Objective:
The aim of this study is to examine the associations between lag times following occupational low back injury and the length of work disability.
Methods:
In a retrospective cohort study using workers’ compensation claims, random effects Tobit models were used to explore how disability length relates to three lag times: the number of days from the date of injury to reporting the injury, the number of days from the date of injury to medical care, and the number of days from the date of injury to initiating work disability.
Results:
In general, shorter lag times for each of the different lags were related to shorter lengths of disability.
Conclusions:
Decreasing the length of the lag times in reporting injuries, receiving medical care, and missing work may help to decrease the length of work disability for workers after low back injury.
Work disability resulting from occupational low back pain (LBP) continues to be a concern for the global workforce.1–4 It has been estimated that 37% of LBP worldwide is attributable to work, and work-related LBP is estimated to cause 818,000 disability-adjusted life years lost annually.1 The total indirect and direct cost of LBP in the U.S. has been estimated to be between $84.1 and $624.8 billion per year.4 As early as 1989, OSHA identified back injuries as the nation's number one workplace safety problem.2 According to the Bureau of Labor Statistics, in 2013, back injuries accounted for 24% of all nonfatal occupational injuries and illnesses involving days absent from work.3 Research suggests that the earlier an individual returns to work (RTW) after an injury, the shorter the duration of work disability and the better the long-term outcomes.5–9
Several studies have examined the associations between work disability as a result of work-related injury and a multitude of factors, such as psychosocial job factors, coordinated workplace-linked care systems, human interactions, organizational structures, patient and clinician expectations, and others.8,10–14 A potential factor in the work disability process following a work-related injury that has not been extensively examined is the role of lag times. There are several potential lag times in the work disability process, which may include the time from work injury to reporting the injury to an employer or to receiving medical treatment for an injury. These lag times may reflect various influences on the work disability process such as hesitance on the part of the employee to report an injury, administrative delays in the health care system, the natural course of gradually worsening symptoms following musculoskeletal injuries, or possibly the desire to try to “tough it out” after injury by delaying reporting and seeking treatment for an injury.
Few studies have examined the various lag times in the work disability process, such as the time from work injury to reporting an injury to an employer, receiving medical treatment for an injury, and taking time off of work or initiating light duty work. In studies that did address these lag times, the lag time was often one of many factors studied.15–18 For example, Shaw et al,19 in a multivariate analysis of early disability risk factors for LBP, found that earlier injury reporting to the employer, along with other factors, predicted earlier RTW.
In a limited number of studies, the lag time between when an injury occurs and when an individual seeks medical treatment has been explored. In one study, Infante-Rivard and Lortie15 investigated the factors related to returning to work following an episode of compensated back pain. Among the factors found to relate to returning to work, the likelihood of returning to work was lower for workers who sought treatment 30 days or more after an incident had occurred than those who sought treatment within 30 days.15 Similarly, another study of union carpenters experiencing back injuries found that workers with a delay of 30 days or longer in receiving medical care after back injury were more likely to take 90 days or longer to RTW than those receiving medical care within 30 days of injury.17 In contrast, when examining the association between lag times in medical care after work-related injury and RTW outcomes, Kominski et al18 did not find differences in RTW outcomes for workers receiving medical care on the day of the injury compared with those receiving medical care 1 to 3 days after injury or those receiving medical care 4 or more days after injury.
Prior studies have also examined lag times in referrals by a treating physician to medical specialists, therapists, and disability managers. In a cohort of Canadian workers who were compensated for LBP, workers who received physical therapy services within 30 days of LBP after having been referred by their physician were less likely to be absent from work for more than 60 days compared with those who never got referred to physical therapy or who were not referred to physical therapy within 30 days.20 Another study found that injured workers were less likely to be working if they had difficulty receiving care from physical/occupational therapists or other specialists when it was recommended in comparison to those injured workers in whom a physical/occupational therapist or other specialist was not needed.18 Research also suggests that among workers compensated for LBP, an increased lag time from injury to receiving physical therapy is related to a greater amount of time receiving workers’ compensation benefits.16 Finally, Pransky et al21 found that delayed referral to a nurse case manager was associated with prolonged length of disability in occupational LBP. To our knowledge, no studies have examined the lag time from work injury to taking time off of work or initiating light duty work.
The purpose of this study was to explore the associations between three lag times following occupational low back injury and the length of work disability. The three lag times we examined include (1) the lag time between when an injury occurred and when the injury was first reported to the workers’ compensation insurer; (2) the lag time between when an injury occurred and when a worker first received medical treatment for that injury; and (3) the lag time between when an injury occurred and when a worker first took time off of work or initiated light duty work as a result of that injury. A conceptual diagram of the lag times and the length of disability is presented in Figure 1. These lag times are among the first measurable factors in the work disability process. Examining these lag times and determining their associations with the length of work disability are an essential part of understanding occupational LBP and the work disability process.
FIGURE 1.
