Abstract
Background
Cancer disparities are associated with a broad range of sociocultural determinants of health that operate in community contexts. High-risk populations may be more vulnerable to social and environmental factors that lead to chronic stress. Theoretical and empirical research indicates that exposure to contextual and sociocultural stress alters biological systems, thereby influencing cancer risk, progression, and, ultimately, mortality.
Objective
We sought to describe contextual pathways through which stress likely increases cancer risk in high-risk, underserved populations.
Methods
This review presents a description of the link between contextual stressors and disease risk disparities within underserved communities, with a focus on 1) stress as a proximal link between biological processes, such as cytokine responses, inflammation, and cancer and 2) stress as a distal link to cancer through biobehavioral risk factors such as poor diet, physical inactivity, circadian rhythm or sleep disruption, and substance abuse. These concepts are illustrated through application to populations served by three National Cancer Institute-funded Community Networks Program Centers (CNPCs): African Americans in the Deep South (the South Carolina Cancer Disparities Community Network [SCCDCN]), Native Hawaiians (‘Imi Hale—Native Hawaiian Cancer Network), and Latinos in the Lower Yakima Valley of Washington State (The Center for Hispanic Health Promotion: Reducing Cancer Disparities).
Conclusions
Stress experienced by the underserved communities represented in the CNPCs is marked by social, biological, and behavioral pathways that increase cancer risk. A case is presented to increase research on sociocultural determinants of health, stress, and cancer risk among racial/ethnic minorities in underserved communities.
Keywords: Psychological stress, vulnerable populations, cancer, community networks, racism, discrimination, African Americans, Hispanic Americans, Hawaii, Oceanic Ancestry Group
Cancer disparities are associated with a broad range of social determinants of health1 that are related to exposure to stressors in high-risk, underserved populations.2–6 In this article, concepts linking stress, biological sequelae, and putative effects on cancer risk profiles are related to examples drawn from populations served by three National Cancer Institute-funded CNPCs.
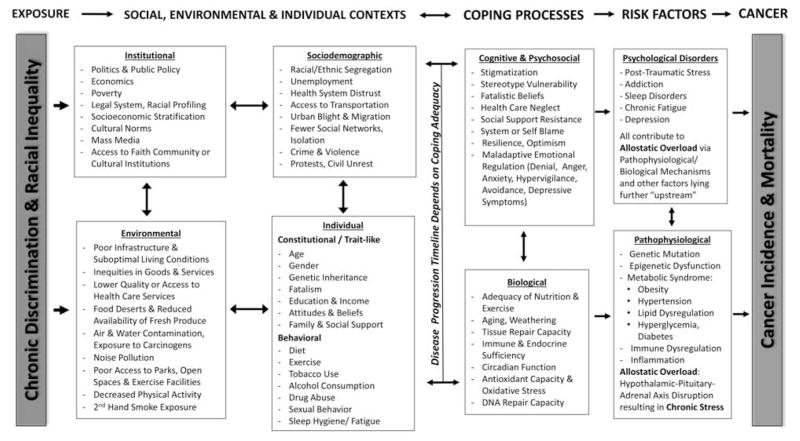
Existing conceptual models and frameworks describe the influence of social determinants on health, and many focus on the role of chronic stress in mediating biological processes that can cause disease.7,8 An example of this as it relates to cancer is provided in Figure 1. Empirical research links social factors and stress to disparate health outcomes, including a variety of human cancers.9–11 Low socioeconomic status, for example, is linked with a higher risk for many diseases and health practices.12–15 Social position is a strong predictor of disease risk, even after accounting for factors that comprise socioeconomic status.16,17 Lower social position is thought to contribute to increased stress and to observed differences in disease incidence18–20 as well as to survival.21,22 Psychosocial stressors can contribute to susceptibility to chronic diseases, including cancer.23–25 Specifically, socially disadvantaged groups experience these impacts owing to their increased exposure to chronic unpredictable, uncontrollable stressors across the life span.15,26 Marginalized groups may suffer from stressor overload, exhaustion of endogenous and exogenous coping mechanisms,27 and contextual demands that exceed their adaptive capacity.15,28
Figure 1. Pathways from Stress to Cancer.
Adapted from: Cells to Society: Overcoming Health Disparities. Centers for Population Health and Health Disparities. National Institutes of Health, Bethesda, MD, Nov., 2007.
Unhealthy behaviors, such as smoking, alcohol and drug abuse, poor diet/overeating, and sedentary behavior, are common high-risk coping responses to stressful situations29 that can increase cancer risk.30–32 Low-grade inflammation, caused by the release of inflammatory cytokines and adipokines from central adipose tissue, is another effect33,34 and dysregulated cortisol responses are a primary product of stress reactivity in relation to adiposity.35–37
Chronic maladaptive coping, depressive symptomology, and “sickness behavior”38–41 among populations exposed to chronic stress may alter neuropsychological, immune, and endocrine function along the hypothalamic–pituitary–adrenal axis that may, in turn, affect cancer prevention, incidence, and survival.11 For instance, “sickness behavior” and, similarly, depression, which are associated with lethargy, inability to concentrate, and reduction in self-care behaviors, can be induced by stress-related increases in proinflammatory cytokines’ (e.g., interleukin–6, tumor necrosis factor-α) effects on the brain.42 Other stress-related behaviors, such as a preference for sweet43,44 and/or high-fat45 foods, are thought to be mediated by cortisol and may be associated with abdominal adiposity,46 a risk factor for several cancers.47
Circadian disruption and chronobiological dysregulation often accompany stress.48 Individuals in low-control, high-stress jobs49 often work at odd hours of the day,50 and those who are insecure about their employment may have disturbed sleep.51,52 Symptoms of circadian disruption such as fatigue, sleep disruption, and depressive symptoms are associated with altered neuroendocrine and immune signaling and are accompanied by proinflammatory cytokine secretion.53,54 Fatigue, poor sleep quality, and depression are associated with cancer and are often symptoms experienced by those with disrupted circadian patterns.55 These symptoms are reported to vary by race/ethnicity.56 For example, African Americans differ in their endogenous circadian timing relative to European Americans,57 and they are more likely than are European Americans to participate in shift work58,59 (a risk factor for cancer and other chronic diseases48) and to experience poorly timed ambient light exposures60,61 and poor sleep quality.58,62
Discrimination functions as both a chronic63,64 and acute stressor,65 producing mental and physical health effects.66 Several studies show that discrimination is associated with increased levels of stress, risky health behaviors, and poor mental and physical health outcomes among racial and ethnic minorities.67
Allostatic load refers to the cumulative impact of health risks owing to repeated or prolonged stress over the course of a person’s life that can lead to increased risk of disease.18,68,69 This cumulative effect results in dramatically earlier onset of biological aging or “weathering” associated with increased cancer risk in minorities, with the strongest evidence in African Americans.70–72
Although the terms for describing the problem may vary from population to population, and between high-risk communities and academe, the role of stress in health is well appreciated across populations. Community-based participatory research (CBPR) provides a means for engaging with high-stress groups in designing research studies that would lead to practicable solutions to reduce stress. These could include interventions aimed directly at stress reduction, or at other lifestyle-related behaviors that are thought to reduce stress. There are many viable alternatives to randomized, controlled trials, which are probably inappropriate for such behavioral interventions in any event. These alternatives include randomizing before consent, single-arm, and selfselection study designs.
Examples
To illustrate possible relationships between stress and cancer issues, we focus on three minority groups represented in the 23 CNPCs—African Americans, Latinos, and Native Hawaiians. All CNPCs use CBPR methods to engage communities to address cancer-related health disparities.73
African Americans in South Carolina
The genotype of most African-American South Carolinians can be traced to purposeful selection of West African agrarian populations on the “Rice Coast” or the “Windward Coast,” in the “Gambia” and “Sierra Leone.” 74–76 Seventeenth-century South Carolina planters unfamiliar with rice cultivation used African slaves’ rice cultivation skills to develop large plantations.77,78 This led to creation of a lucrative market for “Rice Coast” slaves.74–77,79 Besides there being a Black majority in South Carolina,80 two other factors contributed to the retention of African culture and health behaviors81–83: 1) plantation hypersegregation between Whites and Blacks and 2) geographic, topographical, and climactic similarity to the African “Rice Coast.”
