Abstract
Objective
To quantify changes in private insurance payments for and utilization of abdominal/pelvic computed tomography scans (CTs) after 2011 changes in CPT coding and Medicare reimbursement rates, which were designed to reduce costs stemming from misvalued procedures.
Data Sources
TruvenHealth Analytics MarketScan Commercial Claims and Encounters database.
Study Design
We used difference‐in‐differences models to compare combined CTs of the abdomen/pelvis to CTs of the abdomen or pelvis only. Our main outcomes were inflation‐adjusted log payments per procedure, daily utilization rates, and total annual payments.
Data Extraction Methods
Claims data were extracted for all abdominal/pelvic CTs performed in 2009–2011 within noncapitated, employer‐sponsored private plans.
Principal Findings
Adjusted payments per combined CTs of the abdomen/pelvis dropped by 23.8 percent (p < .0001), and their adjusted daily utilization rate accelerated by 0.36 percent (p = .034) per month after January 2011. Utilization rate of abdominal‐only or pelvic‐only CTs dropped by 5.0 percent (p < .0001). Total annual payments for combined CTs of the abdomen/pelvis decreased in 2011 despite the increased utilization.
Conclusions
Private insurance payments for combined CTs of the abdomen/pelvis declined and utilization accelerated significantly after 2011 policy changes. While growth in total annual payments was contained in 2011, it may not be sustained if 2011 utilization trends persist.
Keywords: Health insurance reimbursement, utilization, health policy, CPT codes, computed tomography, fee‐for‐service plans
Diagnostic imaging accounts for a significant portion of U.S. health care spending (Iglehart 2006; Armao, Semelka, and Elias 2012). The frequency of computed tomography (CT) scanning in the United States has increased from roughly 3 million scans in 1980 to 85 million scans in 2011 (Mettler et al. 2009; IMV Medical Information Division 2012). Although some studies suggested that this growth rate has recently slowed (Levin, Rao, and Parker 2010; Lee and Levy 2012), more recent research revealed increased growth resumption (Horný et al. 2014). In addition, future growth is likely as the baby‐boomer generation reaches retirement age, as older patients utilize the greatest proportion of imaging services (Keehan et al. 2008).
Given the expected burden of growing health care costs in general and imaging costs in particular to the U.S. government and other payers, the American Medical Association (AMA)/Specialty Society Relative Value Scale Update Committee (RUC) worked with the Center for Medicare and Medicaid Services (CMS) to examine potentially misvalued services in the CMS payment guidelines (Silva 2010). Diagnostic imaging was one target for review through the examination of Current Procedural Terminology (CPT) codes that were paired together more than 95 percent of the time.
Prior to 2011, the AMA maintained three CPT codes to describe CT scans of the abdomen and three CPT codes to describe CT scans of the pelvis (one code each for scans performed without contrast, scans performed with contrast, and scans performed first without and then with contrast). However, as the abdomen and pelvis represent one anatomically contiguous body cavity, CTs of the abdomen and pelvis are frequently ordered simultaneously and performed in the same imaging session. In this case, the procedure was recorded using two CPT codes—one for the abdominal scan and one for the pelvic scan—and billed to payers as two separate procedures. In this paper, we will refer to the CT of the abdomen and pelvis as the “combined scan,” and to the CT of either abdomen or pelvis only as the “single scan.”
In an effort to more accurately describe the medical procedure being performed and its value, the RUC/CPT workgroup recommended creating three new CPT codes, again divided by timing of contrast administration, to represent the combined scan (i.e., when an abdominal CT and pelvic CT were performed back to back in the same imaging session). The existing CPT codes for single scans were retained for instances when only one scan was performed per imaging session. The AMA approved and released this change with the CPT code update that became effective on January 1, 2011. Concurrently, CMS assigned the newly created codes for the combined scans a level of relative value units that was approximately 75 percent of the sum of an abdomen‐only and pelvis‐only scan (Silva 2011).
While the impact of the creation of a single CPT code for combined abdominal/pelvic CTs on global payments and utilization has been examined in the Medicare population (Levin, Rao, and Parker 2014), no analysis of changes in scanning in privately insured patients has been performed. More important, it is unknown if payment reductions were associated with any subsequent changes in rates of service utilization for each type of CT scan individually. To address this gap in knowledge, we used a large national dataset of private health insurance medical claims to identify any changes following the implementation of new CPT codes and change in Medicare payments. We predicted a drop in private insurance payments of combined CTs of the abdomen and pelvis in 2011, given prior evidence that private insurers often follow Medicare's example in setting reimbursement levels (Clemens and Gottlieb 2013). In light of prior research showing increased utilization after other payment reductions as physicians strive to maintain a target income (McGuire and Pauly 1991), we also predicted an increase in the utilization of combined CTs in 2011 accompanied by a possible decrease in utilization of the single scans when compared to utilization rates prior to the coding policy change.
