Abstract
Background
Early post-discharge follow-up after heart failure (HF) hospitalization is associated with lower 30-day readmission rates.
Objectives
Evaluate an inter-hospital collaborative approach to improve 7-day post-discharge follow-up (7dFU) rates and reduce 30-day readmissions in HF patients.
Methods
Observational analysis of Medicare HF patients discharged from 10 collaborating hospitals (CH) participating in the Southeast Michigan See You in 7 Collaborative. We compared pre-intervention (May 1, 2011–April 30, 2012) and intervention (May 1, 2012–April 30, 2013) 7dFU, unadjusted 30-day readmission, risk-standardized 30-day readmission (RSRR), and Medicare payments in CH and Michigan non-participating hospitals (NPH).
Results
7dFU increased but remained low in both groups (CH: 31.1% to 34.4%, p<0.001; NPH: 30.2% to 32.6%, p<0.001). During the intervention period, unadjusted readmissions significantly decreased in both groups (CH: 29.0% to 27.3%, p<0.001; NPH: 26.4% to 25.8%, p=0.004); mean RSRR decreased more in CH than NPH (CH: 31.1% to 28.5%, p<0.001; NPH: 26.7% to 26.1%, p=0.02; p=0.015 for inter-group comparison). Findings were similar when CH was matched 1:1 with similar NPH. Combined Medicare payments for inpatient and 30 days of post-discharge care decreased by $182 in the CH and by $63 in NPH (per eligible HF discharge).
Conclusions
See you in 7 Collaborative participation was associated with significantly lower 30-day readmission and Medicare payments in HF patients. Increases in 7dFU were modest, but associated processes aimed at this goal may have improved the transition from inpatient to outpatient care. Regional hospital collaboration to share best practices could potentially reduce HF readmissions and associated costs.
Keywords: Heart Failure, Readmissions, Outcomes, Care Transitions
INTRODUCTION
Heart failure (HF) affects over 5 million adults and is a leading cause of hospitalizations among those 65 years and older in the United States (1). For patients hospitalized with HF, readmissions following hospital discharge are common and can indicate healthcare inefficiencies (2, 3). The Medicare Payment Advisory Commission estimates that preventable readmissions account for at least $12 billion of Medicare annual spending (3, 4). Approximately 50% of readmissions are possibly or probably preventable (5), with potentially remediable factors including inadequate transitions from inpatient to outpatient care (3). To address these issues, the American College of Cardiology and the Institute for Healthcare Improvement launched the national Hospital-to-Home Initiative in 2009. Hospital-to-Home aims to reduce 30-day, all-cause, risk-standardized readmission rates for patients discharged with HF or acute myocardial infarction by creating a rapid learning community where experts and clinical providers at multiple levels of care share best practices.(6). One area of focus for Hospital-to-Home is promoting early post-discharge outpatient follow-up, which is associated with lower risk for 30-day readmission in HF patients.(7)
In 2011, the Greater Detroit Area Health Council, the American College of Cardiology's Michigan Chapter, the Michigan Peer Review Organization (Michigan's Quality Improvement Organization), and 11 previously non-affiliated hospitals teamed up to establish the Southeast Michigan “See You in 7” Collaborative, with the common goals to increase 7-day post-discharge follow-up and reduce all-cause 30-day readmission rates in HF patients (7). In this study, we examine the relationship between SY7 Collaborative participation and the rates of 7-day follow-up and 30-day readmissions in Medicare fee-for-service HF patients discharged from the collaborating hospitals (CH), and compare these findings to secular statewide trends in the remaining 82 Michigan non-participating hospitals (NPH).
METHODS
Hospital Recruitment and Group Definition
In 2011, Great Detroit Area Health Council conducted open recruitment of hospitals in Southeast Michigan for the SY7 Collaborative utilizing recruitment letters, teleconferences, and face to face scheduled meetings with stakeholders to discuss the expectations of the project. As a result, 11 urban and suburban acute care hospitals, including large teaching (n=7), large non-teaching (n=3), and medium urban (n=1) hospitals, enrolled in the year-long program. A large teaching Veterans Affairs hospital participated in the collaborative activities, but since comparable outcomes data could not be obtained through Michigan Peer Review Organization, only non-federal hospitals are included in this analysis. Michigan Peer Review Organization privately provided the CH with quarterly 7-day follow-up and 30-day readmission data. Each institution was de-identified, and only aggregate data reported to the participants.
Intervention and Intended Improvement
The intervention period was divided into 3 phases over a period of 1 year: pre-implementation (May 1, 2012 through July 31, 2012), test-intervention (August 1, 2012 through January 31, 2013), and evaluation (February 1, 2013 through April 30, 2013). Table 1 shows the timeframes, scheduled activities for the collaborative, and the evaluation plan. Over the 12-month intervention, See You in 7 Collaborative activities included quarterly face-to-face meetings and several telephone conferences/webinars; participating hospitals submitted a total of 8 assignments for review and discussion.
Table 1.
