Abstract
Issues
Preoperative alcohol use is associated with an increase in postoperative morbidity and mortality. Short-term abstinence prior to elective surgery has been shown to reduce postoperative risks. Therefore, behavioural intervention (BI) targeting risky drinking may have significant utility in preventing surgical complications.
Approach
The literature was systematically reviewed to identify the scope and outcomes of BIs aiming to reduce alcohol use in risky drinkers before they underwent surgery. Five databases were searched using PRISMA criteria. Of 1243 studies identified, four met pre-established inclusion criteria: (i) implementation of a BI prior to an elective surgery; (ii) the BI-targeted alcohol use among risky drinkers; and (iii) printed in English.
Key Findings
Two studies indicated significant reductions in alcohol use at follow ups, and one study demonstrated reductions in postoperative risks. These findings are encouraging, but in light of methodological limitations, the efficacy of preoperative BIs for risky drinking could not be determined.
Implications
Future efforts to screen and implement BIs addressing alcohol use in preoperative patients should carefully define risky drinking, allow ample time for recruitment prior to surgery, implement empirically supported interventions, examine the impact of relevant covariates, and consider the statistical power needed to detect change in postoperative complications.
Conclusion
Given the strong link between preoperative alcohol use and postoperative risks, additional research on preoperative BIs is critically needed. Existing research suggests several promising directions for research that may enhance future intervention efforts with this high-risk population.
Keywords: alcohol drinking, preoperative period, elective surgical procedure, brief psychotherapy, behavioural medicine
Background
Alcohol use is now the third most common cause of disease worldwide [1]. Alcohol use is implicated in 3.8% of global deaths, and accounts for 4.6% of global disability adjusted life years (i.e. the number of life years lost to ill health) [2]. In terms of economic costs, the consequences of alcohol use account for approximately 1% of the gross domestic product in high- and middle-income countries [1], and a large proportion of this spending is attributed to health-care costs [3]. In the USA, the estimated economic cost of excessive drinking is approximately $223.5 billion annually, or $1.90 per alcoholic drink, with 11% of this cost attributed to health-care expenditures [4]. On average, each high-income nation spends $23 billion on alcohol-related health-care annually.
Individuals interacting with the medical system are more likely to have alcohol use disorders (AUD) relative to the general population. AUDs are defined as ‘medical conditions’ diagnosed when a person’s drinking causes distress or harm, and include diagnoses of ‘alcohol abuse’ and ‘alcohol dependence’ [5]. Among medical patients, prevalence of AUDs is above 20% [6–8]. While there may be some health benefits to light drinking, the impact of alcohol on health and disease is largely detrimental [9,10]. AUDs contribute to many disease categories including diabetes mellitus, hypertension, cardiovascular disease, stroke, numerous cancers and pneumonia [10,11].
Alcohol use and postoperative morbidity and mortality
The detrimental impact of alcohol use on health extends to surgical risk and recovery. Risky drinking (defined as approximately two to three standard drinks per day or >24 g day for women; >36 g day for men [12]); is one of the 10 most common preoperative surgical risks in the USA, and is one of the few that is modifiable [13]. The pathophysiological effects of excessive alcohol consumption on the body that may impact surgery include increased susceptibility to bacterial infection [14], decreased immune functioning [15,16], organ dysfunction [17], bleeding complications [18,19] and nutrition deficiency [20]. These pathophysiological effects that impact the body’s ability to heal and recover from ill health have important implications for surgical recovery.
A growing body of research indicates that risky drinking prior to surgery can have a detrimental impact on postoperative recovery [19,21–27]. Rates of risky alcohol use prior to elective surgeries range from 30.0% to 88.5% among otolaryngology surgeries, from 29% to 33% among vascular and thoracic surgeries and from 7.7% to 28.0% among other types of surgery [28]. The research linking risky drinking and postoperative problems is robust. A recent meta-analysis of 55 studies (n = 1,234,923) linked risky alcohol use to an increase in overall morbidity, general infections, wound complications and pulmonary complications following surgery [12]. This meta-analysis also found ‘very risky’ drinking (defined as >60 g day) was associated with a two- to fourfold increase in postoperative complications [12,19] and increased rates of postoperative mortality [12].
As an individual’s alcohol consumption increases, so does postoperative risk; every additional point scored on the consumption questions of the Alcohol Use Disorder Identification Test (AUDIT-C [29] ) is associated with a 29% increase in the expected number of postsurgical complications [30]. In a study of 8811 surgical patients in the US Veterans Affairs Health Care System, patients drinking two or more drinks a day combined with an AUDIT-C score ≥5 were significantly more likely to experience postoperative complications and those with an AUDIT-C score ≥9 had a higher risk of complications, longer hospital length of stay and more days spent in the intensive care unit [31].
The timing of drinking may also be important with regards to postoperative risk and recovery. In one study, risky drinking in the 2 weeks immediately preceding surgery was associated with postoperative risks, while a more remote history of risky drinking did not predict postoperative complications [31]. A randomised controlled trial (RCT) demonstrated that 4 weeks of preoperative abstinence reduced postoperative complications by over 50% among colorectal surgery patients who reported daily drinking ≥60 g of ethanol at baseline [32].
Need for preoperative alcohol use interventions
Abstinence from alcohol for 4–8 weeks is recommended prior to surgery [33]. Therefore, there is a need to develop and implement effective interventions that reduce alcohol during this critical time period. However, the best method to identify and intervene in alcohol use among preoperative patients is yet to be determined. Behavioural interventions (BI), particularly brief interventions using motivational interviewing, are an accepted and recommended approach to reduce risky drinking in medical and non-medical settings [30,33,34] and may therefore be a viable approach to reduce preoperative risky drinking. In this review, a BI is defined as any therapeutic encounter designed to reduce alcohol use through psychological means (e.g. talk therapy, motivational interviewing). A number of empirically supported BIs exist, including brief motivational interventions (BMI) [35,36]; screening, brief intervention, and referral to treatment (SBIRT) [37]; cognitive behavioural therapies [38]; other individual and group therapies; and even telephone and computer-delivered interventions [39,40]. Brief interventions may be an appropriate approach for many patients, particularly those drinking at risky, but non-dependent levels [41]. Furthermore, brief interventions have demonstrated cost-effectiveness when compared with treatment as usual (TAU), and as such have been increasingly applied in medical settings to reduce alcohol use and alcohol-related consequences among at-risk patients [42–46].
Objective
In light of research indicating preoperative alcohol use can lead to significant complications following surgery, the primary aim of this review was to identify and provide a summary of the research literature on BIs for preoperative alcohol use. We chose to focus on BIs to expand on a past review that summarised research on pharmacotherapy for preoperative alcohol use [33]. In addition, given this nascent area of research, we aimed to provide a narrative summary of existing study designs, objectives, participants, interventions used and research outcomes. The secondary aim of this review was to use this burgeoning literature base to make recommendations for future research.