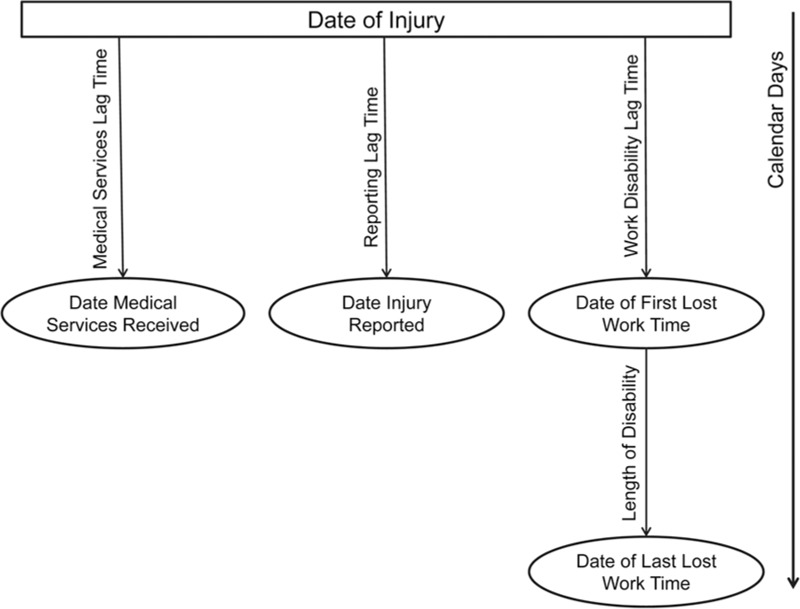
Conceptual model of how the respective lag times are measured and their relationship with the length of disability.
METHODS
The current study utilizes data from the administrative records of a large workers’ compensation insurance company in the United States that included claims from a variety of different states, industries, organizations, and company sizes. All workers’ compensation claims with complete data for individuals who had an injury date between January 1, 2002, and December 31, 2008, were assessed for inclusion. We included all claims with at least 1 day of paid lost work time within 1 year of the injury date. Lost work time comprised both days of temporary total disability (TTD) and days of temporary partial disability (TPD).
Two sets of criteria were used to identify LBP claims on the basis of the ICD-9 diagnosis codes that were reported in the claimant's medical service bills for the first 15 days of medical treatment. Medical treatment typically began within 2 weeks of the injury date (90% of claims), although all claimants who received medical treatment within 1 year of the injury date and who had lost work time were included in the database. First, 99,127 claims were classified as a possible LBP claim based on having at least one ICD-9 diagnosis code within the first 15 days of medical treatment relating to specific low back injuries or disorders, which are listed in supplemental Table 1. Second, from those identified as possible LBP claims, we required that over two-thirds of the claimant's ICD-9 diagnosis codes in the diseases of the nervous system and sense organs (320–389), diseases of the musculoskeletal system and connective tissue (710–739), and injury and poisoning (800–777) chapters within the first 15 days of medical treatment be for specific low back injuries or disorders (supplemental Table 1 or nonspecific back injuries or disorders (supplemental Table 2). In total, 76,955 claims met these criteria and approximately 70% of these claims had 100% of their ICD-9 diagnosis codes within the first 15 days coming from the codes listed in supplemental Tables 1 or 2.
Our sample was further restricted to claimants who had only one claim within a single calendar year. For some claimants with multiple claims in a single year, the claims were for different injuries. However, in certain cases, there were multiple episodes of disability for a single claim for individuals resulting from the same injury. This occurred in cases wherein an individual went back to work after an injury but after having returned to work went back out on TTD or TPD. In this study, we only included claims for individuals in whom multiple episodes of disability within the same claim had less than 14 days between episodes, in which case we considered this a single episode. If the duration between episodes was 14 days or longer, these claims were excluded. We also excluded claims for individuals who received a lump sum payment within 1 year of the injury date. Claims were excluded in cases wherein the first date of lost work time was more than 1 year after the injury date. Finally, only claims for individuals 18 to 80 years of age were included in this study. In total, 64,004 claims were used in our analyses. A flow chart of the inclusion specifications is presented in Figure 2.
FIGURE 2.
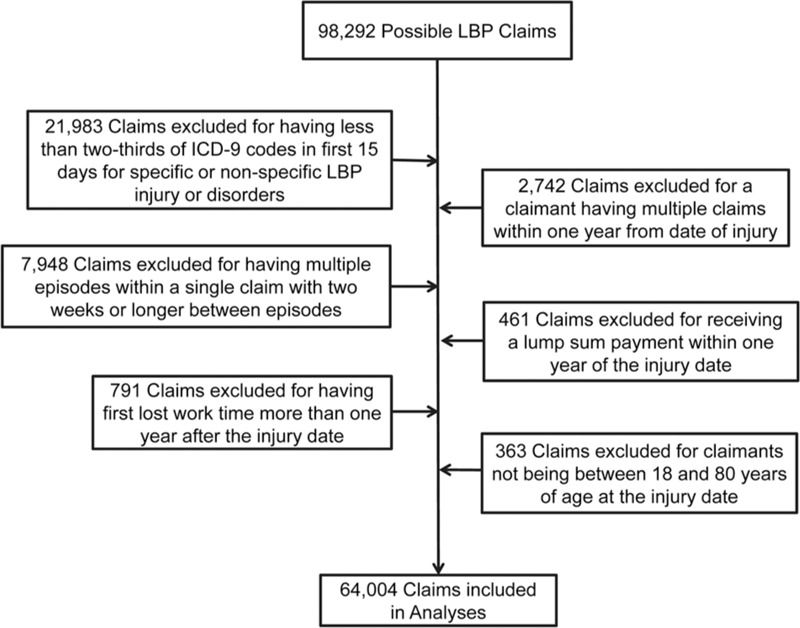
Flow chart of data restrictions for the analytic sample.
MEASURES
Predictor Variables
This study focuses on three lag times in the workers’ compensation process. The first lag time is referred to as the “reporting lag time” and represents the number of days from the date of injury to the date at which the injury was first reported to the workers’ compensation insurer. The second lag time, which we refer to as the “medical services lag time,” is the number of days from the date of injury to the date at which a claimant first sought medical care for that injury. The third lag time is referred to as the “work disability lag time” and represents the number of days from the date of injury to the date at which a claimant first took TPD or TTD. Each of the three lag times were categorized into seven categories: 0 days lag (reference group), 1 to 3 days lag, 4 to 6 days lag, 1 week up to 2 weeks lag, 2 weeks up to 30 days lag, 30 days up to 60 days lag, and 60 days up to 1 year lag.
