Abstract
Background:
Professional basketball players are at risk for lumbar disc herniation (LDH), yet the evidence guiding treatment after operative or nonoperative management of this condition in the National Basketball Association (NBA) is limited.
Hypothesis:
NBA players with LDH will have different performance outcomes based on treatment type.
Study Design:
Case-control study.
Level of Evidence:
Level 4.
Methods:
Athletes in the NBA with an LDH were identified through team injury reports, transaction records, and public sports archives. A 1:2 case-control study was performed in which LDH players and players without LDH were matched for player variables. Statistical analysis was employed to compare pre- and postindex season performance (games played and player efficiency rating [PER]) and career longevity between test subjects and controls in the operatively treated (OT) and nonoperatively treated (NOT) cohorts.
Results:
A total of 61 NBA players with LDH were included, of whom 34 underwent discectomy and 27 were managed nonoperatively. Return-to-play (RTP) rates did not differ between NOT and OT players (77.8% vs 79.4%). When compared with controls, OT players played significantly fewer games and had a lower PER than controls during the first postoperative season, but no difference was seen 2 and 3 years after surgery, with no difference in postoperative career length. In contrast, no difference in games played or PER was seen between NOT players and controls, although NOT players played significantly fewer postindex seasons.
Conclusion:
NBA players have a high RTP rate regardless of type of treatment for LDH; however, postindex performance differs between surgically and nonoperatively managed patients when compared with players without an LDH. However, further studies with a larger sample size are required for more definitive recommendations.
Clinical Relevance:
There is a high RTP rate after LDH in the NBA, although postindex performance may differ based on operative versus nonoperative treatment.
Keywords: lumbar spine, herniated disc, NBA, discectomy
Lumbar disc herniations (LDHs) are common in the general population and contribute to morbidity, disability, and significant socioeconomic costs.14 Depending on the comorbidities, preferences, and severity of pain of the patient, either operative or nonoperative management can be effectively used to treat LDH.4,19,20,25,26 While the clinical success of such treatment is determined by relief of symptoms and return to typical daily function, these data may not be applicable to highly functioning athletes who have substantially greater physical demands than this population.13 Professional athletes are predisposed to LDH from daily unnatural dynamic loading, lateral bending, and shear and compressive forces on the spine.18 Previous literature has examined the impact of LDH on athletes in the National Football League (NFL), National Hockey League (NHL), and Major League Baseball (MLB).11,12,22,24 These studies have shown a return-to-play (RTP) rate of 75% to 100%, career longevity of 2.6 to 4.8 years, and postinjury statistics ranging from 64.4% to >100% of preinjury player performance, depending on the sport played.6,11,12,24,27 Although LDHs are career-threatening injuries, these data suggest that many of these players are able to achieve preinjury performance.
The National Basketball Association (NBA) is unique to other professional leagues in that rosters are smaller and players have different body habitus. Because the sample sizes are smaller than other professional leagues, conclusions made from retrospective studies are more challenging with the data available.2,12 Consequently, although Anakwenze et al2 demonstrated few differences in postoperative season performance in 24 NBA players with LDH treated surgically over a 16-year period, confounding variables such as the control group selection criteria may have biased the conclusions, and long-term results were not examined. Particularly in basketball, the wide variability in position demands, physical characteristics, and skill sets makes the appropriate selection of control subjects challenging. Additionally, long-term results and career longevity were not evaluated, which are also fundamental in guiding treatment options and setting expectations.
This is the first assessment of nonoperative treatment of LDH in the NBA as well as how it relates to player performance outcomes while assessing long-term performance and career longevity for both treatment modalities.