Method
Search strategy and selection of studies
We applied the PRISMA systematic review criteria [47] to search for and identify published studies that examined behavioural alcohol use interventions among preoperative populations. Literature searches were conducted within five databases including PsycINFO, PubMed, CINAHL, Medline, Web of Science and Cochrane databases. The search was conducted using combinations of the following terms to ascertain relevant papers: [ (surgery OR surgical OR preoperative OR perioperative) AND (alcohol OR alcoholic OR drinker OR drinking) AND (intervention OR psychosocial OR behavioural) ]. For Cochrane databases, search terms were confined to ‘Title’ and ‘Abstract’ fields.
Once identified through database searches, duplicates were deleted and all papers were screened at the abstract and title level to determine eligibility for full-text screening. Papers that explicitly mentioned a behavioural alcohol intervention for preoperative patients were obtained and their text reviewed. Papers were included if they met the following a priori criteria: (i) original research published in a peer-reviewed journal (thus excluding conference proceedings, dissertations and book chapters); (ii) the study sample included preoperative patients drinking alcohol at risky levels (risk was defined as drinking above recommended health guidelines in the nation the study was conducted); and (iii) the study included a BI that addressed alcohol use reduction prior to elective surgery. Study inclusion criteria were not limited solely to RCTs; pre-post experimental designs were also included. The experimental treatment had to include a behavioural alcohol use treatment component as a stand-alone intervention or within a broader intervention context. Studies were excluded if they were not available in the English language, targeted trauma or emergency surgeries only, or recruited transplant or bariatric surgery exclusively. Studies published up to October 2013 were eligible for inclusion. No date range parameters were included in the search terms.
Two researchers independently coded each included study. Operational definitions were provided in a code-book to ensure consistent and accurate categorisation throughout the coding process. Satisfactory intercoder reliability was established with an average percentage of agreement across all categories of 94%. Any disparities in judgment that emerged during the coding process were resolved through discussion.
Assessment of risk of bias in included studies
Three researchers independently assessed risk of bias. Risk of bias was assessed for RCTs using guidelines outlined by Higgins and colleagues [48], and for non-randomised trials using guidelines outlined by Barnaby and colleagues [49].
Results
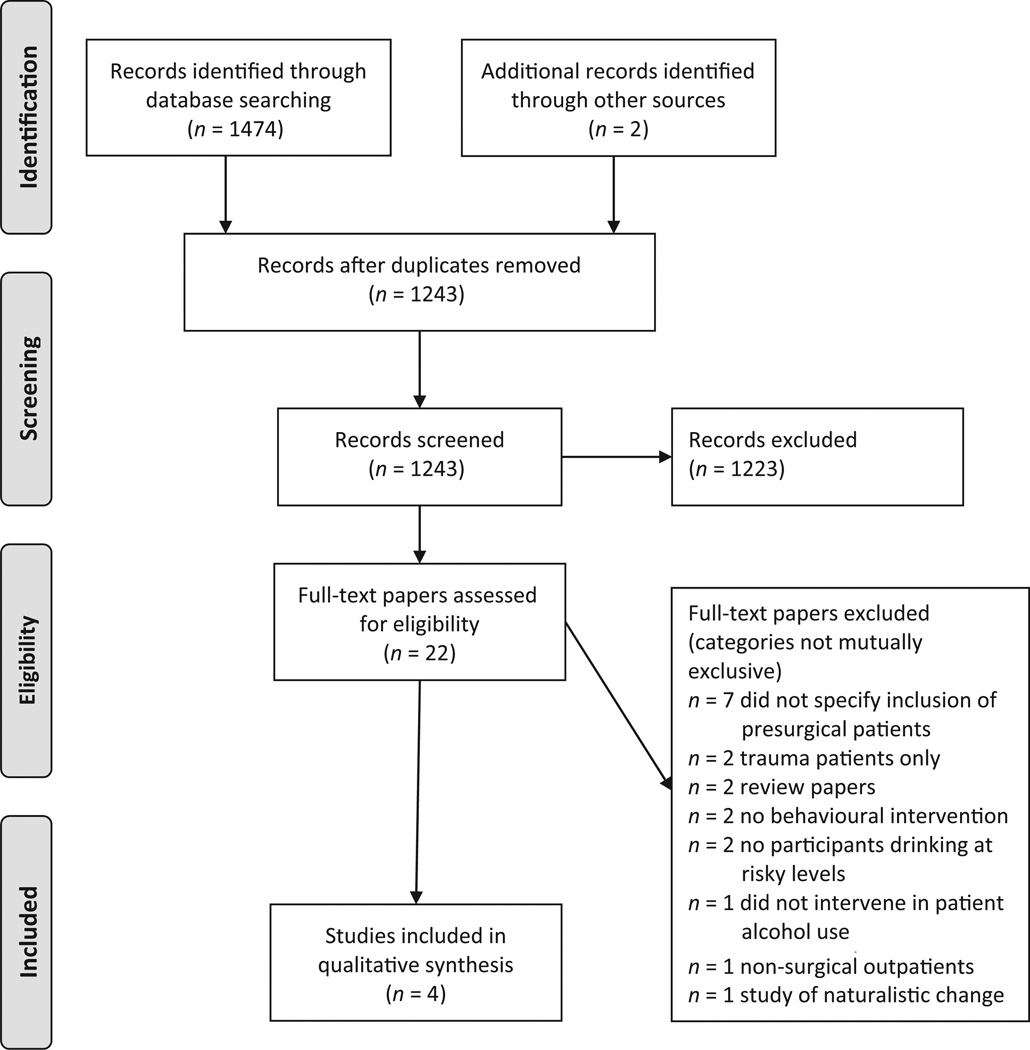
Through searching online databases, 1476 papers were identified (see Figure 1). After removing duplicates (n = 233), 1243 unique papers were identified. After screening, 22 papers underwent full-text review to determine eligibility. Of these, four studies represented original research that implemented a BI that aimed to reduce preoperative alcohol use among ‘risky drinking’ patients scheduled for elective surgeries. Unpublished data were requested from two authors, of whom one responded and agreed to share data for this review. Because of the small numbers of studies and heterogeneity in assessment and methodology, we elected to provide a narrative, descriptive summary of the research emphasising study design, participants, recruitment and retention issues, the interventions studied, and research outcomes.
Figure 1.
Study flow diagram
Study design and participants
The study design and participant information for all four studies are presented in Table 1. All four studies [50–53] used a pre-/post-test experimental controlled design, but only two randomised participants to study condition [50,51]. TAU control groups were used for comparison in all studies. The included studies were conducted in either Australia or Europe. Participants were scheduled for a range of elective surgeries including general surgery, hip and knee arthroplasty, and coronary bypass surgery. Participants were typically recruited in hospitals, although one study used a mailed letter to recruit patients. The samples ranged from n = 98 to n = 136. All studies included women, but men were overrepresented at a rate of about 3:1. The average age of participants across studies ranged from 52 to 70 years old. None of the studies reported race or ethnicity of participants. Studies targeted a range of outcomes related to alcohol use and postoperative complications.
Table 1.