Methods and Data
Study Data
We used data from the Truven Health Analytics MarketScan Commercial Claims and Encounters databases of 2009–2011. These data consist of individual‐level, deidentified health care claims information from large employers and health plans across the United States. As the number and composition of health plans included in the database vary by year, we extracted only data of those individuals who were enrolled in a health plan, and thus contained in the database, for the entire observed period (from January 2009 until December 2011). As these data are only for commercial coverage, patients covered exclusively from government insurance programs, such as Medicare and Medicaid, are not captured.
The abdominal and pelvic CT procedures were identified in the database by their CPT codes (72192, 72193, 72194, 74150, 74160, and 74170 in 2009–2011; and also 74176, 74177, and 74178 in 2011). As no code specified a combined CT scan of the abdomen and pelvis prior to 2011, in these years, we identified instances when both a CT scan of the abdomen and a CT scan of the pelvis were performed on the same patient on the same day, and considered these scans as a single encounter, that is, as a combined scan. We then summed the payments for the separate procedures and assigned this encounter the appropriate CPT code according to the new classification scheme introduced in 2011. This methodology allowed us to maintain consistent CT scan classification before and after the coding policy change. Procedures covered by capitation payments were not included in the analysis.
In our study, we analyze global payments per procedure from the payer to the health care provider including both the professional and the technical component. Negative payments were identified in some procedures (1.0 percent) even after incorporating corrections to previous claims and other insurer adjustments, owing most likely to erroneous data entries. These procedures were excluded from the analysis. We used a GDP deflator to adjust payments for inflation (Huskamp and Newhouse 1994) to the last quarter of 2011 U.S. dollars. Values of the GDP deflator were obtained from the International Monetary Fund official website (International Monetary Fund 2013).
In addition to claims data, we also retrieved information about age, gender, the type of health plan, and state of residence of each enrollee. The MarketScan database classifies health plans into the following types: preferred provider organization (PPO), health maintenance organization (HMO), point‐of‐service (POS), exclusive provider organization (EPO), consumer‐driven health plan (CDHP), high deductible health plan (HDHP), and comprehensive insurance. The MarketScan database does not include information about race or ethnicity. Finally, we used publicly available U.S. Census Bureau data for 2010 (U.S. Census Bureau 2012) to evaluate how well our study sample represented the general population of the United States.
Statistical Methods
The study was designed as a difference‐in‐differences model with the interruption on January 1, 2011 (the date when the new CPT codes for the combined scan were implemented), using the combined scans as the treatment group and the single scans as the reference group. The treatment group and reference group are distinct with no changes or spillovers over the course of the study. We are not aware of any other events at the time, other than the introduction of the new coding scheme and change in Medicare reimbursement rates, that might affect payments for or utilization of the combined scans in privately insured individuals.
The payments model used natural logs of the outcome variable and assumed normal distribution of residuals. We expected some variation in payments across states and health plan types and adjusted the model for these variables. After fitting the model, we tested whether the assumption of homoscedasticity of standard errors was violated, and whether the trends in the treatment group and the reference group were parallel prior to the intervention. As the outcome variable was log‐transformed and therefore a change was measured in percentages rather than in absolute terms, the baseline payment levels could not have impacted the payments‐change after the new reimbursement policy introduction.
We modeled daily utilization rates of the CT scans using a negative binomial difference‐in‐differences model with a log link. We controlled for variation in utilization rates across states and health plan types and applied an offset to the model by log of the number of beneficiaries in the particular state and health plan type. Visual inspection of the daily utilization rate distribution clearly showed two distinct clusters of data corresponding to weekdays (higher rates) and weekends (lower rates), and thus we adjusted the utilization model by adding a weekend indicator. After we fitted the model, we tested whether the trends in the treatment group and the reference group were parallel prior to the intervention. Again, as the outcome variable was log‐transformed, there is no concern that the baseline utilization levels could be related to expectations for changes of the utilization after the coding policy change.
Both the models of payments and utilization were estimated for an arbitrarily chosen reference of PPO health plans in Massachusetts. All analyses were conducted using SAS 9.4 (SAS Corp., Cary, NC, US). The Boston University Medical Campus Institutional Review Board determined that this study was nonhuman subjects research and therefore exempt from review.