Methods
Using a previously published methodology,1,2,24,27 NBA players with symptomatic LDH were identified through team medical records, newspaper archives, injury reports, team transaction reports, player profiles, and press releases between the 1984-1985 and 2013-2014 NBA seasons. Inclusion criteria were players missing at least 1 game during the regular or postseason due to LDH, or placement on the injured list for LDH, confirmed by team transaction reports, cross-checked from official NBA team websites, and corroborated by at least 2 independent public sources. Diagnosis of LDH was primarily made through magnetic resonance imaging (MRI) for players whom we could find through public records. However, for other players, particularly those diagnosed in the late 1980s to early 1990s, players were simply noted to have LDH without reference to how the diagnosis was made. Nonoperatively managed players included those undergoing physical therapy, epidural injections, and/or pharmacological treatment for LDH while playing in the NBA.
Demographic information, including age, height, weight, body mass index (BMI), position, and years of experience during the index season (defined as the season during which the player was diagnosed with LDH and missed at least 1 game) was compiled. In addition, player variables, including games played and player efficiency rating (PER) recorded for the preindex season as well as each of the postindex seasons were recorded from the official website of the NBA (http://www.nba.com) and ESPN (http://espn.go.com/nba/). PER is an objective and standardized measure in professional basketball that adds positive performance metrics (eg, points, assists, rebounds) and subtracts negative measure (eg, turnovers and fouls), adjusted for team pace and playing style, and is normalized to a league mean of 15.0. PER allows for direct comparison of players in different eras and has been used as the primary measure of player performance in a number of recent studies regarding injuries in the NBA.1,5,28 In addition, RTP rates, defined as playing at least 1 game in the NBA during the postoperative season, were also recorded.
Data were used from the past 30 NBA seasons to determine player characteristics and rates of return from both operative (OT) and nonoperative treatment (NOT) of LDH, player characteristics associated with a career-ending injury, and an assessment of player performance changes after 3 postinjury/surgery seasons and career longevity with a carefully matched group for physical and career attributes. The comparison group was assembled by matching players by position, height, weight, and BMI as well as preinjury/surgery performance statistics. This method provides the most robust and accurate information available regarding the control group for postinjury changes in player performance. For each player of the OT and NOT cohorts, 1:2 matching was performed between test and control players who returned to play and who did not have a season-ending injury or surgery during pre- and postinjury seasons. Players were matched based on data during preindex seasons, including all aforementioned player characteristics and performance variables, along with over 15 other player variables (see Appendix 1, available at http://sph.sagepub.com/content/by/supplemental-data).
Statistical Analysis
IBM SPSS Version 22 was used to perform all descriptive and comparative analyses. Categorical player variables (based on 1 SD above the mean) between players returning to play during the postinjury season were compared with those of players who did not RTP using the Fisher exact test.
Index seasons for the controls were matched in time with those of the test players. Mean difference between preindex and each of the 3 postindex seasons played and PER was compared using independent t tests and the Levene test of equality. Finally, career longevity between test and control groups was compared using Kaplan-Meyer survivorship analysis and the log-rank Mantel-Cox test. A P value ≤0.05 was deemed statistically significant.
Results
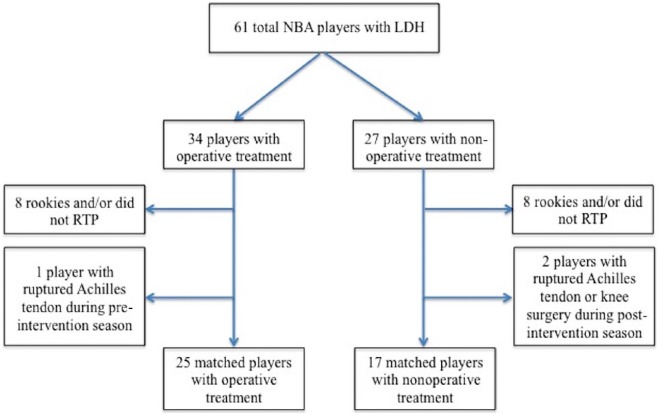
A power analysis was performed (0.80), and the minimum number of players in each test group required to detect a significant difference (α, 0.05) between test subjects and controls, calculated using independent t tests, was 25. A total of 61 players met the inclusion criteria of this study, of whom 34 (55.7%) and 27 (44.3%) were treated operatively (OT) and nonoperatively (NOT), respectively. For the 13 players (21.3 %) who did not RTP the following season (regardless of treatment), both height and the position of center were negative predictors (P = 0.002) (Table 1). Additionally, there was no difference in RTP rates between OT and NOT cohorts (P = 0.999).
