Abstract
Objective
We examined the interdependent, dyadic, mental health of adolescent and young adult (AYA) cancer patients and their caregivers. Our aims were as follows: (1) to investigate the degree to which patients' and caregivers' subjective perceptions of illness severity are congruent with objective severity (i.e., medical indicators), (2) to compare patients' and caregivers' subjective perceptions of illness severity and cancer-related posttraumatic stress symptoms (PTSS), and (3) to evaluate whether subjective perceptions of illness severity are linked to patients' and caregivers' cancer-related PTSS.
Methods
The AYA cancer patients (n = 110; ages 12–24 years; 52% male) undergoing active treatment at an outpatient clinic and their caregivers (n = 110; 97% parents; ages 24–68 years; 89% female) independently reported their PTSS and subjective illness severity.
Results
Overall, neither patients' nor caregivers' reports of subjective illness severity were associated with objective illness severity. Caregivers reported higher PTSS than did patients and higher illness severity than younger, but not older, patients. Actor–partner interdependence model analyses indicated that AYA patients' subjective illness severity is the strongest predictor of their own PTSS and is a significant correlate of their caregivers' PTSS. Caregivers' subjective illness severity is associated with their own PTSS only. Results remained robust after controlling for demographic and illness characteristics.
Conclusions
The AYA patients' and caregivers' illness perceptions are distinct from each other and from objective medical indicators of illness severity. Patients' reports of subjective illness severity may be a marker for their own and their caregivers' mental health. Patient care and efficacious psychosocial interventions may require consideration of both patients' and caregivers' subjective perceptions of illness severity.
Background
Over 70,000 adolescents and young adults (AYAs), typically defined between the ages of 15 and 39 years, are newly diagnosed with cancer in the USA each year [1], yet they remain an understudied patient population. AYA cancer patients have not experienced the same increase in survival rates nor quality of life as their younger and older counterparts [2]. In addition, they bring to the cancer experience several unique psychosocial circumstances [3]. Along with illness-related stressors typically experienced by cancer patients (e.g., frequent medical visits and fatigue), AYAs face rapid social, biological, and cognitive changes because of their developmental life stage [4]. Young AYA patients may also have limited self-sufficiency, legal authority, and self-regulation skills. Combined, these factors may render AYA patients especially reliant on their caregiver (typically, a parent). As patients and caregivers manage the demands of the illness together, their social and leisure activities may be restricted [5], and their relationship with one another may serve as the primary social context in which they experience, cope with, and adjust to the illness [6]. The present study sought to investigate the shared cancer experience of AYA patients and their primary caregivers in light of their interdependent relationship by using a dyadic framework in which they are considered as a single unit. Understanding AYA patients and their caregivers as an intertwined ‘psychological system’ [7] has important implications for effective disease management [8] and patient functioning [9].
Growing evidence indicates that young cancer patients and their caregivers experience illness-related posttraumatic stress symptoms (PTSS), including repeated disturbing thoughts about the illness, avoidance of illness-related discussions, and hyperarousal [10-12]. PTSS may present during the initial diagnosis period [13] and beyond [14] and may hinder patients' medical care (e.g., lead to noncompliance). PTSS may also be experienced by caregivers, impeding their ability to provide for patients' emotional and practical needs, make treatment decisions, and oversee adherence to lifestyle regimens that AYA patients are unable to accomplish on their own [13]. Nevertheless, even though patients and caregivers go through cancer together and technically are coping with the same illness (the patient's cancer), they can experience different illness-related psychological reactions (e.g., depression and anxiety) [15,16] or develop distinct attitudes and ideas about it [17]. That is, both patients and caregivers can integrate and process information from various aspects of the illness in their own way, thereby attributing their own meaning to it [18]. Although both are exposed to the same objective clinical indicators of its severity (e.g., cancer prognosis), patients and caregivers may also develop distinct emotional and cognitive conceptualizations about the illness (e.g., its expected duration). Combined, these conceptualizations make up their subjective perceptions of illness severity, hereto called subjective illness severity.
Consistent evidence demonstrates the importance of these perceptions for patients' and caregivers' psychological functioning [19,20] and patients' treatment outcomes, adherence, and healthcare utilization [21,22]. Although the role of subjective illness severity in patient–caregiver dyads is less well researched, it is extremely important. Given their shared cancer experience, patients and caregivers likely are continually exposed to one another's subjective illness severity, which may cross over (contribute) to each other's psychological health. For instance, even if patients do not perceive their illness as particularly severe, they may experience more PTSS if their caregiver's subjective illness severity is high. Identifying factors that contribute to patients' and caregivers' mental health is crucial for designing effective interventions that target the appropriate dyad member(s).