Outcome Variable
The outcome variable was the length of disability, which was calculated from the date that a claimant first took TPD or TTD until the date at which TPD or TTD ended. TPD or TTD was considered to have ended when no disability days were taken for at least 14 days consecutively. For claims in which the length of disability exceeded 1 year, the value was top coded at 365. This occurred in 6887 claims. To address issues with normality, the natural log of the length of disability was used in the analyses.
Covariates
The following covariates were used: gender, annual income, industry, litigation status, injury severity, year of injury, age, and tenure. Gender was coded 1 for female and 0 for male. Sixteen ordered categories were used to assess annual income: $0 to $9999, $10000 to $19,999, $20,000 to $29,999, $30,000 to $39,999, $40,000 to $49,999, $50,000 to $59,999, $60,000 to $69,999, $70,000 to $79,999, $80,000 to $89,999, $90,000 to $99,999, $100,000 to $109,999, $110,000 to $119,999, $120,000 to $129,999, $130,000 to $139,999, $140,000 to $149,999, and $150,000 or more. Industry was categorized into 10 groups, including agriculture, forestry and fishing, construction, finance and insurance, manufacturing, mining, retail trade, services, transportation, public administration, and wholesale trade. These industry groupings match the U.S. Department of Labor's Standard Industry Classification (SIC) groups.22 Litigation status was coded 1 if the workers’ compensation insurer assigned an attorney to the claim and 0 if not. Injury severity was coded on the basis of the primary ICD-9 diagnosis. We used a similar procedure to that used by Webster et al.23 The codes in the more severe and less severe categories can be found in supplemental Tables 1 and 2. Injury severity was coded 1 for having at least one more severe diagnosis within the first 15 days of medical treatment and 0 for having only less severe diagnoses within the first 15 days of medical treatment. The more severe codes generally included diagnoses related to herniated disc, lumbar radiculopathy or neuropathy, spinal stenosis, sciatica, or possible instability. The less severe codes generally referred to diagnoses associated with degenerative changes, nonspecific back pain, or miscellaneous diagnoses. In addition, efforts were made to exclude cases of “complicated” back pain, such as those with diagnoses that were consistent with experiencing multiple work-related injuries or disorders, very severe injuries, or back pain due to cancer, infection, severe trauma, or an autoimmune disorder. Since the database included claims from 2002 to 2008, the analyses were controlled for the year of the injury. Age was measured continuously on the basis of the date of injury. Tenure was also measured continuously on the basis of a claimant's organizational tenure at the time of injury.
ANALYSES
The relationships between the three lag times and length of disability were estimated using Random Effects Tobit models. We were only interested in following claimants for 1 year from the time of disability onset; however, for some claimants, disability may not have ended by 365 days and it is necessary for our models to take this into account. Tobit models or censored regression models, as they are sometimes referred to, were chosen to deal with the nature of the data used in the current study wherein length of disability was restricted to a range between 3 and 365 days. Similar to ordinary least squared regression models (OLS), Tobit models are generally used when estimating linear relationships between variables; however, OLS generally assumes a continuous distribution without censored values, whereas the Tobit model is able to accommodate left- and/or right-censoring of values.24 OLS produces biased estimates when values are censored, while Tobit models eliminate that bias.25 In order to take into account the non-independence of observations across industry groupings, Random Effects Tobit models were selected instead of standard Tobit models. Participants drawn from different industry groups may be thought of as representing subsamples within the larger sample. Participants’ disability durations may be clustered within these different industry groups such that the residuals are dependent on one another within groups. Random effects models take this clustering into account by allowing the constant to vary across groups, in this case industries, while at the same time, keeping the other estimates fixed.26
For all lag times, the 0 days lag category was used as the reference group. Separate analyses were conducted for each of the three lag times due to concerns about collinearity among the lag times. In addition to the main analyses, differences in the coefficients for the non-reference group lag time categories were assessed using Wald Tests. Analyses were adjusted for gender, annual income, industry, litigation status, injury severity, year of injury, age, and tenure. To reduce issues with multicollinearity, all continuous variables in the models were mean-centered. STATA 13 was used to perform the analyses (Stata Corporation, College Station, TX). In the analyses, there was a relatively large sample size. On the basis of this, we used a more conservative P value of less than 0.001 to represent statistical significance. Confidence intervals for all estimates are presented.
RESULTS
In total, 64,004 claims were included in the analyses. The majority of claims (69.4%) were for men. The age of claimants at the time of injury ranged from 18 to 80 years, with an average age of 40 years (SD 11.2 years). The length of tenure at the time of injury ranged from 0 to 53 years, with an average tenure of 6 years (SD 7.7 years). Over half of the claimants had an annual income of $20,000 to $50,000 and only 1% of claimants had an annual income of over $100,000. The large majority of claims were for less severe low back injuries (81%) and less than 30% (28%) of claims were involved in litigation. The length of disability ranged from 3 to 365 days, with an average length of disability of 96 days (SD 118.5 days). The breakdown of claims in each of the lag time categories is presented in Table 1. For all of the lag times, the greatest percentage of claims had a 1 to 3-day lag time (36% reporting lag time; 36% medical services lag time; 57% work disability lag time).
TABLE 1.