Southeast Michigan See You in 7 Collaborative Time Periods, Methods, Tools, and Evaluation Plan
| Focus | Methods/Tools | Evaluation Plan | Meetings |
|---|---|---|---|
| Pre-Implementation period May - July 2013 |
Hospitals: Establish collaborative partnerships among hospitals serving Southeast Michigan beneficiaries Hospital-to-Home “SY7” Toolkit |
Gap analysis | Kickoff Meetings 2 Conferences Calls/Webinars |
|
Planning Team Activity Pre-Implementation Data Submission CH Selection of “See You in 7” Process Measures |
|||
| Test- Intervention period Aug - Jan 2013 |
SY7 Toolkit process goals: Identify HF patients prior to discharge: |
Proportion of HF patients identified prior to discharge | 2 Quarterly Meetings 4 Conferences Calls/Webinars |
| Schedule and document a follow-up visit with cardiologist or PCP that takes place within 7 days of discharge. | Proportion of discharges with scheduled 7-day follow-up visit with Cardiologist or PCP | ||
| Provide all patients with documentation of the scheduled follow-up appt. | Proportion of patients with documentation of 7-day follow-up appointments | ||
| Identify and address barriers to keeping appointment. | Follow-up phone calls or risk assessments conducted to identify barriers | ||
| Ensure all HF patients arrive at scheduled appointment within 7 days of discharge | Proportion of patients who had 7-day follow-up appointments scheduled Proportion of patients who kept scheduled 7-day follow-up appointments. |
||
| Make discharge summary available to follow-up health care providers for all HF patients. | Proportion of discharge summaries transferred to PCP within 24 hours of discharge. | ||
|
Planning Team Activity Collaborative hospitals shared best practices. Quarterly Progress Reports |
|||
| Evaluation period Feb – April 2013 |
Data and Information - Medicare fee-for-service claims data, aggregate and hospital level descriptive readmission and 7-day follow-up reports Policy - Hospital Compare Reporting, Hospital-wide Lessons learned shared among CH Quarterly Progress Report Post-Implementation Data Submission |
Continued assessment and improvement based on rates of 7-day follow-up. | 2 Conferences Calls/Webinars 1 Quarterly Meeting |
Abbreviations: CH, collaborating hospitals; HF, heart failure; PCP, primary care provider
During the pre-implementation phase, CH reviewed baseline data, conducted gap analysis, identified process improvement measurements, and selected strategies from the Hospital to Home “See you in 7” Toolkit (6). During the test-intervention period, based on the hospital-specific gap analysis, each collaborating hospital selected 1 or several of the 7 care process goals (Table 1) from the Toolkit to focus efforts and measure progress. Once these metrics were identified, CH conducted ‘gap analyses’ of their current care processes to identify areas of need, then designed and implemented institution-specific quality improvement plans. During the evaluation phase, the CH continued implementation of quality improvement processes and received feedback from Michigan Peer Review Organization on 7-day follow-up and 30-day readmissions. Further information on the See You in 7 structure is contained in Supplementary Table 1 and in a recently published manuscript describing the Collaborative process.(8)
The pre-specified evaluation metrics for the See You in 7 Collaborative were changes between the pre-intervention period (May 1, 2011 through April 30, 2012), and the intervention period (May 1, 2012 through April 30, 2013) in 7-day follow up and unadjusted 30-day readmission rates for HF patients discharged from the CH. Preliminary results for these metrics have recently been reported.(8) For this study, we also calculated and examined changes in mean risk-standardized 30-day all-cause readmission rates (RSRR), and then evaluated differences in these rates between CH, non-participating hospitals, and matched non-participating hospitals (see below for information on matching). We also compared unadjusted 30-day readmission rates and mean RSRR for patients with and without 7-day follow up visit.
Outcome Definitions and Data Acquisition
We linked Medicare FFS Standard Analytic Inpatient and enrollment files to outpatient claims using beneficiary health insurance identification codes to identify eligible discharges, determine 7-day follow up rates, and calculate all cause 30-day readmission rates for the period of May 1, 2011 through April 30, 2013. Eligible discharges were defined as those with diagnosis of HF as determined by the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes. ICD-9-CM codes were identical to those used by the Centers for Medicare and Medicaid Services Hospital Compare public reporting program for HF (9). We included all Medicare fee-for-service and dual eligible claims. Provider Certification Numbers were used to extract and aggregate 7-day follow up and 30-day readmission rates. We used patient-level Medicare payment data to estimate the HF-related costs at CH and NPH.
A 7-day follow up visit was defined as claims identified for any physician outpatient visit within 7 days of discharge for HF patients regardless of provider type. All-cause 30-day readmission was defined as eligible discharges that readmitted to the same or different hospital for any diagnosis within 30-days of discharge. Multiple readmissions within 30 days were captured in this measure as each readmission counted as an index admission, and a subsequent admission within a 30-day period was counted as a readmission for the previous claim. Admissions involving beneficiaries who expired during inpatient hospitalization, were readmitted for rehabilitation services, had less than 30-day Medicare fee-for-service enrollment post inpatient discharge, or were transferred on the day of discharge to another acute care or critical access hospital were excluded from analysis.