A sparse literature, based mostly on adult dyads, suggests that caregivers' subjective illness severity is important for patients' psychological adjustment [23,24], social functioning, and vitality [25]. Limited research conducted on young patients mimics these findings, showing links between caregivers' subjective illness severity and psychological distress among pediatric cancer patients [26] and adolescents with atopic eczema [27]. However, as these investigations studied other patient populations or other dyads (e.g., spouses), their findings may not translate to AYA cancer patient–caregiver dyads [3,4]. Adolescence and young adulthood are sensitive developmental periods during which interpersonal relationships are rapidly and frequently shifting, identities are formed, and autonomy and independence are sought [4]. This may make AYA patients' dependence on their caregiver, as well as the caregiver's attempts to protect and guide their child through the illness, uniquely challenging, creating dynamics unlike those seen in other dyads. Moreover, little is known about caregivers' psychological health in relation to patients' subjective illness severity because most studies focus solely on patients' outcomes. Finally, the magnitude of the associations between subjective illness severity and PTSS within dyads is an important issue that has not been adequately assessed. Knowing the relative importance of patients' and caregivers' subjective illness severity for their own and each other's PTSS is critical for identifying the most influential source of distress within dyads. With this information, healthcare providers can offer additional reassurance or clarification about the illness.
The present study is the first to examine subjective illness severity and PTSS in AYA patient–caregiver dyads using the actor–partner interdependence model (APIM) [28]. The APIM is an advanced statistical approach that treats the dyad (instead of its constituents) as the unit of analysis (see Online Supplement for additional details). This is ideal for examining individuals whose experiences are unique yet interrelated. It is also ideal for our purposes because it can help identify which dyad member's perceptions contribute to whose PTSS and can compare the relative importance of each dyad member's perceptions for his or her own and each other's PTSS. This has important implications for clinical intervention because interpreting illness-related adjustment in either dyad member without the other provides an incomplete picture of factors contributing to their psychological outcomes.
The aim of this study was to contribute to the understanding of the shared cancer experience of AYA patient–caregiver dyads so as to help ensure that they receive optimal healthcare and service provisions. To do so, we tested the following hypotheses in 110 dyads (220 independent self-reports) based on existing research: (1) patients' and caregivers' levels of subjective illness severity will differ as will their levels of PTSS, (2) patients' and caregivers' subjective illness severity will be correlated with their own PTSS, and (3) patients' and caregivers' subjective illness severity will be correlated with each other's PTSS. We also addressed two important questions in need of attention. First, are patients' and caregivers' own or each other's subjective illness severity stronger predictors of their PTSS? Second, do patients' and caregivers' subjective illness severity differ from objective indicators of illness severity (healthcare utilization days, medical costs, and risk prognosis)?
In addition, we explored the role of demographics (gender, age, and ethnicity), patients' diagnostic characteristics (cancer type and time since diagnosis), and objective indicators of illness severity since they may impact patients' and caregivers' reports of subjective illness severity as well as the degree to which they are susceptible to each other's perceptions. For instance, young men may have distinct relationships with their parents compared with young women [29], and ethnic differences have been observed in families' health beliefs about young patients' cancer (e.g., causes attributed to the illness) [30]. Adolescence (ages 12–17) and young adulthood (ages 18–24) are marked by differences in power of authority in relation to caregivers [4]; thus younger (versus older) patients are likely to be more reliant on and perhaps more influenced by their caregivers. Regarding patients' diagnostic characteristics and objective illness severity, research linking them to psychological health is sparse, and the findings are mixed [31–33]. The extant literature warranted further exploration of these variables.
Methods
Procedures
Participants were recruited from the outpatient cancer clinic and outpatient infusion center at Children's Hospital of Orange County. AYA patients aged between 12 and 24 years were eligible if they were receiving active or follow-up treatment. The primary caregiver (designated by the family) and the patient were informed of the study and were invited to participate. All had to be English or Spanish speaking. Professional translators were used for preparation of all bilingual study materials, and bilingual speakers were used for consenting procedures for Spanish-speaking participants. Informed consent was obtained from each caregiver/guardian and patient ≥18 years; patients <18 years provided assent.
Based on the oncology unit roster, 387 potentially eligible AYA patients were identified. Research personnel approached 194 dyads during the fielding period and consented 133 dyads, of which 86% (n=110) provided completed surveys from both patient and caregiver (N=220). There were no significant differences in demographics or patient illness characteristics between eligible dyads who enrolled in the study versus those who did not (ps> 0.05).
Patients and caregivers independently completed a survey and were each compensated with a $25 gift card. The study was conducted after approval by all relevant institutional review boards and in accord with an assurance filed with and approved by the Department of Health and Human Services. (See Online Supplement for additional recruitment and procedural details.)
Adolescent and young adult patient and caregiver measures
Demographics
Participants reported age, gender, and ethnicity; caregivers reported highest education level, marital status, and annual household income. Because of their distinct developmental profiles, a dichotomous variable was used for patients' age (18-24 years of age coded 1; 12-17 years of age coded 0). Dyads' ethnicity (Caucasian coded 1; non-Caucasian coded 0) was based on the caregiver's response (using patient's response yielded similar results).
Diagnostic characteristics
Medical records were used to code cancer type and time since diagnosis (based on the date of diagnosis and the date the patient completed the survey).
Objective illness severity
Three measures of objective illness severity were recorded (higher numbers indicate greater objective severity). Healthcare utilization, collected from hospital billing records, was based on the total number of days the patient received any outpatient, inpatient, and/or intensive care unit services. Medical costs were calculated based on the total healthcare services billed to the hospital (from all expenses procured). A monthly average was calculated for healthcare utilization and medical costs across the 12 months prior to survey completion (or since the patient's time of diagnosis if diagnosed <12 months). To ease interpretation of coefficients, dollar amounts were scaled; one unit change is equal to $1000.