Distribution of Claims by Lag Times
| Length of Lag Time | Lag Time | |||||
| Reporting | Medical Services | Work Disability | ||||
| No. of Claims | % of Claims | No. of Claims | % of Claims | No. of Claims | % of Claims | |
| 0 days | 10,010 | 15.64% | 21,321 | 33.31% | 2827 | 4.42% |
| 1–3 days | 22,921 | 35.81% | 23,095 | 36.08% | 36,472 | 56.98% |
| 4–6 days | 11,433 | 17.86% | 7521 | 11.75% | 6063 | 9.47% |
| 1 week up to 2 weeks | 10,540 | 16.47% | 5690 | 8.89% | 5083 | 7.94% |
| 2 weeks up to 30 days | 5631 | 8.80% | 3613 | 5.64% | 4226 | 6.60% |
| 30 days up to 60 days | 2108 | 3.29% | 1552 | 2.42% | 3734 | 5.83% |
| 60 days up to 1 year | 1361 | 2.13% | 1212 | 1.89% | 5599 | 8.75% |
Results of the Random Effects Tobit model are presented in Table 2. For the reporting lag time, in comparison to the 0 days lag time category, having a 1 to 3 days lag time was related to a shorter length of disability, whereas having a lag time of 2 weeks up to 30 days, 30 days up to 60 days, or 60 days up to a year was associated with a longer length of disability. For the medical services lag time, having a lag time of 4 to 6 days, 1 week up to 2 weeks, 2 weeks up to 30 days, 30 days up to 60 days, or 60 days up to a year were all related to a longer duration of disability than having 0 days of lag time. Finally, for the work disability lag time, in comparison to all other lag time categories, having 0 days of lag time was associated with a shorter length of disability.
TABLE 2.
Random Effects Tobit Model for Lag Times Predicting Length of Disability
| Predictors | Length of Disability† | ||||
| Coef. | Std. Err. | 95% CI | P | ||
| Reporting lag time* | |||||
| 1–3 days | −0.049 | 0.015 | −0.078 | −0.021 | 0.001 |
| 4–6 days | −0.025 | 0.017 | −0.058 | 0.008 | 0.140 |
| 1 week up to 2 weeks | 0.027 | 0.017 | −0.006 | 0.061 | 0.113 |
| 2 weeks up to 30 days | 0.237 | 0.020 | 0.197 | 0.277 | 0.001 |
| 30 days up to 60 days | 0.371 | 0.029 | 0.313 | 0.428 | 0.001 |
| 60 days up to 1 year | 0.438 | 0.036 | 0.368 | 0.508 | 0.001 |
| Medical services lag time* | |||||
| 1–3 days | −0.006 | 0.011 | −0.028 | 0.016 | 0.585 |
| 4–6 days | 0.087 | 0.016 | 0.056 | 0.119 | 0.001 |
| 1 week up to 2 weeks | 0.191 | 0.018 | 0.156 | 0.226 | 0.001 |
| 2 weeks up to 30 days | 0.382 | 0.022 | 0.339 | 0.425 | 0.001 |
| 30 days up to 60 days | 0.421 | 0.032 | 0.359 | 0.484 | 0.001 |
| 60 days up to 1 year | 0.410 | 0.036 | 0.339 | 0.481 | 0.001 |
| Work disability lag time* | |||||
| 1–3 days | 0.204 | 0.023 | 0.159 | 0.249 | 0.001 |
| 4–6 days | 0.383 | 0.027 | 0.331 | 0.436 | 0.001 |
| 1 week up to 2 weeks | 0.570 | 0.027 | 0.516 | 0.624 | 0.001 |
| 2 weeks up to 30 days | 0.711 | 0.029 | 0.655 | 0.767 | 0.001 |
| 30 days up to 60 days | 0.786 | 0.030 | 0.728 | 0.844 | 0.001 |
| 60 days up to 1 year | 0.783 | 0.028 | 0.729 | 0.837 | 0.001 |
Note: Analyses adjusted for litigation status, severity, income, gender, age, tenure, and loss use.
Full results available upon request.
Model fit for reporting lag time: AIC = 195,114.6; BIC = 195,305.0; χ2 = 28,626.27, P < 0.001.
Model fit for medical services lag time: AIC = 195,037.7; BIC = 195,228.1; χ2 = 28,752.44, P < 0.001.
Model fit for work disability lag time: AIC = 193,271.7; BIC = 193,462.1; χ2 = 31,329.45, P < 0.001.
CI, confidence interval.
*0 days lag time is the reference group.
†Natural log of length of disability.
To further compare the differences in the length of disability across the different lag times, in Figure 3, we plotted the predicted values for the length of disability for each of the lag time categories. We also assessed significant differences across the lag time categories for each of the respective lag times using Wald tests. The results are presented in Table 3.
FIGURE 3.
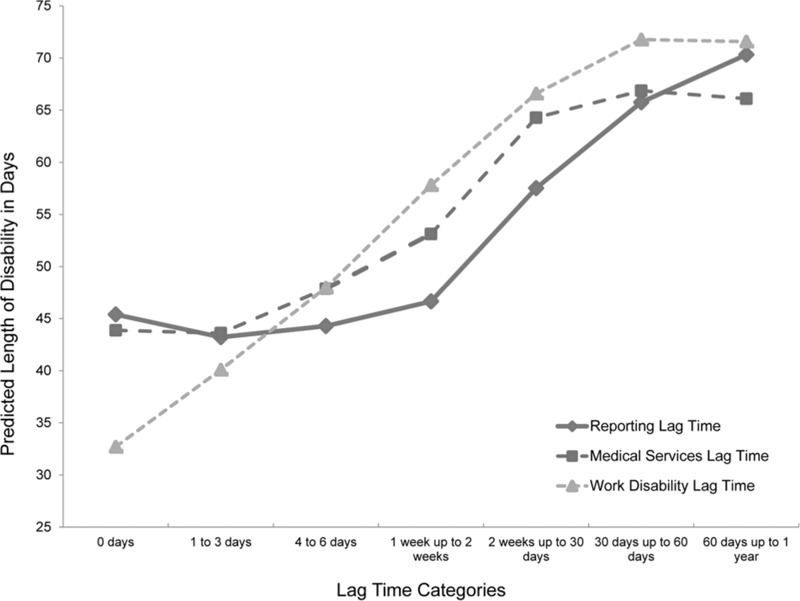
Plot of the predicted length of disability for each of the lag time categories. Note: This figure is based on the predicted values for the length of disability at each of the respective lag times.