Analysis Methods
Descriptive statistics were used to describe demographic characteristics and key clinical variables of the sample. The chi-square test was conducted to test for changes in 7-day follow up and unadjusted 30-day readmission rates between the pre-intervention and intervention periods for the CH and NPH. The within-group RSRR was compared between pre-intervention and intervention using paired t-tests. The inter-group RSRR was compared between collaborative hospitals and non-participating hospitals using 2-sample t-tests. Throughout the analyses, the .05 level on a 2-sided design-based test represented the cut-off value for assessing statistical significance. All analyses were conducted with SAS 9.13 (SAS Institute Inc., Cary, NC).
The HF cohorts were risk-standardized using the Centers for Medicare and Medicaid Services claims-based model used for public reporting of RSRR. This hierarchical logistic regression modeling strategy accounts for within-hospital correlation of the observed readmission rates and reflects the assumption that after adjustment for patient risk and sampling variability, remaining variation is due to hospital quality. The RSRR were obtained as the ratio of the number of “predicted” to “expected” readmissions, multiplied by the Michigan unadjusted readmission rate for the time period in question. The predicted number of readmissions for each hospital was estimated using the risk model given its own patient mix and with its own hospital-specific intercept. The expected number of readmissions for each hospital was estimated with its own patient mix and the average hospital-specific intercept based on all hospitals in our sample (9, 10).
In order to estimate the economic impact of See You in 7 Collaborative participation, we defined the total number of readmissions prevented for each hospital by multiplying the absolute percentage reduction in 30-day readmissions between the pre-intervention and intervention periods by the total number of eligible HF discharges during the intervention period. We calculated cost savings related to readmission via multiplying the average Medicare payment per HF hospitalization by the number of readmissions prevented at that hospital during the intervention period. To evaluate outpatient costs at each hospital, we derived the change (between the pre-intervention and intervention periods) in average Medicare outpatient payments over the first 30 days after hospital discharge. We multiplied this change in outpatient payments by the total number of eligible HF discharges at that hospital during the intervention period.
Additional Analyses
We performed several additional analyses to clarify our results. First, while Hospital-to-Home recommends follow-up within 7 days of hospital discharge, follow-up within 14 days is also associated with reduced 30-day readmission rates.(6, 8) We obtained 14-day follow-up rates for all hospitals and evaluated associations with 30-day readmission rates as above. Hospitalized older adults have high risk for adverse events that could be reduced through hospital-wide efforts to improve care transitions regardless of admitting diagnosis (11). Therefore, we evaluated if See you in 7 Collaborative participation, a HF patient-specific hospital-wide effort, affected readmission rates for non-HF diagnoses.
Finally, we re-analyzed HF outcomes at the CH and 1:1 matched NPH, using Blue Cross Blue Shield hospital peer group categories to match hospitals within the same geographic region having similar size, teaching status, patient demographics, and HF patient volume. We compared 7-day follow up rates, unadjusted 30-day readmission rates, and RSRR between CH and matched NPH as described above.
RESULTS
Descriptive Characteristics
Approximately 20% of statewide 30-day HF readmissions at baseline were from the CH, indicating a prime opportunity to make an impact on readmission reduction. Each collaborating hospital chose at least two “See You in 7” Toolkit process goals (Table 1), with the overall breakdown as follows: scheduling 7-day follow up visits, 9 hospitals; providing 7-day follow up appointment documentation, assessing and addressing barriers to 7-day follow up, and confirming that 7-day follow up appointment was attended, 6 hospitals each; making discharge summaries available to outpatient providers, 5 hospitals; identification of HF patients early in the hospital stay, 4 hospitals.
Table 2 contains information on the eligible HF discharges and patient exclusions for the study sample at CH and NPH during both study periods. Of note, in-hospital mortality did not significantly change between the pre-intervention and intervention time periods. For the 10 CH, the number of eligible HF discharges ranged from 1203 to 4359 and in the 10 matched NPH, from 1046 to 6636. The range of unadjusted 30-day readmission rates during the pre-intervention period was similar for CH and matched NPH (25.5% to 32.7% vs. 24.8% to 34.2%). Table 3 shows key demographic and clinical characteristics for the CH and NPH. On average, the CH cared for an older patient population than the NPH, with slightly higher proportion of female and minority patients. Additional information on HF patient comorbidities and clinical characteristics relevant to the RSRR risk model is contained in Supplementary Table 2.
Table 2.
