Abstract
One of the unique features of prenatal alcohol exposure in humans is impaired cognitive and behavioral function resulting from damage to the central nervous system (CNS), which leads to a spectrum of impairments referred to as fetal alcohol spectrum disorder (FASD). Human FASD phenotypes can be reproduced in the rodent CNS following prenatal ethanol exposure. Several mechanisms are expected to contribute to the detrimental effects of prenatal alcohol exposure on the developing fetus, particularly in the developing CNS. These mechanisms may act simultaneously or consecutively and differ among a variety of cell types at specific developmental stages in particular brain regions. Studies have identified numerous potential mechanisms through which alcohol can act on the fetus. Among these mechanisms are increased oxidative stress, mitochondrial damage, interference with the activity of growth factors, glia cells, cell adhesion molecules, gene expression during CNS development and impaired function of signaling molecules involved in neuronal communication and circuit formation. These alcohol-induced deficits result in long-lasting abnormalities in neuronal plasticity and learning and memory and can explain many of the neurobehavioral abnormalities found in FASD. In this review, the author discusses the mechanisms that are associated with FASD and provides a current status on the endocannabinoid system in the development of FASD.
Keywords: fetal alcohol, learning and memory, CB1 receptors, brain development, synaptic plasticity, intellectual disability
1. Introduction
The influence of alcohol use during pregnancy on children has received widespread research attention since early reports that prenatal alcohol exposure can have devastating and enduring consequences [1]. Among the many potential outcomes of prenatal alcohol exposure, alterations in the developing brain and the resulting lifelong neurobehavioral deficits have been the most devastating. One of the many recognized consequences of prenatal alcohol exposure is fetal alcohol syndrome (FAS) [2], which is characterized by pre- and postnatal growth deficiencies, craniofacial anomalies and central nervous system (CNS) dysfunction. FAS is now recognized as an important cause of intellectual disabilities and behavior problems in many countries [3,4,5,6,7]. However, over the last 35 years, it has become clear that FAS is not the only outcome resulting from prenatal alcohol exposure. Indeed, the term fetal alcohol spectrum disorders (FASD) [8] has been used to emphasize the continuous nature of the effects of prenatal alcohol exposure, with FAS at the more severe end of the spectrum. While literature regarding the behavioral profile of FASD is relatively limited [9], reported deficits suggest that FASD is one of the main causes of intellectual disability in Western nations [10] and is accompanied by widespread neuropsychological deficits such as verbal learning/recall abilities [11,12], including deficits in learning and memory [13,14]. These substantial neuropsychological deficits create many daily challenges for individuals with FASD. However, the cognitive deficits of FASD are not fully understood, and a characteristic outline has not been identified. This review will provide a comprehensive summary of the neurobehavioral effects of heavy prenatal alcohol exposure. Supporting studies from animal model systems with an emphasis on the molecular events mediated by the endocannabinoid system resulting in brain-behavior associations are included when appropriate.
1.1. Influence of Developmental Stage, Amount and Pattern of Alcohol Use on Neurobehavioral Outcome
The consequences of maternal alcohol use during pregnancy on the neurobehavioral outcome of children are dependent on several factors, including the amount and pattern of alcohol consumption as well as the developmental timing of exposure. In most cases, the amount of alcohol consumed is correlated with the severity of the outcome [15,16]. However, the pattern of alcohol exposure can often undermine these effects, with binge-like exposures resulting in more severe deficits than chronic exposure [17,18]. Developmental timing of the exposure is also important. Alcohol exposure at different periods of fetal development can greatly influence the pattern and severity of the structural and functional abnormalities [19]. In addition, several other factors may contribute to this variation in the consequences of maternal drinking. These factors include, but are not limited to, the following: differences in maternal metabolism, differences in genetic susceptibility, and variation in the vulnerability of different brain regions. Nevertheless, factors that alter the peak blood alcohol concentration (BAC) experienced by the embryo or the fetus (e.g., maternal drinking patterns and maternal metabolism) are most likely to affect the occurrence and severity of alcohol-induced developmental brain disorders. Unfortunately, this level of detail is often difficult to document, particularly in retrospectively recruited samples, and individual studies provide varying degrees of detail concerning the levels and patterns of exposure. These issues highlight the modifying variables that contribute to the considerable range of phenotypes presented in children with FASD.
1.2. Neurobehavioral Abnormalities in Children with FASD
FASD affects an estimated prevalence of as high as 2%–5% in the United States and several Western European countries [20] and is the leading preventable cause of mental retardation [8]. Although publicity campaigns have encouraged women to stop alcohol consumption once they know that they are pregnant, data from a US national survey indicated that 13% of women continue to use alcohol during pregnancy (see [21]).
Prenatal alcohol exposure has been associated with widespread neuropsychological deficits across several domains (Table 1), including general intelligence, memory, language, attention, learning, visuospatial abilities, executive functioning, fine and gross motor skills and social and adaptive functioning [12]. Many FASD individuals exhibit impaired intellectual abilities and growth retardation [22], although children with a diagnosis of FAS tend to have more severe impairments compared to those who were exposed prenatally to alcohol but do not have sufficient dysmorphic features for a diagnosis [23]. However, not all individuals diagnosed with FAS are intellectually disabled (IQ score < 70), and intellectual disability is not a necessary criterion for the diagnosis of FAS. The average IQ estimate of children with prenatal alcohol exposure is 70 for those with FAS [7] and 80 for nondysmorphic children [23]. However, fewer studies have been performed on the intellectual abilities among individuals with moderate levels of alcohol exposure, and these results have been inconsistent [16,24,25,26,27]. The discrepancies among studies with moderate levels of exposure warrant the need for further research and the importance of considering a variety of factors as described in the proceeding section when evaluating studies.
Table 1.
Summary of neuropsychological abnormalities found in individuals with fetal alcohol spectrum disorders (FASD) when compared to typically developing children.
| Cognitive Function | FASD | References |
|---|---|---|
| General Intelligence | Lower IQ (~70) | [7,23,28] |
| Executive Function | Impaired executive functions such as planning, fluency and working memory | [14,29,30,31,32,33,34] |
| Learning and memory | ||
| Verbal | Impaired initial learning without affecting retention of information already learned due to implicit learning strategies. | [12,35,36,37,38,39,40] |
| Nonverbal | Impaired nonverbal learning and memory but impairment of retention of information is inconsistent. | [29,36,39,41,42,43,44] |
| Motor function | Deficits in motor abilities and visual-motor tasks. | [11,35,42,45,46,47,48,49,50,51] |
| Attention and hyperactivity | Deficits in attention and exhibit hyperactivity. | [10,48,52,53,54,55,56,57,58,59,60] |
A number of clinical studies have also reported learning and memory deficits in children with heavy prenatal alcohol exposure. Prenatal alcohol-exposed children display poorer academic achievement and higher learning disability rates than control children [61], which may relate to impairments in their verbal and non-verbal learning and memory [35,36,37]. These deficits were present in both children with and without the dysmorphic features of FAS [12,36]. Some studies have suggested that the long-term retention of verbal information is intact in alcohol-exposed children but that the initial encoding processes may be impaired [36,38]. In addition to non-verbal memory difficulties, children with FASD showed visuospatial processing deficits [35], suggesting damage and abnormalities in the frontal-subcortical pathway. Attention deficits [62,63] and attention deficit hyperactivity disorder (ADHD) [64] were also frequently found in FASD children. A recent collaborative study also suggested that executive function and spatial processing were particularly sensitive to prenatal alcohol exposure [52]. Executive functions are regulated by the frontal-subcortical circuits, which involve projections from the frontal lobes to the basal ganglia and thalamic nuclei [65]. These regions have been found to be affected by prenatal alcohol exposure [66,67]. In addition, FASD children have social and adaptive deficits because they are more likely to be rated as hyperactive, disruptive, impulsive or delinquent compared to non-exposed children [68,69]. Furthermore, children with prenatal alcohol exposure have difficulty resolving conflicts and in anticipating the consequences of their actions [70,71], suggesting the challenges that children with FASD face in interacting with peers.
In summary, the phenotype of children with FASD is characterized by social, behavioral, and language problems that disrupt interactions with peers and appear to be influenced by task complexity. In addition to these disabilities, neuropsychological problems in planning, inhibition, self-regulation, and attention and memory potentially contribute to the challenges faced by these children in school settings. In particular, children with FASD may suffer from social and academic situations because their deficits interfere with their ability to be sufficiently engaged. Student engagement, inferred from performance (attention, work completed, appropriate participation), is key to motivation and, ultimately, learning or mastering knowledge or skills [72]. These observations highlight not only the importance in identifying FASD at early ages, but also the provision of specific treatments to address this developmental disability because early identification and treatment have been demonstrated to be protective against more serious secondary disabilities [73,74,75]. Despite four decades of progress, research on FASD and its treatment continue to be hampered by a lack of specificity in the behavioral diagnostic criteria and a limited understanding of the cellular and molecular substrates of cognitive deficits (e.g., attention, memory, executive functioning) caused by heavy prenatal alcohol consumption. Finally, research on the biomarkers of fetal alcohol damage may help to improve the future of children affected by prenatal alcohol exposure.
1.3. Neurobehavioral Abnormalities in Animal Models of FASD
Animal models provide rigorous experimental control over numerous potentially confounding variables as well as control of the dose and timing of the alcohol exposure. In addition, animal models have the advantage of non-confounding multiple factors, which may be independently manipulated. In contrast, causal conclusions are difficult to reach in human studies due to the clustering of negative events. For example, alcohol consumption and smoking tobacco are often strongly associated with each other, and alcohol use usually affects nutrition intake in people. However, to relate animal models to human development, the relative states of brain development at times of alcohol exposure need to be carefully considered. Some of the behavioral and anatomical outcomes discussed above have also been reported in animal models of FASD. A number of researchers have extended the findings in humans to animal research using tests that have been found to be sensitive to hippocampal function [41,76,77,78,79,80,81,82,83,84,85,86].
Prenatal alcohol exposure has been shown to affect embryonic development, which varies depending on the severity, duration, and frequency of exposure of ethanol during gestation [87,88,89]. During this period, the use of alcohol prevents the proper blastocyst implantation in the uterus, resulting in an increased rate of resorption or early termination of the pregnancy, which generally occurs before a woman realizes she is pregnant. In the third week after fertilization, specific alcohol-induced birth defects begin to affect the developing embryo [90,91,92,93]. Between the third and sixth week after fertilization, when neurulation occurs, the cranial neural crest cell population is vulnerable to alcohol-induced damages [94], which are related to facial abnormalities characteristic of FAS. From the third week through the third trimester, the cellular progenitor pools, known as radial glia, which will give rise to the CNS, become vulnerable to the effects of alcohol and result in morphological abnormalities and an overall reduction in white matter within the brain [95,96]. Specific damage to the brain continues in the sixth and seventh week following fertilization, after the brain has begun to divide into vesicles. The corpus callosum, a midline structure responsible for communication between the left and right hemispheres of the brain, has been shown to be vulnerable to alcohol at this stage of development [97]. The eighth week after fertilization is the end of the embryonic stage and the beginning of the fetal stage of pregnancy. At this stage, the developing brain remains vulnerable to prenatal exposure to alcohol, particularly in the formation of the cerebellum, and the fetus remains vulnerable in terms of prenatal growth restrictions. The cerebellum and hippocampus are vulnerable to the neurotoxic effects of alcohol [98], particularly when alcohol exposure is limited to the third trimester equivalent in the rat (i.e., the first postnatal week) [98,99]. Purkinje cells within the cerebellum [100] appear most vulnerable to the effects of alcohol prior to the 7th postnatal day (PD) [101], while alcohol exposure encompassing all of gestation (gestational days (GD)1–22) or limited to either PD 4–9 or PD 7–9 results in CA1 pyramidal cell reduction within the hippocampus [80,82,84,102,103,104,105]. Limiting alcohol exposure to PD 7–9, therefore, is likely to result in significant hippocampal targeting relative to the cerebellum and may result in severe learning and memory deficits [106,107,108,109,110,111,112].
1.3.1. Potential Mechanisms Responsible for FASD
Anatomical alterations associated with brain dysfunction may range from a gross reduction in brain volume to deficits in cell number in a particular brain region to cellular modifications of individual neurons, resulting in alterations in the communications among neuronal cells. These alterations can have a long-term detrimental effect on behavioral and cognitive development. Experimental evidence has demonstrated that ethanol exposure during brain development could affect several molecular, biochemical and cellular events, which participate in the proper formation of brain structure. Thus, at the cellular level, and depending on the time and amount of alcohol exposure, ethanol could induce deficits in cell proliferation, migration, growth and differentiation and may cause apoptotic neurodegeneration. For example, alcohol exposure during early embryonic development, when cells undergo rapid division, causes a reduction in the number of cells generated [113], including neural progenitor cells [114,115,116], abnormal neuronal migration and may cause subsequent cell death [117,118]. However, if alcohol exposure occurs during the cell differentiation [119,120] and synaptogenesis period [121], it may cause robust neurodegeneration [111,112,121,122,123,124] leading to the loss of synapses. These results support the notion that ethanol exerts its effects by multiple actions at different sites involving several mechanisms.
Several major molecular mechanisms have been identified as potential candidates responsible for FASD [98,125,126]. These mechanisms are likely to participate at different stages of brain development and/or with different doses of ethanol. The major probable mechanisms include the following: (1) alterations in the regulation of gene expression (e.g., expression of anandamide (AEA) and 2-arachidonylglycerol (2-AG) synthesizing enzymes, 2-AG metabolizing enzyme, cannabinoid receptor type 1 [111,127], homeobox gene, histone methyl transferase, altered histone and DNA methylation [109,110,124,128,129,130,131,132], and microRNAs (miRNAs) [133,134]; (2) interference with mitogenic and growth factor responses involved in neural stem cell proliferation, migration and differentiation [135,136,137]; (3) disturbances in the molecules that regulate cell–cell interactions (e.g., L1, NCAM, growth factors) [138,139,140,141,142,143]; (4) activation of the molecular cascade, which regulates cell survival or cell death (growth factor deprivation, oxidative stress, apoptotic signaling through caspase-3 activation, H3 histone methylation mediated histone degradation, suppression of N-Methyl-d-aspartate (NMDA), glutamate and gamma-amino butyric acid-A (GABAA receptors) [111,124,144,145,146,147,148,149,150]; (5) abnormalities in glial proliferation, differentiation and function [95,151] and (6) suppression of the mitogen-activated protein kinase (MAPK) pathway via enhanced endocannabinoid signaling [110,111,127]. This last mechanism is supported by CB1 receptor antagonist and CB1 receptor null mice studies revealing the contribution of this signaling system to neuronal loss through caspase-3 and NMDA receptors, synaptic plasticity and learning and memory abnormalities found in an FASD animal model [110,111,127]. Due to the potential contribution of this novel mechanism to brain development, learning and memory loss with FASD, we will describe the evidence demonstrating that the endocannabinoid signaling system is an important potential target involved in the development of FASD.
1.3.2. Role of the Endocannabinoid System during Brain Development and in Ethanol-Induced Brain Abnormalities
Within the last two decades, cannabinoid research has received tremendous attention due to the breakthrough and discovery of the receptors that bind delta-9-tetrahydrocannabinol (Δ9-THC) (cannabinoid receptors) and their endogenous ligands, endocannabinoids (ECs) (endocannabinoid system) in animal tissues (for a recent review see [152]). This emerging body of research has revealed multiple ways in which the EC system functions to regulate synaptic neurotransmission in various brain areas [153,154,155] in the developing and adult brain. Growing research has demonstrated vital functions for EC signaling in molecular pathways that underlie both short- and long-lasting alterations in synaptic strength [156,157]. In fact, the critical involvement of ECs in some mechanisms of synaptic neurotransmission may change the current working cellular models of learning and memory. These models may be vital in understanding and providing potential treatment for the disease conditions in which the EC system plays an important role.
Potential Role of Endocannabinoids and Their Metabolic Enzymes
ECs consist of lipid signaling molecules that bind to and activate cannabinoid receptors. These lipid compounds are formed from phospholipid precursors [158,159,160,161,162,163] within cells throughout the body and are released from these cells on demand in a nonvascular manner to act in a paracrine fashion [158,160,161,162,163,164].
In 1992, anandamide (arachidonylethanolamide, AEA) was first identified as an endogenous cannabinoid. Its name is derived from the Sanskrit word, ananda, which means “internal bliss”, making a reference to its chemical structure (the amide of arachidonic acid and ethanolamine) [165]. Subsequently, another endogenous cannabinoid receptor ligand, 2-arachidonylglycerol (2-AG), was discovered and characterized [166,167]. The third ether-type EC, 2-arachidonylglycerol ether (noladin ether), was isolated from the CNS and shown to display pharmacological properties similar to AEA [168]. The fourth type of EC, virodhamine, in contrast to the previously described ECs, is a partial agonist with in vivo antagonist activity on the CB1 receptor [169]. The fifth type of EC, N-arachidonyl-dopamine (NADA), not only binds to the CB1 receptor but also stimulates vanilloid receptors (VR1) [170]. Importantly, except for AEA and 2-AG, to date, there is little evidence regarding the physiological actions of these compounds.
AEA is thought to be synthesized by several pathways (see review for details [171]). Importantly, there is strong evidence for a calcium dependence in both of these synthesis steps, which may underlie the requirement for postsynaptic Ca2+ in specific forms of depolarization-induced synaptic plasticity (For details see [157]). Biosynthesis of AEA from membrane phospholipid precursors is catalyzed by several enzymes. The most well-studied of these is N-acylphosphatidylethanolamine-specific phospholipase D (NAPE-PLD; [172,173]), but others include glycerophosphodiesterase (GDE1) [174], abhydrolase domain 4 (ABHD4) [175] and phosphatase PTPN22 [176] (Figure 1). In our recent study, we found that NAPE-PLD protein levels were significantly lower during the synaptogenic period of mouse brain development and gradually increased to adult levels [111]. Similar patterns of NAPE-PLD expression were also found during rat brain development [177]. Overwhelming data suggested that the lack of NAPE-PLD significantly reduced the levels of AEA and other NAE [178,179] in the brain, although some controversy exists on whether NAPE-PLD contributes to the formation of AEA in the brain [180]. Interestingly, studies have suggested a significant reduction in the accumulation of brain NAEs, including AEA, in GDE1/NAPE-PLD double KO mice treated with an FAAH inhibitor that blocks NAE degradation [181]. Our study suggested that postnatal ethanol treatment enhanced AEA levels via transcriptional activation of both the NAPE-PLD and GDE1 genes, resulting in the enhanced expression of NAPE-PLD and GDE1 mRNA and proteins in neonatal mouse brain regions [111].
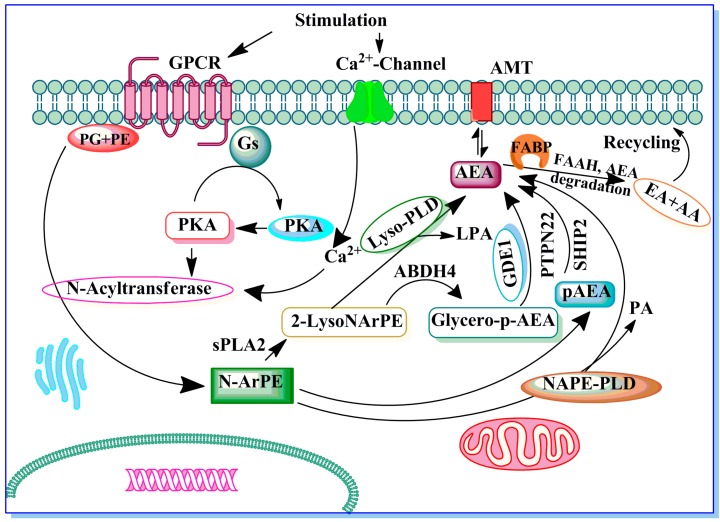
Figure 1.