Results
Demographics
The demographic characteristics of the 14,047,817 individuals included in our sample are summarized in Table 1. There were slightly more women than men in our sample, which closely represents the U.S. population in 2010. Overall, 61.1 percent of enrollees were in PPO insurance plans, 17.5 percent were in HMOs, 9.1 percent were in POS plans, and 10.0 percent in other health plan types. Health plan type classification was missing for less than 2.4 percent of individuals. While the South was overrepresented compared to the actual proportion of the U.S. population, the regional distribution of enrollees in our study sample fairly well represented the actual distribution of individuals in the United States. Information about regional assignment was missing for only 0.13 percent of individuals. While there was some variation in distribution of our fixed‐study population across health plan types and states throughout the study period as people changed health plans and moved, this variation was negligible. Finally, the distribution of age of individuals in our sample was slightly skewed toward older individuals compared to the general U.S. population of individuals younger than 65 years.
Table 1.
Sample Demographics
| N (SE) | % | U.S. Census 2010 (%) | |
|---|---|---|---|
| Sample size | 14,047,817 | 100.0 | |
| Gender | |||
| Males | 6,768,572 | 48.2 | 49.2 |
| Females | 7,279,245 | 51.8 | 50.8 |
| Age groupsa | |||
| 0–17 years | 3,368,052 | 24.0 | 30.3c |
| 18–34 years | 2,603,079 | 18.5 | 23.1c |
| 35–44 years | 2,354,489 | 16.8 | 15.4 |
| 45–54 years | 3,066,812 | 21.8 | 17.1 |
| 55–64 years | 2,655,385 | 18.9 | 14.1 |
| Health plan typesb | |||
| Comprehensive | 302,485 (8,198) | 2.2 | n/a |
| EPO | 262,977 (19,299) | 1.9 | n/a |
| HMO | 2,455,361 (21,645) | 17.5 | n/a |
| POS | 1,270,819 (9,319) | 9.1 | n/a |
| PPO | 8,580,713 (25,366) | 61.1 | n/a |
| CDHP | 635,185 (22,783) | 4.5 | n/a |
| HDHP | 208,654 (11,829) | 1.5 | n/a |
| n/a | 331,623 (8,220) | 2.4 | |
| Regionsb | |||
| Northeast | 2,074,781 (2,252) | 14.8 | 17.9 |
| Midwest | 3,567,712 (1,966) | 25.4 | 21.7 |
| South | 5,735,955 (4,067) | 40.8 | 37.1 |
| West | 2,651,218 (255) | 18.9 | 23.3 |
| n/a | 18,151 (93) | .1 | |
As of December 2011.
Average across 2009–2011.
U.S. Census age groupings are reported as 0–19 and 20–34 years, and have been placed with the closest corresponding age group of our sample.
Payments
The median adjusted payments per CT procedure are presented in Table 2. There were only minor changes in payments per single or combined scan between January 2009 and December 2010, but, as predicted, there was a sharp drop in payments for the combined CT scan of the abdomen and pelvis in January 2011 when the new CPT codes were introduced (Figure 1). From 2010 to 2011, the median adjusted payment for the combined scan in our sample dropped by $269 to $303, depending on contrast administration.
Table 2.
Absolute Utilization and Adjusted Payments Per Procedure
| 2009 | 2010 | 2011 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| N | Median | IQR | N | Median | IQR | N | Median | IQR | |
| CT of the abdomen | 45,334 | 43,755 | 41,159 | ||||||
| Without contrast | 8,766 | $330 | 455 | 8,400 | $332 | 480 | 7,454 | $312 | 447 |
| With contrast | 17,222 | $466 | 653 | 17,315 | $483 | 723 | 17,246 | $496 | 733 |
| Without & with contrast | 19,346 | $551 | 590 | 18,040 | $556 | 600 | 16,459 | $553 | 601 |
| CT of the pelvis | 12,158 | 11,490 | 10,871 | ||||||
| Without contrast | 5,256 | $356 | 599 | 4,979 | $360 | 622 | 4,854 | $341 | 592 |
| With contrast | 5,504 | $430 | 690 | 5,210 | $441 | 736 | 4,959 | $430 | 740 |
| Without & with contrast | 1,398 | $432 | 406 | 1,301 | $423 | 448 | 1,058 | $431 | 410 |
| CT of the abdomen and pelvis | 433,218 | 445,879 | 483,954 | ||||||
| Without contrast | 149,814 | $655 | 1,156 | 155,949 | $673 | 1,235 | 159,892 | $379 | 979 |
| With contrast | 192,474 | $827 | 1,462 | 205,679 | $850 | 1,561 | 229,411 | $547 | 1,247 |
| Without & with contrast | 90,930 | $967 | 1,114 | 84,251 | $960 | 1,144 | 94,651 | $691 | 1,052 |
| Total | 490,710 | – | – | 501,124 | – | – | 535,984 | – | – |
Figure 1.
