Abstract
Background:
Evidence has shown a link between allergic disease and inflammatory bowel diseases (IBDs). We investigated food allergy in Iranian pediatric IBD patients.
Materials and Methods:
A cross-sectional study was conducted on a consecutive sample of children with newly diagnosed IBD referring to Mofid Children's University Hospital in Tehran (Iran) between November 2013 and March 2015. Data on age, gender, history of cow's milk allergy (CMA), IBD type, routine laboratory tests, and colonoscopic and histopathological findings were gathered. Food allergy was assessed with the skin prick test (SPT).
Results:
A total of 28 patients including 19 ulcerative colitis (UC), 7 Cronh's disease (CD), and two with unclassified colitis with a mean age of 8.3 ± 4.4 years. (57.1% females, 42.9% were studied. History of CMA was present in eight patients (28.6%). Seventeen patients (60.7%) had at least one food allergy (68.4% of UC vs. 42.9% of CD, P = 0.230). Ten patients (35.7%) had multiple food allergies (36.8% of UC vs. 42.9% of CD, P > 0.999). Common allergic foods were cow's milk (28.6%), beef, seafood, albumen, wheat, and walnuts (each 10.7%), and peanuts and chestnuts (each 7.1%). The SPT showed CMA in 68.4% (8/17) of UC but none of the CD patients (P = 0.077).
Conclusion:
Food allergy is frequent in Iranian pediatric IBD patients with CMA being the most common observed allergy. The CMA seems to be more frequent in UC than in CD patients.
Keywords: Crohn's disease, food hypersensitivity, inflammatory bowel diseases, pediatrics, ulcerative colitis
INTRODUCTION
Crohn's disease (CD) and ulcerative colitis (UC) are chronic, relapsing, and inflammatory diseases of the gastrointestinal tract which affects both adults and children of different ages.[1] The incidence of pediatric inflammatory bowel diseases (IBDs) ranges variously from 0.2 to 13.3 cases per 100,000 populations per year in the different geographic area, but it is reported to be rising worldwide.[2] The pathogenesis of IBDs is complex, and of course not completely understood. It is suggested to be due to inappropriate immune reactions in response to the antigens presented into the gut in a genetically susceptible individual.[1] However, known genetic variations cannot completely explain geographic differences in the incidence of IBD, suggesting a role for gene-environmental interactions in the pathophysiology of the disease[3] as well as in the observed increasing incidence.[4]
Environmental factors implicated in the development of pediatric IBD include diet, early life infections and antibiotic use, exposure to air pollutions, and the hygiene hypothesis.[5] However, due to lack of studies, such factors are not yet confirmed to play a role in the increased incidence of pediatric IBD. The rising trend in the incidence of pediatric IBD has been paralleled by an increase in allergic diseases over the past decades.[6,7,8] Accordingly, an association between IBD and allergic diseases can be hypothesized.
A number of studies have shown a link between IBD and atopic diseases such as eczema, allergic rhinitis, and asthma.[9] Data are also available on the possible role of food allergy in the development of IBD.[9] Dietary intake may affect the gastrointestinal immune response through presenting various food antigens, altering the immunological balance, and changing the gut microbiota.[5] Indeed, gastrointestinal symptoms are among the most common clinical manifestations of food allergy.[10,11] Available data have shown a link between a history of cow's milk allergy (CMA) in infancy and increased risk of both CD and UC in childhood.[12,13] However, very few studies are conducted in this regard particularly in our population, that is, Iran. Accordingly, we aimed to evaluate the frequency of food allergy in a sample of Iranian children with IBD.
MATERIALS AND METHODS
Patients and settings
This cross-sectional study was conducted on a consecutive sample of children with newly diagnosed IBD referring to the pediatric gastroenterology clinic of the Mofid Children's Hospital (Tehran, Iran) between November 2013 and March 2015. Inclusion criteria were the age between 2 and 18 years and diagnosis of IBD based on clinical presentation, laboratory tests, upper and lower gastrointestinal endoscopy, and histopathological examinations.[14] Those with dermatographic urticaria and those who had consumed antihistamines in the preceding week or were already on corticosteroid or immunosuppressive therapy were not included. Sample size was calculated as 25 cases, considering type I error probability of 0.05, study power of 0.8, and expecting frequency of food allergy in at least 17.7% of the IBD children according to previous data.[15] The study was approved by the Ethics Committee of the Shahid Beheshti University of Medical Sciences, and informed consent was obtained from the parents.