The potential enzymes involved in anandamide (AEA) biosynthesis. Stimulation of G-protein coupled receptor (GPCR) mediated adenylate cyclase and cAMP-dependent protein kinase (protein kinase A, PKA) potentiate N-acyltransferase (Ca2+-dependent transacylase) (NAT). A fatty arachidonic acid chain is transferred by NAT from the sn-1 position of phospholipids (phosphoglycerides, PG) to the primary amine of phosphatidylethanolamine (PE) in a Ca2+-dependent manner, forming an N-arachidonyl phosphatidylethanolamine (N-ArPE). This N-ArPE intermediate is then hydrolyzed by a phospholipase D (PLD)-like enzyme to generate AEA. In addition, potential alternative pathways for AEA formation from N-ArPE through 2-lysoNArPE and pAEA catalysed by sPLA2, lyso-PLD, ABDH4, GDE1 or PTPN22 and SHIP2 are shown (see text for details). Once synthesized, AEA can be metabolized into ethanolamine (EA) and arachidonic acid (AA) or transported to the outside of the cell through a process that has not yet been well characterized. Fatty acid binding proteins (FABPs) serve as intracellular carrier of AEA and play an important role in the AEA degradation by FAAH. EMT, ECmembrane transporter.
As a putative neuromodulator, AEA released into the synaptic cleft is expected to be rapidly inactivated. In general, two mechanisms are known that could remove ECs from the synaptic cleft to ensure rapid signal inactivation: re-uptake or enzymatic degradation. AEA is inactivated by reuptake [182,183] via an uncharacterized membrane transport molecule, the “AEA membrane transporter” (AMT) [163,182,184,185,186,187,188], and subsequent intracellular enzymatic degradation. AEA is metabolized into arachidonic acid and ethanolamine via the action of the fatty acid amide hydrolase (FAAH), and this activity plays a significant role in the rapid clearance of AEA from extracellular compartments [189,190]. In addition, fatty acid binding proteins (FABPs) are suggested to serve as intracellular carrier of AEA and play an important role in the pathway for AEA inactivation by FAAH. Inhibition of FAAH activity by pharmacological blockade or genetic ablation has been shown to cause an accumulation of AEA in the brain [191,192,193]. Similar to FAAH inhibition, inhibitors of FABPs also reduce hydrolysis of AEA and its uptake into cells, raising levels of extracellular AEA [194,195,196,197]. In addition to hydrolysis by FAAH, AEA is metabolized by COX-2, LOX and cytochrome P450 [187,198,199,200]. Further research is required to elucidate the precise mechanism and enzymes involved in this pathway of AEA metabolism. It was previously shown that the FAAH distribution during postnatal development was very similar to the adult pattern [201]. In our study, postnatal ethanol treatment did not considerably alter either the FAAH protein or the mRNA levels in neonatal brain regions [111]. Moreover, FAAH has been detected in radial glia during late gestation and postnatal periods [202]. These distribution patterns of FAAH, together with the EC control of astrogliogenesis [202], suggest the involvement of EC signaling in neural progenitor differentiation in vivo. A fine balance between progenitor cell proliferation and programmed death ensures the generation of adequate quantities of neural cells during brain development.
The second widely recognized endogenous CB1 agonist is 2-AG, which was characterized soon after the discovery of AEA [166,167]. 2-AG has been characterized as a unique molecular species of monoacylglycerol isolated from both the canine gut [166] and rat brain [203], where it presumably functions as an endogenous cannabinoid receptor ligand. 2-AG biosynthesis occurs via two possible routes in neurons (see recent review [204]). DAGL-α and β both contribute to a large extent the regulation of steady-state levels of 2-AG in the brain and other tissues. However in mice lacking DAGL-α, 2-AG levels are reduced by up to 80% in the brain and up to 50% in the DAGL-β null mouse brain [205]. DAGL-α and β are expressed lower during early development and gradually increase throughout development to adulthood [127]. 2-AG, similar to AEA, is found in a variety of tissues throughout the body and brain and appears to be released from cells in response to specific stimuli. Although the 2-AG concentration in the rodent brain is in the nanomolar range, which is one hundred times higher than that of AEA, it is 20 times less potent than AEA at the CB1 receptor [166]. 2-AG is also inactivated by reuptake [182,183] via an uncharacterized AMT [163,182,184,185,186,187,188], and subsequent intracellular enzymatic degradation [158,189,206] by monoacylglycerol (MAGL) lipase, similar to other monoacylglycerols [207]. MAGL expression levels are lower during early development and gradually increase throughout development to adulthood [127]. Furthermore, 2-AG is metabolized by enzymatic oxygenation of 2-AG by COX-2 into PGH2 glycerol esters. The biological activity and role of oxygenated 2-AG have yet to be determined. Furthermore, postnatal ethanol treatment did not significantly enhanced 2-AG levels in neonatal brain regions. Taken together, these findings raise an important question of whether AEA and 2-AG may exhibit distinct functions and warrant future studies to understand their specific role during brain development. In our recent studies postnatal ethanol treatment consistently enhanced DAGL-β and MAGL, resulting in no significant change in the 2-AG levels [127]. Although these events are not economical to cells’ overall function, these observations suggest that the enhancement of AEA over 2-AG by postnatal ethanol constitutes an example of the generation of unique cellular responses depending on the environment of the cell.
The molecular distribution of EC metabolism and their receptor systems during brain development suggest that ECs may effectively regulate cellular specification programs [208]. A broad range of developmentally regulated receptors and ion channels [209,210,211] has suggested divergent roles of EC signaling during brain development. AEA and 2-AG levels vary substantially throughout prenatal development [212,213]. In the beginning stages, between days four and six of pregnancy, AEA in the uterus enables embryo implantation [214]. AEA levels are low in the brain at midgestation, and their levels gradually increase throughout the perinatal developmental period until adult levels are reached [212]. Similar to adult brains, 2-AG concentrations (2–8 nmol/g tissue) exceed those of AEA (3–6 pmol/g tissue) throughout brain development [212,213]. Importantly, fetal 2-AG levels are similar to those in young and adult rat brains, with a remarkably distinct peak on the first day after birth [212,213]. It has become increasingly evident that ECs and related lipid mediators regulate neural progenitor commitment, survival [202,215,216] and synaptic connectivity in the developing brain [217,218].
ECs have also been shown to regulate neuronal migration, suggesting a role in specifying the morphological, physiological and molecular characteristics that occur during terminal neuronal differentiation. AEA and WIN552122 and cooperatively with brain-derived neurotrophic factor (BDNF), a principal pro-differentiating neurotrophin, induce migration of GABA-expressing interneurons in the embryonic cortex [219]. Similarly, Δ9-THC increased the density of cholecystokinin-expressing interneurons in the rat hippocampus in vivo [219]. AEA [219] and WIN552122 [220] strongly inhibited neurite formation and elongation in GABA-expressing interneurons. In these studies, AEA abolished the morphogenic potential of BDNF. Similarly, cannabinoids, including Δ9-THC, antagonized forskolin-induced synaptogenesis in cultured hippocampal neurons [221]. In N1E-115 neuroblastoma cells, AEA and HU210 reduced the rates of neurogenic differentiation [222]. These morphological changes were mediated through the Rho family of small guanosine triphosphatases and spatially controlled its activation, which regulated cytoskeletal integrity [223]. In contrast, the synthetic cannabinoid, HU210 promoted neurite outgrowth in Neuro 2A cells via Gαo/i-mediated degradation of Rap–GAPII and the subsequent activation of Rap1 [224]. 2-AG also stimulated neurite outgrowth in cerebellar neurons through a mechanism that was dependent on intrinsic diacylglycerollipase (DAGL) activity within axonal growth cones, whereas CB1 receptor antagonists abolished N-cadherin- and Fgf8-induced neurite extension [225]. These observations indicated that EC signaling might regulate aspects of growth cone differentiation and axon guidance [226]. Further support for the potential role of ECs in the regulation of neuritogenesis was obtained from the similar functional effects of other lipid mediators such as lysophosphatidic acid and sphingosine-1-phosphate [222]. Further research is required to understand the precise molecular events by which ECs regulate dendritic and axonal development. Identification of ECs and the characterization of their metabolic enzymes and second messenger signaling cascades will enable a better understanding of the physiological role of EC signaling and will reveal the neural basis of developmental defects that are imposed by prenatal drug abuse including ethanol.
A Major Role of Cannabinoid Receptors and Their Signaling
Evidence for the existence of a marijuana receptor has been demonstrated since the 1980s [227,228]. It has now been shown that cannabinoids consist of two specific receptor subtypes, known as CB1 and CB2, which have been cloned. Evidence for a third receptor (“CB3” or the “AEA receptor”) in brain and endothelial tissues has been reported in the literature [229,230,231,232]. However, the cloning, expression and characterization of CB3 has not yet been performed.
CB1 and CB2 receptors belong to a large superfamily of heptahelical G protein-coupled receptors (GPCR) and couple to Gi/o proteins (for more details, see reviews [171,233,234]). The CB1 receptor is mainly expressed in the brain and spinal cord and is thus often referred to as the “brain cannabinoid receptor”. CB1 receptors are among the most abundant GPCRs in the brain, and their expression levels are similar to the levels of GABA- and glutamate-gated ion channels [235]. The presence of functional CB2 receptors in the CNS has provoked considerable controversy over the past few years. Formerly considered as an exclusively peripheral receptor [236,237] and often referred to as a “peripheral cannabinoid receptor”, it is now accepted that CB2 is also present in limited amounts and in distinct locations in the brain of several animal species, including humans [238,239]. However, the functional relevance of this receptor in the CNS is emerging slowly [240].
The CB1 receptor displays a wide expression pattern in the developing nervous system and its expression corresponds with neuronal differentiation in the embryo from its earliest stages. Several studies have described the expression pattern of CB1 receptor mRNA and the distribution of CB1 receptors in the fetal and neonatal rat brain [212,241,242,243]. CB1 receptor mRNA levels and receptor binding can be detected from GD 14 in rats, which coincides with the time of phenotypic expression of most neurotransmitters (for review, see [244]). At this fetal age, CB1 receptors appear to be functional because they are already coupled to GTP-binding proteins [241]. The developing human and rat brain contain higher levels of CB1 receptors [245,246] compared to the adult brain [212]. However, the distribution of CB1 receptors is atypical in the fetal and early neonatal brain, particularly in white matter areas [243] and in the subventricular zones of the forebrain [212,241] compared to the adult brain [235,246]. This atypical location of CB1 receptors is a transient phenomenon because the receptors are progressively acquired during the course of late postnatal development, subsequently resulting in the classic pattern of distribution observed in the adult brain [241,243]. The existence of CB1 receptors during early brain development suggests the potential involvement of CB1 receptors during fetal and early postnatal periods in specific events of CNS development, such as cell proliferation and migration, axonal elongation and, subsequently, synaptogenesis and myelinogenesis (for review, see [213]). Thus CB1 receptors contribute to the generation of neuronal diversity in specific brain regions during early brain development.
Activation of a cannabinoid receptor promotes its interaction with G proteins, resulting in guanosine diphosphate/guanosine triphosphate exchange and subsequent dissociation of the α and βγ subunits. These subunits regulate the activity of multiple effector proteins to elicit biological functions. CB1 receptor is coupled with Gi or Go proteins. CB1 receptors differ from many other GPCR proteins in that they are constitutively active because they are pre-coupled with G-proteins in the absence of exogenously added agonists [247]. Among its cellular actions is the inhibition of adenylate cyclase activity [248,249,250], inhibition of N- type voltage-gated channels [251,252,253,254], inhibition of N-type, P/Q-type calcium channels and D-type potassium channels [250,255], activation of A-type and inwardly rectifying potassium channels [256] and inhibition of synaptic transmission [255,257]. On the basis of these findings, it has been suggested that CB1 receptors play a role in the regulation of neurotransmitter release [255,257].
In addition, one of the most interesting research areas is the regulation of neuritogenesis, axonal growth and synaptogenesis by CB1 receptors (for references, see recent article [218]). However, the molecular mechanisms involved in this process are still unclear. The CB1 receptor activates the MAPK pathway [258]. In some cells, CB1 receptor-mediated activation of MAPK was mediated via the PI3 kinase pathway [258,259]. AEA, CP, 55,940 and WIN 55,212-2 increased phosphorylation of focal adhesion kinase (FAK+6,7) a neural isoform of FAK, in hippocampal slices and in cultured neurons [260]. Moreover, CB1 receptor activation stimulated the phosphorylation of the Tyr-397 residue of FAK in the hippocampus, which is crucial for FAK activation [261] and increased phosphorylation of p130-Cas, a protein associated with FAK in the hippocampus. CB1 receptor-stimulated FAK-autophosphorylation was shown to be upstream of the Src family kinases [261]. These new downstream effectors of CB1 receptors are most likely to play a role in some forms of synaptic plasticity via gene regulation; however, further investigation is required.
There is evidence that perinatal exposure to cannabinoids modifies the maturation of neurotransmitter systems and their related behaviors [213,262,263,264,265]. These effects were caused via the activation of CB1 receptors, which emerge early in the developing brain [212,213,241,265]. Activity in the adult brain of a specific neurotransmitter is the result of a temporally ordered sequence of events that occurs during early CNS development. Dysregulation of this pattern may result in alterations in some of the functions related to this neurotransmitter. For example, a disturbance in the expression of the genes implicated in the synthesis of receptors in a very specific moment of development can result in alterations in some of the activities related to the physiological functions of these receptors. These alterations may also be a consequence of an increase or decrease in their concentrations or a modification in the activity of the CB1 receptor signaling pathways. Administration of cannabinoids, at doses similar to those found in marijuana consumers, was found to modify normal neurotransmitter development, which likely produced neurobehavioral disturbances. Thus, adult animals that are perinatally exposed to cannabinoids exhibit, among other symptoms, long-term alterations in male copulatory behavior [266], open-field activity [267], learning ability [268], stress response [269], pain sensitivity [270], social interaction and sexual motivation [271], drug seeking behavior [272], neuroendocrine disturbances [273] among others (for review, see [262,263,264,268]). Furthermore, most of these neurobehavioral effects were originated by changes in the development of several neurotransmitter systems caused by exposure to cannabinoids and most likely through the activation of CB1 receptors during critical prenatal and early postnatal periods of brain development.
During specific periods of development, CB1 receptors might also be expressed in some subpopulations of glial cells, which play an important role in neural development. Cannabinoids induce arachidonic acid mobilization in cortical glial cells, and this effect was reversed by the selective CB1 receptor antagonist, SR141716A [274], suggesting that the CB1 receptor might play a role in neural-glial signaling in the brain. This may result in AEA being released from neuronal cells, which might act on astrocyte function via the activation of CB1 receptor located in these cells. It has been observed that cannabinoid-induced increase in basal and forskolin-inhibited glucose oxidation and phospholipid synthesis was observed in cortical glial cells [275] or C6 glioma cells [276]. These effects were reversed by pertussis toxin or SR141716A, indicating an involvement of a Gi/Go protein-coupled CB1 receptor. These studies also suggested that sphingomyelin hydrolysis and mitogen-activated protein kinase stimulation were also involved in this metabolic effect [275]. Cannabinoids in hippocampal glial cell cultures induced the expression of kros-24, which was reversed by SR141716A [277], suggesting the involvement of CB1 receptors. Similarly, acute administration of Δ9-THC (1–10 mg/kg) markedly enhanced the proapoptotic properties of ethanol in the neonatal rat brain. However, Δ9-THC did not induce neurodegeneration by itself, although neuronal degeneration became disseminated and severe when Δ9-THC was combined with a mildly intoxicating ethanol dose. This Δ9-THC and ethanol dose combination resembled the massive neurodegeneration observed when ethanol was administered alone at much higher doses [278]. In addition, Δ9-THC and co-administration of a low dose of ethanol enhanced CB1 receptor levels without affecting CB2 receptor levels in the thalamus and dorsal subiculum brain regions. The effect of Δ9-THC on neurodegeneration was mimicked by the synthetic cannabinoid WIN 55,212-2 (1–10 mg/kg) and counteracted by the CB1 receptor antagonist SR141716A (0.4 mg/kg). In addition, neonatal CB1 receptor knock-out mice were less susceptible to the neurotoxic effects of a low dose of ethanol. Furthermore, the CB1 receptor antagonist SR141716A ameliorated the neurotoxic effects of ethanol [278].
In our recent studies, we used a higher dose of postnatal ethanol, which induced a massive widespread neurodegeneration in postnatal day 7 mouse brains. In addition to enhanced AEA and associated biosynthetic enzymes, we also found transcriptional activation of the CB1 receptor gene, which results in enhanced levels of CB1 receptor mRNA as well as protein expression in a time-dependent manner in cortical and hippocampal brain regions [111]. Interestingly, we found that postnatal ethanol treatment of mice enhances acetylation of histone (H4) on lysine 8 (H4K8ace) at CB1R exon1, CB1R binding as well as the CB1R agonist-stimulated GTPγS binding in cortical and hippocampal brain regions [110]. Pre-administration of SR141716A or genetic ablation of CB1 receptors (KO) prior to ethanol treatment prevented neurodegeneration [110,111]. Interestingly, the protective effects of CB1R blockade through pharmacological or genetic deletion resulted in normal adult synaptic plasticity and learning and memory including social memory in mice exposed to ethanol at P7. The AEA/CB1R signaling pathway may be directly responsible for the synaptic and memory deficits associated with fetal alcohol spectrum disorders [110,111].
The EC signaling pathway responsible for the specific role during brain development has not been well characterized. The available literature suggests the participation of ERK 1/2 via a mechanism involving the upstream inhibition of Rap1 and B-Raf (for review see [208]). Activation of CB1Rs also prevented the recruitment of new synapses by inhibiting the formation of cAMP [221]. Although the intracellular signaling events involving mitogen-activated protein kinase (MAPK) coupled to the activation of CB1Rs have been shown in embryonic developmental stage [217] and are not known during postnatal development, several studies using cell lines have suggested both up- and downregulation of MAPK in Δ9-THC-mediated apoptosis [279,280]. Moreover, cannabis use during brain development also induced a veriety of deficits that are similar to several specific human developmental disorders [281], and may overlap with, those observed in fetal alcohol syndrome [282], which was likely mediated via the activation of CB1Rs.