As the South Carolina Slave Codes were instigated and cotton replaced rice as the dominant crop, slaves’ diets became more controlled by plantation owners.84 Preservative salt added to the diet of a highly sodium-responsive population could add to the stressors of slavery by inducing exaggerated neural responses to stress.85–87 Unpredictable, uncontrollable violence, lack of control over personal health decisions, physical exhaustion, and environmental stressors also accompanied this shift in Deep South slave-holding practices,88 which resulted in the loss of stress-buffering cultural traditions.89,90
The lingering effects of racism include psychosocial stress91–93 and “downstream” effects on factors that have implications for cancer, such as inflammation94 and sleep disturbances.95 Indeed, we found that, in a population of overweight and obese African-American churchgoers experiencing racism, there were very high levels of C-reactive protein, a marker of systemic inflammation, that decreased with an intervention that included stress reduction.96 In another study we found that African-American Medicaid recipients with type II diabetes (a condition known to be related to inflammation and stress) had an elevated risk of colorectal cancer, beyond that of diabetic European Americans.97
Historical factors provide the backdrop to current stressors, which may produce epigenetic effects98 for the descendants of African Slaves.26 Epigenetic effects among African Americans in South Carolina occur not only through diet, allostatic overload, and destruction of adaptive social ties,99 but also through chronic poverty and chronic unpredictable, uncontrollable exposure to contextual stressors.98 In other work, we demonstrated that skin color is related to stress, blood pressure, and body mass index,63 risk factors associated with numerous health outcomes, including cancer. Cultural adaptations, in particular strengthening gender roles in positive modifiable health behaviors100 and a prominent focus on religion and spirituality,96,101 provide both ameliorating effects and opportunities for effective intervention. Indeed, other work conducted through the SCCDCN shows the influence of African-American pastors’ food identity101 on church-level factors related to food/diet and physical activity messaging.102 In addition to obesity,63 SCCDCN researchers also have found that racism-related stress is associated with psychosocial103 and cognitive cancer risk factors,104 as well as higher resting blood pressure.105,106
Today, African Americans in our target communities often are employed in low-status,107 low-control,108 insecure, service sector jobs that typically entail little physical activity and frequently require working odd and/or long hours.109 Disproportionately, they reside in rural and impoverished urban communities that are unsafe, offer limited access to healthy foods, and provide little opportunity for physical activity.110,111 Calorie-dense/nutrient sparse diets,112,113 physical inactivity (worse in the rural South than anywhere else in the United States),114 and high rates of obesity and diabetes,113,115,116 are all known cancer risk factors.97,117,118
The SCCDCN recognizes that economic development undergirds social, environmental, and health-related justice. Our work with churches, as cited, and other community partners is predicated on making connections with social and economic structures in which the community operates to promote health and sustain change. The SCCDCN has developed programs that engage women, who are disproportionately represented as community leaders and heads of households, as a means to address the range of “upstream” factors, from examining institutional racism to increasing economic opportunity and enabling healthy lifestyle choices (e.g., building on plant-based dietary traditions of the African Diaspora, promoting social ties among community members,99,108 and engaging in culturally salient physical activities).
Latinos in the Lower Yakima Valley
As with African Americans, Hispanics in the United States have experienced historical trauma. From initial Spanish domination to Bracero (guest worker) programs,119,120 the Hispanic population has been subjected to domination by populations of European ancestry.119 The population that has emerged is characterized by poverty and stigma.120–122 The literature suggests that this ethnic group is associated with worse mental and physical health as compared with the non-Hispanic White (NHW) population.123–128 As a group, Hispanics have limited access to health care, with 38.3% having no health insurance compared with 12.0% for NHWs. Overweight prevalence is higher in Hispanics (67.0%) than NHWs (59.2%).129 Additionally, Hispanics are, on average, much less likely than others to utilize mental health services.130
Although Hispanics have a lower incidence of many cancers, they tend to have higher mortality.131 Part of the reason may be biological, but much is related to low access to care and late diagnoses and treatment of disease.131 For example, Latinas have a significantly lower breast cancer incidence compared with NHWs; however, their mortality rates are comparable.131 Further, when asked about stress in their lives, more than 50% of Hispanics reported having high mental and physical stress owing to jobs that entail physical labor and low wages.130 For example, Latinos hold 48.9% of the jobs in agriculture,132 an occupation that involves hard work and low pay. Another large proportion of Latinos hold jobs in the service industry and in housekeeping, also physically demanding, low-paying occupations.132
The Hispanic Community Network to Reduce Cancer Disparities began working in Yakima Valley in Eastern Washington in 2005. The lower Yakima Valley is a “majority minority” area, with Hispanics’ comprising approximately 67% of the population. Many Hispanics work in agriculture as well as in the service industry. It is the mission of the CNPC to improve the lives of Hispanics who live in the valley by providing education and research to enhance accessibility to cancer screening, treatment, and survivorship. To learn more about Latino experiences with perceived racism and other forms of discrimination, the CNPC conducted qualitative, in-depth interviews among Latino residents of the lower Yakima Valley (unpublished data provided by B. Thompson). Respondents reported exposure to several types of perceived racism, including discrimination based on race/ethnicity, language, and legal status. The most common settings in which discrimination occurred were at work and in local businesses. Coping responses to perceived racism included ignoring it, avoiding it, talking with someone about it, and praying. Respondents reported health effects of perceived racism and other stressors, including problems sleeping, changes in diet and physical activity, and increased alcohol use.
In a study examining 70 Hispanics and 87 NHWs in the area, all of whom had type II diabetes, we found that Hispanics were much less likely than NHWs to engage in activities such as diet and physical activity to control their diabetes.133 This difference may have been due to having few resources to purchase appropriate foods and/or living in neighborhoods where physical activity was unsafe or impractical. Further, the more acculturated the Hispanics, the more likely they were to engage in lifestyle behaviors to address their diabetes. Thus, acculturative stress may have an impact on chronic disease management.
In a study examining Hispanic agricultural workers and Hispanic nonagricultural workers, differences in perceived stress were examined (unpublished data provided by B. Thompson). Agricultural workers were more likely to experience stress in all five stress categories (work, community, family, psychological, and acculturation) that influenced their well-being compared with nonagricultural workers. Specifically, as stress increased, well-being, as measured by the World Health Organization Well-Being Index, decreased. The Well-Being Index includes mental well-being, physical well-being, sleep disturbances, and interest in daily life.
The data indicate that the underserved Hispanic population is subject to chronic stressors that have an impact on health, including chronic diseases. More work is needed to understand this phenomenon in the population, and ways to alleviate the stress should be identified and tested using rigorous methods.