TABLE 3.
Comparisons of Predicted Length of Disability across Lag Time Categories
| Lag Time Category | Reporting Lag Time | Medical Services Lag Time | Work Disability Lag Time | |||
| Predicted Length of Disability | Pairwise Comparisons* | Predicted Length of Disability | Pairwise Comparisons* | Predicted Length of Disability | Pairwise Comparisons* | |
| 1. 0 days | 45.39 | 1>2; 1<5, 6, 7 | 43.87 | 1<3, 4, 5, 6, 7 | 32.70 | 1<2, 3, 4, 5, 6, 7 |
| 2. 1–3 days | 43.21 | 2<1, 4, 5, 6, 7 | 43.60 | 2<3, 4, 5, 6, 7 | 40.09 | 2>1; 2<3, 4, 5, 6, 7 |
| 3. 4–6 days | 44.28 | 3<4, 5, 6, 7 | 47.88 | 3>1, 2; 3 <4, 5, 6, 7 | 47.97 | 3>1, 2; 3<4, 5, 6, 7 |
| 4. 1 week up to 2 weeks | 46.64 | 4>2, 3; 4<5, 6, 7 | 53.12 | 4>1, 2, 3; 4<5, 6, 7 | 57.81 | 4>1, 2, 3; 4<5, 6, 7 |
| 5. 2 weeks up to 30 days | 57.52 | 5>1, 2, 3, 4; 5<6, 7 | 64.28 | 5>1, 2, 3, 4 | 66.59 | 5>1, 2, 3, 4; 5<6, 7 |
| 6. 30 days up to 60 days | 65.76 | 6>1, 2, 3, 4, 5 | 66.87 | 6>1, 2, 3, 4 | 71.77 | 6>1, 2, 3, 4, 5 |
| 7. 60 days up to 1 year | 70.32 | 7>1, 2, 3, 4, 5 | 66.10 | 7>1, 2, 3, 4 | 71.57 | 7>1, 2, 3, 4, 5 |
*Wald tests used. All reported comparisons significant at P < 0.001.
Although not all of the differences among the lag time groups were statistically significant, across all three of the lag times, the trend was generally positive with the predicted length of disability increasing as the length of the lag increased. There were a few exceptions to this positive trend, specifically, for the 0 days and 1 to 3 days categories in the reporting lag time and the medical services lag time, the predicted length of disability actually decreased slightly as the length of the lag increased (Note: the decrease was only statistically significant for the reporting lag time). In addition, the predicted length of disability again decreased slightly going from a lag time of 30 days up to 60 days to a lag time of 60 days up to a year in the medical services and work disability lag times (Note: these decreases were not statistically significant).
When examining the reporting lag time, there was over a 20-day difference in the predicted length of disability going from a lag time of 1 to 3 days to a lag time of 60 days up to a year. Overall, there was roughly a 10-day difference or slightly more for having less than 2 weeks of lag time in reporting the injury compared with having 2 weeks or longer for the lag time. For the medical services lag time, the greatest difference was between having 1 and 3 days of lag time where the predicted length of disability was 43.6 days and having a lag time of 30 days up to 60 days where the predicted length of disability was 66.9 days. In general, having a reporting lag time of 2 weeks or longer was related to a significantly longer predicted length of disability than having a lag time of less than 2 weeks. The largest difference in the predicted length of disability across the lag time categories was for the work disability lag time. The predicted length of disability was close to 40 days less for having a work disability lag time of 0 days compared with having a lag time of 30 days or longer. In addition, the predicted length of disability increased by approximately a week to a week and a half across each of the work disability lag time categories going from the 0 days category up to the 30 days up to 60 days category.
DISCUSSION
In a sample of workers who experienced work-related low back injuries, the current study examined the associations between the length of work disability and three potential delays in the work disability process including the lag times from the work injury to (1) reporting the injury to an employer, (2) receiving medical treatment, and (3) taking time off of work or initiating light duty work. Understanding how these lag times are related to the length of disability can help guide health practitioners and employers in work disability case management.
For the reporting lag time, our results suggested that the length of disability may be shorter when there is earlier reporting of the injury to the workers’ compensation insurer, as there was approximately a 10-day difference or more in the predicted length of disability when comparing having a lag time of less than 2 weeks to having a lag time of 2 weeks up to a year. However, within the first 2 weeks of the injury, the predicted length of disability was slightly higher when reporting the injury on the same day it occurred, in comparison to reporting it 1 to 3 days after it occurred, but reporting the injury in the first week was associated with a shorter predicted length of disability than reporting the injury after the first week. One possible explanation for this finding is that workers may attempt to wait to report an injury in hopes that the injury will get better on its own; however, some workers with more severe injuries may find that the injury does not resolve and ultimately have to report the injury in order to start the workers’ compensation process. This would result in those workers who delay reporting an injury having more severe injuries that do not get better on their own. Similarly, some workers may feel pressure from their supervisors to delay reporting an injury until they are sure that the injury is serious enough to require medical attention and time off of work, which again would result in a greater length of disability for those who delay the report of the injury.