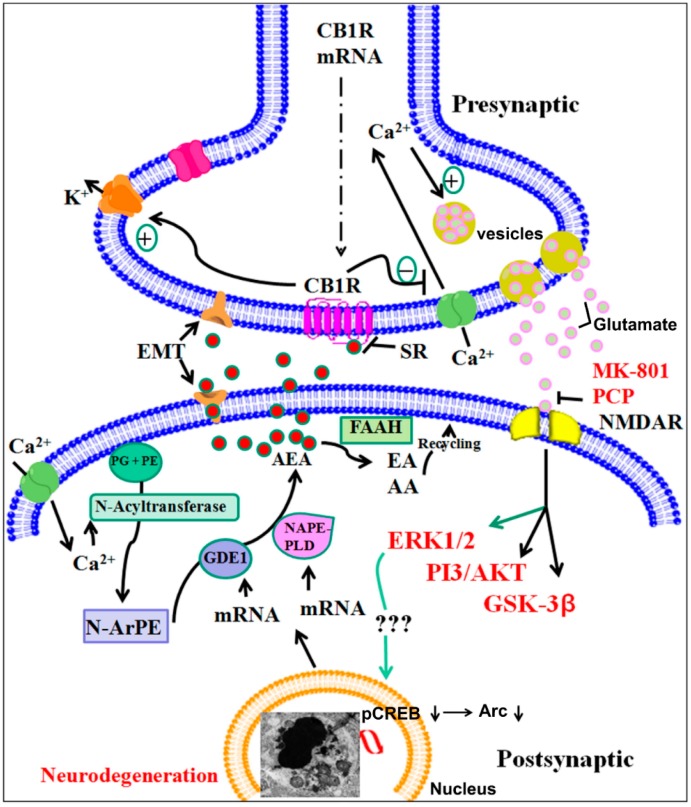
Our recent study demonstrated a specific role of CB1 receptor-mediated ERK1/2, cAMP response element-binding protein (CREB) phosphorylation, AKT and activity-regulated cytoskeleton-associated protein (Arc) expression in postnatal ethanol-induced neurodegeneration. P7 ethanol treatment significantly reduced pERK1/2, pAKT, pCREB and Arc protein levels but not total ERK1/2 or AKT or CREB protein levels in the hippocampus and neocortex. Interestingly, ERK1/2, CREB phosphorylation and Arc expression were rescued by SR pre-treatment. However, AKT phosphorylation was not rescued by SR pre-treatment. Similarly, CB1R KO mice, which did not show ethanol-induced neurodegeneration, provided protection against P7 ethanol-induced inhibition of ERK1/2, pCREB phosphorylation and Arc expression but failed to rescue the inhibition of AKT phosphorylation. Thus, P7 ethanol-activated CB1R-induced neurodegeneration was regulated by the AEA/CB1R/pERK1/2/pCREB/Arc cascade but not by the PI3-kinase/AKT pathway in the developing brain [110,111] (Figure 2).
Figure 2.
A proposed model suggesting that AEA/CB1R/ERK1/2/pCREB/Arc signaling regulates ethanol-induced neurodegeneration, resulting in neurobehavioral deficits in adult mice. P7 ethanol-enhances AEA levels (postsynaptic neuron) through transcriptional activation of NAPE-PLD and GDE1 enzymes. AEA acting through CB1Rs (AEA tone) (presynaptic neuron) may result in decreased glutamate release, which causes N -Methyl-d-aspartate (NMDA) receptor hypofunction, ERK1/2 and cAMP response element-binding protein (CREB) hypophosphorylation deficits in Arc expression and leads to neonatal neurodegeneration (condensed chromatin balls, electron microscopic image). Previous studies have shown that CB1R activation inhibits NMDA receptor function in several experimental models [283,284] and ethanol was shown to inhibit glutamatergic neurotransmission via CB1 receptor activation [285]. These events during postnatal development may disrupt the refinement of neuronal circuits [112,123] and lead to long-lasting deficits in synaptic plasticity and memory in adult animals. The inhibition of CB1Rs (AEA tone) prevents pERK1/2, CREB hypophosphorylation, deficits in Arc expression and neonatal neurodegeneration (Tau and caspase-3 cleavage), which results in normal neurobehavioral function in adult mice. Genetic ablation of the CB1R does not affect NMDA receptor antagonist-induced apoptosis, but does provide protection against ethanol-induced neonatal neurodegeneration, synaptic and memory deficits in adult mice. Thus, the putative AEA/CB1R/pERK1/2/pCREB/Arc signaling mechanism may have a potential regulatory role in neuronal function in the developing brain and may be a valuable therapeutic target for FASD.
During periods of development when the brain experiences a growth spurt, blockade of the NMDA receptor for a few hours has been found to trigger massive and widespread apoptotic neurodegeneration in the rodent brain [286]. NMDA receptor antagonists were the most effective in inducing apoptosis in the rat forebrain at P7. Thus, during this developmental period, the survival of NMDA receptor-expressing neurons was dependent on the glutamatergic input being regulated within narrow time periods [286]. Endocannabinoids and cannabinoids are well known to affect glutamatergic signaling [287,288], and therefore, ethanol-induced endocannabinoids [111,285] or cannabinoid-induced alterations in glutamate levels [289,290,291] might contribute to neonatal neurodegeneration or lasting behavioral deficits [111,112,123] observed after binge-like ethanol exposure during this specific vulnerable period of brain development. Furthermore, pharmacological blockade or genetic deletion of CB1 receptors removed the endocannabinoid-mediated inhibition of glutamate release by ethanol, resulting in a lack of ethanol-induced neurodegeneration (Figure 2). Thus, CB1 receptors served as good candidate targets for modulating NMDA receptor function in developmental disorders. Interestingly, NMDA receptor antagonists were able to induce apoptotic neurodegeneration in CB1 receptor KO mice [111], further strengthening the mechanism by which postnatal ethanol exerts its deleterious effects in the developing brain (Figure 2). Findings obtained from neonatal rats suggested that ethanol might actually affect CA3 pyramidal neurons via inhibition of postsynaptic amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid receptor (AMPARs), which result in a decrease in glutamatergic release [292]. Moreover, this study was consistent with the study conducted by Twitchell et al. in 1997 in which exogenous cannabinoids inhibited glutamatergic release by activating CB1R-mediated inhibition of N-type and P/Q-type calcium channels [283] and might be responsible for the enhanced susceptibility of the immature brain to ethanol neurotoxicity [278] and long-lasting learning and memory deficits [108,109,110,111,112,293].
While the molecular mechanism is still unclear, ethanol treatment during early brain development caused deficits in synaptic function [294], which persisted into adulthood [108,109,110,111,112,293]. It is also possible that ethanol-enhanced AEA-CB1 receptor tone disrupts the refinement of neuronal circuits, leading to persistent synaptic dysfunction. This could explain why some cortical maps [295,296,297,298] and olfacto-hippocampal networks [112,123] are altered in FASD models. Consistent with this notion, pre-administration of CB1 receptor antagonist (SR141716A) completely rescued the P7 ethanol-induced defects in the LTP magnitude of field excitatory postsynaptic currents (fEPSPs), both in the initial induction and maintenance. Interestingly, the genetic deletion of CB1 receptors provided complete protection against P7 ethanol-induced defects in LTP. However, CB1R KO mice exhibited an enhanced LTP magnitude compared to WT or normal C57BL/6J saline-treated mice [109,110,111] as observed in other studies [299,300]. In addition, ethanol treatment at P7 impaired object recognition, spatial and social interaction memory performance and was rescued in mice treated with SR [109,110,111]. P7 ethanol administration showed no significant effects on adult CB1R WT or KO mice exploration times in the object recognition memory (ORM) task. Because deletion of CB1 receptors has been shown to enhance their ability to perform better on a learning task [300], we found enhanced object recognition performance and spatial memory in CB1 receptor KO mice compared to WT mice. Furthermore, CB1 receptor KO mice provided protection against P7 ethanol-induced deficits in object recognition memory performance, spatial memory and social interaction memory as observed in LTP. Therefore, suppression of CB1 receptor function via pharmacological blockade or genetic deletion of CB1 receptors prior to postnatal ethanol exposure prevented synaptic and memory deficits in adult mice. Taken together, these findings emphasize the importance of this mechanism in the understanding and development of therapeutic strategies used to treat FASD.
It is also possible that activation of CB1 receptors during the critical period of brain development can affect both the glutamatergic system and the development of multiple neurotransmitter systems, including the catecholaminergic, serotonergic, GABAergic and opioid systems [213,301,302], resulting in an altered hippocampal circuit and long-term behavioral deficits [303] (Table 2). Activation of CB1 receptors during postnatal development, although less well investigated, may also result in long-term behavioral deficits [304] mediated through NMDA receptor function [111]. However, further research is required to establish the effect of CB1 receptor activation during brain development on the function of multiple neurotransmitter systems, which may cause lasting morphological changes underlying the synaptic and memory deficits.
Table 2.
Summary of Long-lasting behavioral abnormalities found in animals as consequences of cannabinoid exposure and CB1 receptor activation during brain development.
| Cannabinoid Exposure | References | |
|---|---|---|
| Learning and memory | Learning deficits in the Morris water maze. | [305] |
| Impairment in the inhibitory avoidance test and impaired olfactory short-term memory in the social discrimination task. | [306] | |
| Poorer performance in homing behavior and impaired active avoidance performance. | [307] | |
| Disruption of memory retention in the passive avoidance task. | [308] | |
| Reduced novel object recognition. | [309,310] | |
| Impaired working memory on Y maze. | [311] | |
| Reduced social interaction. | [309,310] |
2. Conclusions
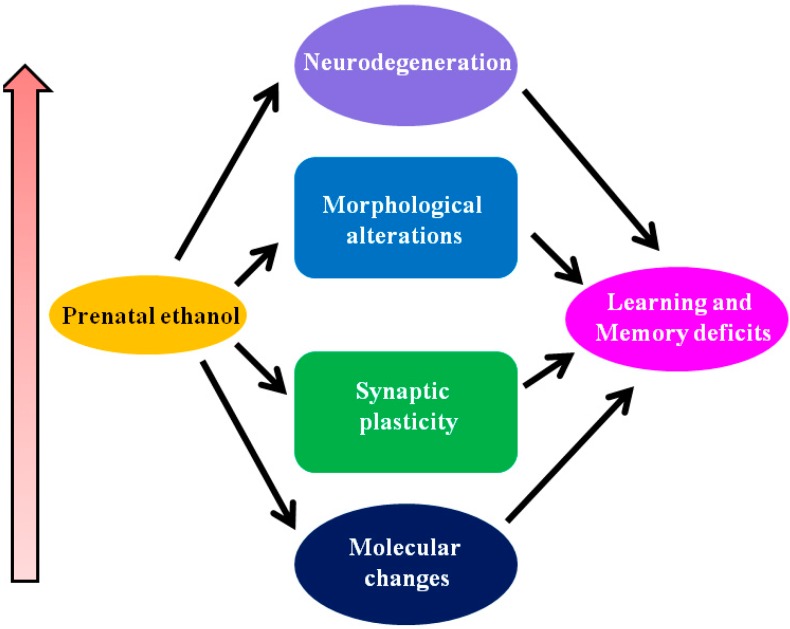
In summary, several molecular mechanisms are expected to contribute to the damaging effects of prenatal alcohol exposure on the developing fetus. These events including endocannabinoid mechanisms contribute to impaired development and function of neuronal communication and circuit formation. These alcohol-induced deficits result in long-lasting abnormalities in neuronal plasticity and learning and memory and can explain many of the neurobehavioral abnormalities found in FASD (Figure 3). The physiological role of the EC system during early brain development has not yet been fully elucidated. The search for additional functions is underway, and the strategies used to identify them are improving. However, there is not sufficient attention focused in this direction. Modulation of this system using pharmacological and gene knockout approaches support a role for the EC system in learning and memory, emotion and anxiety, reward, eating, nociception and motor systems, among others; however, none of these behavioral responses are critically dependent on the veracity of the EC system, indicating that it functions in a modulatory or facilitatory manner, thus making it a highly attractive target for the development of therapeutic agents to treat FASD.
Figure 3.
Molecular events leading to loss of learning and memory as found in FASD. Depending on the developmental stage, pattern, concentration and duration of prenatal ethanol exposure can lead to molecular alterations (for example, activity of growth factors, changes in the regulation of gene expression, changes in adhesion, changes in endocannabinoid system) and impaired in neuronal communication and circuit formation. These events may lead to several transient and permanent changes in the hippocampus, including molecular changes, modifications in synaptic plasticity, morphological changes and neuronal loss. These prenatal ethanol-associated changes in the brain can potentially induce deficits in learning-and-memory processes found in the adult animals of FASD.
Acknowledgments
This work was supported by NIH/NIAAA grant AA019443.
Abbreviations
CB1, cannabinoid receptor type 1; EC, endocannabinoid; FAS, fetal alcohol syndrome; FASD, fetal alcohol spectrum disorder; BAC, blood alcohol concentration; ADHD, attention deficit hyperactivity disorder; miRNAs, microRNAs; NCAM, neural cell adhesion molecule; GABAA, gamma-amino butyric acid-A receptor; MAPK, mitogen-activated protein kinase; Δ9-THC, delta-9-tetrahydrocannabinol; AEA, arachidonylethanolamide (anandamide); 2-AG, 2-arachidonylglycerol; NADA, N-arachidonyl-dopamine; VR1, vanilloid receptor type 1; NAPE-PLD, N-acylphosphatidylethanolamine-specific phospholipase D; GDE1, glycerophosphodiesterase; ABHD4, abhydrolase domain 4; PTPN22, phosphatase; AMT, AEA membrane transporter; FAAH, fatty acid amide hydrolase; COX, cyclooxygenase; LOX, lipoxygenase; MAGL, monoacylglycerol lipase; PGH2, prostaglandin H2; BDNF, brain-derived neurotrophic factor; DAGL, diacylglycerollipase; FAK, focal adhesion kinase; AMPAR, α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid receptor; fEPSCs, field excitatory postsynaptic currents; GPCR, G protein coupled receptor; NAT, N-acyltransferase; N-ArPE, N-arachidonyl phosphatidylethanolamine; NMDA, N-methyl-d-aspartate.
Conflict of Interest
The authors declare no conflict of interest.