Measurements
Parents were interviewed, children were examined, and patients’ documents were reviewed by a pediatric gastroenterology fellow. The following data were gathered: Age, gender, history of CMA, history of skin atopic diseases, IBD type, duration of symptoms before diagnosis, laboratory data (at the time of diagnosis), colonoscopic and histopathological findings, and extraintestinal involvement related to IBD. History of CMA was considered positive, if the child had experienced gastrointestinal bleeding after consuming a diary product and improved by eliminating it from the diet.
Skin prick test
Positive and negative control tests were performed with histamine hydrochloride (1 mg/ml) and normal saline on the forearm. Those with the positive response to normal saline or negative response to histamine were excluded from the study. Using a commercial available kit (GreerPick™, Lenoir, NC, USA), the skin prick test (SPT) was performed for the evaluation of allergy to the following foods: Yolk, albumen, cow's milk, wheat, barley, soya, rice, chicken, beef, seafood, walnuts, chestnut, peanuts, tomatoes, potato, bananas, melons, orange, strawberries, kiwi, apple, celery, onion, vanilla, mushroom, sesame, cacao, ginger, black pepper, green pepper, carrots, olive, and blackberry. This list of foods was selected based on the necessity and conventionality of the food in the Iranian children's diet and according to other reports on food allergy in children.[16] The skin test was performed on the forearm, with a drop of the allergen was placed at each test site, and then test sites were scratched with a lancet. Skin reaction was assessed after 20 min, and the size of flare and wheal was measured. A wheal of 3 mm above and a flare of 5 mm greater than the negative control site were considered as positive test results.
Statistical analysis
Data were analyzed using the SPSS software for windows version 16.0 (SPSS Inc., Chicago, IL, USA). Data are presented as mean ± standard deviation (SD) and (range), median (interquartile range of 25-75%), or number (%). Comparisons of quantitative and qualitative data were checked with the Chi-square or Fisher's exact tests. A P < 0.05 was considered statistically significant.
RESULTS
Patients characteristics
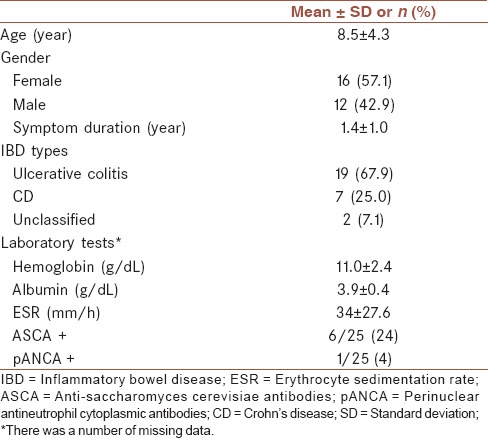
A total of 32 children with IBD were evaluated during the study period from which 28 were eligible and entered into the study including 16 females and 12 males with mean age of 8.5 ± 4.3 years old and symptoms’ duration of 1.4 ± 1 year. Patients and disease characteristics are summarized in Table 1.
Table 1.
Patients and disease characteristics (n = 28)
History of CMA and skin atopic diseases were positive in 8 (28.6%) and 5 (17.9%) of the patients, respectively. Seventeen patients (60.7%) had an allergy to at least one food, and 10 patients (35.7%) had multiple food allergies. The frequency of food allergies is presented in Figure 1. In order, patients had allergy to cow's milk (28.6%), beef, seafood, albumen, wheat, and walnuts (each 10.7%), peanuts and chestnuts (each 7.1%), and strawberries, potatoes, sesame, bananas, barley, apple, olive, soya, tomatoes, kiwi, cacao, and orange (each 3.6%).
Figure 1.
