Abstract
Objectives.
Multilevel models assessed the effects of cognitive speed of processing training (SPT) on older adults’ self-reported driving using intention-to-treat (ITT, randomization to training or control conditions) and dosage (treatment-received via number of training sessions) analyses across 5 years.
Method.
Participants randomized to SPT (n = 598) were compared with those randomized to either the no-contact control (n = 598) or memory training, which served as an active control (n = 610). Driving mobility (frequency, exposure, and space) was assessed over time.
Results.
No significant effects were found within the ITT analyses. However, number of SPT sessions did affect driving mobility outcomes. In the full sample (N = 1,806), higher SPT doses were associated with maintained driving frequency as compared with both control groups, but no effects were found for driving exposure or space. Subsample analyses (n = 315) revealed that persons at-risk for mobility declines (i.e., poor initial processing speed) who received additional booster SPT sessions reported greater maintenance of both driving frequency and exposure over time as compared with the no-contact and active control groups.
Discussion.
These results and prior research indicate that cognitive SPT transfers to prolonged driving mobility among older adults. Future research should investigate the mechanisms behind transfer effects to real-world activities, such as driving.
Key Words: Cognitive training, Divided attention, Driving mobility, Speed of processing training, Training transfer, UFOV.
By 2030, over 70 million Americans are projected to be aged 65 or older, and 85%–90% of these individuals will be licensed drivers (AAA Senior Driving, 2014). This trend raises a number of safety and well-being concerns. Numerous negative consequences are associated with reductions in driving mobility and cessation, including increased depressive symptoms (Fonda, Wallace, & Herzog, 2001), decreased engagement in productive activities (Alzheimer’s Association, 2012), and health declines (Edwards, Lunsman, Perkins, Rebok, & Roth, 2009). Thus, interventions that may enhance driving mobility among older adults are of great interest.
Predictors of Driving Mobility
Older age (Campbell, Bush, & Hale, 1993), poorer health (Anstey, Windsor, Luszcz, & Andrews, 2006; Campbell et al., 1993), female sex (Anstey et al., 2006; Campbell et al., 1993), and poor vision (Ball et al., 1998) are all related to reduced driving mobility. One of the most salient predictors of driving mobility is cognitive speed of processing (Anstey et al., 2006; Ball et al., 1998; Edwards et al., 2008). According to Salthouse (1996), persons with reduced processing speed have difficulty processing incoming information and using previously learned information efficiently. Because driving requires a large amount of cognitive, physical, and sensory information manipulation from a constantly changing environment (Anstey, Wood, Lord, & Walker, 2005; Salvucci, 2006), individuals with slower processing speed may be less able to enact appropriate and efficient decisions while driving.
Indeed, longitudinal studies have consistently found that processing speed difficulties, particularly for higher-order visual attention tasks, are related to reduced driving safety and mobility. Older drivers who have slower processing speed for visual attention tasks, as measured by the Useful Field of View Test (UFOV), crash more frequently (Owsley et al., 1998), avoid more challenging driving situations (Ball et al., 1998; Ross et al., 2009), and reduce or cease driving more often than those with better UFOV performance (Edwards et al., 2008; Ross et al., 2009). These findings are especially of interest given that UFOV performance can be improved by cognitive speed of processing training (SPT).
Cognitive Speed of Processing Training
SPT is a computerized, process-based, training program designed to increase the speed at which persons can process increasingly complex amounts of visual information (Ball, Edwards, & Ross, 2007). Speed of Processing Training (SPT) enhances UFOV performance, particularly for individuals with slower initial processing speed (Ball et al., 2007; Edwards et al., 2005; Roenker, Cissell, Ball, Wadley, & Edwards, 2003; Vance et al., 2007; Wadley et al., 2006). More importantly, SPT transfers to distal (i.e., far transfer) real-world outcomes including health, well-being, performance of instrumental activities of daily living (IADL), and driving mobility (Edwards, Delahunt, & Mahncke, 2009; Edwards et al., 2005; Edwards, Myers et al., 2009; Wolinsky et al., 2009, 2010). With regard to driving performance, older adults randomized to SPT, relative to control groups, exhibited: fewer dangerous driving maneuvers (Roenker et al., 2003); 48% fewer at-fault crashes across 6 years (Ball, Edwards, Ross, & McGwin, 2010); reduced risk of driving cessation across 3 years (Edwards, Delahunt et al., 2009); and maintenance of self-reported driving exposure, space, and difficulty across 3 years (Edwards, Myers et al., 2009). While these findings are promising, there are important limitations that warrant further investigation.
First, to our knowledge, no studies have examined the effects of SPT dosage (or treatment-received) on driving outcomes. Ball, Ross, Roth, and Edwards (2013) emphasized the importance of considering dosage when evaluating far transfer effects for SPT, as number of SPT sessions predicted changes in Timed IADL performance, even though primary intention-to-treat (ITT) analyses were not significant. There is no information about the amount of SPT needed to affect changes in driving mobility, or whether subsequent booster sessions provide greater benefits than initial training. Second, no study to date has examined if SPT transfers to driving mobility beyond 3 years. Finally, this is the first study to use both no-contact and active control groups to investigate changes in driving mobility as a function of SPT.
The current study addressed these limitations by examining the effects of SPT on changes in self-reported driving mobility over a 5-year period among older adults in the Advanced Cognitive Training for Independent and Vital Elderly (ACTIVE) study. Driving mobility was quantified by self-reported driving frequency, driving exposure, and driving space (Edwards, Myers et al., 2009). ITT (study arm or group randomization) and dosage (treatment-received analyses) were used to compare SPT against a no-contact control group and against an active control group (memory training). ITT analyses investigated the effects of randomization to a study arm on later driving mobility trajectories (regardless of actual training exposure). The dosage (treatment-received) analyses investigated the impact of the amount of SPT training (hours) participants actually completed on these mobility trajectories. Additional dosage (treatment-received) subsample analyses were conducted to investigate the impact of number of booster training sessions among participants at-risk for mobility declines (i.e., poor baseline UFOV), given prior results that such individuals are most likely to benefit from SPT (Ball et al., 2007; Edwards, Myers et al., 2009). Finally, the possible influence of participation in a longitudinal behavioral training study (e.g., social contact, changes in self-efficacy, general cognitive stimulation, etc.) was investigated by comparing participants randomized to memory training (active control group) and SPT. Given the importance of dosage in previous research (Ball et al., 2013), it was hypothesized that participants who received the most SPT would maintain self-reported indices of driving mobility as compared with the control groups. We expected that transfer effects would be greatest for participants who were at-risk for future mobility declines (i.e., poor baseline UFOV performance) who received the highest training dosage (i.e., booster).