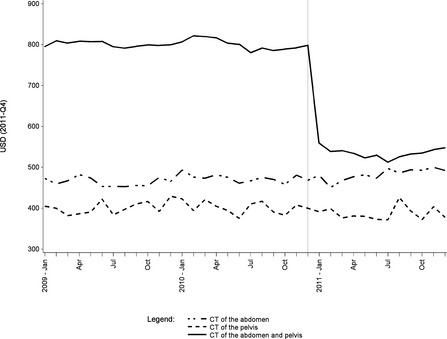
Median Adjusted Payment Per Procedure
Consistent with previous research on health care payment (Williams, Rousseau, and Glaudemans 2005; MedPAC 2011), preintervention payment levels varied between insurance plans types, with PPOs reimbursing at a significantly higher rate than POS and HMO plans (Figure S1). However, each of these insurance plan types reduced reimbursement in January 2011 by a similar percentage. Furthermore, while there was variation in payment levels across regions of the United States, a similar level of decline in reimbursement was evidenced in each region (Figure S2).
The estimated parameters of the difference‐in‐differences model with single scans as the reference group and combined scans as the treatment group, adjusted for state and health plan type, are summarized in Table 3. The assumption of homoscedastic standard errors was violated (p < .0001); thus, we report the heteroscedasticity‐consistent standard errors as suggested by White (1980). Prior to the coding change, inflation‐adjusted payments for single scans were growing at a pace of 0.13 percent (p = .0017) per month, while there was a nonsignificant difference (p = .9919) between the single scans and the combined scans. In other words, the trends in the treatment group and the reference group were parallel prior to the intervention.
Table 3.
Estimated Impacts of the 2011 Coding Change on Payments and Utilization
| Parameter | Estimate | % Change | SE | p |
|---|---|---|---|---|
| Payments | ||||
| CT of the abdomen or of the pelvis (the reference group) | ||||
| Intercept | 6.0418 | – | 0.0087 | <.0001*** |
| Slope | 0.0013 | +0.13 | 0.0004 | .0017** |
| Change in intercept in 2011 | −0.0055 | −0.55 | 0.0097 | .5735 |
| Change in slope in 2011 | 0.0033 | +0.33 | 0.0013 | .0089** |
| CT of the abdomen and pelvis (w.r.t. the reference group) | ||||
| Intercept | 0.5665 | +76.21 | 0.0057 | <.0001*** |
| Slope | −0.0000 | −0.00 | 0.0004 | .9919 |
| Change in intercept in 2011 | −0.2740 | −23.97 | 0.0104 | <.0001*** |
| Change in slope in 2011 | −0.0036 | −0.36 | 0.0014 | .0083** |
| Other covariates | ||||
| Health plan type | – | – | – | <.0001*** |
| State | – | – | – | <.0001*** |
| Utilization | ||||
| CT of the abdomen or of the pelvis (the reference group) | ||||
| Intercept | −10.8499 | – | 0.0105 | <.0001*** |
| Slope | −0.0012 | −0.12 | 0.0005 | .0171* |
| Change in intercept in 2011 | −0.0511 | −4.98 | 0.0120 | <.0001*** |
| Change in slope in 2011 | 0.0044 | +0.44 | 0.0016 | .0045** |
| CT of the abdomen and pelvis (w.r.t. the reference group) | ||||
| Intercept | 1.6169 | +403.74 | 0.0074 | <.0001*** |
| Slope | 0.0018 | +0.18 | 0.0006 | .0010*** |
| Change in intercept in 2011 | 0.0663 | +6.85 | 0.0131 | <.0001*** |
| Change in slope in 2011 | 0.0036 | +0.36 | 0.0017 | .0338* |
| Other covariates | ||||
| Health plan type | – | – | – | <.0001*** |
| State | – | – | – | <.0001*** |
| Weekend indicator | −0.8456 | −57.07 | 0.0032 | <.0001*** |
| Dispersion | 0.0726 | – | 0.0007 | – |
Estimates of effects for individual health plan types and states are not reported due to limited space. Full table with all estimated coefficients is available in the appendix.
*p ≤ .05; **p ≤ .01; ***p ≤ .001.