As no standardized measure exists across different types of cancer, the attending oncologist, blind to participants' survey results, reviewed each patient's medical chart to classify him or her into a low (coded 0) or high (coded 1) risk prognosis group based on cancer diagnosis, stage, and treatment. All recurring cancers and solid tumors with stage 4 were classified as high risk; leukemia cases were classified based on eligibility criteria for enrollment in Children's Oncology Group studies (see www.childrensoncologygroup.org).
Subjective illness severity
Six items from the Brief Illness Perception Questionnaire (Brief IPQ) [34] were used as an index of subjective illness severity. Participants rated six items on a scale from 0 to 10; higher scores indicate longer perceived illness duration, greater control over the illness, more effective illness treatment, greater symptoms, greater concern over the illness, and better understanding of the illness. Items were combined to form a composite score; some items were reverse coded so that higher scores indicate higher perceived illness severity. The Brief IPQ has been validated across several patient groups (e.g., asthma and diabetes) [20]. Because this measure is not typically used as a single score, initial analyses were conducted using both the composite and individual items.
Posttraumatic stress symptoms
Participants' PTSS were assessed with the Posttraumatic Stress Disorder Checklist (PCL) [35]. Participants reported how much they experienced each of 16 symptoms of intrusion, avoidance, and arousal during the past month in response to cancer and/or its consequences on a scale from 1 (not at all) to 4 (a lot). One item (‘suddenly acting or feeling as if the traumatic event was happening again’) was removed from the original PCL because the cancer was ongoing. A mean score was computed; higher scores indicate greater cancer-related PTSS. The PCL has good reliability and validity in cancer patients [36] and has been used in prior studies of AYA cancer patients [37] and their caregivers [38] (in this sample, Cronbach's alphas: patients = 0.82 and caregivers = 0.93).
Analytic strategies
Independent t-tests examined differences in subjective illness severity (composite and individual items) and PTSS in patients aged 12–17 years versus those aged 18–24 years. Paired t-tests compared patients' and caregivers' subjective illness severity and PTSS; analyses were run separately by patient age groups. To compare subjective illness severity (composite and individual items) to objective illness severity, Ordinary Least Squares (OLS) regressions, controlling for time since diagnosis and patient age, were used for healthcare utilization and medical costs, and paired t-tests run separately by patient age groups were used for risk prognosis.
Associations between subjective illness severity (composite scores) and PTSS in patients aged 12–24 years and caregivers were tested with the APIM using structural equation modeling in MPlus 7.0 (Muthen & Muthen, Los Angeles, CA). Structural equation modeling simultaneously examines all paths in the APIM: two within-person effects (i.e., each person's PTSS regressed on his or her own subjective illness severity) and two crossover effects (i.e., each person's PTSS regressed on the other's subjective illness severity). Our baseline APIM examined these effects first with and then without covariates (patient age, diagnostic characteristics, and objective severity). Next, a series of APIMs were run with constraints on the model paths (i.e., set to be equal) to test whether differences in the magnitude of the within-person and crossover effects were significant. Finally, multigroup APIMs with constrained paths were used to test for moderation of all within-person and crossover effects by patients' age and gender (caregivers' gender was not tested because of unequal group sizes), dyads' ethnicity, and risk prognosis.
Results
Sample information
Patients were diagnosed with different types of cancer on average 3.84 years previously (SD=1.86); 78% (n=86) of the sample was 12–17 years of age and 22% (n=24) was 18–24 years of age at the time of the study. Most were classified as high risk (73%) and had an average of 3.64 days (SD =4.80) of healthcare utilization and $1315 in medical costs (SD=$1870) monthly. Caregivers were mostly mothers (84%), with a mean age of 45.20 (SD = 7.03) years; three-quarters were married/in domestic partnerships, half completed some college or less, and the median household income was ∼$50,000. Most dyads were Caucasian (45%) or Hispanic (40%). (See Online Supplement Tables 1 and 2 for detailed illness characteristics and demographic information.)
Within-dyad comparisons
Individual descriptives and within-dyad comparisons by patient age groups appear in Table 1. Among dyads with patients aged 12–17 years, patients reported significantly lower overall subjective illness severity and lower perceived severity than caregivers on all individual illness perceptions, with one exception: there were no significant differences in patients' and caregivers' perceptions of treatment effectiveness. Among dyads with patients aged 18–24 years, there were no significant differences in overall subjective illness severity or any individual illness perceptions, except for one: caregivers reported greater concern about the patient's illness than patients themselves. PTSS were significantly higher in caregivers than in patients among both age groups.