References
- 1.Jones K.L., Smith D.W., Ulleland C.N., Streissguth P. Pattern of malformation in offspring of chronic alcoholic mothers. Lancet. 1973;1:1267–1271. doi: 10.1016/S0140-6736(73)91291-9. [DOI] [PubMed] [Google Scholar]
- 2.Jones K.L., Smith D.W. Recognition of the fetal alcohol syndrome in early infancy. Lancet. 1973;2:999–1001. doi: 10.1016/S0140-6736(73)91092-1. [DOI] [PubMed] [Google Scholar]
- 3.Alati R., al Mamun A., Williams G.M., O’Callaghan M., Najman J.M., Bor W. In utero alcohol exposure and prediction of alcohol disorders in early adulthood: A birth cohort study. Arch. Gen. Psychiatry. 2006;63:1009–1016. doi: 10.1001/archpsyc.63.9.1009. [DOI] [PubMed] [Google Scholar]
- 4.Autti-Ramo I., Fagerlund A., Ervalahti N., Loimu L., Korkman M., Hoyme H.E. Fetal alcohol spectrum disorders in Finland: Clinical delineation of 77 older children and adolescents. Am. J. Med. Genet. Part A. 2006;140:137–143. doi: 10.1002/ajmg.a.31037. [DOI] [PubMed] [Google Scholar]
- 5.Ceccanti M., Alessandra Spagnolo P., Tarani L., Luisa Attilia M., Chessa L., Mancinelli R., Stegagno M., Francesco Sasso G., Romeo M., Jones K.L., et al. Clinical delineation of fetal alcohol spectrum disorders (FASD) in Italian children: Comparison and contrast with other racial/ethnic groups and implications for diagnosis and prevention. Neurosci. Biobehav. Rev. 2007;31:270–277. doi: 10.1016/j.neubiorev.2006.06.024. [DOI] [PubMed] [Google Scholar]
- 6.Spohr H.L., Willms J., Steinhausen H.C. Fetal alcohol spectrum disorders in young adulthood. J. Pediatr. 2007;150:175–179. doi: 10.1016/j.jpeds.2006.11.044. [DOI] [PubMed] [Google Scholar]
- 7.Streissguth A.P., Aase J.M., Clarren S.K., Randels S.P., LaDue R.A., Smith D.F. Fetal alcohol syndrome in adolescents and adults. JAMA. 1991;265:1961–1967. doi: 10.1001/jama.1991.03460150065025. [DOI] [PubMed] [Google Scholar]
- 8.Sokol R.J., Delaney-Black V., Nordstrom B. Fetal alcohol spectrum disorder. JAMA. 2003;290:2996–2999. doi: 10.1001/jama.290.22.2996. [DOI] [PubMed] [Google Scholar]
- 9.Burd L., Klug M.G., Martsolf J.T., Kerbeshian J. Fetal alcohol syndrome: Neuropsychiatric phenomics. Neurotoxicol. Teratol. 2003;25:697–705. doi: 10.1016/j.ntt.2003.07.014. [DOI] [PubMed] [Google Scholar]
- 10.Mattson S.N., Crocker N., Nguyen T.T. Fetal alcohol spectrum disorders: Neuropsychological and behavioral features. Neuropsychol. Rev. 2011;21:81–101. doi: 10.1007/s11065-011-9167-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mattson S.N., Riley E.P. A review of the neurobehavioral deficits in children with fetal alcohol syndrome or prenatal exposure to alcohol. Alcohol. Clin. Exp. Res. 1998;22:279–294. doi: 10.1111/j.1530-0277.1998.tb03651.x. [DOI] [PubMed] [Google Scholar]
- 12.Mattson S.N., Riley E.P., Gramling L., Delis D.C., Jones K.L. Neuropsychological comparison of alcohol-exposed children with or without physical features of fetal alcohol syndrome. Neuropsychology. 1998;12:146–153. doi: 10.1037/0894-4105.12.1.146. [DOI] [PubMed] [Google Scholar]
- 13.Goodman A.M., Delis D.C., Mattson S.N. Normative data for 4-year-old children on the California Verbal Learning Test-Children’s Version. Clin. Neuropsychol. 1999;13:274–282. doi: 10.1076/clin.13.3.274.1748. [DOI] [PubMed] [Google Scholar]
- 14.Mattson S.N., Goodman A.M., Caine C., Delis D.C., Riley E.P. Executive functioning in children with heavy prenatal alcohol exposure. Alcohol. Clin. Exp. Res. 1999;23:1808–1815. doi: 10.1111/j.1530-0277.1999.tb04077.x. [DOI] [PubMed] [Google Scholar]
- 15.Sood B., Delaney-Black V., Covington C., Nordstrom-Klee B., Ager J., Templin T., Janisse J., Martier S., Sokol R.J. Prenatal alcohol exposure and childhood behavior at age 6 to 7 years: I. dose-response effect. Pediatrics. 2001;108:E34. doi: 10.1542/peds.108.2.e34. [DOI] [PubMed] [Google Scholar]
- 16.Streissguth A.P., Bookstein F.L., Sampson P.D., Barr H.M. Neurobehavioral effects of prenatal alcohol: Part III. PLS analyses of neuropsychologic tests. Neurotoxicol. Teratol. 1989;11:493–507. doi: 10.1016/0892-0362(89)90026-3. [DOI] [PubMed] [Google Scholar]
- 17.Bailey B.N., Delaney-Black V., Covington C.Y., Ager J., Janisse J., Hannigan J.H., Sokol R.J. Prenatal exposure to binge drinking and cognitive and behavioral outcomes at age 7 years. Am. J. Obstet. Gynecol. 2004;191:1037–1043. doi: 10.1016/j.ajog.2004.05.048. [DOI] [PubMed] [Google Scholar]
- 18.Bonthius D.J., Goodlett C.R., West J.R. Blood alcohol concentration and severity of microencephaly in neonatal rats depend on the pattern of alcohol administration. Alcohol. 1988;5:209–214. doi: 10.1016/0741-8329(88)90054-7. [DOI] [PubMed] [Google Scholar]
- 19.Guerri C., Bazinet A., Riley E.P. Foetal Alcohol Spectrum Disorders and alterations in brain and behaviour. Alcohol Alcohol. 2009;44:108–114. doi: 10.1093/alcalc/agn105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.May P.A., Gossage J.P., Kalberg W.O., Robinson L.K., Buckley D., Manning M., Hoyme H.E. Prevalence and epidemiologic characteristics of FASD from various research methods with an emphasis on recent in-school studies. Dev. Disabil. Res. Rev. 2009;15:176–192. doi: 10.1002/ddrr.68. [DOI] [PubMed] [Google Scholar]
- 21.Bertrand J., Floyd R.L., Weber M.K., O’Connor M., Riley E.P., Johnson K.A., Cohen D.E. Fetal Alcohol Syndrome: Guidelines for Referral and Diagnosis. Centers for Disease Control and Prevention; Atlanta, GA, USA: 2004. [Google Scholar]
- 22.Dalen K., Bruaroy S., Wentzel-Larsen T., Laegreid L.M. Cognitive functioning in children prenatally exposed to alcohol and psychotropic drugs. Neuropediatrics. 2009;40:162–167. doi: 10.1055/s-0029-1243176. [DOI] [PubMed] [Google Scholar]
- 23.Mattson S.N., Riley E.P., Gramling L., Delis D.C., Jones K.L. Heavy prenatal alcohol exposure with or without physical features of fetal alcohol syndrome leads to IQ deficits. J. Pediatr. 1997;131:718–721. doi: 10.1016/S0022-3476(97)70099-4. [DOI] [PubMed] [Google Scholar]
- 24.Alati R., Clavarino A., Najman J.M., O’Callaghan M., Bor W., Mamun A.A., Williams G.M. The developmental origin of adolescent alcohol use: Findings from the Mater University Study of Pregnancy and its outcomes. Drug Alcohol Depend. 2008;98:136–143. doi: 10.1016/j.drugalcdep.2008.05.011. [DOI] [PubMed] [Google Scholar]
- 25.Fried P.A., Watkinson B. 12- and 24-month neurobehavioural follow-up of children prenatally exposed to marihuana, cigarettes and alcohol. Neurotoxicol. Teratol. 1988;10:305–313. doi: 10.1016/0892-0362(88)90032-3. [DOI] [PubMed] [Google Scholar]
- 26.Streissguth A.P., Barr H.M., Sampson P.D. Moderate prenatal alcohol exposure: Effects on child IQ and learning problems at age 7 1/2 years. Alcohol. Clin. Exp. Res. 1990;14:662–669. doi: 10.1111/j.1530-0277.1990.tb01224.x. [DOI] [PubMed] [Google Scholar]
- 27.Willford J.A., Leech S.L., Day N.L. Moderate prenatal alcohol exposure and cognitive status of children at age 10. Alcoholism. 2006;30:1051–1059. doi: 10.1111/j.1530-0277.2006.00119.x. [DOI] [PubMed] [Google Scholar]
- 28.Chasnoff I.J., Wells A.M., Telford E., Schmidt C., Messer G. Neurodevelopmental functioning in children with FAS, pFAS, and ARND. J. Dev. Behav. Pediatr. 2010;31:192–201. doi: 10.1097/DBP.0b013e3181d5a4e2. [DOI] [PubMed] [Google Scholar]
- 29.Aragon A.S., Kalberg W.O., Buckley D., Barela-Scott L.M., Tabachnick B.G., May P.A. Neuropsychological study of FASD in a sample of American Indian children: Processing simple versus complex information. Alcohol. Clin. Exp. Res. 2008;32:2136–2148. doi: 10.1111/j.1530-0277.2008.00802.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Green C.R., Mihic A.M., Nikkel S.M., Stade B.C., Rasmussen C., Munoz D.P., Reynolds J.N. Executive function deficits in children with fetal alcohol spectrum disorders (FASD) measured using the Cambridge Neuropsychological Tests Automated Battery (CANTAB) J. Child Psychol. Psychiatry. 2009;50:688–697. doi: 10.1111/j.1469-7610.2008.01990.x. [DOI] [PubMed] [Google Scholar]
- 31.Kodituwakku P.W., Adnams C.M., Hay A., Kitching A.E., Burger E., Kalberg W.O., Viljoen D.L., May P.A. Letter and category fluency in children with fetal alcohol syndrome from a community in South Africa. J. Stud. Alcohol. 2006;67:502–509. doi: 10.15288/jsa.2006.67.502. [DOI] [PubMed] [Google Scholar]
- 32.Kodituwakku P.W., Handmaker N.S., Cutler S.K., Weathersby E.K., Handmaker S.D. Specific impairments in self-regulation in children exposed to alcohol prenatally. Alcohol. Clin. Exp. Res. 1995;19:1558–1564. doi: 10.1111/j.1530-0277.1995.tb01024.x. [DOI] [PubMed] [Google Scholar]
- 33.Schonfeld A.M., Mattson S.N., Lang A.R., Delis D.C., Riley E.P. Verbal and nonverbal fluency in children with heavy prenatal alcohol exposure. J. Stud. Alcohol. 2001;62:239–246. doi: 10.15288/jsa.2001.62.239. [DOI] [PubMed] [Google Scholar]
- 34.Vaurio L., Riley E.P., Mattson S.N. Differences in executive functioning in children with heavy prenatal alcohol exposure or attention-deficit/hyperactivity disorder. J. Int. Neuropsychol. Soc. 2008;14:119–129. doi: 10.1017/S1355617708080144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mattson S.N., Riley E.P., Delis D.C., Stern C., Jones K.L. Verbal learning and memory in children with fetal alcohol syndrome. Alcohol. Clin. Exp. Res. 1996;20:810–816. doi: 10.1111/j.1530-0277.1996.tb05256.x. [DOI] [PubMed] [Google Scholar]
- 36.Mattson S.N., Roebuck T.M. Acquisition and retention of verbal and nonverbal information in children with heavy prenatal alcohol exposure. Alcohol. Clin. Exp. Res. 2002;26:875–882. doi: 10.1111/j.1530-0277.2002.tb02617.x. [DOI] [PubMed] [Google Scholar]
- 37.Roebuck-Spencer T.M., Mattson S.N. Implicit strategy affects learning in children with heavy prenatal alcohol exposure. Alcohol. Clin. Exp. Res. 2004;28:1424–1431. doi: 10.1097/01.ALC.0000139826.25247.5B. [DOI] [PubMed] [Google Scholar]
- 38.Willford J.A., Richardson G.A., Leech S.L., Day N.L. Verbal and visuospatial learning and memory function in children with moderate prenatal alcohol exposure. Alcohol. Clin. Exp. Res. 2004;28:497–507. doi: 10.1097/01.ALC.0000117868.97486.2D. [DOI] [PubMed] [Google Scholar]
- 39.Kaemingk K.L., Mulvaney S., Halverson P.T. Learning following prenatal alcohol exposure: Performance on verbal and visual multitrial tasks. Arch. Clin. Neuropsychol. 2003;18:33–47. doi: 10.1093/arclin/18.1.33. [DOI] [PubMed] [Google Scholar]
- 40.Willoughby K.A., Sheard E.D., Nash K., Rovet J. Effects of prenatal alcohol exposure on hippocampal volume, verbal learning, and verbal and spatial recall in late childhood. J. Int. Neuropsychol. Soc. 2008;14:1022–1033. doi: 10.1017/S1355617708081368. [DOI] [PubMed] [Google Scholar]
- 41.Hamilton D.A., Kodituwakku P., Sutherland R.J., Savage D.D. Children with Fetal Alcohol Syndrome are impaired at place learning but not cued-navigation in a virtual Morris water task. Behav. Brain Res. 2003;143:85–94. doi: 10.1016/S0166-4328(03)00028-7. [DOI] [PubMed] [Google Scholar]
- 42.Kaemingk K.L., Halverson P.T. Spatial memory following prenatal alcohol exposure: More than a material specific memory deficit. Child Neuropsychol. 2000;6:115–128. doi: 10.1076/chin.6.2.115.7058. [DOI] [PubMed] [Google Scholar]
- 43.Rasmussen C., Horne K., Witol A. Neurobehavioral functioning in children with fetal alcohol spectrum disorder. Child Neuropsychol. 2006;12:453–468. doi: 10.1080/09297040600646854. [DOI] [PubMed] [Google Scholar]
- 44.Uecker A., Nadel L. Spatial but not object memory impairments in children with fetal alcohol syndrome. Am. J. Ment. Retard. 1998;103:12–18. doi: 10.1352/0895-8017(1998)103<0012:SBNOMI>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 45.Aronson M., Hagberg B. Neuropsychological disorders in children exposed to alcohol during pregnancy: A follow-up study of 24 children to alcoholic mothers in Goteborg, Sweden. Alcohol. Clin. Exp. Res. 1998;22:321–324. doi: 10.1111/j.1530-0277.1998.tb03655.x. [DOI] [PubMed] [Google Scholar]
- 46.Chiodo L.M., Janisse J., Delaney-Black V., Sokol R.J., Hannigan J.H. A metric of maternal prenatal risk drinking predicts neurobehavioral outcomes in preschool children. Alcohol. Clin. Exp. Res. 2009;33:634–644. doi: 10.1111/j.1530-0277.2008.00878.x. [DOI] [PubMed] [Google Scholar]
- 47.Conry J. Neuropsychological deficits in fetal alcohol syndrome and fetal alcohol effects. Alcohol. Clin. Exp. Res. 1990;14:650–655. doi: 10.1111/j.1530-0277.1990.tb01222.x. [DOI] [PubMed] [Google Scholar]
- 48.Janzen L.A., Nanson J.L., Block G.W. Neuropsychological evaluation of preschoolers with fetal alcohol syndrome. Neurotoxicol. Teratol. 1995;17:273–279. doi: 10.1016/0892-0362(94)00063-J. [DOI] [PubMed] [Google Scholar]
- 49.Simmons R.W., Thomas J.D., Levy S.S., Riley E.P. Motor response programming and movement time in children with heavy prenatal alcohol exposure. Alcohol. 2010;44:371–378. doi: 10.1016/j.alcohol.2010.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Simmons R.W., Wass T., Thomas J.D., Riley E.P. Fractionated simple and choice reaction time in children with prenatal exposure to alcohol. Alcohol. Clin. Exp. Res. 2002;26:1412–1419. doi: 10.1111/j.1530-0277.2002.tb02686.x. [DOI] [PubMed] [Google Scholar]
- 51.Wass T.S., Simmons R.W., Thomas J.D., Riley E.P. Timing accuracy and variability in children with prenatal exposure to alcohol. Alcohol. Clin. Exp. Res. 2002;26:1887–1896. doi: 10.1111/j.1530-0277.2002.tb02497.x. [DOI] [PubMed] [Google Scholar]
- 52.Mattson S.N., Roesch S.C., Fagerlund A., Autti-Ramo I., Jones K.L., May P.A., Adnams C.M., Konovalova V., Riley E.P. Collaborative Initiative on Fetal Alcohol Spectrum Disorders (CIFASD). Toward a neurobehavioral profile of fetal alcohol spectrum disorders. Alcohol. Clin. Exp. Res. 2010;34:1640–1650. doi: 10.1111/j.1530-0277.2010.01250.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Aragon A.S., Coriale G., Fiorentino D., Kalberg W.O., Buckley D., Gossage J.P., Ceccanti M., Mitchell E.R., May P.A. Neuropsychological characteristics of Italian children with fetal alcohol spectrum disorders. Alcohol. Clin. Exp. Res. 2008;32:1909–1919. doi: 10.1111/j.1530-0277.2008.00775.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Brown R.T., Coles C.D., Smith I.E., Platzman K.A., Silverstein J., Erickson S., Falek A. Effects of prenatal alcohol exposure at school age. II. Attention and behavior. Neurotoxicol. Teratol. 1991;13:369–376. doi: 10.1016/0892-0362(91)90085-B. [DOI] [PubMed] [Google Scholar]
- 55.Burden M.J., Jacobson S.W., Sokol R.J., Jacobson J.L. Effects of prenatal alcohol exposure on attention and working memory at 7.5 years of age. Alcohol. Clin. Exp. Res. 2005;29:443–452. doi: 10.1097/01.ALC.0000156125.50577.EC. [DOI] [PubMed] [Google Scholar]
- 56.Burden M.J., Mitchell D.B. Implicit memory development in school-aged children with attention deficit hyperactivity disorder (ADHD): Conceptual priming deficit? Dev. Neuropsychol. 2005;28:779–807. doi: 10.1207/s15326942dn2803_3. [DOI] [PubMed] [Google Scholar]
- 57.Jacobson S.W., Jacobson J.L., Sokol R.J. Effects of fetal alcohol exposure on infant reaction time. Alcohol. Clin. Exp. Res. 1994;18:1125–1132. doi: 10.1111/j.1530-0277.1994.tb00092.x. [DOI] [PubMed] [Google Scholar]
- 58.Jacobson S.W., Jacobson J.L., Sokol R.J., Martier S.S., Ager J.W. Prenatal alcohol exposure and infant information processing ability. Child Dev. 1993;64:1706–1721. doi: 10.2307/1131464. [DOI] [PubMed] [Google Scholar]
- 59.Nash K., Rovet J., Greenbaum R., Fantus E., Nulman I., Koren G. Identifying the behavioural phenotype in Fetal Alcohol Spectrum Disorder: Sensitivity, specificity and screening potential. Arch. N.A. Ment. Health. 2006;9:181–186. doi: 10.1007/s00737-006-0130-3. [DOI] [PubMed] [Google Scholar]
- 60.Streissguth A.P., Sampson P.D., Olson H.C., Bookstein F.L., Barr H.M., Scott M., Feldman J., Mirsky A.F. Maternal drinking during pregnancy: Attention and short-term memory in 14-year-old offspring—A longitudinal prospective study. Alcohol. Clin. Exp. Res. 1994;18:202–218. doi: 10.1111/j.1530-0277.1994.tb00904.x. [DOI] [PubMed] [Google Scholar]
- 61.Howell K.K., Lynch M.E., Platzman K.A., Smith G.H., Coles C.D. Prenatal alcohol exposure and ability, academic achievement, and school functioning in adolescence: A longitudinal follow-up. J. Pediatr. Psychol. 2006;31:116–126. doi: 10.1093/jpepsy/jsj029. [DOI] [PubMed] [Google Scholar]
- 62.Coles C.D., Platzman K.A., Lynch M.E., Freides D. Auditory and visual sustained attention in adolescents prenatally exposed to alcohol. Alcohol. Clin. Exp. Res. 2002;26:263–271. doi: 10.1111/j.1530-0277.2002.tb02533.x. [DOI] [PubMed] [Google Scholar]
- 63.Mattson S.N., Calarco K.E., Lang A.R. Focused and shifting attention in children with heavy prenatal alcohol exposure. Neuropsychology. 2006;20:361–369. doi: 10.1037/0894-4105.20.3.361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Fryer S.L., McGee C.L., Matt G.E., Riley E.P., Mattson S.N. Evaluation of psychopathological conditions in children with heavy prenatal alcohol exposure. Pediatrics. 2007;119:e733–e741. doi: 10.1542/peds.2006-1606. [DOI] [PubMed] [Google Scholar]