In January 2011, when the new coding policy was implemented, there was a substantial drop by almost 24 percent (p < .0001) in payments for the combined scan, adjusted for regional and health insurance payer differences. There was no significant immediate change in payments for the single scans at this time, but the growth in payments for the single scans increased by 0.33 percent (p = .0089) per month. Growth in payments for the combined scans was lower by 0.36 percent (p = .0083) per month in 2011 with respect to the single scans (the reference group), but as there was an increase in almost exactly the same magnitude in growth of payments for the single scans in this period, we can reasonably infer that payments for the combined scan experienced only a substantial drop in the intercept, but the slope remained the same as in the period prior to the coding policy change.
Utilization
Utilization by scan type is summarized in Table 2; for visual clarity, standardized monthly utilization rates are depicted in Figure 2. Annual number of performed single scans was decreasing between 2009 and 2011. Our estimates from the negative binomial difference‐in‐differences model adjusted for state, health plan type, and weekend indicator (see Table 3) show that the daily utilization rate of the single scans was decreasing by 0.12 percent (p = .0171) per month prior to 2011. The coding policy change resulted in a 5 percent (p < .0001) decline in the daily utilization rate of the single scans; but then the trend turned in the opposite direction increasing by 0.44 percent (p = .0045) per month.
Figure 2.
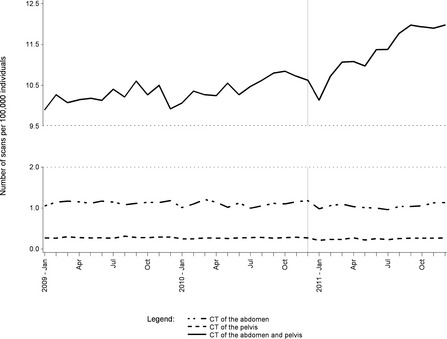
Median Daily Utilization Rate Per 100,000 Individuals
The situation in combined CT scans of the abdomen and pelvis was different. The daily utilization rate was growing by 0.18 percent (p = .001) per month in 2009 and 2010 with respect to the reference group, which corresponds to an annual growth of 2.18 percent, implying the utilization trends were not exactly parallel prior to the intervention. However, we observed a 6.85 percent (p < .0001) shift in daily utilization rate of the combined CT scans after the coding policy change, which substantially exceeds the simultaneous decline in utilization rate of the single scans. Furthermore, the growth of the daily utilization rate accelerated by additional 0.36 percent (p = .0338) per month with respect to the reference group. In other words, the adjusted daily utilization rate of the combined CT scan was growing annually by 0.72 percent in 2009 and 2010, while the annual growth increased to 10.85 percent in 2011.
Total Payments
Total annual adjusted payments for single scans decreased throughout the observed period (CT scans of the abdomen: $28.1 million in 2009, $27.7 million in 2010, $27.0 million in 2011; CT scans of the pelvis: $6.7 million in 2009, $6.4 million in 2010, $5.9 million in 2011). Total annual adjusted payments for the combined CT scans of the abdomen and pelvis increased between 2009 and 2010 from $486.0 million to $514.8 million, but dropped in 2011 to $475.3 million.
Discussion
Using a difference‐in‐differences approach, our study is the first to examine the effect of the January 1, 2011, changes in CPT coding and Medicare reimbursement policies for combined CT scans of the abdomen and pelvis on the reimbursement for and utilization of these scans in privately insured individuals. We found a sharp drop in the payments for the combined scans in 2011 and a significant increase in the utilization of these scans over time, even after controlling for preintervention trends in CT scans of this body area. While the decrease in payments was enough to offset the increase in utilization in terms of decreased overall expenditures for combined abdominal/pelvic CT scanning, this overall cost savings will not persist if growth in utilization continues at the observed rate.
Payments for the combined scans from private insurers dropped significantly beginning in January 2011, concordant with Medicare payment changes. The 24 percent decline in private insurer payments is consistent with the contemporaneous Medicare reimbursement changes, which also reduced payments of the combined scans by an amount equal to one‐half of a single scan (approximately 25 percent of the overall cost). This decrease in payments is a stark contrast to the relative stability of payments for abdominal CTs and pelvic CTs performed alone.
Given that the original intent of efforts to bundle CPT codes was to reduce misvaluation of health care procedures, our documentation of the drop in payments for combined CT of the abdomen and pelvis gives both providers and policy makers data against which to judge whether payments are now more commensurate with physician effort and technical investments. Current evidence is mixed regarding the appropriateness of lowered Medicare and private insurer payments for the combined scans. For instance, an analysis of work efficiencies achieved when multiple services are provided for the same patient at the same time found that these efficiencies are highly variable from patient to patient and are significantly less than those estimated by entities such as the Government Accountability Office (GAO) and CMS (Allen et al. 2011; Duszak et al. 2013). However, prior analysis of actual versus reimbursed professional and technical costs involved in CT scanning found that Medicare underreimbursed professional costs and overreimbursed technical costs (Nisenbaum et al. 2000). As the debate over appropriate payment levels for procedures such as combined abdominal/pelvic CT scans continues, it is important for objective reports of current private insurance payments and utilization be available to inform decision making.