Table 1. Within dyad descriptives (M(SD)) and comparisons of subjective illness severity and posttraumatic stress symptoms (t(df) and CIs) by patient age groups (n = 110 dyads).
| Paired t-tests | |||||||
|---|---|---|---|---|---|---|---|
|
|
|||||||
| Patients 12–17 years (n = 86) | Patients 18–24 years (n = 24) | Caregivers (n= 110) | 12–17 year-old patient–caregiver dyads | 18–24 year-old patient–caregiver dyads | |||
| Subjective illness severity | 3.29(1.28)a | 4.11(l.38)a | 4.73(1.33) | 8.08(83)*** | 1.06 to 1.75 | 2.04(23) | −0.01 to 1.58 |
| Longer duratior | 2.57(1.98) | 3.54(2.99) | 4.36(3.22) | 4.63(78)*** | −2.19 to −0.84 | 1.21(23) | 0.94 to 2.53 |
| Greater control | 6.89(2.93) | 5.71 (2.60) | 4.50(3.14) | −6.06(78)*** | 1.35 to 2.85 | −0.84(22) | −2.42 to 1.03 |
| Better treatment effectiveness | 9.20(1.69) | 9.00(1.50) | 9.16(1.54) | −0.21(81) | −0.41 to 0.39 | 0.53(23) | −0.61 to 1.03 |
| More symptoms | 3.68(2.51)b | 4.83(2.43)b | 4.79(3.03) | 2.12(79)* | −1.56 to −0.16 | 1.16(23) | −0.59 to 2.09 |
| Greater concerr | 4.55(3.03)c | 6.21(2.93)c | 8.17(2.59) | 9.39(80)*** | −4.01 to −2.58 | 2.35(23)* | 0.22 to 3.45 |
| Better understanding | 7.91(2.47) | 8.21(1.84) | 8.41(1.80) | 2.11 (80)* | −1.07 to 0.17 | −0.83(23) | −1.89 to 0.8 |
| Posttraumatic stress symptoms | 1.54(0.43) | 1.70(0.60) | 1.96(0.81) | 4.48(85)*** | −0.56 to −0.24 | 2.13(22)* | 0.01 to 0.47 |
Subjective illness severity and individual illness perceptions range from 1 to 10. Posttraumatic stress symptoms range from 1 to 5. Means sharing a common superscript differ significantly (p < 0.05). Different sample sizes due to missing data.
p < 0.05.
p< 0.01.
p< 0.001.
Subjective illness severity versus objective indicators
Controlling for time since diagnosis, patients' perceptions of illness severity (composite and individual items) were not significantly associated with risk prognosis, healthcare utilization, or medical costs (ps > 0.05). Caregivers' perceptions of illness severity (composite and individual items) were not associated with risk prognosis, healthcare utilization, or medical costs, with one exception. Caregivers' perceptions of more patient symptoms were associated with greater healthcare utilization (b(SE) = 0.24(0.08), p = 0.003, CI = 0.09, 0.39) and higher medical costs (b(SE) = 0.54(0.20), p = 0.007, CI = 0.15, 0.93), and among dyads with patients aged 12–17 years, with higher risk prognosis (Mlow risk=3.40, Mhigh risk=4.98; t(81) = −2.17, p = 0.03, CI = −3.03, −0.13).
Within-person and crossover effects
The baseline APIM tested within-person and crossover effects of subjective illness severity on PTSS in patient–caregiver dyads (Figure 1). Average subjective illness severity scores for patients aged 12–24 years were 3.47 (SD=1.34); average PTSS scores were 1.56 (SD = 0.46) (see Table 1 for comparable means for caregivers). The model was fully saturated or just identified (i.e., the observed and model-implied covariance matrices are equal; df = 0); as such, conventional model fit statistics (R2) are reported. Results indicated two significant within-person effects: higher subjective illness severity was linked with greater PTSS in both dyad members. Only one significant crossover effect was observed: greater patient subjective illness severity was associated with greater caregiver PTSS; caregivers' subjective illness severity was not associated with patients' PTSS. Patient age, cancer type, time since diagnosis, and objective severity were not significantly associated with dyad members' PTSS (ps > 0.05) and did not significantly change any model results; these variables were excluded in subsequent analyses to maintain parsimonious models. All APIM analyses were rerun using individual illness perception items as the independent variables; the overall pattern of results was similar (results not shown).
Figure 1.
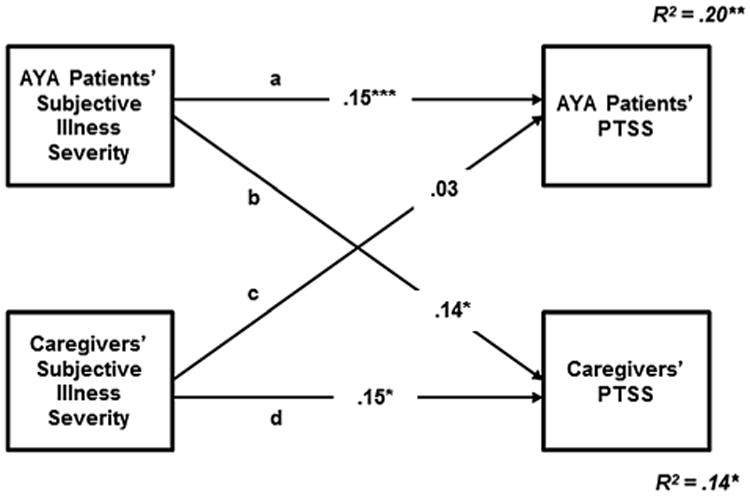
Actor–partner interdependence model analyses regressing adolescent and young adult (AYA) patients' and caregivers' perceptions of subjective illness severity on posttraumatic stress symptoms (PTSS) (n= 110 dyads). Baseline model shown with standardized estimates and standard errors. Paths a and d: within-person effects. Paths b and c: crossover effects. R2: variance in AYA patients' and caregivers' PTSS explained by the model. Ninety-five percent CIs: path a [0.09, 0.21], path b [0.03, 0.25], path c [−0.04, 0.09], and path d [0.04, 0.26]. Standard errors of estimate: path a (0.03), path b (0.06), path c (0.03), and path d (0.06). *p < 0.05; **p < 0.01; ***p < 0.001
Effect size comparisons of within-person and crossover effects
There were no significant differences in associations between patients' and caregivers' subjective illness severity and their own PTSS (χ2(1) < 0.001, p = 0.99) or the associations between their subjective illness severity and each other's PTSS (χ2(1) = 3.01, p = 0.08). Patients' (versus their caregivers') subjective illness severity was a significantly stronger predictor of their PTSS (χ2(1) = 6.16, p = 0.01). Caregivers' (compared to patients') subjective illness severity was not a stronger predictor of their own PTSS (χ2(1) = 0.02, p = 0.89).