Study design, participants, and interventions for included studies
| Paper | Design | Groups | n | Country | Surgery | Women | Age (M) | Alcohol risk definition |
Intervention | Behavioural targets of intervention |
Interventionist | Intervention timing |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Kummel et al. [50] |
RCT | IG vs. TAU | 117 | Finland | Coronary artery bypass |
27.3% | IG=61 TAU = 63 | Not specified | Group ‘health counselling, guidance, and adjustment education’ to |
‘Physical, mental-emotional, and social abilities’ including alcohol use |
Nurse | Not specified; 1 of 5 sessions took place prior to surgery |
| McHugh et al. [51] |
RCT | IG vs. TAU | 98 | Scotland | Coronary artery bypass |
24.5% | IG=70 TAU = 71 | Not specified | Home-based health education and motivational interviewing |
Tailored to patient risk (smoking, physical activity, diet, alcohol use and hypertension). |
Nurse | Monthly for an average of 8 months |
| Shourie et al. [52] |
CT | IG vs. TAU | 136 | Australia | Elective | 19.8% | IG=55 TAU = 52 | AUDIT-C > 4, > 60 g day−1— men; > 40 g day−1 women; and CIDI |
‘Drink-less’ Intervention. Dependent drinkers also receive treatment referral. |
Alcohol use only | Member of research team |
IG > 7 days prior to surgery; TAU < 7 days prior to surgery |
| Hansen et al. [53] |
CT | IG vs. TAU | 132 | Denmark | Hip and knee |
49.2% | IG=68 TAU = 69 | Men > 21 g week−1; Women > 14 g week−1 |
‘Motivational conversation’ followed by information and recommendations. |
Tailored to patient risks (nutrition, health/ medication, physical activity, smoking, and alcohol use) |
Nurse | Average 4 weeks prior to surgery |
BI, brief intervention; CIDI, composite international diagnostic interview; CT, clinical trial; IG, intervention group; RCT, randomised clinical trial; TAU, treatment as usual.
Recruitment and retention
Recruitment periods across the four studies ranged from 4 months to 3.5 years. Shourie and colleagues [52] spent 2 years and 10 months screening elective surgery patients in two hospitals. Of 3783 patients approached 3139 (83%) were successfully screened and 617 met initial alcohol screening criteria (≥5 on the AUDIT-C). After additional screening, 136 patients (4.3%) were recruited. At the 6 month follow up, 119 (88%) were retained. The authors also reported difficulty recruiting patients at least 7 days to surgery. As a result, they abandoned randomisation and allocated groups to the intervention and control conditions based on the interval from screening to surgery.
McHugh and colleagues [51] invited all patients on a coronary bypass surgery waitlist to participate in their study over the 15 month study period. Of the 147 invited, 125 (85%) agreed to participate and 98 (78%) completed baseline and final follow ups. Kummel and colleagues [50] screened 449 patients scheduled for cardio artery bypass at a single hospital over a 3.5 year period. Of those, 38% (n = 173) met inclusion criteria (≥65 years old and scheduled for elective surgery). More than half of the eligible patients (n = 117; 68%) completed baseline and 3 month follow up and were included in the study analysis. Hansen and colleagues [53] screened all patients scheduled for surgery during 2 month blocks in the winter and spring of the study year. A total of 140 patients were eligible and eight (6%) refused participation. In total, 132 patients were recruited. Medical data were obtained for all participants at the 3 month follow up.
Interventions
Interventions varied in terms of theoretical orientation, behavioural targets and frequency of sessions. Single-session [52,53] and multiple-session [50,51] treatments were utilised. Interventions were delivered by nurses (n = 3), or a ‘member of the research team’ (n = 1). Three studies examined the efficacy of interventions targeting alcohol use in addition to other preoperative risk factors such as physical activity, nutrition, emotional stress and medication non-adherence [50,51,53].
In terms of intervention theory and framework, one study [52] used a protocol-based, empirically supported intervention based on the World Health Organization-based ‘Drink-less’ program [54,55]. In this study, all participants received ‘Drink-less’, and dependent drinkers were also offered a consult with a drug and alcohol specialist for management of withdrawal symptoms and pharmacotherapy. Two additional studies reported using a motivational ‘conversation’ or motivational interviewing as part of their intervention approach, but did not cite the use of specific intervention techniques or protocols, or fidelity monitoring [51,53].
Study outcomes
Alcohol use
All four studies assessed alcohol use at baseline and targeted alcohol use in an intervention. Only two studies reported alcohol use outcomes [50,52] and a third [51] provided de-identified alcohol use data for this review (see Table 2). Overall, findings were mixed. Shourie and colleagues [52] reported the entire sample (intervention and TAU) reduced alcohol use at the 6 month follow up. Average daily alcohol use fell from 70 g day−1 at baseline to 26 g day−1 in the entire sample, a 63% reduction (natural log transformed, t= 25.6; P < 0.001), but between-group comparisons were not significant. In contrast, Kummel and colleagues [50] reported a significant time by group interaction (P < 0.001), such that the intervention group was more likely to report ‘no drinking’ at the 3 month follow up relative to baseline, odds ratio (OR) = 2.2, 95% confidence interval (95% CI) [1.5, 3.3] than the control group OR= 1.3, 95% CI [1.1, 1.4].
Table 2.
Assessment-timing, outcomes and results of included studies
| Paper | Follow-up assessments time points |
Alcohol outcomes | Postoperative physical health outcomes |
Other intervention Outcomes |
Summary of significant results: alcohol use |
Summary of significant results: physical health |
|---|---|---|---|---|---|---|
| Kummel et al. [50] |
3, 6 and 12 months | Alcohol use frequency (none, one to two times a month or less, or weekly) |
Angina pectoris Health and functioning (e.g. ability to climb stairs) |
Exercise/PA Diet/nutrition ‘Nervousness’ Depression |
Relative to baseline, the IG decreased alcohol use at 3 months while the CG increased alcohol use at 6 and 12 months |
Relative to baseline, the IG was more likely to report ‘no angina pectoris symptoms at 3 months; however, the CG was more likely to report ‘no angina pectoris symptoms’ at 6 and 12 months. |
| McHugh et al. [51] |
15 months | Grams per week alcohola | Body mass index Blood pressure Plasma cholesterol General health status |
Smoking Exercise/PA |
From baseline to follow up, average weekly alcohol consumption decreased in the IG and increased in the CG. |
Relative to the CG, the IG had a significant decrease in body mass index, cholesterol and blood pressure at follow up. The IG also had significant increases in general health status and functioning. |
| Shourie et al. [52] |
Hospital discharge and 6 months |
AUDIT-C score Average daily alcohol consumption Alcohol dependence diagnosis (DSM-IV) |
Major postoperative complications (e.g. repeat surgery, transfusion) Minor postoperative complications (e.g. wound infections) Mortality Physical functioning |
Number of visits to GP Hospital admissions Days unable to work Smoking |
The entire sample reduced alcohol use at follow up, but there were not significant between-group differences in AUDIT-C score, daily alcohol use or diagnosis of alcohol dependence. |
No between-group differences in postoperative morbidity, mortality or health-care utilisation. |
| Hansen et al. [53] |
3 months | Number of patients meeting alcohol risk criteria reported for baseline assessment only |
Unintentional patient pathb Sum of postoperative complications Mortality General health status ‘Disease Specific Outcome Score’ (e.g. walking distance) |
Hospital length of stay Hospital readmission |
Post-intervention alcohol use was not reported |
There were significantly fewer unintentional patient pathsb in the IG relative to the CG. |
Unpublished result. Data provided by author.