Strikingly, utilization of combined CT scans of the abdomen and pelvis experienced significantly accelerated growth in 2011. While new uses for abdominal/pelvic CTs are advancing diagnostic and treatment capabilities (Fletcher et al. 2009), warranting some growth in these scans, such a sharp upturn in 2011 may be plausibly attributed to the coding policy change and thus may reflect medically unnecessary overuse in response to changing financial incentives. It is possible that increased rate of utilization of the combined CTs and decreased utilization of the single CTs was caused as providers responded to the drop in payments by ordering more combined scans to keep total payments at a steady level. Given our finding of a significant drop in utilization of abdomen‐only scans, providers may have also ordered combined scans rather than single scans due to the former's higher reimbursement rate (an example of “up‐coding”). Prior research has shown that physicians do engage in practices to ensure their overall income remains stable (McGuire and Pauly 1991), and past bundling of other CPT codes has been shown to affect total income earned by providers. A relationship between increased physician referral for imaging services due to financial incentives has been documented in both Medicare and private insurance populations (Congress of the United States 2008; Mettler et al. 2009).
Finally, even with the increase in utilization observed in 2011, overall annual payments for combined CT scans of the abdomen and pelvis decreased between 2010 and 2011. Prior policy measures have had similar effects on imaging payments. The Deficit Reduction Act of 2005, which took effect on January 1, 2007, reduced Medicare reimbursement for the technical component of most outpatient advanced imaging. An analysis by the GAO estimated that in response, overall Medicare Part B payments for imaging procedures declined 12.7 percent, despite a 3.9 percent increase in the utilization of advanced imaging (U.S. Government Accountability Office 2008; Levin, Rao, and Parker 2010). However, given that combined abdomen/pelvis CT utilization is growing at a more rapid rate, the decline in overall payments may not be sustainable in the long run.
Our study does have some limitations. As a retrospective observational analysis, our results cannot prove causality. Other changes in policy or clinical use that occurred at the start of 2011 could also have affected our results. To our knowledge, no new policies of shifts in clinical practice related to imaging payments or utilization occurred at this time, which supports our hypothesis that the observed changes in payments for and utilization of the combined CTs of the abdomen and pelvis were caused by the new coding policy and change in Medicare reimbursement scheme. However, as this is a claim‐based study without access to detailed medical records, further investigation of trends in the clinical indicators for CT scans—including appropriateness of a single or combined scan—is warranted.
Given the nature of the claims database this information was drawn from, our study is not generalizable to the entire U.S. population, as it only represents persons under age 65 who are covered by employer‐sponsored private insurance. Given that we had to recode combined CT scans of the abdomen and pelvis performed before 2011 (as no one single CPT code captured these scans), it is possible some combined scans were misclassified, and actually represented an abdomen CT scan performed during one part of the day, and a pelvis CT scan performed at an entirely different imaging session later that day. Another limitation of our study is the short 3‐year time frame. Finally, we could not capture utilization of CT scans if a claim was never submitted or was submitted to a secondary insurer not included in the MarketScan database.
Despite these limitations, our study has many strengths that make the results important for providers and policy makers alike. Our use of a nonintervention control group (CT scans of abdomen or pelvis alone) significantly strengthens the plausibility of a causal link between the CPT coding and Medicare reimbursement changes of 2011, and the decline in private insurance payments and increase in utilization of combined CT scans of the abdomen and pelvis. As our analysis was restricted to enrollees for whom data were available on for all 3 years of the study period, our utilization results cannot be due to random differences in study samples from year to year. Finally, our ability to report payments, rather than charges, allows us to comment on the actual health care expenditures being outlaid by payers and received by providers. This information is crucial in understanding the efficacy of policy changes in controlling health care costs.
In the wake of the Affordable Care Act, policy makers are preparing to leverage comprehensive cost‐control measures on the health care industry in a way that has never been seen in the American private sector (Baldwin 2012). While policy makers should try to address other factors related to imaging overutilization, such as variation in practice behaviors, uncertainty about the appropriate use of scans, and duplicate imaging (Hendee et al. 2010), our data suggest financial incentives and reimbursement remains a significant problem that requires special attention. Our analysis shows that policy makers and researchers can use administrative claims databases to effectively monitor the effects (both intended and unintended) of major payment reforms. Future investigation of the tradeoff between potential cost savings of bundling similar services and incentivizing increased utilization would inform health care policy makers and practitioners. For example, in 2012, Medicare reassigned the CPT codes for combined CT scans of the abdomen and pelvis to two newly created ambulatory payment classifications levels with higher associated payment rates than the 2011 categories. Claims databases can provide a valuable resource for analysis of this change in reimbursement levels, as well as any corresponding changes in private insurance reimbursement, and will provide insight into the incremental effects of payment modifications on utilization.