These findings for the reporting lag time are somewhat in line with a previous study of workers with low back injury, which reported that earlier injury reporting was related to a greater likelihood of having returned to work at 1 month following the LBP onset.19 In this previous study, all workers in the sample had reported the injury within 14 days of the pain onset and thus our findings for claimants reporting the injury after 14 days may not be comparable. Our results differ from the previous findings as we found an initially higher length of disability, but that was only for a zero-day lag time. This small difference may be the result of differences in outcome variables. We measured length of disability and the previous study measured the likelihood of work disability at 1 month after the injury. It is also possible that the differences in findings resulted from differences in the lag time categories used in the current study compared with the study by Shaw et al,19 which measured the lag time continuously.
Our findings for the lag time between injury and receiving medical treatment were fairly similar to those for the reporting lag time with shorter lag times relating to a shorter length of disability. For the medical services lag time, we found a two and half week increase or more in the predicted length of disability when waiting 2 weeks or longer to receive medical treatment for a low back injury compared with receiving medical treatment within the first week of injury. Also of note, the predicted length of disability was about a week shorter when receiving medical treatment in the first 3 days of injury than receiving treatment 1 week to up to 2 weeks after the injury occurred. These findings could reflect that earlier treatment for low back injuries may help to prevent acute LBP from transitioning to chronic LBP. Seeking medical treatment for low back injuries in the first 2 weeks can provide workers with assurance about the course of their condition, as well as help to avoid further reinjury. It is possible that those workers who delayed seeking medical treatment for low back injuries did not take proper measures to stop further aggravation to the back injury, which may have ultimately resulted in a greater length of disability.
For the medical services lag time, the findings are generally in line with previous studies of medical services lag times, which found that receiving medical treatment within 30 days of injury was associated with improved RTW outcomes.15,17 However, another previous study did not find a significant association between RTW and the lag time in receiving medical services when comparing a lag time of zero days with a lag time of 1 to 3 days or 4 days or more.18 Although our findings did not show a difference in the predicted length of disability for a lag time of 1 to 3 days when compared with zero days, we did find differences between a zero days lag time and a lag time of 4 days or more. It is possible that the differences in findings with this previous study could result from the difference in injury types examined. Our study focused specifically on low back injury, while the other study included all work-related injuries. In addition, the outcome variable used in the previous study was a dichotomous survey item indicating whether the worker was currently working, whereas we measured the length of disability continuously using retrospective claims data.
For the work disability lag time, the predicted length of disability was found to increase by approximately a week to a week and half going across the different lag time categories. For example, the predicted length of disability was approximately a week longer for claimants with a 1 to 3 days lag time than those with a zero days lag time. The predicted length of disability seemed to plateau at 30 days lags time, with a little difference observed between the 30 days up to 60 days lag time group and the 60 days up to 1 year lag time group. It is possible that these findings reflect workers trying to “tough it out” in hopes of not having to take time off of work due to injury. However, after several days or weeks, workers may then find themselves in a situation in which the injury is too severe to remain at work. As a result, workers in this delayed group may have more severe injuries that lead to a greater length of disability. To our knowledge, no studies exist that examine the association between lag times in initiating work disability and the length of disability. Our findings provide a critical first examination of this relationship and indicate that, in general, workers who initiated work disability earlier had a shorter predicted length of disability.
IMPLICATIONS
The results of the current study suggest that occupational low back injuries should be reported to the workers’ compensation insurer within the first week the injury occurs. Workers who reported the injury within the first 2 weeks after injury had on average a predicted length of disability over 14 days less compared with those whose injuries were reported 30 days or more after injury. With this in mind, interested parties, such as employers or insurers, may consider creating benchmarks for reporting a work-related injury no later than 2 weeks after the injury has occurred. Future research may also seek to investigate how to further mitigate barriers to reporting and facilitate trouble-free reporting, as this may help to shorten the lag time in reporting an injury.
For the medical services lag time, this study demonstrated that the predicted length of disability was the shortest for individuals who received medical treatment within the first 3 days of injury. However, significant proportions of workers did not receive timely medical care. Approximately 10% of the sample did not receive any medical treatment during the first 2 weeks following the injury. For these individuals, the predicted length of disability was more than 2 weeks longer than those who received medical treatment within the first 3 days after injury. Stakeholders might consider systems to ensure that medical care is rendered within the first 3 days after injury, and to investigate the circumstances that lead to delays in seeking treatment. On the contrary, encouraging workers to seek immediate medical care may have unintended consequences such as increasing the quantity of unnecessary tests and procedures, and ultimately delaying returning to work. As our study was correlational, we are unable to assess whether early seeking of medical treatment directly causes shorter disability duration. Future experimental research is needed to test this possibility. In addition, the medical services gap in this study focused specifically on seeking any medical treatment. For some claimants, this may have been intensive medical care, which included a large number of tests and procedures, while for others, it may have been more passive where a doctor recommended waiting a few days to see how the injury progressed. Our implications must be interpreted cautiously with this in mind.
With regard to the work disability lag time, surprisingly, there were approximately 14% of workers who worked for 1 month or more after injury before initiating work disability. For these workers, the predicted length of disability is more than doubled compared with those who initiated work disability the same day as the injury. An explanation for this doubling may be that a more severe reinjury or aggravation of the initial back injury could have occurred as a result of remaining at work after the injury, ultimately leading to an increase in the length of disability. Alternatively, some workers who delayed taking time off of work may have tried to self-manage their LBP, but eventually left work as their symptoms failed to resolve. In this case, these workers would represent a group of cases with likely greater severity of LBP. In either case, had workers more promptly taken time off of work or started light duty after the initial injury, then the length of disability may have been shorter.