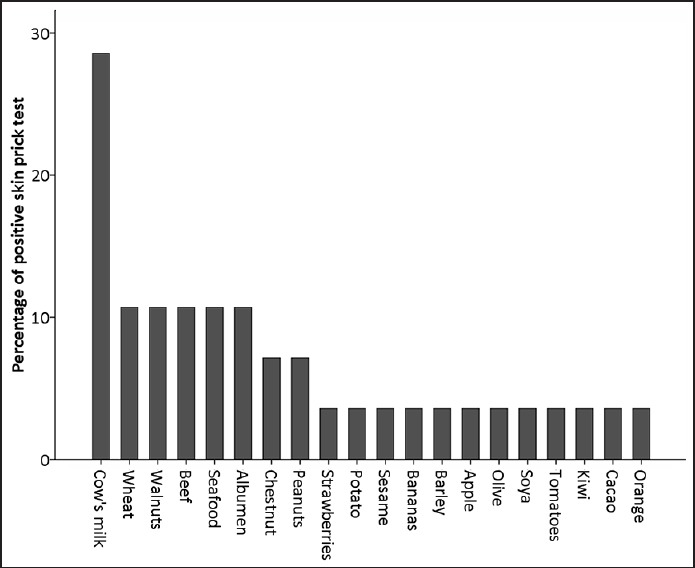
Frequency of positive skin prick test to each of the foods
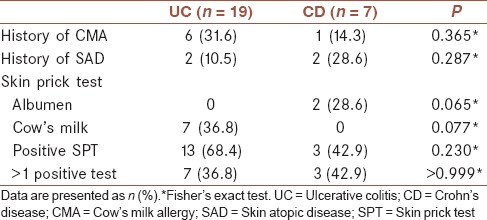
Comparison of UC and CD patients regarding the history of allergy and skin test results are presented in Table 2. Frequency of having at least one food allergy on the skin test was slightly, but not significantly, higher in UC than CD patients (68.4% vs. 42.9%, P = 0.230). Among the UC patients, 36.8% had multiple food allergies compared to 42.9% of those with CD (P > 0.999). Among those who had at least one food allergy, 53.8% (7/13) of UC and 100% (3/3) of CD patients had multiple food allergies (P = 0.250). With regards to specific food tests results, allergy to albumin was present only in CD patients (28.6) while allergy to cow's milk was present only in UC patients (36.8%), Table 2.
Table 2.
Comparison of ulcerative colitis and CD patients regarding food allergy test results
DISCUSSION
The aim of this study was to evaluate the frequency of food allergy in a sample of Iranian pediatric IBD patients. The frequency of allergy to at least one food in our study (60%) was comparable to that is reported in Iranian children with allergic complaints (53%),[17] atopic dermatitis (51%),[18] and asthma (47%)[19] and higher than that is reported from general population (12%).[20] In addition, we found multiple food allergies in at least one-third of the pediatric IBD patients which is quite higher than that is observed in the general population (2.4%),[21] and even compared with children with atopic diseases (12%).[22] Similar to children with atopic diseases, CMA allergy was the most common type of food allergy in Iranian pediatric IBD. We had no control group for direct comparison of data. The only available data on the frequency of food allergy in children of the general population in our society has reported a total food allergy of 12%.[20] Studies in Western populations revealed that about 8% of the children in the general population have at least one food allergy with the CMA being the most common type of food allergy.[16] Accordingly, our study result can indicate a higher frequency of food allergy in Iranian pediatric IBD patients compared with the general population.
A limited number of studies are conducted up to now on the association of food allergies and IBD in the pediatric population. The first report is from Glassman et al. who retrospectively investigated symptoms compatible with CMA during infancy in a sample of 78 children with IBD and 36 healthy children. Authors found CMA symptoms in 20.9% of UC and 8.5% of CD cases, compared with 2.8% in controls.[13] In a larger study, Virta et al. studied 595 Finnish children with IBD and 2380 matched controls with regards to the presence of CMA. These investigators found the history of CMA in 8.2% of CD, 6.4% of UC, and 4% of the controls.[12] Compared with these studies, we found a considerably higher frequency of positive history for CMA in those with UC than in CD patients (31.6% vs. 14.3%); though positive history of CMA in CD patients was still higher than that reported in the general population by previous studies (2.8-4%).[12,13] In contrast to previous studies which retrospectively evaluated CMA by history taking or from a disease registry, we tested CMA also by a SPT and found a high frequency of CMA in UC patients (about 37%), but none of the CD cases. Frequency of having an allergy to at least one of the evaluated foods was relatively higher in UC than CD patients in our study, but the frequency of multiple food allergies were almost the same between UC and CD patients. However, all of the CD cases who had positive SPT had indeed multiple food allergies; compared to half of the UC patients with positive SPT. Despite these results, a clear conclusion cannot be made whether food allergy is associated with increased risk of a specific type of IBD due to the small sample size of our study, and further studies are required in this regard.