Table 1.
Comparison of characteristics between players who did and did not return to play
| Did Not RTP (n = 13) |
RTP (n = 48) |
||||
|---|---|---|---|---|---|
| Characteristic | n | % | n | % | P |
| Rookie | 3 | 23.10 | 3 | 6.30 | 0.105 |
| Years of experience >9 | 3 | 23.10 | 7 | 14.60 | 0.432 |
| Age at intervention >31 y | 8 | 61.50 | 19 | 39.60 | 0.212 |
| Height >83 in | 8 | 61.50 | 9 | 18.80 | 0.005a |
| Weight >252 lbs | 3 | 23.10 | 8 | 16.70 | 0.687 |
| BMI >26.5 kg/m2 | 5 | 38.50 | 18 | 37.50 | 0.999 |
| Position | |||||
| PG | 0 | 0.00 | 6 | 12.50 | 0.326 |
| SG | 2 | 15.40 | 8 | 16.70 | 0.999 |
| SF | 1 | 7.70 | 10 | 20.80 | 0.429 |
| PF | 1 | 7.70 | 14 | 29.20 | 0.156 |
| C | 9 | 69.20 | 10 | 20.80 | 0.002a |
| Surgical management | 7 | 53.80 | 27 | 56.30 | 0.999 |
BMI, body mass index; C, center; PF, power forward; PG, point guard; RTP, return to play; SF, small forward; SG, shooting guard.
Statistically significant.
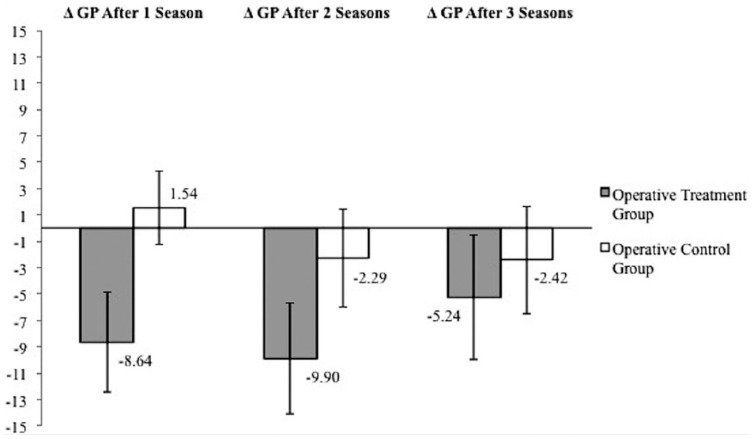
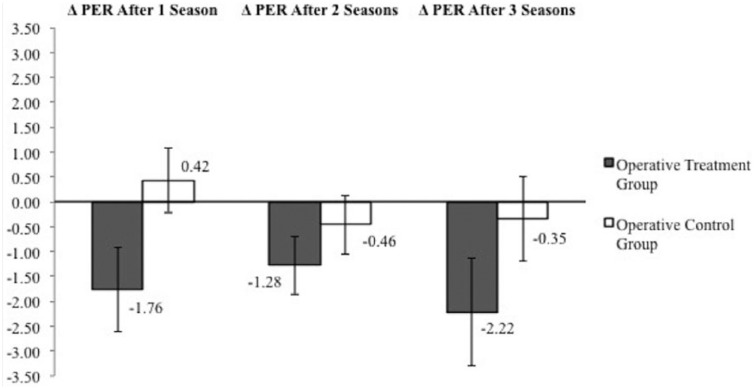
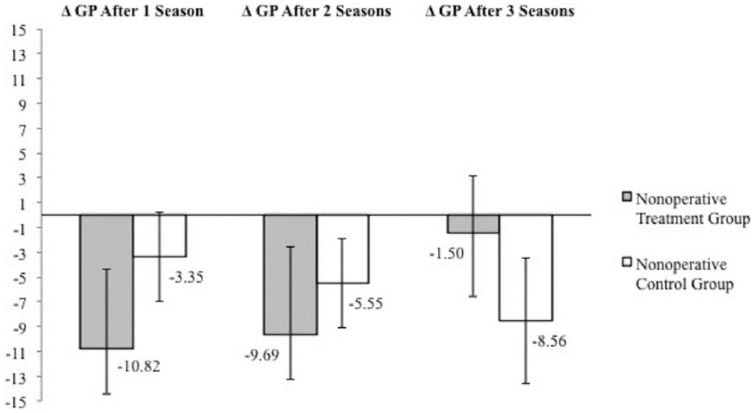
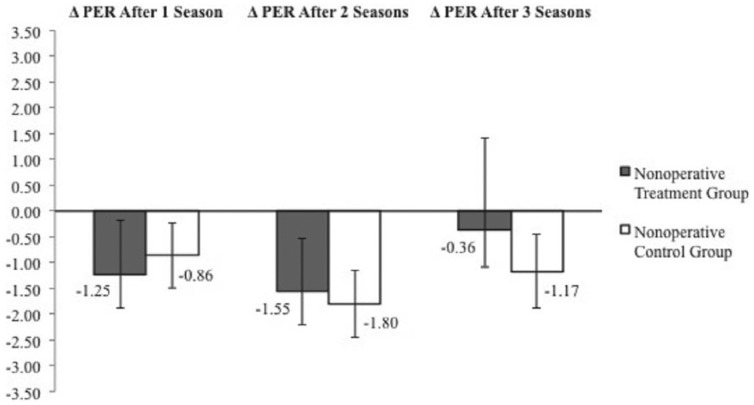
After excluding rookies and those that did not successfully RTP (Figure 1), no significant differences were found in player characteristics between treatment and control players (P > 0.05), demonstrating adequate matching (see Appendix 1). Athletes treated operatively had played significantly fewer games (–8.64 ± 3.80 vs 1.54 ± 2.82, P = 0.038) during the first postindex