Taking into consideration that this study does not account for workers who received medical care but never lost a day of work, for those who are likely to go out on work disability, or who have persistent symptoms that significantly interfere with their function, they should be encouraged to not delay a transition to temporary light duty work, seeking medical care, or taking off work altogether. For disability case managers and employers, this may equate to more swiftly arranging accommodations or care for these injured workers. More research is needed to understand the reasons for delayed work disability for 30 days or more. It is possible that these individuals may represent unique cases in need of additional resources to fully RTW after this long initial delay.
STRENGTHS AND LIMITATIONS
There were a number of strengths to this study, including the use of a wide range of workers’ compensation claims representing a variety of different industries, companies, and states. However, there are also several important limitations to note. As this study focused on the administrative data from a large, workers’ compensation insurer, this study does not provide any explanations as to why we observed differences in the lag times. For example, it may be assumed that individuals would seek treatment immediately after a work-related injury, but this study's findings suggest this is not always the case, although in this study we have little information as to why there was a delay. Gaining a better understanding of why there are lag times in the work disability process may help to shorten the length of disability following a work-related low back injury. Along these lines, there are several other variables of interest that may confound the relationship between lag times and the length of disability that were not available in the administrative data. Some of these factors include the availability of workplace accommodations, the quality of the relationship with the supervisor, the level of physical demands associated with a claimant's occupation, and a claimant's motivation to return to work. It is possible that if these variables were available, they may help to explain the relationship between lag times and the length of disability or possibility reduce the strength of the relationship. In addition, our measure of injury severity may be problematic for certain claims, as it could be an indicator of comorbidity. No true measure of comorbidity existed in this study. We focused only on the primary diagnosis relating to the main injury with no information about comorbid diagnoses that might impact recovery from the main injury. It is possible though that for certain diagnoses, comorbid conditions are likely.
Another limitation associated with using administrative data is that we lacked a true measure of RTW. For analytic purposes, the length of disability was calculated on the basis of indemnity payments, with the assumption that the end of indemnity payments coincided with RTW. Although for many the end of indemnity payments is the result of returning to work, it is possible that in some cases, indemnity payments may have ended for a reason other than RTW.
A major limitation in this study was that the analyses were limited to workers who at some point had lost work time compensated through the workers’ compensation system. This was done for practical reasons, as our analyses focused on the length of disability as an outcome, but it is well known that a large majority of workers’ compensation claims are for medical treatment only. As such, our findings must be interpreted with this in mind as they may only apply to workers who receive wage replacement for time off of work. Accordingly, the implications of our findings may be biased, as we only have the length of disability for individuals who did actually experience lost work time and our recommendation of earlier reporting and seeking of medical treatment may be detrimental for individuals who do not ultimately take time off of work, as early medical treatment may result in a greater number of unnecessary services. In addition, it is possible that some workers may have used vacation days to take off work for recovery purposes in order to avoid receiving lower wages in the workers’ compensation system, and thus, these cases were not included in our sample. Along these lines, our sample may suffer from the Immortal time bias.27 In the administrative data, we only have information on individuals who did ultimately have a claim accepted for a given injury. We do not have information on individuals who may have had an injury but never filed a claim. It is possible that some of these individuals that never filed a claim did not do so because they recovered and returned to work relatively quickly after injury and felt that they did not need to file a claim. If this were the case, following our recommendation in all cases of encouraging early reporting of a claim and early commencement of work disability would be problematic, as it would result in more claims and more time away from work cases. It is therefore important to interpret our results with this in mind as our sample is selective to those who did file claims. Thus, these recommendations may make sense only for those persons who are likely to file a disability claim.
One of the major findings of our study was that the amount of time individuals waited before taking time off of work was related to the length of disability. Although this was a major focus of the study, this may also present a potential limitation of our findings, as we are treating the length of disability as independent of when an injury actually occurred in relation to work disability onset. When calculating the length of disability, we utilize the date that lost work time began and the date that lost work time ended, without considering how many days there were between when the injury occurred and when lost work time started. The work disability lag time does include this information directly, but this variable could not be included in the models for the other two lag times because of collinearity concerns. Moreover, we have no information about what claimants with lag times higher than zero days were doing in those days before time off work began. Some of these individuals may have already been off work but not collecting benefits, others may have been using sick time, while others could have still been at work. Unfortunately, we are not able to account for this in our analyses. Our study focused solely on the length of disability on the basis of receiving indemnity payments for lost wages, despite the fact that individuals may have lost wages for which indemnity payments were not received. Our findings are therefore limited to this specific definition of length of disability.
Finally, there were two issues with our measure of the lag times. First, due to the highly skewed distributions, for analytic purposes, the three lag time variables were measured as categorical variables. It would have been more ideal to run models with these variables coded continuously in order to be more informative about how a day or a week of difference in the lag times was related to the length of disability. We attempted to select meaningful categories for our analyses, but it is possible that valuable information was lost in the process. The second issue was that the three lag times were highly collinear and needed to be analyzed in separate models. As a result, in our analyses, we did not consider the relative strength of the different lag time relationships with the length of disability. It is possible that one lag time may be more influential than another. Moreover, there may be combinations among the lag time categories that may further contribute to the relationship with the length of disability. Future research may seek to address this possibility.
CONCLUSIONS
Overall, the current study showed that across all three of the lag times, shorter lag times are related to shorter lengths of disability. These findings suggest that in workers with occupational low back injuries that are expected to go out on work disability, the length of disability may be decreased by earlier injury reporting, earlier receipt of medical care, and earlier initiation of light duty work and/or time off work.