Native Hawaiians in Hawai‘i
Native Hawaiians are descendants of the original inhabitants of the Pacific archipelago now called Hawai’i. European explorers to Hawai’i in 1778 found a robust and vibrant native population, numbering about 800,000, with a sophisticated socioreligious order that ensured equitable distribution of life-sustaining resources. U.S. influence and aspirations led to the overthrow of the Hawaiian Kingdom in 1883, followed by its annexation in 1898 and statehood in 1959, all of which were strongly opposed by Native Hawaiians.134
Many scholars postulate that the health and well-being of Native Hawaiians were adversely affected by the U.S. occupation of Hawai’i and its compulsory acculturation process.135–139 Today, Native Hawaiians have a much greater prevalence of obesity (44%), diabetes (20%), depression (13%), cigarette smoking (27%), and alcohol and drug abuse (26%) than do NHWs and other ethnic groups in the state.140 Native Hawaiians are more likely to work in low-paying jobs and to be undereducated, incarcerated, and living in poorer conditions than are other ethnic groups in Hawai’i.141 These conditions manifest in a much shorter life expectancy for Native Hawaiians, as compared with Chinese, Japanese, Korean, Filipino, and NHW residents.142
Researchers affiliated with ‘Imi Hale Native Hawaiian Cancer Network have found evidence that acculturative stress and ethnic discrimination could be increasing Native Hawaiians’ risk for stress-related diseases. In a study of 496 adult Native Hawaiians, the prevalence of type 2 diabetes was examined across four modes of acculturation: integrated (high ethnic and high mainstream identity), traditional (exclusively high ethnic identity), assimilated (exclusively high mainstream identity), and marginalized (low ethnic and mainstream identity). 143 After accounting for differences in sociodemographics, degree of Hawaiian ancestry, and biological correlates, researchers found that the prevalence of type 2 diabetes was nearly two times greater among Native Hawaiians categorized as having a traditional mode of acculturation, as compared with those with an integrated mode of acculturation (28% vs. 15%, respectively). This suggests that the differences are owing to the experience of greater acculturative stress and unique psychosocial factors, such as perceived racism.143
A study of 94 adult Native Hawaiians examined the effects of perceived racism and other acculturation factors on the prevalence of hypertension.144 Native Hawaiians who had a stronger Hawaiian ethnic identity were more likely to report that other social groups discriminated against them. Further, perceptions of discrimination were associated significantly with self-reported hypertension, after adjusting for sociodemographics and degree of Hawaiian ethnic and American cultural identity. Perceptions of discrimination seemed to have mediated the relationship between Hawaiian cultural identity and hypertension status, which supports the possibility that Native Hawaiians in a traditional mode of acculturation are experiencing more acculturative stressors.
A third study examined effects of perceived racism on cortisol levels and blood pressure as two indices of physiological health.93 Among 143 adult Native Hawaiians, those who reported a stronger Hawaiian ethnic identity also perceived more racism in their environment, and perception of racism was associated significantly with lower diurnal cortisol levels and higher systolic blood pressure. However, after adjusting for different sociodemographic, biological, and psychosocial characteristics, the researchers noted that only the significant correlation between cortisol level and perceived racism persisted. Contrary to the normal response of increased cortisol in situations of acute stress, a low level of cortisol output is believed to be indicative of chronic stress and has been observed in victims of domestic violence,145 caregivers for ill family members,146 and people diagnosed with posttraumatic stress disorder.147 Hypocortisolism is associated with a risk for stress-related disorders, such as atherosclerosis, hypertension, obesity, and diabetes.148,149
Collectively, these studies support the notion that racial/ethnic discrimination may be a chronic psychosocial stressor for Native Hawaiians. Strong perceptions of discrimination seem to be associated with stress-related chronic diseases, such as hypertension and diabetes. Associations between perceived discrimination and cancer have not been reported for Native Hawaiians, and further research in this area is recommended.
Discussion
Psychological stress experienced by the underserved populations discussed here manifests in both biological and behavioral outcomes150,151 that can result in increased cancer risk. However, research on social determinants of health, stress, and cancer risk among racial/ethnic minorities must overcome serious barriers: 1) a history of distrust in minority communities contributing to their underrepresentation in clinical, psychosocial, and biomedical studies including, but not limited to, randomized trials, 2) researchers not actively seeking methods to improve communication and trust with racial/ethnic minority populations, and 3) linguistic and sociocultural differences that limit effectiveness of psychosocial intervention research.
The CNPCs are committed to using CBPR approaches to define and identify solutions to problems that increase risk of disease and disability.152 This has the effect of markedly reducing the probability of type III error (incorrect inference resulting from a faulty conception of how things work or selection of a study design that produces an answer [even if correct] to the wrong question [because it is fundamentally biased]).153,154 Rather than researchers’ requiring changes that are culturally inappropriate, untimely, or unwise, the underserved community works with researchers to develop solutions and strategies to attain solutions. In South Carolina, for example, the partnership with the Baptist Church, which ensures that education and health activities correspond with the prevailing culture and attitudes, taps into the roles of resilience155 and spirituality156,157 that are important stress buffers in the face of adversity. In the Yakima Valley of Washington State, the CNPC conducts activities with the Hispanic community during Mexican activities, such as Cinco de Mayo. They also conduct activities with extended families, because this is important in the Mexican-American culture. In the Hawaiian CNPC, well-received interventions have incorporated traditional cultural values, been based in Hawaiian churches and civic clubs, and featured traditional activities, such as hula dancing and canoe paddling. Further, Hawaiian community members have been empowered to lead, deliver, and test these interventions.
In short, by working with communities, rather than imposing the will of culturally different groups, we have an opportunity to prevent and control cancer in a way that is meaningful for the populations we are trying to reach. When cancer prevention and control interventions are part of a group’s culture, they are more likely to engage the group. Such efforts may contribute to the reduction of cancer disparities among the underserved.
The World Health Organization Commission on Social Determinants of Health provides several strategies for taking action on social determinants of health.17,158 Approaches include creating policies that reduce oppressed groups’ vulnerability to the health effects of social inequality and prevent the unequal health consequences of social inequality. Strategies that use this approach involve increasing racial/ethnic minorities’ resources to deal with stressors, such as efforts to increase community empowerment or encourage positive coping strategies, which may reduce the negative health effects of stress. What we have shown is that race/ethnicity-related stress operates through two, related pathways: 1) through direct proinflammatory, epigenetic, or other biological processes that can exert toxic effects and 2) through unhealthy coping lifestyles and behaviors that are themselves risk factors for cancer. The history of public health has shown that improving the economic circumstances of individuals can have a ripple effect through a variety of processes such as stress reduction, increased opportunities to improve diet and physical activity, and better access to health care.159,160
Acknowledgments
The authors thank the members of the community advisory groups of each of the projects described in this article for their ongoing insights and generous feedback to ensure the relevance of each of the research projects for their communities.
This study was supported by grants U54 CA153502 (to the Fred Hutchinson Cancer Research Center), U54 CA153459 (to Papa Ola Lōkahi), and U54 CA153461(to the University of South Carolina), from the National Cancer Institute. Dr. Hebert was supported by an Established Investigator Award in Cancer Prevention and Control from the Cancer Training Branch of the National Cancer Institute (K05 CA136975). All opinions expressed herein are the sole responsibility of the authors and do not reflect the views of the National Institutes of Health.