- 65.Cummings J.L. Frontal-subcortical circuits and human behavior. Arch. Neurol. 1993;50:873–880. doi: 10.1001/archneur.1993.00540080076020. [DOI] [PubMed] [Google Scholar]
- 66.Fryer S.L., Tapert S.F., Mattson S.N., Paulus M.P., Spadoni A.D., Riley E.P. Prenatal alcohol exposure affects frontal-striatal BOLD response during inhibitory control. Alcohol. Clin. Exp. Res. 2007;31:1415–1424. doi: 10.1111/j.1530-0277.2007.00443.x. [DOI] [PubMed] [Google Scholar]
- 67.Mattson S.N., Riley E.P., Sowell E.R., Jernigan T.L., Sobel D.F., Jones K.L. A decrease in the size of the basal ganglia in children with fetal alcohol syndrome. Alcohol. Clin. Exp. Res. 1996;20:1088–1093. doi: 10.1111/j.1530-0277.1996.tb01951.x. [DOI] [PubMed] [Google Scholar]
- 68.McGee C.L., Fryer S.L., Bjorkquist O.A., Mattson S.N., Riley E.P. Deficits in social problem solving in adolescents with prenatal exposure to alcohol. Am. J. Drug Alcohol. Abuse. 2008;34:423–431. doi: 10.1080/00952990802122630. [DOI] [PubMed] [Google Scholar]
- 69.Schonfeld A.M., Mattson S.N., Riley E.P. Moral maturity and delinquency after prenatal alcohol exposure. J. Stud. Alcohol. 2005;66:545–554. doi: 10.15288/jsa.2005.66.545. [DOI] [PubMed] [Google Scholar]
- 70.Timler G.R., Olswang L.B. Variable structure/variable performance: Parent and teacher perspectives on a school-age child with FAS. J. Posit. Behav. Interv. 2001;3:48–56. doi: 10.1177/109830070100300107. [DOI] [Google Scholar]
- 71.Timler G.R., Olswang L.B., Coggins T.E. “Do I know what I need to do?” A social communication intervention for children with complex clinical profiles. Lang. Speech Hear. Serv. Sch. 2005;36:73–85. doi: 10.1044/0161-1461(2005/007). [DOI] [PubMed] [Google Scholar]
- 72.Newmann F., Wehlage G., Lamborn S. The significance and sources of student engagement. In: Newman F., editor. Student Engagement and Achievement in American Secondary Schools. Teachers College Press; New York, NY, USA: 1992. pp. 11–39. [Google Scholar]
- 73.Floyd R.L., Weber M.K., Denny C., O’Connor M.J. Prevention of fetal alcohol spectrum disorders. Dev. Disabil. Res. Rev. 2009;15:193–199. doi: 10.1002/ddrr.75. [DOI] [PubMed] [Google Scholar]
- 74.O’Connor M.J., Paley B. Psychiatric conditions associated with prenatal alcohol exposure. Dev. Disabil. Res. Rev. 2009;15:225–234. doi: 10.1002/ddrr.74. [DOI] [PubMed] [Google Scholar]
- 75.Paley B., O’Connor M.J. Intervention for individuals with fetal alcohol spectrum disorders: Treatment approaches and case management. Dev. Disabil. Res. Rev. 2009;15:258–267. doi: 10.1002/ddrr.67. [DOI] [PubMed] [Google Scholar]
- 76.Abdollah S., Catlin M.C., Brien J.F. Ethanol neuro-behavioural teratogenesis in the guinea pig: Behavioural dysfunction and hippocampal morphologic change. Can. J. Physiol. Pharmacol. 1993;71:776–782. doi: 10.1139/y93-116. [DOI] [PubMed] [Google Scholar]
- 77.Butters N.S., Gibson M.A., Reynolds J.N., Brien J.F. Effects of chronic prenatal ethanol exposure on hippocampal glutamate release in the postnatal guinea pig. Alcohol. 2000;21:1–9. doi: 10.1016/S0741-8329(99)00096-8. [DOI] [PubMed] [Google Scholar]
- 78.Christie B.R., Swann S.E., Fox C.J., Froc D., Lieblich S.E., Redila V., Webber A. Voluntary exercise rescues deficits in spatial memory and long-term potentiation in prenatal ethanol-exposed male rats. Eur. J. Neurosci. 2005;21:1719–1726. doi: 10.1111/j.1460-9568.2005.04004.x. [DOI] [PubMed] [Google Scholar]
- 79.Driscoll C.D., Streissguth A.P., Riley E.P. Prenatal alcohol exposure: Comparability of effects in humans and animal models. Neurotoxicol. Teratol. 1990;12:231–237. doi: 10.1016/0892-0362(90)90094-S. [DOI] [PubMed] [Google Scholar]
- 80.Iqbal U., Rikhy S., Dringenberg H.C., Brien J.F., Reynolds J.N. Spatial learning deficits induced by chronic prenatal ethanol exposure can be overcome by non-spatial pre-training. Neurotoxicol. Teratol. 2006;28:333–341. doi: 10.1016/j.ntt.2006.01.011. [DOI] [PubMed] [Google Scholar]
- 81.Johnson T.B., Goodlett C.R. Selective and enduring deficits in spatial learning after limited neonatal binge alcohol exposure in male rats. Alcohol. Clin. Exp. Res. 2002;26:83–93. doi: 10.1111/j.1530-0277.2002.tb02435.x. [DOI] [PubMed] [Google Scholar]
- 82.Reyes E., Wolfe J., Savage D.D. The effects of prenatal alcohol exposure on radial arm maze performance in adult rats. Physiol. Behav. 1989;46:45–48. doi: 10.1016/0031-9384(89)90319-3. [DOI] [PubMed] [Google Scholar]
- 83.Richardson D.P., Byrnes M.L., Brien J.F., Reynolds J.N., Dringenberg H.C. Impaired acquisition in the water maze and hippocampal long-term potentiation after chronic prenatal ethanol exposure in the guinea-pig. Eur. J. Neurosci. 2002;16:1593–1598. doi: 10.1046/j.1460-9568.2002.02214.x. [DOI] [PubMed] [Google Scholar]
- 84.Savage D.D., Becher M., de la Torre A.J., Sutherland R.J. Dose-dependent effects of prenatal ethanol exposure on synaptic plasticity and learning in mature offspring. Alcohol. Clin. Exp. Res. 2002;26:1752–1758. doi: 10.1111/j.1530-0277.2002.tb02480.x. [DOI] [PubMed] [Google Scholar]
- 85.Sutherland R.J., McDonald R.J., Savage D.D. Prenatal exposure to moderate levels of ethanol can have long-lasting effects on hippocampal synaptic plasticity in adult offspring. Hippocampus. 1997;7:232–238. doi: 10.1002/(SICI)1098-1063(1997)7:2<232::AID-HIPO9>3.3.CO;2-O. [DOI] [PubMed] [Google Scholar]
- 86.Tan S.E., Berman R.F., Abel E.L., Zajac C.S. Prenatal alcohol exposure alters hippocampal slice electrophysiology. Alcohol. 1990;7:507–511. doi: 10.1016/0741-8329(90)90040-J. [DOI] [PubMed] [Google Scholar]
- 87.Cebral E., Lasserre A., Rettori V., de Gimeno M.A. Impaired mouse fertilization by low chronic alcohol treatment. Alcohol Alcohol. 1997;32:563–572. doi: 10.1093/oxfordjournals.alcalc.a008297. [DOI] [PubMed] [Google Scholar]
- 88.Cebral E., Lasserre A., Rettori V., de Gimeno M.A. Alterations in preimplantation in vivo development after preconceptional chronic moderate alcohol consumption in female mice. Alcohol Alcohol. 2000;35:336–343. doi: 10.1093/alcalc/35.4.336. [DOI] [PubMed] [Google Scholar]
- 89.Coll T.A., Tito L.P., Sobarzo C.M., Cebral E. Embryo developmental disruption during organogenesis produced by CF-1 murine periconceptional alcohol consumption. Birth Defects Res. Part B Dev. Reprod. Toxicol. 2011;92:560–574. doi: 10.1002/bdrb.20329. [DOI] [PubMed] [Google Scholar]
- 90.Lipinski R.J., Hammond P., O’Leary-Moore S.K., Ament J.J., Pecevich S.J., Jiang Y., Budin F., Parnell S.E., Suttie M., Godin E.A., et al. Ethanol-induced face-brain dysmorphology patterns are correlative and exposure-stage dependent. PLOS ONE. 2012;7:e43067. doi: 10.1371/journal.pone.0043067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Sulik K.K. Craniofacial defects from genetic and teratogen-induced deficiencies in presomite embryos. Birth Defects Orig. Artic. Ser. 1984;20:79–98. [PubMed] [Google Scholar]
- 92.Sulik K.K., Johnston M.C. Sequence of developmental alterations following acute ethanol exposure in mice: Craniofacial features of the fetal alcohol syndrome. Am. J. Anat. 1983;166:257–269. doi: 10.1002/aja.1001660303. [DOI] [PubMed] [Google Scholar]
- 93.Sulik K.K., Johnston M.C., Webb M.A. Fetal alcohol syndrome: Embryogenesis in a mouse model. Science. 1981;214:936–938. doi: 10.1126/science.6795717. [DOI] [PubMed] [Google Scholar]
- 94.Cartwright M.M., Smith S.M. Stage-dependent effects of ethanol on cranial neural crest cell development: Partial basis for the phenotypic variations observed in fetal alcohol syndrome. Alcohol. Clin. Exp. Res. 1995;19:1454–1462. doi: 10.1111/j.1530-0277.1995.tb01007.x. [DOI] [PubMed] [Google Scholar]
- 95.Guerri C., Pascual M., Renau-Piqueras J. Glia and fetal alcohol syndrome. Neurotoxicology. 2001;22:593–599. doi: 10.1016/S0161-813X(01)00037-7. [DOI] [PubMed] [Google Scholar]
- 96.Rubert G., Minana R., Pascual M., Guerri C. Ethanol exposure during embryogenesis decreases the radial glial progenitorpool and affects the generation of neurons and astrocytes. J. Neurosci. Res. 2006;84:483–496. doi: 10.1002/jnr.20963. [DOI] [PubMed] [Google Scholar]
- 97.Fred B.L., Sampson P.D., Connor P.D., Streissguth A.P. Midline Corpus Callosum is a Neuroanatomical Focus of Fetal Alcohol Damage. New Anat. Rec. 2002;269:162–174. doi: 10.1002/ar.10110. [DOI] [PubMed] [Google Scholar]
- 98.Guerri C. Neuroanatomical and neurophysiological mechanisms involved in central nervous system dysfunctions induced by prenatal alcohol exposure. Alcohol. Clin. Exp. Res. 1998;22:304–312. doi: 10.1111/j.1530-0277.1998.tb03653.x. [DOI] [PubMed] [Google Scholar]
- 99.Mazer C., Muneyyirci J., Taheny K., Raio N., Borella A., Whitaker-Azmitia P. Serotonin depletion during synaptogenesis leads to decreased synaptic density and learning deficits in the adult rat: A possible model of neurodevelopmental disorders with cognitive deficits. Brain Res. 1997;760:68–73. doi: 10.1016/S0006-8993(97)00297-7. [DOI] [PubMed] [Google Scholar]
- 100.Thomas J.D., Goodlett C.R., West J.R. Alcohol-induced Purkinje cell loss depends on developmental timing of alcohol exposure and correlates with motor performance. Brain Res. Dev. Brain Res. 1998;105:159–166. doi: 10.1016/S0165-3806(97)00164-8. [DOI] [PubMed] [Google Scholar]
- 101.Hamre K.M., West J.R. The effects of the timing of ethanol exposure during the brain growth spurt on the number of cerebellar Purkinje and granule cell nuclear profiles. Alcohol. Clin. Exp. Res. 1993;17:610–622. doi: 10.1111/j.1530-0277.1993.tb00808.x. [DOI] [PubMed] [Google Scholar]
- 102.Bonthius D.J., West J.R. Alcohol-induced neuronal loss in developing rats: Increased brain damage with binge exposure. Alcohol. Clin. Exp. Res. 1990;14:107–118. doi: 10.1111/j.1530-0277.1990.tb00455.x. [DOI] [PubMed] [Google Scholar]
- 103.Bonthius D.J., West J.R. Permanent neuronal deficits in rats exposed to alcohol during the brain growth spurt. Teratology. 1991;44:147–163. doi: 10.1002/tera.1420440203. [DOI] [PubMed] [Google Scholar]
- 104.Livy D.J., Miller E.K., Maier S.E., West J.R. Fetal alcohol exposure and temporal vulnerability: Effects of binge-like alcohol exposure on the developing rat hippocampus. Neurotoxicol. Teratol. 2003;25:447–458. doi: 10.1016/S0892-0362(03)00030-8. [DOI] [PubMed] [Google Scholar]
- 105.Tran T.D., Kelly S.J. Critical periods for ethanol-induced cell loss in the hippocampal formation. Neurotoxicol. Teratol. 2003;25:519–528. doi: 10.1016/S0892-0362(03)00074-6. [DOI] [PubMed] [Google Scholar]
- 106.Goodlett C.R., Peterson S.D., Lundahl K.R., Pearlman A.D. Binge-like alcohol exposure of neonatal rats via intragastric intubation induces both Purkinje cell loss and cortical astrogliosis. Alcohol. Clin. Exp. Res. 1997;21:1010–1017. doi: 10.1111/j.1530-0277.1997.tb04246.x. [DOI] [PubMed] [Google Scholar]
- 107.Izumi Y., Kitabayashi R., Funatsu M., Izumi M., Yuede C., Hartman R.E., Wozniak D.F., Zorumski C.F. A single day of ethanol exposure during development has persistent effects on bi-directional plasticity, N-methyl-d-aspartate receptor function and ethanol sensitivity. Neuroscience. 2005;136:269–279. doi: 10.1016/j.neuroscience.2005.07.015. [DOI] [PubMed] [Google Scholar]
- 108.Noel M., Norris E.H., Strickland S. Tissue plasminogen activator is required for the development of fetal alcohol syndrome in mice. Proc. Natl. Acad. Sci. USA. 2011;108:5069–5074. doi: 10.1073/pnas.1017608108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Subbanna S., Basavarajappa B.S. Pre-administration of G9a/GLP inhibitor during synaptogenesis prevents postnatal ethanol-induced LTP deficits and neurobehavioral abnormalities in adult mice. Exp. Neurol. 2014;261:34–43. doi: 10.1016/j.expneurol.2014.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Subbanna S., Nagaraja N.N., Umapathy N.S., Pace B.S., Basavarajappa B.S. Ethanol exposure induces neonatal neurodegeneration by enhancing CB1R Exon1 histone H4K8 acetylation and up-regulating CB1R function causing neurobehavioral abnormalities in adult mice. Int. J. Neuropsychopharmacol. 2015 doi: 10.1093/ijnp/pyu028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Subbanna S., Shivakumar M., Psychoyos D., Xie S., Basavarajappa B.S. Anandamide-CB1 receptor signaling contributes to postnatal ethanol-induced neonatal neurodegeneration, adult synaptic and memory deficits. J. Neuosci. 2013;33:6350–6366. doi: 10.1523/JNEUROSCI.3786-12.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Wilson D.A., Peterson J., Basavaraj B.S., Saito M. Local and regional network function in behaviorally relevant cortical circuits of adult mice following postnatal alcohol exposure. Alcohol. Clin. Exp. Res. 2011;35:1974–1984. doi: 10.1111/j.1530-0277.2011.01549.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Miller M.W. Effect of pre- or postnatal exposure to ethanol on the total number of neurons in the principal sensory nucleus of the trigeminal nerve: Cell proliferation and neuronal death. Alcohol. Clin. Exp. Res. 1995;19:1359–1363. doi: 10.1111/j.1530-0277.1995.tb01625.x. [DOI] [PubMed] [Google Scholar]
- 114.Noctor S.C., Flint A.C., Weissman T.A., Dammerman R.S., Kriegstein A.R. Neurons derived from radial glial cells establish radial units in neocortex. Nature. 2001;409:714–720. doi: 10.1038/35055553. [DOI] [PubMed] [Google Scholar]
- 115.Valles S., Pitarch J., Renau-Piqueras J., Guerri C. Ethanol exposure affects glial fibrillary acidic protein gene expression and transcription during rat brain development. J. Neurochem. 1997;69:2484–2493. doi: 10.1046/j.1471-4159.1997.69062484.x. [DOI] [PubMed] [Google Scholar]
- 116.Valles S., Sancho-Tello M., Minana R., Climent E., Renau-Piqueras J., Guerri C. Glial fibrillary acidic protein expression in rat brain and in radial glia culture is delayed by prenatal ethanol exposure. J. Neurochem. 1996;67:2425–2433. doi: 10.1046/j.1471-4159.1996.67062425.x. [DOI] [PubMed] [Google Scholar]
- 117.Cartwright M.M., Tessmer L.L., Smith S.M. Ethanol-induced neural crest apoptosis is coincident with their endogenous death, but is mechanistically distinct. Alcohol. Clin. Exp. Res. 1998;22:142–149. doi: 10.1111/j.1530-0277.1998.tb03630.x. [DOI] [PubMed] [Google Scholar]
- 118.Liesi P. Ethanol-exposed central neurons fail to migrate and undergo apoptosis. J. Neurosci. Res. 1997;48:439–448. doi: 10.1002/(SICI)1097-4547(19970601)48:5<439::AID-JNR5>3.0.CO;2-F. [DOI] [PubMed] [Google Scholar]
- 119.Camarillo C., Miranda R.C. Ethanol exposure during neurogenesis induces persistent effects on neural maturation: Evidence from an ex vivo model of fetal cerebral cortical neuroepithelial progenitor maturation. Gene Exp. 2008;14:159–171. [PMC free article] [PubMed] [Google Scholar]
- 120.Prock T.L., Miranda R.C. Embryonic cerebral cortical progenitors are resistant to apoptosis, but increase expression of suicide receptor DISC-complex genes and suppress autophagy following ethanol exposure. Alcohol. Clin. Exp. Res. 2007;31:694–703. doi: 10.1111/j.1530-0277.2007.00354.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Ikonomidou C., Bittigau P., Ishimaru M.J., Wozniak D.F., Koch C., Genz K., Price M.T., Stefovska V., Hörster F., Tenkova T., et al. Ethanol-induced apoptotic neurodegeneration and fetal alcohol syndrome. Science. 2000;287:1056–1060. doi: 10.1126/science.287.5455.1056. [DOI] [PubMed] [Google Scholar]
- 122.Guerri C., Climent E., Pascual M. Ethanol exposure emhances apoptosis during brain development and affects brain-derived neurotrophic factor and its TrkB receptors. Alcohol Alcohol. 2001;36:437. [Google Scholar]
- 123.Sadrian B., Subbanna S., Wilson D.A., Basavarajappa B.S., Saito M. Lithium prevents long-term neural and behavioral pathology induced by early alcohol exposure. Neuroscience. 2012;206:122–135. doi: 10.1016/j.neuroscience.2011.12.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Subbanna S., Shivakumar M., Umapathy N.S., Saito M., Mohan P.S., Kumar A., Nixon R.A., Verin A.D., Psychoyos D., Basavarajappa B.S. G9a-mediated histone methylation regulates ethanol-induced neurodegeneration in the neonatal mouse brain. Neurobiol. Dis. 2013;54:475–485. doi: 10.1016/j.nbd.2013.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Goodlett C.R., Horn K.H., Zhou F.C. Alcohol teratogenesis: Mechanisms of damage and strategies for intervention. Exp. Biol. Med. 2005;230:394–406. doi: 10.1177/15353702-0323006-07. [DOI] [PubMed] [Google Scholar]
- 126.Guerri C. Mechanisms involved in central nervous system dysfunctions induced by prenatal ethanol exposure. Neurotox. Res. 2002;4:327–335. doi: 10.1080/1029842021000010884. [DOI] [PubMed] [Google Scholar]
- 127.Subbanna S., Psychoyos D., Shan X., Basavarajappa B.S. Postnatal ethanol exposure alters levels of 2-arachidonylglycerol-metabolizing enzymes and pharmacological inhibition of monoacylglycerol (MAGL) does not cause neurodegeneration in neonatal mice. J. Neurochem. 2015;134:276–287. doi: 10.1111/jnc.13120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Deltour L., Ang H.L., Duester G. Ethanol inhibition of retinoic acid synthesis as a potential mechanism for fetal alcohol syndrome. FASEB J. 1996;10:1050–1057. [PubMed] [Google Scholar]