The mechanisms underlying the observed association between IBD and food allergy are not yet identified. Abdominal pain, nausea/vomiting, and diarrhea are common symptoms of gastrointestinal food allergy resulting from immune responses to dietary antigens.[23] In addition, endoscopic appearance can mimic those characteristics that are seen in IBD patients.[24,25] Accordingly, it is possible that a number of patients with food allergy are misdiagnosed as IBD cases.[23] Indeed, diagnosis of gastrointestinal food allergy is a challenge for clinicians.[23] A comprehensive history including the family history of atopic disease, laboratory tests, and histopathological findings from gastrointestinal biopsies can be helpful in the proper diagnosis of food allergy.[23,24] Besides misdiagnosis, the association between food allergy and IBD may be as a result of shared genetic (e.g., risk variant alleles) as well as environmental (e.g., Vitamin D deficiency, hygiene hypothesis, and gut microbiota) risk factors.[9] Moreover, the two entities may become associated comorbidities through their pathophysiology. Patients with IBD have mucosal barrier dysfunction through which food antigens can cross and evoke further allergic reactions.[26] Gastrointestinal inflammation and subsequent treatments in IBD patients can alter the gut microbiota leading to loss of immunologic tolerance to the food antigens and development of hypersensitivity.[27] The same processes may be present in those with food allergy increasing the risk of IBD in genetic susceptible individuals. Further studies are required to better investigate possible mechanisms behind the association of food allergy and IBD in children.
Our study has a number of limitations. The sample size was small, and there was no control group for comparison of data. In addition, we evaluated food allergy by SPT, which, compared with other methods (e.g., immunoglobulin E specific antigens), may not be an optimal measure.[28] Although reliable diagnosis of allergy to one food allergen is according to history taking and duration between ingestion of food and occurrence of signs and symptoms and challenge test, the IBD patient was symptomatic and some IBD clinical manifestation are the same as food allergy. In addition, legal parameters challenge test was not choose as the diagnosis tool in our study. Hence, SPT prefer as the possible and suitable modality for evaluation of allergy to food allergens.[29]
In summary, we found that food allergy is frequent in Iranian pediatric IBD patients with CMA being the most common observed allergy. According to our results, CMA seems to be more frequently present in UC than in CD patients, while CD patients with food allergy were more probably allergic to multiple foods compared with UC patients. However, a clear conclusion cannot be drawn due to the study limitations. Further studies with a larger sample of patients and including control cases are warranted in this regard. Also, studies on the possible role of food allergy on the clinical course of pediatric IBD are warranted.
Financial support and sponsorship
Pediatric Infections Research Center, Shahid Beheshti University of Medical Sciences (grant # 5350).
Conflicts of interest
There are no conflicts of interest.
AUTHOR'S CONTRIBUTIONS
FI contributed in the conception and design of the work, conducting the study, revising the draft, approval of the final version of the manuscript, and agreed for all aspects of the work. PN contributed in the conception and design of the work, conducting the study, drafting and revising the draft, approval of the final version of the manuscript, and agreed for all aspects of the work. SS contributed in the conception of the work, conducting the study, revising the draft, approval of the final version of the manuscript, and agreed for all aspects of the work. AS contributed in the conception of the work, revising the draft, approval of the final version of the manuscript, and agreed for all aspects of the work. ND contributed in the conception of the work, conducting the study, revising the draft, approval of the final version of the manuscript, and agreed for all aspects of the work. KA contributed in the conception of the work, revising the draft, approval of the final version of the manuscript, and agreed for all aspects of the work. YN contributed in the conception of the work, revising the draft, approval of the final version of the manuscript, and agreed for all aspects of the work. MM contributed in the design of the work, revising the draft, approval of the final version of the manuscript, and agreed for all aspects of the work. KKH contributed in the conception and design of the work, drafting and revising the draft, approval of the final version of the manuscript, and agreed for all aspects of the work. PR contributed in the conception and design of the work, drafting and revising the draft, approval of the final version of the manuscript, and agreed for all aspects of the work. BO contributed in the conception and design of the work, drafting and revising the draft, approval of the final version of the manuscript, and agreed for all aspects of the work.