An unintentional patient path was defined as ‘a path by which the patient did not reach the discharge criteria within five days (minor complications), or had any postoperative complication within three months (major complications) leading to a non-planned inpatient visit, was readmitted within three months irrespective of cause, or died within three months postoperatively irrespective of cause.’
AUDIT-C, Alcohol Use Identification Test; CG, control group; DSM-IV, Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition; GP, general practitioner; IG, intervention group; PA, physical activity.
The third study did not report alcohol use outcomes [51], but provided unpublished, de-identified alcohol use outcome data to the authors of this review (ncontrol = 42; nintervention = 43). Using the data provided, we conducted a repeated-measures analysis of variance to analyse mean differences in weekly alcohol use across group and time. Alcohol quantity is presented in standard drinks, equivalent to 25 mL of 40% alcohol (8 g of pure alcohol). The main effect of time was not significant, F(1, 83) = 0.045, P = 0.83, but the time by group interaction was significant F(1, 83) =47.262, P = 0.002, η2 = 0.11. From baseline to follow up, the intervention group decreased their average quantity of weekly alcohol consumption from 6.93 drinks per week (SD = 10.49) to 5.77 drinks week (SD = 7.38). In contrast, the control group increased their quantity of alcohol consumption from 6.55 drinks week−1 [standard deviation (SD) = 8.51] at baseline to 7.88 drinks per week (SD = 10.11) at follow up.
Postoperative mortality
Two studies examined postoperative mortality, Hansen and colleagues [53] reported no group differences at 3 month follow up (no deaths in either group). Shourie and colleagues [52] reported no group differences in mortality at the 6 month follow up (one death in each group).
Postoperative morbidity
Two of the four studies reported outcomes related to postoperative complications. Shourie and colleagues [52] reported no significant differences in postoperative morbidity, length of hospital stay, number of doctor visits or hospital admissions. In contrast, Hansen and colleagues [53] reported significant differences in the number of ‘unintended patient paths’ defined as minor postoperative complications, major postoperative complications, readmissions or death within 3 months postoperatively. There were significantly fewer unintended paths in the intervention group (n = 14; 18%) relative to the control group (n = 19; 35%), P = 0.025, adjusted OR = 0.34, 95% CI [0.13, 0.84]. There were nine complications (e.g. pneumonia, infections, swelling) in the control group and seven in the intervention group in the 3 months postoperatively, and the median hospital length of stay was 1 day shorter in the intervention group, P < 0.001, 95% CI [0.3, 1.7].
Results of bias assessment
The risk of bias in RCTs was unclear because of limited reporting of trial details (see Table 3). However, some areas of risk were identified such as higher dropout rates among older and less healthy women in one study [50] and lack of blinding of participants and personnel in another study [51]. Non-randomised trials used appropriate prospective design, hypothesis generation and compared groups at baseline.
Table 3.
Risk of bias summary for included trials
| Random sequence generation (selection bias) |
Allocation concealment (selection bias) |
Blinding of participants and personnel (performance bias) |
Blinding of outcome assessment (detection bias) |
Incomplete outcome data (attrition bias) |
Selective reporting (reporting bias) |
|
|---|---|---|---|---|---|---|
| Randomised controlled trials | ||||||
| Kummel et al. [50] | ||||||
| McHugh et al. [51] | ||||||
| Was there a comparison? |
How were the groups assigned? |
Was the baseline and allocation prospective? |
Was outcome assessment prospective? |
Was hypothesis generation prospective? |
Was comparability of groups assessed? |
|
| Non-randomised controlled trials | ||||||
| Shourie et al. [52] | Yes | Time to surgery | Yes | Yes | Yes | Yes |
| Hansen et al. [53] | Yes | Time to surgery | Yes | Yes | Yes | Yes |
+, indicates high risk of bias; −, indicates low risk of bias; ?, indicates unclear risk of bias.
Discussion
This systematic literature review summarised the methods and results of four controlled trials of BIs for risky alcohol use in preoperative patients. The small number of studies attempting to reduce preoperative alcohol use is perhaps the most striking findings of this review, especially given the potential benefits of reducing alcohol use prior to surgery. The small literature base provides two important themes. First, BIs appear to be feasible and acceptable to preoperative patients. All four studies completed recruitment with relatively low rates of refusal and were able to retain study participants through intervention and follow-up periods. Second, BIs were linked to significant reductions in alcohol use in two studies, and significant reduction in postoperative complications was reported in one. One study reported null findings for between-group differences in alcohol use and postoperative morbidity. The small number of studies and methodological limitations of this research makes it premature to draw conclusions regarding the efficacy of preoperative behavioural alcohol use interventions. Therefore, more targeted and carefully designed trials of preoperative BIs are needed.
Recommendations and future directions for research and practice
The literature summarised in this review highlights many considerations and challenges that researchers may want to consider when implementing and studying BIs prior to surgery. The next section presents strategies to anticipate and ameliorate these challenges, as well as highlights promising directions for future research.
Recruitment and sample selection
Recruitment and sample selection were significant issues in all four reviewed studies. For example, Shourie and colleagues [52] took close to 3 years to recruit 136 patients from two hospitals. Although 9.7% of screened patients met initial alcohol use inclusion criteria, only 4.3% of the original screened patients were recruited after excluding outpatient surgeries and refusals. Future researchers should be aware that the length of time needed to identify and recruit risky drinkers prior to surgery may be considerable. There are several potential reasons for such delays. There are a finite number of patients awaiting surgery at any one time, and many surgeries occur in an urgent/emergency-care setting where there is not time for intervention and behaviour change. In addition, patient alcohol use is often overlooked by healthcare providers [56], and alcohol use data are often inadequate or unavailable in patient medical charts. This makes identifying and recruiting eligible patients more difficult. Therefore, researchers may want to use broad recruitment strategies such as recruiting from large medical centres and/or multiple sites, allow ample time for study recruitment and implement universal alcohol screening rather than relying on medical charts or physician referral. In addition, in some subpopulations, rates of risky drinking may be low. For example, one study of surgical ‘prehabilitation’ was excluded from this review because none of the participants met risky drinking criteria at baseline [57].
Patient diversity
None of the studies in this review reported patient race or ethnicity, thus limiting the conclusions about intervention outcomes in diverse groups. In terms of age, the majority of participants in the reviewed literature were between 52 and 70 years old. Therefore, researchers and practitioners may want to consider the unique needs of older adults when designing interventions. Alcohol misuse among the ageing population is common [58,59] and contributes to harmful health outcomes as a result of physiological changes in alcohol metabolism and prevalence of comorbid diseases that may be exacerbated by alcohol use [60,61].