References
- 1.Krieger N. Defining and investigating social disparities in cancer: Critical issues. Cancer Causes Control. 2005;16:5–14. doi: 10.1007/s10552-004-1251-5. [DOI] [PubMed] [Google Scholar]
- 2.Antoni MH, Pereira DB, Marion I, Ennis N, Andrasik MP, Rose R, et al. Stress management effects on perceived stress and cervical neoplasia in low-income HIV-infected women. J Psychosom Res. 2008;65:389–401. doi: 10.1016/j.jpsychores.2008.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dodd SM, Pereira DB, Marion I, Andrasik M, Rose R, Simon T, et al. Depressive symptoms and cervical neoplasia in HIV+ low-income minority women with human papillomavirus infection. Int J Behav Med. 2009;16:181–8. doi: 10.1007/s12529-008-9025-1. [DOI] [PubMed] [Google Scholar]
- 4.Douma KF, Aaronson NK, Vasen HF, Gerritsma MA, Gundy CM, Janssen EP, et al. Psychological distress and use of psychosocial support in familial adenomatous polyposis. Psychooncology. 2010;19:289–98. doi: 10.1002/pon.1570. [DOI] [PubMed] [Google Scholar]
- 5.Lim JW, Ashing-Giwa KT. Examining the effect of minority status and neighborhood characteristics on cervical cancer survival outcomes. Gynecol Oncol. 2011;121:87–93. doi: 10.1016/j.ygyno.2010.11.041. [DOI] [PubMed] [Google Scholar]
- 6.Schneider MG, Chiriboga DA. Associations of stress and depressive symptoms with cancer in older Mexican Americans. Ethn Dis. 2005;15:698–704. [PubMed] [Google Scholar]
- 7.Clark R, Anderson NB, Clark VR, Williams DR. Race, ethnicity, and health: A public health reader. San Francisco: Jossey-Bass; 2002. Racism as a stressor for African Americans: A biopsychosocial model; pp. 369–89. [Google Scholar]
- 8.Krieger N. Ecosocial theory. In: Anderson N, editor. Encyclopedia of health and behavior. Thousand Oaks (CA): Sage; 2004. pp. 292–4. [Google Scholar]
- 9.Hebert JR, Hurley TG, Harmon BE, Heiney S, Hebert CJ, Steck SE. A diet, physical activity, and stress reduction intervention in men with rising prostate-specific antigen after treatment for prostate cancer. Cancer Epidemiol. 2012;36:e128–36. doi: 10.1016/j.canep.2011.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ledesma D, Kumano H. Mindfulness-based stress reduction and cancer: A meta-analysis. Psychooncology. 2009;18:571–9. doi: 10.1002/pon.1400. [DOI] [PubMed] [Google Scholar]
- 11.Ellison GL, Coker AL, Hebert JR, Sanderson M, Royal CD, Weinrich SP. Psychosocial stress and prostate cancer: A theoretical model. Ethn Dis. 2001;11:484–95. [PubMed] [Google Scholar]
- 12.Anderson NB, Armstead CA. Toward understanding the association of socioeconomic status and health: A new challenge for the biopsychosocial approach. Psychosom Med. 1995;57:213–25. doi: 10.1097/00006842-199505000-00003. [DOI] [PubMed] [Google Scholar]
- 13.Landrine H, Corral I. Separate and unequal: Residential segregation and black health disparities. Ethn Dis. 2009;19:179–84. [PubMed] [Google Scholar]
- 14.Jerant AF, Fenton JJ, Franks P. Determinants of racial/ethnic colorectal cancer screening disparities. Arch Intern Med. 2008;168:1317–24. doi: 10.1001/archinte.168.12.1317. [DOI] [PubMed] [Google Scholar]
- 15.Adler NE, Rehkopf DH. U.S. disparities in health: Descriptions, causes, and mechanisms. Ann Rev Public Health. 2008;29:235–52. doi: 10.1146/annurev.publhealth.29.020907.090852. [DOI] [PubMed] [Google Scholar]
- 16.Marmot MG. Status syndrome: A challenge to medicine. JAMA. 2006;295:1304–7. doi: 10.1001/jama.295.11.1304. [DOI] [PubMed] [Google Scholar]
- 17.Marmot M, Friel S, Bell R, Houweling TAJ, Taylor S Commission on Social Determinants of Health. Closing the gap in a generation: Health equity through action on the social determinants of health. Lancet. 2008;372:1661–9. doi: 10.1016/S0140-6736(08)61690-6. [DOI] [PubMed] [Google Scholar]
- 18.Seeman TE, McEwen BS, Rowe JW, Singer BH. Allostatic load as a marker of cumulative biological risk: MacArthur studies of successful aging. Proc Natl Acad Sci U S A. 2001;98:4770–5. doi: 10.1073/pnas.081072698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cuello C, Correa P, Haenszel W. Socio-economic class differences in cancer incidence in Cali, Colombia. Int J Cancer. 1982;29:637–43. doi: 10.1002/ijc.2910290607. [DOI] [PubMed] [Google Scholar]
- 20.Johansen C, Olsen JH. Psychological stress, cancer incidence and mortality from non-malignant diseases. Br J Cancer. 1997;75:144–8. doi: 10.1038/bjc.1997.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Classen C, Hermanson KS, Spiegel D. Psychotherapy, stress, and survival in breast cancer. In: Lewis C, O’Sullivan C, Barraclough J, editors. The psychoimmunology of cancer. Oxford: Oxford University Press; 1994. p. 123. [Google Scholar]
- 22.Ell K, Nishimoto R, Mediansky L, Mantell J, Hamovitch M. Social relations, social support and survival among patients with cancer. J Psychosom Res. 1992;36:531–41. doi: 10.1016/0022-3999(92)90038-4. [DOI] [PubMed] [Google Scholar]
- 23.Marmot M, Shipley M, Hemingway H, Head J, Brunner E. Biological and behavioural explanations of social inequalities in coronary heart disease: The Whitehall II study. Diabetologia. 2008;51:1980–8. doi: 10.1007/s00125-008-1144-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cooper CL, Cooper R, Faraghaer EB. Incidence and perception of psychosocial stress: The relationship with breast cancer. Psychol Med. 1989;19:415–22. doi: 10.1017/s0033291700012459. [DOI] [PubMed] [Google Scholar]
- 25.Sarkar DK, Murugan S, Zhang C, Boyadjieva N. Regulation of cancer progression by -endorphin neuron. Cancer Res. 2012;72:836–40. doi: 10.1158/0008-5472.CAN-11-3292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lekan D. Sojourner syndrome and health disparities in African American women. Adv Nursing Sci. 2009;32:307–21. doi: 10.1097/ANS.0b013e3181bd994c. [DOI] [PubMed] [Google Scholar]
- 27.Myers H, Lewis T, Parker-Dominguez T. Stress, coping and minority health. In: Bernal JT, Burlew A, Leong F, editors. Handbook of racial and ethnic minority psychology. Thousand Oaks (CA): Sage; 2003. pp. 377–400. [Google Scholar]
- 28.Abdou CM, Schetter CD, Jones F, Roubinov D, Tsai S, Jones L, et al. Community perspectives: Mixed-methods investigation of culture, stress, resilience, and health. Ethn Dis. 2010;20:S2–41. [PMC free article] [PubMed] [Google Scholar]
- 29.Walsh JL, Senn TE, Carey MP. Longitudinal associations between health behaviors and mental health in low-income adults. Transl Behav Med. 2013;3:104–13. doi: 10.1007/s13142-012-0189-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jackson JS, Knight KM, Rafferty JA. Race and unhealthy behaviors: Chronic stress, the HPA axis, and physical and mental health disparities over the life course. Am J Public Health. 2010;100:933–9. doi: 10.2105/AJPH.2008.143446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sloan FA, Costanzo PR, Belsky D, Holmberg E, Malone PS, Wang Y, et al. Heavy drinking in early adulthood and outcomes at mid life. J Epidemiol Community Health. 2011;65:600–5. doi: 10.1136/jech.2009.102228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Aldworth J, Colpe LJ, Gfroerer JC, Novak SP, Chromy JR, Barker PR, et al. The National Survey on Drug Use and Health Mental Health Surveillance Study: Calibration analysis. Int J Meth Psych Res. 2010;1:61–87. doi: 10.1002/mpr.312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ouchi N, Parker JL, Lugus JJ, Walsh K. Adipokines in inflammation and metabolic disease. Nature Rev Immunol. 2011;11:85–97. doi: 10.1038/nri2921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Percik R, Stumvoll M. Obesity and cancer. Exp Clin Endocrinol Diabetes. 2009;117:563–6. doi: 10.1055/s-0029-1241870. [DOI] [PubMed] [Google Scholar]
- 35.Epel E, McEwen B, Seeman T, Matthews K, Castellazzo G, Brownell KD, et al. Stress and body shape: Stress-induced cortisol secretion is consistently greater among women with central fat. Psychosom Med. 2000;62:623–32. doi: 10.1097/00006842-200009000-00005. [DOI] [PubMed] [Google Scholar]