REFERENCES
- 1.Hanauer SB. Inflammatory bowel disease: Epidemiology, pathogenesis, and therapeutic opportunities. Inflamm Bowel Dis. 2006;12:S3–9. doi: 10.1097/01.mib.0000195385.19268.68. [DOI] [PubMed] [Google Scholar]
- 2.Benchimol EI, Fortinsky KJ, Gozdyra P, Van den Heuvel M, Van Limbergen J, Griffiths AM. Epidemiology of pediatric inflammatory bowel disease: A systematic review of international trends. Inflamm Bowel Dis. 2011;17:423–39. doi: 10.1002/ibd.21349. [DOI] [PubMed] [Google Scholar]
- 3.Ananthakrishnan AN. Environmental risk factors for inflammatory bowel diseases: A review. Dig Dis Sci. 2015;60:290–8. doi: 10.1007/s10620-014-3350-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Henderson P, Wilson DC. The rising incidence of paediatric-onset inflammatory bowel disease. Arch Dis Child. 2012;97:585–6. doi: 10.1136/archdischild-2012-302018. [DOI] [PubMed] [Google Scholar]
- 5.Aujnarain A, Mack DR, Benchimol EI. The role of the environment in the development of pediatric inflammatory bowel disease. Curr Gastroenterol Rep. 2013;15:326. doi: 10.1007/s11894-013-0326-4. [DOI] [PubMed] [Google Scholar]
- 6.Branum AM, Lukacs SL. Food allergy among U.S. children: Trends in prevalence and hospitalizations. NCHS Data Brief. 2008;10:1–8. [PubMed] [Google Scholar]
- 7.Gupta R, Sheikh A, Strachan DP, Anderson HR. Time trends in allergic disorders in the UK. Thorax. 2007;62:91–6. doi: 10.1136/thx.2004.038844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jackson KD, Howie LD, Akinbami LJ. Hyattsville, MD: National Center for Health Statistics; 2013. Trends in allergic conditions among children: United States, 1997-2011. NCHS data brief, no. 121. [PubMed] [Google Scholar]
- 9.Walker MM, Powell N, Talley NJ. Atopy and the gastrointestinal tract – A review of a common association in unexplained gastrointestinal disease. Expert Rev Gastroenterol Hepatol. 2014;8:289–99. doi: 10.1586/17474124.2014.881716. [DOI] [PubMed] [Google Scholar]
- 10.Perry TT, Pesek RD. Clinical manifestations of food allergy. Pediatr Ann. 2013;42:96–101. doi: 10.3928/00904481-20130522-09. [DOI] [PubMed] [Google Scholar]
- 11.Mansoor DK, Sharma HP. Clinical presentations of food allergy. Pediatr Clin North Am. 2011;58:315–26. doi: 10.1016/j.pcl.2011.02.008. [DOI] [PubMed] [Google Scholar]
- 12.Virta LJ, Ashorn M, Kolho KL. Cow's milk allergy, asthma, and pediatric IBD. J Pediatr Gastroenterol Nutr. 2013;56:649–51. doi: 10.1097/MPG.0b013e318285e9d8. [DOI] [PubMed] [Google Scholar]
- 13.Glassman MS, Newman LJ, Berezin S, Gryboski JD. Cow's milk protein sensitivity during infancy in patients with inflammatory bowel disease. Am J Gastroenterol. 1990;85:838–40. [PubMed] [Google Scholar]
- 14.Ibd Working Group of the European Society for Paediatric Gastroenterology H, Nutrition. Inflammatory bowel disease in children and adolescents: Recommendations for diagnosis-the Porto criteria. J Pediatr Gastroenterol Nutr. 2005;41:1–7. doi: 10.1097/01.mpg.0000163736.30261.82. [DOI] [PubMed] [Google Scholar]
- 15.Dainese R, Galliani EA, De Lazzari F, D’Incà R, Mariné-Barjoan E, Vivinus-Nebot MH, et al. Role of serological markers of activated eosinophils in inflammatory bowel diseases. Eur J Gastroenterol Hepatol. 2012;24:393–7. doi: 10.1097/MEG.0b013e328350f91f. [DOI] [PubMed] [Google Scholar]