Researchers who want to recruit a more diverse population should consider whether alcohol screening is taking place among all groups. Physicians often overlook women and younger patients when screening for alcohol problems prior to surgery [56], and recent research among preoperative patients indicates that most patients drinking at risky levels appear relatively healthy and have health problems unrelated to alcohol use [19,23]. Without unbiased screening, most patients drinking at risky levels will not be detected. Researchers may also want to consider increasing recruitment of more diverse samples by accessing hospital/medical centre data on patient demographics to determine how and where to recruit underrepresented patients, collaborating with women’s clinics and other specialty clinics, setting recruitment quotas based on demographic factors, and including diverse research and clinical staff to recruit patients and serve clinical roles.
Selecting and evaluating a preoperative BI
Research has yet to determine the best intervention for preoperative risky drinking and careful consideration of therapeutic approach is imperative for testing pre-existing approaches or developing new treatments. In this review, only one study used a protocol-based, empirically supported intervention approach, the ‘Drink-less’ intervention [52,55]. Two studies reported using motivational-based approaches, but did not provide details on treatment, training and fidelity of their techniques.
Moving forward, researchers and practitioners should carefully consider the type of intervention best suited to their clinical setting as well as the empirical research on such interventions. One option is to implement empirically supported treatments from other medical settings such as BMI or SBIRT. Brief interventions may be an appropriate behavioural approach for surgical settings given the narrow window for treatment and behaviour change prior to surgery. They are typically less than an hour in length, can be as brief as 5 min, and can be delivered by medical staff including nurses, doctors, social workers or psychologists. Brief interventions have been implemented widely in hospital and clinic settings to reduce alcohol use and alcohol-related consequences among at-risk patients [42–46] and have demonstrated efficacy among hospital inpatients [42] and emergency department and trauma patients following acute alcohol-related injury [35,36,62]. Several reviews of brief alcohol interventions in medical settings are available [42,46], and research supports their cost-effectiveness [63,64].
Intervention delivery and timing
The timing of preoperative alcohol interventions has important implications for intervention outcomes. Specifically, delivering an intervention 1–2 weeks prior to surgery may not provide a sufficient period of alcohol use reduction to impact postoperative outcomes, a methodological problem encountered by one study in this review [52]. Instead, at least 4 weeks of preoperative alcohol abstinence has been recommended to achieve reductions in postoperative complications [33,65–67]. Given the narrow window between surgery referral and completion, researchers and real-world practitioners may consider screening patients as soon as they are referred to surgery and deliver interventions in conjunction with medical appointments early in the referral process. Many patients receiving elective, non-emergency surgeries are monitored for months prior to surgery referral. These patients, if identified through preoperative clinics, could be screened and recruited prior to surgery referral, and receive an intervention when surgeries referral takes place. Likewise, researchers could examine treatments that can be disseminated quickly and easily such as brief in-person sessions, or telephone and computer-based interventions that will ease implementation challenges [39,40].
Data collection and analysis
Improved research methodology is vital to improving our understanding of the impact of alcohol use and alcohol use reduction on surgical outcomes. For example, assessing change in alcohol use following intervention, but preceding surgery is imperative for determining the temporal relationship between alcohol use reduction and postoperative complications. Researchers should also verify abstinence using toxicology screening prior to surgery, as biological verification of sobriety was not reported in any of the reviewed studies. In terms of statistical power, researchers should calculate sample size based on the expected effect size for the intervention and take into account the baseline rate of surgical complications. Only one study conducted power analysis [52], raising the possibility that studies in this review were not able to assess change in some complications because of low number of occurrences. As such, large samples may need to be recruited to detect effects for outcomes with low base rates (e.g. postoperative mortality). In addition, future research could carefully consider and assess covariates related to alcohol use and postoperative recovery, such as smoking, hypertension, diabetes, and other health and demographic variables.
Assessing cost-effectiveness
In this era of limited resources, institutional decision makers frequently demand that interventions and treatments have fiscal as well as clinical justification. Although no study has formally examined the economic impact of preoperative alcohol use, extant data suggest risky drinking results in longer hospital stays and increased utilisation of healthcare services [12,22]. This, combined with research estimating that each avoidable post-surgical complication costs an additional $12 000 to the health-care system [68], clearly indicates the potential cost savings of reducing preoperative alcohol use. Explicitly including cost-effectiveness analyses in future clinical trials will provide detailed estimates of how much can be saved through the implementation of preoperative BIs.
Alternative study designs
Alternatives to RCTs are another avenue for researchers to consider. Hybrid implementation-effectiveness studies may be useful for researchers interested in the concurrent assessment of clinical effectiveness and implementation outcomes of a preoperative BI [69]. In contrast, randomised encouragement designs may be appropriate in some settings where true randomisation is not possible or desirable [70]. Dog leg designs could also be used by researchers who want to compare interventions to ‘usual care’ and reduce the number of patients needed to test an intervention [71].
Limitations of this review
The findings of this review should be considered in the context of some limitations. First, the small number of studies meeting inclusion criteria and the limited reporting of alcohol use and postoperative outcomes made a qualitative review more appropriate than a quantitative review, such as a meta-analysis. Second, postoperative interventions or other hospital-based interventions were not reviewed despite their potential influence on postoperative alcohol use [72]. Third, formal analysis of within-study bias was limited because of lack of detail regarding randomisation (when used), blinding and outcome assessment in randomised trials. Identified bias, such as lack of blinding of participants and personnel is common and often unavoidable in psychosocial intervention literature.
Conclusion
Critical life-events, such as illness and surgery, can represent a ‘window of opportunity’ for health behaviour change [73–76]. At this time, the research on BIs for preoperative alcohol use is promising, but limited in breadth and depth. Several strategies could improve future development and testing of preoperative BIs such as implementing theory-based interventions, at appropriate times, in adequately powered trials. The findings of such well-designed research will greatly enhance the development of efficacious alcohol interventions among this at-risk population.
Acknowledgements
We would like to acknowledge Dr Frederick Burgess for his helpful comments on this paper. The contributions of Drs Fernandez and Claborn were supported in part by grant number T32 AA07459 from the National Institute on Alcohol Abuse and Alcoholism at the National Institute of Health. Dr Borsari’s contribution to this paper was supported by the National Institute on Alcohol Abuse and Alcoholism Grant R01-AA017427 and VISN1 Career Development Award V1CDA2012-18. The contents of this paper are those of the authors and do not necessarily represent the views of the National Institute on Alcohol Abuse and Alcoholism, the Department of Veterans Affairs or the US government.