Supporting information
Appendix SA1: Author Matrix.
Table S1. Estimated Impact of the 2011 Coding Change on Payments (Full Model).
Table S2. Estimated Impact of the 2011 Coding Change on Utilization (Full Model).
Figure S1. Median Adjusted Payment Per Combined CT Scan of the Abdomen and Pelvis by Health Plan Type.
Figure S2. Median Adjusted Payment Per Combined CT Scan of the Abdomen and Pelvis by Region.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: The authors thank Howard J. Cabral, Ph.D.; Randall P. Ellis, Ph.D.; and Lewis E. Kazis, Ph.D., for their comments on earlier drafts of this manuscript. They also appreciate feedback received from participants of the BU SPH Health Services Research M.S./Ph.D. seminars and the Boston University Health Reading Group.
Disclosures: None.
Disclaimers: None.
Jake R. Morgan and Vanessa L. Merker contributed equally to the publication.
References
- Allen, B., Jr , Donovan W. D., McGinty G., Barr R. M., Silva E. III, Duszak R. Jr, Kim A. J., and Kassing P.. 2011. “Professional Component Payment Reductions for Diagnostic Imaging Examinations When More Than One Service Is Rendered by the Same Provider in the Same Session: An Analysis of Relevant Payment Policy.” Journal of the American College of Radiology 8: 610–6. [DOI] [PubMed] [Google Scholar]
- Armao, D. , Semelka R. C., and Elias J. Jr. 2012. “Radiology's Ethical Responsibility for Healthcare Reform: Tempering the Overutilization of Medical Imaging and Trimming Down a Heavyweight.” Journal of Magnetic Resonance Imaging 35: 512–7. [DOI] [PubMed] [Google Scholar]
- Baldwin, G. 2012. “Tight Squeeze: Imaging is Facing Ever‐Closer Scrutiny on Reimbursement and Utilization. Is a New Role for Radiologists in the Making?” Health Data Management 20: 26–8, 30, 32. [PubMed] [Google Scholar]
- Clemens, J. , and Gottlieb J. D.. 2013. Bargaining in the Shadow of a Giant: Medicare's Influence on Private Payment Systems. NBER Working Paper 19503. Washington, DC: National Bureau of Economic Research. [Google Scholar]
- Congress of the United States . 2008. Budget Options. Vol. 1, Health Care. Washington, DC: Congressional Budget Office. [Google Scholar]
- Duszak, R., Jr , Silva E. III, Kim A. J., Barr R. M., Donovan W. D., Kassing P., McGinty G., and Allen B. Jr. 2013. “Professional Efficiencies for Diagnostic Imaging Services Rendered by Different Physicians: Analysis of Recent Medicare Multiple Procedure Payment Reduction Policy.” Journal of the American College of Radiology 10: 682–8. [DOI] [PubMed] [Google Scholar]
- Fletcher, J. G. , Takahashi N., Hartman R., Guimaraes L., Huprich J. E., Hough D. M., Yu L., and McCollough C. H.. 2009. “Dual‐Energy and Dual‐Source CT: Is There a Role in the Abdomen and Pelvis?” Radiologic Clinics of North America 47: 41–57. [DOI] [PubMed] [Google Scholar]
- Hendee, W. R. , Becker G. J., Borgstede J. P., Bosma J., Casarella W. J., Ericsson B. A., Maynard C. D., Thrall J. H., and Wallner P. E.. 2010. “Addressing Overutilization in Medical Imaging.” Radiology 257: 240–5. [DOI] [PubMed] [Google Scholar]
- Horný, M. , Burgess J. F., Horwitt J., and Cohen A. B.. 2014. “Advanced Diagnostic Imaging in Privately Insured Patients: Recent Trends in Utilization and Payments.” Journal of the American College of Radiology 11: 692–7. [DOI] [PubMed] [Google Scholar]
- Huskamp, H. A. , and Newhouse J. P.. 1994. “Is Health Spending Slowing Down?” Health Affairs (Millwood) 13: 32–8. [DOI] [PubMed] [Google Scholar]
- Iglehart, J. K. 2006. “The New Era of Medical Imaging: Progress and Pitfalls.” New England Journal of Medicine 354: 2822–8. [DOI] [PubMed] [Google Scholar]
- IMV Medical Information Division . 2012. IMV 2012 CT Market Outlook Report. Des Plaines, IL: IMV Medical Information Division. [Google Scholar]