- 16.Sicherer SH, Sampson HA. Food allergy: Epidemiology, pathogenesis, diagnosis, and treatment. J Allergy Clin Immunol. 2014;133:291–307. doi: 10.1016/j.jaci.2013.11.020. [DOI] [PubMed] [Google Scholar]
- 17.Pourpak Z, Farhoudi A, Arshi S, Movahedi M, Gharegozlou M, Yazdani F, et al. Common food allergens in children (a report from a referral center in tehran university of medical sciences) Acta Med Iran. 2003;41:40. [Google Scholar]
- 18.Moghtaderi M, Farjadian S, Kashef S, Alyasin S, Afrasiabi M, Orooj M. Specific IgE to common food allergens in children with atopic dermatitis. Iran J Immunol. 2012;9:32–8. [PubMed] [Google Scholar]
- 19.Farjadian S, Moghtaderi M, Kashef S, Alyasin S. Sensitization to food allergens in Iranian children with mild to moderate persistent asthma. World J Pediatr. 2012;8:317–20. doi: 10.1007/s12519-012-0375-z. [DOI] [PubMed] [Google Scholar]
- 20.Farrokhi S, Gheybi MK, Dehdari R, Keshvari S, Gholampour H, Mansourian Z. Prevalence of seafood allergy in student living in bushehr and borazjan. ISMJ. 2014;17:407. [PubMed] [Google Scholar]
- 21.Gupta RS, Springston EE, Warrier MR, Smith B, Kumar R, Pongracic J, et al. The prevalence, severity, and distribution of childhood food allergy in the United States. Pediatrics. 2011;128:e9–17. doi: 10.1542/peds.2011-0204. [DOI] [PubMed] [Google Scholar]
- 22.Friedlander JL, Sheehan WJ, Baxi SN, Kopel LS, Gaffin JM, Ozonoff A, et al. Food allergy and increased asthma morbidity in a School-based Inner-City Asthma Study. J Allergy Clin Immunol Pract. 2013;1:479–84. doi: 10.1016/j.jaip.2013.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sicherer SH. Clinical aspects of gastrointestinal food allergy in childhood. Pediatrics. 2003;111:1609–16. [PubMed] [Google Scholar]
- 24.Hill SM, Milla PJ. Colitis caused by food allergy in infants. Arch Dis Child. 1990;65:132–3. doi: 10.1136/adc.65.1.132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Poddar U, Yachha SK, Krishnani N, Srivastava A. Cow's milk protein allergy: An entity for recognition in developing countries. J Gastroenterol Hepatol. 2010;25:178–82. doi: 10.1111/j.1440-1746.2009.06017.x. [DOI] [PubMed] [Google Scholar]
- 26.Scharl M, Rogler G. Inflammatory bowel disease pathogenesis: What is new? Curr Opin Gastroenterol. 2012;28:301–9. doi: 10.1097/MOG.0b013e328353e61e. [DOI] [PubMed] [Google Scholar]
- 27.Dupaul-Chicoine J, Dagenais M, Saleh M. Crosstalk between the intestinal microbiota and the innate immune system in intestinal homeostasis and inflammatory bowel disease. Inflamm Bowel Dis. 2013;19:2227–37. doi: 10.1097/MIB.0b013e31828dcac7. [DOI] [PubMed] [Google Scholar]
- 28.Turnbull JL, Adams HN, Gorard DA. Review article: The diagnosis and management of food allergy and food intolerances. Aliment Pharmacol Ther. 2015;41:3–25. doi: 10.1111/apt.12984. [DOI] [PubMed] [Google Scholar]
- 29.Boyce JA, Assa’ad A, Burks AW, Jones SM, Sampson HA, et al. NIAID-Sponsored Expert Panel. Guidelines for the diagnosis and management of food allergy in the United States: Report of the NIAID-sponsored expert panel. J Allergy Clin Immunol. 2010;126:S1–58. doi: 10.1016/j.jaci.2010.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]