Method
Participants
Active baseline drivers (N = 1,806) from three of the original four ACTIVE study arms were included, namely SPT (n = 598), memory training (n = 610), and no-contact controls (n = 598). Active drivers were defined as those who reported having driven within the last 12 months and those who indicated that they “would drive today” if they needed to do so. See Table 1 for sample descriptives across training and control arms.
Table 1.
Study Demographics: Baseline Drivers Who Were Randomized to the Speed of Processing Training, Memory Training, or the No-Contact Control Arms
| Variable | No-contact control arm (n = 598) M (SD) or % |
Speed of processing training arm (n = 598) M (SD) or % |
Memory training arm (n = 610) M (SD) or % |
|---|---|---|---|
| Age | 73.60 (5.78) | 73.13 (5.55) | 73.21 (5.87) |
| Sex, female | 71.4% | 73.6% | 74.3% |
| Race | |||
| Caucasian | 75.3% | 76.3% | 76.0% |
| African American | 23.8% | 23.0% | 23.5% |
| Other | 0.9% | 0.7% | 0.5% |
| Turn-360 | 6.85 (1.91) | 6.76 (1.86) | 6.76 (1.90) |
| Self-rated health | 2.59 (0.87) | 2.50 (0.87) | 2.56 (0.83) |
| Vision (0–90) | 73.73 (11.63) | 73.80 (11.30) | 74.50 (10.63) |
| Years of education | 13.63 (2.68) | 13.84 (2.70) | 13.80 (2.72) |
| Baseline driving frequency (0–7) | 5.58 (1.71) | 5.66 (1.78) | 5.58 (1.80) |
| Baseline driving exposure (0–8) | 7.28 (1.27) | 7.35 (1.22) | 7.22 (1.45) |
Materials and Procedure
The ACTIVE study is detailed elsewhere (Jobe et al., 2001; Willis et al., 2006). Briefly, this longitudinal, multi-site, single-blind, randomized clinical trial investigated the effects of three forms of cognitive training upon subsequent daily functioning, health, and well-being. Adults ages 65 and older were screened from six sites throughout the U.S. Study. Eligibility criteria included: intact mental status (Mini-Mental State Exam score of 23 or higher and no self-reported diagnosis of dementia); intact functional health (reported ability to perform activities of daily living); unremarkable physical health (no reported stroke within the last year, no report of certain types of cancer, or no recent chemotherapy/radiation treatment); intact vision (a score of 39 or greater, which is equivalent to 20/50 far visual acuity or better); ability to verbally communicate; and no recent cognitive training participation.
Eligible participants completed in-person baseline assessments and were randomized (N = 2,802) to one of four conditions: an SPT arm, a reasoning training arm, a memory training arm, or a no-contact control arm. Compliant participants (e.g., those who completed eight or more of the 10 training sessions) were then randomized within each training arm to receive an additional four booster sessions (60–75min each) just prior to assessments at years 1 and 3. Participants were reassessed on the relevant baseline assessments immediately after initial training sessions (<10 days) and at years 1, 2, 3, and 5.
Intervention: cognitive training.
The three training arms of ACTIVE were standardized such that the initial training consisted of ten 60- to 75-min sessions over approximately 6 weeks. The training occurred in small groups of three to four participants led by a certified trainer. The exercises practiced in the first five sessions were standardized (the same for all participants within that training arm), and the last five sessions were adapted to meet the needs of the participants as determined by the certified trainer and standardized protocol.
Speed of processing training.
SPT is a computerized, process-based, adaptive cognitive intervention designed to increase the speed at which participants can accurately decipher increasingly complex stimuli. The training included 18 different processing speed, divided attention, and inhibition tasks presented at 10 different display speeds. Tasks required combinations of visual and auditory target identification, discrimination, and localization (Ball et al., 2007; Edwards et al., 2005). Throughout the training, the primary adaptation was the speed at which the tasks were displayed, ranging between 20 and 500ms. Based upon ongoing participant performance, the difficulty of the tasks was modified according to the protocol in order to increase the speed at which participants could process information, as well as the amount and complexity of that information.
Memory training.
Memory training consisted of instruction and practice of several mnemonic strategies (such as organization, visualization, etc.) that focused on verbal episodic memory (Rasmusson, Rebok, Bylsma, & Brandt, 1999; Rebok & Balcerak, 1989). This training transferred to improved memory performance and attenuated declines in everyday functioning (IADLs); however, it has not been shown to impact driving (Rebok et al., 2014). As such, the memory training group served as the active control arm in the current analyses. The participants received the same amount of study-related contact and encouragement as participants in the SPT arm.
No-contact control.
Participants randomized to this arm came to the study sites at screening/baseline, posttest, years 1, 2, 3, and 5 for evaluation. No intervention was conducted with this arm.
Main outcome measures.
Three self-reported outcome measures of driving habits were assessed using the Mobility Questionnaire (MQ), which has good construct validity and test–retest reliability (Owsley, Stalvey, Wells, & Sloane, 1999). Per the MQ and as in prior research, drivers at baseline were self-identified as having driven within the past 12 months and who would drive if needed; participants not meeting this definition were coded as nondrivers. This questionnaire was repeated at years 1, 2, 3, and 5. Participants were coded as nondrivers at the wave they reported not driving and through the remainder of the study (incident nondrivers). Less than 1% of incident nondrivers later reported driving again at a subsequent study wave.
Driving frequency.
Data on the reported number of days driven in an average week (0–7) formed the driving frequency measure. Incident nondrivers were coded as driving zero days per week for that and each subsequent year.
Driving exposure.
Participants were asked if they had driven alone, made lane changes, turned left onto oncoming traffic, driven in high traffic, at night, in the rain, merged with traffic, or driven during rush-hour over the last 2 months. These dichotomous items were coded and summed such that higher scores indicated more exposure to these eight driving situations (range 0–8). Persons reporting driving cessation at any year were coded with a driving exposure of zero for that and subsequent years.
Driving space.
A composite was calculated that consisted of six dichotomous questions as to whether or not the participant had personally driven beyond a certain radius. These areas were asked in relation to either the last 7 days (beyond property, beyond neighborhood, or beyond town/community), or the last 2 months (beyond county/city, beyond state, or beyond region). Items were coded and summed so that larger numbers indicated larger driving space (range 0–6). Persons reporting subsequent driving cessation were coded with a driving space of zero for that and each subsequent year.
Other Measures
Training.