- International Monetary Fund . 2013. “GDP Deflator” [accessed on June 5, 2013]. Available at http://elibrary-data.imf.org/public/FrameReport.aspx?v=3&c=20840382
- Keehan, S. , Sisko A., Truffer C., Smith S., Cowan C., Poisal J., and Clemens M. K., and National Health Expenditure Accounts Projections Team . 2008. “Health Spending Projections through 2017: The Baby‐Boom Generation Is Coming to Medicare.” Health Affairs (Millwood) 27: w145–55. [DOI] [PubMed] [Google Scholar]
- Lee, D. W. , and Levy F.. 2012. “The Sharp Slowdown in Growth of Medical Imaging: An Early Analysis Suggests Combination of Policies Was the Cause.” Health Affairs (Millwood) 31: 1876–84. [DOI] [PubMed] [Google Scholar]
- Levin, D. C. , Rao V. M., and Parker L.. 2010. “Physician Orders Contribute to High‐Tech Imaging Slowdown.” Health Affairs (Millwood) 29: 189–95. [DOI] [PubMed] [Google Scholar]
- Levin, D. C. , Rao V. M., and Parker L.. 2014. “Financial Impact of Medicare Code Bundling of CT of the Abdomen and Pelvis.” American Journal of Roentgenology 202 (5): 1069–71. [DOI] [PubMed] [Google Scholar]
- McGuire, T. G. , and Pauly M. V.. 1991. “Physician Response to Fee Changes with Multiple Payers.” Journal of Health Economics 1991 (10): 385–410. [DOI] [PubMed] [Google Scholar]
- MedPAC . 2011. Variations in Private Sector Payment Rates. Report to the Congress: Medicare and the Health Care Delivery System. Washington DC: MedPAC. [Google Scholar]
- Mettler, F. A., Jr , Bhargavan M., Faulkner K., Gilley D. B., Gray J. E., Ibbott G. S., Lipoti J. A., Mahesh M., McCrohan J. L., Stabin M. G., Thomadsen B. R., and Yoshizumi T. T.. 2009. “Radiologic and Nuclear Medicine Studies in the United States and Worldwide: Frequency, Radiation Dose, and Comparison with Other Radiation Sources–1950–2007.” Radiology 253: 520–31. [DOI] [PubMed] [Google Scholar]
- Nisenbaum, H. L. , Birnbaum B. A., Myers M. M., Grossman R. I., Gefter W. B., and Langlotz C. P.. 2000. “The Costs of CT Procedures in an Academic Radiology Department Determined by an Activity‐Based Costing (ABC) Method.” Journal of Computer Assisted Tomography 24: 813–23. [DOI] [PubMed] [Google Scholar]
- Silva, E., III . 2010. “New Codes from a New Source: The Rolling Five‐Year Review.” Journal of the American College of Radiology 7: 10–2. [DOI] [PubMed] [Google Scholar]
- Silva, E., III . 2011. “The Significance of 2011's New Codes.” Journal of the American College of Radiology 8: 10–1. [DOI] [PubMed] [Google Scholar]
- U.S. Census Bureau . 2012. Current Population Reports, P25‐1095; Table US‐EST90INT‐04‐Intercensal Estimates of the United States Resident Population by Age Groups and Sex 2010. Washington, DC: U.S. Census Bureau. [Google Scholar]
- U.S. Government Accountability Office . 2008. Medicare: Trends in Fees, Utilization and Expenditures for Imaging Services before and after Implementation of the Deficit Reduction Act of 2005. Pub. No. GAO‐08‐1102R. Washington, DC: GAO. [Google Scholar]
- White, H. 1980. “A Heteroscedasticity‐Consistent Covariance Matrix Estimator and a Direct Test for Heteroscedasticity.” Econometrica 48 (4): 817–38. [Google Scholar]
- Williams, R. D. , Rousseau A., and Glaudemans J.. 2005. Pricing Variations in the Consumer Market for Diagnostic Imaging Services. Washington, DC: Avalere Health. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix SA1: Author Matrix.
Table S1. Estimated Impact of the 2011 Coding Change on Payments (Full Model).
Table S2. Estimated Impact of the 2011 Coding Change on Utilization (Full Model).
Figure S1. Median Adjusted Payment Per Combined CT Scan of the Abdomen and Pelvis by Health Plan Type.
Figure S2. Median Adjusted Payment Per Combined CT Scan of the Abdomen and Pelvis by Region.