Eligible heart failure discharges at collaborating and non-participating hospitals
| Hospital group/time interval | Total Sample with HF | Final Sample | ||||||
|---|---|---|---|---|---|---|---|---|
| # of hospitals | Total patients | Age<65 y | In-Hospital Deaths | Transfers Out | Discharge AMA | N | % | |
| CH Pre-Intervention | 10 | 28238 | 14.98% | 3.63% | 1.39% | 0.59% | 26744 | 94.7 |
| CH Intervention | 10 | 26358 | 14.89% | 3.91% | 1.56% | 0.56% | 24849 | 94.3 |
| NPH Pre-Intervention | 82 | 100866 | 16.68% | 4.30% | 2.12% | 0.64% | 93928 | 94.5 |
| NPH Intervention | 82 | 99391 | 16.60% | 4.42% | 2.14% | 0.62% | 92321 | 92.9 |
| Matched NPH Pre-Intervention | 10 | 28722 | 16.64% | 3.79% | 1.55% | 0.61% | 27049 | 94.2 |
| Matched NPH Intervention | 10 | 27350 | 16.03% | 3.74% | 1.62% | 0.59% | 25709 | 94.0 |
Abbreviations: AMA, against medical advice; CH: collaborating hospitals; HF: heart failure; NPH: non-participating hospitals
Table 3.
Selected demographic and clinical characteristics at collaborating and non-participating hospitals
| Population Segment | CH Total Discharges Eligible for Readmission | NPH Total Discharges Eligible for Readmission | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Pre-intervention | Intervention | Pre-intervention | Intervention | ||||||
| N | % | N | % | N | % | N | % | ||
| Race | White | 19,617 | 73.35 | 17,999 | 72.43 | 72,709 | 77.41 | 71,451 | 77.39 |
| Black | 6,677 | 24.97 | 6,294 | 25.33 | 19,115 | 20.35 | 18,724 | 20.28 | |
| Other | 450 | 1.68 | 556 | 2.24 | 2,104 | 2.24 | 2,146 | 2.32 | |
| Age | <65 | 3,974 | 14.86 | 3687 | 14.84 | 15,559 | 16.56 | 15,201 | 16.47 |
| 65-74 | 6,333 | 23.68 | 6164 | 24.81 | 23,868 | 25.41 | 24,186 | 26.20 | |
| >75 | 16,437 | 61.46 | 4,511 | 27.44 | 54,501 | 58.02 | 52,934 | 57.34 | |
| Gender | F | 15,474 | 57.86 | 14,145 | 56.92 | 52,122 | 55.49 | 50,853 | 55.08 |
| M | 11,270 | 42.14 | 10,704 | 43.08 | 41,806 | 44.51 | 41,468 | 44.92 | |
| Length of Index Admission | < 4 days | 9,264 | 34.64 | 8,712 | 35.06 | 33,667 | 35.84 | 32,915 | 35.65 |
| 4-8 days | 12,297 | 45.98 | 11,441 | 46.04 | 41,399 | 44.08 | 41,372 | 44.81 | |
| > 8 days | 5,183 | 19.38 | 4696 | 18.9 | 18,862 | 20.08 | 18,034 | 19.53 | |
| # of Admits in prior 3 months | 0 | 13,808 | 51.63 | 13,335 | 53.66 | 51,502 | 54.83 | 51,531 | 55.82 |
| 1 | 7,433 | 27.79 | 6,902 | 27.78 | 25,396 | 27.04 | 24,883 | 26.95 | |
| 2 | 3,439 | 12.86 | 2948 | 11.86 | 10,721 | 11.41 | 10,338 | 11.20 | |
| >2 | 2,064 | 7.72 | 1664 | 6.7 | 6,309 | 6.72 | 5,569 | 6.03 | |
| Total | 26,774 | 24,849 | 93,928 | 92,321 | |||||
Abbreviations: CH, collaborating hospitals; NPH, non-participating hospitals
7-Day Follow Up and 30-day Readmission Rates
The primary findings of the study are shown in Table 4. The See You in 7 Collaborative's primary process goal was to improve 7-day follow up rates between the pre-intervention and intervention periods. Modest but statistically significant increases in 7-day follow up, as well as in 14-day follow up, occurred in both the CH and the NPH during the intervention time period.
Table 4.