Training was assessed through ITT and dosage (treatment-received) variables (see Analyses section). ITT analyses used group randomization through dummy-coded variables comparing SPT (1) to the relative control conditions (0). Dosage analyses included the number of SPT sessions completed as a time-varying variable.
Attrition.
Participants missing fifth year data were coded as dropouts. A dummy-coded attrition variable was created in which non-dropouts = 1 and dropouts = 0.
Demographics.
Age, sex, and years of education were examined as covariates, as they have been found to predict driving behaviors (Anstey et al., 2006; Campbell et al., 1993). Sex was dummy-coded with women as the reference category.
Health.
Self-rated health was evaluated as a covariate, as health has been found to be related to driving behaviors (Campbell et al., 1993). Using the SF-36 (Ware & Sherbourne, 1992), participants were asked to rate their health on a five-point Likert scale (Excellent = 1, Very Good = 2, Good = 3, Fair = 4, Poor = 5).
Vision.
A GoodLite Model 600A light box with an Early Treatment for Diabetic Retinopathy Study chart was used to measure far visual acuity with standard procedures. Participants were asked to stand 10 feet from the chart and were tested with corrective lenses if worn. Scores were assigned from 0 to 90 based upon how many letters were correctly discriminated (0 is equivalent to Snellen score 20/125; 90 to Snellen score 20/16).
Physical function.
Turn 360 (Steinhagen-Thiessen & Borchelt, 1999) was used to measure lower-limb physical function. Participants were asked to make a 360 degree turn from a standing position. The number of steps taken to complete the turn was recorded, with more steps indicating poorer performance. The average of the two turns was examined as a covariate given the previous association with driving outcomes (Edwards et al., 2008).
Processing speed for visual attention.
The UFOV test assesses processing speed for visual attention tasks and has been shown to be a valid and reliable predictor of driving mobility outcomes (e.g., Owsley et al., 1998; Ross et al., 2009). The UFOV test is administered on a touch-screen computer and consists of four subtests (Ball & Roenker, 2014). Each subtest increases in difficulty and assesses the display speed (16–500ms) at which participants can accurately perform the task 75% of the time. Subtest 1 (processing speed) requires a central identification of either a car or truck (2cm by 1.5cm). Subtest 2 (divided attention) adds a peripheral location task to the central identification task simultaneously. Subtest 3 (divided attention and inhibition) is similar to subtest 2; however, distractor triangles are added to the display. The final subtest requires a central discrimination task (discernment of two central figures as the same or different) along with the simultaneous peripheral localization task within distractors. Scores in ms were given for each subtest, with smaller scores (shorter display durations) representing better performance and faster processing speed.
Baseline performance on the UFOV test was used to identify persons who were at-risk for future driving declines. Using the standardized scoring system provided in the UFOV testing manual, participants were grouped into low- (risk categories of 1–2) and high-risk (risk categories of 3–5) groups (Ball & Roenker, 2014).
Analyses
Baseline group differences in demographics, driving outcomes, health, vision, and education were examined through analysis of variance and Chi-square analyses (Table 1). This process was also repeated to compare demographics of participants with a high level of risk for future mobility declines with those participants with a low level of risk (Table 2).
Table 2.
Study Demographics: Participants Divided by High and Low Risk of Future Mobility Declines (Baseline Useful Field of View Scores)
| Variable | Low risk | High risk |
|---|---|---|
| (n = 1,271) | (n = 508) | |
| M (SD) or % | M (SD) or % | |
| Age*** | 72.03 (5.05) | 76.23 (6.11) |
| Sex, female | 72.7% | 73.6% |
| Race** | ||
| Caucasian | 78.0% | 70.4% |
| African American | 21.2% | 29.6% |
| Other | 0.8% | 0% |
| Turn 360*** | 6.56 (1.62) | 7.32 (2.31) |
| Self-rated health*** | 2.46 (0.85) | 2.75 (0.83) |
| Vision (0–90)*** | 75.60 (10.52) | 70.16 (11.78) |
| Years of education*** | 1.98 (2.67) | 13.24 (2.67) |
| Baseline driving frequency (0–7)*** | 5.72 (1.70) | 5.38 (1.85) |
| Baseline driving exposure (0–8)*** | 7.41 (1.24) | 7.00 (1.44) |
| Baseline driving space (0–6)*** | 3.47 (1.33) | 3.14 (1.30) |
Notes. UFOV is Useful Field of View Test. Twenty-seven participants had missing baseline UFOV scores and were not included in any models investigating at-risk subsamples (see Table 4). Outcome measures were driving frequency, driving exposure, and driving space. Driving frequency was the average number of days driven in a week. Driving exposure was the sum of driving in challenging situations (e.g., driven alone, in the rain, etc.) over the previous 2 months. Driving space was the furthest driving radius reported (e.g., beyond neighborhood, state, etc.) over the previous week through 2 months.
***p < .001. **p < .01.
In order to compare the change in driving outcomes, each dependent variable was standardized by subtracting the baseline mean from each respective year score (baseline through year 5) and dividing by the baseline standard deviation. Time was scaled in number of months since baseline. Base models were developed using the no-contact control group. Potential covariates (sex, age, education, race, self-rated health, vision, Turn 360, and attrition) were examined, and significant covariates were included in the resulting final driving frequency, driving exposure, and driving space base models. Any training analyses (ITT or dosage) were then conducted using these base models. Covariates were centered at the baseline mean for each respective variable.
In order to investigate the impact of SPT on subsequent driving mobility, both ITT (randomization to study arm) and dosage (treatment-received via number of training sessions completed as a time-varying variable) analyses were conducted through a series of multilevel longitudinal models (Singer & Willett, 2003). The first set of analyses investigated the impact of randomization (ITT) to training on driving mobility within the full sample and included additional analyses to investigate the trajectories of participants who were and were not randomized to booster training. The second set of models repeated this process and only included those participants who were at-risk (via baseline UFOV) for future mobility declines, as this sample has previously demonstrated greater training gains and transfer (Ball et al., 2007; Edwards, Myers et al., 2009).
The above two sets of analyses were then repeated using dosage (treatment-received analyses) to account for participants who did not comply with training. This is also important as the first five sessions of SPT in the ACTIVE study were standardized, rather than adaptive. Thus, participants who did not receive booster had a lower dose of adaptive training as compared with other studies of SPT (Edwards, Myers et al., 2009; Edwards et al., 2005; Roenker et al., 2003). Subsequent research and theory indicate that adaptive training techniques are most effective (Lövdén, Bäckman, Lindenberger, Schaefer, & Schmiedek, 2010). SPT dosage was compared with the no-contact control group (0 sessions) and to the memory trained group. Number of training sessions was changed to 0 for the memory trained group so that the impact of SPT dosage specifically could be investigated. All models used restricted maximum likelihood estimation with an unstructured covariance matrix and were conducted with SPSS, version 21. Significance was evaluated at p < .05 for two-tailed tests. Cohen’s d effect sizes for significant SPT effects were calculated per outcome (year five SPT group mean of outcome − year five no-contact control group mean of outcome/baseline outcome standard deviation).