References
- 1.Lim SS, Vos T, Flaxman AD, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2013;380:2224–2260. doi: 10.1016/S0140-6736(12)61766-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rehm J, Mathers C, Popova S, Thavorncharoensap M, Teerawattananon Y, Patra J. Global burden of disease and injury and economic cost attributable to alcohol use and alcohol-use disorders. Lancet. 2009;373:2223–2233. doi: 10.1016/S0140-6736(09)60746-7. [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization. Global status report on alcohol and health. Switzerland: World Health Organization; 2011. [Google Scholar]
- 4.Bouchery EE, Harwood HJ, Sacks JJ, Simon CJ, Brewer RD. Economic costs of excessive alcohol consumption in the U.S., 2006. Am J Prev Med. 2011;41:516–524. doi: 10.1016/j.amepre.2011.06.045. [DOI] [PubMed] [Google Scholar]
- 5.NIAAA. [accessed December 2013];Alcohol Use Disorders. 2013 Available at: http://www.niaaa.nih.gov/alcohol-health/overview-alcohol-consumption/alcohol-use-disorders.
- 6.Roche AM, Freeman T, Skinner N. From data to evidence, to action: findings from a systematic review of hospital screening studies for high risk alcohol consumption. Drug Alcohol Depend. 2006;83:1–14. doi: 10.1016/j.drugalcdep.2005.10.011. [DOI] [PubMed] [Google Scholar]
- 7.Madras BK, Compton WM, Avula D, Stegbauer T, Stein JB, Clark HW. Screening, brief interventions, referral to treatment (SBIRT) for illicit drug and alcohol use at multiple healthcare sites: comparison at intake and 6 months later. Drug Alcohol Depend. 2009;99:280–295. doi: 10.1016/j.drugalcdep.2008.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ruback MJ, Galbiatti AL, Arantes LM, et al. Clinical and epidemiological characteristics of patients in the head and neck surgery department of a university hospital. Sao Paulo Med J. 2012;130:307–313. doi: 10.1590/S1516-31802012000500007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.National Institute on Alcohol Abuse and Alcoholism. Health risks and benefits of alcohol consumption. Alcohol Res Health. 2000;24:5–11. [PMC free article] [PubMed] [Google Scholar]
- 10.Rehm J, Room R, Graham K, Monteiro M, Gmel G, Sempos CT. The relationship of average volume of alcohol consumption and patterns of drinking to burden of disease: an overview. Addiction. 2003;98:1209–1228. doi: 10.1046/j.1360-0443.2003.00467.x. [DOI] [PubMed] [Google Scholar]
- 11.Molina PE, Gardner JD, Souza-Smith FM, Whitaker AM. Alcohol abuse: critical pathophysiological processes and contribution to disease burden. Physiology. 2014;29:203–215. doi: 10.1152/physiol.00055.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Eliasen M, Grønkjær M, Skov-Ettrup LS, et al. Preoperative alcohol consumption and postoperative complications: a systematic review and meta-analysis. Ann Surg. 2013;258:930–942. doi: 10.1097/SLA.0b013e3182988d59. [DOI] [PubMed] [Google Scholar]
- 13.Khuri SF, Henderson WG, Daley J, et al. Successful implementation of the Department of Veterans Affairs’ national surgical quality improvement program in the private sector: the patient safety in surgery study. Ann Surg. 2008;248:329–336. doi: 10.1097/SLA.0b013e3181823485. [DOI] [PubMed] [Google Scholar]
- 14.Wood S, Pithadia R, Rehman T, et al. Chronic alcohol exposure renders epithelial cells vulnerable to bacterial infection. PLoS ONE. 2013;8:e54646. doi: 10.1371/journal.pone.0054646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Spies C, Eggers V, Szabo G, et al. Intervention at the level of the neuroendocrine-immune axis and postoperative pneumonia rate in long-term alcoholics. Am J Respir Crit Care Med. 2006;174:408–414. doi: 10.1164/rccm.200506-907OC. [DOI] [PubMed] [Google Scholar]
- 16.Von Dossow V, Schilling C, Beller S, et al. Altered immune parameters in chronic alcoholic patients at the onset of infection and of septic shock. Crit Care. 2004;8:R312–R321. doi: 10.1186/cc2911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Von Heymann C, Langenkamp J, Dubisz N, et al. Posttraumatic immune modulation in chronic alcoholics is associated with multiple organ dysfunction syndrome. J Trauma. 2002;52:95–103. doi: 10.1097/00005373-200201000-00017. [DOI] [PubMed] [Google Scholar]
- 18.Schoenfeld H, Perka C, Ziemer S, et al. The perioperative von Willebrand factor activity and factor VIII levels among alcohol use disorder patients undergoing total knee or hip replacement. Subst Use Misuse. 2010;45:1216–1229. doi: 10.3109/10826081003688906. [DOI] [PubMed] [Google Scholar]
- 19.Tonnesen H, Petersen KR, Hojgaard L, et al. Postoperative morbidity among symptom-free alcohol misusers. Lancet. 1992;340:334–337. doi: 10.1016/0140-6736(92)91405-w. [DOI] [PubMed] [Google Scholar]
- 20.Green PH. Alcohol, nutrition and malabsorption. Clin Gastroenterol. 1983;12:563–574. [PubMed] [Google Scholar]
- 21.Bradley KA, Rubinsky AD, Sun H, et al. Alcohol screening and risk of postoperative complications in male VA patients undergoing major non-cardiac surgery. J Gen Intern Med. 2011;26:162–169. doi: 10.1007/s11606-010-1475-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rubinsky AD, Sun H, Blough DK, et al. AUDIT-C alcohol screening results and postoperative inpatient health care use. J Am Coll Surg. 2012;214:296–305. e1. doi: 10.1016/j.jamcollsurg.2011.11.007. [DOI] [PubMed] [Google Scholar]
- 23.Bradley KA, Rubinsky AD, Sun H, et al. Prevalence of alcohol misuse among men and women undergoing major noncardiac surgery in the Veterans Affairs health care system. Surgery. 2012;152:69–81. doi: 10.1016/j.surg.2012.02.007. [DOI] [PubMed] [Google Scholar]
- 24.Neumayer L, Hosokawa P, Itani K, El-Tamer M, Henderson WG, Khuri SF. Multivariable predictors of postoperative surgical site infection after general and vascular surgery: results from the patient safety in surgery study. J Am Coll Surg. 2007;204:1178–1187. doi: 10.1016/j.jamcollsurg.2007.03.022. [DOI] [PubMed] [Google Scholar]
- 25.Lau A, von Dossow V, Sander M, MacGuill M, Lanzke N, Spies C. Alcohol use disorder and perioperative immune dysfunction. Anesth Analg. 2009;108:916–920. doi: 10.1213/ane.0b013e318193fd89. [DOI] [PubMed] [Google Scholar]