Moderation effects
Three different moderation effects were independently tested in multigroup APIMs with constrained paths for dyads: female (n = 53) versus male (n = 57) patients, patients aged 12–17 years (n = 86) versus those aged 18–24 years (n = 24), Caucasian (n = 44) versus other ethnicities (n = 66), and high-risk (n = 80) versus low-risk (n=30) patients. No significant moderation for within-person or crossover effects was indicated (all Model χ2 ps > 0.05).
Conclusions
We examined the shared cancer experience of AYA patient–caregiver dyads. Regardless of patients' age, caregivers reported more PTSS than patients. Cancer may be less distressing for patients compared with caregivers who worry about the patient's survival, spend many hours a week providing care [39], and navigate the practicalities of managing the illness alongside other responsibilities (e.g., missed work and caring for other children) [40]. While older patients reported similar perceptions of the illness as their caregivers, younger patients did not. Perhaps cancer is perceived as less severe by younger patients because their cognitive processing of risk is still developing and they are instead focused on the rapid biological, cognitive, and social changes that come with their maturation (e.g., pubertal growth and identity formation) [4,41].
If subjective illness severity varies between younger patients and their caregivers, whose feedback should oncologists give precedence to? Conflicting accounts of the illness make it challenging to accurately judge medication effectiveness and make treatment decisions. It may be best for healthcare professionals to take heed of feedback from both individuals as each of their accounts may be useful in understanding the specific case. Yet, it is important to note that patients' and caregivers' perceptions of subjective illness severity may not necessarily reflect medical indicators of illness severity, a point we turn to next.
Caring for adolescent and young adult patients and for their caregivers
In general, results suggest that patients' and caregivers' beliefs about the illness's severity may not be based on clinical indicators often used by healthcare professionals. Overall, the majority of patients' and caregivers' illness perceptions were not associated with risk prognosis, healthcare utilization, or treatment-related expenses. Perhaps dyads were not explicitly informed about the objective illness severity by their healthcare provider. However, patients' primary oncologists are privy to this information, and this undoubtedly influences their treatment recommendations. Nonetheless, knowing that patient–caregiver dyads may be responding to a conceptually different experience than the illness being treated is important for patient care. To our knowledge, little work has examined whether healthcare professionals attend to dyad members' perceptions of illness severity. However, because patients feel more understood and supported when others share a similar understanding of their illness [42], patient care would undoubtedly benefit from clinicians speaking directly about illness perceptions with dyad members. Indeed, empathic accuracy can help facilitate a unified and cooperative approach among doctors, patients, and caregivers to optimize treatment outcomes [42].
One exception to these findings was that caregivers' perceptions of the severity of patients' symptoms were associated with objective illness severity, perhaps because frequent healthcare utilization, high medical costs, and poor prognoses bias caregivers to have negative perceptions about the patient's symptoms. Alternatively, perhaps caregivers who perceive greater symptomatology in patients bring them to the hospital more often, utilizing more services and acquiring higher medical expenses. Future research should examine these and other potential explanations.
Subjective illness severity is associated with posttraumatic stress symptoms
Greater subjective illness severity was associated with greater PTSS in patient–caregiver dyads. Although prior research has shown patients' illnesses have a substantial impact on their caregivers [7], our findings are the first to show that patients' subjective illness severity can cross over to their caregivers' PTSS and that patients' subjective illness severity may be just as important for caregivers' PTSS as caregivers' own perceptions. In contrast, patients appear less susceptible to their caregivers' reports of subjective illness severity, perhaps because they are primarily focused on themselves during this developmental life stage [41]. Alternatively, caregivers may be hiding their perceptions from patients in order to protect them. Future research might examine these possibilities directly.
Do different dyads experience cancer differently?
Associations between subjective illness severity and PTSS within and between AYA patients and their caregivers did not vary based on patients' age, gender, risk prognosis, or dyads' ethnicity. Similarly, cancer type, time since diagnosis, healthcare utilization, and medical costs were not associated with PTSS and did not change the results when included as covariates in the APIM. These findings hint that the observed associations between subjective illness severity and PTSS are robust among developmentally diverse dyads coping with different types of cancer for various amounts of time and with varying levels of objective severity. It also further supports our finding that subjective illness severity appears to be independent of objective severity.