Results
Baseline Group Differences
There were no significant baseline demographic, driving mobility, health or vision differences between the three training arms (Table 1). As would be expected, there were differences between those participants who were at a higher risk versus those who were at a lower risk for future mobility declines at baseline (Table 2). At-risk participants were, on average, older with less reported education, less reported baseline driving mobility, poorer reported health, and poorer physical functioning and health. Risk category also differed by race such that there was a greater proportion of African Americans classified as at-risk. Chi-square analyses revealed that compliance with training did not differ by training group or mobility risk category (p’s > .05).
Model Covariates
Base models were developed for each outcome using the control group. The following baseline covariates were significant in the base models and were thus included in the training models. Models for driving frequency were adjusted for age, vision, Turn 360, education, attrition, sex, age*time, vision*time, and attrition*time. Models for driving exposure controlled for age, vision, Turn 360, education, attrition, age*time, Turn 360*time, and attrition*time. Finally, models for driving space included sex, age, vision, Turn 360, education, attrition, age*time, Turn 360*time, and attrition*time.
Intention-to-Treat
No significant training effects were found across any of the groups in ITT analyses (p > .05).
Dosage (Treatment-Received) Analyses
Total sample analyses.
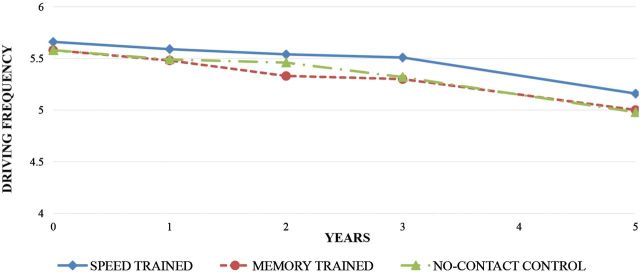
The dosage models investigated the impact of dosage (number of SPT sessions completed, 0–18 sessions, time-varying) upon self-reported driving mobility trajectories after accounting for covariates (see Table 3). There was a significant impact of SPT sessions for driving frequency (est. = 0.008 [SE = 0.003], 95% confidence interval [CI]: 0.003, 0.013, p < .01) such that more SPT sessions were predictive of greater driving frequency across the 5 years as compared with the no-contact control group (Cohen’s d effect size = 0.10). This effect was tested against the memory trained group to investigate if the effect could be due to activity in a behavioral intervention trial (e.g., self-efficacy, social engagement, etc.). Again, SPT sessions were predictive of greater driving frequency (est. = 0.008 [SE = 0.003], 95% CI: 0.003, 0.014, p < .01) when compared with the active control group. However, number of SPT sessions was not a significant predictor of changes in driving exposure or driving space (p > .05). Figure 1 depicts driving frequency changes across the 5 years by study arm.
Table 3.
Final Models With Significant Dosage Training Effects for Full Sample Analyses
| Speed of processing training (n = 598) versus no-contact control (n = 598) | Speed of processing training (n = 598) versus memory training (n = 610) | |||
|---|---|---|---|---|
| Est. (SE) | 95% CI | Est. (SE) | 95% CI | |
| Driving frequency | ||||
| Fixed effects | ||||
| Intercept | −0.17 (0.05)** | −0.27, −0.06 | −0.11 (0.06)* | −0.22, −0.003 |
| Age | −0.02 (0.01)*** | −0.03, 0.01 | −0.01 (0.01)** | −0.02, −0.004 |
| Vision | 0.01 (0.002)** | 0.002, 0.01 | 0.01 (0.003)** | 0.003, 0.01 |
| Physical function | −0.06 (0.01)*** | −0.09, −0.03 | −0.02 (0.01) | −0.05, 0.01 |
| Education | 0.04 (0.01)*** | 0.02, 0.06 | 0.03 (0.01)** | 0.01, 0.05 |
| Attrition, (non-dropouts) | 0.12 (0.06)* | 0.01, 0.24 | 0.06 (0.06) | −0.07, 0.18 |
| Sex (males) | 0.40 (0.06)*** | 0.28, 0.51 | 0.38 (0.06)*** | 0.26, 0.50 |
| Time | 0.01 (0.002)*** | −0.01, −0.01 | −0.01 (0.002)*** | −0.02, −0.01 |
| Age*time | −0.001 (<0.001)*** | −0.001, <−0.001 | −0.001 (<0.001)*** | −0.001, <−0.001 |
| Attrition*time | 0.002 (0.002) | −0.003, 0.01 | 0.004 (0.002) | −0.001, 0.01 |
| Vision*time | <0.001 (<0.001) | <−0.001, <0.001 | <−0.001 (<0.001) | <−0.001, <0.001 |
| SPT sessions | 0.01 (0.003)** | 0.003, 0.01 | 0.01 (0.003)** | 0.003, 0.01 |
| Random effects | ||||
| Residual | 0.28 (0.008)*** | 0.26, 0.29 | 0.30 (0.009)*** | 0.28, 0.31 |
| Intercept | 0.64 (0.03)*** | 0.58, 0.71 | 0.71 (0.04)*** | 0.64, 0.79 |
| Time | <0.001 (<0.001)*** | 0.0001, 0.0002 | <0.001 (<0.001)*** | 0.0002, 0.0003 |
| Covariance (intercept, time) | <0.001 (<0.001) | −0.001, 0.001 | −0.003 (<0.001)*** | −0.004, −0.001 |
Notes. Driving frequency was the average number of days driven in a week. Unstandardized estimates are presented. CI = confidence interval; SPT = speed of processing training.
***p < .001. **p < .01. *p < .05.
Figure 1.
Driving frequency by training and control groups in full sample. Note: Driving frequency means are presented (range 0–7). Driving frequency was the average number of days driven in a week. Training and control groups did not differ on baseline driving frequency (see Table 1, p > .05). Booster training occurred at years 1 and 3. Cohen’s d for speed of processing trained group compared with no-contact control group was 0.10.
At-Risk for Mobility Declines Subsample Analyses
No booster training.