- 26.Spies CD, von Dossow V, Eggers V, et al. Altered cell-mediated immunity and increased postoperative infection rate in long-term alcoholic patients. Anesthesiology. 2004;100:1088–1100. doi: 10.1097/00000542-200405000-00010. [DOI] [PubMed] [Google Scholar]
- 27.Tonnesen H, Kehlet H. Preoperative alcoholism and postoperative morbidity. Br J Surg. 1999;86:869–874. doi: 10.1046/j.1365-2168.1999.01181.x. [DOI] [PubMed] [Google Scholar]
- 28.Harris AHS, Frey MS, Debenedetti AF, Bradley KA. Alcohol misuse prevalence and associations with postoperative complications in US surgical patients: a review. Open J Surg. 2008;2:50–58. [Google Scholar]
- 29.Bush K, Kivlahan DR, McDonnell MB, Fihn SD, Bradley KA. The AUDIT alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking. Ambulatory Care Quality Improvement Project (ACQUIP). Alcohol use disorders identification test. Arch Intern Med. 1998;158:1789–1795. doi: 10.1001/archinte.158.16.1789. [DOI] [PubMed] [Google Scholar]
- 30.Harris AHS, Reeder R, Ellerbe L, Bradley KA, Rubinsky AD, Giori NJ. Preoperative alcohol screening scores: association with complications in men undergoing total joint arthroplasty. J Bone Joint Surg Am. 2011;93:321–327. doi: 10.2106/JBJS.I.01560. [DOI] [PubMed] [Google Scholar]
- 31.Rubinsky AD, Bishop MJ, Maynard C, et al. Postoperative risks associated with alcohol screening depend on documented drinking at the time of surgery. Drug Alcohol Depend. 2013;132:521–527. doi: 10.1016/j.drugalcdep.2013.03.022. [DOI] [PubMed] [Google Scholar]
- 32.Tonnesen H, Rosenberg J, Nielsen HJ, et al. Effect of preoperative abstinence on poor postoperative outcome in alcohol misusers: randomised controlled trial. BMJ. 1999;318:1311–1316. doi: 10.1136/bmj.318.7194.1311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Oppedal K, Møller A, Pedersen B, Tønnesen H. Preoperative alcohol cessation prior to elective surgery. Cochrane Database Syst Rev. 2012;(7):CD008343. doi: 10.1002/14651858.CD008343.pub2. [DOI] [PubMed] [Google Scholar]
- 34.Vasilaki EI, Hosier SG, Cox WM. The efficacy of motivational interviewing as a brief intervention for excessive drinking: a meta-analytic review. Alcohol Alcohol. 2006;41:328–335. doi: 10.1093/alcalc/agl016. [DOI] [PubMed] [Google Scholar]
- 35.Monti PM, Colby SM, Barnett NP, et al. Brief intervention for harm reduction with alcohol-positive older adolescents in a hospital emergency department. J Consult Clin Psychol. 1999;67:989–994. doi: 10.1037//0022-006x.67.6.989. [DOI] [PubMed] [Google Scholar]
- 36.Monti PM, Barnett NP, Colby SM, et al. Motivational interviewing versus feedback only in emergency care for young adult problem drinking. Addiction. 2007;102:1234–1243. doi: 10.1111/j.1360-0443.2007.01878.x. [DOI] [PubMed] [Google Scholar]
- 37.Babor TF, McRee BG, Kassebaum PA, Grimaldi PL, Ahmed K, Bray J. Screening, Brief Intervention, and Referral to Treatment (SBIRT) toward a public health approach to the management of substance abuse. Subst Abus. 2008;28:7–30. doi: 10.1300/J465v28n03_03. [DOI] [PubMed] [Google Scholar]
- 38.Marlatt GA, George WH. Relapse prevention: introduction and overview of the model. Br J Addict. 1984;79:261–273. doi: 10.1111/j.1360-0443.1984.tb00274.x. [DOI] [PubMed] [Google Scholar]
- 39.Mello MJ, Baird J, Nirenberg TD, Lee C, Woolard R, Longabaugh R. DIAL: a randomised trial of a telephone brief intervention for alcohol. Inj Prev. 2012;51:755–764. doi: 10.1136/injuryprev-2012-040334. [DOI] [PubMed] [Google Scholar]
- 40.Neumann T, Neuner B, Weiss-Gerlach E, et al. The effect of computerized tailored brief advice on at-risk drinking in subcritically injured trauma patients. J Trauma. 2006;61:805–814. doi: 10.1097/01.ta.0000196399.29893.52. [DOI] [PubMed] [Google Scholar]
- 41.Saitz R. Alcohol screening and brief intervention in primary care: absence of evidence for efficacy in people with dependence or very heavy drinking. Drug Alcohol Rev. 2010;29:631–640. doi: 10.1111/j.1465-3362.2010.00217.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.McQueen J, Howe TE, Allan L, Mains D, Hardy V. Brief interventions for heavy alcohol users admitted to general hospital wards. Cochrane Database Syst Rev. 2011;(8):CD005191. doi: 10.1002/14651858.CD005191.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Tsai MC, Tsai YF, Hwang FM, Liu CY. Effectiveness of a brief intervention for managing hazardous drinking problems of inpatients in Taiwan. J Adv Nurs. 2011;67:2038–2046. doi: 10.1111/j.1365-2648.2011.05623.x. [DOI] [PubMed] [Google Scholar]
- 44.Saitz R, Palfai TP, Cheng DM, et al. Brief intervention for medical inpatients with unhealthy alcohol use: a randomized, controlled trial. Ann Intern Med. 2007;146:167–176. doi: 10.7326/0003-4819-146-3-200702060-00005. [DOI] [PubMed] [Google Scholar]
- 45.Broyles LM, Rosenberger E, Hanusa BH, Kraemer KL, Gordon AJ. Hospitalized patients’ acceptability of nurse-delivered screening, brief intervention, and referral to treatment. Alcohol Clin Exp Res. 2012;36:725–731. doi: 10.1111/j.1530-0277.2011.01651.x. [DOI] [PubMed] [Google Scholar]
- 46.Kaner EF, Dickinson HO, Beyer FR, et al. Effectiveness of brief alcohol interventions in primary care populations (review) Cochrane Database Syst Rev. 2009;(4):CD004148. doi: 10.1002/14651858.CD004148.pub3. [DOI] [PubMed] [Google Scholar]
- 47.Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Higgins JPT, Altman DG. Chapter 8: assessing risk of bias in included studies. In: Higgins JPT, Green S, editors. Cochrane handbook for systematic reviews of interventions. Version 5.1.0 [updated September 2008] The Cochrane Collaboration; 2008. Available at: http://www.cochrane-handbook.org. [Google Scholar]
- 49.Reeves BC, Deeks JJ, Higgins JPT, Wells GA. Chapter 13: including non-randomized studies. In: Higgins JPT, Green S, editors. Cochrane handbook for systematic reviews of interventions. Version 5.0.1 [updated September 2008] The Cochrane Corporation; 2008. Available at: http://www.cochrane-handbook.org. [Google Scholar]
- 50.Kummel M, Vahlberg T, Ojanlatva A, Kärki R, Mattila T, Kivelä S-L. Effects of an intervention on health behaviors of older coronary artery bypass (CAB) patients. Arch Gerontol Geriatr. 2008;46:227–244. doi: 10.1016/j.archger.2007.04.003. [DOI] [PubMed] [Google Scholar]