Follow-up and 30-day readmission rates in collaborating, non-participating, and matched non-participating hospitals
| Rates | CH | NPH | Matched NPH | |||
|---|---|---|---|---|---|---|
| Pre-intervention | Intervention | Pre-intervention | Intervention | Pre-intervention | Intervention | |
| Post-discharge follow-up | ||||||
| 7-day follow-up† | 31.1% | 34.4%*** | 30.2% | 32.6%*** | 31.5% | 33.8%*** |
| 14-day follow-up† | 47.2% | 50%*** | 46.3% | 47.9%*** | 47.3% | 48.7%** |
| Overall 30-day readmission | ||||||
| Unadjusted 30-day readmission† | 29.0% | 27.3%*** | 26.4% | 25.8%** | 29.8% | 28.9%** |
| Mean 30-day RSRR§ | 31.1% | 28.5%*** | 26.7% | 26.1%* | 31.0% | 29.9% |
| Weighted 30-day RSRR† | 30.7% | 28.2% | 28.5% | 27.4% | 31.1% | 29.9% |
| Readmission by follow-up status | ||||||
| Mean RSRR, with 7-day follow-up§ | 31.1% | 28.5% | 26.7% | 26.1% | 31.0% | 29.9% |
| Mean RSRR, no 7-day follow-up§ | 31.1% | 28.5% | 27.0% | 26.0% | 31.0% | 29.9% |
| Mean RSRR, with 14-day follow-up§ | 31.1% | 28.5% | 26.7% | 26.1% | 31.0% | 29.9% |
| Mean RSRR, no 14-day follow-up§ | 31.1% | 28% | 27.0% | 26.0% | 31.0% | 29.9% |
| Inter-group comparison | ||||||
| Pre-post Δ mean RSRR¥ | 0.0259 | 0.0065* | 0.0112* | |||
| Pre-post Δ mean RSRR, with 7-day follow-up¥ | 0.026 | 0.0064* | 0.0111* | |||
Abbreviations: CH, collaborating hospitals; NPH, non-participating hospitals; RSRR, risk-standardized readmission rate
Note:
p < .05
p< .01
p < .001
Pre-post comparison
for χ2
for 2-sample t-test
inter-group comparison:
for 2-sample t-test comparison with CH group
In the CH, unadjusted 30-day readmissions were substantially more common than in the NPH during the pre-intervention period (X2=72.57; p<0.001) but similar to those in matched NPH (X2=3.56; p=0.06). The unadjusted 30-day readmission rate in HF patients significantly decreased during the intervention period in CH (p<0.001) and statewide NPH(p=0.004), but not in matched NPH (p=0.06). 30-day readmission rates were lower in non-HF patients and decreased similarly in all three hospital groups during the intervention period (CH: 18.8 to 18.1%, NPH 17.4 to 16.8%, matched NPH 19.6% to 18.9%).
Hospital 30-day Risk Standardized Readmission Rates
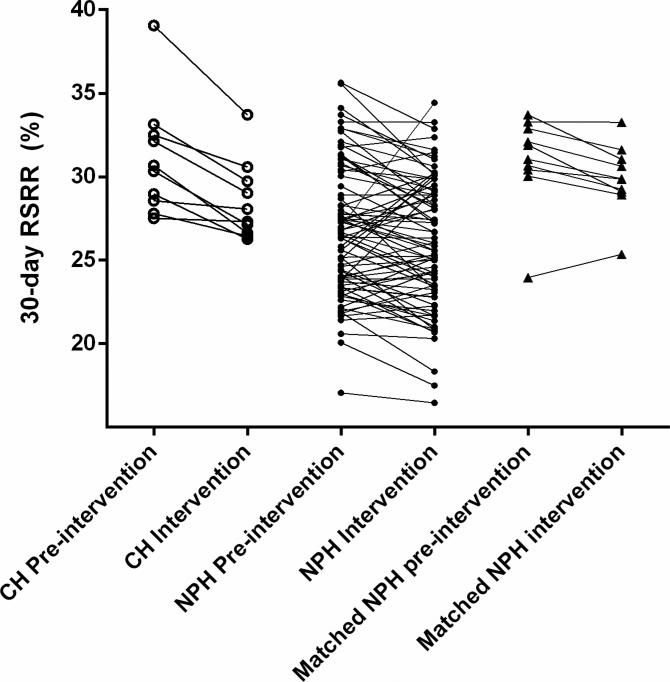
The overall discrimination of the RSRR model was similar to that in the original derivation cohort, with c-statistic of 0.60 for 30-day readmission in both time periods at CH and NPH. Again, results are shown in Table 4. As with unadjusted 30-day readmission rates, RSRR in CH were higher at baseline than in the NPH, but comparable to those in matched NPH. The mean RSRR for the CH decreased significantly during the intervention period (relative improvement ratio/RIR=8.3%; p < .001). In NPH, the mean RSRR also improved slightly during the intervention period (RIR=2.5%; p=0.02), but significantly less so than in the CH (p=0.015). Mean RSRR did not significantly decline during the intervention period in matched NPH (RIR=3.6%, p=0.32)
When mean RSRR was weighted by each contributing hospital's number of eligible HF discharges, during the intervention period the RSRR ‘gap’ between CH and NPH narrowed, and that between collaborating and matched NPH further widened (Table 4). The Figure demonstrates that RSRR decreased in all collaborative hospitals during the intervention period. Individually, the NPH had variable changes in the RSRR.
Figure.
Changes in risk-standardized 30-day readmission in collaborating vs. non-participating hospitals
Abbreviations: CH, collaborating hospitals; NPH, non-participating hospitals; RSRR, risk-standardized 30-day readmission rate
Relationship between follow-up and 30-day readmission
As seen in Table 4, unadjusted 30-day readmission rates for patients with 7-day follow up were significantly higher than those who did not attend 7-day follow up appointments. However, risk-standardization eliminated these baseline readmission rate differences between patients with and without 7-day follow up in all three hospital groups. Moreover, within each hospital group, improvements in mean RSRR during the intervention period were nearly identical whether or not patients attended 7-day follow up visits. Results were similar for 14-day follow up, i.e. baseline RSRR and reductions in RSRR during the intervention were unrelated to whether or not patients attended 14-day follow up appointments.
