G, Sanlioglu S. Differential Expression of TRAIL and its Receptors in Benign and Malignant Prostate Tissues. J Urol. 2007; 177(1): 359–364. 10.1016/j.juro.2006.08.087 [DOI] [PubMed] [Google Scholar]
- 173. Nunez C, Cansino JR, Bethencourt F, Perez-Utrilla M, Fraile B, Martinez-Onsurbe P, et al. TNF/IL-1/NIK/NF-kappa B transduction pathway: a comparative study in normal and pathological human prostate (benign hyperplasia and carcinoma). Histopathology. 2008; 53(2): 166–176. 10.1111/j.1365-2559.2008.03092.x [DOI] [PubMed] [Google Scholar]
- 174. Zhang M, Zhang L, Zou J, Yao C, Xiao H, Liu Q, et al. Evaluating reproducibility of differential expression discoveries in microarray studies by considering correlated molecular changes. Bioinformatics. 2009; 25(13): 1662–1668. 10.1093/bioinformatics/btp295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175. Moore JD. The Ran-GTPase and cell-cycle control. Bioessays. 2001; 23(1): 77–85. [DOI] [PubMed] [Google Scholar]
- 176. Clarke PR, Zhang C. Spatial and temporal coordination of mitosis by Ran GTPase. Nat Rev Mol Cell Biol. 2008; 9(6): 464–477. 10.1038/nrm2410 [DOI] [PubMed] [Google Scholar]
- 177. Abe H, Kamai T, Shirataki H, Oyama T, Arai K, Yoshida K. High expression of Ran GTPase is associated with local invasion and metastasis of human clear cell renal cell carcinoma. Int J Cancer. 2008; 122(10): 2391–2397. 10.1002/ijc.23400 [DOI] [PubMed] [Google Scholar]
- 178. Ouellet V, Provencher DM, Maugard CM, Le Page C, Ren F, Lussier C, et al. Discrimination between serous low malignant potential and invasive epithelial ovarian tumors using molecular profiling. Oncogene. 2005; 24(29): 4672–4687. [DOI] [PubMed] [Google Scholar]
- 179. Ouellet V, Guyot MC, Le Page C, Filali-Mouhim A, Lussier C, Tonin PN, et al. Tissue array analysis of expression microarray candidates identifies markers associated with tumor grade and outcome in serous epithelial ovarian cancer. Int J Cancer. 2006; 119(3): 599–607. 10.1002/ijc.21902 [DOI] [PubMed] [Google Scholar]
- 180. Hung KE, Faca V, Song K, Sarracino DA, Richard LG, Krastins B, et al. Comprehensive proteome analysis of an Apc mouse model uncovers proteins associated with intestinal tumorigenesis. Cancer Prev Res (Phila). 2009; 2(3): 224–233. 10.1158/1940-6207.CAPR-08-0153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181. Xia F, Lee CW, Altieri DC. Tumor cell dependence on Ran-GTP-directed mitosis. Cancer Res. 2008; 68(6): 1826–1833. 10.1158/0008-5472.CAN-07-5279 [DOI] [PubMed] [Google Scholar]
- 182. Azuma K, Sasada T, Takedatsu H, Shomura H, Koga M, Maeda Y, et al. Ran, a small GTPase gene, encodes cytotoxic T lymphocyte (CTL) epitopes capable of inducing HLA-A33-restricted and tumor-reactive CTLs in cancer patients. Clin Cancer Res. 2004; 10(19): 6695–6702. [DOI] [PubMed] [Google Scholar]
- 183. Barres V, Ouellet V, Lafontaine J, Tonin PN, Provencher DM, Mes-Masson AM. An essential role for Ran GTPase in epithelial ovarian cancer cell survival. Mol Cancer. 2010; 9: 272 10.1186/1476-4598-9-272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184. Kurisetty VV, Johnston PG, Johnston N, Erwin P, Crowe P, Fernig DG, et al. RAN GTPase is an effector of the invasive/metastatic phenotype induced by osteopontin. Oncogene. 2008; 27(57): 7139–7149. 10.1038/onc.2008.325 [DOI] [PubMed] [Google Scholar]
- 185. Katayama H, Brinkley WR, Sen S. The Aurora kinases: role in cell transformation and tumorigenesis. Cancer Metastasis Rev. 2003; 22(4): 451–464. [DOI] [PubMed] [Google Scholar]