- 129.Liu F., Chen X., Allali-Hassani A., Quinn A.M., Wasney G.A., Dong A., Barsyte D., Kozieradzki I., Senisterra G., Chau I., et al. Discovery of a 2,4-diamino-7-aminoalkoxyquinazoline as a potent and selective inhibitor of histone lysine methyltransferase G9a. J. Med. Chem. 2009;52:7950–7953. doi: 10.1021/jm901543m. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Nagre N.N., Subbanna S., Shivakumar M., Psychoyos D., Basavarajappa B.S. CB1-receptor knockout neonatal mice are protected against ethanol-induced impairments of DNMT1, DNMT3A and DNA methylation. J. Neurochem. 2015;132:429–442. doi: 10.1111/jnc.13006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Rifas L., Towler D.A., Avioli L.V. Gestational exposure to ethanol suppresses msx2 expression in developing mouse embryos. Proc. Natl. Acad. Sci. USA. 1997;94:7549–7554. doi: 10.1073/pnas.94.14.7549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Subbanna S., Nagre N.N., Shivakumar M., Umapathy N.S., Psychoyos D., Basavarajappa B.S. Ethanol induced acetylation of histone at G9a Exon1 and G9a-mediated histone H3 dimethylation leads to neurodegeneration in neonatal mice. Neuroscience. 2014;258C:422–432. doi: 10.1016/j.neuroscience.2013.11.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Miranda R.C. MicroRNAs and fetal brain development: Implications for ethanol teratology during the second trimester period of neurogenesis. Front. Genet. 2012;3:77. doi: 10.3389/fgene.2012.00077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Sathyan P., Golden H.B., Miranda R.C. Competing interactions between micro-RNAs determine neural progenitor survival and proliferation after ethanol exposure: Evidence from an ex vivo model of the fetal cerebral cortical neuroepithelium. J. Neurosci. 2007;27:8546–8557. doi: 10.1523/JNEUROSCI.1269-07.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Miller M. Early exposure to ethanol affects the proliferation of neuronal precursors. In: Miller M., editor. Brain Development Normal Processes and Effects of Alcohol and Nicotine. Oxford University Press; Oxford, UK: 2006. pp. 182–198. [Google Scholar]
- 136.Mooney S.M., Miller M.W., Henderson G.I. Intracellular events in ethanol-induced neuronal death. In: Miller M., editor. Brain Development Normal Processes and Effects of Alcohol and Nicotine. Oxford University Press; Oxford, UK: 2006. pp. 267–278. [Google Scholar]
- 137.Siegenthaler J.A., Miller M.W. Mechanisms of ethanol-induced alterations in neuronal migration. In: Miller M.W., editor. Brain Development Normal Processes and Effects of Alcohol and Nicotine. Oxford University Press; Oxford, UK: 2006. pp. 216–229. [Google Scholar]
- 138.Cui S.J., Tewari M., Schneider T., Rubin R. Ethanol promotes cell death by inhibition of the insulin-like growth factor I receptor. Alcohol. Clin. Exp. Res. 1997;21:1121–1127. doi: 10.1111/j.1530-0277.1997.tb04262.x. [DOI] [PubMed] [Google Scholar]
- 139.Minana R., Climent E., Barettino D., Segui J.M., Renau-Piqueras J., Guerri C. Alcohol exposure alters the expression pattern of neural cell adhesion molecules during brain development. J. Neurochem. 2000;75:954–964. doi: 10.1046/j.1471-4159.2000.0750954.x. [DOI] [PubMed] [Google Scholar]
- 140.Ramanathan R., Wilkemeyer M.F., Mittal B., Perides G., Charness M.E. Alcohol inhibits cell-cell adhesion mediated by human L1. J. Cell Biol. 1996;133:381–390. doi: 10.1083/jcb.133.2.381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Wilkemeyer M.F., Menkari C.E., Charness M.E. Novel antagonists of alcohol inhibition of l1-mediated cell adhesion: Multiple mechanisms of action. Mol. Pharmacol. 2002;62:1053–1060. doi: 10.1124/mol.62.5.1053. [DOI] [PubMed] [Google Scholar]
- 142.Wilkemeyer M.F., Sebastian A.B., Smith S.A., Charness M.E. Antagonists of alcohol inhibition of cell adhesion. Proc. Natl. Acad. Sci. USA. 2000;97:3690–3695. doi: 10.1073/pnas.97.7.3690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Zhang F.X., Rubin R., Rooney T.A. Ethanol induces apoptosis in cerebellar granule neurons by inhibiting insulin-like growth factor 1 signaling. J. Neurochem. 1998;71:196–204. doi: 10.1046/j.1471-4159.1998.71010196.x. [DOI] [PubMed] [Google Scholar]
- 144.Guerri C., Montoliu C., Renau-Piqueras J. Involvement of free radical mechanism in the toxic effects of alcohol: Implications for fetal alcohol syndrome. Adv. Exp. Med. Biol. 1994;366:291–305. doi: 10.1007/978-1-4615-1833-4_20. [DOI] [PubMed] [Google Scholar]
- 145.Olney J.W., Ishimaru M.J., Bittigau P., Ikonomidou C. Ethanol-induced apoptotic neurodegeneration in the developing brain. Apoptosis. 2000;5:515–521. doi: 10.1023/A:1009685428847. [DOI] [PubMed] [Google Scholar]
- 146.Olney J.W., Tenkova T., Dikranian K., Muglia L.J., Jermakowicz W.J., D’Sa C., Roth K.A. Ethanol-induced caspase-3 activation in the in vivo developing mouse brain. Neurobiol. Dis. 2002;9:205–219. doi: 10.1006/nbdi.2001.0475. [DOI] [PubMed] [Google Scholar]
- 147.Olney J.W., Wozniak D.F., Farber N.B., Jevtovic-Todorovic V., Bittigau P., Ikonomidou C. The enigma of fetal alcohol neurotoxicity. Ann. Med. 2002;34:109–119. doi: 10.1080/07853890252953509. [DOI] [PubMed] [Google Scholar]
- 148.Olney J.W., Young C., Wozniak D.F., Jevtovic-Todorovic V., Ikonomidou C. Do pediatric drugs cause developing neurons to commit suicide? Trends Pharmacol. Sci. 2004;25:135–139. doi: 10.1016/j.tips.2004.01.002. [DOI] [PubMed] [Google Scholar]
- 149.Saito M., Chakraborty G., Hegde M., Ohsie J., Paik S.M., Vadasz C. Involvement of ceramide in ethanol-induced apoptotic neurodegeneration in the neonatal mouse brain. J. Neurochem. 2010;115:168–177. doi: 10.1111/j.1471-4159.2010.06913.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Young C., Roth K.A., Klocke B.J., West T., Holtzman D.M., Labruyere J., Qin Y.Q., Dikranian K., Olney J.W. Role of caspase-3 in ethanol-induced developmental neurodegeneration. Neurobiol. Dis. 2005;20:608–614. doi: 10.1016/j.nbd.2005.04.014. [DOI] [PubMed] [Google Scholar]
- 151.Guerri C., Rubert G., Pascual M. Glial targets of developmental exposure to ethanol. In: Miller M.W., editor. Brain Development. Oxford University Press; Oxford, UK: 2006. pp. 295–312. [Google Scholar]
- 152.Mechoulam R., Parker L.A. The endocannabinoid system and the brain. Annu. Rev. Psychol. 2013;64:21–47. doi: 10.1146/annurev-psych-113011-143739. [DOI] [PubMed] [Google Scholar]
- 153.Kreitzer A.C., Regehr W.G. Retrograde inhibition of presynaptic calcium influx by endogenous cannabinoids at excitatory synapses onto Purkinje cells. Neuron. 2001;29:717–727. doi: 10.1016/S0896-6273(01)00246-X. [DOI] [PubMed] [Google Scholar]
- 154.Ohno-Shosaku T., Maejima T., Kano M. Endogenous cannabinoids mediate retrograde signals from depolarized postsynaptic neurons to presynaptic terminal. Neuron. 2001;29:729–738. doi: 10.1016/S0896-6273(01)00247-1. [DOI] [PubMed] [Google Scholar]
- 155.Wilson R.I., Nicoll R.A. Endogenous cannabinoids mediate retrograde signalling at hippocampal synapses. Nature. 2001;410:588–592. doi: 10.1038/35069076. [DOI] [PubMed] [Google Scholar]
- 156.Alger B.E. Retrograde signaling in the regulation of synaptic transmission: Focus on endocannabinoids. Prog. Neurobiol. 2002;68:247–286. doi: 10.1016/S0301-0082(02)00080-1. [DOI] [PubMed] [Google Scholar]
- 157.Basavarajappa B.S., Arancio O. Synaptic plasticity: Emerging role for endocannabinoid system. In: Kaiser T.F., Peters F.J., editors. Synaptic Plasticity New Research. Nova Science Publishers, Inc.; New York, NY, USA: 2008. pp. 77–112. [Google Scholar]
- 158.Di Marzo V., Fontana A., Cadas H., Schinelli S., Cimino G., Schwartz J.C., Piomelli D. Formation and inactivation of endogenous cannabinoid anandamide in central neurons. Nature. 1994;372:686–691. doi: 10.1038/372686a0. [DOI] [PubMed] [Google Scholar]
- 159.Cadas H., di Tomaso E., Piomelli D. Occurrence and biosynthesis of endogenous cannabinoid precursor, N-arachidonoyl phosphatidylethanolamine, in rat brain. J. Neurosci. 1997;17:1226–1242. doi: 10.1523/JNEUROSCI.17-04-01226.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Mechoulam R., Fride E., di Marzo V. Endocannabinoids. Eur. J. Pharmacol. 1998;359:1–18. doi: 10.1016/S0014-2999(98)00649-9. [DOI] [PubMed] [Google Scholar]
- 161.Basavarajappa B.S., Hungund B.L. Chronic ethanol increases the cannabinoid receptor agonist, anandamide and its precursor N-arachidonyl phosphatidyl ethanolamine in SK-N-SH Cells. J. Neurochem. 1999;72:522–528. doi: 10.1046/j.1471-4159.1999.0720522.x. [DOI] [PubMed] [Google Scholar]
- 162.Basavarajappa B.S., Saito M., Cooper T.B., Hungund B.L. Stimulation of cannabinoid receptor agonist 2-arachidonylglycerol by chronic ethanol and its modulation by specific neuromodulators in cerebellar granule neurons. Biochem. Biophys. Acta. 2000;1535:78–86. doi: 10.1016/S0925-4439(00)00085-5. [DOI] [PubMed] [Google Scholar]
- 163.Basavarajappa B.S., Saito M., Cooper T.B., Hungund B.L. Chronic ethanol inhibits the anandamide transport and increases extracellular anandamide levels in cerebellar granule neurons. Eur. J. Pharmacol. 2003;466:73–83. doi: 10.1016/S0014-2999(03)01557-7. [DOI] [PubMed] [Google Scholar]
- 164.Giuffrida A., Parsons L.H., Kerr T.M., Rodriguez de Fonseca F., Navarro M., Piomelli D. Dopamine activation of endogenous cannabinoid signaling in dorsal striatum. Nat. Neurosci. 1999;2:358–363. doi: 10.1038/7268. [DOI] [PubMed] [Google Scholar]
- 165.Devane W.A., Hanus L., Breuer A., Pertwee R.G., Stevenson L.A., Griffin G., Gibson D., Mandelbaum A., Etinger A., Mechoulam R. Isolation and structure of a brain constituent that binds to the cannabinoid receptor. Science. 1992;258:1946–1949. doi: 10.1126/science.1470919. [DOI] [PubMed] [Google Scholar]
- 166.Mechoulam R., Ben-Shabat S., Hanus L., Ligumsky M., Kaminski N.E., Schatz A.R., Gopher A., Almog S., Martin B.R., Compton D.R., et al. Identification of an endogenous 2-monoglyceride, present in canine gut, that binds to cannabinoid receptors. Biochem. Pharmacol. 1995;50:83–90. doi: 10.1016/0006-2952(95)00109-D. [DOI] [PubMed] [Google Scholar]
- 167.Sugiura T., Kondo S., Sukagawa A., Nakane S., Shinoda A., Itoh K., Yamashita A., Waku K. 2-Arachidonoylglycerol: A possible endogenous cannabinoid receptor ligand in brain. Biochem. Biophys. Res. Commun. 1995;215:89–97. doi: 10.1006/bbrc.1995.2437. [DOI] [PubMed] [Google Scholar]
- 168.Hanus L., Abu-Lafi S., Fride E., Breuer A., Vogel Z., Shalev D.E., Kustanovich I., Mechoulam R. 2-arachidonyl glyceryl ether, an endogenous agonist of the cannabinoid CB1 receptor. Proc. Natl. Acad. Sci. 2001;98:3662–3665. doi: 10.1073/pnas.061029898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Porter A.C., Sauer J.M., Knierman M.D., Becker G.W., Berna M.J., Bao J., Nomikos G.G., Carter P., Bymaster F.P., Leese A.B., et al. Characterization of a novel endocannabinoid, virodhamine, with antagonist activity at the CB1 receptor. J. Pharmacol. Exp. Ther. 2002;301:1020–1024. doi: 10.1124/jpet.301.3.1020. [DOI] [PubMed] [Google Scholar]
- 170.Huang S.M., Bisogno T., Trevisani M., Al-Hayani A., de Petrocellis L., Fezza F., Tognetto M., Petros T.J., Krey J.F., Chu C.J., et al. An endogenous capsaicin-like substance with high potency at recombinant and native vanilloid VR1 receptors. Proc. Natl. Acad. Sci. USA. 2002;99:8400–8405. doi: 10.1073/pnas.122196999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Basavarajappa B.S. Neuropharmacology of the endocannabinoid signaling system-Molecular mechanisms, biological actions and synaptic plasticity. Curr. Neuropharmacol. 2007;5:81–97. doi: 10.2174/157015907780866910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Okamoto Y., Morishita J., Tsuboi K., Tonai T., Ueda N. Molecular characterization of a phospholipase D generating anandamide and its congeners. J. Biol. Chem. 2004;279:5298–5305. doi: 10.1074/jbc.M306642200. [DOI] [PubMed] [Google Scholar]
- 173.Ueda N., Kurahashi Y., Yamamoto S., Tokunaga T. Partial purification and characterization of the porcine brain enzyme hydrolyzing and synthesizing anandamide. J. Biol. Chem. 1995;270:23823–23827. doi: 10.1074/jbc.270.40.23823. [DOI] [PubMed] [Google Scholar]
- 174.Simon G.M., Cravatt B.F. Anandamide biosynthesis catalyzed by the phosphodiesterase GDE1 and detection of glycerophospho-N-acyl ethanolamine precursors in mouse brain. J. Biol. Chem. 2008;283:9341–9349. doi: 10.1074/jbc.M707807200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Liu J., Wang L., Harvey-White J., Huang B.X., Kim H.Y., Luquet S., Palmiter R.D., Krystal G., Rai R., Mahadevan A., et al. Multiple pathways involved in the biosynthesis of anandamide. Neuropharmacology. 2008;54:1–7. doi: 10.1016/j.neuropharm.2007.05.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Liu J., Wang L., Harvey-White J., Osei-Hyiaman D., Razdan R., Gong Q., Chan A.C., Zhou Z., Huang B.X., Kim H.Y., et al. A biosynthetic pathway for anandamide. Proc. Natl. Acad. Sci. USA. 2006;103:13345–13350. doi: 10.1073/pnas.0601832103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Morishita J., Okamoto Y., Tsuboi K., Ueno M., Sakamoto H., Maekawa N., Ueda N. Regional distribution and age-dependent expression of N-acylphosphatidylethanolamine-hydrolyzing phospholipase D in rat brain. J. Neurochem. 2005;94:753–762. doi: 10.1111/j.1471-4159.2005.03234.x. [DOI] [PubMed] [Google Scholar]
- 178.Nyilas R., Dudok B., Urban G.M., Mackie K., Watanabe M., Cravatt B.F., Freund T.F., Katona I. Enzymatic machinery for endocannabinoid biosynthesis associated with calcium stores in glutamatergic axon terminals. J. Neurosci. 2008;28:1058–1063. doi: 10.1523/JNEUROSCI.5102-07.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Tsuboi K., Okamoto Y., Ikematsu N., Inoue M., Shimizu Y., Uyama T. Enzymatic formation of N-acylethanolamines from N-acylethanolamine plasmalogen through N-acylphosphatidylethanolamine-hydrolyzing phospholipase D-dependent and -independent pathways. Biochim. Biophys. Acta. 2011;1811:565–577. doi: 10.1016/j.bbalip.2011.07.009. [DOI] [PubMed] [Google Scholar]
- 180.Leung D., Saghatelian A., Simon G.M., Cravatt B.F. Inactivation of N-acyl phosphatidylethanolamine phospholipase D reveals multiple mechanisms for the biosynthesis of endocannabinoids. Biochemistry (Mosc.) 2006;45:4720–4726. doi: 10.1021/bi060163l. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Simon G.M., Cravatt B.F. Characterization of mice lacking candidate N-acyl ethanolamine biosynthetic enzymes provides evidence for multiple pathways that contribute to endocannabinoid production in vivo. Mol. Biosyst. 2010;6:1411–1418. doi: 10.1039/c000237b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Beltramo M., Piomelli D. Carrier-mediated transport and enzymatic hydrolysis of the endogenous cannabinoid 2-arachidonylglycerol. Neuroreport. 2000;11:1231–1235. doi: 10.1097/00001756-200004270-00018. [DOI] [PubMed] [Google Scholar]
- 183.Bisogno T., MacCarrone M., de Petrocellis L., Jarrahian A., Finazzi-Agro A., Hillard C., di Marzo V. The uptake by cells of 2-arachidonoylglycerol, an endogenous agonist of cannabinoid receptors. Eur. J. Biochem. 2001;268:1982–1989. doi: 10.1046/j.1432-1327.2001.02072.x. [DOI] [PubMed] [Google Scholar]
- 184.Hillard C.J., Edgemond W.S., Jarrahian A., Campbell W.B. Accumulation of N-arachidonoylethanolamine (anandamide) into cerebellar granule cells occurs via facilitated diffusion. J. Neurochem. 1997;69:631–638. doi: 10.1046/j.1471-4159.1997.69020631.x. [DOI] [PubMed] [Google Scholar]
- 185.Beltramo M., Stella N., Calignano A., Lin S.Y., Makriyannis A., Piomelli D. Functional role of high-affinity anandamide transport, as revealed by selective inhibition. Science. 1997;277:1094–1097. doi: 10.1126/science.277.5329.1094. [DOI] [PubMed] [Google Scholar]
- 186.Hillard C.J., Jarrahian A. The movement of N-arachidonoylethanolamine (anandamide) across cellular membranes. Chem. Phys. Lipids. 2000;108:123–134. doi: 10.1016/S0009-3084(00)00191-2. [DOI] [PubMed] [Google Scholar]
- 187.Maccarrone M., van der Stelt M., Rossi A., Veldink G.A., Vliegenthart J.F., Agro A.F. Anandamide hydrolysis by human cells in culture and brain. J. Biol. Chem. 1998;273:32332–32339. doi: 10.1074/jbc.273.48.32332. [DOI] [PubMed] [Google Scholar]
- 188.Giuffrida A., Beltramo M., Piomelli D. Mechanisms of endocannabinoid inactivation: Biochemistry and pharmacology. J. Pharmacol. Exp. Ther. 2001;298:7–14. [PubMed] [Google Scholar]
- 189.Deutsch D.G., Glaser S.T., Howell J.M., Kunz J.S., Puffenbarger R.A., Hillard C.J., Abumrad N. The cellular uptake of anandamide is coupled to its breakdown by fatty-acid amide hydrolase. J. Biol. Chem. 2001;276:6967–6973. doi: 10.1074/jbc.M003161200. [DOI] [PubMed] [Google Scholar]