- 36.Weber-Hamann B, Hentschel F, Kniest A, Deuschle M, Colla M, Lederbogen F, et al. Hypercortisolemic depression is associated with increased intra-abdominal fat. Psychosom Med. 2002;64:274–7. doi: 10.1097/00006842-200203000-00010. [DOI] [PubMed] [Google Scholar]
- 37.Rebuffe-Scrive M, Walsh UA, McEwen B, Rodin J. Effect of chronic stress and exogenous glucocorticoids on regional fat distribution and metabolism. Physiol Behav. 1992;52:583–90. doi: 10.1016/0031-9384(92)90351-2. [DOI] [PubMed] [Google Scholar]
- 38.Jean-Louis G, Magai C, Consedine N, Zizi F, Casimir GJ, Solomon W, et al. Cancer worry and insomnia complaints among American women. Behav Sleep Med. 2009;7:63–72. doi: 10.1080/15402000902762303. [DOI] [PubMed] [Google Scholar]
- 39.Kendzor DE, Cofta-Woerpel LM, Mazas CA, Li Y, Vidrine JI, Reitzel LR, et al. Socioeconomic status, negative affect, and modifiable cancer risk factors in African-American smokers. Cancer Epidemiol Biomarkers Prev. 2008;17:2546–54. doi: 10.1158/1055-9965.EPI-08-0291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Niederdeppe J, Levy AG. Fatalistic beliefs about cancer prevention and three prevention behaviors. Cancer Epidemiol Biomarkers Prev. 2007;16:998–1003. doi: 10.1158/1055-9965.EPI-06-0608. [DOI] [PubMed] [Google Scholar]
- 41.Wilcox S, Ainsworth BE, LaMonte MJ, DuBose KD. Worry regarding major diseases among older African-American, Native-American, and Caucasian women. Women Health. 2002;36:83–99. doi: 10.1300/J013v36n03_06. [DOI] [PubMed] [Google Scholar]
- 42.Dantzer R, Kelley KW. Twenty years of research on cytokine- induced sickness behavior. Brain Behav Immunol. 2007;21:153–60. doi: 10.1016/j.bbi.2006.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Grunberg NE, Straub RO. The role of gender and taste class in the effects of stress on eating. Health Psychol. 1992;11:97–100. doi: 10.1037//0278-6133.11.2.97. [DOI] [PubMed] [Google Scholar]
- 44.Oliver G, Wardle J. Perceived effects of stress on food choice. Physiol Behav. 1999;66:511–5. doi: 10.1016/s0031-9384(98)00322-9. [DOI] [PubMed] [Google Scholar]
- 45.Wardle J, Steptoe A, Oliver G, Lipsey Z. Stress, dietary restraint and food intake. J Psychosom Res. 2000;48:195–202. doi: 10.1016/s0022-3999(00)00076-3. [DOI] [PubMed] [Google Scholar]
- 46.Grossniklaus DA, Gary RA, Higgins MK, Dunbar SB. Bio-behavioral and psychological differences between overweight adults with and without waist circumference risk. Res Nurs Health. 2010;33:539–51. doi: 10.1002/nur.20411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Matthews CE, Sui X, LaMonte MJ, Adams SA, Hebert JR, Blair SN. Metabolic syndrome and risk of death from cancers of the digestive system. Metabolism. 2010;59:1231–9. doi: 10.1016/j.metabol.2009.11.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Vogel M, Braungardt T, Meyer W, Schneider W. The effects of shift work on physical and mental health. J Neural Transm. 2012;119:1121–32. doi: 10.1007/s00702-012-0800-4. [DOI] [PubMed] [Google Scholar]
- 49.Karasek R. Encyclopedia of Occupational Health and Safety. 4. Geneva: International Labor Organization; 1995. Job stress theories: Status of the demand/control model. [Google Scholar]
- 50.Burch JB, Yost MG, Johnson W, Allen E. Melatonin, sleep, and shift work adaptation. J Occup Environ Med. 2005;47:893–901. doi: 10.1097/01.jom.0000177336.21147.9f. [DOI] [PubMed] [Google Scholar]
- 51.Jansson-Frojmark M, Lundqvist D, Lundqvist N, Linton SJ. Psychosocial work stressors for insomnia: A prospective study on 50–60-year-old adults in the working population. Int J Behav Med. 2007;14:222–8. doi: 10.1007/BF03002996. [DOI] [PubMed] [Google Scholar]
- 52.Akerstedt T. Psychosocial stress and impaired sleep. Scandinavian J Work Environ Health. 2006;32:493–501. [PubMed] [Google Scholar]
- 53.Simpson N, Dinges DF. Sleep and inflammation. Nutr Rev. 2007;65:S244–52. doi: 10.1111/j.1753-4887.2007.tb00371.x. [DOI] [PubMed] [Google Scholar]
- 54.Eismann EA, Lush E, Sephton SE. Circadian effects in cancer-relevant psychoneuroendocrine and immune pathways. Psychoneuroendocrinology. 2010;35:963–76. doi: 10.1016/j.psyneuen.2009.12.011. [DOI] [PubMed] [Google Scholar]
- 55.Qin Y, Zhou Y, Zhang X, Wei X, He J. Sleep duration and breast cancer risk: A meta-analysis of observational studies. Int J Cancer. 2014;134:1166–73. doi: 10.1002/ijc.28452. [DOI] [PubMed] [Google Scholar]
- 56.Thomas KS, Bardwell WA, Ancoli-Israel S, Dimsdale JE. The toll of ethnic discrimination on sleep architecture and fatigue. Health Psychol. 2006;25:635–42. doi: 10.1037/0278-6133.25.5.635. [DOI] [PubMed] [Google Scholar]
- 57.Eastman CI, Molina TA, Dziepak ME, Smith MR. Blacks (African Americans) have shorter free-running circadian periods than whites (Caucasian Americans) Chronobiol Int. 2012;29:1072–7. doi: 10.3109/07420528.2012.700670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Durrence HH, Lichstein KL. The sleep of African Americans: A comparative review. Behav Sleep Med. 2006;4:29–44. doi: 10.1207/s15402010bsm0401_3. [DOI] [PubMed] [Google Scholar]
- 59.McMenamin TM. A time to work: Recent trends in shift work and flexible schedules. Monthly Labor Review. 2007;130:3–15. [Google Scholar]
- 60.Jean-Louis G, Kripke DF, Elliott JA, Zizi F, Wolintz AH, Lazzaro DR. Daily illumination exposure and melatonin: Influence of ophthalmic dysfunction and sleep duration. J Circadian Rhythms. 2005;3:13. doi: 10.1186/1740-3391-3-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kripke DF, Jean-Louis G, Elliott JA, Klauber MR, Rex KM, Tuunainen A, et al. Ethnicity, sleep, mood, and illumination in postmenopausal women. BMC Psychiatr. 2004;4:8. doi: 10.1186/1471-244X-4-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Ruiter ME, Decoster J, Jacobs L, Lichstein KL. Normal sleep in African-Americans and Caucasian-Americans: A metaanalysis. Sleep Med. 2011;12:209–14. doi: 10.1016/j.sleep.2010.12.010. [DOI] [PubMed] [Google Scholar]
- 63.Armstead CA, Hebert JR, Griffin EK, Prince GM. A question of color: The influence of skin color and stress on resting blood pressure and body mass among African American women. J Black Psychol. 2014;40:121–450. doi: 10.1177/0095798413494404. [DOI] [Google Scholar]
- 64.Russell EF, Kramer MR, Cooper HL, Gabram-Mendola S, Senior-Crosby D, Jacob Arriola KR. Metropolitan area racial residential segregation, neighborhood racial composition, and breast cancer mortality. Cancer Causes Control. 2012;23:1519–27. doi: 10.1007/s10552-012-0029-4. [DOI] [PubMed] [Google Scholar]
- 65.Armstead CA, Lawler KA, Gorden G, Cross J, Gibbons J. Relationship of racial stressors to blood pressure responses and anger expression in black college students. Health Psychol. 1989;8:541–56. doi: 10.1037//0278-6133.8.5.541. [DOI] [PubMed] [Google Scholar]
- 66.Williams DR, Mohammed SA. Discrimination and racial disparities in health: Evidence and needed research. J Behav Med. 2009;32:20–47. doi: 10.1007/s10865-008-9185-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Williams DR, Neighbors HW, Jackson JS. Racial/ethnic discrimination and health: Findings from community studies. Am J Public Health. 2003;93:200–8. doi: 10.2105/ajph.93.2.200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.McEwen BS, Stellar E. Stress and the individual: Mechanisms leading to disease. Arch Intern Med. 1993;153:2093–101. [PubMed] [Google Scholar]
- 69.McEwen BS. Stressed or stressed out: What is the difference? J Psychiatr Neurosci. 2005;30:315–8. [PMC free article] [PubMed] [Google Scholar]
- 70.Geronimus AT. The weathering hypothesis and the health of African-American women and infants: Evidence and speculations. Ethn Dis. 1992;2:207–21. [PubMed] [Google Scholar]
- 71.Geronimus AT. Understanding and eliminating racial inequalities in women’s health in the United States: The role of the weathering conceptual framework. J Am Med Womens Assoc. 2001;56:133–6. [PubMed] [Google Scholar]