The above process was repeated investigating only those participants who were at-risk for future mobility declines at baseline (Edwards et al., 2008; Ross et al., 2009) and therefore had the greatest potential for training gains (Ball et al., 2007; Edwards, Myers et al., 2009). For at-risk participants who did not receive booster training, number of SPT sessions was not a significant predictor of change in driving frequency, driving exposure, or driving space (p > .05).
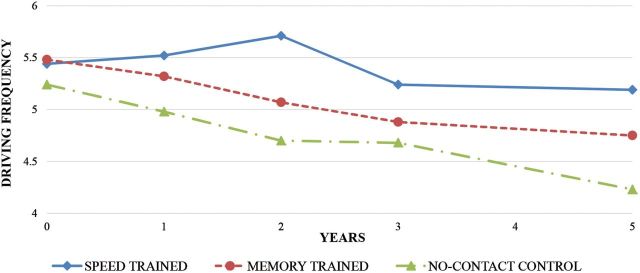
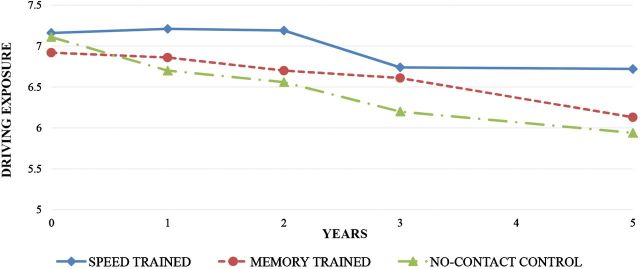
Booster training received.
The same process outlined in the previous analyses was repeated within the subsample of participants who were at-risk for mobility declines and who were received booster SPT sessions (total sessions 11–18). There was a significant impact of number of SPT sessions (est. = 0.018 [SE = 0.007], 95% CI: 0.004, 0.03, p < .05) on driving frequency. There was also a significant effect of number of SPT sessions (est. = 0.021 [SE = 0.01], 95% CI: 0.001, 0.04, p < .05) on driving exposure. The Cohen’s d effect sizes were 0.53 for driving frequency and 0.60 for driving exposure. However, number of SPT sessions was not significant for driving space (p > .05).
As before, the SPT group was also compared with the memory trained group to investigate if the effect could be due to activity in a behavioral intervention trial. As with the SPT versus no-contact control group, more SPT sessions were predictive of greater driving frequency (est. = 0.019 [SE = 0.008], 95% CI: 0.004, 0.033, p < .05) and driving exposure (est. = 0.02 [SE = 0.01], 95% CI: 0.001, 0.039, p < .05) in this subsample. See Table 4 for final models for driving frequency and driving exposure comparing SPT to both control groups. Figures 2 and 3 depict driving frequency and driving exposure changes across the 5 years by study arm.
Table 4.
Final Models With Significant Speed of Processing Training Dosage Effects for At-Risk Participants Who Received Booster Training
| Speed of processing training (n = 64) versus no-contact control (n = 171) | Speed of processing training (n = 64) versus memory training (n = 80) | |||
|---|---|---|---|---|
| Est. (SE) | 95% CI | Est. (SE) | 95% CI | |
| Driving frequency | ||||
| Fixed effects | ||||
| Intercept | −0.26 (0.13)* | −0.52, −0.01 | −0.13 (0.17) | −0.46, 0.19 |
| Age | −0.04 (0.01)*** | −0.06, −0.01 | −0.01 (0.01) | −0.04, 0.01 |
| Vision | −0.002 (0.01) | −0.01, 0.01 | 0.01 (0.01) | −0.004, 0.02 |
| Physical function | −0.05 (0.03) | −0.11, 0.01 | −0.04 (0.04) | −0.12, 0.04 |
| Education | 0.08 (0.03)** | 0.03, 0.13 | 0.02 (0.03) | −0.04, 0.08 |
| Attrition (non-dropouts) | 0.23 (0.14) | −0.03, 0.50 | 0.16 (0.18) | −0.20, 0.52 |
| Sex (males) | 0.50 (0.15)*** | 0.21, 0.79 | 0.21 (0.18) | −0.13, 0.56 |
| Time | −0.02 (0.005)*** | −0.03, −0.01 | −0.02 (0.01)** | −0.03, −0.004 |
| Age*time | −0.001 (<0.001)* | −0.001, −<0.001 | −0.001 (<0.001)* | −0.002, −0.0001 |
| Attrition*time | 0.10 (0.005) | <−0.001, 0.02 | 0.01 (0.01) | −0.01, 0.02 |
| Vision*time | <0.001 (<0.001) | <−0.001, 0.001 | <−0.001 (<0.001) | −0.001, 0.0003 |
| SPT sessions | 0.02 (0.007)* | 0.004, 0.03 | 0.02 (0.008)* | 0.004, 0.03 |
| Random effects | ||||
| Residual | 0.40 (0.03)*** | 0.35, 0.46 | 0.41 (0.03)*** | 0.35, 0.48 |
| Intercept | 0.61 (0.09)*** | 0.47, 0.80 | 0.64 (0.11)*** | 0.45, 0.90 |
| Time | <0.001 (<0.001)*** | 0.0001, 0.0004 | 0.001 (<0.001) | 0.0003, 0.001 |
| Covariance (intercept, time) | 0.002 (0.002) | −0.002, 0.005 | −0.007 (0.003)* | −0.01, −0.001 |
| Driving exposure | ||||
| Fixed effects | ||||
| Intercept | −0.06 (0.12) | −0.30, 0.18 | −0.30 (0.15) | −0.60, 0.01 |
| Age | −0.02 (0.01) | −0.04, 0.001 | −0.01 (0.01) | −0.04, 0.02 |
| Vision | 0.01 (0.01)* | 0.003, 0.02 | 0.01 (0.01)* | 0.003, 0.03 |
| Physical function | −0.04 (0.03) | −0.10, 0.02 | −0.04 (0.04) | −0.12, 0.05 |
| Education | 0.07 (0.03)** | 0.02, 0.13 | 0.08 (0.03)** | 0.03, 0.14 |
| Attrition (non-dropouts) | 0.14 (0.14) | −0.13, 0.41 | 0.34 (0.17) | −0.001, 0.69 |
| Time | −0.04 (0.01)*** | −0.05, −0.03 | −0.02 (0.01)** | −0.04, −0.01 |
| Age*time | −0.001 (0.001)** | −0.002, −0.0004 | −0.001 (0.001) | −0.002, 0.0001 |
| Physical Function*time | −0.003 (0.001)* | −0.006, −0.0003 | −0.004 (0.002) | −0.01, <0.001 |
| Attrition*time | 0.03 (0.01)*** | 0.01, 0.04 | 0.01 (0.01) | −0.01, 0.03 |
| SPT sessions | 0.02 (0.01)* | 0.001, 0.04 | 0.02 (0.01)* | 0.001, 0.04 |
| Random effects | ||||
| Residual | 0.64 (0.05)*** | 0.56, 0.74 | 0.67 (0.06)*** | 0.57, 0.79 |
| Intercept | 0.46 (0.09)*** | 0.32, 0.67 | 0.37 (0.10)*** | 0.22, 0.64 |
| Time | 0.001 (<0.001)*** | 0.0005, 0.001 | 0.001 (<0.001)*** | 0.0005, 0.001 |
| Covariance (intercept, time) | 0.01 (<0.001)*** | 0.005, 0.01 | −0.001 (0.003) | −0.007, 0.006 |
Notes. UFOV is Useful Field of View Test. Twenty-seven participants had missing baseline UFOV scores and were not included in these subsample models. Driving frequency was the average number of days driven in a week. Driving exposure was the sum of driving in challenging situations (e.g., driven alone, in the rain, etc.) over the previous 2 months. Unstandardized estimates are presented. CI = confidence interval; SPT = speed of processing training.