Limitations
Several limitations must be acknowledged. First, the cross-sectional design precludes our ability to make causal inferences about subjective illness severity and PTSS. Longitudinal assessments could better test how dyad members' perceptions influence each other over the course of the illness. Second, the sample size for the older patient group (18–24 years) was relatively small, which may have underpowered our analyses. Future work with larger or homogenous samples should start assessments immediately after diagnosis for increased power and more in-depth examinations of the importance of demographic and illness-related characteristics. Third, the Brief IPQ [34] was not designed for use as a composite measure with high internal consistency. Yet, conducting our analyses with both the composite score and individual illness perception items yielded comparable results, suggesting that there may be utility in using the scale in this manner. Future research might examine patients' quality of life in conjunction with objective and subjective measures to provide a more comprehensive assessment of illness severity. Finally, it is plausible that our chosen medical indicators did not entirely reflect objective illness severity. For example, medical costs may not be a true indicator of illness severity when comparing across different types of diagnoses requiring differential treatments/procedures, and healthcare utilization may be misleading if a treatment is complex but the outlook is good. However, there are no standard objective cancer severity indicators (even patients with equivalent cancer stages do not necessarily have a similar illness severity), and while standardized measures of patient functioning are certainly helpful, they are less likely to be used in routine medical visits. Thus, we took a novel approach by using medical data to create surrogate markers for objective illness severity: risk prognosis was based on diagnostics from patients' medical charts, which determine clinicians' prognosis assessment (i.e., objective medical rating of illness severity), and dyads with greater average healthcare utilization and medical costs are presumably coping with a more serious case of cancer that requires more medical attention. Nonetheless, we hope that our work demonstrates the need to establish a standardized tool for determining patients' personalized risk prognosis based on unique illness characteristics that may be used to guide treatment plans and provide patients (and their families) with a better understanding of the illness with which they are coping.
Clinical implications
This study provides strong evidence that cancer is a dyadic illness shared between AYA patients and their caregivers. The APIM is a helpful analytic tool for identifying contributing sources of PTSS within dyads and allows for a comparison of these sources. Our results suggest that interpreting correlates of PTSS without considering the role of close others can result in false conclusions about contributing sources of distress. Specifically, psychological and social services should be readily available to help both AYA patients and caregivers cope with their illness perceptions and distress. Therapeutic efforts could include both patients and caregivers, but be tailored according to their different illness-related cognitions. Recent research demonstrates that interventions directed at changing illness perceptions can improve self-management behaviors in patients with chronic illness (e.g., asthma) [43]. Efforts to incorporate such interventions into routine care [44] and extend them to patients' family members [7]—especially caregivers—would be useful.
Overall, our findings support existing evidence encouraging intervention efforts to target patients and caregivers as a dyad rather than as independent individuals. Providing effective treatment for patient-caregiver dyads requires recognizing that those coping with severe forms of cancer by medical standards may not always be the ones with the most negative illness perceptions. Thus, healthcare professionals are encouraged to open the discussion for patients and caregivers to share their concerns and perceptions about the illness, regardless of medical indicators of disease severity. Such an approach will ensure that the psychosocial needs of AYA patients and their families are given as much attention as their clinical ones so as to provide this population with the best possible care.
Supplementary Material
Acknowledgments
The authors thank Van Huynh, MD, Keri Zabokrtsky, and CHOC Children's staff for their support with the project and Kelly Block, Jessica Castronuovo, and Paulina Franco for their assistance with participant recruitment and data collection.
The project was supported in part by the Kathryn T. McCarty Oncology Endowment and the Hyundai Cancer Institute at CHOC Children's. First author was supported by T32 award #UL1 RR031985 from the Institute of Clinical and Translational Science at the University of California, Irvine, through grant #UL1 TR000153 from the National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Conflict of interest: The authors indicate no potential conflicts of interest.
Supporting information: Additional supporting information may be found in the online version of this article at the publisher's web site.