- 72.Stevens-Simon C. The weathering hypothesis. Am J Public Health. 2002;92:507–8. doi: 10.2105/ajph.92.4.507-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Braun KL, Nguyen TT, Tanjasiri SP, Campbell J, Heiney SP, Brandt HM, et al. Operationalization of community-based participatory research principles: Assessment of the National Cancer Institute’s Community Network Programs. Am J Public Health. 2012;102:1195–203. doi: 10.2105/AJPH.2011.300304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Littlefield DC. Rice and slaves: Ethnicity in the slave trade in Colonial South Carolina. Baton Rouge: Louisiana State University Press; 1981. [Google Scholar]
- 75.Solow BL, editor. Slavery and the rise of the Atlantic system. Boston: Harvard University Press; 1991. [Google Scholar]
- 76.Ehret C. The civilization of Africa: A history to 1800. Charlottesville: University Press of Virginia; 2002. [Google Scholar]
- 77.Coclanis PA, editor. The Atlantic economy during the seventeenth and eighteenth centuries. Columbia: University of South Carolina Press; 2005. [Google Scholar]
- 78.Fields-Black EL. Deep roots: Rice farmers in West Africa and the African Diaspora. Bloomington: Indiana University Press; 2008. [Google Scholar]
- 79.Clowse CD. Economic beginnings in colonial South Carolina 1670–1730. Columbia: University of South Carolina Press; 2005. [Google Scholar]
- 80.Edgar W. South Carolina: A history. Columbia: University of South Carolina Press; 1998. [Google Scholar]
- 81.Airhihenbuwa CO, Kumanyika SK, TenHave TR, Morssink CB. Cultural identity and health lifestyles among African Americans: A new direction for health intervention research? Ethn Dis. 2000;10:148–64. [PubMed] [Google Scholar]
- 82.Airhihenbuwa CO, Webster JD. Culture and African contexts of HIV/AIDS prevention, care and support. SAHARA J. 2004;1:4–13. doi: 10.1080/17290376.2004.9724822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Airhihenbuwa CO, Liburd L. Eliminating health disparities in the African American population: The interface of culture, gender, and power. Health Educ Behav. 2006;33:488–501. doi: 10.1177/1090198106287731. [DOI] [PubMed] [Google Scholar]
- 84.Cooper TP. Compilation of statutes of South Carolina, and decisions of court concerning the land office, granting and location of lands in this state, and duties of deputy surveyors. Columbia (SC): Steam Power Press of R.W. Gibbs & Co; 1854. South Carolina. [Google Scholar]
- 85.Buchholz K, Schachinger H, Wagner M, Schorr U, Sharma AM, Deter HC. Enhanced affective startle modulation in salt-sensitive subjects. Hypertension. 2001;38:1325–9. doi: 10.1161/hy1101.096055. [DOI] [PubMed] [Google Scholar]
- 86.Deter HC, Buchholz K, Schorr U, Mathiak K, Sharma AM. Salt-sensitivity and other predictors of stress-related cardiovascular reactivity in healthy young males. Clin Exp Hypertens. 2001;23:213–25. doi: 10.1081/ceh-100102661. [DOI] [PubMed] [Google Scholar]
- 87.Weber CS, Thayer JF, Rudat M, Sharma AM, Perschel FH, Buchholz K, et al. Salt-sensitive men show reduced heart rate variability, lower norepinephrine and enhanced cortisol during mental stress. J Human Hypertens. 2008;22:423–31. doi: 10.1038/jhh.2008.11. [DOI] [PubMed] [Google Scholar]
- 88.Kelley JO, Angel JL. Life stresses of slavery. Am J Phys Anthropol. 1987;74:199–211. doi: 10.1002/ajpa.1330740208. [DOI] [PubMed] [Google Scholar]
- 89.Green TL, Darity WA., Jr Under the skin: Using theories from biology and the social sciences to explore the mechanisms behind the black-white health gap. Am J Public Health. 2010;100(Suppl 1):S36–40. doi: 10.2105/AJPH.2009.171140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Mann K. Shifting paradigms in the study of the African diaspora and of Atlantic history and culture. Slavery Abol. 2001;22:3–21. doi: 10.1080/714005179. [DOI] [PubMed] [Google Scholar]
- 91.Griffith DM, Ellis KR, Allen JO. An intersectional approach to social determinants of stress for African American men: Men’s and women’s perspectives. Am J Mens Health. 2013;7:19S–30S. doi: 10.1177/1557988313480227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Jamieson JP, Koslov K, Nock MK, Mendes WB. Experiencing discrimination increases risk taking. Psychol Sci. 2013;24:131–9. doi: 10.1177/0956797612448194. [DOI] [PubMed] [Google Scholar]
- 93.Kaholokula JK, Grandinetti A, Keller S, Nacapoy AH, Kingi TK, Mau MK. Association between perceived racism and physiological stress indices in Native Hawaiians. J Behav Med. 2012;35:27–37. doi: 10.1007/s10865-011-9330-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Das A. How does race get “under the skin”? Inflammation, weathering, and metabolic problems in late life. Soc Sci Med. 2013;77:75–83. doi: 10.1016/j.socscimed.2012.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Hicken MT, Lee H, Ailshire J, Burgard SA, Williams DR. “Every shut eye, ain’t sleep”: The role of racism-related vigilance in racial/ethnic disparities in sleep difficulty. Race and Social Problems. 2013;5:100–12. doi: 10.1007/s12552-013-9095-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Hebert JR, Wirth M, Davis L, Davis B, Harmon BE, Hurley TG, et al. Decreasing C-Reactive Protein in African Americans: Results of a diet and lifestyle randomized community trial. Am J Prev Med. 2013;45:430–40. doi: 10.1016/j.amepre.2013.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Cavicchia PP, Adams SA, Steck SE, Hussey JR, Liu J, Daguise VG, et al. Racial disparities in colorectal cancer incidence by type 2 diabetes mellitus status. Cancer Causes Control. 2012;24:277–85. doi: 10.1007/s10552-012-0095-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Combs-Orme T. Epigenetics and the social work imperative. Social Work. 2013;58:23–30. doi: 10.1093/sw/sws052. [DOI] [PubMed] [Google Scholar]
- 99.Wong CF, Schrager SM, Holloway IW, Meyer IH, Kipke MD. Minority stress experiences and psychological well-being: The impact of support from and connection to social networks within the Los Angeles house and ball communities. Prev Sci. 2014;15:44–55. doi: 10.1007/s11121-012-0348-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Salas A, Richards M, Lareu MV, Scozzari R, Coppa A, Torroni A, et al. The African diaspora: Mitochondrial DNA and the Atlantic slave trade. Am J Human Genet. 2004;74:454–65. doi: 10.1086/382194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Harmon BE, Blake CE, Armstead CA, Hebert JR. Intersection of identities: Food, role, and the African-American pastor. Appetite. 2013;67C:44–52. doi: 10.1016/j.appet.2013.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Harmon BE, Blake CE, Thrasher JF, Hebert JR. An evaluation of diet and physical activity messaging in African-American Churches. Health Educ Behav. 2013;41:216–24. doi: 10.1177/1090198113507449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.McNeilly M, Anderson NB, Robinson E, McManus C, Armstead C, Clark R, Pieper C, et al. The convergent, discriminant, and concurrent criterion validity of the perceived racism scale: A multidimensional assessment of White racism among African Americans. In: Jones J, editor. Handbook tests and measurements for black populations. Hampton (VA): Cobb and Henry Publishers; 1996. pp. 359–74. [Google Scholar]
- 104.McNeilly MD, Anderson NB, Armstead CA, Clark R, Corbett M, Robinson EL, et al. The perceived racism scale: A multidimensional assessment of the experience of white racism among African Americans. Ethn Dis. 1996;6:154–66. [PubMed] [Google Scholar]
- 105.Clark R, Armstead C. Preliminary study examining relationship between family environment and resting mean arterial pressure in African-American youth. J Adolesc Health. 2000;27:3–5. doi: 10.1016/s1054-139x(99)00127-5. [DOI] [PubMed] [Google Scholar]
- 106.Clark R, Armstead C. Family conflict predicts blood pressure changes in African-American adolescents: A preliminary examination. J Adolesc. 2000;23:355–8. doi: 10.1006/jado.2000.0320. [DOI] [PubMed] [Google Scholar]
- 107.Black unemployment rate spiked to 13.5 percent in May: The national unemployment rate rose to 7.6 percent. BET News. [updated 2013; cited 2013 Jun 24]. Available from: www.bet.com/news/national/2013/06/07/may-black-unemploymentrate.html.