- 186. Vainio P, Mpindi JP, Kohonen P, Fey V, Mirtti T, Alanen KA, et al. High-throughput transcriptomic and RNAi analysis identifies AIM1, ERGIC1, TMED3 and TPX2 as potential drug targets in prostate cancer. PLoS One. 2012; 7(6): e39801 10.1371/journal.pone.0039801 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187. Neumayer G, Belzil C, Gruss OJ, Nguyen MD. TPX2: of spindle assembly, DNA damage response, and cancer. Cell Mol Life Sci. 2014; 71(16): 3027–3047. 10.1007/s00018-014-1582-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188. Carter SL, Eklund AC, Kohane IS, Harris LN, Szallasi Z. A signature of chromosomal instability inferred from gene expression profiles predicts clinical outcome in multiple human cancers. Nat Genet. 2006; 38(9): 1043–1048. [DOI] [PubMed] [Google Scholar]
- 189. Pannu V, Rida PC, Ogden A, Turaga RC, Donthamsetty S, Bowen NJ, et al. HSET overexpression fuels tumor progression via centrosome clustering-independent mechanisms in breast cancer patients. Oncotarget. 2015; 6(8): 6076–6091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190. Li P, Yu X, Ge K, Melamed J, Roeder RG, Wang Z. Heterogeneous Expression and Functions of Androgen Receptor Co-Factors in Primary Prostate Cancer. 2002; 161(4): 1467–1474. 10.1016/S0002-9440(10)64422-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191. Hsiao P-, Lin D-, Nakao R, Chang C. The Linkage of Kennedy's Neuron Disease to ARA24, the First Identified Androgen Receptor Polyglutamine Region-associated Coactivator. J Biol Chem. 1999; 274(29): 20229–20234. 10.1074/jbc.274.29.20229 [DOI] [PubMed] [Google Scholar]
- 192. Harada N, Ohmori Y, Yamaji R, Higashimura Y, Okamoto K, Isohashi F, et al. ARA24/Ran enhances the androgen-dependent NH2- and COOH-terminal interaction of the androgen receptor. Biochem Biophys Res Commun. 2008; 373(3): 373–377. 10.1016/j.bbrc.2008.06.024 [DOI] [PubMed] [Google Scholar]
- 193. Heldin CH, Landstrom M, Moustakas A. Mechanism of TGF-beta signaling to growth arrest, apoptosis, and epithelial-mesenchymal transition. Curr Opin Cell Biol. 2009; 21(2): 166–176. 10.1016/j.ceb.2009.01.021 [DOI] [PubMed] [Google Scholar]
- 194. Blobe GC, Schiemann WP, Lodish HF. Role of transforming growth factor beta in human disease. N Engl J Med. 2000; 342(18): 1350–1358. 10.1056/NEJM200005043421807 [DOI] [PubMed] [Google Scholar]
- 195. Massague J. TGFbeta in Cancer. Cell. 2008; 134(2): 215–230. 10.1016/j.cell.2008.07.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196. Ravitz MJ, Wenner CE. Cyclin-dependent kinase regulation during G1 phase and cell cycle regulation by TGF-beta. Adv Cancer Res. 1997; 71: 165–207. [DOI] [PubMed] [Google Scholar]
- 197. Aalinkeel R, Nair MP, Sufrin G, Mahajan SD, Chadha KC, Chawda RP, et al. Gene expression of angiogenic factors correlates with metastatic potential of prostate cancer cells. Cancer Res. 2004; 64(15): 5311–5321. 10.1158/0008-5472.CAN-2506-2 [DOI] [PubMed] [Google Scholar]
- 198. Wan Y, Yang M, Kolattukudy S, Stark GR, Lu T. Activation of cAMP-responsive-element-binding protein by PI3 kinase and p38 MAPK is essential for elevated expression of transforming growth factor beta2 in cancer cells. J Interferon Cytokine Res. 2010; 30(9): 677–681. 10.1089/jir.2009.0117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199. Dallas SL, Zhao S, Cramer SD, Chen Z, Peehl DM, Bonewald LF. Preferential production of latent transforming growth factor beta-2 by primary prostatic epithelial cells and its activation by prostate-specific antigen. J Cell Physiol. 2005; 202(2): 361–370. 10.1002/jcp.20147 [DOI] [PubMed] [Google Scholar]
- 200. Kim IY, Ahn HJ, Zelner DJ, Shaw JW, Lang S, Kato M, et al. Loss of expression of transforming growth factor beta type I and type II receptors correlates with tumor grade in human prostate cancer tissues. Clin Cancer Res. 1996; 2(8): 1255–1261. [PubMed] [Google Scholar]
- 201. Kim IY, Ahn HJ, Lang S, Oefelein MG, Oyasu R, Kozlowski JM, et al. Loss of expression of transforming growth factor-beta receptors is associated with poor prognosis in prostate cancer patients. Clin Cancer Res. 1998; 4(7): 1625–1630. [PubMed] [Google Scholar]
- 202. Wikstrom P, Stattin P, Franck-Lissbrant I, Damber JE, Bergh A. Transforming growth factor beta1 is associated with angiogenesis, metastasis, and poor clinical outcome in prostate cancer. Prostate. 1998; 37(1): 19–29. [DOI] [PubMed] [Google Scholar]