***p < .001. **p < .01. *p < .05.
Figure 2.
Driving frequency by training and control groups in at-risk participants who received booster sessions. Note: Driving frequency means are presented (range 0–7). Driving frequency was the average number of days driven in a week. Training and control groups did not differ on baseline driving frequency (see Table 1, p > .05). Participants were at-risk for future mobility declines based on the baseline Useful Field of View Test score. Booster training occurred at years 1 and 3. Cohen’s d for speed of processing trained group compared with no-contact control group was 0.53.
Figure 3.
Driving exposure by training and control groups in at-risk participants who received booster sessions. Note: Driving exposure means are presented (range 0–8). Driving exposure was the sum of driving in challenging situations (e.g., driven alone, in the rain, etc.) over the previous 2 months. Training and control groups did not differ on baseline driving exposure (see Table 1, p > .05). Participants were at-risk for future mobility declines based on the baseline Useful Field of View Test score. Booster training occurred at years 1 and 3. Cohen’s d for speed of processing trained group compared with no-contact control group was 0.60.
Discussion
These results reveal that greater amounts of SPT prolong some indices of driving mobility (e.g., driving frequency and driving exposure), mainly among at-risk older adult drivers with poor baseline processing speed. The intervention transferred to greater driving frequency (but not driving exposure or space) in the total sample and translated to greater driving frequency and exposure (but not driving space) in at-risk participants who received booster training. Given the importance of driving for older adults’ well-being and independence, these findings are noteworthy. Moreover, the current study establishes that such transfer effects can still be detected 5 years after the initial intervention and are contingent upon the dose of training received.
In correspondence with prior research, the present findings indicate that transfer of SPT to enhanced driving mobility was primarily found among individuals at-risk for future mobility declines (i.e., with slow baseline processing speed; Edwards, Myers et al., 2009; Roenker et al., 2003). This may be the case because older adults with subtle cognitive difficulties at baseline are most likely to experience larger training effects and immediate transfer of training (Ball et al., 2007). The implications are that transfer of cognitive training may be more likely when targeted toward older adults in most need of training. Additionally, ACTIVE differed from previous SPT studies as it included five standardized and five adaptive sessions rather than 10 adaptive sessions. Continuous adaptation of the training exercises is likely an important factor for training transfer and warrants further investigation (Lövdén et al., 2010).
Our finding that greater doses of SPT transferred to driving frequency across the whole sample is similar to other ACTIVE findings of protective effects of cognitive training among older adults across long periods of time (Ball et al., 2010, 2013; Rebok et al., 2014; Wolinsky et al., 2010). Further investigation of cognitive training mechanisms and dosage effects among impaired and nonimpaired subsamples of older adults is warranted. Although most cognitive training has targeted all older adults, prescribing training type based on initial cognitive difficulties may be the most effective approach.
Of particular note was the impact of the booster sessions (thereby the greatest dose of training) upon driving mobility in participants who were at-risk for reduced driving mobility. The current study is the first to investigate the impact of SPT dosage on self-reported driving outcomes. As compared with the no-contact and active control (memory trained) groups, persons who had the more training (up to 18 sessions) maintained greater levels of self-reported driving frequency across 5 years (Table 3 and Figure 1). Additionally, participants at-risk for mobility declines who received booster sessions had greater driving frequency and exposure as compared with the no-contact control and memory training groups (Table 4 and Figures 2 and 3). This finding likely reflects the effect of a full dose of adaptive training. Studies using 10 sessions of individualized, adaptive SPT, as was used in training sessions 6 through 10 in this study, have found larger training gains and greater transfer to real-world outcomes (Ball et al., 2007; Edwards et al., 2005; Roenker et al., 2003). Further research on the dose and schedule of SPT necessary to produce training gains and transfer is needed.
The training effects reported here are not likely due to social contact, increased self-efficacy, or similar factors resulting from participation in a longitudinal behavioral intervention study. The active control (memory training group) experienced the same amount of study-related social contact and encouragement as did the SPT group, and comparisons between SPT and the active control revealed the same pattern of transfer effects from SPT. This is not surprising as previous research has established that memory training results in improved memory, but does not transfer to speed of processing or driving outcomes (Ball et al., 2010; Willis et al., 2006). Similarly, previous studies have found that older adults randomized to SPT experienced enhanced performance of IADL, including driving, relative to social-contact control conditions (Ball et al., 2010; Edwards, Delahunt et al., 2009; Edwards, Myers et al., 2009; Edwards et al., 2005). Wadley and colleagues (2006) employed both a social- and no-contact control condition when examining SPT and found no differences between these two control groups, but enhanced processing speed among those who were trained as compared with either control condition. Finally, recent work has found that self-efficacy does not impact training gains in SPT (Sharpe, Holup, Hansen, & Edwards, 2014).
These results indicate that SPT impacts driving mobility outcomes differentially. It is important to consider the construction of the self-reported mobility outcomes. Driving frequency, the most robust outcome in terms of training effects, involves recall of how many days per week the participants drove in an average 7 day week. This is a very concrete item which does not rely heavily on memory. Alternatively, driving space asks more complicated questions (e.g., “during the last seven days, but not counting today, have you been to places outside your immediate neighborhood but within your community?”) with timeframes ranging from 1 week to 2 months of recall. Specificity of driving items and length of recall should be considered in self-reported driving measures. It is possible that more simply worded and concrete items may have increased sensitivity when examining change over time, resulting in greater sensitivity to detect training effects. Reliance on broad items over lengthy periods of time (such as reported mileage across a year) should be investigated in future research and compared with more detailed self-reported and objective measures of driving.