- 190.Glaser S.T., Abumrad N.A., Fatade F., Kaczocha M., Studholme K.M., Deutsch D.G. Evidence against the presence of an anandamide transporter. Proc. Natl. Acad. Sci. USA. 2003;100:4269–4274. doi: 10.1073/pnas.0730816100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Ahn K., Johnson D.S., Mileni M., Beidler D., Long J.Z., McKinney M.K., Weerapana E., Sadagopan N., Liimatta M., Smith S.E., et al. Discovery and characterization of a highly selective FAAH inhibitor that reduces inflammatory pain. Chem. Biol. 2009;16:411–420. doi: 10.1016/j.chembiol.2009.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Cravatt B.F., Demarest K., Patricelli M.P., Bracey M.H., Giang D.K., Martin B.R., Lichtman A.H. Supersensitivity to anandamide and enhanced endogenous cannabinoid signaling in mice lacking fatty acid amide hydrolase. Proc. Natl. Acad. Sci. USA. 2001;98:9371–9376. doi: 10.1073/pnas.161191698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Kathuria S., Gaetani S., Fegley D., Valino F., Duranti A., Tontini A., Giustino A., Tattoli M., Palmery M., Cuomo V., et al. Modulation of anxiety through blockade of anandamide hydrolysis. Nat. Med. 2003;9:76–81. doi: 10.1038/nm803. [DOI] [PubMed] [Google Scholar]
- 194.Berger W.T., Ralph B.P., Kaczocha M., Sun J., Balius T.E., Rizzo R.C., Haj-Dahmane S., Ojima I., Deutsch D.G. Targeting fatty acid binding protein (FABP) anandamide transporters—A novel strategy for development of anti-inflammatory and anti-nociceptive drugs. PLoS ONE. 2012;7:e50968. doi: 10.1371/journal.pone.0050968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Kaczocha M., Glaser S.T., Deutsch D.G. Identification of intracellular carriers for the endocannabinoid anandamide. Proc. Natl. Acad. Sci. USA. 2009;106:6375–6380. doi: 10.1073/pnas.0901515106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Kaczocha M., Rebecchi M.J., Ralph B.P., Teng Y.H., Berger W.T., Galbavy W., Elmes M.W., Glaser S.T., Wang L., Rizzo R.C., et al. Inhibition of fatty acid binding proteins elevates brain anandamide levels and produces analgesia. PLoS ONE. 2014;9:e94200. doi: 10.1371/journal.pone.0094200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Kaczocha M., Vivieca S., Sun J., Glaser S.T., Deutsch D.G. Fatty acid-binding proteins transport N-acylethanolamines to nuclear receptors and are targets of endocannabinoid transport inhibitors. J. Biol. Chem. 2012;287:3415–3424. doi: 10.1074/jbc.M111.304907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Burstein S.H., Rossetti R.G., Yagen B., Zurier R.B. Oxidative metabolism of anandamide. Prostaglandins Other Lipid Mediat. 2000;61:29–41. doi: 10.1016/S0090-6980(00)00053-8. [DOI] [PubMed] [Google Scholar]
- 199.Kozak K.R., Crews B.C., Morrow J.D., Wang L.H., Ma Y.H., Weinander R., Jakobsson P.J., Marnett L.J. Metabolism of the endocannabinoids, 2-arachidonylglycerol and anandamide, into prostaglandin, thromboxane, and prostacyclin glycerol esters and ethanolamides. J. Biol. Chem. 2002;277:44877–44885. doi: 10.1074/jbc.M206788200. [DOI] [PubMed] [Google Scholar]
- 200.Ross R.A., Craib S.J., Stevenson L.A., Pertwee R.G., Henderson A., Toole J., Ellington H.C. Pharmacological characterization of the anandamide cyclooxygenase metabolite: Prostaglandin E2 ethanolamide. J. Pharmacol. Exp. Ther. 2002;301:900–907. doi: 10.1124/jpet.301.3.900. [DOI] [PubMed] [Google Scholar]
- 201.Morozov Y.M., Ben-Ari Y., Freund T.F. The spatial and temporal pattern of fatty acid amide hydrolase expression in rat hippocampus during postnatal development. Eur. J. Neurosci. 2004;20:459–466. doi: 10.1111/j.1460-9568.2004.03507.x. [DOI] [PubMed] [Google Scholar]
- 202.Aguado T., Palazuelos J., Monory K., Stella N., Cravatt B., Lutz B., Marsicano G., Kokaia Z., Guzmán M., Galve-Roperh I. The endocannabinoid system promotes astroglial differentiation by acting on neural progenitor cells. J. Neurosci. 2006;26:1551–1561. doi: 10.1523/JNEUROSCI.3101-05.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Sugiura T., Yoshinaga N., Kondo S., Waku K., Ishima Y. Generation of 2-arachidonoylglycerol, an endogenous cannabinoid receptor ligand, in picrotoxinin-administered rat brain. Biochem. Biophys. Res. Commun. 2000;271:654–658. doi: 10.1006/bbrc.2000.2686. [DOI] [PubMed] [Google Scholar]
- 204.Basavarajappa B.S. Critical Enzymes Involved in Endocannabinoid Metabolism. Protein Peptide Lett. 2007;14:237–246. doi: 10.2174/092986607780090829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Gao Y., Vasilyev D.V., Goncalves M.B., Howell F.V., Hobbs C., Reisenberg M., Shen R., Zhang M.Y., Strassle B.W., Lu P., et al. Loss of retrograde endocannabinoid signaling and reduced adult neurogenesis in diacylglycerol lipase knock-out mice. J. Neurosci. 2010;30:2017–2024. doi: 10.1523/JNEUROSCI.5693-09.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Day T.A., Rakhshan F., Deutsch D.G., Barker E.L. Role of fatty acid amide hydrolase in the transport of the endogenous cannabinoid anandamide. Mol. Pharmacol. 2001;59:1369–1375. doi: 10.1124/mol.59.6.1369. [DOI] [PubMed] [Google Scholar]
- 207.Konrad R.J., Major C.D., Wolf B.A. Diacylglycerol hydrolysis to arachidonic acid is necessary for insulin secretion from isolated pancreatic islets: Sequential actions of diacylglycerol and monoacylglycerol lipases. Biochemistry (Mosc.) 1994;33:13284–13294. doi: 10.1021/bi00249a015. [DOI] [PubMed] [Google Scholar]
- 208.Harkany T., Guzman M., Galve-Roperh I., Berghuis P., Devi L.A., Mackie K. The emerging functions of endocannabinoid signaling during CNS development. Trends Pharmacol. Sci. 2007;28:83–92. doi: 10.1016/j.tips.2006.12.004. [DOI] [PubMed] [Google Scholar]
- 209.Matias I., di Marzo V. Endocannabinoid synthesis and degradation, and their regulation in the framework of energy balance. J. Endocrinol. Investig. 2006;29:15–26. [PubMed] [Google Scholar]
- 210.Piomelli D. The molecular logic of endocannabinoid signalling. Nat. Rev. Neurosci. 2003;4:873–884. doi: 10.1038/nrn1247. [DOI] [PubMed] [Google Scholar]
- 211.Van der Stelt M., Fox S.H., Hill M., Crossman A.R., Petrosino S., di Marzo V., Brotchie J.M. A role for endocannabinoids in the generation of parkinsonism and levodopa-induced dyskinesia in MPTP-lesioned non-human primate models of Parkinson’s disease. FASEB J. 2005;19:1140–1142. doi: 10.1096/fj.04-3010fje. [DOI] [PubMed] [Google Scholar]
- 212.Berrendero F., Sepe N., Ramos J.A., di Marzo V., Fernandez-Ruiz J.J. Analysis of cannabinoid receptor binding and mRNA expression and endogenous cannabinoid contents in the developing rat brain during late gestation and early postnatal period. Synapse. 1999;33:181–191. doi: 10.1002/(SICI)1098-2396(19990901)33:3<181::AID-SYN3>3.0.CO;2-R. [DOI] [PubMed] [Google Scholar]
- 213.Fernandez-Ruiz J., Berrendero F., Hernandez M.L., Ramos J.A. The endogenous cannabinoid system and brain development. Trends Neurosci. 2000;23:14–20. doi: 10.1016/S0166-2236(99)01491-5. [DOI] [PubMed] [Google Scholar]
- 214.Paria B.C., Song H., Wang X., Schmid P.C., Krebsbach R.J., Schmid H.H., Bonner T.I., Zimmer A., Dey S.K. Dysregulated cannabinoid signaling disrupts uterine receptivity for embryo implantation. J. Biol. Chem. 2001;276:20523–20528. doi: 10.1074/jbc.M100679200. [DOI] [PubMed] [Google Scholar]
- 215.Guzman M. Cannabinoids: Potential anticancer agents. Nat. Rev. Cancer. 2003;3:745–755. doi: 10.1038/nrc1188. [DOI] [PubMed] [Google Scholar]
- 216.Guzman M., Sanchez C., Galve-Roperh I. Cannabinoids and cell fate. Pharmacol. Ther. 2002;95:175–184. doi: 10.1016/S0163-7258(02)00256-5. [DOI] [PubMed] [Google Scholar]
- 217.Berghuis P., Rajnicek A.M., Morozov Y.M., Ross R.A., Mulder J., Urban G.M., Monory K., Marsicano G., Matteoli M., Canty A., et al. Hardwiring the brain: Endocannabinoids shape neuronal connectivity. Science. 2007;316:1212–1216. doi: 10.1126/science.1137406. [DOI] [PubMed] [Google Scholar]
- 218.Mulder J., Aguado T., Keimpema E., Barabas K., Ballester Rosado C.J., Nguyen L., Monory K., Marsicano G., di Marzo V., Hurd Y.L., et al. Endocannabinoid signaling controls pyramidal cell specification and long-range axon patterning. Proc. Natl. Acad. Sci. USA. 2008;105:8760–8765. doi: 10.1073/pnas.0803545105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Berghuis P., Dobszay M.B., Wang X., Spano S., Ledda F., Sousa K.M., Schulte G., Ernfors P., Mackie K., Paratcha G., et al. Endocannabinoids regulate interneuron migration and morphogenesis by transactivating the TrkB receptor. Proc. Natl. Acad. Sci. USA. 2005;102:19115–19120. doi: 10.1073/pnas.0509494102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Berghuis P., Dobszay M.B., Ibanez R.M., Ernfors P., Harkany T. Turning the heterogeneous into homogeneous: Studies on selectively isolated GABAergic interneuron subsets. Int. J. Dev. Neurosci. 2004;22:533–543. doi: 10.1016/j.ijdevneu.2004.07.012. [DOI] [PubMed] [Google Scholar]
- 221.Kim D., Thayer S.A. Cannabinoids inhibit the formation of new synapses between hippocampal neurons in culture. J. Neurosci. 2001;21:RC146. doi: 10.1523/JNEUROSCI.21-10-j0004.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Galve-Roperh I., Aguado T., Rueda D., Velasco G., Guzman M. Endocannabinoids: A new family of lipid mediators involved in the regulation of neural cell development. Curr. Pharm. Des. 2006;12:2319–2325. doi: 10.2174/138161206777585139. [DOI] [PubMed] [Google Scholar]
- 223.Jaffe A.B., Hall A. Rho GTPases: Biochemistry and biology. Annu. Rev. Cell Dev. Biol. 2005;21:247–269. doi: 10.1146/annurev.cellbio.21.020604.150721. [DOI] [PubMed] [Google Scholar]
- 224.Jordan J.D., He J.C., Eungdamrong N.J., Gomes I., Ali W., Nguyen T., Bivona T.G., Philips M.R., Devi L.A., Iyengar R. Cannabinoid receptor-induced neurite outgrowth is mediated by Rap1 activation through Gαo/I-triggered proteasomal degradation of Rap1GAPII. J. Biol. Chem. 2005;280:11413–11421. doi: 10.1074/jbc.M411521200. [DOI] [PubMed] [Google Scholar]
- 225.Williams E.J., Walsh F.S., Doherty P. The FGF receptor uses the endocannabinoid signaling system to couple to an axonal growth response. J. Cell Biol. 2003;160:481–486. doi: 10.1083/jcb.200210164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Bisogno T., Howell F., Williams G., Minassi A., Cascio M.G., Ligresti A., Matias I., Schiano-Moriello A., Paul P., Williams E.J., et al. Cloning of the first sn1-DAG lipases points to the spatial and temporal regulation of endocannabinoid signaling in the brain. J. Cell Biol. 2003;163:463–468. doi: 10.1083/jcb.200305129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Howlett A.C., Johnson M.R., Melvin L.S., Milne G.M. Nonclassical cannabinoid analgetics inhibit adenylate cyclase: Development of a cannabinoid receptor model. Mol. Pharmacol. 1988;33:297–302. [PubMed] [Google Scholar]
- 228.Devane W.A., Dysarz F.A.I., Johnson M.R., Melvin L.S., Howlett A.C. Determination and characterization of a cannabinoid receptor in rat brain. Mol. Pharmacol. 1988;34:605–613. [PubMed] [Google Scholar]
- 229.Jarai Z., Wagner J.A., Varga K., Lake K.D., Compton D.R., Martin B.R., Zimmer A.M., Bonner T.I., Buckley N.E., Mezey E., et al. Cannabinoid-induced mesenteric vasodilation through an endothelial site distinct from CB1 or CB2 receptors. Proc. Natl. Acad. Sci. USA. 1999;96:14136–14141. doi: 10.1073/pnas.96.24.14136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Wagner J.A., Varga K., Jarai Z., Kunos G. Mesenteric vasodilation mediated by endothelial anandamide receptors. Hypertension. 1999;33:429–434. doi: 10.1161/01.HYP.33.1.429. [DOI] [PubMed] [Google Scholar]
- 231.Di Marzo V., Breivogel C.S., Tao Q., Bridgen D.T., Razdan R.K., Zimmer A.M., Zimmer A., Martin B.R. Levels, metabolism, and pharmacological activity of anandamide in CB(1) cannabinoid receptor knockout mice: Evidence for non-CB(1), non-CB(2) receptor-mediated actions of anandamide in mouse brain. J. Neurochem. 2000;75:2434–2444. doi: 10.1046/j.1471-4159.2000.0752434.x. [DOI] [PubMed] [Google Scholar]
- 232.Breivogel C.S., Griffin G., di Marzo V., Martin B.R. Evidence for a new G protein-coupled cannabinoid receptor in mouse brain. Mol. Pharmacol. 2001;60:155–163. [PubMed] [Google Scholar]
- 233.Basavarajappa B.S. Endocannabinoid signaling and alcohol addiction. In: Baye D.R., editor. New Research on Alcoholism. Nova Science Publishers, Inc.; New York, NY, USA: 2007. pp. 1–55. [Google Scholar]
- 234.Basavarajappa B.S., Yalamanchili R., Cooper T.B., Hungund B.L. Endocannabinoid system. In: Lajtha A., Sylvester E.V., editors. Handbook of Neurochemistry and Molecular Neurobiology. Springer; New York, NY, USA: 2008. pp. 343–384. [Google Scholar]
- 235.Herkenham M., Lynn A.B., Johnson M.R., Melvin L.S., de Cost B.R., Rice K.C. Characterization and localization of cannabinoid receptors in rat brain: A quantitative in vitro autoradiographic study. J. Neurosci. 1991;16:8057–8066. doi: 10.1523/JNEUROSCI.11-02-00563.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Munro S., Thomas K.L., Abu-Shaar M. Molecular characterization of a peripheral receptor for cannabinoids. Nature. 1993;365:61–65. doi: 10.1038/365061a0. [DOI] [PubMed] [Google Scholar]
- 237.Facci L., dal Toso R., Romanello S., Buriani A., Skaper S.D., Leon A. Mast cells express a peripheral cannabinoid receptor with differential sensitivity to anandamide and palmitoylethanolamide. Proc. Natl. Acad. Sci. USA. 1995;92:3376–3380. doi: 10.1073/pnas.92.8.3376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Onaivi E.S., Ishiguro H., Gong J.P., Patel S., Perchuk A., Meozzi P.A., Myers L., Mora Z., Tagliaferro P., Gardner E., et al. Discovery of the presence and functional expression of cannabinoid CB2 receptors in brain. Ann. N. Y. Acad. Sci. 2006;1074:514–536. doi: 10.1196/annals.1369.052. [DOI] [PubMed] [Google Scholar]
- 239.Van Sickle M.D., Duncan M., Kingsley P.J., Mouihate A., Urbani P., Mackie K., Stella N., Makriyannis A., Piomelli D., Davison J.S., et al. Identification and functional characterization of brainstem cannabinoid CB2 receptors. Science. 2005;310:329–332. doi: 10.1126/science.1115740. [DOI] [PubMed] [Google Scholar]
- 240.Onaivi E.S., Ishiguro H., Gong J.P., Patel S., Meozzi P.A., Myers L., Perchuk A., Mora Z., Tagliaferro P.A., Gardner E., et al. Brain neuronal CB2 cannabinoid receptors in drug abuse and depression: From mice to human subjects. PLoS ONE. 2008;3:e1640. doi: 10.1371/journal.pone.0001640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Berrendero F., Garcia-Gil L., Hernandez M.L., Romero J., Cebeira M., de Miguel R., Ramos J.A., Fernández-Ruiz J.J. Localization of mRNA expression and activation of signal transduction mechanisms for cannabinoid receptor in rat brain during fetal development. Development. 1998;125:3179–3188. doi: 10.1242/dev.125.16.3179. [DOI] [PubMed] [Google Scholar]
- 242.Buckley N.E., Hansson S., Harta G., Mezey E. Expression of the CB1 and CB2 receptor messenger RNAs during embryonic development in the rat. Neuroscience. 1998;82:1131–1149. doi: 10.1016/S0306-4522(97)00348-5. [DOI] [PubMed] [Google Scholar]
- 243.Romero J., Garcia-Palomero E., Berrendero F., Garcia-Gil L., Hernandez M.L., Ramos J.A., Fernández-Ruiz J.J. Atypical location of cannabinoid receptors in white matter areas during rat brain development. Synapse. 1997;26:317–323. doi: 10.1002/(SICI)1098-2396(199707)26:3<317::AID-SYN12>3.0.CO;2-S. [DOI] [PubMed] [Google Scholar]
- 244.Insel T.R. The Development of Brain and Behavior. In: Bloom F.E., Kupfer D.J., editors. Psychopharmacology: The Four Generation of Progress. Raven Press; New York, NY, USA: 1995. pp. 683–694. [Google Scholar]
- 245.Glass M., Dragunow M., Faull R.L. Cannabinoid receptors in the human brain: A detailed anatomical and quantitative autoradiographic study in the fetal, neonatal and adult human brain. Neuroscience. 1997;77:299–318. doi: 10.1016/S0306-4522(96)00428-9. [DOI] [PubMed] [Google Scholar]
- 246.Mailleux P., Vanderhaeghen J.J. Distribution of neuronal cannabinoid receptor in the adult rat brain: A comparative receptor binding radioautography and in situ hybridization histochemistry. Neuroscience. 1992;48:655–668. doi: 10.1016/0306-4522(92)90409-U. [DOI] [PubMed] [Google Scholar]
- 247.Mukhopadhyay S., McIntosh H.H., Houston D.B., Howlett A.C. The CB(1) cannabinoid receptor juxtamembrane C-terminal peptide confers activation to specific G proteins in brain. Mol. Pharmacol. 2000;57:162–170. [PubMed] [Google Scholar]
- 248.Childers S.R., Sexton T., Roy M.B. Effects of anandamide on cannabinoid receptors in rat brain membranes. Biochem. Pharmacol. 1994;47:711–715. doi: 10.1016/0006-2952(94)90134-1. [DOI] [PubMed] [Google Scholar]
- 249.Pinto J.C., Potie F., Rice K.C., Boring D., Johnson M.R., Evans D.M., Wilken G.H., Cantrell C.H., Howlett A.C. Cannabinoid receptor binding and agonist activity of amides and esters of arachidonic acid. Mol. Pharmacol. 1994;46:516–522. [PubMed] [Google Scholar]
- 250.Howlett A.C., Mukhopadhyay S. Cellular signal transduction by anandamide and 2-arachidonoylglycerol. Chem. Phys. Lipids. 2000;108:53–70. doi: 10.1016/S0009-3084(00)00187-0. [DOI] [PubMed] [Google Scholar]