Supplementary Material
REFERENCES
- 1.Punnett L, Pruss-Utun A, Nelson DI, et al. Estimating the global burden of low back pain attributable to combined occupational exposures. Am J Ind Med 2005; 48:459–469. [DOI] [PubMed] [Google Scholar]
- 2.U.S. Department of Labor. Back Injuries---Nation's Number One Workplace Safety Problem. Washington, DC: U.S. Department of Labor: Occupational Safety and Health Administration; 1989. [Google Scholar]
- 3.Bureau of Labor Statistics Nonfatal Occupational Injuries and Illnesses Requiring Days Away From Work 2013. Washington, DC: U.S. Department of Labor; 2014. [Google Scholar]
- 4.Dagenais S, Caro J, Haldeman S. A systematic review of low back pain cost of illness studies in the United States and internationally. Spine J 2008; 8:8–20. [DOI] [PubMed] [Google Scholar]
- 5.Waddell G. Simple low back pain: rest or active exercise? Ann Rheum Dis 1993; 52:317–319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Abenhaim L, Suissa S. Importance and economic burden of occupational back pain: a study of 2,500 cases representative of Quebec. J Occup Med 1987; 29:670–674. [PubMed] [Google Scholar]
- 7.Krause N, Ragland DR. Occupational disability due to low back pain: a new interdisciplinary classification based on a phase model of disability. Spine 1994; 19:1011–1020. [DOI] [PubMed] [Google Scholar]
- 8.Frank J, Sinclair S, Hogg-Johnson S, et al. Preventing disability from work-related low-back pain. New evidence gives new hope--if we can just get all the players onside. CMAJ 1998; 158:1625–1631. [PMC free article] [PubMed] [Google Scholar]
- 9.Costa-Black KM, Loisel P, Anema JR, et al. Back pain and work. Best Pract Res Clin Rheumatol 2010; 24:227–240. [DOI] [PubMed] [Google Scholar]
- 10.Krause N, Ragland DR, Greiner BA, et al. Psychosocial job factors associated with back and neck pain in public transit operators. Scand J Work Environ Health 1997; 23:179–186. [DOI] [PubMed] [Google Scholar]
- 11.Friesen MN, Yassi A, Cooper J. Return-to-work: the importance of human interactions and organizational structures. Work 2001; 17:11–22. [PubMed] [Google Scholar]
- 12.Pransky G, Benjamin K, Hill-Fotouhi C, et al. Work-related outcomes in occupational low back pain: a multidimensional analysis. Spine 2002; 27:864–870. [DOI] [PubMed] [Google Scholar]
- 13.Kapoor S, Shaw WS, Pransky G, et al. Initial patient and clinician expectations of return to work after acute onset of work-related low back pain. J Occup Environ Med 2006; 48:1173–1180. [DOI] [PubMed] [Google Scholar]
- 14.Shaw WS, Pransky G, Winters T. The Back Disability Risk Questionnaire for work-related, acute back pain: prediction of unresolved problems at 3-month follow-up. J Occup Environ Med 2009; 51:185–194. [DOI] [PubMed] [Google Scholar]
- 15.Infante-Rivard C, Lortie M. Prognostic factors for return to work after a first compensated episode of back pain. Occup Environ Med 1996; 53:488–494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McIntosh G, Frank J, Hogg-Johnson S, et al. Prognostic factors for time receiving workers’ compensation benefits in a cohort of patients with low back pain. Spine 2000; 25:147–157. [DOI] [PubMed] [Google Scholar]
- 17.Kucera KL, Lipscomb HJ, Silverstein B, et al. Predictors of delayed return to work after back injury: a case-control analysis of union carpenters in Washington State. Am J Ind Med 2009; 52:821–830. [DOI] [PubMed] [Google Scholar]
- 18.Kominski GF, Pourat N, Roby DH, et al. Return to work and degree of recovery among injured workers in California's Workers’ Compensation system. J Occup Environ Med 2008; 50:296–305. [DOI] [PubMed] [Google Scholar]
- 19.Shaw WS, Pransky G, Patterson W, et al. Early disability risk factors for low back pain assessed at outpatient occupational health clinics. Spine 2005; 30:572–580. [DOI] [PubMed] [Google Scholar]
- 20.Ehrmann-Feldman D, Rossignol M, Abenhaim L, et al. Physician referral to physical therapy in a cohort of workers compensated for low back pain. Phys Ther 1996; 76:150–156. [DOI] [PubMed] [Google Scholar]
- 21.Pransky GS, Verma SK, Okurowski L, et al. Length of disability prognosis in acute occupational low back pain: development and testing of a practical approach. Spine 2006; 31:690–697. [DOI] [PubMed] [Google Scholar]
- 22.Occupational Safety and Health Administration Occupational Safety & Health Administration SIC Manual. Washington, DC: U.S. Department of Labor; 2014. [Google Scholar]
- 23.Webster BS, Choi Y, Bauer AZ, et al. The cascade of medical services and associated longitudinal costs due to nonadherent magnetic resonance imaging for low back pain. Spine 2014; 39:1433–1440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.UCLA: Statistical Consulting Group. Tobit Analysis. Los Angeles, CA: Institute for Digital Research and Education; 2015. [Google Scholar]
- 25.Henningsen A. Estimating Censored Regression Models in R Using the censReg Package. 2010. Available at: cran.r-project.org Accessed September 8, 2015. [Google Scholar]
- 26.Baum C. An introduction to modern econometrics using stata. College Station, TX: Stata Press:2006. [Google Scholar]
- 27.Suissa S. Immortal time bias in pharmacoepidemiology. Am J Epidemiol 2008; 167:492–499. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