- 203. Shariat SF, Kattan MW, Traxel E, Andrews B, Zhu K, Wheeler TM, et al. Association of pre- and postoperative plasma levels of transforming growth factor beta(1) and interleukin 6 and its soluble receptor with prostate cancer progression. Clin Cancer Res. 2004; 10(6): 1992–1999. [DOI] [PubMed] [Google Scholar]
- 204. Ajiboye S, Sissung TM, Sharifi N, Figg WD. More than an accessory: implications of type III transforming growth factor-ß receptor loss in prostate cancer. BJU Int. 2010; 105(7): 913–916. 10.1111/j.1464-410X.2009.08999.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205. Lucia MS, Sporn MB, Roberts AB, Stewart LV, Danielpour D. The role of transforming growth factor-beta1, -beta2, and -beta3 in androgen-responsive growth of NRP-152 rat prostatic epithelial cells. J Cell Physiol. 1998; 175(2): 184–192. [DOI] [PubMed] [Google Scholar]
- 206. Zhang YE. Non-Smad pathways in TGF-beta signaling. Cell Res. 2009; 19(1): 128–139. 10.1038/cr.2008.328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207. Zavadil J, Bitzer M, Liang D, Yang YC, Massimi A, Kneitz S, et al. Genetic programs of epithelial cell plasticity directed by transforming growth factor-beta. Proc Natl Acad Sci U S A. 2001; 98(12): 6686–6691. 10.1073/pnas.111614398 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208. Savli H, Szendroi A, Romics I, Nagy B. Gene network and canonical pathway analysis in prostate cancer: a microarray study. Exp Mol Med. 2008; 40(2): 176–185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209. Jia P, Liu Y, Zhao Z. Integrative pathway analysis of genome-wide association studies and gene expression data in prostate cancer. BMC Syst Biol. 2012; 6 Suppl 3: S3–S13. 10.1186/1752-0509-6-S3-S13 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Differentially expressed genes are highlighted in red.
(PNG)
Differentially expressed genes are highlighted in red.
(PNG)
Differentially expressed genes are highlighted in red.
(PNG)
This file includes the RNAseq expression data for the 225 age- and stage-matched prostate cancer non-malignant and tumor samples downloaded from The Cancer Genome Atlas and used for the analyses presented in this work.
(XLSX)
This is the set of KEGG pathways used in Gene Set Enrichment Analysis and Signaling Pathway Impact Analysis. Pathways likely to have little relevance to prostate cancer (e.g. parasitic, bacterial, and viral infectious diseases, substance dependencies, and specific immune, neurodegenerative, and cardiovascular diseases) have been excluded.
(XLSX)
A total of 11,115 genes and transcripts were differentially expressed according to DESeq2 analysis using Wald statistics. All statistical parameters plus the calculated log2 fold change are presented.
(XLSX)
Complete results of DESeq2 analysis with statistical parameters and calculated log2 fold change.
(XLSX)
Complete classification based on PANTHER protein class, GO Molecular Function and GO Biological Process terms.
(XLSX)
This is the full pathway overrepresentation analysis of protein class and GO Biological Process categories among DEGs from the dataset.
(XLSX)
(XLSX)
These genes and transcripts from the evaluated TCGA dataset contribute to the enrichment of the KEGG Calcium Signaling Pathway in non-malignant samples.
(XLSX)
(XLSX)
These genes and transcripts from the evaluated TCGA dataset contribute to the enrichment of the KEGG Calcium Signaling Pathway in non-malignant samples.
(XLSX)
These genes and transcripts from the evaluated TCGA dataset contribute to the enrichment of the KEGG Calcium Signaling Pathway in non-malignant samples.
(XLSX)
These genes and transcripts from the evaluated TCGA dataset contribute to the enrichment of the KEGG Calcium Signaling Pathway in non-malignant samples.
(XLSX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.