- 251.Caulfield M.P., Brown D.A. Cannabinoid receptor agonists inhibit Ca current in NG108-15 neuroblastoma cells via a pertussis toxin-sensitive mechanism. Br. J. Pharmacol. 1992;106:231–232. doi: 10.1111/j.1476-5381.1992.tb14321.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252.Mackie K., Hille B. Cannabinoids inhibit N-type calcium channels in neuroblastoma-glioma cells. Proc. Natl. Acad. Sci. USA. 1992;89:3825–3829. doi: 10.1073/pnas.89.9.3825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253.Nogueron M.I., Porgilsson B., Schneider W.E., Stucky C.L., Hillard C.J. Cannabinoid receptor agonists inhibit depolarization-induced calcium influx in cerebellar granule neurons. J. Neurochem. 2001;79:371–381. doi: 10.1046/j.1471-4159.2001.00567.x. [DOI] [PubMed] [Google Scholar]
- 254.Pan X., Ikeda S.R., Lewis D.L. Rat brain cannabinoid receptor modulates N-type Ca2+ channels in a neuronal expression system. Mol. Pharmacol. 1996;49:707–714. [PubMed] [Google Scholar]
- 255.Howlett A.C., Barth F., Bonner T.I., Cabral G., Casellas P., Devane W.A., Felder C.C., Herkenham M., Mackie K., Martin B.R., et al. International Union of Pharmacology. XXVII. Classification of cannabinoid receptors. Pharmacol. Rev. 2002;54:161–202. doi: 10.1124/pr.54.2.161. [DOI] [PubMed] [Google Scholar]
- 256.Mu J., Zhuang S.Y., Kirby M.T., Hampson R.E., Deadwyler S.A. Cannabinoid receptors differentially modulate potassium A and D currents in hippocampal neurons in culture. J. Pharmacol. Exp. Ther. 1999;291:893–902. [PubMed] [Google Scholar]
- 257.Freund T.F., Katona I., Piomelli D. Role of endogenous cannabinoids in synaptic signaling. Physiol. Rev. 2003;83:1017–1066. doi: 10.1152/physrev.00004.2003. [DOI] [PubMed] [Google Scholar]
- 258.Wartmann M., Campbell D., Subramanian A., Burstein S.H., Davis R.J. The MAP kinase signal transduction pathway is activated by the endogenous cannabinoid anandamide. FEBS Lett. 1995;359:133–136. doi: 10.1016/0014-5793(95)00027-7. [DOI] [PubMed] [Google Scholar]
- 259.Bouaboula M., Poinot-Chazel C., Bourrie B., Canat X., Calandra B., Rinaldi-Carmona M., le Fur G., Casellas P. Activation of mitogen-activated protein kinases by stimulation of the central cannabinoid receptor CB1. Biochem. J. 1995;312:637–641. doi: 10.1042/bj3120637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.Derkinderen P., Toutant M., Burgaya F., le Bert M., Siciliano J.C., de Franciscis V., Gelman M., Girault J.A. Regulation of a neuronal form of focal adhesion kinase by anandamide. Science. 1996;273:1719–1722. doi: 10.1126/science.273.5282.1719. [DOI] [PubMed] [Google Scholar]
- 261.Derkinderen P., Toutant M., Kadare G., Ledent C., Parmentier M., Girault J.A. Dual role of Fyn in the regulation of FAK+6,7 by cannabinoids in hippocampus. J. Biol. Chem. 2001;276:38289–38296. doi: 10.1074/jbc.M105630200. [DOI] [PubMed] [Google Scholar]
- 262.Ferna’ndez-Ruiz J.J., Bonnin A., Cebeira M., Ramos J.A. Ontogenic and adults changes in the activity of hypothalamic and extrahypothalamic dopaminergic neurons after perinatal cannabinoid exposure. In: Palomo T., Archer T., editors. Strategies for Studying Brain Disorders. Farrand Press; England, UK: 1994. pp. 357–390. [Google Scholar]
- 263.Ferna’ndez-Ruiz J.J., Rodriguez F., Navarro M., Ramos J.A. Maternal cannabinoid exposure and brain development: Changes in the ontogeny of dopaminergic neurons. In: Bartke AaM L.L., editor. Neurobiology and Neurophysiology of Cannabinoids: Biochemistry and Physiology of Substance Abuse. CRC Press; Boca Raton, FL, USA: 1992. pp. 119–164. [Google Scholar]
- 264.Ferna’ndez-Ruiz J.J., Romero J., Garcı’a-Gil L., Garcı’a-Palomero E., Ramos J.A. Dopaminergic neurons as neurochemical substrates of neurobehavioral effects of marihuana: Developmental and adult studies. In: Beninger R.J., Archer T., Palomo T., editors. Dopamine Disease States. CYM Press; Madrid, Spain: 1996. pp. 359–387. [Google Scholar]
- 265.Fernandez-Ruiz J.J., Berrendero F., Hernandez M.L., Romero J., Ramos J.A. Role of endocannabinoids in brain development. Life Sci. 1999;65:725–736. doi: 10.1016/S0024-3205(99)00295-7. [DOI] [PubMed] [Google Scholar]
- 266.Dalterio S.L. Perinatal or adult exposure to cannabinoids alters male reproductive functions in mice. Pharmacol. Biochem. Behav. 1980;12:143–153. doi: 10.1016/0091-3057(80)90429-3. [DOI] [PubMed] [Google Scholar]
- 267.Navarro M., Rodriguez de Fonseca F., Hernandez M.L., Ramos J.A., Fernandez-Ruiz J.J. Motor behavior and nigrostriatal dopaminergic activity in adult rats perinatally exposed to cannabinoids. Pharmacol. Biochem. Behav. 1994;47:47–58. doi: 10.1016/0091-3057(94)90110-4. [DOI] [PubMed] [Google Scholar]
- 268.Dalterio S.L. Cannabinoid exposure: Effects on development. Neurobehav. Toxicol. Teratol. 1986;8:345–352. [PubMed] [Google Scholar]
- 269.Mokler D.J., Robinson S.E., Johnson J.H., Hong J.S., Rosecrans J.A. Neonatal administration of delta-9-tetrahydrocannabinol (THC) alters the neurochemical response to stress in the adult Fischer-344 rat. Neurotoxicol. Teratol. 1987;9:321–327. doi: 10.1016/0892-0362(87)90023-7. [DOI] [PubMed] [Google Scholar]
- 270.Vela G., Fuentes J.A., Bonnin A., Fernandez-Ruiz J., Ruiz-Gayo M. Perinatal exposure to Δ9-tetrahydrocannabinol (Δ9-THC) leads to changes in opioid-related behavioral patterns in rats. Brain Res. 1995;680:142–147. doi: 10.1016/0006-8993(95)00255-O. [DOI] [PubMed] [Google Scholar]
- 271.Navarro M., de Miguel R., Rodriguez de Fonseca F., Ramos J.A., Fernandez-Ruiz J.J. Perinatal cannabinoid exposure modifies the sociosexual approach behavior and the mesolimbic dopaminergic activity of adult male rats. Behav. Brain Res. 1996;75:91–98. doi: 10.1016/0166-4328(96)00176-3. [DOI] [PubMed] [Google Scholar]
- 272.Vela G., Martin S., Garcia-Gil L., Crespo J.A., Ruiz-Gayo M., Fernandez-Ruiz J.J., García-Lecumberri C., Pélaprat D., Fuentes J.A., Ramos J.A., et al. Maternal exposure to Δ9-tetrahydrocannabinol facilitates morphine self-administration behavior and changes regional binding to central mu opioid receptors in adult offspring female rats. Brain Res. 1998;807:101–109. doi: 10.1016/S0006-8993(98)00766-5. [DOI] [PubMed] [Google Scholar]
- 273.Dalterio S., Bartke A. Perinatal exposure to cannabinoids alters male reproductive function in mice. Science. 1979;205:1420–1422. doi: 10.1126/science.472762. [DOI] [PubMed] [Google Scholar]
- 274.Shivachar A.C., Martin B.R., Ellis E.F. Anandamide- and Δ9-tetrahydrocannabinol-evoked arachidonic acid mobilization and blockade by SR141716A [N-(Piperidin-1-yl)-5-(4-chlorophenyl)-1-(2,4-dichlorophenyl)-4-methyl-1H-pyrazole-3-carboximide hydrochloride] Biochem. Pharmacol. 1996;51:669–676. doi: 10.1016/S0006-2952(95)02248-1. [DOI] [PubMed] [Google Scholar]
- 275.Sanchez C., Galve-Roperh I., Rueda D., Guzman M. Involvement of sphingomyelin hydrolysis and the mitogen-activated protein kinase cascade in the Δ9-tetrahydrocannabinol-induced stimulation of glucose metabolism in primary astrocytes. Mol. Pharmacol. 1998;54:834–843. doi: 10.1124/mol.54.5.834. [DOI] [PubMed] [Google Scholar]
- 276.Sanchez C., Velasco G., Guzman M. Δ9-tetrahydrocannabinol stimulates glucose utilization in C6 glioma cells. Brain Res. 1997;767:64–71. doi: 10.1016/S0006-8993(97)00631-8. [DOI] [PubMed] [Google Scholar]
- 277.Bouaboula M., Bourrie B., Rinaldi-Carmona M., Shire D., le Fur G., Casellas P. Stimulation of cannabinoid receptor CB1 induces krox-24 expression in human astrocytoma cells. J. Biol. Chem. 1995;270:13973–13980. doi: 10.1074/jbc.270.23.13973. [DOI] [PubMed] [Google Scholar]
- 278.Hansen H.H., Krutz B., Sifringer M., Stefovska V., Bittigau P., Pragst F., Marsicano G., Lutz B., Ikonomidou C. Cannabinoids enhance susceptibility of immature brain to ethanol neurotoxicity. Ann. Neurol. 2008;64:42–52. doi: 10.1002/ana.21287. [DOI] [PubMed] [Google Scholar]
- 279.De Petrocellis L., Melck D., Palmisano A., Bisogno T., Laezza C., Bifulco M., di Marzo V. The endogenous cannabinoid anandamide inhibits human breast cancer cell proliferation. Proc. Natl. Acad. Sci. USA. 1998;95:8375–8380. doi: 10.1073/pnas.95.14.8375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 280.Galve-Roperh I., Sanchez C., Cortes M.L., Gomez del Pulgar T., Izquierdo M., Guzman M. Anti-tumoral action of cannabinoids: Involvement of sustained ceramide accumulation and extracellular signal-regulated kinase activation. Nat. Med. 2000;6:313–319. doi: 10.1038/73171. [DOI] [PubMed] [Google Scholar]
- 281.Stefanis N.C., Delespaul P., Henquet C., Bakoula C., Stefanis C.N., van Os J. Early adolescent cannabis exposure and positive and negative dimensions of psychosis. Addiction. 2004;99:1333–1341. doi: 10.1111/j.1360-0443.2004.00806.x. [DOI] [PubMed] [Google Scholar]
- 282.Wu C.S., Jew C.P., Lu H.C. Lasting impacts of prenatal cannabis exposure and the role of endogenous cannabinoids in the developing brain. Future Neurol. 2011;6:459–480. doi: 10.2217/fnl.11.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 283.Twitchell W., Brown S., Mackie K. Cannabinoids inhibit N- and P/Q-type calcium channels in cultured rat hippocampal neurons. J. Neurophysiol. 1997;78:43–50. doi: 10.1152/jn.1997.78.1.43. [DOI] [PubMed] [Google Scholar]
- 284.Hampson R.E., Miller F., Palchik G., Deadwyler S.A. Cannabinoid receptor activation modifies NMDA receptor mediated release of intracellular calcium: Implications for endocannabinoid control of hippocampal neural plasticity. Neuropharmacology. 2011;60:944–952. doi: 10.1016/j.neuropharm.2011.01.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 285.Basavarajappa B.S., Ninan I., Arancio O. Acute Ethanol Suppresses Glutamatergic Neurotransmission through Endocannabinoids in Hippocampal Neurons. J. Neurochem. 2008;107:1001–1013. doi: 10.1111/j.1471-4159.2008.05685.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 286.Ikonomidou C., Bosch F., Miksa M., Bittigau P., Vockler J., Dikranian K., Tenkova T.I., Stefovska V., Turski L., Olney J.W. Blockade of NMDA receptors and apoptotic neurodegeneration in the developing brain. Science. 1999;283:70–74. doi: 10.1126/science.283.5398.70. [DOI] [PubMed] [Google Scholar]
- 287.Gerdeman G., Lovinger D.M. CB1 cannabinoid receptor inhibits synaptic release of glutamate in rat dorsolateral striatum. J. Neurophysiol. 2001;85:468–471. doi: 10.1152/jn.2001.85.1.468. [DOI] [PubMed] [Google Scholar]
- 288.Huang C.C., Lo S.W., Hsu K.S. Presynaptic mechanisms underlying cannabinoid inhibition of excitatory synaptic transmission in rat striatal neurons. J. Physiol. 2001;532:731–748. doi: 10.1111/j.1469-7793.2001.0731e.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 289.Chevaleyre V., Castillo P.E. Endocannabinoid-mediated metaplasticity in the hippocampus. Neuron. 2004;43:871–881. doi: 10.1016/j.neuron.2004.08.036. [DOI] [PubMed] [Google Scholar]
- 290.Sullivan J.M. Cellular and molecular mechanisms underlying learning and memory impairments produced by cannabinoids. Learn. Mem. 2000;7:132–139. doi: 10.1101/lm.7.3.132. [DOI] [PubMed] [Google Scholar]
- 291.Wilson R.I., Nicoll R.A. Endocannabinoid Signaling in the Brain. Science. 2002;296:678–682. doi: 10.1126/science.1063545. [DOI] [PubMed] [Google Scholar]
- 292.Mameli M., Zamudio P.A., Carta M., Valenzuela C.F. Developmentally regulated actions of alcohol on hippocampal glutamatergic transmission. J. Neurosci. 2005;25:8027–8036. doi: 10.1523/JNEUROSCI.2434-05.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 293.Sadrian B., Lopez-Guzman M., Wilson D.A., Saito M. Distinct neurobehavioral dysfunction based on the timing of developmental binge-like alcohol exposure. Neuroscience. 2014;280C:204–219. doi: 10.1016/j.neuroscience.2014.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 294.Vaglenova J., Pandiella N., Wijayawardhane N., Vaithianathan T., Birru S., Breese C., Suppiramaniam V., Randal C. Aniracetam reversed learning and memory deficits following prenatal ethanol exposure by modulating functions of synaptic AMPA receptors. Neuropsychopharmacology. 2008;33:1071–1083. doi: 10.1038/sj.npp.1301496. [DOI] [PubMed] [Google Scholar]
- 295.Margret C.P., Li C.X., Chappell T.D., Elberger A.J., Matta S.G., Waters R.S. Prenatal alcohol exposure delays the development of the cortical barrel field in neonatal rats. Exp. Brain Res. 2006;172:1–13. doi: 10.1007/s00221-005-0319-0. [DOI] [PubMed] [Google Scholar]
- 296.Medina A.E., Krahe T.E., Ramoa A.S. Early alcohol exposure induces persistent alteration of cortical columnar organization and reduced orientation selectivity in the visual cortex. J. Neurophysiol. 2005;93:1317–1325. doi: 10.1152/jn.00714.2004. [DOI] [PubMed] [Google Scholar]
- 297.Powrozek T.A., Zhou F.C. Effects of prenatal alcohol exposure on the development of the vibrissal somatosensory cortical barrel network. Brain Res. Dev. Brain Res. 2005;155:135–146. doi: 10.1016/j.devbrainres.2005.01.003. [DOI] [PubMed] [Google Scholar]
- 298.Zhou F.C., Sari Y., Powrozek T.A. Fetal alcohol exposure reduces serotonin innervation and compromises development of the forebrain along the serotonergic pathway. Alcohol. Clin. Exp. Res. 2005;29:141–149. doi: 10.1097/01.ALC.0000150636.19677.6F. [DOI] [PubMed] [Google Scholar]
- 299.Bohme G.A., Laville M., Ledent C., Parmentier M., Imperato A. Enhanced long-term potentiation in mice lacking cannabinoid CB1 receptors. Neuroscience. 2000;95:5–7. doi: 10.1016/S0306-4522(99)00483-2. [DOI] [PubMed] [Google Scholar]
- 300.Reibaud M., Obinu M.C., Ledent C., Parmentier M., Bohme G.A., Imperato A. Enhancement of memory in cannabinoid CB1 receptor knock-out mice. Eur. J. Pharmacol. 1999;379:R1–R2. doi: 10.1016/S0014-2999(99)00496-3. [DOI] [PubMed] [Google Scholar]
- 301.Fernandez-Ruiz J., Gomez M., Hernandez M., de Miguel R., Ramos J.A. Cannabinoids and gene expression during brain development. Neurotox. Res. 2004;6:389–401. doi: 10.1007/BF03033314. [DOI] [PubMed] [Google Scholar]
- 302.Wang X., Dow-Edwards D., Anderson V., Minkoff H., Hurd Y.L. Discrete opioid gene expression impairment in the human fetal brain associated with maternal marijuana use. Pharm. J. 2006;6:255–264. doi: 10.1038/sj.tpj.6500375. [DOI] [PubMed] [Google Scholar]
- 303.Schneider M. Cannabis use in pregnancy and early life and its consequences: Animal models. Eur. Arch. Psychiatry Clin. Neurosci. 2009;259:383–393. doi: 10.1007/s00406-009-0026-0. [DOI] [PubMed] [Google Scholar]
- 304.Campolongo P., Trezza V., Ratano P., Palmery M., Cuomo V. Developmental consequences of perinatal cannabis exposure: Behavioral and neuroendocrine effects in adult rodents. Psychopharmacology (Berl.) 2011;214:5–15. doi: 10.1007/s00213-010-1892-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 305.Kawash G.F., Yeung D.L., Berg S.D. Effects of administration of cannabis resin during pregnancy on emotionality and learning in rats’ offspring. Percept. Mot. Skills. 1980;50:359–365. doi: 10.2466/pms.1980.50.2.359. [DOI] [PubMed] [Google Scholar]
- 306.Campolongo P., Trezza V., Cassano T., Gaetani S., Morgese M.G., Ubaldi M., Soverchia L., Antonelli T., Ferraro L., Massi M., et al. Perinatal exposure to Δ-9-tetrahydrocannabinol causes enduring cognitive deficits associated with alteration of cortical gene expression and neurotransmission in rats. Addict. Biol. 2007;12:485–495. doi: 10.1111/j.1369-1600.2007.00074.x. [DOI] [PubMed] [Google Scholar]
- 307.Antonelli T., Tomasini M.C., Tattoli M., Cassano T., Tanganelli S., Finetti S., Mazzoni E., Trabace L., Steardo L., Cuomo V., et al. Prenatal exposure to the CB1 receptor agonist WIN 55,212-2 causes learning disruption associated with impaired cortical NMDA receptor function and emotional reactivity changes in rat offspring. Cereb. Cortex. 2005;15:2013–2020. doi: 10.1093/cercor/bhi076. [DOI] [PubMed] [Google Scholar]
- 308.Mereu G., Fa M., Ferraro L., Cagiano R., Antonelli T., Tattoli M., Ghiglieri V., Tanganelli S., Gessa G.L., Cuomo V. Prenatal exposure to a cannabinoid agonist produces memory deficits linked to dysfunction in hippocampal long-term potentiation and glutamate release. Proc. Natl. Acad. Sci. USA. 2003;100:4915–4920. doi: 10.1073/pnas.0537849100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 309.O’Shea M., McGregor I.S., Mallet P.E. Repeated cannabinoid exposure during perinatal, adolescent or early adult ages produces similar longlasting deficits in object recognition and reduced social interaction in rats. J. Psychopharmacol. 2006;20:611–621. doi: 10.1177/0269881106065188. [DOI] [PubMed] [Google Scholar]
- 310.O’Shea M., Singh M.E., McGregor I.S., Mallet P.E. Chronic cannabinoid exposure produces lasting memory impairment and increased anxiety in adolescent but not adult rats. J. Psychopharmacol. 2004;18:502–508. doi: 10.1177/0269881104047277. [DOI] [PubMed] [Google Scholar]
- 311.O’Shea M., Mallet P.E. Impaired learning in adulthood following neonatal Δ9-THC exposure. Behav. Pharmacol. 2005;16:455–461. doi: 10.1097/00008877-200509000-00019. [DOI] [PubMed] [Google Scholar]