References
- 1.American Cancer Society. Cancer Facts & Figures. Atlanta, GA: American Cancer Society; 2012. 2012. [Google Scholar]
- 2.Zebrack B, Mathews-Bradshaw B, Siegel S. Quality cancer care for adolescents and young adults: a position statement. J Clin Oncol. 2010;28:1–6. doi: 10.1200/JCO.2010.30.5417. [DOI] [PubMed] [Google Scholar]
- 3.Haase JE, Phillips CR. The adolescent/young adult experience. J Pediatr Oncol Nurs. 2004;21:145–149. doi: 10.1177/1043454204264385. [DOI] [PubMed] [Google Scholar]
- 4.Steinberg L, Morris A. Adolescent development. Annu Rev Psychol. 2000;52:83–110. doi: 10.1146/annurev.psych.52.1.83. [DOI] [PubMed] [Google Scholar]
- 5.Stenberg U, Ruland CM, Miaskowski C. Review of the literature on the effects of caring for a patient with cancer. Psycho-Oncology. 2010;19:1013–1025. doi: 10.1002/pon.1670. [DOI] [PubMed] [Google Scholar]
- 6.Woodgate RL. The importance of being there: perspectives of social support by adolescents with cancer. J Pediatr Oncol Nurs. 2006;23:122–134. doi: 10.1177/1043454206287396. [DOI] [PubMed] [Google Scholar]
- 7.Kazak AE, Kassam-Adams N, Schneider S, et al. An integrative model of pediatric medical traumatic stress. J Pediatr Psychol. 2006;31:343–355. doi: 10.1093/jpepsy/jsj054. [DOI] [PubMed] [Google Scholar]
- 8.Miller VA, Drotar D. Decision-making competence and adherence to treatment in adolescents with diabetes. J Pediatr Psychol. 2007;32:178–188. doi: 10.1093/jpepsy/jsj122. [DOI] [PubMed] [Google Scholar]
- 9.Logan DE, Guite JW, Sherry DD, et al. Adolescent-parent relationships in the context of adolescent chronic pain conditions. Clin J Pain. 2006;22:576–583. doi: 10.1097/01.ajp.0000210900.83096.ca. [DOI] [PubMed] [Google Scholar]
- 10.Kazak AE, Alderfer M, Rourke MT, et al. Posttraumatic stress disorder (PTSD) and posttraumatic stress symptoms (PTSS) in families of adolescent childhood cancer survivors. J Pediatr Psychol. 2004;29:211–219. doi: 10.1093/jpepsy/jsh022. [DOI] [PubMed] [Google Scholar]
- 11.Best M, Streisand R, Catania L, Kazak AE. Parental distress during pe-diatric leukemia and posttraumatic stress symptoms (PTSS) after treatment ends. J Pediatr Psychol. 2001;26:299–307. doi: 10.1093/jpepsy/26.5.299. [DOI] [PubMed] [Google Scholar]
- 12.Landolt MA, Vollrath M, Ribi K, et al. Incidence and associations of parental and child posttraumatic stress symptoms in pediatric patients. J Child Psychol Psychiatry. 2003;44:1199–1207. doi: 10.1111/1469-7610.00201. [DOI] [PubMed] [Google Scholar]
- 13.Dunn MJ, Rodriguez EM, Barnwell AS, et al. Posttraumatic stress symptoms in parents of children with cancer within six months of diagnosis. Health Psychol. 2011;31:176–185. doi: 10.1037/a0025545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tremolada M, Bonichini S, Aloisio D, et al. Post-traumatic stress symptoms among mothers of children with leukemia undergoing treatment: a longitudinal study. Psycho-Oncology. 2013;22:1266–1272. doi: 10.1002/pon.3132. [DOI] [PubMed] [Google Scholar]
- 15.Ben-Zur H, Gilbar O, Lev S. Coping with breast cancer: patient, spouse, and dyad models. Psychosom Med. 2001;63:32–39. doi: 10.1097/00006842-200101000-00004. [DOI] [PubMed] [Google Scholar]
- 16.Langer S, Abrams J, Syrjala K. Caregiver and patient marital satisfaction and affect following hematopoietic stem cell transplantation: a prospective, longitudinal investigation. Psycho-Oncology. 2003;12:239–253. doi: 10.1002/pon.633. [DOI] [PubMed] [Google Scholar]
- 17.Weinman J, Petrie KJ, Moss-Morris R, et al. The illness perceptions questionnaire: a new method for assessing the cognitive representation of illness. Psychol Health. 1996;11:431–445. [Google Scholar]
- 18.Leventhal H, Meyer D, Nerenz D. The Common Sense Model of Illness Danger. In: Rachman S, editor. Medical psychology. Vol. 2. New York, NY: Pergamon; 1980. pp. 7–30. [Google Scholar]
- 19.Hagger MS, Orbell S. A meta-analytic review of the common-sense model of illness representations. Psychol Health. 2003;18:141–184. [Google Scholar]
- 20.Kazak AE, Rourke MT, Crump TA. Families and Other Systems in Pediatric Psychology. In: Roberts M, editor. Handbook of pediatric psychology. New York, NY: Guilford; 2003. pp. 159–175. [Google Scholar]
- 21.Vance YH, Morse RC, Jenney ME, Eiser C. Issues in measuring quality of life in childhood cancer: measures, proxies, and parental mental health. J Child Psychol Psychiatry Allied Disciplines. 2001;42:661–667. [PubMed] [Google Scholar]
- 22.Litzelman K, Catrine K, Gangnon R, Witt WP. Quality of life in parents of children with cancer or brain tumors: the role of child clinical characteristics and parental psychosocial factors. Qual Life Res. 2011;20:1261–1269. doi: 10.1007/s11136-011-9854-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Twiddy M, House A, Jones F. The association between discrepancy in illness representations on distress in stroke patients and carers. Psychosom Med. 2012;72:220–225. doi: 10.1016/j.jpsychores.2011.12.004. [DOI] [PubMed] [Google Scholar]