Medicare Payments for Care
Total Medicare payments for acute HF care and post-discharge outpatient care decreased substantially between the pre-intervention and intervention periods at the 10 CH, with overall reduction of $4.5M ($451,000 per hospital). In the much larger group of 82 NPH, Medicare payments decreased $5.8M ($70,000 per hospital) over the same time period. The average decrease in Medicare payment per discharged Medicare HF beneficiary was $182 at CH and $63 at NPH.
DISCUSSION
The Southeast Michigan See you in 7 Collaborative aimed to increase rates of early outpatient follow-up after HF hospital discharge, and reduce 30-day readmission rates in Medicare HF patients. In our analysis, See You in 7 Collaborative participation was associated with only modest improvement in early post-discharge follow up rates. Both CH and NPH reduced readmissions during the intervention period, likely influenced by federal financial penalties for excessive readmissions that took effect in 2013. However, 30-day readmission rates and overall Medicare payments for HF care decreased substantially more in CH than statewide non-participating hospital comparators.
In recent years, national trends toward shorter hospital length of stay in complex patients with multi-morbidity illness have been associated with increased 30-day all-cause readmission rates (12). Recently implemented financial penalties for excessive readmissions have focused attention on preventable causes of rehospitalization. According to the American Heart Association and the American College of Cardiology, an early post-acute follow up visit following an inpatient HF discharge can reduce preventable readmissions (13). However, even at higher-performing hospitals the majority of Medicare HF patients are not evaluated by a physician within 7 days of hospital discharge (7).
The regional See You in 7 Collaborative effort engaged providers from neighboring, and often directly competing, health systems serving HF patients at several levels of care. The collaborative created a multidisciplinary learning and action network designed to test best practices, quantify findings, share information, and spread evidence. In spite of these extensive efforts, 7-day follow up rates at CH during the intervention period remained below the national median of 38%, and increases in 14-day follow up were similarly small (7). Our observations clearly illustrate the significant challenge of coordinating early post-acute care follow-up. We speculate that inter-hospital collaboration did not produce the desired improvements because individual hospitals can face entirely different barriers to 7-day follow up (e.g. insufficient outpatient provider availability, communication with and between multiple separate outpatient practice settings, different patient and community characteristics).
Prior root-cause analysis among the Southeast Michigan recruited communities has identified several obstacles to timely follow-up care following HF hospitalization. Individual and system barriers in this region include lower health care access (14), lack of transportation, and poorer patient activation, all underlying determinants of poor health. The Medicare patient mix in the CH includes a larger proportion of dual-eligible beneficiaries compared to the state as a whole. Hospitals in this area also serve more patients with complex healthcare and socio- economic needs. Other causes include clustering of multiple health systems within close proximity yet poor designation of primary care providers and access to specialists. Patients in this region often bounce between hospitals, increasing the likelihood of poor care coordination after hospital discharge. These same challenges to 7-day follow up also increase the risk for 30-day readmission (15).
By working to address the Hospital to Home ‘See You in 7’ toolkit process goals in an iterative and collaborative manner, CH self-identified deficient areas, learned potentially useful strategies from peer hospitals, and appointed champions to implement and evaluate solutions in the context of a multidisciplinary team. For example, the collaborating hospital established methods to prospectively identify hospitalized patients with HF early in the hospital stay, e.g. by tracking admitting diagnosis of shortness of breath and administration of diuretics in the emergency department or during the first hospitalization day, obtaining updates from regular case management meetings, and incorporating multi-disciplinary rounds. After identifying patients, the collaborative hospitals worked to increase direct interaction between outpatient team members, patients and families during the hospital stay in order to assess barriers to early follow-up. Many CH incorporated discharge summaries into the electronic medical records, and patients were provided copies of their discharge summaries to take with them to their first outpatient appointment. A designated staff member at collaborating hospital followed up with the patients and outpatient providers to document successful 7-day follow up visits or investigate reasons why the appointment did not take place. Overall, this process engaged patients and caregivers, and helped both sides better understand barriers to care and address them prior to and following discharge. These efforts likely enhanced care coordination for the medically and socioeconomically vulnerable Medicare HF patients served by the CH, and may have contributed to the observed decreases in 30-day readmission.
One additional finding of our analysis merits further discussion. Early post-discharge follow-up is described by Hospital to Home as an evidence-based strategy to reduce readmissions.(6) While hospitals in the highest quartile of 7-day follow up rates tend to have lower 30-day readmission rates,(7) no prior multicenter studies have reported the direct effects of early follow-up on RSRR. Previous work by others suggests that the timing of early post-discharge outpatient visits is confounded by severity of illness (16). Indeed, we observed consistently higher unadjusted 30-day readmission rates in patients presenting for 7-day follow up than in those who did not have early follow up.