season when compared with controls. A significant difference was not seen during postindex season 2 (P = 0.221) or postindex season 3 (P = 0.684) (Figure 2). Similarly, operatively treated LDH players had a decline in PER (–1.76 ± 0.85 vs 0.42 ± 0.64, P = 0.049) during the first postindex season compared with controls but no difference during postindex season 2 (P = 0.396) or 3 (P = 0.093) (Figure 3). In contrast, players treated nonoperatively had no significant decline in games played during any of the postindex seasons (P = 0.282-0.567) (Figure 4) or in PER (P = 0.618-0.842) (Figure 5) when compared with controls.
Figure 1.
Player attrition diagram. LDH, lumbar disc herniation; NBA, National Basketball Association; RTP, return to play.
Figure 2.
Comparison of change in games played (ΔGP) in operative treatment cohorts.
Figure 3.
Comparison of change in player efficiency rating (ΔPER) in operative treatment cohorts.
Figure 4.
Comparison of change in games played (ΔGP) in nonoperative treatment cohorts.
Figure 5.
Comparison of change in player efficiency rating (ΔPER) in nonoperative treatment cohorts.
Survivorship analysis showed that operatively treated players who successfully returned to play did not have a decreased career length statistically when compared with controls (4.26 vs 5.68 seasons, P = 0.155). Conversely, nonoperatively treated players had a significantly decreased career length when compared with controls (3.25 vs 5.79 seasons, P = 0.016).