- 24.Dempster M, McCorry NK, Brennan E, et al. Psychological distress among family carers of oesophageal cancer survivors: the role of illness cognitions and coping. Psycho-Oncology. 2011;20:698–705. doi: 10.1002/pon.1760. [DOI] [PubMed] [Google Scholar]
- 25.Heijmans M, de Ridder D, Bensing J. Dissimilarity in patients' and spouses' representations of chronic illness: exploration of relations to patient adaptation. Psychol Health. 1999;14:451–466. [Google Scholar]
- 26.Mereuta OC, Cracium C. Parents' illness perceptions, maladaptive behaviors, and their influence on the emotional distress of the child: a pilot study on a Romanian pediatric cancer group. Cogn Brain Behav. 2009;13:207–219. [Google Scholar]
- 27.Salewski C. Illness representations in families with a chronically ill adolescent: differences between family members and impact on patients' outcome variables. J Health Psychol. 2003;8:587–598. doi: 10.1177/13591053030085009. [DOI] [PubMed] [Google Scholar]
- 28.Cook WL, Kenny DA. The actor-partner interdependence model: a model of bidirectional effects in developmental studies. International J of Behavioral Development. 2005;29:101–109. [Google Scholar]
- 29.Hill J, Kondryn H, Mackie E, McNally R, Eden T. Adult psychosocial functioning following childhood cancer: the different roles of sons' and daughters' relationships with their fathers and mothers. J Child Psychol Psychiatry. 2003;44:752–762. doi: 10.1111/1469-7610.00161. [DOI] [PubMed] [Google Scholar]
- 30.Munet-Vilaro F. Delivery of culturally competent care to children with cancer and their families—the Latino experience. J Pediatr Oncol Nurs. 2004;21:155–159. doi: 10.1177/1043454204264405. [DOI] [PubMed] [Google Scholar]
- 31.Zabora J, Brintzenhofe-Szoc K, Curbow B, et al. The prevalence of psychological distress by cancer site. Psycho-Oncology. 2001;10:19–28. doi: 10.1002/1099-1611(200101/02)10:1<19::aid-pon501>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 32.Sloper P. Predictors of distress in parents of children with cancer: a prospective study. J Pediatr Psych. 2000;25:79–91. doi: 10.1093/jpepsy/25.2.79. [DOI] [PubMed] [Google Scholar]
- 33.Hutchinson KC, Willard VW, Hardy KK, Bonner MJ. Adjustment of caregivers of pediatric patients with brain tumours: a cross sectional analysis. Psycho-Oncology. 2009;18:515–523. doi: 10.1002/pon.1421. [DOI] [PubMed] [Google Scholar]
- 34.Broadbent E, Petrie KJ, Main J, et al. The Brief Illness Perception Questionnaire. J Psychosom Res. 2006;60:631–637. doi: 10.1016/j.jpsychores.2005.10.020. [DOI] [PubMed] [Google Scholar]
- 35.Weathers FW, Litz BT, Herman DS, et al. The PTSD Checklist: Reliability, Validity, and Diagnostic Utility; Presented at the meeting of the International Society for Traumatic Stress Studies; San Antonio, TX. 1993. [Google Scholar]
- 36.Smith MY, Redd W, DuHamel K, et al. Validation of the PTSD Checklist—civilian version in survivors of bone marrow transplantation. J Trauma Stress. 1999;12:485–499. doi: 10.1023/A:1024719104351. [DOI] [PubMed] [Google Scholar]
- 37.Kwak M, Zebrack BJ, Meeske KA, et al. Prevalence and predictors of post-traumatic stress symptoms in adolescent and young adult cancer survivors: a 1-year follow-up study. Psycho-Oncology. 2013;22:1798–1806. doi: 10.1002/pon.3217. [DOI] [PubMed] [Google Scholar]
- 38.Norberg AL, Poder U, von Essen L. Early avoidance of disease- and treatment-related distress predicts post-traumatic stress in parents of children with cancer. Eur J Oncol Nurs. 2011;15:80–84. doi: 10.1016/j.ejon.2010.05.009. [DOI] [PubMed] [Google Scholar]
- 39.National Alliance for Caregiving: Caregiving in the U. S. 2009. (Available from: http://www.caregiving.org/research.)
- 40.King G, King S, Rosenbaum P, et al. Family-centered caregiving and well-being of parents of children with disabilities: linking process with outcome. J Pediatr Psychol. 1999;24:41–53. [Google Scholar]
- 41.Steinberg L. Cognitive and affective development in adolescence. Cogn Sciences. 2005;9:69–74. doi: 10.1016/j.tics.2004.12.005. [DOI] [PubMed] [Google Scholar]
- 42.Norfolk T, Birdi K, Walsh D. The role of empathy in establishing rapport in the consultation: a new model. Med Educ. 2007;41:690–697. doi: 10.1111/j.1365-2923.2007.02789.x. [DOI] [PubMed] [Google Scholar]
- 43.Petrie KJ, Perry K, Broadbent E, et al. A text message programme designed to modify patients' illness and treatment beliefs improves self-reported adherence to asthma preventer medication. Br J Health Psychol. 2012;17:74–84. doi: 10.1111/j.2044-8287.2011.02033.x. [DOI] [PubMed] [Google Scholar]
- 44.Petrie KJ, Weinman J. Patients' perceptions of their illness: the dynamo of volition in health care. Curr Dir Psychol Sci. 2012;21:60–65. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