- 108.Cleek EN, Wofsy M, Boyd-Franklin N, Mundy B, Howell TJ. The family empowerment program: An interdisciplinary approach to working with multi-stressed urban families. Family Proc. 2012;51:207–17. doi: 10.1111/j.1545-5300.2012.01392.x. [DOI] [PubMed] [Google Scholar]
- 109.Hardaway CR, McLoyd VC. Escaping poverty and securing middle class status: How race and socioeconomic status shape mobility prospects for African Americans during the transition to adulthood. J Youth Adolesc. 2009;38:242–56. doi: 10.1007/s10964-008-9354-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Adams SA, Butler WM, Fulton J, Heiney SP, Williams EM, Delage AF, et al. Racial disparities in breast cancer mortality in a multiethnic cohort in the Southeast. Cancer. 2012;118:2693–9. doi: 10.1002/cncr.26570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.South Carolina Office of Research and Statistics. South Carolina Rural Health Report. Columbia: South Carolina Budget and Control Board; 2005. [Google Scholar]
- 112.Wilcox S, Sharpe PA, Parra-Medina D, Granner M, Hutto B. A randomized trial of a diet and exercise intervention for overweight and obese women from economically disadvantaged neighborhoods: Sisters Taking Action for Real Success (STARS) Contemp Clin Trials. 2011;32:931–45. doi: 10.1016/j.cct.2011.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Roberts JR, Kennedy SA, Darden PM, Basco WT., Jr Prevalence of obesity in children: Comparing children from the South Carolina pediatric practice research network with a national sample. Clin Pediatr. 2010;49:750–5. doi: 10.1177/0009922810364655. [DOI] [PubMed] [Google Scholar]
- 114.Martin SL, Kirkner GJ, Mayo K, Matthews CE, Durstine JL, Hebert JR. Urban, rural, and regional variations in physical activity. J Rural Health. 2005;21:239–44. doi: 10.1111/j.1748-0361.2005.tb00089.x. [DOI] [PubMed] [Google Scholar]
- 115.Roundtree S, Malvern L, Heidari K, Dean A, Hil T, Kirby E. Management of obesity and overweight: Statewide survey of attitudes, barriers, skills, and educational needs among South Carolina health care professionals. J SC Med Assoc. 2009;105:55–8. [PubMed] [Google Scholar]
- 116.Jia H, Lubetkin EI. The statewide burden of obesity, smoking, low income and chronic diseases in the United States. J Public Health. 2009;31:496–505. doi: 10.1093/pubmed/fdp012. [DOI] [PubMed] [Google Scholar]
- 117.He J, Stram DO, Kolonel LN, Henderson BE, Le Marchand L, Haiman CA. The association of diabetes with colorectal cancer risk: The Multiethnic Cohort. Br J Cancer. 2010;103:120–6. doi: 10.1038/sj.bjc.6605721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Flood A, Strayer L, Schairer C, Schatzkin A. Diabetes and risk of incident colorectal cancer in a prospective cohort of women. Cancer Causes Control. 2010;21:1277–84. doi: 10.1007/s10552-010-9555-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Hernandez JA. Mexican American colonization during the nineteenth century: A history of the US-Mexico borderlands. Cambridge (MA): Cambridge University Press; 2012. [Google Scholar]
- 120.Rothenberg D. With these hands: The hidden world of migrant farmworkers today. Oakland: University of California Press; 2000. [Google Scholar]
- 121.Knouse SB, Rosenfeld PE, Culbertson AL. Hispanics in the workplace. Thousand Oaks (CA): Sage; 1992. [Google Scholar]
- 122.Morales R, Bonilla F. Latinos in a changing US economy: Comparative perspectives on growing inequality. Thousand Oaks (CA): Sage; 1993. [Google Scholar]
- 123.Cook B, Alegria M, Lin JY, Guo J. Pathways and correlates connecting Latinos’ mental health with exposure to the United States. Am J Public Health. 2009;99:2247–54. doi: 10.2105/AJPH.2008.137091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Finch BK, Hummer RA, Kol B, Vega WA. The role of discrimination and acculturative stress in the physical health of Mexican-Origin adults. Hisp J Behav Sci. 2001;23:399–429. [Google Scholar]
- 125.Finch BK, Kolody B, Vega WA. Perceived discrimination and depression among Mexican-origin adults in California. J Health Soc Behav. 2000;41:295–313. [PubMed] [Google Scholar]
- 126.Lee M-A, Ferraro KF. Perceived discrimination and health among Puerto Rican and Mexican Americans: Buffering effect of the Lazo matrimonial? Soc Sci Med. 2009;68:1966–74. doi: 10.1016/j.socscimed.2009.02.052. [DOI] [PubMed] [Google Scholar]
- 127.Perez DJ, Fortuna L, Alegria M. Prevalence and correlates of everyday discrimination among U.S. Latinos. J Community Psychol. 2008;36:421–33. doi: 10.1002/jcop.20221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Ryan AM, Gee GC, Laflamme DF. The association between self-reported discrimination, physical health and blood pressure: Findings from African Americans, Black immigrants, and Latino immigrants in New Hampshire. J Health Care Poor Underserv. 2006;17:116–32. doi: 10.1353/hpu.2006.0092. [DOI] [PubMed] [Google Scholar]
- 129.Pew Research Center. Hispanics and Health Care in the United States. [updated 2008; cited 2013 Jul 5.] Available from: http://www.pewhispanic.org/2008/08/13/hispanics-and-health-care-in-the-united-states-access-information-and-knowledge.