Reductions in 30-day readmission rates could occur without substantially increasing the number of 7-day follow up visits is if higher-risk HF patients were specifically targeted for early discharge follow-up. Recognizing that post-discharge resources are limited, Amarasingham and colleagues recently reported impressive results with this strategy (17). In our study, CH used a variety of methods to identify high-risk HF patients who might benefit from 7-day follow up, including previously published instruments such as the BOOST (Better Outcomes for Older adults through Safe Transitions) tool, previously associated with readmission reduction in a multi-hospital collaborative (18). However, following risk standardization with the model currently used for public reporting, 30-day readmission rates were identical pre-intervention and decreased identically during the intervention regardless of whether or not patients attended a 7-day follow up visit. This finding was remarkably consistent across CH, NPH and matched NPH (Table 4), suggesting that other aspects of care beyond simply attending a 7-day follow up appointment contributed to readmission reduction at CH.
Limitations
Administrative data sets were used to calculate the outcomes of interest: 7-day follow up, 30-day readmission, and cost. Administrative data does not provide information on the functional status of beneficiaries, severity of illness, or the quality of care delivered by the post-hospital care provider(s). We did not have financial data beyond Medicare payments, and our analysis therefore does not include non-Medicare related expenditures by hospitals aimed at HF readmission reduction.
The limitations of observational analyses must be considered, including bias due to unmeasured confounding variables and lack of random assignment for the intervention and comparison groups. These limitations are similar to other observational studies. In order to reduce these biases as much as possible, we also evaluated outcomes at closely matched NPH. We compared multiple outcomes between hospital groups, making a type I error (incorrect rejection of the null hypothesis) more probable. However, given the consistent nature of the observed differences between hospital groups across these outcomes (Table 4), type I error seems unlikely to completely explain our findings.
The open recruitment nature of the project introduced selection bias. Recruited hospitals that chose not to participate cited competing priorities, reduced revenue, and limited staff and time as barriers to participation. As seen in the baseline data, CH presented higher baseline early follow up rates and 30-day readmission rates compared to the NPH. As such, the CH may be characterized as highly motivated and possessing increased readiness to address the problem compared to other hospitals. In addition, higher baseline rates present an opportunity for regression to the mean rather than true improvement. However, 1:1 matched NPH in the same geographic region had similar baseline 7-day follow up, unadjusted 30-day readmission rates, and RSRR but did not experience similar declines in readmission during the intervention period.
Given the observational nature of the study, we cannot confirm that improvements in 7-day follow up or 30-day readmission rates directly resulted from See You in 7 Collaborative participation. As each hospital created an individualized plan based on gap analysis of shortcomings and resources, we are unable to formally report the degree of exposure of the intervention components in the collaborative hospitals. Our results may not be generalizable to hospitals outside of the study sample.
Clinical Implications
Despite an intensive and sustained multidisciplinary effort, the Southeast Michigan See You in 7 Collaborative only modestly improved 7-day follow up rates for hospitalized Medicare HF patients beyond secular trends. These disappointing results do not support inter-hospital collaboration focused specifically on this goal. However, Collaborative data on readmission rates were more promising, as the absolute decrease in 30-day RSRR during the intervention period was four times greater in CH than NPH and twice as great at CH as in closely matched NPH. Reductions in RSRR in all hospital groups were unrelated to whether or not patients had 7-day follow up, suggesting that other improvements in care coordination were responsible. Further study is needed to clarify the most helpful aspects of inter-hospital collaboration, assess the sustainability of readmission reduction following participation, and understand the optimal resource allocation to 7-day follow up vs. other aspects of the post-discharge transition.
CONCLUSIONS
Hospital participation in the Southeast Michigan See You in7 Collaborative was associated with substantial reductions in 30-day readmission rates and Medicare payments related to HF care. Increases in post-discharge 7-day follow up were modest, but associated processes aimed at this goal may have improved the overall transition from inpatient to outpatient care. Our study suggests that regional hospital collaboration to share best practices can be an effective strategy to reduce HF readmissions and associated costs.
Supplementary Material
CLINICAL PERSPECTIVES.
Clinical Competencies: An inter-hospital collaborative approach only modestly increased early post-discharge follow-up from heart failure hospitalization, but was associated with substantial reductions in 30-day readmission rates and Medicare payments. Collaborating hospitals performed system-specific gap analysis to identify challenges and limitations in processes related to transitions of care, then implemented and evaluated quality improvement measures recommended by the national Hospital-to-Home initiative.
Transitional Outlook: Each collaborating hospital developed its own targets and strategies for improvement based on its specific needs and resources. Further study is needed to determine which aspects of the collaborative process would be helpful in other regions and patient populations.
ACKNOWLEDGMENTS
The authors are grateful for the invaluable assistance of Joy Pollard, RN, PhD, ACNP (St. Joseph Mercy Oakland Hospital, Pontiac, MI), Lisa Mason, RN, BSN and Annie Melia, BS (Greater Detroit Area Health Council), Shilpa Patel, BS (American College of Cardiology), Robert Yellan MPH, JD, FACHE (MPRO), Diane Smith RN, and Prashanti Boinapally MS.