Discussion
The sport of basketball requires unique physical demands, such as high-impact jumping, trunk rotation, lateral bending, and collisions, all of which can place significant torsional and axial compressive forces on the lumbar spine.7,8 When compared with professional athletes of other sports, the effects of significant injuries may be more detrimental to the player’s career in the NBA. For example, the negative effects of an anterior cruciate ligament reconstruction and Achilles tendon rupture are significantly greater in NBA players than that seen in the NFL.1,3,9,15 With significantly fewer players in the NBA compared with other leagues, high levels of competition may create a more difficult threshold for achieving playing time after injury, such as with an LDH. Although the efficacy of LDH treatment is often determined in the general population with the Oswestry Disability Index, visual analog scale, and Short Form–36, elite athletes often require more applicable objective outcome measures to their profession, such as RTP rate, career longevity, and performance-based outcomes.16 This information may be vital for physicians during decision making, preoperative counseling, and setting long-term expectations for professional as well as elite high school, college, and recreational basketball athletes.
A total of 61 NBA players with a confirmed LDH that led to treatment and missed time were included in this analysis, with 78.7% successfully returning to play the following season, which is consistent with previously published data.2,12 RTP rates did not differ significantly between treatment groups, which is similar to reported results from other sports.12,23,24 Notably, taller players and those who played center were significantly more likely not to RTP after management of LDH (P = 0.005 and 0.002, respectively). Although literature is lacking on anthropomorphic effects on LDH outcomes in the general population, previous studies demonstrate an increased risk of clinically significant LDH with taller patients.10,21
While other studies have evaluated changes in performance-based outcomes in athletes after treatment for LDH, control players were only matched for a couple of demographic variables such as height, weight, BMI, position, and experience.1,2,9,17 Because preinjury performance is an important predictor of postsurgery performance, similar to studies published for other injuries, the current methodology incorporated this variable to improve the selection of appropriate controls. The players that returned to play after undergoing discectomy of LDH played significantly fewer games the following season and had a larger decrease in PER as compared with controls, which was not seen in the nonoperative group. Conversely, in a previously published analysis of 24 NBA athletes with LDH, operative management of LDH did not lead to poorer on-court performance after successful RTP.2 Notably, this study did not analyze changes in PER, which is an objective and standardized method of assessing player performance and has been used in former studies analyzing injuries in the NBA.1,5,28 PER allows for direct comparison of players of different eras and is adjusted for team pace and playing style, arguably making it a more accurate and clinically relevant metric of player performance than many other player statistics. These results, however, showed that by the second postoperative season, players are able to return to the level of play in terms of games played per season and PER, as the control cohort and career longevity is not significantly affected. This suggests that player performance 1 year after lumbar discectomy may not be indicative of future prognosis and success.
In contrast, NBA players undergoing nonoperative treatment of LDH played significantly fewer years after the index season, with no significant differences in games played or PER. The reasons for these disparate outcomes are unclear. Because of this small cohort size, accurate conclusions could not be made directly comparing OT and NOT groups. It is possible that this patient group may have residual effects of the LDH that lead to a difference in career length.
The limitations of this study include the inability to control for inherent confounding variables that may affect player performance such as team offense, concomitant injuries, and other reasons for retirement. While this study analyzes an association of treatment modality and outcomes, it is not known which symptoms related to treatment were the cause of retirement. Moreover, because of the small sample size, a direct comparison through case-control matching with an adequate power could not be made between the OT and NOT cohorts. This methodology could not use potentially helpful variables such as symptoms at presentation, radiographic signs, and preexisting pathology. Additionally, details in treatment modality, such as the type and duration of nonoperative treatment, prior to operative management of LDH were often not stated, and hence, may have been another confounder in these results. Selection bias toward more well-known players is also possible with the capture methods; however, the preindex PER (mean, 13.9 ± 3.8; range, 4.2-26.1) is similar to the league PER (mean, 15.0; range, 5.2-29.9 in the 2013-2014 season), suggesting a representative sample of the entire NBA player population. Finally, the sample size in this study was relatively small, and because of this, definitive recommendations cannot be made.