- 130.Hispanics and stress: Mind/body health. [updated 2006; cited 2013 Jul 5]. Available from: http://www.apa.org/news/press/releases/2006/10/hispanic-stress-tips.pdf.
- 131.Cancer facts and figures for Hispanics/Latinos 2012 – 2014. [updated 2012; cited 2013 Jul 5]. Available from: http://www.cancer.org/acs/groups/content/@epidemiologysurveilance/documents/document/acspc-034778.pdf.
- 132.Bureau of Labor Statistics. Labor Force Statistics from the Current Population Survey. [updated 2012; cited 2013 Jul 5]. Available from: www.bls.gov/cps/cpsaat11.htm.
- 133.Coronado GD, Thompson B, Tejeda S, Godina R, Chen L. Sociodemographic factors and self-management practices related to type 2 diabetes among Hispanics and non-Hispanic whites in a rural setting. J Rural Health. 2007;23:49–54. doi: 10.1111/j.1748-0361.2006.00067.x. [DOI] [PubMed] [Google Scholar]
- 134.Silva N. Aloha betrayed: Native Hawaiian resistance to American colonialism. Durham (NC): Duke University Press; 2004. [Google Scholar]
- 135.Crabbe K. Conceptions of depression: A Hawaiian perspective. Pacific Health Dialog. 1999;6:122–6. [Google Scholar]
- 136.Kaholokula J. Colonialism acculturation and depression among Kānaka Maoli of Hawai’i. In: Culbertson P, Agee M, Makasiale K, editors. Penina uliuli: Confronting challenges in mental health for Pacific peoples. Honolulu: University of Hawai’i Pres; 2007. [Google Scholar]
- 137.Kaholokula JK, Nacapoy AH, Dang KL. Social justice as a public health imperative for Kānaka Maoli. AlterNative: An International Journal of Indigenous Peoples. 2009;5:117–37. [Google Scholar]
- 138.McCubbin LD, Marsella A. Native Hawaiians and psychology: The cultural and historical context of indigenous ways of knowing. Cultur Divers Ethnic Minor Psychol. 2009;15:374–87. doi: 10.1037/a0016774. [DOI] [PubMed] [Google Scholar]
- 139.Rezentes W. Ka lama kukui: Hawaiian psychology: An introduction. Honolulu: ‘A’ali’i Books; 1996. [Google Scholar]
- 140.Balabis J, Pobutsky A, Kromer-Baker K, Tottori C, Salvail F. The burden of cardiovascular disease in Hawaii 2007. Honolulu: Hawaii State Department of Health; 2007. [Google Scholar]
- 141.Native Hawaiian Data Book 2007. Honolulu: Office of Hawaiian Affairs; 2006. [Google Scholar]
- 142.Park CB, Braun KL, Horiuchi BY, Tottori C, Onaka AT. Longevity disparities in multiethnic Hawaii: An analysis of 2000 life tables. Public Health Rep. 2009;124:579–84. doi: 10.1177/003335490912400415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Kaholokula JK, Nacapoy AH, Grandinetti A, Chang HK. Association between acculturation modes and type 2 diabetes among Native Hawaiians. Diabetes Care. 2008;31:698–700. doi: 10.2337/dc07-1560. [DOI] [PubMed] [Google Scholar]
- 144.Kaholokula JK, Iwane MK, Nacapoy AH. Effects of perceived racism and acculturation on hypertension in Native Hawaiians. Hawaii Med J. 2010;69:11–5. [PMC free article] [PubMed] [Google Scholar]
- 145.Seedat S, Stein MB, Kennedy CM, Hauger RL. Plasma cortisol and neuropeptide Y in female victims of intimate partner violence. Psychoneuroendocrinology. 2003;28:796–808. doi: 10.1016/s0306-4530(02)00086-0. [DOI] [PubMed] [Google Scholar]
- 146.Miller GE, Cohen S, Ritchey AK. Chronic psychological stress and the regulation of pro-inflammatory cytokines: A glucocorticoid- resistance model. Health Psychol. 2002;21:531–41. doi: 10.1037//0278-6133.21.6.531. [DOI] [PubMed] [Google Scholar]
- 147.Yehuda R, Bierer LM, Schmeidler J, Aferiat DH, Breslau I, Dolan S. Low cortisol and risk for PTSD in adult offspring of holocaust survivors. Am J Psychiatr. 2000;157:1252–9. doi: 10.1176/appi.ajp.157.8.1252. [DOI] [PubMed] [Google Scholar]
- 148.Bjorntorp P, Holm G, Rosmond R. Hypothalamic arousal, insulin resistance and type 2 diabetes mellitus. Diabet Med. 1999;16:373–83. doi: 10.1046/j.1464-5491.1999.00067.x. [DOI] [PubMed] [Google Scholar]
- 149.Cohen S, Schwartz JE, Epel E, Kirschbaum C, Sidney S, Seeman T. Socioeconomic status, race, and diurnal cortisol decline in the Coronary Artery Risk Development in Young Adults (CARDIA) Study. Psychosom Med. 2006;68:41–50. doi: 10.1097/01.psy.0000195967.51768.ea. [DOI] [PubMed] [Google Scholar]
- 150.Gravlee CC. How race becomes biology: Embodiment of social inequality. Am J Phys Anthropol. 2009;139:47–57. doi: 10.1002/ajpa.20983. [DOI] [PubMed] [Google Scholar]
- 151.Marmot M, Friel S. Global health equity: Evidence for action on the social determinants of health. J Epidemiol Community Health. 2008;62:1095–7. doi: 10.1136/jech.2008.081695. [DOI] [PubMed] [Google Scholar]
- 152.Israel BA, Schulz AJ, Parker EA, Becker AB. Review of community- based research: Assessing partnership approaches to improve public health. Ann Rev Public Health. 1998;19:173–202. doi: 10.1146/annurev.publhealth.19.1.173. [DOI] [PubMed] [Google Scholar]
- 153.Hebert JR, Brandt HM, Armstead CA, Adams SA, Steck SE. Interdisciplinary, translational, and community-based participatory research: Finding a common language to improve cancer research. Cancer Epidemiol Biomark Prev. 2009;18:1213–7. doi: 10.1158/1055-9965.EPI-08-1166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Schwartz S, Carpenter KM. The right answer for the wrong question: Consequences of type III error for public health research. Am J Public Health. 1999;89:1175–80. doi: 10.2105/ajph.89.8.1175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Orr E, Westman M. Does hardiness moderate stress and how? A review. In: Rosenbaum M, editor. Learned resourcefulness. New York: Springer; 1990. pp. 64–94. [Google Scholar]
- 156.Archibald PC, Dobson Sydnor K, Daniels K, Bronner Y. Explaining African-Americans’ depressive symptoms: A stres-sdistress and coping perspective. J Health Psychol. 2013;18:321–31. doi: 10.1177/1359105312440297. [DOI] [PubMed] [Google Scholar]
- 157.Walters KL, Simoni JM. Reconceptualizing native women’s health: An “indigenist” stress-coping model. Am J Public Health. 2002;92:520–4. doi: 10.2105/ajph.92.4.520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Friel S, Marmot M, McMichael AJ, Kjellstrom T, Vagero D. Global health equity and climate stabilisation: A common agenda. Lancet. 2008;372:1677–83. doi: 10.1016/S0140-6736(08)61692-X. [DOI] [PubMed] [Google Scholar]
- 159.Franke RW, Chasin BH. Kerala State, India: Radical reform as development. Int J Health Serv. 1992;22:139–56. doi: 10.2190/HMXD-PNQF-2X2L-C8TR. [DOI] [PubMed] [Google Scholar]
- 160.Geiger HJ. Community-oriented primary care: a path to community development. Am J Public Health. 2002;92:1713–6. doi: 10.2105/ajph.92.11.1713. [DOI] [PMC free article] [PubMed] [Google Scholar]