Limitations
The primary limitation of the study is that the driving outcomes were self-reported. It should be noted that these measures are valid and reliable among older adults and have been used in previous studies (Edwards, Myers et al., 2009; Ross et al., 2009). Further research should validate the impact of SPT on driving mobility using objective measures such as global positioning systems and geographic information software.
Conclusions
In conclusion, while the results of the current analyses are generally small to moderate in magnitude, any influence of SPT on maintaining driving mobility over a 5-year period is noteworthy. Given the negative psychological and social ramifications of driving reduction and cessation (e.g., risk for nursing home placement), interventions like SPT may contribute to improvements in well-being and quality of life. Small improvements in mobility and independence at an individual level may be aggregated into large benefits for society as a whole.
This study adds important information to the cognitive intervention literature as the first study to demonstrate that SPT can impact driving mobility across a 5-year period. At the same time, it highlighted the importance of dosage (treatment received) analyses, and the impact of booster training sessions on far transfer. Finally, it included both no-contact and active control conditions. These are important considerations in terms of transportation interventions as the no-contact controls can be seen as normal treatment for at-risk older adults while the active control group can be used to investigate if such SPT transfer effects are due to simply participation in a longitudinal behavioral intervention study factors (e.g., social engagement, potential changes in efficacy, etc.). Future research should further investigate the exact dosage of training needed to maintain driving mobility among older adults at-risk for driving cessation or reduced mobility. Elucidating the mechanisms of training is also necessary in order to improve training interventions and produce wider and more generalizable training effects to a larger population. Other cognitive, physical and combined interventions, the best age to begin such interventions, and ways to improve adherence should be investigated. It is likely that a combination of training methods, individualized to meet the needs of the person, provide the best method for maintaining functional independence.
Funding
This work was supported by grants from the National Institute on Aging and the National Institute of Nursing Research to Hebrew Senior Life (U01 NR04507), Indiana University School of Medicine (U01 NR04508), Johns Hopkins University (U01AG14260), New England Research Institutes (U01 AG14282), Pennsylvania State University (U01 AG14263), University of Alabama at Birmingham (U01 AG14289), University of Florida (U01AG14276). These analyses were supported by the National Institute on Aging, Cognitive Training Gains and Mobility Outcomes in ACTIVE (5 R03 AG23078-02), K. K. Ball, PhD, (PI).
Conflict of Interest
Dr. K. K. Ball owns stock in the Visual Awareness Research Group (formerly Visual Awareness, Inc.), and Posit Science, Inc., the companies that market the Useful Field of View Test and Speed of Processing Training software. Posit Science acquired Visual Awareness, and Dr. K. K. Ball continues to collaborate on the design and testing of these assessment and training programs as a member of the Posit Science Scientific Advisory Board. Drs. J. D. Edwards and D. E. Vance have worked as limited consultants to Posit Science, Inc. No other authors have a financial disclosure or conflict of interest.
Acknowledgments
The authors would like to acknowledge the ACTIVE team. The ACTIVE principal investigators included: K. K. Ball, PhD; Richard N. Jones, ScD; Jonathan W. King, PhD; Michael Marsiske, PhD; John Morris, PhD; George Rebok, PhD; Sharon Tennstedt, PhD; Frederick W. Unverzagt, PhD; and Sherry Willis, PhD. We would also like to thank Kerry Sargent and Jeffrey Meadows for their suggestions.
References
- AAA Senior Driving. (2014). Facts & Research Retrieved July 13, 2014 from http://seniordriving.aaa.com/resources-family-friends/conversations-about-driving/facts-research
- Alzheimer’s Association. (2012). 2012 Alzheimer’s disease facts and figures. Alzheimer’s and Dementia, 8, 131–168. 10.1016/j.jalz.2012.02.001 [DOI] [PubMed] [Google Scholar]
- Anstey K. J., Windsor T. D., Luszcz M. A., Andrews G. R. (2006). Predicting driving cessation over 5 years in older adults: Psychological well-being and cognitive competence are stronger predictors than physical health. Journal of the American Geriatrics Society, 54, 121–126. 10.1111/j.1532-5415.2005.00471.x [DOI] [PubMed] [Google Scholar]
- Anstey K. J., Wood J., Lord S., Walker J. G. (2005). Cognitive, sensory and physical factors enabling driving safety in older adults. Clinical Psychology Review, 25, 45–65. 10.1016/j.cpr.2004.07.008 [DOI] [PubMed] [Google Scholar]
- Ball K., Edwards J. D., Ross L. A. (2007). The impact of speed of processing training on cognitive and everyday functions. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences, 62 Spec No 1, 19–31. [DOI] [PubMed] [Google Scholar]
- Ball K., Edwards J. D., Ross L. A., McGwin G., Jr (2010). Cognitive training decreases motor vehicle collision involvement of older drivers. Journal of the American Geriatrics Society, 58, 2107–2113. 10.1111/j.1532-5415.2010.03138.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ball K., Owsley C., Stalvey B., Roenker D. L., Sloane M. E., Graves M. (1998). Driving avoidance and functional impairment in older drivers. Accident; Analysis and Prevention, 30, 313–322. 10.1016/S0001-4575(97)00102-4 [DOI] [PubMed] [Google Scholar]
- Ball K. K., Ross L. A., Roth D. L., Edwards J. D. (2013). Maintaining processing speed improvements with booster sessions: How much training is enough? Journal of Aging and Health, 25(8 Suppl), 65S–84S. 10.1177/0898264312470167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ball K. K., Roenker D. L. (2014). The useful field of view user’s manual, ed., 7.1.0. Punta Gorda, FL: Visual Awareness Research Group, Inc. [Google Scholar]
- Campbell M. K., Bush T. L., Hale W. E. (1993). Medical conditions associated with driving cessation in community-dwelling, ambulatory elders. Journal of Gerontology, 48, S230–S234. 10.1093/geronj/48.4.S230 [DOI] [PubMed] [Google Scholar]