Conclusion
Regardless of treatment type, players had similar rates of return to play. While operatively treated players had a decline in games played and PER during the first postoperative season, no difference in either statistic was seen by the second season compared with controls. Nonoperatively treated players, in contrast, did not have a significantly greater decline in games played or PER, but had a shorter career length compared with controls.
Supplementary Material
Footnotes
The following author declared potential conflicts of interest: Wellington K. Hsu, MD, is a paid consultant for AONA, Bacterin, Bioventus, CeramTec, Globus, Graftys, Lifenet, Medtronic, Pioneer, Relievant, Stryker Spine, and Synthes.
References
- 1. Amin NH, Old AB, Tabb LP, Garg R, Toossi N, Cerynik DL. Performance outcomes after repair of complete Achilles tendon ruptures in National Basketball Association players. Am J Sports Med. 2013;41:1864-1868. [DOI] [PubMed] [Google Scholar]
- 2. Anakwenze OA, Namdari S, Auerbach JD, et al. Athletic performance outcomes following lumbar discectomy in professional basketball players. Spine (Phila Pa 1976). 2010;35:825-828. [DOI] [PubMed] [Google Scholar]
- 3. Brophy RH, Gill CS, Lyman S, Barnes RP, Rodeo SA, Warren RF. Effect of anterior cruciate ligament reconstruction and meniscectomy on length of career in National Football League athletes: a case control study. Am J Sports Med. 2009;37:2102-2107. [DOI] [PubMed] [Google Scholar]
- 4. Buttermann GR. The effect of spinal steroid injections for degenerative disc disease. Spine J. 2004;4:495-505. [DOI] [PubMed] [Google Scholar]
- 5. Cerynik DL, Lewullis GE, Joves BC, Palmer MP, Tom JA. Outcomes of microfracture in professional basketball players. Knee Surg Sports Traumatol Arthrosc. 2009;17:1135-1139. [DOI] [PubMed] [Google Scholar]
- 6. Earhart JS, Roberts D, Roc G, Gryzlo S, Hsu W. Effects of lumbar disk herniation on the careers of professional baseball players. Orthopedics. 2012;35:43-49. [DOI] [PubMed] [Google Scholar]
- 7. Hangai M, Kaneoka K, Hinotsu S, et al. Lumbar intervertebral disk degeneration in athletes. Am J Sports Med. 2009;37:149-155. [DOI] [PubMed] [Google Scholar]
- 8. Hangai M, Kaneoka K, Okubo Y, et al. Relationship between low back pain and competitive sports activities during youth. Am J Sports Med. 2010;38:791-796. [DOI] [PubMed] [Google Scholar]
- 9. Harris JD, Erickson BJ, Bach BR, Jr, et al. Return-to-sport and performance after anterior cruciate ligament reconstruction in National Basketball Association players. Sports Health. 2013;5:562-568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Heliovaara M. Body height, obesity, and risk of herniated lumbar intervertebral disc. Spine (Phila Pa 1976). 1987;12:469-472. [DOI] [PubMed] [Google Scholar]
- 11. Hsu WK. Performance-based outcomes following lumbar discectomy in professional athletes in the National Football League. Spine (Phila Pa 1976). 2010;35:1247-1251. [DOI] [PubMed] [Google Scholar]
- 12. Hsu WK, McCarthy KJ, Savage JW, et al. The professional athlete spine initiative: outcomes after lumbar disc herniation in 342 elite professional athletes. Spine J. 2011;11:180-186. [DOI] [PubMed] [Google Scholar]
- 13. Jansson KA, Nemeth G, Granath F, Jonsson B, Blomqvist P. Health-related quality of life in patients before and after surgery for a herniated lumbar disc. J Bone Joint Surg Br. 2005;87:959-964. [DOI] [PubMed] [Google Scholar]