- 51.McHugh F, Lindsay GM, Hanlon P. Nurse led shared care for patients on the waiting list for coronary artery bypass surgery: a randomised controlled trial. Heart. 2001;86:317–323. doi: 10.1136/heart.86.3.317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Shourie S, Conigrave KM, Proude EM, Ward JE, Wutzke SE, Haber PS. The effectiveness of a tailored intervention for excessive alcohol consumption prior to elective surgery. Alcohol Alcohol. 2006;41:643–649. doi: 10.1093/alcalc/agl059. [DOI] [PubMed] [Google Scholar]
- 53.Hansen TB, Bredtoft HK, Larsen K. Preoperative physical optimization in fast-track hip and knee arthroplasty. Dan Med J. 2012;59:A4381. [PubMed] [Google Scholar]
- 54.Gomel M, Saunders JB, Burns L. Dissemination of early intervention for harmful alcohol consumption in general practice. Health Promot J Aust. 1994;4:65–69. [Google Scholar]
- 55.Proude EM, Conigrave KM, Haber PS. Effectiveness of skills-based training using the Drink-less package to increase family practitioner confidence in intervening for alcohol use disorders. BMC Med Educ. 2006;6:8. doi: 10.1186/1472-6920-6-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kip MJ, Neumann T, Jugel C, et al. New strategies to detect alcohol use disorders in the preoperative assessment clinic of a German university hospital. Anesthesiology. 2008;109:171–179. doi: 10.1097/ALN.0b013e31817f5be3. [DOI] [PubMed] [Google Scholar]
- 57.Nielsen PR, Jørgensen LD, Dahl B, Pedersen T, Tønnesen H. Prehabilitation and early rehabilitation after spinal surgery: randomized clinical trial. Clin Rehabil. 2010;24:137–148. doi: 10.1177/0269215509347432. [DOI] [PubMed] [Google Scholar]
- 58.Breslow RA, Smothers B. Drinking patterns of older Americans: national health interview surveys, 1997–2001. J Stud Alcohol. 2004;65:232–240. doi: 10.15288/jsa.2004.65.232. [DOI] [PubMed] [Google Scholar]
- 59.Kirchner JE, Zubritsky C, Cody M, et al. Alcohol consumption among older adults in primary care. J Gen Intern Med. 2007;22:92–97. doi: 10.1007/s11606-006-0017-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Brennan PL, Schutte KK, Moos BS, Moos RH. Twenty-year alcohol-consumption and drinking-problem trajectories of older men and women. J Stud Alcohol Drugs. 2011;72:308–321. doi: 10.15288/jsad.2011.72.308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.McEvoy LK, Kritz-Silverstein D, Barrett-Connor E, Bergstrom J, Laughlin GA. Changes in alcohol intake and their relationship with health status over a 24-year follow-up period in community-dwelling older adults. J Am Geriatr Soc. 2013;61:1303–1308. doi: 10.1111/jgs.12366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Woolard R, Cherpitel C, Kathleen T. Brief intervention for emergency department patients with alcohol misuse: implications for current practice. Alcohol Treat Q. 2011;29:146–57. doi: 10.1080/07347324.2011.557978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Neighbors CJ, Barnett NP, Rohsenow DJ, Colby SM, Monti PM. Cost-effectiveness of a motivational intervention for alcohol-involved youth in a hospital emergency department. J Stud Alcohol Drugs. 2010;71:384–394. doi: 10.15288/jsad.2010.71.384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Mundt MP, French MT, Roebuck MC, Manwell LB, Barry KL. Brief physician advice for problem drinking among older adults: an economic analysis of costs and benefits. J Stud Alcohol. 2005;66:389–394. doi: 10.15288/jsa.2005.66.389. [DOI] [PubMed] [Google Scholar]
- 65.Tonnesen H, Nielsen PR, Lauritzen JB, Moller AM. Smoking and alcohol intervention before surgery: evidence for best practice. Br J Anaesth. 2009;102:297–306. doi: 10.1093/bja/aen401. [DOI] [PubMed] [Google Scholar]
- 66.Tonnesen H, Kaiser AH, Nielsen BB, Pedersen AE. Reversibility of alcohol-induced immune depression. Br J Addict. 1992;87:1025–1028. doi: 10.1111/j.1360-0443.1992.tb03119.x. [DOI] [PubMed] [Google Scholar]
- 67.Tonnesen H. Alcohol abuse and postoperative morbidity. Dan Med Bull. 2003;50:139–160. [PubMed] [Google Scholar]
- 68.Dimick JB, Chen SL, Taheri PA, Henderson WG, Khuri SF, Campbell DA. Hospital costs associated with surgical complications: a report from the private-sector National Surgical Quality Improvement Program. J Am Coll Surg. 2004;199:531–537. doi: 10.1016/j.jamcollsurg.2004.05.276. [DOI] [PubMed] [Google Scholar]
- 69.Curran GM, Bauer M, Mittman B, Pyne JM, Stetler C. Effectiveness-implementation hybrid designs: combining elements of clinical effectiveness and implementation research to enhance public health impact. Med Care. 2012;50:217–226. doi: 10.1097/MLR.0b013e3182408812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.West SG, Duan N, Pequegnat W, et al. Alternatives to the randomized controlled trial. Am J Public Health. 2008;98:1359–1366. doi: 10.2105/AJPH.2007.124446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Hooper R, Bourke L. The dog-leg design that can give clinical trials more power to their elbow. Trials. 2013;14(Suppl. 1):P16. [Google Scholar]
- 72.Saitz R. Brief intervention for medical inpatients with unhealthy alcohol use. Ann Intern Med. 2007;146:167–176. doi: 10.7326/0003-4819-146-3-200702060-00005. [DOI] [PubMed] [Google Scholar]
- 73.Longabaugh R, Woolard RE, Nirenberg TD, et al. Evaluating the effects of a brief motivational intervention for injured drinkers in the emergency department. J Stud Alcohol. 2001;62:806–816. doi: 10.15288/jsa.2001.62.806. [DOI] [PubMed] [Google Scholar]
- 74.Bischof G, Freyer-Adam J, Meyer C, John U, Rumpf H-J. Changes in drinking behavior among control group participants in early intervention studies targeting unhealthy alcohol use recruited in general hospitals and general practices. Drug Alcohol Depend. 2012;125:81–88. doi: 10.1016/j.drugalcdep.2012.03.018. [DOI] [PubMed] [Google Scholar]
- 75.McBride CM, Emmons KM, Lipkus IM. Understanding the potential of teachable moments: the case of smoking cessation. Health Educ Res. 2003;18:156–170. doi: 10.1093/her/18.2.156. [DOI] [PubMed] [Google Scholar]
- 76.Lau K, Freyer-Adam J, Gaertner B, Rumpf H-J, John U, Hapke U. Motivation to change risky drinking and motivation to seek help for alcohol risk drinking among general hospital inpatients with problem drinking and alcohol-related diseases. Gen Hosp Psychiatry. 2010;32:86–93. doi: 10.1016/j.genhosppsych.2009.10.002. [DOI] [PubMed] [Google Scholar]