- Edwards J. D., Delahunt P. B., Mahncke H. W. (2009). Cognitive speed of processing training delays driving cessation. The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences, 64, 1262–1267. 10.1093/gerona/glp131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwards J. D., Lunsman M., Perkins M., Rebok G. W., Roth D. L. (2009). Driving cessation and health trajectories in older adults. The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences, 64, 1290–1295. 10.1093/gerona/glp114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwards J. D., Myers C., Ross L. A., Roenker D. L., Cissell G. M., McLaughlin A. M., Ball K. K. (2009). The longitudinal impact of cognitive speed of processing training on driving mobility. The Gerontologist, 49, 485–494. 10.1093/geront/gnp042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwards J. D., Ross L. A., Ackerman M. L., Small B. J., Ball K. K., Bradley S., Dodson J. E. (2008). Longitudinal predictors of driving cessation among older adults from the ACTIVE clinical trial. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences, 63, P6–P12. [DOI] [PubMed] [Google Scholar]
- Edwards J. D., Wadley V. G., Vance D. E., Wood K., Roenker D. L., Ball K. K. (2005). The impact of speed of processing training on cognitive and everyday performance. Aging & Mental Health, 9, 262–271. 10.1080/13607860412331336788 [DOI] [PubMed] [Google Scholar]
- Fonda S. J., Wallace R. B., Herzog A. R. (2001). Changes in driving patterns and worsening depressive symptoms among older adults. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences, 56, S343–S351. 10.1093/geronb/56.6.S343 [DOI] [PubMed] [Google Scholar]
- Jobe J. B., Smith D. M., Ball K., Tennstedt S. L., Marsiske M., Willis S. L., Kleinman K. (2001). ACTIVE: A cognitive intervention trial to promote independence in older adults. Controlled Clinical Trials, 22, 453–479. 10.1016/S0197-2456(01)00139-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lövdén M., Bäckman L., Lindenberger U., Schaefer S., Schmiedek F. (2010). A theoretical framework for the study of adult cognitive plasticity. Psychological Bulletin, 136, 659–676. 10.1037/a0020080 [DOI] [PubMed] [Google Scholar]
- Owsley C., Ball K., McGwin G., Jr., Sloane M. E., Roenker D. L., White M. F., Overley E. T. (1998). Visual processing impairment and risk of motor vehicle crash among older adults. JAMA, 279, 1083–1088. 10.1001/jama.279.14.1083 [DOI] [PubMed] [Google Scholar]
- Owsley C., Stalvey B., Wells J., Sloane M. E. (1999). Older drivers and cataract: Driving habits and crash risk. The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences, 54, M203–M211. 10.1093/gerona/54.4.M203 [DOI] [PubMed] [Google Scholar]
- Rasmusson D. X., Rebok G. W., Bylsma F. W., Brandt J. (1999). Effects of three types of memory training in normal elderly. Aging, Neuropsychology, and Cognition, 6, 56–66. 10:1076.anec.6.1.56.790 [Google Scholar]
- Rebok G., Balcerak L. J. (1989). Memory self-efficacy and performance differences in young and old adults: Effects of mnemonic training. Developmental Psychology, 25, 714–721. 10.1037/0012-1649.25.5.714 [Google Scholar]
- Rebok G. W., Ball K., Guey L. T., Jones R. N., Kim H.-Y., King J. W., Willis S. L. (2014). Ten-year effects of the advanced cognitive training for independent and vital elderly cognitive training trial on cognition and everyday functioning in older adults. Journal of the American Geriatrics Society, 62, 16–24. 10.1111/jgs.12607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roenker D. L., Cissell G. M., Ball K. K., Wadley V. G., Edwards J. D. (2003). Speed-of-processing and driving simulator training result in improved driving performance. Human Factors, 45, 218–233. 10.1518/hfes.45.2.218.27241 [DOI] [PubMed] [Google Scholar]
- Ross L. A., Clay O. J., Edwards J. D., Ball K. K., Wadley V. G., Vance D. E., Joyce J. J. (2009). Do older drivers at-risk for crashes modify their driving over time? The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences, 64, 163–170. 10.1093/geronb/gbn034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salthouse T. A. (1996). The processing-speed theory of adult age differences in cognition. Psychological Review, 103, 403–428. 10.1037/0033-295X.103.3.403 [DOI] [PubMed] [Google Scholar]
- Salvucci D. D. (2006). Modeling driver behavior in a cognitive architecture. Human Factors, 48, 362–380. 10.1518/001872006777724417 [DOI] [PubMed] [Google Scholar]
- Sharpe C., Holup A. A., Hansen K. E., Edwards J. D. (2014). Does self-efficacy affect responsiveness to cognitive speed of processing training? Journal of Aging and Health, 26, 786–806. 10.1177/0898264314531615 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singer J. D., Willett J. B. (2003). Applied longitudinal data analysis: Modeling change and event occurrence. NY: Oxford University Press. [Google Scholar]
- Steinhagen-Thiessen E., Borchelt M. (1999). Morbidity, medication, and functional limitations in very old age. In Baltes P. B., Mayer K. U. (Eds.), The Berlin Aging Study: Aging from 70 to 100. Cambridge, UK: Cambridge University Press. 10.1017/CBO9780511586545.006 [Google Scholar]
- Vance D. E., Wadley V. G., Roenker D. L., Dawson J., Edwards J. D., Rizzo M. (2007). The Accelerate Study: The longitudinal effect of speed of processing training on cognitive performance of older adults. Rehabilitation Psychology, 52, 89–96. 10.1037/0090-5550.52.1.89 [Google Scholar]
- Wadley V. G., Benz R. L., Ball K. K., Roenker D. L., Edwards J. D., Vance D. E. (2006). Development and evaluation of home-based speed-of-processing training for older adults. Archives of Physical Medicine and Rehabilitation, 87, 757–763. 10.1016/j.apmr.2006.02.027 [DOI] [PubMed] [Google Scholar]
- Ware J. E., Jr., Sherbourne C. D. (1992). The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Medical Care, 30, 473–483. [PubMed] [Google Scholar]
- Willis S. L., Tennstedt S. L., Marsiske M., Ball K., Elias J., Koepke K. M., Wright E. (2006). Long-term effects of cognitive training on everyday functional outcomes in older adults. JAMA, 296, 2805–2814. 10.1001/jama.296.23.2805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolinsky F. D., Mahncke H., Vander Weg M. W., Martin R., Unverzagt F. W., Ball K., Tennstedt S. L. (2010). Speed of processing training protects self-rated health in older adults: Enduring effects observed in the mulit-site ACTIVE randomized controlled trial. International Psychogeriatrics, 22, 470–478. http://dx.doi.org/10.1017/S1041610209991281 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolinsky F. D., Vander Weg M. W., Martin R., Unverzagt F. W., Ball K. K., Jones R. N., Tennstedt S. L. (2009). The effect of speed-of-processing training on depressive symptoms in ACTIVE. The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences, 64, 468–472. 10.1093/gerona/gln044 [DOI] [PMC free article] [PubMed] [Google Scholar]