- 14. Katz JN. Lumbar disc disorders and low-back pain: socioeconomic factors and consequences. J Bone Joint Surg Am. 2006;88(suppl 2):21-24. [DOI] [PubMed] [Google Scholar]
- 15. McCullough KA, Shaw CM, Anderson RB. Mini-open repair of achilles rupture in the national football league. J Surg Orthop Adv. 2014;23:179-183. [PubMed] [Google Scholar]
- 16. Nair R, Kahlenberg CA, Hsu WK. Outcomes of lumbar discectomy in elite athletes: the need for high-level evidence. Clin Orthop Relat Res. 2015;473:1971-1977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Namdari S, Baldwin K, Anakwenze O, Park MJ, Huffman GR, Sennett BJ. Results and performance after microfracture in National Basketball Association athletes. Am J Sports Med. 2009;37:943-948. [DOI] [PubMed] [Google Scholar]
- 18. Ong A, Anderson J, Roche J. A pilot study of the prevalence of lumbar disc degeneration in elite athletes with lower back pain at the Sydney 2000 Olympic Games. Br J Sports Med. 2003;37:263-266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Osterman H, Seitsalo S, Karppinen J, Malmivaara A. Effectiveness of microdiscectomy for lumbar disc herniation: a randomized controlled trial with 2 years of follow-up. Spine (Phila Pa 1976). 2006;31:2409-2414. [DOI] [PubMed] [Google Scholar]
- 20. Peul WC, van Houwelingen HC, van den Hout WB, et al. ; Leiden-The Hague Spine Intervention Prognostic Study Group. Surgery versus prolonged conservative treatment for sciatica. N Engl J Med. 2007;356:2245-2256. [DOI] [PubMed] [Google Scholar]
- 21. Rihn JA, Kurd M, Hilibrand AS, et al. The influence of obesity on the outcome of treatment of lumbar disc herniation: analysis of the Spine Patient Outcomes Research Trial (SPORT). J Bone Joint Surg Am. 2013;95:1-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Roberts DW, Roc GJ, Hsu WK. Outcomes of cervical and lumbar disk herniations in Major League Baseball pitchers. Orthopedics. 2011;34:602-609. [DOI] [PubMed] [Google Scholar]
- 23. Savage JW, Hsu WK. Statistical performance in National Football League athletes after lumbar discectomy. Clin J Sport Med. 2010;20:350-354. [DOI] [PubMed] [Google Scholar]
- 24. Schroeder GD, McCarthy KJ, Micev AJ, Terry MA, Hsu WK. Performance-based outcomes after nonoperative treatment, discectomy, and/or fusion for a lumbar disc herniation in National Hockey League athletes. Am J Sports Med. 2013;41:2604-2608. [DOI] [PubMed] [Google Scholar]
- 25. Weber H. Lumbar disc herniation. A controlled, prospective study with ten years of observation. Spine (Phila Pa 1976). 1983;8:131-140. [PubMed] [Google Scholar]
- 26. Weinstein JN, Tosteson TD, Lurie JD, et al. Surgical vs nonoperative treatment for lumbar disk herniation: the Spine Patient Outcomes Research Trial (SPORT): a randomized trial. JAMA. 2006;296:2441-2450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Weistroffer JK, Hsu WK. Return-to-play rates in National Football League linemen after treatment for lumbar disk herniation. Am J Sports Med. 2011;39:632-636. [DOI] [PubMed] [Google Scholar]
- 28. Yeh PC, Starkey C, Lombardo S, Vitti G, Kharrazi FD. Epidemiology of isolated meniscal injury and its effect on performance in athletes from the National Basketball Association. Am J Sports Med. 2012;40:589-594. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.