Funding: Funded in part by the Robert Wood Johnson Foundation. SLH is supported by NIH/NHLBI K23HL109176.
Abbreviations
- CH
collaborating hospitals
- HF
heart failure
- NPH
non-participating hospitals
- RIR
relative improvement ratio
- RSRR
risk-standardized 30-day readmission rate
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures: None
REFERENCES
- 1.Go AS, Mozaffarian D, Véronique RL, et al. Heart disease and stroke statistics—2013 update: a report from the American Heart Association. Circulation. 2014;127:e6–e245. doi: 10.1161/CIR.0b013e31828124ad. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dharmarajan K, Hsieh AF, Lin Z, et al. Diagnosis and timing of 30-day readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia. JAMA. 2013;309:355–63. doi: 10.1001/jama.2012.216476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Medicare Payment Advisory Commission . Report to the Congress: promoting greater efficiency in Medicare. MedPAC; Washington, DC: 2007. [October 2, 2013]. http://www.caretransitions.org/documents/MedPAC%20report.pdf. [Google Scholar]
- 4.Henry J, Kaiser Family Foundation [September 15, 2014];The facts on Medicare spending and financing. 2014 Jul 28; http://kff.org/medicare/fact-sheet/medicare-spending-and-financing-fact-sheet/
- 5.Krumholz HM, Parent EM, Tu N, et al. Readmission after hospitalization for congestive heart failure among Medicare beneficiaries. Arch Intern Med. 1997;157:99–104. [PubMed] [Google Scholar]
- 6.American College of Cardiology [February 16, 2015];Hospital to Home. http://cvquality.acc.org/H2H.
- 7.Hernandez AF, Greiner MA, Fonarow GC, et al. Relationship between early physician follow-up and 30-day readmission among Medicare beneficiaries hospitalized for heart failure. JAMA. 2010;303:1716–22. doi: 10.1001/jama.2010.533. [DOI] [PubMed] [Google Scholar]
- 8.Pollard J, Oliver-McNeil SO, Patel S, Mason L, Baker H. Impact of the development of a regional collaborative to reduce 30-day heart failure readmissions. J Nurs Care Qual. 2015 doi: 10.1097/NCQ.0000000000000116. in press. [DOI] [PubMed] [Google Scholar]
- 9.Keenan PS, Normand S-LT, Lin Z, et al. An administrative claims measure suitable for profiling hospital performance on the basis of 30-day all-cause readmission rates among patients with heart failure. Circ Cardiovasc Qual Outcomes. 2008;1:29–37. doi: 10.1161/CIRCOUTCOMES.108.802686. [DOI] [PubMed] [Google Scholar]
- 10.Daniels MJ, Gatsonis C. Hierarchical generalized linear models in the analysis of variations in health care utilization. J Am Stat Assoc. 1999;94:29–42. [Google Scholar]
- 11.Krumholz HM. Post-hospital syndrome — an acquired, transient condition of generalized risk. New Engl J Med. 2013;368:100–2. doi: 10.1056/NEJMp1212324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bueno H, Ross JS, Wang Y, et al. Trends in length of stay and short-term outcomes among Medicare patients hospitalized for heart failure, 1993-2006. JAMA. 2010;303:2141–7. doi: 10.1001/jama.2010.748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.American Heart Association [February 16, 2015];Telephone Follow-up Fact Sheet. 2011 http://www.heart.org/idc/groups/heart-public/@wcm/@hcm/@gwtg/documents/downloadable/ucm_429608.pdf.
- 14.Michigan Department of Community Health [February 16, 2015];Michigan Behavioral Risk Factor Surveillance System. http://www.michigan.gov/documents/mdch/2011-2013_MiBRFS_Reg__LHD_Tables_FINAL_466326_7.pdf.
- 15.Amarasingham R, Moore BJ, Tabak YP, et al. An automated model to identify heart failure patients at risk for 30-day readmission or death using electronic medical record data. Med Care. 2010;48:981–8. doi: 10.1097/MLR.0b013e3181ef60d9. [DOI] [PubMed] [Google Scholar]
- 16.Ezekowitz JA, van Walraven C, McAlister FA, et al. Impact of specialist follow up in outpatient with congestive heart failure. CMAJ. 2005;172:189–94. doi: 10.1503/cmaj.1032017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Amarasingham R, Patel PC, Toto K, et al. Allocating scarce resources in real-time to reduce heart failure readmissions: a prospective, controlled study. BMJ Qual Saf. 2013;0:1–8. doi: 10.1136/bmjqs-2013-001901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hansen LO, Greenwald JL, Budnitz T, et al. Project BOOST: effectiveness of a multihospital effort to reduce rehospitalization. J Hosp Med. 2013;8:421–27. doi: 10.1002/jhm.2054. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.